Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Lesson 38 Parenteral Nutrition
Caricato da
Darren Balbas0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
19 visualizzazioni3 pagineTitolo originale
Lesson 38 Parenteral Nutrition.docx
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
19 visualizzazioni3 pagineLesson 38 Parenteral Nutrition
Caricato da
Darren BalbasCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 3
Lesson 38: Parenteral Nutrition Both PN and PPN must be administered through
tubing with the use of an in-line filter to trap crystals in the
Parenteral nutrition (PN) refers to the administration solution.
of nutrients by a route other than the GI tract (e.g., the A 0.22-µm filter is sufficient for the administration of
bloodstream); PN provides carbohydrates, fats, and proteins solutions without lipid additives.
in the form of amino acids, vitamins, minerals, trace
elements, water, and electrolytes. Lipids (Fat Emulsion)
Insulin may be added to control the blood glucose
level because of the high concentration of glucose in the PN Lipids, or fat emulsion, are administered to prevent
solution. or correct fatty acid deficiency.
Heparin may be added to reduce buildup of a Fat emulsion may be administered into a peripheral
fibrinous clot at the catheter’s tip. vein.
Assess the client for allergy to eggs or any of the
Indications components of the lipid emulsion solution; commercial lipid
PN is used when the gastrointestinal (GI) tract is emulsions are formulations of safflower oil, soybean oil, or a
severely dysfunctional or non-functional. combination, with glycerol added for tonicity and egg
Multiple GI surgeries, GI trauma, intestinal phospholipid as an emulsifying agent.
obstruction, severe intolerance of enteral feedings, and any Examine the bottle for separation of emulsion into
other time that the bowel needs to rest for healing are layers or fat globules and for the accumulation of froth. If any
indications for the use of PN. of these findings is noted, do not use the solution; instead,
Acquired immunodeficiency syndrome return it to the pharmacy.
(AIDS), cancer, and malnutrition are other conditions that Do not put additives into the fat emulsion solution.
sometimes require the use of PN. Do not use an IV filter to administer a lipid emulsion-
only solution; particles in the fat emulsion are too large to
Guidelines for Administering Parenteral Nutrition pass through filters.
Check the components of the solution against the If the fat emulsion has been added to the PN
health care provider’s prescription. solution, use a filter gauge of 1.2 µm or larger to allow it to
The solution should be stored under refrigeration pass through.
and administered within 24 hours of the time when it was The solution is supplied in a glass container for
prepared. (Remove the solution from the refrigerator 30 administration; use vented IV tubing.
minutes to 1 hour before use.) Initially the infusion is usually administered at 1.0
A solution that is cloudy or darkened should not be mL/min; check vital signs every 10 minutes and observe the
used; instead, it should be returned to the pharmacy. client for adverse reactions, especially in the first 30 minutes
As a means of preventing infection and solution of the infusion; if signs of an adverse reaction occur, stop the
incompatibility, intravenous (IV) medications and blood are infusion and notify the health care provider.
not given through the PN line. If no adverse reaction occurs, adjust the flow to the
Monitor electrolytes, albumin, and liver and renal prescribed rate.
function parameters. Monitor serum lipids for 4 hours after the infusion is
A therapeutic response to PN is signaled by weight discontinued.
gain, ideally 1 to 3 lb (0.5 to 1.4 kg) per week. Monitor laboratory values for evidence of impaired
liver function, indicating the liver’s inability to metabolize the
Intravenous Access lipids.
PN is administered by way of central venous access Complications of Parenteral Nutrition
(subclavian or internal jugular vein, shown in the figure) when
the client requires a high concentration of carbohydrates Pneumothorax
(more than 10% glucose). Pneumothorax, an accumulation of air between the
When it is anticipated that PN will be required for an lung and chest cavity, is a rare complication of central line
extended period (more than 4 weeks), a more permanent placement.
catheter (e.g., a peripherally inserted central catheter (a.k.a. a Once the catheter has been inserted, a portable
PICC line), a tunneled catheter, or an implanted vascular chest x-ray is obtained to confirm correct catheter placement
access device may be used. and to detect the presence of a pneumothorax.
Peripheral parenteral nutrition (PPN), administered PN is not initiated until correct catheter placement is
through a peripheral vein, is used for short periods (5 to 7 verified and the absence of pneumothorax is verified.
days) to deliver isotonic or mildly hypertonic solutions; the
delivery of highly hypertonic solutions into peripheral veins Air Embolism
can cause sclerosis, phlebitis, or swelling.
Air embolism — an air bubble in the bloodstream — Watch for other signs of hyperglycemia, especially
is a complication associated with central line placement and the “three P’s”: polydipsia, polyuria, and polyphagia.
tubing changes. Start sliding-scale insulin therapy (regular insulin
Instruct the client in the Valsalva maneuver for administration on the basis of blood glucose level) as
tubing and cap changes. prescribed.
For tubing and cap changes, place the client in a
head-down position with the head turned in the opposite
direction from the insertion site to increase intrathoracic
venous pressure.
Check all catheter connections and tape tubing Hypoglycemia
connections. Hypoglycemia is usually a result of an abrupt
If an air embolism is suspected, place the client in a discontinuation of PN solution.
left side–lying position with the head lower than the feet (to When discontinuing PN, gradually decrease the rate
trap air in right side of the heart), administer oxygen as of infusion; when an infusion of hypertonic glucose is
prescribed, and notify the health care provider. stopped, an infusion of 10% dextrose should be instituted and
maintained for 1 to 2 hours to prevent hypoglycemia.
Infection Assess the blood glucose level 1 hour after
Infection in a client receiving PN is usually catheter- discontinuing PN.
related; the PN solution contains a high concentration of Watch for other signs of hypoglycemia.
glucose, making it an ideal medium for bacterial growth. Prepare to administer glucose if hypoglycemia
Use strict aseptic technique. occurs.
Monitor the client’s temperature and assess the site
of IV access for redness, swelling, tenderness, or drainage. Home Care Instructions for Parenteral Nutrition
If signs of infection appear at the site, the IV line
must be removed and restarted at a different site, the tip of Teach the client how to obtain, store, and administer
the IV catheter is sent to the laboratory for culture, and blood PN fluids.
specimens for culture are obtained. Teach the client how to change a sterile dressing.
Change the PN solution every 12 to 24 hours or in Instruct the client to check his or her weight each
accordance with agency protocol. day, at the same time of day and wearing similar clothing.
Change the IV tubing in accordance with CDC Stress that weight gain of more than 3 lb/wk (1.4
guidelines and agency protocol. kg/week) may indicate excessive fluid intake and should be
Change the dressing at the IV site per CDC guidelines reported to the health care provider.
and agency protocol. Teach the client to check the blood glucose level and
report abnormalities immediately.
Fluid Overload Instruct the client and family to watch for signs and
Fluid overload, an excess of fluid in the body, occurs symptoms of complications; provide the client with a list of
when an IV solution is administered too rapidly. these signs and symptoms and discuss the need to contact
As a means of preventing fluid overload, PN is always the health care provider.
delivered with the use of an electronic infusion device. Instruct the client to report edema of the arm or at
Never increase the infusion rate to catch up if an IV the catheter insertion site, neck pain, or jugular distention as
infusion falls behind. possible signs of thrombosis.
Monitor the client's intake and output. Leakage of fluid from the insertion site or pain or
In addition to watching for other signs of fluid discomfort as the fluid is infused may indicate displacement
overload, weigh the client daily. The ideal weight gain with PN of the catheter and must be reported immediately.
is 1 to 3 lb/wk (0.5 to 1.4 kg), so any greater gain is cause for Stress to the client the importance of follow-up care.
concern.
Priority Points to Remember!
Hyperglycemia
Hyperglycemia is usually caused by the components After a central venous catheter is inserted, a portable
of the PN solution itself. chest radiograph should be performed to confirm correct
Assess the client for history of glucose intolerance catheter placement and to detect pneumothorax. PN should
and review the client’s medication history (e.g., not be initiated until it is determined that no pneumothorax is
corticosteroids may increase blood glucose). present.
Begin the infusion at a slow rate (usually 40 mL/hr), Check the components of the PN solution against the
as prescribed. health care provider’s prescription.
Check the blood glucose concentration every 4 to 6 PN solution should be stored under refrigeration and
hours or in accordance with agency protocol. administered within 24 hours of the time at which the
solution was prepared. (Remove the solution from the
refrigerator 30 minutes to 1 hour before use.)
PN solution that is cloudy or darkened should not be
used; instead, it should be returned to the pharmacy.
PN is always delivered with the use of an electronic
infusion device.
As a means of preventing infection and solution
incompatibility, IV medications and blood are never given
through the PN line.
Before administering lipids, assess the client for an
allergy to eggs or any of the components of the lipid emulsion
solution.
Examine the lipid preparation for separation of
emulsion into layers or fat globules and for the accumulation
of froth; if such separation is noted, do not use the solution
and return it to the pharmacy.
Use strict aseptic technique when caring for the
central venous catheter. (Not only is the central line a possible
avenue for the entry of microorganisms into the body, but the
PN solution also contains a high concentration of glucose,
making it an ideal medium for bacterial growth).
Check the blood glucose level every 4 to 6 hours or in
accordance with agency protocol.
If an air embolism is suspected, place the client in a
left side–lying position with the head lower than the feet
(which traps air in right side of the heart), administer oxygen
as prescribed, and notify the health care provider.
To help prevent hypoglycemia, gradually decrease
the infusion rate when discontinuing PN.
Provide instructions to the client who will be
receiving PN at home.
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Skoog GravimeteryDocumento54 pagineSkoog GravimeteryDarren BalbasNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Lesson 35 Medication Administration and Dose CalculationsDocumento4 pagineLesson 35 Medication Administration and Dose CalculationsDarren RossNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- O o o o o o O: DescriptionDocumento34 pagineO o o o o o O: DescriptionDarren BalbasNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- QSDocumento4 pagineQSDarren BalbasNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- SWSDDDocumento33 pagineSWSDDDarren BalbasNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- DDocumento56 pagineDDarren Balbas100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Lesson 43 Acid-Base BalanceDocumento3 pagineLesson 43 Acid-Base BalanceDarren RossNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Lesson 41: Diagnostic Tests, Treatments, and Procedures: DescriptionDocumento13 pagineLesson 41: Diagnostic Tests, Treatments, and Procedures: DescriptionDarren BalbasNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- O o o o o o o o oDocumento10 pagineO o o o o o o o oDarren BalbasNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- For Sale FinalDocumento1 paginaFor Sale FinalDarren BalbasNessuna valutazione finora
- Lesson 45: Fluid and Electrolyte ImbalancesDocumento6 pagineLesson 45: Fluid and Electrolyte ImbalancesDarren BalbasNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- XaxaxDocumento3 pagineXaxaxDarren BalbasNessuna valutazione finora
- DCDVDocumento2 pagineDCDVDarren BalbasNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Lesson 1: Infant, Child, and Adolescent: NewbornDocumento7 pagineLesson 1: Infant, Child, and Adolescent: NewbornDarren BalbasNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- OMSBExams FAQsDocumento5 pagineOMSBExams FAQsعبد الهادي اشهرNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Report On Monitoring and Evaluation-Ilagan CityDocumento5 pagineReport On Monitoring and Evaluation-Ilagan CityRonnie Francisco TejanoNessuna valutazione finora
- BS 215-2-1970-Aluminium Conductors and Aluminium Conductors Steel-Reinforced For Overhead Power TransmissionDocumento16 pagineBS 215-2-1970-Aluminium Conductors and Aluminium Conductors Steel-Reinforced For Overhead Power TransmissionDayan Yasaranga100% (2)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Measures For FloodsDocumento4 pagineMeasures For FloodsMutsitsikoNessuna valutazione finora
- 6 - European Cluster Partnership For Excellence - European Cluster Collaboration PlatformDocumento5 pagine6 - European Cluster Partnership For Excellence - European Cluster Collaboration PlatformDaniela DurducNessuna valutazione finora
- Model 900 Automated Viscometer: Drilling Fluids EquipmentDocumento2 pagineModel 900 Automated Viscometer: Drilling Fluids EquipmentJazminNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Manual TV Hyundai HYLED3239iNTMDocumento40 pagineManual TV Hyundai HYLED3239iNTMReinaldo TorresNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Under Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisDocumento13 pagineUnder Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisMahmud RahmanNessuna valutazione finora
- Coc 1 ExamDocumento7 pagineCoc 1 ExamJelo BioNessuna valutazione finora
- Face Detection and Recognition Using Opencv and PythonDocumento3 pagineFace Detection and Recognition Using Opencv and PythonGeo SeptianNessuna valutazione finora
- Java Edition Data Values - Official Minecraft WikiDocumento140 pagineJava Edition Data Values - Official Minecraft WikiCristian Rene SuárezNessuna valutazione finora
- Vtoris 100% Clean Paypal Transfer Guide 2015Documento8 pagineVtoris 100% Clean Paypal Transfer Guide 2015Sean FrohmanNessuna valutazione finora
- FM Testbank-Ch18Documento9 pagineFM Testbank-Ch18David LarryNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- MikoritkDocumento6 pagineMikoritkChris Jonathan Showip RouteNessuna valutazione finora
- IELTS Material Writing 1Documento112 pagineIELTS Material Writing 1Lê hoàng anhNessuna valutazione finora
- Limestone Standards PDFDocumento2 pagineLimestone Standards PDFJacqueline BerueteNessuna valutazione finora
- Model DPR & Application Form For Integrated RAS PDFDocumento17 pagineModel DPR & Application Form For Integrated RAS PDFAnbu BalaNessuna valutazione finora
- دور أخلاقيات الأعمال في تحسين أداء المنظماتDocumento14 pagineدور أخلاقيات الأعمال في تحسين أداء المنظماتChaima LaifaNessuna valutazione finora
- Bobcat E34 - E35Z Brochure - Adare MachineryDocumento8 pagineBobcat E34 - E35Z Brochure - Adare MachineryNERDZONE TVNessuna valutazione finora
- How To Make An Effective PowerPoint PresentationDocumento12 pagineHow To Make An Effective PowerPoint PresentationZach Hansen100% (1)
- Historical Perspective of OBDocumento67 pagineHistorical Perspective of OBabdiweli mohamedNessuna valutazione finora
- Microbiological Quality Ice CreamDocumento9 pagineMicrobiological Quality Ice CreamocortezlariosNessuna valutazione finora
- NJEX 7300G: Pole MountedDocumento130 pagineNJEX 7300G: Pole MountedJorge Luis MartinezNessuna valutazione finora
- 16-ELS-Final-Module 16-08082020Documento18 pagine16-ELS-Final-Module 16-08082020jeseca cincoNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Partnership LiquidationDocumento46 paginePartnership LiquidationSewale Abate79% (19)
- Beng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtDocumento9 pagineBeng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtMarcelo BaptistaNessuna valutazione finora
- Name of The Business-Rainbow Blooms LLC. Executive SummaryDocumento17 pagineName of The Business-Rainbow Blooms LLC. Executive SummaryAhamed AliNessuna valutazione finora
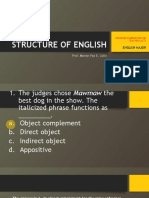
- LET-English-Structure of English-ExamDocumento57 pagineLET-English-Structure of English-ExamMarian Paz E Callo80% (5)
- Aqa Ms Ss1a W QP Jun13Documento20 pagineAqa Ms Ss1a W QP Jun13prsara1975Nessuna valutazione finora
- Philpost RRDocumento6 paginePhilpost RRGene AbotNessuna valutazione finora
- Load Schedule: DescriptionDocumento1 paginaLoad Schedule: Descriptionkurt james alorroNessuna valutazione finora
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora