Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Raman Radiotherapy MRT S. Hombsch
Caricato da
Stuart HombschCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Raman Radiotherapy MRT S. Hombsch
Caricato da
Stuart HombschCopyright:
Formati disponibili
Biological Response to Microbeam Radiation Therapy
Stuart Hombsch , Ewan Blanch [1] [1],
Jeffry Crosbie , Oliver Jones , Jacqueline Donoghue , Leonie Cann
[1] [1] [2] [2]
[1]
RMIT University, University of Melbourne [2]
Background What is MRT?
External beam radiotherapy is one of the most versatile and common methods of cancer treatment. MRT is a preclinical radiotherapy technique that utilises synchrotron generated soft x-rays passed
By irradiating tumours with high energy photons, cancer cells can be killed effectively, but often the through a collimator to produce a characteristic ‘barcode’ pattern with areas of
dose limiting factor is tolerance of the surrounding healthy tissue to radiation. extremely high dose deposition called ‘peaks’ and areas of very low radiation exposure
called ‘valleys’. Peak areas are typically 4 μm wide, separated by valley regions about 400
Microbeam Radiation Therapy (MRT), a preclinical radiotherapy technique that employs spatially μm in width.
fractionated kilovoltage x-rays, has recently gained attention for its remarkable tissue sparing effects
while still achieving good tumour control. Understanding the radiation response mechanisms of Preclinical animal studies have shown many tissue types are able to tolerate peak doses
healthy tissue is an important step in maximising the efficacy of this important treatment. of MRT at least an order of magnitude higher than conventional radiotherapy[1]. The
underlying biological processes allowing these tissue sparing effects while still
This study aims to use Raman microscopy to examine the biochemical response of murine brain achieving good tumour control are poorly understood. Leading hypotheses include the
Figure 1: H&E stained tissue
tissue to both conventional broadbeam radiotherapy and MRT. participation of the immune system, preferential damage to tumour microvasculature of weaned piglet brain tissue
following MRT treatment
and cell signalling processes .
[1-3]
with a peak dose of 300 Gy. [4]
Methods Tissue Imaging
A total of 15 formalin fixed, paraffin embedded brain tissue sections from three treatment types Raman imaging experiments were used to look
(control, broadbeam irradiated (12 Gy) and microbeam irradiated (295 Gy peak dose)) were cut to 7 μ for different response mechanisms in peak and
m sections and placed on CaF2 slides for Raman analysis. valley regions of MRT treated tissues.
Raman spectra were acquired from the cerebellum of each tissue section in a raster scan pattern Clear track marks that can be seen in the
using a Horiba LabRAM HR Evolution Raman spectrometer, 50x dry objective lens (NA = 0.55), 600 optical image of the tissue due to peak MRT
l/mm diffraction grating with 30 second acquisition time per point and 550 – 1800 cm-1 spectral doses do not appear in the Raman image,
window. A 785 nm laser was used for excitation with an output of 100 mW. 400 μm indicating the biological response to MRT
extends far beyond the highly irradiated
Spectra were individually pre-processed in-house MATLAB algorithms before being analysed with Figure 2: Optical and Raman image of MRT treated murine brain tissue. Red, green regions.
and blue pixel intensity represent normalised magnitues of principal component
principal component analysis using standard MATLAB algorithms. scores 1, 2, and 3, respectivley.
Results
Mean Spectra
140
Control Raman Shift
* MRT (295 Gy peak)
Broadbeam MRT Band Assignment
120
Broadbeam (12 Gy)
(cm-1)
100 *
756 Decrease (weak) Decrease Tryptophan
Intensity
80
*
60 830 Increase O-P-O asym str/Tyr br
*
40 *
850 Decrease Increase Tyr ring br, glycogen
20
935 Decrease C-C sym str bk, α-helix
0
600 800 1000 1200 1400 1600
Wavenumber (cm-1) 1082 Decrease (weak) Increase Carbohydrate
Figure 3: Mean spectra of control, microbeam and conventionally irradiated tissues. Parrafin resudue is present in all samples even after de-waxing in xylene, denoted with *.
1207 Increase Increase Phenylalanine
1339 Decrease Decrease (weak) DNA
a b Loadings for PC 4
0.8
20
1665 Decrease Amide-I
Control
Principal Component 5 (1.6%)
Intensity
MRT
0.6 Broadbeam
10
0
0.4 Table 1: Notable differences in mean spectra of treatment types relative to the control spectrum. Band assignment was based on similar published
-10
studies[5-7].
0.2 -20
600 800 1000 1200 1400 1600
0 20
Loadings for PC 5
10
Intensity
-0.2
-0.4
-10
0
Conclusion
-20
-0.6 -0.4 -0.2 0 0.2 0.4 0.6 0.8 1 600 800 1000 1200 1400 1600
Principal Component 4 (2.1%) Wavenumber (cm ) -1
Group mean spectra reveal several subtle differences between each treatment type, many
Figure 4: a) PCA scatter plot showing grouping of all three treatment types. The contol contorl group the largest spread while there is a small amount of overlap between Broad-
beam and MRT treated tissues. b) Loadings plots of PC4 and 5 show minimal variation in AmideI-III bands, with most variation occuring below 1200 cm-1.
of which indicate changes in protein side chains, while differences in nucleic acids and
carbohydrates were also observed. Lipids of biological origin were not examined as
sources of variation as the paraffin removal process can artificially alter the lipid content of
tissues.
Acknowledgements These early results indicate that MRT induces a separate biochemical response to
conventional radiotherapy in healthy tissues. Future work includes repeating this
I would like to thank RMIT University for funding my PhD scholarship, and ICORS 2018 for awarding experiment on snap frozen tissues to examine the role of lipids in radiation response of
me a student travel grant to allow me to present my research. healthy tissues and additional Raman imaging experiments to confirm tissue response to
MRT is not confined to regions receiving the peak dose.
References
1. Smyth, L.M., et al., The normal tissue effects of microbeam radiotherapy: What do we know, and what do we need to know to plan a human clinical trial? Int J Radiat Biol, 2016. 92(6): p. 302-11. 2. Smith, R.W., et al., Proteomic changes in the rat brain induced by homogenous irradiation and by the bystander effect resulting from high energy synchrotron X-ray microbeams. Int J Radiat Biol,
2013. 89(2): p. 118-27. 3. Fontanella, A.N., et al., Effects of high-dose microbeam irradiation on tumor microvascular function and angiogenesis. Radiat Res, 2015. 183(2): p. 147-58. 4. Barber, H.B., et al., <title>Weanling piglet cerebellum: a surrogate for tolerance to MRT (microbeam radiation therapy) in pediatric neuro-oncology</title>. 2001. 4508: p. 65-73. 5. Harder, S.J., et al., Raman
spectroscopy identifies radiation response in human non-small cell lung cancer xenografts. Sci Rep, 2016. 6: p. 21006. 6. Meksiarun, P., et al., Breast cancer subtype specific biochemical responses to radiation. Analyst, 2018. 143(16): p. 3850-3858. 7. Matthews, Q., et al., Radiation-Induced Glycogen Accumulation Detected by Single Cell Raman Spectroscopy Is Associated with Radioresistance
that Can Be Reversed by Metformin. PLoS One, 2015. 10(8): p. e0135356.
Potrebbero piacerti anche
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Decoding The Flu: Modified From A Case Study byDocumento7 pagineDecoding The Flu: Modified From A Case Study byStanleyWu0% (1)
- CHAPTERS 2-4 CROSSWORD #1 SolvedDocumento4 pagineCHAPTERS 2-4 CROSSWORD #1 SolvedYu LucyNessuna valutazione finora
- Chapter 15Documento15 pagineChapter 15nfnf otupyooorefnNessuna valutazione finora
- Otagiri, 2016. Albumin in Medicine. EBOOKDocumento279 pagineOtagiri, 2016. Albumin in Medicine. EBOOKFinda Istiqomah100% (1)
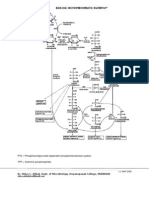
- Hexose Monophosphate Pathway PathwayDocumento3 pagineHexose Monophosphate Pathway PathwayShiva100% (6)
- BIOL2262 Assignment Sheet 2 - 2013Documento2 pagineBIOL2262 Assignment Sheet 2 - 2013Melissa T100% (1)
- General Biology Lab Manual - F2016 PDFDocumento114 pagineGeneral Biology Lab Manual - F2016 PDFDuncan ComptonNessuna valutazione finora
- AFLP Manual InvitrogenDocumento24 pagineAFLP Manual InvitrogenJanani SNessuna valutazione finora
- 1 s2.0 S0022282816302176 MainDocumento85 pagine1 s2.0 S0022282816302176 MainNia Rukman100% (1)
- Natural Science. Level 6. Unit 3. ReproductionDocumento3 pagineNatural Science. Level 6. Unit 3. ReproductionAna Rosa Camacho Cornejo50% (2)
- Pablo Borbon Main II Batangas City: Republic of The Philippines Batangas State UniversityDocumento5 paginePablo Borbon Main II Batangas City: Republic of The Philippines Batangas State UniversityChichiri NomiNessuna valutazione finora
- Circadian Rhythm NEJMDocumento12 pagineCircadian Rhythm NEJMtjelongNessuna valutazione finora
- Hatching and BroodingDocumento22 pagineHatching and BroodingToha PutraNessuna valutazione finora
- HURDCO International School: Subject-Biology Chapter 3: Diffusion, Osmosis and Surface Area: Volume RatioDocumento26 pagineHURDCO International School: Subject-Biology Chapter 3: Diffusion, Osmosis and Surface Area: Volume RatioMahin IslamNessuna valutazione finora
- Dna ExtractionDocumento5 pagineDna ExtractionYsabel Francesca AbadNessuna valutazione finora
- Department of Animal Husbandry and Dairy Science Mahatma Phule Krishi Vidyapeeth Rahuri-413 722, Dist. Ahmednagar (MS)Documento20 pagineDepartment of Animal Husbandry and Dairy Science Mahatma Phule Krishi Vidyapeeth Rahuri-413 722, Dist. Ahmednagar (MS)dahiphale1100% (1)
- Human - Influences - On - Ecosystems - 4 QPDocumento5 pagineHuman - Influences - On - Ecosystems - 4 QPkatise1794Nessuna valutazione finora
- Artículo: Marzolo Et Al. (1997) PNASDocumento6 pagineArtículo: Marzolo Et Al. (1997) PNASConsue HAPPYNessuna valutazione finora
- Crop LifeDocumento7 pagineCrop Life유가연[학생](생명과학대학 유전생명공학과)Nessuna valutazione finora
- HACCPtestDocumento13 pagineHACCPtestDianne Faye ManabatNessuna valutazione finora
- Cacti Biology and Uses (2003) BBSDocumento291 pagineCacti Biology and Uses (2003) BBSAadolfo MUNessuna valutazione finora
- CV Margaret Durdan 17-18Documento3 pagineCV Margaret Durdan 17-18api-428498175Nessuna valutazione finora
- Pre 2010 Part 2Documento527 paginePre 2010 Part 2Fábio CostaNessuna valutazione finora
- Project Manager Biotech Pharmaceutical Healthcare in Boston MA Resume Katinka SteniusDocumento3 pagineProject Manager Biotech Pharmaceutical Healthcare in Boston MA Resume Katinka SteniusKatinkaSteniusNessuna valutazione finora
- Exome Sequencing AnalysisDocumento7 pagineExome Sequencing AnalysisSalman khanNessuna valutazione finora
- Tryptic Soy Agar (7100) : Formula May Be Adjusted And/or Supplemented As Required To Meet Performance SpecificationsDocumento3 pagineTryptic Soy Agar (7100) : Formula May Be Adjusted And/or Supplemented As Required To Meet Performance SpecificationsMulyani Dwi YantiNessuna valutazione finora
- The Past, Present and Future of NeuroplasticityDocumento13 pagineThe Past, Present and Future of NeuroplasticityMaxime Goovaerts100% (3)
- Experiment 3 Bio300Documento5 pagineExperiment 3 Bio300ellymanisNessuna valutazione finora
- Gen Bio Ref1 PDFDocumento25 pagineGen Bio Ref1 PDFGexel Cecilio78% (9)
- OCD Mast Cell Herbal ProtocolDocumento5 pagineOCD Mast Cell Herbal ProtocolIvana CiricNessuna valutazione finora