Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Nanda 2018
Caricato da
Arizal SetyawanCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Nanda 2018
Caricato da
Arizal SetyawanCopyright:
Formati disponibili
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/262440113
The Nursing Outcomes Classification
Article in Acta Paulista de Enfermagem · December 2008
DOI: 10.1590/S0103-21002009000700004
CITATIONS READS
14 3,367
1 author:
Sue Ann Moorhead
University of Iowa
56 PUBLICATIONS 714 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Evaluation of Nurisng Sensitive Outcome Measures View project
All content following this page was uploaded by Sue Ann Moorhead on 16 February 2016.
The user has requested enhancement of the downloaded file.
Palestra
The Nursing Outcomes Classification
Classificação dos Resultados das Intervenções de Enfermagem
Clasificación de los resultados de las intervenciones de Enfermería
Sue Ann Moorhead1
INTRODUCTION
The research to develop the Nursing Outcomes Classification (NOC) began with the formation of the outcomes
research team in 1991. This work grew from previous language development focused on patient problems or
nursing diagnoses by the North American Nursing Diagnosis Association and the development of nursing interventions
by the Nursing Interventions Classification (NIC) research team at Iowa. Outcome terminology was needed to
complete the clinical reasoning model identified as part of the NIC research(1). Figure 1 depicts this model and its
relationship to clinical reasoning.
Nursing Knowledge
Diagnoses Interventions Outcomes
Classification Classification
Classification
Clinical Decision
Making Choice Choice Choice
Figure 1- Relationship of Nursing Knowledge Classifications to the Nurse’s Clinical Decision Making(2)
This model is based on the nursing process and helps the nurse focus on identifying the three knowledge domains
of nursing focused on diagnoses, interventions and outcomes. Clinical decisions about patient care are made considering
the patient problem, possible outcomes, and the interventions that will improve or eliminate the problems faced by
1
Associate Professor Iowa Board of Nursing. The University of Iowa, EUA.
Corresponding Author: Sue Ann Moorhead
1903 West Garfield - Davenport, Iowa - 52804
E-mail: sue-moorhead@uiowa.edu
Acta Paul Enferm 2009;22(Especial - 70 Anos):868-71.
The Nursing Outcomes Classification 869
the patient. This is not a linear process but is based on the reflection of the nurse on the patient’s responses to
treatment. Alterations in the plan are made as vaiations occur in the expected outcomes.
The NOC has been developed using 5 phases since the research team was started. Phase 1 focused on pilot work
to test methodologies for developing outcomes from 1992 to 1993. This phase of the research was funded by
Sigma Theta Tau International. Phase 2 was devoted to the construction of the first set of outcomes (1993-1996)
and the publication of the first edition of the classification(3). Phase 3 (1996-1997) focused on the construction of a
taxonomy of the classification and the beginning of clinical testing of the outcomes. This expanded the classification
from an alphabetical list to a structure to group related concepts in a three-tiered structure and was published in the
second edition(4). Phase 4 (1998-2002) was dedicated to evaluation of the measurement scales in NOC in a variety
of settings. Phase 5 has focused on the refinement and clinical use of the outcomes and has been ongoing since 1997.
Funding for phases 2 through 5 was obtained from the National Institutes of Health, National Institute of Nursing.
The last ten years has been devoted to refining the outcomes previously published, the development of new outcomes,
assisting practicing nurses to implement NOC in their practice, and assisting educators to include NOC in curriculum
revisions.
RESEARCH METHODS USED TO DEVELOP NOC
Multiple research methods have been used in the development of NOC. An inductive approach was used to develop
the outcomes based on current practice and research. Concept analysis and research team review were used in the
construction of the outcomes. Questionnaire surveys of expert nurses were used to assess the content validity and nursing
sensitivity of the outcomes. The taxonomy was constructed using similarity/dis-similarity analysis and hierarchical clustering
techniques. Feedback from clinical test sites and other sites implementing NOC have been used to identify new outcomes
for development and refine current outcomes. Inter-rater reliability and criterion measures were used to evaluate the
reliability, validity, and sensitivity of the outcome measures in clinical sites. This data was included in the third edition of
NOC(5). Expert review continues to be used as new outcomes are developed.
THE BASICS OF USING NOC AND MEASURING OUTCOMES
The fourth edition of NOC published in 2008(6) contains 385 outcomes. Each outcome consists of a definition,
set of indicators, measurement scale(s) and supporting references. Outcomes can be focused on the patient or
caregiver, the family as the unit of analysis, or on a community or population. “A nursing-sensitive patient outcome
is an individual, family, or community stat, behavior or perception that is measured along a continuum in response to
nursing interventions”(6). The outcomes are developed as variable concepts that can be measured along a continuum
using a measurement scale. A 5-point Likert scale is used with all outcomes. The “five” represents that best possible
score on the outcome and the “one” represents the worst possible score. A five-point scale allows for an adequate
number of responses to demonstrate variability in the outcome state, perception, or behavior of interest to the
nurse. The outcome is measured prior to nursing interventions to establish a baseline score. The outcome is then
rated again post intervention to determine a change score for the outcome. Outcome change scores can be positive
(the outcome rating increase), negative (the outcome rating decreased) or there can be no change (the outcome stayed
the same).
We advocate the use of a “reference person” when measuring outcomes. A reference person is an individual of
the same age and gender. For example a female patient who is 30 years old should be compared to a healthy woman
age 30. This is important to keep the rating of “5” as the score for a healthy person across settings and populations.
This does mean that patients with chronic illness that impact the outcomes may not be able to achieve a “5” rating
due to their chronic illness. We do not want the top rating to be undermined by conditions that reflect the best state
of the patients the nurse work. This is especially true for patients with medical conditions such as congestive heart
failure, renal failure, dementia, or other serious conditions.
The NOC outcomes are at a higher level of abstraction than the goals nurses have typically included in care plans. The
indicators provide examples of more specific states, perceptions, or behaviors usually seen as indicative of the outcome.
The indicators can also be rated as individual items to identify key areas to target with the selected nursing interventions.
This may be especially helpful as nurses learn to use NOC. These indicators are not summed to create an overall score
because we know some indicators are more important for determining the outcome than others. Further research is
needed to identify the key indicators for each outcome. These may vary by patient population, setting, or specialty practice.
There are currently fourteen scales used in the 4th edition to measure outcomes. In this edition there are 298
Acta Paul Enferm 2009;22(Especial - 70 Anos):868-71.
870 Moorhead SA.
outcomes that use only one scale. Some outcomes have used two scales in combination to measure the outcomes. In
this case there is a primary scale used to determine change scores. The most commonly used scales are Severely
compromised to Not compromised (measures a patient state); Never demonstrated to Consistently Demonstrated
(measures a patient behavior); No knowledge to Extensive knowledge (to measure patient knowledge) and Not at
all satisfied to Completely satisfied (to measure a perception). Nurses determine the interval for outcome measurement
based on clinical judgment as to when the effects of interventions need to be assessed. This may vary across patient
populations and settings. Organization policies may also affect measurement intervals. At minimum outcomes should
be measured on admission for a baseline, at discharge or transfer to another unit, and when there is a significant
change in status for the outcome.
We have attempted to link knowledge outcomes with corresponding outcomes focused on behavior. We think
these are important outcomes for nurses to determine the behavioral outcomes associated with the teaching
interventions they perform. For example, the outcome Knowledge: Asthma is associated with the following behavioral
outcomes: Asthma Self-Management, Energy Conservation, Health Seeking Behavior, Symptom Control, and Risk
Control: Infectious Process to name a few. These behavioral outcomes reflect the effect of acquiring knowledge to
better control this disease. These behavioral outcomes will help document the value of nursing care for patients with
chronic illness and the importance of interventions focused on teaching the patients about their health conditions.
RESOURCES FOR USING NOC
The Outcome-Present State Test (OPT) Model developed by Pesut and Herman(7) is an excellent model to help
nurses with clinical reasoning in complex patient situations. This model is supportive of the original model of knowledge
development and clinical reasoning developed by the NIC team and focuses on clinical reasoning beginning with the
patient’s story. The key components of the model are cue logic using clinical reasoning webs. These webs help the nurse
identify the capstone issue, or the priority problem to focus care planning. The model uses reflection, framing, testing
and decision-making process to compare the present state with future state following the chosen intervention. NOC
outcomes provide the concepts for comparing present state and future state component of the model and can be
enhanced by using NANDA diagnoses and NIC interventions as concepts for the other knowledge domains.
Another resource for nurses using NANDA diagnoses, NIC Interventions and NOC outcomes is the book devoted
to combing the content of all three knowledge bases. This “linkage book” identified several NOC outcomes and
associated NIC interventions for all NANDA diagnoses published to date(8). There have been two edition of this text
to date(8-9). The current edition focuses on all diagnoses published in the 2006-2008 classification of NANDA
International(10). This book is a useful tool for nurses and students learning to use all three languages to describe the care
they provide to patients, regardless of population or setting. Case studies in this book are helpful for educators to use
in their courses.
CONCLUSION
The use of standardized languages is becoming more prevalent in practice and education because nursing textbooks
are including the use the nursing languages such as NOC and staff nurses and faculty are becoming more familiar
with them. The validation of standardized languages and their use in nursing practice and research is still in its infancy,
but is important to the nursing profession as the implementation of evidence-based practice and the electronic
medical record provide more opportunities to test the use of standardized languages in practice settings. For
standardized, nursing languages such as NOC to become consistently used, it requires consistent incorporation of the
languages in nursing practice, education, and research. Models that support clinical decision making are important
tools for assisting nurses to improve the care they provide to patients and their families.
REFERENCES
1. McCloskey JC, Bulechek GM, editors. Nursing interventions classification (NOC): Iowa Outcomes Project. St. Louis:
classification (NIC): Iowa Intervention Project. St. Louis: Mosby; c1997.
Mosby Year Book; 1992. 4. Johnson M, Maas M, Moorhead S, editors. Nursing
2. McCloskey JC, Bulechek GM, editors. Nursing interventions outcomes classification (NOC). Iowa Outcomes Project: 2nd
classification (NIC): Iowa Intervention Project. 2nd ed. St. ed. St. Louis: Mosby; 2000.
Louis: Mosby; c1996. p.6 5. Moorhead S, Johnson M, Maas M, editors. Nursing
3. Johnson M, Maas M, editors. Nursing outcomes outcomes classification (NOC). 3rd ed. St. Louis: Mosby;
Acta Paul Enferm 2009;22(Especial - 70 Anos):868-71.
The Nursing Outcomes Classification 871
2004. and NIC linkages. St. Louis: Mosby; 2006.
6. Moorhead S, Johnson M, Maas M, Swanson E, editors. 9. Johnson M, Bulechek G, Maas M, McCloskey Dochterman
Nursing outcomes classification (NOC). 4th ed. St. Louis: J, Moorhead S, editors. Nursing diagnoses, outcomes and
Mosby; 2008. interventions: NANDA, NOC, and NIC linkages. St.
7. Pesut DJ, Herman J. Clinical reasoning: the art and science Louis: Mosby; c2001.
of critical & creative thinking. Boston: Delmar; 1999. 10. North American Nursing Diagnosis Association. NANDA
8. Johnson M, Bulechek G, Butcher H, Maas M, McCloskey nursing diagnoses: definitions & classification, 2006-2008.
Dochterman J, Moorhead S, Swanson L. Nursing 7th ed. Philadelphia: North American Nursing Diagnosis
diagnoses, outcomes and interventions: NANDA, NOC, Association; 2006.
Acta Paul Enferm 2009;22(Especial - 70 Anos):868-71.
View publication stats
Potrebbero piacerti anche
- Health Perception and ManagementDocumento4 pagineHealth Perception and ManagementChardaina Angela de MateoNessuna valutazione finora
- Best Practice Statement AuditDocumento2 pagineBest Practice Statement Auditns officeNessuna valutazione finora
- Taylor's Clinical Nursing Skills, Chapter 2 Fundamentals of Nursing, The Art and Science of Nursing, 5 Edition, Chapters 12-16Documento1 paginaTaylor's Clinical Nursing Skills, Chapter 2 Fundamentals of Nursing, The Art and Science of Nursing, 5 Edition, Chapters 12-16Eyji GeronimoNessuna valutazione finora
- Nursing Assessment: Terry White, MBA, BSNDocumento70 pagineNursing Assessment: Terry White, MBA, BSNgireeshsachinNessuna valutazione finora
- The Perioperative NursingDocumento11 pagineThe Perioperative NursingDa BondadNessuna valutazione finora
- SWOT Analysis of The Emergency ServiceDocumento20 pagineSWOT Analysis of The Emergency ServiceScribdTranslationsNessuna valutazione finora
- Bundle Care 2022Documento10 pagineBundle Care 2022Kalla Daniel SharonNessuna valutazione finora
- Standard Treatment Protocol STP For Basic Health Services Bhs Package 2078Documento310 pagineStandard Treatment Protocol STP For Basic Health Services Bhs Package 2078Manang HospitalNessuna valutazione finora
- Diazepam CompiledDocumento41 pagineDiazepam CompiledyayayanizaNessuna valutazione finora
- 260 AssignmentDocumento6 pagine260 Assignmentapi-284107243Nessuna valutazione finora
- Postoperative PhaseDocumento8 paginePostoperative PhasereymarhayNessuna valutazione finora
- of Abg ResearchDocumento20 pagineof Abg ResearchKhirabdhi Tanaya Sahu100% (1)
- Anxiety NCPDocumento4 pagineAnxiety NCPMARK JASON DIAZNessuna valutazione finora
- Betty NeumanDocumento27 pagineBetty Neumanapi-241413796Nessuna valutazione finora
- Nursing Ethics 2018Documento43 pagineNursing Ethics 2018mustafaNessuna valutazione finora
- Nursing Process and DocumentationDocumento96 pagineNursing Process and Documentationkirwat8100% (1)
- N375 Critical Thinking Activity ExampleDocumento6 pagineN375 Critical Thinking Activity ExamplefaizaNessuna valutazione finora
- Nursing Care of Patient With Cushing Syndrome and PheochromocytomaDocumento43 pagineNursing Care of Patient With Cushing Syndrome and PheochromocytomaMaica LectanaNessuna valutazione finora
- MeaslesDocumento32 pagineMeaslesYum C100% (2)
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDocumento2 pagineNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term OutcomesDeanne Carla DalilisNessuna valutazione finora
- NCPDocumento2 pagineNCPMelissa David100% (1)
- Case Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic DisordersDocumento1 paginaCase Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic Disordersclyde i am100% (1)
- PostoperativeDocumento21 paginePostoperativeCitra AyuMerilasariNessuna valutazione finora
- Triage and Priority SettingDocumento10 pagineTriage and Priority SettingekonurcahyaningrumNessuna valutazione finora
- Module 3 Responsibilities of A Beginning Nurse ResearcherDocumento9 pagineModule 3 Responsibilities of A Beginning Nurse ResearcherCaitlynNessuna valutazione finora
- Relationship Between Nursing Handoff Quality and Continuity of Care in Intensive Care UnitDocumento12 pagineRelationship Between Nursing Handoff Quality and Continuity of Care in Intensive Care UnitImpact JournalsNessuna valutazione finora
- The Development of Nursing Care Model in Patients With Total Knee Replacement Reconstructive SurgeryDocumento17 pagineThe Development of Nursing Care Model in Patients With Total Knee Replacement Reconstructive SurgeryGlobal Research and Development ServicesNessuna valutazione finora
- Chapter 7 The Nurse-Client Relationship PDFDocumento9 pagineChapter 7 The Nurse-Client Relationship PDFJa YaNessuna valutazione finora
- Intravenous CannulationDocumento9 pagineIntravenous CannulationjeorjNessuna valutazione finora
- TB QuestionnaireDocumento1 paginaTB QuestionnaireaplesgjskNessuna valutazione finora
- 130300-Standards For Acute and Critical Care NursingDocumento12 pagine130300-Standards For Acute and Critical Care Nursingapi-315277523Nessuna valutazione finora
- Operating RoomDocumento8 pagineOperating Roomjonathan_tinsayNessuna valutazione finora
- Patient ChartDocumento2 paginePatient ChartHydieNessuna valutazione finora
- ICU Burns GuidelineDocumento24 pagineICU Burns GuidelineJonas BlaineNessuna valutazione finora
- Drugs For EmergencyDocumento25 pagineDrugs For EmergencyJunathan L. DelgadoNessuna valutazione finora
- IV Cannulation ChecklistDocumento2 pagineIV Cannulation ChecklistDo0odi AlharbiNessuna valutazione finora
- Nursing Care Plans PresentationDocumento37 pagineNursing Care Plans PresentationRa DiantNessuna valutazione finora
- Pre and Post-Operative Care of Patient For Mastectomy: Prepared By: Gianne T. Gregorio RNDocumento13 paginePre and Post-Operative Care of Patient For Mastectomy: Prepared By: Gianne T. Gregorio RNmalathiNessuna valutazione finora
- This Study Resource Was: Chamberlain College of NursingDocumento5 pagineThis Study Resource Was: Chamberlain College of NursingHugsNessuna valutazione finora
- Wound Healing and Wound CareDocumento15 pagineWound Healing and Wound CareNinaNessuna valutazione finora
- Emergency Document For UHDocumento16 pagineEmergency Document For UHShahidul Islam ChowdhuryNessuna valutazione finora
- JCI Standards Only 6th Ed HospitalDocumento12 pagineJCI Standards Only 6th Ed HospitalHengkyNessuna valutazione finora
- Critical Care - Criteria For Admission & Role of NurseDocumento64 pagineCritical Care - Criteria For Admission & Role of NurseProf. Ramsharan MehtaNessuna valutazione finora
- Pressure SoresDocumento43 paginePressure SoresArpanpatelNessuna valutazione finora
- Skin TractionDocumento5 pagineSkin TractionSuharyono100% (1)
- Activities of Management Functions of Head NurseDocumento4 pagineActivities of Management Functions of Head NurseJennah Ricci TuazonNessuna valutazione finora
- Thoracentesis Reflective EssayDocumento2 pagineThoracentesis Reflective EssayAnjae GariandoNessuna valutazione finora
- Nursing Assessment S - O Pt. May ManifestDocumento4 pagineNursing Assessment S - O Pt. May Manifestk_a1990Nessuna valutazione finora
- Critical Thinking and Clinical ReasoningDocumento39 pagineCritical Thinking and Clinical ReasoningAsad KhanNessuna valutazione finora
- Delmar Cengage Learning Companions - Nursing Fundamentals - Caring & Clinical Decision MakingDocumento3 pagineDelmar Cengage Learning Companions - Nursing Fundamentals - Caring & Clinical Decision MakingjjjNessuna valutazione finora
- Nursing Diagnosis TemplateDocumento6 pagineNursing Diagnosis Templatesdk6972Nessuna valutazione finora
- Perioperative NursingDocumento22 paginePerioperative NursingSusiyadiNessuna valutazione finora
- The 5 Steps of The Nursing ProcessDocumento2 pagineThe 5 Steps of The Nursing ProcessManish DafdaNessuna valutazione finora
- NIC and NOCDocumento4 pagineNIC and NOCFernando Oliveira0% (1)
- Using Client Outcome Monitoring As A Tool For SupervisionDocumento5 pagineUsing Client Outcome Monitoring As A Tool For SupervisionDianaSantiago100% (1)
- Defining The Nursing ProcessDocumento6 pagineDefining The Nursing ProcessBrandy RaeNessuna valutazione finora
- Outcome Assessment in Routine Clinical Practice inDocumento21 pagineOutcome Assessment in Routine Clinical Practice inicuellarfloresNessuna valutazione finora
- Nursing Outcome ClassificationDocumento69 pagineNursing Outcome Classificationjm122894100% (1)
- Critical Appraisal of Systematic Reviews PDFDocumento12 pagineCritical Appraisal of Systematic Reviews PDFMuhammad HidayatNessuna valutazione finora
- Ebp in Nursing PaperDocumento8 pagineEbp in Nursing Paperapi-676526945Nessuna valutazione finora
- Praktikum Mikro 4Documento1 paginaPraktikum Mikro 4Arizal SetyawanNessuna valutazione finora
- Orange Musical PPT TemplateDocumento27 pagineOrange Musical PPT TemplateArizal SetyawanNessuna valutazione finora
- Hasil Try Out Ujikom Keperawatan 2.1Documento69 pagineHasil Try Out Ujikom Keperawatan 2.1Arizal SetyawanNessuna valutazione finora
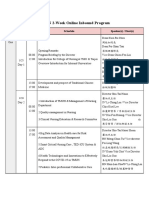
- TMUN 2-Week Online Inbound Program: Week Day Time Schedule Speaker(s) / Host(s)Documento3 pagineTMUN 2-Week Online Inbound Program: Week Day Time Schedule Speaker(s) / Host(s)Biyan MahfudzNessuna valutazione finora
- Kelompok 5Documento6 pagineKelompok 5Arizal SetyawanNessuna valutazione finora
- Ukuran Baju Pramuka NewDocumento2 pagineUkuran Baju Pramuka NewRizKi FerdianNessuna valutazione finora
- Nanda 2018Documento5 pagineNanda 2018Arizal SetyawanNessuna valutazione finora
- ن مقرر علم النفس التأهيليDocumento38 pagineن مقرر علم النفس التأهيليZEINABNessuna valutazione finora
- Philippine Pop CultureDocumento4 paginePhilippine Pop CultureDeez nutNessuna valutazione finora
- 1.1 - Understanding Context in Fiction AnsweredDocumento4 pagine1.1 - Understanding Context in Fiction AnsweredJoãoPauloRisolidaSilvaNessuna valutazione finora
- Innate Human DrivesDocumento13 pagineInnate Human Drivessunny170Nessuna valutazione finora
- Middle Range Theories Application To Nursing Research-2013 - CD PDFDocumento372 pagineMiddle Range Theories Application To Nursing Research-2013 - CD PDFBobby Febri Krisdiyanto100% (11)
- Effective Learning and Teaching: P L T S M TDocumento17 pagineEffective Learning and Teaching: P L T S M TN. SivaNessuna valutazione finora
- Psychogenic Itch: Reviewarticle OpenaccessDocumento8 paginePsychogenic Itch: Reviewarticle OpenaccessRudolf KiraljNessuna valutazione finora
- Personality Recognition Applying Machine LearningDocumento5 paginePersonality Recognition Applying Machine LearningMritunjay KumarNessuna valutazione finora
- CAPE Coommunication Studies Expository PDocumento3 pagineCAPE Coommunication Studies Expository PNarvinLallsaroopNessuna valutazione finora
- Psychoanalytic Theory: (Sigmund Freud)Documento10 paginePsychoanalytic Theory: (Sigmund Freud)Trixie MalinaoNessuna valutazione finora
- The Effectiveness of Creative Writing in Language LearningDocumento44 pagineThe Effectiveness of Creative Writing in Language LearningFebie Grace TorralbaNessuna valutazione finora
- Crucial Conversations 2Documento7 pagineCrucial Conversations 2api-250871125Nessuna valutazione finora
- Performance Management KFCDocumento29 paginePerformance Management KFCEduard Militaru100% (1)
- Smaller and Smaller Circles - OutlineDocumento2 pagineSmaller and Smaller Circles - OutlinevincentNessuna valutazione finora
- Fulltext PDFDocumento15 pagineFulltext PDFece142Nessuna valutazione finora
- SCT-DD Sentence Completion Test QuestionnaireDocumento4 pagineSCT-DD Sentence Completion Test QuestionnaireDharya Nagpal33% (3)
- Summary For Martin Heidegger, "Building, Dwelling, Thinking"Documento3 pagineSummary For Martin Heidegger, "Building, Dwelling, Thinking"Zahid5391Nessuna valutazione finora
- A Study On RetentionDocumento37 pagineA Study On RetentionRakesh SharmaNessuna valutazione finora
- Personal Productivity EbookDocumento26 paginePersonal Productivity Ebookrcoca_1Nessuna valutazione finora
- Case Study Leadership and Power or PoliticsDocumento3 pagineCase Study Leadership and Power or PoliticsLOKESH KUMAR SINHANessuna valutazione finora
- Fiedler's Contingency Model of LeadershipDocumento11 pagineFiedler's Contingency Model of Leadershipjoy pamorNessuna valutazione finora
- List of Undergraduate Majors (Bachelor Degree) in Hebei Normal UniversityDocumento4 pagineList of Undergraduate Majors (Bachelor Degree) in Hebei Normal UniversityKeven KeppiNessuna valutazione finora
- Anthropometry and ErgonomicsDocumento6 pagineAnthropometry and ErgonomicsNIKITA JAINNessuna valutazione finora
- Flanagan (2014) Unmet Needs Maladaptive ModesDocumento15 pagineFlanagan (2014) Unmet Needs Maladaptive ModesCristina ColoteloNessuna valutazione finora
- Gertrude and Paul's RelationshipDocumento3 pagineGertrude and Paul's RelationshipFemSam100% (1)
- Lessonplan How Plants SurviveDocumento8 pagineLessonplan How Plants SurviveEllen DispoNessuna valutazione finora
- TopgradingDocumento7 pagineTopgradingAnone SoreeNessuna valutazione finora
- Resume 2021Documento2 pagineResume 2021api-552423920Nessuna valutazione finora
- Consent For IV SedationDocumento2 pagineConsent For IV Sedationapi-280346448Nessuna valutazione finora