Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Focal Points
Caricato da
pepe_garces_2Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Focal Points
Caricato da
pepe_garces_2Copyright:
Formati disponibili
FocalPoints
Clinical Modules for Ophthalmologists
V O L U M E X X V I I I NUMBER 8
S E P T E M B E R 2 010 (2 of 3)
Basic Principles of
Phacoemulsification
and Fluid Dynamics
Uday Devgan, MD, FACS, FRCS (Glasg)
Reviewers and Contributing Editors Consultants
D. Michael Colvard, MD, FACS; Thomas L. Beardsley, MD, Editors for Cataract Surgery Barry S. Seibel, MD
James C. Bobrow, MD, Basic and Clinical Science, Course Faculty, Section 11 Donald N. Serafano, MD
Edward K. Isbey III, MD, Practicing Ophthalmologists Advisory Committee for Education
FPv28n08_0910.indd 1 7/23/10 1:30 PM
Focal Points Editorial Review Board
Claiming CME Credit George A. Stern, MD, Missoula, MT
Editor in Chief; Cornea & External Disease
Academy members: To claim Focal Points CME cred- William S. Clifford, MD, Garden City, KS
its, visit the Academy web site and access CME Central Glaucoma Surgery; Liaison for Practicing Ophthalmologists Advisory
(http://one.aao.org/CE/MyCMEPortfolio/default.aspx) Committee for Education
to view and print your Academy transcript and report D. Michael Colvard, MD, FACS, Encino, CA
CME credit you have earned. You can claim up to two Cataract Surgery
AMA PRA Category 1 Credits™ per module. This will give
Bradley S. Foster, MD, Springfield, MA
you a maximum of 24 credits for the 2010 subscrip- Retina & Vitreous
tion year. CME credit may be claimed for up to three (3)
Anil D. Patel, MD, Oklahoma City, OK
years from date of issue. Non-Academy members: For
Neuro-Ophthalmology
assistance please send an e-mail to customer_service
Eric P. Purdy, MD, Fort Wayne, IN
@aao.org or a fax to (415) 561-8575.
Oculoplastic, Lacrimal, & Orbital Surgery
Steven I. Rosenfeld, MD, FACS, Delray Beach, FL
Refractive Surgery, Optics & Refraction
Focal Points (ISSN 0891-8260) is published quarterly by the American Acad-
C. Gail Summers, MD, Minneapolis, MN
emy of Ophthalmology at 655 Beach St., San Francisco, CA 94109-1336. For
domestic subscribers, print with online 1-year subscription is $187 for Academy
Pediatric Ophthalmology & Strabismus
members (2 years, $337; 3 years, $477) and $252 for nonmembers (2 years, Albert T. Vitale, MD, Salt Lake City, UT
$455; 3 years, $642). International subscribers, please visit www.aao.org/
Ocular Inflammation & Tumors
focalpoints for more information. Online-only 1-year subscription is $155 for
Academy members (2 years, $277; 3 years, $395) and $209 for nonmembers
(2 years, $375; 3 years, $535). Periodicals postage paid at San Francisco, CA,
and additional mailing offices. POSTMASTER: Send address changes to Focal
Focal Points Staff
Points, P.O. Box 7424, San Francisco, CA 94120-7424.
Susan R. Keller, Acquisitions Editor
The American Academy of Ophthalmology is accredited by the Accredita-
tion Council for Continuing Medical Education to provide continuing medical Kim Torgerson, Publications Editor
education for physicians.
The American Academy of Ophthalmology designates this educational
activity for a maximum of two AMA PRA Category 1 Credits™. Physicians Clinical Education Secretaries and Staff
should only claim credit commensurate with the extent of their participation
in the activity. Gregory L. Skuta, MD, Senior Secretary for Clinical Education,
Reporting your CME online is one benefit of Academy membership. Non- Oklahoma City, OK
members may request a Focal Points CME Claim Form by contacting Focal
Points, 655 Beach St., San Francisco, CA 94109-1336. Louis B. Cantor, MD, Secretary for Ophthalmic Knowledge,
The Academy provides this material for educational purposes only. It is not Indianapolis, IN
intended to represent the only or best method or procedure in every case, nor
to replace a physician’s own judgment or give specific advice for case manage- Richard A. Zorab, Vice President, Ophthalmic Knowledge
ment. Including all indications, contraindications, side effects, and alternative Hal Straus, Director of Print Publications
agents for each drug or treatment is beyond the scope of this material. All
information and recommendations should be verified, prior to use, with current
information included in the manufacturers’ package inserts or other indepen-
dent sources and considered in light of the patient’s condition and history.
Reference to certain drugs, instruments, and other products in this publica-
tion is made for illustrative purposes only and is not intended to constitute
an endorsement of such. Some material may include information on applica-
tions that are not considered community standard, that reflect indications not
included in approved FDA labeling, or that are approved for use only in restricted
research settings. The FDA has stated that it is the responsibility of the physi-
cian to determine the FDA status of each drug or device he or she wishes to
use, and to use them with appropriate informed patient consent in compliance
with applicable law. The Academy specifically disclaims any and all liability for
injury or other damages of any kind, from negligence or otherwise, for any
and all claims that may arise out of the use of any recommendations or other
information contained herein. The author(s) listed made a major contribution
to this module. Substantive editorial revisions may have been made based on
reviewer recommendations.
Subscribers requesting replacement copies 6 months and later from the
cover date of the issue being requested will be charged the current module
replacement rate.
©2010 American Academy of Ophthalmology®. All rights reserved.
ii Focal Points : Module 8, 2010
FPv28n08_0910.indd 2 7/23/10 1:30 PM
Learning Objectives
Upon completion of this module,
Contents
the reader should be able to:
Introduction 1
• Choose appropriate f luidic settings for
phacoemulsification (phaco) depending on the The Phacoemulsification Platform 2
surgical situation • Foot Position 1: Irrigation 2
• Select phaco power modulations to deliver less • Foot Position 2: Vacuum and Aspiration
ultrasonic phaco energy into the eye during
of Fluid 2
cataract surgery • Foot Position 3: Ultrasound Energy 2
• Describe the difference between peristaltic Basic Concepts of Fluidics 2
and venturi f luid pumps and know the clinical • Modulating Phacoemulsification
significance of changing parameters Fluid Flow: Poiseuille’s Equation 2
• Perform safer, less traumatic, and more • Modulating Fluid Inflow 3
efficient cataract surgery by tailoring the • Modulating Fluid Outflow 3
phacoemulsification power and f luidic settings to
the surgical style and patients’ eyes Flow Balance and Tubing Compliance 3
• Inflow Versus Outflow Tubing 3
Financial Disclosures
• Phacoemulsification Needle Sizing 3
The authors, reviewers, and consultants disclose the following
financial relationships. D. Michael Colvard, MD, FACS: (C) Abbott Peristaltic and Venturi Fluid Pumps 4
Medical Optics, Bausch & Lomb; (P) OASIS Medical. Uday Devgan, • Peristaltic Pump (Flow Based) 4
MD, FACS, FRCS (Glasg): (C) Bausch & Lomb Surgical, Hoya
• Venturi Pump (Vacuum Based) 4
Surgical Optics, Inspire, Ista Pharmaceuticals; (L) Accutome, Alcon
Laboratories, Bausch & Lomb Surgical, Carl Zeiss Meditec, Haag-
Optimizing Phacoemulsification
Streit, Hoya Surgical Optics, Ista Pharmaceuticals, Optos, SLACK;
Fluidic Settings 5
(O) Alcon Laboratories, Bausch & Lomb Surgical, Inspire, Ista
Pharmaceuticals, Renaissance Surgical, Specialty Surgical, STAAR Fundamentals of Ultrasonic
Surgical; (P) Accutome; (C,L,O,S) Advanced Medical Optics, Allergan. Phacoemulsification Power 6
Steven I. Rosenfeld, MD, FACS: (C) Inspire Pharmaceuticals;
• Continuous, Pulse, and Burst
(L) Allergan. Barry S. Seibel, MD: (L) Alcon Laboratories, Bausch &
Phacoemulsification Modes 7
Lomb; (O) Calhoun Vision, OptiMedica; (P) Rhein Medical, SLACK.
Donald N. Serafano, MD: (C) Alcon Laboratories. C. Gail Summers, • Hyper Settings for Power Modulation 7
MD: (C) McKesson; (L) BioMarin. Albert T. Vitale, MD: (C) Aciont, • Variable Duty Cycle 8
Bausch & Lomb Surgical.
Conclusion 9
The following contributors state that they have no significant financial
interest or other relationship with the manufacturer of any commer- Clinicians’ Corner 10
cial product discussed in their contributions to this module or with
the manufacturer of any competing commercial product: Thomas
L. Beardsley, MD; William S. Clifford, MD; Bradley S. Foster, MD;
Edward K. Isbey III, MD; Susan R. Keller; Anil D. Patel; MD; Eric P.
Purdy, MD; George A. Stern, MD; Kim Torgerson. Introduction
C = Consultant fee, paid advisory boards or fees for attending a Achievement of the best possible outcomes in phacoemul-
meeting sification requires more than simply the mastery of the
L = Lecture fees (honoraria), travel fees or reimbursements when techniques of the procedure. Optimization of outcomes
speaking at the invitation of a commercial entity requires an understanding of the fundamental physics
O = Equity ownership/stock options of publicly or privately traded of the device, and the ability of the surgeon to modify
firms (excluding mutual funds) basic power and f luidic parameters in order to improve
P = Patents and/or royalties that might be viewed as creating a the performance of the device in challenging clinical set-
potential conflict of interest tings. A thorough understanding of phacodynamics and
S = Grant support
Focal Points : Module 8, 2010 1
FPv28n08_0910.indd 1 7/23/10 1:30 PM
f luidics is necessary before the complete phacoemulsi- the incisions until equilibrium is achieved. An optional
fication surgeon can make these refinements in order switch for continuous f low is available and is useful in
to perform phacoemulsification at the highest level of avoiding inadvertent release of position 1 and potential
proficiency and safety. collapse of the anterior chamber.
Foot Position 2: Vacuum
and Aspiration of Fluid
The Phacoemulsification Position 2 controls the vacuum and the relative aspira-
Platform tion rate of the f luid from the eye. There may be a linear
control of vacuum and f low, so that the top of position 2
All phacoemulsification (phaco) platforms share the provides less vacuum or f low than the middle or bottom
same basic structure and concepts. The phaco machine range of the pedal. This is similar to the gas pedal in a
aims to balance f luidics within the eye, while delivering car, where the car’s throttle opens more as the gas pedal
ultrasonic energy and vacuum in order to emulsify and is further depressed. The vacuum and aspiration levels
aspirate the cataract through a small incision. created during surgery draw the f luid out of the eye and
The main functions of the phaco machine are to pro- into a waste f luid collection via the outf low tubing.
vide irrigation into the eye; to create vacuum/aspiration
to remove the cataract; and to deliver ultrasound energy Foot Position 3: Ultrasound Energy
in order to emulsify the nucleus. These functions corre-
Position 3 controls the delivery of ultrasound energy.
spond to the machine’s 3 foot pedal positions (Figure 1).
There is linear control of the ultrasound energy level so
that further pedal depression results in more ultrasound
Foot Position 1: Irrigation
energy. Note that if the pedal is in position 3, the sur-
The irrigation function of the phacoemulsification geon is already engaging the full function of both posi-
machine provides a source of f luid infusion into the eye tions 1 and 2. The irrigation is on, and the vacuum and
during the surgery. Depressing the foot pedal to posi- aspiration level is at its highest preset level. Ultrasound
tion 1 turns on the infusion. There is no linear control energy should only be applied once the tip of the phaco
of the infusion—the infusion is either turned on or probe is in contact with part of the cataract.
turned off. The height of the infusion bottle determines
the relative infusion pressure and f low rate during the
surgery. To keep the eye inf lated during surgery, the
surgeon needs to make sure that the f luid inf low rate Basic Concepts
is at least as great as the f luid outf low rate, because
any excess inf low will pressurize the eye and leak from of Fluidics
Due to the small volume of the anterior and posterior
chambers, the control of f luidics during phacoemulsifi-
cation surgery is critical. By keeping a constant infusion
pressure and by carefully controlling the outf low, the
surgeon can ensure that the eye stays inf lated and stable
during surgery. If the surgeon allows outf low to exceed
inf low, even for a fraction of a second, the chamber is at
risk of collapse.
Modulating Phacoemulsification
Fluid Flow: Poiseuille’s Equation
The basic equation that governs all f luid f low during
phacoemulsification surgery is Poiseuille’s equation:
Figure 1 Position of the phaco system foot pedal controls
the 3 basic functions of the device. Position 1 delivers irriga- F = ΔP π r 4/8 η L
tion alone, position 2 provides irrigation plus aspiration, and
In this equation, F = f low, ΔP = pressure gradient,
position 3 adds phaco energy to irrigation and aspiration.
r = radius of the tube, η = viscosity of fluid, and L = length
2 Focal Points : Module 8, 2010
FPv28n08_0910.indd 2 7/23/10 1:30 PM
of the tube (meters). The relative relationship is of more from the incisions. The rate of the f luid outf low loss via
concern than the exact values. The viscosity of the f luid the incisions depends on the relative fit of the phaco tip
is relatively constant, as is the length of the tubing; in within the incision.
addition, the values of π and 8 are constant. This leaves Some degree of f luid leakage from the incisions is
a simpler equation: helpful to allow cooling of the phaco needle and to pre-
vent thermal injury during surgery. With the use of
F ~ ΔP r 4
advanced phaco power modulations, more experienced
Flow is proportional to the difference in pressure times phaco surgeons tend to move towards tighter incisions,
the radius of the tubing to the fourth power. Because the which can give more stable f luidics.
value for tubing size is exponential, a small change to
the radius results in a large change in the relative f low.
A common-sense situation clearly illustrates this. When
one drinks through a straw of narrow internal diameter, Flow Balance and
more vacuum is required to move fluid than when drink-
ing through a straw of wider diameter (Figure 2). Tubing Compliance
Modulating Fluid Inflow Inflow Versus Outflow Tubing
The source of f luid inf low is the bottle of balanced salt The inf low tubing has a large bore and thin walls, and
solution. The factors that determine the rate of inf low the tubing is very f lexible. The purpose of this tubing is
are pressure and the radius of the inf low tubing. To to provide a high f low of f luid under low-pressure sit-
modulate the pressure, the surgeon raises or lowers the uations. The maximum pressure achieved within this
height of the bottle relative to the patient’s eye. The inf low tubing is determined by the height of the infu-
inf low tubing has a large radius in order to maximize sion bottle, and this level is not very high.
the f low. The outf low tubing has a smaller bore and thick walls,
and the tubing is very rigid and relatively noncompliant.
Modulating Fluid Outflow Because the f low varies exponentially with the radius
of the tubing, the smaller-bore outf low tubing can help
The sources of f luid outf low are (1) the f luid removed ensure that the outf low does not exceed the inf low. The
via the phacoemulsification probe due to the vacuum outf low tubing has rigid, thick walls in order for it to
level generated by the f luid pump, and (2) f luid leakage have a low compliance, which helps to prevent surge. The
f luid pump of the phacoemulsification machine deter-
mines the maximum pressure achieved within the out-
f low tubing and can easily exceed 500 mm of mercury.
This high vacuum level can cause collapse of the
outf low tubing if its walls are too thin and compliant.
When the outf low tubing collapses, and then rebounds
back to its normal state after the vacuum level drops,
this energy release causes an immediate and dangerous
surge of f luid out of the eye. This occurs most commonly
after occlusion of the phaco probe, when the occlusion
suddenly breaks and the tubing rebounds, causing the
surge. This is called postocclusion surge and is one of the
main causes of posterior capsule rupture during cataract
surgery (Figure 3).
Phacoemulsification Needle Sizing
Figure 2 Poiseuille’s equation shows that smaller-bore tub- The size of the phacoemulsification needle lumen is
ing (a) requires higher vacuum and results in a lower flow, important for phaco f luidics because it affects the out-
as compared to larger-bore tubing (b), which can achieve a
f low rate. The important thing to remember from Poi-
high flow with less vacuum. The change in flow is exponen-
tially related to the radius of the tubing. seuille’s equation is that the f low is proportional to the
radius of the tube to the fourth power. This means that
Focal Points : Module 8, 2010 3
FPv28n08_0910.indd 3 7/23/10 1:30 PM
once an occlusion happens at the tip. However, some
machines also allow surgeons to program this speed
based on their technique. Thus, if the surgeon wants a
faster or slower “rise time” to the maximum value of
vacuum, this can be programmed into the system. On
complete occlusion, the rollers come to a stop, the out-
f low approaches zero, and the vacuum is at its highest
level (Figure 4).
Venturi Pump (Vacuum Based)
The venturi pump makes use of the venturi effect to cre-
ate a vacuum. The venturi effect creates a vacuum by the
f low of a f luid, typically air, over an opening. In many
phacoemulsification machines, this requires nitrogen
tanks or a self-contained air compressor. The vacuum
level is created within a rigid drainage cassette, to which
Figure 3 Compliant outflow tubing can collapse and cause the phaco aspiration tubing is connected. Since there is
surge during cataract surgery.
no milking of the aspiration line, the phaco tubing can
be made rigid with low compliance (Figure 5).
The advantage of the venturi pump is that it is able
a small change in the size of the phaco needle can result to create the preset vacuum level without occlusion of
in a very large change in the f low. Comparing 2 common the phaco needle tip. When the surgeon depresses the
size phaco needles, 0.9 mm (20 gauge) versus 1.1 mm foot pedal, the preset vacuum level is immediately cre-
(19 gauge), with all other factors equal it is surprising to ated, hence the term vacuum based. The venturi and other
see that the f low through the larger 1.1 mm needle is vacuum-based systems typically have the advantage of
more than twice that of the 0.9 mm needle. As the needle much faster rise time, the time required to build up
size decreases, the f low drops exponentially. the desired vacuum level with and without occlusion,
as well as the potential for much higher effective f low
rates within the eye. A disadvantage is that the outf low
Peristaltic and Venturi rate is variable and is determined by the vacuum level
created; the surgeon cannot directly set it.
Fluid Pumps
Two types of vacuum pumps are used in phacoemulsifi-
cation platforms: peristaltic and venturi. Although they
work in different ways, each has its advantages.
Peristaltic Pump (Flow Based)
The peristaltic pump uses rollers to compress the phaco-
emulsification outf low tubing in a peristaltic manner,
thereby creating f low and vacuum. The compression of
the rollers on the tubing with the rotation of the pump
physically moves f luid and creates a continuous “milk-
ing” action on the f luid column. The phaco machine can
directly control this f low level, hence the term flow based;
however, the preset vacuum level is only achieved once
there is occlusion of the outf low line, typically at the Figure 4 The peristaltic pump uses rollers to compress the
phaco needle tip with cataract material. phaco outflow tubing in a peristaltic manner, thereby creat-
As the occlusion happens, the vacuum builds, the roll- ing flow. The compression of the rollers on the tubing with
the rotation of the pump physically moves fluid and creates
ers slow down, and the outf low level decreases. Most
a continuous “milking” action on the fluid column.
manufacturers preprogram how the rollers slow down
4 Focal Points : Module 8, 2010
FPv28n08_0910.indd 4 7/23/10 1:30 PM
vacuum levels to achieve holding power as required in
phaco chop techniques.
The bottle height determines the inf low of f luid into
the eye. In order to help prevent surge, it is important to
keep the inf low of f luid at least as high as the outf low
of f luid at all times, because any excess inf low will pres-
surize the eye and leak from the incision until equilib-
rium is achieved. The inf low of f luid comes from only
1 source, the bottle of balanced salt solution, while the
outf low of f luid comes from 2 sources, the suction via
the phaco needle and the leakage from the incisions. If,
at any time, the outf low outstrips the inf low, the eye
will collapse and there is a high likelihood of posterior
capsule rupture. It is often advantageous to start with a
high bottle height to ensure a sufficient inf low of f luid,
Figure 5 The vacuum level is created within a rigid drainage and then to taper it downwards to minimize the poste-
cassette, to which the phaco aspiration tubing is connected. rior displacement of the lens-iris diaphragm due to the
Since there is no milking of the aspiration line, the phaco infusion pressure.
tubing can be made rigid with low compliance.
For the “phaco chop” method, the holding power of
the needle tip is important in order to fixate the nucleus
securely while using the chopper to disassemble the
Optimizing nucleus mechanically. This requires a relatively high vac-
uum, such as 200 to 250 mmHg with the 1.1 mm nee-
Phacoemulsification dle, or 300 to 400 mmHg with the 0.9 mm needle. Once
the nucleus has been broken into smaller fragments, the
Fluidic Settings peristaltic f low rate determines the speed at which the
fragments are attracted to the phaco tip, with a f low rate
The function of the phacoemulsification f luidics is to of 20 cc/min being very slow and 50 cc/min being very
balance the inf low and outf low of f luid in order to main- fast. During phaco chop, the surgeon can use the same
tain the working space, bring cataract material to the vacuum and f low rate settings for the entire nucleus
phaco tip, and prevent collapse of the eye. Optimizing removal procedure.
the phaco f luidic settings is crucial to maximizing effi- For divide-and-conquer phaco, there are 2 distinct
ciency and safety of phacoemulsification surgery. stages of nucleus removal: sculpting of the nucleus and
In order to optimize the phaco f luidic settings, it is quadrant removal. Different f luidic settings are required
important to match the machine parameters to the sur- for each. For grooving and sculpting of the nucleus, the
geon’s phaco technique. With a typical peristaltic phaco work is being done by the ultrasonic energy and thus the
machine platform, the most common type in the United f low and vacuum settings are quite low—just enough to
States, only a few parameters are adjustable. These aspirate the nuclear material removed from each for-
include needle size, bottle height, f low rate, and maxi- ward stroke of the phaco probe. A vacuum level of less
mum vacuum level. than 100 mmHg and a f low rate of less than 30 cc/min
The selection of phaco needle size is of great impor- are sufficient for this purpose. For quadrant removal, a
tance. The most common sizes are the smaller-bore moderate amount of holding power is required to bring
0.9‑mm needle and the larger-bore 1.1-mm needle. If the each quadrant into the phaco tip. Using a higher vac-
surgeon’s preference is a quicker procedure with rapid uum level of 200 to 300 mmHg and a f low rate of 30 to
nucleus removal, then the larger 1.1‑mm needle size 50 cc/min, depending on the needle size, is typically suf-
is desirable because it will give a significantly greater ficient for this purpose.
f low rate. If the surgeon prefers a slower but more con- With knowledge of the concepts behind the variables,
trolled procedure, then the smaller-bore 0.9-mm needle it is easy to tailor the f luidic settings to the surgeon
is more suited to that technique. The holding power of and technique. Understanding the concepts behind the
the phaco probe on to the cataract nucleus is related phaco f luidic settings is instrumental in optimizing the
to the vacuum level used as well as the surface area of parameters for increasing the efficiency and safety of the
occlusion. Using a larger phaco needle allows for lower surgeon’s phaco technique.
Focal Points : Module 8, 2010 5
FPv28n08_0910.indd 5 7/23/10 1:30 PM
Fundamentals The stroke of the phaco needle creates a mechani-
cal impact as the metal phaco needle hits the cataract
of Ultrasonic material. It also creates cavitation and implosion as a
microvoid is created just in front of the phaco needle.
Phacoemulsification A f luid and particle wave is propagated into the cata-
ract material and finally, heat is created as a by-product.
Power It is important to avoid choosing phaco power settings
that cause excessive heat build-up as this can burn the
The phacoemulsification ultrasound probe delivers cornea and damage the delicate ocular structures. Unre-
energy into the eye that is used to break up the cata- stricted f low through the surrounding irrigating sleeve
ract to facilitate emulsification and aspiration. It accom- is also very important, as the constant cooling effect of
plishes this by vibrating at a fixed frequency when balanced salt solution moving around the phaco probe
the foot pedal is depressed to position 3. To increase helps to prevent heat build-up.
the amount of ultrasound power, the machine simply During surgery, the phaco machine keeps track of
increases the stroke length of the probe. the average phaco power, given as a percentage of maxi-
Traditionally the probe delivers power only in a longi- mum, as well as the total time during which phaco ultra-
tudinal manner, with the phaco needle moving forward sonic power was delivered. The machine displays these
and back. Recent innovations in phaco technology also settings as “U/S AVE,” which stands for “ultrasound aver-
allow for the delivery of power through a lateral motion. age,” and “EPT,” which is “elapsed phaco time.” The total
Delivering ultrasound power through lateral motion can energy delivered into the eye is the product of the phaco
increase cutting efficiency by reducing repulsion of lens power multiplied by the time the power is on, known as
material. the absolute phaco time (APT). The phaco machine will
The 2 types of lateral motion in phacoemulsifica- automatically calculate the APT by multiplying the “U/S
tion are torsional, in which the phaco tip oscillates in AVE” by the “EPT,” so that the surgeon can compare the
a rotational manner along its primary axis, and trans- total ultrasonic energy delivered in different cases.
versal, where the phaco tip moves in an elliptical path. Delivering 15 seconds of 100% power is the same
Because of their types of motion, torsional works best energy as delivering 30 seconds of 50% power, or 60 sec-
with an angled phaco needle while transversal works onds of 25% power. For each of the 3 examples in Fig-
equally well with a straight or angled needle. Combin- ure 7, the APT is 15 seconds.
ing lateral motion phaco with traditional longitudinal It is important to use as little ultrasonic phaco energy
phacoemulsification can aid cutting efficiency, since the as possible during the cataract surgery. The ultrasonic
cataract material is emulsified in more than one direc- energy can damage the corneal endothelial cells, with
tion (Figure 6). excessive damage leading to corneal decompensation.
To decrease the APT maximally, the surgeon needs
to decrease the phaco time and/or the average phaco
power. The average phaco power can be decreased by
limiting the foot pedal depression in position 3 when
Figure 6 Longitudinal as well as rotational or elliptical move-
ment of the phaco needle may be used to emulsify cataract Figure 7 A maximal reduction in the absolute phaco time
material and facilitate aspiration. requires a reduction in both phaco time and phaco power.
6 Focal Points : Module 8, 2010
FPv28n08_0910.indd 6 7/23/10 1:30 PM
using a linear controlled power mode or by decreasing then gives small bursts of phaco power only when nec-
the maximum phaco power level on the machine. The essary. Because one can program these bursts of phaco
phaco time can be decreased by applying the ultrasonic power to be very short (as quick as a few milliseconds),
power only when cataract pieces are at the phaco tip and one can effectively give hundreds of tiny bursts and still
vacuum alone is insufficient to aspirate the piece. Addi- total less than 1 second of total phaco time. Because the
tionally, phaco time can be reduced by delivering shorter phaco foot pedal now controls the rest interval between
pulses or bursts of phaco power instead of continuous identical bursts, one does not have linear control of the
ultrasound power or by decreasing the duty cycle (the phaco power level. For this reason, it is important to use
ratio of the on:off pulses). This method of breaking up a lower phaco power setting when using burst mode as
the ultrasonic power into smaller packets of pulses and compared to pulse or continuous modes. When the foot
bursts is called phaco power modulation. pedal is maximally depressed, the rest interval between
bursts is zero and the phaco probe essentially delivers
Continuous, Pulse, and Burst continuous energy (Figure 8).
Phacoemulsification Modes
Hyper Settings for Power Modulation
The basic power settings are continuous, pulse, and
burst. In the continuous power setting, energy delivery The range of programmability of the pulse and burst
is continuous with variations in power, controlled by the phacoemulsification settings has expanded consider-
amount of foot pedal depression. ably. While previous generations of phaco platforms
In the pulse mode, the pulse power increases linearly had pulse rates of up to 20 pulses per second, the newer-
by how far down the foot pedal is depressed. The far- generation machines have the ability to deliver up to
ther it is depressed, the greater the power will be of each 120 pulses per second. Similarly, the older machines had
sequential pulse of energy. The defining feature of pulse burst widths as narrow as 30 milliseconds, while the new
mode is that after each pulse of energy delivered, there is platforms are able to deliver burst widths as fine as just
a period of time in which no energy is delivered between 4 milliseconds.
increasing pulses of energy, the “off” period. Alternating The advantage of this upgraded range of programma-
between equal “on” and “off” pulse times reduces heat bility is the smoothness and precision of power deliv-
and delivers half the energy into the eye. ery. With the standard settings in pulse mode, where
In burst mode, each burst has the same power but the each pulse is as long as each rest period, the pulse mode
interval between each burst decreases as the foot pedal can deliver good cutting power with half the energy of
is depressed. The farther the foot pedal is depressed, the
shorter the “off” period will be between each burst. As a
result, at maximum foot pedal depression, the bursts of
energy will become continuous delivery of energy.
In referring to modulations of phacoemulsification
power, the terms burst and pulse may seem similar, but
they refer to entirely different concepts. Surgeons are
used to the concept of “continuous” phacoemulsifica-
tion power that is delivered in a linear fashion: as the
phacoemulsification foot pedal is depressed, the power
level increases. “Pulse” mode simply gives the same
linear control of phacoemulsification power; however,
the energy is always delivered in pulses. “Burst” mode
defines a specific and identical “burst” of phacoemulsifi-
cation energy. As the foot pedal is depressed, these iden-
tical bursts of energy are delivered more rapidly, until
the interval of time between bursts is infinitely small. A Figure 8 “Continuous” phaco power is delivered in a linear
fashion. “Pulse” mode gives the same linear control of
key advantage of burst mode is that it allows the surgeon
phaco power, except that the power is delivered in pulses.
to titrate the rate of delivery of these tiny bursts, which
“Burst” mode defines a specific and identical “burst” of
can be as short as a few milliseconds. phaco power. As the foot pedal is depressed, identical
Burst mode allows a true phaco-assisted aspiration of bursts of power are delivered more rapidly, until the interval
the lens nucleus. The surgeon uses the vacuum and f lu- of time between bursts is infinitely small.
idics of the phaco machine to aspirate the cataract and
Focal Points : Module 8, 2010 7
FPv28n08_0910.indd 7 7/23/10 1:30 PM
continuous phaco power. The more pulses per second nucleus; however, this energy also can create significant
given, the smoother the power delivery will be—very heat. The jackhammer effect of ultrasound energy can
similar to serrations on a knife. cause repulsion of the nuclear fragments from the phaco
Power modulation using hyper settings also allows the tip. It is helpful to alternate periods of phacoemulsifica-
surgeon to reduce the total amount of energy released tion energy with rest periods that serve to achieve cool-
in the eye. For example, simply changing from continu- ing of the phaco needle and aspiration of the nuclear
ous phaco power to a hyper pulse rate of 100 pulses per fragments. If the surgeon changes the ratio of the on
second allows the surgeon to cut total energy delivery period, when ultrasound energy is delivered, to a shorter
in half. This halving of the ultrasound energy will result duration, then the surgeon can favor the aspiration and
in less endothelial cell damage, less heat production, cooling of the phaco needle over the heat generation and
clearer corneas, and sharper vision immediately post‑op. jackhammer repulsion effects of the ultrasound.
Surgeons who perform the divide-and-conquer method With the choice of a mode such as pulse mode, which
of nucleus phaco can switch to a hyper pulse mode and alternates phaco power pulses with periods of rest, the
immediately perform better surgery without a change default ratio is 50:50. This is called a 50% duty cycle, as
in technique. each complete cycle is composed of power on for 50% of
Note, however, that simply changing the number of the time, then power off for 50% of the time. This default
pulses per second alone does not change the amount ratio can be changed to alter the ratio of ultrasound
of energy delivered into the eye. Whether the surgeon energy to the rest interval. For example, 40% results in
gives 2 pulses per second or 8 pulses per second, the total 40 msec on, 60 msec off giving a ratio of 40:60. The sur-
energy, as represented by the green blocks (Figure 8) is the geon can then harness the benefits of a lower duty cycle,
same. The same applies when comparing 10 pulses per which results in longer cooling time for the phaco nee-
second to 100 pulses per second. Reduction in the energy dle, thus decreasing the amount of phaco energy deliv-
delivered is accomplished by decreasing the time that the ered to the eye. In addition, during the extended “off”
power is on by altering the ratio of the on:off pulses (Fig- time, no energy is delivered and nuclear fragments can
ure 9). The lower pulse rates tend to be better for emulsi- be easily aspirated (Figure 10).
fying nuclear fragments since there is a significant time When are higher or lower duty cycles preferred? The
interval between pulses for the fluidics to keep the cata- answer depends on the phase of surgery. For sculpting
ract piece attracted to the phaco needle. The higher pulse the nucleus, such as with the technique of divide-and-
rates tend to work better for sculpting or grooving the conquer, the surgeon needs to deliver sufficient energy
nucleus since the narrow time interval between pulses to be able to cut the grooves. This requires a duty cycle of
produces a smoother delivery of ultrasonic energy. about 40% to 60%. Once the surgeon has placed grooves
in the nucleus and has achieved cracking that results
Variable Duty Cycle in quadrants, a lower duty cycle can be used during the
Ultrasound energy creates helpful cavitation and
mechanical forces that are used to break up the cataract
Figure 9 If the duty cycle is held constant, simply increas- Figure 10 The total phaco energy delivered can be reduced
ing the pulses per second (PPS) does not decrease the total significantly by altering the “on-off” duty cycle.
phaco energy delivered.
8 Focal Points : Module 8, 2010
FPv28n08_0910.indd 8 7/23/10 1:30 PM
phaco-assisted aspiration of the quadrants. For this quad- optimize phaco fluid settings and modulate phaco power,
rant removal, a lower duty cycle of 20% to 40% can be especially with regard to pulse, burst and duty cycle, to
used since the principal force for aspiration is the f luid- improve proficiency and safety. A thorough knowledge
ics and not the ultrasound. of these features allows the surgeon to make refine-
Using the variable duty cycle programming allows the ments in phaco parameters in order to enhance cutting
surgeon to deliver just the right amount of ultrasound efficiency, reduce risks of thermal injury, improve “fol-
energy during each phase of surgery. The concept to lowability,” or encourage better chamber maintenance,
remember is that a higher duty cycle results in better depending on the specific techniques of the surgeon and
cutting power but increased heat generation and more the clinical challenges of an individual case. All of this
energy-related damage to the corneal endothelium. helps to make surgery safer, gentler and more success-
Using the lower duty cycle allows more f luidic aspira- ful for our patients.
tion of nuclear fragments while minimizing heat and
phaco power, resulting in clearer corneas immediately
after surgery. Clear corneas on postoperative day 1 make
for good visual acuity and very satisfied patients. Uday Devgan, MD, FACS, FRCS (Glasg) is in private
practice at Devgan Eye Surgery in Los Angeles, Beverly
Hills, and Newport Beach, California. Dr. Devgan is also
the chief of ophthalmology at Olive View–UCLA Medical
Conclusion Center and an associate clinical professor of ophthalmol-
ogy at the Jules Stein Eye Institute, UCLA School of Medi-
An understanding of phacoemulsification technology
cine, Los Angeles, California.
is of fundamental importance to the modern phaco
surgeon. Advances in technology allow the surgeon to
Focal Points : Module 8, 2010 9
FPv28n08_0910.indd 9 7/23/10 1:30 PM
Clinicians’Corner
Clinicians’ Corner provides additional viewpoints on 1. Discuss the relative advantages and disadvantages
of venturi-based and peristaltic phacoemulsifica-
the subject covered in this issue of Focal Points. Con- tion (phaco) systems as they pertain to a surgeon’s
level of experience.
sultants have been invited by the Editorial Review
Dr. Seibel: In one perspective, vacuum-based pumps,
Board to respond to questions posed by the Acade- such as a venturi system, are simpler than f low-based
systems, such as peristaltic pumps, in that they have but
my’s Practicing Ophthalmologists Advisory Committee a single f luidic parameter for the surgeon to adjust. The
surgeon commands only vacuum (mmHg) in a venturi
for Education. While the advisory committee reviews pump and clinically produces f low to the extent that
the aspiration port is open, and grip to the extent that it
the modules, consultants respond without reading the is occluded. The f low pump, by comparison, has at least
2 f luidic parameters (aspiration outf low in cc/minute
module or one another’s responses. – Ed. and vacuum limit in mmHg) as well as additional f low
modulations that may alter rates of pump speed change
with varying degrees of occlusion or vacuum load. This
relative difference in f luidic complexity would seem to
tip the scales in favor of a vacuum pump for less experi-
enced surgeons. However, vacuum pumps have a signif-
icant disadvantage of producing potentially dangerous
f low rates of 60 cc per minute or higher with typical
commanded vacuums of modern phaco techniques (250
to 450 mmHg). For this reason, a peristaltic pump may be
preferred by a less experienced surgeon (or a more expe-
rienced surgeon dealing with compromised anatomy) for
the ability to set a slower, gentler f low rate.
Dr. Serafano: The surgical requirements for successful
phacoemulsification are maintaining a stable anterior
chamber, attracting lens material to the tip, and holding
and emulsifying the lens material with minimum tur-
bulence. Technically this means minimum f luctuation
of IOP, minimizing f low while not occluded, and short
linear vacuum rise time.
Since venturi-based systems are vacuum based and
cannot generally set f low separately, IOP f luctuations in
the range from unobstructed f low to occlusion break are
much greater than with peristaltic systems. This means
that surgeons preferring the venturi system need a high
10 Focal Points : Module 8, 2010
FPv28n08_0910.indd 10 7/23/10 1:30 PM
level of experience in order to anticipate surge. Some stability. venturi systems require more irrigation inf low
surgeons use a venturi patch (mesh to filter particles) to compensate for inability to separately adjust AFR.
attached to the aspiration line to introduce resistance in Although this increased irrigation is necessary to main-
order to reduce surge. Peristaltic systems allow the sur- tain a stable chamber and minimize IOP f luctuations, it
geon to customize f low and vacuum separately to assure may lead to increased turbulence.
consistent and predictable venting. This should allow a If a surgeon prefers phaco chop, then the consid-
safer procedure for surgeons of any level of experience. eration is vacuum. The venturi system is perceived as
faster than a peristaltic system because a chop technique
2. Discuss in greater detail the relative advantages generally requires higher vacuum levels, and the ven-
and disadvantages of venturi and peristaltic phaco- turi system can access high vacuum levels very quickly.
emulsification systems as they pertain to the A peristaltic system allows for the setting of operating
method of cataract removal (“divide and conquer” range of vacuum and rise time, which can be adjusted
versus “phaco chop”). to the surgeon’s personal preference. The key difference
at higher vacuum levels is the management of occlusion
Dr. Seibel: Phaco chop methods involve higher vac-
break. The venturi user needs to anticipate the break and
uum levels and more occlusion of the aspiration port
thus modulate with the foot pedal, whereas the peristal-
as compared to the sculpting-intensive divide-and-con-
tic user is not burdened with this process.
quer methods. Vertical chop methods in particular may
require very high vacuum levels of 350 to 450 mmHg.
3. How are the settings adjusted to alter the “follow-
These higher vacuum levels can have f luidic liabilities in
ability” of nuclear pieces?
both pump types upon abrupt occlusion breaks: peristal-
tic pumps can have more propensity for postocclusion Dr. Seibel: Distal followability brings a fragment to the
surge, and venturi pumps can produce dangerously high phaco tip and is a function of pump f low into the aspi-
associated f low rates. Many newer peristaltic machines ration port; it is adjusted directly on a f low pump (aspir
allow considerable sophistication of programming to ation outf low parameter in cc/min) and indirectly on a
mitigate surge, including modulations to adjust pump vacuum pump by commanding a vacuum level in mmHg
acceleration rate and venting protocols. High-vacuum when the aspiration port is not occluded. Proximal fol-
tubing such as the Intrepid micro-coaxial system (Alcon, lowability refers to the efficiency with which carou-
Fort Worth, TX) can also blunt postocclusion surge. Ven- selling phaco aspiration takes place, with poor function
turi surgeons using phaco chop techniques may need to manifest by chattering of the cataract fragment on the
consciously reduce vacuum prior to an anticipated occlu- tip. Poor proximal followability is an indication of insuf-
sion break, such as for carouselling phacoaspiration of ficient attractive f luidic parameters (f low and vacuum)
chopped fragments after using a higher vacuum level and/or excessive repulsive forces (traditional longitudi-
for chopping. Such dynamic control can be facilitated by nal ultrasound).
dual linear pedal control (Bausch & Lomb, Rochester, NY; In addition to decreasing ultrasound power level,
Abbott Medical Optics [AMO], Santa Ana, CA). other modifications include various ultrasound modula-
tions such as hyperpulse, which differs from continuous
Dr. Serafano: If a surgeon prefers sculpting and quadrant
ultrasound by having varying amounts of “off” cycles
management, then there are 2 considerations. First, dur-
between “on” cycles in order to increase efficiency of
ing the nonocclusive sculpt phase, peristaltic pump sys-
followability by allowing nuclear fragments to re‑engage
tems allow for setting lower aspiration f low rates (AFR).
the aspiration port during “off “ cycles. Another modifi-
This results in less turbulence, thereby allowing greater
cation of traditional ultrasound is to augment or replace
retention of the ophthalmic viscosurgical device (OVD)
the traditional longitudinal vibration of the phaco nee-
to protect the endothelium. Second, during the preoc-
dle with a rotational (Alcon Ozil) or ellipsoidal (AMO
clusive and occlusive quadrant management phase, the
Signature) vibration that is less likely to repel a nuclear
peristaltic pump systems allow for setting a range of lin-
fragment. Fluidic modifications to enhance proximal
ear vacuum that should lead to safer anterior chamber
Focal Points : ModulE 8, 2010 11
FPv28n08_0910.indd 11 7/23/10 1:30 PM
Clinicians’Corner
followability include increasing f low rate (f low pump), Torsional movement allows emulsification to take place
increasing vacuum limit (f low pump), or increasing com- when the tip moves in each cutting direction, or 100%
manded vacuum level (vacuum pump). of the time, whereas longitudinal ultrasonic cuts only in
the forward stroke, or only 50% of the time.
Dr. Serafano: “Followability” is the surgeon’s term for
The advantage of torsional over transverse is that the
how readily the nuclear fragments are attracted to the
tip can be controlled separately in the x and y axis as
ultrasound tip. In peristaltic systems, this can be opti-
2 distinct motions (ie, longitudinal and torsional). The
mized by adjusting the AFR setting. AFR is the rate at
limitation of the transverse motion is that its movement
which f luid is removed from the anterior chamber. It
is along 1 plane only (cannot mix the x with the y axis
is expressed in milliliters per minute. Irrigation inf low
movements of the tip).
must be equal to, and potentially greater than, the sum
of the AFR plus incisional outf low to maintain a steady
5. Discuss settings for patients with a relatively soft
IOP and therefore a stable anterior chamber. In coax-
cataract, such as those with primarily a posterior
ial phaco, inf low entering through the infusion sleeve
subcapsular cataract in a younger patient.
ports creates a f luid current that helps bring nuclear
fragments into the phaco tip if the AFR is balanced for Dr. Seibel: Using phacodynamic principles (Phacodynam-
the surgeon’s technique. The peristaltic system allows ics, 4th ed, Thorofare, NJ: Slack; 2005), the surgeon ascer-
for the direct adjustments of the AFR, whereas most ven- tains the clinical task for each parameter for a given type
turi systems cannot accomplish this. Some venturi sys- of cataract at a given moment in surgery. Ultrasound
tems have introduced “pitch and yaw” to the foot pedal functions to mechanically disrupt lens material that
in order to allow for more control of vacuum and power. would otherwise be too rigid to deform sufficiently for
aspiration under a given vacuum load alone. Therefore,
4. Does either torsional or transverse movement offer in a soft cataract, only minimal amounts of ultrasound
advantage over the other for cataract surgery? energy are required in order to moderately reduce the
amount of f luidics required; 15% to 20% might be a
Dr. Seibel: Controversy exists concerning a blanket supe-
starting point, realizing that there is no industry stan-
riority of one modality over another, and whether either
dardization for phaco power. Vacuum is titrated to allow
is absolutely superior to traditional longitudinal ultra-
deformation and aspiration of the material. In these
sound that is modulated with hyperpulse. Using ultra-
cases, a value of about 150 mmHg is typically sufficient,
highspeed videography, Teruyuki Miyoshi elegantly
assuming augmentation by mild levels of ultrasound.
illustrated the enhanced proximal followability afforded
Flow functions to pull nuclear material into the tip and
by hyperpulsed longitudinal phaco. The best statement
aspirate out of the eye, and for softer nuclei, settings of
for this question would be the recommendation to avoid
20 cc to 25 cc per minute will often suffice. Given these
traditional longitudinal continuous ultrasound in virtu-
relatively moderate f luidic settings, a bottle height of
ally all applications in favor of ellipsoidal, torsional, or
95 cm should provide adequate chamber stability. Such
longitudinal ultrasound with hyperpulse.
settings are starting points, with adjustments made
Dr. Serafano: There are currently 3 movements avail- according to phacodynamic principles based on surgeon
able with phaco tips. First is the traditional longitudinal observations.
movement along one line (x axis) that all machines have
Dr. Serafano: Soft cataracts require less ultrasonic power.
available. Second is torsional movement, which is “side
This allows for “vacuum-assisted phaco.” Once hydrodis-
to side” (y axis). Third is transverse movement, which
section and hydrodelineation have been completed, vac-
closely resembles the longitudinal line motion, but it is
uum levels and aspiration f low rates can be increased
delivered at an angle to the tip shaft (x and z axis).
from normal levels. In order to maintain a steady IOP,
Torsional and transverse are meant to improve effi-
bottle height may have to be increased to balance the
ciency by eliminating or minimizing the repulsive force
increased AFR. Divide and quadrant management or
inherent in the forward stroke of longitudinal phaco.
12 Focal Points : Module 8, 2010
FPv28n08_0910.indd 12 7/23/10 1:30 PM
chop techniques are seldom effective in soft cataracts. induced astigmatism as compared to standard incision;
The soft cataract technique is essentially irrigation and more secure incision closure; and lower intraoperative
aspiration using the large bore of a phaco tip. f luid consumption due to improved f luid dynamics.
6. Discuss the advantages and disadvantages and fluid 7. What adjustments to the surgeon’s usual setting
dynamics for microincisional phacoemulsification. should be made in patients with pre-existing cor-
neal disease such as Fuchs corneal dystrophy?
Dr. Seibel: Advantages include a lower amplitude of
induced incisional astigmatism, as well as a more stable Dr. Seibel: Parameters should be adjusted to mini-
anterior chamber due to less incisional leakage, all other mize further trauma to already compromised corneal
things being equal (eg, rigidity of the infusion sleeve). endothelial cells. Ultrasound usage can be minimized
Originally, microincisional phaco involved a bimanual through more efficient modulations such as hyperpulse,
approach that had the disadvantage of requiring a modi- and by using more efficient occlusion type methods such
fication of technique and at least some learning curve. as chopping, and of course ultrasound should not be
The smaller incisions (typically 1.4 mm wide) required engaged when the tip is anterior to the iris plane. With
smaller-gauge instruments (20 to 23 gauge), and these regard to f luidics, anterior chamber turbulence should
often had difficulty in supplying sufficient infusion be minimized by decreasing the f low rate (either directly
inf low to mitigate against postocclusion surge with with a f low pump or indirectly with a vacuum pump)
higher vacuum levels. Newer coaxial microincisional and by minimizing chamber f luctuations by reducing
systems essentially eliminate the learning curve associ- postocclusion surges, by either raising bottle height,
ated with bimanual methodology but increase incisions reducing vacuum parameter, or dynamically reducing
up to 1.8 to 2.2 mm, depending on the platform, reduc- the commanded vacuum level (with dual linear pedal
ing induced astigmatism (as compared to traditional control) just prior to an occlusion break. Attempts can
19‑gauge phaco) to around 0.25 diopters. Adequate cham- also be made to keep the irrigation ports oriented in the
ber stability is achieved in these systems by restricting iris plane so as not to direct f luid f low with correspond-
outf low, such as with small-bore aspiration line tubing ing shear force directly against the corneal endothelium.
in the Intrepid system (Alcon), or a vacuum surge sup-
Dr. Serafano: Protection of the endothelium is the goal
pressor used in the Stellaris (Bausch & Lomb) platform.
in this situation. This is best achieved by low f low and
Dr. Serafano: I would like to define microincisional phaco low turbulence. Decreasing these parameters will assist
as a phaco incision of 2.4 mm or less. Since the total area in the retention of OVD and therefore endothelial protec-
for f luid exchange is reduced with smaller incisions, irri- tion. Low f low means to lower the bottle height, lower
gation may be reduced depending on the tip and sleeve aspiration f low rate and lower vacuum. Consider replac-
chosen by the surgeon. Therefore, a knowledgeable and ing OVD as needed and try to remove as much nucleus
matching selection of the aspiration and infusion com- as possible below the iris plane.
ponents is mandatory. Depending on component selec-
tion, to compensate for decreased irrigation, AFR and 8. Are there any adjustments to be made in a patient
vacuum levels may have to be reduced to balance f luidics with eyes that have long or extremely long axial
and prevent surge and IOP f luctuations. Some microin- lengths?
cisional ultrasound tips have been modified by slightly
Dr. Seibel: These patients have a greater likelihood of
f laring the port of the tip to maintain holding power and
having weak zonules and/or an excessively deep ante-
decreasing the outer diameter of the shaft to allow for
rior chamber, setting these patients up for lens-iris dia-
more irrigation to f low between the tip and sleeve into
phragm retropulsion syndrome in which the complete
the anterior chamber. The main advantages of micro-
pupil perimeter seals against the anterior lens capsule.
coaxial phacoemulsification are the improved patient
Surgeons would historically have to compensate by low-
outcomes, which include lower postoperative surgically
ering the infusion bottle, which would compromise
Focal Points : ModulE 8, 2010 13
FPv28n08_0910.indd 13 7/23/10 1:30 PM
Clinicians’Corner
surge control in an already unbalanced anterior cham- with large f luctuations in anterior chamber depth is an
ber. Robert Cionni reported on a novel technique to dis- eye having an IOP of 5 mmHg or less after glaucoma fil-
rupt this syndrome and restore normal anterior chamber ter surgery. In eyes with excessive filters, the anterior
depth and architecture by mechanically separating the chamber will not react predictably with normal phaco
iris from the lens, with the phaco/irrigation/aspiration f luidics. In all of these situations, lower the initial f low
tip (in pedal position 1) or a second instrument. These parameters in order to decrease anterior chamber f luctu-
longer eyes often have large anterior segments, and sur- ations. After the initial entry into the anterior chamber
geons must be particularly vigilant about appropriate and establishment of f low, the parameters may be slowly
sizing of the capsulorrhexis; direct measuring is advised, increased to find the proper f luidic balance.
such as with the Rhexis Ruler (MST, Redmond, WA).
Dr. Serafano: Eyes with long axial lengths and postvit-
rectomized eyes do not have normal intracameral resis- Barry S. Seibel, MD, is a practicing ophthalmologist at
tance to support the lens/iris diaphragm when irrigation Seibel Vision Surgery in Los Angeles, California. He is
increases pressure in the anterior chamber. Eyes with also a clinical assistant professor of ophthalmology at
normal axial lengths and formed vitreous exert a resis- the University of California, Los Angeles, Geffen School
tance to support the lens/iris diaphragm and help keep of Medicine.
the anterior chamber stable with standard phaco set- Donald N. Serafano, MD, is a practicing ophthalmolo-
tings. If this support is missing or low, normal fluid phaco gist at Complete Eye Care Association Incorporated in
parameters in the anterior chamber can push the lens/ Los Alamitos, California. He is also an associate clinical
iris diaphragm posterior and cause large f luctuations professor at the University of Southern California.
in IOP and anterior chamber depth. Another situation
Suggested Reading Related Academy Materials
Benjamin L, Little BC, Packard R, Packer M. Phacoemulsifica- Surgery for cataract. In: Lens and Cataract. Basic and Clinical
tion 1. Basic techniques. In: The Video Atlas of Eye Surgery. Science Course, Section 11, 2010–2011. Chapter 8 includes
Surrey, UK: Eye Movies Ltd; 2005. discussion of phacoemulsification, including ultrasonics
terminology, vacuum terminology, phaco instrumentation,
Packard R. Understanding phacodynamics. J Cataract Refract
phaco power delivery, irrigation, aspiration, and advances in
Surg. 2010;36:876–877.
energy delivery; full discussion of a basic phaco procedure;
Seibel BS. Phacodynamics: Mastering the Tools and Techniques of and advances in energy delivery.
Phacoemulsification Surgery, 4th ed, Thorofare, NJ: Slack; 2005.
14 Focal Points : Module 8, 2010 029032C
FPv28n08_0910.indd 14 7/23/10 1:30 PM
Potrebbero piacerti anche
- Posterior Polar Cataract Management: My Approach: 2022, #1Da EverandPosterior Polar Cataract Management: My Approach: 2022, #1Nessuna valutazione finora
- BCSC1718 S11Documento17 pagineBCSC1718 S11ZackychunNessuna valutazione finora
- Clinical Optics: Basic and Clinical Science CourseDocumento18 pagineClinical Optics: Basic and Clinical Science CourseIlham SamodraNessuna valutazione finora
- Corneal Collagen Crosslinking PDFDocumento18 pagineCorneal Collagen Crosslinking PDFpepe_garces_2Nessuna valutazione finora
- The Art of PhacoemulsificationDocumento544 pagineThe Art of PhacoemulsificationDaniel Fernández Gajardo100% (3)
- Recent Advances in Laser Refractive SurgeryDocumento24 pagineRecent Advances in Laser Refractive SurgeryKPJConferenceNessuna valutazione finora
- Retinal Applications of Swept Source Optical Coherence Tomography (OCT) and Optical Coherence Tomography Angiography (OCTA)Documento52 pagineRetinal Applications of Swept Source Optical Coherence Tomography (OCT) and Optical Coherence Tomography Angiography (OCTA)zhu zhuotingNessuna valutazione finora
- Kuhn 2016Documento548 pagineKuhn 2016Karan Kumarswamy100% (1)
- Continue: Stallard's Eye Surgery PDFDocumento3 pagineContinue: Stallard's Eye Surgery PDFCod Mobile100% (1)
- Basic of Operating MicroscopeDocumento48 pagineBasic of Operating MicroscopeNiloy BasakNessuna valutazione finora
- Phaco Fundamentals For The Beginning Phaco Surgeon PDFDocumento29 paginePhaco Fundamentals For The Beginning Phaco Surgeon PDFJosé Eduardo Zaragoza LópezNessuna valutazione finora
- Anesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFDocumento11 pagineAnesthesia Management of Ophthalmic Surgery in Geriatric Patients PDFtiaraleshaNessuna valutazione finora
- RyanDocumento2.486 pagineRyanlunafranca22Nessuna valutazione finora
- Phacodynamics and Phacoemulsification PDFDocumento4 paginePhacodynamics and Phacoemulsification PDFpriti089100% (1)
- Atlas of Cataract SurgeryDocumento196 pagineAtlas of Cataract SurgeryDaniel Fernández Gajardo100% (3)
- Phaco Machine, Fluidics and DynamicsDocumento32 paginePhaco Machine, Fluidics and DynamicsPrathibha M ChachadiNessuna valutazione finora
- Phacoemulsification Agarwal 2007Documento174 paginePhacoemulsification Agarwal 2007Kai SanNessuna valutazione finora
- 1 5053054235202027721Documento175 pagine1 5053054235202027721andifa aziz satriawanNessuna valutazione finora
- Retinal AnatomyDocumento86 pagineRetinal AnatomySean ScogginsNessuna valutazione finora
- PhacoemulsificationDocumento54 paginePhacoemulsificationIshita Kinra100% (1)
- Vol 2 Retinal AtlasDocumento252 pagineVol 2 Retinal AtlasDra. Mitzy Torres - RetinólogaNessuna valutazione finora
- CORNEA Vision2020 DR - RajarathnaDocumento7 pagineCORNEA Vision2020 DR - Rajarathnaadi100% (1)
- Pentacam Guideline 3rd 0218 KDocumento220 paginePentacam Guideline 3rd 0218 KHarshit RajputNessuna valutazione finora
- (Essentials in Ophthalmology) Ahmad A. Aref, Rohit Varma (Eds.) - Advanced Glaucoma Surgery-Springer International Publishing (2015)Documento140 pagine(Essentials in Ophthalmology) Ahmad A. Aref, Rohit Varma (Eds.) - Advanced Glaucoma Surgery-Springer International Publishing (2015)Inna Bujor100% (1)
- MASTER'S GUIDE TO Manual SICSDocumento192 pagineMASTER'S GUIDE TO Manual SICSAndri SaputraNessuna valutazione finora
- The Phaco MachineDocumento18 pagineThe Phaco MachineBMT100% (2)
- Cataract Surgery - Asian Eye HospitalDocumento12 pagineCataract Surgery - Asian Eye HospitalKankariaNessuna valutazione finora
- Morphologic Alterations On Posterior Iris-Claw Intraocular Lenses After Traumatic DisenclavationDocumento5 pagineMorphologic Alterations On Posterior Iris-Claw Intraocular Lenses After Traumatic DisenclavationYanjinlkham Kh100% (1)
- ZEISS AngioPlex Clinical Compendium US 31 025 0070IDocumento4 pagineZEISS AngioPlex Clinical Compendium US 31 025 0070Idarkspawn69Nessuna valutazione finora
- PENTACAM 12 StepsDocumento4 paginePENTACAM 12 StepsRaúl Plasencia SaliniNessuna valutazione finora
- Do's and Dont's in Phaco Surgery Text and AtlasDocumento320 pagineDo's and Dont's in Phaco Surgery Text and AtlassalmanNessuna valutazione finora
- Medical Retina 2017Documento96 pagineMedical Retina 2017Carlos Ortega100% (1)
- Kanski S Clinical Ophthalmology A Systematic.20Documento1 paginaKanski S Clinical Ophthalmology A Systematic.20dyiah ayuNessuna valutazione finora
- LASIK EmergenciesDocumento187 pagineLASIK EmergenciesMike LadhaNessuna valutazione finora
- Phaco Machine Setting PDFDocumento7 paginePhaco Machine Setting PDFAlim SumonNessuna valutazione finora
- Advances in Vitreoretinal SurgeryDocumento63 pagineAdvances in Vitreoretinal Surgerybharti100% (6)
- The Evolution of The Ophthalmic Surgical MicroscopeDocumento33 pagineThe Evolution of The Ophthalmic Surgical MicroscopeSai Naga Sri HarshaNessuna valutazione finora
- Fundamentals and Principles of Ophthalmology: Basic and Clinical Science CourseDocumento4 pagineFundamentals and Principles of Ophthalmology: Basic and Clinical Science Coursenuryusri99Nessuna valutazione finora
- Ocular TraumaDocumento67 pagineOcular TraumaRenita Siwi M WNessuna valutazione finora
- Pediatric Oculoplastic Surgery 2018 James KatowitzDocumento973 paginePediatric Oculoplastic Surgery 2018 James KatowitzJesús Rios LondoñoNessuna valutazione finora
- Guide To Phacoemulsification - Harbans LalDocumento58 pagineGuide To Phacoemulsification - Harbans Lalसुनन्दन भट्ट100% (1)
- Corneal Topography - From Theory To PracticeDocumento404 pagineCorneal Topography - From Theory To PracticeTage50% (2)
- Ophthalmology CurriculumDocumento71 pagineOphthalmology CurriculumEdoga Chima EmmanuelNessuna valutazione finora
- Deh P1yDocumento90 pagineDeh P1yPaulo ChagasNessuna valutazione finora
- Viva and Osce Exams in Ophthalmology A Revision Study Guide 1st Ed 9783030430627 9783030430634 CompressDocumento392 pagineViva and Osce Exams in Ophthalmology A Revision Study Guide 1st Ed 9783030430627 9783030430634 CompressstingbeesparvNessuna valutazione finora
- 0210 IOL HandbookDocumento15 pagine0210 IOL HandbookHombre69Nessuna valutazione finora
- Manual Small Incision Cataract Surgery - HendersonDocumento185 pagineManual Small Incision Cataract Surgery - HendersonRajesh Gupta100% (1)
- Atlas of Refractive Surgery PDFDocumento235 pagineAtlas of Refractive Surgery PDFcongNessuna valutazione finora
- PERIMETRY Introduction GuideDocumento70 paginePERIMETRY Introduction GuideDana Andreea Popescu100% (1)
- Femto Laser in OphthalmologyDocumento11 pagineFemto Laser in Ophthalmologylycan007Nessuna valutazione finora
- 2017 Book PhacoemulsificationCataractSurDocumento223 pagine2017 Book PhacoemulsificationCataractSurPande Gustiana100% (1)
- International Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)Documento4 pagineInternational Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)zaidoonys1Nessuna valutazione finora
- Asia Pacific Glaucoma Guidelines Second EditionDocumento118 pagineAsia Pacific Glaucoma Guidelines Second EditiondrquanNessuna valutazione finora
- VISALIS 500 Family and Visalis 100 From ZEISS: Accessory CatalogDocumento20 pagineVISALIS 500 Family and Visalis 100 From ZEISS: Accessory CatalogAdriana Marcela Briñez LugoNessuna valutazione finora
- Okap Samson Uveitis PDFDocumento12 pagineOkap Samson Uveitis PDFsharu4291Nessuna valutazione finora
- Opinioes Exames Ebo e IcoDocumento8 pagineOpinioes Exames Ebo e Icoapi-3595301060% (1)
- Devgan. Phaco Fundamentals. BookDocumento29 pagineDevgan. Phaco Fundamentals. Bookjuanjorlopez100% (3)
- AAO GoniosDocumento43 pagineAAO GoniosmeliabudiNessuna valutazione finora
- Opmilumera700 en 32 010 0053ii-1Documento16 pagineOpmilumera700 en 32 010 0053ii-1rolandNessuna valutazione finora
- Epithelial Tissues MnemonicsDocumento3 pagineEpithelial Tissues MnemonicsDaniel AyanlekeNessuna valutazione finora
- 2011 Surgery IIDocumento67 pagine2011 Surgery IIamruthkiranbabuji100% (1)
- A Safe and Effective Two-Step Tract Dilation Technique in Totally Ultrasound-Guided Percutaneous NephrolithotomyDocumento7 pagineA Safe and Effective Two-Step Tract Dilation Technique in Totally Ultrasound-Guided Percutaneous NephrolithotomyPhuoc LeNessuna valutazione finora
- Case Study of Gallbladder Polyp Final OneDocumento24 pagineCase Study of Gallbladder Polyp Final OneMayer AlsaberNessuna valutazione finora
- Retinopathy of Prematurity - HandoutDocumento2 pagineRetinopathy of Prematurity - Handoutmusara87Nessuna valutazione finora
- Tibio-Tarsal Luxation and Its Management in A Dog: Ayyappan, S., M. Shiju Simon, B. C. Das and R. Suresh KumarDocumento4 pagineTibio-Tarsal Luxation and Its Management in A Dog: Ayyappan, S., M. Shiju Simon, B. C. Das and R. Suresh KumarEnnur NufianNessuna valutazione finora
- CystsDocumento180 pagineCystsDinesh YadavNessuna valutazione finora
- La HipfracDocumento3 pagineLa HipfracdanishvuNessuna valutazione finora
- Dr. Praveen PresentationDocumento63 pagineDr. Praveen PresentationPraveen KumarNessuna valutazione finora
- Graded RecitationDocumento2 pagineGraded RecitationAngel GarciaNessuna valutazione finora
- CghsDocumento6 pagineCghsFACTS- WORLDNessuna valutazione finora
- Update ACLSDocumento64 pagineUpdate ACLSVenansius Ratno KurniawanNessuna valutazione finora
- Synopsis in The Management of Urinary Incontinence - 2017Documento102 pagineSynopsis in The Management of Urinary Incontinence - 2017Dennise IlieNessuna valutazione finora
- Abstract Book PVSM2021 FinalDocumento374 pagineAbstract Book PVSM2021 FinalnitaNessuna valutazione finora
- Avaliação Objetiva Da Dificuldade de Deglutição Pós-Operatória Através Da Ultrassonografia em Pacientes Submetidos À Tireoidectomia PDFDocumento8 pagineAvaliação Objetiva Da Dificuldade de Deglutição Pós-Operatória Através Da Ultrassonografia em Pacientes Submetidos À Tireoidectomia PDFGiovanna MartinsNessuna valutazione finora
- CSF Catalogue enDocumento76 pagineCSF Catalogue enHarshitShuklaNessuna valutazione finora
- Scaling & Root PlaningDocumento73 pagineScaling & Root PlaningDon Juan100% (2)
- International Journal of Surgery Case ReportsDocumento5 pagineInternational Journal of Surgery Case Reportscarlos javier andraadeNessuna valutazione finora
- Final Guidance Document For Donor HaemovigilanceDocumento60 pagineFinal Guidance Document For Donor HaemovigilanceShiva ChandrakarNessuna valutazione finora
- Recent Developments in MISDocumento4 pagineRecent Developments in MIStingfenggeNessuna valutazione finora
- Roccuzzo Et Al-2012-Clinical Oral Implants ResearchDocumento9 pagineRoccuzzo Et Al-2012-Clinical Oral Implants ResearchAndré MoreiraNessuna valutazione finora
- CataractsDocumento47 pagineCataractsNrs Sani Sule MashiNessuna valutazione finora
- CPAP SlidesDocumento52 pagineCPAP SlidesAnusha Verghese100% (1)
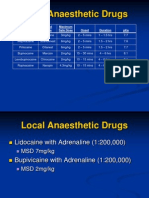
- Local Anaesthetic Drugs 3 Power Point PresentationDocumento30 pagineLocal Anaesthetic Drugs 3 Power Point PresentationJosef Cefai100% (1)
- Changes To Resus Insert For 33rd EditionsDocumento2 pagineChanges To Resus Insert For 33rd EditionsAsmadi MusaNessuna valutazione finora
- Certification Institute: Identify BradycardiaDocumento1 paginaCertification Institute: Identify BradycardiaRicky SetiawanNessuna valutazione finora
- PortforlioDocumento33 paginePortforlioShayne EsponillaNessuna valutazione finora
- Evaluation Thyroid NoduleDocumento35 pagineEvaluation Thyroid Nodulehendra nuraminNessuna valutazione finora
- Post TestDocumento11 paginePost Testoomculun100% (6)
- Nur 146 RleDocumento47 pagineNur 146 RleKeziah Marie Chua Santa-AnaNessuna valutazione finora
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 4.5 su 5 stelle4.5/5 (82)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (254)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (60)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (5)
- To Explain the World: The Discovery of Modern ScienceDa EverandTo Explain the World: The Discovery of Modern ScienceValutazione: 3.5 su 5 stelle3.5/5 (51)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedValutazione: 4 su 5 stelle4/5 (61)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (46)