Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
BMC Pedia
Caricato da
Renette UyDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
BMC Pedia
Caricato da
Renette UyCopyright:
Formati disponibili
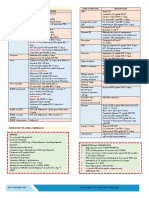
AMOXICILLIN CO-AMOXICLAV ZINC GLUCONATE CETIRIZINE UTI ANIMAL BITE
(+) WBC >5 hpf
250/5mL; 125/5 mL 157/5mL (125/5) 100mg/mL Drops 2.5/mL Urine culture 1st CAT II and III - Add nyo palagi sa Rx:
<1y.o. 100/mL 312/5mL (250/5) < 6 mos = 1mL Syrup 5mg/5mL Start: Amoxicillin or 1 insulin syringe
500mg cap; 250mg cap 457/5mL (400/5) 6-11 mos = 2mL 10 mg/tab Cefixime ( + fever) 1. ARV (Verorab) 0.1 cc ID
542.9/5mL (600/5) > 1 y.o. = 5mL 2. TT 0.5 mL IM
30-50 mkday (40 mkday) 625 mg/tab; 375 mg/tab wt x 0.25 mg ODHS x 5 days For Males: 1st time 3. ATS 1500 units/vial; if ≧6 y/o or if
Q8 x 7 days TID consider anatomic prob. for KUB UTZ no DPT vaccine
30-50 mkday (40 mkday) OMEPRAZOLE PROCATEROL 1-5 y/o #1
Q8 x 7 days TID 6-10 y/o #2
40mg/cap 5mcg/mL 11-16 y/o #3
CEFUROXIME CLOXACILLIN 1 mkdose > 16 y/o #4
wt x 0.25 4. Antibiotic
250/5mL 250/5mL BID x 5 days Cat II: Amoxicillin
125/5mL 125/5mL Cat III: Co-Amox/Cloxacillin/
125 mg/tab; 250 mg/tab; 500 mg/tab 250 mg/tab; 500 mg/tab SALBUTAMOL METRONIDAZOLE Cephalexin
20-40 mkday BID 50-100 mkday (50 mkday) 5. Mupirocin ointment TID x 7 days
Q12 x 7 days Q6 x 7 days QID ER: Q15 x 3 doses 125/5mL 6. ERIG or HRIG (for CAT III)
OPD: Q6 x 5 days QID __ mL Q8 for 10 days Q8 ERIG 5mL/vial: [(wt in kg) x 0.2]
ERYTHROMYCIN CLARITHROMYCIN HRIG 2mL/vial: [(wt in kg x 20)/150]
DIPHENHYDRAMINE AMBROXOL 5 days
100mg/mL 125/5mL CETIRIZINE 7 days HYPERSENSITIVITY COLDS
200/5mL 250/5mL 50 mg/amp MULTIVITAMINS
40-50 mkday (50 mkday) 15 mkdose 1 mkdose ASCORBIC ACID DIPHENHYDRAMINE 30 mg/IV DISUDRIM SYRUP
250 mg/tab; 500 mg/tab Q12 x 7 days BID ZINC 14 days HYDROCORTISONE 100mg/amp wt x 0.25 = __ mL
Q6 x 7 days QID wt x 1 = mg __ mL TID x 7 days
ex: 10 kg x 1 = 10mg IM EMPIRIIC DOSE Take-home meds:
CEFALEXIN CEFIXIME 0-3 mos. = 0.3 Q8 CETIRIZINE ODHS x 5 days
4-6 mos. = 0.6 Q12
250/5mL 100/5mL 7-9 mos. = 0.9 OD ABDOMINAL PAIN BRONCHIAL ASTHMA
25-50 mkdose (30) 200/5mL 10-12 mos. = 1.2 OD
Q6 x 7 days QID 200 mg/tab; 400 mg/tab 1-3 y.o. = 2.5 OD RANITIDINE OD SALBUTAMOL > 6 mos.
1.5-3mkdose 4-6 y.o. = 5 OD 15mg/5mL syrup SALBU + IPRA <6 mos.
Q12 x 7 days BID 7-10 = 7.5 OD 300 mg/tab HYDROCORTISONE
>10 = 10 OD PROCATEROL
IMMUNOMAX PROBIOTICS sachet
Food Supplement AZITHROMYCIN CIPROFLOXACIN ER:
Dissolve 1 sachet in 1/2 glass of SALBUTAMOL + IPRA neb (<6 mos.
Empiric dose: __ mL OD water 250/5mL 250 mg/tab; 500 mg/tab old) OR
For adol: 30 mg/cap Cell Life 10 mkday 10-15 mkday SALBUTAMOL neb(>6 mos. old)
Sachet: TID x 7 days __ mL OD x 3days Q12 x 5 days BID Q15 x 3 doses;
Tablet: BID x 7 days if not relieved → BUDESONIDE neb
Prolexin OD x 5 days PREDNISONE AMBROXOL 1 dose →
Erceflora TID x 5 days HYDROCORTISONE100mg
10mg/5mL Empiric dose TD (10-20)
PARACETAMOL ZINC SULFATE 5 mg/tab For adol: 15 mg/tab
20 mg/tab TID x 5 days TAKE HOME MEDS:
100mg/mL (drops) Drops (<6 mos) = 1mL Q12 x 5 days Salbutamol + Guaidensin
125/5mL Syrup (>6 mos) = 2mL 1 mkday (Ventolin) syrup
250/5mL 55mg/5mL wt x 0.25 = __ mL
10-20 mkday (10 mkdose) For >1 yr old use empiric dose __ mL TID x 3 days
Fever: Q4 for T≥37.8 Prednisone 10/5 mL (1 mkday)
_ mL OD x 14 days wt x 1 = __ mL
__ mL BID or TID x 3 days
Follow-up at OPD after 3 days
PGI Bea Tomboc
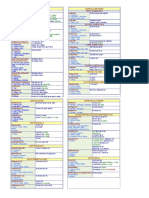
HYPERACIDITY APTHOUS ULCER ALLERGIC RASH SVI OR URTI
MAALOX 500 mg/tab BECLOMETHASONE SPRAY 2-4x HYDROCORTISONE OINTMENT SALBUTAMOL
Chew TID x 7 days; CLORHEXIDINE (ORAHEX) BID (Wt x 0.25) TID x 5 days OR
10mL BID mouthwash AMBROXOL SYRUP OR DROPS 3x
HEXIDINE (BACTIDOL) BID NPO a day
OMEPRAZOLE 20-40mg/tab OD (30 mins.) before and after meals AND
pre-breakfasr CARBENOXOLONE Na ZINC SULFATE (empiric dose)
(ROWAGEL) OD 14 days
HNBB 10mg/tab Q8 for 7 days apply 1-3x after meals and bedtime
— with tingling sensation at 1st; Follow-up after 7 days
expensive
ESSPRIN PEDIA 2 sprays/day x 7 Start Antibiotic if yellowish or
days greenish phlegm
KAMILLOSAN SPRAY 2 puff TID
after meals If at ff. up (+) cracles/rales after 7
NYSTATIN ORAL DROPS 2-3 drops days of Tx:
BID; no meals after. before CLARITHROMYCIN 15mkd/2 every
12 hrs for 7 days OR
DEWORMING AGE ERYTHROMYCIN 30-50 MKD/2
every 12 hours for 7 days
Begin at 1 yr and 3 mos. (15 mos), ORS
then 18 mos. then 24 mos. then <24 mos: 50-100mL every after each
yearly until 14 y/o loose stool/vomiting mkday = [ (mL given x numerator) ÷ denominator] ÷ weight
2-10 y/o: 100-200mL every after each
MEBENDAZOLE 11mkdose BID x 3 loose stool/vomiting Ex: wt = 16 kg, given 4 mL Paracetamol 250/5 mL
days >10 y/o: as much as wanted mkday = [ (4mL x 250) ÷ 5 ] ÷ 16 kg = 12.5 mkday, pasok sa mkday ng
ALBENDAZOLE 400 mg/tab Paracetamol na 10-20 mkd
< 2 y/o: 1/2 tab Approximate ORS can also be
>2 y/o: 1 tab computed by: NEPHROTIC SYNDROME (OPD)
*chewable 1 dose Wt. (in g) x 0.075 Get BP, weight, height, BSA
If vomiting: give ORS 10 mins. after
vomiting episode
ZINC SULFATE (empiric dose)
OD 14 days
PROBIOTICS (Cell Life)
RHD (OPD)
ATP OTITIS MEDIA S > +/- throat pain, fever, cough, colds
O > de kahon
CO-AMOXICLAV CO-AMOXICLAV A > RHD, NIF
__ mL TID x 7 days __ mL TID x 7 days P > For 2D echo after 1 yr
*Refer to ENT *Refer to ENT Pen G 1.2g IM
If (+) throat pain give Amox or Co-Amox
IIH ECZEMA
Get History and PE (SOAP pa din) MUPIROCIN OINTMENT
P > Inguinoscrotal UTZ TID x 7 days
Refer to Sx for further eval and mgt
FUNGAL RASH DIAPER RASH
CLOTRIMOXAZOLE BID ZINC OXIDE
Apply every after cleaning
PGI Bea Tomboc
PCAP (Read CPG) AGE (Read CPG)
PCAP A and B: Hydration (LUDAN’S METHOD)
Amoxicillin 40-50 mkday TID x 7 days OR
Azithromycin 10 mkday x 3 days MILD MODERATE SEVERE
If with hypersensitivity to Amox:
Clarithromycin 15 mkday BID x 7 days <15 kg 50 100 150
< 2 yrs. old
PCAP C:
If with completed HiB vaccine >15 kg 30 60 90
Pen G 100,000 units/kg/day in 4 divided doses >2 yrs. old
If with incomplete immunization or unkown immunization status; or patient is ≤6 D5 0.3 NaCl 1st hr 1/4 1st hr PLRS;
mos. 6-8 hrs PLRS; next 5-7 hr 2/3
Ampicillin 100 mkday in 4 divided doses next 5-7 hr 3/4 D5 0.3 NSS
D5LRS
Maintenance:
<15 kg: D5IMB
>15 kg: D5NM
USE:
MICROset: <10 kg; ≤ 60 microdrops
MACROdrops: > 10kg or > 60 microdrops; divided by 4, yun yung magiging
regulation
FORMULA: [(wt in kg) (multiplier, refer on table)] ÷ 6 or 8 hours = __
Ex:
16kg with MILD Dehydration
If 8 hrs hydration :
[(16) (30)] ÷ 8 hrs]= 60cc/hr; Order: start D5 0.3NaCl 500 cc x 60cc/hr for 8 hrs
8kg with MODERATE Dehydration
(8 kg x 100) ÷ 4 = 200
Order: Give PLR 1L to run for 200 cc/hr for 1 hr;
IVF to follow: D5LR to run for 200cc/hr for 7 hrs
12 kg with SEVERE Dehydration
(12 kg x 90) ÷ 3 = 360
Order: Start PLR 1L to run for 360 cc/hr for 1 hr;
IVF to follow: D5LR to run for 720cc/hr for 7 hrs
PGI Bea Tomboc
CFC (COMPLEX FEBRILE CONVULSION) PCAP-C DENGUE WITH WARNING SIGNS
Date and Time > Please admit to NEURO WARD Date and Time > Please admit to RESPI WARD Date and Time > Please admit to ISO-B1 or ADOL
PR: under the service of Dr. Cruda/Dr. BP: under the service of Dr. Angeles/Dr. BP: P50: WARD under the service of Dr.
RR: (Neuro rotator na resident) PR: (Respi rotator na resident) PR: P95: (Consultant In-Charge) /Dr.(Respi
T: > Secure consent for admission and RR: > Secure consent for admission and RR: rotator na resident)
O2 sat: management T: management T: D_ of illness > Secure consent for admission and
Wt: > Diet: NPO O2 sat: > Diet: NPO for 4 hrs then refer O2 sat: D_ afebrile management
> IVF: Assess degree of dehydration, Wt: > IVF: Assess degree of dehydration, Wt: > Diet: DAT except dark colored food
Physical Exam then refer then refer > (5) IVF: PLR 1L x __ gtts/min for 2
> Diagnostics: Physical Exam > Diagnostics: Physical Exam hrs then refer
A> Complex Febrile Convulsion CBC with PC 6 hrs. CBC with APC > Diagnostics:
Na,K,Cl, Ca post-ictal A> PCAP-C CXR-APL view A> DFS with Warning Signs CBC with APC OD
P > Admission CXR-APL view > Meds: > Meds:
UA P > Admission (100,000) Penicillin G __units TIV Q6 P > Admission Paracetamol syrup or tablet Q4 PRN
For LP ( ) ANST for T≥37.8
> Meds: OR (1) Ranitidine __ mg TIV Q8 PRN for
(100) Ceftriaxone __ mg TIV Q12 ( ) (100) Ampicillin __mg TIV Q6 abdominal pain
ANST Salbutamol neb Q4 > VS Q4
Paracetamol 100 mg TIV Q4 PRN for Zinc syrup __ mL OD > I&O Q shift
T≥37.8 Cetirizine syrup __ mL OD > Refer
Diazepam __ TIV PRN for seizure Paracetamol syrup or tablet Q4 PRN
episodes for T≥37.8 Resident’s trodat/PGI __
> May hook to O2 via nasal cannula > VS Q4
2-3 lpm PRN for seizure > I&O Q shift
> VS Q4 > Refer
> I&O Q shift
> Refer Resident’s trodat/PGI __
Resident’s trodat/PGI __
PGI Bea Tomboc
Potrebbero piacerti anche
- Pedia Notes PDFDocumento32 paginePedia Notes PDFFG ArciagaNessuna valutazione finora
- Ok Ok Notes PediaDocumento14 pagineOk Ok Notes PediaChristian PasicolanNessuna valutazione finora
- Notes On Common Pediatric Drugs FullDocumento1 paginaNotes On Common Pediatric Drugs FullfloramaeyecyecNessuna valutazione finora
- Pedia NotesDocumento9 paginePedia NotesJitendra ChaudharyNessuna valutazione finora
- ImportantPractical Notes PediaDocumento11 pagineImportantPractical Notes PediaJun JunNessuna valutazione finora
- Pedia NotesDocumento11 paginePedia NotesJohn Christopher Luces100% (1)
- PediaidiotnotesDocumento13 paginePediaidiotnotesLeiza Tabora96% (23)
- TicklerDocumento37 pagineTicklerLuis Elijah De CastroNessuna valutazione finora
- Drugs For Tickler PDFDocumento3 pagineDrugs For Tickler PDFBobet ReñaNessuna valutazione finora
- Dem Tickler NotesDocumento1 paginaDem Tickler NotesSeff CausapinNessuna valutazione finora
- Pedia Tickler 2 1 2Documento106 paginePedia Tickler 2 1 2Ma. Bernadette PinedaNessuna valutazione finora
- Tickler 20print 202Documento7 pagineTickler 20print 202Clav RamosNessuna valutazione finora
- Pedia TicklerDocumento66 paginePedia TicklerCharles Jebb Belonio JuanitasNessuna valutazione finora
- Pedia TicklerDocumento21 paginePedia TicklerorangepatieNessuna valutazione finora
- Moonlighting 101Documento20 pagineMoonlighting 101Dayanara Gener100% (1)
- Pedia EZ Notes PDFDocumento102 paginePedia EZ Notes PDFLuisa Paula LioanagNessuna valutazione finora
- TICKLER-PRINT Pedia PDFDocumento8 pagineTICKLER-PRINT Pedia PDFCarlos H. AcuñaNessuna valutazione finora
- OB NotesDocumento4 pagineOB NotesMaris Sarline OpenianoNessuna valutazione finora
- TicklerDocumento11 pagineTicklerJustine Issa YuNessuna valutazione finora
- Beta-Lactams Cephalosporins: Phenoxymethyl PenicillinDocumento3 pagineBeta-Lactams Cephalosporins: Phenoxymethyl PenicillinBobet ReñaNessuna valutazione finora
- Common Drugs Used in The Out Patient DepartmentDocumento1 paginaCommon Drugs Used in The Out Patient DepartmentRenatoCosmeGalvanJuniorNessuna valutazione finora
- Pedia TicklerDocumento71 paginePedia TicklermikayNessuna valutazione finora
- New Intern Guide Quick NotesDocumento8 pagineNew Intern Guide Quick NotesTrisNessuna valutazione finora
- Pedia NotesDocumento2 paginePedia NotesPaolo EvangelistaNessuna valutazione finora
- Fabella NotesDocumento96 pagineFabella NotesAndrassy Twinkle AlineaNessuna valutazione finora
- PEDIA ER FormularyDocumento1 paginaPEDIA ER FormularyAnonymous ic2CDkFNessuna valutazione finora
- Pedia MedicationsDocumento9 paginePedia MedicationsMichael Villavert100% (1)
- Cheat Sheet (Draft)Documento3 pagineCheat Sheet (Draft)bonziebuddyNessuna valutazione finora
- CPG PneumoniaDocumento31 pagineCPG PneumoniaJo Anne100% (3)
- Pediatric Tickler by RemDocumento7 paginePediatric Tickler by RemRem AlfelorNessuna valutazione finora
- Diabetes Mellitus CPGDocumento90 pagineDiabetes Mellitus CPGKristine-Joy Legaspi FrancoNessuna valutazione finora
- Pedia TicklerDocumento55 paginePedia TicklerMa Louize Magbanua100% (1)
- Tickler PDFDocumento177 pagineTickler PDFQueenie FarrahNessuna valutazione finora
- Medical Intern S Handy NotesDocumento23 pagineMedical Intern S Handy Notesdy dyNessuna valutazione finora
- Drugs & DosagesDocumento29 pagineDrugs & DosagesCristina VelasquezNessuna valutazione finora
- Pediatric Doses For Commonly Used OTCsDocumento7 paginePediatric Doses For Commonly Used OTCsCharles Xavier KimNessuna valutazione finora
- Pedia ComputationsDocumento5 paginePedia ComputationsRheenz Fornoles100% (1)
- Pedia NotesDocumento7 paginePedia NotesBonnyong MaNessuna valutazione finora
- Intern TicklerDocumento10 pagineIntern TicklerRem AlfelorNessuna valutazione finora
- Simplified Diagnostic Approach in Acute HepatitisDocumento2 pagineSimplified Diagnostic Approach in Acute HepatitisJohn Christopher LucesNessuna valutazione finora
- Formulas and DripsDocumento6 pagineFormulas and DripsStarlet Rhonadez Bito-onon Oriel100% (1)
- ORDERS (GTLMH Doctors)Documento4 pagineORDERS (GTLMH Doctors)Omie Calzum Yusoph100% (1)
- Pedia Idiot Notes 1Documento12 paginePedia Idiot Notes 1David JonesNessuna valutazione finora
- IV FLUIDS Drugs and DosagesDocumento3 pagineIV FLUIDS Drugs and Dosagesdoc_geloNessuna valutazione finora
- Clerks REVALIDA Review 2017Documento51 pagineClerks REVALIDA Review 2017Mara Medina - BorleoNessuna valutazione finora
- Pedia DosesDocumento7 paginePedia DosesSai Krishna MaddiralaNessuna valutazione finora
- Mcu-Fdt Medical Foundation Hospital Out Patient Services: Chief Complaint: History of Present IllnessDocumento2 pagineMcu-Fdt Medical Foundation Hospital Out Patient Services: Chief Complaint: History of Present IllnessvinbNessuna valutazione finora
- Tickler Final PDFDocumento29 pagineTickler Final PDFSerious LeoNessuna valutazione finora
- Pedia Codigo 2013Documento24 paginePedia Codigo 2013Denise CastroNessuna valutazione finora
- (HGT X 18.18) 140 Units 20Documento3 pagine(HGT X 18.18) 140 Units 20Jorelyn FriasNessuna valutazione finora
- RHU Blue Book 6 - 070852 1Documento14 pagineRHU Blue Book 6 - 070852 1Jm Jm100% (1)
- JI Chart OrdersDocumento4 pagineJI Chart OrdersMel BillonesNessuna valutazione finora
- AntibioticsDocumento7 pagineAntibioticsCeleste Largo Arayan-LedesmaNessuna valutazione finora
- DRUG Formulas Ivtt: Divide With The Number of Times The Drugs Will Be GivenDocumento7 pagineDRUG Formulas Ivtt: Divide With The Number of Times The Drugs Will Be Givenmaymay737Nessuna valutazione finora
- Pediatrics DrugsDocumento7 paginePediatrics DrugsWinz DolleteNessuna valutazione finora
- PedoDocumento2 paginePedoHenyo AkoNessuna valutazione finora
- ObatDocumento3 pagineObatsusiNessuna valutazione finora
- Pedia 2Documento4 paginePedia 2John Christopher LucesNessuna valutazione finora
- Pho Meds ListDocumento1 paginaPho Meds Listmister emdiNessuna valutazione finora
- Pharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamDa EverandPharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamValutazione: 5 su 5 stelle5/5 (1)
- Resitivity LogDocumento30 pagineResitivity LogMuhammad AneesNessuna valutazione finora
- N Giungas Presentation PDocumento73 pagineN Giungas Presentation PGustavo FuentesNessuna valutazione finora
- Inox Tester User Manual EP04Documento36 pagineInox Tester User Manual EP04Ramon PachecoNessuna valutazione finora
- Concrete TestingDocumento32 pagineConcrete TestingAveesh singh100% (1)
- Triple DivideDocumento16 pagineTriple DividePublic HeraldNessuna valutazione finora
- Performance of Volcanic Ash and Pumice Based Blended Cement Concrete in Mixed Sulfate EnvironmentDocumento11 paginePerformance of Volcanic Ash and Pumice Based Blended Cement Concrete in Mixed Sulfate EnvironmentXtem AlbNessuna valutazione finora
- Soil Report MSI 14 041Documento41 pagineSoil Report MSI 14 041frog15Nessuna valutazione finora
- h2 Physics DefinitionsDocumento7 pagineh2 Physics DefinitionsJerald LimNessuna valutazione finora
- Free Particle PropagatorDocumento2 pagineFree Particle PropagatorstephenbankesNessuna valutazione finora
- CHEM1Documento1 paginaCHEM1Cheena Francesca LucianoNessuna valutazione finora
- Studi Kasus Kandungan Formalin Pada Ikan Teri Nasi (Stolephorus Commersoni Lac.) Asin Kering Di Pasar Rau Serang Banten - DocDocumento4 pagineStudi Kasus Kandungan Formalin Pada Ikan Teri Nasi (Stolephorus Commersoni Lac.) Asin Kering Di Pasar Rau Serang Banten - DocRini YanuartiNessuna valutazione finora
- Job Safety Analysis Form: Law M. Mechanical Supervisor Alex A./ Egbejimi Adebayo PSCDocumento4 pagineJob Safety Analysis Form: Law M. Mechanical Supervisor Alex A./ Egbejimi Adebayo PSCChukwuma Emmanuel Onwufuju0% (1)
- (1967) History of The Lenz-Ising ModelDocumento13 pagine(1967) History of The Lenz-Ising ModelJakler NicheleNessuna valutazione finora
- Qsar/qspr DescriptorsDocumento25 pagineQsar/qspr DescriptorsBeatrizCamposNessuna valutazione finora
- Clean ROOM HVACDocumento40 pagineClean ROOM HVACAjay Sastry0% (1)
- LaMotte 1756 Fluoride Tracer PockeTester InstructionsDocumento16 pagineLaMotte 1756 Fluoride Tracer PockeTester InstructionsPromagEnviro.comNessuna valutazione finora
- 2015 JC2 H2 Carboxylic Acids and Derivatives Part 1 Tutorial (Teachers) UpdatedDocumento18 pagine2015 JC2 H2 Carboxylic Acids and Derivatives Part 1 Tutorial (Teachers) UpdatedJohnNessuna valutazione finora
- Cooling Tower Side Stream FiltrationDocumento5 pagineCooling Tower Side Stream FiltrationChandrakant JuikarNessuna valutazione finora
- SRM University: Part - A Answer ALL Questions (10 X 2 20 Marks)Documento2 pagineSRM University: Part - A Answer ALL Questions (10 X 2 20 Marks)Ruby SmithNessuna valutazione finora
- Problem Set 1 Data Regression and Numerical Integration - 2013Documento3 pagineProblem Set 1 Data Regression and Numerical Integration - 2013April TanjayNessuna valutazione finora
- Module 2.2A: Moles, Molar Mass and Avogadro's Number Alexandra Melise D. HulogDocumento17 pagineModule 2.2A: Moles, Molar Mass and Avogadro's Number Alexandra Melise D. HulogDarnell SimmonsNessuna valutazione finora
- Kash - LSADocumento6 pagineKash - LSAJ. S.Nessuna valutazione finora
- Mole Balance: Reaction Engineering CKB 20104Documento7 pagineMole Balance: Reaction Engineering CKB 20104Syafiq Hashim SpikerNessuna valutazione finora
- VSL Primary Gas StandardsDocumento59 pagineVSL Primary Gas Standards分析室信箱Nessuna valutazione finora
- Profile Projector: Prepared and Presented byDocumento25 pagineProfile Projector: Prepared and Presented byMuhammad FaridNessuna valutazione finora
- Alcohols, Phenols and Ethers - MCQs Test - 3Documento3 pagineAlcohols, Phenols and Ethers - MCQs Test - 3Prasant KumarNessuna valutazione finora
- D. Types of Tests On SandDocumento9 pagineD. Types of Tests On SandSandeepNessuna valutazione finora
- Dawlance Report1Documento17 pagineDawlance Report1engr_dkNessuna valutazione finora
- Physics Folio... Simple2 Yg MungkinDocumento15 paginePhysics Folio... Simple2 Yg MungkinMuhammad HaikalNessuna valutazione finora
- Sodium Hexameta Phosphate e CHB 038Documento1 paginaSodium Hexameta Phosphate e CHB 038Wasif KarimNessuna valutazione finora