Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cox2 Inhibitors As Anti-Inflammatory Agents
Caricato da
danny17phTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cox2 Inhibitors As Anti-Inflammatory Agents
Caricato da
danny17phCopyright:
Formati disponibili
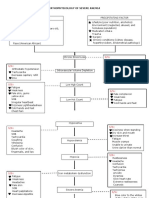
CARDIOVASCULAR DISORDERS 2
UNIT NO. 4
COX2 INHIBITORS AS ANTI-INFLAMMATORY AGENTS
A/P Leong Keng Hong
ABSTRACT celecoxib.
Pain and inflammation are common problems in clinical
practice. Anti-inflammatory drugs are one of the most GUIDELINES FOR CHOICE OF MEDICATION
often prescribed groups of medications. The issue is that
they carry gastrointestinal (GI) and cardiovascular (CV)
risks. Therefore, anti-inflammatory drugs should be used
Therefore, when choosing a medication to reduce pain and
mostly in the setting of inflammation. Non inflammatory inflammation, there are a few considerations. First, does the
pain can be managed with other groups of drugs and pain have a significant inflammatory component? If not, it
therapies. For patients who do need anti-inflammatory may be better to opt for other alternatives such as simple
agents, the choice is dependent on the GI and CV risk analgesics, e.g. paracetamol, or short-term opioid derivatives, e.g.
profile of the patient. Where possible, efforts should be tramadol. An example of such a condition is osteoarthritis.
directed to the underlying cause of the pain and
inflammation.
Second, is there a treatment for the underlying cause? If there
is, then all efforts should be directed at treating the underlying
Keywords: NSAID; Coxib; Anti-inflammatory; disease. An example is gout. For those with tophi, renal stones,
and frequent arthritic flares, the therapeutic goal is to drive the
SFP2017; 43(1): 19-20 serum uric acid to below the saturation point of 6 mg/dl or 360
mmol/l. Another example is rheumatoid arthritis. There are now
INTRODUCTION
so many effective Disease Modifying Anti-Rheumatic Drugs
Pain and inflammation are common problems in the
(DMARDs), including the newer and more effective biological
management of many types of patients. Inflammation can be
DMARDs targeting TNF, IL6, CD20, and JAK3. Third, what
intense, such as in acute gout or severe flares of rheumatoid
is the risk profile of the patient regarding NSAIDs and
arthritis. This requires treatments which reduce inflammation
coxibs? If the patient has significant GI or CV risk and still needs
and pain while waiting for other treatments to take effect which
an NSAID or coxib, then the choice is for one that minimises
will modify and control the underlying disease. On the other
these side effects.
hand, there are causes of pain which have a minimal
component of inflammation. An example is osteoarthritis
The question then arises. Are all NSAIDs and coxibs the same
which is essentially a degenerative non-inflammatory
with regards to GI and CV risks?
condition. These occur in older patients who are more prone to
peptic ulcers and cardiovascular events. Non-steroidal
In the CONDOR trial (Celecoxib versus Omeprazole aNd
anti-inflammatory drugs (NSAIDs), including COX2
Diclofenac in patients with Osteoarthritis and Rheumatoid
inhibitors, can give rise to these two categories of side effects. In
arthritis),2 comparing celecoxib with diclofenac in patients with
addition, they have an adverse impact on control of
rheumatoid arthritis and osteoarthritis, they studied patients
hypertension, may worsen renal function, and cause fluid
with existing GI risk. Earlier studies had shown that in such
retention.
patients, there are similar upper GI outcomes for coxibs alone
versus NSAIDs plus proton pump inhibitor (PPI). In
Aspirin was discovered in the late 19th century but it was not
CONDOR, risks to both upper and lower GI tract were assessed
until the 1970s that the mechanism of the cyclo-oxygenase
and the celecoxib performed better than NSAID plus PPI.
enzyme inhibiting prostaglandin production was clarified by
John Vane and other workers in the field.1 This gave rise to the
In the MEDAL study,3 etoricoxib was compared with
development of NSAIDs and subsequently the COX2
diclofenac. Etoricoxib had fewer GI events but more
inhibitors. However with time, it became clear that although
renovascular adverse events compared to diclofenac, especially
COX2 inhibitors reduce the incidence of gastrointestinal (GI)
hypertension. The 2 drugs were comparable for CV events.
side effects, some of them like rofecoxib, which has been
withdrawn, increased cardiovascular (CV) events. Currently,
Another trial looking at CV events was the CNT trial (Coxib
some parts of the world have given approval to the continued
and traditional NSAID Trialists’ Collaboration Trial).4 This was
use of etoricoxib and most parts of the world continue to use
a meta-analysis of 280 trials which compared NSAID vs placebo
and 474 trials of one NSAID versus another NSAID. The
findings were that high-dose diclofenac, ibuprofen, and coxibs
increased CV risk but naproxen had a lower risk than other
LEONG KENG HONG
NSAIDs, including coxibs. Heart failure risk was doubled and
Consultant Rheumatologist
Leong Keng Hong Arthritis And Medical Clinic interestingly all treatment groups including coxibs had increased
GI risk compared to placebo.
A large-scale trial was started in 2006 and was completed in
T H E S I N G A P O R E F A M I L Y P H Y S I C I A N V O L 4 3(1) J ANUARY -M ARCH 2 0 1 7 : 19
COX2 INHIBITORS AS ANTI-INFLAMMATORY AGENTS
2016. This trial, PRECISION (Prospective Randomised REFERENCES
Evaluation of Celecoxib Integrated Safety versus Ibuprofen Or 1. Flower RJ. The development of COX2 inhibitors. Nat Rev Drug
Discov. 2003;2:179–91.
Naproxen) recruited 24,222 patients with primary outcomes of
2. Chan FK, Lanas A, Scheiman J, Berger MF, Nguyen H, Goldstein JL.
first occurrence of cardiovascular death, non-fatal myocardial Celecoxib versus omeprazole and diclofenac in patients with
infarction, or non-fatal stroke. Secondary outcomes include osteoarthritis and rheumatoid arthritis (CONDOR): a randomised
clinically significant GI events. The trial should further clarify trial. Lancet. 2010;376:173–9.
the choice of NSAIDs or coxibs in the management of patients 3. Combe B, Swergold G, McLay J, McCarthy T, Zerbini C, Emery P,
with GI or CV risk. et al. Cardiovascular safety and gastrointestinal tolerability of
etoricoxib vs diclofenac in a randomized controlled clinical trial (The
For osteoarthritis, a consensus guideline published in 20155 MEDAL study). Rheumatology (Oxford). 2009;48:425–32.
suggested the following approach: 4. Coxib and traditional NSAID Trialists' (CNT) Collaboration.
Vascular
and upper gastrointestinal effects of non-steroidal anti-inflammatory
For patients with low GI and low CV risk, any non-selective drugs:
NSAID (ns-NSAID) is acceptable. meta-analyses of individual participant data from randomised trials.
Lancet. 2013;382:769–79.
For low GI and high CV risk, naproxen is preferred as it has 5. Scarpignato C, Lanas A, Blandizzi C, Lems WF, Hermann M, Hunt
lower CV risk than other ns-NSAIDs or coxibs. Celecoxib at 200 RH, et al. Safe prescribing of non-steroidal anti-inflammatory drugs in
mg once daily is also acceptable. patients with osteoarthritis--an expert consensus addressing benefits
as well as gastrointestinal and cardiovascular risks. BMC Med.
2015;13:55.
For high GI and low CV risk, a coxib alone or ns-NSAID with
PPI is acceptable. Only celecoxib has benefit for both upper and
lower GI tract.
For high GI and high CV risk, it is best to avoid the use of
NSAIDs and coxibs altogether.
In conclusion, anti-inflammatory agents such as NSAIDs and
coxibs are one of the most often used groups of medications in
clinical practice. It is important for the doctor to be vigilant
about the appropriate use of these drugs to gain the maximum
benefit/risk ratio for their patients.
LEARNING POINTS
• For non-inflammatory causes of pain, avoid NSAIDs and coxibs. Opt for other groups of
medications such as simple analgesics.
• If there is an underlying illness causing the pain and inflammation, direct efforts at treating the
condition adequately.
• For those who do need anti-inflammatory agents, choose a specific drug based on the patient’s risk
for GI and CV events.
T H E S I N G A P O R E F A M I L Y P H Y S I C I A N V O L 4 3(1) J ANUARY -M ARCH 2 0 1 7 : 20
Potrebbero piacerti anche
- Treatment and Rehabilitation Center-CARAGA: EmailDocumento1 paginaTreatment and Rehabilitation Center-CARAGA: Emaildanny17phNessuna valutazione finora
- How To Make Homemade Ice CreamDocumento5 pagineHow To Make Homemade Ice Creamdanny17phNessuna valutazione finora
- Rehab in The Time of Drug WarDocumento5 pagineRehab in The Time of Drug Wardanny17phNessuna valutazione finora
- Philippine Eagles HymnDocumento2 paginePhilippine Eagles Hymndanny17ph100% (8)
- Molave Hotel: Carlitos HostelDocumento2 pagineMolave Hotel: Carlitos Hosteldanny17phNessuna valutazione finora
- While in ChinaDocumento1 paginaWhile in Chinadanny17phNessuna valutazione finora
- The Ongoing Evolution of Rotaract Is Redefining Its Place Within RotaryDocumento6 pagineThe Ongoing Evolution of Rotaract Is Redefining Its Place Within Rotarydanny17phNessuna valutazione finora
- Bond Investing Guide 1 To 3Documento4 pagineBond Investing Guide 1 To 3danny17phNessuna valutazione finora
- Primary Care Approach To ProteinuriaDocumento6 paginePrimary Care Approach To Proteinuriadanny17phNessuna valutazione finora
- Diagnosis and Management of Bacterial Meningitis in The Pediatric PopulationDocumento8 pagineDiagnosis and Management of Bacterial Meningitis in The Pediatric Populationdanny17phNessuna valutazione finora
- The Emergency Management and Treatment of Severe BurnsDocumento5 pagineThe Emergency Management and Treatment of Severe Burnsdanny17phNessuna valutazione finora
- Care of The Critically Ill Emergency Department Patient With Acute Kidney InjuryDocumento6 pagineCare of The Critically Ill Emergency Department Patient With Acute Kidney Injurydanny17phNessuna valutazione finora
- JFP - GrandRounds Red Eye, Blurry Vision and CoughDocumento3 pagineJFP - GrandRounds Red Eye, Blurry Vision and Coughdanny17phNessuna valutazione finora
- "Basal Cell Blanche" - A Diagnostic Maneuver To Increase Early Detection of Basal Cell CarcinomasDocumento3 pagine"Basal Cell Blanche" - A Diagnostic Maneuver To Increase Early Detection of Basal Cell Carcinomasdanny17phNessuna valutazione finora
- How Should We Manage An Acute Exacerbation of COPDDocumento3 pagineHow Should We Manage An Acute Exacerbation of COPDdanny17phNessuna valutazione finora
- How Should We Care For Atopic DermatitisDocumento2 pagineHow Should We Care For Atopic Dermatitisdanny17phNessuna valutazione finora
- JFP - GrandRounds Red Eye, Blurry Vision and CoughDocumento5 pagineJFP - GrandRounds Red Eye, Blurry Vision and Coughdanny17phNessuna valutazione finora
- Revisiting Spirometry in The Diagnosis of COPD PDFDocumento1 paginaRevisiting Spirometry in The Diagnosis of COPD PDFdanny17phNessuna valutazione finora
- Neck Mass How Would You TreatDocumento5 pagineNeck Mass How Would You Treatdanny17phNessuna valutazione finora
- Fever, Rash, and Peeling SkinDocumento4 pagineFever, Rash, and Peeling Skindanny17phNessuna valutazione finora
- How Should We Diagnose and Treat Osteoarthritis of The KneeDocumento3 pagineHow Should We Diagnose and Treat Osteoarthritis of The Kneedanny17phNessuna valutazione finora
- How Should We Diagnose and Treat Obstructive Sleep ApneaDocumento2 pagineHow Should We Diagnose and Treat Obstructive Sleep Apneadanny17phNessuna valutazione finora
- Hormone Replacement Therapy The Right Choice For Your PatientDocumento9 pagineHormone Replacement Therapy The Right Choice For Your Patientdanny17phNessuna valutazione finora
- How Should We Evaluate Constipation in Infants and ChildrenDocumento3 pagineHow Should We Evaluate Constipation in Infants and Childrendanny17phNessuna valutazione finora
- Diff Use Abdominal Pain, VomitingDocumento4 pagineDiff Use Abdominal Pain, Vomitingdanny17phNessuna valutazione finora
- Neck Mass How Would You TreatDocumento5 pagineNeck Mass How Would You Treatdanny17phNessuna valutazione finora
- How Should We Evaluate Constipation in Infants and ChildrenDocumento2 pagineHow Should We Evaluate Constipation in Infants and Childrendanny17phNessuna valutazione finora
- Diabetic Foot Ulcer and Poor Compliance How Would You TreatDocumento9 pagineDiabetic Foot Ulcer and Poor Compliance How Would You Treatdanny17phNessuna valutazione finora
- Dyspnea, PancytopeniaDocumento4 pagineDyspnea, Pancytopeniadanny17phNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Causes of Ischemic Stroke: October 2010Documento19 pagineCauses of Ischemic Stroke: October 2010Pajokka 10Nessuna valutazione finora
- Acute Renal FailureDocumento33 pagineAcute Renal FailureAqsa Akbar AliNessuna valutazione finora
- Updated How To Deal ACS in Limited Resources Facilities - Danie Syahrir, DR., SP - JPDocumento32 pagineUpdated How To Deal ACS in Limited Resources Facilities - Danie Syahrir, DR., SP - JPmaria sintaNessuna valutazione finora
- Anterior Triangle of NeckDocumento13 pagineAnterior Triangle of NeckÑäd ÉèmNessuna valutazione finora
- Drug Study: Patient: B.V Age: 58y/oDocumento2 pagineDrug Study: Patient: B.V Age: 58y/oAndrea Sibayan SorianoNessuna valutazione finora
- Xeljanz Initiation ChecklistDocumento8 pagineXeljanz Initiation ChecklistRawan ZayedNessuna valutazione finora
- Duty Report: March 24 2021Documento54 pagineDuty Report: March 24 2021Abi ArifiNessuna valutazione finora
- Gynecology: 3.09 - AmenorrheaDocumento13 pagineGynecology: 3.09 - AmenorrheaAnna Mae MarantanNessuna valutazione finora
- Mksap PulmonaryDocumento77 pagineMksap PulmonaryAna Roman100% (4)
- Guillain Barre Syndrome: M.Widiastuti Samekto Fak - Kedokteran UndipDocumento30 pagineGuillain Barre Syndrome: M.Widiastuti Samekto Fak - Kedokteran UndipDani Yustiardi Munarso100% (1)
- Febrile Convulsion & EpilepsyDocumento17 pagineFebrile Convulsion & EpilepsyprajwalNessuna valutazione finora
- March 7 2013 Mount Ayr Record-NewsDocumento14 pagineMarch 7 2013 Mount Ayr Record-NewsMountAyrRecordNewsNessuna valutazione finora
- Precocious PubertyDocumento13 paginePrecocious PubertyLee Woan ChyiNessuna valutazione finora
- Cirrhosis AndrewDocumento33 pagineCirrhosis Andrewlionel andreaNessuna valutazione finora
- A Clinical Vignette On Raoultella Planticola BacteremiaDocumento5 pagineA Clinical Vignette On Raoultella Planticola BacteremiaJamie FleetNessuna valutazione finora
- Cases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseDocumento3 pagineCases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseIrma Suriani DarwisNessuna valutazione finora
- Student - Surgery - August 27 PDFDocumento242 pagineStudent - Surgery - August 27 PDFAselian BenedictorNessuna valutazione finora
- A 68-Year-Old Man With Swollen Legs: Exemplary CBCR Case 2Documento14 pagineA 68-Year-Old Man With Swollen Legs: Exemplary CBCR Case 2nadim13Nessuna valutazione finora
- Neuro UrologyDocumento53 pagineNeuro UrologymoominjunaidNessuna valutazione finora
- 2.D17 419 Kastriot Meqa Agim BegzatiDocumento6 pagine2.D17 419 Kastriot Meqa Agim BegzatiAndi Ndaru WNessuna valutazione finora
- Fecal IncontinenceDocumento25 pagineFecal IncontinenceBinita ShresthaNessuna valutazione finora
- GBS MCQDocumento6 pagineGBS MCQMoonNessuna valutazione finora
- Pathophysiology of Severe AnemiaDocumento3 paginePathophysiology of Severe AnemiaChrizley Shawn DeroniaNessuna valutazione finora
- Bipolar Disorders and Carbamazepine PharmacokinetiDocumento5 pagineBipolar Disorders and Carbamazepine PharmacokinetiAgr YuroNessuna valutazione finora
- The Medical Management of Abnormal Uterine Bleeding in Reproductive-Aged WomenDocumento14 pagineThe Medical Management of Abnormal Uterine Bleeding in Reproductive-Aged Womendiegoesteban1234Nessuna valutazione finora
- Shin LuluDocumento2 pagineShin LuluEka HimawanNessuna valutazione finora
- 01 Admission Discharge Criteria and TriageDocumento5 pagine01 Admission Discharge Criteria and TriageSuhasani JainNessuna valutazione finora
- Hyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreDocumento7 pagineHyperglycemia in Pregnant Ladies and Its Outcome Out in The Opd, Labor Ward, Gynecology and Obstetrics, Lady Atichison Hospital, LahoreiajpsNessuna valutazione finora
- Paces Guide 2012 From Online NotesDocumento228 paginePaces Guide 2012 From Online NotesThistell ThistleNessuna valutazione finora
- Neurophysiology: Understanding How The Nervous System WorksDocumento72 pagineNeurophysiology: Understanding How The Nervous System WorkshardianNessuna valutazione finora