Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
44 Emergency First Presentation of Colorectal Cancer Predicts Significantly Poorer Outcomes A Review of 356 Consecutive Irish Patients
Caricato da
Joao FonsecaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
44 Emergency First Presentation of Colorectal Cancer Predicts Significantly Poorer Outcomes A Review of 356 Consecutive Irish Patients
Caricato da
Joao FonsecaCopyright:
Formati disponibili
ORIGINAL CONTRIBUTION
Emergency First Presentation of Colorectal
Cancer Predicts Significantly Poorer Outcomes:
A Review of 356 Consecutive Irish Patients
Gary Bass, M.B., B.Ch., B.A.O., M.Sc.1 & Cathy Fleming, M.Sc.2
John Conneely, B.Sc., M.B.A., M.R.C.S.I.1 & Zenia Martin, M.D., M.R.C.S.I.1
Kenneth Mealy, M.D., F.R.C.S.I.1
1 Department of Surgery, Wexford General Hospital, Wexford, Ireland
2 Clinical Trials Resource Unit, St. Luke’s Hospital, Dublin, Ireland
PURPOSE: Colorectal cancer commonly presents first as cancers diagnosed at endoscopy were first seen
an emergency and is likely to be complicated by bowel emergently. These data raise concerns regarding public
obstruction/perforation requiring more difficult awareness of colorectal cancer and resource allocation
procedures, with poorer outcomes. Analysis of all of and reemphasize the need for a national colorectal
the procedures performed on patients diagnosed in screening program.
Wexford General Hospital, Ireland, during the period
2000 to 2006 was carried out to validate this hypothesis in
our western European population. KEY WORDS: Colorectal neoplasms; Survival analysis;
Ireland; Surgical procedures; Elective; Emergency.
METHODS: Retrospective analysis of a prospectively
maintained database of patient demographics,
ancers of the colon and rectum remain the second
diagnosis, procedures, and mode of presentation (elective,
emergency) was undertaken.
RESULTS: A total of 356 patients with colorectal cancer
underwent 498 procedures during the years 2000 to 2006.
C most common malignancy among both males and
females, with an age-adjusted incidence in the Irish
population of 49.8/100,000, which is greater than in the
European Union or the United States.1 Ireland’s overall an-
Eighty-four emergency endoscopies and 100 emergency nual mortality rate for colorectal cancer is 16.6/100,000,
bowel resections were performed. Obstructive lesions 1.5 times the U.S. rate.1
were more likely to require emergency resection The initial diagnosis of colorectal cancer is commonly
(P G 0.001). Median survival time for patients treated made following admission in the emergency department
electively was 82 months vs. 59 months for patients (ED) for the management of symptomatic disease. Few
treated on an emergency basis. data are available for our western European population (a
CONCLUSIONS: Of all colonic resections, 34 percent were health care model different from that in which previous
carried out as emergencies and were significantly more studies were undertaken) regarding the incidence and out-
likely to be complicated by obstruction or perforation comes of patients who initially present with colorectal can-
(P G 0.001). Emergency resections were associated with a cer as an emergency.
significantly poorer perioperative mortality and five-year In the United States, retrospectively gathered admis-
survival rate (P G 0.001). Forty-one percent of colorectal sion data from the Connecticut Tumor Registry revealed
that 20 percent of the 11,023 patients diagnosed with co-
lorectal cancer between 1992 and 1996 were first admitted
Presented at the XXXIInd Sir Peter Freyer Lecture and Surgical to the hospital in the ED.2 Within this cohort, inpatient
Symposium, September 9 to 10, 2007, Galway, Ireland.
admission in an ED was significantly associated with older
Address of correspondence: Gary Bass, M.B., B.Ch., B.A.O., M.Sc., age and was a significant risk factor for more advanced
Department of Surgery, Wexford General Hospital, Wexford, Ireland. stage at diagnosis. A similar study from the United
Email: garbass@rcsi.ie Kingdom reported that 27 percent of their patients first
presented at the ED.3
Dis Colon Rectum 2009; 52: 678Y684
DOI: 10.1007/DCR.0b013e3181a1d8c9 In a smaller retrospective analysis of 102 patients di-
BThe ASCRS 2009 agnosed with colorectal cancer over a 2-year period in an
678 DISEASES OF THE COLON & RECTUM VOLUME 52: 4 (2009)
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
Diseases of the Colon & Rectum Volume 52: 4 (2009) 679
Irish catchment area, 41 percent of patients initially pres- right hemicolectomy, left hemicolectomy, subtotal colec-
ented to an ED, with the remainder attending the out- tomy, anterior/abdominoperineal resection). Sixteen mis-
patient department following referral by their general cellaneous follow-up procedures, such as the reversal of
practitioner.4 This percentage is substantially higher than Hartmann’s procedure or closure of other diverting en-
that reported in other populations,2,3 and thus we wanted terostomy, were excluded from the analysis. Survival was
to determine whether our data, a larger cohort from a calculated from the date of colonic resection until the
similar population, were comparable. date of death from any cause or the last recorded clini-
Using an extensive, single-institution cancer database, cal interaction.
we performed a comprehensive retrospective review of a
prospectively maintained dataset to examine the influence Histopathology
of mode of initial presentation primarily on outcome fol- Final histopathology reports confirmed the presence of a
lowing tumor resection (perioperatively and at 5 years), primary colorectal adenocarcinoma in each of the surgical
and then on tumor location, colonic obstruction or per- specimens included in this study. The anatomic location of
foration, histopathologic characteristics of the tumor, and the tumor and the presence or absence of bowel obstruc-
operative management. tion or perforation was extracted from the database. Pri-
mary tumor size was recorded as the largest diameter axis
through the sectioned specimen. Histologic grade was cate-
PATIENTS AND METHODS gorized into two groups for analysis: poor/undifferentiated
or moderate/well differentiated. A margin-negative
Patients, Mode of Presentation, and Interventions (R0) resection was determined as the absence of micro-
From January 2000 to December 2006, 356 consecutive scopic disease at the specimen resection margins. Total
patients underwent 498 procedures leading to a diagno- lymph node yield (the number of histologically positive
sis of colorectal cancer at Wexford General Hospital, a metastatic lymph nodes) and the presence of extramural
283-bed acute care hospital serving a predominantly rural vascular invasion within each surgical specimen were
catchment area of 131,615 people (Fig. 1). All of the pa- recorded. Cancer staging was based on pathologic findings
tients were identified from a prospectively accrued colo- in the sixth edition of the American Joint Committee on
rectal cancer database containing demographic, clinical, Cancer guidelines for colon and rectal cancer.5
operative, and pathologic data. All 6 consultant surgeons
operating at the hospital during the study period were in- Statistical Analyses
cluded; 2 surgeons accounted for 79 percent of the pro- Statistical analyses were performed with SPSS version
cedures performed. All of the procedures were codified at 15.0 for Windows (SPSS, Chicago, IL). Continuous vari-
the time of entry into the database as either elective or ables were expressed as median T standard deviation or
emergency. These procedures were identified as either di- mean T standard error of the mean and were compared
agnostic (colonoscopy, sigmoidoscopy, or examination un- using a 2-sample t-test. Categorical variables were com-
der anesthesia) or surgical resection (right and extended pared using a # 2 test, with Fisher’s exact test used where
appropriate. Survival probabilities for clinical, pathologic,
and treatment variables were estimated using the Kaplan-
Meier method6 and compared using a log-rank test. The
effect of type of first presentation on the size and stage
of the tumor, the presence of positive lymph nodes, and
extramural vascular invasion on survival were examined
using logistic regression, and optimal cutoffs were deter-
mined using the maximal # 2 method. Significant univar-
iate factors were included in a Cox proportional hazards
regression model to establish independent predictors of
survival. Further substratification analysis was performed
using the Mantel-Haenszel test.7 P values of less than 0.05
were considered statistically significant.
RESULTS
Demographics
The Wexford General Hospital colorectal database docu-
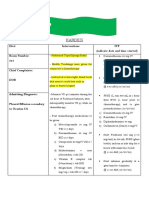
FIGURE 1. Time from first (diagnostic) elective endoscopy to
elective surgical resection. Vertical bar represents the median time ments 498 procedures on 356 patients with a diagnosis of
(15 days) from endoscopy to resection. colorectal carcinoma (Table 1). The median age of these
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
680 BASS ET AL: EMERGENCY VS. ELECTIVE BOWEL RESECTIONS FOR COLORECTAL CANCER
TABLE 1. Patient and procedure characteristics
Characteristics Elective Emergency Total
Total patients 356
Median age, yr (range) 69 72 71 (34Y95)
Sex 2:1 (M 9 F)
Male (% patients, by presentation) 133 (63.6) 81 (57) 217 (67)*
Female (% patients, by presentation) 76 (36.4) 61 (43) 139 (33)*
Endoscopies 120 (58%) 84 (42%) 204
All operations 187 (67%) 91 (33%) 278
Right hemicolectomy 55 (58.5%) 39 (41.5%) 94
Left hemicolectomy 48 (58.5%) 34 (41.5%) 82
Subtotal colectomy 2 (22.2%) 7 (77.8%) 9
Anterior/Abdominoperineal resection 84 (90.3%) 9 (9.7%) 93
*Procedures on three male and two female patients were not codified as either Elective or Emergency on data entry and thus treated as Missing data during analysis.
patients was 71 (range, 34Y95) years; the median age of annum was 68 T 12 (42 T 7.4 elective, 28 T 4.9
elective attendees was 69 (range, 34Y95) years, and the me- emergency). Resection of left colon and rectal tumors
dian age of emergency presentations was 72 (range, 37Y94) (via left hemicolectomy, anterior resection, or abdomi-
years, however, this difference was not significant (P = noperineal resection) accounted for 187 (67 percent)
0.643). Of the total number of patients, 217 (67 percent) surgical interventions. Transverse and right-sided tumors
were male and 107 (33 percent) were female; this 2:1 ratio accounted for the remainder of cases (right and extended
was unaffected by mode of presentation (P = 0.182). right hemicolectomy = 55 elective, 39 emergency; subtotal
colectomy = 2 elective, 7 emergency cases). Anterior and
Procedures Performed abdominoperineal resections were significantly more likely
During the study period, 204 diagnostic endoscopies were to be carried out in the elective setting (P G 0.001), whereas
performed when there was a clinical suspicion of colorectal emergency bowel resections almost entirely comprised
cancer. Of these, 120 (58 percent) were performed on 39 right (43 percent) and 32 left hemicolectomies (35
elective lists and 84 (42 percent) were performed on an percent; P = NS).
emergency basis. Operative management studied 110 of the The indication for bowel resection was analyzed by mode
120 elective endoscopies (92 percent), with a median time of presentation. Bowel resection uncomplicated by obs-
from diagnosis to surgical intervention of 15 T 3.8 days. truction or perforation was significantly more likely to take
Surgeons performed 278 bowel resections for colo- place on an elective operative list (170 vs. 32; P G 0.001).
rectal cancer during the study period (Table 1). Of these, Colorectal cancers complicated by bowel obstruction (55
187 (67 percent) were performed on elective lists and 91 emergency vs. 12 elective resections; P G 0.001) or perfora-
(33 percent) were catalogued as emergency cases. The tion (8 emergency vs. 3 elective resections; P G 0.001) were
median number of bowel resections performed per significantly more likely to require emergency resection.
TABLE 2. Tumor characteristics
Tumor stage
T1 7/196 (3.5%) 1/92 (1%) 8/288 (3%)
T2 45/196 (23%) 6/92 (6%) 51/288 (18%)
T3 118/196 (60%) 50/92 (54%) 168/288 (58%)
T4 26/196 (13%) 35/92 (38%) 61/288 (21%)
Histologic grade
Well/moderately well differentiated 185/196 (94%) 88/92 (96%)
Poorly/undifferentiated 11/196 (6%) 4/92 (4%)
Nodal status
Negative (N0) 120/195 (61%) 38/92 (41%)
Positive (N1) 53/195 (27%) 38/92 (41%)
Positive (N2) 22/195 (11%) 16/92 (17%)
Extramural lymphovascular invasion
Present 12/196 (6%) 4/92 (4%)
Absent 184/196 (93%) 88/92 (95%)
Resection margin status
Negative/total specimens (%) 202/204 (99) 84/93 (90)
Positive/total specimens (%) 2/204 (1) 9/93 (10)
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
Diseases of the Colon & Rectum Volume 52: 4 (2009) 681
Tumor Characteristics Survival Analysis
Histologic examination was carried out on all of the re- Survival analysis by the Kaplan-Meier method (Fig. 2)
sected specimens. Ninety-four percent (185/196) of elective demonstrated a significant survival advantage for patients
specimens were graded ‘‘well or moderately differenti- treated electively compared with those treated emergently
ated’’, and 6 percent (11) of specimens were graded (P G 0.001). The median survival time for patients treated
‘‘poorly or undifferentiated’’ (Table 2). Of all emergency electively was 82 months in comparison to 59 months for
resection specimens, 95 percent (88/92) were graded ‘‘well those treated on an emergency basis. Twelve patients died
or moderately differentiated’’ and 5 percent (4/92) were in the immediate postoperative period; 92 percent (11/12)
graded ‘‘poorly or undifferentiated’’. There was no sig- following emergency resection, and 8 percent (1/12) after
nificant difference in cellular differentiation between elec- an elective operation.
tive and emergency resection specimens (P = 0.653). A multivariate Cox regression was performed with the
The incidence of T1 or T2 stage tumors in electively covariates of type of procedure, presence of complication
resected specimens was 27 percent (52/196), compared (obstruction or perforation), margin status, T stage, N status,
with 8 percent (7/92) in emergency resections. T3 and histologic grade, and presence of ELVI (Table 3). Three of
T4 tumors accounted for 73 percent (144/196) in elective these variables were found to be independent predictors of
resection cases and 92 percent (85/92) in emergency re- outcome. Subtotal colectomy was associated with a poorer
section cases; the proportion of later stage tumors was sig- outcome (hazard ratio [HR] = 6.239; 95 percent confidence
nificantly greater in emergency resection compared with interval [CI] = 1.645Y23.664; P = 0.007). Both uncompli-
those performed electively (P = 0.001). cated carcinoma (HR = 0.234; 95 percent CI =
Macroscopic and microscopic R0 resection was 0.082Y0.671; P = 0.007) and the absence of ELVI (HR =
achieved in 96 percent of all cases (286/297). Only 1 percent 0.370; 95 percent CI = 0.168Y0.815; P = 0.014) were
(2/202) of specimens from elective resections showed evi- independently associated with better outcomes.
dence of tumor at the surgical margin compared with
10 percent (9/93) of emergency resections (P = 0.001).
In patients who underwent elective resection, 39 per- DISCUSSION
cent (75/195) of lymph nodes were involved by tumor (N1 In our experience, patients diagnosed with colorectal cancer
or N2), compared with 59 percent (54/92) of nodes har- who first present to the ED represent a large proportion of all
vested from emergency patients (P = 0.002). Extramural patients undergoing colon resection for primary malignancy.
lymphovascular invasion (ELVI) was noted in 6 percent Indeed, 33 percent of patients in our study first presented at
(12/196) of elective specimens and 20 percent (19/92) of the ED rather than by referral to an outpatient clinic.
emergency specimens, and this difference was found to be This figure compares to 20 percent in a U.S. popula-
significant (P G 0.001) when the Mantel-Haenszel test to tion,2 27 percent in the United Kingdom,3 and 41 percent
control for tumor stage was applied.7 in a smaller study in a rural, western Ireland population.4
The American data are surprisingly low when it is con-
sidered that admission data, not operations, were recorded.
Inpatient admissions data are inadequate surrogates for
rates of surgical intervention and may include patients with
disseminated disease for whom operative management was
not indicated.2Y4 Our data, however, represent all cases of
disease amenable to curative resection in our center during
the study period.
Manning et al.4 argued that the large proportion of
emergency first presentation in colorectal cancer in their
rural Irish population can be explained by an ignorance of
the symptoms associated with the disease. They report that
just 27 percent of 350 patients surveyed at an outpatient
clinic could name a symptom associated with ‘‘bowel can-
cer,’’ compared with 53 percent for ‘‘lung cancer’’ and
72 percent for ‘‘breast cancer.’’ It is likely, given the small
population of the country (4.3 million) and nationwide
public information campaigns, that similar rates of symp-
tom awareness would be found in our population.
The sex ratio (2:1 male to female) and age distribution
FIGURE 2. Annual number of patients requiring elective or
emergency large bowel resection for colorectal carcinoma per year (median age, 71 years) of the 356 patients in our series are
during the study period January 2000 to December 2006. similar to those seen in other studies in Ireland,4 the United
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
682 BASS ET AL: EMERGENCY VS. ELECTIVE BOWEL RESECTIONS FOR COLORECTAL CANCER
TABLE 3. Multivariate analysis of predictors* of survival after colorectal resection
Risk Factor Hazard ratio 95% confidence interval P
Uncomplicated colorectal carcinoma 0.234 0.082Y0.671 0.007
Subtotal colectomy 6.239 1.645Y23.664 0.007
No extramural lymphovascular invasion 0.370 0.168Y0.815 0.014
*Cox proportional hazards regression model (included in multivariate analysis: type of procedure, pathology, T stage, N stage, histologic grade, margin status, and presence
of ELVI).
Kingdom,8Y12 the United States,13Y15 and elsewhere.16,17 rather than the mean, is the appropriate statistical mea-
Diggs et al.18 showed that two-thirds of patients discharged sure because the data were not normally distributed;
following colorectal cancer resections were for those older instead they broadly describe early intervention in the
than 65 years, with the oldest age group (Q85 years) majority of cases, with a small cohort of late operation in
undergoing more emergency colorectal cancer resections. patients undergoing cytoreductive neoadjuvant chemo-
Rabeneck et al.19 reported a small majority of male patients therapy or radiotherapy at other specialist centers before
(53.5 percent), but again most patients were 50 years or definitive operative management.
older. In our population, there was no significant difference Anterior and abdominoperineal resections were sig-
in median age at presentation (P = 0.643) or sex ratio (P = nificantly more likely to be carried out in an elective set-
0.182) when comparing elective and emergency groups; ting, whereas operations for right-sided and left-sided
however, perioperative mortality in our patients was tumors were performed both in the elective and emer-
associated with increased age. The median age of patients gency settings (Table 1). Emergency bowel resection for
who died in the postoperative period was 79.5 years colorectal cancer was significantly more likely in our
(range, 65Y94 years; n = 12), compared with the median study to be complicated by bowel obstruction (P G 0.001).
age of 71 years across all groups; this difference was This finding may be influenced by the symptomatic na-
statistically significant (P = 0.04). ture of a presentation of this type, increasing the likeli-
On examination, our database did not contain a record hood that a patient would seek urgent medical attention.9
of subsequent bowel resection for colorectal carcinoma in Disease resected under emergency circumstances is also
any patient who underwent primary resection of his or her more likely to be of greater bulk, higher histologic grade,
disease; however, this information is a poor surrogate for and exhibit ELVI. Alvarez et al.22 have ascribed symptom-
incidence of recurrent disease in our population. Given the atic emergency presentation to obstruction and perfora-
nature of data collection in this study (retrospective tion. This association is not absolute because a number of
extraction and analysis of a prospectively entered database investigators have demonstrated no correlation in their
of surgical interventions, based on the Lothian Surgical Audit populations between the duration of symptoms before the
System), information on recurrence would only have been first presentation and pathologic staging.16,20,21 It is
codified in our database if a patient in the cohort had intuitive that mechanically obstructing colorectal cancer
undergone repeat colonic or rectal resection in our center. tends to present at a more advanced histologic stage when
The patterns of recurrence in patients resected with curative the tumor (often an annular lesion) is of sufficient bulk
intent in the elective and emergency settings is an interesting to prevent the passage of feces. Patients with obstructing
clinical question which, although not answerable in the tumors have been found to have a lower probability of
present study, merits serious consideration and further work. survival than patients with nonobstructing lesions be-
Of the diagnostic endoscopies carried out during the cause there is higher risk of lymph node positivity, ELVI
study period, 42 percent were performed on an emer- (likely to be related to the high T stage, as demonstrated in
gency basis. Because of the finite nature of resources, both our data and elsewhere), and metastatic tumor recurrence
in terms of equipment and personnel, there is a consid- but not a higher local recurrence rate in such patients.
erable waiting list for access to elective colonoscopy at our Perforation may occur within the friable tumor because of
institution, and the volume of emergency cases seen in necrosis or adjacent inflammatory changes or proximal to
our population further affects the length of this list. This an obstructing tumor because of increasing hydrostatic
is the published experience of many correspondents, es- pressure and distension obeying the law of Laplace. The
pecially those who practice in the United Kingdom, and poorer outcome following perforation is thought to be the
emphasizes the need to establish a national endoscopic result of the cumulative effect of fecal peritonitis and ma-
screening program.4,9,12,18,20,21 lignancy, along with the combination of preexisting co-
The median time from diagnosis of colorectal car- morbidity and a grossly disturbed pathophysiology.
cinoma following an elective diagnostic endoscopy to sur- Tumor size, tumor differentiation, surgical margin status,
gical intervention was 16 days (Fig. 1). The median time, extramural vascular invasion, and lymph node status are
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
Diseases of the Colon & Rectum Volume 52: 4 (2009) 683
among the clinicopathologic features that have been identi- which no comparison could be made because no T1 tu-
fied that predict survival following resection for colorectal mors were resected in the emergency group.
adenocarcinoma.23,24 Pathologic analysis by Burton et al.24 On multivariate analysis (Table 3), 3 variables were
of 445 colonic tumor and rectal tumor specimens retrieved found to be independent indicators of survival probabil-
during elective and emergency operations demonstrated that ity: subtotal colectomy (poorer outcome), uncomplicated
T4, N2, and poorly differentiated tumors (themselves carcinoma, and the absence of ELVI (both associated
indicators of poor outcome) were more likely to present first with improved outcome). A similar study by Rabeneck
in an emergency. Retrieval of an appropriate number of et al.19 found older age, site proximal to the rectum, co-
lymph nodes is important in staging colorectal cancer.25 A morbidities, and lack of primary care to be independently
number of groups have demonstrated that the ratio of the associated, on multivariate analysis, with emergency
number of metastatic lymph nodes to the number of admission.
examined lymph nodes (lymph node ratio, LNR) is an in- Diggs et al.18 found a significant association between
dependent prognostic factor for overall survival, with a de- insurance status and emergency presentation. Although
creasing LNR correlating with a longer overall survival.25,26 the United States health care system is different from the
Because the histopathology reports on the patients in our Irish system, this finding supports the idea that the ac-
series did not report the number of nodes examined, it was cessibility of primary health care leads to a reduction in
not possible to perform the LNR calculation. emergency presentations. They also showed that patients
As may be expected, a significantly greater number of requiring emergency surgery had a mean predicted length
higher grade tumors occurred in patients who presented of stay that was 4 days longer than that of nonemergency
in an emergency (P = 0.001). These high-grade tumors patients with an excess cost of US$19,073. It is calculated
were more likely to be node positive (P G 0.001) and that this placed an excess burden on the health care sys-
demonstrate ELVI (P = 0.009), but they did not have a tem of 54,979 hospital days and more than $250 million
greater frequency of positive resection margins (P = 0.08). in hospital charges in 2002.18
In several large studies from the United States and We have demonstrated more advanced disease in pa-
the United Kingdom, poorer outcomes were identified in tients who underwent emergency resection of their pri-
patients with colorectal cancer who initially presented as mary colorectal tumors in comparison with patients who
emergency cases. However, the mode of initial presenta- had elective surgery. These patients experienced sig-
tion and its effect on all-cause mortality have not been nificantly poorer outcomes both perioperatively and at
characterized for the Irish population. In a large retro- five years compared with nonemergent counterparts.
spective analysis of 3200 patients who underwent large Because many patients present without symptoms but
bowel resection in Scotland between 1991 and 1994, the rather because of serendipitous ad hoc screening by their
HR for crude overall 5-year survival was 1.68 for patients primary care physician,3,9 it seems reasonable and cost-
who underwent emergency operations compared with effective18 to consider a national screening program for
those who were operated on electively, whereas the HR colorectal carcinoma in our at-risk population.
for cancer-specific 5-year survival was 1.90 for emergency
vs. elective presentation.27 It has been argued that
the negative impact of emergency procedures is confined ACKNOWLEDGMENTS
to the immediate postoperative period and probably cor-
relate with the acute medical pathology in these pa- The authors thank Ms. Margaret Murphy, stoma care nurse
tients.14,17 Mortality in the perioperative period (n = 12) specialist, for assistance in collating the pathologic data herein,
was associated with emergency surgery for obstruction or and Mr. Ezzat Tadros, M.D., F.R.C.S.I., and the late Mr. John
perforation. All 12 resections were performed for colo- Bosco O’Mahony, M.D., M.R.C.P., F.R.C.S.I., consultant sur-
rectal carcinoma that was complicated: 50 percent (6/12) geons, for access to the Wexford Colorectal Database.
of patients presented with large bowel obstruction, 25
percent (3/12) had perforated large bowel, and 25 percent
(3/12) had another unspecified complication, such as REFERENCES
bleeding or infection. However, our data demonstrate a
poorer patient survival at 5 years following emergency 1. Campo J, Comber H, Gavin A. All-Ireland Cancer Statistics
1998Y2000. Cork, Ireland: National Cancer Registry & Northern
resection in excess of the effect of greater perioperative
Ireland Cancer Registry; 2004.
mortality associated with emergency surgery (Fig. 2). Sur- 2. Polednak AP. Inpatient hospital admission through an emer-
vival analysis demonstrated poorer outcomes for emer- gency department in relation to stage at diagnosis of colorectal
gency operations compared with elective operations both cancer. Cancer Detect Prev 2000;24:283Y9.
overall and after substratification of the data for T stage, 3. Bevis PM, Donaldson OW, Card M, et al. The association be-
nodal status, and ELVI; the difference was significant in tween referral source and stage of disease in patients with colo-
each case (P G 0.001), with the exception of T1 disease, in rectal cancer. Colorectal Dis 2008;10:58Y62.
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
684 BASS ET AL: EMERGENCY VS. ELECTIVE BOWEL RESECTIONS FOR COLORECTAL CANCER
4. Manning AT, Waldron R, Barry K. Poor awareness of colo- 17. Coco C, Verbo A, Manno A, et al. Impact of emergency sur-
rectal cancer symptoms; a preventable cause of emergency and gery in the outcome of rectal and left colon carcinoma. World
late stage presentation. Ir J Med Sci 2006;175:55Y7. J Surg 2005;29:1458Y64.
5. Greene FL, Page DL, Fleming ID, et al. AJCC Cancer Staging 18. Diggs JC, Xu F, Diaz M, et al. Failure to screen: predictors and
Manual. 6th ed. New York: Springer, 2003. burden of emergency colorectal cancer resection. Am J Manag
6. Kaplan E, Meier P. Nonparametric estimation from incom- Care 2007;13:157Y64.
plete observations. Am Stat Assoc J 1958;22:457Y81. 19. Rabeneck L, Paszat LF, Li C. Risk factors for obstruction,
7. Mantel N, Haenszel W. Statistical aspects of the analysis of perforation, or emergency admission at presentation in pa-
data from retrospective studies of disease. J Natl Cancer Inst tients with colorectal cancer: a population-based study. Am J
1959;22:719Y48. Gastroenterol 2006;101:1098Y103.
8. Greig JD, Thomson WO. Colorectal carcinoma: presentation and 20. Chohan DP, Goodwin K, Wilkinson S, et al. How has the
management in a general hospital. Scott Med J 1988;33:263Y7. Ftwo-week wait’ rule affected the presentation of colorectal
9. Khattak I, Eardley NJ, Rooney PS. Colorectal cancerVa cancer? Colorectal Dis 2005;7:450Y3.
prospective evaluation of symptom duration and GP referral 21. Kiran PR, Glass RE. Duration of symptoms and spread of
patterns in an inner city teaching hospital. Colorectal Dis 2006; colorectal cancer: a short history does not mean early disease.
8:518Y21. Ann R Coll Surg Engl 2002;84:381Y5.
10. Mealy K, Salman A, Arthur G. Definitive one-stage emergency 22. Alvarez JA, Baldonedo RF, Bear IG, et al. Presentation, treat-
large bowel surgery. Br J Surg 1988;75:1216Y9. ment, and multivariate analysis of risk factors for obstructive and
11. Waldron RP, Donovan IA, Drumm J, et al. Emergency perforative colorectal carcinoma. Am J Surg 2005;190:376Y82.
presentation and mortality from colorectal cancer in the 23. Olsson L, Bergkvist L, Ekbom A. Symptom duration versus
elderly. Br J Surg 1986;73:214Y6. survival in non-emergency colorectal cancer. Scand J Gastro-
12. Tan E, Tilney H, Thompson M, et al. The United Kingdom enterol 2004;39:252Y8.
National Bowel Cancer Project: epidemiology and surgical risk 24. Burton S, Norman AR, Brown G, et al. Predictive poor prog-
in the elderly. Eur J Cancer 2007;43:2285Y94. nostic factors in colonic carcinoma. Surg Oncol 2006;15:71Y8.
13. Cuffy M, Abir F, Audisio RA, Longo WE. Colorectal cancer 25. Aarons CB, Lamorte WW, Sentovich SM. Lymph node
presenting as surgical emergencies. Surg Oncol 2004;13:149Y57. retrieval and assessment after colorectal cancer resection: are
14. Smothers L, Hynan L, Fleming J, et al. Emergency surgery for pathologists doing an adequate job? Dis Colon Rectum. E-pub
colon carcinoma. Dis Colon Rectum 2003;46:24Y30. 2008 Jun 7 [Retracted].
15. Mitchell AD, Inglis KM, Murdoch JM, Porter GA. Emergency 26. Edler D, Ohrling K, Hallstrom M, et al. The number of
room presentation of colorectal cancer: a consecutive cohort analyzed lymph nodes: a prognostic factor in colorectal cancer.
study. Ann Surg Oncol 2007;14:1099Y104. Acta Oncol 2007;46:975Y81.
16. Pescatori M, Maria G, Beltrani B, Mattana C. Site, emergency, 27. McArdle CS, Hole DJ. Emergency presentation of colorectal can-
and duration of symptoms in the prognosis of colorectal can- cer is associated with poor 5-year survival. Br J Surg 2004;91:
cer. Dis Colon Rectum 1982;25:33Y40. 605Y9.
Copyright @ The ASCRS 2009. Unauthorized reproduction of this article is prohibited.
Potrebbero piacerti anche
- Shoulder-Pad Sign of Amyloidosis: Structure of An Ig Kappa III ProteinDocumento5 pagineShoulder-Pad Sign of Amyloidosis: Structure of An Ig Kappa III ProteinJoao FonsecaNessuna valutazione finora
- 26 Short-Term Outcomes Following The Use of Self-Expanding Metallic Stents in Acute Malignant Colonic Obstruction e A Single Centre ExperienceDocumento5 pagine26 Short-Term Outcomes Following The Use of Self-Expanding Metallic Stents in Acute Malignant Colonic Obstruction e A Single Centre ExperienceJoao FonsecaNessuna valutazione finora
- 50 Postoperative Mortality and Morbidity in Older Patients Undergoing Emergency Right Hemicolectomy For Colon CancerDocumento6 pagine50 Postoperative Mortality and Morbidity in Older Patients Undergoing Emergency Right Hemicolectomy For Colon CancerJoao FonsecaNessuna valutazione finora
- Principlesofhemodialysisfinal2017 171216103708 PDFDocumento53 paginePrinciplesofhemodialysisfinal2017 171216103708 PDFJoao FonsecaNessuna valutazione finora
- Journal Pone 0031932Documento9 pagineJournal Pone 0031932Joao FonsecaNessuna valutazione finora
- The MD Anderson Surgical OncologyDocumento1.160 pagineThe MD Anderson Surgical OncologyJoao Fonseca100% (4)
- Famous Discoveries by Medical StudentsansDocumento8 pagineFamous Discoveries by Medical StudentsansJoao FonsecaNessuna valutazione finora
- Package Meta': June 7, 2018Documento160 paginePackage Meta': June 7, 2018Joao FonsecaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- RFP 19-23 Addendum 3 Closing Date and Additional DataDocumento75 pagineRFP 19-23 Addendum 3 Closing Date and Additional DatagarbagepatchNessuna valutazione finora
- Malignancy Yield of Testis PathologyDocumento7 pagineMalignancy Yield of Testis PathologyadolfoNessuna valutazione finora
- Cancer Statistics, 2011: The Impact of Eliminating Socioeconomic and Racial Disparities On Premature Cancer DeathsDocumento25 pagineCancer Statistics, 2011: The Impact of Eliminating Socioeconomic and Racial Disparities On Premature Cancer DeathshamzaloNessuna valutazione finora
- Costa (2010) - Horizons in Neuroscience ResearchDocumento452 pagineCosta (2010) - Horizons in Neuroscience Researchjonas1808Nessuna valutazione finora
- AcromegalyDocumento14 pagineAcromegalyapi-312256950Nessuna valutazione finora
- Chocolate AnalysisDocumento8 pagineChocolate AnalysisCartoons HDNessuna valutazione finora
- Dosimetric Evaluation of PlansDocumento8 pagineDosimetric Evaluation of PlansQuang-Vu TranNessuna valutazione finora
- PREVENTION OF SUBSTANCE USE AND ABUSE CigarettesDocumento70 paginePREVENTION OF SUBSTANCE USE AND ABUSE CigarettesDor Lenn100% (1)
- Agreement and Thesis Proposal ArnelDocumento5 pagineAgreement and Thesis Proposal ArnelarnelNessuna valutazione finora
- Asimen Ent600Documento30 pagineAsimen Ent600MZZNessuna valutazione finora
- Drinking Water in The MorningDocumento4 pagineDrinking Water in The MorningLuiz Almeida100% (1)
- Multiple MyelomaDocumento2 pagineMultiple MyelomaKolin JandocNessuna valutazione finora
- Euthenics, Report, Maternal and ChildDocumento88 pagineEuthenics, Report, Maternal and ChildJoy JarinNessuna valutazione finora
- ASiT Yearbook 2010, Association of Surgeons in Training PDFDocumento131 pagineASiT Yearbook 2010, Association of Surgeons in Training PDFEd FitzgeraldNessuna valutazione finora
- Pathologic Calcification: Dr. Deepak K. GuptaDocumento25 paginePathologic Calcification: Dr. Deepak K. Guptaاحمد زيد سعيد100% (1)
- Garcinia Kola ThesisDocumento36 pagineGarcinia Kola ThesisDdn RmaNessuna valutazione finora
- The Differential Cell CountDocumento12 pagineThe Differential Cell Countariel100% (1)
- (Hong Et Al 2012) Effects of Fermented Black Soybean Pulp On Lipid and Bone Metabolism in Ovariectomized RatsDocumento7 pagine(Hong Et Al 2012) Effects of Fermented Black Soybean Pulp On Lipid and Bone Metabolism in Ovariectomized RatsSie ningsihNessuna valutazione finora
- Essay ExploratoryDocumento6 pagineEssay Exploratoryapi-240678482Nessuna valutazione finora
- 5th MOSCON Agenda 1012Documento4 pagine5th MOSCON Agenda 1012drgarimaguptaNessuna valutazione finora
- Ami Ashariati - Immunotherapy in CancerDocumento142 pagineAmi Ashariati - Immunotherapy in CancersarijuicyNessuna valutazione finora
- JSS MoUDocumento88 pagineJSS MoUchetanhiremathNessuna valutazione finora
- Breast-Spanish HASTSA 199Documento252 pagineBreast-Spanish HASTSA 199Ely SalazarNessuna valutazione finora
- Kardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313Documento2 pagineKardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313kuro hanabusaNessuna valutazione finora
- Clinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFDocumento41 pagineClinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFVali MocanuNessuna valutazione finora
- Stem Cell BasicsDocumento73 pagineStem Cell BasicsrosesamanthaNessuna valutazione finora
- Exploring Medical Language A Student Directed Approach 8th Edition Brooks Test BankDocumento16 pagineExploring Medical Language A Student Directed Approach 8th Edition Brooks Test BankAnneMuellerqcigf100% (12)
- Surgery Case PresentationDocumento40 pagineSurgery Case PresentationSalsabila Al-Basheer0% (2)
- Viral Hepatitis: by Shalini Hazael, Group 40aDocumento24 pagineViral Hepatitis: by Shalini Hazael, Group 40aAiman TymerNessuna valutazione finora
- Physiology of The PancreasDocumento4 paginePhysiology of The PancreasClayton VerBerkmösNessuna valutazione finora