Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Standard Operating Procedures: C T R C
Caricato da
Carissa CkTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Standard Operating Procedures: C T R C
Caricato da
Carissa CkCopyright:
Formati disponibili
Standard Operating Procedures
Clinical and Translational Research Center
Title: Intravenous Therapy- Initiation and Management of
Peripheral Lines
Approved Effective
March 19, 2012
By: Date:
Number of Page 1 of 5 Revised
Pages: Date:
Purpose:
To provide standards for the initiation and management of peripheral
intravenous therapy, with consideration of participant safety, and comfort,
and to meet study goals.
Policy:
A. All clinical research nurses must be certified in the performance of
I.V. therapy procedures before performing these procedures
without supervision.
B. I.V. certified clinical research nurses may initiate and discontinue
intravenous therapy upon a physician’s order and per protocol.
These nurses may restart a peripheral line without a physician’s
order for site changes due to infiltration, phlebitis, or the inability to
get protocol required blood draws from the site.
C. I.V. certified clinical research nurse may initiate a venipuncture
utilizing the upper extremities.
D. The needle/catheter gauge is determined by the nurse, based upon
protocol requirements, condition of veins, and number and amount
of blood draws, using the largest gauge feasible.
Page | 1 Clinical and Translational Science Institute
E. A physician’s order is necessary for the initiation of the peripheral
line. A physician’s order is necessary for the initiation of I.V. study
infusions. Study drug infusions will be initiated per protocol and
physician order.
F. An IV will not be attempted if the nurse cannot locate an
appropriate site, and/or if the participant expresses the desire to
exit from the study.
G. If a CTRC nurse is unable to start an IV after a thorough participant
assessment and/or two attempts at venipuncture, another CTRC
nurse should be requested to assess and attempt
H. A CTRC nurse will attempt up to two venipunctures.
If unsuccessful, another CTRC nurse or the nurse manager may
attempt to start the IV with the verbal permission of the
participant. If unsuccessful or lacking the permission of the
participant , the Principal Investigator will be notified of the
difficulty in initiating a peripheral catheter and the study procedure
will be aborted.
I. For in-patient participants, peripheral catheters may remain in
place for up to 96 hours if there is no evidence of phlebitis,
infection or infiltration.
J. IV tubing sets for in-patient participants will be changed every 96
hours.
k. Lidocaine 1% (without epinephrine), EMLA cream, Lidocaine patch
or Spray and Stretch may be used as a local anesthetic prior to
catheter insertion if not prohibited by the protocol.
l. A new catheter will be used for each attempt at initiating
venipuncture.
M. Once inserted the catheter may be ordered for KVO to normal
saline or IV saline-lock depending on study protocol.
N. For protocols where study drugs are not given via I.V. infusions,
Heploks or I.V. saline-locks will be placed as a prophylaxis. A
physician’s order will be necessary for the initiation of venous
access.
Page | 2 Clinical and Translational Science Institute
O. When study drug infusions are completed, the infusion bag and
tubing will be removed and the I.V. will be saline-locked while the
participant is in the protocol observation period.
P. The IV bag which contained the study medication will be
photocopied and the copy placed in the participant’s chart.
Q. The intravenous catheter will be removed before the participant
leaves the CTRC, unless the participant is to remain in house, per
protocol.
R. participants with venous access must remain in the CTRC while the
catheter is in place unless accompanied by a staff member.
PROCEDURE:
A. Insertion of IV for saline locks or IV drip
1. Check for signed, dated approved consent form, signed
physician’s orders, and completed inclusion/exclusion
criteria form.
2. Ascertain the participant’s ID, name, date of birth. Assess
the participant’s understanding of the study and the
procedure to done at this visit.
3. Explain procedure to participant.
4. Wash hands thoroughly or use hand sanitizer.
B. Prepare study procedure equipment:
1. Inspect the integrity of equipment.
2. Correct IV solution (study medication) as ordered by the
Principal Investigator and per protocol.
3. Angiocath, largest bore suitable for participant’s veins
4. IV administration set with clave connectors
5. Extension tubing set
6. Stopcock set up for pre and post infusion blood draws
Page | 3 Clinical and Translational Science Institute
7. Tegaderm
8. Alcohol swabs
9. 2x2 sterile gauze pads
10. Tourniquet
11. Squeeze ball
C. Initiation of IV Therapy:
1. If you are not drawing a blood sample immediately after
insertion of the IV catheter, prime the extension tubing
with a normal saline filled syringe. If you are using an IV
drip for his procedure hook IV tubing set to normal saline
bag and prime tubing. Insert and prime stopcocks if
necessary for procedure.
2. Select site considering the purpose and duration of the
procedure. In general look for the largest vein available,
usually anticubital.
3. Assess the condition of the participant’s veins by palpation
4. Apply tourniquet above intended IV site. Tie tourniquet in
a manner to allow release with one hand.
5. Apply tightly enough to impede venous flow, without
occluding arterial flow.
6. Application of heat in the form of heat packs may be used
as indicated for promotion of venous dilatation.
7. Prepare insertion site by cleansing with alcohol prep using
aseptic technique starting from center of proposed site and
in a circular motion away from site for 30 seconds.
8. Do not touch the prepped area with your fingers. If
palpable reassessment of the vein needs to be done, re-
prep the skin prior to venipuncture.
9. Don clean gloves.
10. Insert angiocath at the prepared site, apply pressure to
vein just proximal to insertion site and remove needle.
Page | 4 Clinical and Translational Science Institute
11. Release tourniquet, while applying pressure to vein just
above insertion site to prevent bleeding.
12. Attach extension tubing and IV tubing, if using, and open
roller clamp.
13. Secure angiocath to skin using Tegaderm.
14. If using stopcocks and IV set up, secure stopcocks to skin
of forearm supporting them with folded sterile 2x2 gauze
dressings and paper tape.
15. Ensure that IV drip rate is appropriate.
References:
Appendices:
Page | 5 Clinical and Translational Science Institute
Potrebbero piacerti anche
- Ivf ProcedureDocumento4 pagineIvf ProcedureKATHLEEN JOSOLNessuna valutazione finora
- Standardized Central Line Placement ProcedureDocumento7 pagineStandardized Central Line Placement ProcedurelaneeceshariNessuna valutazione finora
- On IV TherapyDocumento40 pagineOn IV TherapyDeology Juanino77% (13)
- Hematology PROCEDURAL MANUALDocumento70 pagineHematology PROCEDURAL MANUALOscar the GrouchNessuna valutazione finora
- IV TherapyDocumento9 pagineIV TherapyJackson Pukya Gabino PabloNessuna valutazione finora
- IV TXDocumento9 pagineIV TXRenea Joy ArruejoNessuna valutazione finora
- Endotracheal Intubation and Treacheastomy.Documento9 pagineEndotracheal Intubation and Treacheastomy.Savita HanamsagarNessuna valutazione finora
- Iv Insertion ChecklistDocumento3 pagineIv Insertion ChecklistAnvic BernardoNessuna valutazione finora
- IV Therapy: AdvantagesDocumento9 pagineIV Therapy: AdvantagesKaren HutchinsonNessuna valutazione finora
- Nursing Policy for Implantable Portal Access DevicesDocumento14 pagineNursing Policy for Implantable Portal Access DevicesMerika JimenezNessuna valutazione finora
- Topic: Intravenous Cannulation, Therapy and Blood TransfusionDocumento32 pagineTopic: Intravenous Cannulation, Therapy and Blood TransfusionAngelica Kaye BuanNessuna valutazione finora
- IV Therapy PDFDocumento64 pagineIV Therapy PDFNL R Q DONessuna valutazione finora
- Intravenous Therapy (IV) : Ateneo de Zamboanga UniversityDocumento3 pagineIntravenous Therapy (IV) : Ateneo de Zamboanga Universitysenyorakath100% (2)
- IV Infusion ProcedureDocumento6 pagineIV Infusion ProcedureAnonymous B0c72x2Nessuna valutazione finora
- Starting An Intravenous InfusionDocumento2 pagineStarting An Intravenous InfusionAmiel Francisco Reyes100% (1)
- Practicum Procedure – I and II FORMDocumento11 paginePracticum Procedure – I and II FORMNoorwashilaNessuna valutazione finora
- IVT Checklist For StudentsDocumento9 pagineIVT Checklist For StudentsNoorwashila100% (1)
- IVTDocumento11 pagineIVTWilliam UrmanitaNessuna valutazione finora
- IVF Infusion ProcedureDocumento6 pagineIVF Infusion ProcedurepatzieNessuna valutazione finora
- Iv Therapy ChecklistDocumento4 pagineIv Therapy ChecklistRaibert RosalesNessuna valutazione finora
- IV Return DemoDocumento3 pagineIV Return DemoMhianne SarmientoNessuna valutazione finora
- Central Venous Catheters: Iv Terapy &Documento71 pagineCentral Venous Catheters: Iv Terapy &Florence Liem0% (1)
- 4.assignment On Endo TubeDocumento5 pagine4.assignment On Endo Tubesantosh kumarNessuna valutazione finora
- Inserting IV Cannula Utilizing Dummy IV ArmDocumento6 pagineInserting IV Cannula Utilizing Dummy IV ArmNoel100% (17)
- Intravenous TherapyDocumento22 pagineIntravenous TherapyMatt Lao Dionela100% (1)
- NCM - 103Documento5 pagineNCM - 103Delma SimbahanNessuna valutazione finora
- IV TherapyDocumento7 pagineIV TherapyJerika Shane MañosoNessuna valutazione finora
- Starting an Intravenous InfusionDocumento15 pagineStarting an Intravenous InfusionSVPSNessuna valutazione finora
- CUNANAN - Changing Monitoring Discontinuing IVFDocumento6 pagineCUNANAN - Changing Monitoring Discontinuing IVFAbbyNessuna valutazione finora
- IV Insertion SOPDocumento2 pagineIV Insertion SOPCandra AlifNessuna valutazione finora
- Starting An Intravenous Infusion Iv Insertion ChecklistDocumento3 pagineStarting An Intravenous Infusion Iv Insertion ChecklistWeljoy LabbaoNessuna valutazione finora
- Xavier University - Ateneo de Cagayan College of Nursing: Project: Step-By-Step ProcedureDocumento45 pagineXavier University - Ateneo de Cagayan College of Nursing: Project: Step-By-Step ProcedureShamsa AfdalNessuna valutazione finora
- SuctioningDocumento3 pagineSuctioningbern33Nessuna valutazione finora
- Gensan Medical Center Renal Dialysis Catheter Care PolicyDocumento5 pagineGensan Medical Center Renal Dialysis Catheter Care PolicyCynthia RinosNessuna valutazione finora
- Iv CannulationDocumento2 pagineIv CannulationMylene Grace ElarcosaNessuna valutazione finora
- Intrevenous TherapyDocumento5 pagineIntrevenous TherapyCharles DoradoNessuna valutazione finora
- Evaluation ToolDocumento4 pagineEvaluation ToolCarlos TorresNessuna valutazione finora
- Nasogastric Tube InsertionDocumento11 pagineNasogastric Tube InsertionDiane Kate Tobias Magno100% (1)
- IV InsertionDocumento17 pagineIV Insertionleih jsNessuna valutazione finora
- Setting Up An IV InfusionDocumento4 pagineSetting Up An IV InfusionJeric DucayNessuna valutazione finora
- Nasogastric Tube InsertionDocumento2 pagineNasogastric Tube InsertionsoapNessuna valutazione finora
- Discontinuing An IV SolutionDocumento4 pagineDiscontinuing An IV SolutionJustin GallemitNessuna valutazione finora
- Final Osce?Documento5 pagineFinal Osce?Queen ShNessuna valutazione finora
- 3364 110 05 01 PDFDocumento3 pagine3364 110 05 01 PDFSofie DyahNessuna valutazione finora
- Clinical Laboratory Techniques GuideDocumento41 pagineClinical Laboratory Techniques GuideBalaji GandhiNessuna valutazione finora
- Remove External Drain SafelyDocumento4 pagineRemove External Drain SafelyDot DitNessuna valutazione finora
- Intravenous Therapy: Bicol University Tabaco Campus Tabaco CityDocumento4 pagineIntravenous Therapy: Bicol University Tabaco Campus Tabaco CityWeeaboo Franz VlogsNessuna valutazione finora
- Percutaneous Tracheostomy Guideline - 3.26.14 - June 2014Documento5 paginePercutaneous Tracheostomy Guideline - 3.26.14 - June 2014joseL1994Nessuna valutazione finora
- Port-A-Cath: Ayah Omairi Mrs. Boughdana JaberDocumento13 paginePort-A-Cath: Ayah Omairi Mrs. Boughdana Jaberayah omairi100% (1)
- NCM 112 Finals Lab 2022Documento14 pagineNCM 112 Finals Lab 2022micaelaborja24Nessuna valutazione finora
- IV InsertionDocumento22 pagineIV InsertionRA100% (1)
- Discontinuing An IV InfusionDocumento2 pagineDiscontinuing An IV InfusionNoel83% (6)
- Palliative Care, Trials and COVID-19 TribulationsDa EverandPalliative Care, Trials and COVID-19 TribulationsNessuna valutazione finora
- Intravenous Therapy Administration: a practical guideDa EverandIntravenous Therapy Administration: a practical guideValutazione: 4 su 5 stelle4/5 (1)
- Post-cholecystectomy Bile Duct InjuryDa EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNessuna valutazione finora
- Kuesioner Pasien Rawat Inap Rawat Jalan 2010Documento55 pagineKuesioner Pasien Rawat Inap Rawat Jalan 2010Carissa CkNessuna valutazione finora
- 005704Documento113 pagine005704moinpharmNessuna valutazione finora
- Guideline for Peripheral Intravenous Catheter (PIVC) ManagementDocumento26 pagineGuideline for Peripheral Intravenous Catheter (PIVC) ManagementCarissa CkNessuna valutazione finora
- ICD Indication in Patient With Cardiac ChannelopathiesDocumento39 pagineICD Indication in Patient With Cardiac ChannelopathiesCarissa CkNessuna valutazione finora
- ICD Implantation Timing Post-Myocardial InfarctionTITLEGuidelines for Primary and Secondary Prevention of Sudden Cardiac Death with ICD TherapyDocumento36 pagineICD Implantation Timing Post-Myocardial InfarctionTITLEGuidelines for Primary and Secondary Prevention of Sudden Cardiac Death with ICD TherapyCarissa CkNessuna valutazione finora
- Antiarrythmia DrugDocumento36 pagineAntiarrythmia DrugCarissa CkNessuna valutazione finora
- Cardiac DrugsDocumento529 pagineCardiac DrugsSalvatore CiminoNessuna valutazione finora
- ECG Predictors of Sudden Cardiac Death in Cardiomyopathies: Yoga Yuniadi Indonesian Heart Rhythm SocietyDocumento27 pagineECG Predictors of Sudden Cardiac Death in Cardiomyopathies: Yoga Yuniadi Indonesian Heart Rhythm SocietyCarissa CkNessuna valutazione finora
- ICD Implantation Timing Post-Myocardial InfarctionDocumento51 pagineICD Implantation Timing Post-Myocardial InfarctionCarissa CkNessuna valutazione finora
- When To Implant ICD in Cardiomypathy PatientDocumento47 pagineWhen To Implant ICD in Cardiomypathy PatientCarissa CkNessuna valutazione finora
- When To Implant ICD in Cardiomypathy PatientDocumento47 pagineWhen To Implant ICD in Cardiomypathy PatientCarissa CkNessuna valutazione finora
- Cardiac Channelopathies: ECG Review of Brugada, Long QT, Short QT, and CPVT SyndromesDocumento37 pagineCardiac Channelopathies: ECG Review of Brugada, Long QT, Short QT, and CPVT SyndromesCarissa CkNessuna valutazione finora
- Komunikasi Perawat InfeksiDocumento91 pagineKomunikasi Perawat InfeksiCarissa CkNessuna valutazione finora
- Antimicrobial/Test Abbreviation: AbreviationDocumento3 pagineAntimicrobial/Test Abbreviation: AbreviationAkhmad Ikhsan Prafita PutraNessuna valutazione finora
- ECG Predictors of SCD in Ischemic Heart DiseaseDocumento25 pagineECG Predictors of SCD in Ischemic Heart DiseaseCarissa CkNessuna valutazione finora
- ICP1 RAPrev Control of HCAIDocumento12 pagineICP1 RAPrev Control of HCAIbpjsNessuna valutazione finora
- Instrumen Monev Keselamatan PasienDocumento7 pagineInstrumen Monev Keselamatan PasienCarissa CkNessuna valutazione finora
- CC SummaryDocumento2 pagineCC SummaryAdam WarrockNessuna valutazione finora
- Ppi IskDocumento29 paginePpi IskCarissa Ck100% (1)
- Komunikasi Perawat IneksiDocumento91 pagineKomunikasi Perawat IneksiCarissa CkNessuna valutazione finora
- Motivasi PerawatDocumento19 pagineMotivasi PerawatCarissa CkNessuna valutazione finora
- WHO Bio-Safety ManualDocumento186 pagineWHO Bio-Safety ManualrggefrmNessuna valutazione finora
- Table RTL Pembuatan Icra KosongDocumento3 pagineTable RTL Pembuatan Icra KosongvinnyNessuna valutazione finora
- Pencegahan Dan Pengendalian Ineksi Saluran Kemih (Isk)Documento36 paginePencegahan Dan Pengendalian Ineksi Saluran Kemih (Isk)Carissa Ck100% (1)
- Problem Solving in Hais: Dr. Kemala Rita, W, SKP., SP - Kep.Onk., Etn., MarsDocumento17 pagineProblem Solving in Hais: Dr. Kemala Rita, W, SKP., SP - Kep.Onk., Etn., MarsCarissa CkNessuna valutazione finora
- 2-AP-LABOR-bimbjangkar 12-17 PDFDocumento111 pagine2-AP-LABOR-bimbjangkar 12-17 PDFAinun JariahNessuna valutazione finora
- Pencegahan Dan Pengendalian Ineksi Saluran Kemih (Isk)Documento36 paginePencegahan Dan Pengendalian Ineksi Saluran Kemih (Isk)Carissa Ck100% (1)
- Appendix 2 Sample Operations For Pilot Study Sample Pilot Study Schedule OutlineDocumento12 pagineAppendix 2 Sample Operations For Pilot Study Sample Pilot Study Schedule OutlineCarissa CkNessuna valutazione finora
- Appendix 1 The Basic Basket of Indicators Indicator Construction Comments/data SourcesDocumento5 pagineAppendix 1 The Basic Basket of Indicators Indicator Construction Comments/data SourcesCarissa CkNessuna valutazione finora
- Bioactive Compounds in Phytomedicine BookDocumento228 pagineBioactive Compounds in Phytomedicine BookAnil KumarNessuna valutazione finora
- ACCIDENT REPORTING AND INVESTIGATION PROCEDUREDocumento23 pagineACCIDENT REPORTING AND INVESTIGATION PROCEDUREkirandevi1981Nessuna valutazione finora
- UN AIDS Miles-To-Go - enDocumento268 pagineUN AIDS Miles-To-Go - ensofiabloem100% (1)
- MycologyDocumento17 pagineMycologyRachana PurohitNessuna valutazione finora
- Oral Physio FinalDocumento34 pagineOral Physio FinaldraggarwalNessuna valutazione finora
- 9700 w14 QP 23Documento16 pagine9700 w14 QP 23rashmi_harryNessuna valutazione finora
- Chapter - 3 Medical Negligence and It'S Relation With Consumer Protection Act, 1986Documento67 pagineChapter - 3 Medical Negligence and It'S Relation With Consumer Protection Act, 1986Soumiki GhoshNessuna valutazione finora
- 1536106348Documento144 pagine1536106348Saman SarKoNessuna valutazione finora
- Failures in Periodontal Therapy: Review ArticleDocumento6 pagineFailures in Periodontal Therapy: Review ArticlezinniaNessuna valutazione finora
- Nutrition Quiz: Build a Healthy DietDocumento17 pagineNutrition Quiz: Build a Healthy DietJan Angelo OcadoNessuna valutazione finora
- COVID Vaccination Record Printing GuideDocumento4 pagineCOVID Vaccination Record Printing GuideAlice Chains100% (9)
- Bacteria and VirusesDocumento113 pagineBacteria and VirusesMarcelo H Dos SantosNessuna valutazione finora
- Latihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2Documento9 pagineLatihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2AWDNessuna valutazione finora
- 261-Article Text-575-1-10-20180915Documento11 pagine261-Article Text-575-1-10-20180915hector michel galindo hernandezNessuna valutazione finora
- Maria Garcia Dolphin Pose (Ardha Pincha Mayurasana) & Plough Pose (Halasana) Spring 2016 M 2:30-4:00Documento5 pagineMaria Garcia Dolphin Pose (Ardha Pincha Mayurasana) & Plough Pose (Halasana) Spring 2016 M 2:30-4:00api-301722320Nessuna valutazione finora
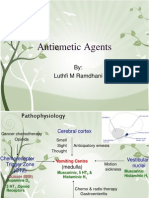
- AntiemeticDocumento36 pagineAntiemeticravannofanizza100% (1)
- Pathophysiology Tia VS CvaDocumento6 paginePathophysiology Tia VS CvaRobby Nur Zam ZamNessuna valutazione finora
- Tabel Interaksi Kolom BetonDocumento10 pagineTabel Interaksi Kolom BetonEndoGutierrezNessuna valutazione finora
- Fluoride: Nature's Cavity FighterDocumento11 pagineFluoride: Nature's Cavity FighterAya OsamaNessuna valutazione finora
- Gregory I. Bain, Eiji Itoi, Giovanni Di Giacomo, Hiroyuki Sugaya Eds. Normal and Pathological Anatomy of The ShoulderDocumento410 pagineGregory I. Bain, Eiji Itoi, Giovanni Di Giacomo, Hiroyuki Sugaya Eds. Normal and Pathological Anatomy of The ShoulderNikolaos Anastasopoulos100% (3)
- Clinical Reasoning FCPDocumento39 pagineClinical Reasoning FCPUlan NoputriNessuna valutazione finora
- Golden NumbersDocumento89 pagineGolden NumbersjoobazhieNessuna valutazione finora
- PHMB-Silver Sulfadiazine - HCDT-20-019Documento7 paginePHMB-Silver Sulfadiazine - HCDT-20-019gloriaNessuna valutazione finora
- Oral and Maxillofacial PathologyDocumento79 pagineOral and Maxillofacial PathologyMai AnhNessuna valutazione finora
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocumento8 pagineThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNessuna valutazione finora
- Child Health Course: Amref Directorate of Learning SystemsDocumento25 pagineChild Health Course: Amref Directorate of Learning SystemsEirehc Eam Aiboro SamorNessuna valutazione finora
- Pharma Module 1 PDFDocumento22 paginePharma Module 1 PDFSheryhan Tahir BayleNessuna valutazione finora
- Bench MarkingDocumento16 pagineBench MarkingNorj BaraniNessuna valutazione finora
- Nurdiana. R PD-B/ 0810713031: Module TaskDocumento10 pagineNurdiana. R PD-B/ 0810713031: Module TaskNurdiana RahmadaniNessuna valutazione finora
- Gastric and Duodenal Disorders - Test 4Documento21 pagineGastric and Duodenal Disorders - Test 4Vickie BuckerNessuna valutazione finora