Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Jaxt10i4p233 PDF
Caricato da
KeerthikaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Jaxt10i4p233 PDF
Caricato da
KeerthikaCopyright:
Formati disponibili
Invited Review www.jcd.org.
in
Endodontic microbiology
L Lakshmi Narayanan, Vaishnavi C
Department of Conservative Dentistry & Endodontics, SRM Kattankulathur Dental College & Hospital, SRM University, Chennai, India
Abstract
Root canal therapy has been practiced ever since 1928 and the success rate has tremendously increased over the years
owing to various advancements in the field. One main reason is the complete understanding of the microbiology involved
in the endodontic pathology. This has helped us to modify the conventional treatment plans and effectively combat the
microorganisms. Now, studies are aiming to explore the characteristics of the “most” resistant organism and the methods
to eliminate them. This article gives an insight of the microbiology involved in endodontic pathology and discusses its
role in our treatment procedure. Information from original reviews listed in PubMed, published from 1995 to 2010, has
been mainly included in this review.
Keywords: Bacterial infections; biofilms; dental pulp microbiology; Enterococcus faecalis; gram positive bacteria; periapical
periodontitis/microbiology.
INTRODUCTION a major deterrent in endodontic infection by the classical
study by Kakehashi et al.[2] There are so many ways by
Preservation of teeth by endodontic therapy has gained lot which the microorganisms reach the pulp and it is of prime
of popularity because of increased and predictable success importance that we know the same for our treatment
rate of our endodontic procedures, the reason for this being planning. The various routes by which the microorganisms
the complete understanding of endodontic pathology reach the pulp are as follows.[3]
and our ability to combat the same. Essentially, endodontic
infection is the infection of the dental root canal Dentinal tubules: After a carious lesion or during dental
system and the major etiologic agent of apical procedures, microorganisms may use the pathway in a
periodontitis.[1] Although various chemical and physical centripetal direction to reach the pulp. Bacteria gain access
factors can induce periradicular inflammation, scientific to the pulp when the dentin distance between the border
evidence clearly indicates that microorganisms are essential of carious lesion and the pulp is 0.2 mm.[4]
for the progression and perpetuation of different forms of
apical periodontitis.[2] Open cavity: Direct pulp exposure of traumatic origin such
as in coronal fracture, or that of iatrogenic nature due to
The rationale for endodontic treatment is to eradicate operative procedures, breaks the physical barrier imposed
the infection, to prevent microorganisms from infecting by dental structures and leaves pulp in contact with the
or re-infecting the root and/or periradicular tissues. Thus, septic oral environment.
a thorough understanding of the endodontic microbiota
associated with different forms of disease is the basis for Periodontal membrane: Microorganisms from gingival
the success of endodontic treatment. This article, based on sulcus may reach the pulp chamber through the periodontal
the search made in PubMed, briefs about the endodontic membrane, using a lateral channel or the apical foramen
microbiology and its importance for the success of
as a pathway. This pathway becomes available to
endodontic treatment.
microorganisms during a dental prophylaxis, due to dental
luxation, and more significantly, as a result of the migration
PATHWA YS OF INFECTION of epithelial insertion to the establishment of periodontal
pockets.
It is proved beyond doubt that presence of microbiota is
Blood stream: A transient bacteremia may occur for any
Address for correspondence:
Dr. L. Lakshmi Narayanan, No: 7, 7th Avenue, number of reasons during the normal day of a healthy
Harrington Road, Chetpet, Chennai – 31, India. individual. The bacteria present in the blood would be
E-mail: vaishnavivenkat@yahoo.com attracted to the dental pulp following trauma or operative
Date of submission: 03.09.2010 procedure that produced inflammation without causing
Review completed: 05.09.2010 pulp exposure. This attraction through blood or lymph
Date of acceptance: 06.09.2010 is known as anachoresis, which serves as a path for
DOI: 10.4103/0972-0707.73386 endodontic infection.
Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4 233
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
Faulty restoration: Studies have proven that salivary anaerobic Gram negative coccobacilli which have been
contamination from the occlusal aspect can reach the consistently detected in endodontic infections.
periapical area in less than 6 weeks in canals obturated with • Dialister pneumosintes and
guttapercha and sealer.[5] If the temporary seal is broken • Dialister invisus.
or if the tooth structure fractures before final restoration, 4) Fusobacterium is also a common member of endodontic
or if the final restoration is inadequate, bacteria may gain microbiota.
access to the periapical tissue and result in infection. • Fusobacterium nucleatum
• Fusobacterium periodonticum
Extent: Microorganisms might reach the principal and/or 5) Spirochetes are highly motile, spiral-shaped, Gram
lateral canals migrating from an infected tooth to a healthy negative bacteria with periplasmic flagella. All oral
pulp as a consequence of the contiguousness of the tissues, spirochetes fall into the genus Treponema.[9] Prevalent
thereby spreading the infection to an adjacent tooth. species are
• Treponema denticola
CORRELATION OF MICROBES TO • Treponema sacranskii
INFECTION • Treponema parvum
• Treponema maltophilum and
Almost 700 bacterial species can be found in the oral
• Treponema lecithinolyticum.
cavity, with any particular individual harboring 100–200 of
6) Gram positive anaerobic rods have also been found in
these species.[6] Once the root canal is infected coronally,
endodontic microbiota like
infection progresses apically until bacterial products or
• Pseudoramibacter alactolyticus
bacteria themselves are in a position to stimulate the
periapical tissues, thereby leading to apical periodontitis. • Filifactor alocis
Endodontic infections have a polymicrobial nature, with • Actinomyces spp.
obligate anaerobic bacteria conspicuously dominating • Propionibacterium propionicum
the microbiota in primary infections. There are various • Olsenella spp.
microorganisms related to intra-radicular and extraradicular • Slackia exigua
infections and organisms involved in persistent infection. • Mogibacterium timidum and
They are discussed below. • Eubacterium spp.
7) Gram positive cocci that are present in endodontic
Intraradicular infections infection:
The endodontic pathogens that cause the primary • Parvimonas micra (previously called Peptostreptococcus
intraradicular infections are the following. micros or Micromonas micros)
• Streptococcus spp. which include
1) Black pigmented Gram negative anaerobic rods include
Streptococcus anginosus
species formerly known as Bacteroides melaninogenicus.
Streptococcus mitisi
These bacteria have been reclassified into two
genera: (a) saccharolytic species – Prevotella and (b) Streptococcus sanguinis
asaccharolytic species – Porphyromonas.[7] • Enterococcus faecalis.
Prevotella species detected in endodontic infections Other bacterial spp. which are present in low to
moderate values include
include
• Campylobacter spp. which are Gram negative
• Prevotella intermedia
anaerobic rods; common species are
• Prevotella nigrescens
Campylobacter rectus and
• Prevotella tannerae
Campylobacter gracilis.
• Prevotella multissacharivorax
• Catonella morbic which is a saccharolytic obligate
• Prevotella baroniae and
anaerobic Gram negative rod
• Prevotella denticola.
• Veillonella parvula
Porphyromonas species detected in endodontic
infections include • Eikenella corrodens
• Porphyromonas endodontalis and • Granulicatella adiacens
• Porphyromonas gingivalis. • Neisseria mucosa
2) Tannerella forsythia (previously called Bacteroides forsythus • Centipeda periodontii
or Tannerella forsythenis) was the first periodontal • Gemella morbillorum
pathogen to be detected in endodontic infection.[8] • Capnocytophaga gingivalis
3) Dialister species are asaccharolytic obligately • Corynebacterium matruchotii
234 Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
• Bifidobacterium dentium and • Propionibacterium propionicum
• anaerobic lactobacilli. • Treponema spp.
• Porphyromonas endodontalis
Apart from these, several uncultivated phylotypes which • Porphyromonas gingivalis
can be unrecognized but play a role in pathogenesis of • Treponema forsythia
apical periodontitis, such as[10]
• Prevotella spp. and
• Dialister oral clone BSO16
• Fusobacterium nucleatum.
• Migasphaera oral clone BSO16
• Solobacterium Bacteria persisting intracanal disinfection
• Olsenella procedures and after root canal treatment
• Eubacterium Some microorganisms are resistant to antimicrobial
• Cytophaga treatment and can survive in the root canal after
• Lachnospiraceae oral clone 55A-34 biomechanical preparation.
• Veillonella oral clone BP 1–85
• Bacteroidetes oral clone XO 83 The most common Gram negative anaerobic rods are
• Prevotella oral clone PUS 9.180 • Fusobacterium nucleatum
• Eubacterium oral clone BP 1–89 and • Prevotella spp. and
• Lachnospiraceae oral clone MCE 7–60. • Campylobacter rectus.
• Other microorganisms in endodontic infections
The most common Gram positive bacteria are
Fungi – particularly, Candida spp. (e.g.,) Candida albicans • Streptococci (Streptococcus mitis, Streptococcus gordonii,
Streptococcus anginosus, Streptococcus oralis)
Archaea – These are diverse group of prokaryotes which • Lactobacilli (Lactobacillus paracasei and Lactobacillus
are distinct from bacteria. They are traditionally recognized acidophilus)
as extremophiles but recently these microorganisms are • Staphylococci
found to thrive in non-extreme environment including • E. faecalis
human body. Methanogenic archaea have been detected in • Olsenella uli
periodontal disease and chronic apical periodontitis.[11] • Parvimonas micra
• Pseudoramibacter alactolyticus
Viruses – Viruses are particles structurally composed of
a nucleic acid molecule (DNA or RNA) and a protein coat. • Propionibacterium spp.
These viruses require viable host cells to infect and use the • Actinomyces spp.
cell’s machinery to replicate the viral genome. Hence, they • Bifidobacterium spp. and
cannot survive in a necrotic root canal. • Eubacterium spp.
The presence of viruses in the root canal has been reported Sometimes, yeasts, commonly C. albicans, are also found in
only for non-inflamed vital pulps of patients infected small amounts.
with human immunodeficiency virus and herpes viruses
where living cells are found in abundance.[12,13] Among E. faecalis and yeast, mainly C. albicans, has been repeatedly
the Herpes spp., the human cytomegalovirus and Epstein– identified as the species most commonly recovered
Barr virus may be implicated in the pathogenesis of apical from root canals undergoing retreatment, in cases of
periodontitis. failed endodontic therapy and canals with persistent
infections.[18,19] E. faecalis are gram positive cocci and
Extraradicular infections facultative anaerobes. They are normal intestinal organisms
Intraradicular microorganisms usually constrain themselves and may inhabit the oral cavity and gingival sulcus. When
in the root canal due to the defense barrier. In specific this bacterium is present in small numbers, it is easily
circumstances, microorganisms can overcome this defense eliminated; but if it is in large numbers, it is difficult to
barrier and establish an extraradicular infection. This may eradicate. E. faecalis has many distinct features which
lead to development of acute apical abscess with purulent make it an exceptional survivor in the root canal. These
inflammation in periapical tissue. The extraradicular microorganisms can perform the following.
infections are dependent on or independent of an • Live and persist in poor nutrient environment
intraradicular infection. The dominant microorganisms • Survive in the presence of several medications
present are anaerobic bacteria[14-17] like (e.g., calcium hydroxide) and irrigants (e.g., sodium
• Actinomyces spp. hypochlorite)
Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4 235
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
• Form biofilms in medicated canals mobilization of inmunosurveillance mechanisms in the
• Invade and metabolize fluids within the dentinal pulp. These endotoxins are associated with pulpal pain,
tubules and adhere to collagen periapical inflammation, activation of complement and
• Convert into a viable but non-cultivable state periapical bone destruction.[24-27]
• Acquire antibiotic resistance
PG: PG is the major component of Gram positive cell
• Survive in extreme environments with low pH, high
wall. Upon cell lysis, PG is released and can react with the
salinity and high temperatures
innate immune system as well as induce upregulation of
• Endure prolonged periods of starvation and utilize
proinflammatory and anti-inflammatory cytokines in T
tissue fluid that flows from the periodontal ligament
cells.[28] PG may facilitate an adaptive immune response via
macrophages.[29] The potency of PG is strongly boosted in
PATHOPHYSIOLOGY the presence of LPS.[30]
The human commensal microbiota populates the mucosal LTA: LTA is a cell wall component of Gram positive bacteria,
surface of the oral cavity, gastrointestinal tract, urogenital composed of echoic acid and lipid.[31] LTA shares many of its
tract and surface of the skin. This commensal microbiota, pathogenic properties with LPS.[32] LTA is released as a result
which has coevolved with its host, has acquired the means of cell lysis and binds to target cells, which then interacts
of surviving and tolerating host defense mechanisms.[20,21] with circulating antibodies and activates complement
However, when the host is compromised, or if invading cascade and cause damage.
microorganisms are sufficiently pathogenic, disease can
develop. Pathogenicity refers to the ability of an organism Fimbriae: Fimbriae are long, filamentous macromolecules
to cause disease in another organism. These organisms found on the surface of many Gram negative bacteria. The
are known as pathogens which include bacteria, fungi, thin hair-like projections are made of protein subunits
viruses, protozoa and parasites. These pathogens are (they are distinct from flagella). Fimbriae are involved
capable of adhering, colonizing, surviving, propagating, at in attachment to surfaces and interactions with other
the same time evading host defense mechanisms such as bacteria.[33]
neutrophils, complement and antibodies. In addition, they
can cause tissue destruction directly or indirectly.[22] Direct Capsules: A capsule is a well-organized layer outside the cell
tissue damage can be induced by enzymes, exotoxins wall of the bacteria, generally composed of polysaccharides
and metabolites. Indirect tissue damage can be induced and other materials. Capsules serve to facilitate protection
from a host immune reaction capable of causing tissue of the bacterial cell against desiccation, phagocytosis,
destruction that is stimulated by bacterial components bacterial viruses and hydrophobic toxic materials such as
which include lipopolysaccharide (LPS), peptidoglycan detergents. Bacteria and fungi utilize capsule formation
(PG), lipoteichoic acid (LTA), fimbriae, outer membrane to inhibit complement activation and resist ingestion by
proteins, capsular components and extracellular vesicles. phagocytes.
The degree of pathogenicity or disease producing ability
of a microorganism is known as virulence. Several Extracellular vesicles: Extracellular vesicles are produced
physicochemical factors in the root canal have the potential by Gram negative bacteria and allow the release of
to influence the pathogenicity of bacteria, which include their products into the extracellular environment. The
the degree of anaerobiosis, pH level, the availability of contents include proteins and lipids that are involved in
exogenous and endogenous nutrients, as well as the a diverse array of activities including hemagglutination,
surfaces available for adherence like dentin. In infected hemolysis, bacterial adhesion and proteolytic activities.[34]
root-filled teeth, any medicament remnants and root filling Extracellular vesicles are a means by which bacteria interact
material are additional factors to influence pathogenicity. with prokaryotic and eukaryotic cells and can modulate
interactions between neighboring bacteria.[35,36]
Virulence factors
Many microorganisms found in endodontic infections are Exotoxins: Exotoxins are toxins released by a living cell,
commensals in the oral cavity, which have gained entry which can trigger excessive and aberrant activation
into the pulp tissue of the root canal typically via the of T cells.[37] Bacterial toxins can also target other
caries process. Identification and characteristics of specific microorganisms, e.g., bacteriocins, proteinaceous toxins
virulence factors that might play a role in endodontic produced by bacteria are bacteriostatic or bacteriocidal to
infections are discussed here. other bacteria.[38]
LPS: This is also known as endotoxin.[23] LPS is an integral Extracellular proteins: Many of these extracellular proteins
part of cell wall of Gram negative bacteria. When are enzymes which are produced by bacteria. These
released, LPS has numerous biologic effects including the enzymes are released during bacterial cell lysis which
236 Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
contributes to spread of infection, including proteases that via leakage. It is difficult to differentiate between the
neutralize immunoglobulins and complement components.[39] microorganisms remaining from primary infections and
Enzymes like hyaluronate lyase, chondroitin sulphatase, new microorganisms contributing to the secondary
beta glucuronidase, DNase and acid phosphatase contribute infection. The remaining microorganisms from primary
to tissue disintegration. infection should have maintained the viability throughout
the treatment procedure. This might occur as a result of an
Short-chain fatty acids: These are major by-products of inability of chemomechanical instrumentation and because
fermentation process performed by obligate anaerobes, of inaccessible locations of bacteria in isthmuses, accessory
and include butyric acid and propionic acid. These acids canal and apical regions of canals.[49]
stimulate the inflammatory response and inflammatory
cytokine release which contribute to infection process.[40,41] Success of non-surgical endodontic treatment is limited by
the heterogeneity of patients and difficulty in maintaining
Polyamines: Polyamines are small, polycationic molecules standardized clinical conditions. Thus, a thorough
like putrescine, cadaverine, spermidine and spermine knowledge and understanding of these persistent
which contribute to clinical symptoms like pain (including endodontic microbes helps us to decide on surgical
percussion pain) and formation of sinus tract.[42] These treatment or retreatment.
polyamines act by modulating a variety of ion channels.[43]
BACTERIAL BIOFILMS
Superoxide anions: Superoxide anions are biologically
toxic and highly reactive free radicals. These are produced Biofilm is a mode of microbial growth where dynamic
by few bacterial species and also by the cells of immune communities of interacting sessile cells are irreversibly
system. They cause lysis of erythrocytes[44] and are involved attached to a solid substratum, as well as to each other,
in interspecies interaction. and are embedded in a self-made matrix of extracellular
polymeric substances.[50] The microorganisms living in a
However, diverse arrays of virulence factors are available community must have the following four basic criteria:[51]
to modulate the participation of microorganisms in host– 1. possess the abilities to self-organize (autopoiesis),
microbe interactions. An absolute cause and relationship 2. resist environmental perturbations (homeostasis),
occurs between the virulence factors and clinical signs and 3. be more effective in association than in isolation
symptoms in root canal infections. Apart from these, there (synergy) and
are additional mechanisms by which the microorganisms 4. respond to environmental changes as a unit rather
might modulate the infection process, which include the than single individuals (communality).
ability of some intracellular bacteria to inactivate the killing
mechanisms of phagocytic cells and thereby avoid being killed Development of biofilm
by macrophages and neutrophils.[45] In addition, some bacteria Bacteria can form biofilms on any surface that is bathed in
can genetically vary their surface antigens, thus causing a nutrient-containing fluid. The three major components
difficulty for the immune system to target these organisms.[46] involved in biofilm formation are bacterial cells, a solid
A thorough understanding of these virulence factors helps to surface and a fluid medium.
identify the therapeutic targets in endodontic infections.
Biofilm formation occurs in three stages given below.
IMPORTANCE OF UNDERSTANDING
MICROBIOLOGY FOR THE SUCCESS Stage 1: Adsorption of inorganic and organic molecules
OF NON-SURGICAL AND SURGICAL to the solid surface occurs, leading to the formation of
ENDODONTIC TREATMENT conditioning layer.
The presence of microorganisms in the dental pulp is Stage 2: Adhesion of microbial cells to the conditioned layer:
directly associated with the development of periapical There are many factors that affect the bacterial attachment
disease. Chemomechanical preparation of the infected root like pH, temperature, surface energy of the substrate,
canal using antimicrobial agents, followed by obturation nutritional availability, time of contact of bacteria, bacterial
and coronal restoration, provides a favorable outcome. cell surface charge and surface hydrophobicity. The bacteria
However, failure of root canal treatment sometimes occurs substrate interaction occurs in three phases:
due to persistent or secondary intraradicular infection.[47,48] • Phase 1: Transport of microbe to substrate surface
which is mediated by fimbriae, pili, flagella and
Microorganisms found in failed endodontically treated extracellular polysaccharides (glycocalyx).
teeth have either remained in the root canal from previous • Phase 2: Initial non-specific microbial–substrate
treatment or have entered during or after treatment adherence which occurs due to combination of
Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4 237
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
electrostatic attraction, covalent and hydrogen Biomaterial-centered infection
bonding, dipole and hydrophobic interaction. Biomaterial centered infection is caused when bacteria
• Phase 3: Specific microbial substrate adherence phase. adhere to an artificial biomaterial surface and form biofilm
In this phase, adhesin or ligand on the bacterial cell structures.[57] Presence of biomaterials in close proximity
surface binds to receptors on the substrate. to the host immune system can increase the susceptibility
to biofilm. In endodontics, biomaterial-centered biofilms
Stage 3: Development of biofilm and biofilm expansion form on root canal obturating materials. These biofilms can
occurs. In this stage, monolayer of microbes attracts be intraradicular or extraradicular depending on whether
secondary colonizers forming microcolony, and the the obturating material is within the root canal or has
collection of microcolonies gives rise to the final structure extruded beyond the root apex.
of biofilm.[52,53]
CONCLUSION
Endodontic biofilms
Endodontic microbiota is established to be less diverse Infection of the root canal is not a random event. The type
compared to oral microbiota. Progression of infection alters and mix of the microbial flora develop in response to the
the nutritional and environmental status within the root surrounding environment. Microorganisms that establish
canal, making it more anaerobic with depleted nutritional in the untreated root canal experience an environment
of nutritional diversity. In contrast, well-filled root canal
levels. These changes offer a tough ecological niche for the
offers the microbial flora a small, dry, nutritionally limited
surviving microorganisms. But complete disinfection of
space. Thus, we should obtain a better understanding of
root canal is very difficult to achieve because of persistent
the characteristics and properties of bacteria and their
microbes in anatomical complexities and apical portion
biofilms along with the environmental changes, to enhance
of root canal. Because biofilm is the manner of bacterial
success.
growth which survives unfavorable environmental and
nutritional conditions, the root canal environment will
favor biofilm formation.
REFERENCES
Endodontic bacterial biofilms can be categorized as 1. Siqueira JF Jr. Microbiology of apical periodontitis. In: PittFord T, editor.
• intracanal biofilms, Essential endodontology. Oxford, UK: Blackwell; 2008. p. 135-96.
2. Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical
• extraradicular biofilms, exposures of dental pulps in germ-free and conventional laboratory rats.
• periapical biofilms and Oral Surg Oral Med Oral Pathol 1965;20:340-9.
3. Bammann LL, Estrela C. Microbiological aspects in endodontics:
• biomaterial-centered infections. Endodontic Science 2009. Vol 1; edition 2:258-81.
4. Dahlen G, Moller A Jr. Microbiology of endodontic infection. In:
Slots J, Taubman MA, editors. Contemporary Oral Microbiology and
Intracanal microbial biofilms immunology. St.Louis: Mosby year Book Inc: 1991. p. 444-55.
5. Torabinejad M. Ung B, Kettering J. Invitro bacterial penetration of coronally
They are microbial biofilms formed on the root canal dentin unsealed endodontically treated teeth. J Endod 1990;16:566-9.
of an endodontically infected tooth.[54] 6. Paster BJ, Olsen I, Aas JA, Dewhirst FE. The breadth of bacterial diversity
in the human periodontal pocket and other oral sites. Periodontol 2000
2006;42:80-7.
Extraradicular microbial biofilms 7. Shah HN, Collins DM. Prevotella, a new genus to include Bacteroides
They are also termed as root surface biofilms which are melaninogenicus and related species formerly classified in the genus
Bacteroides. Int J Syst Bacteriol 1990;40:205-8.
formed on the root (cementum) surface adjacent to the 8. Conrads G, Gharbia SE, Gulabivala K, Lampert F, Shah HN. The use
root apex of endodontically infected teeth.[46] of a 16S rDNA directed PCR for the detection of endodontopathogenic
bacteria. J Endod 1997;23:433-8.
9. Dahle UR, Titterud Sunde P, Tronstad L. Treponemas and endodontic
Extraradicular biofilms are reported with asymptomatic infections. Endod Top 2003;6:160-70.
10. Sakamoto M, Rocas IN, Siqueira JF Jr, Benno Y. Molecular analysis of
periapical periodontitis and in chronic apical abscesses bacteria in asymptomatic and symptomatic endodontic infections. Oral
with sinus tracts. Sometimes, the extraradicular biofilm Microbiol Immunol 2006;21:112-22.
11. Vianna ME, Conrads G, Gomes BP, Horz HP. Identification and
becomes calcified and gets associated with periapical quantification of archaea involved in primary endodontic infections. J
inflammation and delayed periapical healing in spite of Clin Microbiol 2006;44:1274-87.
adequate orthograde root canal treatment.[55] 12. Glick M, Trope M, Bagasra O, Pliskin ME. Human immunodeficiency
virus infection of fibroblasts of dental pulp in seropositive patients. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 1991;71:733-6.
Periapical microbial biofilms 13. Slots J. Herpes viruses in periodontal diseases. Periodontol 2000
2005;38:33-62.
They are isolated biofilms found in the periapical region 14. Sunde PT, Olsen I, Debelian GJ, Tronstad L. Microbiota of periapical
of endodontically infected teeth. Periapical biofilms lesions refractory to endodontic therapy. J Endod 2002;28:304-10.
15. Sunde PT, Tronstad L, Eribe ER, Lind PO, Olsen I. Assessment of
may or may not be dependent on the root canal. These periradicular microbiota by DNA – DNA hybridization. Endod Dent
microorganisms have the ability to overcome host defense Traumatol 2000;16:191-6.
16. Tronstad L, Barnett F, Riso K, Slots J. Extraradicular endodontic
mechanisms, thrive in the inflamed periapical tissue and infections. Endod Dent Traumatol 1987;3:86-90.
subsequently induce a periapical infection.[56] 17. Gatti JJ, Dobeck JM, Smith C, White RR, Socransky SS, Skobe Z.
238 Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4
Lakshmi Narayanan and Vaishnavi: Endodontic microbiology
Bacteria of asymptomatic periradicular endodontic lesions identified by Enterococcus faecalis pheromone – responsive conjugative plasmid
DNA – DNA hybridization. Endod Dent Traumatol 2000;16:197-204. pPDI. J Bacteriol 1997;179:7843-55.
18. Love RM. Enterococcus faecalis - a mechanism of its role in endodontic 39. Sundqvist G, Carlsson J, Herrmann B, Tarnvik A. Degradation of human
failure. Int Endod J 2001;34:399-405. immunoglobulins G and M and complement factors C3 and C5 by
19. Gopikrishna AV, Kandaswamy D, Jeyavel RK. Comparative evaluation black-pigmented bacteroides. J Med Microbiol 1985;19:85-94.
of the antimicrobial efficacy of five endodontic root canal sealers against 40. Niederman R, Zhang J, Kashket S. Short chain carboxylic acid
Enterococcus faecalis and Candida albicans. J Conserv Dent 2006;9:2-12. Stimulated, PMN – mediated gingival inflammation. Crit Rev Oral Biol
20. Henderson B, Wilson M. Commensal communism and the oral cavity. J Med 1997;8:269-90.
Dent Res 1998;77:1674-83. 41. Kurita-Ochiai T, Hashizume T, Yonezawa H, Ochiai K, Yamamoto M.
21. Moine P, Abraham E. Immunomodulation and sepsis: Impact of the Characterization of the effects of butyric acid on cell proliferation,
pathogen. Shock 2004;22:297-308. cell cycle distribution and apoptosis. FEMS Immunol Med Microbiol
22. Lawrence JG. Common themes in the genome strategies of pathogens. 2006;47:67-74.
Curr Opin Genet Dev 2005;15:584-8. 42. Maita E, Horiuchi H. Polyamine analysis of infected root canal contents
23. Schein B, Schilder H. Endotoxin content in endodontically involved related to clinical symptoms. Endod Dent Traumatol 1990;6:213-7.
teeth. J Endod 1975;1:19-21. 43. Thomas T, Thomas TJ. Polyamines in Cell growth and cell death:
24. Horiba N, Maekawa Y, Yamauchi Y, Ito M, Matsumoto T, Nakamura Molecular mechanisms and therapeutic applications. Cell Mol Life Sci
H. Complement activation by lipopolysaccharides purified from root 2001;58:244-58.
canals. Oral Surg Oral Med Oral Pathol 1992;74:648-51. 44. Falcioni GC, Coderoni S, Tedeschi GG, Brunori M, Rotilio G. Red cell
25. Dwyer TG, Torabinejad M. Radiographic and histologic evaluation of the lysis induced by microorganisms as a case of superoxide and hydrogen
effect of endotoxin on periapical tissues of the Cat. J Endod 1980;7:31-5. peroxide dependent hemolysis mediated by oxyhemoglobin. Biochim
26. Khabbaz MG, Anastasiadis PL, Sykaras SN. Determination of endotoxins Biophys Acta 1981;678:437-41.
in the vital pulp of human carious teeth: Association with pulpal pain. 45. Jansen A, Yu J. Differential gene expression of pathogens inside infected
Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:587-93. hosts. Curr Opin Microbiol 2006;9:138-42.
27. Jacinto RC, Gomes BP, Shah HN, Ferraz CC, Zaia AA, Souza-Filho FJ. 46. Frank SA, Barbour AG. Within-host dynamics of antigenic variation.
Quantification of endotoxins in necrotic root canals from symptomatic Infect Genet Evol 2006;6:141-6.
47. Nair PN. On the causes of persistent apical periodontitis, a review. Int
and asymptomatic teeth. J Med Microbiol 2005;54:777-83.
Endod J 2006;39:249-81.
28. Wang JE, Jørgensen PF, Almlöf M, Thiemermann C, Foster SJ, Aasen
48. Siqueira JF Jr. Aetiology of root canal treatment failure: Why well-treated
AO, et al. Peptidoglycan and lipoteichoic acid from Staphylococcus
teeth can fail. Int Endod J 2001;34:1-10.
aureus induce tumor necrosis factor alpha, interleukin 6 (IL-6) and IL-
49. Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root
10 production in both T cells and monocytes in a human whole blood
canal system of human mandibular first molars with primary apical
model. Infect Immun 2000;68:3965-70.
periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med
29. Myhre AE, Aasen AO, Thiemermann C, Wang JE. Peptidoglycan - a
Oral Pathol Oral Radiol Endod 2005;99:231-52.
endotoxin in its own right? Shock 2006;25:227-35.
50. Costerton JW, Lewandowski Z, DeBeer D, Caldwell D, Korber D, James
30. Wang JE, Jørgensen PF, Ellingsen EA, Almiöf M, Thiemermann C, Foster SJ,
G. Biofilms, the customized microniche. J Bacteriol 1994;176:2137-42.
et al. Peptidoglycan primes for LPS – induced release of proinflammatory
51. Caldwell DE, Atuku E, Wilkie DC, Wivcharuk KP, Karthikeyan S, Korber
cytokines in whole human blood. Shock 2001;16:178-82. DR, et al. Germ theory vs. community theory in understanding and
31. Hogg SD, Whiley RA, De Soet JJ. Occurrence of Lipoteichoic acid in oral controlling the proliferation of biofilms. Adv Dent Res 1997;11:4-13.
streptococci. Int J Syst Bacteriol 1997;47:62-6. 52. Costerton J, Stewart PS, Greenberg EP. Bacterial biofilm: A common
32. Cohen J. Mechanisms of tissue injury in sepsis: Contrasts between cause of persistent infections. Science 1999;284:1318-22.
gram positive and gram negative infection. J Chemother 2001;13:153-8. 53. Cowan M, Taylor KG, Doyle RJ. Energetics of the initial phase of
33. Tang G, Yip HK, Samaranayake LP, Chan KY, Luo G, Fang HH. Direct adhesion of streptococcus sanguis to hydroxyapatite. J Bacteriol
detection of cell surface interactive forces of sessile, fimbriated and non- 1987;169:2995-3000.
fimbriated Actinomyces spp. using atomic force microscopy. Arch Oral 54. Nair P. Apical periodontitis: A dynamic encounter between root canal
Biol 2004;49:727-38. infection and host response. Periodontol 2000 1997;13:121-48.
34. Kinder SA, Holt SC. Characterization of coaggregation between 55. Harn WM, Chen YH, Yuan K, Chung CH, Huang PH. Calculus-like
Bacteroides gingivalis T22 and Fusobacterium nucleatum T18. Infect deposit at apex of tooth with refractory apical periodontitis. Endod Dent
Immun 1989;57:3425-33. Traumatol 1998;14:237-40.
35. Beveridge TJ. Structures of gram-negative cell walls and their derived 56. Hornef M, Wick MJ, Rhen M, Normark S. Bacterial strategies for
membrane vesicles. J Bacteriol 1999;181:4725-33. overcoming host innate and adaptive immune responses. Nat Immunol
36. Kuehn MJ, Kesty NC. Bacterial outer membrane vesicles and the host- 2002;113:1033-40.
pathogen interaction. Genes Dev 2005;19:2645-55. 57. Wilson M. Susceptibility of oral bacterial biofilm to antimicrobial agents.
37. Llewelyn M, Cohen J. Superantigens: Microbial agents that corrupt J Med Microbiol 1996;44:79-87.
immunity. Lancet Infect Dis 2002;2:156-62.
38. Tomita H, Fujimoto S, Tanimoto K, Ike Y. Cloning and genetic and
Source of Support: Nil, Conflict of Interest: None declared.
sequence analyses of the bacteriocin 21 determinant encoded on the
Journal of Conservative Dentistry | Oct-Dec 2010 | Vol 13 | Issue 4 239
Potrebbero piacerti anche
- Respiratory PhysiologyDocumento37 pagineRespiratory PhysiologyclarisseNessuna valutazione finora
- Dental Casting Procedures: Snegha S 2Nd Yr BdsDocumento32 pagineDental Casting Procedures: Snegha S 2Nd Yr BdsKeerthikaNessuna valutazione finora
- CaninesDocumento42 pagineCaninesKeerthikaNessuna valutazione finora
- PD-Introduction - Indirect-16-12-14 PDFDocumento35 paginePD-Introduction - Indirect-16-12-14 PDFKeerthikaNessuna valutazione finora
- PD-Introduction - Indirect-16-12-14 PDFDocumento35 paginePD-Introduction - Indirect-16-12-14 PDFKeerthikaNessuna valutazione finora
- Gypsum Products - Dr. Rabab3aDocumento5 pagineGypsum Products - Dr. Rabab3aKeerthikaNessuna valutazione finora
- Dental Anatomy KDocumento3 pagineDental Anatomy KKeerthikaNessuna valutazione finora
- Mandibular IncsorsDocumento42 pagineMandibular IncsorsKeerthikaNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- USMLE Step 1 First Aid 2021-148-184Documento37 pagineUSMLE Step 1 First Aid 2021-148-184mariana yllanesNessuna valutazione finora
- Mechanisms of Disease and Inmunity - Equine Internal Medicine 4th EditionDocumento76 pagineMechanisms of Disease and Inmunity - Equine Internal Medicine 4th EditionASLY LUCIANA MARQUEZ GALLARDONessuna valutazione finora
- Deadly Diseases and Epidemics - Plague, 2nd Edition (121p)Documento121 pagineDeadly Diseases and Epidemics - Plague, 2nd Edition (121p)LinneferNessuna valutazione finora
- Dougan 2014Documento23 pagineDougan 2014alfredoibcNessuna valutazione finora
- Bacterial Skin and Soft Tissue InfectionsDocumento24 pagineBacterial Skin and Soft Tissue InfectionsHafdzi Maulana PK-163Nessuna valutazione finora
- 2002 SIPAbstractsDocumento83 pagine2002 SIPAbstractsAlonso ArroyoNessuna valutazione finora
- The Pathobiology of PeritonitisDocumento12 pagineThe Pathobiology of PeritonitisTri PutraNessuna valutazione finora
- Micr Biology: Chapter 4, Part ADocumento29 pagineMicr Biology: Chapter 4, Part ApradipdeshmukhNessuna valutazione finora
- Food Poisoning Caused by Bacteria (Food Toxins) - IntechOpenDocumento28 pagineFood Poisoning Caused by Bacteria (Food Toxins) - IntechOpenRubina KhatunNessuna valutazione finora
- Model Answer: Important Instructions To ExaminersDocumento24 pagineModel Answer: Important Instructions To ExaminersnikkilakhanNessuna valutazione finora
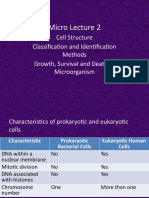
- Micro Lecture 2: Cell Structure Classification and Identification Methods Growth, Survival and Death of MicroorganismDocumento78 pagineMicro Lecture 2: Cell Structure Classification and Identification Methods Growth, Survival and Death of MicroorganismJaellah MatawaNessuna valutazione finora
- Shrivastava Bhanu, Shrivastava Vandana, Shrivastava ArchanaDocumento3 pagineShrivastava Bhanu, Shrivastava Vandana, Shrivastava Archana420192420192Nessuna valutazione finora
- Chapter 3.2-Morphology and Physiology of BacteriaDocumento96 pagineChapter 3.2-Morphology and Physiology of BacteriaAkbar SaleemNessuna valutazione finora
- Basic Bacteriology McqsDocumento25 pagineBasic Bacteriology Mcqshassan qureshi100% (1)
- Acellular CarbsDocumento15 pagineAcellular CarbsstarmittNessuna valutazione finora
- Neisseria Meningitidis PDFDocumento8 pagineNeisseria Meningitidis PDFmulyadiNessuna valutazione finora
- Imunologie MedicalaDocumento224 pagineImunologie MedicalaTo Ma100% (10)
- B.Inggris IPA-IPS P12 A PDFDocumento8 pagineB.Inggris IPA-IPS P12 A PDFShella KhoiriyahNessuna valutazione finora
- Chapter 1: Bacterialcell Structure, Physiology, Metabolism, and GeneticsDocumento19 pagineChapter 1: Bacterialcell Structure, Physiology, Metabolism, and GeneticsNico Loko100% (1)
- Biological Properties of Essential OilsDocumento20 pagineBiological Properties of Essential OilsDébora MarchesineNessuna valutazione finora
- Micro (Volume 1)Documento67 pagineMicro (Volume 1)Dr. noor taherNessuna valutazione finora
- De Pyro Ge NationDocumento21 pagineDe Pyro Ge NationsanthoshkurvaNessuna valutazione finora
- 69 Haines Ely-Is Psoriasis A Bowel DiseaseDocumento14 pagine69 Haines Ely-Is Psoriasis A Bowel DiseaseJoe DoeNessuna valutazione finora
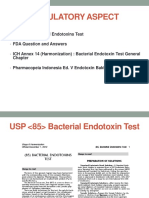
- Bacterial Endotoxin Test 14 03 17 PDFDocumento61 pagineBacterial Endotoxin Test 14 03 17 PDFsumarni rikamNessuna valutazione finora
- Porphyromonas Gingivalis: An: Overview of Periodontopathic Pathogen Below The Gum LineDocumento14 paginePorphyromonas Gingivalis: An: Overview of Periodontopathic Pathogen Below The Gum LineSasa AprilaNessuna valutazione finora
- Microbial Physiology Notes 1Documento9 pagineMicrobial Physiology Notes 1Genalin M. Escobia-Bagas100% (1)
- A Comparison of Two Models of Experimental Periodontitis in RatsDocumento8 pagineA Comparison of Two Models of Experimental Periodontitis in RatsRoza NafilahNessuna valutazione finora
- Can You Diagnose Fibromyalgia With A Poop Test - DR SchillerDocumento7 pagineCan You Diagnose Fibromyalgia With A Poop Test - DR SchillerMaxOzNessuna valutazione finora
- 1 PB PDFDocumento6 pagine1 PB PDFAl Bukhari SubulussalamNessuna valutazione finora
- Kagaw Notes 100Documento33 pagineKagaw Notes 100Stephany PolinarNessuna valutazione finora