Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Respiratory Function Following Onpump Versus Offpump Coronary Bypass Grafting Surgery
Caricato da
Shira michaelCopyright
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Respiratory Function Following Onpump Versus Offpump Coronary Bypass Grafting Surgery
Caricato da
Shira michaelCopyright:
RESEARCH
Respiratory function following
on-Pump versus off-pump
coronary bypass grafting surgery
Objective: Respiratory dysfunction is a very common postoperative complication that occurs after cardiac surgery.
Among the suggested causes is cardiopulmonary bypass. We compared the effect of on-pumpcoronary artery bypass
grafting (ONCABG) versus off-pumpcoronary arterybypass grafting (OPCABG) on postoperative respiratory function.
Methods: Patients were prospectively divided into two groups ONCABG and OPCABG, (n=100 in each). Respiratory
variables (Pao2, Paco2, Sao2, and Pao2/Fio2 ratio) were measured prior to induction of anaesthesia then at seven time
points (ICU admission, postoperative hours 1, 3, 6, 12, 18, and 24). Time to extubation, rates of reintubation, and use of
noninvasive ventilation (NIV) were also evaluated.
Results: Baseline preoperative arterial blood gases and alveolar/arterial oxygen pressure gradients were similar in both
groups. Postoperatively, all values were significantly higher in the OPCABG group only at ICU admission (p<0.05). No
differences were seen in time to extubation, rate of reintubation rate, and use of postoperative NIV.
Conclusion: There is a slightly less incidence of lung injury with OPCABG as compared to ONCABG in low-risk patients
especially in the early postoperative period.
Keywords: cardiac surgery, coronary bypass grafting, postoperative complications, respiratory function, PaO2/
FIO2 ratio, arterial blood gas
Introduction some of the perioperative complications
Mohamed Ali Bakry*1,
Respiratory dysfunction is a common and that may be related to the use of CPB [8].
Mohamed Elhassaini
well recognized postoperative complication There is growing evidence to support Abdelghafar Yousef2
that occurs early after open heart surgery better outcomes and lower risk of occurrence & Hisham Mohamed
[1]. It is associated with high mortality rates of complications with the use of OPCABG as Mohamed Salem2
and manifests as decreased arterial oxygen opposed to the standard on-pumpcoronary
partial pressure, atelectasis, pulmonary artery bypass grafting (ONCABG) technique 1
Department of Anesthesiology,
Faculty of Medicine, Cairo University,
oedema, pleural effusion, pneumonia [2] or [3,8-18]. Most of these studies however 2
Department of Anesthesia, Research
adult respiratory distress syndromeand may did not perform a detailed analysis of gas Institute of Ophthalmology, Egypt
persist over the first days after surgery [3]. exchanges after coronary artery bypass
*Author for correspondence:
The main causes for occurrence of respiratory grafting (CABG). In the current study we
complications are the effects of sternotomy, aimed to compare the effects of OPCABG and mab628@kasralainy.edu.eg
internal mammary artery harvesting, ONCABG on pulmonary gas exchange using
pulmonary ischemia with subsequent controlled assessment of arterialo2 pressure
reperfusion, as well as the inflammatory (Pao2), arterial carbon dioxide pressure
reaction caused by cardiopulmonary bypass (Paco2), arterial O2 saturation (SaO2) and
(CPB) [1]. The risk of occurrence increases ratio of arterial oxygen partial pressure to
depending on several elements, including fractional inspired oxygen (PaO2/FiO2) over
preoperative lung function [5] and smoking the course of the first 24 hours following
history [6], as well as intraoperative factors elective CABG surgery.
such as lung collapse during CPB [7]. The
off-pump coronary artery bypass grafting Methods
(OPCABG) technique has been developed Participants
with the aim of avoiding or at least reducing 200 patients aged between 30-70 years
785 Clin. Pract. (2018) 15(4), 785-791 ISSN 2044-9038
Mohamed Ali Bakry
RESEARCH
who underwent primary elective isolated synchronized intermittent mandatory
CABG between 2014-2016 were enrolled in ventilation + pressure support modality,
this study. with a default PEEP of 5 cm H2O and tidal
volumes kept in the range of 6 to 8 mL/kg of
Exclusion criteria ideal body weight.
(a) patients undergoing emergency Data collected
CABG, (b) patients with acute or chronic
I. Baseline data: (1) demographics: age,
lung disease(c)patients with depressed
sex, height, weight, and body mass index
left ventricular function (ejection fraction
(BMI); (2) preoperative status: diabetes,
<40%) (d) patients who had smoked in the
hypertension, hypercholesterolemia,
preceding 6 months, (e) patients returning
smoking history, creatinine, left
to the operating room within the first 24
ventricular (LV) and right ventricular (RV)
hours, (f ) patients with moderate and/or
systolic function, especially the LV systolic
severe liver disease and (g) patients with
function which was classified according
preoperative organ support as defined by:
to the ejection fraction as good (>55%),
(i) mechanical (intra-aortic balloon-pump
mildly impaired (46%-55%), moderately
[IABP]) or pharmacological hemodynamic
impaired (36%-45%), or severely impaired
support, (ii) renal support with any form
(<35%); and (4) baseline arterial blood
of renal replacement therapy, and (ii)
gas analyses while the subjects were
respiratory support with invasive or
breathing room air spontaneously prior
noninvasive ventilation (NIV).
to induction of anesthesia.
The patients were randomly divided
II. Operative data: including operating and
according to the use of intraoperative
total intubation time and total hospital
CPB into Group A (ONCABG) and Group B stay.
(OPCABG). Each group included 100 patients.
III. Postoperative data: (1) arterial oxygen
The study was approved by the local tension (PaO2), (2) carbon dioxide tension
ethics committee and informed written (PaCO2);(3) arterial O2 saturation (SaO2);
consent was obtained from each patient. (4)ratio of arterial oxygen partial pressure
Operative details to fractional inspired oxygen (PaO2/FiO2)
(5)time to extubation and need for early
Surgery was carried out through a reintubation (within the first 24 hours)
median sternotomy. The standard cardiac and (6) use of any form of noninvasive
anesthesia protocol used in our center was ventilation support NIV support after
implemented. This entailed induction by extubation within the first 24 hours.
midazolum and fentanyl or propofol and These parameters were collected at
fentanyl with pancuronium bromide 0.1 mg/ seven time points: time of admission to
Kg as the muscle relaxant. Maintenance of the ICU and at postoperative hours 1, 3,
anesthesia was by volatile agents (isoflurane) 6, 12, 18, and 24.
and the mechanical ventilation settings
were: tidal volume 5 ml/kg and respiratory Statistical Analysis
rate 12 bpm. Analgesia was maintained Descriptive statistical analysis was used
using fentanyl boluses if needed. and the results are presented as mean ±
SD. The t test was used for comparison of
In group A (on-pump; ONCABG) surgery continuous variables between the two
was carried out using CPB with aortic cross
groups and the Chi-square test or the
clamping and cardioplegic arrest. Patients
Fisher’s exact test was used for categorical
were disconnected from the ventilator
variables.Pearson’s correlation was used to
during the procedure. In group B (off-pump;
explore relationships between quantitative
OPCABG) surgery was carried out using the
variables.A two-sided P < 0.05 was
commercially available coronary stabilizers
considered significant for all comparisons.
[4].
After the surgery, in the intensive care Results
unit (ICU), the ventilator was set at the As demonstrated in TABLE 1, there were
786 10.4172/clinical-practice.1000410 Clin. Pract. (2018) 15(4)
Respiratory function following on-Pump versus off-pump coronary bypass
grafting surgery RESEARCH
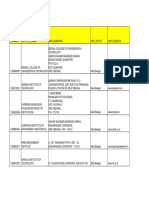
Table 1. Demographic and clinical characteristics of critically ill elderly patients (N=154).
Group A: ONCABG Group B: OPCABG
Characteristic
(n = 100) (n = 100)
Age (year) 60.1 ± 11.5 59.8 ± 12.6
Gender M/F 78/22 84/16
Height (cm) 170.6 ± 5.9 168.4 ± 7.3
Weight (kg) 83.6 ± 11.5 79.4 ± 9.7
Demographics BMI (kg/m2) 29.1 ± 4.0 28.3 ± 3.8
and Baseline
parameters Hypertension (%) 76.1 74.9
Creatinine (µmol/L) 90.1 ± 8.6 94.6 ± 7.2
Hypercholestrolemia (%) 87.9 88.8
Diabetes (%) 57.6 62.0
Former smoker (%) 64 71
Good RV systolic function (%) 92.6 91.8
Good LV systolic function (%) 87.9 89.3
Ejection fraction (%) 58.6 ± 9.3 60.6 ± 8.1
PaO2 (mmHg) 83.5 ± 20.1 82.6 ± 21.9
Preoperative PaCO2 (mmHg) 36.4 ± 4.5 39.6 ± 3.4
Respiratory
Functions SaO2 (%) 92.6 ± 11.4 93.7 ± 9.1
PaO2/FiO2 ratio 344.2 ± 20.3 326.1 ± 27.1
Operating time (mins) 181.1 ± 31.1 167.6 ± 35.3
Aortic cross clamping time (mins) 28 ± 4.8 N/A
Number of grafts performed 3.6 ± 0.1 3..0 ± 0.4
Internal mammary artery use (%) 100 100
Operative
Intubation time (hours) 7.1 ± 6.5 6.9 ± 5.8
Characteristics
Patients requiring reintubation (%) 3 1
Patients requiring NIV (%) 15 14
Blood transfusion (units) 1.6 ± 0.3 1.0 ± 0.3
Hospital stay (days) 6.4 ± 0.7 5.6 ± 0.9
FIGURE 1.Graphs showing (a) mean PaO2 values (mm Hg), (b) mean PaCO2 values (mm Hg), (c) mean SaO2
values (%) and (d) mean Pao2/Fio2 ratio values at each postoperative time point starting from the time
of admission to intensive care unit (ICU), along with 95% confidence interval (error bars) the two groups
(Group A; ONCABG and Group B; OPCABG).
ONCABG, on-pump coronary artery bypass grafting; OPCABG, off-pump coronary artery bypass grafting.
PaCO2: partial pressure of arterial carbon dioxide; PaO2: partial pressure of arterial oxygen; PaO2/FiO2:
ratio of arterial oxygen partial pressure to fractional inspired oxygen; SaO2: arterial oxygen saturation.
Clin. Pract. (2018) 15(4) 10.4172/clinical-practice.1000408 787
Mohamed Ali Bakry
RESEARCH
no significant differences between the two the differences between the on-pump
groupsand they were comparable in terms versus off-pump technique with the aim
of demographic and clinical characteristics of detecting the potential advantages of
as well as the surgical procedures performed. OPCABG.
There were also no differences in intubation
We found similar values in oxygenation
times or need for blood transfusion. We
both overall and at most time points. The
did observe ahigher number of grafts
only significant differences were observed at
performed as well as longer hospital stay
ICU admission, with seemingly better arterial
periods in the ONCABG group. There was
perfusion in the OPCABG group. Similar
also a trend toward more patients with good
findings were also reported by Chiarenza
systolic functions in the OPCABG group but
and his colleagues [3]. It is important to note
these differences were small and statistically
that in concordance with our study they too
insignificant. All of the patients progressed
noted that this difference was not observed at
well following surgery and both groups were
any other time point throughout the course
comparable in terms of need for reintubation
of the first 24 hours postoperatively and
or the postoperative use of NIV.
therefore cannot be taken as indication of
FIGURE 1 shows the results of arterial higher risk of lung injury with ONCABG. They
blood gas analyses alveolar/arterial oxygen postulated that the most likely explanation
pressure gradients for the two groups for a difference only on ICU admission is in
measured at the seven time points over the homogeneities in ventilation during transfer
course of the first 24 hours postoperatively, of the patients from the operating room to
with zero indicating time of admission to the the ICU as they are ventilated with aambu
ICU. bag [3]. This does not explain why better
arterial gas characteristics on ICU admission
The most noteworthy observation is
were only seen in the OPCABG group in both
that significant differences between the
studies with two completely independent
two groups were only found at the zero
study cohorts and surgical teams. It could
time point i.e. upon admission to the ICU.
be that there is very mild intraoperative
At this time point, significantly higher PaO2
lung damage associated with the ONCABG
and PaO2/FiO2 values were found in Group B
technique which is rapidly compensated
(the OPCABG group). Also at this time point
and does not cause permanent deficit. The
a significantly higher PaCO2 value was found
effect of OPCABG on pulmonary function is
in group A (ONCABG group). Other than that,
still unclear. While large randomized studies
no other significant difference in the overall
have found no benefit using OPCABG
course of PaO2, PaCO2 and PaO2/FiO2 values
compared to ONCABG [9-11] and several
and no differences in SaO2 values were
smaller studies have also found no significant
observed at any time point over the course
differences in pulmonary gas exchange, time
of the first 24 hours spent in ICU.
to extubation, or postoperative pulmonary
Discussion function between on-pump and off-pump
In the current study we performed a CABG patients [8,18-23] there are reports
detailed evaluation of respiratory function; of improved static and dynamic lung
specifically gas exchange sequentially over compliance, reduced rates of respiratory
the course of the first postoperative 24 complications, and shorter intubation
hours following CABG surgery. The only times in OPCABG patients [19,24-29]. The
other study that performed such a detailed authors of these studies proposed better
preservation of pulmonary function as an
analysis of these measures to compare the
explanation for this [20,25,27,30].
postoperative respiratory profile between
OPCABG and ONCABG surgery did so In the current study, we used a
retrospectively, by going through what was noninvasive yet sensitive measure of
available in the records of the patients saved pulmonary gas exchange to conduct a
in their database [3]. To our knowledge our controlled comparison between the effects
study is the first study that prospectively of on-pump and off-pump CABG. Our results
collected these data to specifically evaluate can therefore be reliably taken to indicate
788 10.4172/clinical-practice.1000410 Clin. Pract. (2018) 15(4)
Respiratory function following on-Pump versus off-pump coronary bypass
grafting surgery RESEARCH
that there is no advantage using off-pump [32] throughout the first postoperative day,
over on-pump CABG in terms of early confirming the presence of a lung insult
postoperative pulmonary gas exchange in even in elective low-risk patients undergoing
non-smoking (at least for the preceding 6 cardiac surgery, regardless of the use of CPB.
months) patients with good left ventricular Similar findings were reported previously
function and no preexisting lung disease. [3,18]. High risk patients were excluded from
This is further supported by the lack of our studies thus it is difficult to speculate
difference in number of patients requiring if a larger difference in the postoperative
reintubation and/or NIV postoperatively course of respiratory variables would have
between the two groups. This suggests a been found in a population at higher risk
(such as more-than-mild chronic obstructive
very limited role for CPB in the occurrence
pulmonary disease or patients undergoing
of postoperative pulmonary dysfunction,
emergency CABG). This needs to be
and that other factors are responsible for the
addressed by future studies.
development of lung injury during CABG.
These factors may include general anesthesia Acknowledgements
as well as interstitial edema which can cause The authors wish to thank the surgeons,
serious mechanical and gas exchange ICU doctors and nurses and lab technicians
abnormalities [4,31]. It is important to note for their help and Ms Fatima Mohamed and
however that the PaO2/FiO2 ratio maintained Ms Mariam Ibrahim for help with patient
values within the range of acute lung injury rexcruitment and data organization.
Clin. Pract. (2018) 15(4) 10.4172/clinical-practice.1000408 789
Mohamed Ali Bakry
RESEARCH
REFERENCES Shroyer AL, Grover FL, Hattler B. et al. Off-pump surgery decreases
Filsoufi, F, Rahmanian, PB, Castillo, On-pump versus off-pumpcoronary- postoperative complications and
JG, Chikwe, J, Adams DH. Predictors and arterybypass surgery. N. Engl. J. Med. resource utilization in the elderly. Ann.
early and late outcomes of respiratory 361(19), 1827-1837 (2009). Thorac. Surg. 68(4): 1490-1493 (1999).
failure in contemporary cardiac surgery. Mack MJ, Pfister A, Bachandn D. Møller CH, Perko MJ, Lund JT,
Chest. 133(3), 13-721 (2008). Comparison of coronary bypass surgery et al. No major differences in 30-
Jensen, L, Yang, L. Risk factors with and without cardiopulmonary day outcomes in high-risk patients
for postoperative pulmonary bypass in patients with multivessel randomized to off-pump versus on-
complications in coronary artery disease. J. Thorac Cardiovasc. Surg. pump coronary bypass surgery. The
bypass graft surgery patients. Eur. J. 127(1), 167-173 (2004). Best Bypass Surgery Trial. Circulation.
Cardiovasc. Nurs. 6(3), 241-246 (2007). 121(4), 498-504 (2010).
Kara I, Cakalagaoglu C, Ay Y.
Chiarenza F, Tsoutsouras T, Cassisi C, Reoperative coronary artery bypass Sarin EL, Kayatta MO, Kilgo P, et
et al. The Effects of On-Pump and Off- surgery: the role of on-pump and off- al. Short- and longterm outcomes in
Pump Coronary Artery Bypass Surgery pump techniques on factors affecting octogenarian patients undergoing off-
on Respiratory Function in the Early hospital mortality and morbidity. Ann. pump coronary artery bypass grafting
Postoperative Period. J. Intensive Care Thorac. Cardiovasc. Surg. 19(6), 435- compared with on-pump coronary
Med.6(3): 241-246 (2017). 440 (2013). artery bypass grafting. Innovations
(Phila). 6(2), 110-115 (2011).
Wan S, Izzat MB, Lee TW, et al. Sa MP, Lima LP, Rueda FG.
Comparative study between on- Groeneveld AB, Jansen EK and
Avoiding cardiopulmonary bypass in
pump and off-pump coronary artery Verheij J. Mechanisms of pulmonary
multivessel CABG reduces cytokine
bypass graft in women. Rev. Bras. Cir. dysfunction after on-pump and off-
response and myocardial injury. Ann.
Cardiovasc. 25(2), 238-244 (2010). pump cardiac surgery: a prospective
Thorac. Surg. 68(1), 52-57 (1999).
cohort study. J. Cardiothorac. Surg. 11
Narayan P, Caputo M, Jones J, et
Nissinen J, Biancari F, Wistbacka JO. (2007).
al. Postoperative chest radiographic
Pulmonary function and immediate
changes after on- and off- Meharwal Z, Mishra Y, Kohli V, et al.
and late outcome after coronary artery
pumpcoronary surgery. Clin. Radiol. Off-pump multivessel coronary artery
bypass surgery. J. Cardiovasc. Surg.
60(6), 693-699 (2005). surgery in high-risk patients. Ann.
(Torino) 51(6), 915-921 (2016).
Thorac. Surg. 74(4),S1353-S1357.
Engels GE, Gu YJ, van Oeveren W,
Santos NP, Mitsunag, RM, Borges et al. The utility of lung epithelium Gu¨ ler M, Kirali K, Toker ME. Different
DL. Factors associated to hypoxemia specific biomarkers in cardiac surgery: a CABG methods in patients with chronic
in patients undergoing coronary comparison of biomarker profiles in on- obstructive pulmonary disease. Ann.
artery bypass grafting. Rev. Bras. Cir. and off-pumpcoronary bypass surgery. Thorac. Surg. 71(1),152-157 (2001).
Cardiovasc. 28(3), 364-370 (2013). J. Cardiothorac. Surg. 8,4 (2013).
Lamy A, Devereaux PJ, Prabhakaran
Cislaghi F, Condemi AM, Corona A. Angdin M, Settergren G, Vaage D. Off-pump or on-pump coronary
Predictors of prolonged mechanical J. Better preserved pulmonary artery bypass grafting at 30 days. . Engl.
ventilation in a cohort of 3,269 CABG endothelium-dependent vasodilation J. Med. 366(16), 1489-1497 (2012).
patients. Minerva Anestesiol. 73(12), with off-pumpcoronary surgery. Scand.
615-621(2007). Ohkado A, Nakano K, Nakatani H,
Cardiovasc. J. 35(4), 264-269 (2001).
et al. The superiority of pulmonary
Izzat MB, Almohammad F, Raslan Montes FR, Maldonado JD, Paez function after minimally invasive direct
AF. Off-pump grafting does not reduce S, Ariza F. Off-pump versus on-pump coronary artery bypass. Jpn. J. Thorac.
postoperative pulmonary dysfunction. coronary artery bypass surgery and Cardiovasc. Surg. 50(2),66-69 (2002).
Asian Cardiovasc. Thorac. Ann. 25(2), postoperative pulmonary dysfunction.
LaPar DJ, Bhamidipati CM, Reece
113-117 (2017). J. Cardiothorac. Vasc. Anesth. 18(6),
TB, et al. Is off-pump coronary
698-703 (2004).
Diegeler A, BorgermannJ, Kappert artery bypass grafting superior to
U. Off-pump versus on-pumpcoronary- Kochamba GS, Yun KL, Pfeffer conventional bypass in octogenarians?
arterybypass grafting in elderly patients. TA, Sintek CF, Khonsari S. Pulmonary J. Thorac. Cardiovasc. Surg. 141(1), 810-
N. Engl. J. Med. 368(13), 1189-198. abnormalities after coronary 890 (2011).
arterial bypass grafting operation:
Lamy A, Devereaux PJ, Prabhakaran Pawlaczyk R, Swietlik D, Lango R,
cardiopulmonary bypass versus
D. Off-pump or on-pumpcoronary- Rogowski J. Offpump coronary surgery
mechanical stabilization. Ann. Thorac.
arterybypass grafting at 30 days. N. may reduce stroke, respiratory failure
Surg. 69(5): 1466-1470 (2000).
Engl. J. Med. 366(16), 1489-1497 and mortality in octogenarians. Ann.
(2012). Boyd WD, Desai ND, Del Rizzo DF, Thorac. Surg. 94 (1), 29-37 (2012).
790 10.4172/clinical-practice.1000410 Clin. Pract. (2018) 15(4)
Respiratory function following on-Pump versus off-pump coronary bypass
grafting surgery RESEARCH
Moshkovitz Y, Lusky A and Mohr Surg. 110 (4),979-987 (1995). Ferguson, ND, Fan, E, Camporota,
R. Coronary artery bypass without L. The Berlin definition of ARDS: an
Young RW. Prevention of lung
cardiopulmonary bypass: analysis of expanded rationale, justification, and
injury in cardiac surgery: a review. J
short-term and mid-term outcome supplementary material. Intensiv.
Extra Corpor Technol. 46(2), 130-141
in 220 patients. J. Thorac. Cardiovasc. Care. Med. 38(10), 1573-1582 (2012).
(2014).
Clin. Pract. (2018) 15(4) 10.4172/clinical-practice.1000408 791
Potrebbero piacerti anche
- Deep Breath & SpirometerDocumento7 pagineDeep Breath & SpirometerAsmaa GamalNessuna valutazione finora
- Does Pleurotomy Affects Respiratory FunctionsDocumento7 pagineDoes Pleurotomy Affects Respiratory FunctionsBeshoy KhelaNessuna valutazione finora
- Cytokine Clearance With Cytosorb® During Cardiac Surgery: A Pilot Randomized Controlled TrialDocumento12 pagineCytokine Clearance With Cytosorb® During Cardiac Surgery: A Pilot Randomized Controlled Trialgra ndynNessuna valutazione finora
- Cardio1 PDFDocumento7 pagineCardio1 PDFAyu SuprabawatiNessuna valutazione finora
- Effects of Lung Expansion Therapy On Lung Function in Patients With Prolonged Mechanical VentilationDocumento7 pagineEffects of Lung Expansion Therapy On Lung Function in Patients With Prolonged Mechanical Ventilationcard breatheNessuna valutazione finora
- Extubacion en Pacientes Con Enfermedades NeuromuscularesDocumento9 pagineExtubacion en Pacientes Con Enfermedades NeuromuscularesjuliasimonassiNessuna valutazione finora
- CLN 66 01 107 PDFDocumento5 pagineCLN 66 01 107 PDFGloria KartikaNessuna valutazione finora
- JUrNAL 2Documento9 pagineJUrNAL 2RizmaMudzalifahNessuna valutazione finora
- Critical Illness-Related Corticosteroid Insufficiency During Difficult Weaning From Mechanical VentilationDocumento8 pagineCritical Illness-Related Corticosteroid Insufficiency During Difficult Weaning From Mechanical VentilationKarolina VillafuerteNessuna valutazione finora
- (03241750 - Acta Medica Bulgarica) Application of Positive End-Expiratory Pressure (PEEP) in Patients During Prolonged Gynecological SurgeryDocumento6 pagine(03241750 - Acta Medica Bulgarica) Application of Positive End-Expiratory Pressure (PEEP) in Patients During Prolonged Gynecological SurgeryTeodorNessuna valutazione finora
- HemoptisisDocumento7 pagineHemoptisiswiliaNessuna valutazione finora
- 14 - Mazandarani2012Documento7 pagine14 - Mazandarani2012TandeanTommyNovenantoNessuna valutazione finora
- The Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsDocumento5 pagineThe Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsM Ali AdrianNessuna valutazione finora
- Aneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10Documento7 pagineAneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10cooleraid884Nessuna valutazione finora
- Virtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDocumento7 pagineVirtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDaniel Lago BorgesNessuna valutazione finora
- ResuscitationDocumento8 pagineResuscitation85tq5nhsqbNessuna valutazione finora
- Thrombosis Research: Full Length ArticleDocumento8 pagineThrombosis Research: Full Length ArticleMaría José GalvisNessuna valutazione finora
- 2018 - Article Erdocan 8p.pdf - CopieDocumento6 pagine2018 - Article Erdocan 8p.pdf - CopieThomas HussonNessuna valutazione finora
- Reseccion Pulmonar en Hemoptisis SeveraDocumento10 pagineReseccion Pulmonar en Hemoptisis SeverarafodocNessuna valutazione finora
- SugamadexDocumento8 pagineSugamadexPaulina LugoNessuna valutazione finora
- Research Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailureDocumento7 pagineResearch Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailurewiwiNessuna valutazione finora
- Wa0006Documento9 pagineWa0006Venkata Nagaraj MummadisettyNessuna valutazione finora
- Ferrer 2006Documento7 pagineFerrer 2006Fermin LombardiaNessuna valutazione finora
- 10 1016@j Bja 2020 08 060Documento9 pagine10 1016@j Bja 2020 08 060kenjiNessuna valutazione finora
- PDF (8) JurnalDocumento11 paginePDF (8) JurnalIcha Chaphedech hildantraNessuna valutazione finora
- Teknik Acbt Untuk Kasus BronkhiektasisDocumento9 pagineTeknik Acbt Untuk Kasus Bronkhiektasisfister19 rifaudinNessuna valutazione finora
- PreventionOfCardiacSurgery AssDocumento11 paginePreventionOfCardiacSurgery AssOğuz KayıkçıNessuna valutazione finora
- Surgical Endoscopy Journal 1Documento86 pagineSurgical Endoscopy Journal 1Saibo BoldsaikhanNessuna valutazione finora
- Cmmi2022 4590037Documento7 pagineCmmi2022 4590037Paula Andrea Perdomo SalamancaNessuna valutazione finora
- Pre Hospital Cardiac Arrest 1Documento8 paginePre Hospital Cardiac Arrest 1Reka BDNessuna valutazione finora
- The Value of Preoperative Pulmonary Assessment in Predicting Postoperative Pulmonary ComplicationsDocumento47 pagineThe Value of Preoperative Pulmonary Assessment in Predicting Postoperative Pulmonary ComplicationsDr. Hadika Pramana, SpPDNessuna valutazione finora
- Inflamt VMDocumento6 pagineInflamt VMDiana Reaño RuizNessuna valutazione finora
- Rationale and Design of The Consider Af StudyDocumento12 pagineRationale and Design of The Consider Af StudyjafarkassimNessuna valutazione finora
- Review Article: Oxygenation, Ventilation, and Airway Management in Out-of-Hospital Cardiac Arrest: A ReviewDocumento11 pagineReview Article: Oxygenation, Ventilation, and Airway Management in Out-of-Hospital Cardiac Arrest: A ReviewBumySusantiNessuna valutazione finora
- Pulso InvasiveDocumento20 paginePulso InvasivenadiaNessuna valutazione finora
- Artículo PulmonarDocumento9 pagineArtículo PulmonarSamuel GasparNessuna valutazione finora
- Effectiveness of Treatment With High-Frequency Chest Wall Oscillation in Patients With BronchiectasisDocumento8 pagineEffectiveness of Treatment With High-Frequency Chest Wall Oscillation in Patients With BronchiectasisfarahNessuna valutazione finora
- Anaesthesia Concern in Lobectomy NewDocumento63 pagineAnaesthesia Concern in Lobectomy NewAbhi JeetNessuna valutazione finora
- Acute Respiratory FailureDocumento12 pagineAcute Respiratory FailureOrion JohnNessuna valutazione finora
- Ecmo Clase 2 - 4Documento11 pagineEcmo Clase 2 - 4Johanna GiraldoNessuna valutazione finora
- Laparoscopic OvariectomíaDocumento15 pagineLaparoscopic Ovariectomíasimon alfaro gonzálezNessuna valutazione finora
- Recruitment Maneuver in Prevention of Hypoxia During Percutaneous Dilational Tracheostomy: Randomized TrialDocumento7 pagineRecruitment Maneuver in Prevention of Hypoxia During Percutaneous Dilational Tracheostomy: Randomized TrialMelly Susanti PhuaNessuna valutazione finora
- Role of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyDocumento6 pagineRole of Ultrasonographic Inferior Venacaval Assessment in Surgeries Conducted Under General Anaesthesia-A Prospective Observational StudyIJAR JOURNALNessuna valutazione finora
- Riociguat For The Treatment of Chronic Thromboembolic Pulmonary Hypertension: A Long-Term Extension Study (CHEST-2)Documento10 pagineRiociguat For The Treatment of Chronic Thromboembolic Pulmonary Hypertension: A Long-Term Extension Study (CHEST-2)FinaNessuna valutazione finora
- Myofascial Release in Patients During The Early Postoperative Period After Revascularisation of Coronary ArteriesDocumento13 pagineMyofascial Release in Patients During The Early Postoperative Period After Revascularisation of Coronary Arteriesestefy140399Nessuna valutazione finora
- Factors Causing Prolonged Mechanical Ventilation and Peri Operative Morbidity After Robot Assisted Coronary Artery Bypass Graft SurgeryDocumento8 pagineFactors Causing Prolonged Mechanical Ventilation and Peri Operative Morbidity After Robot Assisted Coronary Artery Bypass Graft SurgeryApotik ApotekNessuna valutazione finora
- Effects of Cardiopulmonary Bypass On Mediastinal Drainage and The Use of Blood Products in The Intensive Care Unit in 60-To 80-Year-Old Patients Who Have Undergone Coronary Artery Bypass GraftingDocumento8 pagineEffects of Cardiopulmonary Bypass On Mediastinal Drainage and The Use of Blood Products in The Intensive Care Unit in 60-To 80-Year-Old Patients Who Have Undergone Coronary Artery Bypass GraftingYogi TrilaksonoNessuna valutazione finora
- Robba Et Al-2024-Intensive Care MedicineDocumento13 pagineRobba Et Al-2024-Intensive Care MedicineLeiniker NavarroNessuna valutazione finora
- Resuscitative Endovascular Balloon Occlusion of The Aorta (REBOA) : An Updated ReviewDocumento9 pagineResuscitative Endovascular Balloon Occlusion of The Aorta (REBOA) : An Updated ReviewLuis-alfredo Perez Bolde HernandezNessuna valutazione finora
- DeWaal CCM 2007Documento6 pagineDeWaal CCM 2007Cristina AdamacheNessuna valutazione finora
- Postoperative CareDocumento15 paginePostoperative CarelhalamNessuna valutazione finora
- En 13Documento8 pagineEn 13Bruna CarvalhoNessuna valutazione finora
- Ezs 535Documento6 pagineEzs 535Eko SiswantoNessuna valutazione finora
- 2014 Journal - Patient With Congenital Systemic To Pulmonary Shunts and Increased Pulmonary Vascular ResistanceDocumento7 pagine2014 Journal - Patient With Congenital Systemic To Pulmonary Shunts and Increased Pulmonary Vascular ResistanceAryfKurniawanNessuna valutazione finora
- Sumber DuaDocumento6 pagineSumber DuaadiNessuna valutazione finora
- Tension Pneumothorax During Liver and Kidney Transplantation in A Patient With Adult Polycystic Kidney DiseaseDocumento4 pagineTension Pneumothorax During Liver and Kidney Transplantation in A Patient With Adult Polycystic Kidney DiseaseAsmia SftrNessuna valutazione finora
- Wu 2017Documento7 pagineWu 2017petrus daveNessuna valutazione finora
- Clinical Effects of Pleurotomy On Patients Undergoing CABGDocumento5 pagineClinical Effects of Pleurotomy On Patients Undergoing CABGBeshoy KhelaNessuna valutazione finora
- Essentials in Lung TransplantationDa EverandEssentials in Lung TransplantationAllan R. GlanvilleNessuna valutazione finora
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYDa EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNessuna valutazione finora
- Successful Retrieval of A Dislodged Zotarolimuseluting Coronary Stent in The Ascending AortaDocumento3 pagineSuccessful Retrieval of A Dislodged Zotarolimuseluting Coronary Stent in The Ascending AortaShira michaelNessuna valutazione finora
- Comparison of Rigid and Deformable Image Registration Accuracy of The Liver During Longterm Transition After Proton BeamDocumento6 pagineComparison of Rigid and Deformable Image Registration Accuracy of The Liver During Longterm Transition After Proton BeamShira michaelNessuna valutazione finora
- Comparison of Endotracheal Cuff Pressure Measurements Before and After Nursing Care in Emergency Patients Pilot BalloonDocumento5 pagineComparison of Endotracheal Cuff Pressure Measurements Before and After Nursing Care in Emergency Patients Pilot BalloonShira michaelNessuna valutazione finora
- Successful Retrieval of A Dislodged Zotarolimuseluting Coronary Stent in The Ascending AortaDocumento3 pagineSuccessful Retrieval of A Dislodged Zotarolimuseluting Coronary Stent in The Ascending AortaShira michaelNessuna valutazione finora
- Phytochemical and Antimicrobial Studies of Oroxylum Indicum ExtractsDocumento8 paginePhytochemical and Antimicrobial Studies of Oroxylum Indicum ExtractsShira michaelNessuna valutazione finora
- Highintensity Focused Ultrasound of Uterine Fibroids and Adenomyosis Maneuver Technique For BowelDocumento3 pagineHighintensity Focused Ultrasound of Uterine Fibroids and Adenomyosis Maneuver Technique For BowelShira michaelNessuna valutazione finora
- Promote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportDocumento4 paginePromote Severe Wound Healing by Pvpi Dry Powder Spray Case Series ReportShira michaelNessuna valutazione finora
- CV & Surat Lamaran KerjaDocumento2 pagineCV & Surat Lamaran KerjaAci Hiko RickoNessuna valutazione finora
- Apron CapacityDocumento10 pagineApron CapacityMuchammad Ulil AidiNessuna valutazione finora
- 2022 WR Extended VersionDocumento71 pagine2022 WR Extended Versionpavankawade63Nessuna valutazione finora
- Cummin C1100 Fuel System Flow DiagramDocumento8 pagineCummin C1100 Fuel System Flow DiagramDaniel KrismantoroNessuna valutazione finora
- Lecture 2 Effects of Operating Conditions in VCCDocumento9 pagineLecture 2 Effects of Operating Conditions in VCCDeniell Joyce MarquezNessuna valutazione finora
- Mechanical Production Engineer Samphhhhhle ResumeDocumento2 pagineMechanical Production Engineer Samphhhhhle ResumeAnirban MazumdarNessuna valutazione finora
- EqualLogic Release and Support Policy v25Documento7 pagineEqualLogic Release and Support Policy v25du2efsNessuna valutazione finora
- Bom Details FormatDocumento6 pagineBom Details FormatPrince MittalNessuna valutazione finora
- Tool Charts PDFDocumento3 pagineTool Charts PDFtebengz100% (2)
- Algoritm BackTracking EnglezaDocumento6 pagineAlgoritm BackTracking Englezaionutz_67Nessuna valutazione finora
- SOL LogicDocumento21 pagineSOL LogicJa RiveraNessuna valutazione finora
- Contents EEMUA Publication 190 Edition1 May 2015Documento4 pagineContents EEMUA Publication 190 Edition1 May 2015Aditya JainNessuna valutazione finora
- Literatura Tecnica 3Documento10 pagineLiteratura Tecnica 3Christian PerezNessuna valutazione finora
- Ra 9272Documento6 pagineRa 9272janesamariamNessuna valutazione finora
- Perancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratDocumento8 paginePerancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratSutan AdityaNessuna valutazione finora
- Disassembly Procedures: 1 DELL U2422HB - U2422HXBDocumento6 pagineDisassembly Procedures: 1 DELL U2422HB - U2422HXBIonela CristinaNessuna valutazione finora
- Applications SeawaterDocumento23 pagineApplications SeawaterQatar home RentNessuna valutazione finora
- Brand Strategy - in B2BDocumento6 pagineBrand Strategy - in B2BKrishan SahuNessuna valutazione finora
- Man and Historical ActionDocumento4 pagineMan and Historical Actionmama.sb415Nessuna valutazione finora
- Comparison Between CompetitorsDocumento2 pagineComparison Between Competitorsritesh singhNessuna valutazione finora
- Module 2 MANA ECON PDFDocumento5 pagineModule 2 MANA ECON PDFMeian De JesusNessuna valutazione finora
- UT Dallas Syllabus For Govt4396.002.08s Taught by Gregory Thielemann (Gregt)Documento2 pagineUT Dallas Syllabus For Govt4396.002.08s Taught by Gregory Thielemann (Gregt)UT Dallas Provost's Technology GroupNessuna valutazione finora
- Music 10 (2nd Quarter)Documento8 pagineMusic 10 (2nd Quarter)Dafchen Villarin MahasolNessuna valutazione finora
- CV Augusto Brasil Ocampo MedinaDocumento4 pagineCV Augusto Brasil Ocampo MedinaAugusto Brasil Ocampo MedinaNessuna valutazione finora
- WBDocumento59 pagineWBsahil.singhNessuna valutazione finora
- Lecture2 GranulopoiesisDocumento9 pagineLecture2 GranulopoiesisAfifa Prima GittaNessuna valutazione finora
- MCI Approved Medical College in Uzbekistan PDFDocumento3 pagineMCI Approved Medical College in Uzbekistan PDFMBBS ABROADNessuna valutazione finora
- Eggermont 2019 ABRDocumento15 pagineEggermont 2019 ABRSujeet PathakNessuna valutazione finora
- Sociology As A Form of Consciousness - 20231206 - 013840 - 0000Documento4 pagineSociology As A Form of Consciousness - 20231206 - 013840 - 0000Gargi sharmaNessuna valutazione finora
- Book 1518450482Documento14 pagineBook 1518450482rajer13Nessuna valutazione finora