Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Psoriasis Carries An Increased Risk of Venous Thromboembolism: A Danish Nationwide Cohort Study
Caricato da
Anonymous 1bEPjKTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Psoriasis Carries An Increased Risk of Venous Thromboembolism: A Danish Nationwide Cohort Study
Caricato da
Anonymous 1bEPjKCopyright:
Formati disponibili
Psoriasis Carries an Increased Risk of Venous
Thromboembolism: A Danish Nationwide Cohort Study
Ole Ahlehoff1*, Gunnar Hilmar Gislason1, Jesper Lindhardsen1, Mette Gitz Charlot1, Casper Haslund
Jørgensen1, Jonas Bjerring Olesen1, Ditte-Marie Bretler1, Lone Skov2,3, Christian Torp-Pedersen1,3, Peter
Riis Hansen1
1 Department of Cardiology, Copenhagen University Hospital Gentofte, Hellerup, Denmark, 2 Department of Dermatology, Copenhagen University Hospital Gentofte,
Hellerup, Denmark, 3 Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark
Abstract
Background: Psoriasis is an immunoinflammatory disease associated with cardiovascular risk factors, atherothrombotic
events, and hypercoagulability. Venous thromboembolism (VTE) is potentially lethal and shares risk factors with psoriasis,
but the risk of VTE associated with psoriasis is unknown. The present study investigated the potential association between
psoriasis and VTE.
Methods and Findings: Information from nationwide prospectively recorded registers of hospitalization, drug dispensing
from pharmacies, socio-economic data, and causes of death was linked on an individual level. In an unselected nationwide
cohort, we used multivariate Poisson regression models controlling for age, gender, comorbidity, concomitant medication,
socio-economic data, and calendar year, to assess the risk of VTE associated with psoriasis. A total of 35,138 patients with
mild and 3,526 patients with severe psoriasis were identified and compared with 4,126,075 controls. Patients with psoriasis
had higher incidence rates per 1000 person-years of VTE than controls (1.29, 1.92, and 3.20 for controls, mild psoriasis, and
severe psoriasis, respectively). The rate ratio (RR) of VTE was elevated in all patients with psoriasis with RR 1.35 (95%
confidence interval [CI] 1.21–1.49) and RR 2.06 (CI 1.63–2.61) for mild and severe psoriasis, respectively. Exclusion of patients
with malignancies, and censoring of patients undergoing surgery did not alter the results.
Conclusion: This nationwide cohort study indicates that patients with psoriasis are at increased risk of VTE. The risk was
highest in young patients with severe psoriasis. Physicians should be aware that patients with psoriasis may be at increased
risk of both venous and arterial thromboembolic events.
Citation: Ahlehoff O, Gislason GH, Lindhardsen J, Charlot MG, Jørgensen CH, et al. (2011) Psoriasis Carries an Increased Risk of Venous Thromboembolism: A
Danish Nationwide Cohort Study. PLoS ONE 6(3): e18125. doi:10.1371/journal.pone.0018125
Editor: Stefan Kiechl, Innsbruck Medical University, Austria
Received December 14, 2010; Accepted February 21, 2011; Published March 25, 2011
Copyright: ß 2011 Ahlehoff et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The study was supported by the Department of Cardiology, Copenhagen University Hospital Gentofte. The funders had no role in study design, data
collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: olahha01@geh.regionh.dk
Introduction in a cohort study based on nationwide prospectively recorded
registers with the underlying hypothesis that patients with psoriasis
Psoriasis is a prevalent chronic immunoinflammatory disease carry an increased risk of VTE.
affecting approximately 2% of the population [1,2]. It is associated
with cardiovascular risk factors, atherothrombotic events, and Methods
markers of hypercoagulability, including platelet activation and
hyperhomocysteinemia [3–15]. Venous thromboembolism (VTE), Ethics
i.e., deep venous thrombosis and pulmonary embolism, is This study was approved by The Danish Data Protection
prevalent and potentially lethal, and is associated with various Agency (2007-41-1667), and data at the individual case level were
conditions including cancer, prolonged immobilization, and major made available to us by the national registers in anonymized form.
surgery or trauma (secondary VTE) [16]. Interestingly, VTE is Register studies do not require ethical approval in Denmark. The
also associated with certain cardiovascular risk factors (e.g., authors had full access to all data and take full responsibility for its
obesity, hypertension, and smoking), and arterial cardiovascular integrity.
events [16–18]. Moreover, the risk of VTE is associated with
elevated levels of C-reactive protein [19], and increased risk of Study population and data sources
VTE was recently demonstrated in patients with inflammatory The study population comprised the entire Danish population
bowel disease [20,21]. The potential impact of psoriasis on the risk aged $18 years on January 1, 1997. The population was followed
of VTE, however, has not been examined in detail previously [6]. until December 31, 2006, or death. Patients with prevalent
We therefore examined the risk of VTE in patients with psoriasis psoriasis, a history of previous VTE, and patients receiving
PLoS ONE | www.plosone.org 1 March 2011 | Volume 6 | Issue 3 | e18125
Psoriasis and Risk of Venous Thromboembolism
vitamin K antagonist treatment at baseline were not included. The as events per 1000 person-years. The rate ratios (RRs) and 95%
study was conducted and reported in accordance with the confidence interval (CI) of VTE were estimated by time-dependent
Strengthening the Reporting of Observational Studies in Epide- Poisson regression models adjusted for age, calendar year,
miology (STROBE) recommendations [22]. In Denmark, all concomitant medication, comorbidity, socioeconomic data, and
citizens have a unique personal civil registration number that gender. Psoriasis status was included as a time-dependent variable,
enables individual level-linkage of information across nationwide i.e., patients were only considered at risk from the time they
prospectively recorded registers. All medications dispensed from complied with the inclusion criteria. Age and calendar year were
pharmacies were obtained from the National Prescription Registry also included as time-dependent variables. Comorbidity, socio-
(the Danish Registry of Medicinal Product Statistics), where all economics, and concomitant medication were included as fixed
dispensed prescriptions have been recorded since 1995 ensuring variables obtained at baseline.
complete registration. Patients with psoriasis were identified by Sensitivity analyses with exclusion of patients at increased risk of
their claims of prescriptions for vitamin D derivatives. Patients secondary VTE at baseline, including those with cancer (ICD-10
were included when claiming their second prescription for these C00–C97), the risk of which may be increased in psoriatic patients
agents to ensure persistent medical treatment for psoriasis as [25], and rheumatological disease including psoriatic arthritis
previously accepted [12]. Subjects with prevalent psoriasis were (ICD-10 M05–07.3, M32–34, and M35.3) were conducted. The
defined as patients fulfilling the psoriasis criteria prior to study potential impact of immobilization and hemostatic activation due
start. Morbidity was obtained from the Danish National Patient to surgery (any surgical procedure code) was assessed in a
Register in which all hospital contacts, diagnoses, and invasive sensitivity analysis with censoring of subjects at the time of the
procedures have been recorded since 1978 according to the surgical procedure. Surveillance bias was addressed in analyses
International Classification of Diseases (ICD), i.e. ICD-8 until with inclusion of patients with psoriasis at the time of their first
1994 and ICD-10 thereafter. Patients with severe psoriasis were vitamin D prescription claim or first psoriasis diagnosis, and by
identified by hospitalizations (including out-patient visits) for exclusion of all subjects with a history of hospitalizations up to 1
psoriasis (ICD-10 L40) or psoriatic arthritis (M070–M073) and year prior to study start. A two-sided p-value,0.05 was considered
included at the time of their third diagnosis. The severe psoriasis statistically significant. Interaction between severe psoriasis and
classification has previously been validated and pose an acceptable age was found, and therefore both overall and age-stratified
measure of severe disease [12]. Comorbidity at study entry was estimates are presented. All statistical analyses were performed
described by Charlson’s index, as defined by 19 prespecified with the use of SAS statistical software version 9.2 and STATA
diagnoses at study entry and up to 1 year previously [23]. All software version 11.
deaths were identified from the Central Population Register, in
which deaths are recorded within 2 weeks. Causes of death, Results
recorded according to ICD codes, were obtained from the
National Causes of Death Register. Socioeconomic status was The cohort study had a maximum follow-up of 10 years. A total
defined by the individual average yearly gross income in a 5-year of 35,138 patients with mild psoriasis, 3526 patients with severe
period prior to inclusion and patients were divided into quintiles psoriasis, and 4,126,075 controls were identified. Details on study
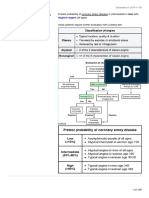
according to their income. population selection are presented in Figure 1. Patients with severe
psoriasis were more often men and more often treated with
Medical treatment cardiovascular medication and glucose-lowering drugs (Table 1).
Prescriptions claimed for topical vitamin-D derivatives (ATC We have previously demonstrated an age- and severity-dependent
D05AX), i.e., topical treatment used exclusively for psoriasis [2], increase in risk of cardiovascular and all-cause mortality with
and vitamin K antagonists (B01AA) were used for in- and exclusion psoriasis in this nationwide cohort [12]. Patients with psoriasis had
of subjects as described above. Pharmacologically managed higher overall VTE rates than controls, i.e., 1.29, 1.92, and 3.20
cardiovascular diseases and cardiovascular risk factors, including per 1000 person-years for controls, mild psoriasis, and severe
hypertension, dyslipidemia, and diabetes mellitus were identified by psoriasis, respectively. This pattern of increased VTE rates was
prescriptions for platelet inhibitors (B01AC), betablockers (C07), sustained in the age-stratified event rates (Table 2), and in analyses
angiotensin-converting enzyme inhibitors (ACEI)/angiotensin 2 of the secondary endpoint of pulmonary embolism, with
receptor antagonists (C09), loop diuretics (C03C), spironolactone corresponding overall pulmonary embolism rates 0.44, 0.61, and
(C03D), statins (C10A), and glucose-lowering drugs (A10) claimed 1.02 per 1000 person-years.
up to 6 months prior to study initiation (Table 1).
Overall and age-stratified time-dependent multivariable
Study endpoints adjusted Poisson regression
The following primary endpoint was assessed: first time in- Psoriasis was associated with a severity- and age-dependent
hospital discharge diagnosis of VTE (ICD-10 I26 and I80.1– increased risk of VTE. The overall RR was 1.35 (CI 1.21–1.49)
I80.9). VTE diagnoses made in emergency departments were not and 2.06 (CI 1.63–2.61) for mild and severe psoriasis, respectively.
included. The diagnosis of VTE (deep venous thrombosis and The corresponding overall risks for pulmonary embolism were
pulmonary embolism) in hospitalized patients has previously been comparable with RRs 1.14 (CI 0.95–1.37) and 1.88 (CI 1.22–
validated in the Danish National Patient Register with a positive 2.89). Age-stratified estimates for VTE are presented in Table 3.
predictive value of 75% when excluding diagnoses from
emergency departments [24]. Hospitalizations with the specific Sensitivity analyses: Influences of secondary VTE and
diagnosis of pulmonary embolism (ICD-10 I26) were evaluated as surveillance bias
a secondary endpoint. Exclusion of all subjects with a history of cancer or
rheumatological disease did not attenuate the association between
Statistical analysis psoriasis and VTE, with RRs 1.34 (CI 1.21–1.49) and 1.99 (CI
Baseline characteristic are presented as percentages and means 1.56–2.53) for mild and severe psoriasis, respectively. Further-
with standard deviations. Unadjusted event rates are summarized more, censoring of participants undergoing a surgical procedure
PLoS ONE | www.plosone.org 2 March 2011 | Volume 6 | Issue 3 | e18125
Psoriasis and Risk of Venous Thromboembolism
Table 1. Baseline characteristics of the study population.
Controls Mild psoriasis Severe psoriasis
Characteristic n = 4,126,075 n = 35,138 n = 3526
Age, years (SD) 46.8 (18) 47.7 (16) 48.4 (16)
Men (%) 2,016,289 (48.9) 17,554 (50.0) 1829(51.9)
Women (%) 2,109,786 (51.1) 17,584 (50.0) 1697(48.1)
No. of person-years 38,503,056 175,384 22,135
Comorbidity (%)
Peripheral vascular disease 5609 (0.14) 43 (0.12) 8 (0.23)
Cerebrovascular disease 12,323 (0.30) 90 (0.26) 8 (0.23)
Coronary heart disease 19,453 (0.47) 190 (0.54) 37 (1.05)
Congestive heart failure 7327 (0.16) 41 (0.11) 9 (0.32)
Hepatic disease 2532 (0.06) 22 (0.06) 31 (0.88)
Chronic obstructive pulmonary disease 11,149 (0.27) 56 (0.16) 10 (0.28)
Cardiac dysrhythmia 11,115 (0.27) 66 (0.19) 16 (0.45)
Renal disease 2330 (0.06) 10 (0.03) 5 (0.14)
Cancer 24,856 (0.60) 156 (0.44) 35 (0.99)
Rheumatological disease 3746 (0.09) 28 (0.08) 9 (0.26)
Treatment (%)
Platelet inhibitor 95,900 (2.32) 844 (2.40) 71 (2.01)
Beta-blocker 134,809 (3.27) 1499 (4.27) 167 (4.74)
ACEI/ARB 116,412 (2,82) 1244(3.54) 133 (3.77)
Loop diuretic 122,929 (2.98) 860(2.45) 151 (4.28)
Statin 27,950 (0.68) 371 (1.06) 33 (0.94)
Spironolactone 14,367 (0.35) 101(0.29) 11 (0.77)
Glucose-lowering drug 71,659 (1.74) 643 (1.83) 96 (2.72)
SD: standard deviation; ACEI: angiotensin-converting enzyme inhibitors; ARB: angiotensin II receptor blocker.
doi:10.1371/journal.pone.0018125.t001
had no significant influence on the VTE risk estimates, i.e., RR surveillance bias, respectively. These findings indicate that VTE
1.20 (CI 0.96–1.51) and 2.55 (CI 1.53–4.24) for mild and severe should be added alongside the list of adverse atherothrombotic
psoriasis, respectively. events, e.g., acute myocardial infarction, which has been linked to
With use of the less restrictive psoriasis diagnosis criterion, psoriasis [3–12].
where patients with psoriasis were identified by their first vitamin Psoriasis is an immunoinflammatory disease characterized by T-
D prescription claim or first psoriasis diagnosis, a total of 55,422 helper (Th)1- and Th17-driven inflammation with a striking
patients with mild psoriasis and 11,532 patients with severe overlap of inflammatory markers and mediators with atheroscle-
psoriasis were included, and 22,018 patients with prevalent rosis [1,26]. Indeed, these mechanisms may form the background,
psoriasis were excluded. This psoriasis diagnosis definition in part, for the increasing evidence linking psoriasis to risk of
corresponded to a 10-year psoriasis prevalence of 2.2%, and the atherothrombotic cardiovascular events, e.g., acute myocardial
VTE risk estimates obtained hereby were comparable to the infarction and cardiovascular mortality [3–12]. While it is well-
results of the primary analyses, including the observed dose- established that inflammation plays a central role in the
response relationship with psoriasis severity, with overall RRs 1.44 pathogenesis of atherosclerosis and atherothrombosis [26], the
(CI 1.34–1.56) and 1.88 (CI 1.62–2.19) for mild and severe potential association between inflammation as determined by
psoriasis, respectively. Exclusion of all subjects with a history of circulating levels of inflammatory markers (e.g., C-reactive protein)
out-patient and/or in-patient hospital contacts up to 1 year prior and risk of VTE is, however, unclear at present [19,27], More
to study start also did not alter the results (mild psoriasis RR 1.33 than three decades ago, a small case-control study suggested that
[CI 1.19–1.48] and severe psoriasis 1.93 [CI 1.50–2.48]). the risk of VTE and other adverse cardiovascular events was
increased in psoriatic patients, but the risk of VTE was not
Discussion specifically addressed in that particular study of highly selected
patients [6], On the other hand, VTE has been associated with the
This nationwide study of VTE risk in patients with psoriasis increased risk of atherothrombotic events and was recently also
suggested an association between psoriasis and increased risk of linked to inflammatory bowel disease [16–20], In addition to
VTE. The present study is, to our knowledge, the first to examine increased markers of systemic inflammation, a psoriasis severity-
the psoriasis-related risk of VTE in a large unselected cohort. We dependent increase in platelet activation, e.g., platelet hyperag-
demonstrated a clear dose-response relationship between VTE risk gregability and increased levels of platelet-derived microparticles
and psoriasis severity, and the results were further corroborated by and soluble P-selectin, has been demonstrated [14,15]. Along this
sensitivity analyses addressing the influence of secondary VTE and line, platelet activity regeneration time following aspirin ingestion
PLoS ONE | www.plosone.org 3 March 2011 | Volume 6 | Issue 3 | e18125
Psoriasis and Risk of Venous Thromboembolism
Figure 1. Flowchart of study population selection. VTE: venous thromboembolism.
doi:10.1371/journal.pone.0018125.g001
may be shorter in psoriasis patients compared to controls [28], and augmented risk of VTE as found in our study was strengthened
hyperhomocysteinemia, which may be associated with athero- by our study cohort design which controlled for important
thrombosis and VTE, has been reported in these patients, measured confounders, the finding of a consistent dose-response
suggestive of a prothrombotic predisposition [13,14]. Moreover, relationship between psoriasis severity and risk of VTE, and the
methotrexate is commonly used in severe psoriasis and though this sensitivity analyses that indicated that the elevated VTE risk was
agent may be associated with lower risk of atherothrombosis in not driven by secondary VTE.
patients with psoriasis and psoriatic arthritis, it is also associated Some further strengths and limitations of the study should be
with hyperhomocysteinemia [3,29]. Finally, it is also interesting, discussed. The main limitation of our study is inherent to its
that statins, which have pleiotropic effects including anti- observational nature that precludes conclusions on causality. The
inflammatory properties, may exert beneficial actions on psoriatic large number of participants, the nationwide coverage of
skin manifestations and may lower the risk of VTE in healthy prospectively recorded registries, and the complete follow-up
individuals and in patients with atherosclerosis [30,31]. In view of strengthens the study. Specifically, the use of nationwide registries
the considerations presented above, several mechanisms may of hospitalizations and dispensed prescriptions from all pharmacies
contribute to the increased risk of VTE in patients with psoriasis, in Denmark where healthcare is readily accessible and essentially
e.g., coincident risk factors, inflammation and hypercoagulability, free of charge enabled us to reduce potential surveillance bias and
and more studies are clearly warranted to examine individual avoid selection bias related to e.g., subject gender, age,
merits of these contributions and, for example, the potential socioeconomic status, healthcare insurance, and labor market
contribution of VTE to the increased cardiovascular and overall association. This was further supported by sensitivity analyses
mortality observed in patients with severe psoriasis [10–12,32]. In addressing this key issue. The use of prospectively identified
addition to the plausible pathophysiological mechanisms, the patients with psoriasis ensured a rational basis for allocation of
likelihood of a causal relationship between psoriasis and
Table 3. Adjusted age-stratified rate ratios and 95%
Table 2. Age-stratified incidence rates per 1000 person-years. confidence intervals of venous thromboembolism (VTE).
Controls Mild psoriasis Severe psoriasis Controls Mild psoriasis Severe psoriasis
VTE VTE
IR (CI),50 years 0.58 (0.57–0.59) 0.73 (0.56–0.95) 2.10 (1.32–3.33) IR (CI),50 years 1.00 1.24 (0.97–1.58) 3.14 (1.98–4.97)
IR (CI)$50 years 2.03 (2.01–2.05) 2.74 (2.45–3.06) 3.93 (3.01–5.13) IR (CI)$50 years 1.00 1.26 (1.13–1.42) 1.74 (1.32–2.28)
IR: incidence rate; CI: 95% confidence interval; VTE: venous thromboembolism. RR: rate ratio; CI: 95% confidence interval.
doi:10.1371/journal.pone.0018125.t002 doi:10.1371/journal.pone.0018125.t003
PLoS ONE | www.plosone.org 4 March 2011 | Volume 6 | Issue 3 | e18125
Psoriasis and Risk of Venous Thromboembolism
exposure time and, due to the very large sample size, did not imply e.g., obesity and smoking. Importantly, we controlled for
any significant loss of information. We were, however, unable to socioeconomic status that correlate with the presence of obesity
identify patients with psoriasis treated with topical corticosteroids and smoking. Finally, the Danish population is predominantly of
alone (due to the liberal indications for these agents), and the Caucasian descent and extrapolation to other ethnicities should
results may not apply to these patients. Since data of in-hospital only be done with caution.
treatment are, at present, not available and as systemic antiin-
flammatory psoriasis treatment, i.e., methotrexate and biological Conclusion
agents, is generally provided directly to the patients by the This first nationwide cohort study indicates that patients with
respective hospital departments and are therefore not captured by psoriasis are at increased risk of VTE. The risk was highest in
the registers, we were unable to use systemic anti-inflammatory young patients with severe disease. Further prospective studies are
treatment as a measure of disease severity and could not address needed to confirm this association, but physicians should be aware
the potential impact of various systemic treatment strategies on the that patients with psoriasis may be at increased risk of both venous
risk of VTE. Indeed, future studies to address the impact of various and arterial thromboembolic events.
psoriasis treatment strategies on cardiovascular risk are likely to
provide important insights [33]. Also, the use of hospitalizations
and prescription claims to describe comorbidity, concomitant Author Contributions
medication, and outcomes implies a possibility of underestimation Conceived and designed the experiments: OA GG LS CTP PRH.
of these variables since we were unable to capture data from those Analyzed the data: OA GG JL JO CJ CTP PRH. Wrote the paper: OA
who did not come to medical attention. The possibility of residual PRH. Revision of manuscript for critical contents: JL MC JO DMB CJ LS
confounding is always present in observational studies, and we GG CTP PRH.
were unable to account for some important risk factors of VTE,
References
1. Nestle FO, Kaplan DH, Barker J (2009) Psoriasis. N Engl J Med 361: 496–509. 18. Sorensen HT, Horvath-Puho E, Pedersen L, Baron JA, Prandoni P (2007)
2. Menter A, Griffiths CE (2007) Current and future management of psoriasis. Venous thromboembolism and subsequent hospitalisation due to acute arterial
Lancet 370: 272–284. cardiovascular events: a 20-year cohort study. Lancet 370: 1773–1779.
3. Friedewald VE, Cather JC, Gelfand JM, Gordon KB, Gibbons GH, et al. (2008) 19. Zacho J, Tybjaerg-Hansen A, Nordestgaard BG (2010) C-reactive protein and
AJC editor’s consensus: psoriasis and coronary artery disease. Am J Cardiol 102: risk of venous thromboembolism in the general population. Arterioscler Thromb
1631–1643. Vasc Biol 30: 1672–1678.
4. Wakkee M, Thio HB, Prens EP, Sijbrands EJ, Neumann HA (2007) 20. Grainge MJ, West J, Card TR (2010) Venous thromboembolism during active
Unfavorable cardiovascular risk profiles in untreated and treated psoriasis disease and remission in inflammatory bowel disease: a cohort study. Lancet
patients. Atherosclerosis 190: 1–9. 375: 657–663.
5. Kimball AB, Robinson D, Jr., Wu Y, Guzzo C, Yeilding N, et al. (2008) 21. Saleh T, Matta F, Yaekoub AY, Danescu SC, Stein PD (2010) Risk of Venous
Cardiovascular disease and risk factors among psoriasis patients in two US Thromboembolism With Inflammatory Bowel Disease. Clin Appl Thromb
healthcare databases, 2001–2002. Dermatology 217: 27–37. Hemost.
6. McDonald CJ, Calabresi P (1978) Psoriasis and occlusive vascular disease. 22. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, et al. (2007) The
Br J Dermatol 99: 469–475. Strengthening the Reporting of Observational Studies in Epidemiology
7. Gelfand JM, Neimann AL, Shin DB, Wang X, Margolis DJ, et al. (2006) Risk of (STROBE) statement: guidelines for reporting observational studies. Lancet
myocardial infarction in patients with psoriasis. JAMA 296: 1735–1741. 370: 1453–1457.
8. Gelfand JM, Dommasch ED, Shin DB, Azfar RS, Kurd SK, et al. (2009) The 23. Nuttall M, van der Meulen J, Emberton M (2006) Charlson scores based on
risk of stroke in patients with psoriasis. J Invest Dermatol 129: 2411–2418. ICD-10 administrative data were valid in assessing comorbidity in patients
9. Prodanovich S, Kirsner RS, Kravetz JD, Ma F, Martinez L, et al. (2009) undergoing urological cancer surgery. J Clin Epidemiol 59: 265–273.
Association of psoriasis with coronary artery, cerebrovascular, and peripheral 24. Severinsen MT, Kristensen SR, Overvad K, Dethlefsen C, Tjonneland A, et al.
vascular diseases and mortality. Arch Dermatol 145: 700–703. (2010) Venous thromboembolism discharge diagnoses in the Danish National
10. Mallbris L, Akre O, Granath F, Yin L, Lindelof B, et al. (2004) Increased risk for Patient Registry should be used with caution. J Clin Epidemiol 63: 223–228.
cardiovascular mortality in psoriasis inpatients but not in outpatients. 25. Brauchli YB, Jick SS, Miret M, Meier CR (2009) Psoriasis and risk of incident
Eur J Epidemiol 19: 225–230. cancer: an inception cohort study with a nested case-control analysis. J Invest
11. Mehta NN, Azfar RS, Shin DB, Neimann AL, Troxel AB, et al. (2010) Patients Dermatol 129: 2604–2612.
with severe psoriasis are at increased risk of cardiovascular mortality: cohort 26. Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease.
study using the General Practice Research Database. Eur Heart J 31: N Engl J Med 352: 1685–1695.
1000–1006. 27. Lippi G, Favaloro EJ, Montagnana M, Franchini M (2010) Review: C-reactive
12. Ahlehoff O, Gislason GH, Charlot M, Jorgensen CH, Lindhardsen J, et al. protein and venous thromboembolism: causal or casual association? Clin Chem
(2010) Psoriasis is associated with clinically significant cardiovascular risk: a Lab Med.
Danish nationwide cohort study. J Intern med doi: 10.1111/j.1365-2796. 28. Berrettini M, Parise P, Constantini V, Grasselli S, Nenci GG (1985) Platelet
2010.02310.x. [Epub ahead of print]. activation in psoriasis. Thromb Haemost 53: 195–197.
13. Gisondi P, Girolomoni G (2009) Psoriasis and atherothrombotic diseases: 29. Prodanovich S, Ma F, Taylor JR, Pezon C, Fasihi T, et al. (2005) Methotrexate
disease-specific and non-disease-specific risk factors. Semin Thromb Hemost 35: reduces incidence of vascular diseases in veterans with psoriasis or rheumatoid
313–324. arthritis. J Am Acad Dermatol 52: 262–267.
14. Karabudak O, Ulusoy RE, Erikci AA, Solmazgul E, Dogan B, et al. (2008) 30. Shirinsky IV, Shirinsky VS (2007) Efficacy of simvastatin in plaque psoriasis: A
Inflammation and hypercoagulable state in adult psoriatic men. Acta Derm pilot study. J Am Acad Dermatol 57: 529–531.
Venereol 88: 337–340. 31. Squizzato A, Galli M, Romualdi E, Dentali F, Kamphuisen PW, et al. (2010)
15. Tamagawa-Mineoka R, Katoh N, Kishimoto S (2010) Platelet activation in Statins, fibrates, and venous thromboembolism: a meta-analysis. Eur Heart J 31:
patients with psoriasis: increased plasma levels of platelet-derived microparticles 1248–1256.
and soluble P-selectin. J Am Acad Dermatol 62: 621–626. 32. Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, et al. (2007) The risk of
16. Goldhaber SZ (2010) Risk factors for venous thromboembolism. J Am Coll mortality in patients with psoriasis: results from a population-based study. Arch
Cardiol 56: 1–7. Dermatol 143: 1493–1499.
17. Holst AG, Jensen G, Prescott E (2010) Risk factors for venous thromboembo- 33. Alexandroff AB, Pauriah M, Camp RD, Lang CC, Struthers AD, et al. (2009)
lism: results from the Copenhagen City Heart Study. Circulation 121: More than skin deep: atherosclerosis as a systemic manifestation of psoriasis.
1896–1903. Br J Dermatol 161: 1–7.
PLoS ONE | www.plosone.org 5 March 2011 | Volume 6 | Issue 3 | e18125
© 2011 Ahlehoff et al. This is an open-access article distributed under the terms
of the Creative Commons Attribution License:
https://creativecommons.org/licenses/by/4.0/ (the “License”), which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited. Notwithstanding the ProQuest Terms
and Conditions, you may use this content in accordance with the terms of the
License.
Potrebbero piacerti anche
- Secondary HypertensionDa EverandSecondary HypertensionAlberto MorgantiNessuna valutazione finora
- Methotrexate Reduces The Occurrence of Cerebrovascular Events Among Taiwanese Psoriatic Patients: A Nationwide Population-Based StudyDocumento4 pagineMethotrexate Reduces The Occurrence of Cerebrovascular Events Among Taiwanese Psoriatic Patients: A Nationwide Population-Based StudyHermayudiNessuna valutazione finora
- TB and PADDocumento7 pagineTB and PADdicky wahyudiNessuna valutazione finora
- Grozdev 2014Documento16 pagineGrozdev 2014mahmoud korieshNessuna valutazione finora
- Jurnal Autoimun PDFDocumento7 pagineJurnal Autoimun PDFRara Anglis AninditaNessuna valutazione finora
- Diabetes Mellitus and Pyogenic Liver Abscess: Risk and PrognosisDocumento8 pagineDiabetes Mellitus and Pyogenic Liver Abscess: Risk and PrognosisJeanetteNessuna valutazione finora
- Hospitalization Due InfectionsDocumento8 pagineHospitalization Due InfectionsHenrique OliveiraNessuna valutazione finora
- Psoriasis and Risk of Cardiovascular Disease: Case Report and DiscussionDocumento4 paginePsoriasis and Risk of Cardiovascular Disease: Case Report and DiscussionAbhishek KushwahNessuna valutazione finora
- Research Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyDocumento13 pagineResearch Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyAns FitriNessuna valutazione finora
- Morbidity and Aging in HIV-Infected Persons: The Swiss HIV Cohort StudyDocumento10 pagineMorbidity and Aging in HIV-Infected Persons: The Swiss HIV Cohort StudyStefania CristinaNessuna valutazione finora
- Oral Health - Atherosclesoris - Cardiovascular DiseaseDocumento11 pagineOral Health - Atherosclesoris - Cardiovascular DiseaseMr.ZeddNessuna valutazione finora
- Lee 2018Documento9 pagineLee 2018AlizaPinkyNessuna valutazione finora
- Mortality and The Use of Antithrombotic Therapies Among Nursing Home Residents With COVID-19Documento6 pagineMortality and The Use of Antithrombotic Therapies Among Nursing Home Residents With COVID-19Shone DayNessuna valutazione finora
- Association Between Psoriasis Vulgaris and Coronary Heart Disease in A Hospital-Based Population in JapanDocumento9 pagineAssociation Between Psoriasis Vulgaris and Coronary Heart Disease in A Hospital-Based Population in JapancutfarahputheNessuna valutazione finora
- Incidence of First Cardiovascular Event in Spanish PatientsDocumento9 pagineIncidence of First Cardiovascular Event in Spanish PatientsJesús Tomás Sánchez CostaNessuna valutazione finora
- Pneumonia in Patients With Diabetes Mellitus: A Single-Center ExperienceDocumento5 paginePneumonia in Patients With Diabetes Mellitus: A Single-Center ExperienceNoer Sidqi MNessuna valutazione finora
- Prevalence and Severity of Coronavirus Disease 2019Documento7 paginePrevalence and Severity of Coronavirus Disease 2019Fabiola VaniaNessuna valutazione finora
- Editorials: Clinical Chemistry 61:2Documento4 pagineEditorials: Clinical Chemistry 61:2YANNessuna valutazione finora
- TB SleDocumento11 pagineTB SlePulmonologi Dan Kedokteran Respirasi FK UNRINessuna valutazione finora
- Pa Nag Iot Akos 2015Documento7 paginePa Nag Iot Akos 2015Gabriel ParizotoNessuna valutazione finora
- Journal Pone 0054555Documento12 pagineJournal Pone 0054555Cesar Antonio Vargas AlayzaNessuna valutazione finora
- Population-Based Analysis of Invasive Fungal Infections, France, 2001-2010Documento7 paginePopulation-Based Analysis of Invasive Fungal Infections, France, 2001-2010Mark ReinhardtNessuna valutazione finora
- Journal Pre-Proof: Journal of Clinical VirologyDocumento18 pagineJournal Pre-Proof: Journal of Clinical VirologyOkki Wahyu AtikasariNessuna valutazione finora
- Pharmaceuticals 15 01146 v2Documento26 paginePharmaceuticals 15 01146 v2Norlando RuizNessuna valutazione finora
- Cross-Sectional Analysis of The Association Between PDFDocumento12 pagineCross-Sectional Analysis of The Association Between PDFGhimpu DanielaNessuna valutazione finora
- 38 Reaserch South AfricaDocumento6 pagine38 Reaserch South AfricaTsigereda AberaNessuna valutazione finora
- Hypertension in Hematologic Malignancies and Hematopoietic Cell Transplantation: An Emerging Issue With The Introduction of Novel TreatmentsDocumento8 pagineHypertension in Hematologic Malignancies and Hematopoietic Cell Transplantation: An Emerging Issue With The Introduction of Novel TreatmentsGabryelNessuna valutazione finora
- Herpes ZosterDocumento8 pagineHerpes ZosterPramita SariNessuna valutazione finora
- Update ON Psoriatic Arthritis: Epidemiology, Pathogenesis, Clinical Assessment and TreatmentDocumento35 pagineUpdate ON Psoriatic Arthritis: Epidemiology, Pathogenesis, Clinical Assessment and TreatmentSudeesh KumarNessuna valutazione finora
- Diabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDocumento12 pagineDiabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDwitari Novalia HaraziNessuna valutazione finora
- AlzheimerDocumento7 pagineAlzheimerMirsa LeanderNessuna valutazione finora
- Coagulation Disorder PDFDocumento4 pagineCoagulation Disorder PDFBrownell TraciNessuna valutazione finora
- Rüthrich2021 Article COVID-19InCancerPatientsClinicDocumento11 pagineRüthrich2021 Article COVID-19InCancerPatientsClinicdianaNessuna valutazione finora
- Tromboembolismo en Covid19Documento7 pagineTromboembolismo en Covid19Nestor Alonso Lopez RubioNessuna valutazione finora
- Ijerph 17 01742Documento12 pagineIjerph 17 01742journal proNessuna valutazione finora
- Full TextDocumento34 pagineFull TextkanNessuna valutazione finora
- Relacionado A IAM y Enf CVDocumento13 pagineRelacionado A IAM y Enf CVCarlos Huaman ZevallosNessuna valutazione finora
- Value of Epi Research in Clinical PracticeDocumento6 pagineValue of Epi Research in Clinical PracticeFouzia ShariqNessuna valutazione finora
- Wu Et Al 2017 - Epidemiology and Risk Factors of Infective Endocarditis in Children in ChinaDocumento10 pagineWu Et Al 2017 - Epidemiology and Risk Factors of Infective Endocarditis in Children in ChinaOktadoni SaputraNessuna valutazione finora
- Sepsis Syndromes in Adults - Epidemiology, Definitions, Clinical Presentation, Diagnosis, and Prognosis - UpToDateDocumento37 pagineSepsis Syndromes in Adults - Epidemiology, Definitions, Clinical Presentation, Diagnosis, and Prognosis - UpToDatejordi carreiroNessuna valutazione finora
- Nihms 595411Documento18 pagineNihms 595411Feer DíazNessuna valutazione finora
- COVID-19 and Psoriasis Should We Fear For Patients Treated With BiologicsDocumento4 pagineCOVID-19 and Psoriasis Should We Fear For Patients Treated With BiologicsEstu Paramadina PratamaNessuna valutazione finora
- 2018 Article 989Documento9 pagine2018 Article 989Evan Nanda AdilistyaNessuna valutazione finora
- Inflammation in ST - Elevation Myocardial Infarction - Risk Factors, Patterns of Presentation and Association With Clinical Picture and OutcomeDocumento8 pagineInflammation in ST - Elevation Myocardial Infarction - Risk Factors, Patterns of Presentation and Association With Clinical Picture and OutcomeRJMNessuna valutazione finora
- Psoriasis NATURE AYFinlayDocumento48 paginePsoriasis NATURE AYFinlayMelly SyafridaNessuna valutazione finora
- Einarson 2018Documento19 pagineEinarson 2018Nikola Dragicka DragicevicNessuna valutazione finora
- Psoriasis and Dermatitis AtopicDocumento11 paginePsoriasis and Dermatitis AtopicsayasajaNessuna valutazione finora
- Association Between Periodontitis and Arterial Hypertension: A Systematic Review and Meta-AnalysisDocumento15 pagineAssociation Between Periodontitis and Arterial Hypertension: A Systematic Review and Meta-AnalysisPentiya Vita AyuniNessuna valutazione finora
- Journal Pbio 3001561Documento23 pagineJournal Pbio 3001561philosophy-thoughtNessuna valutazione finora
- Upward Trend in Dengue Incidence Among Hospitalized Patients, United StatesDocumento6 pagineUpward Trend in Dengue Incidence Among Hospitalized Patients, United StatesArhaMozaNessuna valutazione finora
- MainDocumento14 pagineMainDoménica SánchezNessuna valutazione finora
- 2016 Article 1019Documento7 pagine2016 Article 1019Putri Aisyah RahmaniaNessuna valutazione finora
- Cardiac Dysfunction in Multisystem Inflammatory Syndrome in Children: An Italian Single-Center StudyDocumento9 pagineCardiac Dysfunction in Multisystem Inflammatory Syndrome in Children: An Italian Single-Center Studyriq.ahkNessuna valutazione finora
- Sepsis Syndromes in AdultsDocumento27 pagineSepsis Syndromes in Adultstuan tranNessuna valutazione finora
- Risk Factors For Herpes Zoster Infection: A Meta-Analysis: Review ArticleDocumento8 pagineRisk Factors For Herpes Zoster Infection: A Meta-Analysis: Review Articleyenny handayani sihiteNessuna valutazione finora
- The Role of Immune Suppression and HHV-8 in TheDocumento5 pagineThe Role of Immune Suppression and HHV-8 in TheAbsalom MwazhaNessuna valutazione finora
- Chen 2015Documento6 pagineChen 2015nurminsyahNessuna valutazione finora
- CV Risc in SLE 5pdfDocumento18 pagineCV Risc in SLE 5pdfŞtefaniuc IulianNessuna valutazione finora
- Sepsis Update 2011 PDFDocumento10 pagineSepsis Update 2011 PDFIndahK.WardhaniPutriNessuna valutazione finora
- Obesity and Resp InfectionsDocumento13 pagineObesity and Resp InfectionsDumitru BiniucNessuna valutazione finora
- Chapter27-Assessment and Management of Patients With HypertensionDocumento31 pagineChapter27-Assessment and Management of Patients With HypertensionAhmed 123Nessuna valutazione finora
- Cvs PharmacologyDocumento75 pagineCvs PharmacologyTamratKelelegn100% (1)
- Cardiac Medications TemplateDocumento5 pagineCardiac Medications TemplateErinNessuna valutazione finora
- DIURETICSDocumento40 pagineDIURETICSNiña Jean Tormis AldabaNessuna valutazione finora
- Anti HypertensivesDocumento15 pagineAnti HypertensivesFaye MillanesNessuna valutazione finora
- Guidelines Chronic Urticaria and AngioedemaDocumento20 pagineGuidelines Chronic Urticaria and AngioedemaAnny AunNessuna valutazione finora
- Zanki Step 2 - Cardiovascular SystemDocumento129 pagineZanki Step 2 - Cardiovascular SystemChunlei WangNessuna valutazione finora
- 2Documento13 pagine2RAED GhunaimNessuna valutazione finora
- Pharmacological and Pharmaceutical Profile of Valsartan: A ReviewDocumento8 paginePharmacological and Pharmaceutical Profile of Valsartan: A ReviewWisnu Dwi AntaraNessuna valutazione finora
- Design of This Case Record Form (CRF) : General GuidanceDocumento5 pagineDesign of This Case Record Form (CRF) : General GuidanceCecilia PinedaNessuna valutazione finora
- Advances Management ADHFDocumento14 pagineAdvances Management ADHFAnonymous NeRC5JYiSNessuna valutazione finora
- Nursing Responsibilities in Administering Cardiovascular DrugsDocumento76 pagineNursing Responsibilities in Administering Cardiovascular DrugsNikka Moreen Dagdag67% (6)
- COVID-19 Survival Guide McMaster 2020 07 01Documento29 pagineCOVID-19 Survival Guide McMaster 2020 07 01MUHAMMAD09Nessuna valutazione finora
- Hypertensive Crisis: Instructor'S Guide To Changes in This EditionDocumento6 pagineHypertensive Crisis: Instructor'S Guide To Changes in This Editionnurmaliarizky100% (1)
- CVS & Hypolipidemic Drugs-NursingDocumento71 pagineCVS & Hypolipidemic Drugs-NursingManikanta Guptha100% (1)
- Heart FailureDocumento108 pagineHeart FailureDeasy Rizka Rahmawati100% (1)
- 2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryDocumento24 pagine2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryAna RuizNessuna valutazione finora
- ACLS Drugs (2010)Documento16 pagineACLS Drugs (2010)RN333100% (2)
- Outpatient MedicineDocumento0 pagineOutpatient Medicineclaragustin_53768590Nessuna valutazione finora
- Antihypertensive DrugsDocumento28 pagineAntihypertensive DrugsAdinanta Purnawijaya100% (1)
- Zomen in CKDDocumento12 pagineZomen in CKDClaudiu BalabanNessuna valutazione finora
- Urge Incontinence: +nocturnal Symptoms, Gets Urges All The Time DX: Cystometry: It Will Show Random Peaks RX: Anticholinergics: Oxybutynin, Tolteridine, Frequent VoidingsDocumento44 pagineUrge Incontinence: +nocturnal Symptoms, Gets Urges All The Time DX: Cystometry: It Will Show Random Peaks RX: Anticholinergics: Oxybutynin, Tolteridine, Frequent VoidingsAppu ayyalaNessuna valutazione finora
- Entresto Uses, Dosage, Side Effects & WarningsDocumento6 pagineEntresto Uses, Dosage, Side Effects & WarningspatgarettNessuna valutazione finora
- Kdigo 2021 BP GLDocumento92 pagineKdigo 2021 BP GLAndres Bermudez100% (1)
- Case 2: A 74-Year-Old Man With Acute Renal FailureDocumento11 pagineCase 2: A 74-Year-Old Man With Acute Renal FailureAndiUmarNessuna valutazione finora
- Association of Hypertension andDocumento9 pagineAssociation of Hypertension andDeny Dwi HartantoNessuna valutazione finora
- MBBS Made Easy, Second MBBS Examination, Manoj Vimal, Jaypee Bros., 2nd Edition 2009 PDFDocumento329 pagineMBBS Made Easy, Second MBBS Examination, Manoj Vimal, Jaypee Bros., 2nd Edition 2009 PDFMonica KaranthNessuna valutazione finora
- 300 QuestionsDocumento34 pagine300 QuestionsAhmed Assem78% (9)
- FMcase 8Documento12 pagineFMcase 8Ryan Townsend100% (1)
- Renovascular HypertensionDocumento20 pagineRenovascular Hypertensionalul847474Nessuna valutazione finora