Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
RCT Appraisal Sheets 2005 English-1 1
Caricato da
api-479716004Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
RCT Appraisal Sheets 2005 English-1 1
Caricato da
api-479716004Copyright:
Formati disponibili
Critical Appraisal for Therapy Articles
THERAPY STUDY: Are the results of the trial valid? (Internal Validity)
What question did the study ask?
Patients –
Intervention -
Comparison -
Outcome(s) -
1a. R- Was the assignment of patients to treatments randomised?
What is best? Where do I find the information?
Centralised computer randomisation is ideal and often The Methods should tell you how patients were allocated
used in multi-centred trials. Smaller trials may use an to groups and whether or not randomisation was
independent person (e.g, the hospital pharmacy) to concealed.
“police” the randomization.
This paper: Yes No Unclear
Comment: There were 50 patients (37 male and 13 female participants). Ages ranging
between 22 years and 60 years (the mean was 42 years old). Duration of symptoms
was between 2 weeks and 36 months (the mean was 7.2 months). The mean duration
of symptoms with soft disc prolapse was 6.6 months and hard disc prolapse was 8.1
months. 18 patients had radicular without any neurological deficits while 32 had
radicular pain with neurological deficits.
1b. R- Were the groups similar at the start of the trial?
What is best? Where do I find the information?
If the randomisation process worked (that is, achieved The Results should have a table of "Baseline
comparable groups) the groups should be similar. The Characteristics" comparing the randomized groups on a
more similar the groups the better it is. number of variables that could affect the outcome (ie. age,
There should be some indication of whether differences risk factors etc). If not, there may be a description of group
between groups are statistically significant (ie. p values). similarity in the first paragraphs of the Results section.
This paper: Yes No Unclear
Comment: The groups are similar in respect to each patient having either a soft or hard dis
prolapse. The p-value between soft (0.0), hard (0.05) and none (0.37).
2a. A – Aside from the allocated treatment, were groups treated equally?
What is best? Where do I find the information?
Apart from the intervention the patients in the different Look in the Methods section for the follow-up schedule,
groups should be treated the same, eg., additional and permitted additional treatments, etc and in Results for
treatments or tests. actual use.
This paper: Yes No Unclear
Comment:
--All patients had MRI imaging in addition to the Spurlings test.
--All patients received advice in regards to their outcome.
--Patients that did not require surgery were managed conservatively
--Any patients with significant neurological deficits or failed conservative therapy were
advised surgery. Of these patients (Group 1) 25 patients underwent anterior cervical
discoidectomy
2b. A – Were all patients who entered the trial accounted for? – and were
they analysed in the groups to which they were randomised?
What is best? Where do I find the information?
Losses to follow-up should be minimal – preferably less The Results section should say how many patients were
than 20%. However, if few patients have the outcome of 1andomised (eg., Baseline Characteristics table) and how
interest, then even small losses to follow-up can bias the many patients were actually included in the analysis. You
results. Patients should also be analysed in the groups to will need to read the results section to clarify the number
which they were randomised – ‘intention-to-treat analysis’ . and reason for losses to follow-up.
University of Oxford, 2005 1
Critical Appraisal for Therapy Articles
This paper: Yes No Unclear
Comment: The Spurling’s test resulted in 27 correct detections of positive disc prolapse and
2 incorrect detections of positive disc prolapse . The Spurlings test deems effective as the
number of incorrect detections was less than 20%. The sensitivity was 93.1% and the
specificity was 95% for all disc prolapses. For soft disc prolapse, the sensitivity was 83.5%
and the specificity was 85.7%
3. M - Were measures objective or were the patients and clinicians kept
“blind” to which treatment was being received?
What is best? Where do I find the information?
It is ideal if the study is ‘double-blinded’ – that is, both First, look in the Methods section to see if there is some
patients and investigators are unaware of treatment mention of masking of treatments, eg., placebos with the
allocation. If the outcome is objective (eg., death) then same appearance or sham therapy. Second, the Methods
blinding is less critical. If the outcome is subjective (eg., section should describe how the outcome was assessed
symptoms or function) then blinding of the outcome and whether the assessor/s were aware of the patients'
assessor is critical. treatment.
This paper: Yes No Unclear
Comment: All patients if positive were given the same treatment. The practitioners were
aware of the correct form of treatment. There were no placebos or sham therapies that
were used for disc prolapse within this specific investigation.
University of Oxford, 2005 2
Critical Appraisal for Therapy Articles
What were the results?
1. How large was the treatment effect?
Most often results are presented as dichotomous outcomes (yes or not outcomes that happen or don't happen) and can
include such outcomes as cancer recurrence, myocardial infarction and death. Consider a study in which 15% (0.15) of
the control group died and 10% (0.10) of the treatment group died after 2 years of treatment. The results can be
expressed in many ways as shown below.
What is the measure? What does it mean?
Relative Risk (RR) = risk of the outcome in the The relative risk tells us how many times more likely it is that
treatment group / risk of the outcome in the control an event will occur in the treatment group relative to the control
group. group. An RR of 1 means that there is no difference between the
two groups thus, the treatment had no effect. An RR < 1 means
that the treatment decreases the risk of the outcome. An RR > 1
means that the treatment increased the risk of the outcome.
In our example, the RR = 0.10/0.15 = 0.67 Since the RR < 1, the treatment decreases the risk of death.
Absolute Risk Reduction (ARR) = risk of the The absolute risk reduction tells us the absolute difference in the
outcome in the control group - risk of the outcome rates of events between the two groups and gives an indication
in the treatment group. This is also known as the of the baseline risk and treatment effect. An ARR of 0 means
absolute risk difference. that there is no difference between the two groups thus, the
treatment had no effect.
In our example, the ARR = 0.15 - 0.10 = 0.05 or 5% The absolute benefit of treatment is a 5% reduction in the death
rate.
Relative Risk Reduction (RRR) = absolute risk The relative risk reduction is the complement of the RR and is
reduction / risk of the outcome in the control group. probably the most commonly reported measure of treatment
An alternative way to calculate the RRR is to effects. It tells us the reduction in the rate of the outcome in the
subtract the RR from 1 (eg. RRR = 1 - RR) treatment group relative to that in the control group.
In our example, the RRR = 0.05/0.15 = 0.33 or 33% The treatment reduced the risk of death by 33% relative to that
Or RRR = 1 - 0.67 = 0.33 or 33% occurring in the control group.
Number Needed to Treat (NNT) = inverse of the The number needed to treat represents the number of patients
ARR and is calculated as 1 / ARR. we need to treat with the experimental therapy in order to prevent
1 bad outcome and incorporates the duration of treatment.
Clinical significance can be determined to some extent by looking
at the NNTs, but also by weighing the NNTs against any harms or
adverse effects (NNHs) of therapy.
In our example, the NNT = 1/ 0.05 = 20 We would need to treat 20 people for 2 years in order to prevent
1 death.
2. How precise was the estimate of the treatment effect?
The true risk of the outcome in the population is not known and the best we can do is estimate the true risk based on the
sample of patients in the trial. This estimate is called the point estimate. We can gauge how close this estimate is to
the true value by looking at the confidence intervals (CI) for each estimate. If the confidence interval is fairly narrow then
we can be confident that our point estimate is a precise reflection of the population value. The confidence interval also
provides us with information about the statistical significance of the result. If the value corresponding to no effect falls
outside the 95% confidence interval then the result is statistically significant at the 0.05 level. If the confidence interval
includes the value corresponding to no effect then the results are not statistically significant.
Question 1 does not have any information relating to the type of study conducted
because all the patients had symptoms of disc prolapse. A control group was
therefore not included.
In regards to Question2, the confidence interval of this study was 95% for
sensitivity which equals 83.5 out of 100%. A 95% C1 for specificity which equals
85.7 out of 100% for soft disc prolapse
University of Oxford, 2005 3
Critical Appraisal for Therapy Articles
Will the results help me in caring for my patient? (ExternalValidity/Applicability)
The questions that you should ask before you decide to apply the results of the study to your patient are:
Is my patient so different to those in the study that the results cannot apply?
Is the treatment feasible in my setting?
Will the potential benefits of treatment outweigh the potential harms of treatment for my patient?
Yes. This form of screening had a 95% successful of detecting positive outcomes. The p-value was less
than 0.05 which considered significant.
The future patients we would treat in clinic would not be so different to those in the study that the results cannot
apply
This form of screening is feasible in my setting
The potential benefits of treatment do outweigh the potential harms of treatment for such future patients
10 IPAD QUESTIONS: (Wasn’t Covered but relates to Lecture on the Key points of a public health examination)
Q1: There is a need for this screening because it can help detect painful issues and give a reason and suitable
and appropriate treatment guidline for the condition.
Q2: The object is clear prior to the screening with a clear focus on detecting the presence of a disc prolapse. If
there is no suspicion that this condition is contributing to the pain, then this screening would not be compliant.
Q3: It is hard to define a specific population but you are looking for people with a set of specific symptoms. This
audience can be of any age, gender or race.
Q4: There is clear evidence has highlighted in the article which was analysed earlier. To reiterate, there was a 95%
success rate of positive detections using the Spurling’s screening test. Which was confirmed through MRI imaging.
Q5:
Testing: obviously there is the integration of a well-known practice
Education: No education was specifically included in this study however, the patients would have been made
aware of the procedure and their condition of interest.
Management:
Post management of the Spurlings test included advised surgery if condition was present with significant
neurological deficits. Other management methods included conservative therapy revolving around physical
therapy.
Q6: This was a singular study therefore, quality of testing between the groups was minimal. There was a
consistent procedure for all patients however, because this was on study, consistency between the groups was
unable to be identified. However, all patients were given an MRI after the test to ensure its accuracy.
Q7. All of the patients within the study willingly consented to participate within the investigation and the post
managements processes.
Q8: Everyone within the population studies was given the same screening process and treatment throughout.
Q9: Yes. There is infact no risk related to this form of screening
Q10: There is a high level of confidentiality within this screening process. No names or personal details were
exposed to the general public.
University of Oxford, 2005 4
Critical Appraisal for Therapy Articles
Spurlings test overall is an effective screening method of detecting Disc prolapses. This is advised when patients
are within the “detectable phase” of the condition. Whereby the will be experinecing symptoms such as pain,
discomfort, pinching, inability to perform some movements and have usual range of motion and neurological
deficits
Reference
Shah, K. & Rajshekhar, V. (2004). Reliability of diagnosis of soft cervical disc prolapse using
spurlings test. British Journal of Neurosurgery, 18(5), 480-483.
https://doi.org/10.1080/02688690400012350
Link to Source:
https://www.tandfonline.com/doi/abs/10.1080/02688690400012350
University of Oxford, 2005 5
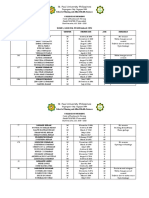
Potrebbero piacerti anche
- MENSTRUATION - (NOT) A TABOO - July 3, 4-56 PMDocumento27 pagineMENSTRUATION - (NOT) A TABOO - July 3, 4-56 PMUtkrashtNessuna valutazione finora
- Basic Principles of NaturopathyDocumento18 pagineBasic Principles of NaturopathyKanak Soni100% (2)
- Nursing Bullets 5Documento268 pagineNursing Bullets 5kate annNessuna valutazione finora
- RCT Appraisal Sheets 2005 English-2Documento4 pagineRCT Appraisal Sheets 2005 English-2Mahardhika AcintyaNessuna valutazione finora
- Obstetrics and Gynaecology Case ProformaDocumento13 pagineObstetrics and Gynaecology Case Proformamd maaz100% (4)
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyDa EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyValutazione: 1 su 5 stelle1/5 (1)
- A List A Statistical Definition For The CICM Fellowship ExamDocumento5 pagineA List A Statistical Definition For The CICM Fellowship ExamSimon WongNessuna valutazione finora
- Centralised Computer Randomisation Is: Critical Appraisal For Therapy ArticlesDocumento4 pagineCentralised Computer Randomisation Is: Critical Appraisal For Therapy ArticleshadzaliegNessuna valutazione finora
- Referat Iktiosis PembahasanDocumento4 pagineReferat Iktiosis PembahasanPatih GajahmadaNessuna valutazione finora
- RCT Appraisal Sheets 2005 EnglishDocumento4 pagineRCT Appraisal Sheets 2005 EnglishAmanda SoebadiNessuna valutazione finora
- Worksheet Therapy-CebmDocumento3 pagineWorksheet Therapy-Cebmteddy sNessuna valutazione finora
- Patients - Intervention - Comparison - Outcome(s)Documento3 paginePatients - Intervention - Comparison - Outcome(s)Intan SetyadewiNessuna valutazione finora
- Therapy Studies What Question Did The Study Ask?Documento2 pagineTherapy Studies What Question Did The Study Ask?Apt RiskaNessuna valutazione finora
- Worksheet Appraisal AZALEADocumento5 pagineWorksheet Appraisal AZALEAArini NurlelaNessuna valutazione finora
- Centralised Computer Randomisation IsDocumento4 pagineCentralised Computer Randomisation IsAhmad BukhariNessuna valutazione finora
- RCT Appraisal Sheets 2005 EnglishDocumento2 pagineRCT Appraisal Sheets 2005 EnglishF NNessuna valutazione finora
- Randomised: Differences Between Groups Are Statistically Significant P ValuesDocumento6 pagineRandomised: Differences Between Groups Are Statistically Significant P ValuesArga PRNessuna valutazione finora
- (OBAT CINA) CAT TherapyDocumento6 pagine(OBAT CINA) CAT TherapyArga PRNessuna valutazione finora
- Worksheet Therapy CebmDocumento3 pagineWorksheet Therapy Cebmandynightmare97Nessuna valutazione finora
- CRITICAL APPRAISAL Mas WikoDocumento10 pagineCRITICAL APPRAISAL Mas WikoEliataMariaMahanaimNessuna valutazione finora
- Patients - Intervention - Comparison - Outcome(s) - Knowledge GapDocumento4 paginePatients - Intervention - Comparison - Outcome(s) - Knowledge GapAmal NajiNessuna valutazione finora
- RCT Appraisal Sheets 2005 English-2Documento6 pagineRCT Appraisal Sheets 2005 English-2tsyrahmaniNessuna valutazione finora
- Critical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Documento4 pagineCritical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Putri Widya AndiniNessuna valutazione finora
- Patients - Intervention - Comparison - Outcome(s)Documento4 paginePatients - Intervention - Comparison - Outcome(s)sahirbuleNessuna valutazione finora
- Patients - Intervention - Comparison - Outcome(s)Documento4 paginePatients - Intervention - Comparison - Outcome(s)Ainur 'iin' RahmahNessuna valutazione finora
- RCT+Appraisal+sheets 2005Documento3 pagineRCT+Appraisal+sheets 2005Otty Mitha OctrizaNessuna valutazione finora
- Critical Appraisal Jurnal Asam Traneksamat Pada MelasmaDocumento4 pagineCritical Appraisal Jurnal Asam Traneksamat Pada MelasmaMsrirrrNessuna valutazione finora
- Critical ApraisalDocumento4 pagineCritical Apraisalfauziah qurrota a'yuniNessuna valutazione finora
- RCT Appraisal Sheets 2005 English-2Documento3 pagineRCT Appraisal Sheets 2005 English-2VeysusanNessuna valutazione finora
- Critical Appraisal TafaDocumento7 pagineCritical Appraisal TafaFabric FameNessuna valutazione finora
- Tugas Farepid - CA - 198114152Documento11 pagineTugas Farepid - CA - 198114152JeanieNessuna valutazione finora
- Therapy RCT Critical Appraisal Worksheet With ExplanationDocumento2 pagineTherapy RCT Critical Appraisal Worksheet With ExplanationAdwin AlamsyaputraNessuna valutazione finora
- CA Therapy Artikel 09Documento5 pagineCA Therapy Artikel 09Christiana TrijayantiNessuna valutazione finora
- Kritisi Artikel - Ni Nengah Susilawati - 152191105 - BDocumento5 pagineKritisi Artikel - Ni Nengah Susilawati - 152191105 - BShilaNessuna valutazione finora
- Telaah Kritis Jurnal 2Documento9 pagineTelaah Kritis Jurnal 2Ayu Vitha ViginiaNessuna valutazione finora
- EBM Dan Critical AppraisalDocumento7 pagineEBM Dan Critical AppraisalNovia Ariani DewiNessuna valutazione finora
- Crit AppDocumento5 pagineCrit AppdikkaNessuna valutazione finora
- Presentation On TherapyDocumento21 paginePresentation On TherapyMarjorie CepeNessuna valutazione finora
- Worksheet Therapy CebmDocumento5 pagineWorksheet Therapy CebmZulfan RifqiawanNessuna valutazione finora
- Critical Appraisal Checklist For An Article On Treatment or PreventionDocumento4 pagineCritical Appraisal Checklist For An Article On Treatment or PreventionSaina AbasNessuna valutazione finora
- Critical Appraisal Checklist For An Article OnDocumento4 pagineCritical Appraisal Checklist For An Article OnTiaz DiniutamiNessuna valutazione finora
- C - II - 3 - Critical AppraisalDocumento10 pagineC - II - 3 - Critical AppraisalWahyu NandaNessuna valutazione finora
- Critical Appraisal Therapy Study by DR BhismaDocumento28 pagineCritical Appraisal Therapy Study by DR BhismaAhmadAfiyyuddinNessuna valutazione finora
- Angel Yudiakristi - Praktikum 5Documento10 pagineAngel Yudiakristi - Praktikum 5Angel MaharaniNessuna valutazione finora
- Anesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Documento4 pagineAnesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Sandra Lydiayana Aisyah AzharNessuna valutazione finora
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Documento6 pagineTherapystudy: Are The Results of The Trial Valid? (Internal Validity)Sinta AgustinaNessuna valutazione finora
- RCT+Appraisal+sheets. TherapyDocumento2 pagineRCT+Appraisal+sheets. Therapydian_c87Nessuna valutazione finora
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Documento10 pagineTherapystudy: Are The Results of The Trial Valid? (Internal Validity)WiraNessuna valutazione finora
- Critical Appraisal of TherapyDocumento34 pagineCritical Appraisal of Therapyapi-19733840Nessuna valutazione finora
- Critical Appraisal of Articles On TherapyDocumento46 pagineCritical Appraisal of Articles On TherapyAditya Rachman Van Der ArjunaqueeNessuna valutazione finora
- Checklist RCTDocumento5 pagineChecklist RCTFajar SukmajayaNessuna valutazione finora
- Confidence Intervals II AJPDocumento5 pagineConfidence Intervals II AJPJu ChangNessuna valutazione finora
- EBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Documento15 pagineEBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Soffatul AzizahNessuna valutazione finora
- Evidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUDocumento40 pagineEvidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUSamuel TanNessuna valutazione finora
- Table 2A: Worksheet Critical Appraisal Article Therapy Questions Your AnswerDocumento10 pagineTable 2A: Worksheet Critical Appraisal Article Therapy Questions Your Answer7CANTIKA PRAMESWARI HANANTONessuna valutazione finora
- Evidence-Based Medicine Therapy: Dr. Rina Amelia, MARSDocumento43 pagineEvidence-Based Medicine Therapy: Dr. Rina Amelia, MARSRezky IlhamNessuna valutazione finora
- Therapy - Siti Setiati Evidence Based MedicineDocumento33 pagineTherapy - Siti Setiati Evidence Based MedicinejoeNessuna valutazione finora
- TherappraisalclrDocumento5 pagineTherappraisalclrMike CabotageNessuna valutazione finora
- Make A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdiDocumento12 pagineMake A NewSenin 26 Januari 2015 EBM GLOSARY Dr. Akhmad EdinaotonaoiNessuna valutazione finora
- Therapy Worksheet Title of Article: Authors: Journal: BackgroundDocumento3 pagineTherapy Worksheet Title of Article: Authors: Journal: BackgroundRandi Kosim SiregarNessuna valutazione finora
- (CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesDocumento159 pagine(CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesKaren Mae PadillaNessuna valutazione finora
- Association MeasurementDocumento5 pagineAssociation Measurementnva1995Nessuna valutazione finora
- Twice Weekly FluticasoneDocumento4 pagineTwice Weekly FluticasoneAudrey GillNessuna valutazione finora
- Rubric Reflective Portfolio 2020Documento3 pagineRubric Reflective Portfolio 2020api-479716004Nessuna valutazione finora
- Reflection 1Documento2 pagineReflection 1api-479716004Nessuna valutazione finora
- Reflection 2Documento2 pagineReflection 2api-479716004Nessuna valutazione finora
- Week 3 Portfolio QuestionsDocumento5 pagineWeek 3 Portfolio Questionsapi-479716004Nessuna valutazione finora
- Week 5 Portfolio QuestionsDocumento4 pagineWeek 5 Portfolio Questionsapi-479716004Nessuna valutazione finora
- Week 8 Portfolio QuestionsDocumento2 pagineWeek 8 Portfolio Questionsapi-479716004Nessuna valutazione finora
- Week 2 Portfolio QuestionsDocumento12 pagineWeek 2 Portfolio Questionsapi-479716004Nessuna valutazione finora
- Study Guide Questions: 10.4: Exemplar For This Activity and Create A Management Plan For This PatientDocumento5 pagineStudy Guide Questions: 10.4: Exemplar For This Activity and Create A Management Plan For This Patientapi-479716004Nessuna valutazione finora
- Week 6 Portfolio QuestionsDocumento6 pagineWeek 6 Portfolio Questionsapi-479716004Nessuna valutazione finora
- Portfolio Exercises Week 9 & 10: Exercise 1 Differential Chart Location DDX Hip Pain DescriptionDocumento6 paginePortfolio Exercises Week 9 & 10: Exercise 1 Differential Chart Location DDX Hip Pain Descriptionapi-479716004Nessuna valutazione finora
- Exercise 1Documento13 pagineExercise 1api-479716004Nessuna valutazione finora
- Self-Directed LearningDocumento3 pagineSelf-Directed Learningapi-479716004Nessuna valutazione finora
- Week 1 Portfolios QuestionsDocumento7 pagineWeek 1 Portfolios Questionsapi-479716004Nessuna valutazione finora
- Exercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 7Documento4 pagineExercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 7api-479716004Nessuna valutazione finora
- Exercise 1Documento4 pagineExercise 1api-479716004Nessuna valutazione finora
- Reflection - Edward AtkinsDocumento2 pagineReflection - Edward Atkinsapi-479716004Nessuna valutazione finora
- Study Guide Questions: 9.4: Magee D, Edition (2014), Page 759-759 Provided As An ExemplarDocumento9 pagineStudy Guide Questions: 9.4: Magee D, Edition (2014), Page 759-759 Provided As An Exemplarapi-479716004Nessuna valutazione finora
- Study Guide Questions Week 5Documento3 pagineStudy Guide Questions Week 5api-479716004Nessuna valutazione finora
- Reflection 4Documento2 pagineReflection 4api-479716004Nessuna valutazione finora
- Week 8 QuestionsDocumento8 pagineWeek 8 Questionsapi-479716004Nessuna valutazione finora
- Reflection 1Documento2 pagineReflection 1api-479716004Nessuna valutazione finora
- Reflection 5Documento2 pagineReflection 5api-479716004Nessuna valutazione finora
- Reliability of Diagnosis of Soft Cervical Disc Prolapse Using Spurling's TestDocumento5 pagineReliability of Diagnosis of Soft Cervical Disc Prolapse Using Spurling's Testapi-479716004Nessuna valutazione finora
- Reflection 2Documento2 pagineReflection 2api-479716004Nessuna valutazione finora
- Reflection 3Documento2 pagineReflection 3api-479716004Nessuna valutazione finora
- Ministry of Health Begins Recruitment For Barbados Nursing JobsDocumento2 pagineMinistry of Health Begins Recruitment For Barbados Nursing JobsKweku ZurekNessuna valutazione finora
- 4 Clonorchis+SinensisDocumento13 pagine4 Clonorchis+SinensiskhaledNessuna valutazione finora
- Contracted Pelvis and ManagementDocumento19 pagineContracted Pelvis and Managementkirtyy20Nessuna valutazione finora
- Lymphoma HandoutDocumento5 pagineLymphoma Handoutapi-244850728Nessuna valutazione finora
- Health-Care Workers' Occupational Exposures To Body Fluids in 21 Countries in Africa: Systematic Review and Meta-AnalysisDocumento17 pagineHealth-Care Workers' Occupational Exposures To Body Fluids in 21 Countries in Africa: Systematic Review and Meta-AnalysisgusdeNessuna valutazione finora
- Hildebert Wagner, Stefan Kraus, Ksenija Jurcic Auth., Prof. Dr. Dr. H.C. H. Wagner Eds. Immunomodulatory Agents From PlantsDocumento377 pagineHildebert Wagner, Stefan Kraus, Ksenija Jurcic Auth., Prof. Dr. Dr. H.C. H. Wagner Eds. Immunomodulatory Agents From PlantsZafer Corlu100% (1)
- Certificate of Community Service: Roselle May AberillaDocumento52 pagineCertificate of Community Service: Roselle May Aberillaucnursingcesdev2008Nessuna valutazione finora
- Family Nursing and Home NursingDocumento35 pagineFamily Nursing and Home NursingSamjhana Neupane100% (1)
- Suicide Competencies For Psychiatric-Mental Health NursesDocumento6 pagineSuicide Competencies For Psychiatric-Mental Health NursesnicolasNessuna valutazione finora
- Canine Protected Occlusion: Indian Journal of Oral Sciences January 2012Documento7 pagineCanine Protected Occlusion: Indian Journal of Oral Sciences January 2012SkAliHassanNessuna valutazione finora
- NCPDocumento3 pagineNCPDyanne BautistaNessuna valutazione finora
- Infectious DiarrheaDocumento85 pagineInfectious DiarrheaTarikNessuna valutazione finora
- A Simpler Prediction Rule For Rebound HyperbilirubinemiaDocumento7 pagineA Simpler Prediction Rule For Rebound HyperbilirubinemiaNoviaNessuna valutazione finora
- A Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDocumento9 pagineA Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Review Jurnal Bahasa Indonesia Kelompok 3-1Documento12 pagineReview Jurnal Bahasa Indonesia Kelompok 3-1Rayhan Al FajriNessuna valutazione finora
- University For Development Studies Field ReportDocumento21 pagineUniversity For Development Studies Field ReportOsman Issaku AlemNessuna valutazione finora
- CV DR - Muhammad Moosa DaudpotaDocumento2 pagineCV DR - Muhammad Moosa DaudpotaMuhammad MoosaNessuna valutazione finora
- Campinha Bacote ModelDocumento2 pagineCampinha Bacote ModelApril Jane PanchoNessuna valutazione finora
- Doctor of Veterinary Medicine: 1st Year 1st SemesterDocumento4 pagineDoctor of Veterinary Medicine: 1st Year 1st SemesterDexter LagrimasNessuna valutazione finora
- Moebius Syndrome: A Guide To UnderstandingDocumento8 pagineMoebius Syndrome: A Guide To Understandingterima kasihNessuna valutazione finora
- Newborn AssessmentDocumento9 pagineNewborn AssessmentSusmita HalderNessuna valutazione finora
- Lecture 9 Obstetrical OperationsDocumento47 pagineLecture 9 Obstetrical OperationsgnpobsNessuna valutazione finora
- Obesity: Carrie Miller, MSN, RN, CNEDocumento30 pagineObesity: Carrie Miller, MSN, RN, CNEJeanIzeanNessuna valutazione finora
- St. Paul University Philippines: School of Nursing and Allied Health SciencesDocumento12 pagineSt. Paul University Philippines: School of Nursing and Allied Health SciencesKarina MadriagaNessuna valutazione finora
- Articulators: DR - Muhammad Aamir Rafiq Assistant ProfDocumento52 pagineArticulators: DR - Muhammad Aamir Rafiq Assistant Profnauman tariqNessuna valutazione finora
- Nursing Care Plan Nursing Diagnosis Analysis Goal Intervention Rationale EvaluationDocumento7 pagineNursing Care Plan Nursing Diagnosis Analysis Goal Intervention Rationale EvaluationHanz Abbigail Roco100% (1)