Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
1933-088x-15 2 106 PDF
Caricato da
Gordana PuzovicTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
1933-088x-15 2 106 PDF
Caricato da
Gordana PuzovicCopyright:
Formati disponibili
PH GRAND ROUNDS
Persistent Pulmonary Artery Filling Defects: Looking
Beyond Anticoagulation Failure
Section Editor Damon A. Forbes, MD
Deborah J. Levine, MD Pulmonary and Critical Care Service
Department of Medicine
Brooke Army Medical Center
San Antonio, TX
Eliot A. Bassett, DO
Internal Medicine Residency
Department of Medicine
Brooke Army Medical Center
San Antonio, TX
William R. Auger, MD
Division of Pulmonary, Critical Care, and
Sleep Medicine
Department of Medicine
University of California, San Diego
San Diego, CA
David M. Ferraro, MD
Pulmonary and Critical Care Service
Department of Medicine
Brooke Army Medical Center
San Antonio, TX
Presentation: A 63-year-old previously with preserved systolic function (Figures ratio was within the therapeutic range.
healthy woman presented to the emer- 2A and 2B). A diagnosis of pulmonary Repeat TTE showed interval devel-
gency department (ED) with a 7-day embolism (PE) was made and she was opment of dilated right-sided heart
history of acute dyspnea on exertion admitted for initiation of anticoagula- chambers, increased RV filling pressure,
and substernal chest pressure. She had tion. She was discharged home 2 days abnormal RV relaxation, and moderate
recently returned from a vacation that later in stable condition on enoxaparin tricuspid valve regurgitation (Figures
included air travel. On evaluation, and warfarin therapy. 2C and 2D). CTPA showed enlarge-
she was found to have mild hypoxia, One month later, she returned to ment of the filling defect within the
requiring 1 liter per minute of oxygen the ED with progressive dyspnea, new main pulmonary artery and right-sided
to maintain SpO2 saturation of 92%. right-sided pleuritic pain, and non- segmental branches, as well as new
Her vital signs and physical examination productive cough. She had a heart rate filling defects within the left superior
were otherwise unremarkable. Comput- of 126 beats per minute, and required lobar artery. There were also peripheral
ed tomography pulmonary angiogram supplemental oxygen at 3 liters per airspace consolidations within the right
(CTPA) demonstrated a large filling minute. A prominent S2 was noted lower lobe (Figures 3A-3D). Right
defect within the main pulmonary artery without associated murmurs or gallops. heart catheterization showed mildly
with extension into the right-sided There was no jugular venous distention elevated pulmonary artery pressures
segmental and subsegmental branches or lower-extremity edema. Lung fields (Table 1). A gadolinium-enhanced
(Figures 1A-1D). Cardiac biomarkers were clear to auscultation bilaterally. chest magnetic resonance imaging
were within normal limits. A transtho- Laboratory studies were notable for a (MRI) study showed no enhancement
racic echocardiogram (TTE) showed pro-brain natriuretic peptide level of within the intraluminal lesion, suggest-
mild right ventricular (RV) dilation 1138 pg/mL; international normalized ing a large bland thrombus (Figures 4A
and 4B).
Key Words— computed tomography pulmonary angiogram, dyspnea, hypoxia, pulmonary artery sarco-
mas, thromboembolic disease Management: The patient underwent
Correspondence: levinedj@uthscsa.edu percutaneous catheter-directed throm-
106 Advances in Pulmonary Hypertension Volume 15, Number 2; 2016
bolysis and suction thrombectomy, bus. However, she did not respond to Diagnosis: Intraoperatively, a large mass-
which provided partial recanalization this therapy, and her cardiopulmonary like structure was excised from the pul-
within the main pulmonary and right status deteriorated. She underwent monary trunk and right pulmonary artery.
superior lobar arteries. Forceps biopsies surgical pulmonary thromboendarterec- Pathologic analysis of an intraoperative
were taken from the intraluminal lesion tomy at our institution, because she was frozen specimen yielded a preliminary
at the time of suction thrombectomy too unstable for transport to a referral diagnosis of an osteogenic sarcoma. The
and were consistent with bland throm- center. tumor was noted to be invading through
Figure 1A: CTPA representative selection demonstrating a large filling defect within the right pulmonary artery and middle and inferior lobar
arteries (red arrow).
Figure 1B: CTPA representative selection demonstrating filling defects within the right segmental pulmonary arteries (red arrows).
Figure 1C: CTPA representative selection of the lung parenchyma.
Figure 1D: CTPA representative selection demonstrating mild flattening of the interventricular septum without significant RV enlargement. No
significant parenchymal disease is noted.
Advances in Pulmonary Hypertension Volume 15, Number 2; 2016 107
Figure 2A: TTE apical 4-chamber view showing mild RV dilation.
Figure 2B: TTE parasternal long axis view showing mild RV dilation.
Figure 2C: Repeat TTE apical 4-chamber view showing worsened RV enlargement, septal bowing, and severely decreased RV systolic function.
Figure 2D: Repeat TTE parasternal long axis view showing RV enlargement and septal bowing.
the walls of the right pulmonary artery stamm in 1923.1 Fewer than 300 cases cific findings. Similarly, ventilation/
into the adjacent lung parenchyma, ne- have been reported in the literature perfusion scans are generally unable
cessitating right pneumonectomy (Figures since that time. The World Health to differentiate between thrombus and
5A and 5B). A complete debulking pro- Organization categorizes PAS into 3 tumor, as both conditions appear as
cedure was not possible because of gross main subtypes: angiosarcoma, leiomyo- discrete perfusion defects.3 CTPA may
evidence of involvement of left pulmonary sarcoma, and intimal sarcoma.2 Clinical be a more useful imaging modality,
artery and its distal branches. A diagnosis presentation is similar regardless of demonstrating large obstructive filling
of metastatic intravascular chondroblastic the tumor subtype, and symptoms may defects in the proximal pulmonary
osteosarcoma was confirmed, complicated include dyspnea, chest pain, coughing, arteries. Nonmalignant thromboembol-
by foci of undifferentiated pleomorphic and hemoptysis. Consequently, many ic disease rarely presents with lesions
sarcoma (Figures 6A and 6B). The post- of these cases are initially misdiagnosed that occupy the entire vascular lumen.3
operative course was complicated by sepsis as acute or chronic thromboembolic This phenomenon has been referred to
and multisystem organ failure. Based on disease. as the “wall eclipsing sign,” and is felt
poor prognosis and rapid deterioration, There is no consensus diagnostic to be pathognomonic for pulmonary
she elected for comfort measures only and algorithm for the evaluation of suspect- artery tumors.4 Gadolinium-enhanced
died two days later. ed PAS. In general, laboratory testing is chest MRI has also been proposed as
of little utility. Echocardiography may a diagnostic imaging study that can
Discussion: Pulmonary artery sarcomas show evidence of pulmonary hyperten- distinguish PAS from PE.5,6 Contrast
(PAS) were first described by Mandel- sion (PH) and RV dysfunction, nonspe- enhancement of the intraluminal lesion
108 Advances in Pulmonary Hypertension Volume 15, Number 2; 2016
Figure 3A: CTPA representative selection demonstrating a large, obstructing filling defect within the pulmonary artery trunk, right pulmonary
artery, and right segmental branches (red arrow).
Figure 3B: CTPA representative selection demonstrating a large, obstructing filling defect within the pulmonary artery trunk, right pulmonary
artery, and right segmental branches (red arrows).
Figure 3C: CTPA representative selection demonstrating a multiple peripheral ground-glass opacities and areas of consolidation (red arrow).
Figure 3D: CTPA representative selection demonstrating a multiple peripheral ground-glass opacities and areas of consolidation (red arrow).
suggests the presence of an intravas- The mainstay of therapy for these fail to respond to appropriate anti-
cular tumor. However, as our case tumors is surgical resection, which may coagulation therapy. PAS should also
illustrates, the absence of contrast en- prolong tumor-free survival.7,8 The role be considered in patients undergoing
hancement is not sufficient to exclude of chemotherapy is unclear, and there evaluation for chronic thromboembolic
intravascular tumors. Another radio- are no consensus recommendations for pulmonary hypertension (CTEPH) who
graphic modality, fluorodeoxyglucose specific therapeutic regimens.9 Overall, have large proximal filling defects. Given
(FDG) positron emission tomography prognosis is poor with mean survival that no single imaging study can rule
(PET), may be helpful in distinguish- rates between 1 and 2 years in most out an intravascular sarcoma, a multi-
ing between thrombi and malignant case series.3,7-9 This is likely due in part modality approach, including CTPA,
lesions. The degree of FDG uptake to delay in diagnosis. A strong index of chest MRI, and PET imaging, may be
tends to be significantly higher in the suspicion is necessary in patients with necessary to improve diagnostic accura-
latter group.6,7 presumed thromboembolic disease who cy. In addition, early referral to a surgical
Advances in Pulmonary Hypertension Volume 15, Number 2; 2016 109
Table 1. Right Heart Catheterization.
Right atrial pressure, mm Hg 6/4 (4)
Right atrial oxygen saturation, % 52
RV pressure, mm Hg 43/3 (16)
Pulmonary artery pressure, mm Hg 42/17 (25)
Pulmonary artery oxygen saturation, % 51
Pulmonary artery occlusion pressure, mm Hg 4
Cardiac output, L/min (thermodilution) 4.4
Cardiac output, L/min/m2 2.75
Pulmonary vascular resistance, Wood units 3.8
Figure 4A: Contrast-enhanced chest MRI
representative selection demonstrating a
large filling defect within the main pulmonary
artery and right-sided pulmonary artery
branches (red arrow).
Figure 4B: Contrast-enhanced chest MRI
axial T1 representative image demonstrating
a large filling defect within the main
pulmonary artery and right-sided pulmonary
artery branches. No significant contrast
enhancement is noted within the lesion (red
arrow).
center of excellence should be strongly
considered.
Expert Commentary*: Pulmonary vas-
cular neoplasms are one of the notorious
mimics of acute and chronic pulmonary
thromboembolic disease. As illustrated
by this case, the initial clinical presenta-
tion and even computed tomography
(CT) angiographic imaging are often
indistinguishable from that associated
with an acute pulmonary embolic event.
At the onset, there was little to suggest
an alternative diagnosis in this patient,
given the abrupt onset of cardiopulmo-
nary symptoms, the predisposition to an
acute thromboembolic event (recent air
travel), and the presence of intralumi-
Figure 5A: Gross specimen of the right lung showing a cartilaginous tumor obstructing the
nal filling defects by CT angiography. pulmonary artery (red arrow).
However, a moment of diagnostic pause Figure 5B: Gross specimen of the right lung showing multiple cartilaginous tumor nodules
throughout the lung parenchyma (red arrows).
110 Advances in Pulmonary Hypertension Volume 15, Number 2; 2016
suggesting a very malignant process. This
patient’s presentation a month after her
initial diagnosis with evidence of right
heart failure was simply a manifestation
of progressive encroachment on the
pulmonary vessels with tumor.
The confirmation of a pulmonary
vascular neoplasm prior to surgical
resection can be difficult. This was again
well illustrated by this case. Gadolini-
um-enhanced chest MRI can be helpful
in the distinction between pulmo-
nary artery neoplasms and thrombus,
though intravascular tumors can result
in false-negative studies. FDG-PET
imaging seems more reliable based on
clinical experience and the limited data
available.7 The variable performance of
these modalities may simply reflect the
degree of malignancy within the spec-
trum of pulmonary artery tumors. And
the success of catheter-based biopsy will
logically be influenced by the extent of
material obtained. Personal experience
with this approach has been limited;
furthermore, there has not been a report
describing the usefulness of this tech-
nique in establishing the diagnosis of
pulmonary artery tumors.
In most cases, the presurgical di-
agnosis is presumptive and generally
based on the clinical presentation,
radiographic features, and the response
Figure 6A: A large-caliber artery is filled and distorted with lobulated, cartilage-predominant to anticoagulants if the initial diagnosis
tumor (blue arrows). Normal lung (lower left), bronchus (upper left), and lymph node (top was a pulmonary embolus. And from a
center) are also present. (10x hematoxylin and eosin stain) practical perspective, unless a patient re-
Figure 6B: Areas of tumor from the peripherally located nodules show osteoid production
by sheets of high-grade cells with large nuclei, prominent nucleoli, and conspicuous mitotic
fuses, surgical exploration and resection
activity. (200x hematoxylin and eosin stain) is warranted even without a presurgical
diagnosis, as typically the differential
is generally warranted when the “throm- observed with acute pulmonary emboli. diagnosis involves CTEPH, and most
bus” appears to disrupt the vascular Isolated, unilateral lesions, the presence of these patients have signs and symp-
tissue plane (as seemingly is the case in of parenchymal nodules, and the absence toms of PH and right heart failure as
Figure 1A where there is “thrombus ad- of a deep vein thrombosis or a venous they present late in the course of their
herent” to the main pulmonary artery). thrombus source should also alert disease. It is therefore advisable, if the
And given the mesenchymal origins of the physician to the possibility of an clinical situation allows, that a center
these vascular tumors, lesions involving alternative diagnosis. Another hint that with expertise in the performance of
the right ventricle and traversing the a neoplasm may be present is “growth endarterectomy surgery should be
pulmonic valve, irregular thickening of of the clot” during what is considered consulted and a referral initiated. The
the RV outflow tract, a “bulging” of a appropriate anticoagulation. Often immediate goals for surgery are similar
main pulmonary artery lesion into the considered an “anticoagulant failure,” the to those for patients with CTEPH: to
outflow tract,4 and adherent lesions in specific enlargement of the previously relieve PH and right heart dysfunction.
the most proximal aspects of the pulmo- imaged clot without new emboli, and This underscores the importance of per-
nary vasculature … especially without the involvement of the very proximal forming as complete an endarterectomy
accompanying emboli in the more distal pulmonary vasculature should again as possible; simply removing visible
vessels … should raise suspicions of a raise concerns that thrombus is not tumor may not provide adequate RV af-
more malignant etiology. These are not the issue. Unusual in this case was the terload. In addition to the possibility of
typical clinical or radiographic features rapidity with which the lesions enlarged, pulmonary hemodynamic improvement,
Advances in Pulmonary Hypertension Volume 15, Number 2; 2016 111
a pulmonary vascular tumor endarterec- to respond to appropriate antico- 54.
tomy will result in tissue acquisition for agulation therapy. 2. Hsing JM, Thakkar SG, Borden EC, Budd
GT. Intimal pulmonary artery sarcoma presenting
diagnostic purposes, tumor debulking, 3. The diagnosis is primarily based
as dyspnea: case report. Int Semin Surg Oncol.
and some survival benefit, albeit variably on imaging studies to include 2007;4:14.
dependent on the extent of resection CTPA, chest MRI, and PET 3. Restrepo CS, Betancourt SL, Martinez-Jime-
and the type of tumor present.5 Rarely scans. nez S, Gutierrez FR. Tumors of the pulmonary
is the tissue type such that a cure is 4. No single imaging study is suf- artery and veins. Semin Ultrasound CT MR.
obtained with surgery. Often surgical ficiently sensitive to exclude the 2012;33(6):580-590.
presence of a pulmonary artery 4. Gan HL, Zhang JQ, Huang XY, Yu W.
resection is simply the first step in the The wall eclipsing sign on pulmonary artery
management of this rare and clinically sarcoma.
computed tomography angiography is pathogno-
challenging neoplasm. Consultation 5. Surgical debulking is the main- monic for pulmonary artery sarcoma. PLoS One.
stay of therapy and may provide a 2013;8(12):e83200.
with radiation and medical oncology is
survival advantage in this patient 5. Blackmon SH, Rice DC, Correa AM, et al.
required to provide the essential multi-
population. Consequently, early Management of primary pulmonary artery sarco-
disciplinary treatment plan to achieve mas. Ann Thorac Surg. 2009;87(3):977-984.
referral to a center of excellence
the best possible outcome. 6. Rafal RB, Nichols JN, Markisz JA. Pulmo-
should be strongly considered.
*William R. Auger, MD nary artery sarcoma: diagnosis and postoperative
University of California, San Diego Acknowledgments: The authors would
follow-up with gadolinium-diethylenetriamine
pentaacetic acid-enhanced magnetic resonance
like to thank Drs David T. Lynch and imaging. Mayo Clin Proc. 1995;70(2):173-176.
Teaching Points Gabriella Cardoza-Favarato from the 7. von Falck C, Meyer B, Fegbeutel C, et al.
Department of Pathology at Brooke Imaging features of primary sarcomas of the great
1. Pulmonary artery sarcomas are Army Medical Center for their assis- vessels in CT, MRI, and PET/CT: a single-center
relatively rare intravascular tumors tance with the preparation and analysis experience. BMC Med Imaging. 2013;13:25.
that may present with signs and of the pathology specimens in this case. 8. Kim HK, Choi YS, Kim K, et al. Surgical
symptoms that mimic acute or treatment for pulmonary artery sarcoma. Eur J
Cardiothorac Surg. 2008;33(4):712-716.
chronic thromboembolic disease.
References 9. Wong HH, Gounaris I, McCormack A, et
2. Pulmonary artery sarcomas should 1. Mandelstamm M. Uber primare Neubildun- al. Presentation and management of pulmonary
be considered in patients who fail gen des Herzens. Virchows Arch. 1923;245(1):43- artery sarcoma. Clin Sarcoma Res. 2015;5(1):3.
ERRATUM
The Volume 15, No 1 issue of Advances in Pulmonary Hypertension contained an error in the PH Grand Rounds col-
umn, “Pulmonary Arterial Hypertension: ‘A Journey to Lung Transplant.” The PVR values in Tables 2 and 3 reflect
an incorrect calculation from the original outside medical records. The editors thank Michael Slack, MD, Professor,
Department of Pediatrics, University of Maryland School of Medicine; Director, Pediatric and Adult Congenital Inter-
ventional Cardiac Catheterization Laboratory, University of Maryland Medical Center, Baltimore, for pointing out this
oversight . Dr Slack reinforces that PVR is the basis for many critical clinical decisions and provides the following 3
different ways to express PVR:
Reference Range
. 5 . 3
Measurement dyn s/cm MPa s/m mmHg.min/l or HRU/Wood units
Pulmonary vascular resistance (PVR) 20-130 2-13 0.25-1.6
In cardiac ICUs, the units of dyn.s/cm5 are often used and the conversion factor between this value and Wood units is,
conveniently, 80. During cardiac catheterization, the convention is to use the Cardiac Index (not cardiac output) and
express the PVR in Wood units, which are indexed to body surface area.
112 Advances in Pulmonary Hypertension Volume 15, Number 2; 2016
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Risk Adjustment Coding PDFDocumento38 pagineRisk Adjustment Coding PDFGordana Puzovic100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Rope NegotiationDocumento4 pagineRope NegotiationTH x TH100% (1)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- A Mindfulness Intervention For Children With Autism Spectrum DisorderDocumento155 pagineA Mindfulness Intervention For Children With Autism Spectrum Disorderclaughlinsr4721Nessuna valutazione finora
- Blood Cells and Its Types With FunctionsDocumento5 pagineBlood Cells and Its Types With Functionskaleb16_2Nessuna valutazione finora
- OrthosisDocumento35 pagineOrthosissinghmenkaNessuna valutazione finora
- Reiki 1 ManualDocumento11 pagineReiki 1 Manualbelgarath2013100% (1)
- The Chemical ImbalanceDocumento70 pagineThe Chemical ImbalancebredabredaNessuna valutazione finora
- Kriya For Balancing The ChakrasDocumento5 pagineKriya For Balancing The ChakrasFedra Fox Cubeddu100% (2)
- Gross Anatomy and Cell Biology of The Lower Urinary Tract: Committee 1Documento66 pagineGross Anatomy and Cell Biology of The Lower Urinary Tract: Committee 1Gordana PuzovicNessuna valutazione finora
- The Spleen1Documento49 pagineThe Spleen1786waqar786Nessuna valutazione finora
- Primary Tracheal Tumors: Review of 37 CasesDocumento4 paginePrimary Tracheal Tumors: Review of 37 CasesGordana PuzovicNessuna valutazione finora
- Renal Cell CarcinomaDocumento70 pagineRenal Cell CarcinomaIsabel ReyNessuna valutazione finora
- Computed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaDocumento6 pagineComputed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaGordana PuzovicNessuna valutazione finora
- Accuracy of Computed Tomography in Small Bowel ObstructionDocumento3 pagineAccuracy of Computed Tomography in Small Bowel ObstructionGordana PuzovicNessuna valutazione finora
- About Lung Cancer: Overview and TypesDocumento13 pagineAbout Lung Cancer: Overview and TypesGordana PuzovicNessuna valutazione finora
- Transient Hepatic Perfusion Differences (THAD/THID) - What? When? Where?Documento35 pagineTransient Hepatic Perfusion Differences (THAD/THID) - What? When? Where?Gordana PuzovicNessuna valutazione finora
- Ho0113 Wu1Documento6 pagineHo0113 Wu1Gordana PuzovicNessuna valutazione finora
- Recurrent Pyogenic Cholangitis: From Imaging To InterventionDocumento8 pagineRecurrent Pyogenic Cholangitis: From Imaging To InterventionGordana PuzovicNessuna valutazione finora
- PIIS1556086416335158Documento12 paginePIIS1556086416335158Gordana PuzovicNessuna valutazione finora
- 1240approach To Pulmonary Nodules - 4Documento18 pagine1240approach To Pulmonary Nodules - 4Gordana PuzovicNessuna valutazione finora
- Spontaneous Ruptured Intercostal and Lumber Artery in Type 1 NeurofibromatosisDocumento15 pagineSpontaneous Ruptured Intercostal and Lumber Artery in Type 1 NeurofibromatosisGordana PuzovicNessuna valutazione finora
- InTech-Advances Bone MetastasesDocumento16 pagineInTech-Advances Bone MetastasesGordana PuzovicNessuna valutazione finora
- Sjogren's Syndrome, Vasculitis, and Cryoglobulinaemia Associated With (Kappa) Paraprotein With Rheumatoid ActivityDocumento3 pagineSjogren's Syndrome, Vasculitis, and Cryoglobulinaemia Associated With (Kappa) Paraprotein With Rheumatoid ActivityGordana PuzovicNessuna valutazione finora
- Role of Triple Phase Computed Tomography Findings For Evaluation of Hepatic LesionsDocumento8 pagineRole of Triple Phase Computed Tomography Findings For Evaluation of Hepatic LesionsGordana PuzovicNessuna valutazione finora
- Prevalence of Solid Tumors in Incidentally Detected Homogeneous Renal Masses Measuring 20 HU On Portal Venous Phase CTDocumento5 paginePrevalence of Solid Tumors in Incidentally Detected Homogeneous Renal Masses Measuring 20 HU On Portal Venous Phase CTGordana PuzovicNessuna valutazione finora
- Guidance on Evaluating and Treating UTIs and ASBDocumento14 pagineGuidance on Evaluating and Treating UTIs and ASBJohn Vincent Dy OcampoNessuna valutazione finora
- Early Onset Pneumonia Likely Caused Stonewall Jackson's DeathDocumento3 pagineEarly Onset Pneumonia Likely Caused Stonewall Jackson's DeathGordana PuzovicNessuna valutazione finora
- Review On Pancreatic Steatosis Detection by Imaging ModalitiesDocumento10 pagineReview On Pancreatic Steatosis Detection by Imaging ModalitiesGordana PuzovicNessuna valutazione finora
- Imaging in Acute Renal Infection: BJU International (2000), 86 Suppl. 1, 70 79Documento10 pagineImaging in Acute Renal Infection: BJU International (2000), 86 Suppl. 1, 70 79Gordana PuzovicNessuna valutazione finora
- Journal of Acute Disease: Study On The Relationship of Acute Ketosis Intoxication and Type 2 Diabetes MellitusDocumento5 pagineJournal of Acute Disease: Study On The Relationship of Acute Ketosis Intoxication and Type 2 Diabetes MellitusGordana PuzovicNessuna valutazione finora
- US and CT Findings in The Diagnosis of Tuberculous PeritonitisDocumento5 pagineUS and CT Findings in The Diagnosis of Tuberculous PeritonitisGordana PuzovicNessuna valutazione finora
- Acute Pancreatitis With Normal Amylase and LipaseDocumento1 paginaAcute Pancreatitis With Normal Amylase and LipaseGordana PuzovicNessuna valutazione finora
- Imaging in Acute Renal Infection: BJU International (2000), 86 Suppl. 1, 70 79Documento10 pagineImaging in Acute Renal Infection: BJU International (2000), 86 Suppl. 1, 70 79Gordana PuzovicNessuna valutazione finora
- Infection and Immunity-1971-Eudy-269.fullDocumento5 pagineInfection and Immunity-1971-Eudy-269.fullGordana PuzovicNessuna valutazione finora
- Early Onset Pneumonia Likely Caused Stonewall Jackson's DeathDocumento3 pagineEarly Onset Pneumonia Likely Caused Stonewall Jackson's DeathGordana PuzovicNessuna valutazione finora
- The Role of HRCT in Post-Traumatic Hypoxemia: Poster No.: Congress: Type: AuthorsDocumento51 pagineThe Role of HRCT in Post-Traumatic Hypoxemia: Poster No.: Congress: Type: AuthorsGordana PuzovicNessuna valutazione finora
- PIIS000349751101188XDocumento7 paginePIIS000349751101188XGordana PuzovicNessuna valutazione finora
- Click Here Click Here To View Optimized Website For Mobile DevicesDocumento4 pagineClick Here Click Here To View Optimized Website For Mobile DevicesFirman SalamNessuna valutazione finora
- Vitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsDocumento70 pagineVitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsRose LiteNessuna valutazione finora
- CCMP 2020 Batch Cardiovascular MCQsDocumento2 pagineCCMP 2020 Batch Cardiovascular MCQsharshad patelNessuna valutazione finora
- Thyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Documento11 pagineThyroid and Antithyroid Drugs - PPTX - 20231126 - 103419 - 0000Vaishnavi SheteNessuna valutazione finora
- PhobiasDocumento10 paginePhobiasapi-276690632Nessuna valutazione finora
- Medical Certificate Guidelines June 2012Documento3 pagineMedical Certificate Guidelines June 2012wudthipanNessuna valutazione finora
- Occupational Therapy Rehabilitation Paraplegic PatientDocumento7 pagineOccupational Therapy Rehabilitation Paraplegic PatientAlina PasăreNessuna valutazione finora
- Don't Steal My Mind!: Extractive Introjection in Supervision and TreatmentDocumento2 pagineDon't Steal My Mind!: Extractive Introjection in Supervision and TreatmentMatthiasBeierNessuna valutazione finora
- Science Blood TransfusionsDocumento10 pagineScience Blood Transfusionsapi-237866019Nessuna valutazione finora
- Giant Skin TagDocumento2 pagineGiant Skin Tagshf.mxlikNessuna valutazione finora
- Expansion Screw Activation Guidelines PDFDocumento1 paginaExpansion Screw Activation Guidelines PDFOsama SayedahmedNessuna valutazione finora
- Science 5Documento81 pagineScience 5Michael Joseph Santos100% (2)
- Diatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDocumento13 pagineDiatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDani Daniela100% (1)
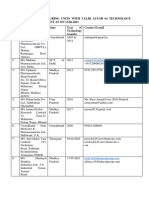
- List of Manufacturing Units With Valid Ayush 64 Technology Transfer Agreement As On 15.06.2021Documento5 pagineList of Manufacturing Units With Valid Ayush 64 Technology Transfer Agreement As On 15.06.2021Sunira EnterprisesNessuna valutazione finora
- Sage Char-Lee ResumeDocumento2 pagineSage Char-Lee Resumeapi-510197139Nessuna valutazione finora
- Staph and Strep Lab Report BMS 501Documento2 pagineStaph and Strep Lab Report BMS 501aruiz93Nessuna valutazione finora
- EFN - PPTX 3Documento9 pagineEFN - PPTX 3Suheni Khotimah IndrianiNessuna valutazione finora
- Ayushman Bharat - KailashDocumento11 pagineAyushman Bharat - KailashKailash NagarNessuna valutazione finora
- Wallen Et Al-2006-Australian Occupational Therapy JournalDocumento1 paginaWallen Et Al-2006-Australian Occupational Therapy Journal胡知行Nessuna valutazione finora
- Clabsi TeamDocumento20 pagineClabsi Teamapi-344209032100% (1)
- NephrologyDocumento5 pagineNephrologyPooja NalluriNessuna valutazione finora
- Navidas-Case StudyDocumento5 pagineNavidas-Case StudyFran LanNessuna valutazione finora
- Jamnagar Thesis 2004Documento12 pagineJamnagar Thesis 2004Swagath NNessuna valutazione finora