Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Inferior Alveolar Nerve Injury in Implant Dentistry: Diagnosis, Causes, Prevention, and Management
Caricato da
maxTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Inferior Alveolar Nerve Injury in Implant Dentistry: Diagnosis, Causes, Prevention, and Management
Caricato da
maxCopyright:
Formati disponibili
LITERATURE REVIEW
Inferior Alveolar Nerve Injury in Implant
Dentistry: Diagnosis, Causes, Prevention,
and Management
Ahmed Ali Alhassani, BDS
Ali Saad Thafeed AlGhamdi, BDS, MS*
Inferior alveolar nerve injury is one of the most serious complications in implant dentistry.
This nerve injury can occur during local anesthesia, implant osteotomy, or implant
placement. Proper understanding of anatomy, surgical procedures, and implant systems and
proper treatment planning is the key to reducing such an unpleasant complication. This
review discusses the causes of inferior alveolar nerve injury and its diagnosis, prevention, and
management.
Key Words: inferior alveolar nerve, nerve injury, complication of dental implant,
diagnosis of nerve injury, management of nerve injury
INTRODUCTION placement.3 This complication is one of the
most unpleasant experiences for both the
D
ental implantology has be-
patient and the dentist, so every precaution
come a widely accepted mode
should be taken to avoid it. Once it happens,
of treatment. Because of its
the dentist should provide the patient with
ability to restore esthetics and
appropriate care and should know when to
function, it has become the
refer the patient to a microneurosurgeon.
preferred option for replacing hopeless and
missing natural teeth. Despite its high success Depending on the degree of nerve injury,
rate, however, many complications have been alteration in sensation varies from mild
encountered with its use. paresthesia to complete anesthesia. Also, it
One of the most serious complications is may be transient, manageable, or, in certain
the alteration of sensation after implant cases, permanent. The purpose of this article
placement in the posterior mandible. The is to provide guidelines for prevention and
prevalence of such a complication has been management of IAN injury during dental
reported as high as 13%.1,2 This can occur as implant placement in the posterior man-
a result of injury to the inferior alveolar nerve dible.
(IAN) or the lingual nerve from traumatic
local anesthetic injections or, most impor-
ALTERATION OF SENSATION
tant, during dental implant osteotomy or
Alteration of sensation can occur in the form
Periodontic Division, Oral Basic & Clinical Sciences
Department, Faculty of Dentistry, King Abdulaziz of paresthesia, dysthesia, analgesia, or an-
University, Jeddah, Saudi Arabia.
* Corresponding author, e-mail: asalghamdi2@kau.edu.sa
esthesia. Paresthesia is an alteration in
DOI: 10.1563/AAID-JOI-D-09-00059 sensation that can be felt as numbness,
Journal of Oral Implantology 401
Inferior Alveolar Nerve Injury
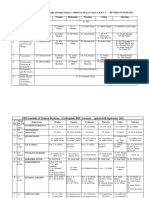
TABLE
Clinical neurosensory tests8,29,30
Name of Test Description
Mechanoceptive
Static light touch detection Patient is asked to tell when he/she feels light touch on the face
and to point to the exact location.
Brush directional discrimination Patient is asked to tell when he/she feels the brush and to
determine the direction of movement.
Two-point discrimination Patient is asked to determine single and 2 points of touch. The
examiner uses any 2 instruments by which the patient can
change the distance between them.
Nociceptive
Pin pressure nociception Patient is asked to determine the feeling of a pin prick.
Thermal discrimination Patient is asked if he/she feels cold or heat.
burning, or prickling sensations, either IAN to evaluate the extent of neural damage
evoked or spontaneous, whereas dysthesia after implant placement. These vary from
is a spontaneous or evoked unpleasant easy methods that can be performed with
abnormal sensation.4 Analgesia is the loss simple instruments available in the operatory
of pain sensation, whereas anesthesia is loss to more sophisticated procedures that re-
of perception of stimulation by any noxious quire high-technology equipment.
or nonnoxious stimulant.5 Simple, clinical neurosensory tests are
Seddon6 classified nerve injuries as neuro- used most commonly, and they can be
praxia, axonotmesis, and neurotmesis. In classified into mechanoceptive tests and
neuropraxia, the continuity of the axon is nociceptive tests (Table). Each test should
preserved and the injury is usually temporary. be performed while the patient closes his or
Axonotmesis is caused by more severe injury, her eyes and is in a comfortable position,
as the axons are disrupted but the overall away from distractions. The clinician should
structure and integrity of the neural tube use the contralateral side as a control, and
remain intact. Neurotmesis is the most severe results must be accurately recorded.7,8
form of nerve injury, wherein the integrity of
the neural tube becomes disrupted.
INFERIOR ALVEOLAR NERVE
Practitioners should be familiar with
these types of nerve injuries and should be The mandibular nerve is the third and most
able to perform standardized neurosensory inferior division of the trigeminal, or fifth,
examinations to determine the degree of cranial nerve. The trigeminal nerve is pre-
change in sensation, should know the dominantly a sensory nerve, innervating
possible outcomes, and should decide when most of the face. The upper branch of the
to refer the patient to a microneurosurgeon. trigeminal nerve is the ophthalmic nerve,
The patient’s neurosensory functions must which innervates the forehead. The middle
be evaluated as part of the initial examina- branch, the maxillary nerve, innervates the
tion before implant treatment is started, maxilla and the midface. The lower branch,
especially patients with a history of altera- the mandibular nerve, innervates the teeth
tion of sensory function of the IAN asso- and the mandible, the lateral mucosa of the
ciated with previous implant or impacted mandible, and the mucosa and skin of the
third molar extraction. cheek, lower lip, and chin. The mandibular
Many neurosensory tests are available to nerve contains both sensory and motor
measure the neurosensory function of the fibers. It runs from the trigeminal ganglion
402 Vol. XXXVI/No. Five/2010
Alhassani and AlGhamdi
through the foramen ovale and gives off 2 canals. Despite the rare occurrence of the
branches from its main trunk (meningeal bifid IAN canal, the clinician must be on the
branch and nerve to the medial pterygoid lookout for these cases when planning for
muscle). Then it divides into anterior and dental implants.
posterior divisions. The anterior branch emits Several methods are used to localize the
1 sensory nerve, the buccal nerve, and 3 IAN during treatment planning. These in-
motor branches to supply the masseter, the clude conventional radiography, tomogra-
temporalis, and the lateral pterygoid mus- phy, and computerized tomography (CT).
cles. The posterior branch of the mandibular Another method is surgical exposure of the
nerve is larger than the anterior branch. It mental nerve by blunt dissection to allow
gives off 2 sensory branches, the auriculo- direct vision of the nerve and to estimate the
temporal and lingual nerves. Just before the distance between the mandibular ridge crest
posterior branch enters the mandibular and the IAN, but the irregular intraosseous
foramen as the inferior alveolar nerve, it course of the nerve limits the value of this
gives off the mylohyoid nerve, which sup- surgical technique.10
plies the mylohyoid and the anterior belly of CT provides the most accurate and
the digastric muscles.9 precise method for localization of the IAN.
The IAN is a branch of the posterior Also, the image can be reconstructed into a
division of the mandibular nerve that con- 3-dimensional model that can be used as an
tains both sensory and motor fibers. It enters accurate surgical guide. This 3-dimensional
the mandibular foramen, runs in the man- image is very useful in determining the
dibular canal, and supplies the mandibular buccolingual width of the bone, as well as
teeth. It leaves the mandibular canal through the buccolingual position of the nerve. This
the mental foramen as the mental nerve. allows positioning of the implant to the
Within the canal, the nerve is about 3 mm in lingual or buccal of the nerve to avoid its
diameter, and its course varies. It can run injury in cases of limited bone height.
with a gentle curve toward the mental Although CT is very useful in dental im-
foramen, or it can have an ascending or plantology, its high cost and level of radia-
descending pathway.7,9,10 tion prevent it from becoming the standard
In a recent study, Kim et al11 classified the of care.
buccolingual location of the IAN into 3 types. To localize the IAN, most clinicians use
Most cases (70%) were type 1, in which the conventional radiography (eg, panoramic
IAN canal follows the lingual cortical plate of views, periapicals), which is sufficient for
the mandibular ramus and body. In type 2 most cases.16 Panoramic radiographs can be
(15%), the IAN canal is located in the middle used safely for most cases but with some
of the mandibular ramus posterior to the limitations. A 2-mm safety zone between the
second molar. It then runs lingually to follow apical part of the implant and the upper
the lingual plate. In type 3 (15%), the IAN border of the IAN canal is strongly recom-
canal is located near the middle of the ramus mended by most implant manufacturers and
and body. practitioners.1,17 The magnification of the X-
A bifid IAN canal has been reported to ray machine must be known; some recom-
occur very infrequently. Nortjé et al12,13 mend placing an object of known dimension
found an occurrence of 0.9%. Grover et al14 in the mouth before taking the radiograph.
were able to find only 0.08% of radiographs This technique allows accurate calculation of
suggestive of bifurcation of the IAN. Langlais the dimensional changes in the panoramic
et al15 found 0.95% of cases to have bifid IAN radiograph.
Journal of Oral Implantology 403
Inferior Alveolar Nerve Injury
Conventional radiography produces only CAUSES OF AN IAN INJURY
a 2-dimensional record; therefore, other
Although injury of an IAN can occur during a
methods must be used to overcome this
traumatic local anesthesia injection,19 the
problem. Palpation and bone sounding
most severe types of injuries are caused by
under local anesthesia are helpful in deter- implant drills and implants themselves. In
mining the buccolingual width of the ridge. addition, flap retraction and pressure on the
In many cases, the crest of the ridge is too mental nerve area can cause injury to that
thin, in which case the implant surgeon nerve, resulting in altered sensation after
should consider these few millimeters to be surgery.20 For appropriate management, the
useless for implant support.18 exact cause of injury should be recognized.
Clinicians who depend mainly on the As mentioned earlier, proper localization
panoramic radiograph for localizing the IAN of the IAN and accurate measurement of the
must take some factors into consideration. available bone are of extreme importance to
The IAN canal typically appears as a well- avoid IAN injuries. Another important point
defined radiolucent bundle with superior is that many implant drills are slightly longer,
and inferior radiopaque borders. The cli- for drilling efficiency, than their correspond-
nician must follow the canal from the ing implants. This is one example of how lack
mandibular foramen to the mental foramen of knowledge about the implant system can
and must keep in mind that magnification is cause avoidable complications.17 Even after
a built-in feature of panoramic radiographs. accurate measurement of available bone,
Knowing the magnification factor, the cli- nerve injury can occur as the result of
nician can calculate the amount of available overpenetration of the drill owing to low
bone using the formula, resistance of the spongy bone; this can lead
to slippage of the drill even by experienced
Clinical bone height surgeons.18
~Radiographic bone height= Immediate implantation following tooth
extraction can sometimes cause nerve dam-
Magnification factor
age. Efforts by the surgeon to achieve
primary stability can lead to unintentional
where radiographic bone height is the apical extension and nerve injury. Remea-
measurement on the radiograph from the surement of the amount of available bone
crest of the ridge to the superior border of after tooth extraction is recommended when
the IAN canal, and the magnification factor is nerve proximity is expected because when
a known number (ie, if a certain X-ray the tooth is in situ, a misleading measure-
machine produces 30% magnification, the ment of the bone crest might be made. In
magnification factor will be 1.3, and if the addition, a few millimeters of the crestal
magnification is 25%, the magnification bone might be lost during extraction.
factor will be 1.25).
After calculating the clinical bone
height, the surgeon must remember to PREVENTION OF IAN INJURY
subtract the 2-mm safety zone between Accurate measurement of the bone available
the implant and the superior border of the for implant support coronal to the IAN canal is
IAN. Clinicians must also bear in mind that the only way to avoid IAN injuries. The use of
the crest of the ridge may contain very thin CT-based surgical stents or navigation systems
bone that cannot be used for implant may also help prevent nerve injury.1 Some
support. practitioners recommend the use of ‘‘drill
404 Vol. XXXVI/No. Five/2010
Alhassani and AlGhamdi
guards’’ provided by some implant systems. recommend using an implant that can be
These guards are attached to the drill close to ‘‘unscrewed’’ after placement. Whichever the
the handpiece to prevent overpenetration of clinician decides to do, he or she must do it
the drill into the bone.18 Many clinicians prefer as soon as possible to prevent or minimize
the use of transverse alveolar implant tech- permanent nerve damage.23 If the implant
niques to slant the implant laterally to engage causing the problem is already osseointe-
the cortical buccal bone, in an attempt to grated, it can be removed by a trephine drill.
avoid IAN injury.21 As an alternative, an apicoectomy of the
Heller et al22 advocate the practice of implant can be done, if feasible.24
using infiltration for local anesthesia instead of Clinicians might face some instances of
an IAN block, because without complete lack altered sensation wherein the implant does
of sensation, the patient will feel pain if the not appear to be impinging on the nerve. In
drill approaches the IAN canal—a significant such a case, nerve injury may have occurred
indication to stop drilling. At the same time, during drilling. Such a scenario should be
an intraoperative radiograph with the pres- strongly suspected if the implant is very
ence of the drill or other gauge in the close to the IAN canal. Other less frequent
osteotomy site is of great value, especially if causes include local anesthesia or aggressive
nerve approximation is expected. retraction of the buccal flap.
To control inflammatory reactions in the
injured nerve, a course of steroids can be
MANAGEMENT OF IAN INJURY
prescribed. An alternative would be a large
If intraoperative nerve injury is suspected, it dose of nonsteroidal anti-inflammatory drugs
must be recorded, and a thorough neuro- (eg, 800 mg ibuprofen) 3 times daily for
sensory examination should be performed as 3 weeks. If the situation improves, the
soon as the local anesthesia effect is lost.17 clinician can prescribe another course of
Results of the examination, as well as the anti-inflammatory drugs.17 Perceptions of
patient’s description of the altered sensation, pain and temperature are usually the first 2
must be recorded throughout follow-up sensations to recover, whereas other sensa-
visits. Events that can lead clinicians to tions may take longer.25
suspect nerve injury include pain or altered Many patients respond well to this line of
sensation during drilling or implant place- treatment. Any improvement in the patient’s
ment, slippage of the drill or implant deeper condition should be recorded, along with
than planned, and the presence of excessive results of a neurosensory examination and
bleeding, especially if nerve proximity is the patient’s description. If the condition fails
suspected. to improve within 2 months, referral to a
Patients may complain of altered sensa- microneurosurgeon is indicated. Early refer-
tion even though clinical procedures were ral will allow for early management before
uneventful. Management of the problem will distant degeneration of the nerve takes
depend on the cause of the IAN injury. As place.17 This degeneration usually occurs
mentioned earlier, nerve injury can occur for within 4–6 months of nerve injury.26–28 This
many reasons. Radiographs must be taken to is the reason why many authors recommend
confirm whether it has been caused by the that microsurgery be performed within the
implant. If the implant is impinging on the first months after injury.25
nerve, it should be removed or at least Strauss et al25 concluded that 50% of the
unscrewed a few threads to relieve the patients who underwent microsurgical repair
pressure on the nerve; this is why we of the IAN reported significant improvement,
Journal of Oral Implantology 405
Inferior Alveolar Nerve Injury
42.9% reported slight improvement, and 10. Anderson LC, Kosinski TF, Mentag PJ. A review
of the intraosseous course of the nerves of the
only 7.1% reported no improvement. They mandible. J Oral Implantol. 1991;17:394–403.
also reported that highly significant improve- 11. Kim ST, Hu KS, Song WC, Kang MK, Park HD,
Kim HJ. Location of the mandibular canal and the
ments were achieved after 1 year of micro- topography of its neurovascular structures. J Craniofac
surgical intervention. Surg. 2009;20:936–939.
12. Nortjé CJ, Farman AG, de V Joubert JJ. The
radiographic appearance of the inferior dental canal: an
additional variation. Br J Oral Surg. 1977;15:171–172.
CONCLUSIONS 13. Nortjé CJ, Farman AG, Grotepass FW. Variations in
the normal anatomy of the inferior dental (mandibular)
One of the serious complications of posterior canal: a retrospective study of panoramic radiographs from
mandibular implant placement is IAN injury. 3612 routine dental patients. Br J Oral Surg. 1977;15:55–63.
14. Grover PS, Lorton L. Bifid mandibular nerve as a
Proper understanding of the involved anat- possible cause of inadequate anesthesia in the
omy, the surgical procedures, and implant mandible. J Oral Maxillofac Surg. 1983;41:177–179.
systems—along with proper treatment plan- 15. Langlais RP, Broadus R, Glass BJ. Bifid mandib-
ular canals in panoramic radiographs. J Am Dent Assoc.
ning—will reduce the chances of such an 1985;110:923–926.
unpleasant complication. If nerve injury oc- 16. Vazquez L, Saulacic N, Belser U, Bernard JP.
Efficacy of panoramic radiographs in the preoperative
curs, early and proper management is the key planning of posterior mandibular implants: a prospec-
to maximizing the chances of recovery. tive clinical study of 1527 consecutively treated
patients. Clin Oral Implants Res. 2008;19:81–85.
17. Kraut RA, Chahal O. Management of patients
with trigeminal nerve injuries after mandibular implant
ABBREVIATIONS placement. J Am Dent Assoc. 2002;133:1351–1354.
18. Worthington P. Injury to the inferior alveolar
CT: computerized tomography nerve during implant placement: a formula for protec-
IAN: inferior alveolar nerve tion of the patient and clinician. Int J Oral Maxillofac
Implants. 2004;19:731–734.
19. Pogrel MA, Bryan J, Regezi J. Nerve damage
associated with inferior alveolar nerve blocks. J Am Dent
REFERENCES Assoc. 1995;126:1150–1155.
20. von Arx T, Hafliger J, Chappuis V. Neurosensory
1. Bartling R, Freeman K, Kraut RA. The incidence of disturbances following bone harvesting in the sym-
altered sensation of the mental nerve after mandibular physis: a prospective clinical study. Clin Oral Implants
implant placement. J Oral Maxillofac Surg. 1999;57: Res. 2005;16:432–439.
1408–1412. 21. Stella JP, Abolenen H. Restoration of the
2. Ellies LG. Altered sensation following mandibular atrophied posterior mandible with transverse alveolar
implant surgery: a retrospective study. J Prosthet Dent. maxillary/mandibular implants: technical note and case
1992;68:664–671. report. Int J Oral Maxillofac Implants. 2002;17:873–879.
3. Hegedus F, Diecidue RJ. Trigeminal nerve 22. Heller AA, Shankland WE 2nd. Alternative to the
injuries after mandibular implant placement—practical inferior alveolar nerve block anesthesia when placing
knowledge for clinicians. Int J Oral Maxillofac Implants. mandibular dental implants posterior to the mental
2006;21:111–116. foramen. J Oral Implantol. 2001;27:127–133.
4. Kipp DP, Goldstein BH, Weiss WW Jr. Dysesthesia 23. Khawaja N, Renton T. Case studies on implant
after mandibular third molar surgery: a retrospective removal influencing the resolution of inferior alveolar
study and analysis of 1377 surgical procedures. J Am nerve injury. Br Dent J. 2009;206:365–370.
Dent Assoc. 1980;100:185–192. 24. Levitt DS. Apicoectomy of an endosseous
5. Merrill RG. Prevention, treatment, and prognosis implant to relieve paresthesia: a case report. Implant
for nerve injury related to the difficult impaction. Dent Dent. 2003;12:202–205.
Clin North Am. 1979;23:471–488. 25. Strauss ER, Ziccardi VB, Janal MN. Outcome
6. Seddon HJ, Medawar PB, Smith H. Rate of assessment of inferior alveolar nerve microsurgery: a
regeneration of peripheral nerves in man. J Physiol. retrospective review. J Oral Maxillofac Surg. 2006;64:
1943;102:191–215. 1767–1770.
7. Akal UK, Sayan NB, Aydogan S, Yaman Z. 26. Colin W, Donoff RB. Restoring sensation after
Evaluation of the neurosensory deficiencies of oral trigeminal nerve injury: a review of current manage-
and maxillofacial region following surgery. Int J Oral ment. J Am Dent Assoc. 1992;123:80–85.
Maxillofac Surg. 2000;29:331–336. 27. Pogrel MA, Maghen A. The use of autogenous
8. Ghali GE, Epker BN. Clinical neurosensory testing: vein grafts for inferior alveolar and lingual nerve
practical applications. J Oral Maxillofac Surg. 1989;47: reconstruction. J Oral Maxillofac Surg. 2001;59:985–
1074–1078. 988; discussion 988–993.
9. Snell RS. Clinical Anatomy for Medical Students. 28. Ruggiero SL. Trigeminal nerve injury and repair.
Baltimore, Md: Lippincott Williams & Wilkins; 2000. N Y State Dent J. 1996;62:36–40.
406 Vol. XXXVI/No. Five/2010
Alhassani and AlGhamdi
29. Hillerup S. Iatrogenic injury to the inferior 30. Poort LJ, van Neck JW, van der Wal KG. Sensory
alveolar nerve: etiology, signs and symptoms, and testing of inferior alveolar nerve injuries: a review of
observations on recovery. Int J Oral Maxillofac Surg. methods used in prospective studies. J Oral Maxillofac
2008;37:704–709. Surg. 2009;67:292–300.
Journal of Oral Implantology 407
Potrebbero piacerti anche
- Types of Implant Surgical Guides in Dentistry A ReviewDocumento10 pagineTypes of Implant Surgical Guides in Dentistry A Reviewmax100% (2)
- Tunnel Access For Guided Bone Regeneration in The Maxillary AnteriorDocumento6 pagineTunnel Access For Guided Bone Regeneration in The Maxillary Anteriormax100% (1)
- Meniere DiseaseDocumento16 pagineMeniere DiseaseNavjot Brar100% (2)
- Anat of Root Apex - Review ArticleDocumento9 pagineAnat of Root Apex - Review ArticleRevathy ParthasarathyNessuna valutazione finora
- Esthetic Excellence PDFDocumento32 pagineEsthetic Excellence PDFZomba ZombariraNessuna valutazione finora
- PLPF PDFDocumento88 paginePLPF PDFmaxNessuna valutazione finora
- National Board Dental Examination Part I 2009 GuideDocumento36 pagineNational Board Dental Examination Part I 2009 GuideutkmangalNessuna valutazione finora
- Roth PhilosophyDocumento120 pagineRoth PhilosophyPARIJAT CHAKRABORTY100% (1)
- OcclusionDocumento49 pagineOcclusionRajsandeep SinghNessuna valutazione finora
- A New Papilla Preservation Technique For Periodontal Regeneration of Severely Compromised TeethDocumento6 pagineA New Papilla Preservation Technique For Periodontal Regeneration of Severely Compromised TeethmaxNessuna valutazione finora
- Minor ConnectorsDocumento35 pagineMinor ConnectorsRoschelle Dominique Lorezco100% (3)
- Instruments MCQDocumento3 pagineInstruments MCQNur Fatima Azzahara100% (1)
- Flexible Dentures 2Documento28 pagineFlexible Dentures 2jquin3100% (1)
- Orim 36 05 401 407Documento7 pagineOrim 36 05 401 407Neil SchembriNessuna valutazione finora
- Dr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique RevisitedDocumento6 pagineDr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique Revisitedabhishekjha0082Nessuna valutazione finora
- Bianchi2017Documento4 pagineBianchi2017Anisakis anisakiosisNessuna valutazione finora
- Corneal Neurotization: A Novel Solution To Neurotrophic KeratopathyDocumento9 pagineCorneal Neurotization: A Novel Solution To Neurotrophic KeratopathyJosé Castro SoaresNessuna valutazione finora
- Antony2017 PDFDocumento8 pagineAntony2017 PDFM. JahangirNessuna valutazione finora
- Antony2017 PDFDocumento8 pagineAntony2017 PDFM. JahangirNessuna valutazione finora
- Scarano 2017Documento9 pagineScarano 2017Lila karla leon villarNessuna valutazione finora
- Akinosi (Tuberosity) Technique A Verity But Under-UtilisedDocumento3 pagineAkinosi (Tuberosity) Technique A Verity But Under-UtilisedJorge López CaNessuna valutazione finora
- Nervio AlveolarDocumento3 pagineNervio AlveolarLuis GustavoNessuna valutazione finora
- A Comparison of Questionnaire Monofilament Assessment Neurosensory Deficit Versus ofDocumento6 pagineA Comparison of Questionnaire Monofilament Assessment Neurosensory Deficit Versus ofodontologia uvNessuna valutazione finora
- Microsurgical Repir of IANDocumento9 pagineMicrosurgical Repir of IANbabukanchaNessuna valutazione finora
- Awake Neurosurgery An UpdateDocumento5 pagineAwake Neurosurgery An UpdatevictoriaefernandezNessuna valutazione finora
- Thetrigeminalnerve Injury: Arshad Kaleem,, Paul Amailuk,, Hisham Hatoum,, Ramzey TursunDocumento13 pagineThetrigeminalnerve Injury: Arshad Kaleem,, Paul Amailuk,, Hisham Hatoum,, Ramzey TursunPriyanka SinhaNessuna valutazione finora
- 74 488 2 PBDocumento3 pagine74 488 2 PBRatna mellaNessuna valutazione finora
- Trigeminal Neuralgia and Atypical Odontalgia 2005Documento2 pagineTrigeminal Neuralgia and Atypical Odontalgia 2005Bima Ewando KabanNessuna valutazione finora
- Laser Therapy For Neurosensory Recovery After Saggital Split Ramus OseotomyDocumento8 pagineLaser Therapy For Neurosensory Recovery After Saggital Split Ramus OseotomyFrancisco ChourioNessuna valutazione finora
- Awake Glioma Surgery: Technical Evolution and NuancesDocumento32 pagineAwake Glioma Surgery: Technical Evolution and NuancesVito MasagusNessuna valutazione finora
- Jomr 06 E3Documento10 pagineJomr 06 E3r1comfupchNessuna valutazione finora
- YlikontiolaDocumento7 pagineYlikontiolaodontologia uvNessuna valutazione finora
- Thopaedic Science: JournalDocumento16 pagineThopaedic Science: JournalCiro Madrid FloresNessuna valutazione finora
- 1 s2.0 S1878875018300159 MainDocumento9 pagine1 s2.0 S1878875018300159 MainAlexandreNessuna valutazione finora
- Adj 12392Documento7 pagineAdj 12392Fahad AliNessuna valutazione finora
- Lesión Nerviosa Causada Por Analgesia Del Bloqueo MandibularDocumento7 pagineLesión Nerviosa Causada Por Analgesia Del Bloqueo Mandibularmrestrepo55501Nessuna valutazione finora
- 9384 - Original ResearchDocumento3 pagine9384 - Original ResearchAnita PrastiwiNessuna valutazione finora
- Diagnostic EvaluationDocumento67 pagineDiagnostic EvaluationMyzing OraaNessuna valutazione finora
- Regional Anesthesia and Eye SurgeryDocumento7 pagineRegional Anesthesia and Eye SurgeryharumNessuna valutazione finora
- The Key To Profound Local Anesthesia: NeuroanatomyDocumento8 pagineThe Key To Profound Local Anesthesia: NeuroanatomyRavik FidayatikaNessuna valutazione finora
- An Endoscopic Technique For Endodontic Surgery: VOL. 25, NO. 2, FEBRUARY 1999Documento4 pagineAn Endoscopic Technique For Endodontic Surgery: VOL. 25, NO. 2, FEBRUARY 1999DrdrNessuna valutazione finora
- Iatrogenic Damage To The Mandibular Nerves As AssessedDocumento4 pagineIatrogenic Damage To The Mandibular Nerves As AssessedAndres Rojas JerezNessuna valutazione finora
- Gow Gates Complications IIIDocumento8 pagineGow Gates Complications IIIBeth AguiarNessuna valutazione finora
- Asked: Frequently Questions About Neuromuscular DentistryDocumento6 pagineAsked: Frequently Questions About Neuromuscular DentistryAhmed HamzaNessuna valutazione finora
- Understanding Neuropathic Corneal Pain PDFDocumento13 pagineUnderstanding Neuropathic Corneal Pain PDFLivros CatólicosNessuna valutazione finora
- Applying Neuromuscular Techniques in The Orthodontic SettingDocumento13 pagineApplying Neuromuscular Techniques in The Orthodontic SettingMahdi ChahrourNessuna valutazione finora
- Peripheral Neurectomies: A Treatment Option For Trigeminal Neuralgia in Rural PracticeDocumento9 paginePeripheral Neurectomies: A Treatment Option For Trigeminal Neuralgia in Rural PracticeMustaqim PrasetyaNessuna valutazione finora
- Applying Neuromuscular Techniques in The Orthodontic SettingDocumento13 pagineApplying Neuromuscular Techniques in The Orthodontic SettingBoom BoomNessuna valutazione finora
- Current Concept in Adult Peripheral Nerve and Brachial Plexus SurgeryDocumento8 pagineCurrent Concept in Adult Peripheral Nerve and Brachial Plexus SurgeryJhon Fredy Castañeda LopezNessuna valutazione finora
- Nerve LateralisationDocumento6 pagineNerve LateralisationAshish PandaNessuna valutazione finora
- Anestesia Regional Cuero CabelludoDocumento7 pagineAnestesia Regional Cuero CabelludoPablo Sousa CasasnovasNessuna valutazione finora
- Nervus Intermedius Neuralgia: Presented by Syed - Khaja Aliuddin M.SC.D - ENDODocumento19 pagineNervus Intermedius Neuralgia: Presented by Syed - Khaja Aliuddin M.SC.D - ENDOAli SyedNessuna valutazione finora
- Nerve Injuries Associated With Gynecological SurgeryDocumento8 pagineNerve Injuries Associated With Gynecological SurgeryLakshmi DheviNessuna valutazione finora
- Craniotomy Nursing JournalDocumento2 pagineCraniotomy Nursing JournalSeann LorescoNessuna valutazione finora
- Review IANBUJOMFSDocumento6 pagineReview IANBUJOMFSIndah AmaliaNessuna valutazione finora
- Temporary Blindness After Inferior Alveolar Nerve BlockDocumento2 pagineTemporary Blindness After Inferior Alveolar Nerve BlockIbramanto WarganegaraNessuna valutazione finora
- EMG Response of Facial Nerve Stimulation Under Different LevelsDocumento9 pagineEMG Response of Facial Nerve Stimulation Under Different LevelsAlejandro CheritNessuna valutazione finora
- Traumatic Optic Neuropathy: Review ArticleDocumento9 pagineTraumatic Optic Neuropathy: Review ArticleTiwi QiraNessuna valutazione finora
- Surgical Approaches To EpilepsyDocumento13 pagineSurgical Approaches To EpilepsyJames E. WalkerNessuna valutazione finora
- Rde 39 215Documento6 pagineRde 39 215danzNessuna valutazione finora
- The Neurologic Examination-PDOUT-MHAMCMDocumento31 pagineThe Neurologic Examination-PDOUT-MHAMCMNorjetalexis CabreraNessuna valutazione finora
- Jaw Surgery: Robert M. Menard, Nikhil K. DesaiDocumento10 pagineJaw Surgery: Robert M. Menard, Nikhil K. DesaiAlain AguirreNessuna valutazione finora
- Vertical Splitting of The Mandibular Body As An Alternative To Inferior Alveolar Nerve LateralizationDocumento7 pagineVertical Splitting of The Mandibular Body As An Alternative To Inferior Alveolar Nerve Lateralizationr1comfupchNessuna valutazione finora
- Challengesinpediatric NeuroanesthesiaDocumento18 pagineChallengesinpediatric NeuroanesthesiaMerlin MuktialiNessuna valutazione finora
- Oral Medicine 8Documento8 pagineOral Medicine 8abdulrazaqNessuna valutazione finora
- Anesthesia: Essays and Researches Inferior Alveolar Nerve Block: Alternative TechniqueDocumento6 pagineAnesthesia: Essays and Researches Inferior Alveolar Nerve Block: Alternative TechniqueMaqbul AlamNessuna valutazione finora
- Locoregional Anesthesia inDocumento14 pagineLocoregional Anesthesia indeisyNessuna valutazione finora
- Peripheral Nerve Injury 2Documento24 paginePeripheral Nerve Injury 2Gargi MPNessuna valutazione finora
- Median, Ulnar and Radial Nerve Injuries: University of Baghdad Al-Kindy College of Medicine Fifth Stage / Group ADocumento13 pagineMedian, Ulnar and Radial Nerve Injuries: University of Baghdad Al-Kindy College of Medicine Fifth Stage / Group ANoor Al Zahraa AliNessuna valutazione finora
- INMFNDocumento6 pagineINMFNAlejandro CheritNessuna valutazione finora
- IntJHealthAlliedSci24225-5153688 141856Documento5 pagineIntJHealthAlliedSci24225-5153688 141856Ramesh lal ShahNessuna valutazione finora
- Echography and Doppler of the BrainDa EverandEchography and Doppler of the BrainChiara RobbaNessuna valutazione finora
- Advanced Platelet-Rich Fibrin A New Concept For Cell-Based Tissue Engineering by Means of Inflammatory CellsDocumento11 pagineAdvanced Platelet-Rich Fibrin A New Concept For Cell-Based Tissue Engineering by Means of Inflammatory CellsmaxNessuna valutazione finora
- Telescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesDocumento15 pagineTelescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesmaxNessuna valutazione finora
- SB RinjaniDocumento16 pagineSB RinjanimaxNessuna valutazione finora
- Telescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesDocumento9 pagineTelescopic Crowns As Attachments For Implant Supported Restorations A Case SeriesmaxNessuna valutazione finora
- Instructions For UseDocumento3 pagineInstructions For UsemaxNessuna valutazione finora
- Instructions For Use: Nobelactive® ImplantDocumento3 pagineInstructions For Use: Nobelactive® ImplantmaxNessuna valutazione finora
- 310 FullDocumento2 pagine310 FullmaxNessuna valutazione finora
- Use of Fisiograft in Intrabony Defects-A Clinical and Radiological StudyDocumento4 pagineUse of Fisiograft in Intrabony Defects-A Clinical and Radiological StudymaxNessuna valutazione finora
- Histological Study On Sinus Lift Grafting by Fisiograft and Bio-OssDocumento6 pagineHistological Study On Sinus Lift Grafting by Fisiograft and Bio-OssmaxNessuna valutazione finora
- Aaid Joi D 10 00146Documento10 pagineAaid Joi D 10 00146maxNessuna valutazione finora
- Flap Advancement: Practical Techniques To Attain Tension-Free Primary ClosureDocumento12 pagineFlap Advancement: Practical Techniques To Attain Tension-Free Primary ClosuremaxNessuna valutazione finora
- FISIOGRAFT ENG Set 17 PDFDocumento28 pagineFISIOGRAFT ENG Set 17 PDFmaxNessuna valutazione finora
- Advanced Platelet-Rich Fibrin A New Concept For Cell-Based Tissue Engineering by Means of Inflammatory CellsDocumento11 pagineAdvanced Platelet-Rich Fibrin A New Concept For Cell-Based Tissue Engineering by Means of Inflammatory CellsmaxNessuna valutazione finora
- Periosteal Releasing Incision For Successful Coverage of Augmented Sites. A Technical NoteDocumento6 paginePeriosteal Releasing Incision For Successful Coverage of Augmented Sites. A Technical NotemaxNessuna valutazione finora
- Somalia Launches First Ever-Cleft Lip and Palate Surgery ClinicDocumento4 pagineSomalia Launches First Ever-Cleft Lip and Palate Surgery ClinicAMISOM Public Information ServicesNessuna valutazione finora
- LegendsDocumento2 pagineLegendsEnrique Serrano VelazquezNessuna valutazione finora
- Peterson's Principals of Oral and Maxyofacial Surgery Ch.0008 - Impacted TeethDocumento18 paginePeterson's Principals of Oral and Maxyofacial Surgery Ch.0008 - Impacted TeethДимитър АлександровNessuna valutazione finora
- Recent Advances in Dental Radiography For Pediatric Patients: A ReviewDocumento6 pagineRecent Advances in Dental Radiography For Pediatric Patients: A ReviewFebriani SerojaNessuna valutazione finora
- Análisis Clínico y Radiográfico de Las Técnicas ART y Remoción Químico-Mecánica de Caries - Estudio PilotoDocumento7 pagineAnálisis Clínico y Radiográfico de Las Técnicas ART y Remoción Químico-Mecánica de Caries - Estudio PilotoValeria RodriguezNessuna valutazione finora
- CHAS Dental Subsidy ScheduleDocumento1 paginaCHAS Dental Subsidy ScheduleEugeneNessuna valutazione finora
- A Comparative Study of Tooth Shade Selection Via Conventional and Digital Methods-An In-Vivo Study.Documento10 pagineA Comparative Study of Tooth Shade Selection Via Conventional and Digital Methods-An In-Vivo Study.bhupendraNessuna valutazione finora
- Eruption of Palatal Canines Following Surgical Exposure: A Review of Outcomes in A Series of Consecutively Treated CasesDocumento5 pagineEruption of Palatal Canines Following Surgical Exposure: A Review of Outcomes in A Series of Consecutively Treated CasesAniket PotnisNessuna valutazione finora
- Test 5 - Oral Surgery, Oral Diagnosis & RoentgenologyDocumento6 pagineTest 5 - Oral Surgery, Oral Diagnosis & Roentgenologydr.jah9Nessuna valutazione finora
- PD Cen TR 12401-2009Documento14 paginePD Cen TR 12401-2009gauravNessuna valutazione finora
- 7 PDFDocumento5 pagine7 PDFRoja AllampallyNessuna valutazione finora
- 4.int Endodontic J - 2024 - Keratiotis - A 22 Year Follow Up Cross Sectional Study On Periapical Health in Relation To TheDocumento16 pagine4.int Endodontic J - 2024 - Keratiotis - A 22 Year Follow Up Cross Sectional Study On Periapical Health in Relation To Theelifsude98Nessuna valutazione finora
- Revised Schedule of BHU SSH OPD (Soft Copy) 2021Documento7 pagineRevised Schedule of BHU SSH OPD (Soft Copy) 2021rajubhagatssmNessuna valutazione finora
- Simon P. Hullihen and The Origin of Orthognathic Surgery: Special ContributionDocumento5 pagineSimon P. Hullihen and The Origin of Orthognathic Surgery: Special ContributionRulo NarvaNessuna valutazione finora
- Decision-Making Process PDFDocumento13 pagineDecision-Making Process PDFVladislava GanevaNessuna valutazione finora
- Dental Hygienist CourseworkDocumento8 pagineDental Hygienist Courseworkrqaeibifg100% (2)
- NobelReplace Conical Connect OverviewDocumento6 pagineNobelReplace Conical Connect Overviewaziz2007Nessuna valutazione finora
- Treatment Planning Assignment - DigmannDocumento8 pagineTreatment Planning Assignment - Digmannapi-508053077Nessuna valutazione finora
- Recommended Fees MDADocumento1 paginaRecommended Fees MDAfcjr79Nessuna valutazione finora
- Policy On Early Childhood Caries (ECC) - Classifications, Consequences, and Preventive StrategiesDocumento4 paginePolicy On Early Childhood Caries (ECC) - Classifications, Consequences, and Preventive StrategiesJeje100% (1)
- Dentaltrauma: Lewis C. JonesDocumento8 pagineDentaltrauma: Lewis C. JonesHusni mubarakNessuna valutazione finora
- Cracked Tooth Syndrome: Presented by Syed - Khaja Ali Uddin M.SC.D (Endo)Documento62 pagineCracked Tooth Syndrome: Presented by Syed - Khaja Ali Uddin M.SC.D (Endo)Ali Syed67% (3)