Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Psychotic Disorders
Caricato da
smacuja0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
5 visualizzazioni15 paginehk
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentohk
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
5 visualizzazioni15 paginePsychotic Disorders
Caricato da
smacujahk
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 15
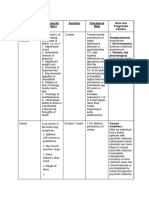
PSYCHOTIC DISORDERS
DURATION OTHER CRITERIA FOR
SYMPTOMATOLOGY PREVALENCE RISK FACTORS
OF ILLNESS DIAGNOSIS
A. The presence of one (or more) delusions with a
duration of 1 month or longer.
B. Criterion A* for schizophrenia has never been met.
*Two (or more) of the following, each present for a
significant portion of time during a
1 -month period (or less if successfully treated1.
D
Delusions.
E
2. Hallucinations.
L
3. Disorganized speech (e.g., frequent derailment or
U
incoherence).
S Lifetime prevalence: ~0.2%
4. Grossly disorganized or catatonic behavior.
I
5. Negative symptoms (i.e., diminished emotional The assessment of cognition,
O Most frequent subtype: persecutory
expression or avolition). depression, and mania symptom
N
domains is vital for making critically
A Gender Distribution: No major
1 month or Note: Hallucinations, if present, are not prominent and important distinctions between the
L gender differences in the overall
longer are related to the delusional various schizophrenia spectrum and
frequency of delusional disorder
theme (e.g., the sensation of being infested with other psychotic disorders.
D
insects associated with delusions of
I *Note: Delusional disorder, jealous
infestation).
S type, is probably more
O common in males than in females
C. Apart from the impact of the delusion(s) or its
R
ramifications, functioning is not markedly
D
impaired, and behavior is not obviously bizarre or odd.
E
D. If manic or major depressive episodes have occurred,
R
these have been brief relative
to the duration of the delusional periods.
E. The disturbance is not attributable to the
physiological effects of a substance or another
medical condition and is not better explained by
another mental disorder, such as body dysmorphic
disorder or obsessive-compulsive disorder.
B
R
I
A. Presence of one (or more) of the following symptoms:
E
1. Delusions.
F Temperamental.
2. Hallucinations.
Preexisting personality
3. Disorganized speech (e.g., frequent derailment or
P disorders and traits (e.g.,
incoherence).
S schizotypal personality
4. Grossly disorganized or catatonic behavior. Prevalence (United States): 9% of
Y The assessment of cognition, disorder; borderline
cases of first-onset psychosis.
C depression, and mania symptom personality disorder; or
B. Duration of an episode of the disturbance is at least 1
H domains is vital for making critically traits in the psychoticism
At least 1 day day but less than 1 month, with Psychotic disturbances are more
O important distinctions between the domain, such
but less than 1 eventual full return to premorbid level of functioning. common in developing countries
T various schizophrenia spectrum and as perceptual
month than in developed countries.
I other psychotic disorders. dysregulation, and the
C negative affectivity domain,
C. The disturbance is not better explained by major Gender Distribution: twofold more
such as suspiciousness)
depressive or bipolar disorder with common in females than in males.
D may predispose the
psychotic features or another psychotic disorder such
I individual to the
as schizophrenia or catatonia,
S development of the
and is not attributable to the physiological effects of a
O disorder.
substance (e.g., a drug of abuse,
R
a medication) or another medical condition.
D
E
R
A. Two (or more) of the following, each present for a
significant portion of time during a 1-month period (or
less if successfully treated).
S 1. Delusions.
C 2. Hallucinations.
H 3. Disorganized speech (e.g., frequent derailment or
I incoherence).
Z 4. Grossly disorganized or catatonic behavior.
O 5. Negative symptoms (i.e., diminished emotional
P expression or avolition).
H
R B. An episode of the disorder lasts at least 1 month but As with schizophrenia, currently
E less than 6 months. When the diagnosis must be there are no laboratory or
N made without waiting for recovery, it should be psychometric tests for Genetic and physiological.
I At least 1 qualified as “provisional.” schizophreniform disorder. There are Higher incidence in developing Relatives of individuals with
F month but less multiple brain regions where countries compared to developed schizophreniform disorder
O than 6 months C. Schizoaffective disorder and depressive or bipolar neuroimaging, neuropathological, countries. have an increased risk for
R disorder with psychotic features have and neurophysiological research has schizophrenia.
M been ruled out because either 1 ) no major depressive indicated abnormalities, but none are
or manic episodes have occurred diagnostic.
D concurrently with the active-phase symptoms, or 2) if
I mood episodes have occurred during
S active-phase symptoms, they have been present for a
O minority of the total duration
R of the active and residual periods of the illness.
D
E
R D. The disturbance is not attributable to the physiological
effects of a substance (e.g., a
drug of abuse, a medication) or another medical
condition.
A. Two (or more) of the following, each present for a Environmental.
significant portion of time during a 1-month period (or Season of birth has been
less if successfully treated). linked to the incidence of
1. Delusions. schizophrenia, including
2. Hallucinations. late winter/early spring in
3. Disorganized speech (e.g., frequent derailment or some locations and
incoherence). summer for the deficit form
4. Grossly disorganized or catatonic behavior. of the disease. The
5. Negative symptoms (i.e., diminished emotional incidence of schizophrenia
expression or avolition). and related disorders is
higher for children growing
B. For a significant portion of the time since the onset of up in an urban environment
the disturbance, level of functioning A schizophrenia diagnosis requires and for some minority
Continuous in one or more major areas, such as work, the presence of delusions or Lifetime prevalence: 0.3%-0.7%, ethnic groups.
signs of the interpersonal relations, or self-care, is hallucinations in the absence of Sex ratio differs across samples
S
disturbance markedly below the level achieved prior to the onset mood episodes. In addition, mood and populations: Genetic and physiological.
C
persist for at (or when the onset is in childhood episodes, taken in total, should be an emphasis on negative There is a strong
H
least 6 or adolescence, there is failure to achieve expected present for only a minority of the symptoms and longer contribution for genetic
I
months. level of interpersonal, academic, total duration of the active and duration of disorder factors in determining
Z
or occupational functioning). residual periods of the illness. (associated with poorer risk for schizophrenia,
O
This 6-month outcome) shows higher although most individuals
P
period C. Continuous signs of the disturbance persist for at least In addition to the five symptom incidence rates for males, who have been diagnosed
H
must include 6 months. This 6-month period domain areas identified in the whereas definitions allowing with schizophrenia have no
R
at least 1 must include at least 1 month of symptoms (or less if diagnostic criteria, the assessment for the inclusion of more family history of psychosis.
E
month of successfully treated) that meet Criterion of cognition, depression, and mania mood symptoms and brief
N
symptoms (or A (i.e., active-phase symptoms) and may include symptom domains is vital for making presentations Pregnancy and birth
I
less if periods of prodromal or residual critically important distinctions (associated with better complications with hypoxia
A
successfully symptoms. During these prodromal or residual between the various schizophrenia outcome) show equivalent and greater paternal age
treated). periods, the signs of the disturbance may spectrum and other psychotic risks for both sexes. are associated
be manifested by only negative symptoms or by two disorders. with a higher risk of
or more symptoms listed in Criterion schizophrenia for the
A present in an attenuated form (e.g., odd beliefs, developing fetus. In
unusual perceptual experiences). addition, other prenatal
and perinatal adversities,
D. Schizoaffective disorder and depressive or bipolar including stress, infection,
disorder with psychotic features malnutrition, maternal
have been ruled out because either 1) no major diabetes, and
depressive or manic episodes have other medical conditions,
occurred concurrently with the active-phase have been linked with
symptoms, or 2) if mood episodes have schizophrenia. However,
occurred during active-phase symptoms, they have the vast majority
been present for a minority of the of offspring with these risk
total duration of the active and residual periods of the factors do not develop
illness. schizophrenia.
E. The disturbance is not attributable to the
physiological effects of a substance (e.g., a
drug of abuse, a medication) or another medical
condition.
F. If there is a history of autism spectrum disorder or a
communication disorder of childhood
onset, the additional diagnosis of schizophrenia is
made only if prominent delusions
or hallucinations, in addition to the other required
symptoms of schizophrenia,
are also present for at least 1 month (or less if
successfully treated).
S
C
H
I A. An uninterrupted period of illness during which there
Z is a major mood episode (major depressive or manic)
O concurrent with Criterion A of schizophrenia.
Genetic and physiological.
A Delusions or Note: The major depressive episode must include a
Among individuals with
F hallucinations depressed mood.
In addition to the five symptom schizophrenia, there may
F for 2 or more
domain areas identified in the be an increased risk for
E weeks in the B. Delusions or hallucinations for 2 or more weeks in the
diagnostic criteria, the assessment schizoaffective disorder in
C absence of a absence of a major mood episode (depressive or
of cognition, depression, and mania Lifetime prevalence: 0.3% first-degree relatives. The
T major mood manic) during the lifetime duration of the illness.
symptom domains is vital for making Gender Distribution: higher in risk for schizoaffective
I episode
critically important distinctions females than in males disorder may be increased
V (depressive or C. Symptoms that meet criteria for a major mood
between the various schizophrenia among individuals who
E manic) during episode are present for the majority of the total
spectrum and other psychotic have a first-degree relative
the lifetime duration of the active and residual portions of the
disorders. with schizophrenia, bipolar
D duration of the illness.
disorder, or schizoaffective
I illness.
disorder.
S D. The disturbance is not attributable to the effects of a
O substance (e.g., a drug of abuse,
R a medication) or another medical condition.
D
E
R
S
U
B A. Presence of one or both of the following symptoms:
S 1. Delusions.
T 2. Hallucinations.
A
N B. There is evidence from the history, physical
C examination, or laboratory findings of both
E/ 1. The symptoms in Criterion A developed during or
M soon after substance intoxication
E
or withdrawal or after exposure to a medication.
D
I
2. The involved substance/medication is capable of
C producing the symptoms in Criterion A.
A
T C. The disturbance is not better explained by a psychotic
I disorder that is not substance/
O medication-induced. Such evidence of an independent
N Prevalence in the general
psychotic disorder could include In addition to the four symptom
- population
the following: domain areas identified in the
I is unknown.
The symptoms preceded the onset of the diagnostic criteria, the assessment
N
substance/medication use; the symptoms of cognition, depression, and mania
D Between 7% and 25% of
U
persist for a substantial period of time (e.g., about 1 symptom domains is vital for making
individuals presenting with a first
C month) after the cessation of critically important distinctions
episode of psychosis in different
E acute withdrawal or severe intoxication: or there is between the various schizophrenia
settings are reported to have
D other evidence of an independent spectrum and other psychotic
substance/medication-induced
non-substance/medication-induced psychotic disorder disorders.
psychotic disorder.
P (e.g., a history of recurrent
S non-substance/medication-related episodes).
Y
C D. The disturbance does not occur exclusively during the
H
course of a delirium.
O
T
I E. The disturbance causes clinically significant distress
C or impairment in social, occupational,
or other important areas of functioning.
D Note: This diagnosis should be made instead of a
I diagnosis of substance intoxication or
S substance withdrawal only when the symptoms in
O Criterion A predominate in the clinical
R picture and when they are sufficiently severe to
D
warrant clinical attention.
E
R
P
S
Y
C
H
O
T
I
C Lifetime prevalence: 0.21% to
D 0.54%
I
S Age Group Distribution:
O Individuals older than 65 years
R One consideration is the presence of
have a significantly greater
D a temporal association between the
E prevalence of
A. Prominent hallucinations or delusions. onset, exacerbation, or remission of Course modifiers.
R 0.74% compared with those in
B. There is evidence from the history, physical the medical condition and that of the Identification and treatment
younger age groups.
Due examination, or laboratory findings that the psychotic disturbance. A second of the underlying medical
To disturbance is the direct pathophysiological consideration is the presence of condition has
Conditions most commonly
consequence of another medical condition. features that are atypical for a the greatest impact on
A associated with psychosis:
C. The disturbance is not better explained by another psychotic disorder (e.g., atypical age course, although
N untreated endocrine and metabolic
O mental disorder. at onset or presence of visual or preexisting central nervous
disorders, autoimmune disorders
T D. The disturbance does not occur exclusively during the olfactory hallucinations). The system injury may
(e.g., SLE, N-methyl-D-aspartate
H course of a delirium. disturbance must also be confer a worse course
E (NMDA) receptor autoimmune
E. The disturbance causes clinically significant distress distinguished from a outcome (e.g., head
R encephalitis), or temporal lobe
or impairment in social, occupational, substance/medication-induced trauma, cerebrovascular
epilepsy.
M or other important areas of functioning. psychotic disorder or another mental disease).
E disorder (e.g., an adjustment
D Gender distribution: higher in
disorder).
I females, although additional
C gender-related features are not
A clear and vary considerably with
L
the gender distributions of the
C underlying medical conditions.
O
N
D
I
T
I
O
N
Applies to presentations in which symptoms characteristic of
a schizophrenia spectrum and other psychotic disorder that
cause clinically significant distress or impairment
in social, occupational, or other important areas of functioning
Other Specified
predominate but do not meet the full criteria for any of the
Schizophrenia
disorders in the schizophrenia spectrum and other
Spectrum and
psychotic disorders diagnostic class.
Other Psychotic
Disorder
Used in cases when the clinician chooses to communicate
the specific reason that the presentation does not meet the
criteria for any specific schizophrenia spectrum and other
psychotic disorder.
Applies to presentations in which symptoms characteristic of
a schizophrenia spectrum and other psychotic disorder that
cause clinically significant distress or impairment
in social, occupational, or other important areas of functioning
predominate but do not meet the full criteria for any of the
Unspecified
disorders in the schizophrenia spectrum and other
Schizophrenia
psychotic disorders diagnostic class.
Spectrum and
Other Psychotic
Used in situations in which the clinician chooses not to
Disorder
specify the reason that the criteria are not met for a specific
schizophrenia spectrum and other psychotic disorder, and
includes presentations in which there is insufficient
information to make a more specific diagnosis (e.g., in
emergency room settings)
For a diagnosis of bipolar I disorder, it is necessary to meet Environmental.
the following criteria for a manic episode. The manic episode Bipolar disorder is more
may have been preceded by and may be followed by common in high-income
hypomanic or major depressive episodes. than in low-income
countries (1.4 vs. 0.7%).
Manic Episode
A. A distinct period of abnormally and persistently Separated, divorced, or
elevated, expansive, or irritable mood and abnormally widowed individuals have
and persistently increased goal-directed activity or higher rates of
Manic episode energy, lasting at least 1 week and present most of bipolar I disorder than do
lasting at least the day, nearly every day (or any duration if individuals who are married
1 week and hospitalization is necessary). or have never been
present most B. During the period of mood disturbance and increased married, but
of the day, energy or activity, three (or more) of the following the direction of the
nearly every symptoms (four if the mood is only irritable) are association is unclear.
The 12-month prevalence estimate
day present to a significant degree and represent a
in the continental United States
noticeable change from usual behavior: Genetic and physiological.
B was 0.6% for bipolar I
(Possibly with 1. Inflated self-esteem or grandiosity. A family history of bipolar
I It is necessary to meet criteria for a disorder.
hypomanic 2. Decreased need for sleep (e.g., feels rested after disorder is one of the
P manic episode to make a diagnosis
episode only 3 hours of sleep). strongest and
O of bipolar I disorder, but it is not Twelve-month prevalence of
lasting at least 3. More talkative than usual or pressure to keep most consistent risk factors
L required to have hypomanic or major bipolar I disorder across 11
4 consecutive talking. for bipolar disorders. There
A depressive episodes. However, they countries ranged from 0.0% to
days and 4. Flight of ideas or subjective experience that is an average 10-fold
R may precede or follow a manic 0.6%.
present most thoughts are racing. increased risk
episode.
of the day, 5. Distractibility (i.e., attention too easily drawn to among adult relatives of
I The lifetime male-to-female
nearly every unimportant or irrelevant external individuals with bipolar I
prevalence ratio is approximately
day and/or stimuli), as reported or observed. and bipolar II disorders.
1.1:1.
major 6. Increase in goal-directed activity (either socially, at Magnitude of
depressive work or school, or sexually) or psychomotor agitation risk increases with degree
episodes (i.e., purposeless non-goal-directed activity). of kinship. Schizophrenia
present during 7. Excessive involvement in activities that have a high and bipolar disorder likely
the same 2- potential for painful consequences (e.g., engaging in share a genetic
week period) unrestrained buying sprees, sexual indiscretions, or origin, reflected in familial
foolish business investments). co-aggregation of
C. The mood disturbance is sufficiently severe to cause schizophrenia and bipolar
marked impairment in social or occupational disorder.
functioning or to necessitate hospitalization to prevent
harm to self or others, or there are psychotic features. Course modifiers.
D. The episode is not attributable to the physiological After an individual has a
effects of a substance (e.g., a drug of abuse, a manic episode with
medication, other treatment) or to another medical psychotic features,
condition. subsequent
Note: A full manic episode that emerges during manic episodes are more
antidepressant treatment (e.g., medication, likely to include psychotic
electroconvulsive therapy) but persists at a fully features. Incomplete
syndromal level beyond the physiological effect of that interepisode recovery is
treatment is sufficient evidence for a manic episode more common when the
and, therefore, a bipolar I diagnosis. current episode is
accompanied by mood in
Note: Criteria A-D constitute a manic episode. At least congruent
one lifetime manic episode is required psychotic features.
for the diagnosis of bipolar I disorder.
Hypomanic Episode
A. A distinct period of abnormally and persistently
elevated, expansive, or irritable mood
and abnormally and persistently increased activity
or energy, lasting at least 4 consecutive
days and present most of the day, nearly every
day.
B. During the period of mood disturbance and
increased energy and activity, three (or
more) of the following symptoms (four if the mood
is only irritable) have persisted, represent
a noticeable change from usual behavior, and
have been present to a significant
degree:
1. Inflated self-esteem or grandiosity.
2. Decreased need for sleep (e.g., feels rested
after only 3 hours of sleep).
3. More talkative than usual or pressure to keep
talking.
4. Flight of ideas or subjective experience that
thoughts are racing.
5. Distractibility (i.e., attention too easily drawn to
unimportant or irrelevant external
stimuli), as reported or observed.
6. Increase in goal-directed activity (either socially,
at work or school, or sexually) or
psychomotor agitation.
7. Excessive involvement in activities that have a
high potential for painful consequences
(e.g., engaging in unrestrained buying sprees,
sexual indiscretions, or
foolish business investments).
C. The episode is associated with an unequivocal
change in functioning that is uncharacteristic
of the individual when not symptomatic.
D. The disturbance in mood and the change in
functioning are observable by others.
E. The episode is not severe enough to cause
marked impairment in social or occupational
functioning or to necessitate hospitalization. If
there are psychotic features, the
episode is, by definition, manic.
F. The episode is not attributable to the physiological
effects of a substance (e.g., a drug
of abuse, a medication, other treatment).
Note: A full hypomanic episode that emerges
during antidepressant treatment (e.g.,
medication, electroconvulsive therapy) but persists
at a fully syndromal level beyond
the physiological effect of that treatment is
sufficient evidence for a hypomanic episode
diagnosis. However, caution is indicated so that
one or two symptoms (particularly increased
irritability, edginess, or agitation following
antidepressant use) are not taken
as sufficient for diagnosis of a hypomanic episode,
nor necessarily indicative of a bipolar
diathesis.
Note: Criteria A-'F constitute a hypomanic
episode. Hypomanic episodes are common in
bipolar I disorder but are not required for the
diagnosis of bipolar I disorder.
Major Depressive Episode
A. Five (or more) of the following symptoms have been
present during the same 2-week period and represent
a change from previous functioning; at least one of the
symptoms is either (1) depressed mood or (2) loss of
interest or pleasure.
Note: Do not include symptoms that are clearly
attributable to another medical condition.
1. Depressed mood most of the day, nearly every day,
as indicated by either subjective
report (e.g., feels sad, empty, or hopeless) or
observation made by others (e.g.,
appears tearful). (Note: In children and adolescents,
can be irritable mood.)
2. Markedly diminished interest or pleasure in all, or
almost all, activities most of the
day, nearly every day (as indicated by either
subjective account or observation).
3. Significant weight loss when not dieting or weight
gain (e.g., a change of more than
5% of body weight in a month), or decrease or
increase in appetite nearly every
day. (Note: In children, consider failure to make
expected weight gain.)
4. Insomnia or hypersomnia nearly every day.
5. Psychomotor agitation or retardation nearly every
day (observable by others; not
merely subjective feelings of restlessness or being
slowed down).
6. Fatigue or loss of energy nearly every day.
7. Feelings of worthlessness or excessive or
inappropriate guilt (which may be delusional)
nearly every day (not merely self-reproach or guilt
about being sick).
8. Diminished ability to think or concentrate, or
indecisiveness, nearly every day (either
by subjective account or as observed by others).
9. Recurrent thoughts of death (not just fear of dying),
recurrent suicidal ideation without
a specific plan, or a suicide attempt or a specific plan
for committing suicide.
B. The symptoms cause clinically significant distress
or impairment in social, occupational,
or other important areas of functioning.
C. The episode is not attributable to the physiological
effects of a substance or another
medical condition.
Note: Criteria A-C constitute a major depressive
episode. Major depressive episodes are
common in bipolar I disorder but are not required for
the diagnosis of bipolar I disorder.
Note: Responses to a significant loss (e.g.,
bereavement, financial ruin, losses from a
natural disaster, a serious medical illness or disability)
may include the feelings of intense
sadness, rumination about the loss, insomnia, poor
appetite, and weight loss noted in Criterion
A, which may resemble a depressive episode.
Although such symptoms may be understandable
or considered appropriate to the loss, the presence of
a major depressive episode in addition to the normal
response to a significant loss should also be carefully
considered. This decision inevitably requires the
exercise of clinical judgment based on the individual’s
history and the cultural norms for the expression of
distress in the context
of loss.^
Genetic and physiological.
The risk of bipolar II
disorder tends to be highest
among relatives
of individuals with bipolar II
disorder, as opposed to
individuals with bipolar I
disorder
or major depressive
disorder. There may be
Compared with individuals with
genetic factors influencing
The major bipolar I disorder, individuals with
the age at
depressive bipolar II disorder have greater
onset for bipolar disorders.
episode must chronicity of illness and spend, on
A. Criteria have been met for at least one hypomanic and
last at least 2 average, more time in the
at least one major depressive episode. Course modifiers.
weeks, and depressive phase of their illness,
B. There has never been a manic episode. A rapid-cycling pattern is
B the hypomanic which can be severe and/ or The 12-month prevalence
C. The occurrence of the hypomanic episode(s) and associated with a poorer
I episode must disabling. Depressive symptoms co- (internationally): 0.3%.
major depressive episode(s) is not better explained by prognosis. Return
P last at least 4 occurring with a hypomanic episode
schizoaffective disorder, schizophrenia, to previous level of social
O days or hypomanic symptoms co- Prevalence rate of bipolar disorder
schizophreniform disorder, delusional disorder, or function for individuals with
L occurring with a depressive episode yield a combined prevalence rate
other specified or unspecified schizophrenia spectrum bipolar II disorder is more
A Mood are common in individuals with of 1.8% in U.S. and non-U.S.
and other psychotic disorder. likely
R episode(s), bipolar disorder and are community samples,
D. The symptoms of depression or the unpredictability for individuals of younger
With overrepresented in females, with higher rates (2.7% inclusive) in
caused by frequent alternation between periods of age and with less severe
II symptoms particularly hypomania with mixed youths age 12 years or older.
depression and hypomania causes clinically depression, suggesting
present most features. Individuals experiencing
significant distress or impairment in social, adverse effects
of the day, hypomania with mixed features may
occupational, or other important areas of functioning. of prolonged illness on
nearly every not label their symptoms as
recovery. More education,
day hypomania, but instead experience
fewer years of illness, and
them as depression with increased
being married
energy or irritability.
are independently
associated with functional
recovery in individuals with
bipolar
disorder, even after
diagnostic type (I vs. II),
current depressive
symptoms, and presence
of psychiatric comorbidity
are taken into account.
Potrebbero piacerti anche
- Psychodynamic Theory: Kathleen Holtz DealDocumento12 paginePsychodynamic Theory: Kathleen Holtz Dealsmacuja100% (1)
- Interpretive Report of WAIS - IV and WMS-IV TestingDocumento22 pagineInterpretive Report of WAIS - IV and WMS-IV Testingsmacuja0% (1)
- About VALSDocumento3 pagineAbout VALSMara Ioana100% (2)
- Archmodels Vol 171 PDFDocumento16 pagineArchmodels Vol 171 PDFMrDingo007Nessuna valutazione finora
- Employee Motivation ThesisDocumento72 pagineEmployee Motivation ThesisShaheryar Khalid100% (5)
- Tugasan 1 SchizophreniaDocumento18 pagineTugasan 1 SchizophreniaRohaizu Ahmad DinNessuna valutazione finora
- SchizopherniaDocumento11 pagineSchizopherniaSa Ra Doh0% (1)
- Ap 7Documento3 pagineAp 7Andrea LuraNessuna valutazione finora
- Tugas UNtar 3Documento40 pagineTugas UNtar 3Daniel Filemon PosoNessuna valutazione finora
- Schizophrenia Spectrum andDocumento5 pagineSchizophrenia Spectrum andjodie pearlNessuna valutazione finora
- Psychopathology MSE NotesDocumento5 paginePsychopathology MSE Noteszubair.19cbaNessuna valutazione finora
- Differential Diagnosis of Bipolar II Disorder and Borderline Personality DisorderDocumento11 pagineDifferential Diagnosis of Bipolar II Disorder and Borderline Personality DisorderManu Cortes OsorioNessuna valutazione finora
- Screenshot 2022-09-28 at 11.29.26 AMDocumento52 pagineScreenshot 2022-09-28 at 11.29.26 AMTheany Be SmilerNessuna valutazione finora
- Notes On SchizophreniaDocumento6 pagineNotes On SchizophreniaUnkown IndividualNessuna valutazione finora
- Clinical Assesment. Table DSM IV and DSM V PDsDocumento11 pagineClinical Assesment. Table DSM IV and DSM V PDsVicky VaronaNessuna valutazione finora
- P$y C@$3 1Documento21 pagineP$y C@$3 1Linds GoNessuna valutazione finora
- Mood Disorders: Disruptive Mood Dysregulation DisorderDocumento12 pagineMood Disorders: Disruptive Mood Dysregulation DisorderAnna ClaroNessuna valutazione finora
- Depressive DisorderDocumento59 pagineDepressive DisorderJoshua RingorNessuna valutazione finora
- GMS Outline and Content FormatDocumento9 pagineGMS Outline and Content FormatMay GalesNessuna valutazione finora
- MDD Mania Bipolar AssignDocumento2 pagineMDD Mania Bipolar AssignMansi AgrawalNessuna valutazione finora
- PSYCH 1.2A Mood DisordersDocumento22 paginePSYCH 1.2A Mood DisordersZazaNessuna valutazione finora
- Chapter 5Documento9 pagineChapter 5Ellyza EvangelistaNessuna valutazione finora
- Group 3 - SchizophreniaAndOtherPsycchoticDisordersDocumento43 pagineGroup 3 - SchizophreniaAndOtherPsycchoticDisordersFAITH EFONDONessuna valutazione finora
- Mood Disorders (Bautista)Documento7 pagineMood Disorders (Bautista)Aljon S. Templo100% (1)
- Schizophrenia and Other Psychotic Disorders: Michael D. Jibson, M.D., Ph.D. Ira D. Glick, M.D. Rajiv Tandon, M.DDocumento14 pagineSchizophrenia and Other Psychotic Disorders: Michael D. Jibson, M.D., Ph.D. Ira D. Glick, M.D. Rajiv Tandon, M.Dserene_tha067746Nessuna valutazione finora
- Abpsychch12notes PDFDocumento14 pagineAbpsychch12notes PDFlevs riversNessuna valutazione finora
- PSYCH-1.1C Quick Review Table-Schizo - Other Psychotic DisorderDocumento1 paginaPSYCH-1.1C Quick Review Table-Schizo - Other Psychotic DisorderMaikka IlaganNessuna valutazione finora
- Chapter 16: Schizophrenia: Tomorrow: Chapter 17: Mood Disorders and SuicideDocumento65 pagineChapter 16: Schizophrenia: Tomorrow: Chapter 17: Mood Disorders and SuicideRainier Moreno-LacalleNessuna valutazione finora
- Bipolar DisorderDocumento16 pagineBipolar Disorderakingarimuzima90Nessuna valutazione finora
- Ca2 Midterm ReviewerDocumento18 pagineCa2 Midterm ReviewerMarjorie DalumayNessuna valutazione finora
- (Psych) Mood Disorders (Trans)Documento4 pagine(Psych) Mood Disorders (Trans)paningbatan.kristine.bNessuna valutazione finora
- Schizophrenia Chapter EditedDocumento15 pagineSchizophrenia Chapter EditedamarnehNessuna valutazione finora
- Schizophrenia Spectrum and Other Psychotic DisordersDocumento8 pagineSchizophrenia Spectrum and Other Psychotic DisordersRain Simonette GuanNessuna valutazione finora
- Schizophrenia Chapter 5Documento126 pagineSchizophrenia Chapter 5Jackson Pukya Gabino PabloNessuna valutazione finora
- Caie A2 Psychology 9990 Psychology and Abnormality v1Documento20 pagineCaie A2 Psychology 9990 Psychology and Abnormality v1ARMANI ROYNessuna valutazione finora
- Tugas UNtar 3Documento28 pagineTugas UNtar 3Daniel Filemon PosoNessuna valutazione finora
- FHHBBCFDocumento53 pagineFHHBBCFAayush AdhikariNessuna valutazione finora
- Mood DisordersDocumento108 pagineMood DisordersAngellene Firmalino50% (2)
- Psychiatry Dr. Praveen Tripath RevisionDocumento6 paginePsychiatry Dr. Praveen Tripath Revisionprikshitjaglan2004Nessuna valutazione finora
- SPMM Smart Revise Descriptive Psychopathology Paper A Syllabic Content 5.22 Mrcpsych NoteDocumento43 pagineSPMM Smart Revise Descriptive Psychopathology Paper A Syllabic Content 5.22 Mrcpsych NoteBakir JaberNessuna valutazione finora
- 1.1 Schizophrenia and Other PsychosisDocumento7 pagine1.1 Schizophrenia and Other PsychosisMark Christian CuiNessuna valutazione finora
- An Introduction To The Types of SchizophreniaDocumento4 pagineAn Introduction To The Types of Schizophreniasarzlasco09Nessuna valutazione finora
- Reviewer (Abpsych)Documento7 pagineReviewer (Abpsych)Joana Vivien Caraan100% (2)
- Schizophrenia Spectrum HandoutDocumento15 pagineSchizophrenia Spectrum HandoutRichelle CortesNessuna valutazione finora
- Cluster ADocumento4 pagineCluster ANobody but youNessuna valutazione finora
- Summarized Abnormal PsychologyDocumento13 pagineSummarized Abnormal PsychologyMa.Janine Torres100% (1)
- 08.06 Abnormal Psychology-Revised NotesDocumento6 pagine08.06 Abnormal Psychology-Revised NotesJesusa Angelika IlustreNessuna valutazione finora
- Reviewer - Mood DisordersDocumento10 pagineReviewer - Mood DisordersAsia EstradaNessuna valutazione finora
- 03.1 PHD Personality DisordersDocumento8 pagine03.1 PHD Personality DisordersDump AccNessuna valutazione finora
- Ffict,: Intofive &Documento1 paginaFfict,: Intofive &rlk7Nessuna valutazione finora
- SchizophreniaDocumento2 pagineSchizophreniaIT’S ME HAYLA100% (1)
- Chapter 4 DelusionsDocumento14 pagineChapter 4 DelusionsCostrut LaurNessuna valutazione finora
- Anxiety and Depression Disorder SummaryDocumento2 pagineAnxiety and Depression Disorder SummaryФранц ГаллагерNessuna valutazione finora
- Psychiatry Dr. Praveen Tripath RevisionDocumento6 paginePsychiatry Dr. Praveen Tripath Revisionprikshitjaglan2004Nessuna valutazione finora
- Schizophrenia Spectrum and Other Psychotic DisorderDocumento7 pagineSchizophrenia Spectrum and Other Psychotic DisorderLorraine0% (1)
- Student Lecture Dissociative DisorderDocumento4 pagineStudent Lecture Dissociative DisorderMarcela DiasNessuna valutazione finora
- 1.02 Psychiatry - Schizophrenia (Dr. Igot, 2021)Documento5 pagine1.02 Psychiatry - Schizophrenia (Dr. Igot, 2021)Danila BagrovNessuna valutazione finora
- Psych Cheat Sheet 2015Documento21 paginePsych Cheat Sheet 2015mounicapaturuNessuna valutazione finora
- NCP FinalDocumento22 pagineNCP FinalAlmira Ahamad100% (1)
- Psych 3 - Evals 1Documento16 paginePsych 3 - Evals 1Kaye NeeNessuna valutazione finora
- Trauma and Stressor Related DisordersDocumento6 pagineTrauma and Stressor Related DisordersSana Sheikh KashifNessuna valutazione finora
- 1.2. Introduction To ABNORMAL PSYCHOLOGYDocumento21 pagine1.2. Introduction To ABNORMAL PSYCHOLOGYCresiel PontijonNessuna valutazione finora
- Schizophrenia Spectrum DisorderDocumento43 pagineSchizophrenia Spectrum DisorderDimple SainNessuna valutazione finora
- Diagnostic and Statistical Manual of The American Psychiatric Association, Fifth Edition DSM-5Documento3 pagineDiagnostic and Statistical Manual of The American Psychiatric Association, Fifth Edition DSM-5Catherine BribonNessuna valutazione finora
- Schizophrenia Unmasked: Personal Stories and Proven Techniques to Reclaim Your LifeDa EverandSchizophrenia Unmasked: Personal Stories and Proven Techniques to Reclaim Your LifeNessuna valutazione finora
- 16PF GuideDocumento17 pagine16PF GuidesmacujaNessuna valutazione finora
- 1.3 Are Professional Profilers Better - EnglishDocumento5 pagine1.3 Are Professional Profilers Better - EnglishsmacujaNessuna valutazione finora
- Mischel's Situational Personality: Bryan Hall Kristi SimmonsDocumento24 pagineMischel's Situational Personality: Bryan Hall Kristi SimmonssmacujaNessuna valutazione finora
- Consent FormDocumento2 pagineConsent FormsmacujaNessuna valutazione finora
- OddDocumento27 pagineOddsmacujaNessuna valutazione finora
- Comparison of Psychometric Properties of Internet Versions of The Marlowe-Crowne Social Desirability Scale Between Two European CountriesDocumento10 pagineComparison of Psychometric Properties of Internet Versions of The Marlowe-Crowne Social Desirability Scale Between Two European CountriessmacujaNessuna valutazione finora
- Personality of Gifted Children in Korea, Finland, U.S., Slovenia, & Slovakia 1Documento10 paginePersonality of Gifted Children in Korea, Finland, U.S., Slovenia, & Slovakia 1smacujaNessuna valutazione finora
- FLANDocumento2 pagineFLANsmacujaNessuna valutazione finora
- Tips - Barcharts Quickstudy Psychology PDFDocumento4 pagineTips - Barcharts Quickstudy Psychology PDFsmacuja100% (1)
- Associations Between Bystanders and Perpetrators of Online Hate: The Moderating Role of Toxic Online DisinhibitionDocumento9 pagineAssociations Between Bystanders and Perpetrators of Online Hate: The Moderating Role of Toxic Online DisinhibitionsmacujaNessuna valutazione finora
- Clinical Research: Epidemiology of Anxiety Disorders: From Surveys To Nosology and BackDocumento10 pagineClinical Research: Epidemiology of Anxiety Disorders: From Surveys To Nosology and BacksmacujaNessuna valutazione finora
- Treatment Facial: Signature SignatureDocumento1 paginaTreatment Facial: Signature SignaturesmacujaNessuna valutazione finora
- PrintDocumento8 paginePrintsmacujaNessuna valutazione finora
- H P C CDocumento1 paginaH P C CsmacujaNessuna valutazione finora
- The Design of Small Slot ArraysDocumento6 pagineThe Design of Small Slot ArraysRoberto B. Di RennaNessuna valutazione finora
- Analysis of Tense Errors in English Written Composition of Senior Secondary School Ii Students in Pankshin Local Government Area of Plateau StateDocumento47 pagineAnalysis of Tense Errors in English Written Composition of Senior Secondary School Ii Students in Pankshin Local Government Area of Plateau StateEbuka Chukwuemeka100% (1)
- PLINEJDocumento21 paginePLINEJMaja KvrgićNessuna valutazione finora
- CloudLabs UserGuide Student enDocumento110 pagineCloudLabs UserGuide Student enJuan De la cruzNessuna valutazione finora
- Periodical Test Diss 11 2023 2024Documento4 paginePeriodical Test Diss 11 2023 2024milaflor zalsosNessuna valutazione finora
- m10 AssignmentDocumento2 paginem10 AssignmentliapajaritoNessuna valutazione finora
- UCSP ReviewDocumento2 pagineUCSP ReviewHyde ParkNessuna valutazione finora
- Test 1Documento5 pagineTest 1Nguyễn TâmNessuna valutazione finora
- Guia Aprendizaje Ingles 5basico Semana14 Mayo 2013Documento3 pagineGuia Aprendizaje Ingles 5basico Semana14 Mayo 2013Yiglia Barile SNessuna valutazione finora
- Oxford Advance English Teacher GuideDocumento388 pagineOxford Advance English Teacher GuideShahroz AsifNessuna valutazione finora
- Practising Cae Use of English Part 3Documento9 paginePractising Cae Use of English Part 3papalazaruNessuna valutazione finora
- Module 1 Language and CommunicationDocumento4 pagineModule 1 Language and CommunicationDarwin Charles IgnacioNessuna valutazione finora
- Individual DifferencesDocumento3 pagineIndividual DifferencesMerlin AlfaneNessuna valutazione finora
- Human Anatomy and Physiology SyllabusDocumento3 pagineHuman Anatomy and Physiology SyllabusVaness MendezNessuna valutazione finora
- Supporting Statements: Do You Find Interesting?Documento5 pagineSupporting Statements: Do You Find Interesting?abdul0% (1)
- DVP FormDocumento9 pagineDVP FormDrSourav ChandraNessuna valutazione finora
- MarkingDocumento1 paginaMarkingpiyushNessuna valutazione finora
- Psychos Marcin Therapy 2018Documento5 paginePsychos Marcin Therapy 2018cangelescuNessuna valutazione finora
- Word Embedding 9 Mar 23 PDFDocumento16 pagineWord Embedding 9 Mar 23 PDFarpan singhNessuna valutazione finora
- Usability MetricsDocumento4 pagineUsability MetricsAna Jiménez NúñezNessuna valutazione finora
- Manufacturing Resource PlanningDocumento5 pagineManufacturing Resource PlanningNicholas WilliamsNessuna valutazione finora
- Differentiated LearningDocumento27 pagineDifferentiated LearningAndi Haslinda Andi SikandarNessuna valutazione finora
- English HL Gr. 4Documento9 pagineEnglish HL Gr. 4nadinevanwykrNessuna valutazione finora
- Case Study-2Documento28 pagineCase Study-2Pung Worathiti ManosroiNessuna valutazione finora
- HF App-Project Tech (Software) - Advt - (F) - 6 July 2023Documento2 pagineHF App-Project Tech (Software) - Advt - (F) - 6 July 2023kalaiarasinanoNessuna valutazione finora
- Asdfghnm, LDocumento5 pagineAsdfghnm, Lziade roalesNessuna valutazione finora
- RACMA Approved Masters Programs - 2020Documento1 paginaRACMA Approved Masters Programs - 2020Crystal ZawNessuna valutazione finora