Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Conlon 2016
Caricato da
asfwegereCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Conlon 2016
Caricato da
asfwegereCopyright:
Formati disponibili
Glaucoma treatment trends: a review
Ronan Conlon, MD,* Hady Saheb, MD, MPH, FRCSC,† Iqbal Ike K. Ahmed, MD, FRCSC‡,§,¶
ABSTRACT ●
Glaucoma is one of the most common causes of blindness worldwide, and its prevalence is increasing. The aim of the present review
is to describe the current medical and surgical treatment trends in the management of open-angle glaucoma. There has been an
increase in the availability of glaucoma medications and the use of laser trabeculoplasty over the past decade, with a subsequent
decrease in invasive incisional surgery. In addition, a new class of glaucoma procedures, termed microinvasive glaucoma surgery,
has emerged, which aims to fill the gap between conservative medical management and more invasive surgery.
GLAUCOMA TREATMENT TRENDS: A REVIEW MEDICAL THERAPIES
Glaucoma is the number one cause of irreversible vision The first approach in the management of OAG is
loss and the second leading cause of blindness worldwide.1 usually through topical medications. An array of drops can
Approximately 66.8 million people worldwide are afflicted be used to lower IOP and can be divided into 5 major
with glaucoma. This number is expected to increase to classes: prostaglandin analogues, beta-blockers, diuretics,
80 million in 2020 because of both demographic expan- cholinergic agonists, and alpha agonists.8 Monotherapy
sion and population aging.2 In Canada, it is estimated with either prostaglandin analogues or beta-blockers is
that 2.7% of people over the age of 40 years have most often the first line. Prostaglandin analogues decrease
glaucoma and 11% over the age of 80 years.3 Unfortu- IOP by reducing outflow resistance, which results in
nately, because of the asymptomatic nature of chronic increased aqueous humor flow through the uveoscleral
glaucoma, up to 50% of people in the industrialized pathway.9 Beta-blockers, on the other hand, reduce IOP
world are unaware of their diagnosis and not receiving by decreasing aqueous formation. The ocular tolerability
treatment.4,5 of beta-blockers is favourable; however, they may cause
Management of glaucoma focuses on lowering intra- cardiac or respiratory side effects.10
ocular pressure (IOP), which remains the principal proven In the past, beta-blockers were the most common first-
method of treatment.6 Target IOP for a particular eye is line topical medication.11 Prostaglandin analogues have
established from a number of factors, including pretreat- been shown to reduce IOP more than beta-blockers in
ment pressure, risk of progression, optic nerve damage, several studies,12–14 with fewer systemic side effects.
and age. It is recommended by the American Academy of During the 1990s, the use of prostaglandin analogues
Ophthalmology that initial treatments aim to reduce IOP increased, whereas that of beta-blockers decreased.15
in primary open-angle glaucoma (OAG) by 25% from A study conducted in Ontario, Canada, demonstrated
baseline.7 The aim of the present review is to describe the an increase in the usage of glaucoma medications between
current medical and surgical treatment trends in the 1992 and 2004, particularly prostaglandin analogues, with
management of OAG. a subsequent decrease in the number of glaucoma sur-
geries.16 In Ontario, the number of glaucoma medications
dispensed almost doubled between 1992 and 2004. In
METHODOLOGY addition, the increase in dispensed prostaglandin ana-
A literature search was conducted with PubMed using logues was strongly correlated (p o 0.001) with a
keywords such as OAG, glaucoma treatment trends, laser decreasing number of performed trabeculectomies.16
trabeculoplasty, nonpenetrating glaucoma surgery, trabe- If monotherapy alone is not effective in controlling
culectomy, glaucoma drainage implants (GDIs), and IOP, other drugs with different mechanisms of action can
microinvasive glaucoma surgery. Articles dating back a replace or be added in conjunction with beta-blockers or
maximum of 50 years were included, with a focus on prostaglandin analogues. Commonly used second-line
studies that have influenced current management trends in agents include alpha-agonists and topical carbonic anhy-
OAG. In addition, information from the Canadian drase inhibitors.17 A major challenge with adding multiple
Ophthalmology Society Guidelines was used. drops is compliance. It has been demonstrated that
& 2016 Canadian Ophthalmological Society.
Published by Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.jcjo.2016.07.013
ISSN 0008-4182/16
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 1
Glaucoma treatment trends: a review—Conlon et al.
increasing the number of drop bottles to a patient’s There continues to be interest in drugs that may protect
treatment regimen negatively affects patient adherence.18 the optic nerve from damage, known as neuroprotection.
To improve patient adherence and reduce exposure to Although in theory this would be extremely useful in the
preservatives, fixed combination therapies have been management of OAG, human trials involving memantine
developed. A number of fixed-combination glaucoma (Namenda; Forest Laboratories, New York, N.Y.) for optic
drops are currently available. Some examples are Cosopt neuroprotection yielded nonsignificant findings.23 Further
(Merck & Co., Inc, Kenilworth, N.Y.), Combigan (Aller- research into the area of neuroprotection needs to be
gan, Irvine, Calif.), Xalacom (Pfizer, New York City, N. explored to examine its role, if any, in the management of
Y.), Azarga (Alcon, Fort Worth, Tex.), DuoTrav (Alcon), glaucoma.
and Simbrinza (Alcon).
Another strategy to increase patient compliance is via
injectable sustained release medications. These devices are LASER THERAPIES
designed to release a drug over a prolonged time interval. Medical management does not reduce IOP to target
A sustained release implant of bimatoprost (Allergan) was levels in all patients, and some continue to experience
recently developed and is capable of delivering medication deterioration of the optic nerve despite maximum medical
for up to 6 months after a single intracameral injection. In therapy. Argon laser trabeculoplasty was introduced as a
a phase 2 trial, in which patients received the implant in treatment modality for OAG by Wise and Witter.24 The
1 eye and topical daily bimatoprost in the other, the mechanism is not well understood, although it is thought
efficacy was comparable and the duration of effect was 4–6 to be caused by thermal energy directed toward the
months.19 trabecular meshwork, which causes focal scarring and
Despite the existence of numerous glaucoma medica- thereby opens space in adjacent structures, or attri-
tions, there is currently no agent that targets the most butable to the inflammation of cytokines and phagocyto-
common pathogenic cause of increased IOP, impaired sis, which induces structural changes with improved
trabecular outflow. Recently, a new class of glaucoma outflow.25
medications, known as rho kinase inhibitors, has emerged. The overall number of laser trabeculoplasty procedures
They have been shown to increase trabecular outflow by and bilateral same-day laser treatments increased dramat-
acting directly on the contractile tone of the trabecular ically in the first half of the 2000s, owing to the advent of
meshwork.20 selective laser trabeculoplasty (SLT).26–30 In Ontario,
AR-13324 (Rhopressa; Aerie Pharmaceuticals, Irvine, Canada, the volume of same-day bilateral laser trabeculo-
Calif.) is a rho kinase and norepinephrine transporter plasties increased from 15.3 per 1000 with OAG in 2000
inhibitor that is believed to lower IOP by 3 main actions: to 74.7 in 2013.30 In addition, the number of laser
reducing aqueous production, increasing trabecular out- iridotomies showed a 1.7-fold increase from 2000 to 2012
flow, and decreasing episcleral venous pressure. In a recent in Ontario.29
phase 2 trial, involving 213 subjects, the efficacy of AR- SLT was introduced by Latina et al. in 1998 and is
13324 was compared to that of latanoprost (Pfizer).21 currently the most widely used and accepted laser therapy
Mean unmedicated baseline diurnal IOP was 25.8, 25.6, for the treatment of OAG.31–35 SLT is less traumatic than
and 25.5 mm Hg in the AR-13324 0.01%, AR-13324 ALT and uses a frequency-doubled Q-switched Nd:YAG
0.02%, and latanoprost groups, respectively. On day 28, a laser (Selecta 7000; Coherent Medical Group, Santa Clara,
total decrease from unmedicated baseline IOP of 5.5, 5.7, Calif.) to achieve similar results without causing visible
and 6.8 mm Hg was observed. Although AR-13324 damage to the trabecular meshwork structures. The exact
0.02% was less effective at lowering IOP by 1 mm Hg, mechanism by which SLT lowers IOP is not well under-
it had a similar efficacy to latanoprost in a prespecified stood. Minimal structural damage to the trabecular mesh-
patient subgroup that excluded patients with baseline work favours theories that SLT acts on a cellular level
IOPs of 426 mm Hg.21 without any thermal effects.35,36 This could be either
Roclatan (Aerie Pharmaceuticals), which is a combina- through phagocytosis of trabecular meshwork debris or by
tion of Rhopressa and latanoprost, demonstrated superior stimulating growth of the trabecular meshwork to increase
IOP-lowering effects compared with latanoprost. In a outflow.37,38
phase 2b clinical trial, Roclatan lowered mean diurnal In the SLT pilot study by Latina et al., 70% of eyes
IOP from 25.1 to 16.5 mm Hg on day 29, which was achieved an IOP reduction of at least 3 mm Hg at 26
about 2 mm Hg greater than that of latanoprost. The most weeks.31 Numerous studies have since followed demon-
common complication with Roclatan was hyperemia, strating the effectiveness of SLT. SLT is effective in
which occurred in approximately 40% of patients and reducing IOP Z20% below baseline in 58%–94% of
was scored as mild in the majority.22 Early clinical trials eyes at 12 months 32,39–41 and 40%–85% at 2 years.35,37,42
suggest that rho kinase inhibitors may soon be used more The IOP-lowering effect of SLT tends to decrease over
frequently in the medical management of glaucoma, time and the mean survival time (time 50% of eyes fail) is
although more data are needed. around 2 years.40,43
2 CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016
Glaucoma treatment trends: a review—Conlon et al.
SLT is being used earlier in the glaucoma treatment Santa Clara, Calif.) to apply a sequence of pattern laser
algorithm, without waiting for maximal medical manage- spots onto the trabecular meshwork. This laser modality is
ment. It has been compared to medication as a primary thought to achieve a cellular response with less tissue
treatment for OAG and has the advantage of not relying scarring.51 Initial pilot studies have been able to demon-
on adherence with glaucoma medications. A meta-analysis strate the IOP-lowering capabilities of both TSLT and
of randomized control studies comparing medication to PLT, although larger-scale studies are warranted to deter-
SLT showed that there was no statistically significant mine their long-term safety and efficacy.52,53
difference in IOP reduction or treatment success.44 SLT’s Another laser therapy, known as cyclophotocoagulation,
current role is either as primary treatment or as an adjunct has been increasingly used among glaucoma surgeons. In
to medical therapy. 1 study, which examined the glaucoma procedure rates in
Economic modeling shows that SLT alone as a primary the United States, cyclophotocoagulation procedures rose
treatment for OAG is cost effective, especially in an aging 248%, from 1995 to 2004.26 Cyclophotocoagulation was
population.45 A study conducted in Ontario, Canada, first introduced in the early 1970s as a last-line surgery to
demonstrated cost savings with SLT over medical therapy lower IOP. During cyclophotocoagulation, a semiconduc-
as a primary treatment for OAG over a 6-year period. The tor diode laser is used to ablate the ciliary processes. Two
study assumed that SLT was repeated every 2–3 years. techniques are currently used to perform cyclophotocoa-
Using the scenario in which SLT is repeated every 2 years, gulation: transscleral diode cyclophotocoagulation (TCP)
it produced 6 year cost savings over mono-, bi-, and tri- and endoscopic diode cyclophotocoagulation (ECP). TCP
drug therapy of $206.45, $1668.64, and $2992.67 per has traditionally been used as a last resort procedure for
patient, respectively.46 cases of refractory glaucoma. ECP is commonly performed
Although SLT is regarded as less traumatic than ALT, in conjunction with cataract surgery.54
pressure spikes and transient inflammation may still occur. Previous studies have demonstrated a wide range of IOP
Micropulse laser trabeculoplasty (MLT) is a new laser reduction, ranging from 12.3% to 66%, using TCP.55,56
therapy that uses an 810 nm diode laser Iridex 1Q810 The amount of energy used seems to directly correlate
(Iridex Corporation, Mountain View, CA). It delivers with treatment success. A meta-analysis performed dem-
energy in repetitive microsecond pulses followed by an onstrated a direct linear correlation between the total
intermittent period of rest, which reduces the buildup of amount of energy applied to the ciliary body and success
thermal energy.47 It has the ability to control thermal rate.57 Although TCP is mainly used in cases of refractory
elevation and does not cause observable coagulative glaucoma, a growing number studies support the use of
damage to the trabecular meshwork on scanning electron TCP as a primary procedure.55,58–62
microscopy.48 ECP is commonly performed in combination with
Several studies have demonstrated the efficacy of cataract surgery. Lindfield et al. conducted a retrospective
MLT.49,50 In a prospective interventional case series that study in which 56 patients who underwent phacoemulsi-
included a total of 20 patients, MLT was successful in 15 fication and ECP were reviewed; mean IOP decreased
patients (75%) with a mean IOP reduction of around from 21.5 to 14.4 mm Hg at 24 months postopera-
20% at 12 months.49 The preliminary data of another tively.63 In another study, 626 phacoemulsification and
study comparing MLT with SLT demonstrated compara- ECP eyes were compared with a cohort of 81 eyes that
ble results. Twelve eyes underwent MLT and 14 had SLT. underwent phacoemulsification alone. The combined
MLT achieved a mean IOP reduction of 3.9 mm Hg, group had a mean reduction in IOP of 3.5 mm Hg,
whereas the reduction in SLT was 2.6 mm Hg. The mean whereas the control group had a mean reduction in IOP of
change in the number glaucoma medications was 0.6 in 0.7 mm Hg.64,65
the MLT group compared with 0.1 in the SLT group.50
MLT has shown promising results in these early clinical
studies. Larger multicentre studies are currently underway, SURGICAL THERAPIES
which will help define its exact role in the management Trabeculectomy
of OAG. When medication and laser therapy alone is not
Other new laser modalities, including titanium-sapphire effective in controlling IOP, more invasive incisional
laser trabeculoplasty (TSLT) and pattern scanning trabe- surgery, such as trabeculectomy or GDIs, is indicated.
culoplasty (PLT), are currently being studied. TSLT is a Overall, there has been a reduction in the number of
subtype of laser trabeculoplasty, which uses a SOLX 790 glaucoma surgeries performed in Canada, United States,
laser (Occulogix, Ont.), emitting near-infrared energy in the Netherlands, Australia, England, Scotland, and
pulses ranging from 5 to 10 mls. This laser modality is Wales.16,26,27,66–71 This decrease can be attributed to the
thought to allow deeper penetration into the juxtacana- introduction of improved glaucoma pharmacotherapy in
licular network as well as the inner wall of Schlemm’s the 1990s. In 1 study, which examined the glaucoma
canal.51 PLT uses a 577-nm laser with computer-guided surgical procedure rates in Canada, a 29% decrease in the
scanning technology (Topcon Medical Laser Systems, number of trabeculectomies performed was observed
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 3
Glaucoma treatment trends: a review—Conlon et al.
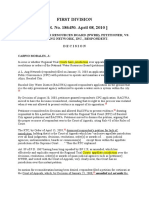
Table 1—Overview of 3 landmark tube studies: Tube versus Trabeculectomy (TVT), Ahmed Baerveldt comparison (ABC), Ahmed
versus Baerveldt (AVB)
TVT.85 ABC.116 AVB.117
Comparison Patients who had previous trabeculectomy and/ Patients with previous intraocular surgery or Patients with uncontrolled or high-risk
groups or cataract extraction and uncontrolled refractory glaucoma and IOP Z18 mm Hg in glaucoma refractory to maximal medical
glaucoma (IOP Z18 on maximal medical whom glaucoma drainage implant (GDI) therapy were randomized to an Ahmed FP7
therapy) were randomized to either tube shunt surgery was planned were randomized to glaucoma valve or an Baerveldt-350 implant.
surgery (350 mm2 Baerveld glaucoma implant) implantation of the Ahmed FP7 glaucoma valve
or trabeculectomy with mitomycin C (AGV) or the Baerveldt 101–350 glaucoma
implant (BGI)
Criteria for Prospectively defined as IOP 421 mm Hg or Defined as IOP Z21 mm Hg or less than a 20% Defined as any of the following: IOP outside
failure less than 20% reduction below baseline on reduction below baseline on 2 consecutive target range (5–18 mm Hg, with Z20%
2 consecutive follow-up visits after 3 months, study visits after 3 months, IOP r5 mm Hg on reduction from baseline) for 2 consecutive
IOP r5 mm Hg on 2 consecutive follow-up 2 consecutive study visits after 3 months, visits after 3 months, vision-threatening
visits after 3 months, reoperation for glaucoma, reoperation for glaucoma, loss of light complications, de novo glaucoma
or loss of light perception perception, or removal of the implant for any procedures, or loss of light perception
reason
Proportion of The cumulative probability of failure was 29.8% The cumulative probability of failure during The cumulative probability of failure at 3 years
success in the tube group and 46.9% in the 5 years of follow-up was 44.7% in the AGV was 51% in the AGV group and 34% in the
trabeculectomy group at 5 years group and 39.4% in the BGI group BGI group
postoperatively
between 1995 and 2004.27 In another study, conducted in validated by the results of the Tube versus Trabeculectomy
the United States, a 53% decrease in trabeculectomies was (TVT) Study (Table 1).85 In this study, patients who had
observed between 1995 and 2004.26 previous trabeculectomy and/or cataract extraction and
Not only has there been a reduction in the number of uncontrolled glaucoma (with IOP Z18) were randomized
glaucoma surgeries performed, there has also been a to either tube shunt surgery (350 mm2 Baerveld glaucoma
decrease in the number of surgeons performing incisional implant) or trabeculectomy with mitomycin C (Mutamy-
glaucoma surgery.72 In a study conducted in Ontario, cin; Bristol-Myers Squibb, New York City, N.Y.). It was
Canada, a 47% decline in the percentage of ophthalmol- found that patients who underwent tube shunt surgery
ogists performing incisional glaucoma surgery between had a higher success rate compared with trabeculectomy
1995 and 2010 was observed (from 35% in 1995 to 19% during 5 years of follow-up. The cumulative probability of
in 2010). At the same time, the proportion of incisional failure was 29.8% in the tube group and 46.9% in the
glaucoma surgery provided by glaucoma surgeons has trabeculectomy group at 5 years postoperatively.85 Pre-
more than doubled. A likely explanation for this trend is viously reported data also demonstrated a higher failure
the expansion in glaucoma fellowship training opportuni- rate with trabeculectomy with mitomycin C at both 1 and
ties, providing general ophthalmologists with easier access 3 years.86,87
to a subspecialist.72 The trabeculectomy failure rate in the TVT study was
Although trabeculectomy remains the “gold standard” similar to other studies88–99; however, the failure rate of
for glaucoma surgery,73–75 it is accompanied by high rates tube shunts was lower than previously reported.100–109 A
of both short- and long-term complications. In the early probable explanation for this difference is that the TVT
postoperative period these complications include choroidal study enrolled eyes at lower risk of failure than eyes that
effusions, hypotony, shallow anterior chambers, and have traditionally underwent tube shunt surgery. It is
hyphema.76–81 Long-term complications are often bleb important to note that the TVT study included only
related and include leakage, blebitis, and endophthalmitis. patients who had a previous failed trabeculectomy or
cataract extraction. The goal of the study was not to
compare 2 surgical techniques on previously unoperated
Glaucoma Drainage Implants eyes. Currently, there is a primary TVT study underway
In recent years, there has been an increased interest in that will address this question.
GDIs.26,29,72 Traditionally, GDIs were used in more All GDIs share a similar design and consist of a tube
refractory glaucoma, although they have been gaining that is used to divert aqueous humor from the anterior
favour, even in cases of nonrefractory glaucoma. In 1 study, chamber of the eye to an external reservoir. The devices
which examined the glaucoma surgical procedure rates in differ with respect to the presence or absence of valves,
the United States, a 184% increase in the use of GDIs, size, and composition of the end plate. Two of the most
from 2728 in 1995 to 7744 in 2004, was observed. commonly used GDIs are the Ahmed valve (New World
Surveys of the membership of the American Glaucoma Medical, Inc, Rancho Cucamonga, Calif.) and Baerveldt
Society performed in 1996, 2002, and 2008 have also implant (Abbott Medical Optics, Inc, Santa Ana, Calif.).
shown a significant increase in the use of GDIs compared The Ahmed implant has a venturi-based flow restrictor,
with trabeculectomy.82–84 designed to reduce postoperative hypotony, although it
The shift in practice pattern toward increased use of has been associated with high rates of encapsulation and
GDIs even in cases of nonrefractory glaucoma was inadequate IOP reduction.107,110–113 The Baerveldt
4 CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016
Glaucoma treatment trends: a review—Conlon et al.
implant is nonvalved and requires intraoperative mechan- trabeculectomy, with fewer complications.119 The main
ical flow restriction to allow adequate time for a capsule to difference between NPGS and trabeculectomy is that the
form. Aqueous drainage begins only after the flow procedures involve the creation of a filtration membrane
restriction reverses, usually 4–6 weeks postoperatively. (the Trabeculo-Descemet’s membrane) rather than a
This delay in aqueous drainage has been reported to cause sclerostomy.
early postoperative IOP volatility.114,115 Most studies agree that NPGS has a lower complication
The Ahmed Baerveldt Comparison (ABC) was a pro- rate than trabeculectomy,120–125 although their efficacy in
spective, randomized study initiated to compare the safety terms of lowering IOP remains a subject of debate. Some
and efficacy of the Ahmed FP7 glaucoma valve (AGV) and studies suggest that NPGS techniques have comparable
the Baerveldt 101–350 glaucoma implant (BGI) IOP-lowering capabilities as the standard trabeculec-
(Table 1).116 Patients with refractory glaucoma and an tomy,124,126 whereas others suggest that NPGS is inferior
IOP Z18 in whom GDI surgery was planned were at lowering IOP.122–132 Randomized prospective studies
enrolled in the study and randomly assigned to implanta- have found success rates of DS and trabeculectomy to be
tion of an AGV or BGI. The primary outcome in the ABC similar.133–136 Cillino et al. found no significant difference
study was cumulative failure rate. The probability of in outcomes between the 2 techniques, but concluded that
failure at 5 years was 44.7% in the AGV group compared trabeculectomy was more suitable with patients with
with 39.4% in the BGI group (p ¼ 0.65), although the higher IOPs.136 A meta-analysis of 10 randomized control
reasons for failure were different. Failure with the AGV trials comparing trabeculectomy and VC concluded that
was mainly attributable to high IOP end points, whereas trabeculectomy had a greater pressure-lowering effect than
failure with the BGI was most often related to safety end VC, but a higher risk profile.137 In 1 prospective random-
points (hypotony, loss of light perception, and implant ized study of 50 eyes, 42% of patients in the trabeculec-
explantation).116 tomy group had a successful outcome compared with 21%
At 5 years, mean IOP decreased from baseline averages in the VC group.125
of 31 to 32 mm Hg to 14.7 mm Hg in the AGV group The main benefit of using NPGS is its increased safety
and 12.7 mm Hg in the BGI group (p ¼ 0.015). profile. The avoidance of full-thickness penetration and its
Although the BGI decreased IOP to a greater extent in potential for sudden hypotony is an enticing option for
the long-term, AGV decreased IOP more in the early patients at high risk for complications with trabeculec-
postoperative period compared with the BGI. In addition, tomy. One of the main limitations to their widespread use
the BGI group required fewer adjunctive medications at is their surgical difficulty.
5 years (2.2 in the AGV group vs 1.8 in the BGI
group).116
The results of the ABC study were supported by a Microinvasive Glaucoma Surgery
similar study, the Ahmed versus Baerveldt Study (AVB), Recently, a new class of glaucoma procedures, termed
which also compared the AGV to BGI (Table 1).117 “microinvasive glaucoma surgery” (MIGS), has emerged.
Again, lower failure rates and a reduction in the need for MIGS procedures are used earlier in the glaucoma treat-
glaucoma medications were observed with the BGI, ment algorithm and aim to fill the gap between medi-
although there were more vision-threatening complica- cation and more invasive surgeries such as trabeculectomy
tions and hypotony in the BGI group.117 or GDIs. Many MIGS procedures are performed in
The ABC and AVB studies do not demonstrate conjunction with cataract surgery, where the patient has
superiority of 1 GDI. Other important considerations, already accepted the risks of intraocular surgery. In
such as individual patient characteristics and surgeon contrast with more invasive glaucoma surgeries, MIGS
experience, are critical in selecting an implant. For procedures use an ab interno approach and are relatively
example, if the surgeon’s goal is to lower pressure as much low risk.
as possible to prevent progression, it may be more MIGS procedures target 3 main outflow channels:
advantageous to use a BGI. On the other hand, if the Schlemm’s canal through trabecular outflow; the supra-
target pressure is higher and the goal is to obtain an IOP choroidal space via the uveoscleral pathway; and the
within normal limits, the AGV may be more suitable given subconjunctival space, by creating an alternative outflow
its superior safety profile. After 5 years of follow-up more pathway for aqueous humor (Table 2). In general, MIGS
reoperations for implant-related complications occurred in procedures share 5 important features: ab interno
the BGI group in the ABC study.118 approach, minimal trauma, ability to lower IOP,
extremely high safety profile, and rapid recovery.138 The
definition of MIGS is subject to debate, and was initially
Nonpenetrating Glaucoma Surgery termed minimally invasive glaucoma surgery (Ahmed I.K.,
Nonpenetrating glaucoma surgery (NPGS), such as personal communication, 2016). It is the opinion of the
deep sclerectomy (DS) and viscocanalostomy (VC), authors that the term micro is more representative of
were popularized in the 1990s as an alternative to MIGS, as it truly differentiates MIGS from other
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 5
Glaucoma treatment trends: a review—Conlon et al.
Table 2—Classification of microinvasive glaucoma surgery implantation in the suprachoroidal space. Clinical trials
(MIGS) devices by outflow channel are currently underway. Auffarth and Kretz implanted the
Outflow channel MIGS device
device in 80 eyes with mild to moderate OAG uncon-
Schlemm’s canal iStent (Glaukos Corporation, Laguna Hills, Calif.) trolled on 2 topical medications and demonstrated a
iStent inject (Glaukos Corporation) significant reduction in IOP and medication burden at
Hydrus (Ivantis, Irvine, Calif.)
Trabectome (Neomedix, Inc, Tustin, Calif.)
18 postoperatively as well as a favourable safety profile.146
Suprachoroidal space iStent supra (Glaukos Corporation) The Hydrus (Ivantis, Irvine, Calif.) is another MIGS
CyPass (Transcend Medical, Menlo Park, Calif.)
device that targets Schlemm’s canal to increase aqueous
Subconjunctival space Xen Gel Stent (Allergan, Irvine, Calif.)
outflow. The device is an 8-mm-long nitinol (nickel–
titanium alloy) Schlemm’s canal scaffold with 3 open-
minimally invasive procedures in nonophthalmic special- ings.147 It is implanted through the trabecular meshwork
ties.139 Either way, MIGS is understood as per the above using a manual inserter. A preclinical study was able to
definition. demonstrate the long-term biocompatibility of the device
The iStent (Glaukos Corporation, Laguna Hills, Calif.) in animal models.148 Randomized controlled trials are
is one of the most widely used and studied MIGS devices. underway, and the results have been promising. Pfeiffer
The microstent is manufactured from heparin-coated et al. compared the efficacy of the microstent in con-
titanium and can be implanted into Schlemm’s canal junction with cataract surgery to cataract surgery alone in
using a preloaded inserter.140 A randomized clinical trial of patients with OAG. The proportion of patients achieving
240 OAG eyes compared cataract surgery alone to iStent a 20% reduction in IOP was significantly higher in the
implantation and cataract surgery combined. The primary Hydrus plus cataract surgery group at 24 months post-
outcome measure was the percent of patients who operatively (80% vs 46%; p ¼ 0.008). In addition, the
achieved an IOP r21 mm Hg without the use of ocular proportion of patients using no hypotensive medication at
hypotensive medications. Seventy-two percent of partic- 24 months was significantly higher in the Hydrus plus
ipants achieved an unmedicated IOP of r21 in the cataract surgery group (73% vs 38%; p ¼ 0.008), and
combined surgery group versus 50% in the cataract adverse event frequency was similar in the 2 groups.149
surgery group at 1 year, with no substantial differences The Trabectome (Neomedix, Inc, Tustin, Calif.) is an
in adverse events.140 After 2 years, a 61% success rate was instrument that uses microelectrocautery to ablate a strip
observed in the combined surgery group versus 50% in the of tissue from the trabecular meshwork, leaving the inner
cataract surgery group.141 wall of Schlemm’s canal intact to preserve collector
Preliminary evidence suggests that the implantation of channel drainage. Studies have demonstrated an acceptable
multiple iStents may be advantageous. Belovay et al.142 safety profile.150,151 In 2010, a study that compared 539
demonstrated a significant reduction in IOP and glaucoma Trabectome and 290 combined cataract surgery and
medications with the use of 2–3 iStents. Mean preoper- Trabectome procedures revealed a 1-year success rate
ative IOP decreased from 18 mm Hg to 14.4 mm Hg at (IOP r21) of 64.9% in the Trabectome group and
1 year postoperatively (p o 0.001). In addition, mean 86.9% in the combined procedure group.150 Francis and
topical hypotensive medications decreased from 2.7 to Winarko prospectively compared eyes undergoing cataract
0.7 at 1 year (p o 0.001).142 and Trabectome surgery to eyes undergoing cataract and
A second-generation iStent, known as iStent inject trabeculectomy surgery. A decrease in IOP from 22.1 to
(Glaukos Corporation), was recently developed. The 15.4 mm Hg was observed in the cataract and Trabectome
device is smaller and designed for more direct implanta- surgery group, and a reduction in IOP from 23.0 to 11.0
tion in Schlemm’s canal. In addition, the device is a 2- mm Hg was seen in the cataract and trabeculectomy
stent system.143 Voskanyan et al. evaluated the safety and surgery group. Although the IOP-lowering effect was
efficacy of the device on 99 patients with OAG. Partic- greater in the cataract and trabeculectomy surgery group,
ipants enrolled in the study were on at least 2 topical a higher rate of postoperative complications was
ocular hypotensive medications and required additional observed.151 Another study demonstrated that a previously
IOP lowering. Mean preoperative IOP decreased from failed Trabectome procedure does not negatively impact
26.3 mm Hg (after medication washout) to 15.7 mm Hg the outcomes of a subsequent trabeculectomy.152 This
at 1 year postoperatively. In addition, 65% of participants study highlights an important feature of the majority of
were medication-free at 1 year.144 Fea et al. conducted a MIGS devices; conventional glaucoma surgery can be
randomized study comparing the iStent inject to ocular performed if necessary.
hypotensive agents and found the device to be at least as Another MIGS pathway to decrease IOP is via the
effective as medications in controlling IOP in patients suprachoroidal space. The CyPass implant (Transcend
with OAG, with an excellent safety profile.145 Medical, Menlo Park, Calif.) is a suprachoroidal shunt
A third-generation iStent (iStent supra), made of made of a polyamide material. The device can be inserted
heparin-coated polyethersulfone and a titanium sleeve, ab interno into the suprachoroidal space using a manual
was recently developed. The device is designed for inserter.138 Early clinical studies have shown that
6 CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016
Glaucoma treatment trends: a review—Conlon et al.
implantation of the device at the time of cataract surgery ophthalmologist (every 3–4 years). Stable early glaucoma
or as a standalone procedure leads to significant reduction patients should be referred to an ophthalmologist in a
in IOP and glaucoma medications.153,154 Hoeh et al. timely fashion. Once stable, these patients can be returned
reported their initial surgical experience with the micro- to the optometrist for monitoring, although they should
stent when combined with cataract surgery. Two analysis be reassessed by an ophthalmologist at least every 2–3
cohorts were prespecified based on medicated IOP: Z21 years. Patients with moderate and advanced disease should
mm Hg (cohort 1, n ¼ 65) or o21 mm Hg (cohort 2, primarily be managed by an ophthalmologist.157
n ¼ 102). At 1 year, cohort 1 showed a 35% decrease in
mean IOP and a 49% reduction in glaucoma medication
usage. Cohort 2 had a 75% reduction in mean medication CONCLUSIONS
use, while maintaining an IOP o21 mm Hg.153 Garcia- Glaucoma remains one of the most common causes of
Feijoo et al. evaluated the efficacy of the device in patients blindness worldwide and with the aging population there
refractory to topical medications. Patients with OAG and is an increasing prevalence.158 The present review outlines
uncontrolled medicated IOPs of 421 were enrolled. the treatment trends in the early management of glaucoma
Baseline IOP was reduced from 24.5 to 16.4 mm Hg (which involves topical medications or laser therapy),
(p o 0.0001) at 12 months. In addition, the mean NPGS, invasive glaucoma surgeries, and the newer MIGS
number of medications was reduced from 2.2 to 1.4 procedures. Overall, there has been an increase in the use
(p ¼ 0.002). No secondary surgery was performed in 83% of topical medications and laser trabeculoplasty, and a
(53/64) of patients, precluding them for more invasive decrease in invasive incisional glaucoma surgery. Fewer
glaucoma surgery.154 ophthalmologists are performing incisional glaucoma sur-
The XEN Gel Stent (Allergan) targets the subconjunc- gery (more restricted to fellowship-trained glaucoma sub-
tival space for aqueous drainage via an ab interno specialists), while general ophthalmologists have increased
approach. The device is 6 mm in length and is composed responsibility for clinical care and laser therapy.159 In
of cross-linked gelatin. It is designed to swell at the time of addition, there has been increased use of and reliance on
implantation to secure the device in place. Initial results optic nerve imaging and reduction in visual field testing.
suggest that, when combined with antimetabolites, IOP- Previously, there was a gap between conservative medical
lowering effects are similar to that of trabeculectomy, management and more invasive glaucoma surgery. The
although the risks may be slightly higher than typical newer MIGS procedures aim to fill this gap and early
MIGS procedures.155,156 In a recent prospective, non- studies have demonstrated their ability to lower IOP with
randomized study, mean IOP decreased from 20.8 mm minimal risk in patients with mild to moderate glaucoma.
Hg preoperatively to 14.4 mm Hg at 6 months and 13.1 More data and longer follow-up are still needed to
mm Hg at 12 months. In addition, glaucoma medications determine their exact role in the glaucoma treatment
decreased from 2.7 to 0.9 at 12 months.155 Another study algorithm.
demonstrated similar results, with a mean preoperative
IOP decreasing from 22.7 to 13.4 mm Hg at 12 months
and glaucoma medication usage decreasing by 64%.156 REFERENCES
Long-term data are still needed to assess the devices
sustained IOP-lowering effect. 1. Resnikoff S, Pascolini D, Etaya’ale D, et al. Global data on visual
impairment in the year 2002. Bull WHO. 2004;82:844-51.
2. Quigley HA, Broman AT. The number of people with glaucoma
worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262-7.
RELATIONSHIP WITH OPTOMETRISTS 3. Perruccio AV, Badley EM, Trope GE. Self-reported glaucoma in
Not only has the medical and surgical management of Canada: findings from population-based surveys, 1994–2003. Can
J Ophthalmol. 2007;42:219-26.
glaucoma evolved, but also so has the role of optometrists, 4. Sommer A, Tielsch JM, Katz J, et al. Relationship between
as the scope of their practice expands. In 2008, the intraocular pressure and primary open angle glaucoma among
membership of the Canadian Glaucoma Society (CGS) white and black Americans. The Baltimore Eye Survey. Arch
Ophthalmol. 1991;109:1090-5.
created a committee to develop a model of interprofes- 5. Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open
sional collaboration between optometrists and ophthal- angle glaucoma in Australia–The Blue Mountains Eye Study.
mologists in the care of glaucoma patients and glaucoma Ophthalmology. 1996;103:1661-9.
6. Boland MV, Ervin AM, Friedman DS, et al. Comparative
suspects. A general principle of this model is that effectiveness of treatments for open angle glaucoma: a systematic
ophthalmologists should evaluate patients early in the review for the US Preventive Services Task Force. Ann Intern Med.
course of their disease.157 2013;158:271-9.
7. AAO. American Academy of Ophthalmology Glaucoma Panel,
According to the model set forth by the CGS, glaucoma Primary Open Angle GlaucomaSan Francisco, CA: AAO PPP
suspects with low/moderate risk can initially be assessed by Glaucoma Panel, Hoskins Center for Quality Eye Care; 2010;
optometrists and do not require referral to an ophthalmol- Available from: 〈http://www.aao.org/ppp〉.
8. Narayanaswamy A, Neog A, Baskaran M, et al. A randomized,
ogist. High-risk glaucoma suspects can also be monitored crossover, open label pilot study to evaluate the efficacy and safety
by optometrists, with periodic consultation to an of Xalatan in comparison with generic Latanoprost (Latoprost) in
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 7
Glaucoma treatment trends: a review—Conlon et al.
subjects with primary open angle glaucoma or ocular hypertension. 30. Szigiato AA, Trope GE, Jin Y, Buys YM. Same-day bilateral
Indian J Ophthalmol. 2007;55:127-31. glaucoma laser treatments in Ontario: 2000 to 2013. J Glaucoma.
9. Gaton DD, Sagara T, Lindsey JD, Gabelt BT, Kaufman PL, 2016;25:339-42.
Weinreb RN. Increased matrix metalloproteinases 1, 2, and 3 in 31. Latina MA, Sibayan SA, Shin DH, Noecker RJ, Marcellino G. Q-
monkey uveoscleral outflow pathway after topic prostaglandin F(2 switched 532-nm Nd:YAG laser trabeculoplasty (selective laser
alpha)-isopropyl ester treatment. Arch Ophthalmol. 2001;119: trabeculoplasty): a multicenter, pilot, clinical study. Ophthalmology.
1165-70. 1998;105:2082-8. discussion 2089–90.
10. Lee DA, Higginbotham EJ. Glaucoma and its treatment: a review. 32. Juzych MS, Chopra V, Banitt MR, et al. Comparison of long-term
Am J Health Syst Pharm. 2005;62:691-9. outcomes of selective laser trabeculoplasty versus argon laser
11. Realini T. A history of glaucoma pharmacology. Optom Vis Sci. trabeculoplasty in open-angle glaucoma. Ophthalmology. 2004;111:
2011;88:36-8. 1853-9.
12. Netland PA, Landry T, Sullivan EK, et al. Travoprost compared 33. Kent SS, Hutnik CM, Birt CM, et al. A randomized clinical
with latanoprost and timolol in patients with open-angle glaucoma trial of selective laser trabeculoplasty versus argon laser trabeculo-
or ocular hypertension. Am J Ophthalmol. 2001;132:472-84. plasty in patients with pseudoexfoliation. J Glaucoma. 2015;24:
13. Sherwood M, Brandt J. Bimatoprost Study Groups 1 and 2. Six- 344-7.
month comparison of bimatoprost once-daily and twice-daily with 34. Holló G. Argon and low energy, pulsed Nd:YAG laser trabeculo-
timolol twice-daily in patients with elevated intraocular pressure. plasty. A prospective, comparative clinical and morphological
Surv Ophthalmol. 2001;45:S361-8. study. Acta Ophthalmol Scand. 1996;74:126-31.
14. Hedman K, Alm A, Gross RL. Pooled-data analysis of three 35. Kramer TR, Noecker RJ. Comparison of the morphologic changes
randomized, double-masked, six-month studies comparing intra- after selective laser trabeculoplasty and argon laser trabeculoplasty
ocular pressure-reducing effects of latanoprost and timolol in in human eye bank eyes. Ophthalmology. 2001;108:773-9.
patients with ocular hypertension. J Glaucoma. 2003;12:463-5. 36. Stein JD, Challa P. Mechanisms of action and efficacy of argon
15. Stein JD, Ayyagari P, Sloan FA, Lee PP. Rates of glaucoma laser trabeculoplasty and selective laser trabeculoplasty. Curr Opin
medication utilization among persons with primary open-angle Ophthalmol. 2007;18:140-5.
glaucoma, 1992 to 2002. Ophthalmology. 2008;115:1315-9. 37. Damji KF, Shah KC, Rock WJ, Bains HS, Hodge WG. Selective
16. Rachmiel R, Trope GE, Chipman ML, Gouws P, Buys YM. Effect laser trabeculoplasty v argon laser trabeculoplasty: a prospective
of medical therapy on glaucoma filtration surgery rates in Ontario. randomised clinical trial. Br J Ophthalmol. 1999;83:718-22.
Arch Ophthalmol. 2006;124:1472-7. 38. Dueker DK, Norberg M, Johnson DH, Tschumper RC, Feeney-
17. Schwartz GF, Reardon G, Mozaffari E. Persistency with latano- Burns L. Stimulation of cell division by argon and Nd:YAG laser
prost or timolol in primary open-angle glaucoma suspects. Am J trabeculoplasty in cynomolgus monkeys. Invest Ophthalmol Vis Sci.
Ophthalmol. 2004;137:S13-6. 1990;31:115-24.
18. Hollo G, Topouzis F, Fechtner RD. Fixed combination intraocular 39. Gracner T, Falez M, Gracner B, Pahor D. [Long-term follow-up of
pressure-lowering therapy for glaucoma and ocular hypertension: selective laser trabeculoplasty in primary open-angle glaucoma].
advantages in clinical practice. Expert Opin Pharmacother. Klin Monbl Augenheilkd. 2006;223:743-7. In German.
2014;15:1737-47. 40. Weinand FS, Althen F. Long-term clinical results of selective laser
19. Business Wire. Allergan announces R&D pipeline update and US trabeculoplasty in the treatment of primary open angle glaucoma.
FDA approval. June 30, 2014. Available from: 〈www.businesswire. Eur J Ophthalmol. 2006;16:100-4.
com/news/home/20140630005687/en/Allergan-Announces-Pipeli 41. Nagar M, Ogunyomade A, O’Brart DP, Howes F, Marshall J. A
ne-Update-U.S.-FDA-Approval〉. VafwQkVFCjw. Accessed November randomised, prospective study comparing selective laser trabecu-
8, 2015. loplasty with latanoprost for the control of intraocular pressure in
20. Pattabiraman PP. Effects of Rho kinase inhibitor AR-13324 on the ocular hypertension and open angle glaucoma. Br J Ophthalmol.
actin cytoskeleton and on TGFβ2- and CTGF-induced fibrogenic 2005;89:1413-7.
activity in Human Trabecular Meshwork Cells. AOPT 2015 Poster 42. McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser
43. Charleston, SC, February 2015. trabeculoplasty as initial and adjunctive treatment for open-angle
21. Bacharach J, Dubiner HB, Levy B, Kopczynski CC, Novack GD. glaucoma. J Glaucoma. 2006;15:124-30.
AR-13324-CS202 Study Group. Double-masked, randomized, 43. Bovell AM, Damji KF, Hodge WG, Rock WJ, Buhrmann RR,
dose-response study of AR-13324 versus latanoprost in patients Pan YI. Long term effects on the lowering of intraocular pressure:
with elevated intraocular pressure. Ophthalmology. 2015;122: selective laser or argon laser trabeculoplasty? Can J Ophthalmol.
302-7. 2011;46:408-13.
22. Aerie Pharmaceuticals Reports Roclatan Phase 2b Results Achieve 44. Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic
All Clinical Endpoints. Available at: 〈http://investors.aeriepharma. review and meta-analysis on the efficacy of selective laser trabecu-
com/releases.cfm?Year=&ReleasesType=&PageNum=2〉. Accessed loplasty in open-angle glaucoma. Surv Ophthalmol. 2015;60:
November 8, 2015. 36-50.
23. Sena DF, Ramchand K, Lindsley K. Neuroprotection for treat- 45. Dirani M, Crowston JG, Taylor PS, et al. Economic impact of
ment of glaucoma in adults. Cochrane Database Syst Rev 2010: primary open-angle glaucoma in Australia. Clin Exp Ophthalmol.
CD006539. 2011;39:623-32.
24. Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma. 46. Lee R, Hutnik CM. Projected cost comparison of selective laser
A pilot study. Arch Ophthalmol. 1979;97:319-22. trabeculoplasty versus glaucoma medication in the Ontario Health
25. Samples JR, Singh K, Lin SC, et al. Laser trabeculoplasty for open- Insurance Plan. Can J Ophthalmol. 2006;41:449-56.
angle glaucoma: a report by the american academy of ophthalmol- 47. Vujosevic S, Bottega E, Casciano M, et al. Microperimetry and
ogy. Ophthalmology. 2011;118:2296-302. fundus autofluorescence in diabetic macular edema: subthreshold
26. Ramulu PY, Corcoran KJ, Corcoran SL, Robin AL. Utilization micropulse diode laser versus modified early treatment diabetic
of various glaucoma surgeries and procedures in Medicare retinopathy study laser photocoagulation. Retina. 2010;30:908-16.
beneficiaries from 1995 to 2004. Ophthalmology. 2007;114: 48. Fudemberg SJ, Myers JS, Katz LJ. Trabecular meshwork tissue
2265-70. examination with scanning electron microscopy: a comparison of
27. Campbell RJ, Trope GE, Rachmiel R, Buys YM. Glaucoma laser MicroPulse Diode Laser (MLT), Selective Laser (SLT), and Argon
and surgical procedure rates in Canada: a long-term profile. Can J laser (ALT) Trabeculoplasty in human cadaver tissue. Invest
Ophthalmol. 2008;43:449-53. Ophthalmol Vis Sci. 2008;49:1236.
28. Jampel HD, Cassard SD, Friedman DS, et al. Trends over time 49. Fea AM, Bosone A, Rolle T, et al. Microdulse diode laser
and regional variations in the rate of laser trabeculoplasty in the trabeculoplasty (MDLT): a phase II clinical study with 12 months
Medicare population. JAMA Ophthalmol. 2014;132:685-90. follow-up. Clin Ophthalmol. 2008;2:247-52.
29. Szigiato AA, Trope GE, Jin Y, Buys YM. Trends in glaucoma 50. Coombs P, Radcliffe NM. Outcomes of micropulse laser trabecu-
surgical procedures in Ontario: 1992–2012. Can J Ophthalmol. loplasty vs. selective laser trabeculoplasty. ARVO 2014. Orlando,
2015;50:338-44. FL, May 2014.
8 CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016
Glaucoma treatment trends: a review—Conlon et al.
51. Tsang S, Cheng J, Lee JW. Developments in laser trabeculoplasty. 74. Netland PA; Ophthalmic Technology Assessment Committee
Br J Ophthalmol. 2016;100:94-7. Glaucoma Panel, American Academy of Ophthalmology. Non-
52. Goldenfeld M, Melamed S, Simon G, Ben Simon GJ. Titanium: penetrating glaucoma surgery. Ophthalmology. 2001;108:416-21.
sapphire laser trabeculoplasty versus argon laser trabeculoplasty in 75. Cairns JE. Trabeculectomy: preliminary report of a new method.
patients with open-angle glaucoma. Ophthalmic Surg Lasers Imag- Am J Ophthalmol. 1968;66:673-9.
ing. 2009;40:264-9. 76. Kao SF, Lichter PR, Musch DC. Anterior chamber depth
53. Turati M, Gil-Carrasco F, Morales A, et al. Patterned laser following filtration surgery. Ophthalmic Surg. 1989;20:332-6.
trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2010;41:538-45. 77. Stewart WC, Shields MB. Management of anterior chamber depth
54. Ishida K. Update on results and complications of cyclophotocoa- after trabeculectomy. Am J Ophthalmol. 1988;106:41-4.
gulation. Curr Opin Ophthalmol. 2013;24:102-10. 78. Brubaker RF, Pederson JE. Ciliochoroidal detachment. Surv
55. Egbert PR, Fiadoyor S, Budenz DL, et al. Diode laser transscleral Ophthalmol. 1983;27:281-9.
cyclopho- tocoagulation as a primary surgical treatment for 79. Gressel MG, Parrish RK II, Heuer DK. Delayed nonexpulsive
primary open-angle glaucoma. Arch Ophthalmol. 2001;119: suprachoroidal hemorrhage. Arch Ophthalmol. 1984;102:1757-60.
345-50. 80. Ruderman JM, Harbin TS Jr, Campbell DG. Post-operative
56. Gupta V, Agarwal HC. Contact trans-scleral diode laser cyclo- suprachoroidal hemorrhage following filtration procedures. Arch
photocoagulation treatment for refractory glaucomas in the Indian Ophthalmol. 1986;104:201-5.
population. Indian J Ophthalmol. 2000;48:29-300. 81. Freedman J, Gupta M, Bunke A. Endophthalmitis after trabecu-
57. Hauber FA, Scherer WJ. Influence of total energy delivery on lectomy. Arch Ophthalmol. 1978;96:1017-8.
success rate after contact diode laser transscleral cyclophotocoagu- 82. Chen PP, Yamamoto T, Sawada A, et al. Use of antifibrosis agents
lation: a retrospective case review and meta-analysis. J Glaucoma. and glaucoma drainage devices in the American and Japanese
2002;11:329-33. Glaucoma Societies. J Glaucoma. 1997;6:192-6.
58. Lai JS, Tham CC, Chan JC, Lam DS. Diode laser transscleral 83. Joshi AB, Parrish RK II, Feuer WF. 2002 survey of the American
cyclophoto- coagulation as primary surgical treatment for medi- Glaucoma Society: practice preferences for glaucoma surgery and
cally uncontrolled chronic angle closure glaucoma: long-term antifibrotic use. J Glaucoma. 2005;14:172-4.
clinical outcomes. J Glaucoma. 2005;14:114-9. 84. Desai MA, Gedde SJ, Feuer WJ, et al. Practice preferences for
59. Kramp K, Vick HP, Guthoff R. Transscleral diode laser contact glaucoma surgery: a survey of the American Glaucoma Society in
cyclophoto-coagulation in the treatment of different glaucomas, 2008. Ophthalmic Surg Lasers Imaging. 2011;42:202-8.
also as primary surgery. Graefes Arch Clin Exp Ophthalmol. 85. Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD,
2002;240:698-703. Budenz DL. Treatment outcomes in the Tube Versus Trabecu-
60. Grueb M, Rohrbach JM, Bartz-Schmidt KU, Schlote T. Trans- lectomy (TVT) study after five years of follow-up. Am J Oph-
scleral diode laser cyclophotocoagulation as primary and secondary thalmol. 2012;153:789-803.
surgical treatment in primary open-angle and pseudoexfoliative 86. Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in
glaucoma. Long-term clinical outcomes. Graefes Arch Clin Exp the Tube Versus Trabeculectomy Study after one year of follow-
Ophthalmol. 2006;244:1293-9. up. Am J Ophthalmol. 2007;143:9-22.
61. Manna A, Foster P, Papadopoulos M, Nolan W. Cyclodiode laser 87. Gedde SJ, Schiffman JC, Feuer WJ, et al. Three-year follow-up of
in the treatment of acute angle closure. Eye. 2012;26:742-5. the Tube Versus Trabeculectomy Study. Am J Ophthalmol.
62. Preussner PR, Ngounou F, Kouogan G. Controlled cyclophoto- 2009;148:670-84.
coagulation with the 940 nm laser for primary open angle 88. The Fluorouracil Filtering Surgery Study Group. Five-year follow-
glaucoma in African eyes. Graefes Arch Clin Exp Ophthalmol. up of the fluorouracil filtering surgery study. Am J Ophthalmol.
2010;248:1473-9. 1996;121:349-66.
63. Lindfield D, Ritchie RW, Griffiths MF. ‘Phaco-ECP’: combined 89. The Fluorouracil Filtering Surgery Study Group. Fluorouracil
endoscopic & cyclophotocoagulation and cataract surgery to aug- filtering surgery study one-year follow-up. Am J Ophthalmol.
ment medical control of glaucoma. BMJ Open. 2012;2:1-6. 1989;108:625-35.
64. Barke SJ, Sturm RT, Caronia RM, et al. Phacoemulsification 90. The Fluorouracil Filtering Surgery Study Group. Three-year
combined with endoscopic cyclophotocoagulation (ECP) in the follow-up of the fluorouracil filtering surgery study. Am J
management of cataract and medically controlled glaucoma: a Ophthalmol. 1993;115:82-92.
large, long term study. In: American Glaucoma Society 16th 91. Heuer DK, Parrish RK, Gressel MG, Hodapp E, Palmberg PF,
Annual Meeting; 2–5 March 2006; Charleston, SC; 2006. Anderson DR. 5-fluorouracil and glaucoma filtering surgery: II. A
Abstract 22:47. pilot study. Ophthalmology. 1984;91:384-94.
65. Berke SJ. Endolaser cyclophotocoagulation in glaucoma manage- 92. Heuer DK, Parrish RK, Gressel MG, et al. 5-fluorouracil and
ment. Tech Ophthalmol. 2006;4:74-81. glaucoma filtering surgery: III. Intermediate follow-up of a pilot
66. Strutton DR, Walt JG. Trends in glaucoma surgery before and study. Ophthalmology. 1986;93:1537-46.
after the introduction of new topical glaucoma pharmacotherapies. 93. Weinreb RN. Adjusting the dose of 5-fluorouracil after filtration
J Glaucoma. 2004;13:221-6. surgery to minimize side effects. Ophthalmology. 1987;94:564-70.
67. van der Valk R, Schouten JS, Webers CA, et al. The impact of a 94. Palmer SS. Mitomycin as adjunct chemotherapy with trabeculec-
nationwide introduction of new drugs and a treatment protocol for tomy. Ophthalmology. 1991;98:317-21.
glaucoma on the number of glaucoma surgeries. J Glaucoma. 95. Prata JA, Minckler DS, Baerveldt G, Lee PP, LaBree L, Heuer
2005;14:239-42. DK. Trabeculectomy in pseudophakic patients: postoperative
68. Walland MJ. Glaucoma treatment in Australia: changing patterns 5-fluorouracil versus intraoperative mitomycin C antiproliferative
of therapy 1994–2003. Clin Exp Ophthalmol. 2004;32:590-6. therapy. Ophthalmic Surg. 1995;26:73-7.
69. Keenan TD, Salmon JF, Yeates D, Goldacre MJ. Trends in rates of 96. Chen CW, Huang HT, Bair JS, Lee CC. Trabeculectomy with
trabeculectomy in England. Eye (Lond). 2009;23:1141-9. simultaneous topical application of mitomycin-C in refractory
70. Macleod SM, Clark R, Forrest J, Bain M, Bateman N, Azuara- glaucoma. J Ocular Pharmacol. 1990;6:175-82.
Blanco A. A review of glaucoma treatment in Scotland 1994– 97. Singh J, O’Brien C, Chawla HB. Success rate and complications of
2004. Eye (Lond). 2008;22:251-5. intraoperative 0. 2 mg/ml mitomycin C in trabeculectomy surgery.
71. Murphy C, Ogston S, Cobb C, MacEwen C. Recent trends in Eye. 1995;9:460-6.
glaucoma surgery in Scotland, England and Wales. Br J Ophthal- 98. Andreanos D, Georgopoulos GT, Vergados J, Papaconstantinou
mol. 2015;99:308-12. D, Liokis N, Theodossiadis P. Clinical evaluation of the effect of
72. Campbell RJ, Bell CM, Gill SS, et al. Subspecialization in mitomycin-C in re-operation for primary open angle glaucoma.
glaucoma surgery. Ophthalmology. 2012;119:2270-3. Eur J Ophthalmol. 1997;7:49-54.
73. Razeghinejad MR, Fudemberg SJ, Spaeth GL. The changing 99. You YA, Gu YS, Fang CT, Ma XQ. Long-term effects of
conceptual basis of trabeculectomy: a review of past and current simultaneous and subscleral mitomycin C application in repeat
surgical techniques. Surv Ophthalmol. 2012;57:1-25. trabeculectomy. J Glaucoma. 2002;11:110-8.
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 9
Glaucoma treatment trends: a review—Conlon et al.
100. Minckler DS, Heuer DK, Hasty B, Baerveldt G, Cutting RC, Barlow management of open angle glaucoma uncontrolled by medical
WE. Clinical experience with the single-plate Molteno implant in therapy. Br J Ophthalmol. 2002;86:748-54.
complicated glaucomas. Ophthalmology. 1988;95:1181-8. 123. Yarangumeli A, Gureser S, Koz OG, Elhan AH. Kural viscocana-
101. Freedman J, Rubin B. Molteno implants as a treatment for lostomy versus trabeculectomy in patients with bilateral high-
refractory glaucoma in black patients. Arch Ophthalmol. 1991; tension glaucoma. Int Ophthalmol. 2004;25:207-13.
109:1417-20. 124. Zimmerman TJ, Kooner KS, Ford VJ, et al. Trabeculectomy vs.
102. Lloyd MA, Sedlak T, Heuer DK, et al. Clinical experience with the nonpenetrating trabeculectomy: a retrospective study of two
single plate Molteno implant in complicated glaucomas. Update of procedures in phakic patients with glaucoma. Ophthalmic Surg.
a pilot study. Ophthalmology. 1992;99:679-87. 1984;15:734-40.
103. Heuer DK, Lloyd MA, Abrams DA, et al. Which is better? One or 125. Gilmour DF, Manners TD, Devonport H, Varga Z, Solebo AL,
two? A randomized clinical trial of single-plate versus double-plate Miles J. Viscocanalostomy versus trabeculectomy for primary open
Molteno implantation for glaucomas in aphakia and pseudphakia. angle glaucoma: 4-year prospective randomized clinical trial. Eye
Ophthalmology. 1992;99:1512-9. (Lond). 2009;23:1802-7.
104. Hodkin MJ, Goldblatt WS, Burgoyne CF, Ball SF, Insler MS. 126. Mermoud A, Schnyder CC, Sickenberg M, et al. Comparison of
Early clinical experience with the Baerveldt implant in complicated deep sclerectomy with collagen implant and trabeculectomy in
glaucomas. Am J Ophthalmol. 1995;120:32-40. open-angle glaucoma. J Cataract Refract Surg. 1999;25:323-31.
105. Mills RP, Reynolds A, Emond MJ, Barlow WE, Leen MM. Long- 127. Jonescu-Cuypers C, Jacobi P, Konen W, et al. Primary viscocana-
term survival of Molteno glaucoma drainage devices. Ophthalmol- lostomy versus trabeculectomy in white patients with open-angle
ogy. 1996;103:299-305. glaucoma: a randomized clinical trial. Ophthalmology. 2001;108:
106. Huang MC, Netland PA, Coleman AL, Siegner SW, Moster MR, 254-8.
Hill RA. Intermediate-term clinical experience with the Ahmed 128. Krieglstein GK. Non-penetrating glaucoma surgery. J Glaucoma.
glaucoma valve implant. Am J Ophthalmol. 1999;127:27-33. 2001;10:S88-90.
107. Broadway DC, Iester M, Schulzer M, Douglas GR. Survival 129. Khaw PT, Siriwardena D. “New” surgical treatments for glaucoma.
analysis for success for Molteno tube implants. Br J Ophthalmol. Br J Ophthalmol. 1999;83:1-2.
2001;85:689-895. 130. Chiselita D. Non-penetrating deep sclerectomy versus trabeculec-
108. Roy S, Ravinet E, Mermoud A. Baerveldt implant in refractory tomy in primary open-angle glaucoma surgery. Eye. 2001;15:
glaucoma: long-term results and factors influencing outcomes. Int 197-201.
Ophthalmol. 2001;24:93-100. 131. Luke C, Dietlein TS, Jacobi PC, et al. A prospective randomized
109. Minckler DS, Francis BA, Hodapp EA, et al. Aqueous shunts in trial of viscocanalostomy versus trabeculectomy in open-angle
glaucoma: a report by the American Academcy of Ophthalmology. glaucoma: a 1-year follow-up study. J Glaucoma. 2002;11:294-9.
Ophthalmology. 2008;115:1089-98. 132. Drusedau MU, von Wolff K, Bull H, et al. Viscocanalostomy for
110. Nouri-Mahdavi K, Caprioli J. Evaluation of the hypertensive phase primary open-angle glaucoma: the Gross Pankow experience.
after insertion of the Ahmed Glaucoma Valve. Am J Ophthalmol. J Cataract Refract Surg. 2000;26:1367-73.
2003;136:1001-8. 133. Mielke C, Dawda VK, Anand N. Deep sclerectomy and low dose
111. Tsai JC, Johnson CC, Dietrich MS. The Ahmed shunt versus the mitomycin C: a randomised prospective trial in West Africa. Br J
Baerveldt shunt for refractory glaucoma: a single-surgeon compar- Ophthalmol. 2006;90:310-3.
ison of outcome. Ophthalmology. 2003;110:1814-21. 134. El Sayyad F, Helal M, El-Kholify H, Khalil M, El-Maghraby A.
112. Tsai JC, Johnson CC, Kammer JA, Dietrich MS. The Ahmed Nonpenetrating deep sclerectomy versus trabeculectomy in bilateral
shunt versus the Baerveldt shunt for refractory glaucoma II: longer- primary open-angle glaucoma. Ophthalmology. 2000;107:1671-4.
term outcomes from a single surgeon. Ophthalmology. 2006;113: 135. Ambresin A, Shaarawy T, Mermoud A. Deep sclerectomy with
913-7. collagen implant in one eye compared with trabeculectomy in the
113. Ayyala RS, Zurakowski D, Smith JA, et al. A clinical study of the other eye of the same patient. J Glaucoma. 2002;11:214-20.
Ahmed glaucoma valve implant in advanced glaucoma. Ophthal- 136. Cillino S, Di Pace F, Casuccio A, et al. Deep sclerectomy versus
mology. 1998;105:1968-76. punch trabeculectomy with and without phacoemulsification: a
114. Krishna R, Godfrey DG, Budenz DL, et al. Intermediate-term randomised clinical trial. J Glaucoma. 2004;13:500-6.
outcomes of 350-mm(2) Baerveldt glaucoma implants. Ophthal- 137. Chai C, Loon SC. Meta-analysis of viscocanalostomy versus trabecu-
mology. 2001;108:621-6. lectomy in uncontrolled glaucoma. J Glaucoma. 2010;19:519-27.
115. Britt MT, LaBree LD, Lloyd MA, et al. Randomized clinical trial 138. Saheb H, Ahmed IK. Micro-invasive glaucoma surgery: current
of the 350-mm2 versus the 500-mm2 Baerveldt implant: longer prospectives and future directions. Curr Opin Ophthalmol.
term results: is bigger better? Ophthalmology. 1999;106:2312-8. 2012;23:96-104.
116. Budenz DL, Barton K, Gedde SJ, et al. Five-year treatment 139. Ahmed II. MIGS and the FDA: what’s in a name? Ophthalmology.
outcomes in the Ahmed Baerveldt comparison. Ophthalmology. 2015;122:1737-9.
2015;122:308-16. 140. Samuelson TW, Katz LJ, Wells JM, et al. Group UIS. Randomized
117. Christakis PG, Tsai JC, Kalenak JW, et al. The Ahmed Versus evaluation of the trabecular micro-bypass stent with phacoemulsi-
Baerveldt Study: three-year treatment outcomes. Ophthalmology. fication in patients with glaucoma and cataract. OPHTHA.
2013;120:2232-40. 2011;118:459-67.
118. Budenz DL, Feuer WJ, Barton K, Schiffman J, Costa VP, Godfrey 141. Craven ER, Katz LJ, Welss MW, et al. Cataract surgery with
DG, Buys YM. Ahmed Baerveldt Comparison Study Group. trabecular micro-bypass stent implantation in patients with mildto-
Postoperative complications in the Ahmed Baerveldt comparison moderate open-angle glaucoma and cataract: two-year follow-up.
study during five years of follow-up. Am J Ophthalmol. J Cataract Refract Surg. 2012;38:1339-45.
2016;163:75-82. 142. Belovay GW, Naqi A, Chan BJ, Rateb M, Ahmed II. Using
119. Sanchez E, Schnyder CC, Sickenberg M, Chiou AG, Hediguer SE, multiple trabecular micro-bypass stents in cataract patients to treat
Mermoud A. Deep sclerectomy: results with and without collagen open-angle glaucoma. J Cataract Refract Surg. 2012;38:1911-7.
implant. Int Ophthalmol. 1996;20:157-62. 143. Bahler CK, Hann CR, Fjield T, Haffner D, Heitzmann H, Fautsch
120. Carassa RG, Bettin P, Fiori M, Brancato R. Viscocanalostomy MP. Second-generation trabecular meshwork bypass stent (iStent
versus trabeculectomy in white adults affected by open-angle inject) increases outflow facility in cultured human anterior seg-
glaucoma: a 2-year randomized, controlled trial. Ophthalmology. ments. Am J Ophthalmol. 2012;153:1206-13.
2003;110:882-7. 144. Voskanyan L, García-Feijoó J, Belda JI, et al. Prospective,
121. Cillino S, Di Pace F, Casuccio A, Cillino G, Lodato G. Deep unmasked evaluation of the iStent s inject system for open-
sclerectomy versus trabeculectomy with low-dosage mitomycin C: angle glaucoma: Synergy trial. Adv Ther. 2014;31:189-201.
four-year follow-up. Ophthalmologica. 2008;222:81-7. 145. Fea AM, Belda JI, Rekas M, et al. Prospective unmasked
122. O’Brart DP, Rowlands E, Islam N, Noury AM. A randomised, randomized evaluation of the iStent inject (s) versus two ocular
prospective study comparing trabeculectomy augmented with hypotensive agents in patients with primary open-angle glaucoma.
antimetabolites with a viscocanalostomy technique for the Clin Ophthalmol. 2014;8:875-82.
10 CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016
Glaucoma treatment trends: a review—Conlon et al.
146. Auffarth G, Kretz F. Open-angle glaucoma in phakic or pseudo- American Society of Cataract and Refractive Surgery Annual
phakic OAG subjects treated with ab interno suprachoroidal stent Meeting, San Diego, California; 2015 .
and postoperative travoprost. Boston, Massachusetts: American 157. Canadian Glaucoma Society Committee on Interprofessional
Society of Cataract and Refractive Surgery Annual Meeting; 2014 . Collaboration in Glaucoma Care. Model of interprofessional
147. Camras LJ, Yuan F, Fan S, et al. A novel Schlemm’s Canal scaffold collaboration in the care of glaucoma patients and glaucoma
increases outflow facility in a human anterior segment perfusion suspects. Can J Ophthalmol. 2011;46:S1-21.
model. Invest Ophthalmol Vis Sci. 2012;53:6115-21. 158. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY.
148. Grierson I, Saheb H, Kahook MY, et al. A novel Schlemm’s canal Global prevalence of glaucoma and projections of glaucoma burden
scaffold: histologic observations. J Glaucoma. 2015;24:460-8. through 2040: a systematic review and meta-analysis. Ophthalmol-
149. Pfeiffer N, Garcia-Feijoo J, Martinez-de-la-Casa J, et al. A ogy. 2014;121:2081-90.
randomized trial of a Schlemm’s canal microstent with phacoe- 159. Campbell RJ, Bell CM, Gill SS, et al. Clinic-based glaucoma care
mulsification for reducing intraocular pressure in open-angle in the era of surgical subspecialization. Am J Ophthalmol. 2014;157
glaucoma. Ophthalmology. 2015;122:1283-93. 631–9.e1–2.
150. Mosaed S, Rhee DJ, Filippopoulos T, et al. Trabectome outcomes
in adult open-angle glaucoma patients: one year follow-up. Clin
Surg Ophthalmol. 2010;28:5-9.
151. Francis BA, Winarko J. Combined trabectome and cataract surgery
versus combined trabeculectomy and cataract surgery in open-angle
glaucoma. Clin Surg Ophtalmol. 2011;29:4-10.
152. Jea SY, Mosaed S, Vold SD, Rhee DJ. Effect of a failed Footnotes and Disclosure:
Trabectome on subsequent trabeculectomy. J Glaucoma. 2012;21:
71-5. The authors have no proprietary or commercial interest in any
153. Hoeh H, Vold SD, Ahmed IK, et al. Initial clinical experience with materials discussed in this article.
the CyPass Micro-Stent: safety and surgical outcomes of a novel
supraciliary MicroStent. J Glaucoma. 2016;25:106-12. From the *University of Ottawa, Ottawa, Ont; †McGill Uni-
154. Garcia-Feijoo J, Rau M, Grisanti S, et al. Supraciliary micro-stent versity, Montreal, Que.; ‡University of Toronto, Toronto, Ont.;
implantation for open-angle glaucoma failing topical therapy: §Trillium Health Partners, Mississauga, Ont.; ¶Prism Eye
1-year results of a multicenter study. Am J Ophthalmol. Institute, Mississauga, Ont.
2015;159:1075-81.
155. Sheybani A, Ahmed IK. Ab interno gelatin stent with mitomycin-c Originally received Feb. 8, 2016. Final revision May. 19, 2016.
combined with cataract surgery for treatment of open-angle Accepted Jul. 28, 2016.
glaucoma: 1-year results. American Society of Cataract and
Refractive Surgery Annual Meeting, San Diego, California; 2015 . Correspondence to Hady Saheb, MD, MPH, FRCSC, McGill
156. Grover D. Ab-Interno gelatin stent procedure in combination with University Health Center Research Institute, 5252 de Maison-
mitomycin-C for treatment of glaucoma: 12-month results. neuve, Montreal, Que. H4A 3S5; hady.saheb@mcgill.ca
CAN J OPHTHALMOL — VOL. ], NO. ], ] 2016 11
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Update/review: The Physics of Phaco: A ReviewDocumento8 pagineUpdate/review: The Physics of Phaco: A ReviewasfwegereNessuna valutazione finora
- Pershing 2011Documento6 paginePershing 2011asfwegereNessuna valutazione finora
- Gender Difference in Coronary Events in Relation To Risk Factors in Japanese Hypercholesterolemic Patients Treated With Low-Dose SimvastatinDocumento5 pagineGender Difference in Coronary Events in Relation To Risk Factors in Japanese Hypercholesterolemic Patients Treated With Low-Dose SimvastatinasfwegereNessuna valutazione finora
- Demography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalDocumento8 pagineDemography and Etiology of Congenital Cataract in A Tertiary Eye Centre of Kathmandu, NepalasfwegereNessuna valutazione finora
- Amaya2003 PDFDocumento20 pagineAmaya2003 PDFasfwegereNessuna valutazione finora
- Kirschner 2009Documento9 pagineKirschner 2009asfwegereNessuna valutazione finora
- Hopayian 2017Documento10 pagineHopayian 2017asfwegereNessuna valutazione finora
- Vaginal Preparation With Antiseptic Solution Before Cesarean Section For Preventing Postoperative Infections (Review)Documento44 pagineVaginal Preparation With Antiseptic Solution Before Cesarean Section For Preventing Postoperative Infections (Review)asfwegereNessuna valutazione finora
- Cesarean Section Surgical Site Infections in Sub-Saharan Africa: A Multi-Country Study From Medecins Sans FrontieresDocumento6 pagineCesarean Section Surgical Site Infections in Sub-Saharan Africa: A Multi-Country Study From Medecins Sans FrontieresasfwegereNessuna valutazione finora
- Sidd Iq 2016Documento11 pagineSidd Iq 2016asfwegereNessuna valutazione finora
- Iatrogenic Brain Foreign Body: S N M S M TDocumento6 pagineIatrogenic Brain Foreign Body: S N M S M TasfwegereNessuna valutazione finora
- Intracranial Metallic Foreign Bodies in A Man With A HeadacheDocumento2 pagineIntracranial Metallic Foreign Bodies in A Man With A HeadacheasfwegereNessuna valutazione finora
- Agarwal 2004Documento5 pagineAgarwal 2004asfwegereNessuna valutazione finora
- MRI of The Peritoneum: Spectrum of AbnormalitiesDocumento12 pagineMRI of The Peritoneum: Spectrum of AbnormalitiesasfwegereNessuna valutazione finora
- Delayed Diagnosis of Intracerebral Foreign Body From The Vietnam WarDocumento4 pagineDelayed Diagnosis of Intracerebral Foreign Body From The Vietnam WarasfwegereNessuna valutazione finora
- Serious Penetrating Craniocerebral Injury Caused by A Nail GunDocumento3 pagineSerious Penetrating Craniocerebral Injury Caused by A Nail GunasfwegereNessuna valutazione finora
- Retained Intracranial Foreign Bodies Metallic: Report of Two CasesDocumento4 pagineRetained Intracranial Foreign Bodies Metallic: Report of Two CasesasfwegereNessuna valutazione finora
- Sharma 2017Documento6 pagineSharma 2017asfwegereNessuna valutazione finora
- Seba Rat Nam 2017Documento1 paginaSeba Rat Nam 2017asfwegereNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- HelloDocumento31 pagineHelloShayne Dela DañosNessuna valutazione finora
- Robot 190 & 1110 Op - ManualsDocumento112 pagineRobot 190 & 1110 Op - ManualsSergeyNessuna valutazione finora
- Novi Hervianti Putri - A1E015047Documento2 pagineNovi Hervianti Putri - A1E015047Novi Hervianti PutriNessuna valutazione finora
- HitchjikersGuide v1Documento126 pagineHitchjikersGuide v1ArushiNessuna valutazione finora
- The Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersDocumento11 pagineThe Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersDM YazdaniNessuna valutazione finora
- Quizo Yupanqui StoryDocumento8 pagineQuizo Yupanqui StoryrickfrombrooklynNessuna valutazione finora
- Dialogue About Handling ComplaintDocumento3 pagineDialogue About Handling ComplaintKarimah Rameli100% (4)
- Statement 876xxxx299 19052022 113832Documento2 pagineStatement 876xxxx299 19052022 113832vndurgararao angatiNessuna valutazione finora
- SBP Notes-1 PDFDocumento7 pagineSBP Notes-1 PDFzeeshanNessuna valutazione finora
- Army War College PDFDocumento282 pagineArmy War College PDFWill100% (1)
- G.R. No. 186450Documento6 pagineG.R. No. 186450Jose Gonzalo SaldajenoNessuna valutazione finora
- Directory of Schools For The Deaf in The PhilippinesDocumento6 pagineDirectory of Schools For The Deaf in The PhilippinesVERA Files100% (1)
- Curriculum Vitae For Modern MutumwaDocumento4 pagineCurriculum Vitae For Modern MutumwaKudakwashe QuQu MaxineNessuna valutazione finora
- Mangaid CoDocumento50 pagineMangaid CoFk Fit RahNessuna valutazione finora
- Law - Midterm ExamDocumento2 pagineLaw - Midterm ExamJulian Mernando vlogsNessuna valutazione finora
- Inventory Management Final ProjectDocumento65 pagineInventory Management Final ProjectMAHESH MUTHYALANessuna valutazione finora
- Seminars - 09-12-2022 - Vanessa AQUINO CHAVESDocumento3 pagineSeminars - 09-12-2022 - Vanessa AQUINO CHAVESVanessa AquinoNessuna valutazione finora
- Determination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriaDocumento5 pagineDetermination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriamiguelNessuna valutazione finora
- 755th RSBDocumento32 pagine755th RSBNancy CunninghamNessuna valutazione finora
- EMP Step 2 6 Week CalendarDocumento3 pagineEMP Step 2 6 Week CalendarN VNessuna valutazione finora
- Bon JourDocumento15 pagineBon JourNikolinaJamicic0% (1)
- Comparing Effect of Adding LDPE, PP, PMMA On The Mechanical Properties of Polystyrene (PS)Documento12 pagineComparing Effect of Adding LDPE, PP, PMMA On The Mechanical Properties of Polystyrene (PS)Jawad K. OleiwiNessuna valutazione finora
- dm00226326 Using The Hardware Realtime Clock RTC and The Tamper Management Unit Tamp With stm32 MicrocontrollersDocumento82 paginedm00226326 Using The Hardware Realtime Clock RTC and The Tamper Management Unit Tamp With stm32 MicrocontrollersMoutaz KhaterNessuna valutazione finora
- Propht William Marrion Branham Vist IndiaDocumento68 paginePropht William Marrion Branham Vist IndiaJoshuva Daniel86% (7)
- Adobe Scan Sep 06, 2023Documento1 paginaAdobe Scan Sep 06, 2023ANkit Singh MaanNessuna valutazione finora
- Kindergarten Report Card SampleDocumento3 pagineKindergarten Report Card Sampleapi-294165063Nessuna valutazione finora
- Project CharterDocumento10 pagineProject CharterAdnan AhmedNessuna valutazione finora
- Lunch Hour Meetings: Kiwanis Mission:: - Officers & Directors, 2018-2019Documento2 pagineLunch Hour Meetings: Kiwanis Mission:: - Officers & Directors, 2018-2019Kiwanis Club of WaycrossNessuna valutazione finora
- Social Networking ProjectDocumento11 pagineSocial Networking Projectapi-463256826Nessuna valutazione finora
- Group 1 Reviewer Social LegislationDocumento5 pagineGroup 1 Reviewer Social Legislationxsar_xNessuna valutazione finora