Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Guideline: Antibiotic Drug Monitoring: Aminoglycosides and Glycopeptides
Caricato da
KenRodulfReyesVillaruelTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
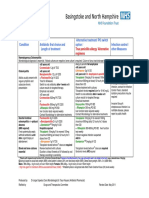
Guideline: Antibiotic Drug Monitoring: Aminoglycosides and Glycopeptides
Caricato da
KenRodulfReyesVillaruelCopyright:
Formati disponibili
Pharmacy
Guideline
Antibiotic drug monitoring:
aminoglycosides and glycopeptides
1 Scope
Trust-wide.
2 Purpose
To improve the prescribing and monitoring of antibiotics with narrow
therapeutic indices.
3 Definitions
IV intravenous
mg milligrams
mg/kg milligrams per kilogram
OD once a day
PO orally
BD twice a day
TDS three times a day
QDS four times a day
stat immediately
4 Guideline
Please refer to the antibiotic drug monitoring: Aminoglycosides and
glycopeptides guideline at the end of this document.
5 Responsibilities
All staff involved in the prescribing and monitoring of antimicrobials are
expected to adhere to the guidelines and seek expert advice if necessary.
6 Monitoring compliance with and the effectiveness of
this document
Prescribing of antibiotics is reviewed routinely for adherence to policy which
offers the measurable standard in terms of recommended prescribing
practices.
Cambridge University Hospitals NHS Foundation Trust Page 1 of 8
Antibiotic drug monitoring: aminoglycosides and glycopeptides
Version 4; Approved May 2016
Pharmacy
This review is achieved on daily ward rounds and more formally through an
annual audit programme.
The Trust antibacterial stewardship group (ASG), which reports to the joint
drug and therapeutics committee (JDTC), is responsible for review of the
policy and receiving audit returns. Audits are reported to directorates for
necessary interventions.
7 References
Drugdex: Vancomycin monograph
Gould F.K. et al. Guidelines for the antibiotic treatment of endocarditis in
adults: a report of the Working Party of the British Society for Antimicrobial
Chemotherapy. Journal of Antimicrobial Chemotherapy 2012. 67:269-289
Leeds Teaching Hospitals NHS Trust: Vancomycin Prescribing Guidelines
November 2009
SPC Vancomycin available at www.medicines.org.uk
Thompson A.H et al. Development and evaluation of vancomycin dosage
guidelines designed to achieve new target concentrations. Journal of
Antimicrobial Chemotherapy. 2009:63,1050-1057
Rybak M. et al. Therapeutic monitoring of vancomycin in adult patients: a
consensus review of the American Society of Health-System Pharmacists,
the Infectious Diseases Society of America, and the Society of Infectious
Diseases Pharmacists. Am J Health-Syst Pharm. 2009; 66:82-98
Renal Drug Handbook, 3rd Edition.
Gilbert D. and Leggett J.E in Mandell, Douglas and Bennett’s Principles and
Practice of Infectious Diseases. 7th Edition. Chapter 26 – Aminoglycosides.
The Sandford Guide to Antimicrobial Therapy 2009. 39th Edition
Equality and diversity statement
This document complies with the Cambridge University Hospitals NHS
Foundation Trust service equality and diversity statement. January 2013
Disclaimer
It is your responsibility to check against the electronic library that this
printed out copy is the most recent issue of this document.
Document management
Approval: Antimicrobial stewardship group (ASG), 09 May 2016
Owning department: Pharmacy
Author(s): Reem Santos, Antibiotic Pharmacist;
Denise Rosembert, Lead Pharmacist- Biologics (and Application Analyst)
File name: Antibiotic drug monitoring Aminoglycosides and glycopeptides Version4 May
2016 (1of2).doc
Supersedes: Version 3, January 2014
Version number: 4 Review date: May 2019
Local reference: Media ID: 20827
Cambridge University Hospitals NHS Foundation Trust Page 2 of 8
Antibiotic drug monitoring: aminoglycosides and glycopeptides
Version 4; Approved May 2016
Dosing and drug monitoring of selected antibiotics in
adults
Vancomycin and Teicoplanin
General information
Dosing should take into account the type of infection, the patient’s weight and renal function.
Teicoplanin is restricted for use in patients requiring glycopeptide therapy but are allergic to
vancomycin or candidates for Outpatient Parenteral Antimicrobial Therapy (OPAT).
Caution is advised when using glycopeptides with other nephrotoxic drugs. This includes
gentamicin, NSAIDS, liposomal amphotericin or loop diuretics. Close monitoring for nephrotoxicity
is recommended.
Paediatric patients are excluded from this guideline (consult a pharmacist for dose
recommendations).
Note that patients receiving oral vancomycin for treatment of C. difficile associated diarrhoea do not
normally require levels checked.
STEP 1: LOADING DOSE
Give a loading dose based on the patient’s actual body weight (table 1 below for details).
Loading are not recommended for patients with CrCl < 20 ml/min
LOADING DOSE
Weight (Actual body weight) <60 kg 60-85 kg > 85kg
Vancomycin (single dose IV) 1g 1.5g 2g
400mg 600mg
Teicoplanin loading dose regimen
(600mg for serious infections)
(3 doses at 12-hourly intervals)
Teicoplanin loading doses are traditionally 3 doses at 12-hourly intervals.
Alternative loading dose regimens may be employed by the OPAT team.
Antibiotic drug monitoring
STEP 2: CONTINUATION PHASE
Dose patient according to body weight and renal function
DOSE RECOMMENDATIONS
Vancomycin Teicoplanin†
Standard dosing based on weight
15mg/kg* (max 2g per doseª) <85kg: 400mg**
(round up to nearest 250mg) ≥85kg: 6mg/kg*
Dose (round up to nearest 100mg)
ª In severe renal impairment (CrCl < 10 ml/min)
max 1g per dose For doses above 1g, please consult Microbiology,
Infectious Diseases or a Pharmacist before
prescribing
Based on renal function for adult patients <65
yrs:
CrCl >50 ml/min: twice daily
CrCl 10-50 ml/min or patients >65 yrs if Give standard loading dose then adjust dosing
CrCl >50 ml/min: once daily interval depending on renal function:†
CrCl <10 ml/min and in patients undergoing CrCl >20 ml/min: continue once daily
Interval renal replacement therapies: single dose and CrCl 10-20 ml/min: reduce dose to 400mg
then check level 24h later, give next dose every 24-48 hours
once trough level <20mg/L CrCl <10 ml/min and in patients undergoing
renal replacement therapies: reduce dose to
Note that all patients >65 yrs with ‘normal 400mg every 48-72 hours
renal function’ should have once daily
vancomycin as per CrCl 10-50 ml/min
Check pre-dose (trough) levels routinely∆ Check pre-dose (trough) levels only if treatment
Timing of CrCl >50ml/min: before 4th dose is likely to exceed 10 days‡
levels CrCl 10-50ml/min: before 3rd dose
CrCl <10 ml/min: before the 2nd dose Pre-dose (trough) levels should be taken after 7
days of therapy
Reference 10-20 mg/L
20-60 mg/L
range (15-20mg/L for Staph aureus infections)
* Use actual body weight however for obese patients with a BMI >40, use ‘adjusted body weight’ . See separate section
below for calculation formulae.
** Higher doses may be recommended in bone or joint infections. Refer to OPAT antibiotic guideline for further details
† For patients with renal impairment, dose adjustment is not required until the fourth day of treatment.
‡ Levels should only be collected Monday to Thursday as the assay is sent to the Antimicrobial Reference Unit in Bristol.
∆
Do not await results of levels before administering the next dose of vancomycin unless severe renal impairment with
CrCl <10ml/min
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
.
Vancomycin and Teicoplanin
STEP 3: AMEND DOSE (IF INDICATED) ACCORDING TO ASSAY RESULT
VANCOMYCIN: INTERPRETATION OF TROUGH LEVELS
Pre-dose
Maintenance dose adjustment
(trough) level
<10 mg/L Subtherapeutic level.
Reassess dose according to renal function. Alternatively, consider increasing
the dose by 500mg increments (as a once daily dose or divided doses).
In some cases where borderline results are reported, administering the same
daily dose at more frequent intervals can lead to therapeutic levels e.g. 1.5g
BD amended to 1g TDS.
Re-assay after third dose.
10-20 mg/L Optimum dose: continue on current dose
Re-assay once or twice weekly if renal function remains stable
For severe infections involving MRSA pneumonia, osteomyelitis, endocarditis
and bacteraemias, adjust dose to achieve an optimal target concentration of
15-20 mg/L
20-25 mg/L Above recommended target level.
Amend regimen by extending the dosage interval (e.g. from BD to OD). Re-
assay after third dose or more frequently if renal function has deteriorated.
>25 mg/L Above recommended target level.
Omit next dose and re-evaluate dosing regimen. Re-assay after 24 hours. Do
not give further doses until level reported to be <20mg/L.
TEICOPLANIN: INTERPRETATION OF TROUGH LEVELS
Antibiotic drug monitoring
Pre-dose
Maintenance dose adjustment
(trough) level
<20 mg/L Subtherapeutic level, especially if treating severe infections
Increase dose by 50%, round up to nearest 100mg†
Re-assay after 5 doses.
20-60 mg/L Optimum dose: continue on current dose
Re-assay not required within 4 weeks unless change in renal function
>60mg/L Above recommended target level.
Reassess dose according to renal function. Consider reducing the daily dose or
extending the dosage interval (eg from daily to every 48 hours). Re-assay
after 5 days.
†Teicoplanin dose can be increased up to 800mg daily. For further advice, consult a pharmacist,
Microbiology or the Infectious Diseases Team.
Instructions to Biochemistry
Instructions for sending trough (pre-dose) samples to biochemistry
Send serum sample (brown top bottle)
The following information is necessary to allow results to be interpreted: -
The time that the last dose was administered
The time that the sample was taken
The dosage regimen that the patient is receiving
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
Once Daily Aminoglycosides
Background
Once daily dosing for aminoglycosides has gained popularity in recent years due to several
factors. The simplified dosing regimen is not as labour-intensive as the multiple daily
dosing. The aim of once daily dosing is to minimise toxicity, reduce treatment failure,
morbidity and mortality.
The rationale for using once daily dosing has many advantages including concentration
dependent bactericidal activity, where the efficacy correlates with achieving drug plasma
levels 5-10 fold greater than the minimum inhibitory concentration (MIC) of the pathogen.
The post-antibiotic effect of aminoglycosides against Gram-negative bacilli is another
feature that translates to continued suppression of bacterial growth even in the presence
of declining aminoglycoside concentration.
The toxicity profile of once daily dosing appears to incur benefit. The renal cortical uptake
of gentamicin, amikacin (but not tobramycin) is saturable and the renal accumulation
appears to be less when given in one large dose compared to divided doses or continuous
infusions. This has resulted in less nephrotoxicity. Similar effects have been noted with
regard to ototoxicity.
Caution for once daily aminoglycosides
Patients with established renal failure. Refer to table below for dosing guidance.
The recommended doses are to be used as a guide only for initial prescribing, with
doses reviewed in light of reported trough levels and alterations in renal function.
Antibiotic drug monitoring
Exclusions
This guideline dose not offers any dose recommendations for Cystic Fibrosis patients,
paediatrics or for surgical prophylaxis.
Contraindications to single daily dose regimen of
aminoglycosides
An alternative antibiotic should be used if possible in the following patients:
Pregnancy
Patients with extensive burns (>20% of body surface area)
Blind patients
Patients with a history or signs of hearing loss or vestibular dysfunction
Discuss therapy with a medical microbiologist if it is thought that the use of
aminoglycoside is still indicated in this group of patients, as traditional (conventional)
aminoglycoside dosing regimens will apply.
Patients with endocarditis also have different aminoglycoside dosing regimens and target
levels; see Cardiovascular infections guideline.
Avoid giving prolonged courses of aminoglycosides (>7-10 days) as this is
associated with increased risk of oto- and nephrotoxicity; discuss alternative
options with Microbiology.
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
Once Daily Aminoglycosides
The doses below are a guide only. Doses should be based on ideal body weight or actual body
weight if patients are considered underweight (see formula below or use UKMI web based
calculator http://www.ukmicentral.nhs.uk/resource/culo.htm) and adjusted according to trough
levels. Seek the advice of a Pharmacist or a Microbiologist.
Normal Renal Moderate Renal
Mild Renal Severe Renal
function Impairment
Impairment Impairment
(CrCl (CrCl 10-
(CrCl 20-40ml/min) (CrCl <10ml/min)
>40ml/min) 20ml/min)
5mg/kg every 24
Gentamicin hours (max
500mg) 2mg/kg single dose
3mg/kg every 48
every 72 hours with
5mg/kg every 24 3mg/kg every 24 hours hours
daily trough levels
Tobramycin hours (max
500mg)
15mg/kg IV every
10mg/kg every 24 3-4mg/kg every 24 2mg/kg every 24 to 48
Amikacin* 24 hours (max
hours hours hours
1.5g)
* Maximum cumulative dose of amikacin is 15g
Regardless of body weight, no single dose of gentamicin or tobramycin should exceed 500mg
Additional dosing information
For adult patients round dose to nearest 40mg for gentamicin and tobramycin, and nearest 50mg for amikacin.
For obese patients (BMI>40), using ‘adjusted body weight’ may be more appropriate. Contact Microbiology for advice.
Patients on renal replacement therapies
For patients on renal replacement therapies requiring repeated dosing (in excess of a single dose) contact Pharmacy for
advice.
Instructions for sending trough (pre-dose) samples to biochemistry
Send serum sample (brown top bottle)
Antibiotic drug monitoring
The following information is necessary to allow results to be interpreted: -
The time that the last dose was administered
The time that the sample was taken
The dosage regimen that the patient is receiving
Trough (pre-dose) levels
When initiating therapy, take the first level 24 hours after the last dose and DO NOT GIVE A FURTHER DOSE –
AWAIT RESULT OF LEVEL. If within normal limits, subsequent dosing can be given while awaiting results provided
renal function is stable.
Peak levels (post dose)
DO NOT SEND POST DOSE LEVELS FOR PATIENTS ON ONCE DAILY AMINOGLYCOSIDE ADMINISTRATION unless treating
for bacterial endocarditis. See separate guidance on Connect.
Frequency of therapeutic drug monitoring
Twice to thrice weekly serum creatinine and aminoglycoside monitoring is recommended if renal function is stable.
In renal impairment or deteriorating renal function, daily trough levels will be necessary.
Deteriorating renal function while on aminoglycoside therapy
Discuss alternative regimens with Microbiology or the Trust Antibiotic Pharmacist.
AMIKACIN trough levels
<5mg/L 5-10mg/L >10mg/L
GENTAMICIN and TOBRAMYCIN trough level interpretations
<1mg/L 1-2mg/L >2mg/L
Continue on current dosage Borderline Unsatisfactory
regimen.
Extend dose to 36 hourly. Change to an alternative agent
Recheck trough (pre) level in 3 if possible or discuss use of
days time and give next dose. Recheck trough (pre) level lower dose regimen with a
before the next dose is due, Microbiologist or Pharmacist
The level can be checked sooner and give the next dose.
if there are signs of renal
deterioration.
Monitoring Auditory Function
Baseline auditory function tests should be considered in patients with suspected hearing deficit prior to commencement of
therapy. There should be a low threshold for checking auditory function with suspected toxicity; early cessation of
aminoglycoside therapy is strongly recommended in such instances.
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
Gentamicin multiple daily dosing for endocarditis
Where indicated, multiple daily dosing for gentamicin is recommended for treatment of
endocarditis, in combination with a beta-lactam or glycopeptides. Not all endocarditis cases
require an aminoglycoside (eg gentamicin) as part of a treatment regimen.
All patients with endocarditis should be referred to a cardiologist for evaluation. In
addition, Microbiology advice should be sought for all patients with endocarditis, especially
for patients with significant renal impairment where gentamicin is indicated.
The optimal antibiotic regimen will vary for each case and is dependent on whether the
patient has a native or prosthetic valve, as well as results of blood cultures and
susceptibility tests. The Trust’s guideline Antibiotic Therapy: Cardiovascular Infections
provides detailed advice on:
assessment
drug choice
prescribing and monitoring of patients with endocarditis
but decisions regarding treatment must be discussed and agreed with a microbiologist.
The table below provides dosing advice where gentamicin is recommended by
Microbiology.
DOSE RECOMMENDATIONS
Gentamicin
1mg/kg* 12-hourly (max 500mg in 24 hours)
(round to nearest 40mg)
Dose
Note: Reduce dose to 1mg/kg OD in patients with mild to severe renal impairment (CrCl
Antibiotic drug monitoring
<40 ml/min)
Pre and post dose serum levels are required.
Monitoring
Levels should be monitored at least three times a week
of levels
.
Post dose levels should be taken one hour after dose administration
Check pre-dose (trough) and post-dose (peak) levels routinely∆
before and after the second dose (do not withhold dose if indication is endocarditis)
thereafter: twice weekly (every third day) if levels are within range and renal function remains
Timing of stable
levels
For the majority of endocarditis patients treated with gentamicin the dose of drug should
continue to be administered whilst awaiting the results of the level, which should be
available within 24 hours.
Reference Pre-dose (trough): < 1 mg/L
range Post-dose (peak): 3-5mg/L
Please ensure that when ordering levels the correct option is selected on HISS or Web OCS. Ordering
levels for gentamicin pre-dose for endocarditis does not differ from once daily gentamicin, however
for post dose ‘peak’ levels the reference ranges differ markedly.
Ordering
levels Instructions for sending trough (pre-dose) samples to biochemistry
For pre-dose gentamicin, select: ‘gentamicin – pre dose’ or code ‘GentPRE’ as for once daily
gentamicin.
For post-dose gentamicin, select: ‘gentamicin endocarditis – post dose’ or code
‘GentPOSTEN’
Comments:
* Doses should be based on ideal body weight or actual body weight if patients are
considered underweight (see formula below or use UKMI web based calculator
http://www.ukmicentral.nhs.uk/resource/culo.htm) and adjusted according to trough levels. Seek
the advice of a Pharmacist or a Microbiologist.
For patients continuing to experience high trough or peak levels on either TDS or BD dosing, consult a
Pharmacist or Microbiologist for advice on appropriate dosage adjustments.
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
Index: Useful Calculation Guides and links
Creatinine clearance
Creatinine clearance should always be used for calculating the doses of potentially toxic
drugs with a narrow therapeutic index (eg aminoglycosides). Do NOT use eGFR for this
purpose, as it is likely to underestimate or overestimate renal function in obese or
underweight patients respectively.
Calculate creatinine clearance (ml/min) using Cockcroft-Gault equation below (or use eBNF calculator
http://cgeneral/bnf/lform1/current/index.htm - type ‘creatinine clearance calculator’ in the search
engine, then click on this when it appears in the left hand side).
MALE: 1.23 x (140 – Age) x ideal body weight* (kg)
Serum Creatinine (micromoles/L)
FEMALE 1.04 x (140 – Age) x ideal body weight* (kg)
Serum Creatinine (micromoles/L)
* Use actual body weight if ideal body weight cannot be calculated (e.g. height not
available) or patient is underweight. ‘Adjusted body weight’ should be used for obese
patients (BMI >40). Use the eBNF to search for ‘Body Mass Index’ calculator.
Alternatively, see separate section below for calculation formulae.
How to calculate Ideal and Adjusted Body Weight
IDEAL BODY WEIGHT (IBW)
Male IBW (kg): 50 + [(2.3 x height in cm above 152.4)/2.54]
Antibiotic drug monitoring
Female IBW (kg): 45.5 + [(2.3 x height in cm above 152.4)/2.54]
Example: A male of 172cm weighing 70kg
IBW = 50 + [(2.3 x (172-152.4)/2.54] = 67.7kg
Alternatively, for electronic calculator click on UKMI link
http://www.ukmicentral.nhs.uk/resource/culo.htm
ADJUSTED BODY WEIGHT (ABW) - for BMIs >40
Adjusted body weight = Ideal body weight + 0.4 (Actual body weight – Ideal
body weight)
Example: A female of 168cm weighing 180kg
IBW (kg) = 45.5 + [(2.3 x 168-152.4)/2.54] = 59.6kg
Adjusted body weight (kg) = 59.6 + 0.4(180-59.6) = 107.8kg
To convert inch and foot to cm:
1 inch = 2.54cm
1 foot = 30.48cm
References
1. Drugdex: Vancomycin monograph
2. Leeds Teaching Hospitals NHS Trust: Vancomycin Prescribing Guidelines November
2009
3. SPC Vancomycin
4. Thompson A.H et al. Development and evaluation of vancomycin dosage guidelines
designed to achieve new target concentrations. Journal of Antimicrobial
Chemotherapy. 2009:63,1050-1057
5. Rybak M. et al. Therapeutic monitoring of vancomycin in adult patients: a
consensus review of the American Society of Health-System Pharmacists, the
Infectious Diseases Society of America, and the Society of Infectious Diseases
Pharmacists. Am J Health-Syst Pharm. 2009; 66:82-98
6. Renal Drug Handbook, 3rd Edition.
7. Gilbert D. and Leggett J.E in Mandell, Douglas and Bennett’s Principles and Practice
of Infectious Diseases. 7th Edition. Chapter 26 – Aminoglycosides.
8. The Sandford Guide to Antimicrobial Therapy 2009. 39th Edition.
Antibiotic drug monitoring guideline; Version 4; Approved May 2016
Potrebbero piacerti anche
- 311 Topotecan Monotherapy 5 DayDocumento4 pagine311 Topotecan Monotherapy 5 DayRuxandra BănicăNessuna valutazione finora
- Heparin Dose Adjustment in The Prescence of Renal ImpairmentDocumento5 pagineHeparin Dose Adjustment in The Prescence of Renal ImpairmentRPR KSVNessuna valutazione finora
- Enoxaparin Info SheetDocumento7 pagineEnoxaparin Info SheetjafarkassimNessuna valutazione finora
- Aminoglycoside & VancomycinDocumento10 pagineAminoglycoside & VancomycinKhor Chin PooNessuna valutazione finora
- Nursing ResponsibilitiesDocumento4 pagineNursing ResponsibilitiesMaureen Joy Cascayan EspirituNessuna valutazione finora
- Antibiotik For Renal FailureDocumento6 pagineAntibiotik For Renal FailureWidhy Joss BangetzNessuna valutazione finora
- Teicoplanin Dosing and Monitoring in AdultsDocumento3 pagineTeicoplanin Dosing and Monitoring in Adultsdps_1976Nessuna valutazione finora
- Targocid Article 30 Referral Annex III - enDocumento32 pagineTargocid Article 30 Referral Annex III - enDR JAMAL WARISNessuna valutazione finora
- CHLVPP (Hodgkin'S Lymphoma) : (Max: 10Mg) (Max: 10Mg)Documento3 pagineCHLVPP (Hodgkin'S Lymphoma) : (Max: 10Mg) (Max: 10Mg)Sindu SankarNessuna valutazione finora
- Leukemia Treatment Regimens 7937Documento3 pagineLeukemia Treatment Regimens 7937Irfan FathurrahmanNessuna valutazione finora
- NICU Drugs GuideDocumento49 pagineNICU Drugs GuideArhanNessuna valutazione finora
- Vancomycin: Group 5 R.M 2Documento31 pagineVancomycin: Group 5 R.M 2vi_wiviaNessuna valutazione finora
- Ovarian Cancer Treatment Regimens - Print Article - Cancer Therapy AdvisorDocumento5 pagineOvarian Cancer Treatment Regimens - Print Article - Cancer Therapy AdvisorAnonymous g1hIPZNessuna valutazione finora
- Chemotherapy Protocol: RegimenDocumento6 pagineChemotherapy Protocol: RegimenAlexandra AndronescuNessuna valutazione finora
- Beacopp Hem HL ADocumento8 pagineBeacopp Hem HL AAnonymous 9dVZCnTXSNessuna valutazione finora
- Id 397 TeicoplaninDocumento2 pagineId 397 TeicoplaninStacey WoodsNessuna valutazione finora
- Intravenous Vancomycin Use in Adults - 2017Documento4 pagineIntravenous Vancomycin Use in Adults - 2017Angy KarakostaNessuna valutazione finora
- Capecitabine 14 DayDocumento6 pagineCapecitabine 14 DaybrystyyNessuna valutazione finora
- Enoxaparin - Prescribing, Administration and MonitoringDocumento6 pagineEnoxaparin - Prescribing, Administration and MonitoringFaheem AlsabriaNessuna valutazione finora
- ALIPIT Midterm Exam April 8,2020Documento1 paginaALIPIT Midterm Exam April 8,2020Jude Micko Bunyi AlipitNessuna valutazione finora
- UKMi-Gentamicin InfoDocumento4 pagineUKMi-Gentamicin InfoAmisha VastaniNessuna valutazione finora
- Vancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., PharmDocumento78 pagineVancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., Pharmkharbosham100% (1)
- L 51 R Hypercvad R MaDocumento7 pagineL 51 R Hypercvad R MaMohamed MahmoudNessuna valutazione finora
- Class Indications: GentamicinDocumento3 pagineClass Indications: GentamicinBer Anne Jaropojop TahilNessuna valutazione finora
- Clinical Guideline For Vancomycin Prescribing and Therapeutic Drug MonitoringDocumento11 pagineClinical Guideline For Vancomycin Prescribing and Therapeutic Drug MonitoringFate ChanNessuna valutazione finora
- 1.13 Hyper-CVAD-MA Version 2.1Documento5 pagine1.13 Hyper-CVAD-MA Version 2.1Alina CrissNessuna valutazione finora
- Pharmacokinetic Training Packet For PharmacistsDocumento24 paginePharmacokinetic Training Packet For PharmacistsGlory Claudia KarundengNessuna valutazione finora
- Neratinib Adjuvant Treatment Breast Cancer Protocol V1.1Documento6 pagineNeratinib Adjuvant Treatment Breast Cancer Protocol V1.1smokkerNessuna valutazione finora
- Medication Fact Sheets: 3rd Edition ContributorsDocumento50 pagineMedication Fact Sheets: 3rd Edition ContributorsIndumathi ThangathirupathiNessuna valutazione finora
- Aida Protocol For Apl: InductionDocumento4 pagineAida Protocol For Apl: InductionGabrielNessuna valutazione finora
- Bone and Joint Infections BNHFT 2010 PDFDocumento3 pagineBone and Joint Infections BNHFT 2010 PDFDanissa Fidia PuteriNessuna valutazione finora
- CetuximabDocumento8 pagineCetuximabcrespo2816100% (1)
- Therapeutic Drug Monitoring and Pharmacokinetics of Intravenous Vancomycin For Pharmacists and Other Healthcare ProfessionalsDocumento3 pagineTherapeutic Drug Monitoring and Pharmacokinetics of Intravenous Vancomycin For Pharmacists and Other Healthcare Professionalsminhmap90_635122804Nessuna valutazione finora
- Accofil Epar Product Information enDocumento155 pagineAccofil Epar Product Information endora192424Nessuna valutazione finora
- Tuberculosis Treatment GuidelinesDocumento2 pagineTuberculosis Treatment GuidelinesMaverick CaoileNessuna valutazione finora
- ABVDDocumento3 pagineABVDEsther WanguiNessuna valutazione finora
- Azithromycin Monograph - PaediatricDocumento7 pagineAzithromycin Monograph - PaediatrictynNessuna valutazione finora
- K25. Malaria Pada AnakDocumento39 pagineK25. Malaria Pada AnakayapillaiNessuna valutazione finora
- Merck Manual: Professional VersionDocumento25 pagineMerck Manual: Professional VersionDwina Wiranti PutriNessuna valutazione finora
- Cilastati Imipenem Drug InfoDocumento19 pagineCilastati Imipenem Drug InfoCosmina GeorgianaNessuna valutazione finora
- Effect DoseDocumento30 pagineEffect DoseXyprus Darina VeloriaNessuna valutazione finora
- GentamiciniDocumento11 pagineGentamiciniBenjie SisonNessuna valutazione finora
- Revision 1Documento21 pagineRevision 1NaifmxNessuna valutazione finora
- Teicoplanin Prescribing and Therapeutic Drug Monitoring Clinical Guideline V2.0 March 2019Documento12 pagineTeicoplanin Prescribing and Therapeutic Drug Monitoring Clinical Guideline V2.0 March 2019nancy voraNessuna valutazione finora
- Kanamycin (Mode of Administration)Documento3 pagineKanamycin (Mode of Administration)Waseem MaroofiNessuna valutazione finora
- Aminogycoside AntibioticsDocumento31 pagineAminogycoside AntibioticsNurul Febrina100% (2)
- Ribociclib Protocol CRP13 B034 v1.0Documento4 pagineRibociclib Protocol CRP13 B034 v1.0Joana JohnNessuna valutazione finora
- L 44 Bendamustine 70 R CLLDocumento7 pagineL 44 Bendamustine 70 R CLLsatishNessuna valutazione finora
- ClarithromycinDocumento4 pagineClarithromycinGAYATHIRINessuna valutazione finora
- Final Anti TB in SP - SituationDocumento50 pagineFinal Anti TB in SP - SituationAbdul JalilNessuna valutazione finora
- Drug Use in Renal and Hepatic Disorders.: Chapter-VDocumento30 pagineDrug Use in Renal and Hepatic Disorders.: Chapter-VBandameedi RamuNessuna valutazione finora
- BendamustineDocumento2 pagineBendamustineagusjatNessuna valutazione finora
- Castration-Recurrent Prostate Cancer First-Line Therapy: No Visceral MetastasesDocumento2 pagineCastration-Recurrent Prostate Cancer First-Line Therapy: No Visceral Metastasesalberto cabelloNessuna valutazione finora
- New Zealand Data Sheet: 1. Product NameDocumento15 pagineNew Zealand Data Sheet: 1. Product NameMhd IjlalNessuna valutazione finora
- DurhamDocumento6 pagineDurhamAdrianus NyomanNessuna valutazione finora
- Therapeutic Drug MonitoringDocumento10 pagineTherapeutic Drug MonitoringAnnie SethiNessuna valutazione finora
- Management of Reactions in Leprosy: How Should Lepra Reactions Be Managed?Documento2 pagineManagement of Reactions in Leprosy: How Should Lepra Reactions Be Managed?Echa AdityaNessuna valutazione finora
- How To RecoverDocumento3 pagineHow To RecoverSterr LiingNessuna valutazione finora
- This Is For The Most Amazing Woman I've Ever MetDocumento1 paginaThis Is For The Most Amazing Woman I've Ever MetKenRodulfReyesVillaruelNessuna valutazione finora
- Learning ContractDocumento1 paginaLearning ContractKenRodulfReyesVillaruelNessuna valutazione finora
- European SurgeryDocumento1 paginaEuropean SurgeryKenRodulfReyesVillaruelNessuna valutazione finora
- Guidelines For Completing Application Form For Personal ID / Access CardDocumento1 paginaGuidelines For Completing Application Form For Personal ID / Access CardKenRodulfReyesVillaruelNessuna valutazione finora
- The Heartstart Course hsc38d0318Documento19 pagineThe Heartstart Course hsc38d0318KenRodulfReyesVillaruelNessuna valutazione finora
- New Login Page and InterfaceDocumento2 pagineNew Login Page and InterfaceKenRodulfReyesVillaruelNessuna valutazione finora
- Labs Final NaDocumento5 pagineLabs Final NaKenRodulfReyesVillaruelNessuna valutazione finora
- Using The Glasgow Coma Scale For Patient AssessmentDocumento7 pagineUsing The Glasgow Coma Scale For Patient AssessmentJasmin Dela TorreNessuna valutazione finora
- OSCE Assessments Candidate Briefing - 1Documento4 pagineOSCE Assessments Candidate Briefing - 1KenRodulfReyesVillaruelNessuna valutazione finora
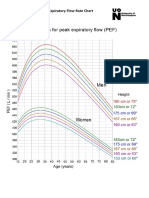
- Peak Expiratory Flow Rate Chart - 3Documento1 paginaPeak Expiratory Flow Rate Chart - 3KenRodulfReyesVillaruelNessuna valutazione finora
- Cambridge: Ad Astra 04/10/2019 10:15 Am 01 X Inf 4.50 G-10 Screen 2Documento1 paginaCambridge: Ad Astra 04/10/2019 10:15 Am 01 X Inf 4.50 G-10 Screen 2KenRodulfReyesVillaruelNessuna valutazione finora
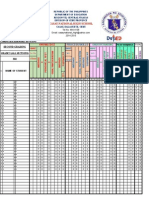
- Grade 6 Grading System NewDocumento344 pagineGrade 6 Grading System NewKenRodulfReyesVillaruelNessuna valutazione finora
- Casay National High School: KnowledgeDocumento2 pagineCasay National High School: KnowledgeKenRodulfReyesVillaruelNessuna valutazione finora
- Inflammatory & Immunology DisorderDocumento15 pagineInflammatory & Immunology DisorderRachelle Sarmiento GarciaNessuna valutazione finora
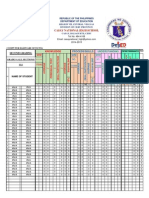
- k12 Grading Systelsam Sample1Documento1 paginak12 Grading Systelsam Sample1KenRodulfReyesVillaruelNessuna valutazione finora
- Grade Sheet 9Documento4 pagineGrade Sheet 9KenRodulfReyesVillaruelNessuna valutazione finora
- Torrent Downloaded From Demonoid - PHDocumento1 paginaTorrent Downloaded From Demonoid - PHRossella GiglioNessuna valutazione finora
- k12 Grading Systelsam Sample1Documento1 paginak12 Grading Systelsam Sample1KenRodulfReyesVillaruelNessuna valutazione finora
- Grade 9 GRADING SHEET TEMPLATEDocumento4 pagineGrade 9 GRADING SHEET TEMPLATEPrince Yahwe RodriguezNessuna valutazione finora
- k12 Grading Systelsam Sample1Documento1 paginak12 Grading Systelsam Sample1KenRodulfReyesVillaruelNessuna valutazione finora
- Summary of RatingDocumento1 paginaSummary of Ratingalvarez9654Nessuna valutazione finora
- Chlorpromazine Drug StudyDocumento3 pagineChlorpromazine Drug StudyEmJay Balansag100% (5)
- Pembagian Barang BPJS So Des 2019 Kfa MdoDocumento56 paginePembagian Barang BPJS So Des 2019 Kfa Mdokf ttrNessuna valutazione finora
- OralMeds - ChecklistDocumento6 pagineOralMeds - ChecklistXandra BasnilloNessuna valutazione finora
- Maximum Recommended Local Anaesthetic Doses For AdultsDocumento2 pagineMaximum Recommended Local Anaesthetic Doses For AdultsadithardanaNessuna valutazione finora
- 1 Pharmacy Practice Therapeutics OTC Drugs Q&A Content Ver1Documento123 pagine1 Pharmacy Practice Therapeutics OTC Drugs Q&A Content Ver1bhaveshnidhi64100% (1)
- Lindi HaksaDocumento5 pagineLindi HaksaLANCAR FOTOCOPYNessuna valutazione finora
- Analisis Waktu Tunggu Pelayanan Resep Rawat Jalan Di Instalasi Farmasi Rumah Sakit Bhayangkara ManadoDocumento7 pagineAnalisis Waktu Tunggu Pelayanan Resep Rawat Jalan Di Instalasi Farmasi Rumah Sakit Bhayangkara Manadodewi weny sariNessuna valutazione finora
- 03) Harga Program 13 Maret 2021-DikonversiDocumento5 pagine03) Harga Program 13 Maret 2021-DikonversiRahmawati FarmacyNessuna valutazione finora
- Experiment 8 Analgesic and Anti-Inflammatory WorksheetDocumento17 pagineExperiment 8 Analgesic and Anti-Inflammatory WorksheetJANNIE BELLE RODRIGUEZNessuna valutazione finora
- ASpectrumof Psychoactive Drugsin AyurvedaDocumento5 pagineASpectrumof Psychoactive Drugsin AyurvedaUPINDERJIT SINGHNessuna valutazione finora
- PharmacologyDocumento68 paginePharmacologyvansal liu80% (5)
- Drug Use During Pregnancy and LactationDocumento42 pagineDrug Use During Pregnancy and LactationMisbahuddin MohammadNessuna valutazione finora
- Cefuroxime, Levofloxacin, Esomeprazole, and Bismuth As First-Line Therapy For Eradicating Helicobacter Pylori in Patients Allergic To PenicillinDocumento9 pagineCefuroxime, Levofloxacin, Esomeprazole, and Bismuth As First-Line Therapy For Eradicating Helicobacter Pylori in Patients Allergic To PenicillinjerryNessuna valutazione finora
- Desensitization ADULT PDFDocumento28 pagineDesensitization ADULT PDFAnonymous 9dVZCnTXSNessuna valutazione finora
- Biosaar Product CardDocumento4 pagineBiosaar Product CardRakesh RockzzNessuna valutazione finora
- Topical Finasteride in The Treatment of Androgenic Alopecia. Preliminary Evaluations After A 16-Month Therapy CourseDocumento4 pagineTopical Finasteride in The Treatment of Androgenic Alopecia. Preliminary Evaluations After A 16-Month Therapy Coursenobody100% (2)
- Risk ManagmentDocumento5 pagineRisk ManagmentRhodora Benipayo100% (3)
- Babesia & Anaplasmosis TreatmentDocumento2 pagineBabesia & Anaplasmosis TreatmentUkya Ching MogNessuna valutazione finora
- D CalDocumento2 pagineD CalShay MNessuna valutazione finora
- DDD 1Documento17 pagineDDD 1Verqueza OdzongNessuna valutazione finora
- Ekatalog 2023 Sulsel RajawaliDocumento50 pagineEkatalog 2023 Sulsel RajawaliSafria HamzaNessuna valutazione finora
- Diagnosis Banding DepresiDocumento9 pagineDiagnosis Banding DepresiHarton MuhammadNessuna valutazione finora
- MCQ PharmacokineticsDocumento10 pagineMCQ PharmacokineticsHarshit Sharma100% (1)
- Autacoids (Local Hormones) and Their Pharmacolo-Gical ModulationDocumento75 pagineAutacoids (Local Hormones) and Their Pharmacolo-Gical ModulationAgung PutraNessuna valutazione finora
- Clinical Medications WorksheetsDocumento2 pagineClinical Medications WorksheetsMichael Kuzbyt0% (1)
- Guidance Format Risk Management Plan RMP Eu Integrated Format Rev 201 enDocumento51 pagineGuidance Format Risk Management Plan RMP Eu Integrated Format Rev 201 enJavierFlórezRNessuna valutazione finora
- Evolution in The Practice of Pharmacy - Not A Revolution!Documento2 pagineEvolution in The Practice of Pharmacy - Not A Revolution!Ana Sofia MartinsNessuna valutazione finora
- NafarinDocumento2 pagineNafarinianecunar100% (2)
- Org MedDocumento11 pagineOrg MedTsukishima KeiNessuna valutazione finora
- Dokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedDocumento54 pagineDokumen - Pub - Current Hospital Medicine Quick Guide For Management of Common Medical Conditions in Acute Care Setting 1stnbspedMahmoud FathyNessuna valutazione finora