Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
6 Giant Cell Arteritis Dan Polireumalgia
Caricato da
RifqiCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
6 Giant Cell Arteritis Dan Polireumalgia
Caricato da
RifqiCopyright:
Formati disponibili
The n e w e ng l a n d j o u r na l of m e dic i n e
clinical practice
Caren G. Solomon, M.D., M.P.H., Editor
Giant-Cell Arteritis
and Polymyalgia Rheumatica
Cornelia M. Weyand, M.D., Ph.D., and Jörg J. Goronzy, M.D., Ph.D.
This Journal feature begins with a case vignette highlighting a common clinical problem.
Evidence supporting various strategies is then presented, followed by a review of formal guidelines,
when they exist. The article ends with the authors’ clinical recommendations.
From the Department of Medicine, Stanford A 79-year-old woman presents with new-onset pain in her neck and both shoulders.
University School of Medicine, Stanford, She takes 7.5 mg of prednisone per day for giant-cell arteritis. Occipital tenderness
CA. Address reprint requests to Dr. Weyand
at the Department of Medicine, Immunolo- and diplopia developed 11 months before presentation. At that time, her erythrocyte
gy and Rheumatology, Stanford University sedimentation rate was elevated, at 78 mm per hour, and a temporal-artery biopsy
School of Medicine, CCSR Bldg. Rm. 2225, revealed granulomatous arteritis. The diplopia resolved after 6 days of treatment
269 Campus Dr. W., Stanford, CA 94305-
5166, or at cweyand@stanford.edu. with 60 mg of prednisone daily. Neither headache nor visual symptoms developed
when the glucocorticoids were tapered. How should this patient’s care be managed?
N Engl J Med 2014;371:50-7.
DOI: 10.1056/NEJMcp1214825
Copyright © 2014 Massachusetts Medical Society. The Cl inic a l Probl em
Giant-cell arteritis is an inflammatory vasculopathy that typically occurs in medi-
um and large arteries with well-developed wall layers and adventitial vasa vasorum.1
The vascular beds that are usually affected include the external carotid branches
(e.g., temporal and occipital arteries), the ophthalmic, vertebral, distal subclavian,
and axillary arteries, and the thoracic aorta.2 Vasculitis leads to luminal occlusion
and therefore ischemic complications, such as ischemic optic neuropathy, which
causes vision loss in 10 to 15% of patients.3 Aortitis can be complicated by dissec-
tion and aneurysm formation.4
Polymyalgia rheumatica causes aching and stiffness in selected muscle groups,
predominantly in the neck, shoulders, upper arms, and pelvic girdle.5 Symptoms are
An audio version most pronounced in the morning. The source of the myalgias is insufficiently defined.
of this article is Imaging studies have revealed inflammation of the bursas and periarticular struc-
available at tures.6 Furthermore, the interstitial fluids from painful muscles contain high cyto-
NEJM.org
kine levels.7,8 Typically, these myalgias are associated with robust systemic inflamma-
tion, as indicated by markedly elevated levels of acute-phase reactants in the blood.
Giant-cell arteritis and polymyalgia rheumatica have multiple risk factors and
pathogenic abnormalities in common.1,5 These conditions may occur simultane-
ously or in isolation. Symmetric proximal myalgias combined with laboratory
abnormalities underlie the diagnosis of polymyalgia rheumatica. Since some pa-
tients with polymyalgia rheumatica have subclinical vasculitis and are subject to
vasculitic complications, follow-up evaluation is needed. Approximately 50% of
patients with giant-cell arteritis present with polymyalgia rheumatica before, at the
time of, or after the diagnosis of vasculitis. Symptoms of polymyalgia rheumatica
often appear when the therapy for giant-cell arteritis is being tapered.
Both giant-cell arteritis and polymyalgia rheumatica are diseases that affect the
elderly, with peak incidences at the age of 70 to 80 years9; age (50 years or older) is
considered a criterion for the diagnosis. Women account for 65 to 75% of patients.
Polymyalgia rheumatica occurs at a frequency that is 3 to 10 times that of giant-cell
arteritis.10 Disease risk varies according to race and geographic region. The incidence
50 n engl j med 371;1 nejm.org july 3, 2014
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
clinical pr actice
key Clinical points
G I AN T- C E L L A R T E R I T I S AND P O LYMYA LG I A RHE UMAT I C A
The immune-mediated diseases giant-cell arteritis and polymyalgia rheumatica occur in patients 50 years
of age or older and are now recognized as chronic conditions.
• The diagnosis of giant-cell arteritis should be confirmed on the basis of histologic findings when possible.
• Glucocorticoids are the standard therapy for both giant-cell arteritis and polymyalgia rheumatica, with
higher doses used for giant-cell arteritis.
• Disease flares in patients with giant-cell arteritis and polymyalgia rheumatica are common during
the tapering of glucocorticoids and often respond to a 10 to 20% increase in dose.
• Arteritic ischemic optic neuropathy, which can result in blindness, should be treated as an emergency
and requires prompt diagnosis and initiation of high-dose glucocorticoid therapy.
• In one quarter of patients with giant-cell arteritis, the aorta and its major branches are involved. Large-
vessel disease is reliably diagnosed with computed tomography or magnetic resonance imaging.
• Longevity is generally not reduced by giant-cell arteritis or polymyalgia rheumatica, but glucocorticoid
treatment often has adverse effects. Patients should be closely monitored, with attention to bone loss
and consideration of prophylaxis against pneumocystis pneumonia.
is highest among whites in northern European pop type 1 helper T-cell (Th1)–interferon-γ axis and
ulations (about 20 cases per 100,000 persons older the interleukin-6–type 17 helper T-cell (Th17)–
than 50 years of age); it is lower in southern Euro- interleukin-17 or interleukin-21 axis17; the latter
pean populations (about 10 cases per 100,000) and (but not the former) is effectively suppressed with
is markedly lower in American populations of Asian glucocorticoid treatment.18 Effector cytokines re-
or African descent (about 1 case per 100,000). HLA leased into the arterial wall activate inflammatory
polymorphisms modulate the risk of disease. An cells and target endothelial cells, vascular smooth-
onset of disease late in life suggests that environ- muscle cells, and fibroblasts, leading to lumen-
mental exposures influence susceptibility factors; obstructive intimal hyperplasia. Elastolytic and pro-
socioeconomic status has no noticeable effect.11 teolytic enzymes (e.g., matrix metalloproteinases)
Longevity is not reduced in patients with giant- and proangiogenic and growth-promoting factors
cell arteritis and polymyalgia rheumatica unless (e.g., vascular endothelial growth factor and platelet-
severe aortitis is also present.12-14 Contrary to the derived growth factor) promote remodeling of
previously held belief that giant-cell arteritis and the arterial wall, giving rise to the characteristic
polymyalgia rheumatica are self-limiting condi- findings on imaging and clinical manifestations.
tions, vasculitis persists in many, if not all, pa-
tients, although in most instances it does not S t r ategie s a nd E v idence
cause life-threatening complications.
Evaluation and Management
Pathoph ysiol o gic a l Fe at ur e s The diagnosis of giant-cell arteritis is consid-
ered on the basis of the medical history, clinical
Molecular studies of large-vessel vasculitis15 suggest evaluation, and laboratory and imaging tests,
that dendritic cells residing in the vessel wall initi- and it is confirmed on the basis of histologic
ate the pathogenic cascade and recruit T cells and findings. The absence of pathognomonic clini-
macrophages to form granulomatous infiltrates. cal and laboratory characteristics makes poly-
Dendritic cells have a territorial distribution in the myalgia rheumatica more difficult to diagnose,
vascular tree16 that may determine the pattern of unless it is accompanied by giant-cell arteritis.
vasculitis. Vascular lesions in inflamed temporal
arteries contain an array of cytokines and inflam- Laboratory Testing
matory mediators.15 Two major immune-response Marked elevations in the erythrocyte sedimenta-
networks have been identified: the interleukin-12– tion rate (ESR) and the level of C-reactive protein
n engl j med 371;1 nejm.org july 3, 2014 51
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
(CRP) are common in giant-cell arteritis and poly- reversible with treatment and should not be used
myalgia rheumatica, as are the presence of throm- to assess the inflammatory burden or disease ac-
bocytosis and anemia. In a cohort of 764 patients tivity. Given the effective use of MRA and CTA,
with suspected giant-cell arteritis who underwent traditional angiography is now reserved for plan-
biopsy, with the diagnosis confirmed in 177 pa- ning revascularization procedures, when required.
tients, the sensitivity of an elevated ESR was 84% The use of 18F-fluorodeoxyglucose (18F-FDG)
and that of an elevated CRP level was 86%; the with positron-emission tomography and computed
specificity of these markers was low, however, at tomography (PET–CT), which detects hypermet-
30%. Only 4% of patients with confirmed giant- abolic cells, has been proposed for quantifying
cell arteritis had both a normal ESR and a normal the inflammatory burden.23 The sensitivity and
CRP level at the time of diagnosis.19 Assessment of specificity of this high-cost imaging method for
inflammatory markers is helpful during diagnos- diagnosing and monitoring giant-cell arteritis
tic evaluation and long-term monitoring, but ele- have not been established. 18F-FDG with PET–CT
vated levels of these markers should not be the cannot be relied on to distinguish vasculitis
only indication for immunosuppressive therapy. from nonvasculitic inflammatory lesions (e.g.,
No highly specific biomarkers for giant-cell atherosclerotic changes in vessel walls), and its
arteritis and polymyalgia rheumatica have been sensitivity for smoldering and treated vasculitis
validated. Levels of interleukin-6, a major inducer is limited24; routine use is not recommended.
of CRP production, are characteristically elevated Color Doppler ultrasonography can be used to
in untreated patients, transiently suppressed by visualize superficial arteries, such as the temporal
therapy, and often higher than normal in patients artery, but its usefulness in evaluating the walls of
with chronic disease.20-22 There is no evidence deeper-seated vessels is limited. Vessel-wall edema
that the measurement of interleukin-6 levels is produces a hypoechoic signal on color Doppler
superior to the measurement of CRP levels in ultrasonography that is referred to as a halo sign.
guiding clinical decisions, and its measurement In a meta-analysis involving a total of 998 patients
is not recommended in routine practice. in 17 studies, the sensitivity of the halo sign for
If clinically indicated, assays for autoantibodies biopsy-positive giant-cell arteritis was only 75%,
(e.g., antineutrophil cytoplasmic antibodies [ANCA] and the specificity was only 83%.25 High-field-
or anti–cyclic citrullinated peptide antibodies) can strength MRI may emerge as a method that is
be used to rule out other rheumatic diseases, and sensitive to the detection of temporal-artery inflam-
serum electrophoresis can be used to detect mono- mation, but neither ultrasonography nor MRI has
clonal gammopathy. Blood cultures are recom- yet replaced temporal-artery biopsy, which is highly
mended to evaluate fever of unknown origin. sensitive for even minor inflammatory changes.26,27
In polymyalgia rheumatica, ultrasonography or
Imaging MRI may identify subacromial, subdeltoid, troch
Large-vessel vasculitis occurs in 25% of patients anteric, and cervical bursitis and tenosynovitis of
with giant-cell arteritis.14 Magnetic resonance angi- the long biceps head.5,6 Peripheral-joint synovitis
ography (MRA) or computed tomographic angiog- should raise suspicion of an alternative diagno-
raphy (CTA) of the aortic arch and its major branch- sis, such as rheumatoid arthritis or inflammatory
es is useful in patients in whom giant-cell arteritis osteoarthritis. Current classification criteria do
has been confirmed on biopsy, in order to assess not require ultrasonography as a means of estab-
the extent of arterial involvement (including the lishing the diagnosis of polymyalgia rheumatica.28
presence of stenosis, dissection, and aneurysms)
and to monitor vascular lesions for any signs of pro- Pathological Analysis
gression6 (Fig. 1). MRA or CTA may also be used to In cases of suspected giant-cell arteritis, histologic
identify large-vessel involvement in patients with verification of vasculitis should be sought by means
suspected giant-cell arteritis that has not been con- of a temporal-artery biopsy with assessment of a
firmed on biopsy and in whom there is clinical evi- vascular segment that is 1.5 to 2.0 cm in length.
dence of peripheral ischemic disease. Intramural Histologic analysis is the standard for diagnosis; it
leaky microvessels give rise to delayed enhancement can detect small inflammatory infiltrates and can
of the arterial wall, which is consistent with but not also distinguish giant-cell arteritis from non–giant-
specific for inflammatory activity. Wall thickening cell arteritis arteritides (e.g., ANCA-associated vas-
and increased intrawall blood pooling may not be culitis). A negative biopsy finding does not rule out
52 n engl j med 371;1 nejm.org july 3, 2014
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
clinical pr actice
giant-cell arteritis; however, biopsy identifies 85
A
to 95% of cases.14 Temporal arteries are frequent-
ly not involved in patients with giant-cell arteritis
who have predominantly subclavian involvement.
Biopsy of a second site should be performed if
there is a strong clinical suspicion in spite of neg-
ative findings at the site of the first biopsy and
negative results of imaging. Routine bilateral bi-
opsies are discouraged. Interpreting biopsy find-
ings as false negative results and treating patients
in the absence of strong diagnostic evidence is
problematic, yet appears to be frequent in current
practice. In a recent study, giant-cell arteritis was
diagnosed clinically in 61% of 112 patients,29 de-
spite negative findings on temporal-artery biopsy.
In such cases, patients may be unnecessarily ex-
posed to the risk of glucocorticoid therapy.
Arteritic optic neuropathy is a true emergency,
B
and therapy should not be delayed because of the
risk of vision loss. The diagnostic sensitivity of
temporal-artery biopsy remains high even after
glucocorticoid therapy has been initiated; the sen-
sitivity declines after several weeks of therapy.18,30
Treatment
Immunosuppressive Therapy
Giant-cell arteritis and polymyalgia rheumatica are
responsive to glucocorticoids, and although there is
no specific indication for their use in the treatment
of these conditions, most cases are managed ef-
fectively with glucocorticoid monotherapy (Fig. 2A).
Most treatment recommendations are based on Figure 1. CTA and MRA of the Aortic Arch in Two Patients
clinical experience rather than the results of ran- with Giant-Cell Arteritis.
domized, controlled trials. Therapy for giant-cell Computed tomographic angiography (CTA) (Panel A)
arteritis is initiated with prednisone at a dose of shows the results of aortic-root repair and aortic-arch re-
placement with an “elephant trunk graft” in a 71-year-old
1 mg per kilogram of body weight per day. Given woman who had biopsy-confirmed giant-cell arteritis. The
the risk of irreversible ischemic complications, graft terminates in the proximal descending thoracic aorta.
new-onset clinical manifestations of disease indi- Arrows indicate an aneurysm that is maximally dilated at
cating an unstable supply of blood to the eyes or the proximal descending thoracic aorta. The image was cre-
the central nervous system (e.g., arteritic optic neu- ated with data from contiguous axial images reformatted in
the sagittal and coronal planes. Contrast-enhanced mag-
ropathy) are typically managed with intravenous netic resonance angiography (MRA) (Panel B) shows the
pulse therapy (e.g., 1000 mg of methylprednisolone aortic arch and its branches in a 72-year-old woman with
per day for 3 consecutive days) to optimize immu- biopsy-positive giant-cell arteritis. Arrows indicate stenotic
nosuppression and suppress tissue edema. Once lesions in the bilateral subclavian and axillary arteries, and
tissue necrosis occurs (e.g., optic-nerve ischemia arrowheads indicate long-segment occlusions of the prox-
imal brachial arteries. Images courtesy of Dr. D. Fleisch-
with blindness for several hours), it is irreversible. mann (Panel A) and Dr. F. Chan (Panel B), Department of
In most patients, the administration of high- Radiology, Stanford University.
dose glucocorticoids is followed by rapid improve-
ment of systemic inflammatory signs, presumably
due to the effective suppression of interleukin-6 ratory values have normalized. The dose is initially
and the acute-phase response. In current practice, reduced by 10 to 20% every 2 weeks; once the dose
the tapering of glucocorticoids is generally started falls below 10 mg of prednisone per day, tapering
once reversible clinical signs have abated and labo- is usually slowed (generally by 1 mg per month).
n engl j med 371;1 nejm.org july 3, 2014 53
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
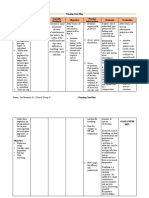
A Giant-Cell Arteritis
Induction Therapy Maintenance Therapy Management of Flares
Prednisone, 1 mg/kg/day Taper prednisone by 10–20%/mo Severe flare: repeat prednisone
Goal: resolution of laboratory Monitor clinically induction therapy
and clinical abnormalities Monitor acute-phase reactants Mild flare: increase prednisone
Course: generally 2–4 wk (ESR and CRP) by 10–20%
Begin bone-protective therapy When dose <10 mg/day, taper by Be cautious in treating elevated
Consider aspirin 1 mg/mo ESR or CRP level in absence of
Consider gastroduodenal clinical symptoms
protection Glucocorticoid-sparing agents:
methotrexate, marginal benefit;
infliximab, no benefit; dapsone,
adalimumab, leflunomide,
hydroxychloroquine,
tocilizumab, azathioprine,
anecdotal use
B Polymyalgia Rheumatica
Induction Therapy Maintenance Therapy Management of Flares
Prednisone, 15–20 mg/day Taper prednisone by 20%/mo Reassess diagnosis, rule out
Goal: remission of myalgias, Monitor clinically vasculitis, consider temporal-
stiffness, constitutional Monitor acute-phase reactants artery biopsy, and consider
symptoms (ESR and CRP) large-vessel imaging
Course: generally 1–2 mo When dose reaches Increase prednisone by 10–20%
Consider bone-protective 10 mg/day, taper slowly Reattempt taper
therapy Glucocorticoid-sparing agents:
methotrexate marginally
effective
Figure 2. Therapeutic Approaches to Giant-Cell Arteritis and Polymyalgia Rheumatica.
The management of giant-cell arteritis (Panel A) depends on the disease stage. Therapeutic interventions for newly di-
agnosed disease (induction therapy), chronic disease (maintenance therapy), and disease flares (management of flares)
are outlined. Glucocorticoids remain the cornerstone of therapy. Other immunosuppressive agents tested to date pro-
vide only marginal or no glucocorticoid-sparing benefits. The management of polymyalgia rheumatica (Panel B) has
much lower glucocorticoid dose requirements. CRP denotes C-reactive protein, and ESR erythrocyte sedimentation rate.
These recommendations match those developed glucocorticoids are discontinued, which may in-
by the British Society for Rheumatology (BSR).31 dicate continuous, smoldering disease activity.
Guidelines from the European League against The doses of glucocorticoids used to treat poly-
Rheumatism (EULAR) suggest a faster initial myalgia rheumatica are much lower than those
tapering to a dose of 10 to 15 mg per day used for the treatment of giant-cell arteritis.5 In the
within 3 months after treatment initiation.32 majority of patients, a dose of 15 to 20 mg of pred-
Inflammatory markers are monitored monthly nisone per day is sufficient to control myalgias.
during the first year of treatment, bimonthly Clinical findings should be used to guide a slow
during the subsequent year, and at intervals of tapering of glucocorticoids (Fig. 2B). The BSR rec-
3 to 6 months during long-term follow-up. ommendations suggest the administration of 10 to
When glucocorticoids are tapered, disease flares 15 mg of prednisolone daily over a period of about
may occur frequently (an average of one to two 10 weeks, followed by a slow taper.31 Recurrent
episodes per person-year) and are often manifested myalgias are common and require dose adjust-
as new-onset or recurrent polymyalgia rheumati- ment. Repetitive flares should prompt diagnostic
ca.22,33 Relapses are rarely manifested as ische reassessment, including evaluation for full-blown
mic complications and often respond to slight giant-cell arteritis and for nonvasculitic conditions.
increases in the dose of glucocorticoids. Elevated The use of glucocorticoids calls for careful
levels of laboratory markers alone, without con- monitoring for adverse effects, especially with
comitant clinical signs, should not automatically the prolonged use of supraphysiologic doses.
trigger substantial intensification of immunosup- During a 10-year follow-up of a population-
pression. Some patients do not fare well when based cohort of patients with giant-cell arteritis,
54 n engl j med 371;1 nejm.org july 3, 2014
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
clinical pr actice
more than 80% had at least one complication subsequent placebo-controlled, randomized tri-
related to glucocorticoid treatment.34 Patients als have not supported the use of TNF blockers
must be monitored for hypertension, hyperglyce- as glucocorticoid-sparing agents in patients with
mia, and bone loss. Measures that are protective giant-cell arteritis or polymyalgia rheumatica.42,43
against bone loss should be provided.35 Prophy- Therapy targeted at disrupting the function of
laxis against Pneumocystis jirovecii pneumonia should interleukin-6 is currently undergoing clinical
be considered in patients receiving doses of pred- testing. In a series of patients with large-vessel
nisone of 20 mg or more daily.36 Physical activity vasculitis, including five patients with giant-cell
and, if indicated, physical therapy aid in main- arteritis, treatment with the interleukin-6 recep-
taining muscle strength and minimizing the side tor antagonist tocilizumab at a dose of 8 mg per
effects of glucocorticoids. Efforts should be made kilogram per month resulted in rapid suppres-
to minimize the duration of treatment and the sion of systemic inflammation.44 However, it is
cumulative glucocorticoid dose. not certain whether interleukin-6 blockade is ef-
fective for the treatment of vascular inflamma-
Glucocorticoid-Sparing Therapy tion. In one patient with large-vessel vasculitis
No glucocorticoid-sparing agents have been ap- who had a clinical response to tocilizumab, per-
proved for the treatment of giant-cell arteritis or sistent vasculitis was identified at autopsy.45
polymyalgia rheumatica. Retrospective case series
and open-label trials have not shown responses to Other Therapies
other immunosuppressive agents that are similar Aspirin (75 to 150 mg per day), which is used in
to those obtained with glucocorticoids. Despite other high-risk populations to reduce the risk of
the lack of rigorous data, a broad spectrum of sec- cardiovascular events, has been suggested as a
ondary agents are used in patients with giant-cell possible means of reducing the risk of ischemic
arteritis. These include infliximab, methotrexate, complications of giant-cell arteritis, but data
cyclophosphamide, azathioprine, and antimalarial from randomized trials showing a benefit in this
agents.37 The findings of a recent meta-analysis of patient population are lacking. If indicated, gas-
10 studies with a total of 638 participants indicate troduodenal mucosal protection should be added
that the use of immunosuppressive agents in ad- whenever aspirin is used. Whereas hydroxymethyl
dition to glucocorticoids did not improve thera- glutaryl coenzyme A reductase inhibitors (statins)
peutic efficacy or safety as compared with the use reduce inflammation, there are no data support-
of glucocorticoids alone,38 raising doubts about ing their use in the management of giant-cell ar-
whether such adjunctive therapy is appropriate. teritis or polymyalgia rheumatica. Observational
Recommendations from the EULAR include the data indicate a similar disease course and similar
use of methotrexate as a potential adjunct to gluco- requirements for glucocorticoid therapy in pa-
corticoids in patients with large-vessel vasculitis,32 tients who do and those who do not take statins.46
but supporting evidence is limited. A meta-analysis
of three placebo-controlled randomized trials in- A r e a s of Uncer ta in t y
volving patients with newly diagnosed giant-cell
arteritis showed that a regimen of glucocorticoid Validated diagnostic criteria for giant-cell arteri-
therapy plus methotrexate as compared with glu- tis and polymyalgia rheumatica are not available.
cocorticoids alone conferred a significant but The diagnosis of polymyalgia rheumatica is par-
modest benefit in lowering the relapse rate and in ticularly challenging, since objective and disease-
reducing the cumulative dose of glucocorticoids, specific findings are often absent. Randomized
without reducing the side effects of the glucocor- trials are needed to determine the best course of
ticoids.39 Data supportive of the adjunctive use of treatment for both conditions. The role of imag-
other immunosuppressive agents are even more ing studies in diagnosis and follow-up has been
limited. In a small randomized, controlled trial, insufficiently defined.
the administration of 2 mg of azathioprine per Giant-cell arteritis and polymyalgia rheumatica
kilogram per day modestly reduced requirements are now recognized as chronic conditions. Often,
for glucocorticoid therapy in patients with giant- inflammatory markers remain abnormally elevated,
cell arteritis and polymyalgia rheumatica.40 Where- even after a 2-year treatment course.22 The best way
as open-label studies of anti–tumor necrosis fac- to manage the postacute phase of disease re-
tor (TNF) agents initially suggested a benefit,41 mains to be determined. It is not clear whether
n engl j med 371;1 nejm.org july 3, 2014 55
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 1. Classification Criteria for Giant-Cell Arteritis and Polymyalgia Rheumatica.* Guidel ine s
ACR classification criteria for giant-cell arteritis, 199047 The American College of Rheumatology (ACR)
At least three criteria must be met: and the Chapel Hill Consensus Conference have
Age at disease onset ≥50 yr developed criteria to distinguish giant-cell arteritis
New headache, either new onset or new type of localized pain in the head from other vasculitides (Table 1).47 The specificity
Abnormal temporal artery, with tenderness to palpation or decreased pul- of these criteria for diagnostic purposes in a gen-
sation eral population is undetermined. The EULAR and
Elevated ESR, >50 mm/hr during first hr of testing (Westergren method) ACR have suggested provisional classification cri-
Biopsy evidence of vasculitis with predominance of mononuclear-cell in- teria for polymyalgia rheumatica,28 but even a
filtration or granulomatous inflammation, usually with multinu-
cleated giant cells score of 5 or more (Table 1)28 has a sensitivity of
Provisional ACR–EULAR classification criteria for polymyalgia rheumatica, 201228 only 66% and a specificity of only 81% for the
Mandatory criteria: purpose of distinguishing polymyalgia rheumatica
Age ≥50 yr from nonpolymyalgic rheumatic conditions. The
Aching in both shoulders BSR has published guidelines for the management
Abnormal C-reactive protein level, ESR, or both of giant-cell arteritis31 and polymyalgia rheumat-
Additional criteria† ica,48 and the EULAR has published guidelines
Morning stiffness lasting >45 min (2 points) for the management of large-vessel vasculitis.32
Hip pain or reduced range of motion (1 point) The recommendations in this article are gener-
Negative rheumatoid factor or antibodies to cyclic citrullinated peptides ally consistent with the available guidelines.
(2 points)
Absence of peripheral synovitis (1 point)
Conclusions and Recommendations
Ultrasonographic findings
At least one shoulder with subdeltoid bursitis, biceps tenosynovitis, The patient in the vignette has biopsy-confirmed
or glenohumeral synovitis, or at least one hip with synovitis or tro-
chanteric bursitis (1 point) giant-cell arteritis, which has responded well to
Subdeltoid bursitis, biceps tenosynovitis, or glenohumeral synovitis high-dose glucocorticoid therapy and subsequent
in both shoulders (1 point) tapering. As is common in such patients, the pa-
tient now presents with symptoms of polymyalgia
* ACR denotes American College of Rheumatology, ESR erythrocyte sedimenta- rheumatica, without evidence of recurrent ischemic
tion rate, and EULAR European League against Rheumatism.
† According to the provisional ACR–EULAR classification criteria for polymyal- manifestations. In this case, the dose of prednisone
gia rheumatica, diagnosis requires that in addition to the mandatory criteria, should be temporarily increased to 10 mg per day to
there must be a score of 4 or more points for additional criteria without ultra- suppress myalgias. Once there are clinical indica-
sonographic findings (diagnostic sensitivity and specificity, 68% and 78%, re-
spectively) and a score of more than 5 points with ultrasonographic findings tions of improvement, an attempt should be made
(diagnostic sensitivity and specificity, 66% and 81% respectively). to taper the dose again while monitoring the clini-
cal response and levels of inflammatory markers.
more aggressive, longer-term immunosuppres- Additional disease recurrences would raise the
sion improves outcomes. possibility of large-vessel involvement, which
The coexistence of several vasculogenic im- should be assessed with MRA or CTA. Careful
mune abnormalities has complicated the devel- follow-up is required to monitor the patient for any
opment of new, glucocorticoid-sparing therapies. adverse effects of treatment with glucocorticoids.
Current therapy offers prompt suppression of some No potential conflict of interest relevant to this article was
reported.
inflammatory pathways, but resistant pathways Disclosure forms provided by the authors are available with
sustain chronic vascular remodeling. the full text of this article at NEJM.org.
References
1. Weyand CM, Goronzy JJ. Medium- and nosis in giant cell arteritis. Ophthalmolo- gia rheumatica. Lancet 2013;381:63-72.
large-vessel vasculitis. N Engl J Med 2003; gy 1993;100:550-5. [Erratum, Lancet 2013;381:28.]
349:160-9. 4. Miller DV, Isotalo PA, Weyand CM, Ed- 6. Salvarani C, Pipitone N, Versari A,
2. Weyand CM, Liao YJ, Goronzy JJ. The wards WD, Aubry MC, Tazelaar HD. Surgi- Hunder GG. Clinical features of polymyal-
immunopathology of giant cell arteritis: cal pathology of noninfectious ascending gia rheumatica and giant cell arteritis. Nat
diagnostic and therapeutic implications. aortitis: a study of 45 cases with emphasis Rev Rheumatol 2012;8:509-21.
J Neuroophthalmol 2012;32:259-65. on an isolated variant. Am J Surg Pathol 7. Kreiner F, Langberg H, Galbo H. In-
3. Aiello PD, Trautmann JC, McPhee TJ, 2006;30:1150-8. creased muscle interstitial levels of in-
Kunselman AR, Hunder GG. Visual prog- 5. Kermani TA, Warrington KJ. Polymyal- flammatory cytokines in polymyalgia
56 n engl j med 371;1 nejm.org july 3, 2014
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
clinical pr actice
rheumatica. Arthritis Rheum 2010;62: 22. Weyand CM, Fulbright JW, Hunder (Hoboken) 2010;62:1515-26. [Erratum,
3768-75. GG, Evans JM, Goronzy JJ. Treatment of Arthritis Care Res (Hoboken) 2012;64:464.]
8. Kreiner F, Galbo H. Elevated muscle giant cell arteritis: interleukin-6 as a bio- 36. Kermani TA, Ytterberg SR, Warrington
interstitial levels of pain-inducing sub- logic marker of disease activity. Arthritis KJ. Pneumocystis jiroveci pneumonia in gi-
stances in symptomatic muscles in pa- Rheum 2000;43:1041-8. ant cell arteritis: a case series. Arthritis
tients with polymyalgia rheumatica. Pain 23. Besson FL, Parienti JJ, Bienvenu B, et Care Res (Hoboken) 2011;63:761-5.
2011;152:1127-32. al. Diagnostic performance of 18F-fluoro- 37. Kötter I, Henes JC, Wagner AD, Loock
9. Gonzalez-Gay MA, Vazquez-Rodri- deoxyglucose positron emission tomogra- J, Gross WL. Does gluco cortico
steroid-
guez TR, Lopez-Diaz MJ, et al. Epidemiol- phy in giant cell arteritis: a systematic re- resistant large-vessel vasculitis (giant cell
ogy of giant cell arteritis and polymyalgia view and meta-analysis. Eur J Nucl Med arteritis and Takayasu arteritis) exist and
rheumatica. Arthritis Rheum 2009;61: Mol Imaging 2011;38:1764-72. how can remission be achieved? A critical
1454-61. 24. Förster S, Tato F, Weiss M, et al. Pat- review of the literature. Clin Exp Rheuma-
10. Crowson CS, Matteson EL, Myasoedo- terns of extracranial involvement in newly tol 2012;30:Suppl 70:S114-S129.
va E, et al. The lifetime risk of adult-onset diagnosed giant cell arteritis assessed by 38. Yates M, Loke YK, Watts RA, Mac-
rheumatoid arthritis and other inflamma- physical examination, colour coded duplex gregor AJ. Prednisolone combined with
tory autoimmune rheumatic diseases. Ar- sonography and FDG-PET. Vasa 2011;40: adjunctive immunosuppression is not su-
thritis Rheum 2011;63:633-9. 219-27. perior to prednisolone alone in terms of
11. Zöller B, Li X, Sundquist J, Sundquist 25. Ball EL, Walsh SR, Tang TY, Gohil R, efficacy and safety in giant cell arteritis:
K. Occupational and socio-economic risk Clarke JM. Role of ultrasonography in the meta-analysis. Clin Rheumatol 2014;33:
factors for giant cell arteritis: a nationwide diagnosis of temporal arteritis. Br J Surg 227-36.
study based on hospitalizations in Sweden. 2010;97:1765-71. 39. Mahr AD, Jover JA, Spiera RF, et al. Ad-
Scand J Rheumatol 2013;42:487-97. 26. Hauenstein C, Reinhard M, Geiger J, et junctive methotrexate for treatment of gi-
12. Matteson EL, Gold KN, Bloch DA, al. Effects of early corticosteroid treatment ant cell arteritis: an individual patient data
Hunder GG. Long-term survival of patients on magnetic resonance imaging and ultra- meta-analysis. Arthritis Rheum 2007;
with giant cell arteritis in the American sonography findings in giant cell arteritis. 56:2789-97.
College of Rheumatology giant cell arteri- Rheumatology (Oxford) 2012;51:1999- 40. De Silva M, Hazleman BL. Azathio-
tis classification criteria cohort. Am J Med 2003. prine in giant cell arteritis/polymyalgia
1996;100:193-6. 27. Maldini C, Dépinay-Dhellemmes C, rheumatica: a double-blind study. Ann
13. Gran JT, Myklebust G, Wilsgaard T, Ja- Tra TT, et al. Limited value of temporal ar- Rheum Dis 1986;45:136-8.
cobsen BK. Survival in polymyalgia rheu- tery ultrasonography examinations for di- 41. Cantini F, Niccoli L, Salvarani C, Padu-
matica and temporal arteritis: a study of 398 agnosis of giant cell arteritis: analysis of la A, Olivieri I. Treatment of longstanding
cases and matched population controls. 77 subjects. J Rheumatol 2010;37:2326-30. active giant cell arteritis with infliximab:
Rheumatology (Oxford) 2001;40:1238-42. 28. Dasgupta B, Cimmino MA, Kremers report of four cases. Arthritis Rheum
14. Kermani TA, Warrington KJ, Crowson HM, et al. 2012 Provisional classification 2001;44:2933-5.
CS, et al. Large-vessel involvement in giant criteria for polymyalgia rheumatica: a Eu- 42. Salvarani C, Macchioni P, Manzini C,
cell arteritis: a population-based cohort ropean League Against Rheumatism/ et al. Infliximab plus prednisone or place-
study of the incidence-trends and progno- American College of Rheumatology col- bo plus prednisone for the initial treat-
sis. Ann Rheum Dis 2013;72:1989-94. laborative initiative. Arthritis Rheum ment of polymyalgia rheumatica: a ran-
15. Weyand CM, Goronzy JJ. Immune 2012;64:943-54. domized trial. Ann Intern Med 2007;146:
mechanisms in medium and large-vessel 29. Saedon H, Saedon M, Goodyear S, Pa- 631-9.
vasculitis. Nat Rev Rheumatol 2013;9:731- pettas T, Marshall C. Temporal artery bi- 43. Hoffman GS, Cid MC, Rendt-Zagar KE,
40. opsy for giant cell arteritis: retrospective et al. Infliximab for maintenance of gluco-
16. Pryshchep O, Ma-Krupa W, Younge BR, audit. JRSM Short Rep 2012;3:73. corticosteroid-induced remission of giant
Goronzy JJ, Weyand CM. Vessel-specific 30. Achkar AA, Hunder GG, Gabriel SE. cell arteritis: a randomized trial. Ann In-
Toll-like receptor profiles in human medi- Effect of previous corticosteroid treatment tern Med 2007;146:621-30.
um and large arteries. Circulation 2008; on temporal artery biopsy results. Ann In- 44. Seitz M, Reichenbach S, Bonel HM,
118:1276-84. tern Med 1998;128:410. Adler S, Wermelinger F, Villiger PM. Rapid
17. Weyand CM, Younge BR, Goronzy JJ. 31. Dasgupta B, Borg FA, Hassan N, et al. induction of remission in large vessel vas-
IFN-γ and IL-17: the two faces of T-cell pa- BSR and BHPR guidelines for the manage- culitis by IL-6 blockade: a case series.
thology in giant cell arteritis. Curr Opin ment of giant cell arteritis. Rheumatology Swiss Med Wkly 2011;141:w13156.
Rheumatol 2011;23:43-9. (Oxford) 2010;49:1594-7. 45. Unizony S, Arias-Urdaneta L, Milo-
18. Deng J, Younge BR, Olshen RA, 32. Mukhtyar C, Guillevin L, Cid MC, et al. slavsky E, et al. Tocilizumab for the treat-
Goronzy JJ, Weyand CM. Th17 and Th1 T- EULAR recommendations for the manage- ment of large-vessel vasculitis (giant cell
cell responses in giant cell arteritis. Circu- ment of large vessel vasculitis. Ann Rheum arteritis, Takayasu arteritis) and poly
lation 2010;121:906-15. Dis 2009;68:318-23. myalgia rheumatica. Arthritis Care Res
19. Kermani TA, Schmidt J, Crowson CS, 33. Mazlumzadeh M, Hunder GG, Easley (Hoboken) 2012;64:1720-9.
et al. Utility of erythrocyte sedimentation KA, et al. Treatment of giant cell arteritis 46. Schmidt J, Kermani TA, Muratore F,
rate and C-reactive protein for the diagno- using induction therapy with high-dose Crowson CS, Matteson EL, Warrington KJ.
sis of giant cell arteritis. Semin Arthritis glucocorticoids: a double-blind, placebo- Statin use in giant cell arteritis: a retro-
Rheum 2012;41:866-71. controlled, randomized prospective clini- spective study. J Rheumatol 2013;40:910-5.
20. Dasgupta B, Panayi GS. Interleukin-6 cal trial. Arthritis Rheum 2006;54:3310-8. 47. Hunder GG, Bloch DA, Michel BA, et
in serum of patients with polymyalgia 34. Proven A, Gabriel SE, Orces C, O’Fallon al. The American College of Rheumatology
rheumatica and giant cell arteritis. Br J WM, Hunder GG. Glucocorticoid therapy 1990 criteria for the classification of giant
Rheumatol 1990;29:456-8. in giant cell arteritis: duration and adverse cell arteritis. Arthritis Rheum 1990;33:
21. Roche NE, Fulbright JW, Wagner AD, outcomes. Arthritis Rheum 2003;49:703-8. 1122-8.
Hunder GG, Goronzy JJ, Weyand CM. Cor- 35. Grossman JM, Gordon R, Ranganath 48. Dasgupta B, Borg FA, Hassan N, et al.
relation of interleukin-6 production and VK, et al. American College of Rheumatol- BSR and BHPR guidelines for the manage-
disease activity in polymyalgia rheumatica ogy 2010 recommendations for the preven- ment of polymyalgia rheumatica. Rheuma-
and giant cell arteritis. Arthritis Rheum tion and treatment of glucocorticoid-in- tology (Oxford) 2010;49:186-90.
1993;36:1286-94. duced osteoporosis. Arthritis Care Res Copyright © 2014 Massachusetts Medical Society.
n engl j med 371;1 nejm.org july 3, 2014 57
The New England Journal of Medicine
Downloaded from nejm.org by HALIM SAMSIRUN on October 25, 2017. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Potrebbero piacerti anche
- Department of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Documento122 pagineDepartment of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Suba Saravanan 12Nessuna valutazione finora
- Rheumatologic Disorders in WomenDocumento25 pagineRheumatologic Disorders in WomenLuiz CruzNessuna valutazione finora
- Transverse Myelitis: Clinical PracticeDocumento9 pagineTransverse Myelitis: Clinical PracticearnabNessuna valutazione finora
- PMR Review in The ClinicDocumento16 paginePMR Review in The Clinickromatin9462Nessuna valutazione finora
- Multiple Myeloma: Differential Diagnoses & Workup Treatment & Medication Follow-Up MultimediaDocumento19 pagineMultiple Myeloma: Differential Diagnoses & Workup Treatment & Medication Follow-Up Multimediaanasarka_01Nessuna valutazione finora
- Seminar: Lionel Adès, Raphael Itzykson, Pierre FenauxDocumento14 pagineSeminar: Lionel Adès, Raphael Itzykson, Pierre FenauxAchmad Teguh Fikri PratamaNessuna valutazione finora
- Jurnal BTKV Edy CLTI 4 FebruariDocumento10 pagineJurnal BTKV Edy CLTI 4 FebruarimcvuNessuna valutazione finora
- Transverse MyelitisDocumento18 pagineTransverse Myelitisanubhav yadavNessuna valutazione finora
- Multiple TeksDocumento21 pagineMultiple TeksPampirBolongNessuna valutazione finora
- Nejmcps 2108909Documento7 pagineNejmcps 2108909GÜLHANE DAHİLİYENessuna valutazione finora
- 1 s2.0 S0268960X08000787 Main PDFDocumento7 pagine1 s2.0 S0268960X08000787 Main PDFmohamedhazemelfollNessuna valutazione finora
- Acute PericarditisDocumento7 pagineAcute PericarditisMirza AlfiansyahNessuna valutazione finora
- VasculitisDocumento184 pagineVasculitisRada NemirovskiNessuna valutazione finora
- Rheumatoid Arthritis Associated Scleritis OPHTHALMOLOGY MCQSDocumento5 pagineRheumatoid Arthritis Associated Scleritis OPHTHALMOLOGY MCQSkishorechandraNessuna valutazione finora
- Fast Facts: Recognizing Refractory Myasthenia GravisDa EverandFast Facts: Recognizing Refractory Myasthenia GravisNessuna valutazione finora
- Review: Ocular and Orbital Involvement in LeukemiaDocumento22 pagineReview: Ocular and Orbital Involvement in LeukemiadechastraNessuna valutazione finora
- Bone Marrow Hypoplasia 2022Documento34 pagineBone Marrow Hypoplasia 2022Jose Angel Cobian GaliciaNessuna valutazione finora
- A Case Report of Rare Acute Ischemic Stroke Due To Meningeal IrritationDocumento7 pagineA Case Report of Rare Acute Ischemic Stroke Due To Meningeal IrritationDayu Punik ApsariNessuna valutazione finora
- Cervicofacial Vascular Anomalies. I. Hemangiomas and Other Benign Vascular TumorsDocumento9 pagineCervicofacial Vascular Anomalies. I. Hemangiomas and Other Benign Vascular TumorsBikash ShresthaNessuna valutazione finora
- Bone Marrow Hypoplasia 2023Documento34 pagineBone Marrow Hypoplasia 2023Dafne LunaNessuna valutazione finora
- Acute Limb Ischemia: Clinical PracticeDocumento9 pagineAcute Limb Ischemia: Clinical PracticeIndah MaulidawatiNessuna valutazione finora
- Chronic Ulceration of The Leg 2013 Surgery OxfordDocumento5 pagineChronic Ulceration of The Leg 2013 Surgery OxfordSanjaya SenevirathneNessuna valutazione finora
- Acute Limb Ischemia: Clinical PracticeDocumento9 pagineAcute Limb Ischemia: Clinical PracticeKezia TambunanNessuna valutazione finora
- Reactive Changes in Blood Film: Integrated Module Phase 1 Third StageDocumento24 pagineReactive Changes in Blood Film: Integrated Module Phase 1 Third Stagerezataheri749Nessuna valutazione finora
- Cardiomyopathies: Lecturer Radu A. Sascău MD, PHDDocumento72 pagineCardiomyopathies: Lecturer Radu A. Sascău MD, PHDASDASDDD2Nessuna valutazione finora
- Group2-Vasculitis-Sec7-2 2Documento7 pagineGroup2-Vasculitis-Sec7-2 2c.caeNessuna valutazione finora
- Pielonefritis Kronis: Tujuan PraktikumDocumento12 paginePielonefritis Kronis: Tujuan PraktikumFp Cyninthia KennedyNessuna valutazione finora
- Clinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudyDocumento6 pagineClinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudySrinath M VNessuna valutazione finora
- Bone Marrow Failure VoiceoverDocumento18 pagineBone Marrow Failure Voiceoverياسر كوثر هانيNessuna valutazione finora
- Anatomy & Medicine MCQs April 14Documento21 pagineAnatomy & Medicine MCQs April 14sb medexNessuna valutazione finora
- Challenges and Opportunities in Pediatric Heart Failure and TransplantationDocumento15 pagineChallenges and Opportunities in Pediatric Heart Failure and TransplantationvijuNessuna valutazione finora
- Mitral Valve ProlapseDocumento5 pagineMitral Valve ProlapseDerofiez Hana RuhyadinNessuna valutazione finora
- Colitis Isquemica PDFDocumento7 pagineColitis Isquemica PDFWaldo ReyesNessuna valutazione finora
- Sle JamaDocumento12 pagineSle Jamalakshminivas PingaliNessuna valutazione finora
- El Nódulo TiroideoDocumento8 pagineEl Nódulo Tiroideoemily peceroNessuna valutazione finora
- Polimialgia ReumaticaDocumento13 paginePolimialgia ReumaticajhonnyNessuna valutazione finora
- CT and MRI of Adrenal Gland PathologiesDocumento23 pagineCT and MRI of Adrenal Gland PathologiesClaudia IrimieNessuna valutazione finora
- Adult Still's Disease and Respiratory Failure in A 74 Year Old WomanDocumento3 pagineAdult Still's Disease and Respiratory Failure in A 74 Year Old WomanEduardo Romero StéfaniNessuna valutazione finora
- CMJ 128 2588Documento7 pagineCMJ 128 2588Le DungNessuna valutazione finora
- Advances in Pathogenesis and TreatmentDocumento6 pagineAdvances in Pathogenesis and TreatmentCristina ElenaNessuna valutazione finora
- Medical Progress: Review ArticlesDocumento12 pagineMedical Progress: Review ArticlesgibsonrajanNessuna valutazione finora
- Diagnosis and Management of Acute Pulmonary.4Documento5 pagineDiagnosis and Management of Acute Pulmonary.4Kemal AtthariqNessuna valutazione finora
- Blue Toe SyndromeDocumento20 pagineBlue Toe SyndromeDaeng MakelloNessuna valutazione finora
- J URNALDocumento9 pagineJ URNALViona PrasetyoNessuna valutazione finora
- Hiperparatiroidismo PrimarioDocumento10 pagineHiperparatiroidismo Primariopruebaprueba321765Nessuna valutazione finora
- Practical Management of Systemic Sclerosis in Clinical PracticeDa EverandPractical Management of Systemic Sclerosis in Clinical PracticeNessuna valutazione finora
- Lecture-3.3.6-Systemic Autoimmune Diseases With Examples-2Documento3 pagineLecture-3.3.6-Systemic Autoimmune Diseases With Examples-2aditya sahuNessuna valutazione finora
- Jurnal 1 Treatment and Management of Scleral DisordersDocumento16 pagineJurnal 1 Treatment and Management of Scleral DisordersIndikator SulSelNessuna valutazione finora
- Lupus 2024Documento12 pagineLupus 2024MarcoNessuna valutazione finora
- Journal Reading: "Aplastic Anemia: Current Concepts in Diagnosis and Management"Documento21 pagineJournal Reading: "Aplastic Anemia: Current Concepts in Diagnosis and Management"Nurfadilah SyamNessuna valutazione finora
- Assessment of Systemic Lupus ErythematosusDocumento13 pagineAssessment of Systemic Lupus ErythematosusBaso AgusofyangNessuna valutazione finora
- Top 5 Causes of Splenomegaly in Dogs - Clinicians BriefDocumento5 pagineTop 5 Causes of Splenomegaly in Dogs - Clinicians Briefludiegues752Nessuna valutazione finora
- Chronic UrticariaDocumento8 pagineChronic UrticariaArezoo JamNessuna valutazione finora
- Myelodysplastic Syndromes PDFDocumento14 pagineMyelodysplastic Syndromes PDFAdriian PortilloNessuna valutazione finora
- A Symptomatic Renal TumorDocumento4 pagineA Symptomatic Renal Tumorarif kurnia timurNessuna valutazione finora
- 1150 6162 2 PBDocumento10 pagine1150 6162 2 PBbella friscaamaliaNessuna valutazione finora
- Proceedings From The 2010 Annual Meeting of The American College of Physicians, Wisconsin ChapterDocumento15 pagineProceedings From The 2010 Annual Meeting of The American College of Physicians, Wisconsin ChapterHarold FernandezNessuna valutazione finora
- CastlemanDocumento6 pagineCastlemanSandra Anastasia GultomNessuna valutazione finora
- Neuroendocrine Tumors: Surgical Evaluation and ManagementDa EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNessuna valutazione finora
- Microcirculation in Cardiovascular DiseasesDa EverandMicrocirculation in Cardiovascular DiseasesEnrico Agabiti-RoseiNessuna valutazione finora
- Nature and Characteristics of Services in HospitalsDocumento7 pagineNature and Characteristics of Services in HospitalsOun MuhammadNessuna valutazione finora
- Food Safety and Sanitation ManagementDocumento71 pagineFood Safety and Sanitation Managementshielad_4100% (1)
- Causes of Metabolic AcidosisDocumento10 pagineCauses of Metabolic AcidosisKimberly Anne SP PadillaNessuna valutazione finora
- Situs Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Documento4 pagineSitus Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Anonymous 9QxPDpNessuna valutazione finora
- San Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityDocumento33 pagineSan Marcelino Campus San Marcelino, Zambales: Ramon Magsaysay Technological UniversityKristine Grace CachoNessuna valutazione finora
- Scenihr o 046Documento116 pagineScenihr o 046Ana NicoletaNessuna valutazione finora
- Coronavirus Disease (COVID-19) : Case Investigation FormDocumento2 pagineCoronavirus Disease (COVID-19) : Case Investigation FormJudeLaxNessuna valutazione finora
- Salmon Dna: Introducing Scientific Breaktrough From JapanDocumento6 pagineSalmon Dna: Introducing Scientific Breaktrough From JapanLeonardo100% (1)
- Burdens of Family Caregiving at The End of LifeDocumento6 pagineBurdens of Family Caregiving at The End of LifeNurul ShahirahNessuna valutazione finora
- Final Coaching NP4 Set 1Documento13 pagineFinal Coaching NP4 Set 1STEFFI GABRIELLE GOLEZNessuna valutazione finora
- Bats MagicDocumento5 pagineBats MagicANDROMEDA1974Nessuna valutazione finora
- K2 - Strongyloides StercoralisDocumento16 pagineK2 - Strongyloides StercoraliswirputNessuna valutazione finora
- Lesson Plan Renal CalculiDocumento17 pagineLesson Plan Renal CalculiAmrita Dean71% (7)
- Maret 18 PDFDocumento178 pagineMaret 18 PDFAnonymous vLgCd0U7Nessuna valutazione finora
- Bioassay For AntidiabetesDocumento39 pagineBioassay For AntidiabetesNita TriadistiNessuna valutazione finora
- Clinical Microbiology and Infection: Original ArticleDocumento6 pagineClinical Microbiology and Infection: Original ArticleAkira Masumi100% (1)
- Wadsworth Publishing Critical Reasoning 6thDocumento468 pagineWadsworth Publishing Critical Reasoning 6thprabindra100% (1)
- Unknown Bacteria Lab ReportDocumento13 pagineUnknown Bacteria Lab Reportapi-529628802Nessuna valutazione finora
- Home Quarantine Compliance 2022 1Documento1 paginaHome Quarantine Compliance 2022 1Puting KahoyNessuna valutazione finora
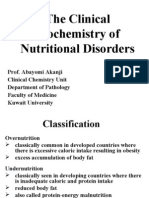
- Lecture 32 - Nutritional DisordersDocumento43 pagineLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Control of Pandemic Infectious Disease Procedure - Landkap - Gitt 00Documento25 pagineControl of Pandemic Infectious Disease Procedure - Landkap - Gitt 00ahar85Nessuna valutazione finora
- Clinical Chemistry QuestionsDocumento5 pagineClinical Chemistry QuestionsEric C. CentenoNessuna valutazione finora
- Diazepam Drug StudyDocumento1 paginaDiazepam Drug StudyAndee Salegon100% (3)
- DengueDocumento99 pagineDengueJames DavidNessuna valutazione finora
- Hipertensi Portal Donny SandraDocumento67 pagineHipertensi Portal Donny SandrabobyNessuna valutazione finora
- CystsDocumento5 pagineCystsranindita maulyaNessuna valutazione finora
- Chapter 12 Glencoe Biology Study GuideDocumento11 pagineChapter 12 Glencoe Biology Study GuideabdulazizalobaidiNessuna valutazione finora
- GAF E-Brochure LATEST 20x28cmDocumento16 pagineGAF E-Brochure LATEST 20x28cmGopinath AgnihotramNessuna valutazione finora
- Growth and DevelopmentDocumento64 pagineGrowth and DevelopmentRahul Dhaker100% (1)
- Nursing Care PlanDocumento13 pagineNursing Care PlanJan DamesNessuna valutazione finora