Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Post-Anesthetic Discharge Scoring System Validated
Caricato da
nasrijaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Post-Anesthetic Discharge Scoring System Validated
Caricato da
nasrijaCopyright:
Formati disponibili
UTTERWORTH
EINEMANN
A Post-Anesthetic Discharge
Scoring System for Home
Readiness after
Ambulatory Surgery
Frances Chung, FRCPC,*
Vincent W.S. Ghan, FRCPC,? Dennis Ong, MD$
Department of Anaesthesia, Toronto Western Division, Toronto Hospital, and
University of Toronto, Toronto, Canada.
Study Objective: To evaluate the validity and reliability of an objective scoring system,
the Post-Anesthetic Discharge Scoring System (PADSS), which was compared against
existing Clinical Discharge Criteria in the ambulatory surgery unit of our hospital.
Design: randomized, open study.
Setting: Ambulatory surgery unit at a university teaching hospital.
Patients: 247 ambulatory surgery patients undergoing general anesthesia.
Interventions: One hour after the operation, the initial assessment using PADSS and
the Clinical Discharge Criteria was made by an independent observer. Evaluations were
repeated at 30-minute intervals until patients obtained a Post-Anesthetic Discharge
Score of at least 9 and fulfilled the Clinical Discharge Criteria.
Measurements and Main Results: There was a close correlation betweenthe end of
anesthesia to time patients were fit for discharge using either PADSS or the Clinical
Discharge Criteria (Pearson’s Correlation Coefficient r = 0.89). The internal consis-
tency reliability of PADSS (alpha = 0.65) was superior to that of the Clinical Dis-
charge Criteria (alpha = 0.14).
Conclusions: We have found PADSS to have superior measurement scaling and
diagnostic properties.
Keywords: Ambulatory surgery; patient discharge; postoperative
complications.
*Associate Professor of Anaesthesia, Uni-
versity of Toronto
TAssistant Professor of Anesthesia, Univer-
sity of California, San Francisco Introduction
*Research Assistant in Anaesthesia, Uni- Ambulatory surgery is becoming more common and not only involves simple
versity of Toronto and short surgical procedures on healthy patients but the trend is towards
Address reprint requests to Dr. Chung at longer procedures in infants, geriatric, and debilitated patients.’ It is pre-
the Toronto Western Division, The Toron- dicted that by the end of this decade, 60% of the hospitals’ surgical caseload
to Hospital, 399 Bathurst Street, Toronto, may be performed on an ambulatory basis.2 The question of how long pa-
Ontario, Canada M5T 2S8, Canada. tients should remain in hospital following ambulatory surgery before they can
Received for publication May 3 1, 1994; re- be discharged safely is crucial to future developments in this area of care.3
vised manuscript accepted for publication Essential to the quality of patient care is the safe timing of patient dis-
February 2, 1995. charge, in relation to recovery from general anesthesia, regional, or local
Journal of Clinical Anesthesia 7:500-506, 1995
0 1995 by Elsevier Science Inc. 0952-8180/95/$10.00
655 Avenue of the Americas, New York, NY 10010 SSDI 0952~81S0(95)00130-A
Ambulatory discharge scoring system: Chung et al.
anesthesia with sedation. At the time of discharge from Materials and Methods
the ambulatory surgery unit, the patients should be
home-ready, clinically stable and able to rest at home
under the care of a responsible adult. The ability to After obtaining Institutional Human Ethics Committee
ambulate, the level of hydration, and the ability to tol- approval, patients scheduled for ambulatory surgery
erate oral intake are unique to the ambulatory surgical were selected at random and informed consent was ob-
patient.4 The time course of recovery can be divided tained. The study included 247 patients who had re-
into early recovery, intermediate recovery, ;and late re- ceived general anesthesia for a variety of operative pro-
covery.5 Early recovery is the time interval during which cedures. After the operation, they were transported to
patients emerge from anesthesia, recovering their pro- the postanesthesia care unit. The initial assessment using
tective reflexes and motor activity. Intermediate recov- PADSS and the Clinical Discharge Criteria was made by
ery is the period during which coordination and physi- an independent investigator not directly involved in the
ologic function normalize and the patient may be care of the patient one hour after the operation (Figure
considered in a state of “home-readiness” and is able to 1). Subsequently, the evaluation was repeated at 30-
return home in the company of a responsible person. minute intervals until the patient obtained a Post-
Later recovery, which can be hours to days, is the period Anesthetic Discharge Score of at least 9 and fulfilled the
after which the patient has fully recovered and is capable Clinical Discharge Criteria, respectively. The hospital
of full psychomotor functioning, including returning to personnel directly involved in the care of the patients
work or driving. were unaware of the scores obtained, and the decision to
Several discharge criteria have been described but discharge the patients was made independently by hos-
none has been evaluated for their validity and reliabil- pital personnel according to the Clinical Discharge Cri-
ity. 611 The patient’s readiness for discharge needs to be teria. The time that the patients were actually dis-
addressed in a simple, clear, reproducible manner. charged from the ambulatory surgery unit was
Nursing staff need to be able to evaluate th.e postoper- recorded.
ative course of the patient in a systemic wa.y and meet To eliminate intraobserver and interobserver bias,
guidelines to seek physician consultation when neces- another 80 patients scheduled for dilatation and curet-
sary.6 tage (D&C) were studied. For the elimination of intraob-
In this study, we have designed a simple cumulative server bias, two investigators, one using PADSS and the
index, the Post-Anesthetic Discharge Scoring System other using Clinical Discharge Criteria, assessed 40 pa-
(PADSS), to measure home-readiness of ambulatory sur- tients at 30-minute intervals. To determine interob-
gery patients. We have evaluated its validity and reliabil- server agreement, two investigators assessed 40 patients
ity against the existing clinical discharge criteria in the separately using both PADSS and the Clinical Discharge
ambulatory surgery unit of The Toronto Hospital, To- Criteria at 30-minute intervals.
ronto Western Division. PADSS is based on five main criteria: (1) vital signs-
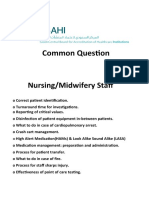
post AnaesthetkDischarge Scoring System (PADS) Clinical Discharge Criteria (CDC)
1. Vital Signs 1. Stable vital signs
2 = Within 20% of preoperative value 2. Patient is alert and oriented
1 = 2040% of preoperative value 3. Patient is free of nausea and/or vomiting
0 = > 40% preoperativevalue 4. Steady of gait
2. Activity and mental status 5. Patient has no significant bleeding
2 = Oriented x3 AND has a steady gait
1 = Oriented x3 OR has a steady gait
0 = Neither
3. Pain, nausea and/or vomiting
2 = Minimal
1 = Moderate, having required treatment
0 = Severe, requiring trealtment
4. Surgical bleeding
2 = Minimal
1 = Moderate
0 = Severe
5. Intake and output
2 = Has had PO fluids AND voided
1 = Has had PO fluids OR voided
0 = Neither
Total pads score is 10; Score 2 9 ccmidered jit for dischaqe
Figure I. The Post-Anesthetic Discharge Scoring System and the Clinical Discharge Criteria used in our ambulatory surgery
unit. PO = oral administration.
J. Clin. Anesth., vol. 7, September 1995 501
Original Contributions
ApPenaix . Post-Operative Evaluation Phone Call
Date and time of post-op call --- I I -Hn
Problems since discharge:
Was there any bleeding significant enough for you to return to
the hospital or to your doctor? ( )Ys( )No
Do you have a sore throat? ( >Yw( )No
Did you have any hoarseness of voice? ( )Y-( )No
Did you feel you had a temperature? ( )Y-( )No
Did you experience any pain at the operative area? ( >Yw( )No
Did you experience any pain at the injection site? ( )Yes( INo
Did you experience any pain in other areas? ( )Y-( )No
Have you been nauseous or felt that you wanted to vomit? ( )Y=J( )No
Did you actually throw up? ( )Ya( )No
Did you experience any headache? ( )Y=J( )No
Did you lind yourself very sleepy or difficult to wake-up? ( )Y@( )No
Did you feel faint, or lightheaded? ( )Y-( )No
Do you feel any form of generalized discomfort, or weakness? ( >Ym( )No
Do you have any other complaints?
What medications did you take?
On a scale of 1 to 10, 1 being no activity and 10 being back to your normal activities, where would you rate
yourself? (Score o-lo)*
Did you have to go back to the ER or the hospital? ( )Y-( )No
Did you have to call you doctor since discharge? ( )Yes( INo
Reason:
Do you wish to make any additional comments?
blood pressure, heart rate, respiratory rate, and temper- from 0 to 2, and a summated score of 9 to 10 indicates
ature; (2) activity and mental status; (3) pain or nausea that patient is fit for discharge.
and/or vomiting; (4) surgical bleeding, and (5) intake/ Qualifications for discharge home included: 1) a post-
output (Figwe 1). Each of the main criteria is graded operative discharge score of greater than or equal to 9;
502 J. Clin. Anesth., vol. 7, September 1995
Ambulatq discharge scoring system: Chung et al.
Table 1. Demographic Data ric test (Mann-Whitney) and the Chi square test. Pear-
son’s Correlation was used to assess the correlation be-
Arthroscopy, tween the times home-readiness was achieved by PADSS
Laparoscopy and the Clinical Discharge Criteria.
and minor When measurements on distinct items are combined
D&C surgery
to a single summary score, statistical evidence that the
items form a scale, or that the scale is internally cohesive,
No. of patients 151 96
must be demonstrated. ‘* Computation of the internal
Gender 151 F 43M:53F
27 t 9 38k 11
consistency reliability coefficients (Cronbach’s Alpha)
Age (yrs) was done to assess the internal consistency of the mea-
ASA physical
status surement scales in all the data.‘*,r3 Cronbach’s Alpha
I 141 75 increases directly with the number of items in the scale
II 9 21 and with the heterogeneity of the individuals mea-
III 1 0 sured. l3 The Cronbach’s Alpha is similar to Pearson’s
Duration of Coefficient in that the higher the value, the better the
Anesthesia internal consistency. Interobserver agreement was as-
(min) Mean + sessed using kappa statisticsI The Kappa Coefficient is
SEM 20 * 7 62 f 26
a measure of interrater agreement beyond what would
End of anesthesia
to PAD% (min) 115 (10 to 210) 125 (0 to 385) be expected by chance alone. Kappa is appropriate when
End of anesthesia the measurement or rating of individuals is on a cate-
to CDC (min) 120 (10 to 230) 140 (0 to 385) gorical or ordinal scale. A Kappa of 0 reflects agreement
End of anesthesia at chance level, while a Kappa of 1.00 reflects perfect
to actual agreement beyond chance. A Kappa of greater than
discharge (min) 170 (20 to 351)* 220 (60 to 485)* 0.75 denotes excellent agreement between the investiga-
tors, i.e. the test is highly reliable. A Kappa between 0.4
Note: D & C = dilatation and curettage; PADSS = Post-Anesthetic
Discharge Scoring System; CDC = Clinical Discharge Criteria.
and 0.75 means good agreement and moderate reliabil-
ity, and a Kappa less than 0.4 means poor agreement
End of Anesthesia to PADS& to CDC, and to actual discharge data
are medians (range).
and poor reliability. Data are presented as medians
(range) or means k SEM. A p value less than 0.05 was
*p < 0.05.
considered statistically significant.
and 2) presence of a competent adult to accompany pa-
tient home. All patients were interviewed 24 hours post- Results
operatively by telephone with a standardized question-
naire to document the postoperative course of the TWO hundred forty-seven patients were entered into the
patient and to detect delayed complications after dis- study. The demographic and clinical characteristics of
charge (Appendix). the patients are summarized in Table 1. The surgical
procedures included 15 1 D&Cs (61.1%), 58 arthrosco-
pies (23.5%), 20 laparoscopies (S.l%), and other minor
Statistical Analysis
surgical procedures (7.3%). The study population was
All data were stored in a computerized database and divided into two groups: D&C (mean duration of anes-
compared for statistical difference using a rmnparamet- thesia of 20 minutes), and other procedures: arthros-
1 1.6 2 2.5 3 3.5
HOURS POSTOP
Figure 2. Percentage of dilatation and curettage patients fit for discharge using the Post-Anesthetic Discharge
Scoring System and the Clinical Discharge Criteria. Postop = postoperative.
J. Clin. Anesth., vol. 7, September 1995 503
Original Contributions
1oc)’
5 601-’
:
T
H 60
P
t: 40 /
%
,
20
0 1
Figure 3. Percentage of patients fit for discharge using the Post-Anesthetic Discharge Scoring System and the
Clinical Discharge Criteria after undergoing arthroscopy, laparoscopy or other minor surgical procedures,
Postop = postoperative.
copy, laparoscopy, and minor surgeries (mean duration anesthesia while coefficients at all other times were close
of anesthesia of 62 minutes). to 0. The Pearson’s Correlation coefficient for the inde-
At 2.5 hours postoperatively, 96% of the patients who pendent observations by two investigators on 40 D&C
had D&C could have been discharged using PADSS patients was higher, r = 0.79.
compared to 94.7% patients using the Clinical Discharge The interrater reliability coefficients (Kappa agree-
Criteria (NS) (F zSure 2). Of the patients in the group with ment coefficients) of PADSS were high, 0.84 at one hour
longer anesthesia, 88.5% were suitable for discharge 3 and 0.80 at 1.5 hours post-surgery respectively. The in-
hours postoperatively by PADSS compared to 86.5% by terrater reliability coefficients of the Clinical Discharge
the Clinical Discharge Criteria (Figure 3). Criteria were 0.87 at one hour and 0.52 at 1.5 hours
On an average, patients who had D&C required 115 post-surgery. All Kappa were significant at a p-value less
(10 to 210) minutes postoperatively to achieve a Post- than 0.001 and were substantial according to the Fleiss
Anesthetic Discharge Score of at least 9 as compared to criteria.14 Kappa agreement coefficients were similar to
120 (10 to 230) minutes needed to satisfactorily fulfill Pearson’s Correlation in that the higher the value, the
the Clinical Discharge Criteria (NS). Patients who un- better the correlation.
derwent arthroscopy, laparoscopy, or other minor sur- There were no hospital readmissions or significant
geries needed 125 (0 to 385) minutes to be discharged postoperative complications by postoperative follow-up
using PADSS versus 140 (0 to 385) minutes needed for telephone call.
satisfactory fulfillment of the Clinical Discharge Criteria
(NV.
The actual postoperative discharge time for the D&C Discussion
patients was 170 (20 to 351) minutes while for the ar-
throscopy/laparoscopy/minor surgeries group was 220 There is a growing need to design a discharge scoring
(60 to 485) minutes. This was significantly longer than system so that home-readiness of patients can be ad-
the time needed to achieve a Post-Anesthetic Discharge dressed in a simple, clear, reproducible manner. It is
Score or fulfill the Clinical Discharge Criteria (Table 1, p important to replace subjective clinical impressions by
< 0.05). The time interval was due to patients obtaining assigning numeric values to parameters indicating
home instructions, making follow-up appointments, recovery so that recovery and achievement of home-
changing into street clothes, and waiting for their escorts readiness become more obvious. The development of
to accompany them home. any scale is a multi-step process, which is aimed at estab-
There was a close correlation between the discharge lishing the scale’s validity and its reliability. A scale is
time assessed by PADSS or the Clinical Discharge Crite- valid if it measures what it intends to measure, while
ria (Pearson’s Correlation Coefficient r = 0.89). reliability refers to its tendency to produce consis-
The internal consistency reliability coefficients (Cron- tent results when applied to the same individual by
bath’s Alpha) of PADSS reached 0.65 overall for the different observers, or by one observer at different
D&C type surgical group. For the arthroscopy/ times.15
laparoscopy/minor surgical group, overall internal con- To determine concurrent validity, we compared the
sistency coefficient reached 0.48 at 150 minutes post sur- discharge times achieved by PADSS with those achieved
gery. In the group with longer anesthesia, the largest by the standard Clinical Discharge Criteria of our hos-
internal consistency reliability coefficient for the Clinical pital. Overall, there was a close correlation in discharge
Discharge Criteria was 0.14 at 120 minutes post- times between the two methods (Pearson’s Correlation
504 J. Clin. Anesth., vol. 7, September 1995
Ambulatory discharge scoring system: Chung et al.
Coefficient r = 0.89). This finding suggests that PADSS surgery unit by the prompt and safe discharge of pa-
can be used to replace the Clinical Discharge Criteria. tients is a cost reduction and labor efficient strategy.
Our results showed that patients stayed longer in hos- Ambulatory surgery in certain procedures is deemed
pital than indicated by the Clinical Discharge Criteria or cheaper even when allowing for treatment failures and
PADSS. If the Clinical Discharge Criteria were strictly readmissions. ‘* However, discharge of patients should
followed, patients undergoing D&C and arthroscopy, be achieved without compromising the quality of patient
laparoscopy, and other minor surgical procedures could care, and the discharge scoring system we developed
have been discharged 50 minutes and 80 minutes sooner enabled us to discharge patients safely. We have now
than actually happened, Delay in discharge may be due discharged 30,000 patients home safely with PADSS.
to failure to evaluate the patients every 30 minutes and These patients had undergone different-types of anes-
escorts not being immediately available to bring patients thesia; general anesthesia, monitored anesthesia care
home. In addition, it is necessary to change thsemind-set and regional anesthesia. The system is used with a com-
and practice habits of physicians and nursing staff to bination of clinical judgment and common sense.
speed up discharge after ambulatory surgery. In conclusion, practical discharge criteria or a post-
A measurement is perceived to be reliable if it yields Anesthetic discharge scoring system should be imple-
essentially the same measure. When it is repeatedly mented in every ambulatory surgery center to ensure
taken under similar conditions on an individual or an safe recovery and discharge after anesthesia. PADSS is
object, the state of the individual or an object is assumed simple, practical, and safe. It establishes a routine of
to be constant. The interrater reliability coefficients of repeated reevaluation of home-readiness, and it pro-
PADSS at 1.0 hour and 1.5 hours post surgery was 0.84 vides a uniform assessment for all outpatients. Home-
and 0.80, respectively, for the D&C patients. The inter- readiness of these patients means that these patients are
rater reliability coefficients of the Clinical Discharge Cri- suitable for discharge from the ambulatory surgery unit
teria, on the other hand, was 0.87 at 1 hour and 0.52 at directly to home. It does not mean street fitness of these
1.5 hours post surgery for the D&C patients. This find- patients. For example, patients who have arthroscopy
ing suggests that PADSS has better interobserver agree- surgery on their knees or lower limb orthopedic surgery,
ment for D&C patients. often do not have steady gait. They are sometimes dis-
The ability to tolerate fluids by mouth before dis- charged by wheelchairs or crutches. Therefore, steady
charge is controversial. Although a patient cannot be gait is never achieved in these patients. Sometimes, el-
discharged when he or she is actively vomiting, the abil- derly patients may have disorientation after sedation
ity to tolerate fluids may not be a necessary criterion for with cataract surgery.lg We discharge these patients
discharge. Schreiner et ~1.‘~ found that requiring chil- home with their spouse. In addition, we also make
dren to drink before hospital discharge appeared to in- home-care arrangements for these patients. Further
crease the rate of vomiting and prolonged thle duration studies on adverse outcomes after discharge are war-
of hospital stay. Similarly, the requirement for patients ranted.
to have voided before discharge is not universally
adopted in most institutions. We have designed a mod-
ified PADSS that has eliminated intake of fluids and has Acknowledgment
voided as a discharge criterion and we are in the process We acknowledgethe assistanceof Dr. C. Seyone and Dr. N. Mati in
of verifying its safety. l7 collecting the data.
In this study, we used 30-minute testing intervals to
evaluate patients. Difference in recovery parameters be-
tween PADSS and the Clinical Discharge Criteria might References
have been missed because of the length of the testing
White PF: Outpatient anesthesia. In: Miller RD (ed): Anesthesia.
intervals. In addition, more frequent testing intervals
New York: Churchill Livingston, 1986: 1895-1919.
probably would result in earlier and shorter discharge
Yee DA, Penning DH: Ambulatory surgery questionnaire. Can
times. / Anaesth 1990;37(4 Pt 2):S8.
To be useful, a scoring system should be practical, Stephenson ME: Discharge criteria in day surgery. J Adu Nurs
simple, easy to remember, and applicable to all postan- 1990;15:601-13.
esthesia situations. Using only the commonly observed 4. Kitz DS, Robinson DM, Schiavone PA, Walsh PR, Conahan TJ
physical signs will avoid any added burden to the post- 3d: Discharging outpatients. Factors nurses consider to deter-
anesthesia care personnel. By assigning numerical val- mine readiness. AORNJ 1988;48:87-91.
ues to parameters indicating patient recovery, progress, 5. Steward DJ, Volgyesi G: Stabilometry: a new tool for the mea-
or lack of it becomes more objective and more easily surement of recovery following general anaesthesia for out-
understood. The scoring system that we have designed is patients. Can Anaesth Sot J 1978;25:4-6.
6. Kuperwasser B, Dierckman D: Quality assurance in ambula-
a simple way of providing uniform assessment for all
tory surgery: “how to do it.” Nurs Manage 1988;19:72A-72C,
patients. It can determine the optimal length of stay in 72F, 72H.
the ambulatory surgery unit so that it is s,afe for the 7. Millar JM: Fitness for discharge after day surgery [Letter].
patient and also may reduce nursing time per patient Anaesthesia 1988;43:418.
and increase the efficiency of nursing staff. 8. Mortensen M, McMullin C: Discharge score for surgical pa-
Reduction in the length of stay in the ambulatory tients. Am J Nurs 1986;86: 1347-9.
J. Clin. Anesth., vol. 7, September 1995 505
Original Contributions
9. Wetchler BV: Postanesthesia scoring system. Discharging am- 15. Carmines EG, Zeller RA: Reliability and validity assessment.
bulatory surgery patients. AORNJ 1985;41:382-4. Sage University paper series on quantitative applications in
10. Korttila K: Recovery period and discharge. In: White PF (ed): the social sequences. Beverly-Hills, CA: Sage Publications,
Outpatient Anesthesia. New York: Churchill Livingston, 1990: 1979.
369-95. 16. Schreiner MS, Nicolson SC, Martin T, Whitney L: Should chil-
11. Pate1 RI: Discharge criteria and postanesthetic complications dren drink before discharge from day surgery? Anesthesiology
following pediatric ambuIatory surgery. J Post An&h Nurs 1992;76:528-33.
1988;3:114-7.
17. Chung F: Are discharge criteria changing? J Clin Anesth
12. Nunnally JC: Psychomettic Theory. New York: McGraw-Hill 1993;5(6 Suppl 1):64S-68%
Book Company, Inc., 1978:229-30.
13. Cracker L, Algina J: Introduction to Classical and Modern Test 18. Davis JE: The major ambulatory surgical center and how it is
Theory. Fort Worth: Holt, Rinhart and Winston, Inc. 1986: developed. Surg Clin North Am 1987;67:671-92.
119-22, 131-54, 157-212. 19. Chung F, Lavelle P, McDonald S, Chung A, McDonald NJ:
14. Fliess JL: Statistical Methodfor Rate and Projmrtion. New York: Cognitive impairment after neuroleptanalgesia in cataract sur-
John Wiley & Sons, 1981:212-36. gery. Anesth Ana% 1989;68:6 14-8.
506 J. Clin. Anesth., vol. 7, September 1995
Potrebbero piacerti anche
- Non Operative ManagementDocumento6 pagineNon Operative ManagementfebriNessuna valutazione finora
- Aldrete Discharge Scoring - Appropriate For Post Anesthesia PhaseDocumento28 pagineAldrete Discharge Scoring - Appropriate For Post Anesthesia PhaseHeather PorterNessuna valutazione finora
- Aldrete ScoreDocumento33 pagineAldrete ScoreIndra PutraNessuna valutazione finora
- Asa 2013Documento1.076 pagineAsa 2013Marwa Mahrous100% (4)
- Bmjopen 2017 016402Documento6 pagineBmjopen 2017 016402Ćatke TkećaNessuna valutazione finora
- AldereteDocumento6 pagineAldereteNadhira W LestariNessuna valutazione finora
- ATLS Tenth EdDocumento45 pagineATLS Tenth Edakreditasi standar2Nessuna valutazione finora
- Aldrete Discharge Scoring - Appropriate For Post Anesthesia Phase PDFDocumento29 pagineAldrete Discharge Scoring - Appropriate For Post Anesthesia Phase PDFSurya BugisNessuna valutazione finora
- Nursing Midwifery Staff CBAHI QuestionsDocumento13 pagineNursing Midwifery Staff CBAHI QuestionsnasserjubranNessuna valutazione finora
- 2022 - Delayed DischargeDocumento4 pagine2022 - Delayed DischargecringlesoreosNessuna valutazione finora
- Evaluation of Two Delirium Screening Tools For Detecting Post-Operative Delirium in The ElderlyDocumento7 pagineEvaluation of Two Delirium Screening Tools For Detecting Post-Operative Delirium in The ElderlySri Siti KhadijahElfNessuna valutazione finora
- Nursing Staff & Anesthesia Technicians in DPUDocumento10 pagineNursing Staff & Anesthesia Technicians in DPUnasserjubranNessuna valutazione finora
- Efficiency and Efficacy of Planning and Care On A Post-Anesthesia Care Unit: A Retrospective Cohort StudyDocumento8 pagineEfficiency and Efficacy of Planning and Care On A Post-Anesthesia Care Unit: A Retrospective Cohort Studypooria shNessuna valutazione finora
- Development, Implementation and Impact of Simple Patient Safety Interventions in A University Teaching HospitalDocumento6 pagineDevelopment, Implementation and Impact of Simple Patient Safety Interventions in A University Teaching HospitalMariale OrdóñezNessuna valutazione finora
- HP May00 Sedat PDFDocumento9 pagineHP May00 Sedat PDFSaurabh SatheNessuna valutazione finora
- Validity and Reliability of A Postoperative Quality of Recovery Score: The Qor-40Documento5 pagineValidity and Reliability of A Postoperative Quality of Recovery Score: The Qor-40Gaetano De BiaseNessuna valutazione finora
- Postoperative Catheter Management After Pelvic Reconstructive Surgery: A Survey of Practice StrategiesDocumento5 paginePostoperative Catheter Management After Pelvic Reconstructive Surgery: A Survey of Practice StrategiesWardah Fauziah El SofwanNessuna valutazione finora
- Using and Understanding Sedation Scoring Systems: A Systematic ReviewDocumento11 pagineUsing and Understanding Sedation Scoring Systems: A Systematic ReviewGihan NakhlehNessuna valutazione finora
- Preoperative Identification of Neurosurgery Patients With A High Risk of In-Hospital Complications: A Prospective Cohort of 418 Consecutive Elective Craniotomy PatientsDocumento11 paginePreoperative Identification of Neurosurgery Patients With A High Risk of In-Hospital Complications: A Prospective Cohort of 418 Consecutive Elective Craniotomy PatientsAzizi AlfyanNessuna valutazione finora
- Postoperative Pain Assessment Tools in Day Surgery Literature ReviewDocumento9 paginePostoperative Pain Assessment Tools in Day Surgery Literature Reviewea0xbk19Nessuna valutazione finora
- Point-Of-Care Testing in Anaesthesiology and Intensive Care - An OverviewDocumento9 paginePoint-Of-Care Testing in Anaesthesiology and Intensive Care - An OverviewDelladuasatu stellaNessuna valutazione finora
- Patient-Initiated Device Removal in Intensive Care Units - A National Prevalence StudyDocumento7 paginePatient-Initiated Device Removal in Intensive Care Units - A National Prevalence StudyJim LinNessuna valutazione finora
- SynopsisDocumento14 pagineSynopsisAqeel AhmadNessuna valutazione finora
- Anesthesia and Sedation Outside ofDocumento9 pagineAnesthesia and Sedation Outside ofPutriRahayuMoidadyNessuna valutazione finora
- Jurnal Skoring SedasiDocumento7 pagineJurnal Skoring SedasiMalvin DyeroNessuna valutazione finora
- Calvillo 2009Documento2 pagineCalvillo 2009Anto RadošNessuna valutazione finora
- Control Del Dolor Postoperatorio en Hemorroidectomía Ambulatoria Mediante Infusión Endovenosa Continua DomiciliariaDocumento7 pagineControl Del Dolor Postoperatorio en Hemorroidectomía Ambulatoria Mediante Infusión Endovenosa Continua DomiciliariaJoaquin MatosNessuna valutazione finora
- Preoperative AssessmentDocumento3 paginePreoperative AssessmentDR BUYINZA TITUSNessuna valutazione finora
- International Journal of Anesthetics and Anesthesiology Ijaa 7 118Documento7 pagineInternational Journal of Anesthetics and Anesthesiology Ijaa 7 118Ferdy RahadiyanNessuna valutazione finora
- POCTDocumento24 paginePOCTHiminNessuna valutazione finora
- Identify: Candidates CareDocumento10 pagineIdentify: Candidates CareJHNessuna valutazione finora
- Early Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients A Randomised Controlled Trial - Barker2010Documento2 pagineEarly Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients A Randomised Controlled Trial - Barker2010RodrigoSachiFreitasNessuna valutazione finora
- Artigo 2 InglesDocumento6 pagineArtigo 2 InglesbeatrizxavierNessuna valutazione finora
- 21 An Discharge CriteriaDocumento13 pagine21 An Discharge CriteriaFajr MuzammilNessuna valutazione finora
- Study of Hospital Discharge Process Viz A Viz Prescribed NABH StandardsDocumento4 pagineStudy of Hospital Discharge Process Viz A Viz Prescribed NABH Standardsrws6vj7699Nessuna valutazione finora
- Artigo Diagnostico de Enf Na UTI PODocumento6 pagineArtigo Diagnostico de Enf Na UTI POMichel Marcossi CintraNessuna valutazione finora
- Shetty, A., & Ravendra, U.S. (2015) - Anesthesia For Day Care Surgery. Nitte University Journal of Health Science, Vol. 5, No. 2, 97-103Documento7 pagineShetty, A., & Ravendra, U.S. (2015) - Anesthesia For Day Care Surgery. Nitte University Journal of Health Science, Vol. 5, No. 2, 97-103kadek gunadiNessuna valutazione finora
- Quality indicators improve anesthesia careDocumento5 pagineQuality indicators improve anesthesia caredrskumarNessuna valutazione finora
- Multicéntrico Lellouche Et AllDocumento7 pagineMulticéntrico Lellouche Et AllterapiafisicapilaresNessuna valutazione finora
- Revista 3Documento7 pagineRevista 3KeylaOrtizIINessuna valutazione finora
- Two-Year Outcome After Endovascular Treatment For Acute Ischemic StrokeDocumento9 pagineTwo-Year Outcome After Endovascular Treatment For Acute Ischemic Strokedoni anandaNessuna valutazione finora
- 10.2478 - Prolas 2014 0023Documento6 pagine10.2478 - Prolas 2014 0023Aliyu Bashir AdamuNessuna valutazione finora
- Anesth Analg-1970-ALDRETE-924-34 PDFDocumento11 pagineAnesth Analg-1970-ALDRETE-924-34 PDFYudiSiswantoWijaya100% (2)
- 2014 - Guidelines For Safety in The Gastrointestinal Endoscopy Unit PDFDocumento10 pagine2014 - Guidelines For Safety in The Gastrointestinal Endoscopy Unit PDFBaim FarmaNessuna valutazione finora
- J Ijnurstu 2017 12 012Documento8 pagineJ Ijnurstu 2017 12 012Osborn KhasabuliNessuna valutazione finora
- Billing & Compliance For Anesthesia Services: Charles Whitten, MD Professor and ChairmanDocumento35 pagineBilling & Compliance For Anesthesia Services: Charles Whitten, MD Professor and ChairmanShimelis AssefaNessuna valutazione finora
- Alexanders Care Patient Surgery 16th Rothrock Test BankDocumento10 pagineAlexanders Care Patient Surgery 16th Rothrock Test BankfahedqNessuna valutazione finora
- Sas 3 Cabahug, Victoria Mae IDocumento3 pagineSas 3 Cabahug, Victoria Mae Ibekbekk cabahugNessuna valutazione finora
- Anesthesia For LiposuctionDocumento26 pagineAnesthesia For Liposuctionjulissand10Nessuna valutazione finora
- Protocolos Weaining 2011Documento14 pagineProtocolos Weaining 2011perla islasNessuna valutazione finora
- Phillips Postanaesthetic 2013Documento11 paginePhillips Postanaesthetic 2013Alex PiecesNessuna valutazione finora
- Protocol of PacuDocumento40 pagineProtocol of PacuMaahiNessuna valutazione finora
- Konsep Clinical PrivilegesDocumento5 pagineKonsep Clinical PrivilegesFebryan Cahya PermanaNessuna valutazione finora
- Use of WhatsApp For Sharing Preanesthesia Evaluation FormDocumento2 pagineUse of WhatsApp For Sharing Preanesthesia Evaluation FormaksinuNessuna valutazione finora
- PacuDocumento93 paginePacunorhafizahstoh89Nessuna valutazione finora
- Recovery of Healthy Patient PACU HandoutDocumento12 pagineRecovery of Healthy Patient PACU HandoutGe NavNessuna valutazione finora
- Healthcare 2Documento8 pagineHealthcare 2Noor KhanNessuna valutazione finora
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANODa EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONessuna valutazione finora
- Case Studies of Postoperative Complications after Digestive SurgeryDa EverandCase Studies of Postoperative Complications after Digestive SurgeryNessuna valutazione finora
- Technical Aspects of Focal Therapy in Localized Prostate CancerDa EverandTechnical Aspects of Focal Therapy in Localized Prostate CancerEric BarretNessuna valutazione finora
- Mo History CRNA Law OrderDocumento30 pagineMo History CRNA Law OrdernasrijaNessuna valutazione finora
- Recognised Standards of Monitoring During Anaesthesia and RecoveryDocumento4 pagineRecognised Standards of Monitoring During Anaesthesia and RecoverynasrijaNessuna valutazione finora
- 1 SM PDFDocumento11 pagine1 SM PDFNeneng EchaNessuna valutazione finora
- Sambutan President of IfnaDocumento1 paginaSambutan President of IfnanasrijaNessuna valutazione finora
- CONSORT Flo of Participants Through Allocation, Follow-UpDocumento5 pagineCONSORT Flo of Participants Through Allocation, Follow-UpnasrijaNessuna valutazione finora
- Registration Form ORP-AdvanceDocumento2 pagineRegistration Form ORP-AdvancenasrijaNessuna valutazione finora
- CONSORT Flo of Participants Through Allocation, Follow-UpDocumento5 pagineCONSORT Flo of Participants Through Allocation, Follow-UpnasrijaNessuna valutazione finora
- 278 816 1 PBDocumento19 pagine278 816 1 PBnasrijaNessuna valutazione finora
- Perangkat Penerjemah Penerjemah SituDocumento1 paginaPerangkat Penerjemah Penerjemah SitunasrijaNessuna valutazione finora
- Study Designs in Epidemiologic Research: Thomas Songer, PHDDocumento33 pagineStudy Designs in Epidemiologic Research: Thomas Songer, PHDnasrijaNessuna valutazione finora
- Translet Trens Isu 2Documento79 pagineTranslet Trens Isu 2nasrijaNessuna valutazione finora
- Perangkat Penerjemah Penerjemah SituDocumento1 paginaPerangkat Penerjemah Penerjemah SitunasrijaNessuna valutazione finora
- Makalah Kepuasan KonsumenDocumento12 pagineMakalah Kepuasan KonsumenrizcamardhaNessuna valutazione finora
- Translet Trens Isu 2Documento79 pagineTranslet Trens Isu 2nasrijaNessuna valutazione finora
- Perangkat Penerjemah Penerjemah SituDocumento1 paginaPerangkat Penerjemah Penerjemah SitunasrijaNessuna valutazione finora
- State-Of-The-Art CFB Technology For Utility-Scale Biomass Power PlantsDocumento10 pagineState-Of-The-Art CFB Technology For Utility-Scale Biomass Power PlantsIrfan OmercausevicNessuna valutazione finora
- Mole Conversions Extra Practice Answer KeyDocumento1 paginaMole Conversions Extra Practice Answer Keyapi-376281962Nessuna valutazione finora
- Lecture Notes in Computational Science and EngineeringDocumento434 pagineLecture Notes in Computational Science and Engineeringmuhammad nurulNessuna valutazione finora
- Newton's Laws of Motion Lab Questions Answer KeyDocumento2 pagineNewton's Laws of Motion Lab Questions Answer KeyAbdulla NassNessuna valutazione finora
- 2023 Key Stage 2 Mathematics Braille Transcript Paper 1 ArithmeticDocumento8 pagine2023 Key Stage 2 Mathematics Braille Transcript Paper 1 ArithmeticMini WorldNessuna valutazione finora
- Astm E1588.1207649 GSRDocumento5 pagineAstm E1588.1207649 GSRjoao carlos100% (1)
- 34 DuPont MECS Startup Shutdown Procedure For MET Plants Sulfuric AcidDocumento4 pagine34 DuPont MECS Startup Shutdown Procedure For MET Plants Sulfuric AcidLouis Andree Bujanda RufattNessuna valutazione finora
- Common MisconceptionsDocumento7 pagineCommon MisconceptionsBoazz750Nessuna valutazione finora
- The Market and Budget ConstraintsDocumento8 pagineThe Market and Budget ConstraintsSnehaNessuna valutazione finora
- Ground Plane AntennaDocumento7 pagineGround Plane AntennaarijeetdguyNessuna valutazione finora
- Perfect Fourths GuitarDocumento8 paginePerfect Fourths Guitarmetaperl6453100% (1)
- Limiting Reagents 1Documento17 pagineLimiting Reagents 1Aldrin Jay Patungan100% (1)
- Section 3 - Vibration MeasurementDocumento24 pagineSection 3 - Vibration MeasurementAbbas AkbarNessuna valutazione finora
- Deep Learning: Huawei AI Academy Training MaterialsDocumento47 pagineDeep Learning: Huawei AI Academy Training Materialsfadhil muhammad hanafiNessuna valutazione finora
- Chapter 11 - MatricesDocumento39 pagineChapter 11 - MatricesJhagantini Palanivelu0% (1)
- LED Linear Highbay LightingDocumento7 pagineLED Linear Highbay LightingMohammed YasarNessuna valutazione finora
- Lewis Structures and Shape of Molecules and HybridizationDocumento12 pagineLewis Structures and Shape of Molecules and HybridizationsanjuanaomiNessuna valutazione finora
- Iota Tangle 2.0: Toward A Scalable, Decentralized, Smart, and Autonomous Iot EcosystemDocumento8 pagineIota Tangle 2.0: Toward A Scalable, Decentralized, Smart, and Autonomous Iot EcosystemMarcos PonceNessuna valutazione finora
- Innovative Lesson PlanDocumento12 pagineInnovative Lesson PlanMurali Sambhu33% (3)
- SAP Table BufferingDocumento31 pagineSAP Table Bufferingashok_oleti100% (3)
- Hacking TechniquesDocumento84 pagineHacking Techniquesgourmetcomidas4Nessuna valutazione finora
- Principles of Differential RelayingDocumento115 paginePrinciples of Differential RelayingelitesankarNessuna valutazione finora
- Binder 1Documento36 pagineBinder 1BobbyNessuna valutazione finora
- Justifying The CMM: (Coordinate Measuring Machine)Documento6 pagineJustifying The CMM: (Coordinate Measuring Machine)pm089Nessuna valutazione finora
- Data Communication & Computer NetworksDocumento32 pagineData Communication & Computer NetworksMuhammad NadeemNessuna valutazione finora
- 034 PhotogrammetryDocumento19 pagine034 Photogrammetryparadoja_hiperbolicaNessuna valutazione finora
- Manual EAP1.5-2kg 040Documento21 pagineManual EAP1.5-2kg 040mykeenzo5658Nessuna valutazione finora
- Foundation DetailsDocumento29 pagineFoundation DetailsSUSOVAN BISWASNessuna valutazione finora
- Qualcomm Snapdragon 660 Mobile Platform Product BriefDocumento2 pagineQualcomm Snapdragon 660 Mobile Platform Product BriefTuxInfoNessuna valutazione finora
- Measurement: Scaling, Reliability, ValidityDocumento34 pagineMeasurement: Scaling, Reliability, ValidityFajar Farhan Muhtasir100% (1)