Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pancreatic Function & Gastrointestinal Function
Caricato da
Mara Gane0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
18 visualizzazioni5 pagineTitolo originale
pancreas.docx
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
18 visualizzazioni5 paginePancreatic Function & Gastrointestinal Function
Caricato da
Mara GaneCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 5
Islet cells secrete at least 4 hormones
Pancreatic Function & into blood: insulin, glucagon, gastrin, &
Gastrointestinal Function somatostatin.
Introduction • Exocrine Component
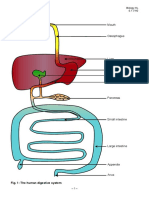
• Gastrointestinal (GI) System Produces digestive fluid rich with
enzymes in acinar cells, which line
Comprises mouth, esophagus, stomach, pancreas & are connected by small
small & large intestines ducts
Digestion: process by which starches, Secretes about 1.5–2 L/day of fluid into
proteins, lipids, & nucleic acids are ducts that empty into duodenum
degraded to molecules for absorption &
use in body • Diagram of the pancreas and its relationship to
the duodenum
• Abdominal structures of the alimentary tract
Pancreatic Fluid
• protein- rich,clear, colorless, and watery
• with an alkaline pH that can reach up to 8.3.
Pancreas • The bicarbonate and chloride concentrations
vary reciprocally
Large gland involved in digestive process, but
lies outside of GI system • same concentrations of potassium and sodium
Located behind peritoneal cavity across upper as serum
abdomen at level of 1st & 2nd lumbar
Pancreatic enzymes
vertebrae, 1–2 inches above umbilicus
Composed of both endocrine & exocrine tissue (1) the proteolytic trypsin,
Liver and pancreas- digestion enzymes chymotrypsin,
pancreas is only second in size to the liver elastase,
collagenase,
weighing about 70–105 g. It
leucine
Physiology of Pancreatic Function aminopeptidase,
and some
• Endocrine Component carboxypeptidases
(2) lipid-digesting lipase and lecithinase
Smaller than exocrine component
enzymes
Consists of islets of Langerhans: well- (3) carbohydrate- Pancreatic amylase
delineated, spherical or ovoid clusters splitting
composed of at least 4 different cell
types
Secretin and cholecystokinin • Tumors in Beta cells
• Secretin is responsible for the production of • Hyperinsulinism
bicarbonate-rich and, therefore, alkaline
• Gastrinomas
pancreatic fluid, which protects the lining of the
intestine from damage. • Pancreatic cell tumors, which overproduce
gastrin,
• Secretin is synthesized in response to the acidic
contents of the stomach reaching the • they cause Zöllinger-Ellison syndrome and can
duodenum. be duodenal in origin.
• It can also affect gastrin activity in the stomach. • watery diarrhea, recurring peptic ulcer, and
significant gastric hypersecretion and
• Secretin and cholecystokinin
hyperacidity
• CCK, formerly called pancreozymin, in the
Pancreatitis
presence of fats or amino acids in the
duodenum, is produced by the cells of the Inflammation of pancreas
intestinal mucosa
Caused by autodigestion of pancreas as a result
• Responsible for release of enzymes from the of reflux of bile or duodenal contents into
acinar cells by the pancreas into the pancreatic pancreatic duct
fluid.
Pathologic changes include acute edema,
Diseases of the Pancreas cellular infiltration, & intrahepatic &
extrahepatic pancreatic fat necrosis.
Cystic Fibrosis
• Results
fibrocystic disease of the pancreas and
mucoviscidosis All 3 conditions can result in severely
diminished pancreatic exocrine
An inherited autosomal recessive disorder,
function, compromising digestion &
characterized by dysfunction of mucous &
absorption.
exocrine glands throughout body
Malabsorption syndrome: abdominal
Manifestations: intestinal obstruction
bloating & discomfort, frequent passage
(newborn), excessive pulmonary infections
of bulky, malodorous feces, & weight
(childhood), pancreatogenous malabsorption
loss
(adults)
Causes ducts & acini to dilate & convert into
small cysts filled with mucus, preventing Tests of Pancreatic Function
secretions from reaching duodenum
1. Secretin/CCK Test
Pancreatic Carcinoma
Direct determination of exocrine
4th most frequent form of fatal cancer; 5-year secretory capacity of pancreas
survival rate <5%
Involves intubation of duodenum
Most tumors arise as adenocarcinomas of without contamination by gastric fluid,
ductal epithelium. which would neutralize any bicarbonate
pain is a prominent feature of the disease. Performed after a 6-hour or overnight
fast
jaundice, weight loss, anorexia, and nausea
Pancreatic secretion is stimulated by
Islet cell tumors
secretin followed by CCK.
Secretions are collected for 30, 60, or In adults, levels above 80 mmol/L are
80 minutes after administration of diagnostic.
stimulants.
Sweat collection involves pilocarpine
pH, secretory rate, enzyme activities, administration by iontophoresis.
bicarbonate are measured.
4. Serum Enzymes
2. Fecal Fat Analysis
Amylase
• Fecal lipids are derived from 4 sources:
Enzyme most commonly used
1. Unabsorbed ingested lipids for detecting pancreatic disease
2. Lipids excreted into intestine Particularly useful in diagnosis
of acute pancreatitis
3. Cells shed into intestine
Serum levels increase within
4. Metabolism of intestinal bacteria
hours of onset of disease, peak
• Qualitative screening: Sudan staining in about 24 hours, & return to
normal within 3–5 days.
Neutral fats & other lipids stain
yellow-orange to red with i. Renal clearance of amylase is
Sudan III because dye is more useful measure for detecting
soluble in lipid. minor or intermittent increases
in serum concentrations.
Increases in fats & undigested
meat fibers indicate Lipase
steatorrhea of pancreatic
i. Some physicians consider lipase
origin.
more sensitive than amylase.
• Quantitative screening: Gravimetric
method
Entire fecal specimen is
emulsified with water. Physiology and Biochemistry of Gastric Secretion
An aliquot is acidified to Stimuli Triggering Gastric Secretion
convert all fatty acid soaps to
free fatty acids. Neurologic impulses from brain transmitted by
vagal nerves
Then most lipids are extracted
into petroleum ether & ethanol. Distention of stomach with food or fluid
After evaporation of organic Contact of protein breakdown products with
solvents, lipid residue is gastric mucosa
weighed. Hormone gastrin (most potent)
3. Sweat Electrolyte Determinations Inhibitors of Gastric Secretion
Measurement of sodium & chloride High gastric acidity, which decreases release of
concentration in sweat is most useful gastrin by G cells
test for diagnosis of cystic fibrosis.
Gastric inhibitory polypeptide, secreted by K
In children, levels of sweat sodium & cells
chloride above 60 mmol/L are
diagnostic. Vasoactive intestinal polypeptide, produced by
H cells
Clinical Aspects of Gastric Analysis Materials enter jejunum & ileum, where 1.5
L of secretion is added; only ~1.5 L of fluid
Purposes of Gastric Analysis
material reaches cecum.
o To detect hypersecretion characteristic of
Mucosal folds, villi, & microvilli in 20-foot-
Zollinger-Ellison syndrome
long small intestine allow massive
o Occasionally, to evaluate pernicious anemia in absorption.
adults
Large intestine absorbs water & stores feces
o Rarely, to aid in determining type of surgical before defecation.
procedure required for ulcer treatment
Stimulus for Gastric Analysis
Clinicopathologic Aspects of Intestinal Function
Pentagastrin is now used as stimulus to
Diseases That Cause Malabsorption
gastric secretion.
Tropical & nontropical or celiac sprue
Tests of Gastric Function
Whipple’s disease
1. Measuring Gastric Acid in Basal, Maximal
Secretory Tests Crohn’s disease
After overnight fast, performed as 1-hour basal Primary intestinal lymphoma
test followed by 1-hour stimulated test after
pentagastrin administration Small intestinal resection
In stimulated-secretion specimens, ability of Intestinal lymphangiectasia
stomach to secrete against a hydrogen ion Ischemia
gradient is determined by measuring pH.
Amyloidosis
Gastrin response to secretin stimulation may be
used to investigate patients with mildly Giardiasis
elevated serum gastrin levels.
In this test, pure porcine secretin is injected &
Tests of Intestinal Function
gastric levels are collected at 5-minute intervals
for next 30 minutes. 1. Lactose Tolerance Test
2. Plasma Gastrin Disaccharidases, lactase, & sucrase are
produced by mucosal cells of small
1. Invaluable in diagnosing Zollinger-
intestine.
Ellison syndrome
Acquired deficiencies of lactase are
Intestinal Physiology
common in adults.
Digestion
Affected patients experience abdominal
Predominantly a function of small intestine discomfort, cramps, & diarrhea after
ingesting milk or milk products.
Necessary for absorption to occur for most
large molecules About 10–20% of whites & 75% of
African Americans are affected.
Process:
Lactose tolerance test established this
7–10 L of ingested water & food & secretion diagnosis but is subject to many false-
from salivary glands, stomach, pancreas, & positive & false-negative results.
biliary tract enters duodenum.
It has been replaced largely by Negative nitrogen balance, decreased
hydrogen breath testing. serum proteins & albumin
2. D-Xylose Absorption Test Deficiencies of fat-soluble vitamins A, D,
E, & K
D-Xylose: a pentose sugar ordinarily not
present in blood Deficiencies of vitamin-K dependent
coagulation factors
Pentose sugars are absorbed unaltered
in proximal small intestine, do not Anemia, diminished iron & calcium
require intervention of pancreatic lytic absorption
enzymes.
Decreased sodium & potassium levels,
Ability to absorb D-xylose helps dehydration
differentiate malabsorption of intestinal
Decreased/flat blood concentration
etiology from that of exocrine
curves in glucose, lactose, & sucrose
pancreatic insufficiency.
tolerance tests
Process
i. After overnight fast, patient
voids & drinks D-xylose
solution.
ii. Patient drinks equivalent
amount of water during next
hour.
iii. Urine is collected for 5 hours
after ingestion; blood specimen
is collected at 2 hours.
3. Serum Carotenoids
Various yellow to orange or purple
pigments widely distributed in animal
tissue
Synthesized by many plants & impart a
yellow color to some vegetables & fruits
Major carotenoids in human serum are
lycopene, xanthophyll, & beta-carotene
(precursor of vitamin A).
Are fat-soluble & are absorbed in small
intestine with lipids
Malabsorption of lipids results in serum
concentration of carotenoids lower
than reference range of 50–250 mg/dL.
4. Other Tests of Intestinal Malabsorption
Diminished appetite & dietary intake
Body wasting or cachexia
Potrebbero piacerti anche
- Bio 212 HW 1 KeyDocumento6 pagineBio 212 HW 1 KeyMitter JonesNessuna valutazione finora
- Healthy Pancreas, Healthy You. Part 3. How to Improve the Exocrine Pancreatic Function, Postpone Pancreatic Deterioration, and Heal Digestive (Pancreatic) DisordersDa EverandHealthy Pancreas, Healthy You. Part 3. How to Improve the Exocrine Pancreatic Function, Postpone Pancreatic Deterioration, and Heal Digestive (Pancreatic) DisordersValutazione: 5 su 5 stelle5/5 (1)
- 2011 A Level H2 Biology P3 AnsDocumento6 pagine2011 A Level H2 Biology P3 AnsjoannetzyNessuna valutazione finora
- GASTROSYSP1Documento11 pagineGASTROSYSP1merlinalra.lucero.mnlNessuna valutazione finora
- GI Review BulletsDocumento19 pagineGI Review Bulletsjanet_alexisNessuna valutazione finora
- Mechanism of DigestionDocumento3 pagineMechanism of DigestionDev BhutamwarNessuna valutazione finora
- D 2 Digestion: - Necessary For Interval Meal. - Nerves and Hormones Ensure - Necessary For Energy ConsumptionDocumento13 pagineD 2 Digestion: - Necessary For Interval Meal. - Nerves and Hormones Ensure - Necessary For Energy ConsumptionSaumya ThakkerNessuna valutazione finora
- Disorders of The Gastrointestinal System and Endocrine SystemDocumento7 pagineDisorders of The Gastrointestinal System and Endocrine SystemNadia AbdurasidNessuna valutazione finora
- Fecal AnalysisDocumento23 pagineFecal AnalysisBabylene MamauagNessuna valutazione finora
- Disorders of The Alimentary TractDocumento25 pagineDisorders of The Alimentary Tract수안현100% (1)
- Small Intestine 1Documento4 pagineSmall Intestine 1Ha Jae kyeongNessuna valutazione finora
- NCM 116 W1 Reading HandoutDocumento13 pagineNCM 116 W1 Reading Handoutriza sarmientoNessuna valutazione finora
- Digestive System PathophysiologyDocumento16 pagineDigestive System PathophysiologyCamryn NewellNessuna valutazione finora
- DigestDocumento84 pagineDigestBella FebrianNessuna valutazione finora
- Lecture 23Documento43 pagineLecture 23sara shloulNessuna valutazione finora
- Digestive Physiology: Movement of MaterialsDocumento14 pagineDigestive Physiology: Movement of MaterialsJãçk SparrowNessuna valutazione finora
- Presentation 05 Human DigestionDocumento45 paginePresentation 05 Human DigestionCarl (Carl)Nessuna valutazione finora
- Presentation 05 Human DigestionDocumento40 paginePresentation 05 Human DigestionCarl (Carl)Nessuna valutazione finora
- Medtech Git Upper and LowerDocumento72 pagineMedtech Git Upper and LowerBabe YamonganNessuna valutazione finora
- Sistem Pencernaan d3 KepDocumento56 pagineSistem Pencernaan d3 KepSura MaduNessuna valutazione finora
- Intestinal Phase of Digestion and AbsorptionDocumento9 pagineIntestinal Phase of Digestion and AbsorptionRand ELABEDNessuna valutazione finora
- L 9. Physiology & Disorders of StomachDocumento52 pagineL 9. Physiology & Disorders of Stomachsjfk1416Nessuna valutazione finora
- Hepatobiliary TransDocumento14 pagineHepatobiliary TransEricson CandelariaNessuna valutazione finora
- Medical School Notes On Pancreatic IssuesDocumento26 pagineMedical School Notes On Pancreatic IssuesDeji KajiNessuna valutazione finora
- 0.digestive, Absorptive & Microbiological ImbalanceDocumento73 pagine0.digestive, Absorptive & Microbiological ImbalanceMuhammad Ricky Julian AdhetiaNessuna valutazione finora
- DigestionDocumento28 pagineDigestionParasakthi MNessuna valutazione finora
- Digestion WiwiDocumento23 pagineDigestion WiwiSCE1-0622 Amni Insyirah Binti Mohd NasarudinNessuna valutazione finora
- Name: (Class: 3EB Chapter 5: Nutrition in AnimalsDocumento10 pagineName: (Class: 3EB Chapter 5: Nutrition in Animalsjanling82Nessuna valutazione finora
- Digestive SystemDocumento49 pagineDigestive SystemDaniel WakaWakaNessuna valutazione finora
- Small Intestine and PancreasDocumento52 pagineSmall Intestine and PancreasLutfi AuliaNessuna valutazione finora
- DigestiDocumento56 pagineDigestiStephanie Putri FonatabaNessuna valutazione finora
- MS PrelimsDocumento50 pagineMS PrelimsDhawell AnnNessuna valutazione finora
- 1 - Adult Gastrointestinal DisorderDocumento17 pagine1 - Adult Gastrointestinal DisorderNica EnriquezNessuna valutazione finora
- Gastro NotesDocumento11 pagineGastro NotesMonica JubaneNessuna valutazione finora
- Digestive SystemDocumento78 pagineDigestive SystemBerrak AydınNessuna valutazione finora
- Fisiologi Traktus DigestivusDocumento39 pagineFisiologi Traktus DigestivusdrhendyjuniorNessuna valutazione finora
- Digestion and Absorption By-Dr. Suntia Saxena Part 2Documento41 pagineDigestion and Absorption By-Dr. Suntia Saxena Part 2Divya AgarawalNessuna valutazione finora
- Pancreatic Function and SecretionDocumento35 paginePancreatic Function and Secretionmus zaharaNessuna valutazione finora
- IB HL Biology Notes: DigestionDocumento9 pagineIB HL Biology Notes: DigestionayushfmNessuna valutazione finora
- Protein Metabolism: by Dr. Mustafa Kahtan Al-BayatyDocumento37 pagineProtein Metabolism: by Dr. Mustafa Kahtan Al-BayatyIraqiNessuna valutazione finora
- Digestivesystem3 3Documento13 pagineDigestivesystem3 3vvNessuna valutazione finora
- Model Answers: Chapter 9 Nutrition and The Human Digestive SystemDocumento4 pagineModel Answers: Chapter 9 Nutrition and The Human Digestive SystemLEE NGIE FONG -Nessuna valutazione finora
- Lec1 Sem4 GITWK1 7 20140320Documento9 pagineLec1 Sem4 GITWK1 7 20140320Uloko ChristopherNessuna valutazione finora
- Physiology, Lecture 8, GIT 2 (Stomach) (Slides)Documento24 paginePhysiology, Lecture 8, GIT 2 (Stomach) (Slides)Ali Al-Qudsi100% (2)
- Sistem Pencernaan Dan Gatah PencernaanDocumento53 pagineSistem Pencernaan Dan Gatah PencernaanLaila NrzntNessuna valutazione finora
- Physiology of Digestion 1Documento55 paginePhysiology of Digestion 1dicksonsamboNessuna valutazione finora
- Small Intestine: Prof Anura WeerasingehDocumento22 pagineSmall Intestine: Prof Anura WeerasingehDilshan Anthony FernandoNessuna valutazione finora
- Colon Targeting DDS - NDDocumento66 pagineColon Targeting DDS - NDneha_dand1591Nessuna valutazione finora
- Draft 203 Gi TractDocumento7 pagineDraft 203 Gi TractMahadi Hasan KhanNessuna valutazione finora
- Day 1 Lecture - GI and NutritionDocumento46 pagineDay 1 Lecture - GI and NutritionRemej SilutgamNessuna valutazione finora
- Class Xi - Digestion and AbsorptionDocumento38 pagineClass Xi - Digestion and AbsorptionketakiNessuna valutazione finora
- Digestion-Food Is BrokenDocumento32 pagineDigestion-Food Is Brokenaerell manuelNessuna valutazione finora
- Fi DioDocumento74 pagineFi DioAlicia NataNessuna valutazione finora
- GIT Physiology Stomach & Small IntestineDocumento49 pagineGIT Physiology Stomach & Small IntestineDinalNessuna valutazione finora
- Nutrition in Human, NoteDocumento7 pagineNutrition in Human, NoteMaheen Farhan VII-G-BNessuna valutazione finora
- GIT صيدلهphysiologyDocumento38 pagineGIT صيدلهphysiologyAbdo HaiderNessuna valutazione finora
- Gastric Juice AnalysisDocumento6 pagineGastric Juice Analysismaynard pascualNessuna valutazione finora
- Fisiologi USUS HALUSDocumento28 pagineFisiologi USUS HALUSSarah AmaniNessuna valutazione finora
- Problem 2 - GI TractDocumento30 pagineProblem 2 - GI Tractfahmi rosyadiNessuna valutazione finora
- FecalysisDocumento7 pagineFecalysisMiki NishiharaNessuna valutazione finora
- PancreatitisDocumento2 paginePancreatitisJelica ConsultadoNessuna valutazione finora
- Nutrition 2021Documento147 pagineNutrition 2021Noel ManyiseNessuna valutazione finora
- Mark Scheme: Double Award Science BiologyDocumento9 pagineMark Scheme: Double Award Science BiologyDaniel LoughreyNessuna valutazione finora
- A Ciência Da Esgrima: Implicações Da Performance e Prevenção de LesõesDocumento18 pagineA Ciência Da Esgrima: Implicações Da Performance e Prevenção de LesõesDaniel GonçalvesNessuna valutazione finora
- Practice Test 2 1st Sem 2013Documento11 paginePractice Test 2 1st Sem 2013Isabel Barredo Del MundoNessuna valutazione finora
- LSM1101 Enzyme2Documento40 pagineLSM1101 Enzyme2givena2ndchanceNessuna valutazione finora
- Chap001 Test Bank Tank PDFDocumento45 pagineChap001 Test Bank Tank PDFHeraNessuna valutazione finora
- DGCA Human Performance & LimitationsDocumento6 pagineDGCA Human Performance & Limitationsabdur rahim100% (1)
- Brain Gym ExercisesDocumento9 pagineBrain Gym ExercisesMuza RasidiNessuna valutazione finora
- Sleep Phylogeny & OntogenyDocumento7 pagineSleep Phylogeny & OntogenyVivian PNessuna valutazione finora
- I. Clinical Summary A. General Data ProfileDocumento8 pagineI. Clinical Summary A. General Data ProfileDayan CabrigaNessuna valutazione finora
- Biology Notes: Cie IgcseDocumento64 pagineBiology Notes: Cie Igcsehamza96Nessuna valutazione finora
- Planning Monitoring Training For Team SportsDocumento52 paginePlanning Monitoring Training For Team SportsSoccerCTC100% (1)
- CVDocumento1 paginaCVapi-377129715Nessuna valutazione finora
- Neuromuscular Taping For The Upper LimbDocumento4 pagineNeuromuscular Taping For The Upper LimbFayza RihastaraNessuna valutazione finora
- Science 9th Chapter 5 Cell Biology NotesDocumento4 pagineScience 9th Chapter 5 Cell Biology NotesavanishNessuna valutazione finora
- Lung Structure - BioNinjaDocumento2 pagineLung Structure - BioNinjaDaniel WalshNessuna valutazione finora
- Atika School-5172016 - Biology Form 2Documento14 pagineAtika School-5172016 - Biology Form 2DenisNessuna valutazione finora
- Biology Nervous SystemDocumento5 pagineBiology Nervous SystemFatima PueblaNessuna valutazione finora
- Test Bank Exam 3Documento81 pagineTest Bank Exam 3Sajjad AhmadNessuna valutazione finora
- Mirror TracingDocumento8 pagineMirror TracingMichael CamusNessuna valutazione finora
- Muscles of MasticationDocumento50 pagineMuscles of MasticationKaran AroraNessuna valutazione finora
- Effects of Soaking On Yield and Quality of Agarwood OilDocumento8 pagineEffects of Soaking On Yield and Quality of Agarwood OilNilamdeen Mohamed ZamilNessuna valutazione finora
- Nursing Care PlanDocumento22 pagineNursing Care PlanjamNessuna valutazione finora
- Hawassa University Daye Campus Plant PhysiologyDocumento170 pagineHawassa University Daye Campus Plant PhysiologySekste MaludaNessuna valutazione finora
- 29 Lab Tech. (MLT)Documento17 pagine29 Lab Tech. (MLT)Anjali JoshiNessuna valutazione finora
- IB Biology HL SyllabusDocumento9 pagineIB Biology HL SyllabusjessicaNessuna valutazione finora
- Bio 130 Chapter 4 NotesDocumento12 pagineBio 130 Chapter 4 Notesgilissa100% (1)
- Fascia of The Head & NeckDocumento8 pagineFascia of The Head & NeckMahesh Jung KhadkaNessuna valutazione finora
- 07 Lecture 1Documento111 pagine07 Lecture 1Obieda NaseefNessuna valutazione finora