Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Statement to Fit Note Guide
Caricato da
emeka2012Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Statement to Fit Note Guide
Caricato da
emeka2012Copyright:
Formati disponibili
The Statement of Fitness for Work – from sick note to fit note
Background Information
From 6 April 2010 the sick note is changing to become a fit note.
Sick notes (or Medical Statements) are the forms issued by doctors to people when they are
ill or injured. They provide advice about whether or not an individual with a health condition
is fit for work.
Many people with health conditions can, with some basic support from their employer,
work as they recover from their condition. This helps the individual because for many
people work can help recovery and also benefits the employer by reducing sickness
absence.
Under the sick note system, doctors could only advise their patient on whether their
health condition meant that they should or should not work. As a result many people who
could benefit from support whilst in work, would be advised that they could not work.
Under the current system employers would not have had the opportunity to consider how
they could help employees achieve an earlier return to work.
To help more people get the support they need to get back to work the new fit note
system will mean that doctors can advise that your employee is either:
• unfit for work; or
• may be fit for work.
A doctor will give a ‘may be fit for work’ Statement if they think that their patient’s health
condition may allow them to work if they get suitable support from their employer.
If an employee is too ill to work the doctor will advise this just like with the sick note.
The changes are not about trying to get people back to work before they are ready, but
about removing the challenges to them returning. This is about you and the people you
manage working together to make the adjustments needed to ensure they are able to
return to work in a supported and structured way.
What is changing?
The changes to the form allow a doctor to provide more information on the employee’s
condition and how they might be able to return to work.
The main changes are:
the removal of the fit for work option;
Information source: Department of Works and Pensions
a new option for a doctor to advise if an employee may be fit for work with some
support;
more space for a doctor to provide information on how the employees condition will
affect what they do;
helpful tick boxes for doctors to use to suggest common ways to help a return to
work.
What stays the same?
The form can still be used as evidence for why an employee cannot work due to an
illness or injury;
the Statement is still not required until after the 7th calendar day of sickness;
the information on the form is advice.
the requirements for the payment of Statutory Sick Pay have not changed; and
employers’ obligations under the Disability Discrimination Act have not changed.
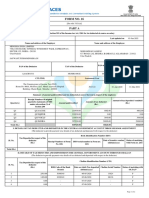
A sample fit note and what it all means.
Information source: Department of Works and Pensions
1. the name of the employee
2. the date the doctor’s assessment of the employee
3. The condition or conditions that affect the employees fitness to work
4. This box will be ticked when the doctor’s assessment of the employee is that they
have or had a health condition that prevents them from working for the stated
period of time. This is strong evidence of the employee’s fitness, or otherwise for
work, for Statutory Sick Pay purposes.
5. This box will be ticked when the doctor’s assessment of the employee is that their
condition does not necessarily stop them from returning to work. However, they
may, for example, not be able to complete all of their normal duties or could benefit
from amended working hours.
6. These four boxes represent common ways to aid a return to work. The doctor will
tick one of these options when they feel they could help the employee return to
work. This list is not exhaustive and there may be other ways to help the employee
return to work. It is important to note that it is the employer’s choice after
discussing the statement with the employee how to act on the doctor’s advice.
Before making any decisions please contact the HR division for advice and
guidance.
7. Where the ‘may be fit for work’ box has been ticked, the doctor will add information
on the functional effects of the employee’s condition and what could help a return
to work. Where a doctor feels an assessment by an occupational health professional
is required, they will state it here.
8. Here the doctor will state the period the advice covers for a forward period, during
which the first six months can be up to a maximum of three months. Any period in
days refers to calendar days not working days. In some cases the employee will be
able to return, with your agreement, to work on their normal duties before the end
of this period. If this happens the employee will not need to see the doctor again for
another statement.
9. The doctor will use this section when they wish to state precise dates for the period
during which the advice applies. This will be for one of three reasons:
a. The statement covers a period based on a previous assessment during which
a Statement was not issued (for example because the doctor did not have
any forms with them); or
b. The statement is for less than 14 days and the doctor does not need to see
the employee again; or
c. The doctor believes it will be helpful to state a specific date for the employee
to return to work as part of their recovery.
Information source: Department of Works and Pensions
10. The doctor will state here if they need to assess their patient’s fitness for work again
at the end of the Statement period. Where the doctor does not need to see the
patient again, in most cases you can expect your employee to return to work or their
usual duties at the end of the Statement period. If the doctor needs to see the
patient again and during the subsequent consultation they feel your employee is
able to return to work without any functional limitations, the doctor will not issue
the employee with a new “fit note”.
11. The doctor will sign, date and stamp or print their address on the Statement.
The information provided in this document should be used in conjunction with the
University’s policy and procedures on managing sickness and absence.
What do I do if I receive a fit note statement from an employee?
The flow chart below explains what you should do if you receive a fit note from an
employee in your department.
Information source: Department of Works and Pensions
In summary
1. A doctor will give a ‘may be fit for work’ Statement if they think that their patient’s
health condition may allow them to work if they get suitable support from their
employer.
2. The new ‘fit note’ is effective from 6 April 2010
3. The ‘fit note’ makes it clear that a phased return to work options is subject to the
employer’s agreement.
4. If a GP states an employee is unfit for work, line managers and employer would NOT
normally contradict the medical opinion.
5. The ‘fit note’ statement is still not required until after the 7th calendar day of
sickness.
6. It is no longer necessary for employees to be signed as fit to return to work.
7. Helpful tick boxes for doctors to use suggested common ways to help an employee
return to work. However, it’s the line manager’s choice (with HR’s input) after
discussing the ‘fit note’ with the employee on how to act on the advice given by the
doctor.
8. The University’s obligations under the Disability Discrimination Act remain
unchanged.
9. Should line managers require any advice they should contact the HR Division by
emailing HRAdvice@le.ac.uk or by calling 0116 252 2439.
Information source: Department of Works and Pensions
Potrebbero piacerti anche
- Sample Doctors Note Work SchoolDocumento2 pagineSample Doctors Note Work SchoolNayeli VazquezNessuna valutazione finora
- Medical RecordsMedical ReportsDocumento24 pagineMedical RecordsMedical ReportshaasviniNessuna valutazione finora
- IMG Orientation Power Point v1.4Documento102 pagineIMG Orientation Power Point v1.4Jora IonNessuna valutazione finora
- SSPDocumento2 pagineSSPMihaela GrosuNessuna valutazione finora
- PDF Fillable Medical CertDocumento4 paginePDF Fillable Medical CertCasey PetersonNessuna valutazione finora
- Payout Amount for Used Toyota LandcruiserDocumento1 paginaPayout Amount for Used Toyota LandcruiserPaul LesterNessuna valutazione finora
- Formulating Design Research Questions: A FrameworkDocumento20 pagineFormulating Design Research Questions: A FrameworkAlemayehu Tilahun HaileNessuna valutazione finora
- Consent For Release of Medical RecordsDocumento1 paginaConsent For Release of Medical RecordsCarrboro Family MedicineNessuna valutazione finora
- Department of State Academic Exchanges Participant Medical History and Examination FormDocumento8 pagineDepartment of State Academic Exchanges Participant Medical History and Examination FormNurman HidayatNessuna valutazione finora
- SC 2Documento2 pagineSC 2Ryan DelaCourt0% (3)
- Emergency Room Assessment Form: Best Eye Opening Best VerbalDocumento2 pagineEmergency Room Assessment Form: Best Eye Opening Best Verbaleliza marie luisNessuna valutazione finora
- Payment in Healthcare OrganizationsDocumento12 paginePayment in Healthcare Organizationsevans kirimiNessuna valutazione finora
- Important Business LetterDocumento42 pagineImportant Business Letterjohn3dNessuna valutazione finora
- Doctors Note Policy 1Documento1 paginaDoctors Note Policy 1api-368387391Nessuna valutazione finora
- Sample Discharge Summary TemplateDocumento3 pagineSample Discharge Summary TemplateBobby Reddy100% (1)
- Salmon Processing Technician Employment ContractDocumento4 pagineSalmon Processing Technician Employment ContractFlorina GeorgianaNessuna valutazione finora
- Pepsi Cola Lottery Promotion Awards £500kDocumento4 paginePepsi Cola Lottery Promotion Awards £500kParag KawleyNessuna valutazione finora
- Self Pay Information FormDocumento1 paginaSelf Pay Information FormPerformax Physical TherapyNessuna valutazione finora
- Discharge Patient From The HospitalDocumento4 pagineDischarge Patient From The HospitalEsamNessuna valutazione finora
- EDC Profit and LossDocumento7 pagineEDC Profit and LossCody WommackNessuna valutazione finora
- Privacy PolicyDocumento3 paginePrivacy Policymerengue100Nessuna valutazione finora
- AhpraDocumento5 pagineAhpraapi-430605312Nessuna valutazione finora
- HIM 200 Health RecordDocumento32 pagineHIM 200 Health RecordMaryamNessuna valutazione finora
- SUPER17983Superannuation Standard Choice Form-1Documento7 pagineSUPER17983Superannuation Standard Choice Form-1RomeoNessuna valutazione finora
- Early Super Release for Mortgage HelpDocumento10 pagineEarly Super Release for Mortgage HelpOzDamo2Nessuna valutazione finora
- Fmcsa: Federal Motor Carrier Safety AdministrationDocumento9 pagineFmcsa: Federal Motor Carrier Safety AdministrationVanessaNessuna valutazione finora
- Illinois Nurse Professional Licensing GuideDocumento12 pagineIllinois Nurse Professional Licensing GuideAnabeth F. PungtilanNessuna valutazione finora
- Ssinc Employee Manual 4-17-13Documento17 pagineSsinc Employee Manual 4-17-13api-20374706Nessuna valutazione finora
- Adventist GlenOaks Hospital 8110116874Documento4 pagineAdventist GlenOaks Hospital 8110116874Mark Richard Hilbert (Rossetti)Nessuna valutazione finora
- Printinvoicerequest 1Documento1 paginaPrintinvoicerequest 1SANI SULEIMAN SAFIYANUNessuna valutazione finora
- Va Form SEP 2009 Supersedes Va Form 21-526, Jan 2004, Which Will Not Be UsedDocumento12 pagineVa Form SEP 2009 Supersedes Va Form 21-526, Jan 2004, Which Will Not Be UsedChris LaytonNessuna valutazione finora
- Application For Trans Tasman Mutual Recognition As A Registered Nurse Enrolled Nurse or Midwife ATMR 04Documento6 pagineApplication For Trans Tasman Mutual Recognition As A Registered Nurse Enrolled Nurse or Midwife ATMR 04binto111Nessuna valutazione finora
- CPR Card 2021Documento2 pagineCPR Card 2021api-545778015Nessuna valutazione finora
- Ronald Regan UCLA Medical Center: Employment ApplicationDocumento3 pagineRonald Regan UCLA Medical Center: Employment Applicationbrookeparker1798Nessuna valutazione finora
- Hasc em CodesDocumento59 pagineHasc em CodesAisy RahmaniaNessuna valutazione finora
- Internships For International Students (2019)Documento11 pagineInternships For International Students (2019)Aakash100% (1)
- Alice Blue Financial Services account statement summaryDocumento4 pagineAlice Blue Financial Services account statement summaryAnup RouthNessuna valutazione finora
- Administration of Hospital Admissions and Discharges PolicyDocumento4 pagineAdministration of Hospital Admissions and Discharges PolicyAnggun DhikaNessuna valutazione finora
- Doctors NoteDocumento6 pagineDoctors Noteitgivesyouwings9Nessuna valutazione finora
- Esi & PF inDocumento30 pagineEsi & PF inkuttyboyNessuna valutazione finora
- Pre-Employment Guiding PrinciplesDocumento14 paginePre-Employment Guiding PrinciplesVivek SNessuna valutazione finora
- Drug Dosing ChartDocumento16 pagineDrug Dosing ChartdnaaziiNessuna valutazione finora
- Medical History and Evaluation FormDocumento22 pagineMedical History and Evaluation FormJobelle Fernandez-SantosNessuna valutazione finora
- PHN SAMPLE AppDocumento3 paginePHN SAMPLE AppRosemaryCastroNessuna valutazione finora
- r123123663 Elesha Casimir CUR123123663Documento1 paginar123123663 Elesha Casimir CUR123123663tefNessuna valutazione finora
- Patient Satisfaction Key to Quality HealthcareDocumento8 paginePatient Satisfaction Key to Quality HealthcareAjlan AliNessuna valutazione finora
- This One Is ItDocumento3 pagineThis One Is Itapi-253737528Nessuna valutazione finora
- Florida COVID-19 Antibody Test ResultsDocumento6 pagineFlorida COVID-19 Antibody Test ResultsDavid Selig0% (1)
- CPSP IMM Congratulations LetterDocumento1 paginaCPSP IMM Congratulations LetterJawad Ul HaqNessuna valutazione finora
- Instructions: After Visit SummaryDocumento10 pagineInstructions: After Visit SummaryKelly Arington McgrealNessuna valutazione finora
- D100Documento20 pagineD100cristianos_cdNessuna valutazione finora
- National Council Licensure Examination (NCLEX®) Authorization To Test (Att)Documento3 pagineNational Council Licensure Examination (NCLEX®) Authorization To Test (Att)dantespiNessuna valutazione finora
- Cms Form1500Documento2 pagineCms Form1500jhite01Nessuna valutazione finora
- FitnoteDocumento9 pagineFitnoteCostel CovaliNessuna valutazione finora
- Fitnote Hospital GuideDocumento9 pagineFitnote Hospital GuiderisnayektiNessuna valutazione finora
- Curbing Abuse of Intermittent FMLA LeaveDocumento4 pagineCurbing Abuse of Intermittent FMLA LeavehospitalitylawyerNessuna valutazione finora
- Guidance on new Fit NoteDocumento6 pagineGuidance on new Fit NoteabhishekmonNessuna valutazione finora
- DEBATEDocumento4 pagineDEBATEMirasol BaykingNessuna valutazione finora
- Fit Note Guidance For Employers and Line ManagersDocumento16 pagineFit Note Guidance For Employers and Line ManagersLiliNessuna valutazione finora
- Absence Due To IllnessDocumento34 pagineAbsence Due To IllnessKesavanNessuna valutazione finora
- Lean Daily ManagementDocumento29 pagineLean Daily ManagementJose Ortega100% (1)
- A Guide To Educational Facility CitingDocumento101 pagineA Guide To Educational Facility Citingemeka2012Nessuna valutazione finora
- IWMS Market Trends to 2026Documento6 pagineIWMS Market Trends to 2026emeka2012Nessuna valutazione finora
- RCA Mini Guide PDFDocumento15 pagineRCA Mini Guide PDFIldzamar Haifa WardhaniNessuna valutazione finora
- IncInvGuide4Empl Dec2015Documento24 pagineIncInvGuide4Empl Dec2015MariMasNessuna valutazione finora
- Compliance Mindset V Value MindsetDocumento20 pagineCompliance Mindset V Value Mindsetemeka2012100% (1)
- The Art of Public SpeakingDocumento467 pagineThe Art of Public SpeakingAiman ArifNessuna valutazione finora
- Traffic Accident Investigation PDFDocumento40 pagineTraffic Accident Investigation PDFyosel sanoyNessuna valutazione finora
- Trends and Patterns of Road Accidents in Nigeria PDFDocumento32 pagineTrends and Patterns of Road Accidents in Nigeria PDFemeka2012Nessuna valutazione finora
- Major Accident Investigation Report: National Truck Accident Research CentreDocumento36 pagineMajor Accident Investigation Report: National Truck Accident Research Centreemeka2012Nessuna valutazione finora
- WAPA - Accident Investigation Report - FinalDocumento50 pagineWAPA - Accident Investigation Report - Finalemeka2012Nessuna valutazione finora
- IncInvGuide4Empl Dec2015Documento24 pagineIncInvGuide4Empl Dec2015MariMasNessuna valutazione finora
- 006 Sample of Report Form F15-11R1-ADocumento4 pagine006 Sample of Report Form F15-11R1-AZilma MarquesNessuna valutazione finora
- 906studyguide - Oil Spill Clean Up PDFDocumento51 pagine906studyguide - Oil Spill Clean Up PDFemeka2012Nessuna valutazione finora
- RCA Mini Guide PDFDocumento15 pagineRCA Mini Guide PDFIldzamar Haifa WardhaniNessuna valutazione finora
- Storypic Fishing FISHIDocumento16 pagineStorypic Fishing FISHIMohammed El-assalNessuna valutazione finora
- 52e40 PDF enDocumento4 pagine52e40 PDF enAldrinNessuna valutazione finora
- Home Polltutants PDFDocumento6 pagineHome Polltutants PDFemeka2012Nessuna valutazione finora
- Whole of Service Report by Calendar YearDocumento4 pagineWhole of Service Report by Calendar Yearemeka2012Nessuna valutazione finora
- Whole of Service Report by Calendar YearDocumento4 pagineWhole of Service Report by Calendar Yearemeka2012Nessuna valutazione finora
- 006 Sample of Report Form F15-11R1-ADocumento4 pagine006 Sample of Report Form F15-11R1-AZilma MarquesNessuna valutazione finora
- Nat-Gas1 - Purging Hazards PDFDocumento15 pagineNat-Gas1 - Purging Hazards PDFemeka2012Nessuna valutazione finora
- Whole of Service Report by Calendar YearDocumento4 pagineWhole of Service Report by Calendar Yearemeka2012Nessuna valutazione finora
- Pecb Iso 45001 Lead Implementer Exam Preparation GuideDocumento16 paginePecb Iso 45001 Lead Implementer Exam Preparation GuideMohammed El-assal100% (1)
- 006 Sample of Report Form F15-11R1-ADocumento4 pagine006 Sample of Report Form F15-11R1-AZilma MarquesNessuna valutazione finora
- OASIS Integrated Management System ManualDocumento45 pagineOASIS Integrated Management System Manualemeka2012Nessuna valutazione finora
- 006 Sample of Report Form F15-11R1-ADocumento4 pagine006 Sample of Report Form F15-11R1-AZilma MarquesNessuna valutazione finora
- Time, Talent, Energy: Overcome Organizational Drag & Unleash Your Team's Productive PowerDocumento7 pagineTime, Talent, Energy: Overcome Organizational Drag & Unleash Your Team's Productive Poweremeka2012Nessuna valutazione finora
- Faqs - Iso 45001 Occupational Health & Safety Management SystemDocumento3 pagineFaqs - Iso 45001 Occupational Health & Safety Management SystemTatiana RiloNessuna valutazione finora
- Sample Worksite Health Budget 508Documento1 paginaSample Worksite Health Budget 508emeka2012Nessuna valutazione finora
- 05 Social Security How Work Affects Your Benefits En-05-10069Documento10 pagine05 Social Security How Work Affects Your Benefits En-05-10069api-309082881Nessuna valutazione finora
- West Bengal Services Death-cum-Retirement Benefit Rules-1971 PDFDocumento127 pagineWest Bengal Services Death-cum-Retirement Benefit Rules-1971 PDFচক্রকূট ভট্টাচার্যNessuna valutazione finora
- Understanding Your Employer ID Number (EINDocumento36 pagineUnderstanding Your Employer ID Number (EINSamj18100% (1)
- Panta budget schedules for production, materials, laborDocumento10 paginePanta budget schedules for production, materials, laborFiles OrganizedNessuna valutazione finora
- The Adamchak, Ponsler, Bordes GroupDocumento14 pagineThe Adamchak, Ponsler, Bordes Groupwhereisthemoon2Nessuna valutazione finora
- GPF - Application For Final WithdrawalDocumento8 pagineGPF - Application For Final WithdrawalNarayanan NMNessuna valutazione finora
- Money Management PhilosophiesDocumento18 pagineMoney Management PhilosophiesSuzaine Camilo100% (1)
- Public Sector AccountingDocumento10 paginePublic Sector AccountingbillNessuna valutazione finora
- Report Industry TrainingDocumento44 pagineReport Industry Trainingaaaa67% (6)
- Actuarial AssistantDocumento2 pagineActuarial Assistantapi-77335013Nessuna valutazione finora
- PCDA(O) Pune Aspects of Pay and AllowancesDocumento58 paginePCDA(O) Pune Aspects of Pay and AllowancesAmartej SinghNessuna valutazione finora
- 2023 Riverside County Pension Advisory Review Committee ReportDocumento24 pagine2023 Riverside County Pension Advisory Review Committee ReportThe Press-Enterprise / pressenterprise.comNessuna valutazione finora
- FORM 16 TDS CERTIFICATEDocumento8 pagineFORM 16 TDS CERTIFICATESaleemNessuna valutazione finora
- Income Tax Planning in India With Respect To Individual Assessee MBA Project - 215080540Documento90 pagineIncome Tax Planning in India With Respect To Individual Assessee MBA Project - 215080540Naveen Kumar67% (3)
- 2016 Icaz Cta Unisa Taxation Tutorial 102 PDFDocumento70 pagine2016 Icaz Cta Unisa Taxation Tutorial 102 PDFArtwell ZuluNessuna valutazione finora
- Tax Treaty Indonesia-United StatesDocumento19 pagineTax Treaty Indonesia-United StatesCindy Claudya CynthiaNessuna valutazione finora
- 04 Profeta V DrilonDocumento3 pagine04 Profeta V DrilonTaz Tanggol Tabao-SumpinganNessuna valutazione finora
- Application Form - New Financial PlanDocumento2 pagineApplication Form - New Financial PlanCamille FreoNessuna valutazione finora
- Equity Investment Cia 3: Reliance PowersDocumento27 pagineEquity Investment Cia 3: Reliance PowersananyaNessuna valutazione finora
- Zimbabwe 2009 Budget Highlights: Taxation ProposalsDocumento46 pagineZimbabwe 2009 Budget Highlights: Taxation ProposalsCarlos Paul NidzaNessuna valutazione finora
- Social Security SystemDocumento2 pagineSocial Security SystemMheca RedondoNessuna valutazione finora
- LCM-MBA Seminar Safety at LafargeDocumento20 pagineLCM-MBA Seminar Safety at LafargeManoj Kumar YadavNessuna valutazione finora
- Corporate Governance Complete ProjectDocumento21 pagineCorporate Governance Complete ProjectEswar Stark100% (1)
- Al n14 Corporate Reporting Exam PaperDocumento18 pagineAl n14 Corporate Reporting Exam Paperzilchhour0% (1)
- Contribution Rate Employee (12%)Documento4 pagineContribution Rate Employee (12%)Kiran MettuNessuna valutazione finora
- Oracle FAQsDocumento15 pagineOracle FAQsjhakanchanjsrNessuna valutazione finora
- Case 10 12 Restrictive Agreement in Employment ContractsDocumento5 pagineCase 10 12 Restrictive Agreement in Employment ContractsPaulino Belga IIINessuna valutazione finora
- Mayberry v. KKR (KRS Lawsuit)Documento146 pagineMayberry v. KKR (KRS Lawsuit)Insider Louisville0% (2)
- Australian Agriculture Visa FaqsDocumento11 pagineAustralian Agriculture Visa FaqsMay LoedvianNessuna valutazione finora
- Value of Life Sample Student EssaysDocumento10 pagineValue of Life Sample Student Essaysbananaboy2Nessuna valutazione finora