Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Osteo Infographic Final
Caricato da
1234choco0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
6 visualizzazioni1 paginaOsteo Infographic Final
Copyright
© © All Rights Reserved
Formati disponibili
PDF o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoOsteo Infographic Final
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
6 visualizzazioni1 paginaOsteo Infographic Final
Caricato da
1234chocoOsteo Infographic Final
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF o leggi online su Scribd
Sei sulla pagina 1di 1
A GP's guide to osteoporosis
TF Te lites Ste-Ti eM Ceo Calg
* 4.74 million Australians
* >1 million have osteoporosis’
>, © By 2022, 6.2 million Australians >50 years will have
osteoporosis or osteopenia —
resulting in nearly 200,000 fractures in that year alone’
5
CrP Devastating consequences
=
* Minimal trauma fractures oeee
affect one in four men 7 7 qT T ae
and one in two women
older than 60?
* Awoman older than 60 has a 44% risk of
having a minimal trauma fracture in her lifetime’
* Even minor minimal trauma fractures increase
morbidity a and mortality ii
* One minimal trauma fracture:
2-4 fold risk of fracture at a different site’
Many people with a minimal trauma fracture are treated only for
the fracture — not the underlying cause”
Despite the increased availability of effective drugs,
fewer than 20% of Australians with minimal trauma fractures
are investigated or treated for osteoporosis”
How GPs can help
* Assess patients older than 50 for risk of osteoporosis and fracture
* Address the problem of under-treatment
* Use the T-score to assess bone mineral density (BMD)’
— T-score: the number of standard deviations of the BMD measurement above
or below that of young healthy adults of the same sex’
— The PBS uses the WHO T-score range to determine eligibility for osteoporosis
medications'
BMD not more
Normal BMD Tscore -1.0 or above. |) trans Osean
young adult
7a BMD between 1.0
Osteopenia C0 e eal and 2.5 SDs bel:
-1.0 and -2.5 young adult
Osteoporosis
- low BMD
— micro-architectural
deterioration of
bone tissue
BMD 2.5 or more
T-score -2.5 or below | SDs below you
adult mean
v,V
X Vhy are GPs not diagnosing those at risk x
* BMD is only one of several factors that contribute to an
individual's risk of fracture’
* About 50% of minimal trauma fractures occur in people {
with “normal” or “osteopenic” T-scores'
* About 30% of radiographically visible vertebral fractures in
women with osteoporosis are not detected’
Making a diagnosis :
Diagnostic assessment:
* Medical history’
* Clinical examination’
* BMD measurement by dual energy X-ray absorption (DXA)'
If applicable:
* Laboratory tests and radiographs of the thoracic and
lumbar spine!
The MBS reimburses BMD testing for:
eo
f=.
* Anyone older than 70 years? * Patients with a minimal trauma fracture®
* Patients older than 50 with no minimal trauma fracture but with major risk factors’?
eR Orn Rea DCC itite tek eueca
PT Utd DY ented
Rheumatoid arthritis Glucocorticoid use for at least three months
Thyroid disease Anti-androgen therapy
Chronic liver or kidney disease
Coeliac disease/malabsorption disorders
Premature menopause
TN etereroue tele
* See RACGP Guidelines.’
z oe
:
z
; t I
= J
z
2 bt
Height loss of 3cm or more’ _Thoracic kyphosis New-onset back pain
(hunchback)* suggestive of fracture’
¥ MBS changes x
As of November 2017:
* DXA scans must be performed by a specialist or a person with a
radiation licence and overseen by a specialist or consultant physician?
* New intervals for people over 70 years:
T-score 2 -1.5: one scan every 5 years
T-score of -1.5 to -2.5: one scan every 2 years
Osteoporosis treatment is recommended for patients with a high absolute fracture risk
* Post-menopausal women and men older than 60 with T scores < —2.5 at: a
the lumbar spine ‘
femoral neck
» CT aa
a
FIRST-LINE
Bisphosphonates Denosumab Raloxifene
Daily, weekly or monthly Monoclonal antibody Aselective oestrogen-
tablets (alendronate, receptor modulator
risedronate)
v
Annual infusion 6-monthly subcutaneous Daily tablet
(zoledronic acid) injection
PBS subsidy for: PBS subsidy for: PBS subsidy for:
minimal trauma fracture minimal trauma fracture postmenopausal women
a a with previous minimal
F F t fracti
> 70 years with > 70 years with aaneeceaae
T-score < -2.5 (< -3.0 for T-score < -2.5 on
zoledronic acid) my
o . v
or Ze
T-score < -1.5 taking bere
long-term oral
corticosteroids 5
Teriparatide
Recombinant parathyroid hormone.
PBS subsidy for:
T-score < -3.0 and very high fracture risk
and
22 minimal trauma fractures
and
new fracture after 12 months on another osteoporosis medicine
and
treatment must be initiated by a specialist or consultant physician =)
References: 1. RACGP & Osteoporosis Australia. Osteoporosis prevention, diagnosis and management in postmenopausal women and men
‘over 50 years of age. 2nd edition 2017. Available from:
hitps://wmw.osteopoross.org,au/sites/default/iles/iles/20439%200steoporosis%20guidelines pal Accessed 20/3/18. 2. Milat F and Ebeling
PR. Med J Aust 2016; 205 (4): 185-90. 3. Australian Government Department of Health. Bone Densitometry. Available online:
worw.health.gov.au/internet/main/publishing.nst/content/diagnosticimaging-bd.htm Accessed 20/3/18. 4. Osteoporosis Australia Medical and
Scientific Advisory Committee. Therapeutic Management 2017. Available from: https://www.osteoporosis.org.aultherapeutic-management
5. NPS MedicineWise. Decision pathway for PBS:lsted treatment selection: management of conficmed osteoporosis 2016. Available from:
hitps://wwwenps.org.2u/_servito/decsion-pathway-for-pbs-listed.treatment-selection-managoment-of-confizmed-osteopoross-7ed5e5af0817eb
This content is produced by Australian Doctor Group, with an independent educational grant from Amgen.
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Blue Veins Sub Theme TVBDocumento4 pagineBlue Veins Sub Theme TVB1234chocoNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- QLD Rail Traim PDFDocumento1 paginaQLD Rail Traim PDF1234chocoNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Blue BirdDocumento7 pagineBlue Bird1234chocoNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Fairy Tail - Main ThemeDocumento3 pagineFairy Tail - Main Theme1234chocoNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Pokemon Theme Song 22Documento4 paginePokemon Theme Song 221234chocoNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Code Geass - StoriesDocumento5 pagineCode Geass - Stories1234chocoNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Mbs Quick Guide: JULY 2020Documento2 pagineMbs Quick Guide: JULY 20201234chocoNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Doctor Talk: Communication Practice Role PlaysDocumento6 pagineDoctor Talk: Communication Practice Role Plays1234chocoNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
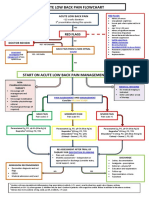
- Acute Low Back Pain Flowchart January 2017Documento1 paginaAcute Low Back Pain Flowchart January 20171234chocoNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- VTE GuidelinesDocumento11 pagineVTE Guidelines1234chocoNessuna valutazione finora
- Topical Steroids (Sep 19) PDFDocumento7 pagineTopical Steroids (Sep 19) PDF1234chocoNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Applying For Jobs Ebook Ed 1Documento41 pagineApplying For Jobs Ebook Ed 11234chocoNessuna valutazione finora
- Topical Steroids (Sep 19) PDFDocumento7 pagineTopical Steroids (Sep 19) PDF1234chocoNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- USMLE Flashcards: Anatomy - Side by SideDocumento190 pagineUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Taking A Social and Cultural HistoryDocumento3 pagineTaking A Social and Cultural History1234chocoNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDocumento7 pagine# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoNessuna valutazione finora
- Metro South Intern Training Form (Logan)Documento3 pagineMetro South Intern Training Form (Logan)1234chocoNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- 2016 Applicant Guide Web V2Documento83 pagine2016 Applicant Guide Web V21234chocoNessuna valutazione finora
- Herd Immunity'' A Rough Guide PDFDocumento6 pagineHerd Immunity'' A Rough Guide PDF1234chocoNessuna valutazione finora
- Fluids ElectrolytesDocumento2 pagineFluids Electrolytes1234chocoNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDocumento1 paginaFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDocumento5 pagineManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoNessuna valutazione finora
- PBM Module1 MTP Template 0Documento2 paginePBM Module1 MTP Template 01234chocoNessuna valutazione finora
- Language of PreventionDocumento9 pagineLanguage of Prevention1234chocoNessuna valutazione finora
- Defining and Assessing Risks To Health PDFDocumento20 pagineDefining and Assessing Risks To Health PDF1234chocoNessuna valutazione finora
- Clinical Contributions To Addressing The Social Determinants of HealthDocumento5 pagineClinical Contributions To Addressing The Social Determinants of Health1234chocoNessuna valutazione finora
- ImprovingMedAdherenceOlderAdultslyer Final 508CDocumento2 pagineImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Effects of Social Networks On Disability in Older AustraliansDocumento22 pagineThe Effects of Social Networks On Disability in Older Australians1234chocoNessuna valutazione finora
- A Conceptual Framework For HealthDocumento1 paginaA Conceptual Framework For Health1234chocoNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)