Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Yes To Suctioning
Caricato da
Monica BorjaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Yes To Suctioning
Caricato da
Monica BorjaCopyright:
Formati disponibili
Suctioning of Newborn Neonates
Clinical question: Does routine oropharyngeal/nasopharyngeal suctioning of newborn infants'
airways compared to no suction have an effect on mortality and morbidity with and without
meconium‐stained amniotic fluid?
Background
The birth of a baby is one of life's most wondrous moments. Few experiences compare to this
event. Newborn babies have amazing abilities. Yet they are dependent on others for feeding,
warmth, and comfort. The transition from fetus to newborn involves the clearing of lung fluid
and expansion of the lungs with air. While airway oro/nasopharyngeal suctioning can be
successful in clearing the airway immediately after birth.
Respiratory diseases are the chief reason for admission of premature neonates to
NICUs. Maintenance of breathing and patency of airway is the main objective in premature
infant care. Due to low consciousness level of neonates and weakness of their respiratory
muscles, efficient removal of secretion could not happen by coughing. Therefore, intubated
patients need to be suctioned, to prevent airway obstruction, atelectasis and pulmonary
infections.
Oro/nasopharyngeal suction is a method used to clear secretions from the oropharynx
or nasopharynx, or both, through the application of negative pressure via a suction cathete or
bulb syringe (Waltman 2004). Negative pressure is used to clear secretions from the mouth,
nose or pharynx while attempting to avoid trauma to the mucosa. If oro/nasopharyngeal
suction of term infants is required, the Australian Resuscitation Council recommends using a
large bore suction catheter (10 to 12 F), passed no more than 5 cm from the lips, with suction
applied for only a few seconds (ARC 2010). The negative pressure used to remove secretions
should not exceed 100 mmHg (13 kPa, 133 cmH2O, 1.9 pounds per square inch (psi)) (ARC
2010). Oro/nasopharyngeal suction can be performed before the delivery of the infant's
shoulders (intrapartum) (Vain 2004) or following vaginal birth (Gungor 2005) or caesarean
section (postpartum) of the infant (Gungor 2006). Traditionally, oro/nasopharyngeal suctioning
at birth has been used routinely to remove fluids in vigorous infants at birth.
Endotracheal suctioning in intubated newborns undergoing Mechanical Ventilation is a
procedure that is routinely performed by physiotherapists, doctors, nurses, and also by nursing
technicians in Brazil as a component of the resuscitation procedure and bronchial hygiene
therapy. The goal is to maintain airway patency and facilitate ventilation and oxygenation.
However, this technique has specific indications and adverse effects. Proper standardization,
clear indications for use and definitions of the procedure all serve to minimize complications.
Endotracheal suctioning is an important element of care for newborns admitted to the NICU
because most of these patients require invasive MV and repeated and frequent suctioning for
the removal of tracheal secretions. According to the American Association of Respiratory Care
(AARC), proper suctioning in intubated individuals improves gas exchange and respiratory
sounds; decreases airway resistance and peak inspiratory pressure of the ventilator; improves
dynamic compliance; increases the TV release when in limited pressure ventilation mode; and
improves arterial blood gas and oxygen saturation (SpO2) values. However, many institutions
attempt to maintain airway patency in intubated individuals by adopting protocols that include
the routine use of endotracheal suctioning without evaluating whether the procedure is
necessary. These protocols are primarily based on the care ritual than on evidence of the
clinical need for suctioning.
All of the studies included in this review described the technique as mandatory that it should be
performed whenever necessary because the accumulation of tracheobronchial secretions may
impair ventilation and oxygenation; lead to ETT occlusion, atelectasis and increased respiratory
work; and predispose the individual to pulmonary infection. However, one of the most
controversial issues regarding endotracheal suctioning in neonates is the precise time and
frequency at which the technique should be performed on intubated individuals.
According to the AARC and Evidence-based guideline for suctioning the intubated neonate and
infant, the procedure is safer when certain variables are monitored before, during and after it is
performed. Moreover, the Center for Disease Control and Prevention standards for invasive
procedures must be respected during the procedure, the procedure must be conducted by at
least two professionals, a maximum of three probe insertions should be performed, with a
return to the ventilator between suctionings.
Potrebbero piacerti anche
- Naso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringDocumento12 pagineNaso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringmeisygraniaNessuna valutazione finora
- Care of Newborn On Respiratory SupportDocumento40 pagineCare of Newborn On Respiratory SupportsyedNessuna valutazione finora
- Endotracheal SuctionDocumento11 pagineEndotracheal SuctionKeshav Singhmaar AryaNessuna valutazione finora
- Suction Document UpdatedDocumento6 pagineSuction Document UpdatedMonica BorjaNessuna valutazione finora
- Airway Management - StatPearls - NCBI BookshelfDocumento7 pagineAirway Management - StatPearls - NCBI BookshelfClarithq LengguNessuna valutazione finora
- Adult NasalDocumento14 pagineAdult NasalillirpohnimNessuna valutazione finora
- Advances in Emergent Airway Management in PediatricsDocumento19 pagineAdvances in Emergent Airway Management in PediatricsLuis Miguel VillanuevaNessuna valutazione finora
- Basic Airway Management in AdultsDocumento7 pagineBasic Airway Management in AdultsBereket temesgenNessuna valutazione finora
- Skills Laboratory: Manual Book Airway ManagementDocumento25 pagineSkills Laboratory: Manual Book Airway ManagementAlif MusemNessuna valutazione finora
- Module: Newborn Infant Suctioning: Learning Material 4Documento8 pagineModule: Newborn Infant Suctioning: Learning Material 4Farah Jelimae BagniNessuna valutazione finora
- Skills Training Manual BookDocumento19 pagineSkills Training Manual BookMuhammad SawalNessuna valutazione finora
- MODEL OF PRACTICE TsaarDocumento6 pagineMODEL OF PRACTICE TsaarCrystal Ann TadiamonNessuna valutazione finora
- Newborn Priorities in The First Days of LifeDocumento12 pagineNewborn Priorities in The First Days of LifeJoanna Bee Rose MagyawiNessuna valutazione finora
- Basic Airway ManagementDocumento24 pagineBasic Airway ManagementFELIPE MEDINANessuna valutazione finora
- ANZCOR Guideline 13.4 - Airway Management and Mask Ventilation of The NewbornDocumento18 pagineANZCOR Guideline 13.4 - Airway Management and Mask Ventilation of The NewbornEssam HassanNessuna valutazione finora
- Neonatal Tracheostomy - JonathanWalsh 2018Documento12 pagineNeonatal Tracheostomy - JonathanWalsh 2018Ismael Erazo AstudilloNessuna valutazione finora
- Airway Clearance Techniques and Hyperinflation Therapy Walsh Chapter 12Documento25 pagineAirway Clearance Techniques and Hyperinflation Therapy Walsh Chapter 12Dennis Páez Torres100% (2)
- AiwaryManagement 1Documento72 pagineAiwaryManagement 1Giselle EstoquiaNessuna valutazione finora
- Pediatrics StridorDocumento13 paginePediatrics StridorEmaNessuna valutazione finora
- Volume-Targeted Ventilation 2021Documento17 pagineVolume-Targeted Ventilation 2021Vladimir FloresNessuna valutazione finora
- Advances in Emergent Airway Management in PediatricsDocumento19 pagineAdvances in Emergent Airway Management in PediatricsJpmspoonNessuna valutazione finora
- CPAPDocumento11 pagineCPAPpreeti19987100% (1)
- Niv in Pediatric Patients - Book - GarciaDocumento62 pagineNiv in Pediatric Patients - Book - GarciaMary ElizabethNessuna valutazione finora
- LaprascopicDocumento6 pagineLaprascopicarhimNessuna valutazione finora
- CHest Physio For NeonatesDocumento7 pagineCHest Physio For Neonateschri23Nessuna valutazione finora
- Neonatos Guias 2010Documento3 pagineNeonatos Guias 2010minessotNessuna valutazione finora
- Basic Airway Management in Adults - UpToDateDocumento28 pagineBasic Airway Management in Adults - UpToDateGia Villavicencio BoniniNessuna valutazione finora
- SuctioningDocumento7 pagineSuctioningKat AlaNessuna valutazione finora
- Adult and Paediatric Oral/nasal-Pharyngeal SuctioningDocumento13 pagineAdult and Paediatric Oral/nasal-Pharyngeal SuctioningRuby Dela RamaNessuna valutazione finora
- EMERGENCY MEDICINE - Basic - Airway - Management - PrintableDocumento8 pagineEMERGENCY MEDICINE - Basic - Airway - Management - PrintableMedic DestinationNessuna valutazione finora
- Care of The Ventilated ChildDocumento5 pagineCare of The Ventilated ChildBrahadheeswaran KannanNessuna valutazione finora
- Role of PhysiotherapyDocumento23 pagineRole of PhysiotherapyVikas ChaitanyaNessuna valutazione finora
- Children: The Respiratory Management of The Extreme Preterm in The Delivery RoomDocumento21 pagineChildren: The Respiratory Management of The Extreme Preterm in The Delivery RoomRhea Kathleen MejiaNessuna valutazione finora
- The Case Against Newborn Suctioning: Evidence-Based MidwiferyDocumento3 pagineThe Case Against Newborn Suctioning: Evidence-Based Midwifery77nurseynurseNessuna valutazione finora
- Children's Community Nursing Team - SOP 12 - Suctioning - Oral & NasopharyngealDocumento7 pagineChildren's Community Nursing Team - SOP 12 - Suctioning - Oral & NasopharyngealMeldaNessuna valutazione finora
- Inserting An NG TubeDocumento67 pagineInserting An NG TubeBalan Andrei MihaiNessuna valutazione finora
- Neonatal ResuscitationDocumento15 pagineNeonatal ResuscitationAmruta GadeNessuna valutazione finora
- Airway and The NurseDocumento7 pagineAirway and The NursecarmenbuleandraNessuna valutazione finora
- Intjprevmed6133-2704195 004504Documento6 pagineIntjprevmed6133-2704195 004504Ade HabibieNessuna valutazione finora
- Airway ManagementDocumento11 pagineAirway Managementmegayani santosoNessuna valutazione finora
- Respiratory Disorders 2.2Documento74 pagineRespiratory Disorders 2.2Deenjane Nishi IgnacioNessuna valutazione finora
- Transient Tachypnea of The Newborn OutlineDocumento7 pagineTransient Tachypnea of The Newborn OutlineMarceline GarciaNessuna valutazione finora
- An Overview of EMS Pediatric Airway Management: Oleh SYAHYUNI SALEH 10542054213Documento13 pagineAn Overview of EMS Pediatric Airway Management: Oleh SYAHYUNI SALEH 10542054213syahyuniNessuna valutazione finora
- Respiratory Distress Syndrome (Iniego Carlo Jay)Documento9 pagineRespiratory Distress Syndrome (Iniego Carlo Jay)Carlojay IniegoNessuna valutazione finora
- NEJM VICM Viewers ChoiceDocumento19 pagineNEJM VICM Viewers ChoiceAnonymous cQWavnNessuna valutazione finora
- Airway Manegement Clinic NaDocumento14 pagineAirway Manegement Clinic Naflor_barrancoNessuna valutazione finora
- Wa0001Documento10 pagineWa0001rini sundariNessuna valutazione finora
- Chest PhysioDocumento6 pagineChest PhysioGoha BashaNessuna valutazione finora
- Acute Stridor in ChildrenDocumento6 pagineAcute Stridor in Childrenmob3Nessuna valutazione finora
- Complicaciones en El PreterminoDocumento4 pagineComplicaciones en El PreterminonadisjaviNessuna valutazione finora
- Ear, Nose and Throat EmergenciesDocumento3 pagineEar, Nose and Throat Emergenciesfmta100% (1)
- Meconium Aspiration SyndromeDocumento4 pagineMeconium Aspiration SyndromeGwEn LimNessuna valutazione finora
- Newborn ResuscitationDocumento7 pagineNewborn ResuscitationYwagar YwagarNessuna valutazione finora
- Paediatric Anaesthetic EquipmentDocumento4 paginePaediatric Anaesthetic Equipmentapi-142637023Nessuna valutazione finora
- Newborn Respiratory Disorders PDFDocumento10 pagineNewborn Respiratory Disorders PDFMax RodriguezNessuna valutazione finora
- SuctioningDocumento13 pagineSuctioningAmanda ScarletNessuna valutazione finora
- Cleft PalateDocumento16 pagineCleft PalateAnu Priya GopuNessuna valutazione finora
- PIIS1744165X23000677Documento10 paginePIIS1744165X23000677crislatorreferNessuna valutazione finora
- 2 Upper Airway Disorders PDFDocumento33 pagine2 Upper Airway Disorders PDFMonica BorjaNessuna valutazione finora
- JUNDocumento1 paginaJUNMonica BorjaNessuna valutazione finora
- AIDS-v 2Documento11 pagineAIDS-v 2Monica BorjaNessuna valutazione finora
- Final MicroparaDocumento5 pagineFinal MicroparaMonica BorjaNessuna valutazione finora
- Inequality in Maternal and Newborn CareDocumento2 pagineInequality in Maternal and Newborn CareMonica BorjaNessuna valutazione finora
- GuideqinbioethicsDocumento1 paginaGuideqinbioethicsMonica BorjaNessuna valutazione finora
- Understanding SelfDocumento4 pagineUnderstanding SelfMonica BorjaNessuna valutazione finora
- Understanding SelfDocumento4 pagineUnderstanding SelfMonica BorjaNessuna valutazione finora
- Learning Paper: Submitted By: Monica L. BorjaDocumento6 pagineLearning Paper: Submitted By: Monica L. BorjaMonica BorjaNessuna valutazione finora
- Learning Paper: Submitted By: Monica L. BorjaDocumento6 pagineLearning Paper: Submitted By: Monica L. BorjaMonica BorjaNessuna valutazione finora
- Plan and Preparation of Selected Therapeutic DietDocumento1 paginaPlan and Preparation of Selected Therapeutic DietMonica BorjaNessuna valutazione finora
- Teratogens and CHDDocumento5 pagineTeratogens and CHDMonica BorjaNessuna valutazione finora
- Ascites PresentationDocumento19 pagineAscites PresentationDanielle FosterNessuna valutazione finora
- Primary Health Care Notes Health What Is Illness and Causes of Illness?Documento22 paginePrimary Health Care Notes Health What Is Illness and Causes of Illness?Nano KaNessuna valutazione finora
- Benign Paratesticlar Cyst - A Mysterical FindingDocumento2 pagineBenign Paratesticlar Cyst - A Mysterical FindingInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Current Cancer Treatment - Novel Beyond Conventional ApproachesDocumento826 pagineCurrent Cancer Treatment - Novel Beyond Conventional Approacheselenac67100% (1)
- Anger: Realized By: Supervised byDocumento15 pagineAnger: Realized By: Supervised byChahinaz Frid-ZahraouiNessuna valutazione finora
- DA Sistemik TerapiDocumento11 pagineDA Sistemik TerapiariyatiNessuna valutazione finora
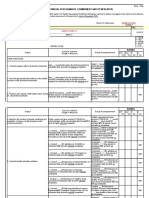
- Individual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledDocumento12 pagineIndividual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledTiffanny Diane Agbayani RuedasNessuna valutazione finora
- Bladder IrrigationDocumento19 pagineBladder IrrigationDwight Kristian CruzNessuna valutazione finora
- RestorilDocumento1 paginaRestorilKatie McPeek100% (1)
- Orthopedic InstrumentsDocumento7 pagineOrthopedic InstrumentsRonnie CanteroNessuna valutazione finora
- History of Nursing and The Development of The ProfessionDocumento4 pagineHistory of Nursing and The Development of The Professionastraia celesteNessuna valutazione finora
- SterilizationDocumento6 pagineSterilizationIndranath ChakrabortyNessuna valutazione finora
- HCM Treatment Italy Ammirati2016Documento13 pagineHCM Treatment Italy Ammirati2016xy manNessuna valutazione finora
- 321 E Lesson 4Documento21 pagine321 E Lesson 4Novia eka PutriNessuna valutazione finora
- Parasite 1Documento22 pagineParasite 1OnSolomonNessuna valutazione finora
- LamaDocumento3 pagineLamarockyNessuna valutazione finora
- Neurodegenerative DiseasesDocumento2 pagineNeurodegenerative DiseasesBerniceTanNessuna valutazione finora
- An Overview of Methods Used For Estimation of Time Since Death PDFDocumento12 pagineAn Overview of Methods Used For Estimation of Time Since Death PDFFajar SodiqiNessuna valutazione finora
- Python Ieee Projects 2021 - 22 JPDocumento3 paginePython Ieee Projects 2021 - 22 JPWebsoft Tech-HydNessuna valutazione finora
- Labor Law 1 Work Disability CasesDocumento108 pagineLabor Law 1 Work Disability CasesAlexis ArejolaNessuna valutazione finora
- Urinary Disorders 2Documento19 pagineUrinary Disorders 2ula mdiNessuna valutazione finora
- Occupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiDocumento99 pagineOccupational Health in Indonesia: Astrid Sulistomo Dep. of Community Medicine FmuiDea MaharaniNessuna valutazione finora
- Aioh Position Paper DPM jdk2gdDocumento26 pagineAioh Position Paper DPM jdk2gdRichardNessuna valutazione finora
- 3 Pocket Size-CriminalisticsDocumento77 pagine3 Pocket Size-CriminalisticsCriminology Criminology CriminologyNessuna valutazione finora
- English XIIDocumento12 pagineEnglish XIIdanielNessuna valutazione finora
- Basic Principles of Blending: Selecting Essential OilsDocumento3 pagineBasic Principles of Blending: Selecting Essential OilsRullya WindyaNessuna valutazione finora
- Urtica Urens William Boericke Cyrus Maxwell Bogar Adolf Zur Lippe John Henry ClarkeDocumento9 pagineUrtica Urens William Boericke Cyrus Maxwell Bogar Adolf Zur Lippe John Henry ClarkeShah FaisalNessuna valutazione finora
- MCQ ChoDocumento31 pagineMCQ Choامجد حسين جواد كاظمNessuna valutazione finora
- Mineral Nutrition Contributes To Plant Disease and Pest ResistanceDocumento5 pagineMineral Nutrition Contributes To Plant Disease and Pest ResistanceHectorSHNessuna valutazione finora
- 302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingDocumento2 pagine302 PpJ. Grayson, Freedom From Obsessive Compulsive Disorder A Personalized Recovery Program For LivingMohammad Shoyyad L IkhsanNessuna valutazione finora
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (393)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nessuna valutazione finora
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDa EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingValutazione: 4 su 5 stelle4/5 (1138)