Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Diabetes Care Standard 2010
Caricato da
Jose SanchezDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Diabetes Care Standard 2010
Caricato da
Jose SanchezCopyright:
Formati disponibili
Introduction
T
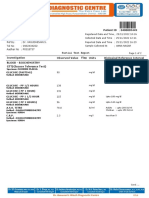
he American Diabetes Association Table 1—ADA evidence-grading system for clinical practice recommendations
(ADA) has been actively involved in
the development and dissemination
Level of
of diabetes care standards, guidelines,
evidence Description
and related documents for many years.
These statements are published in one or A Clear evidence from well-conducted, generalizable, randomized controlled trials
more of the Association’s professional that are adequately powered, including:
journals. This supplement contains the 䡠 Evidence from a well-conducted multicenter trial
latest update of ADA’s major position 䡠 Evidence from a meta-analysis that incorporated quality ratings in the analysis
statement, “Standards of Medical Care in Compelling nonexperimental evidence, i.e., the “all or none” rule developed by the
Diabetes,” which contains all of the Asso- Centre for Evidence-Based Medicine at Oxford
ciation’s key recommendations. In addi- Supportive evidence from well-conducted randomized controlled trials that are
tion, contained herein are selected position adequately powered, including:
statements on certain topics not adequately 䡠 Evidence from a well-conducted trial at one or more institutions
covered in the “Standards.” ADA hopes that 䡠 Evidence from a meta-analysis that incorporated quality ratings in the analysis
this is a convenient and important resource
B Supportive evidence from well-conducted cohort studies, including:
for all health care professionals who care for
䡠 Evidence from a well-conducted prospective cohort study or registry
people with diabetes.
䡠 Evidence from a well-conducted meta-analysis of cohort studies
ADA Clinical Practice Recommenda-
Supportive evidence from a well-conducted case-control study
tions consist of position statements that
represent official ADA opinion as denoted C Supportive evidence from poorly controlled or uncontrolled studies, including:
by formal review and approval by the Pro- 䡠 Evidence from randomized clinical trials with one or more major or three or
fessional Practice Committee and the Ex- more minor methodological flaws that could invalidate the results
ecutive Committee of the Board of 䡠 Evidence from observational studies with high potential for bias (such as case
Directors. Consensus reports and system- series with comparison to historical controls)
atic reviews are not official ADA 䡠 Evidence from case series or case reports
recommendations; however, they are Conflicting evidence with the weight of evidence supporting the recommendation
produced under the auspices of the Asso-
ciation by invited experts. These publica- E Expert consensus or clinical experience
tions may be used by the Professional
and updated as needed. A list of recent sensus panel) of a scientific or medical
Practice Committee as source documents
position statements is included on p. S100 issue related to diabetes. Effective January
to update the “Standards.”
of this supplement. 2010, consensus statements are renamed
ADA has adopted the following defi-
nitions for its clinically related reports. Systematic review. A balanced review consensus reports. The category will also
and analysis of the literature on a scien- include task force, workgroup, and expert
ADA position statement. An official
tific or medical topic related to diabetes. committee reports. Consensus reports
point of view or belief of the ADA. Posi-
Effective January 2010, technical reviews will not have the Association’s name in-
tion statements are issued on scientific or
are replaced with systematic reviews, for cluded in the title or subtitle and will in-
medical issues related to diabetes. They
which a priori search and inclusion/ clude a disclaimer in the introduction
may be authored or unauthored and are
exclusion criteria are developed and pub- stating that any recommendations are not
published in ADA journals and other sci-
lished. The systematic review provides a ADA position. A consensus report is typ-
entific/medical publications as appropri-
scientific rationale for a position state- ically developed immediately following a
ate. Position statements must be reviewed
ment and undergoes critical peer review consensus conference at which presenta-
and approved by the Professional Practice
before submission to the Professional tions are made on the issue under review.
Committee and, subsequently, by the
Practice Committee for approval. A list The statement represents the panel’s col-
Executive Committee of the Board of Di-
of past technical reviews is included on
rectors. ADA position statements are lective analysis, evaluation, and opinion
page S97 of this supplement.
typically based on a systematic review at that point in time based in part on the
or other review of published literature. Consensus report. A comprehensive ex- conference proceedings. The need for a
They are reviewed on an annual basis amination by a panel of experts (i.e., con- consensus report arises when clinicians or
scientists desire guidance on a subject for
which the evidence is contradictory or in-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
complete. Once written by the panel, a
DOI: 10.2337/dc10-S001. consensus report is not subject to subse-
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. quent review or approval and does not
org/licenses/by-nc-nd/3.0/ for details. represent official Association opinion. A
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S1
Introduction
list of recent consensus reports is in- education, disability, and, above all, pa- Curt D. Furberg, MD, PhD, has been a
cluded on p. S96 of this supplement. tients’ values and preferences, must also member of the data safety monitoring
The Association’s Professional Prac- be considered and may lead to different committee for Wyeth.
tice Committee is responsible for review- treatment targets and strategies. Also,
conventional evidence hierarchies, such Sheila Y. Garris, MD, FACP, has been a
ing ADA systematic reviews and position
as the one adapted by the ADA, may miss speaker for Takeda, Osient, Glaxo-
statements, as well as for overseeing revi-
some nuances that are important in dia- SmithKline, and Novartis and has been
sions of the latter as needed. Appointment
betes care. For example, while there is ex- a speaker and consultant for Merck,
to the Professional Practice Committee is
cellent evidence from clinical trials Forrest*, and Daiichi Sankyo.
based on excellence in clinical practice
and/or research. The committee com- supporting the importance of achieving Silvio E. Inzucchi, MD, has been a con-
prises physicians, diabetes educators, and glycemic control, the optimal way to sultant/advisor for Takeda, Merck*,
registered dietitians who have expertise in achieve this result is less clear. It is diffi- Amylin, Daiichi Sankyo, and
a range of areas, including adult and pe- cult to assess each component of such a Medtronic; has accepted honoraria
diatric endocrinology, epidemiology, and complex intervention. from Novo Nordisk; and has received
public health, lipid research, hyperten- ADA will continue to improve and research funding from Eli Lilly*;
sion, and preconception and pregnancy update the Clinical Practice Recommen- Takeda, Merck, Amylin, and Boehringer
care. All members of the Professional dations to ensure that clinicians, health Ingelheim have provided educational
Practice Committee are required to dis- plans, and policymakers can continue to grants* to Yale University for work con-
close potential conflicts of interest (listed rely on them as the most authoritative and ducted by him.
below). current guidelines for diabetes care. Our
Clinical Practice Recommendations are Wahida Karmally, DrPH, RD, CDE,
Grading of scientific evidence. There also available on the Association’s website CLS, reports no duality of interest.
has been considerable evolution in the eval- at www.diabetes.org/diabetescare.
uation of scientific evidence and in the de- Antoinette Moran, MD, has been on the
velopment of evidence-based guidelines advisory committee for Bayer.
since the ADA first began publishing prac- DUALITIES OF INTEREST Peter D. Reaven, MD, has received re-
tice guidelines. Accordingly, we developed search support from Takeda* and Amy-
a classification system to grade the quality Professional Practice Committee lin*, is a member of the speaker’s
of scientific evidence supporting ADA Members bureau for Merck, and is on the advisory
recommendations for all new and revised John E. Anderson, MD, is on the speaker’s panel of and is a board member for Bris-
ADA position statements. bureau for Amylin/Eli Lilly*, Glaxo- tol-Myers Squibb.
Recommendations are assigned rat- SmithKline*, Daichi/Sankyo, and Novo
ings of A, B, or C, depending on the qual- Guillermo Umpierrez, MD, has received
Nordisk. research funding from sanofi-aventis*,
ity of evidence (Table 1). Expert opinion
(E) is a separate category for recommen- Joan Bardsley, RN, MBA, CDE, has re- Novo Nordisk*, Takeda*, and Eli
dations in which there is as yet no evi- ceived research funding from Novo Nor- Lilly*.
dence from clinical trials, in which disk*, has received honoraria from Novo Craig Williams, PharmD, has received
clinical trials may be impractical, or in Nordisk* and GlaxoSmithKline*, and research funding from Merck* and
which there is conflicting evidence. Rec- owns stock in Pfizer* and Amylin. speaker fees from Merck/Schering
ommendations with an “A” rating are Plough and has a relative employed by
John B. Buse, MD, PhD, has conducted
based on large well-designed clinical trials Pfizer.
research and/or consulted under con-
or well-done meta-analyses. Generally,
tract between the University of North David F. Williamson, PhD, reports no
these recommendations have the best
Carolina and Amylin*, Bayhill Thera- duality of interest.
chance of improving outcomes when
peutics, Becton Dickinson*, Bristol-
applied to the population to which they Peter Wilson, MD, has received research
Myers Squibb*, DexCom*, Eli Lilly*,
are appropriate. Recommendations funding from GlaxoSmithKline*.
GI Dynamics, GlaxoSmithKline*,
with lower levels of evidence may be
Halozyme*, Hoffman-LaRoche*, In- Carol H. Wysham, MD, has been a
equally important but are not as well
terkrin*, Johnson & Johnson*, Lipo- speaker for Eli Lilly*, Merck, Novo
supported. The level of evidence sup-
Science*, Mannkind*, Medtronic*, Nordisk, and sanofi-aventis and a con-
porting a given recommendation is
Merck*, Novartis*, Novo Nordisk*, sultant and speaker for Amylin Pharma-
noted either as a heading for a group of
Osiris*, Pfizer*, sanofi-aventis*, Tol- ceuticals*.
recommendations or in parentheses af-
erex*, Transition Therapeutics*, and
ter a given recommendation.
Wyeth; and owns stock in Insulet*.
Of course, evidence is only one com- American Diabetes Association Staff
ponent of clinical decision-making. Clini- Martha Funnell, MS, RN, CDE, has been M. Sue Kirkman, MD, and Stephanie A.
cians care for patients, not populations; on the advisory board for Novo Nor- Dunbar, MPH, RD, report no duality of
guidelines must always be interpreted disk, Eli Lilly, HDI Diagnostics, Intuity interest.
with the needs of the individual patient in Medical, GlaxoSmithKline, and Mann-
mind. Individual circumstances, such as kind and has been a consultant for ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
comorbid and coexisting diseases, age, sanofi-aventis. *Amount ⬎$10,000/year.
S2 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
S U M M A R Y O F R E V I S I O N S
Summary of Revisions for the 2010
Clinical Practice Recommendations
B
eginning with the 2005 supple- Revisions to the “Standards of The section “Diabetes self-management
ment, the Clinical Practice Recom- Medical Care in Diabetes” education” has been extensively revised
mendations contained only the In addition to many small changes related to reflect new evidence.
“Standards of Medical Care in Diabetes” to new evidence since the previous ver- ● The section “Antiplatelet agents” has
and selected other position statements. sion, the following sections have under- been extensively revised to reflect re-
This change was made to emphasize the gone major changes: cent trials questioning the benefit of as-
importance of the “Standards” as the best pirin for primary cardiovascular disease
source to determine American Diabetes ● The section “Diagnosis of diabetes” has prevention in moderate- or low-risk
Association recommendations. The posi- been revised to include the use of A1C patients. The recommendation has
tion statements in the supplement are up- to diagnose diabetes, with a cut point of changed to consider aspirin therapy as
dated yearly. Position statements not ⱖ6.5%. a primary prevention strategy in those
included in the supplement will be up- ● The section previously titled “Diagnosis with diabetes at increased cardiovascu-
dated as necessary and republished when of pre-diabetes” has been renamed
lar risk (10-year risk ⬎10%). This in-
updated. A list of the position statements “Categories of increased risk for diabe-
cludes men ⬎50 years of age or women
not included in this supplement appears tes.” In addition to impaired fasting glu-
on p. S100. cose and impaired glucose tolerance, an ⬎60 years of age with at least one ad-
A1C range of 5.7– 6.4% has been in- ditional major risk factor.
● The section “Retinopathy screening
cluded as a category of increased risk
Additions to the “Standards of for future diabetes. and treatment” has been updated to
Medical Care in Diabetes” ● The section “Detection and diagnosis of include a recommendation on use of
GDM” has been revised to discuss po- fundus photography as a screening
● A section on cystic fibrosis–related dia- tential future changes in the diagnosis strategy.
betes has been added. based on international consensus. ● The section “Diabetes care in the hospi-
tal” has been extensively revised to re-
flect new evidence calling into question
very tight glycemic control goals in crit-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
ically ill patients.
DOI: 10.2337/dc10-S003 ●
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly
The section “Strategies for improving
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. diabetes care” has been extensively re-
org/licenses/by-nc-nd/3.0/ for details. vised to reflect newer evidence.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S3
E X E C U T I V E S U M M A R Y
Executive Summary: Standards of Medical
Care in Diabetes—2010
Current criteria for the diagnosis of Detection and diagnosis of medical nutrition therapy (MNT)
diabetes gestational diabetes mellitus alone, SMBG may be useful as a guide to
● A1C ⱖ6.5%: The test should be per- ● Screen for gestational diabetes mellitus the success of therapy. (E)
formed in a laboratory using a method (GDM) using risk-factor analysis and, if ● To achieve postprandial glucose tar-
that is National Glycohemoglobin Stan- appropriate, the OGTT. (C) gets, postprandial SMBG may be appro-
dardization Program (NGSP) certified ● Women with GDM should be screened priate. (E)
and standardized to the Diabetes Control for diabetes 6 –12 weeks postpartum ● When prescribing SMBG, ensure that
and Complications Trial (DCCT) assay. and should be followed up with subse- patients receive initial instruction in,
● FPG ⱖ126 mg/dl (7.0 mmol/l): Fasting is quent screening for the development of and routine follow-up evaluation of,
defined as no caloric intake for at least diabetes or pre-diabetes. (E) SMBG technique and their ability to use
8 h. data to adjust therapy. (E)
● 2-h plasma glucose ⱖ200 mg/dl (11.1 Prevention of type 2 diabetes ● Continuous glucose monitoring (CGM)
● Patients with IGT (A), IFG (E), or an in conjunction with intensive insulin
mmol/l) during an oral glucose tolerance
test (OGTT): The test should be per- A1C of 5.7– 6.4% (E) should be re- regimens can be a useful tool to lower
formed as described by the World Health ferred to an effective ongoing support A1C in selected adults (age ⬎25 years)
Organization using a glucose load con- program for weight loss of 5–10% of with type 1 diabetes. (A)
body weight and increase in physical ● Although the evidence for A1C-
taining the equivalent of 75 g anhydrous
activity to at least 150 min/week of lowering is less strong in children,
glucose dissolved in water.
● In a patient with classic symptoms of
moderate activity such as walking. teens, and younger adults, CGM may
● Follow-up counseling appears to be im- be helpful in these groups. Success cor-
hyperglycemia or hyperglycemic crisis:
portant for success. (B) relates with adherence to ongoing use
a random plasma glucose ⱖ200 mg/dl ● Based on potential cost savings of dia- of the device. (C)
(11.1 mmol/l). betes prevention, such counseling ● CGM may be a supplemental tool to
should be covered by third-party pay- SMBG in those with hypoglycemia un-
Testing for diabetes in asymptomatic ors. (E) awareness and/or frequent hypoglyce-
patients ● In addition to lifestyle counseling, met- mic episodes. (E)
● Testing to detect type 2 diabetes and formin may be considered in those who
assess risk for future diabetes in asymp- are at very high risk for developing di- A1C
tomatic people should be considered in abetes (combined IFG and IGT plus ● Perform the A1C test at least two times
adults of any age who are overweight or other risk factors such as A1C ⬎6%, a year in patients who are meeting treat-
obese (BMI ⱖ25 kg/m2) and who have hypertension, low HDL cholesterol, el- ment goals (and who have stable glyce-
one or more additional risk factors for evated triglycerides, or family history of mic control). (E)
diabetes in a first-degree relative) and ● Perform the A1C test quarterly in pa-
diabetes (see Table 4 of Standards of
Medical Care in Diabetes—2010). In who are obese and under 60 years of tients whose therapy has changed or
those without these risk factors, testing age. (E) who are not meeting glycemic goals. (E)
● Monitoring for the development of di- ● Use of point-of-care testing for A1C al-
should begin at age 45 years. (B)
● If tests are normal, repeat testing should
abetes in those with pre-diabetes lows for timely decisions on therapy
should be performed every year. (E) changes, when needed. (E)
be carried out at least at 3-year intervals.
(E)
Glucose monitoring Glycemic goals in adults
● To test for diabetes or to assess risk of
● Self-monitoring of blood glucose ● Lowering A1C to below or around 7%
future diabetes, A1C, FPG , or 2-h 75-g (SMBG) should be carried out three or has been shown to reduce microvascu-
OGTT are appropriate. (B) more times daily for patients using mul- lar and neuropathic complications of
● In those identified with increased risk tiple insulin injections or insulin pump type 1 and type 2 diabetes. Therefore,
for future diabetes, identify and, if ap- therapy. (A) for microvascular disease prevention,
propriate, treat other cardiovascular ● For patients using less frequent insulin the A1C goal for nonpregnant adults in
disease (CVD) risk factors. (B) injections, noninsulin therapies, or general is ⬍7%. (A)
● In type 1 and type 2 diabetes, random-
ized controlled trials of intensive versus
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
standard glycemic control have not
shown a significant reduction in CVD
DOI: 10.2337/dc10-S004
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly outcomes during the randomized por-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. tion of the trials. Long-term follow-up
org/licenses/by-nc-nd/3.0/ for details. of the DCCT and UK Prospective Dia-
S4 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Executive Summary
betes Study (UKPDS) cohorts suggests dividuals who have or are at risk for Other nutrition recommendations
that treatment to A1C targets below or diabetes. (A) ● Sugar alcohols and nonnutritive sweet-
around 7% in the years soon after the ● For weight loss, either low-carbohy- eners are safe when consumed within
diagnosis of diabetes is associated with drate or low-fat calorie-restricted diets the acceptable daily intake levels estab-
long-term reduction in risk of macro- may be effective in the short-term (up lished by the Food and Drug Adminis-
vascular disease. Until more evidence to 1 year). (A) tration (FDA). (A)
becomes available, the general goal of ● For patients on low-carbohydrate diets, ● If adults with diabetes choose to use
⬍7% appears reasonable for many monitor lipid profiles, renal function, alcohol, daily intake should be limited
adults for macrovascular risk reduc- and protein intake (in those with ne- to a moderate amount (one drink per
tion. (B) phropathy) and adjust hypoglycemic day or less for adult women and two
● Subgroup analyses of clinical trials such drinks per day or less for adult men).
therapy as needed. (E)
as the DCCT and UKPDS and evidence ● Physical activity and behavior modifi- (E)
for reduced proteinuria in the AD- ● Routine supplementation with antioxi-
cation are important components of
VANCE trial suggest a small but incre- weight loss programs and are most dants, such as vitamins E and C and
mental benefit in microvascular helpful in maintenance of weight loss. carotene, is not advised because of lack
outcomes with A1C values closer to (B) of evidence of efficacy and concern re-
normal. Therefore, for selected individ- lated to long-term safety. (A)
ual patients, providers might reason- ● Benefit from chromium supplementa-
ably suggest even lower A1C goals than Primary prevention of diabetes tion in people with diabetes or obesity
the general goal of ⬍7%, if this can be ● Among individuals at high risk for de- has not been conclusively demon-
achieved without significant hypogly- veloping type 2 diabetes, structured strated and, therefore, cannot be rec-
cemia or other adverse effects of treat- programs emphasizing lifestyle ommended. (C)
ment. Such patients might include changes including moderate weight ● Individualized meal planning should
those with short duration of diabetes, loss (7% body weight) and regular include optimization of food choices
long life expectancy, and no significant physical activity (150 min/week), with to meet recommended dietary allow-
CVD. (B) dietary strategies including reduced ances (RDAs)/dietary reference intakes
● Conversely, less stringent A1C goals calories and reduced intake of dietary (DRIs) for all micronutrients. (E)
than the general goal of ⬍7% may be fat, can reduce the risk for developing
appropriate for patients with a history diabetes and are therefore recom- Bariatric surgery
of severe hypoglycemia, limited life ex- ● Bariatric surgery should be considered
mended. (A)
pectancy, advanced microvascular or ● Individuals at high risk for type 2 dia- for adults with BMI ⬎35 kg/m2 and
macrovascular complications, or exten- betes should be encouraged to achieve type 2 diabetes, especially if the diabe-
sive comorbid conditions and those the U.S. Department of Agriculture tes or associated comorbidities are dif-
with longstanding diabetes in whom (USDA) recommendation for dietary fi- ficult to control with lifestyle and
the general goal is difficult to attain de- ber (14 g fiber/1,000 kcal) and foods pharmacologic therapy. (B)
spite diabetes self-management educa- ● Patients with type 2 diabetes who have
containing whole grains (one-half of
tion, appropriate glucose monitoring, grain intake). (B) undergone bariatric surgery need life-
and effective doses of multiple glucose- long lifestyle support and medical
lowering agents including insulin. (C) monitoring. (E)
Dietary fat intake in diabetes ● Although small trials have shown gly-
management cemic benefit of bariatric surgery in pa-
Medical nutrition therapy ● Saturated fat intake should be ⬍7% of tients with type 2 diabetes and BMI of
General recommendations
● Individuals who have pre-diabetes or
total calories. (A) 30 –35 kg/m2, there is currently insuf-
● Reducing intake of trans fat lowers LDL ficient evidence to generally recom-
diabetes should receive individualized
cholesterol and increases HDL choles- mend surgery in patients with BMI ⬍35
medical nutrition therapy (MNT) as
terol (A); therefore, intake of trans fat kg/m2 outside of a research protocol.
needed to achieve treatment goals, pref-
should be minimized. (E) (E)
erably provided by a registered dietitian ● The long-term benefits, cost-effective-
familiar with the components of diabe-
ness, and risks of bariatric surgery in
tes MNT. (A) Carbohydrate intake in diabetes
● Because MNT can result in cost-savings
individuals with type 2 diabetes should
management be studied in well-designed random-
and improved outcomes (B), MNT ● Monitoring carbohydrate, whether by
ized controlled trials with optimal
should be covered by insurance and carbohydrate counting, exchanges, or medical and lifestyle therapy as the
other payors. (E) experience-based estimation, remains a comparator. (E)
key strategy in achieving glycemic con-
Energy balance, overweight, and trol. (A) Diabetes self-management education
obesity ● For individuals with diabetes, the use of ● People with diabetes should receive di-
● In overweight and obese insulin- the glycemic index and glycemic load abetes self-management education
resistant individuals, modest weight may provide a modest additional bene- (DSME) according to national stan-
loss has been shown to reduce insulin fit for glycemic control over that ob- dards when their diabetes is diagnosed
resistance. Thus, weight loss is recom- served when total carbohydrate is and as needed thereafter. (B)
mended for all overweight or obese in- considered alone. (B) ● Effective self-management and quality
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S5
Executive Summary
of life are the key outcomes of DSME awareness or one or more episodes of style dietary pattern including reducing
and should be measured and moni- severe hypoglycemia should be advised sodium and increasing potassium intake,
tored as part of care. (C) to raise their glycemic targets to strictly moderation of alcohol intake, and in-
● DSME should address psychosocial is- avoid further hypoglycemia for at least creased physical activity. (B)
sues, since emotional well-being is several weeks, to partially reverse hypo- ● Pharmacologic therapy for patients with
associated with positive diabetes out- glycemia unawareness and reduce risk diabetes and hypertension should be
comes. (C) of future episodes. (B) with a regimen that includes either an
● Because DSME can result in cost- ACE inhibitor or an angiotensin receptor
savings and improved outcomes (B), Immunization blocker (ARB). If one class is not toler-
DSME should be reimbursed by third- ● Annually provide an influenza vaccine ated, the other should be substituted. If
party payors. (E) to all diabetic patients 6 months of age. needed to achieve blood pressure targets,
(C) a thiazide diuretic should be added to
Physical activity ● Administer pneumococcal polysaccha- those with an estimated glomerular filtra-
● People with diabetes should be advised ride vaccine to all diabetic patients ⱖ2 tion rate (GFR) (see below) ⱖ30 ml/min
to perform at least 150 min/week of years of age. A one-time revaccination is per 1.73 m2 and a loop diuretic for those
moderate-intensity aerobic physical ac- recommended for individuals ⬎64 with an estimated GFR ⬍30 ml/min per
tivity (50 –70% of maximum heart years of age previously immunized 1.73 m2. (C)
rate). (A) when they were ⬍65 years of age if the ● Multiple drug therapy (two or more
● In the absence of contraindications, vaccine was administered ⬎5 years agents at maximal doses) is generally
people with type 2 diabetes should be ago. Other indications for repeat vacci- required to achieve blood pressure tar-
encouraged to perform resistance train- nation include nephrotic syndrome, gets. (B)
ing three times per week. (A) chronic renal disease, and other immu- ● If ACE inhibitors, ARBs, or diuretics are
nocompromised states, such as after used, kidney function and serum potas-
Psychosocial assessment and care transplantation. (C) sium levels should be closely moni-
● Assessment of psychological and social tored. (E)
situation should be included as an on- Hypertension/blood pressure control ● In pregnant patients with diabetes and
going part of the medical management Screening and diagnosis chronic hypertension, blood pressure
of diabetes. (E) ● Blood pressure should be measured at target goals of 110 –129/65–79 mmHg
● Psychosocial screening and follow-up every routine diabetes visit. Patients are suggested in the interest of long-
should include, but is not limited to, found to have systolic blood pressure term maternal health and minimizing
attitudes about the illness, expectations ⱖ130 mmHg or diastolic blood pres- impaired fetal growth. ACE inhibitors
for medical management and out- sure ⱖ80 mmHg should have blood and ARBs are contraindicated during
comes, affect/mood, general and diabe- pressure confirmed on a separate day. pregnancy. (E)
tes-related quality of life, resources Repeat systolic blood pressure ⱖ130
(financial, social, and emotional), and mmHg or diastolic blood pressure ⱖ80 Dyslipidemia/lipid management
psychiatric history. (E) mmHg confirms a diagnosis of hyperten- Screening
● Screen for psychosocial problems such sion. (C) ● In most adult patients, measure fasting
as depression and diabetes-related dis- lipid profile at least annually. In adults
tress, anxiety, eating disorders, and Goals with low-risk lipid values (LDL choles-
cognitive impairment when self- ● Patients with diabetes should be treated terol ⬍100 mg/dl, HDL cholesterol
management is poor. (C) to a systolic blood pressure ⬍130 ⬎50 mg/dl, and triglycerides ⬍150
mmHg. (C) mg/dl), lipid assessments may be re-
Hypoglycemia ● Patients with diabetes should be treated
peated every 2 years. (E)
● Glucose (15–20 g) is the preferred to a diastolic blood pressure ⬍80
treatment for the conscious individual mmHg. (B)
with hypoglycemia, although any form Treatment recommendations and
of carbohydrate that contains glucose Treatment goals
may be used. If SMBG 15 min after ● Patients with a systolic blood pressure ● Lifestyle modification focusing on the
treatment shows continued hypoglyce- of 130 –139 mmHg or a diastolic blood reduction of saturated fat, trans fat, and
mia, the treatment should be repeated. pressure of 80 – 89 mmHg may be given cholesterol intake; increase of n-3 fatty
Once SMBG glucose returns to normal, lifestyle therapy alone for a maximum acids, viscous fiber, and plant stanols/
the individual should consume a meal of 3 months, and then if targets are not sterols; weight loss (if indicated); and
or snack to prevent recurrence of hypo- achieved, be treated with addition of increased physical activity should be
glycemia. (E) pharmacological agents. (E) recommended to improve the lipid
● Glucagon should be prescribed for all ● Patients with more severe hypertension profile in patients with diabetes. (A)
individuals at significant risk of severe (systolic blood pressure ⱖ140 or dia- ● Statin therapy should be added to life-
hypoglycemia, and caregivers or family stolic blood pressure ⱖ90 mmHg) at style therapy, regardless of baseline
members of these individuals in- diagnosis or follow-up should receive lipid levels, for diabetic patients:
structed in its administration. Gluca- pharmacologic therapy in addition to ● with overt CVD. (A)
gon administration is not limited to lifestyle therapy. (A) ● without CVD who are over the age of
health care professionals. (E) ● Lifestyle therapy for hypertension con- 40 years and have one or more other
● Individuals with hypoglycemia un- sists of: weight loss if overweight, DASH- CVD risk factors. (A)
S6 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Executive Summary
● For lower risk patients than the above ● Combination therapy with ASA (75– Treatment
(e.g., without overt CVD and under the 162 mg/day) and clopidogrel (75 mg/ ● In the treatment of the nonpregnant pa-
age of 40 years), statin therapy should day) is reasonable for up to a year after tient with micro- or macroalbuminuria,
be considered in addition to lifestyle an acute coronary syndrome. (B) either ACE inhibitors or ARBs should
therapy if LDL cholesterol remains be used. (A)
above 100 mg/dl or in those with mul- Smoking cessation ● While there are no adequate head-to-
tiple CVD risk factors. (E) ● Advise all patients not to smoke. (A) head comparisons of ACE inhibitors
● In individuals without overt CVD, the ● Include smoking cessation counseling and ARBs, there is clinical trial support
primary goal is an LDL cholesterol and other forms of treatment as a rou- for each of the following statements:
⬍100 mg/dl (2.6 mmol/l). (A) tine component of diabetes care. (B) ● In patients with type 1 diabetes with
● In individuals with overt CVD, a lower hypertension and any degree of albu-
LDL cholesterol goal of ⬍70 mg/dl (1.8 Coronary heart disease minuria, ACE inhibitors have been
mmol/l), using a high dose of a statin, is Screening shown to delay the progression of ne-
an option. (B) ● In asymptomatic patients, evaluate risk phropathy. (A)
● If drug-treated patients do not reach the factors to stratify patients by 10-year ● In patients with type 2 diabetes, hy-
above targets on maximal tolerated sta- risk, and treat risk factors accordingly. pertension, and microalbuminuria,
tin therapy, a reduction in LDL choles- (B) both ACE inhibitors and ARBs have
terol of ⬃30 – 40% from baseline is an been shown to delay the progression
alternative therapeutic goal. (A) Treatment to macroalbuminuria. (A)
● Triglycerides levels ⬍150 mg/dl (1.7 ● In patients with known CVD, ACE in- ● In patients with type 2 diabetes, hy-
mmol/l) and HDL cholesterol ⬎40 hibitor (C) and aspirin and statin ther- pertension, macroalbuminuria, and
mg/dl (1.0 mmol/l) in men and ⬎50 apy (A) (if not contraindicated) should renal insufficiency (serum creatinine
mg/dl (1.3 mmol/l) in women are desir- be used to reduce the risk of cardiovas- ⬎1.5 mg/dl), ARBs have been shown
able. However, LDL cholesterol– cular events. to delay the progression of nephrop-
targeted statin therapy remains the ● In patients with a prior myocardial in- athy. (A)
preferred strategy. (C) farction, B-blockers should be contin- ● If one class is not tolerated, the other
● If targets are not reached on maximally ued for at least 2 years after the event. should be substituted. (E) Reduction of
tolerated doses of statins, combination (B) protein intake to 0.8 –1.0 g 䡠 kg body
therapy using statins and other lipid- ● Longer term use of B-blockers in the wt–1 䡠 day–1 in individuals with diabetes
lowering agents may be considered to absence of hypertension is reasonable if and the earlier stages of CKD and to
achieve lipid targets but has not been well tolerated, but data are lacking. (E) 0.8 g 䡠 kg body wt–1 䡠 day–1 in the later
evaluated in outcome studies for either ● Avoid TZD treatment in patients with stages of CKD may improve measures
CVD outcomes or safety. (E) symptomatic heart failure. (C) of renal function (urine albumin excre-
● Statin therapy is contraindicated in ● Metformin may be used in patients with tion rate, GFR) and is recommended.
pregnancy. (E) stable congestive heart failure (CHF) if (B)
renal function is normal. It should be ● When ACE inhibitors, ARBs, or diuret-
Antiplatelet agents avoided in unstable or hospitalized pa- ics are used, monitor serum creatinine
● Consider aspirin therapy (75–162 mg/ tients with CHF. (C) and potassium levels for the develop-
day) as a primary prevention strategy in ment of acute kidney disease and hy-
those with type 1 or type 2 diabetes at Nephropathy screening and perkalemia. (E)
increased cardiovascular risk (10-year treatment ● Continued monitoring of urine albu-
risk ⬎10%). This includes most men General recommendations min excretion to assess both response
⬎50 years of age or women ⬎60 years ● To reduce the risk or slow the progres- to therapy and progression of disease is
of age who have at least one additional sion of nephropathy, optimize glucose recommended. (E)
major risk factor (family history of control. (A) ● Consider referral to a physician ex-
CVD, hypertension, smoking, dyslipi- ● To reduce the risk or slow the progres- perienced in the care of kidney dis-
demia, or albuminuria). (C) sion of nephropathy, optimize blood ease when there is uncertainty about
● There is not sufficient evidence to rec- pressure control. (A) the etiology of kidney disease (active
ommend aspirin for primary preven- urine sediment, absence of retinopathy,
tion in lower risk individuals, such as Screening rapid decline in GFR), difficult manage-
men ⬍50 years of age or women ⬍60 ● Perform an annual test to assess urine ment issues, or advanced kidney dis-
years of age without other major risk albumin excretion in type 1 diabetic pa- ease. (B)
factors. In patients in these age-groups tients with diabetes duration of ⱖ5
with multiple other risk factors, clinical years and in all type 2 diabetic patients
judgment is required. (C) starting at diagnosis. (E) Retinopathy screening and treatment
● Use aspirin therapy (75–162 mg/day) ● Measure serum creatinine at least annu- General recommendations
as a secondary prevention strategy in ally in all adults with diabetes regard- ● To reduce the risk or slow the progres-
those with diabetes with a history of less of the degree of urine albumin sion of retinopathy, optimize glycemic
CVD. (A) excretion. The serum creatinine should control. (A)
● For patients with CVD and docu- be used to estimate GFR and stage the ● To reduce the risk or slow the progres-
mented aspirin allergy, clopidogrel (75 level of chronic kidney disease (CKD), sion of retinopathy, optimize blood
mg/day) should be used. (B) if present. (E) pressure control. (A)
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S7
Executive Summary
Screening not increase the risk of retinal hemor- ● Consider age when setting glycemic
● Adults and children aged 10 years or rhage. (A) goals in children and adolescents with
older with type 1 diabetes should have type 1 diabetes, with less stringent goals
an initial dilated and comprehensive Neuropathy screening and treatment for younger children. (E)
eye examination by an ophthalmologist ● All patients should be screened for dis-
or optometrist within 5 years after the tal symmetric polyneuropathy (DPN) at Nephropathy
onset of diabetes. (B) diagnosis and at least annually thereaf- ● Annual screening for microalbumin-
● Patients with type 2 diabetes should ter, using simple clinical tests. (B) uria, with a random spot urine sample
have an initial dilated and comprehen- ● Electrophysiological testing is rarely for microalbumin-to-creatinine ratio,
sive eye examination by an ophthalmol- needed, except in situations where the should be initiated once the child is 10
ogist or optometrist shortly after the clinical features are atypical. (E) years of age and has had diabetes for 5
diagnosis of diabetes. (B) ● Screening for signs and symptoms of years. (E)
● Subsequent examinations for type 1 cardiovascular autonomic neuropathy ● Confirmed, persistently elevated mi-
and type 2 diabetic patients should should be instituted at diagnosis of type croalbumin levels on two additional
be repeated annually by an ophthal- 2 diabetes and 5 years after the diagno- urine specimens should be treated with
mologist or optometrist. Less-frequent sis of type 1 diabetes. Special testing is an ACE inhibitor, titrated to normaliza-
exams (every 2–3 years) may be consid- rarely needed and may not affect man- tion of microalbumin excretion if pos-
ered following one or more normal eye agement or outcomes. (E) sible. (E)
exams. Examinations will be required ● Medications for the relief of specific
more frequently if retinopathy is pro- symptoms related to DPN and auto- Hypertension
gressing. (B) nomic neuropathy are recommended, ● Treatment of high-normal blood pres-
● High-quality fundus photographs can as they improve the quality of life of the sure (systolic or diastolic blood pres-
detect most clinically significant dia- patient. (E) sure consistently above the 90th
betic retinopathy. Interpretation of the percentile for age, sex, and height)
images should be performed by a Foot care should include dietary intervention
trained eye care provider. While retinal ● For all patients with diabetes, perform and exercise, aimed at weight control
photography may serve as a screening an annual comprehensive foot exami- and increased physical activity, if ap-
tool for retinopathy, it is not a substi- nation to identify risk factors predictive propriate. If target blood pressure is not
tute for a comprehensive eye exam, of ulcers and amputations. The foot ex- reached with 3– 6 months of lifestyle
which should be performed at least ini- amination should include inspection, intervention, pharmacologic treatment
tially and at intervals thereafter as rec- assessment of foot pulses, and testing should be initiated. (E)
ommended by an eye care professional. for loss of protective sensation (10-g ● Pharmacologic treatment of hyperten-
(E) monofilament plus testing any one of: sion (systolic or diastolic blood pres-
● Women with preexisting diabetes who vibration using 128-Hz tuning fork, sure consistently above the 95th
are planning pregnancy or who have pinprick sensation, ankle reflexes, or percentile for age, sex, and height or
become pregnant should have a com- vibration perception threshold). (B) consistently greater than 130/80
prehensive eye examination and be ● Provide general foot self-care education mmHg, if 95% exceeds that value)
counseled on the risk of development to all patients with diabetes. (B) should be initiated as soon as the diag-
and/or progression of diabetic retinop- ● A multidisciplinary approach is recom- nosis is confirmed. (E)
athy. Eye examination should occur in mended for individuals with foot ulcers ● ACE inhibitors should be considered
the first trimester with close follow-up and high-risk feet, especially those with for the initial treatment of hyperten-
throughout pregnancy and for 1 year a history of prior ulcer or amputation. sion. (E)
postpartum. (B) (B) ● The goal of treatment is a blood pres-
● Refer patients who smoke, have loss of sure consistently ⬍130/80 or below the
protective sensation and structural ab- 90th percentile for age, sex, and height,
Treatment normalities, or have history of prior whichever is lower. (E)
● Promptly refer patients with any level of lower-extremity complications to foot
macular edema, severe nonproliferative care specialists for ongoing preventive Dyslipidemia
diabetic retinopathy (NPDR), or any care and life-long surveillance. (C) Screening
proliferative diabetic retinopathy ● Initial screening for peripheral artery ● If there is a family history of hypercho-
(PDR) to an ophthalmologist who is disease (PAD) should include a history lesterolemia (total cholesterol ⬎240
knowledgeable and experienced in the for claudication and an assessment of mg/dl) or a cardiovascular event before
management and treatment of diabetic the pedal pulses. Consider obtaining an age 55 years, or if family history is un-
retinopathy. (A) ankle-brachial index (ABI), as many pa- known, then a fasting lipid profile
● Laser photocoagulation therapy is indi- tients with PAD are asymptomatic. (C) should be performed on children ⬎2
cated to reduce the risk of vision loss in ● Refer patients with significant claudica- years of age soon after diagnosis (after
patients with high-risk PDR, clinically tion or a positive ABI for further vascu- glucose control has been established).
significant macular edema, and in some lar assessment and consider exercise, If family history is not of concern, then
cases of severe NPDR. (A) medications, and surgical options. (C) the first lipid screening should be per-
● The presence of retinopathy is not a formed at puberty (ⱖ10 years). All chil-
contraindication to aspirin therapy for Children and adolescents dren diagnosed with diabetes at or after
cardioprotection, as this therapy does Glycemic control puberty should have a fasting lipid pro-
S8 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Executive Summary
file performed soon after diagnosis Hypothyroidism ● Screening for diabetes complications
(after glucose control has been estab- ● Children with type 1 diabetes should be should be individualized in older
lished). (E) screened for thyroid peroxidase and adults, but particular attention should
● For both age-groups, if lipids are abnor- be paid to complications that would
thyroglobulin antibodies at diagnosis.
mal, annual monitoring is recom- (E) lead to functional impairment. (E)
mended. If LDL cholesterol values are ● TSH concentrations should be mea-
within the accepted risk levels (⬍100 sured after metabolic control has Diabetes care in the hospital
mg/dl [2.6 mmol/l]), a lipid profile been established. If normal, they ● All patients with diabetes admitted to
should be repeated every 5 years. (E) should be rechecked every 1–2 years, the hospital should have their diabetes
or if the patient develops symptoms clearly identified in the medical record.
Treatment of thyroid dysfunction, thyromegaly, (E)
● Initial therapy should consist of optimi- or an abnormal growth rate. Free T4 ● All patients with diabetes should have
zation of glucose control and MNT should be measured if TSH is abnor- an order for blood glucose monitoring,
using a Step II American Heart Associ- mal. (E) with results available to all members of
ation diet aimed at a decrease in the the health care team. (E)
amount of saturated fat in the diet. (E) Preconception care ● Goals for blood glucose levels:
● After the age of 10 years, the addition of ● A1C levels should be as close to normal ● Critically ill patients: Insulin ther-
a statin is recommended in patients as possible (⬍7%) in an individual pa- apy should be initiated for treat-
who, after MNT and lifestyle changes, tient before conception is attempted. ment of persistent hyperglycemia
have LDL cholesterol ⬎160 mg/dl (4.1 (B) starting at a threshold of no greater
mmol/l) or LDL cholesterol ⬎130 ● Starting at puberty, preconception than 180 mg/dl (10 mmol/l). Once
mg/dl (3.4 mmol/l) and one or more counseling should be incorporated in insulin therapy is started, a glucose
CVD risk factors. (E) the routine diabetes clinic visit for all range of 140 –180 mg/dl (7.8 to 10
● The goal of therapy is an LDL choles- women of child-bearing potential. (C) mmol/l) is recommended for the
terol value ⬍100 mg/dl (2.6 mmol/l). ● Women with diabetes who are contem- majority of critically ill patients. (A)
(E) plating pregnancy should be evaluated These patients require an intrave-
and, if indicated, treated for diabetic nous insulin protocol that has dem-
Retinopathy retinopathy, nephropathy, neuropathy, onstrated efficacy and safety in
and CVD. (E) achieving the desired glucose range
● The first ophthalmologic examination
● Medications used by such women without increasing risk for severe
should be obtained once the child is 10 should be evaluated prior to concep- hypoglycemia. (E)
years of age and has had diabetes for tion, since drugs commonly used to ● Non– critically ill patients: There is
3–5 years. (E) treat diabetes and its complications no clear evidence for specific blood
● After the initial examination, annual
may be contraindicated or not recom- glucose goals. If treated with insu-
routine follow-up is generally recom- mended in pregnancy, including st- lin, the premeal blood glucose tar-
mended. Less frequent examinations atins, ACE inhibitors, ARBs, and most get should generally be ⬍140 mg/dl
may be acceptable on the advice of an noninsulin therapies. (E) (7.8 mmol/l) with random blood
eye care professional. (E) glucose ⬍180 mg/dl (10.0 mmol/l),
Older adults provided these targets can be safely
Celiac disease ● Older adults who are functional, cogni- achieved. More stringent targets
● Children with type 1 diabetes should tively intact, and have significant life may be appropriate in stable pa-
be screened for celiac disease by mea- expectancy should receive diabetes care tients with previous tight glycemic
suring tissue transglutaminase or using goals developed for younger control. Less stringent targets may
anti-endomysial antibodies, with adults. (E) be appropriate in those with severe
documentation of normal serum IgA ● Glycemic goals for older adults not comorbidites. (E)
levels, soon after the diagnosis of di- meeting the above criteria may be re- ● Scheduled subcutaneous insulin with
abetes. (E) laxed using individual criteria, but hy- basal, nutritional, and correction.
● Testing should be repeated if growth perglycemia leading to symptoms or Components is the preferred method
failure, failure to gain weight, weight risk of acute hyperglycemic complica- for achieving and maintaining glucose
loss, or gastroenterologic symptoms oc- tions should be avoided in all patients. control in noncritically ill patients. (C)
cur. (E) (E) Using correction dose or “supplemen-
● Consideration should be given to peri- ● Other cardiovascular risk factors tal” insulin to correct premeal hyper-
odic re-screening of asymptomatic in- should be treated in older adults with glycemia in addition to scheduled
dividuals. (E) consideration of the time frame of ben- prandial and basal insulin is recom-
● Children with positive antibodies efit and the individual patient. Treat- mended. (E)
should be referred to a gastroenterolo- ment of hypertension is indicated in ● Glucose monitoring should be initiated
gist for evaluation. (E) virtually all older adults, and lipid and in any patient not known to be diabetic
● Children with confirmed celiac disease aspirin therapy may benefit those with who receives therapy associated with
should have consultation with a dieti- life expectancy at least equal to the time high risk for hyperglycemia, including
tian and placed on a gluten-free diet. frame of primary or secondary preven- high-dose glucocorticoid therapy, initi-
(E) tion trials. (E) ation of enteral or parenteral nutrition,
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S9
Executive Summary
or other medications such as octreotide ● A plan for treating hypoglycemia previous 2–3 months is not available.
or immunosuppressive medications. should be established for each patient. (E)
(B) If hyperglycemia is documented Episodes of hypoglycemia in the hospi- ● Patients with hyperglycemia in the hos-
and persistent, treatment is necessary. tal should be tracked. (E) pital who do not have a diagnosis of
Such patients should be treated to the ● All patients with diabetes admitted to diabetes should have appropriate plans
same glycemic goals as patients with the hospital should have an A1C ob- for follow-up testing and care docu-
known diabetes. (E) tained if the result of testing in the mented at discharge. (E)
S10 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
P O S I T I O N S T A T E M E N T
Standards of Medical Care in Diabetes—2010
AMERICAN DIABETES ASSOCIATION
D
iabetes is a chronic illness that re- more detailed information about manage- by the Executive Committee of ADA’s
quires continuing medical care and ment of diabetes, refer to references 1–3. Board of Directors.
ongoing patient self-management The recommendations included are
education and support to prevent acute screening, diagnostic, and therapeutic ac- I. CLASSIFICATION AND
complications and to reduce the risk of tions that are known or believed to favor- DIAGNOSIS
long-term complications. Diabetes care is ably affect health outcomes of patients A. Classification
complex and requires that many issues, with diabetes. A grading system (Table 1), The classification of diabetes includes
beyond glycemic control, be addressed. A developed by the American Diabetes As- four clinical classes:
large body of evidence exists that sup- sociation (ADA) and modeled after exist-
ports a range of interventions to improve ing methods, was used to clarify and ● type 1 diabetes (results from -cell de-
diabetes outcomes. codify the evidence that forms the basis struction, usually leading to absolute
These standards of care are intended for the recommendations. The level of ev- insulin deficiency)
to provide clinicians, patients, research- idence that supports each recommenda- ● type 2 diabetes (results from a progres-
ers, payors, and other interested individ- sive insulin secretory defect on the
tion is listed after each recommendation
uals with the components of diabetes background of insulin resistance)
using the letters A, B, C, or E.
care, general treatment goals, and tools to ● other specific types of diabetes due to
evaluate the quality of care. While indi- These standards of care are revised
annually by the ADA multidisciplinary other causes, e.g., genetic defects in
vidual preferences, comorbidities, and -cell function, genetic defects in insu-
other patient factors may require modifi- Professional Practice Committee, and
new evidence is incorporated. Members lin action, diseases of the exocrine pan-
cation of goals, targets that are desirable creas (such as cystic fibrosis), and drug-
for most patients with diabetes are pro- of the Professional Practice Committee
or chemical-induced diabetes (such as
vided. These standards are not intended and their disclosed conflicts of interest are
in the treatment of AIDS or after organ
to preclude clinical judgment or more ex- listed in the Introduction. Subsequently,
transplantation)
tensive evaluation and management of the as with all position statements, the stan- ● gestational diabetes mellitus (GDM)
patient by other specialists as needed. For dards of care are reviewed and approved (diabetes diagnosed during pregnancy)
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
Originally approved 1988. Most recent review/revision October 2009. Some patients cannot be clearly classified
DOI: 10.2337/dc10-S011 as having type 1 or type 2 diabetes. Clin-
Abbreviations: ABI, ankle-brachial index; ACCORD, Action to Control Cardiovascular Risk in Diabetes;
ADAG, A1C-Derived Average Glucose Trial; ADVANCE, Action in Diabetes and Vascular Disease: Pre-
ical presentation and disease progression
terax and Diamicron Modified Release Controlled Evaluation; ACE, angiotensin converting enzyme; ARB, vary considerably in both types of diabe-
angiotensin receptor blocker; ACT-NOW, ACTos Now Study for the Prevention of Diabetes; BMI, body tes. Occasionally, patients who otherwise
mass index; CBG, capillary blood glucose; CFRD, cystic fibrosis–related diabetes; CGM, continuous have type 2 diabetes may present with ke-
glucose monitoring; CHD, coronary heart disease; CHF, congestive heart failure; CCM, chronic care toacidosis. Similarly, patients with type 1
model; CKD, chronic kidney disease; CMS, Centers for Medicare and Medicaid Services; CSII, continuous
subcutaneous insulin infusion; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hyper- diabetes may have a late onset and slow
tension; DCCT, Diabetes Control and Complications Trial; DKA, diabetic ketoacidosis; DMMP, diabetes (but relentless) progression despite hav-
medical management plan; DPN, distal symmetric polyneuropathy; DPP, Diabetes Prevention Program; ing features of autoimmune disease. Such
DPS, Diabetes Prevention Study; DREAM, Diabetes Reduction Assessment with Ramipril and Rosiglita- difficulties in diagnosis may occur in chil-
zone Medication; DRS, Diabetic Retinopathy Study; DSME, diabetes self-management education; DSMT,
diabetes self-management training; eAG, estimated average glucose; eGFR, estimated glomerular filtration
dren, adolescents, and adults. The true
rate; ECG, electrocardiogram; EDIC, Epidemiology of Diabetes Interventions and Complications; ERP, diagnosis may become more obvious over
education recognition program; ESRD, end-stage renal disease; ETDRS, Early Treatment Diabetic Reti- time.
nopathy Study; FDA, Food and Drug Administration; FPG, fasting plasma glucose; GDM, gestational
diabetes mellitus; GFR, glomerular filtration rate; HAPO, Hyperglycemia and Adverse Pregnancy Out- B. Diagnosis of diabetes
comes; ICU, intensive care unit; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; Look
AHEAD, Action for Health in Diabetes; MDRD, Modification of Diet in Renal Disease; MNT, medical Recommendations
nutrition therapy; NDEP, National Diabetes Education Program; NGSP, National Glycohemoglobin Stan- For decades, the diagnosis of diabetes has
dardization Program; NPDR, nonproliferative diabetic retinopathy; OGTT, oral glucose tolerance test;
PAD, peripheral arterial disease; PCOS, polycystic ovarian syndrome; PDR, proliferative diabetic retinop- been based on plasma glucose (PG) crite-
athy; PPG, postprandial plasma glucose; RAS, renin-angiotensin system; SMBG, self-monitoring of blood ria, either fasting PG (FPG) or 2-h 75-g
glucose; STOP-NIDDM, Study to Prevent Non-Insulin Dependent Diabetes; SSI, sliding scale insulin; oral glucose tolerance test (OGTT) values.
TZD, thiazolidinedione; UKPDS, U.K. Prospective Diabetes Study; VADT, Veterans Affairs Diabetes Trial; In 1997, the first Expert Committee on
XENDOS, XENical in the prevention of Diabetes in Obese Subjects.
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly
the Diagnosis and Classification of Diabe-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. tes Mellitus revised the diagnostic criteria
org/licenses/by-nc-nd/3.0/ for details. using the observed association between
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S11
Standards of Medical Care
Table 1 —ADA evidence grading system for clinical practice recommendations be used (an updated list of A1C assays and
whether abnormal hemoglobins impact
Level of them is available at www.ngsp.org/prog/
evidence Description index3.html). For conditions with abnor-
mal red cell turnover, such as pregnancy or
A Clear evidence from well-conducted, generalizable, randomized controlled trials that anemias from hemolysis and iron defi-
are adequately powered, including: ciency, the diagnosis of diabetes must use
● Evidence from a well-conducted multicenter trial glucose criteria exclusively.
● Evidence from a meta-analysis that incorporated quality ratings in the analysis The established glucose criteria for
Compelling nonexperimental evidence, i.e., ⬙all or none⬙ rule developed by Center the diagnosis of diabetes (FPG and 2-h
for Evidence Based Medicine at Oxford PG) remain valid. Patients with severe hy-
Supportive evidence from well-conducted randomized controlled trials that are perglycemia such as those who present
adequately powered, including: with severe classic hyperglycemic symp-
● Evidence from a well-conducted trial at one or more institutions toms or hyperglycemic crisis can continue
● Evidence from a meta-analysis that incorporated quality ratings in the analysis to be diagnosed when a random (or ca-
B Supportive evidence from well-conducted cohort studies: sual) PG of ⱖ200 mg/dl (11.1 mmol/l) is
● Evidence from a well-conducted prospective cohort study or registry found. It is likely that in such cases the
● Evidence from a well-conducted meta-analysis of cohort studies health care professional would also con-
Supportive evidence from a well-conducted case-control study duct an A1C test as part of the initial as-
C Supportive evidence from poorly controlled or uncontrolled studies sessment of the severity of the diabetes
● Evidence from randomized clinical trials with one or more major or three or and that it would be above the diagnostic
more minor methodological flaws that could invalidate the results cut point. However, in rapidly evolving
● Evidence from observational studies with high potential for bias (such as case diabetes such as the development of type
series with comparison to historical controls) 1 in some children, the A1C may not be
● Evidence from case series or case reports significantly elevated despite frank
Conflicting evidence with the weight of evidence supporting the recommendation diabetes.
E Expert consensus or clinical experience Just as there is ⬍100% concordance
between the FPG and 2-h PG tests, there
is not perfect concordance between A1C
glucose levels and presence of retinopa- the A1C test to diagnose diabetes with a and either glucose-based test. Analyses of
thy as the key factor with which to iden- threshold of ⱖ6.5%, and ADA affirms this National Health and Nutrition Examina-
tify threshold FPG and 2-h PG levels. The decision (6). The diagnostic test should tion Survey (NHANES) data indicate that,
committee examined data from three be performed using a method certified by assuming universal screening of the undi-
cross-sectional epidemiologic studies that the National Glycohemoglobin Standard- agnosed, the A1C cut point of ⱖ6.5%
assessed retinopathy with fundus photog- ization Program (NGSP) and standard- identifies one-third fewer cases of undiag-
raphy or direct ophthalmoscopy and ized or traceable to the Diabetes Control nosed diabetes than a fasting glucose cut
measured glycemia as FPG, 2-h PG, and and Complications Trial (DCCT) refer- point of ⱖ126 mg/dl (7.0 mmol/l) (E.
HbA1c (A1C). The studies demonstrated ence assay. Point-of-care A1C assays are Gregg, personal communication). How-
glycemic levels below which there was lit- not sufficiently accurate at this time to use ever, in practice, a large portion of the
tle prevalent retinopathy and above for diagnostic purposes. diabetic population remains unaware of
which the prevalence of retinopathy in- Epidemiologic datasets show a rela- their condition. Thus, the lower sensitiv-
creased in an apparently linear fashion. tionship between A1C and the risk of ret- ity of A1C at the designated cut point may
The deciles of FPG, 2-h PG, and A1C at inopathy similar to that which has been well be offset by the test’s greater practi-
which retinopathy began to increase were shown for corresponding FPG and 2-h PG cality, and wider application of a more
the same for each measure within each thresholds. The A1C has several advan- convenient test (A1C) may actually in-
population. The analyses helped to in- tages to the FPG, including greater conve- crease the number of diagnoses made.
form a then-new diagnostic cut point of nience, since fasting is not required; As with most diagnostic tests, a test
ⱖ126 mg/dl (7.0 mmol/l) for FPG and evidence to suggest greater preanalytical result diagnostic of diabetes should be re-
confirmed the long-standing diagnostic stability; and less day-to-day perturba- peated to rule out laboratory error, unless
2-h PG value of ⱖ200 mg/dl (11.1 tions during periods of stress and illness. the diagnosis is clear on clinical grounds,
mmol/l) (4). These advantages must be balanced by such as a patient with classic symptoms of
ADA has not previously recom- greater cost, limited availability of A1C hyperglycemia or hyperglycemic crisis. It
mended the use of A1C for diagnosing testing in certain regions of the develop- is preferable that the same test be repeated
diabetes, in part due to lack of standard- ing world, and incomplete correlation be- for confirmation, since there will be a
ization of the assay. However, A1C assays tween A1C and average glucose in certain greater likelihood of concurrence in this
are now highly standardized, and their re- individuals. In addition, the A1C can be case. For example, if the A1C is 7.0% and
sults can be uniformly applied both tem- misleading in patients with certain forms a repeat result is 6.8%, the diagnosis of
porally and across populations. In a of anemia and hemoglobinopathies. For diabetes is confirmed. However, there are
recent report (5), after an extensive review patients with a hemoglobinopathy but scenarios in which results of two different
of both established and emerging epide- normal red cell turnover, such as sickle tests (e.g., FPG and A1C) are available for
miological evidence, an international ex- cell trait, an A1C assay without interfer- the same patient. In this situation, if the
pert committee recommended the use of ence from abnormal hemoglobins should two different tests are both above the di-
S12 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 2—Criteria for the diagnosis of diabetes costs of false positives (falsely identifying
1. A1C ⱖ6.5%. The test should be performed in a laboratory using a method and then spending intervention resources
that is NGSP certified and standardized to the DCCT assay.* on those who were not going to develop
OR diabetes anyway).
2. FPG ⱖ126 mg/dl (7.0 mmol/l). Fasting is defined as no caloric intake for at Linear regression analyses of nation-
least 8 h.* ally representative U.S. data (NHANES
OR 2005–2006) indicate that among the
3. Two-hour plasma glucose ⱖ200 mg/dl (11.1 mmol/l) during an OGTT. nondiabetic adult population, an FPG of
The test should be performed as described by the World Health 110 mg/dl corresponds to an A1C of
Organization, using a glucose load containing the equivalent of 75 g 5.6%, while an FPG of 100 mg/dl corre-
anhydrous glucose dissolved in water.* sponds to an A1C of 5.4%. Receiver op-
OR erating curve analyses of these data
4. In a patient with classic symptoms of hyperglycemia or hyperglycemic indicate that an A1C value of 5.7%, com-
crisis, a random plasma glucose ⱖ200 mg/dl (11.1 mmol/l). pared with other cut points, has the best
combination of sensitivity (39%) and
*In the absence of unequivocal hyperglycemia, criteria 1–3 should be confirmed by repeat testing.
specificity (91%) to identify cases of IFG
(FPG ⱖ100 mg/dl [5.6 mmol/l]) (R.T.
agnostic threshold, the diagnosis of dia- or impaired glucose tolerance (IGT) (2-h Ackerman, Personal Communication).
betes is confirmed. OGTT values of 140 mg/dl [7.8 mmol/l] Other analyses suggest that an A1C of
On the other hand, if two different to 199 mg/dl [11.0 mmol/l]). 5.7% is associated with diabetes risk sim-
tests are available in an individual and the Individuals with IFG and/or IGT have ilar to that of the high-risk participants in
results are discordant, the test whose re- been referred to as having pre-diabetes, the Diabetes Prevention Program (DPP)
sult is above the diagnostic cut point indicating the relatively high risk for the (R.T. Ackerman, personal communica-
should be repeated, and the diagnosis is future development of diabetes. IFG and tion). Hence, it is reasonable to consider
made on the basis of the confirmed test. IGT should not be viewed as clinical en- an A1C range of 5.7– 6.4% as identifying
That is, if a patient meets the diabetes cri- tities in their own right but rather risk individuals with high risk for future dia-
terion of the A1C (two results ⱖ6.5%) but factors for diabetes as well as cardiovas- betes and to whom the term pre-diabetes
not the FPG (⬍126 mg/dl or 7.0 mmol/l), cular disease (CVD). IFG and IGT are may be applied (6).
or vice versa, that person should be con- associated with obesity (especially As is the case for individuals found to
sidered to have diabetes. Admittedly, in abdominal or visceral obesity), dyslipide- have IFG and IGT, individuals with an
most circumstance the “nondiabetic” test mia with high triglycerides and/or low A1C of 5.7– 6.4% should be informed of
is likely to be in a range very close to the HDL cholesterol, and hypertension. their increased risk for diabetes as well
threshold that defines diabetes. Structured lifestyle intervention, aimed at as CVD and counseled about effective
Since there is preanalytic and analytic increasing physical activity and produc- strategies to lower their risks (see IV. PRE-
variability of all the tests, it is also possible ing 5–10% loss of body weight, and cer- VENTION/DELAY OF TYPE 2 DIABETES).
that when a test whose result was above tain pharmacological agents have been As with glucose measurements, the contin-
the diagnostic threshold is repeated, the demonstrated to prevent or delay the de- uum of risk is curvilinear, so that as A1C
second value will be below the diagnostic velopment of diabetes in people with IGT rises, the risk of diabetes rises dispropor-
cut point. This is least likely for A1C, (see Table 7). It should be noted that the tionately. Accordingly, interventions
somewhat more likely for FPG, and most 2003 ADA Expert Committee report re- should be most intensive and follow-up
likely for the 2-h PG. Barring a laboratory duced the lower FPG cut point to define should be particularly vigilant for those
error, such patients are likely to have test IFG from 110 mg/dl (6.1 mmol/l) to 100 with an A1C ⬎6.0%, who should be con-
results near the margins of the threshold mg/dl (5.6 mmol/l), in part to make the sidered to be at very high risk. However,
for a diagnosis. The healthcare profes- prevalence of IFG more similar to that of just as an individual with a fasting glucose of
sional might opt to follow the patient IGT. However, the World Health Organi- 98 mg/dl (5.4 mmol/l) may not be at negli-
closely and repeat the testing in 3– 6 zation (WHO) and many other diabetes gible risk for diabetes, individuals with an
months. organizations did not adopt this change. A1C ⬍5.7% may still be at risk, depending
The current diagnostic criteria for di- As the A1C becomes increasingly on the level of A1C and presence of other
abetes are summarized in Table 2. used to diagnose diabetes in individuals risk factors, such as obesity and family
with risk factors, it will also identify those history.
C. Categories of increased risk for at high risk for developing diabetes in the
diabetes future. As was the case with the glucose Table 3—Categories of increased risk for
In 1997 and 2003, The Expert Committee measures, defining a lower limit of an in- diabetes*
on the Diagnosis and Classification of Di- termediate category of A1C is somewhat FPG 100–125 mg/dl (5.6–6.9 mmol/l)
abetes Mellitus (4,7) recognized an inter- arbitrary, since risk of diabetes with any 关IFG兴
mediate group of individuals whose measure or surrogate of glycemia is a con- 2-h PG on the 75-g OGTT 140–199 mg/dl
glucose levels, although not meeting cri- tinuum extending well into the normal (7.8–11.0 mmol/l) 关IGT兴
teria for diabetes, are nevertheless too ranges. To maximize equity and efficiency A1C 5.7–6.4%
high to be considered normal. This group of preventive interventions, such an A1C
*For all three tests, risk is continuous, extending
was defined as having impaired fasting cut point, should balance the costs of false below the lower limit of the range and becoming
glucose (IFG) (FPG levels of 100 mg/dl negatives (failing to identify those who are disproportionately greater at higher ends of the
[5.6 mmol/l] to 125 mg/dl [6.9 mmol/l]) going to develop diabetes) against the range.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S13
Standards of Medical Care
Table 4—Criteria for testing for diabetes in asymptomatic adult individuals Recommendations for testing for dia-
1. Testing should be considered in all adults who are overweight (BMI ⱖ25 kg/m *) and
2 betes in asymptomatic undiagnosed
have additional risk factors: adults are listed in Table 4. Testing should
● physical inactivity
be considered in adults of any age with
● first-degree relative with diabetes
BMI ⱖ25 kg/m2 and one or more risk fac-
● members of a high-risk ethnic population (e.g., African American, Latino, Native
tors for diabetes. Because age is a major
American, Asian American, Pacific Islander)
risk factor for diabetes, testing of those
● women who delivered a baby weighing ⬎9 lb or were diagnosed with GDM
without other risk factors should begin no
● hypertension (ⱖ140/90 mmHg or on therapy for hypertension)
later than at age 45 years.
● HDL cholesterol level ⬍35 mg/dl (0.90 mmol/l) and/or a triglyceride level ⬎250
Either A1C, FPG, or 2-h OGTT is ap-
mg/dl (2.82 mmol/l)
propriate for testing. The 2-h OGTT identi-
● women with polycystic ovary syndrome
fies people with either IFG or IGT and thus
● A1C ⱖ5.7%, IGT, or IFG on previous testing
more people at increased risk for the devel-
● other clinical conditions associated with insulin resistance (e.g., severe obesity,
opment of diabetes and CVD. It should be
acanthosis nigricans)
noted that the two tests do not necessarily
● history of CVD
detect the same individuals (10). The effi-
2. In the absence of the above criteria, testing diabetes should begin at age 45 years
cacy of interventions for primary preven-
3. If results are normal, testing should be repeated at least at 3-year intervals, with tion of type 2 diabetes (11–17) has
consideration of more frequent testing depending on initial results and risk primarily been demonstrated among indi-
status. viduals with IGT, but not for individuals
with IFG (who do not also have IGT) or
*At-risk BMI may be lower in some ethnic groups.
those with specific A1C levels.
The appropriate interval between
Table 3 summarizes the categories of who the provider tests because of high tests is not known (18). The rationale for
increased risk for diabetes. suspicion of diabetes, to the symptomatic the 3-year interval is that false negatives
patient. The discussion herein is primar- will be repeated before substantial time
II. TESTING FOR DIABETES ily framed as testing for diabetes in indi- elapses, and there is little likelihood that
IN ASYMPTOMATIC viduals without symptoms. Testing for an individual will develop significant
PATIENTS diabetes will also detect individuals at in- complications of diabetes within 3 years
creased future risk for diabetes, herein re- of a negative test result.
Recommendations ferred to as pre-diabetic. Because of the need for follow-up and
● Testing to detect type 2 diabetes and discussion of abnormal results, testing
assess risk for future diabetes in asymp- A. Testing for type 2 diabetes and should be carried out within the health
tomatic people should be considered in risk of future diabetes in adults care setting. Community screening out-
adults of any age who are overweight or Type 2 diabetes is frequently not diag- side a health care setting is not recom-
obese (BMI ⱖ25 kg/m2) and who have nosed until complications appear, and mended because people with positive
one or more additional risk factors for approximately one-fourth of all people tests may not seek, or have access to, ap-
diabetes (Table 4). In those without with diabetes in the U.S. may be undiag- propriate follow-up testing and care.
these risk factors, testing should begin nosed. Although the effectiveness of early Conversely, there may be failure to ensure
at age 45 years. (B) identification of pre-diabetes and diabetes appropriate repeat testing for individuals
● If tests are normal, repeat testing should through mass testing of asymptomatic in- who test negative. Community screening
be carried out at least at 3-year inter- dividuals has not been proven definitively may also be poorly targeted, i.e., it may
vals. (E) (and rigorous trials to provide such proof fail to reach the groups most at risk and
● To test for diabetes or to assess risk of are unlikely to occur), pre-diabetes and inappropriately test those at low risk (the
future diabetes, either A1C, FPG , or diabetes meet established criteria for con- worried well) or even those already diag-
2-h 75-g OGTT are appropriate. (B) ditions in which early detection is appro- nosed (19,20).
● In those identified with increased risk priate. Both conditions are common, are
for future diabetes, identify and, if ap- increasing in prevalence, and impose sig-
propriate, treat other CVD risk factors. nificant public health burdens. There is a B. Testing for type 2 diabetes in
(B) long presymptomatic phase before the di- children
agnosis of type 2 diabetes is usually made. The incidence of type 2 diabetes in ado-
For many illnesses there is a major dis- Relatively simple tests are available to de- lescents has increased dramatically in the
tinction between screening and diagnos- tect preclinical disease (9). Additionally, last decade, especially in minority popu-
tic testing. However, for diabetes the same the duration of glycemic burden is a lations (21), although the disease remains
tests would be used for “screening” as for strong predictor of adverse outcomes, rare in the general pediatric population
diagnosis. Type 2 diabetes has a long and effective interventions exist to pre- (22). Consistent with recommendations
asymptomatic phase and significant clin- vent progression of pre-diabetes to diabe- for adults, children and youth at in-
ical risk markers. Diabetes may be identi- tes (see IV. PREVENTION/DELAY OF creased risk for the presence or the devel-
fied anywhere along a spectrum of clinical TYPE 2 DIABETES) and to reduce risk of opment of type 2 diabetes should be
scenarios ranging from a seemingly low- complications of diabetes (see VI. PRE- tested within the health care setting (23).
risk individual who happens to have glu- VENTION AND MANAGEMENT OF DI- The recommendations of the ADA con-
cose testing, to a higher-risk individual ABETES COMPLICATIONS). sensus statement on type 2 diabetes in
S14 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 5—Testing for type 2 diabetes in asymptomatic children within ranges previously considered nor-
Criteria: Overweight (BMI ⬎85th percentile for age and sex, weight for height mal for pregnancy. For most complica-
⬎85th percentile, or weight ⬎120% of ideal for height) tions there was no threshold for risk.
Plus any two of ● Family history of type 2 diabetes in first- or second-degree relative
These results have led to careful reconsid-
the following ● Race/ethnicity (Native American, African American, Latino, Asian
eration of the diagnostic criteria for GDM.
risk factors: American, Pacific Islander) The IADPSG recommended that all
● Signs of insulin resistance or conditions associated with insulin
women not known to have prior diabetes
resistance (acanthosis nigricans, hypertension, dyslipidemia, undergo a 75-g OGTT at 24 –28 weeks of
polycystic ovary syndrome, or small for gestational age gestation. The group developed diagnos-
birthweight) tic cut points for the fasting, 1-h, and 2-h
● Maternal history of diabetes or GDM during the child’s gestation
PG measurements that conveyed an odds
Age of Age 10 years or at onset of puberty, if puberty occurs at a younger ratio for adverse outcomes of at least 1.75
initiation: age compared with women with the mean
Frequency: Every 3 years glucose levels in the HAPO study.
At the time of this update to the Stan-
dards of Medical Care in Diabetes, ADA is
children and youth, with some modifica- set or first recognition during pregnancy planning to work with U.S. obstetrical or-
tions, are summarized in Table 5. (4). Although most cases resolve with de- ganizations to consider adoption of the
livery, the definition applied whether the IADPSG diagnostic criteria and to discuss
C. Screening for type 1 diabetes condition persisted after pregnancy and the implications of this change. While this
Generally, people with type 1 diabetes did not exclude the possibility that unrec- change will significantly increase the
present with acute symptoms of diabetes ognized glucose intolerance may have an- prevalence of GDM, there is mounting ev-
and markedly elevated blood glucose lev- tedated or begun concomitantly with the idence that treating even mild GDM re-
els, and most cases are diagnosed soon pregnancy. This definition facilitated a duces morbidity for both mother and
after the onset of hyperglycemia. How- uniform strategy for detection and classi- baby (27).
ever, evidence from type 1 diabetes pre- fication of GDM, but its limitations were Because women with a history of
vention studies suggests that measurement recognized for many years. As the ongo- GDM have a greatly increased subsequent
of islet autoantibodies identifies individ- ing epidemic of obesity and diabetes has risk for diabetes (28), they should be
uals who are at risk for developing type 1 led to more type 2 diabetes in women of screened for diabetes 6 –12 weeks post-
diabetes. Such testing may be appropriate childbearing age, the number of pregnant partum, using nonpregnant OGTT crite-
in high-risk individuals, such as those women with undiagnosed type 2 diabetes ria, and should be followed up with
with prior transient hyperglycemia or has increased (24). After deliberations in subsequent screening for the develop-
those who have relatives with type 1 dia- 2008 –2009, the International Associa- ment of diabetes or pre-diabetes, as out-
betes, in the context of clinical research tion of Diabetes and Pregnancy Study lined in II. TESTING FOR DIABETES IN
studies (see, for example, http://www2. Groups (IADPSG), an international con- ASYMPTOMATIC PATIENTS. Informa-
diabetestrialnet.org). Widespread clini- sensus group with representatives from tion on the National Diabetes Education
cal testing of asymptomatic low-risk multiple obstetrical and diabetes organi- Program (NDEP) campaign to prevent
individuals cannot currently be recom- zations, including ADA, recommended type 2 diabetes in women with GDM can
mended, as it would identify very few in- that high-risk women found to have dia- be found at http://ndep.nih.gov/media/
dividuals in the general population who betes at their initial prenatal visit using NeverTooEarly_Tipsheet.pdf.
are at risk. Individuals who screen posi- standard criteria (Table 2) receive a diag-
tive should be counseled about their risk nosis of overt, not gestational, diabetes. IV. PREVENTION/DELAY
of developing diabetes. Clinical studies Approximately 7% of all pregnancies OF TYPE 2 DIABETES
are being conducted to test various meth- (ranging from 1 to 14% depending on the
ods of preventing type 1 diabetes or re- population studied and the diagnostic Recommendations
versing early type 1 diabetes in those with tests used) are complicated by GDM, re- ● Patients with IGT (A), IFG (E), or an
evidence of autoimmunity. sulting in more than 200,000 cases A1C of 5.7– 6.4% (E) should be re-
annually. ferred to an effective ongoing support
III. DETECTION AND Because of the risks of GDM to the program for weight loss of 5–10% of
DIAGNOSIS OF GDM mother and neonate, screening and diag- body weight and an increase in physical
nosis are warranted. Current screening activity of at least 150 min/week of
Recommendations and diagnostic strategies, based on the moderate activity such as walking.
● Screen for GDM using risk factor anal- 2004 ADA position statement on GDM ● Follow-up counseling appears to be im-
ysis and, if appropriate, an OGTT. (C) (25), are outlined in Table 6. portant for success. (B)
● Women with GDM should be screened Results of the Hyperglycemia and Ad- ● Based on potential cost savings of dia-
for diabetes 6 –12 weeks postpartum verse Pregnancy Outcomes (HAPO) study betes prevention, such counseling
and should be followed up with subse- (26), a large-scale (⬃25,000 pregnant should be covered by third-party pay-
quent screening for the development of women) multinational epidemiologic ors. (E)
diabetes or pre-diabetes. (E) study, demonstrated that risk of adverse ● In addition to lifestyle counseling, met-
maternal, fetal, and neonatal outcomes formin may be considered in those who
For many years, GDM has been defined as continuously increased as a function of are at very high risk for developing di-
any degree of glucose intolerance with on- maternal glycemia at 24 –28 weeks, even abetes (combined IFG and IGT plus
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S15
Standards of Medical Care
Table 6—Screening for and diagnosis of GDM other drugs, the issues of cost, side effects,
Carry out diabetes risk assessment at the first prenatal visit.
and lack of persistence of effect in some
Women at very high risk should be screened for diabetes as soon as possible after the studies led the panel to not recommend
confirmation of pregnancy. Criteria for very high risk are: use for diabetes prevention. Metformin
● Severe obesity
use was recommended only for very-
● Prior history of GDM or delivery of large-for-gestational-age infant
high-risk individuals (those with com-
● Presence of glycosuria
bined IGT and IFG who are obese and
● Diagnosis of PCOS
have at least one other risk factor for dia-
● Strong family history of type 2 diabetes
betes) who are under 60 years of age. In
Screening/diagnosis at this stage of pregnancy should use standard diagnostic testing (Table addition, the panel highlighted the evi-
2). dence that in the DPP, metformin was
All women of greater than low risk of GDM, including those above not found to have diabetes most effective compared with lifestyle in
early in pregnancy, should undergo GDM testing at 24–28 weeks of gestation. Low- individuals with BMI ⱖ35 kg/m2 and
risk status, which does not require GDM screening, is defined as women with ALL of those under age 60 years.
the following characteristics:
● Age ⬍25 years
V. DIABETES CARE
● Weight normal before pregnancy
● Member of an ethnic group with a low prevalence of diabetes
A. Initial evaluation
● No known diabetes in first-degree relatives
A complete medical evaluation should be
● No history of abnormal glucose tolerance
performed to classify the diabetes, detect
● No history of poor obstetrical outcome
the presence of diabetes complications,
Two approaches may be followed for GDM screening at 24–28 weeks: review previous treatment and glycemic
1. Two-step approach: control in patients with established diabe-
A. Perform initial screening by measuring plasma or serum glucose 1 h after a 50-g load tes, assist in formulating a management
of ⱖ140 mg/dl identifies ⬃80% of women with GDM, while the sensitivity is further plan, and provide a basis for continuing
increased to ⬃90% by a threshold of ⱖ130 mg/dl. care. Laboratory tests appropriate to the
B. Perform a diagnostic 100-g OGTT on a separate day in women who exceed the chosen evaluation of each patient’s medical con-
threshold on 50-g screening. dition should be performed. A focus on
2. One-step approach (may be preferred in clinics with high prevalence of GDM): Perform the components of comprehensive care
a diagnostic 100-g OGTT in all women to be tested at 24–28 weeks. (Table 8) will assist the health care team to
The 100-g OGTT should be performed in the morning after an overnight fast of at least 8 ensure optimal management of the pa-
h. tient with diabetes.
To make a diagnosis of GDM, at least two of the following plasma glucose values must be
found: B. Management
● Fasting ⱖ95 mg/dl
People with diabetes should receive med-
● 1-h ⱖ180 mg/dl
ical care from a physician-coordinated
● 2-h ⱖ155 mg/dl
team. Such teams may include, but are
● 3-h ⱖ140 mg/dl
not limited to, physicians, nurse practitio-
ners, physician’s assistants, nurses, dieti-
tians, pharmacists, and mental health
other risk factors such as A1C ⬎6%, been shown to decrease incident diabetes professionals with expertise and a special
hypertension, low HDL cholesterol, el- to various degrees. A summary of major interest in diabetes. It is essential in this
evated triglycerides, or family history of diabetes prevention trials is shown in Ta- collaborative and integrated team ap-
diabetes in a first-degree relative) and ble 7. proach that individuals with diabetes as-
who are obese and under 60 years of Two studies of lifestyle intervention sume an active role in their care.
age. (E) have shown persistent reduction in the The management plan should be for-
● Monitoring for the development of di- role of conversion to type 2 diabetes with mulated as a collaborative therapeutic al-
abetes in those with pre-diabetes 3 years (29) to 14 years (30) of postinter- liance among the patient and family, the
should be performed every year. (E) vention follow-up. physician, and other members of the
Based on the results of clinical trials health care team. A variety of strategies
Randomized controlled trials have shown and the known risks of progression of and techniques should be used to provide
that individuals at high risk for develop- pre-diabetes to diabetes, an ADA Consen- adequate education and development of
ing diabetes (those with IFG, IGT, or sus Development Panel (36) concluded problem-solving skills in the various as-
both) can be given interventions that sig- that people with IGT and/or IFG should pects of diabetes management. Imple-
nificantly decrease the rate of onset of di- be counseled on lifestyle changes with mentation of the management plan
abetes (11–17). These interventions goals similar to those of the DPP (5–10% requires that each aspect is understood
include intensive lifestyle modification weight loss and moderate physical activ- and agreed to by the patient and the care
programs that have been shown to be very ity of ⬃30 min/day). Regarding the more providers and that the goals and treat-
effective (58% reduction after 3 years) difficult issue of drug therapy for diabetes ment plan are reasonable. Any plan
and use of the pharmacologic agents met- prevention, the consensus panel felt that should recognize diabetes self-manage-
formin, ␣-glucosidase inhibitors, orlistat, metformin should be the only drug con- ment education (DSME) and on-going di-
and thiazolidinediones, each of which has sidered for use in diabetes prevention. For abetes support as an integral component
S16 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 7—Therapies proven effective in diabetes prevention trials
Incidence in 3-Year
Mean control Relative risk number
age Duration Intervention subjects reduction (%) needed to
Study (ref.) n Population (years) (years) (daily dose) (%/year) (95% CI) treat*
Lifestyle
Finnish DPS (12) 522 IGT, BMI ⱖ25 kg/m2 55 3.2 I-D&E 6 58 (30–70) 8.5
DPP (11) 2,161† IGT, BMI ⱖ24 kg/m2, 51 3 I-D&E 10.4 58 (48–66) 6.9
FPG ⬎5.3 mmol/l
Da Qing (13) 259† IGT (randomized 45 6 G-D&E 14.5 38 (14–56) 7.9
groups)
Toranomon Study (31) 458 IGT (men), BMI ⫽ 24 ⬃55 4 I-D&E 2.4 67 (P ⬍ 0.043)‡ 20.6
kg/m2
Indian DPP (17) 269† IGT 46 2.5 I-D&E 23 29 (21–37) 6.4
Medications
DPP (11) 2,155† IGT, BMI ⬎24 kg/m2, 51 2.8 Metformin 10.4 31 (17–43) 13.9
FPG ⬎5.3 mmol/l (1,700
mg)
Indian DPP (17) 269† IGT 46 2.5 Metformin 23 26 (19–35) 6.9
(500 mg)
STOP NIDDM (15) 1,419 IGT, FPG ⬎5.6 54 3.2 Acarbose 12.4 25 (10–37) 9.6
mmol/l (300 mg)
XENDOS (32) 3,277 BMI ⬎30 kg/m2 43 4 Orlistat (360 2.4 37 (14–54) 45.5
mg)
DREAM (16) 5,269 IGT or IFG 55 3.0 Rosiglitazone 9.1 60 (54–65) 6.9
(8 mg)
Voglibose Ph-3 (33) 1,780 IGT 56 3.0 (1-year Rx) Vogliobose 12.0 40 (18–57) 21 (1-year
(0.2 mg) Rx)
ACT-NOW (34) 602 IGT or IFG 52 2.6 Pioglitizone 6.8 81 (61–91) 6.3
(45 mg)
Modified and reprinted with permission (35). Percentage points: *Number needed to treat to prevent 1 case of diabetes, standardized for a 3-year period to improve
comparisons across studies. †Number of participants in the indicated comparisons, not necessarily in entire study. ‡Calculated from information in the article.
ACT-NOW, ACTos Now Study for the Prevention of Diabetes; DPP, Diabetes Prevention Program; DPS, Diabetes Prevention Study; DREAM, Diabetes Reduction
Assessment with Ramipril and Rosiglitazone Medication; STOP NIDDM, Study to Prevent Non-Insulin Dependent Diabetes; XENDOS, Xenical in the prevention of
Diabetes in Obese Subjects. I, individual; G, group; D&E, diet and exercise.
of care. In developing the plan, consider- tiple insulin injections or insulin pump adherence to ongoing use of the device.
ation should be given to the patient’s age, therapy. (A) (C)
school or work schedule and conditions, ● For patients using less frequent insulin ● CGM may be a supplemental tool to
physical activity, eating patterns, social injections, noninsulin therapies, or SMBG in those with hypoglycemia un-
situation and cultural factors, and pres- medical nutrition therapy (MNT) awareness and/or frequent hypoglyce-
ence of complications of diabetes or other alone, SMBG may be useful as a guide to mic episodes. (E)
medical conditions. the success of therapy. (E)
● To achieve postprandial glucose tar- The ADA consensus and position state-
C. Glycemic control gets, postprandial SMBG may be appro- ments on SMBG provide a comprehensive
priate. (E) review of the subject (37,38). Major clin-
● When prescribing SMBG, ensure that ical trials of insulin-treated patients that
1. Assessment of glycemic control
patients receive initial instruction in, demonstrated the benefits of intensive
Two primary techniques are available for
and routine follow-up evaluation of, glycemic control on diabetes complica-
health providers and patients to assess the
SMBG technique and using data to ad- tions have included SMBG as part of
effectiveness of the management plan on
just therapy. (E) multifactorial interventions, suggesting
glycemic control: patient self-monitoring ● Continuous glucose monitoring (CGM) that SMBG is a component of effective
of blood glucose (SMBG) or interstitial
in conjunction with intensive insulin therapy. SMBG allows patients to eval-
glucose and A1C.
regimens can be a useful tool to lower uate their individual response to ther-
A1C in selected adults (age ⱖ25 years) apy and assess whether glycemic targets
a. Glucose monitoring with type 1 diabetes (A). are being achieved. Results of SMBG can
● Although the evidence for A1C lower- be useful in preventing hypoglycemia
Recommendations ing is less strong in children, teens, and and adjusting medications (particularly
● SMBG should be carried out three or younger adults, CGM may be helpful in prandial insulin doses), MNT, and
more times daily for patients using mul- these groups. Success correlates with physical activity.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S17
Standards of Medical Care
Table 8—Components of the comprehensive diabetes evaluation strument and user dependent (43), it is
Medical history important to evaluate each patient’s mon-
● Age and characteristics of onset of diabetes (e.g., DKA, asymptomatic laboratory finding)
itoring technique, both initially and at
● Eating patterns, physical activity habits, nutritional status, and weight history; growth
regular intervals thereafter. In addition,
and development in children and adolescents optimal use of SMBG requires proper in-
● Diabetes education history
terpretation of the data. Patients should
● Review of previous treatment regimens and response to therapy (A1C records)
be taught how to use the data to adjust
Current treatment of diabetes, including medications, meal plan, physical activity patterns, food intake, exercise, or pharmacological
and results of glucose monitoring and patient’s use of data therapy to achieve specific glycemic goals,
● DKA frequency, severity, and cause
and these skills should be reevaluated
● Hypoglycemic episodes
periodically.
● Hypoglycemia awareness
CGM through the measurement of in-
● Any severe hypoglycemia: frequency and cause
terstitial glucose (which correlates well
● History of diabetes-related complications
with PG) is available. These sensors re-
● Microvascular: retinopathy, nephropathy, neuropathy (sensory, including history of
quire calibration with SMBG, and the lat-
foot lesions; autonomic, including sexual dysfunction and gastroparesis) ter are still recommended for making
● Macrovascular: CHD, cerebrovascular disease, PAD
acute treatment decisions. CGM devices
● Other: psychosocial problems*, dental disease*
also have alarms for hypo- and hypergly-
Physical examination cemic excursions. Small studies in se-
● Height, weight, BMI
lected patients with type 1 diabetes have
● Blood pressure determination, including orthostatic measurements when indicated
suggested that CGM use reduces the time
● Fundoscopic examination*
spent in hypo- and hyperglycemic ranges
● Thyroid palpation
and may modestly improve glycemic con-
● Skin examination (for acanthosis nigricans and insulin injection sites)
trol. A larger 26-week randomized trial of
● Comprehensive foot examination:
322 type 1 diabetic patients showed that
● Inspection
adults age 25 years and older using inten-
● Palpation of dorsalis pedis and posterior tibial pulses
sive insulin therapy and CGM experi-
● Presence/absence of patellar and Achilles reflexes
enced a 0.5% reduction in A1C (from
● Determination of proprioception, vibration, and monofilament sensation
⬃7.6 to 7.1%) compared with usual in-
Laboratory evaluation tensive insulin therapy with SMBG (44).
● A1C, if results not available within past 2–3 months
Sensor use in children, teens, and adults
● If not performed/available within past year:
to age 24 years did not result in significant
● Fasting lipid profile, including total, LDL- and HDL cholesterol and triglycerides
A1C lowering, and there was no signifi-
● Liver function tests
cant difference in hypoglycemia in any
● Test for urine albumin excretion with spot urine albumin/creatinine ratio
group. Importantly, the greatest predictor
● Serum creatinine and calculated GFR
of A1C lowering in this study for all age-
● TSH in type 1 diabetes, dyslipidemia, or women over age 50 years
groups was frequency of sensor use,
Referrals which was lower in younger age-groups.
● Annual dilated eye exam
In a smaller randomized controlled trial of
● Family planning for women of reproductive age
129 adults and children with baseline
● Registered dietitian for MNT
A1C ⬍7.0%, outcomes combining A1C
● DSME
and hypoglycemia favored the group us-
● Dental examination
ing CGM, suggesting that CGM is also
● Mental health professional, if needed
beneficial for individuals with type 1 dia-
betes who have already achieved excellent
* See appropriate referrals for these categories.
control with A1C ⬍7.0% (45). Although
CGM is an evolving technology, emerging
The frequency and timing of SMBG clear. A meta-analysis of SMBG in non– data suggest that it may offer benefit in
should be dictated by the particular needs insulin-treated patients with type 2 appropriately selected patients who are
and goals of the patient. SMBG is espe- diabetes concluded that some regimen of motivated to wear it most of the time.
cially important for patients treated with SMBG was associated with a reduction in CGM may be particularly useful in those
insulin in order to monitor for and pre- A1C of 0.4%. However, many of the stud- with hypoglycemia unawareness and/or
vent asymptomatic hypoglycemia and hy- ies in this analysis also included patient frequent episodes of hypoglycemia, and
perglycemia. For most patients with type education with diet and exercise counsel- studies in this area are ongoing.
1 diabetes and pregnant women taking ing and, in some cases, pharmacologic in-
insulin, SMBG is recommended three or tervention, making it difficult to assess the b. A1C
more times daily. For these populations, contribution of SMBG alone to improved
significantly more frequent testing may be control (39). Several recent trials have Recommendations
required to reach A1C targets safely with- called into question the clinical utility ● Perform the A1C test at least two times
out hypoglycemia. The optimal frequency and cost-effectiveness of routine SMBG in a year in patients who are meeting treat-
and timing of SMBG for patients with type non–insulin-treated patients (40 – 42). ment goals (and who have stable glyce-
2 diabetes on noninsulin therapy is un- Because the accuracy of SMBG is in- mic control). (E)
S18 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
● Perform the A1C test quarterly in pa- Table 9—Correlation of A1C with average ant, clinicians should consider the possi-
tients whose therapy has changed or glucose bilities of hemoglobinopathy or altered
who are not meeting glycemic goals. (E) red cell turnover and the options of more
● Use of point-of-care testing for A1C al- frequent and/or different timing of SMBG
Mean plasma glucose
lows for timely decisions on therapy or use of CGM. Other measures of chronic
changes, when needed. (E) A1C (%) mg/dl mmol/l glycemia such as fructosamine are avail-
6 126 7.0 able, but their linkage to average glucose
Because A1C is thought to reflect average 7 154 8.6 and their prognostic significance are not
glycemia over several months (43) and 8 183 10.2 as clear as is the case for A1C.
has strong predictive value for diabetes 9 212 11.8
complications (11,46), A1C testing 10 240 13.4 2. Glycemic goals in adults
should be performed routinely in all pa- ● Lowering A1C to below or around 7%
11 269 14.9
tients with diabetes, at initial assessment 12 298 16.5 has been shown to reduce microvascu-
and then as part of continuing care. Mea- These estimates are based on ADAG data of ⬃2,700
lar and neuropathic complications of
surement approximately every 3 months glucose measurements over 3 months per A1C mea- type 1 and type 2 diabetes. Therefore,
determines whether a patient’s glycemic surement in 507 adults with type 1, type 2, and no for microvascular disease prevention,
targets have been reached and main- diabetes. The correlation between A1C and average the A1C goal for nonpregnant adults in
tained. For any individual patient, the fre- glucose was 0.92 (49). A calculator for converting general is ⬍7%. (A)
A1C results into estimated average glucose (eAG),
quency of A1C testing should be ● In type 1 and type 2 diabetes, random-
in either mg/dl or mmol/l, is available at
dependent on the clinical situation, the http://professional.diabetes.org/eAG. ized controlled trials of intensive versus
treatment regimen used, and the judg- standard glycemic control have not
ment of the clinician. Some patients with shown a significant reduction in CVD
stable glycemia well within target may do porting both an A1C result and an esti- outcomes during the randomized por-
well with testing only twice per year, mated average glucose (eAG) result when tion of the trials. Long-term follow-up
while unstable or highly intensively man- a clinician orders the A1C test. In previ- of the DCCT and UK Prospective Dia-
aged patients (e.g., pregnant type 1 dia- ous versions of the Standards of Medical betes Study (UKPDS) cohorts suggests
betic women) may be tested more Care in Diabetes, the table describing the that treatment to A1C targets below or
frequently than every 3 months. The correlation between A1C and mean glu- around 7% in the years soon after the
availability of the A1C result at the time cose was derived from relatively sparse diagnosis of diabetes is associated with
that the patient is seen (point-of-care test- data (one seven-point profile over 1 day long-term reduction in risk of macro-
ing) has been reported to result in in- per A1C reading) in the primarily Cauca- vascular disease. Until more evidence
creased intensification of therapy and sian type 1 participants in the DCCT (50). becomes available, the general goal of
improvement in glycemic control Clinicians should note that the numbers ⬍7% appears reasonable for many
(47,48). in the table are now different, as they are adults for macrovascular risk reduc-
The A1C test is subject to certain lim- based on ⬃2,800 readings per A1C in the tion. (B)
itations. Conditions that affect erythro- ADAG trial. ● Subgroup analyses of clinical trials such
cyte turnover (hemolysis, blood loss) and In the ADAG trial, there were no sig- as the DCCT and UKPDS, and evidence
hemoglobin variants must be considered, nificant differences among racial and eth- for reduced proteinuria in the Action in
particularly when the A1C result does not nic groups in the regression lines between Diabetes and Vascular Disease: Preterax
correlate with the patient’s clinical situa- A1C and mean glucose, although there and Diamicron Modified Release Con-
tion (43). In addition, A1C does not pro- was a trend toward a difference between trolled Evaluation (ADVANCE) trial
vide a measure of glycemic variability or Africans/African Americans participants suggest a small but incremental benefit
hypoglycemia. For patients prone to gly- and Caucasians that might have been sig- in microvascular outcomes with A1C
cemic variability (especially type 1 dia- nificant had more Africans/African Amer- values closer to normal. Therefore, for
betic patients, or type 2 diabetic patients icans been studied. A recent study selected individual patients, providers
with severe insulin deficiency), glycemic comparing A1C to CGM data in 48 type 1 might reasonably suggest even lower
control is best judged by the combination diabetic children found a highly statisti- A1C goals than the general goal of
of results of SMBG testing and the A1C. cally significant correlation between A1C ⬍7%, if this can be achieved without
The A1C may also serve as a check on the and mean blood glucose, although the significant hypoglycemia or other ad-
accuracy of the patient’s meter (or the pa- correlation (r ⫽ 0.7) was significantly verse effects of treatment. Such patients
tient’s reported SMBG results) and the ad- lower than in the ADAG trial (51). might include those with short dura-
equacy of the SMBG testing schedule. Whether there are significant differences tion of diabetes, long life expectancy,
Table 9 contains the correlation be- in how A1C relates to average glucose in and no significant CVD. (B)
tween A1C levels and mean PG levels children or in African American patients ● Conversely, less-stringent A1C goals
based on data from the international A1C- is an area for further study. For the time than the general goal of ⬍7% may be
Derived Average Glucose (ADAG) trial being, the question has not led to different appropriate for patients with a history
using frequent SMBG and CGM in 507 recommendations about testing A1C or of severe hypoglycemia, limited life ex-
adults (83% Caucasian) with type 1, type different interpretations of the clinical pectancy, advanced microvascular or
2, and no diabetes (49). ADA and the meaning of given levels of A1C in those macrovascular complications, and ex-
American Association of Clinical Chem- populations. tensive comorbid conditions and those
ists have determined that the correlation For patients in whom A1C/eAG and with longstanding diabetes in whom
(r ⫽ 0.92) is strong enough to justify re- measured blood glucose appear discrep- the general goal is difficult to attain de-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S19
Standards of Medical Care
spite diabetes self-management educa- analyses also suggest that further lowering such as stroke. In an epidemiologic anal-
tion, appropriate glucose monitoring, of A1C from 7 to 6% is associated with ysis of the study cohort, a continuous as-
and effective doses of multiple glucose- further reduction in the risk of microvas- sociation was observed such that for every
lowering agents including insulin. (C) cular complications, albeit the absolute percentage point lower median on-study
risk reductions become much smaller. A1C (e.g., 8 –7%), there was a statistically
Glycemic control is fundamental to the The ADVANCE study of intensive versus significant 18% reduction in CVD events,
management of diabetes. The DCCT, a standard glycemic control in type 2 dia- again with no glycemic threshold. A re-
prospective, randomized, controlled trial betes found a statistically significant re- cent report of 10 years of follow-up of the
of intensive versus standard glycemic duction in albuminuria with an A1C UKPDS cohort described, for the partici-
control in patients with relatively recently target of ⬍6.5% (achieved median A1C pants originally randomized to intensive
diagnosed type 1 diabetes, showed defin- 6.3%) compared with standard therapy glycemic control compared with those
itively that improved glycemic control is achieving a median A1C of 7.0% (63). randomized to conventional glycemic
associated with significantly decreased Given the substantially increased risk of control, long-term reductions in MI (15%
rates of microvascular (retinopathy and hypoglycemia (particularly in those with with sulfonylurea or insulin as initial
nephropathy) as well as neuropathic type 1 diabetes, but also in the recent type pharmacotherapy, 33% with metformin
complications (53). Follow-up of the 2 diabetes trials described below), the as initial pharmacotherapy, both statisti-
DCCT cohorts in the Epidemiology of Di- concerning mortality findings in the Ac- cally significant) and in all-cause mortal-
abetes Interventions and Complications tion to Control Cardiovascular Risk in Di- ity (13 and 27%, respectively, both
(EDIC) study has shown persistence of abetes (ACCORD) trial described below statistically significant) (59).
this effect in previously intensively and the relatively much greater effort re- Because of ongoing uncertainty re-
treated subjects, even though their glyce- quired to achieve near-normoglycemia, garding whether intensive glycemic con-
mic control has been equivalent to that of the risks of lower targets may outweigh trol can reduce the increased risk of CVD
previous standard arm subjects during the potential benefits on microvascular events in people with type 2 diabetes, sev-
follow-up (54,55). complications on a population level. eral large long-term trials were launched
In type 2 diabetes, the Kumamoto However, selected individual patients, es- in the past decade to compare the effects
study (56) and the UKPDS (57,58) dem- pecially those with little comorbidity and of intensive versus standard glycemic
onstrated significant reductions in micro- long life expectancy (who may reap the control on CVD outcomes in relatively
vascular and neuropathic complications benefits of further lowering glycemia be- high-risk participants with established
with intensive therapy. Similar to the low 7%) may, at patient and provider type 2 diabetes. In 2008, results of three
DCCT-EDIC findings, long-term fol- judgment, adopt glycemic targets as close large trials (ACCORD, ADVANCE, and
low-up of the UKPDS cohort has recently to normal as possible as long as significant VADT) suggested no significant reduction
demonstrated a “legacy effect” of early in- hypoglycemia does not become a barrier. in CVD outcomes with intensive glycemic
tensive glycemic control on long-term Whereas many epidemiologic studies control in these populations. Details of
rates of microvascular complications, and meta-analyses (64,65) have clearly these three studies are shown in Table 10,
even with loss of glycemic separation be- shown a direct relationship between A1C and their results and implications are re-
tween the intensive and standard cohorts and CVD, the potential of intensive glyce- viewed more extensively in a recent ADA
after the end of the randomized con- mic control to reduce CVD has been less position statement (52).
trolled trial (59). The more recent Veter- clearly defined. In the DCCT, there was a The ACCORD study randomized
ans Affairs Diabetes Trial (VADT) in type trend toward lower risk of CVD events 10,251 participants with either history of
2 diabetes also showed significant reduc- with intensive control (risk reduction a CVD event or significant CVD risk to a
tions in albuminuria with intensive 41%, 95% CI 10 – 68%), but the number strategy of intensive glycemic control (tar-
(achieved median A1C 6.9%) compared of events was small. However, 9-year get A1C ⬍6.0%) or standard glycemic
with standard glycemic control but no post-DCCT follow-up of the cohort has control (A1C target 7.0 –7.9%). Investiga-
difference in retinopathy and neuropathy shown that participants previously ran- tors used multiple glycemic medications
(60,61). domized to the intensive arm had a 42% in both arms. From a baseline median
In each of these large randomized reduction (P ⫽ 0.02) in CVD outcomes A1C of 8.1%, the intensive arm reached a
prospective clinical trials, treatment regi- and a 57% reduction (P ⫽ 0.02) in the median A1C of 6.4% within 12 months of
mens that reduced average A1C to 7% risk of nonfatal myocardial infarction randomization, while the standard group
(1% above the upper limits of normal) (MI), stroke, or CVD death compared reached a median A1C of 7.5%. Other
were associated with fewer markers of with participants previously in the stan- risk factors were treated aggressively and
long-term microvascular complications; dard arm (66). The benefit of intensive equally in both groups. The intensive gly-
however, intensive control was found to glycemic control in this type 1 diabetic cemic control group had more use of in-
increase the risk of severe hypoglycemia cohort has recently been shown to persist sulin in combination with multiple oral
and led to weight gain (46,60,62). for up to 30 years (67). agents, significantly more weight gain,
Epidemiological analyses of the The UKPDS trial of type 2 diabetes and more episodes of severe hypoglyce-
DCCT and UKPDS (46,53) demonstrate a observed a 16% reduction in cardiovascu- mia than the standard group.
curvilinear relationship between A1C and lar complications (combined fatal or non- In early 2008, the glycemic control
microvascular complications. Such anal- fatal MI and sudden death) in the arm of ACCORD was halted on the rec-
yses suggest that, on a population level, intensive glycemic control arm, although ommendation of the study’s data safety
the greatest number of complications will this difference was not statistically signif- monitoring board due to the finding of an
be averted by taking patients from very icant (P ⫽ 0.052), and there was no sug- increased rate of mortality in the intensive
poor control to fair or good control. These gestion of benefit on other CVD outcomes arm compared with the standard arm
S20 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 10—Comparison of the three trials of intensive glycemic control and CVD outcomes
ACCORD ADVANCE VADT
Participant characteristics
n 10,251 11,140 1,791
Mean age (years) 62 66 60
Duration of diabetes (years) 10 8 11.5
History of CVD (%) 35 32 40
Median baseline A1C (%) 8.1 7.2 9.4
On insulin at baseline (%) 35 1.5 52
Protocol characteristics
A1C goals (%) (I vs. S)* ⬍6.0 vs. 7.0–7.9 ⱕ6.5 vs. “based on local guidelines” ⬍6.0 (action if ⬎6.5) vs.
planned separation of 1.5
Protocol for glycemic control
(I vs. S)* Multiple drugs in both Multiple drugs added to gliclizide vs. Multiple drugs in both arms
arms multiple drugs with no gliclizide
Management of other risk
factors Embedded blood pressure Embedded blood pressure trial Protocol for intensive
and lipid trials treatment in both arms
On-study characteristics
Achieved median A1C (%)
(I vs. S) 6.4 vs. 7.5 6.3 vs. 7.0 6.9 vs. 8.5
On insulin at study end (%)
(I vs. S)* 77 vs. 55* 40 vs. 24 89 vs. 0.74
Weight changes (kg)
Intensive glycemic control arm ⫹3.5 ⫺0.1 ⫹7.8
Standard glycemic control arm ⫹0.4 ⫺1.0 ⫹3.4
Severe hypoglycemia
(participants with one or more
episodes during study) (%)
Intensive glycemic control arm 16.2 2.7 21.2
Standard glycemic control arm 5.1 1.5 9.9
Outcomes
Definition of primary outcome Nonfatal MI, nonfatal Microvascular plus macrovascular Nonfatal MI, nonfatal stroke,
stroke, CVD death (nonfatal MI, nonfatal stroke, CVD CVD death,
death) outcomes hospitalization for heart
failure, revascularization
HR for primary outcome
(95% CI) 0.90 (0.78–1.04) 0.9 (0.82–0.98); 0.88 (0.74–1.05)
macrovascular 0.94 (0.84–1.06)
HR for mortality findings
(95% CI) 1.22 (1.01–1.46) 0.93 (0.83–1.06) 1.07 (0.81–1.42)
*Insulin rates for ACCORD are for any use during the study. I, intensive glycemic control; S, standard glycemic control. Abridged from ref. 52.
(1.41 vs. 1.14%/year, hazard ratio 1.22, The cause of excess deaths in the in- achieved A1C levels ⬍7% or in those who
95% CI 1.01–1.46), with a similar in- tensive group of the ACCORD has been lowered their A1C quickly after trial en-
crease in cardiovascular deaths. The pri- difficult to pinpoint (and is discussed in rollment. In fact, the converse was ob-
mary outcome of ACCORD (MI, stroke, some detail in a 2009 ADA position state- served: those at highest risk for mortality
or cardiovascular death) was lower in the ment [52]). However, exploratory analy- were participants in the intensive arm
intensive glycemic control group due to a ses of the mortality findings of ACCORD with the highest A1C levels.
reduction in nonfatal MI, although this (evaluating variables including weight The ADVANCE study randomized
finding was not statistically significant gain, use of any specific drug or drug participants to a strategy of intensive gly-
when the study was terminated (68). Of combination, and hypoglycemia) were re- cemic control (with primary therapy be-
note, prespecified subset analyses showed portedly unable to identify a clear expla- ing the sulfonylurea gliclizide and
that participants with no previous CVD nation for the excess mortality in the additional medications as needed to
event and those who had a baseline A1C intensive arm. At the 69th Scientific Ses- achieve a target A1C of ⱕ6.5%) or to stan-
⬍8% had a statistically significant reduc- sions of the American Diabetes Associa- dard therapy (in which any medication
tion in the primary CVD outcome, al- tion, the ACCORD investigators but gliclizide could be used and the gly-
though overall mortality was not reduced presented additional analyses showing no cemic target was according to “local
in these groups. increase in mortality in participants who guidelines”). ADVANCE participants
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S21
Standards of Medical Care
were slightly older than those in AC- exploratory analyses suggested that se- A prespecified subgroup analysis sug-
CORD and VADT and had similar high vere hypoglycemia within the past 90 gested that major CVD outcome reduc-
CVD risk. However, they had an average days was a strong predictor of the primary tion occurred in patients without known
duration of diabetes that was 2 years outcome and of CVD mortality (69). CVD at baseline (HR 0.84 [95% CI 0.74 –
shorter, lower baseline A1C (median All three of these trials were carried 0.94]) (71). Conversely, the mortality
7.2%), and almost no use of insulin at out in participants with established diabe- findings in ACCORD and subgroup anal-
enrollment. The median A1C levels tes (mean duration 8 –11 years) and either yses of VADT suggest that the potential
achieved in the intensive and standard known CVD or multiple risk factors sug- risks of very intensive glycemic control
arms were 6.3 and 7.0%, respectively, gesting the presence of established ath- may outweigh its benefits in some pa-
and maximal separation between the erosclerosis. Subset analyses of the three tients, such as those with very long dura-
arms took several years to achieve. Use of trials suggested a significant benefit of in- tion of diabetes, known history of severe
other drugs that favorably impact CVD tensive glycemic control on CVD in par- hypoglycemia, advanced atherosclerosis,
risk (aspirin, statins, and angiotensin en- ticipants with shorter duration of and advanced age/frailty. Certainly, pro-
zyme inhibitors) was lower in ADVANCE diabetes, lower A1C at entry, and/or ab- viders should be vigilant in preventing se-
than in ACCORD or VADT. sence of known CVD. The DCCT-EDIC vere hypoglycemia in patients with
The primary outcome of ADVANCE study and the long-term follow-up of the advanced disease and should not aggres-
was a combination of microvascular UKPDS cohort both suggest that intensive sively attempt to achieve near-normal
events (nephropathy and retinopathy) glycemic control initiated soon after diag- A1C levels in patients in whom such a
and major adverse cardiovascular events nosis of diabetes in patients with a lower target cannot be reasonably easily and
(MI, stroke, and cardiovascular death). level of CVD risk may impart long-term safely achieved.
Intensive glycemic control significantly protection from CVD events. As is the Recommended glycemic goals for
reduced the primary end point, although case with microvascular complications, it nonpregnant adults are shown in Table
this was due to a significant reduction in may be that glycemic control plays a 11. The recommendations are based on
the microvascular outcome, primarily de- greater role before macrovascular disease those for A1C values, with listed blood
velopment of macroalbuminuria, with no is well developed and minimal or no role glucose levels that appear to correlate
significant reduction in the macrovascu- when it is advanced. Consistent with this with achievement of an A1C of ⬍7%. The
lar outcome. There was no difference in concept, data from an ancillary study of issue of pre- versus postprandial SMBG
overall or cardiovascular mortality be- VADT demonstrated that intensive glyce- targets is complex (72). Elevated post-
tween the intensive compared with the mic control was quite effective in reduc- challenge (2-h OGTT) glucose values
standard glycemic control arms (63). ing CVD events in individuals with less have been associated with increased car-
VADT randomized participants with atherosclerosis at baseline (assessed by diovascular risk independent of FPG in
type 2 diabetes uncontrolled on insulin or coronary calcium) but not in people with some epidemiological studies. In diabetic
maximal dose oral agents (median entry more extensive baseline atherosclerosis subjects, some surrogate measures of vas-
A1C 9.4%) to a strategy of intensive gly- (70). cular pathology, such as endothelial dys-
cemic control (goal A1C ⬍6.0%) or stan- The benefits of intensive glycemic function, are negatively affected by
dard glycemic control, with a planned control on microvascular and neuro- postprandial hyperglycemia (73). It is
A1C separation of at least 1.5%. Medica- pathic complications are well established clear that postprandial hyperglycemia,
tion treatment algorithms were used to for both type 1 and type 2 diabetes. AD- like preprandial hyperglycemia, contrib-
achieve the specified glycemic goals, with VANCE and VADT have added to that ev- utes to elevated A1C levels, with its rela-
a goal of using similar medications in both idence base by demonstrating a tive contribution being higher at A1C
groups. Median A1C levels of 6.9 and significant reduction in the risk of new or levels that are closer to 7%. However, out-
8.4% were achieved in the intensive and worsening albuminuria with intensive come studies have clearly shown A1C to
standard arms, respectively, within the glycemic control. The lack of significant be the primary predictor of complica-
1st year of the study. Other CVD risk fac- reduction in CVD events with intensive tions, and landmark glycemic control tri-
tors were treated aggressively and equally glycemic control in ACCORD, AD- als such as the DCCT and UKPDS relied
in both groups. VANCE, and VADT should not lead clini- overwhelmingly on preprandial SMBG.
The primary outcome of VADT was a cians to abandon the general target of an Additionally, a randomized controlled
composite of CVD events. The cumulative A1C ⬍7.0% and thereby discount the trial in patients with known CVD found
primary outcome was nonsignificantly benefit of good control on serious and de- no CVD benefit of insulin regimens tar-
lower in the intensive arm. There were bilitating microvascular complications. geting postprandial glucose compared
more CVD deaths in the intensive arm The evidence for a cardiovascular with those targeting preprandial glucose
than in the standard arm, but the differ- benefit of intensive glycemic control pri- (74). For individuals who have premeal
ence was not statistically significant (60). marily rests on long-term follow-up of glucose values within target but A1C val-
Post hoc subgroup analyses suggested study cohorts treated early in the course ues above target, a reasonable recommen-
that duration of diabetes interacted with of type 1 and type 2 diabetes as well as dation for postprandial testing and targets
randomization such that participants subset analyses of ACCORD, ADVANCE, is monitoring postprandial plasma glu-
with duration of diabetes less than about and VADT. A recent group-level meta- cose (PPG) 1–2 h after the start of the meal
12 years appeared to have a CVD benefit analysis of the three trials suggests that and treatment aimed at reducing PPG val-
of intensive glycemic control while those glucose lowering has a modest (9%) but ues to ⬍180 mg/dl to help lower A1C.
with longer duration of disease prior to statistically significant reduction in major As noted above, less stringent treat-
study entry had a neutral or even adverse CVD outcomes, primarily nonfatal MI, ment goals may be appropriate for adults
effect of intensive glycemic control. Other with no significant increase in mortality. with limited life expectancies or advanced
S22 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 11 —Summary of glycemic recommendations for non-pregnant adults with diabetes b. Therapy for type 2 diabetes. The ADA
A1C ⬍7.0%*
and the European Association for the
Preprandial capillary plasma glucose 70–130 mg/dl (3.9–7.2 mmol/l)
Study of Diabetes (EASD) published a
Peak postprandial capillary plasma glucose† ⬍180 mg/dl (⬍10.0 mmol/l)
consensus statement on the approach to
Key concepts in setting glycemic goals:
management of hyperglycemia in individ-
● A1C is the primary target for glycemic control
uals with type 2 diabetes (80) and a sub-
● Goals should be individualized based on:
sequent update (81). Highlights of this
● duration of diabetes
approach include: intervention at the
● age/life expectancy
time of diagnosis with metformin in com-
● comorbid conditions
bination with lifestyle changes (MNT and
● known CVD or advanced microvascular
exercise) and continuing timely augmen-
complications
tation of therapy with additional agents
● hypoglycemia unawareness
(including early initiation of insulin ther-
● individual patient considerations
apy) as a means of achieving and main-
● More or less stringent glycemic goals may be
taining recommended levels of glycemic
appropriate for individual patients
control (i.e., A1C ⬍7% for most patients).
Postprandial glucose may be targeted if A1C goals are not
The overall objective is to achieve and
met despite reaching preprandial glucose goals
maintain glycemic control and to change
interventions when therapeutic goals are
*Referenced to a nondiabetic range of 4.0 – 6.0% using a DCCT-based assay. †Postprandial glucose mea-
surements should be made 1–2 h after the beginning of the meal, generally peak levels in patients with
not being met.
diabetes. The algorithm took into account the
evidence for A1C lowering of the individ-
ual interventions, their additive effects,
vascular disease. Glycemic goals for chil- ous insulin infusion [CSII] or insulin
and their expense. The precise drugs used
dren are provided in VII.A.1.a. Glycemic pump therapy) was a key part of im-
and their exact sequence may not be as
control. Severe or frequent hypoglycemia proved glycemia and better outcomes
important as achieving and maintaining
is an absolute indication for the modifica- (53,66). At the time of the study, therapy
glycemic targets safely. Medications not
tion of treatment regimens, including set- was carried out with short- and interme-
included in the consensus algorithm, ow-
ting higher glycemic goals. diate-acting human insulins. Despite bet-
ing to less glucose-lowering effectiveness,
Regarding goals for glycemic control ter microvascular outcomes, intensive
limited clinical data, and/or relative ex-
for women with GDM, recommendations insulin therapy was associated with a high pense, still may be appropriate choices for
from the Fifth International Workshop- rate in severe hypoglycemia (62 episodes individual patients to achieve glycemic
Conference on Gestational Diabetes (75) per 100 patient-years of therapy). Since goals. Initiation of insulin at the time of
are to target maternal capillary glucose the time of the DCCT, a number of rapid- diagnosis is recommended for individuals
concentrations of: acting and long-acting insulin analogs presenting with weight loss or other se-
have been developed. These analogs are vere hyperglycemic symptoms or signs.
● Preprandial ⱕ95 mg/dl (5.3 mmol/l) associated with less hypoglycemia with
and either equal A1C lowering in type 1 diabetes
● 1-h postmeal ⱕ140 mg/dl (7.8 (77,78). D. Medical nutrition therapy
mmol/l) Recommended therapy for type 1 di- General recommendations
or abetes therefore consists of the following ● Individuals who have pre-diabetes or
● 2-h postmeal ⱕ120 mg/dl (6.7
components: 1) use of multiple dose in- diabetes should receive individualized
mmol/l) sulin injections (3– 4 injections per day of MNT as needed to achieve treatment
basal and prandial insulin) or CSII ther- goals, preferably provided by a regis-
For women with preexisting type 1 or apy; 2) matching of prandial insulin to tered dietitian familiar with the compo-
type 2 diabetes who become pregnant, a carbohydrate intake, premeal blood glu- nents of diabetes MNT. (A)
recent consensus statement (76) recom- cose, and anticipated activity; and 3) for ● Because it can result in cost savings and
mends the following as optimal glycemic many patients (especially if hypoglycemia improved outcomes (B), MNT should
goals, if they can be achieved without ex- is a problem), use of insulin analogs. be covered by insurance and other pay-
cessive hypoglycemia: There are excellent reviews available that ors (E).
guide the initiation and management of
● premeal, bedtime, and overnight glu- insulin therapy to achieve desired glyce- Energy balance, overweight, and
cose 60 –99 mg/dl (3.3–5.4 mmol/l) mic goals (3,77,79).
● peak postprandial glucose 100 –129 obesity
Because of the increased frequency of ● In overweight and obese insulin-
mg/dl (5.4 –7.1 mmol/l) other autoimmune diseases in type 1 dia-
● A1C ⬍6.0% resistant individuals, modest weight
betes, screening for thyroid dysfunction, loss has been shown to reduce insulin
vitamin B12 deficiency, or celiac disease resistance. Thus, weight loss is recom-
3. Approach to treatment
should be considered based on signs and mended for all overweight or obese in-
a. Therapy for type 1 diabetes. The symptoms. Periodic screening in the ab- dividuals who have or are at risk for
DCCT clearly showed that intensive insu- sence of symptoms has been recom- diabetes. (A)
lin therapy (three or more injections per mended, but the effectiveness and ● For weight loss, either low-carbohy-
day of insulin or continuous subcutane- optimal frequency are unclear. drate or low-fat calorie-restricted diets
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S23
Standards of Medical Care
may be effective in the short-term (up ● If adults with diabetes choose to use Because of the effects of obesity on
to 1 year). (A) alcohol, daily intake should be limited insulin resistance, weight loss is an im-
● For patients on low-carbohydrate diets, to a moderate amount (one drink per portant therapeutic objective for over-
monitor lipid profiles, renal function, day or less for adult women and two weight or obese individuals with pre-
and protein intake (in those with ne- drinks per day or less for adult men). diabetes or diabetes (94). Short-term
phropathy) and adjust hypoglycemic (E) studies have demonstrated that moderate
therapy as needed. (E) ● Routine supplementation with antioxi- weight loss (5% of body weight) in sub-
● Physical activity and behavior modifi- dants, such as vitamins E and C and jects with type 2 diabetes is associated
cation are important components of carotene, is not advised because of lack with decreased insulin resistance, im-
weight loss programs and are most of evidence of efficacy and concern re- proved measures of glycemia and lipemia,
helpful in maintenance of weight loss. lated to long-term safety. (A) and reduced blood pressure (95); longer-
(B) ● Benefit from chromium supplementa- term studies (ⱖ52 weeks) showed mixed
tion in people with diabetes or obesity effects on A1C in adults with type 2 dia-
Primary prevention of diabetes has not been conclusively demon- betes (96 –99), and results were con-
● Among individuals at high risk for de- strated and therefore cannot be recom- founded by pharmacologic weight loss
veloping type 2 diabetes, structured mended. (C) therapy. A systematic review of 80 weight
programs emphasizing lifestyle ● Individualized meal planning should loss studies of ⱖ1 year duration demon-
changes that include moderate weight include optimization of food choices to strated that moderate weight loss
loss (7% body weight) and regular meet recommended dietary allowances achieved through diet alone, diet and ex-
physical activity (150 min/week) with (RDAs)/dietary reference intakes ercise, and meal replacements can be
dietary strategies including reduced (DRIs) for all micronutrients. (E) achieved and maintained over the long
calories and reduced intake of dietary term (4.8 – 8% weight loss at 12 months
fat can reduce the risk for developing MNT is an integral component of diabetes [100]). The multifactorial intensive life-
diabetes and are therefore recom- prevention, management, and self- style intervention used in the DPP, which
mended. (A) management education. In addition to its included reduced intake of fat and calo-
● Individuals at high risk for type 2 dia- role in preventing and controlling diabe- ries, led to weight loss averaging 7% at 6
betes should be encouraged to achieve tes, ADA recognizes the importance of months and maintenance of 5% weight
the U.S. Department of Agriculture nutrition as an essential component of an loss at 3 years, associated with a 58% re-
(USDA) recommendation for dietary fi- overall healthy lifestyle. A full review of duction in incidence of type 2 diabetes
ber (14 g fiber/1,000 kcal) and foods the evidence regarding nutrition in pre- (11). Look AHEAD (Action for Health in
containing whole grains (one-half of venting and controlling diabetes and its Diabetes) is a large clinical trial designed
grain intake). (B) complications and additional nutrition- to determine whether long-term weight
related recommendations can be found in loss will improve glycemia and prevent
Dietary fat intake in diabetes the ADA position statement, Nutrition cardiovascular events in subjects with
management Recommendations and Interventions for type 2 diabetes. One-year results of the
● Saturated fat intake should be ⬍7% of Diabetes, published in 2006 and updated intensive lifestyle intervention in this trial
total calories. (A) for 2008 (82). Achieving nutrition- show an average of 8.6% weight loss, sig-
● Reducing intake of trans fat lowers LDL related goals requires a coordinated team nificant reduction of A1C, and reduction
cholesterol and increases HDL choles- effort that includes the active involvement in several CVD risk factors (101). When
terol (A); therefore intake of trans fat of the person with pre-diabetes or diabe- completed, the Look AHEAD study
should be minimized (E). tes. Because of the complexity of nutrition should provide insight into the effects of
issues, it is recommended that a registered long-term weight loss on important clin-
Carbohydrate intake in diabetes dietitian who is knowledgeable and ical outcomes.
management skilled in implementing nutrition therapy The optimal macronutrient distribu-
● Monitoring carbohydrate intake, into diabetes management and education tion of weight loss diets has not been es-
whether by carbohydrate counting, ex- be the team member who provides MNT. tablished. Although low-fat diets have
changes, or experience-based estima- Clinical trials/outcome studies of traditionally been promoted for weight
tion, remains a key strategy in achieving MNT have reported decreases in A1C at loss, several randomized controlled trials
glycemic control. (A) 3– 6 months ranging from 0.25 to 2.9% found that subjects on low-carbohydrate
● For individuals with diabetes, use of the with higher reductions seen in type 2 di- diets (⬍130 g/day of carbohydrate) lost
glycemic index and glycemic load may abetes of shorter duration. Multiple stud- more weight at 6 months than subjects on
provide a modest additional benefit for ies have demonstrated sustained low-fat diets (102,103); however, at 1
glycemic control over that observed improvements in A1C at 12 months and year, the difference in weight loss be-
when total carbohydrate is considered longer when a registered dietitian pro- tween the low-carbohydrate and low-fat
alone. (B) vided follow-up visits ranging from diets was not significant and weight loss
monthly to three sessions per year (83– was modest with both diets. Another
Other nutrition recommendations 90). Meta-analyses of studies in nondia- study of overweight women randomized
●Sugar alcohols and nonnutritive sweet- betic, free-living subjects report that MNT to one of four diets showed significantly
eners are safe when consumed within reduces LDL cholesterol by 15–25 mg/dl more weight loss at 12 months with the
the acceptable daily intake levels estab- (91) or by up to 16% (92), while clinical Atkins low-carbohydrate diet than with
lished by the Food and Drug Adminis- trials support a role for lifestyle modifica- higher-carbohydrate diets (104).
tration (FDA). (A) tion in treating hypertension (92,93). Changes in serum triglyceride and HDL
S24 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
cholesterol were more favorable with the acids on people with diabetes; therefore, passing or transposing sections of the
low-carbohydrate diets. In one study, the recommended goals are consistent small intestine, when part of a compre-
those subjects with type 2 diabetes dem- with those for individuals with CVD hensive team approach, can be an effec-
onstrated a greater decrease in A1C with a (92,109). tive weight loss treatment for severe
low-carbohydrate diet than with a low-fat The FDA has approved five nonnutri- obesity, and national guidelines support
diet (103). A recent meta-analysis showed tive sweeteners for use in the U.S.: acesul- its consideration for people with type 2
that at 6 months, low-carbohydrate diets fame potassium, aspartame, neotame, diabetes who have BMI ⬎35 kg/m2. Bari-
were associated with greater improve- saccharin, and sucralose. Before being al- atric surgery has been shown to lead to
ments in triglyceride and HDL cholesterol lowed on the market, all underwent rig- near or complete normalization of glyce-
concentrations than low-fat diets; how- orous scrutiny and were shown to be safe mia in ⬃55–95% of patients with type 2
ever, LDL cholesterol was significantly when consumed by the public, including diabetes, depending on the surgical pro-
higher with the low-carbohydrate diets people with diabetes and women during cedure. A meta-analysis of studies of bari-
(105). In a 2-year dietary intervention pregnancy. Reduced calorie sweeteners atric surgery reported that 78% of
study, Mediterranean and low-carbohy- approved by the FDA include sugar alco- individuals with type 2 diabetes had com-
drate diets were found to be effective and hols (polyols) such as erythritol, isomalt, plete “resolution” of diabetes (normaliza-
safe alternatives to a low-fat diet for lactitol, maltitol, mannitol, sorbitol, xyli- tion of blood glucose levels in the absence
weight reduction in moderately obese tol, tagatose, and hydrogenated starch hy- of medications) and that the resolution
participants (99). drolysates. The use of sugar alcohols rates were sustained in studies that had
The RDA for digestible carbohydrate appears to be safe; however, they may follow-up exceeding 2 years (110). Reso-
is 130 g/day and is based on providing cause diarrhea, especially in children. Ste- lution rates are lower with procedures
adequate glucose as the required fuel for via (Rebaudioside A) has been designated that only constrict the stomach and
the central nervous system without reli- by the FDA as being generally recognized higher with those that bypass portions of
ance on glucose production from ingested as safe (GRAS). the small intestine. Additionally, there is a
protein or fat. Although brain fuel needs suggestion that intestinal bypass proce-
can be met on lower-carbohydrate diets, Reimbursement for MNT dures may have glycemic effects that are
long-term metabolic effects of very-low- MNT, when delivered by a registered dieti- independent of their effects on weight.
carbohydrate diets are unclear, and such tian according to nutrition practice guide- A recent randomized controlled trial
diets eliminate many foods that are im- lines, is reimbursed as part of the Medicare compared adjustable gastric banding to
portant sources of energy, fiber, vitamins, program as overseen by the Centers for the “best available” medical and lifestyle
and minerals that are important in dietary Medicare and Medicaid Services (www. therapy in subjects with type 2 diabetes
palatability (106). cms.hhs.gov/ medicalnutritiontherapy). diagnosed ⬍2 years before randomiza-
Although numerous studies have at- tion and with BMI 30 – 40 kg/m2 (111). In
tempted to identify the optimal mix of E. Bariatric surgery this trial, 73% of surgically treated pa-
macronutrients for meal plans of people tients achieved “remission” of their diabe-
with diabetes, it is unlikely that one such Recommendations tes, compared with 13% of those treated
combination of macronutrients exists. ● Bariatric surgery should be considered medically. The latter group lost only 1.7%
The best mix of carbohydrate, protein, for adults with BMI ⬎35 kg/m2 and of body weight, suggesting that their ther-
and fat appears to vary depending on type 2 diabetes, especially if the diabe- apy was not optimal. Overall the trial had
individual circumstances. For those tes or associated comorbidities are dif- 60 subjects, and only 13 had a BMI ⬍35
individuals seeking guidance as to macro- ficult to control with lifestyle and kg/m2, making it difficult to generalize
nutrient distribution in healthy adults, pharmacologic therapy. (B) these results to diabetic patients who are
DRIs may be helpful (106). It must be ● Patients with type 2 diabetes who have less severely obese or with longer dura-
clearly recognized that regardless of the undergone bariatric surgery need life- tion of diabetes.
macronutrient mix, the total caloric in- long lifestyle support and medical moni- Bariatric surgery is costly in the short
take must be appropriate to the weight toring. (E) term and has some risks. Rates of morbidity
management goal. Further, individualiza- ● Although small trials have shown glyce- and mortality directly related to the surgery
tion of the macronutrient composition mic benefit of bariatric surgery in patients have been reduced considerably in recent
will depend on the metabolic status of the with type 2 diabetes and BMI of 30 –35 years, with 30-day mortality rates now
patient (e.g., lipid profile and renal func- kg/m2, there is currently insufficient evi- 0.28%, similar to those of laparoscopic cho-
tion) and/or food preferences. Plant- dence to generally recommend surgery in lecystectomy (112). Longer-term concerns
based diets (vegan or vegetarian) that are patients with BMI ⬍35 kg/m2 outside of a include vitamin and mineral deficiencies,
well planned and nutritionally adequate research protocol. (E) osteoporosis, and rare but often severe hy-
have also been shown to improve meta- ● The long-term benefits, cost-effectiveness, poglycemia from insulin hypersecretion.
bolic control (107,108). and risks of bariatric surgery in individ- Cohort studies attempting to match sub-
The primary goal with respect to di- uals with type 2 diabetes should be jects suggest that the procedure may reduce
etary fat in individuals with diabetes is to studied in well-designed, randomized longer-term mortality rates (113), and it is
limit saturated fatty acids, trans fatty ac- controlled trials with optimal medical reasonable to postulate that there may be
ids, and cholesterol intake so as to reduce and lifestyle therapy as the comparator. recouping of costs over the long term. How-
risk for CVD. Saturated and trans fatty ac- (E) ever, studies of the mechanisms of glycemic
ids are the principal dietary determinants improvement, long-term benefits and risks,
of plasma LDL cholesterol. There is a lack Gastric reduction surgery, either gastric and cost-effectiveness of bariatric surgery in
of evidence on the effects of specific fatty banding or procedures that involve by- individuals with type 2 diabetes will require
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S25
Standards of Medical Care
well-designed, randomized clinical trials diabetes make informed self-management overseen by the Centers for Medicare and
with optimal medical and lifestyle therapy decisions. Care of diabetes has shifted to Medicaid Services (www.cms.hhs.gov/
of diabetes and cardiovascular risk factors as an approach that is more patient centered DiabetesSelfManagement).
the comparators. and places the person with diabetes at the
center of the care model working in col- G. Physical activity
F. Diabetes self-management laboration with health care professionals.
education Patient-centered care is respectful of and Recommendations
responsive to individual patient prefer- ● People with diabetes should be advised
Recommendations ences, needs, and values and ensures that to perform at least 150 min/week of
● People with diabetes should receive patient values guide all decision making moderate-intensity aerobic physical ac-
DSME according to national standards (123). tivity (50 –70% of maximum heart
when their diabetes is diagnosed and as rate). (A)
needed thereafter. (B) 1. Evidence for the benefits of DSME ● In the absence of contraindications,
● Effective self-management and quality Multiple studies have found that DSME is people with type 2 diabetes should be
of life are the key outcomes of DSME associated with improved diabetes encouraged to perform resistance train-
and should be measured and moni- knowledge and self-care behavior (115); ing three times per week. (A)
tored as part of care. (C) improved clinical outcomes such as lower
● DSME should address psychosocial is- A1C (116,117,119,120,124), lower self- ADA technical reviews on exercise in pa-
sues, since emotional well-being is as- reported weight (115), improved quality tients with diabetes, currently being up-
sociated with positive diabetes of life (118,125), and healthy coping dated, have summarized the value of
outcomes. (C) (126); and lower costs (127). Better out- exercise in the diabetes management plan
● Because DSME can result in cost- comes were reported for DSME interven- (143,144). Regular exercise has been
savings and improved outcomes (B), tions that were longer and included shown to improve blood glucose control,
DSME should be reimbursed by third- follow-up support (115,128 –131), that reduce cardiovascular risk factors, con-
party payors. (E) were culturally (132) and age appropriate tribute to weight loss, and improve well
(133,134) and tailored to individual being. Furthermore, regular exercise may
DSME is an essential element of dia- needs and preferences (114), and that ad- prevent type 2 diabetes in high-risk indi-
betes care (114 –120), and national stan- dressed psychosocial issues (114,115, viduals (11–13). Structured exercise in-
dards for DSME (121) are based on 119,135). Both individual and group ap- terventions of at least 8 weeks’ duration
evidence for its benefits. Education helps proaches have been found effective (136 – have been shown to lower A1C by an av-
people with diabetes initiate effective self- 138). There is growing evidence for the erage of 0.66% in people with type 2 di-
management and cope with diabetes role of community health workers and abetes, even with no significant change in
when they are first diagnosed. Ongoing peer (139) and lay leaders (140) in deliv- BMI (145). Higher levels of exercise in-
DSME and support also help people with ering DSME and support in addition to tensity are associated with greater im-
diabetes maintain effective self- the core team (141). provements in A1C and fitness (146).
management throughout a lifetime of di- Diabetes education is associated with
abetes as they face new challenges and as increased use of primary and preventive 1. Frequency and type of exercise
treatment advances become available. services and lower use of acute, inpatient The U.S. Department of Health and Hu-
DSME helps patients optimize metabolic hospital services (127). Patients who par- man Services’ Physical Activity Guide-
control, prevent and manage complica- ticipate in diabetes education are more lines for Americans (147) suggest that
tions, and maximize quality of life in a likely to follow best practice treatment adults over age 18 years perform 150 min/
cost-effective manner (122). recommendations, particularly among week of moderate-intensity or 75 min/
DSME is the on-going process of fa- the medicare population, and to have week of vigorous aerobic physical activity
cilitating the knowledge, skill, and ability lower Medicare and commercial claim or an equivalent combination of the two.
necessary for diabetes self-care (121). costs (142). In addition, the guidelines suggest that
This process incorporates the needs, adults also do muscle-strengthening ac-
goals, and life experiences of the person 2. National Standards for DSME tivities that involve all major muscle
with diabetes. The overall objectives of The National Standards for DSME are de- groups two or more days per week. The
DSME are to support informed decision- signed to define quality diabetes self- guidelines suggest that adults over age 65
making, self-care behaviors, problem- management education and to assist years, or those with disabilities, follow the
solving, and active collaboration with the diabetes educators in a variety of settings adult guidelines if possible or (if this is not
health care team and to improve clinical to provide evidence-based education possible) be as physically active as they
outcomes, health status, and quality of life (121). The standards, most recently re- are able. Studies included in the meta-
in a cost-effective manner (121). vised in 2007, are reviewed and updated analysis of effects of exercise interventions
Current best practice of DSME is a every 5 years by a task force representing on glycemic control (145) had a mean
skills-based approach that focuses on key organizations involved in the field of number of sessions per week of 3.4, with
helping those with diabetes make in- diabetes education and care. a mean of 49 min/session. The DPP life-
formed self-management choices. DSME style intervention, which included 150
has changed from a didactic approach fo- 3. Reimbursement for DSME min/week of moderate intensity exercise,
cusing on providing information, to a DSME, when provided by a program that had a beneficial effect on glycemia in
more theoretically based empowerment meets ADA recognition standards, is re- those with pre-diabetes. Therefore, it
model that focuses on helping those with imbursed as part of the Medicare program seems reasonable to recommend that peo-
S26 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
ple with diabetes try to follow the physical sumption is not altered. For individuals H. Psychosocial assessment and care
activity guidelines for the general on these therapies, added carbohydrate
population. should be ingested if pre-exercise glucose Recommendations
Progressive resistance exercise im- levels are ⬍100 mg/dl (5.6 mmol/l) ● Assessment of psychological and social
proves insulin sensitivity in older men (154,155). Hypoglycemia is rare in dia- situation should be included as an on-
with type 2 diabetes to the same or even to betic individuals who are not treated with going part of the medical management
a greater extent as aerobic exercise (148). insulin or insulin secretagogues, and no of diabetes. (E)
Clinical trials have provided strong evi- preventive measures for hypoglycemia ● Psychosocial screening and follow-up
dence for the A1C-lowering value of re- are usually advised in these cases. should include, but is not limited to,
sistance training in older adults with type attitudes about the illness, expectations
2 diabetes (149,150) and for an additive for medical management and out-
benefit of combined aerobic and resis- 4. Exercise in the presence of specific comes, affect/mood, general and diabe-
tance exercise in adults with type 2 diabe- long-term complications of diabetes tes-related quality of life, resources
tes (151). a. Retinopathy. In the presence of pro- (financial, social, and emotional), and
liferative diabetic retinopathy (PDR) or psychiatric history. (E)
2. Evaluation of the diabetic patient severe non-proliferative diabetic retinop- ● Screen for psychosocial problems such
before recommending an exercise athy (NPDR), vigorous aerobic or resis- as depression and diabetes-related dis-
program tance exercise may be contraindicated tress, anxiety, eating disorders, and
Prior guidelines have suggested that be- because of the risk of triggering vitreous cognitive impairment when self-
fore recommending a program of physical hemorrhage or retinal detachment (156). management is poor. (C)
activity, the provider should assess pa- b. Peripheral neuropathy. Decreased
tients with multiple cardiovascular risk pain sensation in the extremities results in Psychological and social problems can
factors for coronary artery disease (CAD). increased risk of skin breakdown and in- impair the ability of the individual (162–
As further discussed in VI.A.5. Coronary fection and of Charcot joint destruction. 164) or the family to carry out diabetes
heart disease screening and treatment, the Prior recommendations have advised care tasks and therefore compromise
area of screening asymptomatic diabetic non–weight-bearing exercise for patients health status. There are opportunities for
patients for CAD remains unclear, and a with severe peripheral neuropathy. Stud- the clinician to assess psychosocial status
recent ADA consensus statement on this ies have shown that moderate-intensity in a timely and efficient manner so that
issue concluded that routine screening is walking may not lead to increased risk of referral for appropriate services can be
not recommended (152). Providers foot ulcers or reulceration in those with accomplished.
should use clinical judgment in this area. peripheral neuropathy (157). All individ- Key opportunities for screening of
Certainly, high-risk patients should be uals with peripheral neuropathy should psychosocial status occur at diagnosis,
encouraged to start with short periods of wear proper footwear and examine their during regularly scheduled management
low-intensity exercise and to increase the feet daily for early detection of lesions. visits, during hospitalizations, at discov-
intensity and duration slowly. Anyone with a foot injury or open sore ery of complications, or when problems
Providers should assess patients for should be restricted to non–weight- with glucose control, quality of life, or ad-
conditions that might contraindicate cer- bearing activities. herence are identified. Patients are likely
tain types of exercise or predispose to in- c. Autonomic neuropathy. Autonomic to exhibit psychological vulnerability at
jury, such as uncontrolled hypertension, neuropathy can increase the risk of exer- diagnosis and when their medical status
severe autonomic neuropathy, severe pe- cise-induced injury or adverse events changes, i.e., the end of the honeymoon
ripheral neuropathy or history of foot le- through decreased cardiac responsive- period, when the need for intensified
sions, and unstable proliferative ness to exercise, postural hypotension, treatment is evident, and when complica-
retinopathy. The patient’s age and previ- impaired thermoregulation, impaired tions are discovered (164).
ous physical activity level should be night vision due to impaired papillary re- Issues known to impact self-
considered. action, and unpredictable carbohydrate management and health outcomes in-
delivery from gastroparesis predisposing clude but are not limited to: attitudes
3. Exercise in the presence of to hypoglycemia (158). Autonomic neu- about the illness, expectations for medical
nonoptimal glycemic control ropathy is also strongly associated with management and outcomes, affect/mood,
a. Hyperglycemia. When people with CVD in people with diabetes (159,160). general and diabetes-related quality of
type 1 diabetes are deprived of insulin for People with diabetic autonomic neuropa- life, diabetes-related distress (165), re-
12– 48 h and are ketotic, exercise can thy should undergo cardiac investigation sources (financial, social, and emotional)
worsen hyperglycemia and ketosis (153); before beginning physical activity more (166), and psychiatric history (167,168).
therefore, vigorous activity should be intense than that to which they are Screening tools are available for a number
avoided in the presence of ketosis. How- accustomed. of these areas (135). Indications for refer-
ever, it is not necessary to postpone exer- d. Albuminuria and nephropathy. Phys- ral to a mental health specialist familiar
cise simply based on hyperglycemia, ical activity can acutely increase urinary with diabetes management may include
provided the patient feels well and urine protein excretion. However, there is no gross noncompliance with medical regi-
and/or blood ketones are negative. evidence that vigorous exercise increases men (by self or others) (168), depression
b. Hypoglycemia. In individuals taking the rate of progression of diabetic kidney with the possibility of self-harm
insulin and/or insulin secretagogues, disease and likely no need for any specific (169,170), debilitating anxiety (alone or
physical activity can cause hypoglycemia exercise restrictions for people with dia- with depression), indications of an eating
if medication dose or carbohydrate con- betic kidney disease (161). disorder, or cognitive functioning that
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S27
Standards of Medical Care
significantly impairs judgment. It is pref- sured. Infection or dehydration are more Severe hypoglycemia (where the indi-
erable to incorporate psychological as- likely to necessitate hospitalization of the vidual requires the assistance of another
sessment and treatment into routine care person with diabetes than the person person and cannot be treated with oral
rather than waiting for identification of a without diabetes. carbohydrate due to confusion or uncon-
specific problem or deterioration in psy- The hospitalized patient should be sciousness) should be treated using emer-
chological status (135). Although the cli- treated by a physician with expertise in gency glucagon kits, which require a
nician may not feel qualified to treat the management of diabetes. For further prescription. Those in close contact with
psychological problems, using the pa- information on management of patients or who have custodial care of people with
tient-provider relationship as a founda- with hyperglycemia in the hospital, see hypoglycemia-prone diabetes (family
tion for further treatment can increase the VIII.A. Diabetes care in the hospital. For members, roommates, school personnel,
likelihood that the patient will accept re- further information on management of child care providers, correctional institu-
ferral for other services. It is important to DKA or nonketotic hyperosmolar state, tion staff, or coworkers) should be in-
establish that emotional well-being is part refer to the ADA consensus statement on structed in use of such kits. An individual
of diabetes management. hyperglycemic crises (173). does not need to be a health care profes-
sional to safely administer glucagon. Care
I. When treatment goals are not met K. Hypoglycemia should be taken to ensure that unexpired
For a variety of reasons, some people with glucagon kits are available.
diabetes and their health care providers Recommendations Prevention of hypoglycemia is a crit-
do not achieve the desired goals of treat- ● Glucose (15–20 g) is the preferred ical component of diabetes management.
ment (Table 11). Rethinking the treat- treatment for the conscious individual Teaching people with diabetes to balance
ment regimen may require assessment of with hypoglycemia, although any form insulin use, carbohydrate intake, and ex-
barriers including income, health literacy, of carbohydrate that contains glucose ercise is a necessary but not always suffi-
diabetes distress, depression, and com- may be used. If SMBG 15 min after cient strategy. In type 1 diabetes and
peting demands, including those related treatment shows continued hypoglyce- severely insulin-deficient type 2 diabetes,
to family responsibilities and dynamics. mia, the treatment should be repeated. the syndrome of hypoglycemia unaware-
Other strategies may include culturally Once SMBG glucose returns to normal, ness, or hypoglycemia-associated auto-
appropriate and enhanced DSME, co- the individual should consume a meal nomic failure, can severely compromise
management with a diabetes team, refer- or snack to prevent recurrence of hypo- stringent diabetes control and quality of
ral to a medical social worker for glycemia. (E) life. The deficient counter-regulatory hor-
assistance with insurance coverage, or ● Glucagon should be prescribed for all mone release and autonomic responses in
change in pharmacological therapy. Initi- individuals at significant risk of severe this syndrome are both risk factors for
ation of or increase in SMBG, utilization hypoglycemia, and caregivers or family and are caused by hypoglycemia. A corol-
of CGM, frequent contact with the pa- members of these individuals should be lary to this “vicious cycle” is that several
tient, or referral to a mental health profes- instructed in its administration. Gluca- weeks of avoidance of hypoglycemia has
sional or physician with special expertise gon administration is not limited to been demonstrated to improve counter-
in diabetes may be useful. Providing pa- health care professionals. (E) regulation and awareness to some extent
tients with an algorithm for self-titration ● Individuals with hypoglycemia un- in many patients (174,176,177). Hence,
of insulin doses based on SMBG results awareness or one or more episodes of patients with one or more episodes of se-
may be helpful for type 2 patients who severe hypoglycemia should be advised vere hypoglycemia may benefit from at
take insulin (171). to raise their glycemic targets to strictly least short-term relaxation of glycemic
avoid further hypoglycemia for at least targets.
J. Intercurrent illness several weeks to partially reverse hypo-
The stress of illness, trauma, and/or sur- glycemia unawareness and reduce risk
gery frequently aggravates glycemic con- of future episodes. (B) L. Immunization
trol and may precipitate diabetic
ketoacidosis (DKA) or nonketotic hyper- Hypoglycemia is the leading limiting fac-
osmolar state, life-threatening conditions tor in the glycemic management of type 1 Recommendations
that require immediate medical care to and insulin-treated type 2 diabetes (174). ● Annually provide an influenza vaccine
prevent complications and death (172). Treatment of hypoglycemia (PG ⬍70 mg/ to all diabetic patients ⱖ6 months of
Any condition leading to deterioration in dl) requires ingestion of glucose- or car- age. (C)
glycemic control necessitates more fre- bohydrate-containing foods. The acute ● Administer pneumococcal polysaccha-
quent monitoring of blood glucose and glycemic response correlates better with ride vaccine to all diabetic patients ⱖ2
(in ketosis-prone patients) urine or blood the glucose content than with the carbo- years of age. A one-time revaccination is
ketones. Marked hyperglycemia requires hydrate content of the food. Although recommended for individuals ⬎64
temporary adjustment of the treatment pure glucose is the preferred treatment, years of age previously immunized
program and, if accompanied by ketosis, any form of carbohydrate that contains when they were ⬍65 years of age if the
vomiting, or alteration in level of con- glucose will raise blood glucose. Added vaccine was administered ⬎5 years
sciousness, immediate interaction with fat may retard and then prolong the acute ago. Other indications for repeat vacci-
the diabetes care team. The patient treated glycemic response (175). Ongoing activ- nation include nephrotic syndrome,
with noninsulin therapies or MNT alone ity of insulin or insulin secretagogues may chronic renal disease, and other immu-
may temporarily require insulin. Ade- lead to recurrence of hypoglycemia unless nocompromised states, such as after
quate fluid and caloric intake must be as- further food is ingested after recovery. transplantation. (C)
S28 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Influenza and pneumonia are common, such a strategy may be desirable to under- m2 and a loop diuretic for those with an
preventable infectious diseases associated take in adult patients prior to instituting estimated GFR ⬍30 ml 䡠 min/1.73 m2.
with high mortality and morbidity in the preventive therapy. (C)
elderly and in people with chronic dis- ● Multiple drug therapy (two or more
eases. Though there are limited studies 1. Hypertension/blood pressure agents at maximal doses) is generally
reporting the morbidity and mortality of control required to achieve blood pressure tar-
influenza and pneumococcal pneumonia gets. (B)
specifically in people with diabetes, ob- Recommendations ● If ACE inhibitors, ARBs, or diuretics are
servational studies of patients with a vari- used, kidney function and serum potas-
ety of chronic illnesses, including Screening and diagnosis sium levels should be closely moni-
● Blood pressure should be measured at
diabetes, show that these conditions are tored. (E)
associated with an increase in hospitaliza- every routine diabetes visit. Patients ● In pregnant patients with diabetes and
tions for influenza and its complications. found to have systolic blood pressure chronic hypertension, blood pressure
People with diabetes may be at increased ⱖ130 mmHg or diastolic blood pres- target goals of 110 –129/65–79 mmHg
risk of the bacteremic form of pneumo- sure ⱖ80 mmHg should have blood are suggested in the interest of long-
coccal infection and have been reported pressure confirmed on a separate day. term maternal health and minimizing
to have a high risk of nosocomial bactere- Repeat systolic blood pressure ⱖ130 impaired fetal growth. ACE inhibitors
mia, which has a mortality rate as high as mmHg or diastolic blood pressure ⱖ80 and ARBs are contraindicated during
50% (178). mmHg confirms a diagnosis of hyper- pregnancy. (E)
Safe and effective vaccines are avail- tension. (C)
able that can greatly reduce the risk of
serious complications from these diseases Goals Hypertension is a common comorbidity
(179,180). In a case-control series, influ- ● Patients with diabetes should be treated of diabetes that affects the majority of pa-
enza vaccine was shown to reduce diabe- to a systolic blood pressure ⬍130 tients, with prevalence depending on type
tes-related hospital admission by as much mmHg. (C) of diabetes, age, obesity, and ethnicity.
as 79% during flu epidemics (179). There ● Patients with diabetes should be treated Hypertension is a major risk factor for
is sufficient evidence to support that peo- to a diastolic blood pressure ⬍80 both CVD and microvascular complica-
ple with diabetes have appropriate sero- mmHg. (B) tions. In type 1 diabetes, hypertension is
logic and clinical responses to these often the result of underlying nephropa-
vaccinations. The Centers for Disease Treatment thy, while in type 2 diabetes it usually
Control and Prevention’s Advisory Com- ● Patients with a systolic blood pressure coexists with other cardiometabolic risk
mittee on Immunization Practices recom- 130 –139 mmHg or a diastolic blood factors.
mends influenza and pneumococcal pressure 80 – 89 mmHg may be given a. Screening and diagnosis. Measure-
vaccines for all individuals with diabetes lifestyle therapy alone for a maximum ment of blood pressure in the office
(http://www.cdc.gov/vaccines/recs/). For of 3 months, and then if targets are not should be done by a trained individual
a complete discussion on the prevention achieved, patients should be treated and should follow the guidelines estab-
of influenza and pneumococcal disease in with the addition of pharmacological lished for nondiabetic individuals: mea-
people with diabetes, consult the techni- agents. (E) surement in the seated position, with feet
cal review and position statement on this ● Patients with more severe hypertension on the floor and arm supported at heart
subject (178,181). (systolic blood pressure ⱖ140 mmHg level, after 5 min of rest. Cuff size should
or diastolic blood pressure ⱖ90 be appropriate for the upper arm circum-
VI. PREVENTION AND mmHg) at diagnosis or follow-up ference. Elevated values should be con-
MANAGEMENT OF should receive pharmacologic therapy firmed on a separate day. Because of the
DIABETES COMPLICATIONS in addition to lifestyle therapy. (A) clear synergistic risks of hypertension and
● Lifestyle therapy for hypertension con- diabetes, the diagnostic cutoff for a diag-
A. Cardiovascular disease sists of weight loss if overweight, nosis of hypertension is lower in people
CVD is the major cause of morbidity and DASH-style dietary pattern including with diabetes (blood pressure ⱖ130/80
mortality for individuals with diabetes and reducing sodium and increasing potas- mmHg) than in those without diabetes
the largest contributor to the direct and in- sium intake, moderation of alcohol in- (blood pressure ⱖ140/90 mmHg) (184).
direct costs of diabetes. The common con- take, and increased physical activity. Home blood pressure self-monitoring
ditions coexisting with type 2 diabetes (e.g., (B) and 24-h ambulatory blood pressure
hypertension and dyslipidemia) are clear ● Pharmacologic therapy for patients monitoring may provide additional evi-
risk factors for CVD, and diabetes itself con- with diabetes and hypertension should dence of “white coat” and masked hyper-
fers independent risk. Numerous studies be paired with a regimen that includes tension and other discrepancies between
have shown the efficacy of controlling indi- either an ACE inhibitor or an angioten- office and “true” blood pressure, and
vidual cardiovascular risk factors in pre- sin II receptor blocker (ARB). If one studies in nondiabetic populations show
venting or slowing CVD in people with class is not tolerated, the other should that home measurements may correlate
diabetes. Large benefits are seen when mul- be substituted. If needed to achieve better with CVD risk than office measure-
tiple risk factors are addressed globally blood pressure targets, a thiazide di- ments (185,186). However, the prepon-
(182,183). Risk for coronary heart disease uretic should be added to those with an derance of the clear evidence of benefits of
and CVD in general can be estimated using estimated glomerular filtration rate treatment of hypertension in people with
multivariable risk factor approaches, and (GFR) (see below) ⱖ30 ml 䡠 min/1.73 diabetes is based on office measurements.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S29
Standards of Medical Care
b. Treatment goals. Randomized clinical reducing cardiovascular events (194 – optimal doses of at least three antihyper-
trials have demonstrated the benefit (re- 196). However, a variety of other studies tensive agents of different classifications,
duction of coronary heart disease [CHD] have shown no specific advantage to ACE one of which should be a diuretic, clini-
events, stroke, and nephropathy) of low- inhibitors as initial treatment of hyperten- cians should consider an evaluation for
ering blood pressure to ⬍140 mmHg sys- sion in the general hypertensive popula- secondary forms of hypertension.
tolic and ⬍80 mmHg diastolic in tion, but rather an advantage on During pregnancy in diabetic women
individuals with diabetes (184,187–189). cardiovascular outcomes of initial therapy with chronic hypertension, target blood
Epidemiologic analyses show that blood with low-dose thiazide diuretics pressure goals of 110 –129 mmHg sys-
pressure ⬎115/75 mmHg is associated (184,197,198). tolic and 65–79 mmHg diastolic are rea-
with increased cardiovascular event rates In people with diabetes, inhibitors of sonable, as they contribute to long-term
and mortality in individuals with diabetes the renin-angiotensin system (RAS) may maternal health. Lower blood pressure
(184,190,191). Therefore, a target blood have unique advantages for initial or early levels may be associated with impaired
pressure goal of ⬍130/80 mmHg is rea- therapy of hypertension. In a nonhyper- fetal growth. During pregnancy, treat-
sonable if it can be achieved safely. The tension trial of high-risk individuals in- ment with ACE inhibitors and ARBs is
ongoing ACCORD trial is designed to de- cluding a large subset with diabetes, an contraindicated, since they can cause fetal
termine whether blood pressure lowering ACE inhibitor reduced CVD outcomes damage. Antihypertensive drugs known
to systolic blood pressure ⬍120 mmHg (199). In patients with congestive heart to be effective and safe in pregnancy in-
provides greater cardiovascular protec- failure (CHF), including diabetic sub- clude methyldopa, labetalol, diltiazem,
tion than a systolic blood pressure level of groups, ARBs have been shown to reduce clonidine, and prazosin. Chronic diuretic
⬍140 mmHg in patients with type 2 dia- major CVD outcomes (200 –203), and in use during pregnancy has been associated
betes (192). type 2 patients with significant nephrop- with restricted maternal plasma volume,
c. Treatment strategies. Although there athy, ARBs were superior to calcium which might reduce uteroplacental perfu-
are no well-controlled studies of diet and channel blockers for reducing heart fail- sion (209).
exercise in the treatment of hypertension ure (204 –206). Though evidence for dis-
in individuals with diabetes, the Dietary tinct advantages of RAS inhibitors on 2. Dyslipidemia/lipid management
Approaches to Stop Hypertension CVD outcomes in diabetes remains con-
(DASH) study in nondiabetic individuals flicting (187,207), the high CVD risks as-
Recommendations
has shown antihypertensive effects simi- sociated with diabetes, and the high
lar to those of pharmacologic mono- prevalence of undiagnosed CVD, may still Screening
therapy. Lifestyle therapy consists of favor recommendations for their use as ● In most adult patients, measure fasting
reducing sodium intake (to ⬍1,500 mg/ first-line hypertension therapy in people lipid profile at least annually. In adults
day) and excess body weight; increasing with diabetes (184). Recently, the blood with low-risk lipid values (LDL choles-
consumption of fruits, vegetables (8 –10 pressure arm of the ADVANCE trial dem- terol ⬍100 mg/dl, HDL cholesterol
servings/day), and low-fat dairy products onstrated that routine administration of a ⬎50 mg/dl, and triglycerides ⬍150
(2–3 servings/day); avoiding excessive al- fixed combination of the ACE inhibitor mg/dl), lipid assessments may be re-
cohol consumption (no more than two perindopril and the diuretic indapamide peated every 2 years. (E)
servings per day in men and no more than significantly reduced combined micro-
one serving per day in women); and in- vascular and macrovascular outcomes, as Treatment recommendations and goals
creasing activity levels (184,193). These well as CVD and total mortality. The im- ● Lifestyle modification focusing on the
nonpharmacological strategies may also proved outcomes also could have been reduction of saturated fat, trans fat,
positively affect glycemia and lipid con- due to lower achieved blood pressure in and cholesterol intake; increase of n-3
trol. Their effects on cardiovascular the perindopril-indapamide arm (208). fatty acids, viscous fiber, and plant
events have not been established. An ini- In addition, the ACCOMPLISH (Avoiding stanols/sterols; weight loss (if indi-
tial trial of nonpharmacologic therapy Cardiovascular Events in Combination cated); and increased physical activity
may be reasonable in diabetic individu- Therapy in Patients Living with Systolic should be recommended to improve
als with mild hypertension (systolic Hypertension) trial showed a decrease in the lipid profile in patients with dia-
130 –139 mmHg or diastolic 80 – 89 morbidity and mortality in those receiv- betes. (A)
mmHg). If the blood pressure is ⱖ140 ing benazapril and amlodipine versus ● Statin therapy should be added to life-
mmHg systolic and/or ⱖ90 mmHg dia- benazapril and hydrochlorothiazide. The style therapy, regardless of baseline
stolic at the time of diagnosis, pharma- compelling benefits of RAS inhibitors in lipid levels, for diabetic patients:
cologic therapy should be initiated diabetic patients with albuminuria or re- ● with overt CVD. (A)
along with nonpharmacologic therapy nal insufficiency provide additional ratio- ● without CVD who are over the age of
(184). nale for use of these agents (see below, 40 years and have one or more other
Lowering of blood pressure with reg- VI.B. Nephropathy screening and CVD risk factors. (A)
imens based on a variety of antihyperten- treatment). ● For patients at lower risk than de-
sive drugs, including ACE inhibitors, An important caveat is that most pa- scribed above (e.g., without overt CVD
ARBs, -blockers, diuretics, and calcium tients with hypertension require multi- and under the age of 40 years), statin
channel blockers, has been shown to be drug therapy to reach treatment goals, therapy should be considered in addi-
effective in reducing cardiovascular especially diabetic patients whose targets tion to lifestyle therapy if LDL choles-
events. Several studies suggested that are lower. Many patients will require terol remains ⬎100 mg/dl or in those
ACE inhibitors may be superior to dihy- three or more drugs to reach target goals with multiple CVD risk factors. (E)
dropyridine calcium channel blockers in (184). If blood pressure is refractory to ● In individuals without overt CVD, the
S30 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 12—Reduction in 10-year risk of major CVD endpoints (CHD death/non-fatal MI) in major statin trials, or sub-studies of major trials,
in diabetic subjects (N ⴝ 16,032)
LDL
CVD Relative risk Absolute risk cholesterol
Study (ref.) prevention Statin dose and comparator Risk reduction reduction reduction reduction
4S-DM (211) 2° Simvastatin 20–40 mg vs. placebo 85.7 to 43.2% (50%) 42.5% 186 to 119 mg/dl 36%
ASPEN 2° (216) 2° Atorvastatin 10 mg vs. placebo 39.5 to 24.5% (34%) 12.7% 112 to 79 mg/dl 29%
HPS-DM (212) 2° Simvastatin 40 mg vs. placebo 43.8 to 36.3% (17%) 7.5% 123 to 84 mg/dl 31%
CARE-DM (213) 2° Pravastatin 40 mg vs. placebo 40.8 to 35.4% (13%) 5.4% 136 to 99 mg/dl 27%
TNT-DM (214) 2° Atorvastatin 80 mg vs. 10 mg 26.3 to 21.6% (18%) 4.7% 99 to 77 mg/dl 22%
HPS-DM (212) 1° Simvastatin 40 mg vs. placebo 17.5 to 11.5% (34%) 6.0% 124 to 86 mg/dl 31%
CARDS (234) 1° Atorvastatin 10 mg vs. placebo 11.5 to 7.5% (35%) 4.0% 118 to 71 mg/dl 40%
ASPEN 1° (216) 1° Atorvastatin 10 mg vs. placebo 9.8 to 7.9% (19%) 1.9% 114 to 80 mg/dl 30%
ASCOT-DM (215) 1° Atorvastatin 10 mg vs. placebo 11.1 to 10.2% (8%) 0.9% 125 to 82 mg/dl 34%
Studies were of differing lengths (3.3–5.4 years) and used somewhat different outcomes, but all reported rates of CVD death and non-fatal MI. In this tabulation,
results of the statin on 10-year risk of major CVD endpoints (CHD death/non-fatal MI) are listed for comparison between studies. Correlation between 10-year CVD
risk of the control group and the absolute risk reduction with statin therapy is highly significant (P ⫽ 0.0007). Analyses provided by Craig Williams, PharmD, Oregon
Health & Science University, 2007.
primary goal is an LDL cholesterol n i fi c a n t p r i m a r y a n d s e c o n d a r y abetic subgroup of a larger trial (219).
⬍100 mg/dl (2.6 mmol/l). (A) prevention of CVD events with and with- However, in a large trial specific to dia-
● In individuals with overt CVD, a lower out CHD deaths in diabetic populations. betic patients, fenofibrate failed to re-
LDL cholesterol goal of ⬍70 mg/dl (1.8 As shown in Table 12, and similar to find- duce overall cardiovascular outcomes
mmol/l), using a high dose of a statin, is ings in nondiabetic subjects, reduction in (221).
an option. (B) “hard” CVD outcomes (CHD death and b. Dyslipidemia treatment and target
● If drug-treated patients do not reach the nonfatal MI) can be more clearly seen in lipid levels. For most patients with dia-
above targets on maximal tolerated sta- diabetic subjects with high baseline CVD betes, the first priority of dyslipidemia
tin therapy, a reduction in LDL choles- risk (known CVD and/or very high LDL therapy (unless severe hypertriglyceride-
terol of ⬃30 – 40% from baseline is an cholesterol levels), but overall the benefits mia is the immediate issue) is to lower
alternative therapeutic goal. (A) of statin therapy in people with diabetes at LDL cholesterol to a target goal of ⬍100
● Triglycerides levels ⬍150 mg/dl (1.7 moderate or high risk for CVD are mg/dl (2.60 mmol/l) (222). Lifestyle in-
mmol/l) and HDL cholesterol ⬎40 convincing. tervention, including MNT, increased
mg/dl (1.0 mmol/l) in men and ⬎50 Low levels of HDL cholesterol, often physical activity, weight loss, and smok-
mg/dl (1.3 mmol/l) in women, are de- associated with elevated triglyceride lev- ing cessation, may allow some patients to
sirable. However, LDL cholesterol– els, are the most prevalent pattern of dys- reach lipid goals. Nutrition intervention
targeted statin therapy remains the lipidemia in people with type 2 diabetes. should be tailored according to each pa-
preferred strategy. (C) However, the evidence base for drugs that tient’s age, type of diabetes, pharmacolog-
● If targets are not reached on maximally target these lipid fractions is significantly ical treatment, lipid levels, and other
tolerated doses of statins, combination less robust than that for statin therapy medical conditions and should focus on
therapy using statins and other lipid- (217). Nicotinic acid has been shown to the reduction of saturated fat, cholesterol,
lowering agents may be considered to reduce CVD outcomes (218), although and trans unsaturated fat intake and in-
achieve lipid targets but has not been the study was done in a nondiabetic co- creases in n-3 fatty acids, viscous fiber
evaluated in outcome studies for either hort. Gemfibrozil has been shown to de- (such as in oats, legumes, citrus), and
CVD outcomes or safety. (E) crease rates of CVD events in subjects plant stanols/sterols. Glycemic control
● Statin therapy is contraindicated in without diabetes (219,220) and in a di- can also beneficially modify plasma lipid
pregnancy. (E) levels, particularly in patients with very
high triglycerides and poor glycemic
a. Evidence for benefits of lipid-lowering Table 13—Summary of recommendations control.
therapy. Patients with type 2 diabetes for glycemic, blood pressure, and lipid control In those with clinical CVD or who are
have an increased prevalence of lipid ab- for adults with diabetes over age 40 years and have CVD risk fac-
normalities, contributing to their high tors, pharmacological treatment should
risk of CVD. Over the past decade or A1C ⬍7.0%* be added to lifestyle therapy regardless of
Blood pressure ⬍130/80 mmHg
more, multiple clinical trials have demon- baseline lipid levels. Statins are the drugs
Lipids
strated significant effects of pharmaco- of choice for lowering LDL cholesterol.
LDL cholesterol ⬍100 mg/dl (⬍2.6
logic (primarily statin) therapy on CVD In patients other than those described
mmol/l)†
outcomes in subjects with CHD and for above, statin treatment should be consid-
primary CVD prevention (210). Analyses *Referenced to a nondiabetic range of 4.0 – 6.0% ered if there is an inadequate LDL choles-
using a DCCT-based assay. †In individuals with
of diabetic subgroups of larger trials overt CVD, a lower LDL cholesterol goal of ⬍70 terol response to lifestyle modifications
(211–215) and trials specifically in sub- mg/dl (1.8 mmol/l), using a high dose of a statin, is and improved glucose control or if the
jects with diabetes (216,217) showed sig- an option. patient has increased cardiovascular risk
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S31
Standards of Medical Care
(e.g., multiple cardiovascular risk factors brate, ezetimibe, and bile acid seques- for glycemic, blood pressure, and lipid
or long duration of diabetes). Very little trants all offer additional LDL cholesterol control for adults with diabetes, see Table
clinical trial evidence exists for type 2 di- lowering. The evidence that combination 13.
abetic patients under the age of 40 years therapy provides a significant increment
and for type 1 diabetic patients of any age. in CVD risk reduction over statin therapy 3. Antiplatelet agents
In the Heart Protection Study (lower age alone is still elusive.
limit 40 years), the subgroup of 600 pa- d. Treatment of other lipoprotein frac- Recommendations
tients with type 1 diabetes had a propor- tions or targets. Severe hypertriglyceri- ● Consider aspirin therapy (75–162 mg/
tionately similar reduction in risk as demia may warrant immediate therapy of day) as a primary prevention strategy in
patients with type 2 diabetes although not this abnormality with lifestyle and usually those with type 1 or type 2 diabetes at
statistically significant (212). Although pharmacologic therapy (fibric acid deriv- increased cardiovascular risk (10-year
the data are not definitive, consideration ative or niacin) to reduce the risk of acute risk ⬎10%). This includes most men
should be given to lipid-lowering goals pancreatitis. In the absence of severe hy- ⬎50 years of age or women ⬎60 years
for type 1 diabetic patients similar to pertriglyceridemia, therapy targeting of age who have at least one additional
those for type 2 diabetic patients, partic- HDL cholesterol or triglycerides has intu- major risk factor (family history of
ularly if other cardiovascular risk factors itive appeal but lacks the evidence base of CVD, hypertension, smoking, dyslipi-
are present. statin therapy (186). If the HDL choles- demia, or albuminuria). (C)
c. Alternative LDL cholesterol goals. terol is ⬍40 mg/dl and the LDL choles- ● There is not sufficient evidence to rec-
Virtually all trials of statins and CVD out- terol is 100 –129 mg/dl, gemfibrozil or ommend aspirin for primary preven-
come have tested specific doses of statins niacin might be used, especially if a pa- tion in lower risk individuals, such as
against placebo, other doses of statin, or tient is intolerant to statins. Niacin is the men ⬍50 years of age or women ⬍60
other statins, rather than aiming for spe- most effective drug for raising HDL cho- years of age without other major risk
cific LDL cholesterol goals (223). As can lesterol. It can significantly increase blood factors. For patients in these age-groups
be seen in Table 10, placebo-controlled glucose at high doses, but recent studies with multiple other risk factors, clinical
trials generally achieved LDL cholesterol demonstrate that at modest doses (750 – judgment is required. (C)
reductions of 30 – 40% from baseline. 2,000 mg/day), significant improvements ● Use aspirin therapy (75–162 mg/day)
Hence, LDL cholesterol lowering of this in LDL cholesterol, HDL cholesterol, and as a secondary prevention strategy in
magnitude is an acceptable outcome for triglyceride levels are accompanied by those with diabetes with a history of
patients who cannot reach LDL choles- only modest changes in glucose that are CVD. (A)
terol goals due to severe baseline eleva- generally amenable to adjustment of dia- ● For patients with CVD and docu-
tions in LDL cholesterol and/or betes therapy (230,231). mented aspirin allergy, clopidogrel (75
intolerance of maximal, or any, statin Combination therapy with a statin mg/day) should be used. (B)
doses. Additionally, for those with base- and a fibrate or a statin and niacin may be ● Combination therapy with ASA (75–
line LDL cholesterol minimally ⬎100 mg/ efficacious for treatment of all three lipid 162 mg/day) and clopidogrel (75 mg/
dl, prescribing statin therapy to lower fractions, but this combination is associ- day) is reasonable for up to a year after
LDL cholesterol to ⬃30 – 40% from base- ated with an increased risk for abnormal an acute coronary syndrome. (B)
line is probably more effective than pre- transaminase levels, myositis, or rhabdo-
scribing just enough to get LDL myolysis. The risk of rhabdomyolysis is ADA and the American Heart Association
cholesterol slightly ⬍100 mg/dl. higher with higher doses of statins and (AHA) have, in the past, jointly recom-
Recent clinical trials in high-risk pa- with renal insufficiency and seems to be mended that low-dose aspirin therapy be
tients, such as those with acute coronary lower when statins are combined with fe- used as a primary prevention strategy in
syndromes or previous cardiovascular nofibrate than gemfibrozil (232). Several those with diabetes at increased cardio-
events (224 –226), have demonstrated ongoing trials may provide much-needed vascular risk, including those who are
that more aggressive therapy with high evidence for the effects of combination over 40 years of age or those with addi-
doses of statins to achieve an LDL choles- therapy on cardiovascular outcomes. tional risk factors (family history of CVD,
terol of ⬍70 mg/dl led to a significant re- In 2008, a consensus panel convened hypertension, smoking, dyslipidemia, or
duction in further events. Therefore, a by ADA and the American College of Car- albuminuria) (235). These recommenda-
reduction in LDL cholesterol to a goal of diology (ACC) recommended a greater tions were derived from several older tri-
⬍70 mg/dl is an option in very-high-risk focus on non-HDL cholesterol and apo als that included small numbers of
diabetic patients with overt CVD (227). lipoprotein B (apo B) in patients who are patients with diabetes.
In individual patients, LDL choles- likely to have small LDL particles, such as Aspirin has been shown to be effec-
terol lowering with statins is highly vari- people with diabetes (233). The consen- tive in reducing cardiovascular morbidity
able, and this variable response is poorly sus panel suggested that for statin-treated and mortality in high-risk patients with
understood (228). Reduction of CVD patients in whom the LDL cholesterol previous MI or stroke (secondary preven-
events with statins correlates very closely goal would be ⬍70 mg/dl (non-HDL cho- tion). Its net benefit in primary preven-
with LDL cholesterol lowering (229). lesterol ⬍100 mg/dl), apo B should be tion among patients with no previous
When maximally tolerated doses of st- measured and treated to ⬍80 mg/dl. For cardiovascular events is more controver-
atins fail to significantly lower LDL cho- patients on statins with an LDL choles- sial, both for patients with and without
lesterol (⬍30% reduction from patients terol goal of ⬍100 mg/dl (non-HDL cho- a history of diabetes (236). The U.S.
baseline), the primary aim of combination lesterol ⬍130 mg/dl), apo B should be Preventive Services Task Force recently
therapy should be to achieve additional measured and treated to ⬍90 mg/dl. updated its evidence base and recommen-
LDL cholesterol lowering. Niacin, fenofi- For a summary of recommendations dations about aspirin use for primary pre-
S32 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
vention (237,238). The Task Force Based on the currently available evi- set by the incidence of significant bleed-
recommended encouraging aspirin use in dence, aspirin appears to have a modest ing. Clinical judgment should be used for
men 45–79 and women 55–79 years of effect on ischemic vascular events with those at intermediate risk (younger pa-
age and not encouraging aspirin use in the absolute decrease in events depending tients with one or risk factors or older pa-
younger adults and did not differentiate on the underlying CVD risk. The main tients with no risk factors; those with 10-
based on the presence or absence of adverse effects appear to be an increased year CVD risk 5–10%) until further
diabetes. risk of gastrointestinal bleeding. The ex- research is available. Use of aspirin in pa-
Two recent randomized controlled cess risk may be as high as 1–5 per 1,000 tients under the age of 21 years is contra-
trials of aspirin specifically in patients per year in real-world settings. In adults indicated due to the associated risk of
with diabetes failed to show a significant with CVD risk greater than 1% per year, Reye’s syndrome.
reduction in CVD end points, raising fur- the number of CVD events prevented will Clopidogrel has been demonstrated
ther questions about the efficacy of aspi- be similar to or greater than the number of to reduce CVD events in diabetic individ-
rin for primary prevention in people with episodes of bleeding induced, although uals (247). It is recommended as adjunc-
diabetes (239,240). In 2009, ADA AHA, these complications do not have equal ef- tive therapy in the 1st year after an acute
and ACC convened a group of experts to fects on long-term health (241). coronary syndrome or as alternative ther-
review and synthesize the available evi- Average daily dosages used in most apy in aspirin-intolerant patients.
dence and use this information to create clinical trials involving patients with dia-
an updated recommendation. Their re- betes ranged from 50 – 650 mg but were 4. Smoking cessation
port, including analyses in addition to mostly in the range of 100 –325 mg/day.
those described below, will be published There is little evidence to support any spe- Recommendations
in early 2010. cific dose, but using the lowest possible ● Advise all patients not to smoke. (A)
The ATT (Anti-Thrombotic Trialists’) dosage may help reduce side effects ● Include smoking cessation counseling
collaborators recently published an indi- (242). Although platelets from patients and other forms of treatment as a rou-
vidual patient-level meta-analysis of the with diabetes have altered function, it is tine component of diabetes care. (B)
six large trials of aspirin for primary pre- unclear what, if any, impact that finding
vention in the general population (236). has on the required dose of aspirin for Issues of smoking and diabetes are reviewed
These trials collectively enrolled over cardioprotective effects in the patient in detail in the ADA technical review (248)
with diabetes. Many alternate pathways and position statement (249) on this topic.
95,000 participants, including almost
for platelet activation exist that are inde- A large body of evidence from epidemiolog-
4,000 with diabetes. Overall, they found
pendent of thromboxane A2 and thus not ical, case-control, and cohort studies pro-
that aspirin reduced the risk of vascular
sensitive to the effects of aspirin (243). vides convincing documentation of the
events by 12% (RR 0.88 [95% CI 0.82–
Therefore, while “aspirin resistance” ap- causal link between cigarette smoking and
0.94]). The largest reduction was for non-
pears higher in diabetic patients when health risks. Cigarette smoking contributes
fatal MI (0.77 [0.67– 0.89]). Aspirin had
measured by a variety of ex vivo and in to one of every five deaths in the U.S. and is
little effect on CHD death (0.95 [0.78 – vitro methods (platelet aggrenometry,
1.15]) or total stroke (0.95 [0.85–1.06]). the most important modifiable cause of pre-
measurement of thromboxane B2), these
The net effect on total stroke reflected a mature death. Much of the prior work doc-
observations alone are insufficient to em-
relative reduction in risk of ischemic umenting the impact of smoking on health
pirically recommend at this time that
stroke (⫺14%) and a relative increased did not separately discuss results on subsets
higher doses of aspirin be used in the di-
risk of hemorrhagic stroke (⫹32%). of individuals with diabetes, suggesting that
abetic patient (244 –246).
There was some evidence of a difference the identified risks are at least equivalent to
Aspirin use for secondary prevention
in aspirin effect by sex. Aspirin reduced continues to have a strong evidence base those found in the general population.
CHD events in men (0.77 [0.67– 0.89]) and is recommended. Until further evi- Other studies of individuals with diabetes
but not in women (0.95 [0.77–1.17]). dence is available, low-dose (75–162 mg/ consistently found a heightened risk of
Conversely, aspirin had no effect on day) aspirin use for primary prevention is CVD and premature death among smokers.
stroke in men (1.01 [0.74 –1.39]) but re- reasonable for adults with diabetes and no Smoking is also related to the premature de-
duced stroke in women (0.77 [0.59 – previous history of vascular disease who velopment of microvascular complications
0.99]). These potential differences in are at increased CVD risk (10-year risk of of diabetes and may have a role in the de-
effect by sex were of borderline statistical CVD events ⬎10%) and who are not at velopment of type 2 diabetes.
significance, were affected strongly by the increased risk for bleeding. This generally A number of large randomized clini-
results of one trial, and cannot be consid- includes most men over age 50 years and cal trials have demonstrated the efficacy
ered definitive. Notably, sex differences in women over age 60 years who also have and cost-effectiveness of smoking cessa-
aspirin’s effects have not been observed in one or more of the following major risk tion counseling in changing smoking be-
studies of secondary prevention (236). In factors: smoking, hypertension, dyslipi- havior and reducing tobacco use. The
the six trials examined by the ATT collab- demia, family history of premature CVD, routine and thorough assessment of to-
orators, the effect of aspirin on major vas- and albuminuria. bacco use is important as a means of pre-
cular events was similar for patients with Aspirin should not be recommended venting smoking or encouraging
and without diabetes (0.88 [0.67–1.15] for those at low CVD risk (women under cessation. Special considerations should
and 0.87 [0.79 – 0.96], respectively). The age 60 years and men under age 50 years include assessment of level of nicotine de-
CI was wider for those with diabetes be- with no major CVD risk factors; 10-year pendence, which is associated with diffi-
cause of their smaller number. CVD risk ⬍5%), as the low benefit is off- culty in quitting and relapse (250,251).
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S33
Standards of Medical Care
5. Coronary heart disease screening dial perfusion imaging in more than one and ARBs, there is clinical trial support
and treatment in five patients, cardiac outcomes were es- for each of the following statements:
sentially equal (and very low) in screened ● In patients with type 1 diabetes, hy-
Recommendations versus unscreened patients. Accordingly, pertension, and any degree of albu-
the overall effectiveness, especially the minuria, ACE inhibitors have been
Screening cost-effectiveness, of such an indiscrimi- shown to delay the progression of ne-
● In asymptomatic patients, evaluate risk
nate screening strategy is in question. phropathy. (A)
factors to stratify patients by 10-year In all patients with diabetes, cardio- ● In patients with type 2 diabetes, hy-
risk, and treat risk factors accordingly. vascular risk factors should be assessed at pertension, and microalbuminuria,
(B) least annually. These risk factors include both ACE inhibitors and ARBs have
dyslipidemia, hypertension, smoking, a been shown to delay the progression
Treatment positive family history of premature cor- to macroalbuminuria. (A)
● In patients with known CVD, ACE in- onary disease, and the presence of micro- ● In patients with type 2 diabetes, hy-
hibitor (C), aspirin (A), and statin ther- or macroalbuminuria. Abnormal risk pertension, macroalbuminuria, and
apy (A) (if not contraindicated) should factors should be treated as described renal insufficiency (serum creatinine
be used to reduce the risk of cardiovas- elsewhere in these guidelines. Patients at ⬎1.5 mg/dl), ARBs have been shown
cular events. increased CHD risk should receive aspirin to delay the progression of nephrop-
● In patients with a prior MI, -blockers and a statin, and ACE inhibitor, or ARB athy. (A)
should be continued for at least 2 years therapy if hypertensive, unless there are ● If one class is not tolerated, the other
after the event. (B) contraindications to a particular drug should be substituted. (E)
● Longer-term use of -blockers in the class. While clear benefit exists for ACE ● Reduction of protein intake to 0.8 –1.0
absence of hypertension is reasonable if inhibitor and ARB therapy in patients g 䡠 kg body wt–1 䡠 day–1 in individuals
well tolerated, but data are lacking. (E) with nephropathy or hypertension, the with diabetes and the earlier stages of
● Avoid thiazolidinedione (TZD) treat- benefits in patients with CVD in the ab- CKD and to 0.8 g 䡠 kg body wt–1 䡠 day–1
ment in patients with symptomatic sence of these conditions is less clear, in the later stages of CKD may improve
heart failure. (C) especially when LDL cholesterol is con- measures of renal function (urine albu-
● Metformin may be used in patients with comitantly controlled (257,258). min excretion rate and GFR) and is rec-
stable CHF if renal function is normal. ommended. (B)
It should be avoided in unstable or hos- B. Nephropathy screening and ● When ACE inhibitors, ARBs, or diuret-
pitalized patients with CHF. (C) treatment ics are used, monitor serum creatinine
and potassium levels for the develop-
Screening for CAD is reviewed in a re- Recommendations ment of acute kidney disease and hy-
cently updated consensus statement (93). perkalemia. (E)
To identify the presence of CAD in dia- General recommendations ● Continued monitoring of urine albu-
● To reduce the risk or slow the progres-
betic patients without clear or suggestive min excretion to assess both response
symptoms, a risk factor– based approach sion of nephropathy, optimize glucose to therapy and progression of disease is
to the initial diagnostic evaluation and control. (A) recommended. (E)
● To reduce the risk or slow the progres- ●
subsequent follow-up has intuitive ap- Consider referral to a physician experi-
peal. However, recent studies concluded sion of nephropathy, optimize blood enced in the care of kidney disease
that using this approach fails to identify pressure control. (A) when there is uncertainty about the eti-
which patients will have silent ischemia ology of kidney disease (active urine
on screening tests (159,252). Screening sediment, absence of retinopathy, or
Candidates for cardiac testing include ● Perform an annual test to assess urine rapid decline in GFR), difficult manage-
those with 1) typical or atypical cardiac albumin excretion in type 1 diabetic pa- ment issues, or advanced kidney dis-
symptoms and 2) an abnormal resting tients with diabetes duration of 5 years ease. (B)
electrocardiogram (ECG). The screening and in all type 2 diabetic patients, start-
of asymptomatic patients remains contro- ing at diagnosis. (E) Diabetic nephropathy occurs in 20 – 40%
versial, especially since intensive medical ● Measure serum creatinine at least annu- of patients with diabetes and is the single
therapy, indicated in diabetic patients at ally in all adults with diabetes regard- leading cause of end-stage renal disease
high risk for CVD, has an increasing evi- less of the degree of urine albumin (ESRD). Persistent albuminuria in the
dence base for providing equal outcomes excretion. The serum creatinine should range of 30 –299 mg/24 h (microalbu-
to invasive revascularization, including in be used to estimate GFR and stage the minuria) has been shown to be the earliest
diabetic patients (253,254). There is also level of chronic kidney disease (CKD), stage of diabetic nephropathy in type 1
recent preliminary evidence that silent if present. (E) diabetes and a marker for development of
myocardial ischemia may reverse over nephropathy in type 2 diabetes. Mi-
time, adding to the controversy concern- Treatment croalbuminuria is also a well-established
ing aggressive screening strategies (255). ● In the treatment of the nonpregnant pa- marker of increased CVD risk (259,260).
Finally, a recent randomized observa- tient with micro- or macroalbuminuria, Patients with microalbuminuria who
tional trial demonstrated no clinical ben- either ACE inhibitors or ARBs should progress to macroalbuminuria (ⱖ300
efit to routine screening of asymptomatic be used. (A) mg/24 h) are likely to progress to ESRD
patients with type 2 diabetes and normal ● While there are no adequate head-to- (261,262). However, a number of inter-
ECGs (256). Despite abnormal myocar- head comparisons of ACE inhibitors ventions have been demonstrated to re-
S34 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
duce the risk and slow the progression of Table 14—Definitions of abnormalities in al- cation (Table 15) is primarily based on
renal disease. bumin excretion GFR levels and therefore differs from
Intensive diabetes management other systems, in which staging is based
with the goal of achieving near- Spot collection primarily on urinary albumin excretion
normoglycemia has been shown in large (g/mg (284). Studies have found decreased GFR
prospective randomized studies to de- Category creatinine) in the absence of increased urine albumin
lay the onset of microalbuminuria and excretion in a substantial percentage of
the progression of micro- to macroalbu- Normal ⬍30 adults with diabetes (285,286). Epidemi-
minuria in patients with type 1 Microalbuminuria 30–299 ologic evidence suggests that a substantial
(263,264) and type 2 (57,58) diabetes. Macroalbuminuria (clinical) ⱖ300 fraction of those with CKD in the setting
The UKPDS provided strong evidence of diabetes have little or no detectable al-
that control of blood pressure can re- buminuria (285). Serum creatinine
duce the development of nephropathy should be used as additional therapy to should therefore be measured at least an-
(187). In addition, large prospective further lower blood pressure in patients nually in all adults with diabetes, regard-
randomized studies in patients with already treated with ACE inhibitors or less of the degree of urine albumin
type 1 diabetes have demonstrated that ARBs (204) or as alternate therapy in the excretion.
achievement of lower levels of systolic rare individual unable to tolerate ACE in- Serum creatinine should be used to
blood pressure (⬍140 mmHg) resulting hibitors or ARBs. estimate GFR and to stage the level of
from treatment using ACE inhibitors Studies in patients with varying stages CKD, if present. Estimated GFR (eGFR) is
provides a selective benefit over other of nephropathy have shown that protein commonly co-reported by laboratories or
antihypertensive drug classes in delay- restriction helps slow the progression of can be estimated using formulae such as
ing the progression from micro- to mac- albuminuria, GFR decline, and occur- the Modification of Diet in Renal Disease
roalbuminuria and can slow the decline rence of ESRD (278 –281). Protein re- (MDRD) study equation (287). Recent re-
in GFR in patients with macroalbumin- striction should be considered ports have indicated that the MDRD is
uria (205,206,265). In type 2 diabetes particularly in patients whose nephropa- more accurate for the diagnosis and strat-
with hypertension and normoalbuminuria, thy seems to be progressing despite opti- ification of CKD in patients with diabetes
RAS inhibition has been demonstrated to mal glucose and blood pressure control than the Cockcroft-Gault formula (288).
delay onset of microalbuminuria (266). and use of ACE inhibitor and/or ARBs GFR calculators are available at http://
In addition, ACE inhibitors have been (281). www.nkdep.nih.gov.
shown to reduce major CVD outcomes The role of continued annual quanti-
(i.e., MI, stroke, and death) in patients Assessment of albuminuria status tative assessment of albumin excretion af-
with diabetes (199), thus further support- and renal function ter diagnosis of microalbuminuria and
ing the use of these agents in patients with Screening for microalbuminuria can be institution of ACE inhibitor or ARB ther-
microalbuminuria, a CVD risk factor. performed by measurement of the albu- apy and blood pressure control is unclear.
ARBs do not prevent microalbuminuria in min-to-creatinine ratio in a random spot Continued surveillance can assess both
normotensive patients with type 1 or type collection (preferred method); 24-h or response to therapy and progression of
2 diabetes (267,268); however, ARBs timed collections are more burdensome disease. Some suggest that reducing ab-
have been shown to reduce the rate of and add little to prediction or accuracy normal albuminuria (⬎30 mg/g) to the
progression from micro- to macroalbu- (282,283). Measurement of a spot urine normal or near-normal range may im-
minuria as well as ESRD in patients with for albumin only, whether by immunoas- prove renal and cardiovascular prognosis,
type 2 diabetes (269 –271). Some evi- say or by using a dipstick test specific for but this approach has not been formally
dence suggests that ARBs have a smaller microalbumin, without simultaneously evaluated in prospective trials.
magnitude of rise in potassium compared measuring urine creatinine, is somewhat Complications of kidney disease cor-
with ACE inhibitors in people with ne- less expensive but susceptible to false- relate with level of kidney function. When
phropathy (272,273). It is important to negative and -positive determinations as a the eGFR is less than 60 ml 䡠 min/1.73 m2,
note that both ACE inhibitors and ARBs result of variation in urine concentration screening for anemia, malnutrition, and
reduce loss of kidney function in people due to hydration and other factors. metabolic bone disease is indicated. Early
with diabetic nephropathy, above and be- Abnormalities of albumin excretion vaccination against Hepatitis B is indi-
yond any such effect attributable to a re- are defined in Table 14. Because of vari- cated in patients likely to progress to end-
duction in systemic blood pressure. ability in urinary albumin excretion, two stage kidney disease.
Combinations of drugs that block the ren- of three specimens collected within a 3- to Consider referral to a physician expe-
nin-angiotensin-aldosterone system (e.g., 6-month period should be abnormal be- rienced in the care of kidney disease when
an ACE inhibitor plus an ARB, a miner- fore considering a patient to have crossed there is uncertainty about the etiology of
alocorticoid antagonist, or a direct renin one of these diagnostic thresholds. Exer- kidney disease (active urine sediment, ab-
inhibitor) have been shown to provide ad- cise within 24 h, infection, fever, CHF, sence of retinopathy, or rapid decline in
ditional lowering of albuminuria (274 – marked hyperglycemia, and marked hy- GFR), difficult management issues, or ad-
277). However, the long-term effects of pertension may elevate urinary albumin vanced kidney disease. The threshold for
such combinations on renal or cardiovas- excretion over baseline values. referral may vary depending on the fre-
cular outcomes have not yet been evalu- Information on presence of abnormal quency with which a provider encounters
ated in clinical trials. urine albumin excretion in addition to diabetic patients with significant kidney
Other drugs, such as diuretics, cal- level of GFR may be used to stage CKD. disease. Consultation with a nephrologist
cium channel blockers, and -blockers, The National Kidney Foundation classifi- when stage 4 CKD develops has been
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S35
Standards of Medical Care
Table 15—Stages of CKD other disorders of the eye occur earlier
and more frequently in people with
GFR (ml/min per diabetes.
1.73 m2 body In addition to duration of diabetes,
Stage Description surface area) other factors that increase the risk of, or
are associated with, retinopathy include
1 Kidney damage* with normal or increased GFR ⱖ90 chronic hyperglycemia (291), the pres-
2 Kidney damage* with mildly decreased GFR 60–89 ence of nephropathy (292), and hyper-
3 Moderately decreased GFR 30–59 tension (293). Intensive diabetes
4 Severely decreased GFR 15–29 management with the goal of achieving
5 Kidney failure ⬍15 or dialysis near normoglycemia has been shown in
*Kidney damage defined as abnormalities on pathologic, urine, blood, or imaging tests. Adapted from ref. large prospective randomized studies to
283. prevent and/or delay the onset and pro-
gression of diabetic retinopathy
(53,57,58). Lowering blood pressure has
found to reduce cost, improve quality of betic retinopathy. Interpretation of the been shown to decrease the progression
care, and keep people off dialysis longer images should be performed by a of retinopathy (187). Several case series
(289,290). However, nonrenal specialists trained eye care provider. While retinal and a controlled prospective study sug-
should not delay educating their patients photography may serve as a screening gest that pregnancy in type 1 diabetic pa-
about the progressive nature of diabetic tool for retinopathy, it is not a substi- tients may aggravate retinopathy
kidney disease, the renal preservation tute for a comprehensive eye exam, (294,295); laser photocoagulation sur-
benefits of aggressive treatment of blood which should be performed at least ini- gery can minimize this risk (295).
pressure, blood glucose, and hyperlipid- tially and at intervals thereafter as rec- One of the main motivations for
emia, and the potential need for renal re- ommended by an eye care professional. screening for diabetic retinopathy is the
placement therapy. (E) established efficacy of laser photocoagu-
● Women with preexisting diabetes who lation surgery in preventing vision loss.
C. Retinopathy screening and are planning pregnancy or who have Two large trials, the Diabetic Retinopathy
treatment become pregnant should have a com- Study (DRS) and the Early Treatment Di-
prehensive eye examination and be abetic Retinopathy Study (ETDRS), pro-
Recommendations counseled on the risk of development vide the strongest support for the
and/or progression of diabetic retinop- therapeutic benefits of photocoagulation
General recommendations surgery.
● To reduce the risk or slow the progres-
athy. Eye examination should occur in
the first trimester with close follow-up The DRS (296) showed that panreti-
sion of retinopathy, optimize glycemic nal photocoagulation surgery reduced the
control. (A) throughout pregnancy and for 1 year
postpartum. (B) risk of severe vision loss from PDR from
● To reduce the risk or slow the progres-
15.9% in untreated eyes to 6.4% in
sion of retinopathy, optimize blood treated eyes. The benefit was greatest
pressure control. (A) Treatment
among patients whose baseline evalua-
● Promptly refer patients with any level of tion revealed high-risk characteristics
Screening macular edema, severe NPDR, or any (chiefly disc neovascularization or vitre-
● Adults and children aged 10 years or PDR to an ophthalmologist who is ous hemorrhage). Given the risks of mod-
older with type 1 diabetes should have knowledgeable and experienced in the est loss of visual acuity and contraction of
an initial dilated and comprehensive management and treatment of diabetic the visual field from panretinal laser sur-
eye examination by an ophthalmologist retinopathy. (A) gery, such therapy is primarily recom-
or optometrist within 5 years after the ● Laser photocoagulation therapy is indi-
mended for eyes with PDR approaching
onset of diabetes. (B) cated to reduce the risk of vision loss in or having high-risk characteristics.
● Patients with type 2 diabetes should patients with high-risk PDR, clinically The ETDRS (297) established the
have an initial dilated and comprehen- significant macular edema, and in some benefit of focal laser photocoagulation
sive eye examination by an ophthalmol- cases of severe NPDR. (A) surgery in eyes with macular edema,
ogist or optometrist shortly after the ● The presence of retinopathy is not a
particularly those with clinically signif-
diagnosis of diabetes. (B) contraindication to aspirin therapy for icant macular edema, with reduction of
● Subsequent examinations for type 1 cardioprotection, as this therapy does doubling of the visual angle (e.g., 20/
and type 2 diabetic patients should be not increase the risk of retinal hemor- 50 –20/100) from 20% in untreated
repeated annually by an ophthalmolo- rhage. (A) eyes to 8% in treated eyes. The ETDRS
gist or optometrist. Less frequent exams also verified the benefits of panretinal
(every 2–3 years) may be considered Diabetic retinopathy is a highly specific photocoagulation for high-risk PDR,
following one or more normal eye ex- vascular complication of both type 1 and but not for mild or moderate NPDR. In
ams. Examinations will be required type 2 diabetes, with prevalence strongly older-onset patients with severe NPDR
more frequently if retinopathy is pro- related to duration of diabetes. Diabetic or less-than-high-risk PDR, the risk of
gressing. (B) retinopathy is the most frequent cause of severe vision loss or vitrectomy was re-
● High-quality fundus photographs can new cases of blindness among adults aged duced 50% by early laser photocoagu-
detect most clinically significant dia- 20 –74 years. Glaucoma, cataracts, and lation surgery at these stages.
S36 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Laser photocoagulation surgery in D. Neuropathy screening and monofilament pressure sensation at the
both trials was beneficial in reducing the treatment (306) distal plantar aspect of both great toes and
risk of further vision loss, but generally metatarsal joints, and assessment of ankle
Recommendations
not beneficial in reversing already dimin- ● All patients should be screened for dis-
reflexes. Combinations of more than one
ished acuity. This preventive effect and test have ⬎87% sensitivity in detecting
tal symmetric polyneuropathy (DPN) at
the fact that patients with PDR or macular diagnosis and at least annually thereaf- DPN. Loss of 10-g monofilament percep-
edema may be asymptomatic provide ter using simple clinical tests. (B) tion and reduced vibration perception
strong support for a screening program to ● Electrophysiological testing is rarely predict foot ulcers (306).
detect diabetic retinopathy. needed, except in situations where the b. Diabetic autonomic neuropathy (307).
As retinopathy is estimated to take at clinical features are atypical. (E) The symptoms and signs of autonomic
least 5 years to develop after the onset of ● Screening for signs and symptoms of dysfunction should be elicited carefully
hyperglycemia (298), patients with type 1 cardiovascular autonomic neuropathy during the history and physical examina-
diabetes should have an initial dilated and should be instituted at diagnosis of type tion. Major clinical manifestations of dia-
comprehensive eye examination within 5 2 diabetes and 5 years after the diagno- betic autonomic neuropathy include
years after the onset of diabetes. Patients sis of type 1 diabetes. Special testing is resting tachycardia, exercise intolerance,
with type 2 diabetes who generally have rarely needed and may not affect man- orthostatic hypotension, constipation,
had years of undiagnosed diabetes (299) agement or outcomes. (E) gastroparesis, erectile dysfunction, sudo-
and who have a significant risk of preva- ● Medications for the relief of specific motor dysfunction, impaired neurovas-
lent diabetic retinopathy at the time of symptoms related to DPN and auto- cular function, “brittle diabetes,” and
diabetes diagnosis should have an initial nomic neuropathy are recommended, hypoglycemic autonomic failure.
dilated and comprehensive eye examina- as they improve the quality of life of the Cardiovascular autonomic neuropa-
tion soon after diagnosis. Examinations patient. (E) thy, a CVD risk factor (93), is the most
should be performed by an ophthalmolo- studied and clinically important form of
gist or optometrist who is knowledgeable The diabetic neuropathies are heteroge- diabetic autonomic neuropathy. Cardio-
and experienced in diagnosing the pres- neous with diverse clinical manifesta- vascular autonomic neuropathy may be
ence of diabetic retinopathy and is aware tions. They may be focal or diffuse. Most indicated by resting tachycardia (⬎100
of its management. Subsequent examina- common among the neuropathies are bpm), orthostasis (a fall in systolic blood
tions for type 1 and type 2 diabetic pa- chronic sensorimotor DPN and auto- pressure ⬎20 mmHg upon standing
tients are generally repeated annually. nomic neuropathy. Although DPN is a without an appropriate heart rate re-
Less frequent exams (every 2–3 years) diagnosis of exclusion, complex investi- sponse), or other disturbances in auto-
may be cost effective after one or more gations to exclude other conditions are nomic nervous system function involving
normal eye exams (300 –302), while ex- rarely needed. the skin, pupils, or gastrointestinal and
aminations will be required more fre- The early recognition and appropri- genitourinary systems.
quently if retinopathy is progressing. ate management of neuropathy in the pa- Gastrointestinal neuropathies (e.g.,
tient with diabetes is important for a
Examinations can also be done with esophageal enteropathy, gastroparesis,
number of reasons: 1) nondiabetic neu-
retinal photographs (with or without di- constipation, diarrhea, and fecal incon-
ropathies may be present in patients with
lation of the pupil) read by experienced diabetes and may be treatable; 2) a num- tinence) are common, and any section
experts. In-person exams are still nec- ber of treatment options exist for symp- of the gastrointestinal tract may be af-
essary when the photos are unaccept- tomatic diabetic neuropathy; 3) up to fected. Gastroparesis should be sus-
able and for follow-up of abnormalities 50% of DPN may be asymptomatic, and pected in individuals with erratic
detected. Photos are not a substitute for patients are at risk of insensate injury to glucose control or with upper gastroin-
a comprehensive eye exam, which their feet; 4) autonomic neuropathy may testinal symptoms without other identi-
should be performed at least initially involve every system in the body; and 5) fied cause. Evaluation of solid-phase
and at intervals thereafter as recom- cardiovascular autonomic neuropathy gastric emptying using double-isotope
mended by an eye care professional. causes substantial morbidity and mortal- scintigraphy may be done if symptoms
This technology has great potential in ity. Specific treatment for the underlying are suggestive, but test results often cor-
areas where qualified eye care profes- nerve damage is not currently available, relate poorly with symptoms. Constipa-
sionals are not available and may also other than improved glycemic control, tion is the most common lower-
enhance efficiency and reduce costs which may slow progression but not re- gastrointestinal symptom but can
when the expertise of ophthalmologists verse neuronal loss. Effective symptom- alternate with episodes of diarrhea.
can be used for more complex examina- atic treatments are available for some Diabetic autonomic neuropathy is
tions and for therapy (303). manifestations of DPN and autonomic also associated with genitourinary tract
Results of eye examinations should neuropathy. disturbances. In men, diabetic autonomic
be documented and transmitted to the neuropathy may cause erectile dysfunc-
referring health care professional. For a 1. Diagnosis of neuropathy tion and/or retrograde ejaculation. Evalu-
detailed review of the evidence and fur- a. Distal symmetric polyneuropathy. ation of bladder dysfunction should be
ther discussion of diabetic retinopathy, Patients with diabetes should be screened performed for individuals with diabetes
see the ADA technical review and annually for DPN using tests such as pin- who have recurrent urinary tract infec-
position statement on this subject prick sensation, vibration perception (us- tions, pyelonephritis, incontinence, or a
(304,305). ing a 128-Hz tuning fork), 10-g palpable bladder.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S37
Standards of Medical Care
Table 16—Table of drugs to treat symptomatic DPN ● visual impairment
● diabetic nephropathy (especially pa-
Class Examples Typical doses* tients on dialysis)
● poor glycemic control
Tricyclic drugs Amitriptyline 10–75 mg at bedtime ● cigarette smoking
Nortriptyline 25–75 mg at bedtime
Imipramine 25–75 mg at bedtime Many studies have been published pro-
Anticonvulsants Gabapentin 300–1,200 mg t.i.d. posing a range of tests that might usefully
Carbamazepine 200–400 mg t.i.d. identify patients at risk of foot ulceration,
Pregabalin† 100 mg t.i.d. creating confusion among practitioners as
5-Hydroxytryptamine and Duloxetine† 60–120 mg daily fs to which screening tests should be
norepinephrine uptake adopted in clinical practice. An ADA task
inhibitor force was therefore assembled in 2008 to
Substance P inhibitor Capsaicin cream 0.025–0.075% applied t.i.d.-q.i.d. concisely summarize recent literature in
*Dose response may vary; initial doses need to be low and titrated up. †Has FDA indication for treatment of this area and recommend what should be
painful diabetic neuropathy. included in the comprehensive foot exam
for adult patients with diabetes. Their rec-
ommendations are summarized below,
2. Symptomatic treatments for loss of protective sensation (LOPS)
but clinicians should refer to the task
(10-g monofilament plus testing any
a. Distal symmetric polyneuropathy. force report (308) for further details and
one of: vibration using 128-Hz tuning
The first step in management of patients practical descriptions of how to perform
fork, pinprick sensation, ankle reflexes,
with DPN should be to aim for stable and components of the comprehensive foot
or vibration perception threshold). (B)
optimal glycemic control. Although con- ● Provide general foot self-care education examination.
trolled trial evidence is lacking, several to all patients with diabetes. (B) At least annually, all adults with dia-
observational studies suggest that neuro- ●
betes should undergo a comprehensive
A multidisciplinary approach is recom-
pathic symptoms improve not only with foot examination to identify high-risk
mended for individuals with foot ulcers
optimization of control, but also with the conditions. Clinicians should ask about
and high-risk feet, especially those with
avoidance of extreme blood glucose fluc- history of previous foot ulceration or am-
a history of prior ulcer or amputation.
tuations. Patients with painful DPN may putation, neuropathic or peripheral vas-
(B)
benefit from pharmacological treatment ● Refer patients who smoke, have LOPS cular symptoms, impaired vision, tobacco
of their symptoms: many agents have ef- and structural abnormalities, or have use, and foot care practices. A general in-
ficacy confirmed in published random- history of prior lower-extremity com- spection of skin integrity and musculo-
ized controlled trials, with several FDA- plications to foot care specialists for on- skeletal deformities should be done in a
approved for the management of painful going preventive care and life-long well-lit room. Vascular assessment would
DPN. See Table 16 for examples of agents surveillance. (C) include inspection and assessment of
to treat DPN pain. ●
pedal pulses.
Initial screening for peripheral arterial
b. Diabetic autonomic neuropathy. Gas- The neurologic exam recommended
disease (PAD) should include a history
troparesis symptoms may improve with is designed to identify LOPS rather than
for claudication and an assessment of
dietary changes and prokinetic agents early neuropathy. The clinical examina-
the pedal pulses. Consider obtaining an
such as metoclopramide or erythromycin. tion to identify LOPS is simple and re-
ankle-brachial index (ABI), as many pa-
Treatments for erectile dysfunction may tients with PAD are asymptomatic. (C) quires no expensive equipment. Five
include phosphodiesterase type 5 inhibi- ●
simple clinical tests (use of a 10-g mono-
Refer patients with significant claudica-
tors, intracorporeal or intraurethral pros- filament, vibration testing using a 128-Hz
tion or a positive ABI for further vascu-
taglandins, vacuum devices, or penile tuning fork, tests of pinprick sensation,
lar assessment and consider exercise,
prostheses. Interventions for other mani- ankle reflex assessment, and testing vibra-
medications, and surgical options. (C)
festations of autonomic neuropathy are tion perception threshold with a biothesi-
described in the ADA statement on neu- Amputation and foot ulceration, conse- ometer), each with evidence from well-
ropathy (306). As with DPN treatments, quences of diabetic neuropathy and/or conducted prospective clinical cohort
these interventions do not change the un- PAD, are common and major causes of studies, are considered useful in the diag-
derlying pathology and natural history of morbidity and disability in people with nosis of LOPS in the diabetic foot. The
the disease process but may have a posi- diabetes. Early recognition and manage- task force agrees that any of the five tests
tive impact on the quality of life of the ment of risk factors can prevent or delay listed could be used by clinicians to iden-
patient. adverse outcomes. tify LOPS, although ideally two of these
The risk of ulcers or amputations is should be regularly performed during the
E. Foot care increased in people who have the follow- screening exam—normally the 10-g
Recommendations ing risk factors: monofilament and one other test. One or
● For all patients with diabetes, perform more abnormal tests would suggest
an annual comprehensive foot exami- ● previous amputation LOPS, while at least two normal tests (and
nation to identify risk factors predictive ● past foot ulcer history no abnormal test) would rule out LOPS.
of ulcers and amputations. The foot ex- ● peripheral neuropathy The last test listed, vibration assessment
amination should include inspection, ● foot deformity using a biothesiometer or similar instru-
assessment of foot pulses, and testing ● peripheral vascular disease ment, is widely used in the U.S.; however,
S38 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
identification of the patient with LOPS modated with commercial therapeutic will evolve according to, physical, psy-
can easily be carried out without this or footwear may need custom-molded chological, and emotional maturity. MNT
other expensive equipment. shoes. should be provided at diagnosis, and at
Initial screening for PAD should in- Foot ulcers and wound care may re- least annually thereafter, by an individual
clude a history for claudication and an quire care by a podiatrist, orthopedic experienced with the nutritional needs of
assessment of the pedal pulses. A diagnos- or vascular surgeon, or rehabilitation the growing child and the behavioral is-
tic ABI should be performed in any pa- specialist experienced in the manage- sues that have an impact on adolescent
tient with symptoms of PAD. Due to the ment of individuals with diabetes. For a diets, including risk for disordered eating.
high estimated prevalence of PAD in pa- complete discussion, see the ADA con-
tients with diabetes and the fact that sensus statement on diabetic foot wound a. Glycemic control
many patients with PAD are asymptom- care (310). Recommendations
atic, an ADA consensus statement on ● Consider age when setting glycemic
PAD (309) suggested that a screening VII. DIABETES CARE IN goals in children and adolescents with
of ABI be performed in patients over SPECIFIC POPULATIONS type 1 diabetes, with less stringent goals
50 years of age and considered in patients for younger children. (E)
under 50 years of age who have other A. Children and adolescents
PAD risk factors (e.g., smoking, hyperten- While current standards for diabetes
sion, hyperlipidemia, or duration of dia- management reflect the need to maintain
1. Type 1 diabetes glucose control as near to normal as safely
betes ⬎10 years). Refer patients with Three-quarters of all cases of type 1 dia-
significant symptoms or a positive ABI possible, special consideration must be
betes are diagnosed in individuals ⬍18 given to the unique risks of hypoglycemia
for further vascular assessment and con- years of age. Because children are not sim-
sider exercise, medications, and surgical in young children. Glycemic goals need to
ply “small adults,” it is appropriate to con- be modified to take into account the fact
options (309). sider the unique aspects of care and
Patients with diabetes and high-risk that most children ⬍6 or 7 years of age
management of children and adolescents have a form of “hypoglycemic unaware-
foot conditions should be educated re- with type 1 diabetes. Children with dia-
garding their risk factors and appropriate ness.” Their counterregulatory mecha-
betes differ from adults in many respects, nisms are immature and they may lack the
management. Patients at risk should un- including changes in insulin sensitivity cognitive capacity to recognize and re-
derstand the implications of the LOPS, related to sexual maturity and physical spond to hypoglycemic symptoms, plac-
the importance of foot monitoring on a growth, ability to provide self-care, super- ing them at greater risk for severe
daily basis, the proper care of the foot in- vision in child care and school, and hypoglycemia and its sequelae. In addi-
cluding nail and skin care, and the selec- unique neurologic vulnerability to hypo- tion, and unlike the case in adults, young
tion of appropriate footwear. Patients glycemia and DKA. Attention to such is- children under the age of 5 years are at
with LOPS should be educated on ways to sues as family dynamics, developmental risk for permanent cognitive impairment
substitute other sensory modalities (hand stages, and physiologic differences related after episodes of severe hypoglycemia
palpation, visual inspection) for surveil- to sexual maturity are all essential in de- (312–314). Extensive evidence indicates
lance of early foot problems. Patients’ un- veloping and implementing an optimal that near normalization of blood glucose
derstanding of these issues and their diabetes regimen. Although recommen- levels is seldom attainable in children and
physical ability to conduct proper foot dations for children and adolescents are adolescents after the honeymoon (remis-
surveillance and care should be assessed. less likely to be based on clinical trial ev- sion) period. The A1C level achieved in
Patients with visual difficulties, physical idence, because of current and historical the “intensive” adolescent cohort of the
constraints preventing movement, or cog- restraints placed on conducting research DCCT group was ⬎1% higher than that
nitive problems that impair their ability to in children, expert opinion and a review achieved by adult DCCT subjects and
assess the condition of the foot and to in- of available and relevant experimental above current ADA recommendations for
stitute appropriate responses will need data are summarized in the ADA state- patients in general. However, the in-
other people, such as family members, to ment on care of children and adolescents creased frequency of use of basal bolus
assist in their care. with type 1 diabetes (311). regimens (including insulin pumps) in
People with neuropathy or evidence Ideally, the care of a child or adoles- youth from infancy through adolescence
of increased plantar pressure (e.g., ery- cent with type 1 diabetes should be pro- has been associated with more children
thema, warmth, callus, or measured pres- vided by a multidisciplinary team of reaching ADA blood glucose targets
sure) may be adequately managed with specialists trained in the care of children (315,316) in those families in which both
well-fitted walking shoes or athletic with pediatric diabetes. At the very least, parents and the child with diabetes are
shoes that cushion the feet and redis- education of the child and family should motivated to perform the required diabe-
tribute pressure. Callus can be debrided be provided by health care providers tes-related tasks.
with a scalpel by a foot care specialist or trained and experienced in childhood di- In selecting glycemic goals, the bene-
other health professional with experience abetes and sensitive to the challenges fits on long-term health outcomes of
and training in foot care. People with posed by diabetes in this age-group. At achieving a lower A1C must be weighed
bony deformities (e.g., hammertoes, the time of initial diagnosis, it is essential against the unique risks of hypoglycemia
prominent metatarsal heads, or bunions) that diabetes education be provided in a and the difficulties achieving near-
may need extra-wide or -depth shoes. timely fashion, with the expectation that normoglycemia in children and youth.
People with extreme bony deformities the balance between adult supervision Age-specific glycemic and A1C goals are
(e.g., Charcot foot) who cannot be accom- and self-care should be defined by, and presented in Table 17.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S39
Standards of Medical Care
Table 17—Plasma blood glucose and A1C goals for type 1 diabetes by age-group
Plasma blood glucose goal
range (mg/dl)
Bedtime/
Values by age (years) Before meals overnight A1C Rationale
Toddlers and preschoolers (0–6) 100–180 110–200 ⬍8.5% (but ⬎7.5%) High risk and vulnerability to hypoglycemia
School age (6–12) 90–180 100–180 ⬍8% Risks of hypoglycemia and relatively low risk of
complications prior to puberty
Adolescents and young adults (13–19) 90–130 90–150 ⬍7.5% Risk of severe hypoglycemia
Developmental and psychological issues
A lower goal (⬍7.0%) is reasonable if it can be
achieved without excessive hypoglycemia
Key concepts in setting glycemic goals:
● Goals should be individualized and lower goals may be reasonable based on benefit-risk assessment.
● Blood glucose goals should be higher than those listed above in children with frequent hypoglycemia or hypoglycemia unawareness.
● Postprandial blood glucose values should be measured when there is a discrepancy between pre-prandial blood glucose values and A1C
levels and to help assess glycemia in those on basal/bolus regimens.
b. Screening and management of ● ACE inhibitors should be considered profile performed soon after diagnosis
chronic complications in children and for the initial treatment of hyperten- (after glucose control has been estab-
adolescents with type 1 diabetes sion. (E) lished). (E)
● The goal of treatment is a blood pres- ● For both age-groups, if lipids are abnor-
i. Nephropathy sure consistently ⬍130/80 or below the mal, annual monitoring is recom-
90th percentile for age, sex, and height, mended. If LDL cholesterol values are
Recommendations whichever is lower. (E) within the accepted risk levels (⬍100
● Annual screening for microalbumin-
mg/dl [2.6 mmol/l]), a lipid profile
uria, with a random spot urine sample
Hypertension in childhood is defined as should be repeated every 5 years. (E)
for microalbumin-to-creatinine ratio,
an average systolic or diastolic blood pres-
should be initiated once the child is 10
sure 95th percentile for age, sex, and Treatment
years of age and has had diabetes for 5 ● Initial therapy should consist of optimi-
height percentile measured on at least
years. (E)
three separate days. “High-normal” blood zation of glucose control and MNT us-
● Confirmed, persistently elevated mi-
pressure is defined as an average systolic ing a Step II AHA diet aimed at a
croalbumin levels on two additional
or diastolic blood pressure ⱖ90th but decrease in the amount of saturated fat
urine specimens should be treated with
⬍95th percentile for age, sex, and height in the diet. (E)
an ACE inhibitor, titrated to normaliza- ● After the age of 10 years, the addition of
percentile measured on at least 3 separate
tion of microalbumin excretion if pos-
days. Normal blood pressure levels for a statin is recommended in patients
sible. (E)
age, sex, and height and appropriate who, after MNT and lifestyle changes,
ii. Hypertension methods for determinations are available have LDL cholesterol ⬎160 mg/dl (4.1
online at www.nhlbi.nih.gov/health/ mmol/l) or LDL cholesterol ⬎130
Recommendations prof/heart/hbp/hbp_ped.pdf. mg/dl (3.4 mmol/l) and one or more
● Treatment of high-normal blood pres- CVD risk factors. (E)
sure (systolic or diastolic blood pres- ● The goal of therapy is an LDL choles-
iii. Dyslipidemia
sure consistently above the 90th terol value ⬍100 mg/dl (2.6 mmol/l).
percentile for age, sex, and height) (E)
Recommendations
should include dietary intervention
and exercise aimed at weight control Screening People diagnosed with type 1 diabetes in
and increased physical activity, if ap- ● If there is a family history of hypercho- childhood have a high risk of early sub-
propriate. If target blood pressure is not lesterolemia (total cholesterol ⬎240 clinical (317–319) and clinical (320)
reached with 3– 6 months of lifestyle mg/dl) or a cardiovascular event before CVD. Although intervention data are
intervention, pharmacologic treatment age 55 years, or if family history is un- lacking, the AHA categorizes type 1 dia-
should be initiated. (E) known, then a fasting lipid profile betic children in the highest tier for car-
● Pharmacologic treatment of hyperten- should be performed on children ⬎2 diovascular risk and recommends both
sion (systolic or diastolic blood pres- years of age soon after diagnosis (after lifestyle and pharmacologic treatment for
sure consistently above the 95th glucose control has been established). those with elevated LDL cholesterol levels
percentile for age, sex, and height or If family history is not of concern, then (321,322). Initial therapy should be with
consistently ⬎130/80 mmHg, if 95% the first lipid screening should be per- a Step II AHA diet, which restricts satu-
exceeds that value) should be initiated formed at puberty (ⱖ10 years). All chil- rated fat to 7% of total calories and re-
as soon as the diagnosis is confirmed. dren diagnosed with diabetes at or after stricts dietary cholesterol to 200 mg per
(E) puberty should have a fasting lipid day. Data from randomized clinical trials
S40 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
in children as young as 7 months of age odic rescreening of asymptomatic indi- into adolescence. Health care providers
indicate that this diet is safe and does not viduals. (E) who care for children and adolescents
interfere with normal growth and devel- ● Children with positive antibodies therefore must be capable of evaluating
opment (323,324). should be referred to a gastroenterolo- the behavioral, emotional, and psychoso-
For children over the age of 10 years gist for evaluation. (E) cial factors that interfere with implemen-
with persistent elevation of LDL choles- ● Children with confirmed celiac disease tation and then must work with the
terol despite lifestyle therapy, statins should have consultation with a dieti- individual and family to resolve problems
should be considered. Neither long-term tian and be placed on a gluten-free diet. that occur and/or to modify goals as
safety nor cardiovascular outcome effi- (E) appropriate.
cacy has been established for children. d. School and day care. Since a sizable
However, recent studies have shown Celiac disease is an immune-mediated portion of a child’s day is spent in school,
short-term safety equivalent to that seen disorder that occurs with increased fre- close communication with school or day
in adults and efficacy in lowering LDL quency in patients with type 1 diabetes care personnel is essential for optimal di-
cholesterol levels, improving endothelial (1–16% of individuals compared with
abetes management, safety, and maximal
function, and causing regression of ca- 0.3–1% in the general population)
academic opportunities. See VIII.B. Dia-
rotid intimal thickening (325–327). No (328,329). Symptoms of celiac disease in-
betes Care in the School and Day Care
statin is approved for use under the age of clude diarrhea, weight loss or poor weight
10 years, and statin treatment should gen- gain, growth failure, abdominal pain, Setting, for further discussion.
erally not be used in type 1 diabetic chil- chronic fatigue, malnutrition due to mal-
dren prior to this age. absorption, other gastrointestinal prob-
lems, and unexplained hypoglycemia or 2. Type 2 diabetes
iv. Retinopathy erratic blood glucose concentrations. The incidence of type 2 diabetes in ado-
lescents is increasing, especially in ethnic
Recommendations vi. Hypothyroidism minority populations (21). Distinction
● The first ophthalmologic examination between type 1 and type 2 diabetes in
should be obtained once the child is 10 Recommendations children can be difficult, since the preva-
years of age and has had diabetes for ● Children with type 1 diabetes should be lence of overweight in children continues
3–5 years. (E) screened for thyroid peroxidase and to rise and since autoantigens and ketosis
● After the initial examination, annual thyroglobulin antibodies at diagnosis. may be present in a substantial number of
routine follow-up is generally recom- (E) patients with features of type 2 diabetes
mended. Less frequent examinations ● Thyroid-stimulating hormone (TSH) (including obesity and acanthosis nigri-
may be acceptable on the advice of an concentrations should be measured af- cans). Such a distinction at the time of
eye care professional. (E) ter metabolic control has been estab- diagnosis is critical because treatment
lished. If normal, they should be regimens, educational approaches, and
Although retinopathy most commonly rechecked every 1–2 years or if the pa- dietary counsel will differ markedly be-
occurs after the onset of puberty and after tient develops symptoms of thyroid tween the two diagnoses.
5–10 years of diabetes duration, it has dysfunction, thyromegaly, or an abnor- Type 2 diabetes has a significant in-
been reported in prepubertal children mal growth rate. Free T4 should be cidence of comorbidities already
and with diabetes duration of only 1–2 measured if TSH is abnormal. (E) present at the time of diagnosis (334). It
years. Referrals should be made to eye is recommended that blood pressure
care professionals with expertise in dia- Autoimmune thyroid disease is the most measurement, a fasting lipid profile,
betic retinopathy, an understanding of common autoimmune disorder associ- microalbuminuria assessment, and di-
the risk for retinopathy in the pediatric ated with diabetes, occurring in 17–30% lated eye examination be performed at
population, and experience in counseling of patients with type 1 diabetes (330). The the time of diagnosis. Thereafter,
the pediatric patient and family on the presence of thyroid auto-antibodies is screening guidelines and treatment rec-
importance of early prevention/inter- predictive of thyroid dysfunction, gener-
ommendations for hypertension, dys-
vention. ally hypothyroidism and less commonly
lipidemia, microalbuminuria, and
hyperthyroidism (331). Subclinical hy-
retinopathy in youth with type 2 diabe-
v. Celiac disease pothyroidism may be associated with in-
creased risk of symptomatic tes are similar to those for youth with
Recommendations hypoglycemia (332) and with reduced type 1 diabetes. Additional problems
● Children with type 1 diabetes should be linear growth (333). Hyperthyroidism al- that may need to be addressed include
screened for celiac disease by measuring ters glucose metabolism, potentially re- polycystic ovary disease and the various
tissue transglutaminase or anti- sulting in deterioration of metabolic comorbidities associated with pediatric
endomysial antibodies, with documenta- control. obesity such as sleep apnea, hepatic ste-
tion of normal serum IgA levels, soon c. Self-management. No matter how atosis, orthopedic complications, and
after the diagnosis of diabetes. (E) sound the medical regimen, it can only be psychosocial concerns. The ADA con-
● Testing should be repeated if growth as good as the ability of the family and/or sensus statement on this subject (23)
failure, failure to gain weight, weight individual to implement it. Family in- provides guidance on the prevention,
loss, or gastroenterologic symptoms oc- volvement in diabetes remains an impor- screening, and treatment of type 2 dia-
cur. (E) tant component of optimal diabetes betes and its comorbidities in young
● Consideration should be given to peri- management throughout childhood and people.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S41
Standards of Medical Care
B. Preconception care 1.7% of infants) was much lower than the betic agents in the preconception period
incidence in women who did not partici- must be carefully weighed, recognizing
Recommendations pate (range 1.4 –10.9% of infants). One that data are insufficient to establish the
● A1C levels should be as close to normal limitation of these studies is that partici- safety of these agents in pregnancy.
as possible (⬍7%) in an individual pa- pation in preconception care was self- For further discussion of preconcep-
tient before conception is attempted. selected rather than randomized. Thus, it tion care, see the related ADA consensus
(B) is impossible to be certain that the lower statement (76) and position statement
● Starting at puberty, preconception malformation rates resulted fully from (341) on preexisting diabetes and
counseling should be incorporated in improved diabetes care. Nonetheless, the pregnancy.
the routine diabetes clinic visit for all evidence supports the concept that mal-
women of child-bearing potential. (C) formations can be reduced or prevented C. Older adults
● Women with diabetes who are contem- by careful management of diabetes before
plating pregnancy should be evaluated pregnancy. Recommendations
and, if indicated, treated for diabetic Planned pregnancies greatly facilitate ● Older adults who are functional, are
retinopathy, nephropathy, neuropathy, preconception diabetes care. Unfortu- cognitively intact, and have significant
and CVD. (E) nately, nearly two-thirds of pregnancies life expectancy should receive diabetes
● Medications used by such women in women with diabetes are unplanned, care using goals developed for younger
should be evaluated prior to concep- leading to a persistent excess of malfor- adults. (E)
tion because drugs commonly used to mations in infants of diabetic mothers. To ● Glycemic goals for older adults not
treat diabetes and its complications minimize the occurrence of these devas- meeting the above criteria may be re-
may be contraindicated or not recom- tating malformations, standard care for all laxed using individual criteria, but hy-
mended in pregnancy, including st- women with diabetes who have child- perglycemia leading to symptoms or
atins, ACE inhibitors, ARBs, and most bearing potential, beginning at the onset risk of acute hyperglycemic complica-
noninsulin therapies. (E) of puberty or at diagnosis, should include tions should be avoided in all patients.
1) education about the risk of malforma- (E)
Major congenital malformations remain tions associated with unplanned pregnan- ● Other cardiovascular risk factors
the leading cause of mortality and serious cies and poor metabolic control; and 2) should be treated in older adults with
morbidity in infants of mothers with type use of effective contraception at all times, consideration of the time frame of ben-
1 or type 2 diabetes. Observational stud- unless the patient has good metabolic efit and the individual patient. Treat-
ies indicate that the risk of malformations control and is actively trying to conceive. ment of hypertension is indicated in
increases continuously with increasing Women contemplating pregnancy virtually all older adults, and lipid and
maternal glycemia during the first 6 – 8 need to be seen frequently by a multidis- aspirin therapy may benefit those with
weeks of gestation, as defined by first- ciplinary team experienced in the man- life expectancy at least equal to the time
trimester A1C concentrations. There is no agement of diabetes before and during frame of primary or secondary preven-
threshold for A1C values below which pregnancy. The goals of preconception tion trials. (E)
risk disappears entirely. However, mal- care are to 1) involve and empower the ● Screening for diabetes complications
formation rates above the 1–2% back- patient in the management of her diabe- should be individualized in older
ground rate of nondiabetic pregnancies tes, 2) achieve the lowest A1C test results adults, but particular attention should
appear to be limited to pregnancies in possible without excessive hypoglycemia, be paid to complications that would
which first-trimester A1C concentrations 3) assure effective contraception until sta- lead to functional impairment. (E)
are ⬎1% above the normal range for a ble and acceptable glycemia is achieved,
nondiabetic pregnant woman. and 4) identify, evaluate, and treat long- Diabetes is an important health condition
Preconception care of diabetes ap- term diabetes complications such as reti- for the aging population; at least 20% of
pears to reduce the risk of congenital mal- nopathy, nephropathy, neuropathy, patients over the age of 65 years have di-
formations. Five nonrandomized studies hypertension, and CHD (76). abetes, and this number can be expected
compared rates of major malformations in Among the drugs commonly used in to grow rapidly in the coming decades.
infants between women who participated the treatment of patients with diabetes, a Older individuals with diabetes have
in preconception diabetes care programs number may be relatively or absolutely higher rates of premature death, func-
and women who initiated intensive diabe- contraindicated during pregnancy. St- tional disability, and coexisting illnesses
tes management after they were already atins are category X (contraindicated for such as hypertension, CHD, and stroke
pregnant. The preconception care pro- use in pregnancy) and should be discon- than those without diabetes. Older adults
grams were multidisciplinary and de- tinued before conception, as should ACE with diabetes are also at greater risk than
signed to train patients in diabetes self- inhibitors (340). ARBs are category C other older adults for several common ge-
management with diet, intensified insulin (risk cannot be ruled out) in the first tri- riatric syndromes, such as polypharmacy,
therapy, and SMBG. Goals were set to mester but category D (positive evidence depression, cognitive impairment, uri-
achieve normal blood glucose concentra- of risk) in later pregnancy and should nary incontinence, injurious falls, and
tions, and ⬎80% of subjects achieved generally be discontinued before preg- persistent pain.
normal A1C concentrations before they nancy. Among the oral antidiabetic The American Geriatric Society’s
became pregnant (335–339). In all five agents, metformin and acarbose are clas- guidelines for improving the care of the
studies, the incidence of major congenital sified as category B (no evidence of risk in older person with diabetes (342) have in-
malformations in women who partici- humans) and all others as category C. Po- fluenced the following discussion and
pated in preconception care (range 1.0 – tential risks and benefits of oral antidia- recommendations. The care of older
S42 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
adults with diabetes is complicated by adults whose life expectancies equal or agement of CFRD will be found in the
their clinical and functional heterogene- exceed the time frames seen in clinical consensus report to be published in 2010.
ity. Some older individuals developed di- trials.
abetes years earlier and may have Special care is required in prescribing VIII. DIABETES CARE IN
significant complications; others who are and monitoring pharmacologic therapy in SPECIFIC SETTINGS
newly diagnosed may have had years of older adults. Metformin is often contrain-
undiagnosed diabetes with resultant com- dicated because of renal insufficiency or Diabetes care in the hospital
plications or may have few complications significant heart failure. TZDs can cause
from the disease. Some older adults with fluid retention, which may exacerbate or Recommendations
diabetes are frail and have other underly- lead to heart failure. They are contraindi- ● All patients with diabetes admitted to
ing chronic conditions, substantial diabe- cated in patients with CHF (New York the hospital should have their diabetes
tes-related comorbidity, or limited Heart Association class III and IV), and if clearly identified in the medical record.
physical or cognitive functioning. Other used at all should be used very cautiously (E)
older individuals with diabetes have little in those with, or at risk for, milder degrees ● All patients with diabetes should have
comorbidity and are active. Life expectan- of CHF. Sulfonylureas, other insulin an order for blood glucose monitoring,
cies are highly variable for this population secretagogues, and insulin can cause hy- with results available to all members of
but often longer than clinicians realize. poglycemia. Insulin use requires that pa- the health care team. (E)
Providers caring for older adults with di- tients or caregivers have good visual and ● Goals for blood glucose levels
abetes must take this heterogeneity into motor skills and cognitive ability. Drugs ● Critically ill patients: Insulin therapy
consideration when setting and prioritiz- should be started at the lowest dose and should be initiated for treatment of
ing treatment goals. titrated up gradually until targets are persistent hyperglycemia starting at a
There are few long-term studies in reached or side effects develop. threshold of ⱕ180 mg/dl (10 mmol/
older adults that demonstrate the benefits Screening for diabetes complications l). Once insulin therapy is started, a
of intensive glycemic, blood pressure, and in older adults also should be individual- glucose range of 140 –180 mg/dl
lipid control. Patients who can be ex- ized. Particular attention should be paid (7.8 –10 mmol/l) is recommended
pected to live long enough to reap the to complications that can develop over for the majority of critically ill pa-
benefits of long-term intensive diabetes short periods of time and/or that would tients. (A) These patients require an
management and who are active, have significantly impair functional status, intravenous insulin protocol that has
good cognitive function, and are willing such as vision and lower-extremity demonstrated efficacy and safety in
should be provided with the needed edu- complications. achieving the desired glucose range
cation and skills to do so and be treated without increasing risk for severe hy-
using the goals for younger adults with poglycemia. (E)
diabetes. D. Cystic fibrosis–related diabetes ● Non– critically ill patients: There is
For patients with advanced diabetes Cystic fibrosis-related diabetes (CFRD) is no clear evidence for specific blood
complications, life-limiting comorbid ill- the most common comorbidity in people glucose goals. If treated with insulin,
ness, or substantial cognitive or func- with cystic fibrosis, occurring in ⬃20% of the premeal blood glucose target
tional impairment, it is reasonable to set adolescents and 40 –50% of adults. The should generally be ⬍140 mg/dl (7.8
less-intensive glycemic target goals. These additional diagnosis of diabetes in this mmol/l) with random blood glucose
patients are less likely to benefit from re- population is associated with worse nutri- ⬍180 mg/dl (10.0 mmol/l), provided
ducing the risk of microvascular compli- tional status, more severe inflammatory these targets can be safely achieved.
cations and more likely to suffer serious lung disease, and greater mortality from More stringent targets may be appro-
adverse effects from hypoglycemia. How- respiratory failure. For reasons that are priate in stable patients with previous
ever, patients with poorly controlled not well understood, women with CFRD tight glycemic control. Less stringent
diabetes may be subject to acute compli- are particularly vulnerable to excess mor- targets may be appropriate in those
cations of diabetes, including dehydra- bidity and mortality. Insulin insufficiency with severe comorbidites. (E)
tion, poor wound healing, and related to partial fibrotic destruction of ● Scheduled subcutaneous insulin with
hyperglycemic hyperosmolar coma. Gly- the islet mass is the primary defect in basal, nutritional, and correction com-
cemic goals at a minimum should avoid CFRD. Genetically determined function ponents is the preferred method for
these consequences. of the remaining -cells and insulin resis- achieving and maintaining glucose
Although control of hyperglycemia tance associated with infection and in- control in noncritically ill patients. (C)
may be important in older individuals flammation may also play a role. Using correction dose or “supplemen-
with diabetes, greater reductions in mor- Encouraging new data suggest that early tal” insulin to correct premeal hyper-
bidity and mortality may result from con- detection and aggressive insulin therapy glycemia in addition to scheduled
trol of other cardiovascular risk factors have narrowed the gap in mortality be- prandial and basal insulin is recom-
rather than from tight glycemic control tween cystic fibrosis patients with and mended. (E)
alone. There is strong evidence from clin- without diabetes and have eliminated the ● Glucose monitoring should be initiated
ical trials of the value of treating hyper- sex difference in mortality. in any patient not known to be diabetic
tension in the elderly (343,344). There is A consensus conference on CFRD who receives therapy associated with
less evidence for lipid-lowering and aspi- was cosponsored in 2009 by ADA, the high risk for hyperglycemia, including
rin therapy, although the benefits of these Cystic Fibrosis Foundation, and the Law- high-dose glucocorticoid therapy, initi-
interventions for primary and secondary son Wilkins Pediatric Endocrine Society. ation of enteral or parenteral nutrition,
prevention are likely to apply to older Recommendations for the clinical man- or other medications such as octreotide
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S43
Standards of Medical Care
or immunosuppressive medications. glycemia-provoking agents such as glu- of this study lie in stark contrast to a fa-
(B) If hyperglycemia is documented cocorticoids or vasopressors. mous 2001 single-center study that re-
and persistent, treatment is necessary. People with diabetes are more likely ported a 42% relative reduction in
Such patients should be treated to the to be hospitalized and to have longer intensive care unit (ICU) mortality in crit-
same glycemic goals as patients with lengths of stay than those without diabe- ically ill surgical patients treated to a tar-
known diabetes. (E) tes. A recent survey estimated that 22% of get blood glucose of 80 –110 mg/dl.
● A plan for treating hypoglycemia all hospital inpatient days were incurred Importantly, the control group in NICE-
should be established for each patient. by people with diabetes and that hospital SUGAR had reasonably good blood glu-
Episodes of hypoglycemia in the hospi- inpatient care accounted for one-half of cose management, maintained at a mean
tal should be tracked. (E) the $174 billion total U.S. medical expen- glucose of 144 mg/dl, only 29 mg/dl
● All patients with diabetes admitted to ditures for this disease (347). This is due, above the intensively managed patients.
the hospital should have an A1C ob- in part, to the continued expansion of the Accordingly, this study’s findings do not
tained if the result of testing in the pre- worldwide epidemic of type 2 diabetes. In disprove the notion that glycemic control
vious 2–3 months is not available. (E) the U.S. alone, there are ⬃1.6 million new in the ICU is important. However, they do
● Patients with hyperglycemia in the hos- cases of diabetes each year with an overall strongly suggest that it is not necessary to
pital who do not have a diagnosis of prevalence of 23.6 million people (7.8% target blood glucose values ⬍140 mg/dl
diabetes should have appropriate plans of the population, with one-quarter of and that a highly stringent target of ⬍110
for follow-up testing and care docu- cases remaining undiagnosed). An addi- mg/dl actually may be dangerous.
mented at discharge. (E) tional 57 million American adults are at In a recent meta-analysis of 26 trials
high risk for type 2 diabetes (348). While (N ⫽ 13,567), which included the NICE-
The subject of diabetes in the hospital is the costs of illness-related stress hypergly- SUGAR data, the pooled relative risk (RR)
extensively reviewed in an ADA technical cemia are not known, they are likely to be of death with intensive insulin therapy
review (345). A recent updated consensus significant given the poor prognosis of was 0.93 as compared with conventional
statement by the American Association of such patients (349 –352). therapy (95% CI 0.83–1.04) (358). Ap-
Clinical Endocrinologists (AACE) and the There is substantial observational ev- proximately half of these trials reported
ADA (346) form the basis for the discus- idence linking hyperglycemia in hospital- hypoglycemia, with a pooled RR of inten-
sion and guidelines in this section. ized patients (with or without diabetes) to sive therapy of 6.0 (95% CI 4.5– 8.0). The
The literature on hospitalized pa- poor outcomes. Cohort studies as well as specific ICU setting influenced the find-
tients with hyperglycemia typically de- a few early randomized controlled trials ings, with patients in surgical ICUs ap-
scribes three categories: (RCTs) suggested that intensive treatment pearing to benefit from intensive insulin
of hyperglycemia improved hospital out- therapy (RR 0.63 [95% CI 0.44 – 0.91]),
● Medical history of diabetes: diabetes pre- comes (345,351,352). Interventions to while those in other critical care settings
viously diagnosed and acknowledged by normalize glycemia, however, have had did not (medical ICU: 1.0 [0.78 –1.28];
the patient’s treating physician. inconsistent results. Indeed, recent trials “mixed” ICU: 0.99 [0.86 –1.12]). It was
● Unrecognized diabetes: hyperglycemia in critically ill patients have failed to show concluded that overall, intensive insulin
(fasting blood glucose ⱖ126 mg/dl or a significant improvement in mortality therapy increased the risk of hypoglyce-
random blood glucose ⱖ200 mg/dl) with intensive glycemic control mia but provided no overall benefit on
occurring during hospitalization and (353,354) or have even shown increased mortality in the critically ill, although a
confirmed as diabetes after hospitaliza- mortality risk (355). Moreover, these re- benefit to patients admitted to the surgical
tion by standard diagnostic criteria but cent RCTs have highlighted the risk of se- ICU was suggested.
unrecognized as diabetes by the treat- vere hypoglycemia resulting from such It is very clear that the management of
ing physician during hospitalization. efforts (353–358). hyperglycemia in the hospital presents
● Hospital-related hyperglycemia: hyper- The largest study to date, NICE- unique challenges that stem from varia-
glycemia (fasting blood glucose ⱖ126 SUGAR, a multicenter, multinational tions in a patient’s nutritional status and
mg/dl or random blood glucose ⱖ200 RCT, tested the effect of tight glycemic level of consciousness, the practical limi-
mg/dl) occurring during the hospital- control (target 81–108 mg/dl) on out- tations of intermittent glycemic monitor-
ization that reverts to normal after hos- comes among 6,104 critically ill partici- ing, and the ultimate importance of
pital discharge. pants, the majority of whom (⬎95%) patient safety. Accordingly, reasonable
required mechanical ventilation (355). glucose targets in the hospital setting are
The management of hyperglycemia in the Ninety-day mortality was significantly modestly higher than may be routinely
hospital has logically been considered higher in the intensive versus the conven- advised in patients with diabetes in the
secondary in importance to the condition tional group (target 144 –180 mg/dl) (78 outpatient setting. The following recom-
that prompted admission (345). How- more deaths; 27.5 vs. 24.9%, P ⫽ 0.02) in mendations represent a synthesis of the
ever, a body of literature now supports both surgical and medical patients. Mor- evidence base over the past decade and
targeted glucose control in the hospital tality from cardiovascular causes was are somewhat less stringent than prior
setting for potential improved clinical more common in the intensive group (76 recommendations of the ADA Standards
outcomes. Hyperglycemia in the hospital more deaths; 41.6 vs. 35.8%; P ⫽ 0.02). of Medical Care in Diabetes. For a com-
may result from stress; decompensation Severe hypoglycemia was also more com- prehensive review of these data, the
of type 1, type 2, or other forms of dia- mon in the intensively treated group (6.8 reader is referred to the latest consensus
betes; and/or may be iatrogenic due to vs. 0.5%; P ⬍ 0.001). The precise reason statement from AACE and ADA on inpa-
withholding of antihyperglycemic for the increased mortality in the tightly tient management of hyperglycemia
medications or administration of hyper- controlled group is unknown. The results (346).
S44 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
1. Glycemic targets in hospitalized with random blood glucose ⬍180 mg/dl Continued education of staff with peri-
patients (10.0 mmol/l), as long as these targets can odic ongoing review of patient data are
a. Definition of glucose abnormalities in be safely achieved. To avoid hypoglyce- critical for successful implementation of
the hospital setting. Hyperglycemia has mia, consideration should be given to re- any insulin protocol (364 –366).
been defined as any blood glucose ⬎140 assessing the insulin regimen if blood Patients who receive intravenous in-
mg/dl (7.8 mmol/l). Levels that are signif- glucose levels fall below 100 mg/dl (5.6 sulin infusion will usually require transi-
icantly and persistently above this may re- mmol/l). Modification of the regimen is tion to subcutaneous insulin when they
quire treatment in hospitalized patients. required when blood glucose values are begin eating regular meals or are trans-
In patients without a previous diagnosis ⬍70 mg/dl (3.9 mmol/l), unless the event ferred to lower intensity care. Typically, a
of diabetes, elevated blood glucose may is easily explained by other factors (such percentage (usually 75– 80%) of the total
be due to “stress hyperglycemia,” a condi- as a missed meal, etc.). daily intravenous infusion dose is propor-
tion that can be established by a review of Occasional patients with a prior his- tionately divided into basal and prandial
prior records or measurement of an A1C. tory of successful tight glycemic control in components (see below). Importantly,
A1C values ⬎6.5% suggest that diabetes the outpatient setting who are clinically subcutaneous insulin must be given 1– 4
preceded hospitalization (359). Hypogly- stable may be maintained with a glucose h prior to discontinuation of intravenous
cemia has been defined as any blood glu- range below the above cut points. Con- insulin to prevent hyperglycemia (367).
cose ⬍70 mg/dl (3.9 mmol/l). This is the versely, higher glucose ranges may be ac- b. Subcutaneous insulin. Scheduled
standard definition in outpatients and ceptable in terminally ill patients or in subcutaneous insulin is the preferred
correlates with the initial threshold for the patients with severe comorbidities, as method for achieving and maintaining
release of counterregulatory hormones well as in those in patient-care settings glucose control in non-ICU patients with
(177). Severe hypoglycemia in hospital- where frequent glucose monitoring or diabetes or stress hyperglycemia. The rec-
ized patients has been defined by many close nursing supervision is not feasible. ommended components of inpatient sub-
as ⬍40 mg/dl (2.2 mmol/l), although Clinical judgment, combined with cutaneous insulin regimens include a
this is lower than the ⬃50 mg/dl (2.8 ongoing assessment of the patient’s clini- basal, nutritional, and supplemental (cor-
mmol/l) level at which cognitive impair- cal status, including changes in the trajec- rection) component (345,346,368). Each
ment begins in normal individuals tory of glucose measures, severity of component can be met by one of several
(177,360,361). As with hyperglycemia, illness, nutritional status, or concurrent available insulin products, depending on
hypoglycemia among inpatients is also as- use of medications that might affect glu-
the particular hospital situation. The
sociated with adverse short- and long- cose levels (e.g., steroids, octreotide)
reader is referred to several recent publi-
term outcomes. Early recognition and must be incorporated into the day-to-day
cations and reviews that describe cur-
treatment of mild to moderate hypoglyce- decisions regarding insulin dosing (363).
rently available insulin preparations and
mia (40 and 69 mg/dl [2.2 and 3.8 mmol/
protocols (366 –370).
l]) can prevent deterioration to a more 2. Treatment options in hospitalized
A topic that deserves particular atten-
severe episode with potential adverse se- patients
quelae (361,362). In the hospital setting, insulin therapy is tion is the persistent overuse of what has
i. Critically ill patients. Based on the the preferred method of glycemic control been branded as sliding scale insulin (SSI)
weight of the available evidence, for the in majority of clinical situations (346). In for management of hyperglycemia. The
majority of critically ill patients in the ICU the ICU, intravenous infusion is the pre- term “correction insulin,” which refers to
setting, insulin infusion should be used to ferred route of insulin administration. the use of additional short or rapid-acting
control hyperglycemia, with a starting Outside of critical care units, subcutane- insulin with scheduled insulin doses to
threshold of ⱕ180 mg/dl (10.0 mmol/l). ous insulin is used much more frequently. treat blood glucose above desired targets,
Once intravenous insulin is started, the Oral agents have a limited role in the in- is preferred (345). Prolonged therapy
glucose level should be maintained be- patient setting. with SSI as the sole regimen is ineffective
tween 140 and 180 mg/dl (7.8 and 10.0 a. Intravenous insulin infusions. In the in the majority of patients (and potentially
mmol/l). Greater benefit may be realized critical care setting, continuous intrave- dangerous in type 1 diabetes) (370 –375).
at the lower end of this range. Although nous insulin infusion has been shown to c. Noninsulin agents. These agents are
strong evidence is lacking, somewhat be the most effective method for achiev- inappropriate in the majority of hospital-
lower glucose targets may be appropriate ing specific glycemic targets (346). Be- ized patients because they are less titrat-
in selected patients. However, targets cause of the very short half-life of able than insulin in the short tem and are
⬍110 mg/dl (6.1 mmol/l) are not recom- circulating insulin, intravenous delivery meant to be used in patients eating on a
mended. Use of insulin infusion protocols allows rapid dosing adjustments to ad- regular meal schedule. Continuation of
with demonstrated safety and efficacy, re- dress alterations in patients’ status. these agents may be appropriate in se-
sulting in low rates of hypoglycemia, are Intravenous insulin is ideally admin- lected stable patients who are expected to
highly recommended. istered via validated written or computer- consume meals at regular intervals. Spe-
ii. Noncritically ill patients. With no pro- ized protocols that allow for predefined cific caution is required with metformin,
spective, RCT data to inform specific gly- adjustments to the insulin infusion rate due to the possibility that a contraindica-
cemic targets in noncritically ill patients, according to glycemic fluctuations and in- tion may develop during the hospitaliza-
recommendations are based on clinical sulin dose. An extensive review of the tion, such as renal insufficiency, unstable
experience and judgment. For the major- merits and deficiencies of published pro- hemodynamic status, or need for an im-
ity of noncritically ill patients treated with tocols is beyond the intent of this state- aging study that requires a radio-contrast
insulin, premeal glucose targets should ment, and the reader is referred to several dye (345,376). Injectable noninsulin
generally be ⬍140 mg/dl (7.8 mmol/l) available reports and reviews (364 –366). therapies such as exenatide and pramlint-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S45
Standards of Medical Care
ide have limitations similar to those of heart failure, renal or liver disease, malig- conducting self-management in the hos-
oral agents in the hospital setting. nancy, infection, or sepsis (379,379,380). pital, it is imperative that basal, prandial,
d. Specific clinical situations Additional triggering events leading to and correction doses of insulin and results
i. Insulin pumps. Patients who use CSII iatrogenic hypoglycemia include sudden of bedside glucose monitoring be re-
pump therapy in the outpatient setting reduction of corticosteroid dose, altered corded as part of the patient’s hospital
can be candidates for diabetes self- ability of the patient to self-report symp- medical record. While many institutions
management in the hospital, provided toms, reduction of oral intake, emesis, allow patients on insulin pumps to con-
that they have the mental and physical new NPO status, inappropriate timing of tinue these devices in the hospital, others
capacity to do so (346,368). It is impor- short- or rapid-acting insulin in relation express concern regarding use of a device
tant that nursing personnel document to meals, reduction of rate of administra- unfamiliar to staff, particularly in patients
basal rates and bolus doses on a regular tion of intravenous dextrose, and unex- who are not able to manage their own
basis (at least daily). The availability of pected interruption of enteral feedings or pump therapy. If a patient is too ill to
hospital personnel with expertise in CSII parenteral nutrition. self-manage either multiple daily injec-
therapy is essential. Despite the preventable nature of tions or CSII, then appropriate subcuta-
ii. Enteral nutrition. Hyperglycemia is a many inpatient episodes of hypoglyce- neous doses can be calculated on the basis
common side effect of inpatient enteral mia, institutions are more likely to have of their basal and bolus insulin needs dur-
nutrition therapy (377). A recent report nursing protocols for the treatment of hy- ing hospitalization, with adjustments for
using a combination of basal insulin with poglycemia than for its prevention. changes in nutritional or metabolic status.
correction insulin achieved a mean glu- Tracking such episodes and analyzing
cose value of 160 mg/dl (8.9 mmol/l). their causes are important quality im- 5. DSME in the hospital
Similar results were achieved in the group provement activities. Teaching diabetes self-management to
randomized to receive SSI alone; how- patients in hospitals is a challenging task.
ever, 48% of patients required the addi- 3. Diabetes care providers in the Patients are ill, under increased stress re-
tion of intermediate-acting insulin to hospital lated to their hospitalization and diagno-
achieve glycemic targets (373). Inpatient diabetes management may be sis, and in an environment not conducive
iii. Parenteral nutrition. The high glu- effectively provided by primary care phy- to learning. Ideally, people with diabetes
cose load in standard parenteral nutrition sicians, endocrinologists, or hospitalists. should be taught at a time and place con-
frequently results in hyperglycemia, Involvement of appropriately trained spe- ducive to learning—as an outpatient in
which is associated with a higher inci- cialists or specialty teams may reduce a recognized program of diabetes
dence of complications and mortality in length of stay, improve glycemic control, education.
critically ill ICU patients (378). Insulin and improve outcomes (381–384). In the For the hospitalized patient, diabetes
therapy is highly recommended, with glu- care of diabetes, implementation of stan- “survival skills” education is generally a
cose targets as defined previously by se- dardized order sets for scheduled and cor- feasible approach. Patients and/or family
verity of illness. rection-dose insulin may reduce reliance members receive sufficient information
iv. Glucocorticoid therapy. Hyperglyce- on sliding-scale management. A team ap- and training to enable safe care at home.
mia is a common complication of cortico- proach is needed to establish hospital Those newly diagnosed with diabetes or
steroid therapy (363). Several approaches pathways. To achieve glycemic targets who are new to insulin and/or blood glu-
have been proposed for treatment of this associated with improved hospital out- cose monitoring need to be instructed
condition, but there are no published comes, hospitals will need multidisci- before discharge. Those patients hospital-
protocols or studies that investigate the plinary support to develop protocols for ized because of a crisis related to diabetes
efficacy of these approaches. A reasonable subcutaneous insulin therapy that effec- management or poor care at home need
approach is to institute glucose monitor- tively and safely achieve glycemic targets education to prevent subsequent episodes
ing for at least 48 h in all patients receiv- (385). of hospitalization. An assessment of the
ing high dose glucocorticoid therapy and need for a home health referral or referral
initiate insulin as appropriate. In patients 4. Self-management in the hospital to an outpatient diabetes education pro-
who are already being treated for hyper- Self-management of diabetes in the hos- gram should be part of discharge plan-
glycemia, early adjustment of insulin pital may be appropriate for competent ning for all patients.
doses is recommended. Importantly, dur- adult patients who have a stable level of
ing steroid tapers, insulin dosing should consciousness, have reasonably stable 6. MNT in the hospital
be proactively adjusted to avoid daily insulin requirements, successfully Hospital diets continue to be ordered by
hypoglycemia. conduct self-management of diabetes at calorie levels based on the “ADA diet.”
v. Hypoglycemia prevention. Hypogly- home, have physical skills needed to suc- However, since 1994 the ADA has not en-
cemia, especially in insulin-treated pa- cessfully self-administer insulin and per- dorsed any single meal plan or specified
tients, is the leading limiting factor in the form SMBG, have adequate oral intake, percentages of macronutrients, and the
glycemic management of type 1 and type and are proficient in carbohydrate count- term “ADA diet” should no longer be
2 diabetes (174). In the hospital, multiple ing, use of multiple daily insulin injec- used. Current nutrition recommenda-
additional risk factors for hypoglycemia tions, or insulin pump therapy and sick- tions advise individualization based on
are present, even among patients who are day management. The patient and treatment goals, physiologic parameters,
neither “brittle” nor tightly controlled. Pa- physician, in consultation with nursing and medication usage. Because of the
tients with or without diabetes may expe- staff, must agree that patient self- complexity of nutrition issues in the hos-
rience hypoglycemia in the hospital in management is appropriate under the pital, a registered dietitian, knowledge-
association with altered nutritional state, conditions of hospitalization. For patients able and skilled in MNT, should serve as
S46 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
an inpatient team member. The dietitian limited by the lack of reliability in the hy- IX. STRATEGIES FOR
is responsible for integrating information poglycemic range as well as by cost. IMPROVING DIABETES
about the patient’s clinical condition, eat- CARE — The implementation of the
ing, and lifestyle habits and for establish- 8. Discharge planning standards of care for diabetes has been
ing treatment goals in order to determine It is important to anticipate the postdis- suboptimal in most clinical settings. A re-
a realistic plan for nutrition therapy charge antihyperglycemic regimen in all cent report (393) indicated that only
(386,387). patients with diabetes or newly discov- 57.1% of adults with diagnosed diabetes
ered hyperglycemia. The optimal pro- achieved an A1C of ⬍7%, only 45.5%
gram will need to consider the type and had a blood pressure ⬍130/80 mmHg,
7. Bedside blood glucose monitoring severity of diabetes, the effects of the and just 46.5% had a total cholesterol
Bedside blood glucose monitoring using patient’s illness on blood glucose levels, ⬍200 mg/dl. Most distressing was that
point-of-care glucose meters is performed and the capacities and desires of the pa- only 12.2% of people with diabetes
before meals and bedtime in the majority tient. Smooth transition to outpatient achieved all three treatment goals.
of inpatients who are eating usual meals. care should be ensured, especially in While numerous interventions to im-
In patients who are receiving continuous those new to insulin therapy or in prove adherence to the recommended
enteral or parenteral nutrition, glucose whom the diabetes regimen has been standards have been implemented, the
monitoring is optimally performed every substantially altered during the hospi- challenge of providing uniformly effective
4 – 6 h. In patients who are receiving cy- talization. All patients in whom the di- diabetes care has thus far defied a simple
cled enteral or parenteral nutrition, the agnosis of diabetes is new should have, solution. A major contributor to subopti-
schedule for glucose monitoring can be at minimum, “survival skills” training mal care is a delivery system that too often
individualized but should be frequent prior to discharge. is fragmented, lacks clinical information
enough to detect hyperglycemia during It is recommended that the following capabilities, often duplicates services, and
feedings and risk of hypoglycemia when areas be reviewed and addressed prior to is poorly designed for the delivery of
feedings are interrupted (374,376). More hospital discharge: chronic care. The chronic care model
frequent blood glucose testing ranging from (CCM) includes five core elements for the
every 30 min to every 2 h is required for ● level of understanding related to the di- provision of optimal care of patients with
patients on intravenous insulin infusions. agnosis of diabetes chronic disease: delivery system design,
Safe and rational glycemic manage- ● SMBG and explanation of home blood self-management support, decision sup-
ment relies on the accuracy of blood glu- glucose goals port, clinical information systems, and
cose measurements using point-of-care ● definition, recognition, treatment, and community resources and policies. Redef-
blood glucose meters, which have several prevention of hyperglycemia and inition of the roles of the clinic staff and
important limitations. Although the FDA hypoglycemia promoting self-management on the part
allows a ⫾20% error for glucose meters, ● identification of health care provider of the patient are fundamental to the suc-
questions about the appropriateness of who will provide diabetes care after cessful implementation of the CCM
this criterion have been raised (388). Glu- discharge (394). Collaborative, multidisciplinary
cose measures differ significantly between ● information on consistent eating teams are best suited to provide such care
plasma and whole blood, terms which are patterns for people with chronic conditions like
often used interchangeably and can lead ● when and how to take blood glucose– diabetes and to empower patients’ perfor-
to misinterpretation. Most commercially lowering medications including insulin mance of appropriate self-management.
available capillary glucose meters intro- administration (if going home on Alterations in reimbursement that reward
duce a correction factor of ⬃1.12 to re- insulin) the provision of quality care, as defined by
port a “plasma-adjusted” value (389). ● sick-day management the attainment of quality measures devel-
Significant discrepancies between ● proper use and disposal of needles and oped by such programs as the ADA/
capillary, venous, and arterial plasma syringes National Committee for Quality
samples have been observed in patients Assurance Diabetes Provider Recognition
with low or high hemoglobin concentra- More expanded diabetes education can Program, will also be required to achieve
tions, hypoperfusion, and the presence of be arranged in the community. An out- desired outcome goals.
interfering substances (389,390). Analyt- patient follow-up visit with the primary In recent years, numerous health care
ical variability has been described with care provider, endocrinologist, or diabe- organizations, ranging from large health
several point-of-care meters (391). Any tes educator within 1 month of discharge care systems such as the U.S. Veteran’s
glucose result that does not correlate with is advised for all patients having hypergly- Administration to small private practices,
the patient’s status should be confirmed cemia in the hospital. Clear communica- have implemented strategies to improve
through conventional laboratory sam- tion with outpatient providers either diabetes care. Successful programs have
pling of PG. directly or via hospital discharge summa- published results showing improvement
While laboratory measurement of PG ries facilitates safe transitions to outpa- in process measures such as measurement
has less variability and interference, mul- tient care. Providing information of A1C, lipids, and blood pressure. Effects
tiple daily phlebotomies are not practical. regarding the cause or the plan for deter- on in important intermediate outcomes,
The use of indwelling lines as the sam- mining the cause of hyperglycemia, re- such as mean A1C for populations, have
pling source also poses risks for infection. lated complications and comorbidities, been more difficult to demonstrate (395–
Studies performed using continuous in- and recommended treatments can assist 397), although examples do exist (398 –
terstitial glucose monitoring systems in outpatient providers as they assume on- 402), often taking more than 1 year to
the critical care setting (392) currently are going care. manifest (394). Features of successful
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S47
Standards of Medical Care
programs reported in the literature tion. When practices are compared, those betes Association and 1999 World
include that address more of the CCM elements Health Organization criteria for hyper-
demonstrate lower A1C levels and lower glycemia in the diagnosis and prediction
● Delivery of DSME: increases adherence cardiovascular risk scores (408). The of diabetes. Diabetes Care 2000;23:
1108 –1112
to standard of care and educating pa- most successful practices have an institu-
11. Knowler WC, Barrett-Connor E, Fowler
tients on glycemic targets and improves tional priority for quality of care, involve SE, Hamman RF, Lachin JM, Walker EA,
the percentage of patients who reach all of the staff in their initiatives, redesign Nathan DM, Diabetes Prevention Pro-
goal A1C (142,403) their delivery system, activate and edu- gram Research Group. Reduction in the
● Adoption of practice guidelines, with cate their patients, and use electronic incidence of type 2 diabetes with lifestyle
participation of health care profession- health record tools (409,410). intervention or metformin. N Engl J Med
als in the process of development: NDEP maintains an online resource 2002;346:393– 403
Guidelines should be readily accessible (www.betterdiabetescare.nih.gov) to help 12. Tuomilehto J, Lindström J, Eriksson JG,
at the point of service, preferably as health care professionals design and im- Valle TT, Hämäläinen H, Ilanne-Parikka
computerized reminders at the point of plement more effective health care deliv- P, Keinänen-Kiukaanniemi S, Laakso M,
care. Guidelines should begin with a ery systems for those with diabetes. Louheranta A, Rastas M, Salminen V,
Uusitupa M, Finnish Diabetes Preven-
summary of their major recommenda- It is clear that optimal diabetes man- tion Study Group. Prevention of type 2
tions instructing health care profes- agement requires an organized, system- diabetes mellitus by changes in lifestyle
sionals what to do and how to do it. atic approach and involvement of a among subjects with impaired glucose
● Use of checklists that mirror guidelines: coordinated team of dedicated health care tolerance. N Engl J Med 2001;344:
successful at improving adherence to professionals working in an environment 1343–1350
standards of care where quality care is a priority. 13. Pan XR, Li GW, Hu YH, Wang JX, Yang
● Systems changes: such as provision of WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao
automated reminders to health care HB, Liu PA, Jiang XG, Jiang YY, Wang JP,
professionals and patients and audit References Zheng H, Zhang H, Bennett PH, Howard
and feedback of process and outcome 1. American Diabetes Asociation. Medical BV. Effects of diet and exercise in pre-
Management of Type 1 Diabetes. Alexan- venting NIDDM in people with impaired
data to providers glucose tolerance. The Da Qing IGT and
●
dria, VA, American Diabetes Associa-
Quality improvement programs com- tion, 2008 Diabetes Study. Diabetes Care 1997;20:
bining continuous quality improve- 2. American Diabetes Asociation. Medical 537–544
ment or other cycles of analysis and Management of Type 2 Diabetes. Alexan- 14. Buchanan TA, Xiang AH, Peters RK, Kjos
intervention with provider perfor- dria, VA, American Diabetes Associa- SL, Marroquin A, Goico J, Ochoa C, Tan
mance data tion, 2008 S, Berkowitz K, Hodis HN, Azen SP.
● Practice changes: such as availability of 3. American Diabetes Association. Intensive Preservation of pancreatic beta-cell
point of care testing of A1C, scheduling Diabetes Management. Alexandria, VA, function and prevention of type 2 diabe-
planned diabetes visits, clustering of American Diabetes Association, 2009 tes by pharmacological treatment of in-
dedicated diabetes visits into specific 4. Expert Committee on the Diagnosis and sulin resistance in high-risk hispanic
Classification of Diabetes Mellitus. Re- women. Diabetes 2002;51:2796 –2803
times within a primary care practice
port of the Expert Committee on the Di- 15. Chiasson JL, Josse RG, Gomis R,
schedule, or group visits and/or visits agnosis and Classification of Diabetes Hanefeld M, Karasik A, Laakso M,
with multiple health care professionals Mellitus. Diabetes Care 1997;20:1183– STOP-NIDDM Trail Research Group.
on a single day 1197 Acarbose for prevention of type 2 diabe-
● Tracking systems with either an elec- 5. International Expert Committee. Inter- tes mellitus: the STOP-NIDDM random-
tronic medical record or patient regis- national Expert Committee report on the ised trial. Lancet 2002;359:2072–2077
try: helpful at increasing adherence to role of the A1C assay in the diagnosis of 16. DREAM (Diabetes REduction Assess-
standards of care by prospectively iden- diabetes. Diabetes Care 2009;32:1327– ment with ramipril and rosiglitazone
tifying those requiring assessments 1334 Medication) Trial Investigators, Gerstein
and/or treatment modifications. They 6. American Diabetes Association. Diagno- HC, Yusuf S, Bosch J, Pogue J, Sheridan
likely could have greater efficacy if they sis and classification of diabetes mellitus. P, Dinccag N, Hanefeld M, Hoogwerf B,
Diabetes Care 2010;33(Suppl. 1):S62– Laakso M, Mohan V, Shaw J, Zinman B,
suggested specific therapeutic interven- S69 Holman RR. Effect of rosiglitazone on
tions to be considered for a particular 7. Genuth S, Alberti KG, Bennett P, Buse J, the frequency of diabetes in patients
patient at a particular point in time Defronzo R, Kahn R, Kitzmiller J, with impaired glucose tolerance or im-
(404). Knowler WC, Lebovitz H, Lernmark A, paired fasting glucose: a randomised
● Availability of case or (preferably) care Nathan D, Palmer J, Rizza R, Saudek C, controlled trial. Lancet 2006;368:1096 –
management services (405): Nurses, Shaw J, Steffes M, Stern M, Tuomilehto J, 1105
pharmacists, and other nonphysician Zimmet P, Expert Committee on the Di- 17. Ramachandran A, Snehalatha C, Mary S,
health care professionals using detailed agnosis and Classification of Diabetes Mukesh B, Bhaskar AD, Vijay V, Indian
algorithms working under the supervi- Mellitus. Follow-up report on the diag- Diabetes Prevention Programme (IDPP).
sion of physicians have demonstrated nosis of diabetes mellitus. Diabetes Care The Indian Diabetes Prevention Pro-
2003;26:3160 –3167 gramme shows that lifestyle modifica-
the greatest reduction in A1C and 9. Engelgau MM, Narayan KM, Herman tion and metformin prevent type 2
blood pressure (406,407). WH. Screening for type 2 diabetes. Dia- diabetes in Asian Indian subjects with
betes Care 2000;23:1563–1580 impaired glucose tolerance (IDPP-1).
Evidence suggests that these individual 10. Gabir MM, Hanson RL, Dabelea D, Im- Diabetologia 2006;49:289 –297
initiatives work best when provided as peratore G, Roumain J, Bennett PH, 18. Johnson SL, Tabaei BP, Herman WH.
components of a multifactorial interven- Knowler WC. The 1997 American Dia- The efficacy and cost of alternative strat-
S48 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
egies for systematic screening for type 2 28. Kim C, Newton KM, Knopp RH. Gesta- 38. American Diabetes Association: Self-
diabetes in the U.S. population 45–74 tional diabetes and the incidence of type monitoring of blood glucose. Diabetes
years of age. Diabetes Care 2005;28: 2 diabetes: a systematic review. Diabetes Care 1994;17:81– 86
307–311 Care 2002;25:1862–1868 39. Welschen LM, Bloemendal E, Nijpels G,
19. Harris R, Donahue K, Rathore SS, Frame 29. Lindström J, Ilanne-Parikka P, Peltonen Dekker JM, Heine RJ, Stalman WA,
P, Woolf SH, Lohr KN. Screening adults M, Aunola S, Eriksson JG, Hemiö K, Hä- Bouter LM. Self-monitoring of blood
for type 2 diabetes: a review of the evi- mäläinen H, Härkönen P, Keinänen- glucose in patients with type 2 diabetes
dence for the U.S. Preventive Services Kiukaanniemi S, Laakso M, Louheranta who are not using insulin: a systematic
Task Force. Ann Intern Med 2003;138: A, Mannelin M, Paturi M, Sundvall J, review. Diabetes Care 2005;28:1510 –
215–229 Valle TT, Uusitupa M, Tuomilehto J, 1517
20. U.S. Preventive Services Task Force. S. Finnish Diabetes Prevention Study 40. Farmer A, Wade A, Goyder E, Yudkin
Preventive Services Task Force. S. Pre- Group. Sustained reduction in the inci- P, French D, Craven A, Holman R,
ventive Services Task Force: Screening dence of type 2 diabetes by lifestyle in- Kinmonth AL, Neil A. Impact of self
for type 2 diabetes mellitus in adults: tervention: follow-up of the Finnish monitoring of blood glucose in the man-
recommendations and rationale. Ann Diabetes Prevention Study. Lancet 2006; agement of patients with non-insulin
Intern Med 2003;138:212–214 368:1673–1679 treated diabetes: open parallel group
21. Writing Group for the SEARCH for Dia- 30. Li G, Zhang P, Wang J, Gregg EW, Yang randomised trial. BMJ 2007;335:132
betes in Youth Study Group, Dabelea D, W, Gong Q, Li H, Li H, Jiang Y, An Y, 41. O’Kane MJ, Bunting B, Copeland M,
Bell RA, D’Agostino RB Jr, Imperatore G, Shuai Y, Zhang B, Zhang J, Thompson Coates VE, ESMON study group. Effi-
Johansen JM, Linder B, Liu LL, Loots B, TJ, Gerzoff RB, Roglic G, Hu Y, Bennett cacy of self monitoring of blood glucose
Marcovina S, Mayer-Davis EJ, Pettitt DJ, PH. The long-term effect of lifestyle in- in patients with newly diagnosed type 2
Waitzfelder B. Incidence of diabetes in terventions to prevent diabetes in the diabetes (ESMON study): randomised
youth in the United States. JAMA 2007; China Da Qing Diabetes Prevention controlled trial. BMJ 2008;336:1174 –
297:2716 –2724 Study: a 20-year follow-up study. Lancet 1177
22. SEARCH for Diabetes in Youth Study 2008;371:1783–1789 42. Simon J, Gray A, Clarke P, Wade A, Neil
Group, Liese AD, D’Agostino RB Jr, 31. Kosaka K, Noda M, Kuzuya T. Preven- A, Farmer A, Diabetes Glycaemic Educa-
Hamman RF, Kilgo PD, Lawrence JM, tion of type 2 diabetes by lifestyle inter- tion and Monitoring Trial Group. Cost
Liu LL, Loots B, Linder B, Marcovina S, vention: a Japanese trial in IGT males. effectiveness of self monitoring of blood
Rodriguez B, Standiford D, Williams DE. Diabetes Res Clin Pract 2005;67:152– glucose in patients with non-insulin
The burden of diabetes mellitus among 162 treated type 2 diabetes: economic evalu-
US youth: prevalence estimates from the 32. Torgerson JS, Hauptman J, Boldrin MN, ation of data from the DiGEM trial. BMJ
SEARCH for Diabetes in Youth Study. Sjöström L. XENical in the prevention of 2008;336:1177–1180
Pediatrics 2006;118:1510 –1518 diabetes in obese subjects (XENDOS) 43. Sacks DB, Bruns DE, Goldstein DE, Ma-
23. American Diabetes Association: Type 2 study: a randomized study of orlistat as claren NK, McDonald JM, Parrott M.
diabetes in children and adolescents an adjunct to lifestyle changes for the Guidelines and recommendations for
(Consensus Statement). Diabetes Care prevention of type 2 diabetes in obese laboratory analysis in the diagnosis and
2000;23:381–389 patients. Diabetes Care 2004;27:155– management of diabetes mellitus. Clin
24. Lawrence JM, Contreras R, Chen W, 161 Chem 2002;48:436 – 472
Sacks DA. Trends in the prevalence of 33. Kawamori R, Tajima N, Iwamoto Y, 44. Juvenile Diabetes Research Foundation
preexisting diabetes and gestational dia- Kashiwagi A, Shimamoto K, Kaku K, Continuous Glucose Monitoring Study
betes mellitus among a racially/ethni- Voglibose Ph-3 Study Group. Voglib- Group, Tamborlane WV, Beck RW,
cally diverse population of pregnant ose for prevention of type 2 diabetes Bode BW, Buckingham B, Chase HP,
women, 1999 –2005. Diabetes Care mellitus: a randomised, double-blind Clemons R, Fiallo-Scharer R, Fox LA,
2008;31:899 –904 trial in Japanese individuals with im- Gilliam LK, Hirsch IB, Huang ES, Koll-
25. American Diabetes Association: Gesta- paired glucose tolerance. Lancet 2009; man C, Kowalski AJ, Laffel L, Lawrence
tional diabetes mellitus (Position State- 373:1607–1614 JM, Lee J, Mauras N, O’Grady M, Ruedy
ment). Diabetes Care 2004;27(Suppl. 34. DeFronzo RA, for ACT NOW Study KJ, Tansey M, Tsalikian E, Weinzimer S,
1):S88 –S90 Group. ACTos NOW Study for the Pre- Wilson DM, Wolpert H, Wysocki T,
26. HAPO Study Cooperative Research vention of Diabetes (ACT NOW) Study. Xing D: Continuous glucose monitoring
Group, Metzger BE, Lowe LP, Dyer AR, Late-breaking abstract presented at 68th and intensive treatment of type 1 diabe-
Trimble ER, Chaovarindr U, Coustan Annual Scientific Sessions of the Ameri- tes. N Engl J Med 2008; 359:1464 –1476
DR, Hadden DR, McCance DR, Hod M, can Diabetes Association, 6 June 2008, 45. Juvenile Diabetes Research Foundation
McIntyre HD, Oats JJ, Persson B, Rogers San Francisco, CA Continuous Glucose Monitoring Study
MS, Sacks DA. Hyperglycemia and ad- 35. Gerstein HC. Point: If it is important to Group: The effect of continuous glucose
verse pregnancy outcomes. N Engl J Med prevent type 2 diabetes, it is important to monitoring in well-controlled type 1 di-
2008;358:1991–2002 consider all proven therapies within a abetes. Diabetes Care 2009;32:1378 –
27. Landon MB, Spong CY, Thom E, Car- comprehensive approach. Diabetes Care 1383
penter MW, Ramin SM, Casey B, Wap- 2007;30:432– 434 46. Stratton IM, Adler AI, Neil HA, Mat-
ner RJ, Varner MW, Rouse DJ, Thorp JM 36. Nathan DM, Davidson MB, DeFronzo thews DR, Manley SE, Cull CA, Hadden
Jr, Sciscione A, Catalano P, Harper M, RA, Heine RJ, Henry RR, Pratley R, Zin- D, Turner RC, Holman RR. Association
Saade G, Lain KY, Sorokin Y, Peaceman man B, American Diabetes Association. of glycaemia with macrovascular and
AM, Tolosa JE, Anderson GB, Eunice Impaired fasting glucose and impaired microvascular complications of type 2
Kennedy Shriver National Institute of glucose tolerance: implications for care. diabetes (UKPDS 35): prospective ob-
Child Health and Human Development Diabetes Care 2007;30:753–759 servational study. BMJ 2000;321:405–
Maternal-Fetal Medicine Units Network. 37. American Diabetes Association: Consen- 412
A multicenter, randomized trial of treat- sus statement on self-monitoring of 47. Cagliero E, Levina EV, Nathan DM. Im-
ment for mild gestational diabetes. blood glucose. Diabetes Care 1987;10: mediate feedback of HbA1c levels im-
N Engl J Med 2009;361:1339 –1348 95–99 proves glycemic control in type 1 and
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S49
Standards of Medical Care
insulin-treated type 2 diabetic patients. betic microvascular complications in of Diabetes Interventions and Complica-
Diabetes Care 1999;22:1785–1789 Japanese patients with non-insulin-de- tions (DCCT/EDIC) Study Research
48. Miller CD, Barnes CS, Phillips LS, Zi- pendent diabetes mellitus: a randomized Group. Intensive diabetes treatment and
emer DC, Gallina DL, Cook CB, Mary- prospective 6-year study. Diabetes Res cardiovascular disease in patients with
man SD, El-Kebbi IM. Rapid A1c Clin Pract 1995;28:103–117 type 1 diabetes. N Engl J Med 2005;353:
availability improves clinical decision- 57. Effect of intensive blood-glucose control 2643–2653
making in an urban primary care clinic. with metformin on complications in 67. Diabetes Control and Complications
Diabetes Care 2003;26:1158 –1163 overweight patients with type 2 diabetes Trial/Epidemiology of Diabetes Inter-
49. Nathan DM, Kuenen J, Borg R, Zheng H, (UKPDS 34): UK Prospective Diabetes ventions and Complications (DCCT/
Schoenfeld D, Heine RJ, A1c-Derived Study (UKPDS) Group. Lancet 1998; EDIC) Research Group, Nathan DM,
Average Glucose Study Group. Translat- 352:854 – 865 Zinman B, Cleary PA, Backlund JY, Ge-
ing the A1C assay into estimated average 58. Intensive blood-glucose control with nuth S, Miller R, Orchard TJ. Modern-
glucose values. Diabetes Care 2008;31: sulphonylureas or insulin compared day clinical course of type 1 diabetes
1473–1478 with conventional treatment and risk of mellitus after 30 years’ duration: the di-
50. Rohlfing CL, Wiedmeyer HM, Little RR, complications in patients with type 2 di- abetes control and complications trial/
England JD, Tennill A, Goldstein DE. abetes (UKPDS 33): UK Prospective Di- epidemiology of diabetes interventions
Defining the relationship between abetes Study (UKPDS) Group. Lancet and complications and Pittsburgh epide-
plasma glucose and HbA(1c): analysis of 1998;352:837– 853 miology of diabetes complications expe-
glucose profiles and HbA(1c) in the Di- 59. Holman RR, Paul SK, Bethel MA, Mat- rience (1983–2005). Arch Intern Med
abetes Control and Complications Trial. thews DR, Neil HA: 10-Year follow-up of 2009;169:1307–1316
Diabetes Care 2002;25:275–278 intensive glucose control in type 2 dia- 68. Action to Control Cardiovascular Risk in
51. Diabetes Research in Children Network betes. N Engl J Med 2008;359:1577– Diabetes Study Group, Gerstein HC,
(DirecNet) Study Group, Wilson DM, 1589 Miller ME, Byington RP, Goff DC Jr, Big-
Kollman. Relationship of A1C to glucose 60. Duckworth W, Abraira C, Moritz T, ger JT, Buse JB, Cushman WC, Genuth
concentrations in children with type 1 Reda D, Emanuele N, Reaven PD, Zieve S, Ismail-Beigi F, Grimm RH Jr, Probst-
diabetes: assessments by high-frequency FJ, Marks J, Davis SN, Hayward R, War- field JL, Simons-Morton DG, Friedewald
glucose determinations by sensors. Dia- ren SR, Goldman S, McCarren M, Vitek WT. Effects of intensive glucose lower-
betes Care 2008;31:381–385 ME, Henderson WG, Huang GD, VADT ing in type 2 diabetes. N Engl J Med
52. Skyler JS, Bergenstal R, Bonow RO, Buse Investigators. Glucose control and vas- 2008;358:2545–2559
J, Deedwania P, Gale EA, Howard BV, cular complications in veterans with 69. Duckworth W. VADT Results. Late-
Kirkman MS, Kosiborod M, Reaven P, type 2 diabetes. N Engl J Med 2009;360: breaking abstract presented at 68th An-
Sherwin RS, American Diabetes Associ- 129 –139 nual Scientific Sessions of the American
ation, American College of Cardiology 61. Moritz T, Duckworth W, Abraira C. Vet- Diabetes Association, 6 June 2008, San
Foundation, American Heart Associa- erans Affairs diabetes trial– corrections. Francisco, CA
tion. Intensive glycemic control and the N Engl J Med 2009;361:1024 –1025 70. Reaven PD, Moritz TE, Schwenke DC,
prevention of cardiovascular events: im- 62. Lawson ML, Gerstein HC, Tsui E, Zin- Anderson RJ, Criqui M, Detrano R,
plications of the ACCORD, ADVANCE, man B. Effect of intensive therapy on Emanuele N, Kayshap M, Marks J, Mu-
and VA diabetes trials: a position state- early macrovascular disease in young in- daliar S, Rao RH, Shah JH, Goldman S,
ment of the American Diabetes Associa- dividuals with type 1 diabetes: A system- Reda DJ, McCarren M, Abraira C, Duck-
tion and a scientific statement of the atic review and meta-analysis. Diabetes worth W: Intensive glucose lowering
American College of Cardiology Foun- Care 1999;22(Suppl. 2):B35–B39 therapy reduces cardiovascular disease
dation and the American Heart Associa- 63. ADVANCE Collaborative Group, Patel events in VADT participants with lower
tion. Diabetes Care 2009;32:187–192 A, MacMahon S, Chalmers J, Neal B, Bil- calcified coronary atherosclerosis. Dia-
53. The effect of intensive treatment of dia- lot L, Woodward M, Marre M, Cooper betes 2009;59:2642–2648
betes on the development and progres- M, Glasziou P, Grobbee D, Hamet P, 71. Turnbull FM, Abraira C, Anderson RJ,
sion of long-term complications in Harrap S, Heller S, Liu L, Mancia G, Mo- Byington RP, Chalmers JP, Duckworth
insulin-dependent diabetes mellitus. gensen CE, Pan C, Poulter N, Rodgers A, WC, Evans GW, Gerstein HC, Holman
The Diabetes Control and Complica- Williams B, Bompoint S, de Galan BE, RR, Moritz TE, Neal BC, Ninomiya T,
tions Trial Research Group. N Engl Joshi R, Travert F. Intensive blood glu- Patel AA, Paul SK, Travert F, Woodward
J Med 1993;329:977–986 cose control and vascular outcomes in M: Intensive glucose control and macro-
54. Retinopathy and nephropathy in pa- patients with type 2 diabetes. N Engl vascular outcomes in type 2 diabetes.
tients with type 1 diabetes four years af- J Med 2008;358:2560 –2572 Diabetologia 2009;52:2288 –2298
ter a trial of intensive therapy. The 64. Selvin E, Marinopoulos S, Berkenblit G, 72. American Diabetes Association: Post-
Diabetes Control and Complications Rami T, Brancati FL, Powe NR, Golden prandial blood glucose (Consensus
Trial/Epidemiology of Diabetes Interven- SH. Meta-analysis: glycosylated hemo- Statement). Diabetes Care 2001;24:775–
tions and Complications Research Group. globin and cardiovascular disease in di- 778
N Engl J Med 2000;342:381–389 abetes mellitus. Ann Intern Med 2004; 73. Ceriello A, Taboga C, Tonutti L, Quagli-
55. Martin CL, Albers J, Herman WH, 141:421– 431 aro L, Piconi L, Bais B, Da Ros R, Motz E.
Cleary P, Waberski B, Greene DA, 65. Stettler C, Allemann S, Jüni P, Cull CA, Evidence for an independent and cu-
Stevens MJ, Feldman EL, DCCT/EDIC Holman RR, Egger M, Krähenbühl S, mulative effect of postprandial hyper-
Research Group. Neuropathy among the Diem P. Glycemic control and macro- triglyceridemia and hyperglycemia on
diabetes control and complications trial vascular disease in types 1 and 2 diabetes endothelial dysfunction and oxidative
cohort 8 years after trial completion. Di- mellitus: Meta-analysis of randomized stress generation: effects of short- and
abetes Care 2006;29:340 –344 trials. Am Heart J 2006;152:27–38 long-term simvastatin treatment. Circu-
56. Ohkubo Y, Kishikawa H, Araki E, Miyata 66. Nathan DM, Cleary PA, Backlund JY, lation 2002;106:1211–1218
T, Isami S, Motoyoshi S, Kojima Y, Fu- Genuth SM, Lachin JM, Orchard TJ, 74. Raz I, Wilson PW, Strojek K, Kowalska I,
ruyoshi N, Shichiri M. Intensive insulin Raskin P, Zinman B, Diabetes Control Bozikov V, Gitt AK, Jermendy G, Cam-
therapy prevents the progression of dia- and Complications Trial/Epidemiology paigne BN, Kerr L, Milicevic Z, Jacober
S50 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
SJ. Effects of prandial versus fasting gly- ble, intensive insulin management to en- terns on blood pressure. DASH Collab-
cemia on cardiovascular outcomes in able dietary freedom in people with type orative Research Group. N Engl J Med
type 2 diabetes: the HEART2D trial. Di- 1 diabetes: dose adjustment for normal 1997;336:1117–1124
abetes Care 2009;32:381–386 eating (DAFNE) randomised controlled 94. Norris SL, Zhang X, Avenell A, Gregg E,
75. Metzger BE, Buchanan TA, Coustan DR, trial. BMJ 2002;325:746 Bowman B, Schmid CH, Lau J. Long-
de Leiva A, Dunger DB, Hadden DR, 84. Franz MJ, Monk A, Barry B, McClain K, term effectiveness of weight-loss inter-
Hod M, Kitzmiller JL, Kjos SL, Oats JN, Weaver T, Cooper N, Upham P, Bergen- ventions in adults with pre-diabetes: a
Pettitt DJ, Sacks DA, Zoupas C. Sum- stal R, Mazze RS. Effectiveness of medi- review. Am J Prev Med 2005;28:126 –
mary and recommendations of the Fifth cal nutrition therapy provided by 139
International Workshop-Conference on dietitians in the management of non-in- 95. Klein S, Sheard NF, Pi-Sunyer X, Daly A,
Gestational Diabetes Mellitus. Diabetes sulin-dependent diabetes mellitus: a Wylie-Rosett J, Kulkarni K, Clark NG,
Care 2007;30(Suppl. 2):S251–S260 randomized, controlled clinical trial. American Diabetes Association, North
76. Kitzmiller JL, Block JM, Brown FM, J Am Diet Assoc 1995;95:1009 –1017 American Association for the Study of
Catalano PM, Conway DL, Coustan DR, 85. Goldhaber-Fiebert JD, Goldhaber-Fiebert Obesity, American Society for Clinical
Gunderson EP, Herman WH, Hoffman SN, Tristán ML, Nathan DM. Randomized Nutrition. Weight management through
LD, Inturrisi M, Jovanovic LB, Kjos SI, controlled community-based nutrition lifestyle modification for the prevention
Knopp RH, Montoro MN, Ogata ES, and exercise intervention improves glyce- and management of type 2 diabetes: ra-
Paramsothy P, Reader DM, Rosenn BM, mia and cardiovascular risk factors in type tionale and strategies: a statement of
Thomas AM, Kirkman MS. Managing 2 diabetic patients in rural Costa Rica. Di- the American Diabetes Association, the
preexisting diabetes for pregnancy: sum- abetes Care 2003;26:24 –29 North American Association for the
mary of evidence and consensus recom- 86. Lemon CC, Lacey K, Lohse B, Hubacher Study of Obesity, and the American So-
mendations for care. Diabetes Care DO, Klawitter B, Palta M. Outcomes ciety for Clinical Nutrition. Diabetes
2008;31:1060 –1079 monitoring of health, behavior, and Care 2004;27:2067–2073
77. DeWitt DE, Hirsch IB. Outpatient insu- quality of life after nutrition intervention 96. Norris SL, Zhang X, Avenell A, Gregg E,
lin therapy in type 1 and type 2 diabetes in adults with type 2 diabetes. J Am Diet Schmid CH, Kim C, Lau J. Efficacy of
mellitus: scientific review. JAMA 2003; Assoc 2004;104:1805–1815 pharmacotherapy for weight loss in
289:2254 –2264 87. Miller CK, Edwards L, Kissling G, San- adults with type 2 diabetes mellitus: a
78. Rosenstock J, Dailey G, Massi-Benedetti ville L. Nutrition education improves meta-analysis. Arch Intern Med 2004;
M, Fritsche A, Lin Z, Salzman A. Re- metabolic outcomes among older adults 164:1395–1404
duced hypoglycemia risk with insulin with diabetes mellitus: results from a 97. Wolf AM, Conaway MR, Crowther JQ,
glargine: a meta-analysis comparing in- randomized controlled trial. Prev Med Hazen KY, L Nadler J, Oneida B, Bovb-
sulin glargine with human NPH insulin 2002;34:252–259 jerg VE, Improving Control with Activity
in type 2 diabetes. Diabetes Care 2005; 88. Wilson C, Brown T, Acton K, Gilliland S. and Nutrition (ICAN) Study. Translat-
28:950 –955 Effects of clinical nutrition education ing lifestyle intervention to practice in
79. Mooradian AD, Bernbaum M, Albert SG. and educator discipline on glycemic obese patients with type 2 diabetes: Im-
Narrative review: a rational approach to control outcomes in the Indian health proving Control with Activity and Nutri-
starting insulin therapy. Ann Intern Med service. Diabetes Care 2003;26:2500 – tion (ICAN) study. Diabetes Care 2004;
2006;145:125–134 2504 27:1570 –1576
80. Nathan DM, Buse JB, Davidson MB, 89. Graber AL, Elasy TA, Quinn D, Wolff K, 98. Manning RM, Jung RT, Leese GP, New-
Heine RJ, Holman RR, Sherwin R, Zin- Brown A. Improving glycemic control in ton RW. The comparison of four weight
man B. Management of hyperglycemia in adults with diabetes mellitus: shared re- reduction strategies aimed at overweight
type 2 diabetes: a consensus algorithm sponsibility in primary care practices. patients with diabetes mellitus: four-
for the initiation and adjustment of ther- South Med J 2002;95:684 – 690 yearfollow-up.DiabetMed1998;15:497–
apy: a consensus statement from the 90. Gaetke LM, Stuart MA, Truszczynska H. 502
American Diabetes Association and the A single nutrition counseling session 99. Shai I, Schwarzfuchs D, Henkin Y, Sha-
European Association for the Study of with a registered dietitian improves har DR, Witkow S, Greenberg I, Golan
Diabetes. Diabetes Care 2006;29:1963– short-term clinical outcomes for rural R, Fraser D, Bolotin A, Vardi H, Tangi-
1972 Kentucky patients with chronic diseases. Rozental O, Zuk-Ramot R, Sarusi B,
81. Nathan DM, Buse JB, Davidson MB, Fer- J Am Diet Assoc 2006;106:109 –112 Brickner D, Schwartz Z, Sheiner E,
rannini E, Holman RR, Sherwin R, Zin- 91. Yu-Poth S, Zhao G, Etherton T, Naglak Marko R, Katorza E, Thiery J, Fiedler
man B, American Diabetes Association, M, Jonnalagadda S, Kris-Etherton PM. GM, Blüher M, Stumvoll M, Stampfer
European Association for Study of Dia- Effects of the National Cholesterol Ed- MJ, Dietary Intervention Randomized
betes. Medical management of hypergly- ucation Program’s Step I and Step II Controlled Trial (DIRECT) Group.
cemia in type 2 diabetes: a consensus dietary intervention programs on car- Weight loss with a low-carbohydrate,
algorithm for the initiation and adjust- diovascular disease risk factors: a meta- Mediterranean, or low-fat diet. N Engl
ment of therapy: a consensus statement analysis. Am J Clin Nutr 1999;69:632– J Med 2008;359:229 –241
of the American Diabetes Association 646 100. Franz MJ, VanWormer JJ, Crain AL,
and the European Association for the 92. Van Horn L, McCoin M, Kris-Etherton Boucher JL, Histon T, Caplan W, Bow-
Study of Diabetes. Diabetes Care 2009; PM, Burke F, Carson JA, Champagne man JD, Pronk NP. Weight-loss out-
32:193–203 CM, Karmally W, Sikand G. The evi- comes: a systematic review and meta-
82. Bantle JP, Wylie-Rosett J, Albright AL, dence for dietary prevention and treat- analysis of weight-loss clinical trials with
Apovian CM, Clark NG, Franz MJ, ment of cardiovascular disease. J Am a minimum 1-year follow-up. J Am Diet
Hoogwerf BJ, Lichtenstein AH, Mayer- Diet Assoc 2008;108:287–331 Assoc 2007;107:1755–1767
Davis E, Mooradian AD, Wheeler ML. 93. Appel LJ, Moore TJ, Obarzanek E, 101. Look AHEAD Research Group, Pi-Su-
Nutrition recommendations and inter- Vollmer WM, Svetkey LP, Sacks FM, nyer X, Blackburn G, Brancati FL, Bray
ventions for diabetes—2006. Diabetes Bray GA, Vogt TM, Cutler JA, GA, Bright R, Clark JM, Curtis JM, Es-
Care 2006;29:2140 –2157 Windhauser MM, Lin PH, Karanja N. A peland MA, Foreyt JP, Graves K, Haffner
83. DAFNE Study Group. Training in flexi- clinical trial of the effects of dietary pat- SM, Harrison B, Hill JO, Horton ES, Ja-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S51
Standards of Medical Care
kicic J, Jeffery RW, Johnson KC, Kahn S, prevention of diabetes and related com- systematic review and methodological
Kelley DE, Kitabchi AE, Knowler WC, plications. Diabetes Care 2002;25:148 – critique of the literature. Arch Intern
Lewis CE, Maschak-Carey BJ, Montgom- 198 Med 2004;164:1641–1649
ery B, Nathan DM, Patricio J, Peters A, 110. Buchwald H, Estok R, Fahrbach K, Banel 121. Funnell MM, Brown TL, Childs BP, Haas
Redmon JB, Reeves RS, Ryan DH, Safford D, Jensen MD, Pories WJ, Bantle JP, LB, Hosey GM, Jensen B, Maryniuk M,
M, Van Dorsten B, Wadden TA, Wagen- Sledge I. Weight and type 2 diabetes af- Peyrot M, Piette JD, Reader D, Siminerio
knecht L, Wesche-Thobaben J, Wing RR, ter bariatric surgery: systematic review LM, Weinger K, Weiss MA. National
Yanovski SZ. Reduction in weight and car- and meta-analysis. Am J Med 2009;122: standards for diabetes self-management
diovascular disease risk factors in individ- 248 –256 education. Diabetes Care 2007;30:
uals with type 2 diabetes: one-year results 111. Dixon JB, O’Brien PE, Playfair J, Chap- 1630 –1637
of the look AHEAD trial. Diabetes Care man L, Schachter LM, Skinner S, Proi- 122. Mulcahy K, Maryniuk M, Peeples M, Pey-
2007;30:1374 –1383 etto J, Bailey M, Anderson M. Adjustable rot M, Tomky D, Weaver T, Yarborough P.
102. Foster GD, Wyatt HR, Hill JO, gastric banding and conventional ther- Diabetes self-management education core
McGuckin BG, Brill C, Mohammed BS, apy for type 2 diabetes: a randomized outcomes measures. Diabetes Educ
Szapary PO, Rader DJ, Edman JS, Klein controlled trial. JAMA 2008;299:316 – 29:768- 2003;84:787
S. A randomized trial of a low-carbohy- 323 123. Glasgow RE, Peeples M, Skovlund SE.
drate diet for obesity. N Engl J Med 112. Buchwald H, Estok R, Fahrbach K, Banel Where is the patient in diabetes perfor-
2003;348:2082–2090 D, Sledge I. Trends in mortality in bari- mance measures? The case for including
103. Stern L, Iqbal N, Seshadri P, Chicano atric surgery: a systematic review and patient-centered and self-management
KL, Daily DA, McGrory J, Williams M, meta-analysis. Surgery 2007;142:621– measures. Diabetes Care 2008;31:1046 –
Gracely EJ, Samaha FF. The effects of 632 1050
low-carbohydrate versus conventional 113. Sjöström L, Narbro K, Sjöström CD, 124. Barker JM, Goehrig SH, Barriga K, Hoff-
weight loss diets in severely obese Karason K, Larsson B, Wedel H, Lystig man M, Slover R, Eisenbarth GS, Norris
adults: one-year follow-up of a random- T, Sullivan M, Bouchard C, Carlsson B, JM, Klingensmith GJ, Rewers M, DAISY
ized trial. Ann Intern Med 2004;140: Bengtsson C, Dahlgren S, Gummesson study. Clinical characteristics of chil-
778 –785 A, Jacobson P, Karlsson J, Lindroos AK, dren diagnosed with type 1 diabetes
104. Gardner CD, Kiazand A, Alhassan S, Lönroth H, Näslund I, Olbers T, Stenlöf through intensive screening and follow-
Kim S, Stafford RS, Balise RR, Kraemer K, Torgerson J, Agren G, Carlsson LM, up. Diabetes Care 2004;27:1399 –1404
HC, King AC. Comparison of the At- Swedish Obese Subjects Study. Effects of 125. Cochran J, Conn VS. Meta-analysis of
kins, Zone, Ornish, and LEARN diets bariatric surgery on mortality in Swedish quality of life outcomes following diabe-
for change in weight and related risk obese subjects. N Engl J Med 2007;357: tes self-management training. Diabetes
factors among overweight premeno- 741–752 Educ 2008;34:815– 823
pausal women. JAMA 2007;297:969 – 114. Piette JD, Glasgow RE: Sttategies for im- 126. Fisher EB, Thorpe CT, Devellis BM, De-
977 proving behavioral and health outcomes vellis RF. Healthy coping, negative emo-
105. Nordmann AJ, Nordmann A, Briel M, among people with diabetes: self man- tions, and diabetes management: a
Keller U, Yancy WS, Jr, Brehm BJ, agement education. In Evidence-Based systematic review and appraisal. Diabe-
Bucher HC. Effects of low-carbohydrate Diabetes Care. Gerstein HC, Hayes RB, tes Educ 2007;33:1080 –1103
vs low-fat diets on weight loss and car- Eds. Ontario, Canada, BC Decker, 2000 127. Robbins JM, Thatcher GE, Webb DA,
diovascular risk factors: a meta-analysis 115. Norris SL, Engelgau MM, Narayan KM. Valdmanis VG. Nutritionist visits, diabe-
of randomized controlled trials. Arch In- Effectiveness of self-management train- tes classes, and hospitalization rates and
tern Med 2006;166:285–293 ing in type 2 diabetes: a systematic re- charges: the Urban Diabetes Study. Dia-
106. Institute of Medicine: DIetary Reference view of randomized controlled trials. betes Care 2008;31:655– 660
Intakes: Energy, Carbohydrate, Fiber, Fat, Diabetes Care 2001;24:561–587 128. Renders CM, Valk GD, Griffin SJ, Wag-
Fatty Acids, Cholesterol, Protein, and 116. Norris SL, Lau J, Smith SJ, Schmid CH, ner EH, Eijk Van JT, Assendelft WJ. In-
Amino Acids. Washington, DC, National Engelgau MM. Self-management educa- terventions to improve the management
Academies Press, 2002 tion for adults with type 2 diabetes: a of diabetes in primary care, outpatient,
107. Barnard ND, Cohen J, Jenkins DJ, Turner- meta-analysis of the effect on glycemic and community settings: a systematic re-
McGrievy G, Gloede L, Jaster B, Seidl K, control. Diabetes Care 2002;25:1159 – view. Diabetes Care 2001;24:1821–
Green AA, Talpers S. A low-fat vegan 1171 1833
diet improves glycemic control and car- 117. Gary TL, Genkinger JM, Guallar E, Pey- 129. Polonsky WH, Earles J, Smith S, Pease
diovascular risk factors in a randomized rot M, Brancati FL. Meta-analysis of ran- DJ, Macmillan M, Christensen R, Taylor
clinical trial in individuals with type 2 domized educational and behavioral T, Dickert J, Jackson RA. Integrating
diabetes. Diabetes Care 2006;29:1777– interventions in type 2 diabetes. Diabe- medical management with diabetes self-
1783 tes Educ 2003;29:488 –501 management training: a randomized
108. Turner-McGrievy GM, Barnard ND, Co- 118. Steed L, Cooke D, Newman S. A system- control trial of the Diabetes Outpatient
hen J, Jenkins DJ, Gloede L, Green AA. atic review of psychosocial outcomes Intensive Treatment program. Diabetes
Changes in nutrient intake and dietary following education, self-management Care 2003;26:3048 –3053
quality among participants with type 2 and psychological interventions in dia- 130. Anderson RM, Funnell MM, Nwankwo
diabetes following a low-fat vegan diet or betes mellitus. Patient Educ Couns R, Gillard ML, Oh M, Fitzgerald JT.
a conventional diabetes diet for 22 2003;51:5–15 Evaluating a problem-based empower-
weeks. J Am Diet Assoc 2008;108: 119. Ellis SE, Speroff T, Dittus RS, Brown A, ment program for African Americans
1636 –1645 Pichert JW, Elasy TA. Diabetes patient with diabetes: results of a randomized
109. Franz MJ, Bantle JP, Beebe CA, Brunzell education: a meta-analysis and meta-re- controlled trial. Ethn Dis 2005;15:
JD, Chiasson JL, Garg A, Holzmeister gression. Patient Educ Couns 2004;52: 671– 678
LA, Hoogwerf B, Mayer-Davis E, Moora- 97–105 131. Brown SA, Blozis SA, Kouzekanani K,
dian AD, Purnell JQ, Wheeler M. Evi- 120. Warsi A, Wang PS, LaValley MP, Avorn Garcia AA, Winchell M, Hanis CL. Dos-
dence-based nutrition principles and J, Solomon DH. Self-management edu- age effects of diabetes self-management
recommendations for the treatment and cation programs in chronic disease: a education for Mexican Americans: the
S52 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Starr County Border Health Initiative. diabetes mellitus: a meta-analysis of 156. Aiello LP, Wong J, Cavallerano J, Bursell
Diabetes Care 2005;28:527–532 controlledclinicaltrials.JAMA2001;286: SE, Aiello LM: Retinopathy. In Handbook
132. Glazier RH, Bajcar J, Kennie NR, Willson 1218 –1227 of Exercise in Diabetes. 2nd ed. Ru-
K. A systematic review of interventions 146. Boulé NG, Kenny GP, Haddad E, Wells derman N, Devlin JT, Kriska A, Eds.
to improve diabetes care in socially dis- GA, Sigal RJ. Meta-analysis of the effect Alexandria, VA, American Diabetes As-
advantaged populations. Diabetes Care of structured exercise training on cardio- sociation, 2002, p. 401– 413
2006;29:1675–1688 respiratory fitness in Type 2 diabetes 157. Lemaster JW, Reiber GE, Smith DG,
133. Sarkisian CA, Brown AF, Norris KC, mellitus. Diabetologia 2003;46:1071– Heagerty PJ, Wallace C. Daily weight-
Wintz RL, Mangione CM. A systematic 1081 bearing activity does not increase the
review of diabetes self-care interventions 147. U.S. Department of Health and Human risk of diabetic foot ulcers. Med Sci
for older, African American, or Latino Services. 2008 Physical Activity Guide- Sports Exerc 2003;35:1093–1099
adults. Diabetes Educ 2003;29:467–479 lines for Americans. Atlanta, GA, 158. Vinik A, Erbas T: Neuropathy. In Hand-
134. Chodosh J, Morton SC, Mojica W, Ma- Centers for Disease Control and Pre- book of Exercise in Diabetes. 2nd ed. Ru-
glione M, Suttorp MJ, Hilton L, Rhodes vention, 2008 derman N, Devlin JT, Kriska A, Eds.
S, Shekelle P. Meta-analysis: chronic dis- 148. Cauza E, Hanusch-Enserer U, Strasser B, Alexandria, VA, American Diabetes As-
ease self-management programs for Ludvik B, Metz-Schimmerl S, Pacini G, sociation, 2002, p. 463– 496
older adults. Ann Intern Med 2005;143: Wagner O, Georg P, Prager R, Kostner K, 159. Wackers FJ, Young LH, Inzucchi SE,
427– 438 Dunky A, Haber P. The relative benefits Chyun DA, Davey JA, Barrett EJ,
135. Peyrot M, Rubin RR. Behavioral and psy- of endurance and strength training on Taillefer R, Wittlin SD, Heller GV, Filip-
chosocial interventions in diabetes: a the metabolic factors and muscle func- chuk N, Engel S, Ratner RE, Iskandrian
conceptual review. Diabetes Care 2007; tion of people with type 2 diabetes mel- AE, Detection of Ischemia in Asymp-
30:2433–2440 litus. Arch Phys Med Rehabil 2005;86: tomatic Diabetics Investigators. Detec-
136. Rickheim PL, Weaver TW, Flader JL, 1527–1533 tion of silent myocardial ischemia in
Kendall DM. Assessment of group versus 149. Dunstan DW, Daly RM, Owen N, Jolley asymptomatic diabetic subjects: the
individual diabetes education: a ran- D, De Courten M, Shaw J, Zimmet P. DIAD study. Diabetes Care 2004;27:
domized study. Diabetes Care 2002;25: High-intensity resistance training im- 1954 –1961
269 –274 proves glycemic control in older patients 160. Valensi P, Sachs RN, Harfouche B,
137. Trento M, Passera P, Borgo E, Tomalino with type 2 diabetes. Diabetes Care Lormeau B, Paries J, Cosson E, Paycha F,
M, Bajardi M, Cavallo F, Porta M. A 2002;25:1729 –1736 Leutenegger M, Attali JR. Predictive
5-year randomized controlled study of 150. Castaneda C, Layne JE, Munoz-Orians value of cardiac autonomic neuropathy
learning, problem solving ability, and L, Gordon PL, Walsmith J, Foldvari M, in diabetic patients with or without si-
quality of life modifications in people Roubenoff R, Tucker KL, Nelson ME. A lent myocardial ischemia. Diabetes Care
with type 2 diabetes managed by group randomized controlled trial of resistance 2001;24:339 –343
care. Diabetes Care 2004;27:670 – 675 exercise training to improve glycemic 161. Mogensen CE: Nephropathy. In Hand-
138. Deakin T, McShane CE, Cade JE, Wil- control in older adults with type 2 dia- book of Exercise in Diabetes. 2nd ed. Ru-
liams RD: Group based training for self- betes. Diabetes Care 2002;25:2335– derman N, Devlin JT, Kriska A, Eds.
management strategies in people with 2341 Alexandria, VA, American Diabetes As-
type 2 diabetes mellitus. Cochrane Da- 151. Sigal RJ, Kenny GP, Boulé NG, Wells sociation, 2002, p. 433– 449
tabase Syst Rev CD003417, 2005 GA, Prud’homme D, Fortier M, Reid RD, 162. Anderson RJ, Grigsby AB, Freedland KE,
139. Heisler, M. Building Peer Support Pro- Tulloch H, Coyle D, Phillips P, Jennings de Groot M, McGill JB, Clouse RE, Lust-
grams to Manage Chronic Disease: Seven A, Jaffey J. Effects of aerobic training, re- man PJ. Anxiety and poor glycemic con-
Models for Success. Oakland, CA, Califor- sistance training, or both on glycemic trol: a meta-analytic review of the
nia Health Care Foundation, 2006 control in type 2 diabetes: a randomized literature. Int J Psychiatry Med 2002;32:
140. Foster G, Taylor SJ, Eldridge SE, Ramsay trial. Ann Intern Med 2007;147: 235–247
J, Griffiths CJ: Self-management educa- 357–369 163. Delahanty LM, Grant RW, Wittenberg E,
tion programmes by lay leaders for peo- 152. Bax JJ, Young LH, Frye RL, Bonow RO, Bosch JL, Wexler DJ, Cagliero E, Meigs
ple with chronic conditions. Cochrane Steinberg HO, Barrett EJ, ADA. Screen- JB. Association of diabetes-related emo-
Database Syst Rev CD005108, 2007 ing for coronary artery disease in pa- tional distress with diabetes treatment in
141. Norris SL, Chowdhury FM, Van Le K, tients with diabetes. Diabetes Care 2007; primary care patients with Type 2 diabe-
Horsley T, Brownstein JN, Zhang X, Jack 30:2729 –2736 tes. Diabet Med 2007;24:48 –54
L Jr, Satterfield DW. Effectiveness of 153. Berger M, Berchtold P, Cüppers HJ, 164. American Diabetes Association: Psycho-
community health workers in the care of Drost H, Kley HK, Müller WA, social factors affecting adherence, qual-
persons with diabetes. Diabet Med Wiegelmann W, Zimmerman-Telschow ity of life, and well-being: Helping
2006;23:544 –556 H, Gries FA, Krüskemper HL, Zimmer- Patients cope. In Medical Management of
142. Duncan I, Birkmeyer C, Coughlin S, Li mann H. Metabolic and hormonal ef- Type 1 Diabetes. 5 ed. Francine R. Kauf-
QE, Sherr D, Boren S. Assessing the fects of muscular exercise in juvenile man, Ed. Alexandria, VA, American Di-
value of diabetes education. Diabetes type diabetics. Diabetologia 1977;13: abetes Association, 2008, p. 173–193
Educ 2009;35:752–760 355–365 165. Fisher L, Skaff MM, Mullan JT, Arean P,
143. Sigal RJ, Kenny GP, Wasserman DH, 154. American Diabetes Association: Physical Mohr D, Masharani U, Glasgow R, Lau-
Castaneda-Sceppa C. Physical activity/ activity/exercise and diabetes (Position rencin G. Clinical depression versus dis-
exercise and type 2 diabetes. Diabetes Statement). Diabetes Care 2004; tress among patients with type 2
Care 2004;27:2518 –2539 27(Suppl. 1):S58 –S62 diabetes: not just a question of seman-
144. Wasserman DH, Zinman B. Exercise in 155. Berger M: Adjustment of insulin and oral tics. Diabetes Care 2007;30:542–548
individuals with IDDM. Diabetes Care agent therapy. In Handbook of Exercise in 166. Surwit RS, Schneider MS, Feinglos MN.
1994;17:924 –937 Diabetes. 2nd ed. Ruderman N, Devlin Stress and diabetes mellitus. Diabetes
145. Boulé NG, Haddad E, Kenny GP, Wells JTSSH, Krisska A, Eds. Alexandria, VA, Care 1992;15:1413–1422
GA, Sigal RJ. Effects of exercise on gly- American Diabetes Association, 2002, p. 167. McCulloch DK, Glasgow RE, Hampson
cemic control and body mass in type 2 365–376 SE, Wagner E. A systematic approach to
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S53
Standards of Medical Care
diabetes management in the post-DCCT 183. Buse JB, Ginsberg HN, Bakris GL, Clark ity: a meta-analysis of individual data for
era. Diabetes Care 1994;17:765–769 NG, Costa F, Eckel R, Fonseca V, Ger- one million adults in 61 prospective
168. Rubin RR, Peyrot M. Psychological is- stein HC, Grundy S, Nesto RW, Pignone studies. Lancet 2002;360:1903–1913
sues and treatments for people with di- MP, Plutzky J, Porte D, Redberg R, Stit- 191. Stamler J, Vaccaro O, Neaton JD, Went-
abetes. J Clin Psychol 2001;57:457– 478 zel KF, Stone NJ, American Heart Asso- worth D. Diabetes, other risk factors,
169. Jacobson AM. Depression and diabetes. ciation, American Diabetes Association. and 12-yr cardiovascular mortality for
Diabetes Care 1993;16:1621–1623 Primary prevention of cardiovascular men screened in the Multiple Risk Fac-
170. Lustman PJ, Griffith LS, Clouse RE, diseases in people with diabetes melli- tor Intervention Trial. Diabetes Care
Cryer PE. Psychiatric illness in diabetes tus: a scientific statement from the 1993;16:434 – 444
mellitus. Relationship to symptoms and American Heart Association and the 192. Cushman WC, Grimm RH Jr, Cutler JA,
glucose control. J Nerv Ment Dis 1986; American Diabetes Association. Diabe- Evans GW, Capes S, Corson MA, Sadler
174:736 –742 tes Care 2007;30:162–172 LS, Alderman MH, Peterson K, Bertoni
171. Blonde L, Merilainen M, Karwe V, 184. Chobanian AV, Bakris GL, Black HR, A, Basile JN, ACCORD Study Group: Ra-
Raskin P, TITRATE Study Group. Pa- Cushman WC, Green LA, Izzo JL Jr, tionale and design for the blood pressure
tient-directed titration for achieving gly- Jones DW, Materson BJ, Oparil S, intervention of the Action to Control
caemic goals using a once-daily basal Wright JT Jr, Roccella EJ, National Cardiovascular Risk in Diabetes (AC-
insulin analogue: an assessment of two Heart, Lung, and Blood Institute Joint CORD) trial. Am J Cardiol 2007;99:44i–
different fasting plasma glucose targets National Committee on Prevention, De- 55i
-the TITRATE study. Diabetes Obes tection, Evaluation, and Treatment of 193. Sacks FM, Svetkey LP, Vollmer WM, Ap-
Metab 2009;11:623– 631 High Blood Pressure, National High Blood pel LJ, Bray GA, Harsha D, Obarzanek E,
172. American Diabetes Association: Hyper- Pressure Education Program Coordinat- Conlin PR, Miller ER 3rd, Simons-Mor-
glycemic crises in diabetes. Diabetes ing Committee. The Seventh Report of the ton DG, Karanja N, Lin PH, DASH-So-
Care 2004;27 (Suppl. 1):S94 –S102 Joint National Committee on Prevention, dium Collaborative Research Group.
173. Kitabchi AE, Umpierrez GE, Miles JM, Detection, Evaluation, and Treatment of Effects on blood pressure of reduced di-
Fisher JN. Hyperglycemic crises in adult High Blood Pressure: the JNC 7 report. etary sodium and the Dietary Ap-
patients with diabetes. Diabetes Care JAMA 2003;289:2560 –2572 proaches to Stop Hypertension (DASH)
2009;32:1335–1343 185. Bobrie G, Chatellier G, Genes N, Clerson diet. DASH-Sodium Collaborative Re-
174. Cryer PE. Hypoglycaemia: the limiting P, Vaur L, Vaisse B, Menard J, Mallion search Group. N Engl J Med 2001;344:
factor in the glycaemic management of JM. Cardiovascular prognosis of 3–10
Type I and Type II diabetes. Diabetolo- “masked hypertension” detected by 194. Tatti P, Pahor M, Byington RP, Di Mauro
gia 2002;45:937–948 blood pressure self-measurement in el- P, Guarisco R, Strollo G, Strollo F. Out-
175. Gannon MC, Nuttall FQ: Protein and derly treated hypertensive patients. come results of the Fosinopril Versus
Diabetes. In American Diabetes Associa- JAMA 2004;291:1342–1349 Amlodipine Cardiovascular Events Ran-
tion Guide to Medical Nutrition Therapy 186. Sega R, Facchetti R, Bombelli M, Cesana domized Trial (FACET) in patients with
for Diabetes. Franz MJ, Bantle JP, Eds. G, Corrao G, Grassi G, Mancia G. Prog- hypertension and NIDDM. Diabetes
Alexandria, VA, American Diabetes As- nostic value of ambulatory and home Care 1998;21:597– 603
sociation, 1999, p. 107–125 blood pressures compared with office 195. Estacio RO, Jeffers BW, Hiatt WR, Big-
176. Cryer PE. Diverse causes of hypoglyce- blood pressure in the general popula- gerstaff SL, Gifford N, Schrier RW. The
mia-associated autonomic failure in dia- tion: follow-up results from the Pres- effect of nisoldipine as compared with
betes. N Engl J Med 2004;350:2272– sioni Arteriose Monitorate e Loro enalapril on cardiovascular outcomes in
2279 Associazioni (PAMELA) study. Circula- patients with non-insulin-dependent di-
177. Cryer PE, Davis SN, Shamoon H. Hypo- tion 2005;111:1777–1783 abetes and hypertension. N Engl J Med
glycemia in diabetes. Diabetes Care 187. UKPDS: Tight blood pressure control 1998;338:645– 652
2003;26:1902–1912 and risk of macrovascular and microvas- 196. Schrier RW, Estacio RO, Mehler PS, Hi-
178. Smith SA, Poland GA. Use of influenza cular complications in type 2 diabetes: att WR. Appropriate blood pressure
and pneumococcal vaccines in people UKPDS 38. UK Prospective Diabetes control in hypertensive and normoten-
with diabetes. Diabetes Care 2000;23: Study Group. BMJ 1998;317:703–713 sive type 2 diabetes mellitus: a summary
95–108 188. Hansson L, Zanchetti A, Carruthers SG, of the ABCD trial. Nat Clin Pract Neph-
179. Colquhoun AJ, Nicholson KG, Botha JL, Dahlöf B, Elmfeldt D, Julius S, Ménard J, rol 2007;3:428 – 438
Raymond NT. Effectiveness of influenza Rahn KH, Wedel H, Westerling S. Ef- 197. ALLHAT Officers and Coordinators for
vaccine in reducing hospital admissions fects of intensive blood-pressure lower- the ALLHAT Collaborative Research
in people with diabetes. Epidemiol In- ing and low-dose aspirin in patients Group. The Antihypertensive and Lipid-
fect 1997;119:335–341 with hypertension: principal results of Lowering Treatment to Prevent Heart
180. Bridges CB, Fukuda K, Uyeki TM, Cox the Hypertension Optimal Treatment Attack Trial: the Antihypertensive and
NJ, Singleton JA. Prevention and control (HOT) randomised trial. HOT Study Lipid-Lowering Treatment to Prevent
of influenza. Recommendations of the Group. Lancet 1998;351:1755–1762 Heart Attack Trial (ALLHAT). JAMA
Advisory Committee on Immunization 189. Adler AI, Stratton IM, Neil HA, Yudkin 2002;288:2981–2997
Practices (ACIP). MMWR Recomm Rep JS, Matthews DR, Cull CA, Wright AD, 198. Psaty BM, Lumley T, Furberg CD, Schel-
2002;51:1–31 Turner RC, Holman RR. Association of lenbaum G, Pahor M, Alderman MH,
181. American Diabetes Association: Influ- systolic blood pressure with macrovas- Weiss NS. Health outcomes associated
enza and pneumococcal immunization cular and microvascular complications with various antihypertensive therapies
in diabetes (Position Statement). Diabe- of type 2 diabetes (UKPDS 36): prospec- used as first-line agents: a network meta-
tes Care 2004;27(Suppl. 1):S111–S113 tive observational study. BMJ 2000;321: analysis. JAMA 2003;289:2534 –2544
182. Gaede P, Lund-Andersen H, Parving 412– 419 199. Effects of ramipril on cardiovascular and
HH, Pedersen O. Effect of a multifacto- 190. Lewington S, Clarke R, Qizilbash N, microvascular outcomes in people with
rial intervention on mortality in type 2 Peto R, Collins R, Prospective Studies diabetes mellitus: results of the HOPE
diabetes. N Engl J Med 2008;358:580 – Collaboration. Age-specific relevance of study and MICRO-HOPE substudy:
591 usual blood pressure to vascular mortal- Heart Outcomes Prevention Evaluation
S54 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Study Investigators. Lancet 2000;355: Hypertension and Diabetes Executive heart disease and diabetes: the Treating
253–259 Committees Working Group. Am J Kid- to New Targets (TNT) study. Diabetes
200. Pfeffer MA, Swedberg K, Granger CB, ney Dis 2000;36:646 – 661 Care 2006;29:1220 –1226
Held P, McMurray JJ, Michelson EL, 207. Psaty BM, Smith NL, Siscovick DS, Ko- 215. Sever PS, Poulter NR, Dahlöf B, Wedel
Olofsson B, Ostergren J, Yusuf S, Pocock epsell TD, Weiss NS, Heckbert SR, Le- H, Collins R, Beevers G, Caulfield M,
S, CHARM Investigators and Commit- maitre RN, Wagner EH, Furberg CD. Kjeldsen SE, Kristinsson A, McInnes GT,
tees. Effects of candesartan on mortality Health outcomes associated with antihy- Mehlsen J, Nieminen M, O’Brien E, Os-
and morbidity in patients with chronic pertensive therapies used as first-line tergren J. Reduction in cardiovascular
heart failure: the CHARM-Overall pro- agents: a systematic review and meta- events with atorvastatin in 2,532 pa-
gramme. Lancet 2003;362:759 –766 analysis. JAMA 1997;277:739 –745 tients with type 2 diabetes: Anglo-Scan-
201. Granger CB, McMurray JJ, Yusuf S, Held 208. Patel A, ADVANCE Collaborative dinavian Cardiac Outcomes Trial–lipid-
P, Michelson EL, Olofsson B, Ostergren Group, MacMahon S, Chalmers J, Neal lowering arm (ASCOT-LLA). Diabetes
J, Pfeffer MA, Swedberg K, CHARM In- B, Woodward M, Billot L, Harrap S, Care 2005;28:1151–1157
vestigators and Committees. Effects of Poulter N, Marre M, Cooper M, Glasziou 216. Knopp RH, d’Emden M, Smilde JG, Po-
candesartan in patients with chronic P, Grobbee DE, Hamet P, Heller S, Liu cock SJ. Efficacy and safety of atorvasta-
heart failure and reduced left-ventricular LS, Mancia G, Mogensen CE, Pan CY, tin in the prevention of cardiovascular
systolic function intolerant to angioten- Rodgers A, Williams B. Effects of a fixed end points in subjects with type 2 di-
sin-converting-enzyme inhibitors: the combination of perindopril and indap- abetes: the Atorvastatin Study for Pre-
CHARM-Alternative trial. Lancet 2003; amide on macrovascular and microvas- vention of Coronary Heart Disease
362:772–776 cular outcomes in patients with type 2 Endpoints in non-insulin-dependent di-
202. McMurray JJ, Ostergren J, Swedberg K, diabetes mellitus (the ADVANCE trial): abetes mellitus (ASPEN). Diabetes Care
Granger CB, Held P, Michelson EL, a randomised controlled trial. Lancet 2006;29:1478 –1485
Olofsson B, Yusuf S, Pfeffer MA, 2007;370:829 – 840 217. Singh IM, Shishehbor MH, Ansell BJ.
CHARM Investigators and Committees. 209. Sibai BM. Treatment of hypertension in High-density lipoprotein as a therapeu-
Effects of candesartan in patients with pregnant women. N Engl J Med 1996; tic target: a systematic review. JAMA
chronic heart failure and reduced left- 335:257–265 2007;298:786 –798
ventricular systolic function taking an- 210. Baigent C, Keech A, Kearney PM, Black- 218. Canner PL, Berge KG, Wenger NK,
giotensin-converting-enzyme well L, Buck G, Pollicino C, Kirby A, Stamler J, Friedman L, Prineas RJ,
inhibitors: the CHARM-Added trial. Sourjina T, Peto R, Collins R, Simes R, Friedewald W. Fifteen year mortality in
Lancet 2003;362:767–771 Cholesterol Treatment Trialists’ (CTT) Coronary Drug Project patients: long-
203. Lindholm LH, Ibsen H, Dahlöf B, De- Collaborators. Efficacy and safety of term benefit with niacin. J Am Coll Car-
vereux RB, Beevers G, de Faire U, Fyhr- cholesterol-lowering treatment: pro- diol 1986;8:1245–1255
quist F, Julius S, Kjeldsen SE, spective meta-analysis of data from 219. Rubins HB, Robins SJ, Collins D, Fye CL,
Kristiansson K, Lederballe-Pedersen O, 90,056 participants in 14 randomised Anderson JW, Elam MB, Faas FH, Lin-
Nieminen MS, Omvik P, Oparil S, trials of statins. Lancet 2005;366:1267– ares E, Schaefer EJ, Schectman G, Wilt
Wedel H, Aurup P, Edelman J, Snapinn 1278 TJ, Wittes J. Gemfibrozil for the second-
S, LIFE Study Group. Cardiovascular 211. Pyŏrälä K, Pedersen TR, Kjekshus J, ary prevention of coronary heart disease
morbidity and mortality in patients with Faergeman O, Olsson AG, Thorgeirsson in men with low levels of high-density
diabetes in the Losartan Intervention For G. Cholesterol lowering with simvasta- lipoprotein cholesterol. Veterans Affairs
Endpoint reduction in hypertension tin improves prognosis of diabetic pa- High-Density Lipoprotein Cholesterol
study (LIFE): a randomised trial against tients with coronary heart disease: a Intervention Trial Study Group. N Engl
atenolol. Lancet 2002;359:1004 –1010 subgroup analysis of the Scandinavian J Med 1999;341:410 – 418
204. Berl T, Hunsicker LG, Lewis JB, Pfeffer Simvastatin Survival Study (4S). Diabe- 220. Frick MH, Elo O, Haapa K, Heinonen
MA, Porush JG, Rouleau JL, Drury PL, tes Care 1997;20:614 – 620 OP, Heinsalmi P, Helo P, Huttunen JK,
Esmatjes E, Hricik D, Parikh CR, Raz I, 212. Collins R, Armitage J, Parish S, Sleigh P, Kaitaniemi P, Koskinen P, Manninen V:
Vanhille P, Wiegmann TB, Wolfe BM, Peto R, Heart Protection Study Collabo- Helsinki Heart Study: primary-preven-
Locatelli F, Goldhaber SZ, Lewis EJ, rative Group: MRC/BHF Heart Protec- tion trial with gemfibrozil in middle-
Irbesartan Diabetic Nephropathy Trial. tion Study of cholesterol-lowering with aged men with dyslipidemia: safety of
Collaborative Study Group. Collabora- simvastatin in 5963 people with diabe- treatment, changes in risk factors, and
tive Study Group. Cardiovascular out- tes: a randomised placebo-controlled incidence of coronary heart disease.
comes in the Irbesartan Diabetic trial. Lancet 2003;361:2005–2016 N Engl J Med 1987;317:1237–1245
Nephropathy Trial of patients with type 213. Goldberg RB, Mellies MJ, Sacks FM, 221. Keech A, Simes RJ, Barter P, Best J, Scott
2 diabetes and overt nephropathy. Ann Moyé LA, Howard BV, Howard WJ, R, Taskinen MR, Forder P, Pillai A, Davis
Intern Med 2003;138:542–549 Davis BR, Cole TG, Pfeffer MA, Braun- T, Glasziou P, Drury P, Kesäniemi YA,
205. Laffel LM, McGill JB, Gans DJ. The ben- wald E. Cardiovascular events and their Sullivan D, Hunt D, Colman P, d’Emden
eficial effect of angiotensin-converting reduction with pravastatin in diabetic M, Whiting M, Ehnholm C, Laakso M,
enzyme inhibition with captopril on di- and glucose-intolerant myocardial in- FIELD study investigators. Effects of
abetic nephropathy in normotensive farction survivors with average choles- long-term fenofibrate therapy on cardio-
IDDM patients with microalbuminuria. terol levels: subgroup analyses in the vascular events in 9795 people with type
North American Microalbuminuria cholesterol and recurrent events (CARE) 2 diabetes mellitus (the FIELD study):
Study Group. Am J Med 1995;99:497– trial. The Care Investigators. Circulation randomised controlled trial. Lancet
504 1998;98:2513–2519 2005;366:1849 –1861
206. Bakris GL, Williams M, Dworkin L, El- 214. Shepherd J, Barter P, Carmena R, Deed- 222. Expert Panel on Detection, Evaluation,
liott WJ, Epstein M, Toto R, Tuttle K, wania P, Fruchart JC, Haffner S, Hsia J, and Treatment of High Blood Choles-
Douglas J, Hsueh W, Sowers J. Preserv- Breazna A, LaRosa J, Grundy S, Waters terol in Adults: Executive Summary of
ing renal function in adults with hyper- D. Effect of lowering LDL cholesterol The Third Report of The National Cho-
tension and diabetes: a consensus substantially below currently recom- lesterol Education Program (NCEP) Ex-
approach: National Kidney Foundation mended levels in patients with coronary pert Panel on Detection, Evaluation,
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S55
Standards of Medical Care
And Treatment of High Blood Choles- study: A randomized trial. Arterial Dis- Force recommendation statement. Ann
terol In Adults (Adult Treatment Panel ease Multiple Intervention Trial. JAMA Intern Med 2009;150:396 – 404
III). JAMA 2001;285:2486 –2497 2000;284:1263–1270 239. Ogawa H, Nakayama M, Morimoto T,
223. Hayward RA, Hofer TP, Vijan S. Nar- 231. Grundy SM, Vega GL, McGovern ME, Uemura S, Kanauchi M, Doi N, Jinnou-
rative review: lack of evidence for rec- Tulloch BR, Kendall DM, Fitz-Patrick D, chi H, Sugiyama S, Saito Y, Japanese Pri-
ommended low-density lipoprotein Ganda OP, Rosenson RS, Buse JB, Rob- mary Prevention of Atherosclerosis With
treatment targets: a solvable problem. ertson DD, Sheehan JP, Diabetes Multi- Aspirin for Diabetes (JPAD) Trial Inves-
Ann Intern Med 2006;145:520 –530 center Research Group. Efficacy, safety, tigators. Low-dose aspirin for primary
224. Cannon CP, Braunwald E, McCabe CH, and tolerability of once-daily niacin for prevention of atherosclerotic events in
Rader DJ, Rouleau JL, Belder R, Joyal SV, the treatment of dyslipidemia associated patients with type 2 diabetes: a random-
Hill KA, Pfeffer MA, Skene AM, Prava- with type 2 diabetes: results of the as- ized controlled trial. JAMA 2008;300:
statin or Atorvastatin Evaluation and sessment of diabetes control and evalu- 2134 –2141
Infection Therapy-Thrombolysis in ation of the efficacy of niaspan trial. Arch 240. Belch J, MacCuish A, Campbell I, Cobbe
Myocardial Infarction 22 Investigators. Intern Med 2002;162:1568 –1576 S, Taylor R, Prescott R, Lee R, Bancroft J,
Intensive versus moderate lipid lowering 232. Jones PH, Davidson MH. Reporting rate MacEwan S, Shepherd J, Macfarlane P,
with statins after acute coronary syn- of rhabdomyolysis with fenofibrate ⫹ Morris A, Jung R, Kelly C, Connacher A,
dromes. N Engl J Med 2004;350:1495– statin versus gemfibrozil ⫹ any statin. Peden N, Jamieson A, Matthews D, Leese
1504 Am J Cardiol 2005;95:120 –122 G, McKnight J, O’Brien I, Semple C, Pet-
225. de Lemos JA, Blazing MA, Wiviott SD, 233. Brunzell JD, Davidson M, Furberg CD, rie J, Gordon D, Pringle S, MacWalter R.
Lewis EF, Fox KA, White HD, Rouleau Goldberg RB, Howard BV, Stein JH, Wit- The prevention of progression of arterial
JL, Pedersen TR, Gardner LH, Mukher- ztum JL, American Diabetes Association, disease and diabetes (POPADAD) trial:
jee R, Ramsey KE, Palmisano J, Bilhei- American College of Cardiology Foun- factorial randomised placebo controlled
mer DW, Pfeffer MA, Califf RM, dation. Lipoprotein management in trial of aspirin and antioxidants in pa-
Braunwald E, A to Z Investigators. Early patients with cardiometabolic risk: con- tients with diabetes and asymptomatic
intensive vs a delayed conservative sim- sensus statement from the American Di- peripheral arterial disease. BMJ 2008;
vastatin strategy in patients with acute abetes Association and the American 337:a1840
coronary syndromes: phase Z of the A to College of Cardiology Foundation. Dia- 241. Pignone M, Earnshaw S, Tice JA,
Z trial. JAMA 2004;292:1307–1316 betes Care 2008;31:811– 822 Pletcher MJ. Aspirin, statins, or both
226. Nissen SE, Tuzcu EM, Schoenhagen P, 234. Colhoun HM, Betteridge DJ, Durrington drugs for the primary prevention of cor-
Brown BG, Ganz P, Vogel RA, Crowe T, PN, Hitman GA, Neil HA, Livingstone SJ, onary heart disease events in men: a
Howard G, Cooper CJ, Brodie B, Grines Thomason MJ, Mackness MI, Charlton- cost-utility analysis. Ann Intern Med
CL, DeMaria AN, REVERSAL Investiga- Menys V, Fuller JH, CARDS investigators. 2006;144:326 –336
tors. Effect of intensive compared with Primary prevention of cardiovascular dis- 242. Campbell CL, Smyth S, Montalescot G,
moderate lipid-lowering therapy on pro- ease with atorvastatin in type 2 diabetes in Steinhubl SR. Aspirin dose for the pre-
gression of coronary atherosclerosis: a the Collaborative Atorvastatin Diabetes vention of cardiovascular disease: a sys-
randomized controlled trial. JAMA Study (CARDS): multicentre randomised tematic review. JAMA 2007;297:2018 –
2004;291:1071–1080 placebo-controlled trial. Lancet 2004;364: 2024
227. Grundy SM, Cleeman JI, Merz CN, 685– 696 243. Davì G, Patrono C. Platelet activation
Brewer HB Jr, Clark LT, Hunninghake 235. Buse JB, Ginsberg HN, Bakris GL, Clark and atherothrombosis. N Engl J Med
DB, Pasternak RC, Smith SC Jr, Stone NJ, NG, Costa F, Eckel R, Fonseca V, Ger- 2007;357:2482–2494
National Heart, Lung, and Blood Institute, stein HC, Grundy S, Nesto RW, Pignone 244. Watala C, Golanski J, Pluta J, Boncler M,
American College of Cardiology Founda- MP, Plutzky J, Porte D, Redberg R, Stit- Rozalski M, Luzak B, Kropiwnicka A,
tion, American Heart Association. Impli- zel KF, Stone NJ, American Heart Asso- Drzewoski J. Reduced sensitivity of
cations of recent clinical trials for the ciation, American Diabetes Association. platelets from type 2 diabetic patients to
National Cholesterol Education Program Primary prevention of cardiovascular acetylsalicylic acid (aspirin)-its relation
Adult Treatment Panel III guidelines. Cir- diseases in people with diabetes melli- to metabolic control. Thromb Res 2004;
culation 2004;110:227–239 tus: a scientific statement from the 113:101–113
228. Chasman DI, Posada D, Subrahmanyan American Heart Association and the 245. Lev EI. Aspirin resistance transient lab-
L, Cook NR, Stanton VP, Jr, Ridker PM. American Diabetes Association. Diabe- oratory finding or important clinical en-
Pharmacogenetic study of statin therapy tes Care 2007;30:162–172 tity? J Am Coll Cardiol 2009;53:678 –
and cholesterol reduction. JAMA 2004; 236. Antithrombotic Trialists’ (ATT) Collab- 680
291:2821–2827 oration, Baigent C, Blackwell L, Collins 246. Santilli F, Rocca B, De Cristofaro R, Lat-
229. Baigent C, Keech A, Kearney PM, Black- R, Emberson J, Godwin J, Peto R, Buring tanzio S, Pietrangelo L, Habib A, Petti-
well L, Buck G, Pollicino C, Kirby A, J, Hennekens C, Kearney P, Meade T, nella C, Recchiuti A, Ferrante E,
Sourjina T, Peto R, Collins R, Simes R, Patrono C, Roncaglioni MC, Zanchetti Ciabattoni G, Davì G, Patrono C. Platelet
Cholesterol Treatment Trialists’ (CTT) A. Aspirin in the primary and secondary cyclooxygenase inhibition by low-dose
Collaborators. Efficacy and safety of prevention of vascular disease: collabo- aspirin is not reflected consistently by
cholesterol-lowering treatment: pro- rative meta-analysis of individual partic- platelet function assays: implications for
spective meta-analysis of data from ipant data from randomised trials. aspirin “resistance”. J Am Coll Cardiol
90,056 participants in 14 randomised Lancet 2009;373:1849 –1860 2009;53:667– 677
trials of statins. Lancet 2005;366:1267– 237. Wolff T, Miller T, Ko S. Aspirin for the 247. Bhatt DL, Marso SP, Hirsch AT, Ringleb
1278 primary prevention of cardiovascular PA, Hacke W, Topol EJ. Amplified ben-
230. Elam MB, Hunninghake DB, Davis KB, events: an update of the evidence for the efit of clopidogrel versus aspirin in pa-
Garg R, Johnson C, Egan D, Kostis JB, U.S. Preventive Services Task Force. tients with diabetes mellitus. Am J
Sheps DS, Brinton EA. Effect of niacin on Ann Intern Med 2009;150:405– 410 Cardiol 2002;90:625– 628
lipid and lipoprotein levels and glycemic 238. US Preventive Services Task Force: As- 248. Haire-Joshu D, Glasgow RE, Tibbs TL.
control in patients with diabetes and pe- pirin for the prevention of cardiovascu- Smoking and diabetes. Diabetes Care
ripheral arterial disease: the ADMIT lar disease: U.S. Preventive Services Task 1999;22:1887–1898
S56 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
249. American Diabetes Asociation: Smoking cet 2008;372:1174 –1183 2 diabetes. N Engl J Med 2001;345:851–
and diabetes (Position Statement). Dia- 259. Garg JP, Bakris GL. Microalbuminuria: 860
betes Care 2004;27(Suppl. 1):S74 –S75 marker of vascular dysfunction, risk fac- 270. Brenner BM, Cooper ME, de Zeeuw D,
250. US Preventive Services Task Force. tor for cardiovascular disease. Vasc Med Keane WF, Mitch WE, Parving HH, Re-
Counseling to Prevent Tobacco Use and To- 2002;7:35– 43 muzzi G, Snapinn SM, Zhang Z, Shahin-
bacco-Related Diseases: Recommendation 260. Klausen K, Borch-Johnsen K, Feldt-Ras- far S, RENAAL Study Investigators.
Statement. Rockville, MD, Agency for mussen B, Jensen G, Clausen P, Effects of losartan on renal and cardio-
Healthcare Research and Quality, 2003 Scharling H, Appleyard M, Jensen JS. vascular outcomes in patients with type
251. Ranney L, Melvin C, Lux L, McClain E, Very low levels of microalbuminuria are 2 diabetes and nephropathy. N Engl
Lohr KN. Systematic review: smoking associated with increased risk of coro- J Med 2001;345:861– 869
cessation intervention strategies for nary heart disease and death indepen- 271. Parving HH, Lehnert H, Bröchner-
adults and adults in special populations. dently of renal function, hypertension, Mortensen J, Gomis R, Andersen S,
Ann Intern Med 2006;145:845– 856 and diabetes. Circulation 2004;110: Arner P, Irbesartan in Patients with Type
252. Scognamiglio R, Negut C, Ramondo A, 32–35 2 Diabetes and Microalbuminuria Study
Tiengo A, Avogaro A. Detection of coro- 261. Gall MA, Hougaard P, Borch-Johnsen K, Group. The effect of irbesartan on the
nary artery disease in asymptomatic pa- Parving HH. Risk factors for develop- development of diabetic nephropathy in
tients with type 2 diabetes mellitus. J Am ment of incipient and overt diabetic ne- patients with type 2 diabetes. N Engl
Coll Cardiol 2006;47:65–71 phropathy in patients with non-insulin J Med 2001;345:870 – 878
253. Boden WE, O’Rourke RA, Teo KK, Har- dependent diabetes mellitus: prospec- 272. Pepine CJ, Handberg EM, Cooper-De-
tigan PM, Maron DJ, Kostuk WJ, Knudt- tive, observational study. BMJ 1997;314: Hoff RM, Marks RG, Kowey P, Messerli
son M, Dada M, Casperson P, Harris CL, 783–788 FH, Mancia G, Cangiano JL, Garcia-Bar-
Chaitman BR, Shaw L, Gosselin G, 262. Ravid M, Lang R, Rachmani R, Lishner reto D, Keltai M, Erdine S, Bristol HA,
Nawaz S, Title LM, Gau G, Blaustein AS, M. Long-term renoprotective effect of Kolb HR, Bakris GL, Cohen JD, Parmley
Booth DC, Bates ER, Spertus JA, Berman angiotensin-converting enzyme inhibi- WW, INVEST Investigators. A calcium
DS, Mancini GB, Weintraub WS, tion in non-insulin-dependent diabetes antagonist vs a non-calcium antagonist
COURAGE Trial Research Group. Opti- mellitus. A 7-year follow-up study. Arch hypertension treatment strategy for pa-
mal medical therapy with or without PCI Intern Med 1996;156:286 –289 tients with coronary artery disease: the
for stable coronary disease. N Engl J Med 263. Reichard P, Nilsson BY, Rosenqvist U. The International Verapamil-Trandolapril
2007;356:1503–1516 effect of long-term intensified insulin study (INVEST): a randomized con-
254. BARI 2D Study Group, Frye RL, August treatment on the development of micro- trolled trial. JAMA 2003;290:2805–
P, Brooks MM, Hardison RM, Kelsey SF, vascular complications of diabetes melli- 2816
MacGregor JM, Orchard TJ, Chaitman tus. N Engl J Med 1993;329:304 –309 273. Bakris GL, Siomos M, Richardson D,
BR, Genuth SM, Goldberg SH, Hlatky 264. Effect of intensive therapy on the devel- Janssen I, Bolton WK, Hebert L, Agarwal
MA, Jones TL, Molitch ME, Nesto RW, opment and progression of diabetic ne- R, Catanzaro D. ACE inhibition or an-
Sako EY, Sobel BE. A randomized trial of phropathy in the Diabetes Control and giotensin receptor blockade: impact on
therapies for type 2 diabetes and coro- Complications Trial. The Diabetes Con- potassium in renal failure. VAL-K Study
nary artery disease. N Engl J Med 2009; trol and Complications (DCCT) Re- Group. Kidney Int 2000;58:2084 –2092
360:2503–2515 search Group. Kidney Int 1995;47: 274. Mogensen CE, Neldam S, Tikkanen I,
255. Wackers FJ, Chyun DA, Young LH, 1703–1720 Oren S, Viskoper R, Watts RW, Cooper
Heller GV, Iskandrian AE, Davey JA, 265. Lewis EJ, Hunsicker LG, Bain RP, Rohde ME. Randomised controlled trial of dual
Barrett EJ, Taillefer R, Wittlin SD, Filip- RD. The effect of angiotensin-convert- blockade of renin-angiotensin system in
chuk N, Ratner RE, Inzucchi SE: Reso- ing-enzyme inhibition on diabetic ne- patients with hypertension, microalbu-
lution of asymptomatic myocardial phropathy. The Collaborative Study minuria, and non-insulin dependent di-
ischemia in patients with type 2 diabetes Group. N Engl J Med 1993;329:1456 – abetes: the candesartan and lisinopril
mellitus in the DIAD Study. Diabetes 1462 microalbuminuria (CALM) study. BMJ
Care 2007;30:2892–2898 266. Remuzzi G, Macia M, Ruggenenti P. Pre- 2000;321:1440 –1444
256. Young LH, Wackers FJ, Chyun DA, vention and treatment of diabetic renal 275. Schjoedt KJ, Jacobsen P, Rossing K,
Davey JA, Barrett EJ, Taillefer R, Heller disease in type 2 diabetes: the BENE- Boomsma F, Parving HH. Dual blockade
GV, Iskandrian AE, Wittlin SD, Filip- DICT study. JAmSocNephrol 2006;17: of the renin-angiotensin-aldosterone
chuk N, Ratner RE, Inzucchi SE, DIAD S90 –S97 system in diabetic nephropathy: the role
Investigators. Cardiac outcomes after 267. Bilous R, Chaturvedi N, Sjølie AK, Fuller of aldosterone. Horm Metab Res 2005;
screening for asymptomatic coronary ar- J, Klein R, Orchard T, Porta M, Parving 37(Suppl. 1):4 – 8
tery disease in patients with type 2 dia- HH. Effect of candesartan on microalbu- 276. Schjoedt KJ, Rossing K, Juhl TR,
betes: the DIAD study: a randomized minuria and albumin excretion rate in Boomsma F, Rossing P, Tarnow L, Parv-
controlled trial. JAMA 2009;301:1547– diabetes: three randomized trials. Ann ing HH. Beneficial impact of spironolac-
1555 Intern Med 2009;151:11–14 tone in diabetic nephropathy. Kidney
257. Braunwald E, Domanski MJ, Fowler SE, 268. Mauer M, Zinman B, Gardiner R, Suissa Int 2005;68:2829 –2836
Geller NL, Gersh BJ, Hsia J, Pfeffer MA, S, Sinaiko A, Strand T, Drummond K, 277. Parving HH, Persson F, Lewis JB, Lewis
Rice MM, Rosenberg YD, Rouleau JL, Donnelly S, Goodyer P, Gubler MC, EJ, Hollenberg NK, AVOID Study Inves-
PEACE Trial Investigators. Angiotensin- Klein R. Renal and retinal effects of ena- tigators. Aliskiren combined with losar-
converting-enzyme inhibition in stable lapril and losartan in type 1 diabetes. tan in type 2 diabetes and nephropathy.
coronary artery disease. N Engl J Med N Engl J Med 2009;361:40 –51 N Engl J Med 2008;358:2433–2446
2004;351:2058 –2068 269. Lewis EJ, Hunsicker LG, Clarke WR, 278. Pijls LT, de Vries H, Donker AJ, van Eijk
258. Effects of the angiotensin-receptor Berl T, Pohl MA, Lewis JB, Ritz E, Atkins JT. The effect of protein restriction on
blocker telmisartan on cardiovascular RC, Rohde R, Raz I, Collaborative Study albuminuria in patients with type 2 dia-
events in high-risk patients intolerant to Group. Renoprotective effect of the an- betes mellitus: a randomized trial.
angiotensin-converting enzyme inhibi- giotensin-receptor antagonist irbesartan Nephrol Dial Transplant 1999;14:1445–
tors: a randomised controlled trial. Lan- in patients with nephropathy due to type 1453
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S57
Standards of Medical Care
279. Pedrini MT, Levey AS, Lau J, Chalmers ment). Diabetes Care 2004;27(Suppl. 304. American Diabetes Association: Reti-
TC, Wang PH. The effect of dietary pro- 1):S79 –S83 nopathy in diabetes. Diabetes Care
tein restriction on the progression of di- 291. Klein R. Hyperglycemia and microvas- 2004;27 Suppl. 1:S84 –S87
abetic and nondiabetic renal diseases: a cular and macrovascular disease in dia- 305. Ciulla TA, Amador AG, Zinman B. Dia-
meta-analysis. Ann Intern Med 1996; betes. Diabetes Care 1995;18:258 –268 betic retinopathy and diabetic macular
124:627– 632 292. Estacio RO, McFarling E, Biggerstaff S, edema: pathophysiology, screening, and
280. Hansen HP, Tauber-Lassen E, Jensen Jeffers BW, Johnson D, Schrier RW. novel therapies. Diabetes Care 2003;26:
BR, Parving HH. Effect of dietary protein Overt albuminuria predicts diabetic ret- 2653–2664
restriction on prognosis in patients with inopathy in Hispanics with NIDDM. 306. Boulton AJ, Vinik AI, Arezzo JC, Bril V,
diabetic nephropathy. Kidney Int 2002; Am J Kidney Dis 1998;31:947–953 Feldman EL, Freeman R, Malik RA, Ma-
62:220 –228 293. Leske MC, Wu SY, Hennis A, Hyman L, ser RE, Sosenko JM, Ziegler D, American
281. Kasiske BL, Lakatua JD, Ma JZ, Louis TA. Nemesure B, Yang L, Schachat AP, Bar- Diabetes Association. Diabetic neuropa-
A meta-analysis of the effects of dietary bados Eye Study Group. Hyperglycemia, thies: a statement by the American Dia-
protein restriction on the rate of decline blood pressure, and the 9-year incidence betes Association. Diabetes Care 2005;
in renal function. Am J Kidney Dis 1998; of diabetic retinopathy: the Barbados 28:956 –962
31:954 –961 Eye Studies. Ophthalmology 2005;112: 307. Vinik AI, Maser RE, Mitchell BD, Free-
282. Eknoyan G, Hostetter T, Bakris GL, He- 799 – 805 man R. Diabetic autonomic neuropathy.
bert L, Levey AS, Parving HH, Steffes 294. Fong DS, Aiello LP, Ferris FL 3rd, Klein Diabetes Care 2003;26:1553–1579
MW, Toto R. Proteinuria and other R. Diabetic retinopathy. Diabetes Care 308. Boulton AJ, Armstrong DG, Albert SF,
markers of chronic kidney disease: a po- 2004;27:2540 –2553 Frykberg RG, Hellman R, Kirkman MS,
sition statement of the national kidney 295. Diabetes Control and Complications Lavery LA, Lemaster JW, Mills JL Sr,
foundation (NKF) and the national insti- Trial Research Group: Effect of preg- Mueller MJ, Sheehan P, Wukich DK,
tute of diabetes and digestive and kidney nancy on microvascular complications American Diabetes Association, Ameri-
diseases (NIDDK). Am J Kidney Dis in the diabetes control and complica- can Association of Clinical Endocrinolo-
2003;42:617– 622 tions trial. The Diabetes Control and gists. Comprehensive foot examination
283. Levey AS, Coresh J, Balk E, Kausz AT, Complications Trial Research Group. and risk assessment: a report of the task
Levin A, Steffes MW, Hogg RJ, Perrone Diabetes Care 2000;23:1084 –1091 force of the foot care interest group of
RD, Lau J, Eknoyan G, National Kidney 296. The Diabetic Retinopathy Study (DRS) the American Diabetes Association, with
Foundation. National Kidney Founda- Research Group. Preliminary report on endorsement by the American Associa-
tion practice guidelines for chronic kid- the effects of photocoagulation therapy: tion of Clinical Endocrinologists. Diabe-
ney disease: evaluation, classification, DRS Report #1. Am J Ophthalmol 1976; tes Care 2008;31:1679 –1685
and stratification. Ann Intern Med 2003; 81:383–396. 309. American Diabetes Association: Periph-
139:137–147 297. Photocoagulation for diabetic macular eral arterial disease in people with dia-
284. Kramer H, Molitch ME. Screening for edema. Early Treatment Diabetic Reti- betes (Consensus Statement). Diabetes
kidney disease in adults with diabetes. nopathy Study report number 1. Early Care 2003;26:3333–3341
Diabetes Care 2005;28:1813–1816 Treatment Diabetic Retinopathy Study 310. American Diabetes Association: Consen-
285. Kramer HJ, Nguyen QD, Curhan G, Hsu research group. Arch Ophthalmol 1985; sus Development Conference on Dia-
CY. Renal insufficiency in the absence of 103:1796 –1806 betic Foot Wound Care, 7– 8 April
albuminuria and retinopathy among 298. Klein R, Klein BE, Moss SE, Davis MD, 1999, Boston, Massachusetts. Diabetes
adults with type 2 diabetes mellitus. DeMets DL. The Wisconsin epidemiologic Care 1999;22:1354 –1360
JAMA 2003;289:3273–3277 study of diabetic retinopathy. II. Preva- 311. Silverstein J, Klingensmith G, Copeland
286. Tsalamandris C, Allen TJ, Gilbert RE, lence and risk of diabetic retinopathy KC, Plotnick L, Kaufman F, Laffel L,
Sinha A, Panagiotopoulos S, Cooper ME, when age at diagnosis is less than 30 years. Deeb LC, Grey M, Anderson BJ, Hol-
Jerums G. Progressive decline in renal Arch Ophthalmol 1984;102:520 –526 zmeister LA, and Clark NG Care of chil-
function in diabetic patients with and 299. Harris MI, Klein R, Welborn TA, dren and adolescents with type 1
without albuminuria. Diabetes 1994;43: Knuiman MW. Onset of NIDDM occurs diabetes mellitus: A statement of the
649 – 655 at least 4 –7 yr before clinical diagnosis. American Diabetes Association. Diabe-
287. Levey AS, Bosch JP, Lewis JB, Greene T, Diabetes Care 1992;15:815– 819 tes Care 2005; 28:186 –212.
Rogers N, Roth D. A more accurate 300. Vijan S, Hofer TP, Hayward RA. Cost- 312. Northam EA, Anderson PJ, Werther GA,
method to estimate glomerular filtration utility analysis of screening intervals for Warne GL, Adler RG, Andrewes D. Neu-
rate from serum creatinine: a new pre- diabetic retinopathy in patients with ropsychological complications of IDDM
diction equation. Modification of Diet in type 2 diabetes mellitus. JAMA 2000; in children 2 years after disease onset.
Renal Disease Study Group. Ann Intern 283:889 – 896 Diabetes Care 1998;21:379 –384
Med 1999;130:461– 470 301. Klein R. Screening interval for retinopa- 313. Rovet J, Alvarez M. Attentional function-
288. Rigalleau V, Lasseur C, Perlemoine C, thy in type 2 diabetes. Lancet 2003;361: ing in children and adolescents with
Barthe N, Raffaitin C, Liu C, Chauveau 190 –191 IDDM. Diabetes Care 1997;20:803– 810
P, Baillet-Blanco L, Beauvieux MC, 302. Younis N, Broadbent DM, Vora JP, Har- 314. Bjørgaas M, Gimse R, Vik T, Sand T.
Combe C, Gin H. Estimation of glomer- ding SP, Liverpool Diabetic Eye Study. Cognitive function in type 1 diabetic
ular filtration rate in diabetic subjects: Incidence of sight-threatening retinopa- children with and without episodes of
Cockcroft formula or modification of thy in patients with type 2 diabetes in the severe hypoglycaemia. Acta Paediatr
Diet in Renal Disease study equation? Liverpool Diabetic Eye Study: a cohort 1997;86:148 –153
Diabetes Care 2005;28:838 – 843 study. Lancet 2003;361:195–200 315. Doyle EA, Weinzimer SA, Steffen AT,
289. Levinsky NG. Specialist evaluation in 303. Ahmed J, Ward TP, Bursell SE, Aiello Ahern JA, Vincent M, Tamborlane WV.
chronic kidney disease: too little, too LM, Cavallerano JD, Vigersky RA. The A randomized, prospective trial compar-
late. Ann Intern Med 2002;137:542– sensitivity and specificity of nonmydri- ing the efficacy of continuous subcuta-
543 atic digital stereoscopic retinal imaging neous insulin infusion with multiple
290. American Diabetes Association: Ne- in detecting diabetic retinopathy. Diabe- daily injections using insulin glargine.
phropathy in diabetes (Position State- tes Care 2006;29:2205–2209 Diabetes Care 2004;27:1554 –1558
S58 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
316. Nimri R, Weintrob N, Benzaquen H, Hypertension, and Obesity in Youth in children and adolescents with Type 1
Ofan R, Fayman G, Phillip M. Insulin Committee, American Heart Association diabetes. Diabet Med 2002;19:518 –521
pump therapy in youth with type 1 dia- Council of Cardiovascular Disease in the 332. Mohn A, Di Michele S, Di Luzio R,
betes: a retrospective paired study. Pedi- Young, American Heart Association Tumini S, Chiarelli F. The effect of sub-
atrics 2006;117:2126 –2131 Council on Cardiovascular Nursing. clinical hypothyroidism on metabolic
317. Krantz JS, Mack WJ, Hodis HN, Liu CR, Drug therapy of high-risk lipid abnor- control in children and adolescents with
Liu CH, Kaufman FR. Early onset of sub- malities in children and adolescents: a Type 1 diabetes mellitus. Diabet Med
clinical atherosclerosis in young persons scientific statement from the American 2002;19:70 –73
with type 1 diabetes. J Pediatr 2004;145: Heart Association Atherosclerosis, Hy- 333. Chase HP, Garg SK, Cockerham RS,
452– 457 pertension, and Obesity in Youth Com- Wilcox WD, Walravens PA. Thyroid
318. Järvisalo MJ, Putto-Laurila A, Jartti L, mittee, Council of Cardiovascular hormone replacement and growth of
Lehtimäki T, Solakivi T, Rönnemaa T, Disease in the Young, with the Council children with subclinical hypothyroid-
Raitakari OT. Carotid artery intima-me- on Cardiovascular Nursing. Circulation ism and diabetes. Diabet Med 1990;7:
dia thickness in children with type 1 di- 2007;115:1948 –1967 299 –303
abetes. Diabetes 2002;51:493– 498 323. Salo P, Viikari J, Hämäläinen M, Lapin- 334. Eppens MC, Craig ME, Cusumano J,
319. Haller MJ, Samyn M, Nichols WW, leimu H, Routi T, Rönnemaa T, Sep- Hing S, Chan AK, Howard NJ, Silink M,
Brusko T, Wasserfall C, Schwartz RF, At- pänen R, Jokinen E, Välimäki I, Simell Donaghue KC. Prevalence of diabetes
kinson M, Shuster JJ, Pierce GL, Silver- O. Serum cholesterol ester fatty acids in complications in adolescents with type 2
stein JH. Radial artery tonometry 7- and 13-month-old children in a pro- compared with type 1 diabetes. Diabetes
demonstrates arterial stiffness in chil- spective randomized trial of a low-satu- Care 2006;29:1300 –1306
dren with type 1 diabetes. Diabetes Care rated fat, low-cholesterol diet: the STRIP 335. Kitzmiller JL, Gavin LA, Gin GD, Jo-
2004;27:2911–2917 baby project. Special Turku coronary vanovic-Peterson L, Main EK, Zigrang
320. Orchard TJ, Forrest KY, Kuller LH, Risk factor Intervention Project for chil- WD. Preconception care of diabetes.
Becker DJ, Pittsburgh Epidemiology of dren. Acta Paediatr 1999;88:505–512 Glycemic control prevents congenital
Diabetes Complications Study. Lipid 324. Efficacy and safety of lowering dietary anomalies. JAMA 1991;265:731–736
and blood pressure treatment goals for intake of fat and cholesterol in children 336. Goldman JA, Dicker D, Feldberg D, Ye-
type 1 diabetes: 10-year incidence data with elevated low-density lipoprotein shaya A, Samuel N, Karp M. Pregnancy
from the Pittsburgh Epidemiology of Di- cholesterol. The Dietary Intervention outcome in patients with insulin-depen-
abetes Complications Study. Diabetes Study in Children (DISC). The Writing dent diabetes mellitus with preconcep-
Care 2001;24:1053–1059 Group for the DISC Collaborative Re- tional diabetic control: a comparative
321. Kavey RE, Allada V, Daniels SR, Hayman search Group. JAMA 1995;273:1429 – study. AmJ Obstet Gynecol 1986;155:
LL, McCrindle BW, Newburger JW, 1435 293–297
Parekh RS, Steinberger J, American 325. McCrindle BW, Ose L, Marais AD. Effi- 337. Rosenn B, Miodovnik M, Combs CA,
Heart Association Expert Panel on Pop- cacy and safety of atorvastatin in chil- Khoury J, Siddiqi TA. Pre-conception
ulation and Prevention Science, Ameri- dren and adolescents with familial management of insulin-dependent dia-
can Heart Association Council on hypercholesterolemia or severe hyper- betes: improvement of pregnancy out-
Cardiovascular Disease in the Young, lipidemia: a multicenter, randomized, come. Obstet Gynecol 1991;77:846 –
American Heart Association Council on placebo-controlled trial. J Pediatr 2003; 849
Epidemiology and Prevention, Ameri- 143:74 – 80 338. Tchobroutsky C, Vray MM, Altman JJ.
can Heart Association Council on Nutri- 326. de Jongh S, Lilien MR, op’t RJ, Stroes ES, Risk/benefit ratio of changing late ob-
tion, Physical Activity and Metabolism, Bakker HD, Kastelein JJ. Early statin stetrical strategies in the management of
American Heart Association Council on therapy restores endothelial function in insulin-dependent diabetic pregnancies.
High Blood Pressure Research, Ameri- children with familial hypercholesterol- A comparison between 1971–1977 and
can Heart Association Council on Car- emia. J Am Coll Cardiol 2002;40:2117– 1978 –1985 periods in 389 pregnancies.
diovascular Nursing, American Heart 2121 Diabete Metab 1991;17:287–294
Association Council on the Kidney in 327. Wiegman A, Hutten BA, de Groot E, Ro- 339. Willhoite MB, Bennert HW, Jr, Palomaki
Heart Disease, Interdisciplinary Work- denburg J, Bakker HD, Büller HR, Si- GE, Zaremba MM, Herman WH, Wil-
ing Group on Quality of Care and Out- jbrands EJ, Kastelein JJ. Efficacy and liams JR, Spear NH. The impact of pre-
comes Research. Cardiovascular risk safety of statin therapy in children with conception counseling on pregnancy
reduction in high-risk pediatric patients: familial hypercholesterolemia: a ran- outcomes. The experience of the Maine
a scientific statement from the American domized controlled trial. JAMA 2004; Diabetes in Pregnancy Program. Diabe-
Heart Association Expert Panel on Pop- 292:331–337 tes Care 1993;16:450 – 455
ulation and Prevention Science; the 328. Holmes GK. Screening for coeliac dis- 340. Cooper WO, Hernandez-Diaz S, Arbo-
Councils on Cardiovascular Disease in ease in type 1 diabetes. Arch Dis Child gast PG, Dudley JA, Dyer S, Gideon PS,
the Young, Epidemiology and Preven- 2002;87:495– 498 Hall K, Ray WA. Major congenital mal-
tion, Nutrition, Physical Activity and 329. Rewers M, Liu E, Simmons J, Redondo formations after first-trimester exposure
Metabolism, High Blood Pressure Re- MJ, Hoffenberg EJ: Celiac disease asso- to ACE inhibitors. N Engl J Med 2006;
search, Cardiovascular Nursing, and the ciated with type 1 diabetes mellitus. En- 354:2443–2451
Kidney in Heart Disease; and the Inter- docrinol Metab Clin North Am 2004;33: 341. American Diabetes Association: Precon-
disciplinary Working Group on Quality 197–214, xi ception care of women with diabetes
of Care and Outcomes Research: en- 330. Roldan MB, Alonso M, Barrio R. Thyroid (Position Statement). Diabetes Care
dorsed by the American Academy of Pe- autoimmunity in children and adoles- 2004;27(Suppl. 1):S76 –S78
diatrics. Circulation 2006;114:2710 – cents with Type 1 diabetes mellitus. Di- 342. Brown AF, Mangione CM, Saliba D,
2738 abetes Nutr Metab 1999;12:27–31 Sarkisian CA, California Healthcare
322. McCrindle BW, Urbina EM, Dennison 331. Kordonouri O, Deiss D, Danne T, Foundation/American Geriatrics Society
BA, Jacobson MS, Steinberger J, Roc- Dorow A, Bassir C, Grüters-Kieslich A. Panel on Improving Care for Elders with
chini AP, Hayman LL, Daniels SR, Amer- Predictivity of thyroid autoantibodies Diabetes. Guidelines for improving the
ican Heart Association Atherosclerosis, for the development of thyroid disorders care of the older person with diabetes
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S59
Standards of Medical Care
mellitus. J Am Geriatr Soc 2003;51: betes mellitus and acute myocardial in- 32:591–595
S265–S280 farction: long-term results from the 363. Donihi AC, Raval D, Saul M, Koryt-
343. Curb JD, Pressel SL, Cutler JA, Savage Diabetes and Insulin-Glucose Infusion in kowski MT, DeVita MA. Prevalence and
PJ, Applegate WB, Black H, Camel G, Acute Myocardial Infarction (DIGAMI) predictors of corticosteroid-related hy-
Davis BR, Frost PH, Gonzalez N, Guthrie study. Circulation 1999;99:2626 –2632 perglycemia in hospitalized patients.
G, Oberman A, Rutan GH, Stamler J. Ef- 353. Wiener RS, Wiener DC, Larson RJ. Ben- Endocr Pract 2006;12:358 –362
fect of diuretic-based antihypertensive efits and risks of tight glucose control in 364. Goldberg PA, Siegel MD, Sherwin RS,
treatment on cardiovascular disease risk critically ill adults: a meta-analysis. Halickman JI, Lee M, Bailey VA, Lee SL,
in older diabetic patients with isolated JAMA 2008;300:933–944 Dziura JD, Inzucchi SE. Implementation
systolic hypertension. Systolic Hyper- 354. Brunkhorst FM, Engel C, Bloos F, Meier- of a safe and effective insulin infusion
tension in the Elderly Program Cooper- Hellmann A, Ragaller M, Weiler N, Mo- protocol in a medical intensive care unit.
ative Research Group. JAMA 1996;276: erer O, Gruendling M, Oppert M, Grond Diabetes Care 2004;27:461– 467
1886 –1892 S, Olthoff D, Jaschinski U, John S, Ros- 365. Rea RS, Donihi AC, Bobeck M, Herout P,
344. Beckett NS, Peters R, Fletcher AE, Staes- saint R, Welte T, Schaefer M, Kern P, McKaveney TP, Kane-Gill SL, Koryt-
sen JA, Liu L, Dumitrascu D, Stoyanovsky Kuhnt E, Kiehntopf M, Hartog C, Natan- kowski MT. Implementing an intrave-
V, Antikainen RL, Nikitin Y, Anderson C, son C, Loeffler M, Reinhart K, German nous insulin infusion protocol in the
Belhani A, Forette F, Rajkumar C, Thijs L, Competence Network Sepsis (SepNet). intensive care unit. Am J Health Syst
Banya W, Bulpitt CJ, HYVET Study Intensive insulin therapy and pen- Pharm 2007;64:385–395
Group. Treatment of hypertension in pa- tastarch resuscitation in severe sepsis. 366. Nazer LH, Chow SL, Moghissi ES. Insu-
tients 80 years of age or older. N Engl N Engl J Med 2008;358:125–139 lin infusion protocols for critically ill pa-
J Med 2008;358:1887–1898 355. NICE-SUGAR Study Investigators, Fin- tients: a highlight of differences and
345. Clement S, Braithwaite SS, Magee MF, fer S, Chittock DR, Su SY, Blair D, Foster similarities. Endocr Pract 2007;13:137–
Ahmann A, Smith EP, Schafer RG, Hir- D, Dhingra V, Bellomo R, Cook D, 146
sch IB, Hirsh IB, American Diabetes As- Dodek P, Henderson WR, Hébert PC, 367. DeSantis AJ, Schmeltz LR, Schmidt K,
sociation Diabetes in Hospitals Writing Heritier S, Heyland DK, McArthur C, O’Shea-Mahler E, Rhee C, Wells A,
Committee. Management of diabetes McDonald E, Mitchell I, Myburgh JA, Brandt S, Peterson S, Molitch ME. Inpa-
and hyperglycemia in hospitals. Diabe- Norton R, Potter J, Robinson BG, Ronco tient management of hyperglycemia: the
tes Care 2004;27:553–591 JJ. Intensive versus conventional glucose Northwestern experience. Endocr Pract
346. Moghissi ES, Korytkowski MT, DiNardo control in critically ill patients. N Engl 2006;12:491–505
M, Einhorn D, Hellman R, Hirsch IB, In- J Med 2009;360:1283–1297 368. Noschese M, Donihi AC, Koerbel G,
zucchi SE, Ismail-Beigi F, Kirkman MS, 356. Krinsley JS, Grover A. Severe hypoglyce- Karslioglu E, DiNardo M, Curll M, Ko-
Umpierrez GE, American Association of mia in critically ill patients: risk factors rytkowski MT. Effect of a diabetes order
Clinical Endocrinologists, American and outcomes. Crit Care Med 2007;35: set on glycaemic management and con-
Diabetes Association. American Asso- 2262–2267 trol in the hospital. Qual Saf Health Care
ciation of Clinical Endocrinologists 357. Van den Berghe G, Wilmer A, Hermans 2008;17:464 – 468
and American Diabetes Association G, Meersseman W, Wouters PJ, Milants 369. Umpierrez GE, Hor T, Smiley D, Tem-
consensus statement on inpatient gly- I, Van Wijngaerden E, Bobbaers H, poni A, Umpierrez D, Ceron M, Munoz
cemic control. Diabetes Care 2009;32: Bouillon R. Intensive insulin therapy in C, Newton C, Peng L, Baldwin D. Com-
1119 –1131 the medical ICU. N Engl J Med 2006; parison of inpatient insulin regimens
347. American Diabetes Association: Eco- 354:449 – 461 with detemir plus aspart versus neutral
nomic costs of diabetes in the U.S. In 358. Griesdale DE, de Souza RJ, van Dam RM, protamine hagedorn plus regular in
2007. Diabetes Care 2008;31:596 – 615 Heyland DK, Cook DJ, Malhotra A, medical patients with type 2 diabetes.
348. Centers for Disease Control and Preven- Dhaliwal R, Henderson WR, Chittock J Clin Endocrinol Metab 2009;94:564 –
tion. National Diabetes Fact Sheet: Gen- DR, Finfer S, Talmor D. Intensive insulin 569
eral Information and National Estimates on therapy and mortality among critically 370. Moghissi ES, Hirsch IB. Hospital man-
Diabetes in the United States, 2007. At- ill patients: a meta-analysis including agement of diabetes. Endocrinol Metab
lanta, GA, US Department of Health and NICE-SUGAR study data. CMAJ 2009; Clin North Am 2005;34:99 –116
Human Services, 2008 180:821– 827 371. Umpierrez GE, Smiley D, Zisman A, Pri-
349. Levetan CS, Passaro M, Jablonski K, Kass 359. Saudek CD, Herman WH, Sacks DB, eto LM, Palacio A, Ceron M, Puig A, Me-
M, Ratner RE. Unrecognized diabetes Bergenstal RM, Edelman D, Davidson jia R. Randomized study of basal-bolus
among hospitalized patients. Diabetes MB. A new look at screening and diag- insulin therapy in the inpatient manage-
Care 1998;21:246 –249 nosing diabetes mellitus. J Clin Endocri- ment of patients with type 2 diabetes
350. Umpierrez GE, Isaacs SD, Bazargan N, nol Metab 2008;93:2447–2453 (RABBIT 2 trial). Diabetes Care 2007;30:
You X, Thaler LM, Kitabchi AE. Hyper- 360. Mitrakou A, Ryan C, Veneman T, Mokan 2181–2186
glycemia: an independent marker of in- M, Jenssen T, Kiss I, Durrant J, Cryer P, 372. Umpierrez GE, Palacio A, Smiley D.
hospital mortality in patients with Gerich J. Hierarchy of glycemic thresholds Sliding scale insulin use: myth or insan-
undiagnosed diabetes. J Clin Endocrinol for counterregulatory hormone secretion, ity? Am J Med 2007;120:563–567
Metab 2002;87:978 –982 symptoms, and cerebral dysfunction. Am J 373. Queale WS, Seidler AJ, Brancati FL. Gly-
351. van den Berghe G, Wouters P, Weekers Physiol 1991;260:E67–E74 cemic control and sliding scale insulin
F, Verwaest C, Bruyninckx F, Schetz M, 361. Korytkowski M, DiNardo M, Donihi AC, use in medical inpatients with diabetes
Vlasselaers D, Ferdinande P, Lauwers P, Bigi L, Devita M. Evolution of a diabetes mellitus. Arch Intern Med 1997;157:
Bouillon R. Intensive insulin therapy in inpatient safety committee. Endocr Pract 545–552
the critically ill patients. N Engl J Med 2006;12(Suppl. 3):91–99 374. Korytkowski MT, Salata RJ, Koerbel GL,
2001;345:1359 –1367 362. DiNardo M, Noschese M, Korytkowski Selzer F, Karslioglu E, Idriss AM, Lee
352. Malmberg K, Norhammar A, Wedel H, M, Freeman S. The medical emergency KK, Moser AJ, Toledo FG. Insulin ther-
Rydén L. Glycometabolic state at admis- team and rapid response system: find- apy and glycemic control in hospitalized
sion: important risk marker of mortality in ing, treating, and preventing hypoglyce- patients with diabetes during enteral nu-
conventionally treated patients with dia- mia. Jt Comm J Qual Patient Saf 2006; trition therapy: a randomized controlled
S60 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
clinical trial. Diabetes Care 2009;32: 389. D’Orazio P, Burnett RW, Fogh- 1):124 –130
594 –596 Andersen N, Jacobs E, Kuwa K, Külp- 400. Mahoney JJ. Reducing patient drug ac-
375. Hirsch IB. Sliding scale insulin–time to mann WR, Larsson L, Lewenstam A, quisition costs can lower diabetes health
stop sliding. JAMA 2009;301:213–214 Maas AH, Mager G, Naskalski JW, claims. Am J Manag Care 2005;11:
376. Umpierrez GE. Basal versus sliding-scale Okorodudu AO, International Federa- S170 –S176
regular insulin in hospitalized patients tion of Clinical Chemistry Scientific Di- 401. Maney M, Tseng CL, Safford MM, Miller
with hyperglycemia during enteral nu- vision Working Group on Selective DR, Pogach LM. Impact of self-reported
trition therapy. Diabetes Care 2009;32: Electrodes and Point of Care Testing. patient characteristics upon assessment
751–753 Approved IFCC recommendation on re- of glycemic control in the Veterans
377. Pancorbo-Hidalgo PL, García-Fernan- porting results for blood glucose (abbre- Health Administration. Diabetes Care
dez FP, Ramírez-Pérez C. Complications viated). Clin Chem 2005;51:1573–1576 2007;30:245–251
associated with enteral nutrition by na- 390. Dungan K, Chapman J, Braithwaite SS, 402. Bergenstal RM. Treatment models from
sogastric tube in an internal medicine Buse J. Glucose measurement: con- the International Diabetes Center: ad-
unit. J Clin Nurs 2001;10:482– 490 founding issues in setting targets for in- vancing from oral agents to insulin ther-
378. Nylen ES, Muller B. Endocrine changes patient management. Diabetes Care apy in type 2 diabetes. Endocr Pract
in critical illness. J Intensive Care Med 2007;30:403– 409 2006;12(Suppl. 1):98 –104
2004;19:67– 82 391. Boyd JC, Bruns DE. Quality specifica- 403. Berikai P, Meyer PM, Kazlauskaite R,
379. Shilo S, Berezovsky S, Friedlander Y, tions for glucose meters: assessment by Savoy B, Kozik K, Fogelfeld L. Gain in
Sonnenblick M. Hypoglycemia in hospi- simulation modeling of errors in insulin patients’ knowledge of diabetes manage-
talized nondiabetic older patients. J Am dose. Clin Chem 2001;47:209 –214 ment targets is associated with better
Geriatr Soc 1998;46:978 –982 392. Goldberg PA, Siegel MD, Russell RR, Sh- glycemic control. Diabetes Care 2007;
380. Fischer KF, Lees JA, Newman JH. Hypo- erwin RS, Halickman JI, Cooper DA, 30:1587–1589
glycemia in hospitalized patients. Dziura JD, Inzucchi SE. Experience with 404. O’Connor PJ. Electronic medical records
Causes and outcomes. N Engl J Med the continuous glucose monitoring sys- and diabetes care improvement: are we
1986;315:1245–1250 tem in a medical intensive care unit. Di- waiting for Godot? Diabetes Care 2003;
381. Markovitz LJ, Wiechmann RJ, Harris N, abetes Technol Ther 2004;6:339 –347 26:942–943
Hayden V, Cooper J, Johnson G, Harel- 393. Cheung BM, Ong KL, Cherny SS, Sham 405. Shojania KG, Ranji SR, McDonald KM,
stad R, Calkins L, Braithwaite SS. De- PC, Tso AW, Lam KS. Diabetes preva- Grimshaw JM, Sundaram V, Rushakoff
scription and evaluation of a glycemic lence and therapeutic target achieve- RJ, Owens DK. Effects of quality im-
management protocol for patients with ment in the United States, 1999 to 2006.
provement strategies for type 2 diabetes
diabetes undergoing heart surgery. En- Am J Med 2009;122:443– 453
on glycemic control: a meta-regression
docr Pract 2002;8:10 –18 394. Coleman K, Austin BT, Brach C, Wagner
analysis. JAMA 2006;296:427– 440
382. Levetan CS, Salas JR, Wilets IF, Zumoff EH. Evidence on the Chronic Care
406. Davidson MB. How our current medical
B. Impact of endocrine and diabetes Model in the new millennium. Health
care system fails people with diabetes:
team consultation on hospital length of Aff (Millwood) 2009;28:75– 85
lack of timely, appropriate clinical deci-
stay for patients with diabetes. Am J Med 395. Clark CM, Jr, Snyder JW, Meek RL, Stutz
1995;99:22–28 LM, Parkin CG. A systematic approach sions. Diabetes Care 2009;32:370 –372
383. Levetan CS, Passaro MD, Jablonski KA, to risk stratification and intervention 407. McLean DL, McAlister FA, Johnson JA,
Ratner RE. Effect of physician specialty within a managed care environment im- King KM, Makowsky MJ, Jones CA,
on outcomes in diabetic ketoacidosis. proves diabetes outcomes and patient Tsuyuki RT, SCRIP-HTN Investigators. A
Diabetes Care 1999;22:1790 –1795 satisfaction.DiabetesCare2001;24:1079 – randomized trial of the effect of commu-
384. Koproski J, Pretto Z, Poretsky L. Effects 1086 nity pharmacist and nurse care on improv-
of an intervention by a diabetes team in 396. Meigs JB, Cagliero E, Dubey A, Murphy- ing blood pressure management in
hospitalized patients with diabetes. Dia- Sheehy P, Gildesgame C, Chueh H, patients with diabetes mellitus: study of
betes Care 1997;20:1553–1555 Barry MJ, Singer DE, Nathan DM. A con- cardiovascular risk intervention by phar-
385. Furnary AP, Braithwaite SS. Effects of trolled trial of web-based diabetes dis- macists-hypertension (SCRIP-HTN). Arch
outcome on in-hospital transition from ease management: the MGH diabetes Intern Med 2008;168:2355–2361
intravenous insulin infusion to subcuta- primary care improvement project. Dia- 408. Parchman ML, Zeber JE, Romero RR,
neous therapy. Am J Cardiol 2006;98: betes Care 2003;26:750 –757 Pugh JA. Risk of coronary artery disease
557–564 397. O’Connor PJ, Desai J, Solberg LI, Reger in type 2 diabetes and the delivery of
386. American Diabetes Association: Diabe- LA, Crain AL, Asche SE, Pearson TL, care consistent with the chronic care
tes nutrition recommendations for Clark CK, Rush WA, Cherney LM, model in primary care settings: a STAR-
health care institutions (Position State- Sperl-Hillen JM, Bishop DB. Random- Net study. Med Care 2007;45:1129 –
ment). Diabetes Care 2004;27(Suppl. ized trial of quality improvement inter- 1134
1):S55–S57 vention to improve diabetes care in 409. Feifer C, Nemeth L, Nietert PJ, Wessell
387. Boucher JL, Swift CS, Franz MJ, primary care settings. Diabetes Care AM, Jenkins RG, Roylance L, Ornstein
Kulkarni K, Schafer RG, Pritchett E, 2005;28:1890 –1897 SM. Different paths to high-quality care:
Clark NG. Inpatient management of di- 398. Sperl-Hillen JM, O’Connor PJ. Factors three archetypes of top-performing
abetes and hyperglycemia: implications driving diabetes care improvement in a practice sites. Ann Fam Med 2007;5:
for nutrition practice and the food and large medical group: ten years of 233–241
nutrition professional. J Am Diet Assoc progress. Am J Manag Care 2005;11: 410. Ornstein S, Nietert PJ, Jenkins RG, Wes-
2007;107:105–111 S177–S185 sell AM, Nemeth LS, Feifer C, Corley
388. Scott MG, Bruns DE, Boyd JC, Sacks DB. 399. Siminerio LM. Implementing diabetes ST. Improving diabetes care through a
Tight glucose control in the intensive self-management training programs: multicomponent quality improvement
care unit: are glucose meters up to the breaking through the barriers in pri- model in a practice-based research net-
task? Clin Chem 2009;55:18 –20 mary care. EndocrPract 2006;12(Suppl. work. Am J Med Qual 2007;22:34 – 41
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S61
P O S I T I O N S T A T E M E N T
Diagnosis and Classification of Diabetes
Mellitus
AMERICAN DIABETES ASSOCIATION fore do not require insulin. Other
individuals who have some residual insu-
lin secretion but require exogenous insu-
DEFINITION AND cardiovascular symptoms and sexual dys- lin for adequate glycemic control can
DESCRIPTION OF DIABETES function. Patients with diabetes have an in- survive without it. Individuals with ex-
MELLITUS — Diabetes is a group of creased incidence of atherosclerotic tensive -cell destruction and therefore
metabolic diseases characterized by hy- cardiovascular, peripheral arterial, and ce- no residual insulin secretion require insu-
perglycemia resulting from defects in in- rebrovascular disease. Hypertension and lin for survival. The severity of the meta-
sulin secretion, insulin action, or both. abnormalities of lipoprotein metabolism are bolic abnormality can progress, regress,
The chronic hyperglycemia of diabetes is often found in people with diabetes. or stay the same. Thus, the degree of hy-
associated with long-term damage, dys- The vast majority of cases of diabetes perglycemia reflects the severity of the un-
function, and failure of differentorgans, fall into two broad etiopathogenetic cate- derlying metabolic process and its
especially the eyes, kidneys, nerves, heart, gories (discussed in greater detail below). treatment more than the nature of the
and blood vessels. In one category, type 1 diabetes, the cause process itself.
Several pathogenic processes are in- is an absolute deficiency of insulin secre-
volved in the development of diabetes. tion. Individuals at increased risk of de- CLASSIFICATION OF
These range from autoimmune destruc- veloping this type of diabetes can often be DIABETES MELLITUS AND
tion of the -cells of the pancreas with identified by serological evidence of an OTHER CATEGORIES
consequent insulin deficiency to abnor- autoimmune pathologic process occur- OF GLUCOSE
malities that result in resistance to insulin ring in the pancreatic islets and by genetic REGULATION — Assigning a type of
action. The basis of the abnormalities in markers. In the other, much more preva- diabetes to an individual often depends
carbohydrate, fat, and protein metabo- lent category, type 2 diabetes, the cause is on the circumstances present at the time
lism in diabetes is deficient action of in- a combination of resistance to insulin ac- of diagnosis, and many diabetic individu-
sulin on target tissues. Deficient insulin tion and an inadequate compensatory in- als do not easily fit into a single class. For
action results from inadequate insulin se- sulin secretory response. In the latter example, a person with gestational diabe-
cretion and/or diminished tissue re- category, a degree of hyperglycemia suffi- tes mellitus (GDM) may continue to be
sponses to insulin at one or more points in cient to cause pathologic and functional hyperglycemic after delivery and may be
the complex pathways of hormone action. changes in various target tissues, but determined to have, in fact, type 2 diabe-
Impairment of insulin secretion and de- without clinical symptoms, may be tes. Alternatively, a person who acquires
fects in insulin action frequently coexist present for a long period of time before diabetes because of large doses of exoge-
in the same patient, and it is often unclear diabetes is detected. During this asymp- nous steroids may become normoglyce-
which abnormality, if either alone, is the tomatic period, it is possible to demon- mic once the glucocorticoids are
primary cause of the hyperglycemia. strate an abnormality in carbohydrate discontinued, but then may develop dia-
Symptoms of marked hyperglycemia metabolism by measurement of plasma betes many years later after recurrent ep-
include polyuria, polydipsia, weight loss, glucose in the fasting state or after a chal- isodes of pancreatitis. Another example
sometimes with polyphagia, and blurred lenge with an oral glucose load. would be a person treated with thiazides
vision. Impairment of growth and suscep- The degree of hyperglycemia (if any) who develops diabetes years later. Because
tibility to certain infections may also ac- may change over time, depending on the thiazides in themselves seldom cause severe
company chronic hyperglycemia. Acute, extent of the underlying disease process hyperglycemia, such individuals probably
life-threatening consequences of uncon- (Fig. 1). A disease process may be present have type 2 diabetes that is exacerbated by
trolled diabetes are hyperglycemia with but may not have progressed far enough the drug. Thus, for the clinician and patient,
ketoacidosis or the nonketotic hyperos- to cause hyperglycemia. The same disease it is less important to label the particular
molar syndrome. process can cause impaired fasting glu- type of diabetes than it is to understand the
Long-term complications of diabetes cose (IFG) and/or impaired glucose toler- pathogenesis of the hyperglycemia and to
include retinopathy with potential loss of ance (IGT) without fulfilling the criteria treat it effectively.
vision; nephropathy leading to renal fail- for the diagnosis of diabetes. In some in-
ure; peripheral neuropathy with risk of dividuals with diabetes, adequate glyce- Type 1 diabetes (-cell destruction,
foot ulcers, amputations, and Charcot mic control can be achieved with weight usually leading to absolute insulin
joints; and autonomic neuropathy caus- reduction, exercise, and/or oral glucose- deficiency)
ing gastrointestinal, genitourinary, and lowering agents. These individuals there- Immune-mediated diabetes. This form
of diabetes, which accounts for only
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
5–10% of those with diabetes, previously
Sections on diagnosis revised Fall 2009. encompassed by the terms insulin-
DOI: 10.2337/dc10-S062
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly dependent diabetes, type 1 diabetes, or
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. juvenile-onset diabetes, results from a cel-
org/licenses/by-nc-nd/3.0/ for details. lular-mediated autoimmune destruction
S62 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Figure 1—Disorders of glycemia: etiologic types and stages. *Even after presenting in ketoacidosis, these patients can briefly return to normogly-
cemia without requiring continuous therapy (i.e., “honeymoon” remission); **in rare instances, patients in these categories (e.g., Vacor toxicity, type
1 diabetes presenting in pregnancy) may require insulin for survival.
of the -cells of the pancreas. Markers of childhood and adolescence, but it can oc- Type 2 diabetes (ranging from
the immune destruction of the -cell in- cur at any age, even in the 8th and 9th predominantly insulin resistance
clude islet cell autoantibodies, autoanti- decades of life. with relative insulin deficiency to
bodies to insulin, autoantibodies to GAD Autoimmune destruction of -cells predominantly an insulin secretory
(GAD65), and autoantibodies to the ty- has multiple genetic predispositions and defect with insulin resistance)
rosine phosphatases IA-2 and IA-2. One is also related to environmental factors This form of diabetes, which accounts for
and usually more of these autoantibodies that are still poorly defined. Although pa- ⬃90 –95% of those with diabetes, previ-
are present in 85–90% of individuals tients are rarely obese when they present ously referred to as non–insulin-
when fasting hyperglycemia is initially with this type of diabetes, the presence of dependent diabetes, type 2 diabetes, or
detected. Also, the disease has strong HLA obesity is not incompatible with the diag- adult-onset diabetes, encompasses indi-
associations, with linkage to the DQA and nosis. These patients are also prone to viduals who have insulin resistance and
DQB genes, and it is influenced by the other autoimmune disorders such as usually have relative (rather than abso-
DRB genes. These HLA-DR/DQ alleles can Graves’ disease, Hashimoto’s thyroiditis, lute) insulin deficiency At least initially,
be either predisposing or protective. Addison’s disease, vitiligo, celiac sprue, and often throughout their lifetime, these
In this form of diabetes, the rate of autoimmune hepatitis, myasthenia gravis, individuals do not need insulin treatment
-cell destruction is quite variable, being to survive. There are probably many dif-
and pernicious anemia.
rapid in some individuals (mainly infants ferent causes of this form of diabetes. Al-
Idiopathic diabetes. Some forms of type
and children) and slow in others (mainly though the specific etiologies are not
1 diabetes have no known etiologies.
adults). Some patients, particularly chil- known, autoimmune destruction of
dren and adolescents, may present with Some of these patients have permanent -cells does not occur, and patients do
ketoacidosis as the first manifestation of insulinopenia and are prone to ketoacido- not have any of the other causes of diabe-
the disease. Others have modest fasting sis, but have no evidence of autoimmu- tes listed above or below.
hyperglycemia that can rapidly change to nity. Although only a minority of patients Most patients with this form of diabe-
severe hyperglycemia and/or ketoacidosis with type 1 diabetes fall into this category, tes are obese, and obesity itself causes
in the presence of infection or other stress. of those who do, most are of African or some degree of insulin resistance. Patients
Still others, particularly adults, may retain Asian ancestry. Individuals with this form who are not obese by traditional weight
residual -cell function sufficient to pre- of diabetes suffer from episodic ketoaci- criteria may have an increased percentage
vent ketoacidosis for many years; such in- dosis and exhibit varying degrees of insu- of body fat distributed predominantly in
dividuals eventually become dependent lin deficiency between episodes. This the abdominal region. Ketoacidosis sel-
on insulin for survival and are at risk for form of diabetes is strongly inherited, dom occurs spontaneously in this type of
ketoacidosis. At this latter stage of the dis- lacks immunological evidence for -cell diabetes; when seen, it usually arises in
ease, there is little or no insulin secretion, autoimmunity, and is not HLA associated. association with the stress of another ill-
as manifested by low or undetectable lev- An absolute requirement for insulin re- ness such as infection. This form of dia-
els of plasma C-peptide. Immune- placement therapy in affected patients betes frequently goes undiagnosed for
mediated diabetes commonly occurs in may come and go. many years because the hyperglycemia
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S63
Diagnosis and Classification
develops gradually and at earlier stages is of insulin secretion. The less common noma. With the exception of that caused
often not severe enough for the patient to forms result from mutations in other tran- by cancer, damage to the pancreas must
notice any of the classic symptoms of di- scription factors, including HNF-4␣, be extensive for diabetes to occur; adre-
abetes. Nevertheless, such patients are at HNF-1, insulin promoter factor (IPF)-1, nocarcinomas that involve only a small
increased risk of developing macrovascu- and NeuroD1. portion of the pancreas have been associ-
lar and microvascular complications. Point mutations in mitochondrial ated with diabetes. This implies a mecha-
Whereas patients with this form of diabe- DNA have been found to be associated nism other than simple reduction in
tes may have insulin levels that appear with diabetes and deafness The most -cell mass. If extensive enough, cystic
normal or elevated, the higher blood glu- common mutation occurs at position fibrosis and hemochromatosis will also
cose levels in these diabetic patients 3,243 in the tRNA leucine gene, leading damage -cells and impair insulin secre-
would be expected to result in even to an A-to-G transition. An identical le- tion. Fibrocalculous pancreatopathy may
higher insulin values had their -cell sion occurs in the MELAS syndrome (mi- be accompanied by abdominal pain radi-
function been normal. Thus, insulin se- tochondrial myopathy, encephalopathy, ating to the back and pancreatic calcifica-
cretion is defective in these patients and lactic acidosis, and stroke-like syn- tions identified on X-ray examination.
insufficient to compensate for insulin re- drome); however, diabetes is not part of Pancreatic fibrosis and calcium stones in
sistance. Insulin resistance may improve this syndrome, suggesting different phe- the exocrine ducts have been found at
with weight reduction and/or pharmaco- notypic expressions of this genetic lesion. autopsy.
logical treatment of hyperglycemia but is Genetic abnormalities that result in Endocrinopathies. Several hormones
seldom restored to normal. The risk of the inability to convert proinsulin to in- (e.g., growth hormone, cortisol, gluca-
developing this form of diabetes increases sulin have been identified in a few fami- gon, epinephrine) antagonize insulin ac-
with age, obesity, and lack of physical ac- lies, and such traits are inherited in an tion. Excess amounts of these hormones
tivity. It occurs more frequently in autosomal dominant pattern. The result- (e.g., acromegaly, Cushing’s syndrome,
women with prior GDM and in individu- ant glucose intolerance is mild. Similarly, glucagonoma, pheochromocytoma, re-
als with hypertension or dyslipidemia, the production of mutant insulin mole- spectively) can cause diabetes. This gen-
and its frequency varies in different racial/ cules with resultant impaired receptor erally occurs in individuals with
ethnic subgroups. It is often associated binding has also been identified in a few preexisting defects in insulin secretion,
with a strong genetic predisposition, families and is associated with an autoso- and hyperglycemia typically resolves
more so than is the autoimmune form of mal inheritance and only mildly impaired when the hormone excess is resolved.
type 1 diabetes. However, the genetics of or even normal glucose metabolism. Somatostatinoma- and aldoster-
this form of diabetes are complex and not Genetic defects in insulin action. There onoma-induced hypokalemia can cause
clearly defined. are unusual causes of diabetes that result diabetes, at least in part, by inhibiting in-
from genetically determined abnormali- sulin secretion. Hyperglycemia generally
Other specific types of diabetes ties of insulin action. The metabolic ab- resolves after successful removal of the
Genetic defects of the -cell. Several normalities associated with mutations of tumor.
forms of diabetes are associated with mo- the insulin receptor may range from hy- Drug- or chemical-induced diabetes.
nogenetic defects in -cell function. perinsulinemia and modest hyperglyce- Many drugs can impair insulin secretion.
These forms of diabetes are frequently mia to severe diabetes. Some individuals These drugs may not cause diabetes by
characterized by onset of hyperglycemia with these mutations may have acanthosis themselves, but they may precipitate dia-
at an early age (generally before age 25 nigricans. Women may be virilized and betes in individuals with insulin resis-
years). They are referred to as maturity- have enlarged, cystic ovaries. In the past, tance. In such cases, the classification is
onset diabetes of the young (MODY) and this syndrome was termed type A insulin unclear because the sequence or relative
are characterized by impaired insulin se- resistance. Leprechaunism and the Rabson- importance of -cell dysfunction and in-
cretion with minimal or no defects in in- Mendenhall syndrome are two pediatric sulin resistance is unknown. Certain tox-
sulin action. They are inherited in an syndromes that have mutations in the insu- ins such as Vacor (a rat poison) and
autosomal dominant pattern. Abnormali- lin receptor gene with subsequent alter- intravenous pentamidine can perma-
ties at six genetic loci on different chro- ations in insulin receptor function and nently destroy pancreatic -cells. Such
mosomes have been identified to date. extreme insulin resistance. The former has drug reactions fortunately are rare. There
The most common form is associated characteristic facial features and is usually are also many drugs and hormones that
with mutations on chromosome 12 in a fatal in infancy, while the latter is associated can impair insulin action. Examples in-
hepatic transcription factor referred to as with abnormalities of teeth and nails and clude nicotinic acid and glucocorticoids.
hepatocyte nuclear factor (HNF)-1␣. A pineal gland hyperplasia. Patients receiving ␣-interferon have been
second form is associated with mutations Alterations in the structure and func- reported to develop diabetes associated
in the glucokinase gene on chromosome tion of the insulin receptor cannot be dem- with islet cell antibodies and, in certain
7p and results in a defective glucokinase onstrated in patients with insulin-resistant instances, severe insulin deficiency. The
molecule. Glucokinase converts glucose lipoatrophic diabetes. Therefore, it is as- list shown in Table 1 is not all-inclusive,
to glucose-6-phosphate, the metabolism sumed that the lesion(s) must reside in the but reflects the more commonly recog-
of which, in turn, stimulates insulin secre- postreceptor signal transduction pathways. nized drug-, hormone-, or toxin-induced
tion by the -cell. Thus, glucokinase Diseases of the exocrine pancreas. Any forms of diabetes.
serves as the “glucose sensor” for the process that diffusely injures the pancreas Infections. Certain viruses have been as-
-cell. Because of defects in the glucoki- can cause diabetes. Acquired processes sociated with -cell destruction. Diabetes
nase gene, increased plasma levels of glu- include pancreatitis, trauma, infection, occurs in patients with congenital rubella,
cose are necessary to elicit normal levels pancreatectomy, and pancreatic carci- although most of these patients have HLA
S64 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 1—Etiologic classification of diabetes mellitus and immune markers characteristic of
I. Type 1 diabetes (-cell destruction, usually leading to absolute insulin deficiency) type 1 diabetes. In addition, coxsackievi-
A. Immune mediated rus B, cytomegalovirus, adenovirus, and
B. Idiopathic mumps have been implicated in inducing
II. Type 2 diabetes (may range from predominantly insulin resistance with relative insulin deficiency
to a predominantly secretory defect with insulin resistance)
certain cases of the disease.
III. Other specific types Uncommon forms of immune-medi-
A. Genetic defects of -cell function ated diabetes. In this category, there are
1. Chromosome 12, HNF-1␣ (MODY3) two known conditions, and others are
2. Chromosome 7, glucokinase (MODY2)
3. Chromosome 20, HNF-4␣ (MODY1)
likely to occur. The stiff-man syndrome is
4. Chromosome 13, insulin promoter factor-1 (IPF-1; MODY4) an autoimmune disorder of the central
5. Chromosome 17, HNF-1 (MODY5) nervous system characterized by stiffness
6. Chromosome 2, NeuroD1 (MODY6) of the axial muscles with painful spasms.
7. Mitochondrial DNA
8. Others
Patients usually have high titers of the
B. Genetic defects in insulin action GAD autoantibodies, and approximately
1. Type A insulin resistance one-third will develop diabetes.
2. Leprechaunism Anti-insulin receptor antibodies can
3. Rabson-Mendenhall syndrome
4. Lipoatrophic diabetes cause diabetes by binding to the insulin
5. Others receptor, thereby blocking the binding of
C. Diseases of the exocrine pancreas insulin to its receptor in target tissues.
1. Pancreatitis However, in some cases, these antibodies
2. Trauma/pancreatectomy
3. Neoplasia can act as an insulin agonist after binding
4. Cystic fibrosis to the receptor and can thereby cause hy-
5. Hemochromatosis poglycemia. Anti-insulin receptor anti-
6. Fibrocalculous pancreatopathy bodies are occasionally found in patients
7. Others
D. Endocrinopathies with systemic lupus erythematosus and
1. Acromegaly other autoimmune diseases. As in other
2. Cushing’s syndrome states of extreme insulin resistance, pa-
3. Glucagonoma tients with anti-insulin receptor antibod-
4. Pheochromocytoma
5. Hyperthyroidism ies often have acanthosis nigricans. In the
6. Somatostatinoma past, this syndrome was termed type B
7. Aldosteronoma insulin resistance.
8. Others Other genetic syndromes sometimes
E. Drug or chemical induced
1. Vacor associated with diabetes. Many genetic
2. Pentamidine syndromes are accompanied by an in-
3. Nicotinic acid creased incidence of diabetes. These in-
4. Glucocorticoids clude the chromosomal abnormalities of
5. Thyroid hormone
6. Diazoxide Down syndrome, Klinefelter syndrome,
7. -adrenergic agonists and Turner syndrome. Wolfram’s syn-
8. Thiazides drome is an autosomal recessive disorder
9. Dilantin characterized by insulin-deficient diabe-
10. ␥-Interferon
11. Others tes and the absence of -cells at autopsy.
F. Infections Additional manifestations include diabe-
1. Congenital rubella tes insipidus, hypogonadism, optic atro-
2. Cytomegalovirus phy, and neural deafness. Other
3. Others
G. Uncommon forms of immune-mediated diabetes syndromes are listed in Table 1.
1. “Stiff-man” syndrome
2. Anti-insulin receptor antibodies Gestational diabetes mellitus
3. Others For many years, GDM has been defined as
H. Other genetic syndromes sometimes associated with diabetes
1. Down syndrome any degree of glucose intolerance with on-
2. Klinefelter syndrome set or first recognition during pregnancy.
3. Turner syndrome Although most cases resolve with deliv-
4. Wolfram syndrome ery, the definition applied whether or not
5. Friedreich ataxia
6. Huntington chorea the condition persisted after pregnancy
7. Laurence-Moon-Biedl syndrome and did not exclude the possibility that
8. Myotonic dystrophy unrecognized glucose intolerance may
9. Porphyria have antedated or begun concomitantly
10. Prader-Willi syndrome
11. Others with the pregnancy. This definition facil-
IV. Gestational diabetes mellitus itated a uniform strategy for detection and
Patients with any form of diabetes may require insulin treatment at some stage of their disease. Such use of classification of GDM, but its limitations
insulin does not, of itself, classify the patient. were recognized for many years. As the
ongoing epidemic of obesity and diabetes
has led to more type 2 diabetes in women
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S65
Diagnosis and Classification
Table 2—Categories of increased risk for dominal or visceral obesity), dyslipidemia nication). Finally, evidence from the Dia-
diabetes* with high triglycerides and/or low HDL betes Prevention Program (DPP), wherein
FPG 100 mg/dl (5.6 mmol/l) to 125 mg/dl cholesterol, and hypertension. Structured the mean A1C was 5.9% (SD 0.5%), indi-
(6.9 mmol/l) 关IFG兴 lifestyle intervention, aimed at increasing cates that preventive interventions are ef-
2-h PG in the 75-g OGTT 140 mg/dl (7.8 physical activity and producing 5–10% fective in groups of people with A1C
mmol/l) to 199 mg/dl (11.0 mmol/l) 关IGT兴 loss of body weight, and certain pharma- levels both below and above 5.9% (9). For
A1C 5.7–6.4% cological agents have been demonstrated these reasons, the most appropriate A1C
to prevent or delay the development of level above which to initiate preventive
*For all three tests, risk is continuous, extending
below the lower limit of the range and becoming diabetes in people with IGT; the potential interventions is likely to be somewhere in
disproportionately greater at higher ends of the impact of such interventions to reduce the range of 5.5– 6%.
range. mortality or the incidence of cardiovascu- As was the case with FPG and 2-h PG,
lar disease has not been demonstrated to defining a lower limit of an intermediate
date. It should be noted that the 2003 category of A1C is somewhat arbitrary, as
of childbearing age, the number of preg- ADA Expert Committee report reduced the risk of diabetes with any measure or
nant women with undiagnosed type 2 di- the lower FPG cut point to define IFG surrogate of glycemia is a continuum, ex-
abetes has increased. from 110 mg/dl (6.1 mmol/l) to 100 tending well into the normal ranges. To
After deliberations in 2008 –2009, mg/dl (5.6 mmol/l), in part to ensure that maximize equity and efficiency of preven-
the International Association of Diabetes prevalence of IFG was similar to that of tive interventions, such an A1C cut point
and Pregnancy Study Groups (IADPSG), IGT. However, the World Health Organi- should balance the costs of “false nega-
an international consensus group with zation (WHO) and many other diabetes tives” (failing to identify those who are
representatives from multiple obstetrical organizations did not adopt this change in going to develop diabetes) against the
and diabetes organizations, including the the definition of IFG. costs of “false positives” (falsely identify-
American Diabetes Association (ADA), As A1C is used more commonly to ing and then spending intervention re-
recommended that high-risk women diagnose diabetes in individuals with risk sources on those who were not going to
found to have diabetes at their initial pre- factors, it will also identify those at higher develop diabetes anyway).
natal visit, using standard criteria (Table risk for developing diabetes in the future. Compared to the fasting glucose cut-
3), receive a diagnosis of overt, not gesta- When recommending the use of the A1C point of 100 mg/dl (5.6 mmol/l), an A1C
tional, diabetes. Approximately 7% of all to diagnose diabetes in its 2009 report, cutpoint of 5.7% is less sensitive but more
pregnancies (ranging from 1 to 14%, de- the International Expert Committee (3) specific and has a higher positive predic-
pending on the population studied and stressed the continuum of risk for diabe- tive value to identify people at risk for
the diagnostic tests employed) are com- tes with all glycemic measures and did not later development of diabetes. A large
plicated by GDM, resulting in more than formally identify an equivalent intermedi- prospective study found that a 5.7% cut-
200,000 cases annually. ate category for A1C. The group did note point has a sensitivity of 66% and speci-
that those with A1C levels above the lab- ficity of 88% for the identification of
CATEGORIES OF oratory “normal” range but below the di- subsequent 6-year diabetes incidence
INCREASED RISK FOR agnostic cut point for diabetes (6.0 to (10). Receiver operating curve analyses
DIABETES — In 1997 and 2003, The ⬍6.5%) are at very high risk of develop- of nationally representative U.S. data
Expert Committee on Diagnosis and Clas- ing diabetes. Indeed, incidence of diabe- (NHANES 1999-2006) indicate that an
sification of Diabetes Mellitus (1,2) recog- tes in people with A1C levels in this range A1C value of 5.7% has modest sensitivity
nized an intermediate group of is more than 10 times that of people with (39-45%) but high specificity (81-91%)
individuals whose glucose levels do not lower levels (4 –7). However, the 6.0 to to identify cases of IFP (FPG ⬎100 mg/dl)
meet criteria for diabetes, yet are higher ⬍6.5% range fails to identify a substantial (5.6 mmol/l) or IGT (2-h glucose ⬎ 140
than those considered normal. These peo- number of patients who have IFG and/or mg/dl) (R.T. Ackerman, personal com-
ple were defined as having impaired fast- IGT. Prospective studies indicate that munication). Other analyses suggest that
ing glucose (IFG) [fasting plasma glucose people within the A1C range of 5.5– 6.0% an A1C of 5.7% is associated with diabe-
(FPG) levels 100 mg/dl (5.6 mmol/l) to have a 5-year cumulative incidence of di- tes risk similar to the high-risk partici-
125 mg/dl (6.9 mmol/l)], or impaired glu- abetes that ranges from 12 to 25% (4 –7), pants in the DPP (R.T. Ackerman,
cose tolerance (IGT) [2-h values in the which is appreciably (three- to eightfold) personal communication). Hence, it is
oral glucose tolerance test (OGTT) of 140 higher than incidence in the U.S. popula- reasonable to consider an A1C range of
mg/dl (7.8 mmol/l) to 199 mg/dl (11.0 tion as a whole (8). Analyses of nationally 5.7 to 6.4% as identifying individuals
mmol/l)]. representative data from the National with high risk for future diabetes and to
Individuals with IFG and/or IGT have Health and Nutrition Examination Survey whom the term pre-diabetes may be ap-
been referred to as having pre-diabetes, (NHANES) indicate that the A1C value plied if desired.
indicating the relatively high risk for the that most accurately identifies people Individuals with an A1C of 5.7– 6.4%
future development of diabetes. IFG and with IFG or IGT falls between 5.5 and should be informed of their increased risk
IGT should not be viewed as clinical en- 6.0%. In addition, linear regression anal- for diabetes as well as cardiovascular dis-
tities in their own right but rather risk yses of these data indicate that among the ease and counseled about effective strate-
factors for diabetes as well as cardiovas- nondiabetic adult population, an FPG of gies, such as weight loss and physical
cular disease. They can be observed as in- 110 mg/dl (6.1 mmol/l) corresponds to an activity, to lower their risks. As with glu-
termediate stages in any of the disease A1C of 5.6%, while an FPG of 100 mg/dl cose measurements, the continuum of
processes listed in Table 1. IFG and IGT (5.6 mmol/l) corresponds to an A1C of risk is curvilinear, so that as A1C rises, the
are associated with obesity (especially ab- 5.4% (R.T. Ackerman, personal commu- risk of diabetes rises disproportionately.
S66 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Accordingly, interventions should be Table 3—Criteria for the diagnosis of diabetes
most intensive and follow-up should be 1. A1C ⱖ6.5%. The test should be performed in a laboratory using a method that is NGSP
particularly vigilant for those with A1C certified and standardized to the DCCT assay.*
levels above 6.0%, who should be consid- OR
ered to be at very high risk. However, just 2. FPG ⱖ126 mg/dl (7.0 mmol/l). Fasting is defined as no caloric intake for at least 8 h.*
as an individual with a fasting glucose of OR
98 mg/dl (5.4 mmol/l) may not be at neg- 3. 2-h plasma glucose ⱖ200 mg/dl (11.1 mmol/l) during an OGTT. The test should be
ligible risk for diabetes, individuals with performed as described by the World Health Organization, using a glucose load containing
A1C levels below 5.7% may still be at risk, the equivalent of 75 g anhydrous glucose dissolved in water.*
depending on level of A1C and presence OR
of other risk factors, such as obesity and 4. In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random
family history. plasma glucose ⱖ200 mg/dl (11.1 mmol/l).
Table 2 summarizes the categories of
*In the absence of unequivocal hyperglycemia, criteria 1–3 should be confirmed by repeat testing.
increased risk for diabetes. Evaluation of
patients at risk should incorporate a
global risk factor assessment for both di- microvascular and, to a lesser extent, ma- tion, the A1C can be misleading in pa-
abetes and cardiovascular disease. crovascular complications and is widely tients with certain forms of anemia and
Screening for and counseling about risk of used as the standard biomarker for the hemoglobinopathies, which may also
diabetes should always be in the prag- adequacy of glycemic management. Prior have unique ethnic or geographic distri-
matic context of the patient’s comorbidi- Expert Committees have not recom- butions. For patients with a hemoglobi-
ties, life expectancy, personal capacity to mended use of the A1C for diagnosis of nopathy but normal red cell turnover,
engage in lifestyle change, and overall diabetes, in part due to lack of standard- such as sickle cell trait, an A1C assay
health goals. ization of the assay. However, A1C assays without interference from abnormal he-
are now highly standardized so that their moglobins should be used (an updated
DIAGNOSTIC CRITERIA FOR results can be uniformly applied both list is available at www.ngsp.org/prog/
DIABETES MELLITUS — For de- temporally and across populations. In index3.html). For conditions with abnor-
cades, the diagnosis of diabetes has been their recent report (3), an International mal red cell turnover, such as anemias
based on glucose criteria, either the FPG Expert Committee, after an extensive re- from hemolysis and iron deficiency, the
or the 75-g OGTT. In 1997, the first Ex- view of both established and emerging ep- diagnosis of diabetes must employ glu-
pert Committee on the Diagnosis and idemiological evidence, recommended cose criteria exclusively.
Classification of Diabetes Mellitus revised the use of the A1C test to diagnose diabe- The established glucose criteria for
the diagnostic criteria, using the observed tes, with a threshold of ⱖ6.5%, and ADA the diagnosis of diabetes remain valid.
association between FPG levels and pres- affirms this decision. The diagnostic A1C These include the FPG and 2-h PG. Addi-
ence of retinopathy as the key factor with cut point of 6.5% is associated with an tionally, patients with severe hyperglyce-
which to identify threshold glucose level. inflection point for retinopathy preva- mia such as those who present with severe
The Committee examined data from three lence, as are the diagnostic thresholds for classic hyperglycemic symptoms or hy-
cross-sectional epidemiologic studies that FPG and 2-h PG (3). The diagnostic test perglycemic crisis can continue to be di-
assessed retinopathy with fundus photog- should be performed using a method that agnosed when a random (or casual)
raphy or direct ophthalmoscopy and is certified by the National Glycohemo- plasma glucose of ⱖ200 mg/dl (11.1
measured glycemia as FPG, 2-h PG, and globin Standardization Program (NGSP) mmol/l) is found. It is likely that in such
A1C. These studies demonstrated glyce- and standardized or traceable to the Dia- cases the health care professional would
mic levels below which there was little betes Control and Complications Trial also measure an A1C test as part of the
prevalent retinopathy and above which reference assay. Point-of-care A1C assays initial assessment of the severity of the di-
the prevalence of retinopathy increased in are not sufficiently accurate at this time to abetes and that it would (in most cases) be
an apparently linear fashion. The deciles use for diagnostic purposes. above the diagnostic cut point for diabe-
of the three measures at which retinopa- There is an inherent logic to using a tes. However, in rapidly evolving diabe-
thy began to increase were the same for more chronic versus an acute marker of tes, such as the development of type 1
each measure within each population. dysglycemia, particularly since the A1C is diabetes in some children, A1C may not
Moreover, the glycemic values above already widely familiar to clinicians as a be significantly elevated despite frank
which retinopathy increased were similar marker of glycemic control. Moreover, diabetes.
among the populations. These analyses the A1C has several advantages to the Just as there is less than 100% con-
helped to inform a new diagnostic cut FPG, including greater convenience, cordance between the FPG and 2-h PG
point of ⱖ126 mg/dl (7.0 mmol/l) for since fasting is not required, evidence to tests, there is not full concordance be-
FPG and confirmed the long-standing di- suggest greater preanalytical stability, and tween A1C and either glucose-based test.
agnostic 2-h PG value of ⱖ200 mg/dl less day-to-day perturbations during pe- Analyses of NHANES data indicate that,
(11.1 mmol/l). riods of stress and illness. These advan- assuming universal screening of the undi-
A1C is a widely used marker of tages, however, must be balanced by agnosed, the A1C cut point of ⱖ6.5%
chronic glycemia, reflecting average greater cost, the limited availability of identifies one-third fewer cases of undiag-
blood glucose levels over a 2- to 3-month A1C testing in certain regions of the de- nosed diabetes than a fasting glucose cut
period of time. The test plays a critical role veloping world, and the incomplete cor- point of ⱖ126 mg/dl (7.0 mmol/l) (cdc
in the management of the patient with di- relation between A1C and average website tbd). However, in practice, a large
abetes, since it correlates well with both glucose in certain individuals. In addi- portion of the population with type 2 di-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S67
Diagnosis and Classification
abetes remains unaware of their condi- the diagnostic threshold is repeated, the group with a high prevalence of diabe-
tion. Thus, it is conceivable that the lower second value will be below the diagnostic tes (e.g., Hispanic American, Native
sensitivity of A1C at the designated cut cut point. This is least likely for A1C, American, Asian American, African
point will be offset by the test’s greater somewhat more likely for FPG, and most American, Pacific Islander)
practicality, and that wider application of likely for the 2-h PG. Barring a laboratory
a more convenient test (A1C) may actu- error, such patients are likely to have test
Risk assessment for GDM should be
ally increase the number of diagnoses results near the margins of the threshold
made. for a diagnosis. The healthcare profes- undertaken at the first prenatal visit.
Further research is needed to better sional might opt to follow the patient Women with clinical characteristics con-
characterize those patients whose glyce- closely and repeat the testing in 3– 6 sistent with a high risk of GDM (marked
mic status might be categorized differ- months. obesity, personal history of GDM, glyco-
ently by two different tests (e.g., FPG and The decision about which test to use suria, or a strong family history of diabe-
A1C), obtained in close temporal approx- to assess a specific patient for diabetes tes) should undergo glucose testing (see
imation. Such discordance may arise from should be at the discretion of the health below) as soon as feasible. If they are
measurement variability, change over care professional, taking into account the found not to have GDM at that initial
time, or because A1C, FPG, and postchal- availability and practicality of testing an screening, they should be retested be-
lenge glucose each measure different individual patient or groups of patients. tween 24 and 28 weeks of gestation.
physiological processes. In the setting of Perhaps more important than which diag- Women of average risk should have test-
an elevated A1C but “nondiabetic” FPG, nostic test is used, is that the testing for ing undertaken at 24 –28 weeks of
the likelihood of greater postprandial glu- diabetes be performed when indicated. gestation.
cose levels or increased glycation rates for There is discouraging evidence indicating An FPG level ⬎126 mg/dl (7.0
a given degree of hyperglycemia may be that many at-risk patients still do not receive mmol/l) or a casual plasma glucose ⬎200
present. In the opposite scenario (high adequate testing and counseling for this in- mg/dl (11.1 mmol/l) meets the threshold
FPG yet A1C below the diabetes cut creasingly common disease, or for its fre- for the diagnosis of diabetes. In the ab-
point), augmented hepatic glucose pro- quently accompanying cardiovascular risk sence of unequivocal hyperglycemia, the
duction or reduced glycation rates may be factors. The current diagnostic criteria for diagnosis must be confirmed on a subse-
present. diabetes are summarized in Table 3. quent day. Confirmation of the diagnosis
As with most diagnostic tests, a test precludes the need for any glucose chal-
result diagnostic of diabetes should be re- Diagnosis of GDM lenge. In the absence of this degree of hy-
peated to rule out laboratory error, unless At the time of publication of this state- perglycemia, evaluation for GDM in
the diagnosis is clear on clinical grounds, ment, the criteria for abnormal glucose women with average or high-risk charac-
such as a patient with classic symptoms of tolerance in pregnancy are those of Car- teristics should follow one of two
hyperglycemia or hyperglycemic crisis. It penter and Coustan (11). Recommenda- approaches.
is preferable that the same test be repeated tions from ADA’s Fourth International One-step approach. Perform a diagnos-
for confirmation, since there will be a Workshop-Conference on Gestational tic OGTT without prior plasma or serum
greater likelihood of concurrence in this Diabetes Mellitus held in March 1997 glucose screening. The one-step approach
case. For example, if the A1C is 7.0% and support the use of the Carpenter/Coustan may be cost-effective in high-risk patients
a repeat result is 6.8%, the diagnosis of diagnostic criteria as well as the alterna- or populations (e.g., some Native-
diabetes is confirmed. However, there are tive use of a diagnostic 75-g 2-h OGTT. American groups).
scenarios in which results of two different These criteria are summarized below. Two-step approach. Perform an initial
tests (e.g., FPG and A1C) are available for Testing for gestational diabetes. Previ- screening by measuring the plasma or se-
the same patient. In this situation, if the ous recommendations included screening rum glucose concentration 1 h after a
two different tests are both above the di- for GDM performed in all pregnancies. 50-g oral glucose load (glucose challenge
agnostic thresholds, the diagnosis of dia- However, there are certain factors that test [GCT]) and perform a diagnostic
betes is confirmed. place women at lower risk for the devel- OGTT on that subset of women exceeding
On the other hand, when two differ- opment of glucose intolerance during the glucose threshold value on the GCT.
ent tests are available in an individual and pregnancy, and it is likely not cost- When the two-step approach is used, a
the results are discordant, the test whose effective to screen such patients. Pregnant glucose threshold value ⬎140 mg/dl (7.8
result is above the diagnostic cut point women who fulfill all of these criteria mmol/l) identifies ⬃80% of women with
should be repeated, and the diagnosis is need not be screened for GDM. GDM, and the yield is further increased to
made on the basis of the confirmed test. This low-risk group comprises 90% by using a cutoff of ⬎130 mg/dl (7.2
That is, if a patient meets the diabetes cri- women who: mmol/l).
terion of the A1C (two results ⱖ6.5%) but With either approach, the diagnosis
not the FPG (⬍126 mg/dl or 7.0 mmol/l), ● are ⬍25 years of age of GDM is based on an OGTT. Diagnostic
or vice versa, that person should be con- ● are a normal body weight criteria for the 100-g OGTT are derived
sidered to have diabetes. Admittedly, in ● have no family history (i.e., first-degree from the original work of O’Sullivan and
most circumstance the “nondiabetic” test relative) of diabetes Mahan (12) modified by Carpenter and
is likely to be in a range very close to the ● have no history of abnormal glucose Coustan (11) and are shown at the top of
threshold that defines diabetes. metabolism Table 4. Alternatively, the diagnosis can
Since there is preanalytic and analytic ● have no history of poor obstetric be made using a 75-g glucose load and the
variability of all the tests, it is also possible outcome glucose threshold values listed for fasting,
that when a test whose result was above ● are not members of an ethnic/racial 1 h, and 2 h (Table 4, bottom); however,
S68 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
Table 4—Diagnosis of GDM with a 100-g or obstetrical organizations to consider cose and A1C is effective for the
75-g glucose load adoption of the IADPSG diagnostic crite- prediction of type 2 diabetes: the Kansai
ria and to discuss the implications of this Healthcare Study. Diabetes Care 2009;32:
change. While this change will signifi- 644 – 646
mg/dl mmol/l 7. Shimazaki T, Kadowaki T, Ohyama Y,
cantly increase the prevalence of GDM, Ohe K, Kubota K. Hemoglobin A1c
100-g glucose load there is mounting evidence that treating (HbA1c) predicts future drug treatment
Fasting 95 5.3 even mild GDM reduces morbidity for for diabetes mellitus: a follow-up study
1-h 180 10.0 both mother and baby (14). using routine clinical data in a Japanese
2-h 155 8.6 university hospital. Translational Re-
3-h 140 7.8 search 2007;149:196 –204
75-g glucose load Acknowledgments — The American Diabe- 8. Geiss LS, Pan L, Cadwell B, Gregg EW, Ben-
Fasting 95 5.3 tes Association thanks the following volunteer jamin SM, Engelgau MM. Changes in inci-
1-h 180 10.0 members of the writing group for the updated dence of diabetes in U.S. adults, 1997–
2-h 155 8.6 sections on diagnosis and categories of in- 2003. Am J Prev Med 2006;30:371–377
creased risk: Silvio Inzucchi, MD; Richard Ber- 9. Knowler WC, Barrett-Connor E, Fowler
Two or more of the venous plasma concentrations genstal, MD; Vivian Fonseca, MD; Edward
must be met or exceeded for a positive diagnosis.
SE, Hamman RF, Lachin JM, Walker EA,
Gregg, PhD; Beth Mayer-Davis, MSPH, PhD, Nathan DM, Diabetes Prevention Pro-
The test should be done in the morning after an
overnight fast of between 8 and 14 h and after at least RD; Geralyn Spollett, MSN, CDE, ANP; and gram Research Group. Reduction in the
3 days of unrestricted diet (ⱖ150 g carbohydrate per Richard Wender, MD. incidence of type 2 diabetes with lifestyle
day) and unlimited physical activity. The subject intervention or metformin. N Engl J Med
should remain seated and should not smoke 2002;346:393– 403
throughout the test. References 10. Droumaguet C, Balkau B, Simon D, Caces
1. Expert Committee on the Diagnosis and E, Tichet J, Charles MA, Eschwege E, the
Classification of Diabetes Mellitus. Report of DESIR Study Group. Use of HbA1c in pre-
this test is not as well validated as the the Expert Committee on the Diagnosis and dicting progression to diabetes in French
100-g OGTT. Classification of Diabetes Mellitus. Diabetes men and women: data from an Epidemi-
Care 1997;20:1183–1197 ological Study on the Insulin Resistance
Results of the Hyperglycemia and 2. Genuth S, Alberti KG, Bennett P, Buse J, Syndrome (DESIR) Diabetes Care 2006;
Adverse Pregnancy Outcomes study Defronzo R, Kahn R, Kitzmiller J, Knowler 29:1619 –1625.
(13), a large-scale (⬃25,000 pregnant WC, Lebovitz H, Lernmark A, Nathan D, 11. Carpenter MW, Coustan DR. Criteria for
women) multinational epidemiologic Palmer J, Rizza R, Saudek C, Shaw J, Ste- screening tests for gestational diabetes. Am J
study, demonstrated that risk of adverse ffes M, Stern M, Tuomilehto J, Zimmet P, Obstet Gynecol 1982;144:768 –773
maternal, fetal, and neonatal outcomes Expert Committee on the Diagnosis and 12. O’Sullivan JB, Mahan CM. Criteria for the
continuously increased as a function of Classification of Diabetes Mellitus2, the oral glucose tolerance test in pregnancy.
maternal glycemia at 24 –28 weeks, Expert Committee on the Diagnosis and Diabetes 1964;13:278
even within ranges previously consid- Classification of Diabetes Mellitus. Fol- 13. HAPO Study Cooperative Research
ered normal for pregnancy. For most low-up report on the diagnosis of dia- Group, Metzger BE, Lowe LP, Dyer AR,
betes mellitus. Diabetes Care 2003;26: Trimble ER, Chaovarindr U, Coustan DR,
complications, there was no threshold 3160 –3167 Hadden DR, McCance DR, Hod M, McIn-
for risk. These results have led to careful 3. International Expert Committee. Interna- tyre HD, Oats JJ, Persson B, Rogers MS,
reconsideration of the diagnostic crite- tional Expert Committee report on the Sacks DA. Hyperglycemia and adverse
ria for GDM. The IADPSG recom- role of the A1C assay in the diagnosis pregnancy outcomes. N Engl J Med 2008;
mended that all women not known to of diabetes. Diabetes Care 2009;32:1327– 358:1991–2002
have prior diabetes undergo a 75-g 1334 14. Landon MB, Spong CY, Thom E, Carpen-
OGTT at 24 –28 weeks of gestation. The 4. Edelman D, Olsen MK, Dudley TK, Harris ter MW, Ramin SM, Casey B, Wapner RJ,
group developed diagnostic cut points AC, Oddone EZ. Utility of hemoglobin Varner MW, Rouse DJ, Thorp JM Jr,
for the fasting, 1-h, and 2-h plasma glu- A1c in predicting diabetes risk. J Gen In- Sciscione A, Catalano P, Harper M, Saade
cose measurements that conveyed an tern Med 2004;19:1175–1180 G, Lain KY, Sorokin Y, Peaceman AM, To-
5. Pradhan AD, Rifai N, Buring JE, Ridker PM. losa JE, Anderson GB, Eunice Kennedy
odds ratio for adverse outcomes of at Hemoglobin A1c predicts diabetes but not Shriver National Institute of Child Health
least 1.75 compared with women with cardiovascular disease in nondiabetic and Human Development Maternal-Fetal
the mean glucose levels in the HAPO women. Am J Med 2007;120:720 –727 Medicine Units Network. A multicenter,
study. 6. Sato KK, Hayashi T, Harita N, Yoneda T, randomized trial of treatment for mild
At the time of publication of this up- Nakamura Y, Endo G, Kambe H. Com- gestational diabetes. N Engl J Med 2009;
date, ADA is planning to work with U.S. bined measurement of fasting plasma glu- 361:1339 –1348
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S69
P O S I T I O N S T A T E M E N T
Diabetes Care in the School and Day Care
Setting
AMERICAN DIABETES ASSOCIATION
D
iabetes is one of the most common the child’s usual school setting with as lit- personnel must have an understanding of
chronic diseases of childhood (1). tle disruption to the school’s and the diabetes and must be trained in its man-
There are ⬃186,300 individuals child’s routine as possible and allowing agement and in the treatment of diabetes
⬍20 years of age with diabetes in the U.S. the child full participation in all school emergencies (3,18,19,20,34,36). Knowl-
Based on 2002–2003 data, the rate of new activities (8,9). edgeable trained personnel are essential if
type 1 diabetes cases was 19.0 per Despite these protections, children in the student is to avoid the immediate
100,000 children and of type 2 diabetes the school and day care setting still face health risks of low blood glucose and to
was 5.3 per 100,000 (2). The majority of discrimination. For example, some day achieve the metabolic control required to
these young people attend school and/or care centers may refuse admission to chil- decrease risks for later development of di-
some type of day care and need knowl- dren with diabetes, and children in the abetes complications (3,20). Studies have
edgeable staff to provide a safe school en- classroom may not be provided the assis- shown that the majority of school person-
vironment. Both parents and the health tance necessary to monitor blood glucose nel have an inadequate understanding of
care team should work together to pro- and administer insulin and may be pro- diabetes (21,22). Consequently, diabetes
vide school systems and day care provid- hibited from eating needed snacks. The education must be targeted toward day
ers with the information necessary to American Diabetes Association works to care providers, teachers, and other school
allow children with diabetes to participate ensure the safe and fair treatment of chil- personnel who interact with the child, in-
fully and safely in the school experience dren with diabetes in the school and day cluding school administrators, school
(3,4). care setting (10 –15) (www.diabetes.org/ nurses, coaches, health aides, bus drivers,
schooldiscrimination). secretaries, etc. (3,20). Current recom-
DIABETES AND mendations and up-to-date resources re-
THE LAW — Federal laws that protect Diabetes care in schools garding appropriate care for children with
children with diabetes include Section Appropriate diabetes care in the school diabetes in the school are universally
504 of the Rehabilitation Act of 1973 (5), and day care setting is necessary for the available to all school personnel (3,23).
the Individuals with Disabilities Educa- child’s immediate safety, long-term well The purpose of this position state-
tion Act (originally the Education for All being, and optimal academic perfor- ment is to provide recommendations for
Handicapped Children Act of 1975) (6), mance. The Diabetes Control and Com- the management of children with diabetes
and the Americans with Disabilities Act plications Trial showed a significant link in the school and day care setting.
(7). Under these laws, diabetes has been between blood glucose control and later
considered to be a disability, and it is il- development of diabetes complications,
GENERAL GUIDELINES FOR
legal for schools and/or day care centers to with improved glycemic control decreas-
THE CARE OF THE CHILD IN
discriminate against children with dis- ing the risk of these complications
THE SCHOOL AND DAY CARE
abilities. In addition, any school that re- (16,17). To achieve glycemic control, a
SETTING
ceives federal funding or any facility child must check blood glucose fre-
considered open to the public must rea- quently, monitor food intake, take medi-
I. Diabetes Medical Management
sonably accommodate the special needs cations, and engage in regular physical
Plan
of children with diabetes. Indeed, federal activity. Insulin is usually taken in multi-
An individualized Diabetes Medical Man-
law requires an individualized assessment ple daily injections or through an infusion
agement Plan (DMMP) should be devel-
of any child with diabetes. The required pump. Crucial to achieving glycemic con-
oped by the student’s personal diabetes
accommodations should be documented trol is an understanding of the effects of
health care team with input from the par-
in a written plan developed under the ap- physical activity, nutrition therapy, and
ent/guardian. Inherent in this process are
plicable federal law such as a Section 504 insulin on blood glucose levels.
delineated responsibilities assumed by all
Plan or Individualized Education Pro- To facilitate the appropriate care of
parties, including the parent/guardian,
gram (IEP). The needs of a student with the student with diabetes, the school
the school personnel, and the student
diabetes should be provided for within nurse as well as other school and day care
(3,24,25). These responsibilities are out-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
lined in this position statement. In addi-
Originally approved 1998. Revised 2008. tion, the DMMP should be used as the
DOI: 10.2337/dc10-S070
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly basis for the development of written edu-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. cation plans such as the Section 504 Plan
org/licenses/by-nc-nd/3.0/ for details. or the IEP. The DMMP should address the
S70 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
specific needs of the child and provide maintenance of the blood glucose lows: level 1 training for all school
specific instructions for each of the fol- monitoring equipment (i.e., cleaning staff members, which includes a ba-
lowing: and performing controlled testing sic overview of diabetes, typical
per the manufacturer’s instructions) needs of a student with diabetes, rec-
1. Blood glucose monitoring, including and must provide materials neces- ognition of hypoglycemia and hyper-
the frequency and circumstances re- sary to ensure proper disposal of ma- glycemia, and who to contact for
quiring blood glucose checks, and use terials. A separate logbook should be help; level 2 training for school staff
of continuous glucose monitoring if kept at school with the diabetes sup- members who have responsibility for
utilized. plies for the staff or student to record a student or students with diabetes,
2. Insulin administration (if necessary), blood glucose and ketone results; which includes all content from level
including doses/injection times pre- blood glucose values should be trans- 1 plus recognition and treatment of
scribed for specific blood glucose val- mitted to the parent/guardian for re- hypoglycemia and hyperglycemia
ues and for carbohydrate intake, the view as often as requested. Some and required accommodations for
storage of insulin, and, when appro- students maintain a record of blood those students; and level 3 training
priate, physician authorization of par- glucose results in meter memory for a small group of school staff mem-
ent/guardian adjustments to insulin rather than recording in a logbook, bers who will perform student-
dosage. especially if the same meter is used at specific routine and emergency care
3. Meals and snacks, including food con- home and at school. tasks such as blood glucose monitor-
tent, amounts, and timing. 2. The DMMP completed and signed by ing, insulin administration, and glu-
4. Symptoms and treatment of hypogly- the student’s personal diabetes health cagon administration when a school
cemia (low blood glucose), including care team. nurse is not available to perform
the administration of glucagon if rec- 3. Supplies to treat hypoglycemia, in- these tasks and which will include
ommended by the student’s treating cluding a source of glucose and a glu- level 1 and 2 training as well.
physician. cagon emergency kit, if indicated in 3. Immediate accessibility to the treat-
5. Symptoms and treatment of hypergly- the DMMP. ment of hypoglycemia by a knowl-
cemia (high blood glucose). 4. Information about diabetes and the edgeable adult. The student should
6. Checking for ketones and appropriate performance of diabetes-related remain supervised until appropriate
actions to take for abnormal ketone tasks. treatment has been administered,
levels, if requested by the student’s 5. Emergency phone numbers for the and the treatment should be available
health care provider. parent/guardian and the diabetes as close to where the student is as
7. Participation in physical activity. health care team so that the school possible.
8. Emergency evacuation/school lock- can contact these individuals with di- 4. Accessibility to scheduled insulin at
down instructions. abetes-related questions and/or dur- times set out in the student’s DMMP
ing emergencies. as well as immediate accessibility to
A sample DMMP (http://www.diabe 6. Information about the student’s treatment for hyperglycemia includ-
tes.org/uedocuments/DMMP-finalfor meal/snack schedule. The parent ing insulin administration as set out
matted.pdf) may be accessed online and should work with the school during by the student’s DMMP.
customized for each individual student. the teacher preparation period before 5. A location in the school that provides
For detailed information on the symp- the beginning of the school year or privacy during blood glucose moni-
toms and treatment of hypoglycemia and before the student returns to school toring and insulin administration, if
hyperglycemia, refer to Medical Manage- after diagnosis to coordinate this desired by the student and family, or
ment of Type 1 Diabetes (26). A brief de- schedule with that of the other stu- permission for the student to check
scription of diabetes targeted to school dents as closely as possible. For his or her blood glucose level and
and day care personnel is included in the young children, instructions should take appropriate action to treat hypo-
APPENDIX; it may be helpful to include this be given for when food is provided glycemia in the classroom or any-
information as an introduction to the during school parties and other activ- where the student is in conjunction
DMMP. ities. with a school activity, if indicated in
7. In most locations, and increasingly, a the student’s DMMP.
II. Responsibilities of the various signed release of confidentiality from 6. School nurse and back-up trained
care providers (3) the legal guardian will be required so school personnel who can check
that the health care team can commu- blood glucose and ketones and ad-
A. The parent/guardian should provide nicate with the school. Copies should minister insulin, glucagon, and other
the school or day care provider with be retained both at the school and in medications as indicated by the stu-
the following: the health care professionals’ offices. dent’s DMMP.
7. School nurse and back-up trained
1. All materials, equipment, insulin, B. The school or day care provider school personnel responsible for the
and other medication necessary for should provide the following: student who will know the schedule
diabetes care tasks, including blood of the student’s meals and snacks and
glucose monitoring, insulin adminis- 1. Opportunities for the appropriate work with the parent/guardian to co-
tration (if needed), and urine or level of ongoing training and diabetes ordinate this schedule with that of
blood ketone monitoring. The par- education for the school nurse. the other students as closely as pos-
ent/guardian is responsible for the 2. Training for school personnel as fol- sible. This individual will also notify
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S71
American Diabetes Association
Table 1—Resources for teachers, child care providers, parents, and health professionals tasks and in the treatment of diabetes
Helping the Student with Diabetes Succeed: A Guide for School Personnel. National Diabetes Education
emergencies. This training should be pro-
Program, 2003. Available at http://www.ndep.nih.gov/Diabetes/pubs/Youth_SchoolGuide.pdf vided by the school nurse or another
Diabetes Care Tasks at School: What Key Personnel Need to Know. Alexandria, VA, American qualified health care professional with ex-
Diabetes Association, 2008. Available online at www.diabetes.org/assets/pdfs/schools/ pertise in diabetes. Members of the stu-
forward2008.pdf dent’s diabetes health care team should
Your School & Your Rights: Protecting Children with Diabetes Against Discrimination in Schools provide school personnel and parents/
and Day Care Centers. Alexandria, VA, American Diabetes Association, 2005 (brochure). guardians with educational materials
Available online at http://www.diabetes.org/your-school-your-rights.* from the American Diabetes Association
Children with Diabetes: Information for School and Child Care Providers. Alexandria, VA, and other sources targeted to school per-
American Diabetes Association, 2004 (brochure). Available at http://www.diabetes.org/ sonnel and/or parents. Table 1 includes a
assets/pdfs/schools/chren-wdiabetes-brochure-caregivers.pdf.* listing of appropriate resources.
ADA’s Safe at School campaign and information on how to keep children with diabetes safe at
school. Call 1-800-DIABETES and go to www.diabetes.org/living-with-diabetes/parents- III. Expectations of the student in
and-kids/diabetes-care-at-school/ diabetes care
American Diabetes Association: Complete Guide to Diabetes. Alexandria, VA, American Children and youth should be allowed to
Diabetes Association, 2005. Call 1-800-232–6733. provide their own diabetes care at school
Raising a Child with Diabetes: A Guide for Parents. Alexandria, VA, American Diabetes to the extent that is appropriate based on
Association, 2000. Call 1-800-232–6733. the student’s development and his or her
Clarke W: Advocating for the child with diabetes. Diabetes Spectrum 12:230–236, 1999. experience with diabetes. The extent of
School Discrimination Resources. Alexandria, VA, American Diabetes Association, 2006. Avail- the student’s ability to participate in dia-
able at http://www.diabetes.org/living-with-diabetes/know-your-rights/discrimination/school- betes care should be agreed upon by the
discrimination/* school personnel, the parent/guardian,
Wizdom: A Kit of Wit and Wisdom for Kids with Diabetes (and their parents). Alexandria, VA, and the health care team, as necessary.
American Diabetes Association, 2000. Order information and select resources available at The ages at which children are able to per-
www.diabetes.org/wizdom. form self-care tasks are variable and de-
ADA’s Planet D, on-line information for children and youth with diabetes. Accessible at pend on the individual, and a child’s
http://tracker.diabetes.org/index.php. capabilities and willingness to provide
self-care should be respected (18).
*Available in the American Diabetes Association’s Education Discrimination Packet by calling 1-800-
DIABETES.
1. Toddlers and preschool-aged children:
unable to perform diabetes tasks in-
the parent/guardian in advance of 13. An appropriate location for insulin dependently and will need an adult
any expected changes in the school and/or glucagon storage, if necessary. to provide all aspects of diabetes care.
schedule that affect the student’s 14. A plan for the disposal of sharps Many of these younger children will
meal times or exercise routine and based upon an agreement with the have difficulty in recognizing hypo-
will remind young children of snack student’s family, local ordinances, glycemia, so it is important that
times. and Universal Precaution Standards. school personnel are able to recog-
8. Permission for self-sufficient and ca- 15. Information on serving size and ca- nize and provide prompt treatment.
pable students to carry equipment, loric, carbohydrate, and fat content However, children in this age range
supplies, medication, and snacks; to of foods served in the school (27). can usually determine which finger
perform diabetes management tasks; to prick, can choose an injection site,
and to have cell phone access to reach The school nurse should be the key and are generally cooperative.
parent/guardian and health care pro- coordinator and provider of care and 2. Elementary school–aged children: de-
vider. should coordinate the training of an ade- pending on the length of diagnosis
9. Permission for the student to see the quate number of school personnel as and level of maturity, may be able to
school nurse and other trained specified above and ensure that if the perform their own blood glucose
school personnel upon request. school nurse is not present at least one checks, but usually will require su-
10. Permission for the student to eat a adult is present who is trained to perform pervision. Older elementary school–
snack anywhere, including the class- these procedures in a timely manner aged children are generally
room or the school bus, if necessary while the student is at school, on field beginning to self-administer insulin
to prevent or treat hypoglycemia. trips, participating in school-sponsored with supervision and understand the
11. Permission to miss school without extracurricular activities, and on trans- effect of insulin, physical activity,
consequences for illness and re- portation provided by the school or day and nutrition on blood glucose lev-
quired medical appointments to care facility. This is needed in order to els. Unless the child has hypoglyce-
monitor the student’s diabetes man- enable full participation in school activi- mic unawareness, he or she should
agement. This should be an excused ties (3,18,20). These school personnel usually be able to let an adult know
absence with a doctor’s note, if re- need not be health care professionals when experiencing hypoglycemia.
quired by usual school policy. (3,9,20,28,33,35). 3. Middle school and high school–aged
12. Permission for the student to use the It is the school’s responsibility to pro- children: usually able to provide self-
restroom and have access to fluids vide appropriate training of an adequate care depending on the length of diag-
(i.e., water) as necessary. number of school staff on diabetes-related nosis and level of maturity but will
S72 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
always need help when experiencing APPENDIX lin, too much food, or too little exercise; it
severe hypoglycemia. Independence may also be caused by stress or an illness
in older children should be encour- Background information on diabetes such as a cold. The most common symp-
aged to enable the child to make his for school personnel (3) toms of hyperglycemia are thirst, frequent
or her decisions about his or her own Diabetes is a serious, chronic disease that urination, and blurry vision. If untreated
care. impairs the body’s ability to use food. In- over a period of days, hyperglycemia and
sulin, a hormone produced by the pan- insufficient insulin can lead to a serious
creas, helps the body convert food into condition called diabetic ketoacidosis
Students’ competence and capability
energy. In people with diabetes, either the (DKA), which is characterized by nausea,
for performing diabetes-related tasks are
pancreas does not make insulin or the vomiting, and a high level of ketones in
set out in the DMMP and then adapted to
body cannot use insulin properly. With- the blood and urine. For students using
the school setting by the school health
out insulin, the body’s main energy insulin infusion pumps, lack of insulin
team and the parent/guardian. At all ages,
source— glucose— cannot be used as supply may lead to DKA more rapidly.
individuals with diabetes may require
fuel. Rather, glucose builds up in the DKA can be life-threatening and thus re-
help to perform a blood glucose check
blood. Over many years, high blood glu- quires immediate medical attention (32).
when the blood glucose is low. In addi-
cose levels can cause damage to the eyes,
tion, many individuals require a reminder
kidneys, nerves, heart, and blood vessels.
to eat or drink during hypoglycemia and Acknowledgments — The American Diabe-
The majority of school-aged youth
should not be left unsupervised until such tes Association thanks the members of the
with diabetes have type 1 diabetes. People
treatment has taken place and the blood health care professional volunteer writing
with type 1 diabetes do not produce insu-
glucose value has returned to the normal group for this updated statement: William
lin and must receive insulin through ei-
range. Ultimately, each person with dia- Clarke, MD; Larry C. Deeb, MD; Paula Jame-
ther injections or an insulin pump.
betes becomes responsible for all aspects son, MSN, ARNP, CDE; Francine Kaufman,
Insulin taken in this manner does not cure MD; Georgeanna Klingensmith, MD; Des-
of routine care, and it is important for
diabetes and may cause the student’s mond Schatz, MD; Janet H. Silverstein, MD;
school personnel to facilitate a student in
blood glucose level to become danger- and Linda M. Siminerio, RN, PhD, CDE.
reaching this goal. However, regardless of
ously low. Type 2 diabetes, the most com-
a student’s ability to provide self-care,
mon form of the disease, typically
help will always be needed in the event of
afflicting obese adults, has been shown to References
a diabetes emergency.
be increasing in youth. This may be due to 1. American Diabetes Association: American
the increase in obesity and decrease in Diabetes Association Complete Guide to Di-
MONITORING BLOOD physical activity in young people. Stu- abetes. 4th ed. Alexandria, VA, American
GLUCOSE IN THE dents with type 2 diabetes may be able to Diabetes Association, 2005
control their disease through diet and ex- 2. Centers for Disease Control and Preven-
CLASSROOM — It is best for a stu- tion: National Diabetes Fact Sheet: General
dent with diabetes to monitor blood glu- ercise alone or may require oral medica-
tions and/or insulin injections. All people Information and National Estimates on Dia-
cose levels and respond to the results as betes in the U.S., 2007. Atlanta, GA, U.S.
quickly and conveniently as possible. with type 1 and type 2 diabetes must care-
Department of Health and Human Ser-
This is important to avoid medical prob- fully balance food, medications, and ac- vices, Centers for Disease Control and
lems being worsened by a delay in moni- tivity level to keep blood glucose levels as Prevention, 2008
toring and treatment and to minimize close to normal as possible. 3. National Diabetes Education Program:
educational problems caused by missing Low blood glucose (hypoglycemia) is Helping the Student with Diabetes Succeed: A
instruction in the classroom. Accord- the most common immediate health Guide for School Personnel. Bethesda, MD,
ingly, as stated earlier, a student should be problem for students with diabetes. It oc- National Institutes of Health (NIH publi-
curs when the body gets too much insu- cation no. 03-5127), 2003
permitted to monitor his or her blood glu- 4. Nabors L, Troillett A, Nash T, Masiulis B:
cose level and take appropriate action to lin, too little food, a delayed meal, or more
than the usual amount of exercise. Symp- School nurse perceptions of barriers and
treat hypoglycemia and hyperglycemia in supports for children with diabetes. J Sch
the classroom or anywhere the student is toms of mild to moderate hypoglycemia
Health 75:119 –124, 2005
in conjunction with a school activity, if include tremors, sweating, light- 5. Section 504 of the Rehabilitation Act of
preferred by the student and indicated in headedness, irritability, confusion, and 1973, 29 U.S.C. 794, implementing reg-
the student’s DMMP (3,24). However, drowsiness. In younger children other ulations at 35 CFR Part 104
some students desire privacy for blood symptoms may include inattention, fall- 6. Individuals with Disabilities Education
glucose monitoring and other diabetes ing asleep at inappropriate times, unex- Act, 20 U.S.C. 111 et seq., implementing
care tasks, and this preference should also plained behavior, and temper tantrums. A regulations at 34 CRF Part 300
student with this degree of hypoglycemia 7. Title II of the Americans with Disabilities
be accommodated. Act of 1990, 42 U.S.C. 12134 et seq., im-
will need to ingest carbohydrates
In summary, with proper planning promptly and may require assistance. Se- plementing regulations at 28 CFR Part 35
and the education and training of school vere hypoglycemia, which is rare, may 8. Rapp J: Students with diabetes in schools.
In Inquiry & Analysis. Alexandria, VA, Na-
personnel, children and youth with dia- lead to unconsciousness and convulsions tional School Boards Association Council
betes can fully participate in the school and can be life-threatening if not treated of School Attorneys, June 2005
experience. To this end, the family, the promptly with glucagon as per the stu- 9. Arent S, Kaufman F: Federal laws and di-
health care team, and the school should dent’s DMMP (18,24,29,30,31). abetes management at school. School
work together to ensure a safe learning High blood glucose (hyperglycemia) Nurse News, November 2004
environment. occurs when the body gets too little insu- 10. Jesi Stuthard and ADA v. Kindercare Learn-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S73
American Diabetes Association
ing Centers, Inc. Case no. C2-96-0185 20. Jameson P: Developing diabetes training Rights Education Defense Fund, Juvenile
(USCD South Ohio 8/96) programs for school personnel. School Diabetes Research Foundation, Lawson
11. Calvin Davis and ADA v. LaPetite Academy, Nurse News, September 2004 Wilkins Pediatric Endocrine Society, Pe-
Inc. Case no. CIV97-0083-PHX-SMM 21. Wysocki T, Meinhold P, Cox DJ, Clarke diatric Endocrine Nursing Society [article
(USCD Arizona 1997) WL: Survey of diabetes professionals re- online]. Available from http://www.
12. Agreement, Loudoun County Public garding developmental charges in diabe- diabetes.org/advocacy-and-legalresources/
Schools (VA) and the Office for Civil tes self-care. Diabetes Care 13:65– 68, discrimination/safeatschoolprinciples.jsp
Rights, United States Department of Edu- 1990 29. Evert A: Managing hypoglycemia in the
cation (Complaint nos. 11-99-1003, 11- 22. Lindsey R, Jarrett L, Hillman K: Elemen- school setting. School Nurse News, No-
99-1064, 11-99-1069, 1999) tary schoolteachers’ understanding of di- vember 2005
13. Henderson County (NC) Pub. Schls., Com- abetes. Diabetes Educ 13:312–314, 1987 30. Bulsara MD, Holman CD, David EA, Jones
plaint no. 11-00-1008, 34 IDLER 43 23. American Diabetes Association: Diabetes TW: The impact of a decade of changing
(OCR 2000) Care Tasks at School: What Key Personnel treatment on rates of severe hypoglycemia
14. Rapp J, Arent S, Dimmick B, Jackson C: Need to Know. Alexandria, VA, American in a population-based cohort of children
Legal Rights of Students with Diabetes. 1st Diabetes Association, 2005 (available on- with type 1 diabetes. Diabetes Care 27:
ed. Alexandria, VA, American Diabetes line at www.diabetes/schooltraining) 2293–2298, 2004
Association, October 2005, updated Oc- 24. Jameson P: Helping students with diabe- 31. Nabors L, Lehmkuhl H, Christos N, An-
tober 2007 tes thrive in school. In On the Cutting Edge, dreone TF: Children with diabetes: per-
15. Greene MA: Diabetes legal advocacy American Dietetic Association’s Diabetes ceptions of supports for self-management
comes of age. Diabetes Spectr 19:171–179, Care and Education Practice Group Newslet- at school. J Sch Health 73:216 –221, 2003
2006 ter. Summer 2006, p. 26 –29 32. Kaufman FR: Diabetes mellitus. Pediatr
16. Diabetes Control and Complications Trial 25. Owen S: Pediatric pumps— barriers and Rev 18:383–392, 1997
Research Group: Effect of intensive diabe- breakthroughs. Pediatric Pumps 32
33. Pediatric Endocrine Nursing Society:
tes treatment on the development and (Suppl. 1), January/February 2006
Children With Diabetes at School. Septem-
progression of long-term complications 26. American Diabetes Association: Medical
ber 2005. Available from the Pediatric En-
in insulin-dependent diabetes mellitus. Management of Type 1 Diabetes. 5th ed. Al-
docrinology Nursing Society, 7794 Grow
N Engl J Med 329:977–986, 1993 exandria, VA, American Diabetes Associ-
Dr., Pensacola, FL 32514
17. Diabetes Control and Complications Trail ation, 2008
Research Group: Effect of intensive diabe- 27. Accommodating Children with Special Dietary 34. Committee on School Health, American
tes treatment on the development and Needs in the School Nutrition Program: Guid- Academy of Pediatrics: Guidelines for the
progression of long-term complications ance for School Food Service Staff. Washing- administration of medication in school.
in adolescents with insulin-dependent di- ton, DC, U.S. Department of Agriculture Pediatrics 112 (3 Pt. 1):697– 699, 2003
abetes mellitus. J Pediatr 125:177–188, Food and Nutrition Service, 2001 35. Hellems MA, Clarke WL: Safe at school: a
1994 28. American Diabetes Association: Safe at Virginia experience. Diabetes Care
18. American Diabetes Association: Care of School Campaign Statement of Principles 30:1396 –1398, 2007
children and adolescents with type 1 dia- endorsed by American Academy of Pedi- 36. American Medical Association: Report 4
betes (Position Statement). Diabetes Care atrics, American Association of Clinical of the Council on Science and Public
28:186 –212, 2005 Endocrinologists, American Association Health (A-08): Ensuring the Best In-School
19. Barrett JC, Goodwin DK, Kendrick O: of Diabetes Educators, American Diabetes Care for Children with Diabetes [article on-
Nursing, food service, and the child with Association, American Dietetic Associa- line], June 2008. Available at http://www.
diabetes. J Sch Nurs 18:150 –156, 2002 tion, Children with Diabetes, Disability ama-assn.org/ama/pub/category/18643.html.
S74 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
P O S I T I O N S T A T E M E N T
Diabetes Management in Correctional
Institutions
AMERICAN DIABETES ASSOCIATION Intake screening
Patients with a diagnosis of diabetes
should have a complete medical history
and physical examination by a licensed
A
t any given time, over 2 million peo- loss, renal failure, and amputation. Early
ple are incarcerated in prisons and identification and intervention for people health care provider with prescriptive au-
jails in the U.S (1). It is estimated with diabetes is also likely to reduce thority in a timely manner. If one is not
that nearly 80,000 of these inmates have short-term risks for acute complications available on site, one should be consulted
diabetes, a prevalence of 4.8% (2). In ad- requiring transfer out of the facility, thus by those performing reception screening.
dition, many more people pass through improving security. The purposes of this history and physical
the corrections system in a given year. In This document provides a general set examination are to determine the type of
1998 alone, over 11 million people were of guidelines for diabetes care in correc- diabetes, current therapy, alcohol use,
released from prison to the community tional institutions. It is not designed to be and behavioral health issues, as well as to
(1). The current estimated prevalence of a diabetes management manual. More de- screen for the presence of diabetes-related
diabetes in correctional institutions is tailed information on the management of complications. The evaluation should re-
somewhat lower than the overall U.S. diabetes and related disorders can be view the previous treatment and the past
prevalence of diabetes, perhaps because found in the American Diabetes Associa- history of both glycemic control and dia-
the incarcerated population is younger tion (ADA) Clinical Practice Recommen- betes complications. It is essential that
than the general population. The preva- dations, published each year in January as medication and medical nutrition therapy
lence of diabetes and its related comor- the first supplement to Diabetes Care, as (MNT) be continued without interrup-
bidities and complications, however, will well as the “Standards of Medical Care in tion upon entry into the correctional sys-
continue to increase in the prison popu- Diabetes” (4) contained therein. This dis- tem, as a hiatus in either medication or
lation as current sentencing guidelines cussion will focus on those areas where appropriate nutrition may lead to either
continue to increase the number of aging the care of people with diabetes in correc- severe hypo- or hyperglycemia that can
prisoners and the incidence of diabetes in tional facilities may differ, and specific rapidly progress to irreversible complica-
young people continues to increase. recommendations are made at the end of tions, even death.
People with diabetes in correctional each section.
facilities should receive care that meets Intake physical examination and
national standards. Correctional institu- INTAKE MEDICAL laboratory
tions have unique circumstances that ASSESSMENT All potential elements of the initial medi-
need to be considered so that all standards cal evaluation are included in Table 5 of
of care may be achieved (3). Correctional Reception screening the ADA’s “Standards of Medical Care in
institutions should have written policies Reception screening should emphasize Diabetes,” referred to hereafter as the
and procedures for the management of patient safety. In particular, rapid identi- “Standards of Care” (4). The essential
diabetes and for training of medical and fication of all insulin-treated persons with components of the initial history and
correctional staff in diabetes care prac- diabetes is essential in order to identify physical examination are detailed in Fig.
tices. These policies must take into con- those at highest risk for hypo- and hyper- 1. Referrals should be made immediately
sideration issues such as security needs, glycemia and diabetic ketoacidosis if the patient with diabetes is pregnant.
transfer from one facility to another, and (DKA). All insulin-treated patients should
access to medical personnel and equip- have a capillary blood glucose (CBG) de- Recommendations
ment, so that all appropriate levels of care termination within 1–2 h of arrival. Signs ● Patients with a diagnosis of diabetes
are provided. Ideally, these policies and symptoms of hypo- or hyperglycemia should have a complete medical history
should encourage or at least allow pa- can often be confused with intoxication or and undergo an intake physical exami-
tients to self-manage their diabetes. Ulti- withdrawal from drugs or alcohol. Indi- nation by a licensed health professional
mately, diabetes management is viduals with diabetes exhibiting signs and in a timely manner. (E)
dependent upon having access to needed symptoms consistent with hypoglycemia, ● Insulin-treated patients should have a
medical personnel and equipment. Ongo- particularly altered mental status, agita- CBG determination within 1–2 h of ar-
ing diabetes therapy is important in order tion, combativeness, and diaphoresis, rival. (E)
to reduce the risk of later complications, should have finger-stick blood glucose ● Medications and MNT should be con-
including cardiovascular events, visual levels measured immediately. tinued without interruption upon entry
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● into the correctional environment. (E)
Originally approved 1989. Most recent revision, 2008.
Abbreviations: CBG, capillary blood glucose; DKA, diabetic ketoacidosis; GDM, gestational diabetes mel- SCREENING FOR DIABETES —
litus; MNT, medical nutrition therapy. Consistent with the ADA Standards of
DOI: 10.2337/dc10-S075
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly
Care, patients should be evaluated for di-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. abetes risk factors at the intake physical
org/licenses/by-nc-nd/3.0/ for details. and at appropriate times thereafter. Those
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S75
Correctional Institutions
Figure 1—Essential components of the initial history and physical examination. Alb/Cr ratio, albumin-to-creatinine ratio; ALT, alanine amino-
transferase; AST, aspartate aminotransferase.
who are at high risk should be considered viduals with comorbid conditions (4). tional institution. Common housing not
for blood glucose screening. If pregnant, a This plan should be documented in the only can facilitate mealtimes and medica-
risk assessment for gestational diabetes patient’s record and communicated to all tion administration, but also potentially
mellitus (GDM) should be undertaken at persons involved in his/her care, includ- provides an opportunity for diabetes self-
the first prenatal visit. Patients with clin- ing security staff. Table 1, taken from the management education to be reinforced
ical characteristics consistent with a high ADA Standards of Care, provides a sum- by fellow patients.
risk for GDM should undergo glucose mary of recommendations for setting gly-
testing as soon as possible. High-risk cemic control goals for adults with NUTRITION AND FOOD
women not found to have GDM at the diabetes. SERVICES — Nutrition counseling and
initial screening and average-risk women People with diabetes should ideally menu planning are an integral part of the
should be tested between 24 and 28 receive medical care from a physician- multidisciplinary approach to diabetes
weeks of gestation. For more detailed in- coordinated team. Such teams include, management in correctional facilities. A
formation on screening for both type 2 but are not limited to, physicians, nurses, combination of education, interdisciplinary
and gestational diabetes, see the ADA Po- dietitians, and mental health profession- communication, and monitoring food in-
sition Statement “Screening for Type 2 Di- als with expertise and a special interest in take aids patients in understanding their
abetes” (5) and the Standards of Care (4). diabetes. It is essential in this collabora- medical nutritional needs and can facilitate
tive and integrated team approach that in- diabetes control during and after incarcera-
MANAGEMENT PLAN — Glyce- dividuals with diabetes assume as active a tion.
mic control is fundamental to the man- role in their care as possible. Diabetes self- Nutrition counseling for patients with
agement of diabetes. A management plan management education is an integral diabetes is considered an essential compo-
to achieve normal or near-normal glyce- component of care. Patient self- nent of diabetes self-management. People
mia with an A1C goal of ⬍7% should be management should be emphasized, and with diabetes should receive individualized
developed for diabetes management at the plan should encourage the involve- MNT as needed to achieve treatment goals,
the time of initial medical evaluation. ment of the patient in problem solving as preferably provided by a registered dietitian
Goals should be individualized (4), and much as possible. familiar with the components of MNT for
less stringent treatment goals may be ap- It is helpful to house insulin-treated persons with diabetes.
propriate for patients with a history of se- patients in a common unit, if this is pos- Educating the patient, individually or
vere hypoglycemia, patients with limited sible, safe, and consistent with providing in a group setting, about how carbohy-
life expectancies, elderly adults, and indi- access to other programs at the correc- drates and food choices directly affect di-
S76 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
risk for hypoglycemia (i.e., those on insulin
Table 1—Summary of recommendations for glycemic, blood pressure, and lipid control for or oral hypoglycemic agents) should be ed-
adults with diabetes ucated in the emergency response protocol
for recognition and treatment of hypoglyce-
A1C ⬍7.0%*
mia. Every attempt should be made to doc-
Blood pressure ⬍130/80 mmHg
ument CBG before treatment. Patients must
Lipids
have immediate access to glucose tablets or
LDL cholesterol ⬍100 mg/dl (⬍2.6 mmol/l)†
other glucose-containing foods. Hypogly-
*Referenced to a nondiabetic range of 4.0 – 6.0% using a DCCT-based assay. †In individuals with overt CVD, cemia can generally be treated by the patient
a lower LDL cholesterol goal of ⬍70 mg/dl (1.8 mmol/l), using a high dose of a statin, is an option.
with oral carbohydrates. If the patient can-
not be relied on to keep hypoglycemia treat-
abetes control is the first step in range, as determined by the treating phy- ment on his/her person, staff members
facilitating self-management. This educa- sician (e.g., ⬍50 or ⬎350 mg/dl). should have ready access to glucose tablets
tion enables the patient to identify better or equivalent. In general, 15–20 g oral glu-
food selections from those available in the Hyperglycemia cose will be adequate to treat hypoglycemic
dining hall and commissary. Such an ap- Severe hyperglycemia in a person with di- events. CBG and treatment should be re-
proach is more realistic in a facility where abetes may be the result of intercurrent peated at 15-min intervals until blood glu-
the patient has the opportunity to make illness, missed or inadequate medication, cose levels return to normal (⬎70 mg/dl).
food choices. or corticosteroid therapy. Correctional Staff should have glucagon for intra-
The easiest and most cost-effective institutions should have systems in place muscular injection or glucose for intrave-
means to facilitate good outcomes in pa- to identify and refer to medical staff all nous infusion available to treat severe
tients with diabetes is instituting a heart- patients with consistently elevated blood hypoglycemia without requiring transport
healthy diet as the master menu (6). There glucose as well as intercurrent illness. of the hypoglycemic patient to an outside
should be consistent carbohydrate con- The stress of illness in those with type facility. Any episode of severe hypoglycemia
tent at each meal, as well as a means to 1 diabetes frequently aggravates glycemic or recurrent episodes of mild to moderate
identify the carbohydrate content of each control and necessitates more frequent hypoglycemia require reevaluation of the
food selection. Providing carbohydrate monitoring of blood glucose (e.g., every diabetes management plan by the medical
content of food selections and/or provid- 4 – 6 h). Marked hyperglycemia requires staff. In certain cases of unexplained or re-
ing education in assessing carbohydrate temporary adjustment of the treatment current severe hypoglycemia, it may be ap-
content enables patients to meet the re- program and, if accompanied by ketosis, propriate to admit the patient to the medical
quirements of their individual MNT interaction with the diabetes care team. unit for observation and stabilization of di-
goals. Commissaries should also help in Adequate fluid and caloric intake must be abetes management.
dietary management by offering healthy ensured. Nausea or vomiting accompa- Correctional institutions should have
choices and listing the carbohydrate con- nied with hyperglycemia may indicate systems in place to identify the patients at
tent of foods. DKA, a life-threatening condition that re- greater risk for hypoglycemia (i.e., those
The use of insulin or oral medications quires immediate medical care to prevent on insulin or sulfonylurea therapy) and to
may necessitate snacks in order to avoid complications and death. Correctional in- ensure the early detection and treatment
hypoglycemia. These snacks are a part of stitutions should identify patients with of hypoglycemia. If possible, patients at
such patients’ medical treatment plans type 1 diabetes who are at risk for DKA, greater risk of severe hypoglycemia (e.g.,
and should be prescribed by medical staff. particularly those with a prior history of those with a prior episode of severe hypo-
Timing of meals and snacks must be frequent episodes of DKA. For further in- glycemia) may be housed in units closer
coordinated with medication administra- formation see “Hyperglycemic Crisis in to the medical unit in order to minimize
tion as needed to minimize the risk of hy- Diabetes” (8). delay in treatment.
poglycemia, as discussed more fully in the
MEDICATION section of this document. For Hypoglycemia Recommendations
further information, see the ADA Position Hypoglycemia is defined as a blood glu- ● Train correctional staff in the recogni-
Statement “Nutrition Principles and Rec- cose level ⬍70 mg/dl. Severe hypoglyce- tion, treatment, and appropriate refer-
ommendations in Diabetes” (7). mia is a medical emergency defined as ral for hypo- and hyperglycemia. (E)
hypoglycemia requiring assistance of a ● Train appropriate staff to administer
URGENT AND EMERGENCY third party and is often associated with glucagon. (E)
ISSUES — All patients must have access mental status changes that may include ● Train staff to recognize symptoms and
to prompt treatment of hypo- and hypergly- confusion, incoherence, combativeness, signs of serious metabolic decompensa-
cemia. Correctional staff should be trained somnolence, lethargy, seizures, or coma. tion, and immediately refer the patient
in the recognition and treatment of hypo- Signs and symptoms of severe hypoglyce- for appropriate medical care. (E)
and hyperglycemia, and appropriate staff mia can be confused with intoxication or ● Institutions should implement a policy
should be trained to administer glucagon. withdrawal. Individuals with diabetes ex- requiring staff to notify a physician of
After such emergency care, patients should hibiting signs and symptoms consistent all CBG results outside of a specified
be referred for appropriate medical care to with hypoglycemia, particularly altered range, as determined by the treating
minimize risk of future decompensation. mental status, agitation, and diaphoresis, physician (e.g., ⬍50 or ⬎350 mg/dl).
Institutions should implement a pol- should have their CBG levels checked im- (E)
icy requiring staff to notify a physician of mediately. ● Identify patients with type 1 diabetes
all CBG results outside of a specified Security staff who supervise patients at who are at high risk for DKA. (E)
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S77
Correctional Institutions
MEDICATION — Formularies should more injections a day) can be effective The following complications should
provide access to usual and customary oral means of implementing intensive diabe- be considered.
medications and insulins necessary to treat tes management with the goal of achiev-
diabetes and related conditions. While not ing near-normal levels of blood glucose ● Foot care: Recommendations for foot
every brand name of insulin and oral med- (9). While the use of these modalities may care for patients with diabetes and no
ication needs to be available, individual pa- be difficult in correctional institutions, history of an open foot lesion are de-
tient care requires access to short-, every effort should be made to continue scribed in the ADA Standards of Care. A
medium-, and long-acting insulins and the multiple daily insulin injection or contin- comprehensive foot examination is rec-
various classes of oral medications (e.g., in- uous subcutaneous insulin infusion in ommended annually for all patients
sulin secretagogues, biguanides, ␣-glucosi- people who were using this therapy be- with diabetes to identify risk factors
dase inhibitors, and thiazolidinediones) fore incarceration or to institute these predictive of ulcers and amputations.
necessary for current diabetes management. therapies as indicated in order to achieve Persons with an insensate foot, an open
Patients at all levels of custody should blood glucose targets. foot lesion, or a history of such a lesion
have access to medication at dosing fre- It is essential that transport of patients should be referred for evaluation by an
quencies that are consistent with their from jails or prisons to off-site appoint- appropriate licensed health profes-
treatment plan and medical direction. If ments, such as medical visits or court ap- sional (e.g., podiatrist or vascular sur-
feasible and consistent with security con- pearances, does not cause significant geon). Special shoes should be
cerns, patients on multiple doses of short- disruption in medication or meal timing. provided as recommended by licensed
acting oral medications should be placed Correctional institutions and police lock- health professionals to aid healing of
in a “keep on person” program. In other ups should implement policies and pro- foot lesions and to prevent develop-
situations, patients should be permitted cedures to diminish the risk of hypo- and ment of new lesions.
to self-inject insulin when consistent with hyperglycemia by, for example, providing ● Retinopathy: Annual retinal examina-
security needs. Medical department carry-along meals and medication for pa- tions by a licensed eye care professional
nurses should determine whether pa- tients traveling to off-site appointments or should be performed for all patients
tients have the necessary skill and respon- changing the insulin regimen for that day. with diabetes, as recommended in the
sible behavior to be allowed self- The availability of prefilled insulin “pens” ADA Standards of Care. Visual changes
administration and the degree of provides an alternative for off-site insulin that cannot be accounted for by acute
supervision necessary. When needed, this delivery. changes in glycemic control require
skill should be a part of patient education. prompt evaluation by an eye care pro-
Reasonable syringe control systems fessional.
should be established. Recommendations ● Nephropathy: An annual spot urine test
In the past, the recommendation that ● Formularies should provide access to for determination of microalbumin-to-
regular insulin be injected 30 – 45 min be- usual and customary oral medications creatinine ratio should be performed.
fore meals presented a significant prob- and insulins to treat diabetes and re- The use of ACE inhibitors or angioten-
lem when “lock downs” or other lated conditions. (E) sin receptor blockers is recommended
disruptions to the normal schedule of ● Patients should have access to medica-
for all patients with albuminuria. Blood
meals and medications occurred. The use tion at dosing frequencies that are con- pressure should be controlled to
of multiple-dose insulin regimens using sistent with their treatment plan and ⬍130/80 mmHg.
rapid-acting analogs can decrease the dis- medical direction. (E) ● Cardiac: People with type 2 diabetes are
ruption caused by such changes in sched- ● Correctional institutions and police
at a particularly high risk of coronary
ule. Correctional institutions should have lock-ups should implement policies artery disease. Cardiovascular disease
systems in place to ensure that rapid- and procedures to diminish the risk of risk factor management is of demon-
acting insulin analogs and oral agents are hypo- and hyperglycemia during off- strated benefit in reducing this compli-
given immediately before meals if this is site travel (e.g., court appearances). (E) cation in patients with diabetes. Blood
part of the patient’s medical plan. It pressure should be measured at every
should be noted however that even mod- routine diabetes visit. In adult patients,
est delays in meal consumption with these ROUTINE SCREENING FOR test for lipid disorders at least annually
agents can be associated with hypoglyce- AND MANAGEMENT OF and as needed to achieve goals with
mia. If consistent access to food within 10 DIABETES COMPLICATIONS — treatment. Use aspirin therapy (75–162
min cannot be ensured, rapid-acting in- All patients with a diagnosis of diabetes mg/day) in all adult patients with dia-
sulin analogs and oral agents are ap- should receive routine screening for dia- betes and cardiovascular risk factors or
proved for administration during or betes-related complications, as detailed in known macrovascular disease. Current
immediately after meals. Should circum- the ADA Standards of Care (4). Interval national standards for adults with dia-
stances arise that delay patient access to chronic disease clinics for persons with betes call for treatment of lipids to goals
regular meals following medication ad- diabetes provide an efficient mechanism of LDL ⱕ100, HDL ⬎40, triglycerides
ministration, policies and procedures to monitor patients for complications of ⬍150 mg/dl and blood pressure to a
must be implemented to ensure the pa- diabetes. In this way, appropriate referrals level of ⬍130/80 mmHg.
tient receives appropriate nutrition to to consultant specialists, such as optome-
prevent hypoglycemia. trists/ophthalmologists, nephrologists,
Both continuous subcutaneous insu- and cardiologists, can be made on an as- MONITORING/TESTS OF
lin infusion and multiple daily insulin in- needed basis and interval laboratory test- GLYCEMIA — Monitoring of CBG is
jection therapy (consisting of three or ing can be done. a strategy that allows caregivers and peo-
S78 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
ple with diabetes to evaluate diabetes ing to occur at the frequency necessi- ● what diabetes is
management regimens. The frequency of tated by the individual patient’s ● signs and symptoms of diabetes
monitoring will vary by patients’ glycemic glycemic control and diabetes regimen. ● risk factors
control and diabetes regimens. Patients (E) ● signs and symptoms of, and emergency
with type 1 diabetes are at risk for hypo- ● A1C should be checked every 3– 6 response to, hypo- and hyperglycemia
glycemia and should have their CBG months. (E) ● glucose monitoring
monitored three or more times daily. Pa- ● medications
tients with type 2 diabetes on insulin need ● exercise
to monitor at least once daily and more SELF-MANAGEMENT ● nutrition issues including timing of
frequently based on their medical plan. EDUCATION — Self-management meals and access to snacks
Patients treated with oral agents should education is the cornerstone of treatment
have CBG monitored with sufficient fre- for all people with diabetes. The health Recommendations
quency to facilitate the goals of glycemic staff must advocate for patients to partic- ● Include diabetes in correctional staff
control, assuming that there is a program ipate in self-management as much as pos- education programs. (E)
for medical review of these data on an sible. Individuals with diabetes who learn
ongoing basis to drive changes in medica- self-management skills and make lifestyle
tions. Patients whose diabetes is poorly changes can more effectively manage ALCOHOL AND DRUGS — P a -
controlled or whose therapy is changing their diabetes and avoid or delay compli- tients with diabetes who are withdrawing
should have more frequent monitoring. cations associated with diabetes. In the from drugs and alcohol need special consid-
Unexplained hyperglycemia in a patient development of a diabetes self- eration. This issue particularly affects initial
with type 1 diabetes may suggest impend- management education program in the police custody and jails. At an intake facility,
ing DKA, and monitoring of ketones correctional environment, the unique cir- proper initial identification and assessment
should therefore be performed. cumstances of the patient should be con- of these patients are critical. The presence of
Glycated hemoglobin (A1C) is a mea- sidered while still providing, to the diabetes may complicate detoxification. Pa-
sure of long-term (2- to 3-month) glyce- greatest extent possible, the elements of tients in need of complicated detoxification
mic control. Perform the A1C test at least the “National Standards for Diabetes Self- should be referred to a facility equipped to
two times a year in patients who are meet- Management Education” (11). A staged deal with high-risk detoxification. Patients
ing treatment goals (and who have stable approach may be used depending on the with diabetes should be educated in the
glycemic control) and quarterly in pa- needs assessment and the length of incar- risks involved with smoking. All inmates
tients whose therapy has changed or who ceration. Table 2 sets out the major com- should be advised not to smoke. Assistance
are not meeting glycemic goals. ponents of diabetes self-management in smoking cessation should be provided as
Discrepancies between CBG monitor- education. Survival skills should be ad- practical.
ing results and A1C may indicate a hemo- dressed as soon as possible; other aspects
globinopathy, hemolysis, or need for of education may be provided as part of
evaluation of CBG monitoring technique an ongoing education program. TRANSFER AND
and equipment or initiation of more fre- Ideally, self-management education is DISCHARGE — Patients in jails may
quent CBG monitoring to identify when coordinated by a certified diabetes educa- be housed for a short period of time be-
glycemic excursions are occurring and tor who works with the facility to develop fore being transferred or released, and it is
which facet of the diabetes regimen is polices, procedures, and protocols to en- not unusual for patients in prison to be
changing. sure that nationally recognized education transferred within the system several
In the correctional setting, policies guidelines are implemented. The educa- times during their incarceration. One of
and procedures need to be developed and tor is also able to identify patients who the many challenges that health care pro-
implemented regarding CBG monitoring need diabetes self-management educa- viders face working in the correctional
that address the following. tion, including an assessment of the pa- system is how to best collect and commu-
tients’ medical, social, and diabetes nicate important health care information
● infection control in a timely manner when a patient is in
histories; diabetes knowledge, skills, and
● education of staff and patients initial police custody, is jailed short term,
behaviors; and readiness to change.
● proper choice of meter or is transferred from facility to facility.
● disposal of testing lancets The importance of this communication
● quality control programs becomes critical when the patient has a
● access to health services STAFF EDUCATION — Policies and chronic illness such as diabetes.
● size of the blood sample procedures should be implemented to en- Transferring a patient with diabetes
● patient performance skills sure that the health care staff has adequate from one correctional facility to another
● documentation and interpretation of knowledge and skills to direct the man- requires a coordinated effort. To facilitate
test results agement and education of persons with a thorough review of medical information
● availability of test results for the health diabetes. The health care staff needs to be and completion of a transfer summary, it
care provider (10) involved in the development of the cor- is critical for custody personnel to provide
rectional officers’ training program. The medical staff with sufficient notice before
Recommendations staff education program should be at a lay movement of the patient.
● In the correctional setting, policies and level. Training should be offered at least Before the transfer, the health care
procedures need to be developed and biannually, and the curriculum should staff should review the patient’s medical
implemented to enable CBG monitor- cover the following. record and complete a medical transfer
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S79
Correctional Institutions
care and facilitate entry into commu-
Table 2—Major components of diabetes self-management education nity diabetes care. (E)
Survival skills Daily management issues
• hypo-/hyperglycemia • disease process SHARING OF MEDICAL
• sick day management • nutritional management INFORMATION AND
• medication • physical activity RECORDS — Practical considerations
• monitoring • medications may prohibit obtaining medical records
• foot care • monitoring from providers who treated the patient
• acute complications before arrest. Intake facilities should im-
• risk reduction plement policies that 1) define the cir-
• goal setting/problem solving cumstances under which prior medical
• psychosocial adjustment records are obtained (e.g., for patients
• preconception care/pregnancy/gestational diabetes who have an extensive history of treat-
management ment for complications); 2) identify per-
son(s) responsible for contacting the prior
summary that includes the patient’s cur- care provider upon arrival at the receiving provider; and 3) establish procedures for
rent health care issues. At a minimum, the institution. tracking requests.
summary should include the following. Planning for patients’ discharge from Facilities that use outside medical
prisons should include instruction in the providers should implement policies and
● the patient’s current medication sched- long-term complications of diabetes, the procedures for ensuring that key informa-
ule and dosages necessary lifestyle changes and examina- tion (e.g., test results, diagnoses, physi-
● the date and time of the last medication tions required to prevent these complica- cians’ orders, appointment dates) is
administration tions, and, if possible, where patients may received from the provider and incorpo-
● any recent monitoring results (e.g., obtain regular follow-up medical care. A rated into the patient’s medical chart after
CBG and A1C) quarterly meeting to educate patients each outside appointment. The proce-
● other factors that indicate a need for with upcoming discharges about commu- dure should include, at a minimum, a
immediate treatment or management at nity resources can be valuable. Inviting means to highlight when key information
the receiving facility (e.g., recent epi- community agencies to speak at these has not been received and designation of a
sodes of hypoglycemia, history of se- meetings and/or provide written materi- person responsible for contacting the out-
vere hypoglycemia or frequent DKA, als can help strengthen the community side provider for this information.
concurrent illnesses, presence of diabe- link for patients discharging from correc- All medical charts should contain
tes complications) tional facilities. CBG test results in a specified, readily ac-
● information on scheduled treatment/ Discharge planning for the patients cessible section and should be reviewed
appointments if the receiving facility is with diabetes should begin 1 month be- on a regular basis.
responsible for transporting the patient fore discharge. During this time, applica-
to that appointment tion for appropriate entitlements should
● name and telephone/fax number of a be initiated. Any gaps in the patient’s CHILDREN AND
contact person at the transferring facil- knowledge of diabetes care need to be ADOLESCENTS WITH
ity who can provide additional infor- identified and addressed. It is helpful if DIABETES — Children and adoles-
mation, if needed the patient is given a directory or list of cents with diabetes present special prob-
community resources and if an appoint- lems in disease management, even
The medical transfer summary, ment for follow-up care with a commu- outside the setting of a correctional insti-
which acts as a quick medical reference nity provider is made. A supply of tution. Children and adolescents with di-
for the receiving facility, should be trans- medication adequate to last until the first abetes should have initial and follow-up
ferred along with the patient. To supple- postrelease medical appointment should care with physicians who are experienced
ment the flow of information and to be provided to the patient upon release. in their care. Confinement increases the
increase the probability that medications The patient should be provided with a difficulty in managing diabetes in chil-
are correctly identified at the receiving in- written summary of his/her current heath dren and adolescents, as it does in adults
stitution, sending institutions are encour- care issues, including medications and with diabetes. Correctional authorities
aged to provide each patient with a doses, recent A1C values, etc. also have different legal obligations for
medication card to be carried by the pa- children and adolescents.
tient that contains information concern-
ing diagnoses, medication names, Recommendations Nutrition and activity
dosages, and frequency. Diabetes sup- ● For all interinstitutional transfers, com- Growing children and adolescents have
plies, including diabetes medication, plete a medical transfer summary to be greater caloric/nutritional needs than
should accompany the patient. transferred with the patient. (E) adults. The provision of an adequate
The sending facility must be mindful ● Diabetes supplies and medication amount of calories and nutrients for ado-
of the transfer time in order to provide the should accompany the patient during lescents is critical to maintaining good
patient with medication and food if transfer. (E) nutritional status. Physical activity should
needed. The transfer summary or medical ● Begin discharge planning with ade- be provided at the same time each day. If
record should be reviewed by a health quate lead time to insure continuity of increased physical activity occurs, addi-
S80 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
tional CBG monitoring is necessary and change these standards. Patients must (Position Statement). Diabetes Care 33
additional carbohydrate snacks may be have access to medication and nutrition (Suppl. 1):S11–S61, 2010
required. needed to manage their disease. In pa- 5. American Diabetes Association: Screening
tients who do not meet treatment targets, for type 2 diabetes (Position Statement). Di-
abetes Care 27 (Suppl. 1):S11–S14, 2004
Medical management and follow-up medical and behavioral plans should be 6. Krauss RM, Eckel RH, Howard B, Appel
Children and adolescents who are incarcer- adjusted by health care professionals in LJ, Daniels SR, Deckelbaum RJ, Erdman
ated for extended periods should have fol- collaboration with the prison staff. It is JW Jr, Kris-Etherton P, Goldberg IJ,
low-up visits at least every 3 months with critical for correctional institutions to Kotchen TA, Lichtenstein AH, Mitch WE,
individuals who are experienced in the care identify particularly high-risk patients in Mullis R, Robinson K, Wylie-Rosett J, St
of children and adolescents with diabetes. need of more intensive evaluation and Jeor S, Suttie J, Tribble DL, Bazzarre TL:
Thyroid function tests and fasting lipid and therapy, including pregnant women, pa- American Heart Association Dietary
tients with advanced complications, a his- Guidelines: revision 2000: a statement for
microalbumin measurements should be
tory of repeated severe hypoglycemia, or healthcare professionals from the Nutri-
performed according to recognized stan- tion Committee of the American Heart As-
dards for children and adolescents (12) in recurrent DKA.
sociation. Stroke 31:2751–2766, 2000
order to monitor for autoimmune thyroid A comprehensive, multidisciplinary 7. American Diabetes Association: Nutrition
disease and complications and comorbidi- approach to the care of people with dia- recommendations and interventions for
ties of diabetes. betes can be an effective mechanism to diabetes (Position Statement). Diabetes
Children and adolescents with diabe- improve overall health and delay or pre- Care 31 (Suppl. 1):S61–S78, 2008
tes exhibiting unusual behavior should vent the acute and chronic complications 8. American Diabetes Association: Hyper-
have their CBG checked at that time. Be- of this disease. glycemic crisis in diabetes (Position State-
cause children and adolescents are re- ment). Diabetes Care 27 (Suppl. 1):S94 –
S102, 2004
ported to have higher rates of nocturnal Acknowledgments — The following mem- 9. American Diabetes Association: Continu-
hypoglycemia (13), consideration should bers of the American Diabetes Association/ ous subcutaneous insulin infusion (Posi-
be given regarding the use of episodic National Commission on Correctional Health tion Statement). Diabetes Care 27 (Suppl.
overnight blood glucose monitoring in Care Joint Working Group on Diabetes Guide- 1):S110, 2004
these patients. In particular, this should lines for Correctional Institutions contributed 10. American Diabetes Association: Tests of gly-
be considered in children and adolescents to the revision of this document: Daniel L. cemia in diabetes (Position Statement). Di-
who have recently had their overnight in- Lorber, MD, FACP, CDE (chair); R. Scott abetes Care 27 (Suppl. 1):S91–S93, 2004
sulin dose changed. Chavez, MPA, PA-C; Joanne Dorman, RN, 11. American Diabetes Association: National
CDE, CCHP-A; Lynda K. Fisher, MD; standards for diabetes self-management
Stephanie Guerken, RD, CDE; Linda B. Haas, education (Standards and Review Crite-
PREGNANCY — P r e g n a n c y i n a CDE, RN; Joan V. Hill, CDE, RD; David Ken- ria). Diabetes Care 31 (Suppl. 1):S97–
woman with diabetes is by definition a dall, MD; Michael Puisis, DO; Kathy S104, 2008
Salomone, CDE, MSW, APRN; Ronald M. 12. International Society for Pediatric and
high-risk pregnancy. Every effort should
Shansky, MD, MPH; and Barbara Wakeen, Adolescent Diabetes: Consensus Guidelines
be made to ensure that treatment of the RD, LD. 2000: ISPAD Consensus Guidelines for the
pregnant woman with diabetes meets ac- Management of Type 1 Diabetes Mellitus in
cepted standards (14,15). It should be Children and Adolescents. Zeist, Nether-
noted that glycemic standards are more References lands, Medical Forum International,
stringent, the details of dietary manage- 1. National Commission on Correctional 2000, p. 116, 118
ment are more complex and exacting, in- Health Care: The Health Status of Soon- 13. Kaufman FR, Austin J, Neinstein A, Jeng L,
sulin is the only antidiabetic agent to-Be Released Inmates: A Report to Con- Halyorson M, Devoe DJ, Pitukcheewanont
approved for use in pregnancy, and a gress. Vol. 1. Chicago, NCCHC, 2002 P: Nocturnal hypoglycemia detected with
number of medications used in the man- 2. Hornung CA, Greifinger RB, Gadre S: A the continuous glucose monitoring system
agement of diabetic comorbidities are Projection Model of the Prevalence of Se- in pediatric patients with type 1 diabetes.
lected Chronic Diseases in the Inmate Popu- J Pediatr 141:625– 630, 2002
known to be teratogenic and must be dis- lation. Vol. 2. Chicago, NCCHC, 2002, p. 14. American Diabetes Association: Gesta-
continued in the setting of pregnancy. 39 –56 tional diabetes mellitus (Position State-
3. Puisis M: Challenges of improving quality ment). Diabetes Care 27 (Suppl. 1):S88 –
in the correctional setting. In Clinical S90, 2004
SUMMARY AND KEY Practice in Correctional Medicine. St. Louis, 15. Jovanovic L (Ed.): Medical Managementof
POINTS — People with diabetes MO, Mosby-Yearbook, 1998, p. 16 –18 Pregnancy Complicated by Diabetes. 3rd ed.
should receive care that meets national 4. American Diabetes Association: Stan- Alexandria, VA, American Diabetes Asso-
standards. Being incarcerated does not dards of medical care in diabetes—2010 ciation, 2000
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S81
P O S I T I O N S T A T E M E N T
Diabetes and Employment
AMERICAN DIABETES ASSOCIATION
A
s of 2007, approximately 23.6 mil- cations used to the tools used to vidualized assessment of the candidate or
lion Americans have diabetes (1), administer them and to monitor blood employee with diabetes.
most of whom are or wish to be par- glucose levels.
ticipating members of the workforce. Di- Employment decisions should not be Role of diabetes health care
abetes usually has no impact on an based on generalizations or stereotypes professionals
individual’s ability to do a particular job, regarding the effects of diabetes. The im- When questions arise about the medical
and indeed an employer may not even pact of diabetes and its management var- fitness of a person with diabetes for a par-
know that a given employee has diabetes. ies widely among individuals. Therefore, ticular job, a health care professional with
In 1984, the American Diabetes Associa- a proper assessment of individual candi- expertise in treating diabetes should per-
tion adopted the following position on dates for employment or current employ- form an individualized assessment. The
employment: ees must take this variability into account. involvement of the diabetes health care
Any person with diabetes, whether insulin
In addition, federal and state laws re- professional should occur before any ad-
[treated] or non–insulin [treated], should quire employers to make decisions that verse employment decision, such as fail-
be eligible for any employment for which are based on assessment of the circum- ure to hire or promote or termination. A
he/she is otherwise qualified. stances and capabilities of the individual health professional who is familiar with
with diabetes for the particular job in the person with diabetes and who has ex-
Questions are sometimes raised by em- question (2,3). Application of blanket pertise in treating diabetes is best able to
ployers about the safety and effectiveness policies to individuals with diabetes re- perform such an assessment. In some sit-
of individuals with diabetes in a given job. sults in people with diabetes being denied uations and in complex cases, an endocri-
When such questions are legitimately employment for which they are well qual- nologist or a physician who specializes in
raised, a person with diabetes should be ified and fully capable of performing ef- treating diabetes or its complications is
individually assessed to determine fectively and safely. It should be noted the best qualified health professional to
whether or not that person can safely and that, as a result of amendments to the assume this responsibility (4). The indi-
effectively perform the particular duties of Americans with Disabilities Act, which vidual’s treating physician is generally the
the job in question. This document pro- became effective on 1 January 2009, all health care professional with the best
vides a general set of guidelines for eval- persons with diabetes are considered to knowledge of an individual’s diabetes.
uating individuals with diabetes for have a “disability” within the meaning of Thus, even when the employer utilizes its
employment, including how an assess- that law. This is because, among other own physician to perform the evaluation,
ment should be performed and what the opinions of the treating physician and
reasons, diabetes constitutes a substantial
changes (accommodations) in the work- other health care professionals with clin-
limitation on endocrine system function-
place may be needed for an individual ical expertise in diabetes should be sought
ing—the Act was amended to extend its
with diabetes. out and carefully considered. In situations
coverage to persons with a substantial where there is disagreement between the
I. EVALUATING limitation in, among other things, a major opinion of the employee’s treating physi-
INDIVIDUALS WITH bodily function, such as the endocrine cian and that of the employer’s physician,
DIABETES FOR system. Therefore, persons with diabetes the evaluation should be handed over to
EMPLOYMENT — It was once com- are protected from discrimination in em- an independent health care professional
mon practice to restrict individuals with ployment and other areas. The amend- with significant clinical expertise in
diabetes from certain jobs or classes of ments overturned a series of Supreme diabetes.
employment solely because of the diagno- Court decisions that had severely nar-
sis of diabetes or the use of insulin, with- rowed who was covered by the law and
resulted in many people with diabetes Individual assessment
out regard to an individual’s abilities or
and other chronic illnesses being denied A medical evaluation of an individual
circumstances. Such “blanket bans” are
protection from discrimination. This sec- with diabetes may occur only in limited
medically inappropriate and ignore the
circumstances (3). Employers may not in-
many advancements in diabetes manage- tion provides an overview of the factors
quire about an individual’s health sta-
ment that range from the types of medi- relevant to a medically appropriate indi-
tus— directly or indirectly and regardless
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
of the type of job— before making a job
Revised Fall 2009. offer, but may require a medical examina-
DOI: 10.2337/dc10-S082
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly tion or make a medical inquiry once an
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. offer of employment has been extended
org/licenses/by-nc-nd/3.0/ for details. and before the individual begins the job.
S82 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
The job offer may be conditioned on the considered. Only health care profession- based on sufficient and appropriate
results of the medical inquiry or examina- als tasked with such evaluations should medical data and should never be made
tion. An employer may withdraw an offer have access to employee medical informa- based solely on one piece of data. (E)
from an applicant with diabetes only if it tion, and this information must be kept ● Screening guidelines and protocols can
becomes clear that he or she cannot do the separate from personnel records (3). be useful tools in making decisions
essential functions of the job or would about employment if they are used in
pose a direct threat (i.e., a significant risk Screening guidelines an objective way and based on the latest
of substantial harm) to health or safety A number of screening guidelines for scientific knowledge about diabetes
and such threat could not be eliminated evaluating individuals with diabetes in and its management. (E)
with an accommodation (a workplace various types of high risk jobs have been
change that enables a worker with a dis- developed in recent years. Examples in- II. EVALUATING THE
ability to safely and effectively perform clude the American College of Occupa- SAFETY RISK OF
job duties). Another situation in which a tional and Environmental Medicine’s EMPLOYEES WITH
medical evaluation is permissible is when National Consensus Guideline for the DIABETES — Employers who deny
a problem potentially related to the em- Medical Evaluation of Law Enforcement job opportunities because they perceive
ployee’s diabetes arises on the job and Officers, the National Fire Protection As- all people with diabetes to be a safety risk
such problem could affect job perfor- sociation’s Standard on Comprehensive do so based on misconceptions, misinfor-
mance and/or safety. In this situation, a Occupational Medical Program for Fire mation, or a lack of current information
physician may be asked to evaluate the Departments, the U.S. Department of about diabetes. The following guidelines
employee’s fitness to remain on the job Transportation’s Federal Motor Carrier provide information for evaluating an in-
and/or his or her ability to safely perform Safety Administration’s Diabetes Exemp- dividual with diabetes who works or
the job. tion Program, and the U.S. Marshall Ser- seeks to work in what may be considered
Employers also may obtain medical vice and Federal Occupational Health a safety-sensitive position.
information about an employee when Law Enforcement Program Diabetes
the employee has requested an accomo- Protocol. Safety concerns
dation and his or her disability or need Such guidelines and protocols can be The first step in evaluating safety con-
for accommodation is not obvious. An useful tools in making decisions about in- cerns is to determine whether the con-
employer should not rely on a medical dividual candidates or employees if they cerns are reasonable in light of the job
evaluation to deny an employment op- are used in an objective way and based on duties the individual must perform. For
portunity to an individual with diabetes the latest scientific knowledge about dia- most types of employment (such as jobs
unless it is conducted by a health care betes and its management. These proto- in an office, retail, or food service environ-
professional with expertise in diabetes cols should be regularly reevaluated and ment) there is no reason to believe that the
and based on sufficient and appropriate updated to reflect changes in diabetes individual’s diabetes will put employees
medical data. The information sought and knowledge and evidence and should be or the public at risk. In other types of em-
assessed must be properly limited to data developed and reviewed by health care ployment (such as jobs where the individ-
relevant to the individual’s diabetes and professionals with significant experience ual must carry a firearm or operate
job performance (3). The data needed will in diabetes and its treatment. Individuals dangerous machinery) the safety concern
vary depending on the type of job and the who do not meet the standards set forth in is whether the employee will become sud-
reason for the evaluation, but an evalua- such protocols should be given the op- denly disoriented or incapacitated. Such
tion should never be made based only on portunity to demonstrate exceptional cir- episodes, which are usually due to se-
one piece of data, such as a single blood cumstances that would justify deviating verely low blood glucose (hypoglycemia),
glucose result or A1C result. Since diabe- from the guidelines. Such guidelines or occur only in people receiving certain
tes is a chronic disease in which health protocols are not absolute criteria but treatments such as insulin or secreta-
status and management requirements rather the framework for a thorough indi- gogues such as sulfonylureas and even
naturally change over time, it is inappro- vidualized assessment. then occur infrequently. Workplace ac-
priate—and medically unnecessary—for commodations can be made that are min-
examiners to collect all past laboratory Recommendations imal yet effective in helping the individual
values or information regarding office vis- ● People with diabetes should be individ- to manage his or her diabetes on the job
its whether or not related to diabetes. ually considered for employment based and avoid severe hypoglycemia.
Only medical information relevant to on the requirements of the specific job
evaluating an individual’s current capac- and the individual’s medical condition, Hypoglycemia
ity for safe performance of the particular treatment regimen, and medical his- Hypoglycemia is defined as a blood glu-
job at issue should be collected. For ex- tory. (E) cose level ⬍70 mg/dl (4,6). It is a poten-
ample, in some circumstances a review of ● When questions arise about the medi- tial side effect of some diabetes
an individual’s hypoglycemia history may cal fitness of a person with diabetes for treatments, including insulin and sulfo-
be relevant to the evaluation and should a particular job, a health care profes- nlyureas. It can usually be effectively self-
be collected. sional with expertise in treating diabe- treated by ingestion of glucose
Information about the individual’s di- tes should perform an individualized (carbohydrate) and is not often associated
abetes management (such as the current assessment; input from the treating with loss of consciousness or a seizure.
treatment regimen, medications, and physician should always be included. Severe hypoglycemia, requiring the assis-
blood glucose logs), job duties, and work (E) tance of another person, is a medical
environment are all relevant factors to be ● Employment evaluations should be emergency. Symptoms of severe hypogly-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S83
Diabetes and Employment
cemia may include confusion or, rarely, thy), eyes (retinopathy), kidneys (ne- careful changes to their diabetes manage-
seizure or loss of consciousness (6). Most phropathy), or heart, not all individuals ment regimen (for example, more fre-
individuals with diabetes never experi- with diabetes develop these long-term quent blood glucose testing or frequent
ence an episode of severe hypoglycemia complications. Such complications be- meals).
because either they are not on medication come relevant in employment decisions Presence of diabetes-related complica-
that causes it or they recognize the early only when they are established and inter- tions. Chronic complications that may
warning signs and can quickly self-treat fere with the performance of the actual result from long-term diabetes involve the
the problem by drinking or eating. Also, job being considered. Evaluations should blood vessels and nerves. These compli-
with self-monitoring of blood glucose lev- not be based on speculation as to what cations may involve nerve (neuropathy),
els, most people with diabetes can man- might occur in the future. Job evaluations eye (retinopathy), kidney (nephropathy),
age their condition in such a manner that should take high blood glucose levels into and heart disease. In turn, these problems
there is minimal risk of incapacitation account only if they have already caused can lead to amputation, blindness or
from hypoglycemia because mildly low long-term complications such as visual other vision problems, including vision
glucose levels can be easily detected and impairment that interfere with perfor- loss, kidney failure, stroke, or heart at-
treated (4,7). mance of the specific job. tack. As these complications could poten-
A single episode of severe hypoglyce- tially affect job performance and safety,
mia should not per se disqualify an indi- Aspects of a safety assessment such complications should be evaluated
vidual from employment. Rather, an When an individual with diabetes is as- by a specialist in the specific area related
appropriate evaluation should be under- sessed for safety risk there are several as- to the complication. If complications are
taken by a health care professional with pects that must be considered. not present, their possible future develop-
expertise in diabetes to determine the Blood glucose test results. A single ment should not be addressed, both be-
cause of the low blood glucose, the cir- blood glucose test result only gives infor- cause of laws prohibiting such
cumstances of the episode, whether it was mation about an individual’s blood glu- consideration and because with medical
an isolated incident, whether adjustment cose level at one particular point in time. monitoring and therapies, long-term
to the insulin regimen may mitigate this Because blood glucose levels fluctuate complications can now often be avoided
risk, and the likelihood of such an episode throughout the day (this is also true for or delayed. Thus, many people with dia-
happening again. Some episodes of severe people without diabetes), one test result is betes never develop any of these compli-
hypoglycemia can be explained and cor- of no use in assessing the overall health of cations, and those that do generally
rected with the assistance of a diabetes a person with diabetes. The results of a develop them over a period of years.
health care professional. series of self-monitored blood glucose
However, recurrent episodes of se- measurements over a period of time, how- Inappropriate assessments
vere hypoglycemia may indicate that an ever, can give valuable information about The following tools and terms do not ac-
individual may in fact not be able to safely an individual’s diabetes health. Blood glu- curately reflect the current state of diabe-
perform a job, particularly jobs or tasks cose records should be assessed by a tes treatment and should be avoided in an
involving significant risk of harm to em- health care professional with expertise in assessment of whether an individual with
ployees or the public, especially when diabetes (7). diabetes is able to safely and effectively
these episodes cannot be explained. The History of severe hypoglycemia. Of- perform a particular job.
person’s medical history and details of ten, a key factor in assessing employment Urine glucose tests. Urine glucose re-
any history of severe hypoglycemia safety and risk is documentation of inci- sults are no longer considered to be an
should be examined closely to determine dents of severe hypoglycemia. An individ- appropriate and accurate methodology
whether it is likely that such episodes will ual who has managed his or her diabetes for assessing diabetes control (8). Before
recur on the job. In all cases, job duties over an extended period of time without the mid-1970s, urine glucose tests were
should be carefully examined to deter- experiencing severe hypoglycemia is un- the best available method of monitoring
mine whether there are ways to minimize likely to experience this condition in the blood glucose levels. However, the urine
the risk of severe hypoglycemia (such as future. Conversely, multiple incidents of test is not a reliable or accurate indicator
adjustment of the insulin regimen or pro- severe hypoglycemia may in some situa- of blood glucose levels and is a poor mea-
viding additional breaks to check blood tions be disqualifying for high-risk occu- sure of the individual’s current health sta-
glucose levels). pations. However, the circumstances of tus. Blood glucose monitoring is a more
each incident should be examined, as accurate and timely means to measure
Hyperglycemia some incidents can be explained due to glycemic control. Urine glucose tests
In contrast to hypoglycemia, high blood changes in insulin dosage, illness, or other should never be used to evaluate the em-
glucose levels (hyperglycemia) can cause factors and thus will be unlikely to recur ployability of a person with diabetes.
long-term complications over years or de- or have already been addressed by the in- A1C and estimated average glucose
cades but does not normally lead to any dividual through changes to his or her di- (eAG). Hemoglobin A1C (A1C) test re-
adverse effect on job performance. The abetes treatment regimen or education. sults reflect average glycemia over several
symptoms of hyperglycemia generally de- Hypoglycemia unawareness. Some in- months and correlate with mean plasma
velop over hours or days and do not occur dividuals over time lose the ability to rec- glucose levels (4). An eAG is directly re-
suddenly. Therefore, hyperglycemia does ognize the early warning signs of lated to A1C and also provides an individ-
not pose an immediate risk of sudden in- hypoglycemia. These individuals are at ual with an estimate of average blood
capacitation. While over years or decades, increased risk for a sudden episode of se- glucose over a period of time, but it uses
high blood glucose may cause long-term vere hypoglycemia. Some of these indi- the same values and units that are ob-
complications to the nerves (neuropa- viduals may be able to lessen this risk with served when using a glucose meter or re-
S84 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Position Statement
cording a fasting glucose value on a lab are relevant in employment decisions care tasks that should be provided when-
report (5). A1C/eAG values provide only when they are established and in- ever feasible.
health care providers with important in- terfere with the performance of the ac- Administering insulin. Employees may
formation about the effectiveness of an in- tual job being considered. (E) need short breaks during the workday to
dividual’s treatment regimen (4) but are ● Proper safety assessments should in- administer insulin when it is needed. In-
often misused in assessing whether an in- clude review of blood glucose test re- sulin can be safely administered wherever
dividual can safely perform a job. Because sults, history of severe hypoglycemia, the employee happens to be. The em-
they identify only averages and not presence of hypoglycemia unaware- ployee may also need a place to store in-
whether the person had severe extreme ness, and presence of diabetes-related sulin and other supplies if work
blood glucose readings, A1C/eAG results complications and should not include conditions (such as extreme tempera-
are of no value in predicting short-term urine glucose or AIC/eAG tests or be tures) prevent the supplies from being
complications of diabetes and thus have based on a general assessment of level carried on the person (10).
no use in evaluating individuals in em- of control. (E) Food and drink. Employees may need
ployment situations. access to food and/or beverages during
The American Diabetes Association III. ACCOMMODATING the workday. This is particularly impor-
recommends that in most patients A1C EMPLOYEES WITH tant in the event that the employee needs
levels be kept below 7% (4), or eAG below DIABETES — Individuals with diabe- to quickly respond to low blood glucose
154 mg/dl. This recommendation sets a tes may need certain changes or accom- levels or maintain hydration if glucose
target in order to lessen the chances of modations on the job in order to perform levels are high. Employees should be per-
long-term complications of high blood their work responsibilities effectively and mitted to consume food or beverages as
glucose levels but does not provide useful safely. Federal and state laws require the needed at their desk or work station (ex-
information on whether the individual is provision of “reasonable accommoda- cept in an extremely rare situation in
at significant risk for hypoglycemia or tions” to help an employee with diabetes which this would pose a hazard and cre-
suboptimal job performance and is not a to perform the essential functions of the ate a safety issue, and if this is the case, an
measure of “compliance” with therapy. job (3). Additional laws provide for leave alternative site should be provided).
An A1C or eAG cut off score is not med- for an employee to deal with his or her Leave. Employees may need leave or a
ically justified in employment evaluations medical needs or those of a family mem- flexible work schedule to accommodate
and should never be a determinative fac- ber (9). Although there are some typical medical appointments or other diabetes
tor in employment. accommodations that many people with care needs. Occasionally, employees may
“Uncontrolled” or “brittle” diabetes. diabetes use, the need for accommoda- need to miss work due to unanticipated
Sometimes an individual’s diabetes is de- tions must be assessed on an individual- events (severe hypoglycemic episode) or
scribed as “uncontrolled,” “poorly con- ized basis (2). illness.
trolled,” or “brittle.” These terms are not Work schedules. Certain types of work
well defined and are not relevant to job Accommodating daily diabetes schedules, such as rotating or split shifts,
evaluations. As such, giving an opinion management needs can make it especially difficult for some
on the level of “control” an individual has Many of the accommodations that em- individuals to manage diabetes
over diabetes is not the same as assessing ployees with diabetes need on a day-to- effectively.
whether that individual is qualified to day basis are those that allow them to
perform a particular job and can do so manage their diabetes in the workplace as Accommodating complications of
safely. Such an individual assessment is they would elsewhere. They are usually diabetes
the only relevant evaluation. simple accommodations, can be provided In addition to accommodating the day-to-
without any cost to the employer, and day management of diabetes in the work-
Recommendations should cause little or no disruption in the place, for some individuals it is also
● Evaluating the safety risk of employees workplace. Most employers are required necessary to seek modifications for long-
with diabetes includes determining to provide accommodations unless those term diabetes-related complications.
whether the concerns are reasonable in accommodations would create an undue Such people can remain productive em-
light of the job duties the individual burden (3). Some accommodations that ployees if appropriate accommodations
must perform. (E) may be needed include the following. are implemented.
● Most people with diabetes can manage Testing blood glucose. Breaks may be For example, an employee with dia-
their condition in such a manner that needed to allow an individual to test betic retinopathy or other vision impair-
there is no or minimal risk of incapaci- blood glucose levels when needed. Such ments may benefit from using a big screen
tation from hypoglycemia at work. A checks only take minutes to complete. computer or other visual aids, while an
single episode of severe hypoglycemia Some individuals use continuous glucose employee with nerve pain may benefit
should not per se disqualify an individ- monitors but will still need an opportu- from reduced walking distances or having
ual from employment, but an individ- nity to check blood glucose with a meter. the ability to sit down on the job. Individ-
ual with recurrent episodes of severe Blood glucose can be checked wherever uals with kidney problems may need to
hypoglycemia may be unable to safely the employee is without putting other have flexibility to take time off work for
perform certain jobs, especially when employees at risk, and employers should dialysis treatment.
those episodes cannot be explained. (E) not limit where employees with diabetes It is impossible to provide an exhaus-
● Hyperglycemia does not pose an imme- are permitted to manage their diabetes. tive list of potential accommodations. The
diate risk of sudden incapacitation on Some employees may prefer to have a pri- key message in accommodating an em-
the job, and long-term complications vate location for testing or other diabetes ployee with diabetes is to ensure that ac-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S85
Diabetes and Employment
commodations are tailored to the jobs. The therapies for, and effects of, di- 2. Equal Employment Opportunity Com-
individual and effective in helping the in- abetes vary greatly from person to person, mission, “Questions and Answers About
dividual perform his or her job. Input so employers must consider each person’s Diabetes in the Workplace and the Amer-
from health care professionals who spe- capacities and needs on an individual ba- icans with Disabilities Act (ADA)” Oct.
cialize in the particular complication, or sis. People with diabetes should always be 29, 2003. Available from http://www
from vocational rehabilitation specialists evaluated individually with the assistance .eeoc.gov/facts/diabetes.html. Accessed
26 May 2008
or organizations, may help identify ap- of experienced diabetes health care pro-
3. Americans with Disabilities Act of 1990,
propriate accommodations. fessionals. The requirements of the spe- 42 U.S.C. §12101 et seq.
cific job and the individual’s ability to 4. American Diabetes Association: Stan-
perform that job, with or without reason- dards of Medical Care in Diabetes—2010
Recommendations able accommodations, always need to be
● Individuals with diabetes may need ac- (Position Statement). Diabetes Care 33
considered. (Suppl. 1):S11–S61, 2010
commodations on the job in order to
5. Nathan DM, Kuenen J, Borg R, Zheng H,
perform their work responsibilities ef- Schoenfeld D, Heine R: Translating the A1C
fectively and safely; these include ac- Acknowledgments — The American Diabe- assay into estimated average glucose values.
commodating daily diabetes needs and, tes Assocation thanks the members of the Diabetes Care 31:1473–1478, 2008
when present, the complications of di- volunteer writing group for this updated state- 6. American Diabetes Association: Defining
abetes. All such accommodations must ment: John E. Anderson, MD; Michael A.
and reporting hypoglycemia in diabetes, a
be tailored to the individual and effec- Greene, JD; John W. Griffin, Jr., JD; Daniel B.
report from the American Diabetes Asso-
Kohrman, JD; Daniel Lorber, MD, FACP,
tive in helping the individual perform ciation Workgroup on Hypoglycemia. Di-
CDE; Christopher D. Sandek, MD; Desmond
his or her job. (E) Shatz, MD; and Linda Siminerio, RN, PhD, abetes Care 28:1245–1249, 2005
CDE. 7. American Diabetes Association: Self-moni-
toring of blood glucose (Consensus State-
CONCLUSION — Individuals with
ment). Diabetes Care 17:81– 86, 1994
diabetes can and do serve as highly pro- 8. American Diabetes Association: Tests of gly-
ductive members of the workforce. While References
1. Centers for Disease Control and Preven- cemia in diabetes (Position Statement). Di-
not every individual with diabetes will be tion: National Diabetes Fact Sheet: General abetes Care 27 (Suppl. 1):S91–S93, 2004
qualified for, nor can perform, every Information and National Estimates on Dia- 9. Family Medical Leave Act of 1993, 29
available job, reasonable accommoda- betes in the U.S., 2007. Atlanta, GA, U.S. U.S.C. §2601 et seq.
tions can readily be made that allow the Department of Health and Human Ser- 10. American Diabetes Association: Insulin ad-
vast majority of people with diabetes to vices, Centers for Disease Control and ministration (Position Statement). Diabetes
effectively perform the vast majority of Prevention, 2008 Care 27 (Suppl. 1):S106 –S109, 2004
S86 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
P O S I T I O N S T A T E M E N T
Third-Party Reimbursement for Diabetes
Care, Self-Management Education,
and Supplies
AMERICAN DIABETES ASSOCIATION health care costs, individuals with diabe-
tes must have access to the integral com-
ponents of diabetes care, such as health
care visits, diabetes supplies, self-
D
iabetes is a chronic disease that af- outlines appropriate medical care for peo-
fects ⬎20 million Americans (1) ple with diabetes (5). management education, and diabetes
and is characterized by serious, An integral component of diabetes medications. As such, insurers must reim-
costly, and often fatal complications. The care is self-management education (inpa- burse for diabetes-related medical treat-
total cost of diagnosed diabetes in the U.S. tient and/or outpatient) delivered by an ment as well as for self-management
in 2007 was estimated to be $174 billion interdisciplinary team. Self-management education programs that have met ac-
(2). To prevent or delay costly diabetes training helps people with diabetes adjust cepted standards, such as the American
complications and to enable people with their daily regimen to improve glycemic Diabetes Association’s National Standards
diabetes to lead healthy, productive lives, control. Diabetes self-management edu- for Diabetes Self-Management Education.
appropriate medical care based on current cation teaches individuals with diabetes Furthermore, third-party payers must
standards of practice, self-management to assess the interplay among medical nu- also reimburse for medications and sup-
education, and medication and supplies trition therapy, physical activity, emo- plies related to the daily care of diabetes.
must be available to everyone with diabe- tional/physical stress, and medications, These same standards should also apply
tes. This paper is based on technical re- and then to respond appropriately and to organizations that purchase health care
views titled “Diabetes Self-Management continually to those factors to achieve and benefits for their members or employees,
Education” (3) and “National Standards maintain optimal glucose control. as well as managed care organizations that
for Diabetes Self-Management Education Today, self-management education is provide services to participants.
Programs” (4). understood to be such a critical part of It is recognized that the use of formu-
The goal of medical care for people diabetes care that medical treatment of laries, prior authorization, competitive
with diabetes is to optimize glycemic con- diabetes without systematic self-manage- bidding, and related provisions (hereafter
trol and minimize complications. The Di- ment education is regarded as inadequate. referred to as “controls”) can manage pro-
abetes Control and Complications Trial The “National Standards for Diabetes Self- vider practices and costs to the potential
(DCCT) demonstrated that treatment that Management Education” establish spe- benefit of payors and patients. Social Se-
maintains blood glucose levels near nor- cific criteria against which diabetes curity Act Title XIX, section 1927, states
mal in type 1 diabetes delays the onset education programs can be measured, that excluded medications should not
and reduces the progression of microvas- and a quality assurance program has been have “a significant clinically meaningful
cular complications. The U.K. Prospective developed and subsequently revised (6). therapeutic advantage in terms of safety,
Diabetes Study (UKPDS) documented Treatments and therapies that im- effectiveness or clinical outcomes of such
that optimal glycemic control can also prove glycemic control and reduce the treatment of such population.” A variety
benefit most individuals with type 2 dia- complications of diabetes will also signif- of laws, regulations, and executive orders
betes. To achieve optimal glucose control, icantly reduce health care costs (7,8). Nu- also provide guidance on the use of such
the person with diabetes must be able to merous studies have demonstrated that controls to oversee the purchase and use
access health care providers who have ex- self-management education leads to re- of durable medical equipment (hereafter
pertise in the field of diabetes. Treatment ductions in the costs associated with all referred to as “equipment”) and single-
plans must also include self-management types of diabetes. Participants in self- use medical supplies (hereafter referred to
training and tools, regular and timely lab- management education programs have as “supplies”) associated with the man-
oratory evaluations, medical nutrition been found to have decreased lower- agement of diabetes.
therapy, appropriately prescribed medi- extremity amputation rates, reduced Certain principles should guide the
cation(s), and regular self-monitoring of medication costs, and fewer emergency creation and enforcement of controls in
blood glucose levels. The American Dia- room visits and hospitalizations. order to insure that they meet the com-
betes Association position statement To achieve optimal glycemic control, prehensive medical needs of people living
“Standards of Medical Care in Diabetes” thus achieving long-term reduction in with diabetes. A wide array of medica-
tions and supplies are correlated with
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● improved glycemic outcomes and a re-
The recommendations in this paper are based on the evidence reviewed in the following publications: duction in the risk of diabetes-related
Diabetes self-management education (Technical Review). Diabetes Care 18:1204 –1214, 1995; and Na- complications. Because no single diabe-
tional standards for diabetes self-management education. Diabetes Care 33:S89 –S96, 2010. tes treatment regimen is appropriate for
Approved 1995. Revised 2008. all people with diabetes, providers and
DOI: 10.2337/dc10-S087
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly
patients should have access to a broad
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. array of medications and supplies to de-
org/licenses/by-nc-nd/3.0/ for details. velop an effective treatment modality.
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S87
Third-party reimbursement
However, the Association also recog- patients with diabetes. Protections should
References
nizes that there may be a number of ensure that patients with diabetes can 1. Centers for Disease Control and Preven-
medications and/or supplies within any readily comply with therapy in the widely tion. National Diabetes Fact Sheet, United
given class. As such, any controls variable circumstances encountered in States, 2005. Atlanta, GA, U.S. Depart-
should ensure that all classes of anti- daily life. These protections should guar- ment of Health and Human Services, Cen-
diabetic agents with unique mecha- antee access to an acceptable range and all ters for Disease Control and Prevention,
nisms of action are available to facilitate classes of antidiabetic medications, equip- 2005
achieving glycemic goals to reduce the ment, and supplies. Furthermore, fair and 2. American Diabetes Association: Eco-
risk of complications. Similar issues oper- nomic costs of diabetes in the U.S. in
reasonable appeals processes should 2007. Diabetes Care 31:596 – 615, 2008
ate in the management of lipid disorders, ensure that diabetic patients and their 3. Clement S: Diabetes self-management ed-
hypertension, and other cardiovascular medical care practitioners can obtain ucation (Technical Review). Diabetes Care
risk factors, as well as for other diabetes medications, equipment, and supplies that 18:1204 –1214, 1995
complications. Furthermore, any controls are not contained within existent controls. 4. Funnell MM, Haas LB: National standards
should ensure that all classes of equip- Diabetes management needs individ- for diabetes self-management education
ment and supplies designed for use with ualization in order for patients to reach programs (Technical Review). Diabetes
such equipment are available to facilitate glycemic targets. Because there is diver- Care 18:100 –116, 1995
achieving glycemic goals to reduce the 5. American Diabetes Association: Stan-
sity in the manifestations of the disease dards of medical care in diabetes—2009
risk of complications. It is important to
and in the impact of other medical condi- (Position Statement). Diabetes Care 32
note that medical advances are rapidly
tions upon diabetes, it is common that (Suppl. 1):S13–S61, 2009
changing the landscape of diabetes
medications and supplies. To ensure practitioners will need to uniquely tailor 6. American Diabetes Association: National
treatment for their patients. To reach dia- standards for diabetes self-management
that patients with diabetes have access education (Standards and Review Crite-
to beneficial updates in treatment mo- betes treatment goals, practitioners
should have access to all classes of antidi- ria). Diabetes Care 31 (Suppl. 1):S97–
dalities, systems of controls must em- S104, 2008
ploy efficient mechanisms through abetic medications, equipment, and sup- 7. Herman WH, Dasbach DJ, Songer TJ,
which to introduce and approve new plies without undue controls. Without Thompson DE, Crofford OB: Assessing
products. appropriate safeguards, these controls the impact of intensive insulin therapy on
Though it can seem appropriate for could constitute an obstruction of effec- the health care system. Diabetes Rev
controls to restrict certain items in chronic tive care. 2:384 –388, 1994
disease management, particularly with a The value of self-management edu- 8. Wagner EH, Sandu N, Newton KM, Mc-
cation and provision of diabetes sup- Cullock DK, Ramsey SD, Grothaus LC:
complex disorder such as diabetes, it
Effects of improved glycemic control on
should be recognized that adherence is a plies has been acknowledged by the
health care costs and utilization. JAMA
major barrier to achieving targets. Any passage of the Balanced Budget Act of 285:182–189, 2001
controls should take into account the 1997 (9) and by stated medical policy 9. Balanced Budget Act of 1997. U.S. Govt.
huge mental and physical burden that in- on both diabetes education and medical Printing Office, 1997, p. 115–116 (publ.
tensive disease management exerts upon nutrition therapy. no. 869-033-00034-1)
S88 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
S T A N D A R D S A N D R E V I E W C R I T E R I A
National Standards for Diabetes Self-
Management Education
MARTHA M. FUNNELL, MS, RN, CDE1 MARK PEYROT, PHD8 1. Diabetes education is effective for im-
TAMMY L. BROWN, MPH, RD, BC-ADM, CDE2 JOHN D. PIETTE, PHD9,10 proving clinical outcomes and quality
BELINDA P. CHILDS, ARNP, MN, CDE, BC-ADM3 DIANE READER, RD, CDE11 of life, at least in the short-term (1–7).
LINDA B. HAAS, PHC, CDE, RN4 LINDA M. SIMINERIO, PHD, RN, CDE12 2. DSME has evolved from primarily di-
GWEN M. HOSEY, MS, ARNP, CDE5 KATIE WEINGER, EDD, RN7 dactic presentations to more theoreti-
BRIAN JENSEN, RPH6 MICHAEL A. WEISS, JD13
MELINDA MARYNIUK, MED, RD, CDE7 cally based empowerment models
(3,8).
3. There is no one “best” education pro-
gram or approach; however, programs
D
iabetes self-management education their appropriateness, relevance, and sci- incorporating behavioral and psycho-
(DSME) is a critical element of care entific basis. The Standards were then re- social strategies demonstrate im-
for all people with diabetes and is viewed and revised based on the available proved outcomes (9 –11). Additional
necessary in order to improve patient out- evidence and expert consensus. The com- studies show that culturally and age-
comes. The National Standards for DSME mittee convened on 31 March 2006 and 9 appropriate programs improve out-
are designed to define quality diabetes September 2006, and the Standards were comes (12–16) and that group
self-management education and to assist approved 25 March 2007. education is effective (4,6,7,17,18).
diabetes educators in a variety of settings
4. Ongoing support is critical to sustain
to provide evidence-based education. Be- DEFINITION AND
progress made by participants during
cause of the dynamic nature of health care OBJECTIVES — Diabetes self-man-
the DSME program (3,13,19,20).
and diabetes-related research, these Stan- agement education (DSME) is the ongo-
dards are reviewed and revised approxi- ing process of facilitating the knowledge, 5. Behavioral goal-setting is an effective
mately every 5 years by key organizations skill, and ability necessary for diabetes strategy to support self-management
and federal agencies within the diabetes self-care. This process incorporates the behaviors (21).
education community. needs, goals, and life experiences of the
A Task Force was jointly convened by person with diabetes and is guided by ev- STANDARDS
the American Association of Diabetes Edu- idence-based standards. The overall ob-
cators and the American Diabetes Associa- jectives of DSME are to support informed Structure
tion in the summer of 2006. Additional decision-making, self-care behaviors, Standard 1. The DSME entity will have
organizations that were represented in- problem-solving and active collaboration documentation of its organizational struc-
cluded the American Dietetic Association, with the health care team and to improve ture, mission statement, and goals and will
the Veteran’s Health Administration, the clinical outcomes, health status, and qual- recognize and support quality DSME as an
Centers for Disease Control and Prevention, ity of life. integral component of diabetes care.
the Indian Health Service, and the Ameri- Documentation of the DSME organi-
can Pharmaceutical Association. Members GUIDING PRINCIPLES — Before zational structure, mission statement, and
of the Task Force included a person with the review of the individual Standards, goals can lead to efficient and effective
diabetes; several health services researchers/ the Task Force identified overriding prin- provision of services. In the business lit-
behaviorists, registered nurses, and regis- ciples based on existing evidence that erature, case studies and case report in-
tered dietitians; and a pharmacist. would be used to guide the review and vestigations on successful management
The Task Force was charged with re- revision of the DSME Standards. These strategies emphasize the importance of
viewing the current DSME standards for are: clear goals and objectives, defined rela-
tionships and roles, and managerial sup-
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● port (22–25). While this concept is
The previous version of the “National Standards for Diabetes Self-Management Education” was originally relatively new in health care, business and
published in Diabetes Care 23:682– 689, 2000. This version received final approval in March 2007. health policy experts and organizations
From the 1Department of Medical Education, Diabetes Research and Training Center, University of Michi- have begun to emphasize written com-
gan, Ann Arbor, Michigan; 2Indian Health Service, Albuquerque, New Mexico; 3MidAmerica Diabetes
Associates, Wichita, Kansas; the 4VA Puget Sound Health Care System, Seattle, Washington; the 5Division mitments, policies, support, and the im-
of Diabetes Translation, National Center for Chronic Diseases Prevention and Health Promotion, Centers portance of outcome variables in quality
for Disease Control and Prevention, Atlanta, Georgia; 6Lakeshore Apothacare, Two Rivers, Wisconsin; the improvement efforts (22,26 –37). The
7
Joslin Diabetes Center, Harvard Medical School, Boston, Massachusetts; 8Loyola College, Baltimore, continuous quality improvement litera-
Maryland; the 9VA Ann Arbor Health Care System, Ann Arbor, Michigan; the 10Department of Internal
Medicine, Diabetes Research and Training Center, University of Michigan, Ann Arbor, Michigan; the
ture also stresses the importance of devel-
11
International Diabetes Center, Minneapolis, Minnesota; the 12Diabetes Institute, University of Pitts- oping policies, procedures, and
burgh Medical Center, Pittsburgh, Pennsylvania; and 13Patient Centered Solutions, Pittsburgh, Pennsyl- guidelines (22,26).
vania. Documentation of the organizational
Corresponding author: Martha M. Funnell, mfunnell@umich.edu. structure, mission statement, and goals
DOI: 10.2337/dc10-S089
© 2010 by the American Diabetes Association. Readers may use this article as long as the work is properly can lead to efficient and effective provi-
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons. sion of DSME. Documentation of an orga-
org/licenses/by-nc-nd/3.0/ for details. nizational structure that delineates
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S89
Standards and Review Criteria
channels of communication and repre- viduals with diabetes do not receive any titian, and the registered pharmacist as
sents institutional commitment to the ed- formal diabetes education (56,57). Thus, the key primary instructors for diabetes
ucational entity is critical for success (38 – identification of access issues is an essen- education and members of the multidis-
42). According to the Joint Commission tial part of the assessment process (58). ciplinary team responsible for designing
on Accreditation of Health Care Organi- Demographic variables, such as ethnic the curriculum and assisting in the deliv-
zations (JCAHO) (26), this type of docu- background, age, formal educational ery of DSME (1–7,77). In addition to reg-
mentation is equally important for small level, reading ability, and barriers to par- istered nurses, registered dietitians, and
and large health care organizations. ticipation in education, must also be con- pharmacists, a number of studies reflect
Health care and business experts over- sidered to maximize the effectiveness of the ever-changing and evolving health
whelmingly agree that documentation of DSME for the target population (13– care environment and include other
the process of providing services is a crit- 19,43– 47,59 – 61). health professionals (e.g., a physician, be-
ical factor in clear communication and Standard 4. A coordinator will be desig- haviorist, exercise physiologist, ophthal-
provides a solid basis from which to de- nated to oversee the planning, implementa- mologist, optometrist, podiatrist)
liver quality diabetes education (22,26, tion, and evaluation of diabetes self- (48,80 – 84) and, more recently, lay
33,35–37). In 2005, JACHO published management education. The coordinator will health and community workers (85–91)
the Joint Commission International Stan- have academic or experiential preparation in and peers (92) to provide information,
dards for Disease or Condition-Specific chronic disease care and education and in behavioral support, and links with the
Care, which outlines national standards program management. health care system as part of DSME.
and performance measurements for dia- The role of the coordinator is essential Expert consensus supports the need
betes and addresses diabetes self- to ensure that quality diabetes education for specialized diabetes and educational
management education as one of seven is delivered through a coordinated and training beyond academic preparation for
critical elements (26). systematic process. As new and creative the primary instructors on the diabetes
Standard 2. The DSME entity shall appoint methods to deliver education are ex- team (64,93–97). Certification as a diabe-
an advisory group to promote quality. This plored, the coordinator plays a pivotal tes educator by the National Certification
group shall include representatives from the role in ensuring accountability and conti- Board for Diabetes Educators (NCBDE) is
health professions, people with diabetes, the nuity of the educational process (23,60 – one way a health professional can demon-
community, and other stakeholders. 62). The individual serving as the strate mastery of a specific body of knowl-
Established and new systems (e.g., coordinator will be most effective if there edge, and this certification has become an
committees, governing bodies, advisory is familiarity with the lifelong process of accepted credential in the diabetes com-
groups) provide a forum and a mecha- managing a chronic disease (e.g., diabe- munity (98). An additional credential that
nism for activities that serve to guide and tes) and with program management. indicates specialized training beyond ba-
sustain the DSME entity (30,39 – 41). sic preparation is board certification in
Broad participation of organization(s) Process advanced Diabetes Management (BC-
and community stakeholders, including Standard 5. DSME will be provided by one ADM) offered by the American Nurses
health professionals, people with diabe- or more instructors. The instructors will have Credentialing Center (ANCC), which is
tes, consumers, and other community in- recent educational and experiential prepara- available for master’s prepared nurses, di-
terest groups, at the earliest possible tion in education and diabetes management etitians, and pharmacists (48,84,99).
moment in the development, ongoing or will be a certified diabetes educator. The DSME has been shown to be most ef-
planning, and outcomes evaluation pro- instructor(s) will obtain regular continuing fective when delivered by a multidisci-
cess (22,26,33,35,36,41) can increase education in the field of diabetes manage- plinary team with a comprehensive plan
knowledge and skills about the local com- ment and education. At least one of the in- of care (7,31,52,100 –102). Within the
munity and enhance collaborations and structors will be a registered nurse, dietitian, multidisciplinary team, team members
joint decision-making. The result is a or pharmacist. A mechanism must be in place work interdependently, consult with one
DSME program that is patient-centered, to ensure that the participant’s needs are met another, and have shared objectives
more responsive to consumer-identified if those needs are outside the instructors’ (7,103,104). The team should have a col-
needs and the needs to the community, scope of practice and expertise. lective combination of expertise in the
more culturally relevant, and of greater Diabetes education has traditionally clinical care of diabetes, medical nutrition
personal interest to consumers (43–50). been provided by nurses and dietitians. therapy, educational methodologies,
Standard 3. The DSME entity will deter- Nurses have been utilized most often as teaching strategies, and the psychosocial
mine the diabetes educational needs of the instructors in the delivery of formal and behavioral aspects of diabetes self-
target population(s) and identify resources DSME (2,3,5,63– 67). With the emer- management. A referral mechanism
necessary to meet these needs. gence of medical nutrition therapy (66 – should be in place to ensure that the in-
Clarifying the target population and 70), registered dietitians became an dividual with diabetes receives education
determining its self-management educa- integral part of the diabetes education from those with appropriate training and
tional needs serve to focus resources and team. In more recent years, the role of the credentials. It is essential in this collabo-
maximize health benefits (51–53). The diabetes educator has expanded to other rative and integrated team approach that
assessment process should identify the disciplines, particularly pharmacists (73– individuals with diabetes are viewed as
educational needs of all individuals with 79). Reviews comparing the effectiveness leaders of their team and assume an active
diabetes, not just those who frequently of different disciplines for education re- role in designing their educational expe-
attend clinical appointments (51). DSME port mixed results (3,5,6). Generally, the rience (7,20,31,100 –102,104).
is a critical component of diabetes treat- literature favors current practice that uti- Standard 6. A written curriculum reflecting
ment (2,54,55), yet the majority of indi- lizes the registered nurse, registered die- current evidence and practice guidelines, with
S90 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Standards and Review Criteria
criteria for evaluating outcomes, will serve as have been shown to be effective calls), may augment face-to-face assess-
the framework for the DSME entity. Assessed (83,119,121,122,125–127). ments (97,99).
needs of the individual with pre-diabetes and These content areas are presented in While there is little direct evidence on
diabetes will determine which of the content ar- behavioral terms and thereby exemplify the impact of documentation on patient
eas listed below are to be provided: the importance of action-oriented, behav- outcomes, it is required to receive pay-
ioral goals and objectives (13,21,55,121– ment for services. In addition, documen-
● Describing the diabetes disease process 123,128,129). Creative, patient-centered tation of patient encounters guides the
and treatment options experience-based delivery methods are educational process, provides evidence of
● Incorporating nutritional management effective for supporting informed deci- communication among instructional
into lifestyle sion-making and behavior change and go staff, may prevent duplication of services,
● Incorporating physical activity into life- beyond the acquisition of knowledge. and provides information on adherence
style Standard 7. An individual assessment and to guidelines (37,64,100,131,153). Pro-
● Using medication(s) safely and for max- education plan will be developed collabora- viding information to other members of
imum therapeutic effectiveness tively by the participant and instructor(s) to the patient’s health care team through
● Monitoring blood glucose and other pa- direct the selection of appropriate educa- documentation of educational objectives
rameters and interpreting and using the tional interventions and self-management and personal behavioral goals increases
results for self-management decision support strategies. This assessment and edu- the likelihood that all of the members will
making cation plan and the intervention and out- address these issues with the patient
● Preventing, detecting, and treating comes will be documented in the education (37,98,153).
acute complications record. The use of evidence-based perfor-
● Preventing detecting, and treating Multiple studies indicate the impor- mance and outcome measures has been
chronic complications tance of individualizing education based adopted by organizations and initiatives
● Developing personal strategies to ad- on the assessment (1,56,68,131–135). such as the Centers for Medicare and Med-
dress psychosocial issues and concerns The assessment includes information icaid Services (CMS), the National Com-
● Developing personal strategies to pro- about the individual’s relevant medical mittee for Quality Assurance (NCQA), the
mote health and behavior change history, age, cultural influences, health Diabetes Quality Improvement Project
beliefs and attitudes, diabetes knowledge, (DQIP), the Health Plan Employer Data
self-management skills and behaviors, and Information Set (HEDIS), the Veter-
People with diabetes and their families ans Administration Health System, and
and caregivers have a great deal to learn in readiness to learn, health literacy level,
JCAHO (26,154).
order to become effective self-managers of physical limitations, family support, and
Research suggests that the development
their diabetes. A core group of topics are financial status (10 –17,19,131,136 –
of standardized procedures for documenta-
commonly part of the curriculum taught 138). The majority of these studies sup-
tion, training health professionals to docu-
in comprehensive programs that have port the importance of attitudes and
ment appropriately, and the use of
demonstrated successful outcomes health beliefs in diabetes care outcomes structured standardized forms based on
(1,2,3,6,105–109). The curriculum, a co- (1,68,134,135,138,139). current practice guidelines can improve
ordinated set of courses and educational In addition, functional health literacy documentation and may ultimately im-
experiences, includes learning outcomes (FHL) level can affect patients’ self- prove quality of care (100,153–155).
and effective teaching strategies (110 – management, communication with clini- Standard 8. A personalized follow-up plan
112). The curriculum is dynamic and cians, and diabetes outcomes (140,141). for ongoing self management support will be
needs to reflect current evidence and Simple tools exist for measuring FHL as developed collaboratively by the participant
practice guidelines (112–117). Current part of an overall assessment process and instructor(s). The patient’s outcomes and
educational research reflects the impor- (142–144). goals and the plan for ongoing self manage-
tance of emphasizing practical, problem- Many people with diabetes experi- ment support will be communicated to the
solving skills, collaborative care, ence problems due to medication costs, referring provider.
psychosocial issues, behavior change, and and asking patients about their ability to While DSME is necessary, it is not
strategies to sustain self-management ef- afford treatment is important (144). Co- sufficient for patients to sustain a lifetime
forts (31,39,42,48,98,118 –122). morbid chronic illness (e.g., depression of diabetes self-care (55). Initial improve-
The content areas delineated above and chronic pain) as well as more general ments in metabolic and other outcomes
provide instructors with an outline for de- psychosocial problems can pose signifi- diminish after ⬃6 months (3). To sustain
veloping this curriculum. It is important cant barriers to diabetes self-management behavior at the level of self-management
that the content be tailored to match each (104,146 –151); considering these issues needed to effectively manage diabetes,
individual’s needs and adapted as neces- in the assessment may lead to more effec- most patients need ongoing diabetes self-
sary for age, type of diabetes (including tive planning (149 –151). management support (DSMS).
pre-diabetes and pregnancy), cultural in- Periodic reassessment determines at- DSMS is defined as activities to assist
fluences, health literacy, and other co- tainment of the educational objectives or the individual with diabetes to implement
morbidities (123,124). The content areas the need for additional and creative inter- and sustain the ongoing behaviors needed
are designed to be applicable in all set- ventions and future reassessment to manage their illness. The type of sup-
tings and represent topics that can be de- (7,97,100,152). A variety of assessment port provided can include behavioral, ed-
veloped in basic, intermediate, and modalities, including telephone fol- ucational, psychosocial, or clinical
advanced levels. Approaches to education low-up and other information technolo- (13,121–123).
that are interactive and patient-centered gies (e.g., Web-based, automated phone A variety of strategies are available for
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S91
Standards and Review Criteria
providing DSMS both within and outside The AADE Outcome Standards for Di- MD, CDE, of the American Diabetes Associa-
the DSME entity. Some patients benefit abetes Education specify self-management tion; Lori Porter, MBA, RD, CAE, of the Amer-
from working with a nurse case manager behavior as the key outcome (112,160). ican Association of Diabetes Educators; and
(7,20,98,157). Case management for Knowledge is an outcome to the degree that Karmeen Kulkarni, MS, RD, BC-ADM, Past
President, Health Care and Education of the
DSMS can include reminders about it is actionable (i.e., knowledge that can be American Diabetes Association; Malinda
needed follow-up care and tests, medica- translated into self-management behavior). Peeples, MS, RN, CDE, Past President of the
tion management, education, behavioral In turn, effective self-management is one American Association of Diabetes Educators;
goal-setting, and psychosocial support/ (but not the only) contributor to longer- and Carole’ Mensing, RN, MA, CDE, for their
connection to community resources. term, higher-order outcomes such as clini- insights and helpful suggestions.
The effectiveness of providing DSMS cal status (e.g., control of glycemia, blood We also gratefully acknowledge the work of
through disease-management programs, pressure, and cholesterol), health status the previous Task Force for the National Stan-
trained peers and health community (e.g., avoidance of complications), and sub- dards for DSME: Carole’ Mensing, RN, MA,
workers, community-based programs, jective quality of life. Thus, patient self- CDE; Jackie Boucher, MS, RD, LD, CDE; Mar-
use of technology, ongoing education and management behaviors are at the core of the jorie Cypress, MS, C-ANP, CDE; Katie
Weinger, EdD, RN; Kathryn Mulcahy, MSN,
support groups, and medical nutrition outcomes evaluation. RN, CDE; Patricia Barta, RN, MPH, CDE;
therapy has also been established Standard 10. The DSME entity will mea- Gwen Hosey, MS, ARNP, CDE; Wendy Ko-
(7,13,89 –92,101,121–123,158 –159). sure the effectiveness of the education process pher, RN, C, CDE, HTP; Andrea Lasichak, MS,
While the primary responsibility for and determine opportunities for improve- RD, CDE; Betty Lamb, RN, MSN; Mavourneen
diabetes education belongs to the DSME ment using a written continuous quality im- Mangan, RN, MS, ANP, C, CDE; Jan Norman,
entity, patients benefit by receiving rein- provement plan that describes and RD, CDE; Jon Tanja, BS, MS, RPH; Linda
forcement of content and behavioral goals documents a systematic review of the entities’ Yauk, MS, RD, LD, CDE; Kimberlydawn Wis-
from their entire health care team (100). process and outcome data. dom, MD, MS; and Cynthia Adams, PhD
Additionally, many patients receive Diabetes education must be respon-
DSMS through their provider. Thus, com- sive to advances in knowledge, treatment
munication is essential to ensure that pa- strategies, educational strategies, psycho- References
tients receive the support they need. social interventions, and the changing 1. Brown SA: Interventions to promote di-
abetes self-management: state of the sci-
health care environment. Continuous ence. Diabetes Educ 25 (6 Suppl.):52–
Outcomes quality improvement (CQI) is an iterative, 61, 1999
Standard 9. The DSME entity will measure planned process (161) that leads to im- 2. Norris SL, Engelgau MM, Naranyan
attainment of patient-defined goals and pa- provement in the delivery of patient edu- KMV: Effectiveness of self-management
tient outcomes at regular intervals using ap- cation (162). The CQI plan should define training in type 2 diabetes: a systematic
propriate measurement techniques to quality based on and consistent with the review of randomized controlled trials.
evaluate the effectiveness of the educational organization’s mission, vision, and strate- Diabetes Care 24:561–587, 2001
intervention. gic plan and include identifying and pri- 3. Norris SL, Lau J, Smith SJ, Schmid CH,
In addition to program-defined goals oritizing improvement opportunities Engelgau MM: Self-management educa-
and objectives (e.g., learning goals, meta- (163). Once improvement projects are tion for adults with type 2 diabetes: a
meta-analysis on the effect on glycemic
bolic, and other health outcomes), the identified and selected, the plan should control. Diabetes Care 25:1159 –1171,
DSME entity needs to assess each patient’s incorporate timelines and important 2002
personal self-management goals and his/ milestones including data collection, 4. Norris SL: Self-management education
her progress toward those personal goals. analysis, and presentation of results in type 2 diabetes. Practical Diabetology
The AADE7 self-care behaviors provide a (163). Outcome measures indicate the re- 22:713, 2003
useful framework for assessment and doc- sult of a process (i.e., whether changes are 5. Gary TL, Genkinger JM, Guallar E, Pey-
umentation. Diabetes self-management actually leading to improvement), while rot M, Brancati FL: Meta-analysis of ran-
behaviors include physical activity, process measures provide information domized educational and behavioral
healthy eating, medication taking, moni- about what caused those results (163– interventions in type 2 diabetes. Diabetes
toring blood glucose, diabetes self-care 164). Process measures are often targeted Educ 29:488 –501, 2003
6. Deakin T, McShane CE, Cade JE, et al.
related problem solving, reducing risks of to those processes that typically impact Review: group based education in self-
acute and chronic complications, and the most important outcomes. Measuring management strategies improves out-
psychosocial aspects of living with diabe- both process and outcomes helps to en- comes in type 2 diabetes mellitus.
tes (112,160). Assessments of patient out- sure that change is successful without Cochrane Database Syst Rev (2):
comes should occur at appropriate causing additional problems in the system CD003417, 2005
intervals. The interval depends on the (164). 7. Renders CM, Valk GD, Griffin SJ, Wag-
outcome itself and the timeframe pro- ner EH, Eijk van JThM, Assendelft WJJ:
vided within the selected goals. For some Interventions to improve the manage-
areas, the indicators, measures, and time- Acknowledgments — Work on this article ment of diabetes in primary care, outpa-
frames may be based on guidelines from was supported in part by grant nos. NIH5P60 tient, and community settings: a
DK20572 and 1 R18 0K062323 from the Na- systematic review. Diabetes Care 24:
professional organizations or government tional Institute of Diabetes and Digestive and 1821–1833, 2001
agencies. In addition to assessing progress Kidney Diseases of the National Institutes of 8. Funnell MM, Anderson RM: Patient em-
toward personal behavioral goals, a plan Health. powerment: a look back, a look ahead.
needs to be in place to communicate per- The Task Force gratefully acknowledges the Diabetes Educ 29:454 – 464, 2003
sonal goals and progress to other team assistance and support of Paulina Duker, 9. Roter DL, Hall JA, Merisca R, Nordstrom
members. MPH, APRN-BC, CDE, and Nathanial Clark, B, Cretin D, Svarstad B: Effectiveness of
S92 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Standards and Review Criteria
interventions to improve patient compli- 23. Drucker PF: The objectives of a business tern Med 127:1097–1102, 1997
ance: a meta-analysis. Medical Care 36: (Chapter 7); Managing service institu- 38. Fox CH, Mahoney MC: Improving dia-
1138 –1161, 1998 tions for performance in management betes preventative care in a family prac-
10. Barlow J, Wright C, Sheasby J, et al: tasks, responsibilities, practices (Chap- tice residency program: a case study in
Self-management approaches for peo- ter 14). In The Practice of Management. continuous quality improvement. Fam-
ple with chronic conditions: a review. New York, Harper & Row, 1993 ily Medicine 30:441– 445, 1998
Patient Education and Counseling 48: 24. Drucker PF: Management: Tasks, Respon- 39. Siminerio L, Piatt G, Emerson S, Ruppert
177–187, 2002 sibilities, Practices. New York, Harper- K, Saul M, Solano F, Stewart A, Zgibor J:
11. Skinner TC, Cradock S, Arundel F, Gra- business, 1993 Deploying the chronic care model to im-
ham W: Lifestyle and behavior: four theo- 25. Garvin DA: The processes of organiza- plement and sustain diabetes self-man-
ries and a philosophy: self-management tion and management. Sloan Manage Rev agement training programs. Diabetes
education for individuals newly diagnosed (summer):30 –50, 1998 Educ 32:1– 8, 2006
with type 2 diabetes. Diabetes Spectrum 16: 26. Joint Commission on Accreditation of 40. Siminerio LM, Zgibor JC, Solano FX: Im-
75– 80, 2003 Healthcare Organizations: Joint Commis- plementing the chronic care model for
12. Brown SA, Hanis CL: Culturally compe- sion International Standards for Disease or improvements in diabetes practice and
tent diabetes education for Mexican Condition-Specific Care. 1st ed. Oak- outcomes in primary care: The Univer-
Americans: the Starr County Study. Di- brook Terrace. IL, Joint Accreditation on sity of Pittsburgh Medical Center Expe-
abetes Educ 25:226 –236, 1999 Healthcare Organizations, 2005 rience. Clinical Diabetes 22:54 –58, 2003
13. Anderson RM, Funnell MM, Nowankwo 27. Berwick DM: A primer on leading the 41. Heins JM, Nord Wr, Cameron M: Estab-
R, et al: Evaluating a problem based em- improvement of systems. BMJ 312:619 – lishing and sustaining state-of-the-art
powerment program for African Ameri- 622, 1996 diabetes education programs: research
cans with diabetes: results of a randomized 28. Clemmer TP, Spuhler VJ, Berwick DM, and recommendations. Diabetes Educ
controlled trial. Ethnicity and Disease 15: Nolan TW: Cooperation: the foundation 18:501–598, 1992
671– 678, 2005 of improvement. Annals Internal Medi- 42. Mangan M: Diabetes self-management
14. Sarkisian CA, Brown AF, Norris CK, cine 128:1004 –1009, 1998 education programs in the Veterans
Wintz RL, Mangione CM: A systematic 29. Courtney L, Gordon M, Romer L: A clin- Health Administration. Diabetes Educ
review of diabetes self-care interventions ical path for adult diabetes. The Diabetes 23:687– 695, 1997
for older, African American or Latino Educator 23:664 – 671, 1997 43. Griffin JA, Gilliland Ss, Perez G, Helitzer
adults. Diabetes Educ 28:467– 47915, 30. Glasgow RE, Hiss RG, Anderson RM, D, Carter JS.: Participants satisfaction
2003 Friedman NM, Hayward RA, Marrero with culturally appropriate diabetes ed-
15. Chodosh J, Morton SC, Mojica W, Ma- DG, Taylor CB, Vinicor F: Report of the ucation program: the Native American
glione M, Suttorp MJ, Hilton L, Rhodes Health Care Delivery Work Group. Dia- diabetes education program in a north-
S, Shekelle P: Meta-analysis: chronic dis- betes Care 24:124 –130, 2001 west Indian tribe. Diabetes Educ 25:351–
ease self-management programs for 31. Wagner EH, Austin BT, Von Korff M: 363, 1999
older adults. Ann Intern Med 143:427– Organizing care for patients with 44. Hiss RG: Barriers to care in non-insulin-
438, 2005 chronic illness. Milllbank Quarterly 74: dependent diabetes mellitus: the Michi-
16. Anderson-Loftin W, Barnett S, Bunn P, 511–544, 1996 gan experience. Ann Intern Med 124:
et al: A. Soul food light: culturally com- 32. Community Health Improvement Part- 146 –148, 1996
petent diabetes education. Diabetes Educ ners: From the board room to the com- 45. Simmons D, Voyle J, Swinburn B, O’Dea
31:555–563, 2005 munity room: a health improvement K: Community-based approaches for the
17. Mensing CR, Norris SL: Group educa- collaboration that’s working. Journal of primary prevention of non-insulin-de-
tion in diabetes: effectiveness and imple- Quality Improvement 24:549 –564, 1998 pendent diabetes mellitus. Diabet Med
mentation. Diabetes Spectrum 16:96 – 33. Kiefe CI, Allison JJ, Willais OD, Person 14:519 –526, 1997
103, 2003 SD, Weaver MT, Weissman NW: Im- 46. Gamm LD: Advancing community
18. Rickheim PL, Weaver TK, Flader JL, proving quality improvement using health through community health part-
Kendall DM: Assessment of group versus achievable benchmarks for physician nerships. J Healthcare Management 43:
individual education: a randomized feedback. JAMA 285:2871–2879, 2001 51– 67, 1998
study. Diabetes Care 25:269 –274, 2002 34. Solberg LI, Reger LA, Pearson TL, Cher- 47. Snoek FJ: Quality of life: a closer look at
19. Brown SA, Blozis SA, Kouzekanani K, ney LM, O’Connor PJ, Freeman SL, measuring patients’ well-being. Diabetes
Garcia AA, Winchell M, Hanis CL: Dos- Lasch SL, Bishop DB: Using continuous Spectrum 13:24 –28, 2000
age effects of diabetes self-management quality improvement to improve diabe- 48. Piatt G, Brooks MM, Orchard TJ,
education for Mexican Americans. Dia- tes care in populations: the IDEAL Kortykowski M, Emerson S, Siminerio L,
betes Care 28:527–532, 2005 model. J Qual Improv 23:531–591, 1997 Simmons D, Ahmad U, Soner TJ, Zgibor
20. Polonsky WH, Earles J, Smith S, Pease 35. O’Connor PJ, Rush WA, Peterson J, Mor- JC: Translating the chronic care model
DJ, Macmillan M, Christensen R, Taylor ben P, Cherney L, Keogh C, Lasch S: into the community. Diabetes Care 29:
T, Dickert J, Jackson RA: Integrating Continuous quality improvement can 811– 816, 2006
medical management with diabetes self- improve glycemic control for HMO pa- 49. Harris SB, Zinman B: Primary preven-
management training: a randomized tients with diabetes. Archives Family tion of type 2 diabetes in high-risk
control trial of the Diabetes Outpatient Medicine 5:502–506, 1996 populations. Diabetes Care 23:87–881,
Intensive Treatment Program. Diabetes 36. Wagner EH, Davis C, Schaefer J, Von 2000
Care 26:3094 –3053, 2003 Korff M, Austin B: A survey of leading 50. Rothman J: Approaches to community
21. Bodenheimer T, MacGregor K, Sharifi C: chronic disease management programs: intervention. In Strategies of Community
Helping Patients Manage Their Chronic Con- are they consistent with the literature? Intervention. 5th ed. Itasca, IL, F. Pea-
ditions. Oakland, CA, California Health- Journal of Nursing Care Quality 16:67– cock, 2001, p. 26 – 63
care Foundation, 2005 80, 2002 51. O’Connor PJ, Pronk NP: Integrating
22. Deming WE: Out of the Crisis. Cam- 37. Von Korff M, Gruman J, Schaefer J, population health concepts, clinical
bridge, MA, Massachusetts Institute of Curry SJ, Wagner EH: Collaborative guidelines, and ambulatory medical care
Technology, 2000 management of chronic illness. Ann In- systems to improve diabetes care. J Am-
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S93
Standards and Review Criteria
bulatory Care Manager 21:67–73, 1998 tients with non-insulin dependent 79. Shane-McWhorter L, Fermo JD, Bulte-
52. Wagner EH: The role of patient care diabetes mellitus: impact on glycemic meir NC, Oderda GM: National survey
teams in chronic disease management. control and health-related quality of life. of pharmacist certified diabetes educa-
Br Med J 320:569 –572, 2000 J Gen Intern Med 10:59 – 66, 1995 tors. Pharmacotherapy 22:1579 –1593,
53. Hiss RG, Gillard ML, Armbruster BA, 67. Spellbring AM: Nursing’s role in health 2002
McClure LA: Comprehensive evaluation promotion. Nurs Clin North Am 26:805– 80. Franz MJ, Callahan T, Castle G: Chang-
of community-based diabetic patients. 814, 1991 ing roles: educators and clinicians. Clin
Diabetes Care 24:690 – 694, 2001 68. Glasgow RE, Toobert DJ, Hampson SE, Diabetes 12:53–54, 1994
54. Jack L: Diabetes Self-Management Edu- Brown JE, Lewinsohn PM, Donnelly J: 81. Rubin RR, Peyrot M, Saudek CD: Effect
cation Research: An international review Improving self-care among older pa- of diabetes education on self-care, met-
of intervention methods, theories, com- tients with type II diabetes: the “sixty- abolic control, and emotional well-be-
munity partners and outcomes. Disease something.” study. Patient Educ Couns ing. Diabetes Care 12:673– 679, 1989
Management and Health Outcomes 19:61–74, 1992 82. Campbell EM, Redman S, Moffitt PS,
11:415– 428, 2003 69. Diabetes Control and Complications Sanson-Fisher RW: The relative effec-
55. Piette JD, Glasgow R: Strategies for im- Trial Research Group: Expanded role of tiveness of educational and behavioral
proving behavioral health outcomes the dietitian in the Diabetes Control and instruction programs for patients with
among patients with diabetes: self-man- Complications Trial: implications for NIDDM: a randomized trial. Diabetes
agement, education. In Evidence-Based practice. J Am Diet Assoc 93:758 –767, Educ 22:379 –386, 1996
Diabetes Care. Gerstein HC, Haynes RB, 1993 83. Rubin RR, Peyrot M, Saudek CD: The
Eds. Ontario, Canada, BC Decker Pub- 70. Delahanty LM, Halford BH: The role of effect of a diabetes education program
lishers 2001, p. 207–251 diet behaviors in achieving improved incorporating coping skills, training
56. Coonrod BA, Betschart J, Harris MI: Fre- glycemic control in intensively treated on emotional well-being, and diabetes
quency and determinants of diabetes pa- patients in the Diabetes Control and self-efficacy. Diabetes Educ 19:210 –
tient education among adults in the U.S. Complications Trial. Diabetes Care 16: 214, 1993
population. Diabetes Care 17:852– 858, 1453–1458, 1993 84. Emerson S: Implementing diabetes self-
1994 71. Franz MJ, Monk A, Barry B, McLain K, management education in primary care.
57. Pearson J, Mensing C, Anderson R: Weaver T, Cooper N, Upham P, Bergen- Diabetes Spectrum 19:79 – 83, 2006
Medicare reimbursement and diabetes stal R, Mazze R: Effectiveness of medical 85. Satterfield D, Burd, C Valdez L, Hosey G,
self-management training: national sur- nutrition therapy provided by dietitians Eagle Shield J: The “In-Between People”:
vey results. Diabetes Educ 30:914 –927, in the management of non-insulin-de- participation of community health rep-
2004 pendent diabetes mellitus: a random- resentatives and lay health workers in
58. Siminerio L, Piatt G, Zgibor J: Imple- ized, controlled clinical trial. J Am Diet diabetes prevention and care in Ameri-
menting the chronic care model in a ru- Assoc 95:1009 –1017, 1995 can Indian and Alaska Native communi-
ral practice. Diabetes Educ 31:225–234, 72. Khakpour D, Thompson L: The nutri- ties. Health Promotion Practice 3:66 –175,
2005 tion specialist on the diabetes manage- 2002
59. Anderson RM, Goddard CE, Garcia R, ment team. Clin Diabetes 16:21–22, 86. American Association of Diabetes Ed-
Guzman JR, Vazquez F: Using focus 1998 ucators: American Association of Dia-
groups to identify diabetes care and ed- 73. Baran R, Crumlish K, Patterson H, Shaw betes Educators Position Statement:
ucation issues for Latinos with diabetes. J, Erwin G, Wylie J, Duong P: Improving diabetes community health workers.
Diabetes Educ 24:618 – 625, 1998 outcomes of community-dwelling older Diabetes Educ 29:818 – 823, 2003
60. Zgibor JC, Simmons D: Barriers to blood patients with diabetes through pharma- 87. American Public Health Association
glucose monitoring in a multiethnic cist counseling. Am J Health Syst Pharm (APHA) Policy Statement No. 2001–15.
community. Diabetes Care 25:1772– 56:1535–1539, 1999 Recognition and support for community
1777, 2002 74. Coast-Senior EA, Kroner BA, Kelley CL, health workers’ contributions to meeting
61. Johnson K, Schubring L: The evolution Trilli LE: Management of patients with our nation’s health care needs. Policy
of a hospital-based decentralized case type 2 diabetes by pharmacists in pri- Statements Adopted by the Governing
management model. Nursing Economics mary care clinics. Ann Pharmacother 32: Council of the American Public Health
17:29 – 48, 1999 636 – 641, 1998 Association, October 24, 2001. Am J
62. Diabetes Control and Complications 75. Huff PS, Ives TJ, Almond SN, Griffin Public Health 92:451– 483, 2002
Trial Research Group: The impact of the NW: Pharmacist-managed diabetes edu- 88. Norris SL, Chowdhury FE, VanLet K,
trial coordinator in the Diabetes Control cation service. Am J Hosp Pharm 40:991– Horsley T, Brownstein JN, Zhang X, Jack
and Complications Trial (DCCT). Diabe- 993, 1983 L Jr, Satterfield DW: Effectiveness of
tes Educ 19:509 –512, 1993 76. Canter CL: The Asheville Project: Long community health workers in the care of
63. Koproski J, Pretto Z, Poretsky L: Effects term-clinical and economic outcomes of persons with diabetes. Diabet Med 23:
of an intervention by a diabetes team in a community pharmacy diabetes care 544 –556, 2006
hospitalized patients with diabetes. Dia- program. J Am Pharm Assoc (Wash) 43: 89. Lewin SA, Dick J, Pond P, Zwarenstein
betes Care 20:1553–1555, 1997 173–184, 2003 M, Aja G, van Wyk B, Bosch-Copblanch
64. Davis ED: Role of the diabetes nurse ed- 77. Van Veldhuizen-Scott MK, Widmer LB, Z, Patrick M: Lay health workers in pri-
ucator in improving patient education. Stacey SA, Popovich NG: Developing mary and community health care. Co-
Diabetes Educ 16:36 – 43, 1990 and implementing a pharmaceutical care chrane Database Syst Rev 1:2005
65. Fedderson E, Lockwood DH: An inpa- model in an ambulatory care setting for 90. Norris SL, Nichols PJ, Caspersen CJ, et
tient diabetes educator’s impact on patients with diabetes. Diabetes Educ 21: al: Increasing diabetes self-management
length of hospital stay. Diabetes Educ 20: 117–123, 1995 education in community settings. a sys-
125–128, 1994 78. Garrentt DG, Blumi BM: Patient self- tematic review. Am J Prev Med 22:39 –
66. Weinberger M, Kirkman MS, Samsa GP, management program for diabetes: 43, 2002
Shortliffe EA, Landsman PB, Cowper PA, first-year clinical, humanistic, and 91. Lorig KR, Ritter P, Stewart AL, et al:
Simel DL, Feussner JR: A nurse-coordi- economic outcomes. J Am Pharm Assoc Chronic disease self-management pro-
nated intervention for primary care pa- 45:130 –137, 2005 grams. Medical Care 39:1217–1221, 2001
S94 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Standards and Review Criteria
92. Heisler M: Building peer support pro- 104. Skovlund SE, Peyrot M, on behalf of the outcomes. J Am Dietetic Association 9:
grams to manage chronic disease: seven DAWN International Advisory Panel: 1426 –1433, 2006
models for success. Oakland, CA, Cali- The Diabetes Attitudes, Wishes, and 117. Kulkarni K, Boucher JL, Daly A, Shwide-
fornia Health Care Foundation, 2006 Needs (DAWN) program: a new ap- Slavin C, Silvers BT, O-Sullivan-Maillet
93. Anderson RM, Donnelly MB, Gressard proach to improving outcomes of diabe- J, Pritchett E, American Dietetic Associ-
CP: The attitudes of nurses, dietitians, tes care. Diabetes Spectrum 18:136 –142, ation, Diabetes Care and Education
and physicians toward diabetes. Diabetes 2005 Practice Group, American Dietetic Asso-
Educ 17:261–268, 1991 105. Norris SL, Nichols PJ, Caspersen CJ, ciation: Standards of practice and stan-
94. Lorenz RA, Bubb J, Davis D, Jacobson A, Glasgow RE, Emgelgau MM, Jack J, Sny- dards of professional performance for
Jannasch K, Kramer J, Lipps J, Schlundt der SR, Carande-Kulis VG, Isham G, registered dietitians (generalist, spe-
D: Changing behavior: practical lessons Garfield S, Briss P, McCulloch D, and the cialty, and advanced) in diabetes care.
from the Diabetes Control and Compli- Task Force on Community Preventive J Am Dietetic Association 105:819 – 824,
cations Trial. Diabetes Care 19:648 –652, Services. Increasing diabetes self-man- 2005
1996 agement education in community set- 118. Blanchard MA, Rose LE, Taylor J, Mc-
95. Ockene JK, Ockene IS, Quirk ME, He- tings: a systematic review. Am J Prev Med Entee MA, Latchaw L: Using a focus
bert JR, Saperia GM, Luippold RS, Mer- 22:33– 66, 2002 group to design a diabetes program for
riam PA, Ellis S: Physician training for 106. Norris SL, Zhang X, Avenell A, Gregg E, an African American population. Diabe-
patient-centered nutrition counseling in Bowman B, Serdula M, Brown TJ, tes Educ 25:917–923, 1999
a lipid intervention trial. Prev Med 24: Schmid CH, Lau J: Long term effective- 119. Sarkadi A, Rosenqvist U: Study circles at
563–570, 1995 ness of lifestyle and behavioral weight the pharmacy – a new model for diabetes
96. Cypress M, Wylie-Rosett J, Engel SS, loss interventions in adults with type 2 education in groups. Patient Ed and
Stager TB: The scope of practice of dia- diabetes: a meta-analysis. Am J Med 117: Counselling 37:89 –96, 1999
betes educators in a metropolitan area. 762–74, 2004 120. Norris SL: Health related quality of life
Diabetes Educ 18:111–114, 1992 107. Ellis SE, Speroff T, Dittus RS, Brown A, among adults with diabetes. Curr Diab
97. Leggett-Frazier N, Swanson MS, Vincent Pichert JW, Elasy TA: Diabetes patient Reports 5:124 –30, 2005
PA, Pokorny ME, Engelke MK: Tele- education: a meta-analysis and meta-re- 121. Tang TS, Gillard ML, Funnell MM, et al:
phone communication between diabetes gression. Patient Educ Counsel 52:97– Developing a new generation of ongoing
clients and nurse educators. Diabetes 105, 2004 diabetes self-management support inter-
Educ 23:287–293, 1997 108. Brown SA: Studies of educational inter- ventions (DSMS): a preliminary report.
98. American Association of Diabetes Edu- ventions in diabetes care: a meta-analy- Diabetes Educ 31:91–97, 2005
cators: The scope of practice for diabetes sis revisited. Patient Educ Counsel 16: 122. Funnell MM, Nwankwo R, Gillard ML,
educators and the standards of practice 189 –215, 1990 Anderson RM, Tang TS: Implementing
for diabetes educators. Diabetes Educ 26: 109. Armour TA, Norris SL, Jack L Jr, Zhang an empowerment-based diabetes self-
25–31, 2000 X, Fisher L: The effectiveness of family management education program. Diabe-
99. Valentine V, Kulkarni K, Hinnen D: interventions in people with diabetes tes Educ 31:53– 61, 2005
Evolving roles: from diabetes educators mellitus: a systematic review. Diabet Med 123. Glazier RH, Bajcar J, Kennie NR, Willson
to advanced diabetes managers. Diabetes 10:1295–1305, 2005 K: A systematic review of interventions
Spectrum 16:27–31, 2004 110. Redman BK: The Practice of Patient Edu- to improve diabetes care in socially dis-
100. Glasgow RE, Funnell MM, Bonomi AE, cation. 10th ed. St. Louis, MO, Mosby, advantaged populations. Diabetes Care
Davis CL, Beckham V, Wagner EH: Self- 2007 26:1675– 88, 2006
management aspects of the Improving 111. Wikipedia. Curriculum definition. 124. Samuel-Hodge CD, Keyserling TC,
Chronic Illness Care Breakthrough se- Available at http://en.wikipedia.org/ France R, Ingram AF, Johnston LF,
ries: design and implementation with di- wiki/Curriculum. Accessed 7 January Pullen Davis L, Davis G, Cole AS: A
abetes and heart failure teams. Ann Behav 2007 church based diabetes self-management
Med 24:80 – 87, 2002 112. Mulcahy K, Maryniuk M, Peeples M, education program for African Ameri-
101. Ofman JJ, Badamgarav E, Henning JM, Peyrot M, Tomky D, Weaver T, Yarbor- cans with type 2 diabetes. Prev Chronic
Knight K, Gano AD Jr, Levan RK, Gur- ough P: Diabetes self-management edu- Dis 3:A93, 2006
Arie S, Richards MS, Hasselblad V, Wein- cation core outcome measures. Diabetes 125. Trento M, Passera P, Borgo E, Tomalino
garten SR: Does disease management Educ 29:768 – 803, 2003 M, Bajardi M, Cavallo F, Porta M: A
improve clinical and economic out- 113. American Association of Diabetes Edu- 5-year randomized controlled study of
comes in patients with chronic diseases? cators: The scope of practice, standards learning, problem solving ability, and
A systematic review. Am J Med 117:182– of practice, and standards of profes- quality of life modifications in people
192, 2004 sional performance for diabetes educa- with type 2 diabetes managed by group
102. Wensing M, Wollersheim H, Grol R: Or- tors. Diabetes Educ 31:487–513, 2005 care. Diabetes Care 27:670 – 675, 2004
ganizational interventions to implement 114. American Diabetes Association: Stan- 126. Izquierdo RE, Knudson PE, Meyer S,
improvements in patient care: a struc- dards of medical care in diabetes— Kearns J, Ploutz-Snyder R, Weinstock R:
tured review of reviews. Implementation 2009. Diabetes Care 32 (Suppl. 1):S13– A comparison of diabetes education ad-
Sci 1:2, 2006 S61, 2009 ministered through telemedicine versus
103. Mazze R, Albin J, Friedman J, Hahn S, 115. American Diabetes Association: Nutri- in person. Diabetes Care 26:1002–1007,
Murphy JA, Reese P, Rosen S, Scaggs C, tion recommendations and interven- 2003
Shamoon H, Vaccaro-Olko MJ: Diabetes tions for diabetes: a position statement 127. Garrett N, Hageman CM, Sibley SD,
education teams. Professional Education of the American Diabetes Association Davern M, Berger M, Brunzell C, Ma-
in Diabetes: Proceedings of the DRTC Con- (Position Statement). Diabetes Care 30 lecha K, Richards SW: The effectiveness
ference. National Diabetes Information (Suppl. 1):S48 –S65, 2007 of an interactive small group diabetes in-
Clearinghouse and National Institute of 116. Reader D, Splett P, Gunderson EP: Im- tervention in improving knowledge,
Diabetes and Digestive and Kidney Dis- pact of gestational diabetes mellitus nu- feeling of control and behavior. Health
eases, National Institutes of Health, De- trition practice guidelines implemented Promot Pract 6:320 –328, 2005
cember 1980 by registered dietitians on pregnancy 128. Hayes JT, Boucher JL, Pronk NP, Gehlin
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S95
Standards and Review Criteria
E, Spencet M, Waslaski J: The role of the Diaz Sullivan G, Bindman AB: Associa- and Safety 29:563–574, 2003
certified diabetes educator in telephone tion of health literacy with diabetes out- 154. Daly A, Leontos C: Legislation for health
counseling. Diabetes Educ 27:377–386, comes. JAMA 288:475– 482, 2002 care coverage for diabetes self-manage-
2001 142. Nurss JR, Parker R, Williams M, Baker ment training, equipment and supplies:
129. Carlson A, Rosenqvist U: Diabetes care D: STOFHLA Teaching Edition. Snow past, present and future. Diabetes Spec-
organization, process and patient out- Camp, NC, Peppercorn Books, 2003 trum 12:222–230, 1999
comes: effects of a diabetes control pro- 143. Chew LD, Bradley KA, Boyko EJ: Brief 155. Grebe SKG, Smith RBW Clinical audit
gram. Diabetes Educ 17:42– 48, 1991 questions to identify patients with inad- and standardized follow-up improve
130. Handley M, MacGregor K, Schillinger D, equate health literacy. Family Medicine quality of documentation in diabetes
Scharifi C, Wong S, Bodenheimer T: Us- 36:588 –594, 2006 care. N Z Med J 108:339 –342, 1995
ing action plans to help primary care pa- 144. Shillinger D, Piette J, Grumbach K, 156. Schriger DL, Baraff LJ, Rogers WH, Cre-
tients adopt healthy behaviors: A Wang F, Wilson C, Daher C, et al.: Clos- tin S: Implementation of clinical guide-
descriptive study. J Am Board Fam Med ing the loop: physician communication lines using a computer charting system:
19:224 –231, 2006 with diabetic patients who have low effect on the initial care of health care
131. Gilden JL, Hendryx M, Casia C, Singh health literacy. Arch Intern Med 163:83– workers exposed to body fluids. JAMA
SP: The effectiveness of diabetes educa- 90, 2003 278:1585–1590, 1997
tion programs for older patients and 145. Piette JD, Heisler M, Wagner TH: Prob- 157. Aubert RE, Herman WH, Waters J,
their spouses. J Am Geriatr Soc 37:1023– lems paying out of pocket medication Moore W, Sutton D, Peterson BL, Bailey
1030, 1989 costs among older adults with diabetes. CM, Koplan JP Nurse case management
132. Brown SA: Effects of educational inter- Diabetes Care 27:384 –391, 2004 to improve glycemic control in diabetic
ventions in diabetes care: a meta-analy- 146. Peyrot M, Rubin RR, Lauritzen T, Snoek patients in a health maintenance organi-
sis of findings. Nurs Res 37:223–230, FJ, Matthews DR, Skovlund SE: Psycho- zation: a randomized, controlled trial.
1988 social problems and barriers to im- Ann Intern Med 129 605– 612, 1998
133. Davis WK, Hull AL, Boutaugh ML: Fac- proved diabetes management: results of 158. Knight K, Badamgarav E, Henning JM,
tors affecting the educational diagnosis the cross-national Diabetes Attitudes, Hasselblad V, Gano AD Jr, Ofman JJ,
of diabetic patients. Diabetes Care 4: Wishes, and Needs study. Diabet Med Weingarten SR: A systematic review of
275–278, 1981 22:1379 –1385, 2005 diabetes disease management programs.
134. Anderson RM, Fitzgerald JT, Oh M: The 147. Peyrot M, Rubin RR, Siminerio L, on be- Am J Managed Care 11:242–50, 2005
relationship between diabetes-related half of the International DAWN Advi- 159. Two Feathers J, Kieffer EC, Palmisano G,
attitudes and patients’ self-reported ad- sory Panel: Physician and nurse use of et al: Racial and ethnic approaches to
herence. Diabetes Educ 19:287–292, 1993 psychosocial strategies in diabetes care: community health (REACH) Detroit
135. Funnell MM, Anderson RM: AADE Po- results of the cross-national Diabetes At- partnership: improving diabetes-related
sition Statement: individualization of titudes, Wishes, and Needs study. Dia- outcomes among African American and
diabetes self-management education. betes Care 29:1256 –1262, 2006 Latino adults. Am J Public Health 95:
Diabetes Educ 33:45– 49, 2007 148. Rubin RR, Peyrot M, Siminerio L, on be- 1552–1560, 2005
136. Davis TC, Crouch MA, Wills G, Miller S, half of the International DAWN Advi- 160. Mulcahy K, Maryniuk M, Peeple M, Pey-
Abdehou DM: The gap between patient sory Panel: Health care and patient- rot M, Tomky D, Weaver T, Yarborough
reading comprehension and the read- reported outcomes: results of the cross- P: AADE Position Statement: standards
ability of patient education materials. J national Diabetes Attitudes, Wishes, and for outcomes measurement of diabetes
Fam Pract 31:533–538, 1990 Needs study. Diabetes Care 29:1249 – self-management education. Diabetes
137. Hosey GM, Freeman WL, Stracqualursi 1255, 2006 Educ 29:804 – 816, 2003
F, Gohdes D: Designing and evaluating 149. McKellar JD, Humphreys K, Piette JD: 161. Institute of Healthcare Improvement: How
diabetes education material for Ameri- Depression increases diabetes symp- to improve: improvement methods. Avail-
can Indians. Diabetes Educ 16:407– 414, toms by complicating patients’ self-care able at http://www.ihi.org/IHI/Topics/Im
1990 adherence. Diabetes Educ 30:485– 492, provement/improvementmethods\.
138. Thomson FJ, Masson EA: Can elderly 2004 Accessed 24 April 2006
patients co-operate with routine foot 150. Krein SL, Heisler M, Piette JD, Makki F, 162. Bardsley J, Bronzini B, Harriman K,
care? Diabetes Spectrum 8:218 –219, Kerr EA: The effect of chronic pain on Lumber T: CQI: A Step by Step Guide for
1995 diabetes patients’ self-management. Di- Quality Improvement in Diabetes Educa-
139. Assal JP, Jacquemet S, Morel Y: The abetes Care 28:65–70, 2005 tion. Chicago, IL, American Association
added value of therapy in diabetes: the 151. Piette JD, Kerr E: The role of comorbid of Diabetes Educators, 2005
education of patients for self-manage- chronic conditions on diabetes care. Di- 163. Joint Commission Resources: Cost-Effec-
ment of their disease. Metabolism 46:61– abetes Care 29:239 –253, 2006 tive Performance Improvement in Ambula-
64, 1997 152. Estey AL, Tan MH, Mann K: Follow-up tory Care. Oakbrook Terrace, IL, Joint
140. Ad Hoc Committee on Health Literacy intervention: its effect on compliance Commission on Accreditation of Health-
for the Council on Scientific Affairs, behavior to a diabetes regimen. Diabetes care Organizations, 2003
American Medical Association: Health Educ 16:291–295, 1990 164. Institute of Healthcare Improvement:
literacy: report of the Council on Scien- 153. Glasgow RE, Davis CL, Funnell MM, et Measures: diabetes. Available at http://
tific Affairs. JAMA 281:552–557, 1999 al: Implementing practical interventions www.ihi.org/IHI/Topics/ChronicCondi
141. Schillinger D, Grumbach K, Piette J, to support chronic illness self-manage- tions/Diabetes/Measures. Accessed 24
Wang F, Osmond D, Daher C, Palacios J, ment. Joint Commission Journal on Quality April 2006
S96 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Technical Reviews
A technical review is a balanced review in patients with diabetes. Diabetes Care Nutrition Recommendations and Prin-
and analysis of the literature on a scien- 24:131–153, 2001 ciples
tific or medical topic related to diabetes. Franz MJ, Bantle JP, Beebe CA, Brunzell
The technical review provides a scientific Hypertension JD, Chiasson JL, Garg A, Holzmeister LA,
rationale for a position statement and un- Arauz-Pacheco C, Parrott MA, Raskin P: Hoogwerf B, Mayer-Davis E, Mooradian
dergoes critical peer review before sub- The treatment of hypertension in adult AD, Purnell JS, Wheeler M: Evidence-
mission to the Professional Practice patients with diabetes. Diabetes Care 25: based nutrition principles and recom-
Committee for approval. Effective Janu- 134 –147, 2002
mendations for the treatment and
ary 2010, technical reports are replaced prevention of diabetes and related com-
with systematic reviews, for which a pri- Hypoglycemia
Cryer PE, Davis SN, Shamoon H: Hypo- plications. Diabetes Care 25:148 –198,
ori search and inclusion/exclusion criteria
glycemia in diabetes. Diabetes Care 26: 2002
are developed and published. Listed be-
low are recent technical reviews. 1902–1912, 2003
Pancreas Transplantation
Economic Analysis of Diabetes Inter- Immunizations Robertson RP, Davis C, Larsen J, Stratta R,
ventions Smith SA, Poland GA: Use of influenza Sutherland DER: Pancreas and islet trans-
Klonoff DC, Schwartz DM: An economic and pneumococcal vaccines in people plantation for patients with diabetes. Di-
analysis of interventions for diabetes. Di- with diabetes. Diabetes Care 23:95–108, abetes Care 23:112–116, 2000
abetes Care 23:390 – 404, 2000 2000
Retinopathy
Exercise Laboratory Analysis Fong DS, Aiello LP, Ferris FL III, Klein R:
Sigal RJ, Kenny GP, Wasserman DH, Cas- Sacks DB, Bruns DE, Goldstein DE, Ma- Diabetic retinopathy. Diabetes Care 27:
taneda-Sceppa C: Physical activity/ claren NK, McDonald JM, Parrott M: 2540 –2553, 2004
exercise and type 2 diabetes. Diabetes Guidelines and recommendations for lab-
Care 27:2518 –2539, 2004 oratory analysis in the diagnosis and man- Screening for Type 2 Diabetes
agement of diabetes mellitus. Diabetes Engelgau MM, Narayan KM, Herman
Hospitals Care 25:750 –786, 2002 (Reprinted from WH: Screening for type 2 diabetes. Dia-
Clement S, Braithwaite SS, Magee MF, Clin Chem 48:436 – 472, 2002) betes Care 23:1563–1580, 2000
Ahmann A, Smith EP, Schafer RG, Hirsh
IB: Management of diabetes and hyper- Neuropathy Tests of Glycemia
glycemia in hospitals. Diabetes Care 27: Vinik AI, Maser RE, Mitchell BD, Freeman Goldstein DE, Little RR, Lorenz RA, Ma-
553–591, 2004 R: Diabetic autonomic neuropathy. Dia- lone JI, Nathan D, Peterson CM, Sacks
betes Care 26:1553–1579, 2003 DB: Tests of glycemia in diabetes. Diabetes
Hyperglycemic Crises
Care 27:1761–1773, 2004
Kitabchi AE, Umpierrez GE, Murphy MB, Boulton AJ, Malik RA, Arezzo JC, Sosenko
Barrett EJ, Kreisberg RA, Malone JI, Wall JM: Diabetic somatic neuropathies. Dia-
BM: Management of hyperglycemic crises betes Care 27:1458 –1486, 2004
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S97
Consensus Reports
Effective January 2010, prior reports of the types listed below are renamed “consensus reports.”
EXPERT COMMITTEE REPORTS man, Robert Sherwin, and Bernard Zin- Managing Preexisting Diabetes for
man Pregnancy: Summary of Evidence and
International Expert Committee Re- Diabetes Care 32:193–203, 2009 Consensus Recommendations for Care
port on the Role of the A1C Assay in John L. Kitzmiller, Jennifer M. Block, Flo-
the Diagnosis of Diabetes American Association of Clinical Endo- rence M. Brown, Patrick M. Catalano, De-
International Expert Committee crinologists and American Diabetes As- borah L. Conway, Donald R. Coustan,
Diabetes Care 32:1327–1334, 2009 sociation Consensus Statement on Erica P. Gunderson, William H. Herman,
Follow-Up Report on the Diagnosis of Inpatient Glycemic Control Lisa D. Hoffman, Maribeth Inturrisi, Lois
Diabetes Mellitus Etie S. Moghissi, Mary T. Korytkowski, B. Jovanovic, Siri I. Kjos, Robert H.
Expert Committee on the Diagnosis and Monica DiNardo, Daniel Einhorn, Rich- Knopp, Martin N. Montoro, Edward S.
Classification of Diabetes ard Hellman, Irl B. Hirsch, Silvio E. In- Ogata, Pathmaja Paramsothy, Diane M.
Diabetes Care 26:3160 –3167, 2003 zucchi, Faramarz Ismail-Beigi, M. Sue Reader, Barak M. Rosenn, Alyce M.
Kirkman, and Guillermo E. Umpierrez Thomas, and M. Sue Kirkman
WORKGROUP REPORTS Diabetes Care 32:1119 –1131, 2009 Diabetes Care 31:1060 –1079, 2008
Comprehensive Foot Examination and Hyperglycemic Crises in Adult Pa- Influence of Race, Ethnicity, and Culture
Risk Assessment: a Report of the Task tients With Diabetes on Childhood Obesity: Implications for
Force of the Foot Care Interest Group Abbas E. Kitabchi, Guillermo E. Umpier- Prevention and Treatment: A Consensus
of the American Diabetes Association, rez, John M. Miles, and Joseph N. Fisher Statement of Shaping America’s Health
With Endorsement by the American Diabetes Care 32:1335–1343, 2009 and the Obesity Society
Association of Clinical Endocrinolo- Sonia Caprio, Stephen R. Daniels, Adam
gists How Do We Define Cure of Diabetes? Drewnowski, Francine R. Kaufman, Law-
Andrew J.M. Boulton, David G. Arm- John B. Buse, Sonia Caprio, William T. rence A. Palinkas, Arlan L. Rosenbloom,
strong, Stephen F. Albert, Robert G. Fryk- Cefalu, Antonio Ceriello, Stefano Del and Jeffrey B. Schwimmer
berg, Richard Hellman, M. Sue Kirkman, Prato, Silvio E. Inzucchi, Sue McLaughlin, Diabetes Care 31:2211–2221, 2008
Lawrence A. Lavery, Joseph W. LeMaster, Gordon L. Phillips II, R. Paul Robertson,
Joseph L. Mills, Sr., Michael J. Mueller, Screening for Coronary Artery Disease
Francesco Rubino, Richard Kahn, and M.
Peter Sheehan, and Dane K. Wukich in Patients With Diabetes
Sue Kirkman.
Diabetes Care 31:1679 –1685, 2008 Jeroen J. Bax, Lawrence H. Young, Robert
Diabetes Care 32:2133–2135, 2009
L. Frye, Robert O. Bonow, Helmut O.
American Diabetes Association State- Steinberg, and Eugene J. Barrett
ment on Emergency and Disaster Pre- Management of Hyperglycemia in Type
Diabetes Care 30:2729 –2736, 2007
paredness: a Report of the Disaster 2 Diabetes: A Consensus Algorithm for
Response Task Force the Initiation and Adjustment of Ther- Consensus Statement on the World-
Disaster Response Task Force apy: Update Regarding Thiazo- wide Standardization of the Hemoglo-
Diabetes Care 30:2395–2398, 2007 lidinediones: a Consensus Statement bin A1C Measurement: the American
From the American Diabetes Associa- Diabetes Association, European Asso-
Defining and Reporting Hypoglycemia tion and the European Association for
in Diabetes: a Report From the Ameri- ciation for the Study of Diabetes, Inter-
the Study of Diabetes national Federation of Clinical
can Diabetes Association Workgroup David M. Nathan, John B. Buse, Mayer B.
on Hypoglycemia Chemistry and Laboratory Medicine,
Davidson, Ele Ferrannini, Rury R. Hol- and the International Diabetes Federa-
American Diabetes Association Work- man, Robert Sherwin, and Bernard Zin-
group on Hypoglycemia tion
man Consensus Committee
Diabetes Care 28:1245–1249, 2005
Diabetes Care 31:173–175, 2008 Diabetes Care 30:2399 –2400, 2007
CONSENSUS STATEMEMENTS Lipoprotein Management in Patients Use of Insulin Pump Therapy in the Pe-
Medical Management of Hyperglyce- With Cardiometabolic Risk: Consen- diatric Age-Group: Consensus State-
mia in Type 2 Diabetes: A Consensus sus Statement From the American Dia- ment From the European Society for
Algorithm for the Initiation and Ad- betes Association and the American Paediatric Endocrinology, the Lawson
justment of Therapy: A Consensus College of Cardiology Foundation Wilkins Pediatric Endocrine Society,
Statement of the American Diabetes John D. Brunzell, Michael Davidson, Curt and the International Society for Pedi-
Association and the European Associa- D. Furberg, Ronald B. Goldberg, Barbara atric and Adolescent Diabetes, En-
tion for the Study of Diabetes V. Howard, James H. Stein, and Joseph L. dorsed by the American Diabetes
David M. Nathan, John B. Buse, Mayer B. Witztum Association and the European Associa-
Davidson, Ele Ferrannini, Rury R. Hol- Diabetes Care 31:811– 822, 2008 tion for the Study of Diabetes
S98 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Moshe Phillip, Tadej Battelino, Henry Computer Modeling of Diabetes and Physical Activity/Exercise and Type 2
Rodriguez, Thomas Danne, Francine Its Complications: a Report on the Diabetes: A Consensus Statement
Kaufman for the Consensus forum par- Fourth Mount Hood Challenge Meet- From the American Diabetes Associa-
ticipants ing tion
Diabetes Care 30:1653–1662, 2007 The Mount Hood 4 Modeling Group Ronald J. Sigal, Glen P. Kenny, David H.
Diabetes Care 30:1638 –1646, 2007 Wasserman, Carmen Castaneda-Sceppa,
Waist Circumference and Cardiometa- and Russell D. White
bolic Risk: a Consensus Statement Diabetes Care 29:1433–1438, 2006
From Shaping America’s Health: Asso-
ciation for Weight Management and
Obesity Prevention; NAASO, The Obe- Impaired Fasting Glucose and Im-
sity Society; the American Society for paired Glucose Tolerance: Implica- Diabetic Ketoacidosis in Infants, Chil-
Nutrition; and the American Diabetes tions for Care dren, and Adolescents: A Consensus
Association David M. Nathan, Mayer B. Davidson, Statement From the American Diabe-
Samuel Klein, David B. Allison, Steven B. Ralph A. DeFronzo, Robert J. Heine, Rob- tes Association
Heymsfield, David E. Kelley, Rudolph L. ert R. Henry, Richard Pratley, and Ber- Joseph Wolfsdorf, Nicole Glaser, and
Leibel, Cathy Nonas, and Richard Kahn nard Zinman Mark A. Sperling
Diabetes Care 30:1647–1652, 2007 Diabetes Care 30:753–759, 2007 Diabetes Care 29:1150 –1159, 2006
care.diabetesjournals.org DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 S99
Position Statements
A position statement is an official point Unproven Therapies Nephropathy in Diabetes
of view or belief of the ADA. Position Diabetes Care 27 (Suppl. 1):S135, 2004 Diabetes Care 27 (Suppl. 1):S79 –S83,
statements are issued on scientific or 2004
medical issues related to diabetes. They Prevention of Type 1 Diabetes
may be authored or unauthored and are Diabetes Care 27 (Suppl. 1):S133, 2004 Preconception Care of Women With
published in ADA journals and other Diabetes
scientific/medical publications as ap- Concurrent Care Diabetes Care 27 (Suppl. 1):S76 –S78,
propriate. Position statements must be Diabetes Care 27 (Suppl. 1):S132, 2004 2004
reviewed and approved by the Profes-
sional Practice Committee and, subse- Influenza and Pneumococcal Smoking and Diabetes
quently, by the Executive Committee of Immunization in Diabetes Diabetes Care 27 (Suppl. 1):S74 –S75,
the Board of Directors. ADA position Diabetes Care 27 (Suppl. 1):S111–S113, 2004
statements are typically based on a tech- 2004
nical review or other review of published Aspirin Therapy in Diabetes
literature. They are reviewed on an annual Continuous Subcutaneous Insulin Diabetes Care 27 (Suppl. 1):S72–S73,
basis and updated as needed. In addition Infusion 2004
to those published in this supplement, Diabetes Care 27 (Suppl. 1):S110, 2004
listed below are recent position state- Dyslipidemia Management in Adults
ments. Insulin Administration With Diabetes
Diabetes Care 27 (Suppl. 1):S106 –S109, Diabetes Care 27 (Suppl. 1):S68 –S71,
Intensive Glycemic Control and 2004 2004
Prevention of Cardiovascular Events
Diabetes Care 32:187–192, 2009 Hypertension Management in Adults
Pancreas Transplantation in Type 1
With Diabetes
Diabetes
Nutrition Diabetes Care 27 (Suppl. 1):S65–S67,
Diabetes Care 27 (Suppl. 1):S105, 2004
Diabetes Care 31 (Suppl. 1):S61–S78, 2004
2008
Bedside Blood Glucose Monitoring Preventive Foot Care in Diabetes
Generic Drugs in Hospitals Diabetes Care 27 (Suppl. 1):S63–S64,
Diabetes Care 30:173, 2007 Diabetes Care 27 (Suppl. 1):S104, 2004 2004
Pancreas and Islet Transplantation Hospital Admission Guidelines for Physical Activity/Exercise and
in Type 1 Diabetes Diabetes Diabetes
Diabetes Care 29:935, 2006 Diabetes Care 27 (Suppl. 1):S103, 2004 Diabetes Care 27 (Suppl. 1):S58 –S62,
2004
Metabolic Syndrome Hyperglycemic Crises in Diabetes
Diabetes Care 28:2289, 2005 Diabetes Care 27 (Suppl. 1):S94 –S102, Diabetes Nutrition
2004 Recommendations for Health Care
Neuropathy Institutions
Diabetes Care 28:956, 2005 Tests of Glycemia in Diabetes Diabetes Care 27 (Suppl. 1):S55–S57,
Diabetes Care 27 (Suppl. 1):S91–S93, 2004
Children and Adolescents With Type 2004
1 Diabetes Prevention or Delay of Type 2
Diabetes Care 28:186, 2005 Gestational Diabetes Mellitus Diabetes
Diabetes Care 27 (Suppl. 1):S88 –S90, Diabetes Care 27 (Suppl. 1):S47–S54,
Dietary Carbohydrate 2004 2004
Diabetes Care 27:2266, 2004
Retinopathy in Diabetes Screening for Type 2 Diabetes
Weight Management Diabetes Care 27 (Suppl. 1):S84 –S87, Diabetes Care 27 (Suppl. 1):S11–S14,
Diabetes Care 27:2067, 2004 2004 2004
S100 DIABETES CARE, VOLUME 33, SUPPLEMENT 1, JANUARY 2010 care.diabetesjournals.org
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Diabetes in PregnancyDocumento88 pagineDiabetes in PregnancyKathleenZunigaNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Diabetes Clinical Guidelines-V21.0 27.07.10Documento117 pagineDiabetes Clinical Guidelines-V21.0 27.07.10Michelle WellsNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Case Presentation - DM (Tantsa Tamia)Documento58 pagineCase Presentation - DM (Tantsa Tamia)tantsaNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Principle Behind Special Collection Procedures, Special Supplies or EquipmentDocumento50 paginePrinciple Behind Special Collection Procedures, Special Supplies or EquipmentSofia JuliaNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- 6969 Lab ProtocolDocumento2 pagine6969 Lab ProtocolJohn CenaNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Mrs Nandhinidevi.M 04007180: Sid No. Patient ID 0400005449Documento2 pagineMrs Nandhinidevi.M 04007180: Sid No. Patient ID 040000544911F10 RUCHITA MAARANNessuna valutazione finora
- Insulin in Pregnancy: Dr. Kyar Nyo Soe Myint Consultant Endocrinologist University of Medicine 2, NOGTHDocumento39 pagineInsulin in Pregnancy: Dr. Kyar Nyo Soe Myint Consultant Endocrinologist University of Medicine 2, NOGTHYadanar KyawNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Fdocuments - in Metabolic Disorders of Pregnancy Gestational Disorders of Pregnancy GestationalDocumento42 pagineFdocuments - in Metabolic Disorders of Pregnancy Gestational Disorders of Pregnancy GestationalSoniya100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Type 1 DiabetesDocumento8 pagineType 1 DiabetesSam SyawallNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- AERGDocumento12 pagineAERGsupaidi97Nessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Blood Glucose Practical Handout For 2nd Year MBBSDocumento10 pagineBlood Glucose Practical Handout For 2nd Year MBBSIMDCBiochemNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Diabetes Guidelines FinalDocumento55 pagineDiabetes Guidelines FinalMocanu Cristina-VioricaNessuna valutazione finora
- Finals MCCCCNDocumento70 pagineFinals MCCCCNNaomi Anne AsuntoNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Gestational DiabetesDocumento37 pagineGestational DiabetesSm BadruddozaNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Exercise in DiabetesDocumento77 pagineExercise in DiabetesAkshay BangadNessuna valutazione finora
- Glucose Tolerance TestDocumento3 pagineGlucose Tolerance TestdechychyNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- PMLS Lec 5 7 FinalsDocumento13 paginePMLS Lec 5 7 FinalsEthel JerricaNessuna valutazione finora
- Ayuno Intermitente y Diabeticos 2Documento10 pagineAyuno Intermitente y Diabeticos 2vicenteNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Management of DiabetesDocumento164 pagineManagement of Diabetesvivek_win95Nessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Diabetes Mellitus Type 1 and 2Documento11 pagineDiabetes Mellitus Type 1 and 2Ibrar AliNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Gestational Diabetes Mellitus Case StudiesDocumento21 pagineGestational Diabetes Mellitus Case Studiesdiabetes asia100% (3)
- Study GuideDocumento8 pagineStudy GuideericNessuna valutazione finora
- Leicester Diabetes Diagnosis PathwayDocumento3 pagineLeicester Diabetes Diagnosis PathwayPaul MazziottaNessuna valutazione finora
- Glycosuria Diagnosis and TreatmentDocumento6 pagineGlycosuria Diagnosis and TreatmentMuthuvel ShanmugasundaramNessuna valutazione finora
- Diabetes Med Surg Questions 1Documento6 pagineDiabetes Med Surg Questions 1Trish Hồ0% (1)
- Gestational Diabetes MellitusDocumento3 pagineGestational Diabetes MellitusJustine DumaguinNessuna valutazione finora
- Diabetes Ferri 2019Documento12 pagineDiabetes Ferri 2019cochipinkNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Dm-Type-2 With Geno GramDocumento77 pagineDm-Type-2 With Geno GramRhajeeb Aennas SugalaNessuna valutazione finora
- Idf GDM Model of Care Implementation Protocol Guidelines For Healthcare ProfessionalsDocumento20 pagineIdf GDM Model of Care Implementation Protocol Guidelines For Healthcare Professionalsdiabetes asiaNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)