Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
GI Disorders
Caricato da
sajjad hussainCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
GI Disorders
Caricato da
sajjad hussainCopyright:
Formati disponibili
Gastrointestinal
Disorders
Your Guide to
Healthy Digestion
(A part of the Blueprint for Men’s Health series of publications.)
Table of Contents
Introduction........................................................................................................................ 1
A Quick Tour of Your Gastrointestinal (GI) Tract................................................. 2
Functional Gastrointestinal Disorders (FGID)...................................................... 3
Irritable Bowel Syndrome........................................................................................6
Chronic Constipation................................................................................................. 8
Inflammatory Bowel Diseases (IBD)...................................................................... 10
Crohn’s Disease........................................................................................................ 10
Ulcerative Colitis........................................................................................................12
Gastroesophageal Reflux Disease (GERD).......................................................13
You and Your Doctor: A Critical Partnership........................................................15
At Your Appointment................................................................................................15
Seeing a Specialist...................................................................................................16
Preventing GI Tract Disorders: Keeping Your Intestines Healthy...............18
Resources..........................................................................................inside back cover
Introduction
A t least 1 in 4 people in the U.S. have stomach- or intestinal
problems that are so severe that they interfere with the
person’s daily activities and quality of life. Problems with
the intestines or digestion are collectively referred to as
Gastrointestinal (or GI) Disorders, and can be divided into two
broad categories:
Functional Gastrointestinal Disorders (sometimes called
FGIDs), which are the result of abnormal functioning of the GI
tract (that’s the system of connected organs that starts at the
mouth and ends at the anus. See the illustration on the next
page). FGIDs are often hard to diagnose because even though
they produce frequent symptoms, there is no visible damage
to the GI tract, and there are no screening tests to identify
them.
GI Diseases (sometimes referred to as Inflammatory GI
diseases) also produce symptoms, but they are the result of
something being physically wrong or damaged somewhere
in the GI tract, such as cancer, growths, ulcers, infection, or
inflammation. GI diseases are often diagnosed with the help
of x-rays, blood tests, and other tools. In the pages that follow,
we’ll discuss both types of GI disorders, what causes them,
and how to treat (and/or prevent) them.
As you read through this book, pay close attention to the
symptoms we describe. In the United States, women are 3-4
times more likely than men to see a primary care doctor or a
specialist for GI-related problems.
If you think you have any of the conditions discussed
in this book, we strongly encourage you to schedule an
appointment with a healthcare provider right away.
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 1
A Quick Tour of Your
Gastrointestinal (GI) Tract
The GI tract is basically a hollow tube that takes food from
your mouth, down your throat (esophagus), into your stomach,
and on to the intestines. Along the way, your body extracts
nutrients from the food and turns them into the fuel you need
to walk, talk, think, read, play, and everything else you do.
After that, the GI tract takes what’s left over and moves it down
to your rectum where it eventually leaves your body as feces.
Esophagus
Liver
Stomach
Gallbladder
Large
Intestine
Pancreas
Small
Intestine
Rectum
2 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
Functional Gastrointestinal
Disorders (FGID)
Just about everyone experiences symptoms of FGIDs at some
point in his or her life. But for millions of people, those symptoms
are chronic (meaning they happen frequently or have been going
on for a long time). Unfortunately, many people—especially
men—with chronic symptoms don’t get the help they need because
they don’t know where to go, they’re afraid of what they’ll find
out, or they’re just embarrassed to talk to anyone about their
problem. Read through the list of symptoms below. If any of them
are chronic or are interfering with your daily activities, see your
healthcare provider right away.
Symptoms
n Abdominal pain (in or around the stomach,
either chronic or sudden)
n Anal or rectal pain (chronic or sudden)
n Belching (frequent, repetitive)
n Bloating (in the abdomen)
n Chest pain
n Constipation (straining to defecate and/or hard
or lumpy stool)
n Cramping (below your belly button)
n Diarrhea
n Gas (sometimes called flatulence)
n Heartburn
n Indigestion (sometimes called dyspepsia)
n Nausea
n Trouble swallowing
n Vomiting (frequently)
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 3
Causes and Risk Factors
While healthcare experts don’t know exactly what causes FGIDs,
many believe that it’s the result of a communication breakdown
between the brain and the intestinal tract. For example, abnormal
signaling could cause the GI tract to overreact (which would lead
to diarrhea) or underreact (which would lead to constipation).
They also know that FGIDs can be caused—or made worse—by a
number of other factors, including:
n Regularly consuming a diet low in fiber
n Not drinking enough water or other liquids daily
n Lack of exercise
n Travel or another change in routine
n Eating large amounts of dairy products
n Stress
n Resisting the urge to have a bowel movement
n Pain from hemorrhoids that is bad enough that it
makes you resist bowel movements
n Overuse of laxatives (stool softeners) which can
weaken the bowel muscles
n Antacids that contain calcium or aluminum
n Medication, including antidepressants and iron
supplements, and many narcotics and other powerful
drugs for pain.
n Pregnancy
4 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
Diagnosis and Treatment
As we mentioned above, even though FGIDs produce symptoms,
examinations and tests will not be able to identify the cause.
Your entire GI tract may look fine, but there’s clearly something
wrong. That means your healthcare provider will rely on your
description of the symptoms. That’s why it’s important that you
keep track of what your symptoms are, when each one started,
how frequently you have them, how long they last, how severe they
are, and so on.
On the following page we discuss the specific symptoms,
diagnosis, and treatment of two of the most common FGIDs.
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 5
IRRITABLE BOWEL SYNDROME
Irritable Bowel Syndrome is one of the most common FGIDs. It can
affect people of any age, but is most common among people 30-50.
Some people use the phrases “Irritable Bowel Syndrome” (IBS) and
“Inflammatory Bowel Disease” (IBD) interchangeably. However, although
they may sound similar, the two are quite different. While IBS is certainly
unpleasant, it’s not a disease. In fact, it’s actually a group of symptoms
that occur together. IBD, on the other hand, is a far more serious
condition, which we’ll discuss on page 10.
Symptoms
No two people with IBS have exactly the same symptoms. For some, the
symptoms are manageable, while for others, they are debilitating. Many
of the symptoms of IBS are the same as those of other functional GI
disorders. However, there are several things that set IBS apart:
n Pain and discomfort in the abdomen. It can be sharp or dull
and may feel like gas or cramping. In most cases, the pain and
discomfort will lessen after a bowel movement.
n Changes in bowel habits, most notably a change in the frequency
or consistency of your stool. In other words, you could be
constipated, have diarrhea, or go back and forth between
the two.
n Feeling full after eating very little.
n Feeling that even though you just had a bowel movement, you
didn’t get everything out.
n Urgency. You need to find a restroom right now.
In addition, there can be several symptoms that have nothing to do with
your intestines:
n Fatigue
n Muscle and/or low-back pain
n Headaches
n Sexual dysfunction
If you’re a little confused about the symptoms, you’re certainly not alone.
6 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
But if you’re even the slightest bit suspicious about whether you’ve got
IBS, ask yourself these questions:
n Do I have recurrent abdominal pain or discomfort?
n Do I often feel bloated?
n Am I often constipated?
n Does mucus occasionally come out with my stool?
If you answered Yes to one or more of these questions, speak to your
healthcare provider right away.
Causes and Risk Factors
As with other functional GI disorders, the exact causes behind IBS are
a mystery. One theory is that people with IBS may have an excess of
natural chemicals in the body that produce contractions in the intestines
and make them especially sensitive to pain.
Diagnosis and Treatment
Unfortunately, without understanding what causes IBS, it’s impossible to
cure. There are, however, a number of changes you can make that may
relieve your symptoms or at least make them more manageable. For
example:
n Eat a diet high in fiber. Avoid fatty foods, chocolate, alcohol, dairy
products, soda, and caffeine as these foods may make symptoms
worse.
n Quit smoking
n Ask your healthcare provider about appropriate medications.
This may include laxatives, antidepressants (which may reduce
abdominal discomfort or pain), antispasmodics (to control
contractions in colon), or approved IBS agents
n Reduce your stress levels. Less stress will mean less cramping and
less pain.
IBS is a long-term condition and symptoms can change or come and go
over time. For that reason, it’s helpful to keep a diary of your symptoms
and when they occurred. This may help you and your healthcare
provider identify certain behaviors or foods that are making your
symptoms worse or causing them to flare up in the first place.
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 7
CHRONIC CONSTIPATION
Constipation is a condition in which a person either has three or fewer
bowel movements per week or has bowel movements that are hard or
difficult to pass. We all deal with occasional constipation. However, when
the symptoms last for months or years rather than days, it becomes
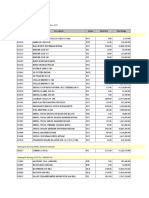
what’s called Chronic Constipation. The chart below illustrates the
differences between occasional and chronic constipation.
Occasional Constipation Chronic Constipation
Short-term problem Long-term problem
Symptoms resolve in a
Symptoms last three or more
relatively short time, usually no
months may persist for years.
more than a few days.
In addition to poor diet, lack of
May be caused by poor diet,
exercise, illness, or medication,
lack of exercise, illness, or
may also be caused by physical
certain medications.
problems.
May be relieved by change in
Requires medical attention and
diet, exercise, and over-the-
possibly prescription medication.
counter (OTC) medications.
Symptoms
n Infrequent bowel movements and/or difficulty having bowel
movements
n Swollen abdomen or abdominal pain
n Straining during bowel movements
Causes and Risk Factors
n Not eating enough fiber
n Eating too much dairy
n Ignoring the urge to have a bowel movement
n Not drinking enough water or liquids
n Lack of physical activity
n Medications (especially those for pain) and antacids that contain
aluminum and calcium
n Life changes or daily routine changes
n Eating disorders
n Overuse of laxatives and/or stool softeners.
8 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
Diagnosis and Treatment
If you suffer from chronic constipation, your healthcare provider will
decide how to treat it depending on what’s causing your symptoms,
how severe they are, and how long you’ve had them. Treatment typically
includes one or more of the following:
n Changing your diet—specifically, eat more fiber, less dairy, and
drink more water.
n Getting more exercise and/or making other lifestyle changes.
n Taking prescribed medication, possibly including laxatives,
enemas, and/or stool softeners, and/or approved IBS agents.
n Surgery. This will be used as a last resort by your healthcare
provider.
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 9
Inflammatory Bowel Diseases (IBD)
There are several types of IBD. We’ll discuss three of the most
common below.
CROHN’S DISEASE
Crohn’s disease is a form of Inflammatory Bowel Disease (IBD). With
IBD, the immune system misidentifies harmless bacteria as a threat and
starts attacking the intestines. Unlike Irritable Bowel Syndrome (IBS), IBD
causes the intestines to become inflamed and may lead to ulcers (small,
open sores) or other damage.
Symptoms
The symptoms of Crohn’s Disease can be mild or severe and may include
any or all of the following:
n Abdominal pain
n Diarrhea (possibly bloody)
n Slight fever
n Cramping
n Vomiting
n Occasional rectal bleeding
n Weight loss
If you experience frequent abdominal pain, blood in your stool,
unexplained fever that lasts more than a few days, and/or frequent
diarrhea, consult your medical provider immediately.
In addition, Crohn’s disease affects the intestines, its effects show up
in many other parts of the body as well. For example, Crohn’s may be
associated with arthritis, blood clots, depression, eye disease (and
vision loss), headaches, kidney stones, liver disease, mouth sores,
osteoporosis, seizures, skin disorders, and strokes.
Causes and Risk Factors
Crohn’s disease can affect anyone at any time. However, there are a few
things that may affect your risk.
n Your age. Most people develop Crohn’s disease before they turn 30.
n Smoking. Smoking may not cause Crohn’s, but it can make many of
the symptoms a lot worse.
n Your ethnicity. Anyone can get Crohn’s, but Caucasians are the
most likely. If you’re of Ashkenzai (Eastern European Jewish)
descent, your chances are higher.
10 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
n Your family history. If anyone else in your immediate family has
Crohn’s, your risk of developing it are higher than for those without
a family history of the disease.
Diagnosis and Treatment
Because there are so many possible symptoms—and because those
symptoms can range from mild to severe and may even disappear for
a short while—it’s often very difficult to diagnose Crohn’s Disease. That
said, if your medical provider suspects that you have Crohn’s, he or she
may order one or more tests, including an endoscopy (inserting a small,
flexible tube with a camera through the patient’s mouth to see the lining
of the upper GI tract and stomach) and/or colonoscopy (inserting a small
camera through the patient’s rectum to view the intestines), specialized
x-rays and other scans, stool samples, and blood tests.
There is no sure-fire cure for Crohn’s Disease. However, there are
treatments that may help relieve and manage your symptoms. In most
cases, your provider will prescribe drugs. These may include:
n Anti-inflammatory drugs to reduce inflammation
n Drugs to suppress your immune system. These are important
because Crohn’s causes your immune system to overreact and
attack the rest of your body.
n Antibiotics to help fight infections caused by the disease.
n Other drugs to treat diarrhea, pain, constipation, low levels of iron
in the blood.
In addition, your provider may recommend that you make some lifestyle
changes, such as:
n Limiting dairy products (milk, cheese)
n Limiting fiber—if they make your symptoms worse
n Eliminating other foods that you believe trigger your symptoms or
make them worse.
n Making other diet changes, such as reducing fatty foods, alcohol,
or spices
n Taking nutritional supplements to counteract the loss of nutrients
caused by Crohn’s.
n Quitting smoking
n Reducing your stress
If medication and lifestyle changes haven’t improved your symptoms,
your doctor may recommend surgery to remove the damaged sections
of your intestines
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 11
ULCERATIVE COLITIS
Ulcerative Colitis is another form of Inflammatory Bowel Disease (IBD)
in which the immune system misidentifies harmless intestinal bacteria
as a threat. When the immune system gets switched on, it’s very hard
to get it to turn off again. Unlike Crohn’s, which can affect any part of
the intestinal tract, ulcerative colitis attacks only the lining of the colon
(also called the large intestines), causing inflammation and creating small
ulcers that produce pus or mucous.
Unfortunately, medical professionals don’t know what causes ulcerative
colitis. Many suspect, however, that it’s a combination of several
factors, including the genes of the person who has the disease, his
immune system, and coming into contact with certain substances in the
environment.
Symptoms
n Abdominal discomfort
n Urgent bowel movement
n Blood in the stool
n Anemia
n Fatigue
n Weight loss
n Loss of appetite
n Rectal bleeding
As with other chronic diseases, the symptoms may appear in periods
of flare-ups and then subside for a period of time.
Causes and Risk Factors
Some of the factors that increase your risk of Crohn’s Disease also
increase your risk of developing Ulcerative Colitis, including age,
ethnicity, and family history (see page 10 for more).
Diagnosis and Treatment
These are essentially the same as for Crohn’s Disease. See page 10 for
more.
12 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
Gastroesophageal reflux disease (GERD) is a serious, chronic, or
long-lasting form of Acid Reflux (also known as GER). Acid Reflux is
when stomach contents flow backwards, from the stomach up into the
esophagus (the tube that carries food and liquids from your mouth down
to your stomach).
When Acid Reflux occurs more than twice a week for a few weeks,
it could be GERD, which over time can lead to more serious health
problems.
Symptoms
n Frequent heartburn or acid indigestion, particularly after consuming
acidic foods and drinks, caffeine, and fatty foods
n Persistent sore throat, hoarseness, or laryngitis (swelling and
irritation of the voice box that results in losing your voice)
n Wheezing
n Pain or difficulty when swallowing
n Chronic cough
n Frequent nausea and/or vomiting
n Pain in the chest or the upper part of the abdomen
n Dental erosion and bad breath
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 13
Causes and Risk Factors
n Obesity
n Abnormalities in the body such as hiatal hernias. Hiatal hernias are
common among people over 50 and occur when the upper part of
your stomach pushes up through the diaphragm (a sheet of muscle
that normally separates the stomach from the chest) into your
chest.
n Pregnancy
n Certain medications, such as asthma medications, calcium channel
blockers, and many antihistamines, pain killers, sedatives, and
antidepressants
n Smoking
n Having another condition such as asthma or diabetes
Diagnosis and Treatment
If your healthcare provider tells you that you have GERD, her or she will
decide how to treat it depending on what’s causing your symptoms, how
severe they are, and how long you’ve had them. Common treatments
include:
n Losing weight (if necessary)
n Making dietary and lifestyle changes, such as:
l Avoiding foods that make your symptoms worse
l Quitting smoking and avoiding being around smokers
n Not laying down within 3 hours of eating (this may prevent acid
from rising)
n Raising your head off the bed 6 to 8 inches with a pillow
n Wearing loose-fitting clothing around the stomach area (tight
clothing can increase reflux)
n Medications including:
l Antacids for relief or heartburn
l Proton pump inhibitors or H2 blockers to help heal the
esophagus
l Antibiotics, including those which improve gastric emptying
n Surgery (as a last resort)
14 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
You and Your Doctor:
A Critical Partnership
If you think you have any of the stomach problems or conditions
we’ve described in this book, we strongly recommend that you
speak with your healthcare provider immediately. Ignoring your
symptoms or hoping they’ll go away on their own could make
your condition worse.
Preparing for Your Visit
Although your provider may want you to have certain tests, most of
what he or she will use to diagnose your condition will come from
what’s called a patient history—the information you provide about your
symptoms. Before meeting with your provider, it’s as good idea to write
down in a notebook the following information:
n What your symptoms are and how long you’ve had them
n Anything you think triggers your symptoms, makes them worse, or
relieves them
At Your Appointment
Even after reading the detailed journal of your symptoms, your
provider will ask you a lot of questions. Be sure to answer honestly and
completely. This is no time to be shy or to be keeping secrets. Some
detail that you think is insignificant could possibly make the difference
between life and death or between a healthy life and an unhealthy one.
When your provider has finished with his or her questions, it’s your turn.
Again, don’t be shy. The more you know about your condition, the better
you’ll be able to manage it and the better your outcome will be. Below,
you’ll find a number of questions to ask your provider. We recommend
that you bring it with you to your appointment.
Questions to Ask about Your GI Condition
n What is the name of my condition?
n How severe is my condition? Is my condition considered chronic
(long-lasting)?
n Is it hereditary or related to my environment or lifestyle?
n What complications might I experience?
n Does my condition increase my risk for developing any other
medical problems?
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 15
Questions to Ask about Diagnosing Your Conditions
n What tests are available to diagnose my condition?
n Which of them do you recommend and why?
n What does the test involve?
n What are the side effects of each test?
n How should I prepare for this diagnostic test?
n How long will the test take?
n Will I be able to drive myself home immediately following the test?
n How long will it take to get the results of the test? Should I call for
the results, or will someone contact me?
n If my test finds a problem, what will our next steps be?
Questions to Ask about Your Treatment
n Is there a cure for my condition?
n What are my treatment options and which do you recommend?
n What are the potential benefits and drawbacks of this treatment?
n What are the common side effects of the recommended treatment?
n What should I do if I experience severe side effects?
Telephone # to call: ________________________
n Should I take any over-the-counter medications (e.g., antacids,
aspirin) during treatment? Over-the-counter medications to avoid:
__________________________________________________
n How long should it take for the treatment to work?
n Are there any medications that I am already taking or am likely to
take that can interact with the medications you are prescribing?
n What types of lifestyle and dietary changes may be helpful to
manage my condition during and after treatment?
n Should I schedule appointments with a nutritionist, dietician, or
other healthcare specialist? How often should I be seen for follow-
up appointments?
n Are there any clinical trials available for my condition?
Seeing a Specialist
If your healthcare provider determines that you have a GI Disorder,
he or she may refer you to a Gastroenterologist (a GI doctor).
Gastroenterologists go through the same medical training as other
physicians, but they also spend several more years studying and
learning to treat conditions and diseases of the digestive tract.
16 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
Gastrointestinal Disorders | Your Guide to Healthy Digestion • 17
Preventing GI Tract Disorders:
Keeping Your Intestines Healthy
Constipation and other digestive problems are no fun, especially
for people who suffer from them often. They can cause disruption
in your daily life. Fortunately, these diseases are often
manageable—and sometimes even preventable—through diet and
lifestyle. Here are some tips that will help keep your intestines
and digestive system healthy:
1. Eat to beat disease. This means a healthy diet with plenty of fruits,
high fiber foods, green leafy vegetables, and yellow vegetables.
2. Cut the fat. Excess fat slows digestion and can lead to heartburn,
bloating, and constipation. It also increases your risk of heart disease,
diabetes, and perhaps even colon cancer.
3. Hydrate. Get in the habit of drinking plenty of water every day.
Drinking 6 to 8 glasses of water every day will help you maintain your
natural digestive process.
4. Lose weight. Heartburn, bloating, and constipation are more
common—and more severe—in people who are overweight.
5. Exercise regularly. Being physically active is good for healthy
digestion.
6. Avoid alcohol and tobacco. More than one or two alcoholic drinks
per day, or chewing or smoking tobacco can lead to serious
digestive disorders. When combined, tobacco and alcohol greatly
increase your risk of mouth and esophageal cancer.
7. Take medication only as directed. Anti-inflammatory medications
such as aspirin, ibuprofen (Advil/Motrin), and naproxen (Aleve) can
be hard on your intestines and digestive system. If you need to take
them, do it with food.
18 • Gastrointestinal Disorders | Your Guide to Healthy Digestion
Resources
For more info on GI conditions visit:
AMERICAN GASTROENTEROLOGICAL ASSOCIATION
www.gastro.org
CENTERS FOR DISEASE CONTROL
www.cdc.gov/ibd
INTERNATIONAL FOUNDATION FOR FUNCTIONAL
GASTROINTESTINAL DISORDERS
www.iffgd.org
NATIONAL INSTITUTE OF DIABETES AND DIGESTIVE
AND KIDNEY DISEASES
www2.niddk.nih.gov
MEN’S HEALTH LIBRARY
www.menshealthlibrary.com
MEN’S HEALTH RESOURCE CENTER
www.menshealthresourcecenter.com
Want to Learn More?
For more information on other health problems that affect men,
boys and their families visit www.menshealthnetwork.org
Men’s Health Network
P.O. Box 75972
Washington, DC 20013
202-543-MHN-1
info@menshealthnetwork.org
www.menshealthnetwork.org
Follow us on Twitter
twitter.com/menshlthnetwork
Like us on Facebook
facebook.com/menshealthnetwork
This Gastrointestinal Disorders book
has been supported by:
Potrebbero piacerti anche
- Basic Principle and Theoretical Background of PIGEDocumento21 pagineBasic Principle and Theoretical Background of PIGEsajjad hussainNessuna valutazione finora
- Different Types of Mouse StrainsDocumento1 paginaDifferent Types of Mouse Strainssajjad hussainNessuna valutazione finora
- Mod1 PDFDocumento31 pagineMod1 PDFsajjad hussainNessuna valutazione finora
- Nanobiotechnology and BionanotechnologyDocumento32 pagineNanobiotechnology and Bionanotechnologysajjad hussainNessuna valutazione finora
- Monte Carlo Simulation TechniqueDocumento48 pagineMonte Carlo Simulation TechniquediajengNessuna valutazione finora
- Monte Carlo Simulation TechniqueDocumento48 pagineMonte Carlo Simulation TechniquediajengNessuna valutazione finora
- Endocrine System 1Documento54 pagineEndocrine System 1chloe parkNessuna valutazione finora
- Proteins As Products: Powerpoint Lecture By: Melissa Rowland-Goldsmith Chapman UniversityDocumento74 pagineProteins As Products: Powerpoint Lecture By: Melissa Rowland-Goldsmith Chapman Universitysajjad hussainNessuna valutazione finora
- Intro To NanotechnologyDocumento20 pagineIntro To NanotechnologyAnbarasan RSNessuna valutazione finora
- Nupecc - Long Range Plan 2010: Working Group 6 Nuclear Physics Tools and ApplicationsDocumento37 pagineNupecc - Long Range Plan 2010: Working Group 6 Nuclear Physics Tools and Applicationssajjad hussainNessuna valutazione finora
- Ion Beam Analysis: Joele Mira From Uwc and Ithemba Labs Tinyiko Maluleke From Us Supervisor: Dr. Alexander KobzevDocumento18 pagineIon Beam Analysis: Joele Mira From Uwc and Ithemba Labs Tinyiko Maluleke From Us Supervisor: Dr. Alexander Kobzevsajjad hussainNessuna valutazione finora
- Mini Solid State Tesla Coil - Abd Majid B Bachuk - TK3431.A42 2009 24 PagesDocumento24 pagineMini Solid State Tesla Coil - Abd Majid B Bachuk - TK3431.A42 2009 24 Pagessajjad hussainNessuna valutazione finora
- Proteins As Products: Powerpoint Lecture By: Melissa Rowland-Goldsmith Chapman UniversityDocumento74 pagineProteins As Products: Powerpoint Lecture By: Melissa Rowland-Goldsmith Chapman Universitysajjad hussainNessuna valutazione finora
- Nupecc - Long Range Plan 2010: Working Group 6 Nuclear Physics Tools and ApplicationsDocumento37 pagineNupecc - Long Range Plan 2010: Working Group 6 Nuclear Physics Tools and Applicationssajjad hussainNessuna valutazione finora
- What Is BufferDocumento9 pagineWhat Is Buffersajjad hussainNessuna valutazione finora
- Torrent Downloaded From Demonoid - OooDocumento1 paginaTorrent Downloaded From Demonoid - Ooosajjad hussainNessuna valutazione finora
- Biotech MCQs NumanDocumento14 pagineBiotech MCQs Numansajjad hussainNessuna valutazione finora
- Biotech MCQs NumanDocumento28 pagineBiotech MCQs NumansajjaddrNessuna valutazione finora
- 1 PDFDocumento10 pagine1 PDFsajjad hussainNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Higgs Boson-2012Documento99 pagineHiggs Boson-2012sajjad hussainNessuna valutazione finora
- Questions Bank For Molecular Biology Answer Sheet PDFDocumento51 pagineQuestions Bank For Molecular Biology Answer Sheet PDFsajjad hussainNessuna valutazione finora
- 1 PDFDocumento10 pagine1 PDFsajjad hussainNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- INDIRECT QUESTIONS AND REPORTED SPEECHDocumento7 pagineINDIRECT QUESTIONS AND REPORTED SPEECHOmar Chavez100% (1)
- Health and Hygiene Essentials for TeenagersDocumento39 pagineHealth and Hygiene Essentials for Teenagersparisha dhebar100% (1)
- A Day OutDocumento5 pagineA Day OutTamer AmrNessuna valutazione finora
- MUSHROOM INSPIRATION BOARDDocumento4 pagineMUSHROOM INSPIRATION BOARDRemyaNessuna valutazione finora
- Tariff Rulings MARCH 2022 Final 3 1Documento22 pagineTariff Rulings MARCH 2022 Final 3 1milanNessuna valutazione finora
- BTP (Sweetener 2016)Documento56 pagineBTP (Sweetener 2016)Sarii Sifati AuliyaNessuna valutazione finora
- List of English Homophones ExplainedDocumento3 pagineList of English Homophones ExplainedbllgNessuna valutazione finora
- M4-L2 Information ArchitectureDocumento66 pagineM4-L2 Information ArchitectureAnonymous 7PmasFlc6yNessuna valutazione finora
- Gastronomy Tourism Events & DestinationsDocumento10 pagineGastronomy Tourism Events & DestinationsRita SalibaNessuna valutazione finora
- True All Undertale Text Ver.4Documento143 pagineTrue All Undertale Text Ver.4CrasherGaleNessuna valutazione finora
- Manual Frigider GrundigDocumento329 pagineManual Frigider GrundigAndyFoxNessuna valutazione finora
- 7 Layer Cake From Petite Patisserie by Cheryl WakerhauserDocumento3 pagine7 Layer Cake From Petite Patisserie by Cheryl WakerhauserAshNessuna valutazione finora
- Taste BrochureDocumento2 pagineTaste BrochureCourtney GomezNessuna valutazione finora
- Lesson 8 - Review of Conditional SentencesDocumento9 pagineLesson 8 - Review of Conditional SentenceskhanhNessuna valutazione finora
- A4 Food Spoilage & PreservationDocumento15 pagineA4 Food Spoilage & PreservationRavi kishore KuchiyaNessuna valutazione finora
- Distribution Supply Chain Management of AmulDocumento24 pagineDistribution Supply Chain Management of AmulGuneet Singh ChabraNessuna valutazione finora
- Economic Insight Food PricesDocumento8 pagineEconomic Insight Food PricesVivek AgarwalNessuna valutazione finora
- 1d Present Simple (Negative and Interrogative) PDFDocumento1 pagina1d Present Simple (Negative and Interrogative) PDFKarina RossiNessuna valutazione finora
- DR AzmilDocumento26 pagineDR AzmilAisaNessuna valutazione finora
- Buff ColorationDocumento273 pagineBuff ColorationJan Frederik Valkenberg CastroNessuna valutazione finora
- Present simple past and past participle verbs in English and SpanishDocumento8 paginePresent simple past and past participle verbs in English and Spanishramirom_3Nessuna valutazione finora
- Group 2Documento13 pagineGroup 2Albert Reyes Doren Jr.Nessuna valutazione finora
- Nicole Erwin Professional Resume 2015-16 ClinicalDocumento1 paginaNicole Erwin Professional Resume 2015-16 Clinicalapi-318488586Nessuna valutazione finora
- Satvic Kids BookDocumento29 pagineSatvic Kids Bookmahesh gole100% (4)
- Collective Nouns WorksheetsDocumento14 pagineCollective Nouns WorksheetsGina Singh100% (1)
- The Role of Traditional Belief Systems and Indigenous Practices in Natural Resource Conservation and Its Challenges: The Case of Wonago Woreda, Gedeo Zone, Southern EthiopiaDocumento23 pagineThe Role of Traditional Belief Systems and Indigenous Practices in Natural Resource Conservation and Its Challenges: The Case of Wonago Woreda, Gedeo Zone, Southern Ethiopiayoseph maruNessuna valutazione finora
- Module 3Documento3 pagineModule 3Cherry Ann Joy AbonNessuna valutazione finora
- Meat Importer Application FormDocumento2 pagineMeat Importer Application FormKatrizia FauniNessuna valutazione finora
- GIAE L0A The Longer Read U4Documento2 pagineGIAE L0A The Longer Read U4flor alejoNessuna valutazione finora
- LAPORAN RATA-RATA HARGA BELIDocumento315 pagineLAPORAN RATA-RATA HARGA BELIfadjaroeddinNessuna valutazione finora