Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
GPHT1 Inflammation
Caricato da
Rachel ManaloTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
GPHT1 Inflammation
Caricato da
Rachel ManaloCopyright:
Formati disponibili
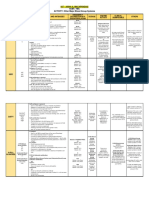
ACUTE & CHRONIC INFLAMMATION - Increased permeability
(Based on Dr. Unas’ Presentation) o Cellular Response
- Margination
INFLAMMATION - Rolling
o A response of vascularized tissues to infections and tissue - Adhesion
damage that brings cells and molecules of host defense from the - Transmigration
circulation to where they are needed - Migration
o Consists of vascular responses, migration and activation of
leukocytes, and systemic reactions STEPS OF THE INFLAMMATORY RESPONSE
o A protective response 1. Recognition
- Its goal is to remove the initial cause of injury as well as the 2. Recruitment of Leukocytes
necrotic cells and tissues resulting from the original insult, 3. Removal of the agent
and to initiate the process of repair 4. Regulation or control of the response
- Removes the consequences of injury 5. Resolution or Repair
o Although it helps clear infections and other noxious stimuli and
initiates repair, the inflammatory reaction and the subsequent
repair process can themselves cause considerable harm
o Important in tissue repair:
- Destroys or dilutes the wall of infectious process
- Sets in motion tissue repair (regeneration and scarring)
o Has unique features:
- Reaction of blood vessels
- Accumulation of fluids and electrolytes in the extravascular
space
Disorders Cells & Molecules Involved in
Injury
CARDINAL SIGNS OF INFLAMMATION
Acute
o Heat (Calor)
Acute Respiratory Distress Neutriphils
Syndrome o Redness (Rubor)
Asthma Eosinophils; IgE antibodies o Swelling (Tumor)
Glomerulonephritis Antibodies and complement; o Pain (Dolor)
neutrophils, monocytes o Loss of Function (Functio Laesa)
Septic Shock Cytokines
Chronic *Inflammation is terminated when the inciting agent is eliminated and
Arthritis Lymphocytes, macrophages; the mediators have degenerated
antibodies
Artherosclerosis Macrophages; lymphocytes ACUTE INFLAMMATION
Pulmonary Fibrosis Macrophages; fibroblasts o A rapid response to an injurious agent that aims to rapidly bring
mediators of inflammation to the site of injury
CAUSES OF INFLAMMATION o Major components:
o Infections - Dilatation of small blood vessels >> increased blood flow
o Tissue necrosis - Increased vascular permeability >> plasma proteins and
o Foreign bodies leukocytes leave circulation
o Immune reaction - Emigration, accumulation, and activation of neutrophils
o Infiltration by polymorphonuclear cells (neutrophils, eosinophils,
INFLAMMATION CONT’D basophils)
o Tissues and cells are involved in this reaction
- Fluid and plasma proteins, blood vessels, circulating cells STIMULI FOR ACUTE INFLAMMATION
(WBCs), CT cells (mast cells, fibroblasts, macrophages), o Infections
extracellular matrix (collagen, elastin), adhesive o Trauma
glycoproteins o Physical and chemical agents
o The cells and molecules of host defense including leukocytes and o Tissue necrosis
plasma proteins, normally circulate in the blood and the goal of o Foreign bodies
inflammatory reaction is to bring them to the site of infection or o Immune reactions
tissue damage
MEDIATORS OF ACUTE INFLAMMATION
COMPONENTS OF INFLAMMATORY RESPONSE o Substances that initiate and regulate inflammatory reactions
o Vascular Reaction - Vasoactive amines (Histamine and Serotonin)
- Vasodilation - Kinins (Bradykinin)
- Complement System (C3 and C3a) - Produced by proteolytic cleavage of precursors, mediate
vascular reaction, pain
Mediator Source Action
Vasodilation, ↑ Reaction of Inflammation Principal Mediators
Mast cells, vascular Vasodilation Histamine
Histamine basophils, platelets permeability, Prostaglandins
endothelial Histamine
activation Increased Vascular C3a and C5a (by liberating
Prostaglandins Vasodilation, pain, Permeability vasoactive amines from mast
fever cells, other cells)
Mast cells, ↑ vascular Leukotrienes 𝐶4 , 𝐷4 , 𝐸4
leukocytes permeability, TNF, IL-1
Leukotrienes chemotaxis, Chemotaxis, Leukocyte Chemokines
leukocyte adhesion, Recruitment and Activation C3a, C5a
and activation Leukotriene 𝐵4
Local: endothelial Fever IL-1, TNF
activation Prostaglandins
(expression of Pain Prostaglandins
Cytokines Macrophages, adhesion Bradykinins
(TNF, IL-1, IL-6) endothelial cells, molecules) Tissue Damage Lysosomal enzymes of
mast cells leukocytes
Systemic: fever, Reactive oxygen species
metabolic
abnormalities,
hypotension (shock)
Leukocytes, Chemotaxis,
Chemokines activated leukocyte activation
macrophages
Vasodilation, ↑
vascular
Platelet Activating Leukocytes, mast permeability,
Factor cells leukocyte adhesion,
chemotaxis,
degranulation,
oxidative burst
Leukocyte
chemotaxis and
activation, direct
Complement target killing
(membrane attack
Plasma complex),
(produced in the vasodilation (mast CLOTTING SYSTEM
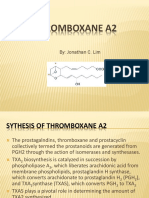
liver) cell stimulation) 1. Arachidonic Acid Metabolites
Kinins ↑ vascular - Prostaglandin, Prostacyclin, Thromboxane A2, Leukotrienes
permeability, (B4, C4, D4, and E4)
smooth muscle 2. Oxygen Metabolites
contraction, 3. Platelet Aggregating Factor
vasodilation, pain 4. Nitric Oxide
5. Cytokines
PRINCIPAL MEDIATORS OF INFLAMMATION - Interleukins, TNF
o Vasoactive Amines
- Vasodilation and ↑ vascular permeability HALLMARK OF ACUTE INFLAMMATION
o Arachidonic Acid Metabolites (PGs and Leukotrienes) o Dilation of small blood vessels
- Involved in vascular reactions, leukocyte chemotaxis and o Accumulation of leukocytes and fluid in the extravascular tissue
other reactions of inflammation
o Cytokines EDEMA
- Proteins produced by many cell types, multiple effects o Refers to an excess fluid in the interstitial tissue or serous cavities
mainly in leukocyte recruitment and migration
o Complement
EXUDATION
- Leads to generation of multiple breakdown products >>
o The escape of fluid, proteins and blood cells from the vascular
leukocyte chemotaxis, opsonization and phagocytosis
system into interstitial tissue or body cavities
o Kinins
o 2 types: exudate and transudate
Exudate Transudate
Protein Content High Low (Albumin) MUCINOUS/ CATARRHAL
Specific Gravity >1.020 <1.020 o When mucus hypersecretion accompanies acute inflammation
Cellular Inflammatory cells, None of a mucous membrane
Components cellular debris o Contains a large amount of mucous and epithelial cells
o Inflammatory conditions like allergenic rhinitis are common
PUS
o An exudate rich in inflammatory cells (leukocytes) and cellular TYPES OF INFLAMMATION ACCORDING TO LOCATION
debris ABSCESS
o Localized collection of pus in a part of the body surrounded by
MORPHOLOGIC PATTERNS an inflamed area
SEROUS o The area will most likely look like a giant boil or cyst that can
o Exudation of cell poor fluid into spaces created by cell injury or become extremely red and infected
into body cavities lined by the peritoneum, pleura or
pericardium ULCER
o May be derived from plasma (increased vascular permeability) o An open sore of the skin, eyes or mucous membrane often
or from mesothelial cells (local irritation) caused by an initial abrasion and generally maintained by an
o Accumulation of fluid >> effusion inflammation and/or an infection
o Early inflammation, heart failure, pleural effusions
CATARRHAL
PURULENT/ SUPPURATIVE o Mucosal surface
o The terms “suppurative” and “purulent” denote the production o Thick mucous and white blood cells
of pus, an exudate composed of neutrophils, liquefied debris of
necrotic cells and edema fluid MEMBRANOUS
o Caused by pyogenic bacteria o An epithelium becomes coated by fibrin, desquamated epithelial
o The pus may become walled-off by granulation tissue or fibrous cells and inflammatory cells
tissue to produce an abscess (a localized collection of purulent o An example is the grey membrane seen in pharyngitis or
inflammatory tissue) buried in a tissue, an organ or a confined laryngitis due to Corynebactrium diptheriae
space
o If a hollow viscus fills with pus, this is called an empyema PSEUDOMEMBRANOUS
o Formed by the fibrin and necrotic cell surface epithelium
FIBRINOUS o A structure which resembles the luminal surface of the tissue
o Increased vascular permeability >> large molecules pass out of (looks like the affected tissue is covered by a membrane)
the blood >> fibrin is deposited in extracellular space
o Develops when vascular leaks are large or there is a local TYPES OF INFLAMMATION ACCORDING TO DISTRIBUTION/
procoagulant stimulus LOCATION
o Characteristic of inflammation in the lining of the body cavities
FOCAL
(meninges, pericardium, pleura)
o Single abnormality/ inflamed area w/in tissue
o Forms eosinophilic meshwork of threads or sometimes as an o Size varies from 1mm to several centimeters in diameter
amorphous coagulum
o May be dissolved by fibrinolysis, if not lead to fibrosis MULTIFOCAL
o Often seen in acute pericarditis giving the parietal and visceral
o Arising from one/ pertaining to many foci (several foci separated
pericardium a “bread and butter” appearance
from one another)
o Size is variable
MEMBRANOUS o Each focus of inflammation is separated from the other
o Contains fibrinous or fibrinopurulent material with necrotic cells
o Often found in mucous membranes, some microbial infection LOCALLY EXTENSIVE
o Involvement of considerable area w/in an organ
SEROSANGUINOUS o Aka focally extensive
o Contains both serous and hemorrhagic materials o Possible origin:
o Caused by bleeding, serous exudation like injury and burns - Severe local rxns that spread into adjacent tx
- Coalescence of foci in a multifocal rxn
EXUDATES IN INFLAMMATORY PROCESSES
HEMORRHAGIC DIFFUSE
o Contains a large amount of RBCs and other cells o Involve all the tx/ organ in w/c the inflammation is present
o Damaged or vascular injury or permeable blood vessels or o Variations in severity may exist
depletion of coagulation factors o Interstitial pneumonia
o Acute pancreatitis due to proteolytic destruction of vascular
walls, and in meningococcal septicemia due to disseminated OUTCOMES OF ACUTE INFLAMMATION
intravascular coagulation
o Complete resolution SIMPLE RESOLUTION
o Healing by connective tx replacement (scarring/ fibrosis) o No destruction of normal tx
- Tissues incapable of regeneration o Offending agent is neutralized
- Abundant fibrin exudation in tissues/ cavities o Vessels return to their normal permeability state
o Progression to chronic inflammation o Excess fluid is reabsorbed
o Clearance of mediators & inflammatory cells
REGENERATION
o Replacement of lost/ necrotic tx w/ a new tx that is structurally
& functionally similar to those that were destroyed
o The intact, healthy neighboring cells surrounding the dead cells
will proliferate to replace the affected cells
REPLACEMENT BY A CT SCAR
o Formation of a new type of tx that causes fibrous scar production
w/ some loss of tx fxn
o Angiogenesis
o Migration & proliferation of fibroblasts
o Deposition of ECM
o Remodeling (reorganization of the fibrous tx, contraction of
CHRONIC INFLAMMATION wound edges)
o An inflammation of prolonged duration o Cicatrization
o Infiltration by mononuclear cells (macrophages, lymphocytes, - Formation of the mature scar
plasma cells) - Cicatrix
Scar
CAUSES OF CHRONIC INFLAMMATION Less vascular, pale, contracting scar tx
o Follows an acute inflammation o Epithelialization
o Repeated bouts of acute inflammation
- Persistent infections of intracellular microbes (tubercle SYSTEMIC EFFECTS OF INFLAMMATION
bacilli, viral infections) o Fever, increase in pulse & blood pressure, decreased in
- Prolonged exposure to non-degradable but potentially sweating, rigors, chills, anorexia, somnolence, malaise,
harmful substances (silicosis, asbestosis) lymphadenopathy
- Immune rxns (autoimmune diseases) o Increase plasma levels of acute phase proteins (CRP, serum
amyloid A protein)
MORPHOLOGIC OF CHRONIC INFLAMMATION o Leukocytosis
o Infiltration of mononuclear cells (macrophages, lymphocytes, o Sepsis
plasma cells, mast cells, eosinophils) o Shock
o Tx destruction
o Attempts at healing by CT replacement (angiogenesis & fibrosis) FACTORS MODIFYING THE INFLAMMATORY-REPARATIVE
RESPONSE
GRANULOMATOUS INFLAMMATION o Adequacy of blood supply
o A distinctive pattern of chronic inflammation o Nutritional status of the patient
o Characterized by formation of granulomas o Presence/ absence of infection
o Granuloma o Presence/ absence of diabetes mellitus
- Focal aggregation of activated macrophages w/c are o Presence/ absence of immunosuppressive drugs (ex.
transformed in an epithelial-like (epithelioid) cells glucocorticosteroids)
- Have an abundant pink cytoplasm o Adequate levels of circulating, normal fxning WBCs
- Surrounded by numerous lymphocytes & plasma cells
o Tuberculosis, leprosy, syphilis
o 2 types of granuloma:
- Foreign body granuloma
Caused by inert foreign bodies
Material (talc), sutures
No inflammatory/ immune rxns present
- Immune granuloma
Caused by immune T-cell mediated rxns
Insoluble particles (microbial parts)
Inflammatory rxns present
RESOLUTION INFLAMMATION (HEALING)
Potrebbero piacerti anche
- Dr. H. Soekimin, Sppa: Bagian Patologi Anatomi Fakultas KedokteranDocumento45 pagineDr. H. Soekimin, Sppa: Bagian Patologi Anatomi Fakultas KedokteranRommy Kurniawan DeskyNessuna valutazione finora
- Pathology ReviewDocumento26 paginePathology ReviewSafiya James100% (1)
- Inflammation: Deske MuhadiDocumento36 pagineInflammation: Deske MuhadiYUSMAWATI YUSRANNessuna valutazione finora
- Patologi AnatomiDocumento26 paginePatologi AnatomiNia AnestyaNessuna valutazione finora
- Inflammation PPT - OdpDocumento82 pagineInflammation PPT - OdpBhanu PraseedhaNessuna valutazione finora
- WaaazzzzzzDocumento21 pagineWaaazzzzzzSydjad Karl Ursal MiraflorNessuna valutazione finora
- Chronic Inflammation and RepairDocumento44 pagineChronic Inflammation and RepairFu Xiao Shan100% (1)
- InflammationDocumento2 pagineInflammationAndrew BonusNessuna valutazione finora
- Handouts - 6BIOM002W.2 - Inflammation 2018-9 PDFDocumento66 pagineHandouts - 6BIOM002W.2 - Inflammation 2018-9 PDFFatima HusseinNessuna valutazione finora
- Inflammation and RepairDocumento5 pagineInflammation and RepairDENILLE AIRA NOGOYNessuna valutazione finora
- Patho A 1. 3 Inflammation and Repair (Dy-Quiangco, 2015)Documento13 paginePatho A 1. 3 Inflammation and Repair (Dy-Quiangco, 2015)kristineNessuna valutazione finora
- Inflammation Inflammatory Response and FeverDocumento5 pagineInflammation Inflammatory Response and FeverPrincess Denice OrtalezaNessuna valutazione finora
- Muhammad Usman: Associate Professor of Pathology Consultant PathologistDocumento89 pagineMuhammad Usman: Associate Professor of Pathology Consultant PathologistSmithNessuna valutazione finora
- Chapter 2 - Acute and Chronic InflammationDocumento12 pagineChapter 2 - Acute and Chronic InflammationAgnieszka WisniewskaNessuna valutazione finora
- Physiology: Anatomy LectureDocumento4 paginePhysiology: Anatomy Lecturewesrdftyghuijkol wasedrftgyhuijkolNessuna valutazione finora
- Acute InflmmationDocumento39 pagineAcute InflmmationBean GemboelzNessuna valutazione finora
- Pathology 2 PDFDocumento18 paginePathology 2 PDFfadoNessuna valutazione finora
- InflammationDocumento8 pagineInflammationGhazi Uddin AhmedNessuna valutazione finora
- Patho Unit 4.1Documento20 paginePatho Unit 4.1Lily ChouNessuna valutazione finora
- 01.inflammation 1Documento30 pagine01.inflammation 1Shameena KnNessuna valutazione finora
- Inflammation & Wound Healing Part 1Documento2 pagineInflammation & Wound Healing Part 1Julia Rae Delos SantosNessuna valutazione finora
- 03 InflammationDocumento10 pagine03 InflammationAlexa UyNessuna valutazione finora
- Acute InflammationDocumento25 pagineAcute Inflammationa194801Nessuna valutazione finora
- Acute InflammationDocumento76 pagineAcute InflammationOmor faruk HridoyNessuna valutazione finora
- Inflammation & Repair: Tim Dosen PatologiDocumento32 pagineInflammation & Repair: Tim Dosen PatologiNdaru SetyaningrumNessuna valutazione finora
- Histopathology - c3 - Acute and Chronic Inflammation - MasterDocumento28 pagineHistopathology - c3 - Acute and Chronic Inflammation - MasterGhinescu AdrianNessuna valutazione finora
- Inflammation 2Documento21 pagineInflammation 2Umar'Farouq OniNessuna valutazione finora
- Sirs 2013Documento96 pagineSirs 2013wildan acalipha wilkensiaNessuna valutazione finora
- Acute InflammationDocumento55 pagineAcute InflammationMohammad_Islam8790% (10)
- In Ammation, Immunity and Allergy: Learning ObjectivesDocumento6 pagineIn Ammation, Immunity and Allergy: Learning ObjectivesJavier VeraNessuna valutazione finora
- Concept of Inflammatory and Immune SystemDocumento15 pagineConcept of Inflammatory and Immune SystemUchiha Dominic100% (1)
- Acute InflammationDocumento51 pagineAcute InflammationNayela AkramNessuna valutazione finora
- 2.INFLAMMATION AND ITS IMPLICATIONS ..... FinalDocumento81 pagine2.INFLAMMATION AND ITS IMPLICATIONS ..... Finalsaloni singhNessuna valutazione finora
- Inflammation, Wound Healing and Foreign Body ResponseDocumento22 pagineInflammation, Wound Healing and Foreign Body Responseharry potterNessuna valutazione finora
- Acute InflammationDocumento71 pagineAcute Inflammationsi_miaomiao100% (1)
- His To PathologyDocumento7 pagineHis To PathologyDessa MartinezNessuna valutazione finora
- Harsh Mohan Quick Review InflammationDocumento23 pagineHarsh Mohan Quick Review InflammationTanaya PujareNessuna valutazione finora
- II Inflam-PatoDocumento27 pagineII Inflam-Patozenitha firdausNessuna valutazione finora
- Inflammation. Etiology. Vascular Changes. Cellular Events in Inflammation. Acute Inflammation. Morphologic PatternsDocumento57 pagineInflammation. Etiology. Vascular Changes. Cellular Events in Inflammation. Acute Inflammation. Morphologic PatternsZauzaNessuna valutazione finora
- Histopathology - c4 - Adaptations of Cellular Growth and Differentiation - MasterDocumento25 pagineHistopathology - c4 - Adaptations of Cellular Growth and Differentiation - MasterGhinescu AdrianNessuna valutazione finora
- Appendicitis Meningitis: Vascular Cellular Response The Inflammatory Process RepairDocumento10 pagineAppendicitis Meningitis: Vascular Cellular Response The Inflammatory Process RepairYaff DthNessuna valutazione finora
- Pathophysiology Notes - Inflammation and HealingDocumento6 paginePathophysiology Notes - Inflammation and HealingKateNessuna valutazione finora
- Inflammation and RepairDocumento34 pagineInflammation and RepairJoshua HonoridezNessuna valutazione finora
- Anti-Inflammatory Properties of Local Anesthetics and Their Present and Potential Clinical ImplicationsDocumento18 pagineAnti-Inflammatory Properties of Local Anesthetics and Their Present and Potential Clinical ImplicationsXavierLuqueNessuna valutazione finora
- 07 InflammationDocumento69 pagine07 InflammationSangameswaran B.BNessuna valutazione finora
- PathoLec InflammationDocumento10 paginePathoLec InflammationMiguel Cuevas DolotNessuna valutazione finora
- 1 PATHO 2a - Inflammation - Dr. BailonDocumento12 pagine1 PATHO 2a - Inflammation - Dr. BailontonNessuna valutazione finora
- Lecture 3Documento56 pagineLecture 3w2tz2qrqxdNessuna valutazione finora
- 7.2 Muscular System: Human Anatomy and Physiology With Pathophysiology LectureDocumento3 pagine7.2 Muscular System: Human Anatomy and Physiology With Pathophysiology LectureRamea LamanoNessuna valutazione finora
- Pathology Week 5 - 6 FKHDocumento15 paginePathology Week 5 - 6 FKHAnna TohNessuna valutazione finora
- Unit 4.1Documento8 pagineUnit 4.1Bloody MarieNessuna valutazione finora
- INFLAMAATIONDocumento6 pagineINFLAMAATIONSabbir AhmedNessuna valutazione finora
- Care of Preschoolers With Health ProblemsDocumento5 pagineCare of Preschoolers With Health ProblemsmajoodhNessuna valutazione finora
- Robbins Pathology - Chapter 3 TransDocumento18 pagineRobbins Pathology - Chapter 3 Transnath nath100% (7)
- 10 - Body Defense MechanismDocumento6 pagine10 - Body Defense MechanismPrince Mark BadilloNessuna valutazione finora
- Week 1 Study GuideDocumento16 pagineWeek 1 Study GuideKateNessuna valutazione finora
- UntitledDocumento4 pagineUntitledSushmitha GandhiNessuna valutazione finora
- GenpathDocumento10 pagineGenpathNatural Science BiologyNessuna valutazione finora
- #27 - Aisha A. Macapundag 4Cmt TMC ACTIVITY: Other Major Blood Group SystemsDocumento5 pagine#27 - Aisha A. Macapundag 4Cmt TMC ACTIVITY: Other Major Blood Group SystemsRachel ManaloNessuna valutazione finora
- 4C-Mt TMC Rapid Plasma Reagin (RPR) TestDocumento3 pagine4C-Mt TMC Rapid Plasma Reagin (RPR) TestRachel ManaloNessuna valutazione finora
- QUALITY CONTROL (Last Day)Documento5 pagineQUALITY CONTROL (Last Day)Rachel ManaloNessuna valutazione finora
- Activity:: Summative Assessment (By Pair)Documento7 pagineActivity:: Summative Assessment (By Pair)Rachel ManaloNessuna valutazione finora
- Blood ComponentsDocumento5 pagineBlood ComponentsRachel ManaloNessuna valutazione finora
- Abo PanelDocumento2 pagineAbo PanelRachel ManaloNessuna valutazione finora
- CASE 1: A Patient Was Seen in The Emergency Room and A Crossmatch Was Ordered. The ABO Forward and Reverse Grouping Results Are As FollowsDocumento3 pagineCASE 1: A Patient Was Seen in The Emergency Room and A Crossmatch Was Ordered. The ABO Forward and Reverse Grouping Results Are As FollowsRachel ManaloNessuna valutazione finora
- Other Blood Group SystemsDocumento2 pagineOther Blood Group SystemsRachel ManaloNessuna valutazione finora
- 04 - (Second Half) Nitric Oxide in Cellular Adaptation and Disease PDFDocumento11 pagine04 - (Second Half) Nitric Oxide in Cellular Adaptation and Disease PDFRachel ManaloNessuna valutazione finora
- 05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedDocumento7 pagine05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedRachel ManaloNessuna valutazione finora
- 04 - (Second Half) Nitric Oxide in Cellular Adaptation and Disease PDFDocumento11 pagine04 - (Second Half) Nitric Oxide in Cellular Adaptation and Disease PDFRachel ManaloNessuna valutazione finora
- 05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedDocumento7 pagine05 - Cellular Adaptations - SimpleMed - Learning Medicine, SimplifiedRachel ManaloNessuna valutazione finora
- CELLSDocumento8 pagineCELLSRachel ManaloNessuna valutazione finora
- A Review On Plant-Based Rutin Extraction Methods and Its Pharmacological ActivitiesDocumento13 pagineA Review On Plant-Based Rutin Extraction Methods and Its Pharmacological ActivitieswahyuniNessuna valutazione finora
- Manual of Definitive Surgical Trauma CareDocumento256 pagineManual of Definitive Surgical Trauma Carebovine splendor100% (3)
- Indomethacin 392Documento17 pagineIndomethacin 392Mahadie Hasan JahadNessuna valutazione finora
- Thromboxane A2Documento16 pagineThromboxane A2Concepcion R. Aquino0% (1)
- Induction of C-Fos by Prostaglandin F in Human Ciliary Smooth Muscle CellsDocumento9 pagineInduction of C-Fos by Prostaglandin F in Human Ciliary Smooth Muscle Cellsanandhamide81Nessuna valutazione finora
- Pathology Week 2 p1-18Documento18 paginePathology Week 2 p1-18zeroun24100% (1)
- Lotus Notes Bleeding Letting For ClinicalDocumento26 pagineLotus Notes Bleeding Letting For ClinicalMatthieu Decalf100% (2)
- PainoxiaDocumento66 paginePainoxiaOmar WahbiNessuna valutazione finora
- Prostaglandins and LeukotrienesDocumento40 pagineProstaglandins and LeukotrienesParul SinghNessuna valutazione finora
- Understanding Turmeric Anti-In Ammatory Effects and Its Clinical UseDocumento19 pagineUnderstanding Turmeric Anti-In Ammatory Effects and Its Clinical UseBilly JamesNessuna valutazione finora
- Lipids 31 2012 NotesDocumento20 pagineLipids 31 2012 Notesapi-178321548Nessuna valutazione finora
- Chapter: One: Introduction and Aim of The ThesisDocumento12 pagineChapter: One: Introduction and Aim of The ThesislichenresearchNessuna valutazione finora
- The Logic of Chemical SynthesisDocumento462 pagineThe Logic of Chemical SynthesisJohnny KrazeNessuna valutazione finora
- EicosanoidsDocumento4 pagineEicosanoidsFrancis GathiraNessuna valutazione finora
- Nonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharDocumento97 pagineNonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharTarek NasrallahNessuna valutazione finora
- Non Steroidal Anti Inflammatory Drugs: NsaidsDocumento58 pagineNon Steroidal Anti Inflammatory Drugs: NsaidsmahamoudNessuna valutazione finora
- Topic 2. Pharmacology For Pain and Inflammation RDocumento52 pagineTopic 2. Pharmacology For Pain and Inflammation RKendrick GalosoNessuna valutazione finora
- Aspectos Fisiopatologicos Da InflamaçãoDocumento25 pagineAspectos Fisiopatologicos Da InflamaçãoMaria das Dores BarretoNessuna valutazione finora
- Prostaglandin: Continued DonationsDocumento27 pagineProstaglandin: Continued DonationsrajeevmkNessuna valutazione finora
- Screenshot 2022-06-13 at 16.29.48Documento34 pagineScreenshot 2022-06-13 at 16.29.48Indira NoormaliyaNessuna valutazione finora
- Burn UnitDocumento206 pagineBurn UnitJeisson Osorio Trujillo100% (1)
- Pharmacodynamics and PharmacokineticsDocumento99 paginePharmacodynamics and PharmacokineticsMAMA LALANessuna valutazione finora
- Pain Relievers TGDocumento26 paginePain Relievers TGLilis nurhayatiNessuna valutazione finora
- Fatty Acids and Polyketides PaperDocumento62 pagineFatty Acids and Polyketides PaperKarina Narciso100% (1)
- BylawsDocumento136 pagineBylawsdannyfiguracion45Nessuna valutazione finora
- Eicosanoids: (Prostaglandins, Thromboxanes, Leukotrienes)Documento26 pagineEicosanoids: (Prostaglandins, Thromboxanes, Leukotrienes)BOsch VakilNessuna valutazione finora
- Recent Advances in Anaesthesia and Intensive CareDocumento323 pagineRecent Advances in Anaesthesia and Intensive CaresurasuarezlopezNessuna valutazione finora
- Conservation Therapy (Celibacy)Documento9 pagineConservation Therapy (Celibacy)ShivamMishraNessuna valutazione finora
- Prostaglandins, Immunoglobulins: Prepared by Dr. Poonam MondalDocumento10 pagineProstaglandins, Immunoglobulins: Prepared by Dr. Poonam MondalPoonam MondalNessuna valutazione finora
- Inflammation and Inflammatory MediatorsDocumento40 pagineInflammation and Inflammatory MediatorsQuty Papa KannaNessuna valutazione finora