Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Thedacare: Community Paramedicine Pilot Health Assessment: October 2017
Caricato da
Risely SutarsaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Thedacare: Community Paramedicine Pilot Health Assessment: October 2017
Caricato da
Risely SutarsaCopyright:
Formati disponibili
OCTOBER 2017
ThedaCare:
Community Paramedicine Pilot Health Assessment
1. Spiritual/cultural
Yes No
2. Health maintenance providers
Primary care provider Specialty care provider Community paramedic
At-home service Complex care team Social worker
Other
3. Patient barriers
No barriers Financial Caregiver
Transportation Cognitive disability Language
Vision Emotional Cultural
Disease state Family Pain
Other
4. Patient exercises. If yes, frequency: duration:
Yes No
5. Current diet
As tolerated General Low fat
Low cholesterol No caffeine No added sodium
No restrictions Special formula/diet TPN
Diabetic diet Other
6. Patient’s perceived health
Good health Is alert In no apparent distress
In mild distress In moderate distress In severe distress
Is appropriately interactive Other
7. Caregiver’s perceived health
Good health Is alert In no apparent distress
In mild distress In moderate distress In severe distress
Is appropriately interactive Other
8. Medications effective
Yes No
9. Medication concerns
ABOUT THIS SOCIAL DETERMINANTS OF HEALTH ASSESSMENT TOOL
This resource is a companion to the Center for Health Care Strategies’ brief, Screening for Social Determinants of
Health in Populations with Complex Needs: Implementation Considerations. The brief examines how organizations
participating in Transforming Complex Care (TCC), a multi-site national initiative funded by the Robert Wood
Johnson Foundation, are assessing and addressing social determinants of health for populations with complex
needs. To download the brief and view additional assessment tools, visit www.chcs.org/sdoh-screening/.
Advancing innovations in health care delivery for low-income Americans | www.chcs.org
ThedaCare: Community Paramedicine Pilot Health Assessment
10. Patient’s ambulation
Ambulatory Wheelchair Cart
Cane Walker Other
11. Fear of falling
Yes No
12. Frequency of falls
Never Rarely Infrequently Occasionally Daily Other
13. Tripping hazards in home
Yes No
14. Tripping hazards present
Throw rugs Cords/cables Clutter Thresholds Other
15. Focus of today’s visit
Medication Wound education Pneumonia education
Sepsis education Diabetic education CHF/weight/BP education
Blood sugar logs Diabetic foot logs Wound care
Social services Other
16. Education and resources given to patient
Wound Pneumonia Sepsis
Diabetes CHF/Weight/BP ADRC
LEAVEN Food pantry Other
17. New barriers identified
No barriers Financial Caregiver
Transportation Cognitive disability Language
Vision Emotional Cultural
Disease state Family Pain
Other
18. Life hazards
No employment No home No community
No transportation Inhalants (employment) Noise (employment)
Fire concerns (home) Air pollution (home) Clutter (home)
Noise (community) Clean water (community) Air pollution (community)
Seatbelt use (transportation) Vision (transportation) Vehicle (transportation)
Other
19. Transportation screening completed
Yes No
Advancing innovations in health care delivery for low-income Americans | www.chcs.org 2
Potrebbero piacerti anche
- End of Life Care For Nurses DMH FinalDocumento39 pagineEnd of Life Care For Nurses DMH FinalpradeepNessuna valutazione finora
- Contingency PlansDocumento8 pagineContingency PlansNoel GalangNessuna valutazione finora
- 10Documento19 pagine10Bruno100% (3)
- ALZI - Dementia in IndonesiaDocumento23 pagineALZI - Dementia in IndonesiaRehabilitasi Medik RSUD Sosodoro DjatikoesoemoNessuna valutazione finora
- Mental Health in The Workplace: A Call To ActionDocumento27 pagineMental Health in The Workplace: A Call To ActionNational Press FoundationNessuna valutazione finora
- BRC Issue 8 Whitepaper WebDocumento12 pagineBRC Issue 8 Whitepaper WebGaganpreet KaurNessuna valutazione finora
- MEDSURGDocumento39 pagineMEDSURGShane SappayaniNessuna valutazione finora
- Facilities ManagementDocumento21 pagineFacilities ManagementEduardo Viana100% (1)
- 01 Public Health NursingDocumento20 pagine01 Public Health NursingKailash NagarNessuna valutazione finora
- The Costs of Eating Disorders Final OriginalDocumento76 pagineThe Costs of Eating Disorders Final Originalmadequal2658Nessuna valutazione finora
- User Manual FotonaDocumento103 pagineUser Manual Fotonarasheeque100% (4)
- Basic Nutrition: Lesson 2Documento13 pagineBasic Nutrition: Lesson 2Shaina DaquilNessuna valutazione finora
- Medsurg Reviewer1Documento27 pagineMedsurg Reviewer1Angelie BigayNessuna valutazione finora
- Centre For Community Medicine, All India Institute of Medical Sciences, New Delhi, INDIADocumento25 pagineCentre For Community Medicine, All India Institute of Medical Sciences, New Delhi, INDIAKayle PinlacNessuna valutazione finora
- WWK 7 PewDocumento27 pagineWWK 7 Pewapi-235454491Nessuna valutazione finora
- Clinical Aspects of Palliative CareDocumento71 pagineClinical Aspects of Palliative CarePhaimNessuna valutazione finora
- Concept and PSS - ILCCDocumento34 pagineConcept and PSS - ILCCMichaelNessuna valutazione finora
- Community Health Nursing Lecture 107-Pages-Pg.-116-222Documento107 pagineCommunity Health Nursing Lecture 107-Pages-Pg.-116-222ShiraishiNessuna valutazione finora
- Brief Overview of Palliative CareDocumento42 pagineBrief Overview of Palliative CarepradeepNessuna valutazione finora
- Day 4 - Common Session 1 - Ped PC - DR Maryann MuckadenDocumento82 pagineDay 4 - Common Session 1 - Ped PC - DR Maryann Muckadenm debNessuna valutazione finora
- Final Nursing Care PlanDocumento12 pagineFinal Nursing Care PlanBerina SelimovicNessuna valutazione finora
- Community Health NursingDocumento5 pagineCommunity Health NursingLucile LlevaNessuna valutazione finora
- Outline To A Geriatric Medicine Inpatient ConsultationDocumento5 pagineOutline To A Geriatric Medicine Inpatient ConsultationEllieNessuna valutazione finora
- Pediatric Palliative Care: Comprehensive Support For ChildrenDocumento6 paginePediatric Palliative Care: Comprehensive Support For ChildrenDra. Wendy Cristhyna Gómez GarcíaNessuna valutazione finora
- Community Health Nursing NotesDocumento8 pagineCommunity Health Nursing NotesSachi Reuel BernateNessuna valutazione finora
- Hidden Pain - 2021,12,08Documento80 pagineHidden Pain - 2021,12,08RubenNessuna valutazione finora
- Part 1 - Care For Palliative and Bedridden Patients in Communities On ECQ (Updated)Documento22 paginePart 1 - Care For Palliative and Bedridden Patients in Communities On ECQ (Updated)Louije MombzNessuna valutazione finora
- Asha NCD Module - 270117Documento72 pagineAsha NCD Module - 270117akshay dhootNessuna valutazione finora
- Jambore-Pkb (Lazuardi Dwipa, DR - SPPD, K-Ger)Documento65 pagineJambore-Pkb (Lazuardi Dwipa, DR - SPPD, K-Ger)UPT PKM UJUNGBERUNG INDAHNessuna valutazione finora
- Abstract Favouring For The Given Articles 1 1234Documento7 pagineAbstract Favouring For The Given Articles 1 1234ashverya agrawalNessuna valutazione finora
- PPC FCMLDocumento59 paginePPC FCMLAs Minhas OrigensNessuna valutazione finora
- Mental Health: Dr. S. M. Raysul Haque School of Public Health, IubDocumento22 pagineMental Health: Dr. S. M. Raysul Haque School of Public Health, IubMashfique AhmedNessuna valutazione finora
- Social Determinants of Health and Well-Being Among Young PeopleDocumento28 pagineSocial Determinants of Health and Well-Being Among Young Peoplealex kNessuna valutazione finora
- My Care My RightDocumento42 pagineMy Care My RightpradeepNessuna valutazione finora
- 1.-Humanity in Action - Rapid - Assessment - TemplateDocumento4 pagine1.-Humanity in Action - Rapid - Assessment - TemplateXamse Cabdi AarNessuna valutazione finora
- CMHNDocumento48 pagineCMHNvikaNessuna valutazione finora
- E PortfolioDocumento12 pagineE PortfolioMohammed AlomarNessuna valutazione finora
- Expanding The Narrative About What Creates Health One News Story at A TimeDocumento40 pagineExpanding The Narrative About What Creates Health One News Story at A TimeNational Press FoundationNessuna valutazione finora
- School District Health Assessment FormDocumento2 pagineSchool District Health Assessment FormAnuvratha NarayananNessuna valutazione finora
- 3 Revised Presentation of Sec. Ubial 6 13 2017Documento24 pagine3 Revised Presentation of Sec. Ubial 6 13 2017Kristel Joy Verzon-BunaganNessuna valutazione finora
- COVID19 Rapid Assessment Tool KAP IFRC UNICEF WHO 0503Documento4 pagineCOVID19 Rapid Assessment Tool KAP IFRC UNICEF WHO 0503dear sinandangNessuna valutazione finora
- Cultural Perspective Mental HealthDocumento7 pagineCultural Perspective Mental HealthkgjtertijNessuna valutazione finora
- 1 CombineDocumento52 pagine1 Combineasal bakhtyariNessuna valutazione finora
- Saint Francis of Assisi College College of NursingDocumento4 pagineSaint Francis of Assisi College College of NursingCarolyn CalupitanNessuna valutazione finora
- Meet Family Medicine: Information, Facts, and Answers To Frequently Asked Questions Altynai AkparalievnaDocumento45 pagineMeet Family Medicine: Information, Facts, and Answers To Frequently Asked Questions Altynai AkparalievnaAltynayNessuna valutazione finora
- Ethics-Morality-Law Jigsaws 1. Law: Emergency Decree On Public Admin. in Emergency SituationsDocumento2 pagineEthics-Morality-Law Jigsaws 1. Law: Emergency Decree On Public Admin. in Emergency SituationsKirana Aulia PutriNessuna valutazione finora
- Nstp1 Hiv AidsDocumento38 pagineNstp1 Hiv AidsLyza DayegoNessuna valutazione finora
- The Child's Right To Palliative Care - The Next Horizon For Pediatrics - PPT DownloadDocumento15 pagineThe Child's Right To Palliative Care - The Next Horizon For Pediatrics - PPT DownloadDania AlansariNessuna valutazione finora
- Adolescent Health EditedDocumento27 pagineAdolescent Health Editedstephen karikariNessuna valutazione finora
- Chapter 1 The GuideDocumento69 pagineChapter 1 The Guidemirabel IvanaliNessuna valutazione finora
- Socio 148 (09:12:19)Documento1 paginaSocio 148 (09:12:19)Janelle DyNessuna valutazione finora
- Konsep Keperawatan PaliatifDocumento17 pagineKonsep Keperawatan Paliatifshintiaazningrum21Nessuna valutazione finora
- Health Promotion: A Concept: Tim Ajar PKIPDocumento34 pagineHealth Promotion: A Concept: Tim Ajar PKIPMacan TultulNessuna valutazione finora
- CMD Course OutlineDocumento3 pagineCMD Course OutlineEvans SieleNessuna valutazione finora
- Care of The Adult Cancer Patient at The End of Life: ESMO Clinical Practice GuidelinesDocumento13 pagineCare of The Adult Cancer Patient at The End of Life: ESMO Clinical Practice GuidelinesDewi SunnnNessuna valutazione finora
- Patient'S ProfileDocumento17 paginePatient'S ProfileLucas JelmarNessuna valutazione finora
- Medicine General HXDocumento5 pagineMedicine General HXudazxfNessuna valutazione finora
- HIV Prevention Among Vulnerable Populations The Pathfinder International ApproachDocumento45 pagineHIV Prevention Among Vulnerable Populations The Pathfinder International ApproachKarlinaNessuna valutazione finora
- Nutrition Expo Case StudyDocumento5 pagineNutrition Expo Case Studyapi-609285533Nessuna valutazione finora
- Welcome To The COVID-19 and Cancer ECHO Series: Answering Your Questions LiveDocumento47 pagineWelcome To The COVID-19 and Cancer ECHO Series: Answering Your Questions LiveDazenNessuna valutazione finora
- 2506-Main Article Text (Blinded Article File) - 5212-1-10-20200910Documento4 pagine2506-Main Article Text (Blinded Article File) - 5212-1-10-20200910tania luarteNessuna valutazione finora
- Lecture 1 - Overview of CHNDocumento7 pagineLecture 1 - Overview of CHNAlannes AndalNessuna valutazione finora
- Duchenne MD EHusbandsDocumento33 pagineDuchenne MD EHusbandsfirst name last nameNessuna valutazione finora
- Family PlanningDocumento22 pagineFamily Planningjairadedios53Nessuna valutazione finora
- Right To Life, Liberty, and Insurance Coverage: Eating Disorder Treatment Abigail Mills Legal Studies Academy First Colonial High School December 22, 2016Documento18 pagineRight To Life, Liberty, and Insurance Coverage: Eating Disorder Treatment Abigail Mills Legal Studies Academy First Colonial High School December 22, 2016api-286768429Nessuna valutazione finora
- TNPSC SURESH IAS ACADEMY July Current Affairs (E)Documento60 pagineTNPSC SURESH IAS ACADEMY July Current Affairs (E)Siva Raman KNessuna valutazione finora
- Team Ubasan Brgy. Pasong Camachile 1: Certificate of RecognitionDocumento4 pagineTeam Ubasan Brgy. Pasong Camachile 1: Certificate of RecognitionReienel FerrerNessuna valutazione finora
- The Bold and The Beautiful. Influence of Body Size of Televised Media Models On Body Dissatisfaction and Actual Food IntakeDocumento8 pagineThe Bold and The Beautiful. Influence of Body Size of Televised Media Models On Body Dissatisfaction and Actual Food IntakeKATALINA IGNACIA AZÓCARNessuna valutazione finora
- THE Center: Anxiety DisordersDocumento13 pagineTHE Center: Anxiety DisordersOti VuraNessuna valutazione finora
- Mean Arterial PressureDocumento3 pagineMean Arterial Pressureleslie vasquez lucumiNessuna valutazione finora
- DNAlysis MygeneRx Sample ReportDocumento13 pagineDNAlysis MygeneRx Sample ReportTrustNessuna valutazione finora
- Henry Schein Orthodontics Catalog - General SuppliesDocumento8 pagineHenry Schein Orthodontics Catalog - General SuppliesOrtho OrganizersNessuna valutazione finora
- Trainee's CharacteristicDocumento3 pagineTrainee's CharacteristicRoldan EstibaNessuna valutazione finora
- Poverty Is General Scarcity or The State of One Who Lacks A Certain Amount of Material Possessions or MoneyDocumento41 paginePoverty Is General Scarcity or The State of One Who Lacks A Certain Amount of Material Possessions or MoneyChristian Cañon GenterolaNessuna valutazione finora
- ANNEX III ASEAN GL On Limits of Contaminations TMHS V1.0 (13nov14)Documento11 pagineANNEX III ASEAN GL On Limits of Contaminations TMHS V1.0 (13nov14)Bambang PriyambodoNessuna valutazione finora
- Sce550 PresentDocumento57 pagineSce550 Presentapi-289477817Nessuna valutazione finora
- Fatimah Kti FixDocumento71 pagineFatimah Kti FixOktaviani MuhaddistNessuna valutazione finora
- Manual Steamvection ThermasolDocumento6 pagineManual Steamvection ThermasolJosse RuizNessuna valutazione finora
- Cummins Prem Blue 15w40 1-18 L Sing Ssv3028m18 Asia-Pacific Purple Book (GHS) - EnglishDocumento14 pagineCummins Prem Blue 15w40 1-18 L Sing Ssv3028m18 Asia-Pacific Purple Book (GHS) - EnglishjosephvanbacNessuna valutazione finora
- Restobar FSDocumento58 pagineRestobar FSGabrielle Alonzo100% (1)
- Assessor Guide EntryLevelSHCODocumento12 pagineAssessor Guide EntryLevelSHCOEka BNessuna valutazione finora
- Harga Obat Generik E-KatalogueDocumento4 pagineHarga Obat Generik E-KatalogueMuhammad FarilNessuna valutazione finora
- Factors Affecting Demand For Soft DrinksDocumento8 pagineFactors Affecting Demand For Soft Drinksخلود البطاحNessuna valutazione finora
- 1.causes For Neonatal Sepsis, Newborn Sepsis, Neonatal Infection, Sepsis TreatmentDocumento12 pagine1.causes For Neonatal Sepsis, Newborn Sepsis, Neonatal Infection, Sepsis TreatmentlardiyahNessuna valutazione finora
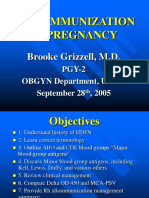
- Alloimmunization in Pregnancy: Brooke Grizzell, M.DDocumento40 pagineAlloimmunization in Pregnancy: Brooke Grizzell, M.DhectorNessuna valutazione finora
- Toxicology Procedures ManualDocumento206 pagineToxicology Procedures ManualDrMd IdrisNessuna valutazione finora
- Pseudo Bezoar in An Elderly ManDocumento4 paginePseudo Bezoar in An Elderly Manchidiebere peter echiehNessuna valutazione finora
- Is Our Brain Really Necessary-LorberDocumento3 pagineIs Our Brain Really Necessary-Lorberbigjon1359100% (1)
- Training Report BorocapsDocumento20 pagineTraining Report BorocapsCrimson TienNessuna valutazione finora