Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Shared Psychotic Disorder Case Report in Elderly Sisters
Caricato da
Putra TridiyogaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Shared Psychotic Disorder Case Report in Elderly Sisters
Caricato da
Putra TridiyogaCopyright:
Formati disponibili
Case Report | WVMJ OA
Case Report of Shared Psychotic Disorder or ‘Folie a Deux’ in
Two Geriatric Sisters
Kamal Patel, MD a detailed and implausible story of can be described as a transfer of
Adam Schindzielorz, MD kidnapping and extortion which, delusional beliefs from one person,
Suzanne Holroyd, MD surprisingly, was validated by the the primary patient, to another, the
Marshall University Joan C. Edwards School of patient’s younger sister. Investigation secondary patient.3 The primary
Medicine, Department of Psychiatry
of the story by police and others patient is known as the “dominant”
Corresponding Author: Kamal Patel, MD, Marshall
confirmed it to be false. A diagnosis or “principle” partner and the
University, JCESOM, Dept. of Psychiatry, 1115 20th of shared psychotic disorder was secondary patient, who is influenced
Street, Suite 205, Huntington, WV 25703. Email: made. The delusions appeared by the primary patient, is known as
patelk@live.marshall.edu.
to occur with a rapid onset and “submissive partner” or “associate.”4
resolution. This case highlights the The disorder is mainly presented
Abstract unusual presentation of shared within families, most commonly
Folie a Deux or shared psychotic psychotic disorder in two elderly between husband and wife, as well
disorder is a rare and poorly women, well outside the typical age as between two siblings. Average
understood disorder characterized of onset for the disorder as well age of onset for disorder in both
as transfer of delusional beliefs from as its rapid onset and resolution, primary and secondary patient is
one person, the primary patient, to rather than in the setting of a in the adult age group,4,5,6 however
another, the secondary patient, who chronic psychiatric illness such as may affect any age of population.7
are closely related. The disorder delusional disorder or schizophrenia. Review of literature revealed
is mainly seen within a family, only 17 cases of shared psychotic
most often between spouses or Introduction disorder in the geriatric population,
between siblings, although it has Shared psychotic disorder, also ages 65 and older.8 The disorder
been noted in other relationships. known as “Folie A Deux,” is a rare is more common in females
Females are more likely than males clinical disorder which was first than males for both primary and
to both primary and secondary described by Lasegue and Flare secondary patients.4,5,9 Primary
partner. We present a case of in 18871 and was later divided into patients are typically observed to
a 77-year-old female who was four subgroups by Gralnick in 1942. be more intelligent, older, and more
admitted for myasthenia gravis The disorder now includes the aggressive/dominant whereas the
exacerbation with a two-day history divisions of; Folie Imposee, Folie secondary patients are generally
of generalized weakness, multiple Simultanee, Folie Communiquee, younger, less intelligent, passive,
falls, decreased appetite and blurred and Folie Induit which are further and dependent.3,10 Associated
vision. However, she also described described in Table 1.2 The disorder comorbidity in the primary patient
Table 1: Classification of 4 folie á deux subtypes2
Subtype A – Folie Imposée Most common form of folie a deux, in which the inducer is typically dominant,
intelligent, forceful, and autonomous. The recipient is typically dependent,
submissive, less intelligent, and more passive. Both individual are closely
associated and delusions often disappear upon separation.
Subtype B – Folie Simultanée Appearance of identical psychosis simultaneous in individual who are closely
related and often have genetic link between the two. Folie simultanée has
higher prevalence in elderly. Separation of the individual does not subside the
symptoms of delusion.
Subtype C – Folie Communiquée Transfer of delusion after a long period of resistance by recipient. Recipient
typically develops his or her own delusion, independent of inducer, which
typically persist after separation.
Subtype D – Folie Induite New delusions acquired by individual with delusion under the influence of
another deluded subject.
West Virginia Medical Journal — OA 1
Case Report | WVMJ OA
includes primary psychotic disorders and brought to a secluded property On admission vital signs showed
such as delusional disorder, mood out of state. The patient reported blood pressure 160/90, temperature.
disorder, often with persecutory they were taken into “a complex” 98.2 F., pulse 70, respiratory rate
or grandiose fixations, and called “Care House”, where a 18, and O2 saturation 92% on room
schizophrenia. The secondary nurse told them to sign over their air. Physical exam was remarkable
patient, other than a diagnosis checks, took their belongings and for severe ptosis bilaterally without
of Shared Psychotic Disorder, removed their clothing. The patient exercise, mild limitations with EOMs
typically has no other psychiatric reported she was pulled by her hair and diplopia with vertical gaze.
diagnosis. Here, we report a case and suffered damage to her scalp. There was no breakage of hair was
of shared psychotic disorder in an She reported meeting a man at the noted where the patient reported
elderly 77-year-old female with “complex” who helped them escape. her hair was pulled, however there
no known previous psychiatric She also reported being taken was an area of partial baldness
history and her elderly sister in a to another shelter where she was noted. The rest of the physical
general medical inpatient setting. held captive again, interrogated exam including neurological exam
The case is notable given the age for approximately four hours, was was unrevealing. Head CT without
range of the patients, as well as the hit in the face repeatedly with a contrast did not demonstrate
short duration of the disorder and newspaper and pushed into garbage any acute intracranial process,
that neither patient had a history bags. At some point both patient but did show mild to moderate
of chronic psychiatric illness. and her sister were freed. At that white matter disease. Chest x-ray
point, the patient was reportedly showed no evidence for acute
Case Presentation quite stressed and was admitted cardiopulmonary disease. Complete
The primary patient was a 77-year- to a psychiatric facility for suicidal blood count with differential,
old Caucasian female with a past ideation per hospital record, but complete metabolic panel and
medical history of myasthenia gravis, was discharged in two days after urinalysis were within normal limits
paroxysmal atrial fibrillation, chronic being psychiatrically cleared, noting aside from moderately elevated
obstructive pulmonary disease that her reported suicidality had leukocyte esterase on urinalysis.
(COPD), coronary artery disease, “been falsified”. The sisters then Psychiatry consultation was
hypertension, hyperlipidemia, moved back in with the son until her obtained. She was noted to be in
and gastroesophageal reflux current admission. The patient was clear consciousness, and scored
disease. Years of hospital records noted to dominate the conversation a 30/30 on the Mini-mental status
revealed no history of psychiatric while the sister was present. The examination (MMSE).11 Rapid
disorder. She was admitted to the patient’s sister was also noted to be plasma reagin (RPR), Lyme titers,
hospital with a two-day history of quieter, younger and less aggressive and thyroid tests were within normal
generalized weakness, blurred of the two. Surprisingly, she fully limits. Vitamin B12 was low normal
vision and falls, with a diagnosis of corroborated the patient’s story, at 262. Urine culture was positive for
myasthenia gravis exacerbation. even when interviewed away from E. Coli and she received a one-time
On admission, the patient reported the patient. Per son both patient and dose of fosfomycin. The psychosis
that following a hospital discharge sister were in fact missing four to did not change after her UTI was
approximately one month earlier five days prior to moving back home treated. Psychiatry recommended
for COPD exacerbation, she and with him after being discharged from low-dose risperidone at 0.25mg
sister had temporarily lived with the psychiatric facility. Investigation QHS and outpatient psychiatry
her son, as they were homeless. by police, other agencies and follow-up. Electroencephalogram
She reported going to “Heisted the patient’s son, confirmed the (EEG) was recommended which
House” described as a homeless story to be false, however we are was done on day 6 of inpatient
shelter, to apply for housing with unable to corroborate the locations hospitalization which showed mild
“Mr. J”, however reported being told of both patient and sister during diffuse background slowing, however
it would take some days so to wait those several days they were EEG study was discontinued
outside for a ride to go home. While missing. Although based on the midway due to patient compliance.
waiting, she reported meeting an old description provided by patient The patient was treated with
acquaintance who offered them a it seemed they were most likely pyridostigmine 60 mg TID and
ride, instead they were blindfolded living at a homeless shelter. prednisone 40mg daily for her
West Virginia Medical Journal — OA 2
Case Report | WVMJ OA
myasthenia gravis flare. Following so vividly. Another possibility is an of dominant partner was 38 years
improvement in symptoms, the exacerbation of the myasthenia old and average age of submissive
patient was discharged, but did not gravis (MG), although MG is rarely partner was 36 years old.4 Another
show for her outpatient psychiatric associated with psychosis. However, review of 42 cases from 1993-2005
appointment. Since discharge chronic and long standing MG has showed the mean age in primary
the patient has presented to the been linked to psychotic illness in patient was 52.7 and mean age
emergency department several times several case reports.12 Patient also in secondary patient was 45.9.5
and has been admitted several times was on pyridostigmine for MG which Nevertheless, shared psychotic
for non-psychiatric reasons without is known to have adverse event of disorder may present in any age
any further psychotic symptoms. psychosis. In our case however, group.6,7 To our knowledge, there
psychosis had not been reported are only a small number of shared
Discussion prior or after this admission, making psychotic disorder in the geriatric
There is limited literature on the it less likely that this psychosis was population reported. A review of
prevalence and incidence of shared due to MG or medication. Finally, literature found only 17 cases
psychotic disorder, in part because the patient had multiple vascular of shared psychotic disorder in
patients may not seek treatment risk factors and Head CT revealed individuals aged 65 or older.8
as they don’t recognize their small vessel vascular lesions. It is Interestingly the presentation
symptoms as untrue.9 In this case, it also possible that vascular brain in the geriatric population was
is difficult to be sure of the etiology disease, and perhaps a recent similar to presentation in other
of the psychosis of the primary small vascular event, could have age groups.8 Similarities included
patient. The patient’s lengthy, well been associated with the acute occurring in those who face isolation,
documented history in the hospital onset of the psychosis, although poverty, dependency, presence of
records as well as reports of the we have no direct evidence disorder mainly within the family
son, indicated the patient had no supporting this possibility. and a high rate of persecutory
prior psychiatric history. She had Whatever the cause of the primary delusions.8 Differences between
been seen many times in the ER for patient’s psychosis, it was fully geriatric presentation and other
MG or COPD exacerbation. There believed and accepted by the sister, age groups was that 8 out 17,
was no documentation of psychosis the secondary patient. Our case is or 47% of cases, were classified
in prior admissions. Given how consistent with reported cases in as the “folie simultanee subtype”
open and spontaneous she was that the secondary patient was less where the identical delusion
with describing her psychosis, it is dominant than the primary patient. arises at the same time of two
likely prior psychosis would have However, our case is unusual as the genetically related individuals.8
been noted had it been present onset of shared psychotic disorder Our case has features of folie
in prior records. Thus, given the is typically more gradual and less simultanee but also folie imposee,
acuteness of the development of rapid than what was seen in our characterized by the dominant
this psychosis, it was likely related to case, where the psychotic illness primary patient and the younger,
medical condition, atypical delirium, arose rapidly (within a month) and more submissive secondary patient.
medication or encephalopathy. was quickly adopted by the sister. It
Possible medical causes for is unusual for a delirium psychosis Conclusion
the delirium include her UTI, to be adopted by another, as prior Overall, our case manifests
although her intact cognition, clear cases report the primary patient has multiple unique features of shared
consciousness and remaining a long standing psychiatric illness, psychotic disorder. Our case
psychotic symptoms after the and that was not seen in this case. appears to have been of relatively
treatment of UTI rule against this. Another facet of this case rapid onset and has a strong medical
However, patients who suffer that makes it significant is that it component associated with the
psychosis from delirium due to occurred in two elderly individuals, psychiatric presentation, something
a medical cause may continue well outside of the average age not previously reported in the current
to believe the delusional event of onset for shared psychotic literature. As well, our case adds
happened, even after the resolution disorder. A review of 97 cases to a very small literature of shared
of the delirium because they of shared psychotic disorder in psychotic disorder occurring in
remember the psychotic symptoms Japan revealed the average age elderly persons. Further research
West Virginia Medical Journal — OA 3
Case Report | WVMJ OA
is needed to learn and understand literature. Acta Psychiatrica Scandinavica 9. Sevda Korkmaz, Murat Kuloglu, Mura d
1997: 96: 231-234. Atmaca, and Bulent Bahceci. “Shared
more about this interesting disorder. Psychotic Disorder: A Case Report.” The
5. Danilo Arnone, Anish Patel, Giles Ming-Yee
Tan; The nosological significance of Folie a Journal of Psychiatry and Neurological
Reference Deux: a review of the literature. Annals of Sciences 2010; 23: 206-209
General Psychiatry. 2006, 5:11 10. Haqqi, Sobia, and Nisreen Ali. “Folie a Deux:
1. Lasègue C, Falret J: La folie à deux. Ann Med
A Case Report.” F1000Research 1 (2012): 18.
Psychol. 1877; 18: 321–355. 6. Silveira, J. & Seeman, M. (1995). Shared
PMC. Web. 24 Oct. 2016.
2. Nishihara, Ryan M. and Nakamura, Craig T. Psychotic Disorder: A Critical Review of The
11. Folstein MF, Folstein SE, McHugh PR.
(1993) “A Case Report of Folie’a Deux: Literature. Canadian Journal of Psychiatry, 40,
Husband-and-Wife,” Jefferson Journal of “Mini-mental state”. A practical method for
389–95.
Psychiatry: Vol. 11: Iss. 1, Article 9. grading the cognitive state of patients for the
7. Ghosh P. Shared delusional disorder: A case
3. Benjamin J. Sadock, M.D., Virginia A. Sadock clinician. J Psychiatr Res. 1975
report of Folie a trois. Eur J Psychol Educ Nov;12(3):189-98.
M.D., Pedro Ruiz M.D.; Kaplan & Sadock’s
Studies 2014;1:36-40 12. Musha M, Tanaka F, Ohuti M.Psychoses in
Synopsis of Psychiatry Behavioral Sciences/
Clinical Psychiatry. Eleventh Edition, 2015; pg 8. McNiel, J. N., Verwoerdt, A and Peak, D. three cases with myasthenia gravis and
336 (1972), Folie à Deux in the Aged: Review and thymoma. Proposal of a paraneoplastic
4. Kashiwase H, Kato M. Folie a duex in Case Report of Role Reversal. Journal of the autoimmune neuropsychiatric syndrome.
Japan-analysis of 97 cases in the Japanese American Geriatrics Society, 20: 316–323. Tohoku J Exp Med. 1993;169:335–344.
West Virginia Medical Journal — OA 4
Potrebbero piacerti anche
- Shared Psychotic Disorder - NCBIDocumento8 pagineShared Psychotic Disorder - NCBI5KevNessuna valutazione finora
- Shared Psychotic Disorder: A Case of "Folie A Deux" With A Delusion of PregnancyDocumento3 pagineShared Psychotic Disorder: A Case of "Folie A Deux" With A Delusion of PregnancyJAVED ATHER SIDDIQUINessuna valutazione finora
- Delusional DisorderDocumento47 pagineDelusional DisorderAbelNessuna valutazione finora
- FOLIE A DEUX REVIEWDocumento8 pagineFOLIE A DEUX REVIEWGrandfather NurgleNessuna valutazione finora
- A Romantic Delusion: de Clerambault's Syndrome in Dementia: ReviewarticleDocumento5 pagineA Romantic Delusion: de Clerambault's Syndrome in Dementia: ReviewarticleJenivia LulileloNessuna valutazione finora
- A Case Series of Shared Delusional Infestation: Folie À Deux RevisitedDocumento5 pagineA Case Series of Shared Delusional Infestation: Folie À Deux RevisitednardiniyanNessuna valutazione finora
- Coexistence of Folie Communique e and Folie SimultaneeDocumento4 pagineCoexistence of Folie Communique e and Folie SimultaneeAna Rosa González Barroso0% (1)
- Shared Psychotic Disorder A Case Study Submitted byDocumento27 pagineShared Psychotic Disorder A Case Study Submitted byChin Lee100% (1)
- Pseudoseizures and Dissociative DisordersDocumento5 paginePseudoseizures and Dissociative DisordersLaura AndreiNessuna valutazione finora
- NCMB317: Shared Psychotic DisorderDocumento21 pagineNCMB317: Shared Psychotic DisorderArmand Bong Santiago100% (1)
- Folie en Famille - Case ReportDocumento2 pagineFolie en Famille - Case ReportMarineNessuna valutazione finora
- Delirium: Continuum Lifelong Learning Neurol 2010 16 (2) :120-134Documento15 pagineDelirium: Continuum Lifelong Learning Neurol 2010 16 (2) :120-134Maria Isabel Montañez RestrepoNessuna valutazione finora
- Sexual Delusions in Shared Psychotic Disorder CaseDocumento6 pagineSexual Delusions in Shared Psychotic Disorder CaseAnonymous AVWh40E0O5Nessuna valutazione finora
- Recurrent Depression and Borderline Personality Disorder in A Patient With Ehlers-Danlos SyndromeDocumento4 pagineRecurrent Depression and Borderline Personality Disorder in A Patient With Ehlers-Danlos SyndromeAide SeanezNessuna valutazione finora
- Delusion and Delusional DisordersDocumento63 pagineDelusion and Delusional Disorderssudesh KhanalNessuna valutazione finora
- Basal Cell Carcinoma Develops in Old Chickenpox ScarDocumento2 pagineBasal Cell Carcinoma Develops in Old Chickenpox ScarShubham SinghNessuna valutazione finora
- DELIRIUMDocumento9 pagineDELIRIUMCaio AlvesNessuna valutazione finora
- Chapter 4 DelusionsDocumento14 pagineChapter 4 DelusionsCostrut LaurNessuna valutazione finora
- Headache - 2001 - Jacome - Transitional Interpersonality Thunderclap HeadacheDocumento4 pagineHeadache - 2001 - Jacome - Transitional Interpersonality Thunderclap HeadacheactualashNessuna valutazione finora
- PDFDocumento18 paginePDFaymenNessuna valutazione finora
- Late-onset schizophrenia: Making the right diagnosis in older adultsDocumento6 pagineLate-onset schizophrenia: Making the right diagnosis in older adultsVijay MgNessuna valutazione finora
- Understanding Schizophrenia: Causes, Symptoms, and Treatment ApproachesDocumento57 pagineUnderstanding Schizophrenia: Causes, Symptoms, and Treatment ApproachesBorlongan PaulineNessuna valutazione finora
- Kleine LevinDocumento11 pagineKleine LevinAnonymous GdBua151uNessuna valutazione finora
- Ulhas Mayekar - Folie Á DeuxDocumento3 pagineUlhas Mayekar - Folie Á DeuxJOSEF GABRIEL SCHREINERNessuna valutazione finora
- International Journal of Health Sciences and ResearchDocumento4 pagineInternational Journal of Health Sciences and Researchmamal malikaNessuna valutazione finora
- 385 FullDocumento10 pagine385 FullClínica Dental BludenNessuna valutazione finora
- Pridmore S. Download of Psychiatry, Chapter 4. Last Modified: March, 2022. 1Documento19 paginePridmore S. Download of Psychiatry, Chapter 4. Last Modified: March, 2022. 1vaidyam78Nessuna valutazione finora
- Unusual Mental Illnesses ExploredDocumento3 pagineUnusual Mental Illnesses ExploredJorge Pawee DuranNessuna valutazione finora
- Cotard's Syndrome in A Patient With Schizophrenia Case Report and Review of The LiteratureDocumento8 pagineCotard's Syndrome in A Patient With Schizophrenia Case Report and Review of The LiteratureJeff David Huarcaya VictoriaNessuna valutazione finora
- 2 Bipolar DisorderDocumento9 pagine2 Bipolar DisorderJuan Carlos Veloso RetamalNessuna valutazione finora
- Subtypes of SchizophreniaDocumento5 pagineSubtypes of SchizophreniaAbove BeyondNessuna valutazione finora
- Delusional Disorder MedscapeDocumento14 pagineDelusional Disorder MedscapeHandhy Tanara100% (1)
- Southwestern Internal Medicine Conference: Etiology and Management of DeliriumDocumento11 pagineSouthwestern Internal Medicine Conference: Etiology and Management of DeliriumRenjun HuangNessuna valutazione finora
- Bipolar Disorder - Nejm-31-Junio-2020 PDFDocumento9 pagineBipolar Disorder - Nejm-31-Junio-2020 PDForlandom61Nessuna valutazione finora
- Paranoid SchizophreniaDocumento26 pagineParanoid SchizophreniaCrisha Ann Billones BacutaNessuna valutazione finora
- SCHIZOPHRENIADocumento12 pagineSCHIZOPHRENIAjahanavi12Nessuna valutazione finora
- Alzheimer Early 2010Documento8 pagineAlzheimer Early 2010Matchas MurilloNessuna valutazione finora
- Psychiatry Nursing Seminar: Delusion DisordersDocumento84 paginePsychiatry Nursing Seminar: Delusion DisordersGulmoharNessuna valutazione finora
- Case Study TGDocumento14 pagineCase Study TGapi-545898677Nessuna valutazione finora
- Latah SyndromeDocumento2 pagineLatah SyndromenazNessuna valutazione finora
- Delusional DisorderDocumento4 pagineDelusional DisorderNajm Us Saqib BhatNessuna valutazione finora
- Hysteria, Somatization and The Sick Role: R E KendellDocumento9 pagineHysteria, Somatization and The Sick Role: R E KendellAnisa PersiaNessuna valutazione finora
- The Wrong Answer: by Harold D. Foster, PHD © 2003Documento6 pagineThe Wrong Answer: by Harold D. Foster, PHD © 2003JOSH USHERNessuna valutazione finora
- Administrator,+Journal+manager,+368-1206-1-CE (1)Documento3 pagineAdministrator,+Journal+manager,+368-1206-1-CE (1)Sameer KhanNessuna valutazione finora
- Paranoid Personality Disorder: Case ReportDocumento3 pagineParanoid Personality Disorder: Case ReporttTTNessuna valutazione finora
- Delusional DisorderDocumento22 pagineDelusional Disordernatalauma1Nessuna valutazione finora
- Mental Health Case StudyDocumento12 pagineMental Health Case Studyapi-400900026Nessuna valutazione finora
- Delusional Disorder DSM 5Documento11 pagineDelusional Disorder DSM 5Mohamed Asri Zaini100% (1)
- holguin1967_migraineDocumento8 pagineholguin1967_migraineArif Erdem KöroğluNessuna valutazione finora
- Biology 2 JournalDocumento5 pagineBiology 2 JournalKadymars JaboneroNessuna valutazione finora
- Book Excerpt: 'Psychology's Ghost: The Crisis in The Profession and The Way Back'Documento5 pagineBook Excerpt: 'Psychology's Ghost: The Crisis in The Profession and The Way Back'WBURNessuna valutazione finora
- Dissociation PDFDocumento4 pagineDissociation PDFQonita Amelia SuherlanNessuna valutazione finora
- The True "Mental Block": Origin of Mental Health Stigma and Perception of Filipinos Towards Mental Health and Treatment Over TimeDocumento15 pagineThe True "Mental Block": Origin of Mental Health Stigma and Perception of Filipinos Towards Mental Health and Treatment Over TimeAshleyNessuna valutazione finora
- Bipolar Disorders-KaplanDocumento40 pagineBipolar Disorders-KaplanMarco Dave Gutierrez ParedesNessuna valutazione finora
- LIDZ THEODORE - A Psicosocial Orientation To Schizophrenic DisordersDocumento9 pagineLIDZ THEODORE - A Psicosocial Orientation To Schizophrenic DisordersRodrigo G.Nessuna valutazione finora
- Hypochondriacal DisorderDocumento61 pagineHypochondriacal Disorderdrkadiyala2Nessuna valutazione finora
- Early Alzheimer's Disease: Clinical PracticeDocumento8 pagineEarly Alzheimer's Disease: Clinical Practicemarcolin0Nessuna valutazione finora
- Benign Stupors: A Study of a New Manic-Depressive Reaction TypeDa EverandBenign Stupors: A Study of a New Manic-Depressive Reaction TypeNessuna valutazione finora
- Diabetic Retinopathy Screening UpdateDocumento16 pagineDiabetic Retinopathy Screening UpdatePutra TridiyogaNessuna valutazione finora
- Bulbar Conjunctival Metastasis From Mucoepidermoid Carcinoma of Parotid - A Case Report and Review of LiteratureDocumento3 pagineBulbar Conjunctival Metastasis From Mucoepidermoid Carcinoma of Parotid - A Case Report and Review of LiteraturePutra TridiyogaNessuna valutazione finora
- Diabetic Retinopathy Screening UpdateDocumento16 pagineDiabetic Retinopathy Screening UpdatePutra TridiyogaNessuna valutazione finora
- Shanghai Child Eye Study Tracks Myopia ProgressionDocumento27 pagineShanghai Child Eye Study Tracks Myopia ProgressionPutra TridiyogaNessuna valutazione finora
- The Egyptian Journal of Radiology and Nuclear Medicine: Tamer F. Taha Ali, Abdel-Naser GhareepDocumento6 pagineThe Egyptian Journal of Radiology and Nuclear Medicine: Tamer F. Taha Ali, Abdel-Naser GhareepPutra TridiyogaNessuna valutazione finora
- 1111 PDFDocumento4 pagine1111 PDFPutra TridiyogaNessuna valutazione finora
- Risk factors for high myopia in 22-year studyDocumento9 pagineRisk factors for high myopia in 22-year studyPutra TridiyogaNessuna valutazione finora
- Skripsi Tanpa PembahasanDocumento56 pagineSkripsi Tanpa PembahasanPutri EmNessuna valutazione finora
- Ocular Manifestations of Systemic Lupus Erythematosus 2155 9899.1000191 PDFDocumento9 pagineOcular Manifestations of Systemic Lupus Erythematosus 2155 9899.1000191 PDFPutra TridiyogaNessuna valutazione finora
- The Egyptian Journal of Radiology and Nuclear Medicine: Tamer F. Taha Ali, Abdel-Naser GhareepDocumento6 pagineThe Egyptian Journal of Radiology and Nuclear Medicine: Tamer F. Taha Ali, Abdel-Naser GhareepPutra TridiyogaNessuna valutazione finora
- 1111 PDFDocumento4 pagine1111 PDFPutra TridiyogaNessuna valutazione finora
- The Effect of Herings Law On Different Ptosis RepaDocumento8 pagineThe Effect of Herings Law On Different Ptosis RepaPutra TridiyogaNessuna valutazione finora
- 21 MitrasevicDocumento4 pagine21 MitrasevicPutra TridiyogaNessuna valutazione finora
- Choroidal Tuberculoma As A Presenting Sign of Tube PDFDocumento4 pagineChoroidal Tuberculoma As A Presenting Sign of Tube PDFPutra TridiyogaNessuna valutazione finora
- Mucoepidermoid Carcinoma in The Head and Neck May 2014Documento10 pagineMucoepidermoid Carcinoma in The Head and Neck May 2014Putra TridiyogaNessuna valutazione finora
- Understanding Ocular MelanomaDocumento2 pagineUnderstanding Ocular MelanomaPutra TridiyogaNessuna valutazione finora
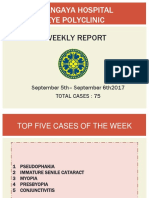
- Wangaya (4-5 September 2017)Documento14 pagineWangaya (4-5 September 2017)Putra TridiyogaNessuna valutazione finora
- Pi Is 0039625711002797Documento10 paginePi Is 0039625711002797Putra TridiyogaNessuna valutazione finora
- Weekly AdiDocumento18 pagineWeekly AdiPutra TridiyogaNessuna valutazione finora
- Hyponatremic Dehydration PathoDocumento4 pagineHyponatremic Dehydration PathoENessuna valutazione finora
- The Complete Hematopathology GuideDocumento113 pagineThe Complete Hematopathology GuideJenny SNessuna valutazione finora
- Depression and Anxiety Among College StudentsDocumento2 pagineDepression and Anxiety Among College StudentsAnonymous 5WUUQijWNessuna valutazione finora
- Acute GastroenteritisDocumento48 pagineAcute Gastroenteritisansam kamalNessuna valutazione finora
- Sir 2Documento5 pagineSir 2Patziedawn GonzalvoNessuna valutazione finora
- Faktor-Faktor Yang Mempengaruhi Gangguan Tidur Pada Pasien Diabetes MelitusDocumento6 pagineFaktor-Faktor Yang Mempengaruhi Gangguan Tidur Pada Pasien Diabetes MelitusImron BuhoriNessuna valutazione finora
- Pediatric Tuberculosis: Causes, Symptoms and TreatmentDocumento112 paginePediatric Tuberculosis: Causes, Symptoms and TreatmentFenny RahmadaniNessuna valutazione finora
- Factors Influencincing Discharge Against Medical Advice Among Paediatric Patients in Abakaliki, Southeastern NigeriaDocumento3 pagineFactors Influencincing Discharge Against Medical Advice Among Paediatric Patients in Abakaliki, Southeastern NigeriaMorayo TimothyNessuna valutazione finora
- PNSS Drug StudyDocumento2 paginePNSS Drug Studyrain peregrinoNessuna valutazione finora
- ID Analisis Sistem Manajemen Program p2 Ispa Di Puskesmas Pegandan Kota PDFDocumento10 pagineID Analisis Sistem Manajemen Program p2 Ispa Di Puskesmas Pegandan Kota PDFFarida HanumNessuna valutazione finora
- The Road To Diagnosis and Treatment in Girls and Boys With ADHD Gender Differences in The Diagnostic ProcessDocumento6 pagineThe Road To Diagnosis and Treatment in Girls and Boys With ADHD Gender Differences in The Diagnostic ProcessOana OrosNessuna valutazione finora
- Exam MCQs - A-1تمDocumento12 pagineExam MCQs - A-1تممصطفى محمد جواد كاظمNessuna valutazione finora
- Functional neurological disorder new subtypes and shared mechanisms - CLINICALKEY - Dr Rivas (1)Documento14 pagineFunctional neurological disorder new subtypes and shared mechanisms - CLINICALKEY - Dr Rivas (1)Fernando Pérez MuñozNessuna valutazione finora
- Tah BsoDocumento27 pagineTah BsoCephradine DolienteNessuna valutazione finora
- Shan AsfDocumento2 pagineShan AsfM.Fizan JavedNessuna valutazione finora
- HAAD Exam For Nurses Questions 2018Documento46 pagineHAAD Exam For Nurses Questions 2018Asif Newaz100% (6)
- Courvosier Law PDFDocumento6 pagineCourvosier Law PDFElno TatipikalawanNessuna valutazione finora
- Understanding Radiation TherapyDocumento24 pagineUnderstanding Radiation Therapyabhilashreddy45Nessuna valutazione finora
- The Floppy Infant:: Evaluation of HypotoniaDocumento13 pagineThe Floppy Infant:: Evaluation of HypotoniaminipredatorNessuna valutazione finora
- Nursing Care Plan for Hiatal Hernia ReliefDocumento3 pagineNursing Care Plan for Hiatal Hernia ReliefLalaine Nadulpit100% (2)
- Cicatricial Atelectasis - Print Friendly - STATdxDocumento2 pagineCicatricial Atelectasis - Print Friendly - STATdxmihaelaNessuna valutazione finora
- COVID-19 Isolation Effects on Mental Health and EconomyDocumento10 pagineCOVID-19 Isolation Effects on Mental Health and EconomyRimsHa ShAbbirNessuna valutazione finora
- VAERS Report Details Deaths and Adverse Events Following COVID VaccinesDocumento234 pagineVAERS Report Details Deaths and Adverse Events Following COVID VaccinesbeneNessuna valutazione finora
- Suppurative Lung DiseasesDocumento39 pagineSuppurative Lung Diseasesmatchees-gone rogueNessuna valutazione finora
- Tif30Documento49 pagineTif30HCX dghhqNessuna valutazione finora
- Dynamics and Neurocognitive Correlates of BPDDocumento27 pagineDynamics and Neurocognitive Correlates of BPDPriya PuriNessuna valutazione finora
- Tatalaksana Tekanan Tinggi Intrakranial Pada Anak-DikonversiDocumento48 pagineTatalaksana Tekanan Tinggi Intrakranial Pada Anak-DikonversiAbdurrahman Arsyad As SiddiqiNessuna valutazione finora
- Oral Pathology in Paediatric Patients-Mini-Systematic ReviewDocumento7 pagineOral Pathology in Paediatric Patients-Mini-Systematic ReviewYuganya SriNessuna valutazione finora
- Cervical SpondylosisDocumento9 pagineCervical SpondylosisNurHidayah Borhanudin100% (1)
- Ekstravasation AssesmentDocumento2 pagineEkstravasation AssesmentHelena Christy100% (1)