Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Antiseizure, Sedative & Hypnotics
Caricato da
Thulasi tootsieTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Antiseizure, Sedative & Hypnotics
Caricato da
Thulasi tootsieCopyright:
Formati disponibili
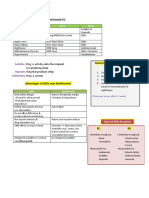
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
ANTISEIZURE DRUGS
M.O.A Enhancement of GABA -increase GABA actions at receptor: BZD, phenobarbital
action
- inhibits GABA transaminase: vigabatrin
- blocks GABA uptake: tiagabin
Inhibition of sodium -phenytoin, carbamazepine, valproic acid, lamotrigine
channel function
Inhibition of Calcium T- Ethosuximide
type channels
Only enhances GABAergic Gabapentin
action
target synaptic vesicle Levetiracetam
protein SV2A
USES Drugs used in Partial Phenytoin, Carbamazepine, Lamotrigine, Vigabatrin, Gabapentin, Topiamate
seizures and Generalized
tonic-clonic seizures
Drugs used in Generalized Ethosuximide, Valproic acid, trimethadione
seizures
Other drugs used in Benzodiazepines; Acetazolamide
epilepsy
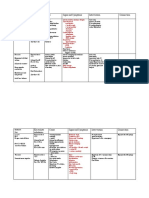
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
SODIUM CHANNEL BLOCKER
•
Phenytoin, • They stabilize & prolong the inactivated state of Na+ channels
• Carbamazepine preventing entry of Na+ for a long time.
• Lamotrigine
EXAMPLES CLINICAL USES M.O.A ADVERSE EFFECTS
Phenytoin for generalized tonic *Absorption is slow & complete, in the *gingival hyperplasia
clonic (grand mal) duodenum only. Highly bound to plasma *mild peripheral
seizures. albumin (90%). Metabolized in liver by neuropathy
microsomal enzymes *osteomalacia
*Elimination: first-order at low dose, zero- *hirsutism
order at higher dose. Excreted in urine. *diplopia
*Induction of liver microsomal enzymes *megaloblastic anaemia
Drug interactions (↓plasma level) with *cleft palate
Isoniazid, cimetidine, sulfonamides, warfarin
Carbamazepine Drug of choice for *Similar to that of phenytoin Dose related:
partial seizures *acts presynaptically to decrease synaptic *Diplopia and ataxia (Rx
Generalized tonic- transmission rearrange divided doses)
clonic seizures *Mild GI disturbances
Trigeminal neuralgia *Drowsiness (at much
Mania higher doses)
*Hyponatremia and
water intoxication
Idiosyncratic:
*Skin rash (the most
common)
*blood dyscrasias in the
form of:
aplastic anaemia and
agranulocytosis
leukopenia (requires
careful monitoring)
Lamotrigine *Monotherapy in blockage of voltage dependent sodium *Dizziness headache and
partial seizures. channels (similar to phenytoin). somnolence
*Add on therapy actions on voltage-activated Ca⁺²channels *Diplopia
*Absence seizures in (accounting for its efficacy in absence *Nausea
children. seizures) *Skin rash
(hypersensitivity).
*Life-threatening
dermatitis
Vigabatrin Add-on drug for cases *irreversible inhibitor of GABA-transaminase eye check needed as the
(inhibits GABA not responding to (covalent binding) ↑GABA drug may cause
transaminase) other drug *short plasma t ½ but long acting peripheral visual field
defect on long-term
Gabapentin *effective against *aminoacid analog of GABA,
Pregabalin partial seizures *Not metabolized, excreted in urine. Does not
(Only enhances induce liver enzymes
GABAergic action)
Topiamate for partial and
generalized seizures
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
ENHANCEMENT OF GABA ACTION
EXAMPLES CLINICAL USES M.O.A ADVERSE EFFECTS
Valproic acid *Absence seizures *Block voltage-dependent sodium *Hepatic failure,
(Sodium Valproate) *myoclonic seizure channels & T-type Calcium channel specially children
*partial seizures with *Increase in brain GABA <2yrs
complex symptoms (A) facilitate GAD *Neural tube defects
(enzyme for synthesis of GABA) when pregnant
(B) Inhibit GABA transporter GAT-1 mother given in 1st
*increase membrane potassium trimester
conductance leading to hyperpolarization *Thinning and curly
of the neuronal membrane. hair
Pharmacokinetics
• well absorbed following an oral
dose
• Valproic acid is 90% bound to
plasma proteins
Drug interactions:
1. Valproic acid inhibits the
metabolism of several drugs,
including phenobarbital,
carbamazepine, and phenytoin,
leading to an increased blood
level of these compounds.
2. At high doses, valproic acid can
inhibit its own metabolism.
CALCIUM T-TYPE CHANNELS INHIBITORS
EXAMPLES CLINICAL USES M.O.A ADVERSE EFFECTS
Ethosuximide Used for absence seizure inhibits Ca2+ currents (low threshold T- May exacerbate other
(pure petit mal drug) type) that mediate thalamocortical types of epilepsy
oscillations (3/sec firing rhythm) seen in
absence seizure
PHARMACOKINETICS:
complete absorption, NOT protein-
bound, completely metabolized by
hydroxylation, t ½ 40 hr
STATUS EPILEPTICUS
-Diazepam i.v. up to 20- -Lorazepam i.v. -Midazolem i.m. -Phenytoin i.v. (long-lasting)
30 mg (the effect is not (longer lasting) (slower onset, short- -Phenytoin is precipitated by
lasting) action) glucose; Need to monitor cardiac
rhythm (d/t propylene glycol in
which drug is dissolved)
-Fosphenytoin is freely -Phenobarbital 100- For Absence status epilepticus:
soluble, alternative 200 mg i.v. up to 800 BZD are drug of choice
mg, but monitor
respiratory
depression.
DRUG RESISTANT EPILEPSY
*High risk of premature *Combination therapy: *Newer Drugs: *Early evaluation for surgery- anterior
death, injuries & One drug should be Na+ new Na channel lobectomy for resistant temporal lobe
psychosocial dysfunction in channel blocker & the blockers- epilepsy
these patients. other drug with lacosamide,
GABAergic properties. eslicarbazepine
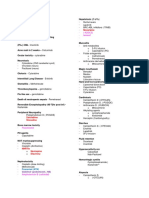
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
SEDATIVE-HYPNOTIC DRUGS
SEDATIVE (anxiolytic) drug reduces anxiety, moderates excitement and calms the recipient.
HYPNOTIC drug produces drowsiness and facilitates the onset and maintenance of a state of
sleep and from which the recipient can be aroused easily
SEDATIVE-HYPNOTIC DRUGS
SEDATIVE-HYPNOTICS CLASSIFICATION
Benzodiazepines Barbiturates Miscellaneous agents
Short Ultra short
acting acting
Intermediate Short Buspirone
acting acting Chloral hydrate
Long Long Zaleplon
acting acting Zolpidem
Ramelteon
CHARACTERISTIC • Lipid soluble
• Absorbed well from the GIT
• Good distribution to the brain
• Metabolized before elimination from the body by hepatic enzymes
DRUG A - BARBITURATES
DRUG B - BDZ
- flatter dose response
curve
- greater margin of safety
↑DOSE =
↑ CNS DEPRESSION
• Dose dependent depression of CNS.
• Cross tolerance and cross dependence between
all CNS sedatives (Barbiturates, BZD, Ethanol)
All sedative-hypnotics:
• Cross the placenta fetal depression.
• detectable in breast milk depress infant CNS
NORMAL RELIEF FROM ANXIETY DISINHIBITION
SEDATION HYPNOTICS G.A COMA DEATH
CLINICAL USES • Acute & chronic anxiety disorders
• Insomnia
• Epilepsy & seizures
• Sedation, Amnesia, Anesthesia
• Muscle relaxation
• Alcohol & Sedative Hypnotic withdrawal
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
Benzodiazepines (BZD)
MODE OF • Bind to an allosteric site on GABA receptor (pocket between & subunit)
ACTION • Promote binding of GABA to two binding sites between & subunits of GABAA receptor.
• This triggers ligand-gated chloride channel opening (↑frequency), with resulting
membrane hyperpolarization.
• Neuronal firing is decreased as a result, producing observed CNS depressant effects.
GABAA • The GABA-A receptor is a ligand gated ion channel receptor
Receptors • GABA binding causes the channel to open and Cl enters into the neuron
• Creates a negative charge in the transmembrane potential.
• This makes GABA an Inhibitory neurotransmitter
Binding sites: GABA / BZD / Flumazenil / Zolpidem / Barbiturates
PHARMCO. CNS (uses) Peripheral
ACTION • Sedation • Coronary vasodilation (after i.v. of
• Decreased anxiety diazepam)
• Hypnosis • Neuromuscular Blockade (overdose)
• Anticonvulsant activity
• Muscle-Relaxation
• Anterograde amnesia
ADVERSE • BZD have few SE (vs other • Overdose: Rare fatalities if BZD alone
EFFECTS psychotropics) • Severe CNS & Respiratory Depression if
• Sedation, CNS Depression combined with:
– Worse if combined with EtOH – alcohol
• Behavioral Disinhibition – barbiturates
– Irritab, excitement, aggression – narcotics
(<1%), rage – tricyclic antidepressants
• Psychomotor & Cognitive Impairment
– coordination, attention (driving)
– poor visual-spatial ability (not
aware of it)
– Ataxia, confusion
ANTEDOTE: • Drug used to treat BZD over dosage.
FLUMAZENIL • It reverses the effects of benzodiazepines by competitive inhibition at the benzodiazepine
binding site on the GABAA receptor
• It has been found to be effective in overdoses of non-benzodiazepine sleep enhancers,
zolpidem and zaleplon
• Action lasts 2 hr, caution: shorter action than BZDs - repeat dose might be needed
• convulsion rarely occurs, esp. patient taking TCA
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
DRUG ROA T½ (H) INDICATION COMMENT
Short-Acting Oral 3+1 Insomnia Daytime side
effects
Triazolem (Halcion) IM, IV 2+0.6 Insomnia
Rapid metabolism
Midazolem (Versed)
Intermediate-Acting Oral 12+2 Anxiety, agoraphobia Severe withdrawal
$
Alprazolam (Xanax) Oral 11+6 Insomnia
Metab.Conjugation
Temazepam (Restoril) O,IM, IV 10+3 Anxiety, alcohol w/d
Chlordiazepoxide anaesthetic premed. Active metabolite
O,IM, IV 14+5
(Librium)
Anxiety, premed. Metab.Conjugation
Lorazepam (Ativan)
Long-Acting O,IM, IV, 43+13 Status epilepticus, Prototype BZD
Rectal anxiety, sk. muscle
Diazepam (Valium) 74+24 relaxation, premed. Active metab.
Oral
Flurazepam (Dalmane) 23+5 Insomnia Tolerance to anti-
O,IM, IV convulsant effect
Clonazepam (Klonopin) Seizures, acute mania
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
BARBITURATES
INTRO • Main hypnotics until 60s
• Depresses CNS CVS collapse (no more used as anxiolytic / hypnotic)
• Those with 6 -12hrs duration of action (e.g. pentobarbital) sparingly used
• Phenobarbital still used as anticonvulsant and Thiopental for induction of anaesthesia
KINETICS • Well absorbed in GIT
• It is a weak acid alkaline urine ionisation and elimination
• Induces hepatic enzymes conc. of several drugs e.g. steroids, oral contraceptives,
warfarin, tricyclic antidepressants
MODE OF • Barbiturates bind to the GABA-A
ACTION receptor at a nearby site
• Potentiate the effect of GABA in
increasing the Cl- flow
• Barbiturates also block the AMPA
receptor which is sensitive to
glutamate, the excitatory
neurotransmitter, (opposite effect from
GABA)
CLINICAL Epilepsy (pnenobarbitone)
USES overdose of stimulants e.g. amphetamine;
Induction of anaesthesia (thiopental i.v.)
ADVERSE • Sedation (within therapeutic dose)
EFFECTS • Tolerance (not enough to cancel motor and cognitive impairment)
• Megaloblastic anemia
• Mild hypersensitivity
• Osteomalacia
• Overdose Resp and CVS failure coma
• Precipitates porphyria
• Withdrawal Sx: anxiety, nausea, vomiting, hypotension, seizure, psychosis, CVS collapse &
death
SEDATIVE, HYPNOTICS, & ANTI-CONVULSANT DRUGS
OTHER DRUGS
BUSPIRONE • 5HT1A agonist, no hypnotic but little sedative action
• Doesn’t potentiate CNS depressant effect of sedative hypnotics
• No rebound anxiety
• Anxiolysis may take > 1 wk (mainly for generalised anxiety states, not suitable for
panic disorders, phobia; administered p.o.)
• Related compounds:
Ipsapirone, Gepirone, Tandospirone
ZOLPIDEM • Structurally unrelated to BZD
• Zolpidem, zaleplon, eszopiclone bind to 1 subunit of GABAA R enhancing GABA
effect
• Produces deep sleep
• Minimal anxiolytic, muscle relaxant and anticonvulsant effect
• Use: short-term Rx of insomnia
• High doses depress resp (esp with other CNS depressants, alcohol)
• Less risk of dependence (cf BZD)
• Metabolized in liver
RAMELTEON • Indicated for patient with difficulty in falling asleep
• Agonist action at MT1 & MT2 melatonin receptors in the suprachiasmatic nuclei of
brain
• No direct effect on GABAergic neurotransmission
• PK: rapid absorption, metabolized by CYP1A2 (mainly) and CYP2C9, metabolite also
active.
• SE: dizziness, somnolence, fatigue.
ANTIHISTAMINES • Sedation is a side effect of their antihistaminic effect
Diphenhydramine
Promethazine
Β-ADRENAGIC • Treat anxiety due to somatic symptoms or performance anxiety (stage fright)
BLOCKERS
Potrebbero piacerti anche
- Cherokee Herbal RemediesDocumento292 pagineCherokee Herbal RemediesAlek Phabiovsky100% (2)
- Adrenergic AgentsDocumento45 pagineAdrenergic AgentsAmit ShahNessuna valutazione finora
- ANS DrugsDocumento2 pagineANS Drugsmed testNessuna valutazione finora
- Ninja - Anti-HTN PDFDocumento6 pagineNinja - Anti-HTN PDFErica Hyeyeon Lee100% (2)
- Common Drug Stems Cheat Sheet: Drug Stem Drug Class And/or Stem Explanation ExamplesDocumento2 pagineCommon Drug Stems Cheat Sheet: Drug Stem Drug Class And/or Stem Explanation ExamplesjthsNessuna valutazione finora
- Opioids PDFDocumento2 pagineOpioids PDFErica Hyeyeon LeeNessuna valutazione finora
- Critical Care Drug Reference SheetDocumento12 pagineCritical Care Drug Reference SheetYanina CoxNessuna valutazione finora
- Week 10 - Hypertension, Atherosclerosis, ArrhythmiaDocumento14 pagineWeek 10 - Hypertension, Atherosclerosis, Arrhythmiashivani patel100% (1)
- Renal Guide and Charts: AlbuminDocumento16 pagineRenal Guide and Charts: AlbuminYaima JimenezNessuna valutazione finora
- Sphere: These DiarrheaDocumento3 pagineSphere: These Diarrheamed testNessuna valutazione finora
- Pharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDocumento5 paginePharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDana20SNessuna valutazione finora
- Drugclasses Pharmacologypart 1 PDFDocumento25 pagineDrugclasses Pharmacologypart 1 PDFSutanya100% (2)
- Cranial Nerves ListDocumento4 pagineCranial Nerves Listashdmb217Nessuna valutazione finora
- Respiratory System Notes - KEYDocumento3 pagineRespiratory System Notes - KEYjoy100% (1)
- Meninges, Ventricles - CSF - Study GuideDocumento3 pagineMeninges, Ventricles - CSF - Study Guideshivani patelNessuna valutazione finora
- Physician Assistant Certification and Recertification Exam Review - PANRE - PANCEDocumento14 paginePhysician Assistant Certification and Recertification Exam Review - PANRE - PANCEThe Physician Assistant Life100% (3)
- Clinical SignsDocumento26 pagineClinical SignswiraandiniNessuna valutazione finora
- T Bringing Classical and Contemporary Homoeopathy Ogether: Research Oriented Homoeopathic ApproachDocumento107 pagineT Bringing Classical and Contemporary Homoeopathy Ogether: Research Oriented Homoeopathic ApproachVarshaNessuna valutazione finora
- Pharm C Exam 10 Drug ListDocumento2 paginePharm C Exam 10 Drug ListVokdadaNessuna valutazione finora
- DIT Pharmacology MnemonicsDocumento5 pagineDIT Pharmacology MnemonicsqiqizNessuna valutazione finora
- Journal Hydrodynamic Theory by Brnnstrm1986Documento5 pagineJournal Hydrodynamic Theory by Brnnstrm1986Fifth TsuchikageNessuna valutazione finora
- Respiratory SystemDocumento32 pagineRespiratory SystemThulasi tootsieNessuna valutazione finora
- Concise SEO-Optimized Title for Clotting DocumentDocumento3 pagineConcise SEO-Optimized Title for Clotting DocumentRyan TurnerNessuna valutazione finora
- Kriya For Balancing The ChakrasDocumento5 pagineKriya For Balancing The ChakrasFedra Fox Cubeddu100% (2)
- Glutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationDocumento3 pagineGlutamate: Neurotransmitters Disturbed Increased Sympathetic Stimulation Increased Autonomic StimulationCM NajitoNessuna valutazione finora
- Epilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsDocumento19 pagineEpilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsMourian AmanNessuna valutazione finora
- Ninja - Antianginal Drugs PDFDocumento2 pagineNinja - Antianginal Drugs PDFErica Hyeyeon LeeNessuna valutazione finora
- Combined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDDocumento1 paginaCombined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDnkuligowskiNessuna valutazione finora
- Transport of Critically Ill Adults 2011Documento1 paginaTransport of Critically Ill Adults 2011velocity25Nessuna valutazione finora
- Pharm Expansion 17 NDFDocumento1 paginaPharm Expansion 17 NDFNokz M. Raki-inNessuna valutazione finora
- Bam Slam Drug CardDocumento4 pagineBam Slam Drug CardLeticia GonzalezNessuna valutazione finora
- Drugs in Blood DisordersDocumento1 paginaDrugs in Blood DisordersSantosh patelNessuna valutazione finora
- Anti FungalsDocumento5 pagineAnti FungalskakuNessuna valutazione finora
- Parkinson's Disorder - Classification and MechanismDocumento1 paginaParkinson's Disorder - Classification and MechanismVương TúNessuna valutazione finora
- Pharmacology Main DrugsDocumento14 paginePharmacology Main DrugsSabir KhanNessuna valutazione finora
- MC Tumors and Cancers of Various OrgansDocumento12 pagineMC Tumors and Cancers of Various OrgansRyan TurnerNessuna valutazione finora
- Drug of Abuse (Table) PDFDocumento2 pagineDrug of Abuse (Table) PDFtchanochNessuna valutazione finora
- List of Look-Alike MedicationsDocumento5 pagineList of Look-Alike MedicationsAhmad TaramsyNessuna valutazione finora
- Dysrhythmias: Cardiac Conduction System Rhythm Strip RecognitionDocumento5 pagineDysrhythmias: Cardiac Conduction System Rhythm Strip Recognitiontantalizin marieNessuna valutazione finora
- Common Prefixes and SuffixesDocumento5 pagineCommon Prefixes and Suffixestriddle1969100% (1)
- Somatosensory Pathways: Primary Sensory and Motor AreasDocumento36 pagineSomatosensory Pathways: Primary Sensory and Motor AreasAnonymous w3vYureNessuna valutazione finora
- Ultimate Pharm GuideDocumento41 pagineUltimate Pharm GuideeanguyenNessuna valutazione finora
- Drug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsDocumento7 pagineDrug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsJenny NguyenNessuna valutazione finora
- Sodium Imbalances (Hyponatremia Vs Hypernatremia)Documento17 pagineSodium Imbalances (Hyponatremia Vs Hypernatremia)Angel FiloteoNessuna valutazione finora
- Ninja - Anemias PDFDocumento1 paginaNinja - Anemias PDFErica Hyeyeon LeeNessuna valutazione finora
- Therapeutic IndexDocumento8 pagineTherapeutic IndexMary Jennel RosNessuna valutazione finora
- IMG EmpAposterDocumento1 paginaIMG EmpAposterChiu LeoNessuna valutazione finora
- Hierarchy of O2 Delivery SystemsDocumento1 paginaHierarchy of O2 Delivery SystemsRevNessuna valutazione finora
- (CV2) Pharmacology of AnticoagulantsDocumento6 pagine(CV2) Pharmacology of AnticoagulantsHanifa Shereen B. AliNessuna valutazione finora
- Pre-op Evaluation SummaryDocumento1 paginaPre-op Evaluation Summarysabbo morsNessuna valutazione finora
- Dysrhythmias 1: Cardiac Conduc1on System Rhythm Strip Recogni1onDocumento4 pagineDysrhythmias 1: Cardiac Conduc1on System Rhythm Strip Recogni1ontantalizin marieNessuna valutazione finora
- NHS Antibiotice PDFDocumento2 pagineNHS Antibiotice PDFHoratiu OanaNessuna valutazione finora
- Table of Sedative, Hypnotic, AntianxietyDocumento4 pagineTable of Sedative, Hypnotic, AntianxietyirfanzukriNessuna valutazione finora
- Electrolyte Imbalances: Causes, Signs, Symptoms and InterventionsDocumento6 pagineElectrolyte Imbalances: Causes, Signs, Symptoms and InterventionsmkninnyNessuna valutazione finora
- Fluids Electrolytes Visual NotesDocumento8 pagineFluids Electrolytes Visual NotesVin Lorenzo CampbellNessuna valutazione finora
- Drug Classes and Brand NamesDocumento6 pagineDrug Classes and Brand Namesremyde07Nessuna valutazione finora
- Pharmacology A - NSAIDSDocumento14 paginePharmacology A - NSAIDSselflessdoctorNessuna valutazione finora
- Drug toxicity and adverse effects guideDocumento2 pagineDrug toxicity and adverse effects guidekatNessuna valutazione finora
- Meds For HypertensionDocumento3 pagineMeds For HypertensionZonicsNessuna valutazione finora
- Pharm Drug Outline AdrDocumento1 paginaPharm Drug Outline AdrCess Lagera YbanezNessuna valutazione finora
- Drug CardsDocumento3 pagineDrug CardsDave HillNessuna valutazione finora
- Exam 2 Study Guide 2018Documento21 pagineExam 2 Study Guide 2018EvanNessuna valutazione finora
- EAR First AidDocumento4 pagineEAR First Aidr_lakshmi2722Nessuna valutazione finora
- Sedative-Hypnotic Drugs - AMBOSSDocumento8 pagineSedative-Hypnotic Drugs - AMBOSSRuva Oscass JimmyNessuna valutazione finora
- Approximate Equivalents:: 0.100 Gmn. 1.00 GMDocumento8 pagineApproximate Equivalents:: 0.100 Gmn. 1.00 GMakane ryuNessuna valutazione finora
- 14 Fun Facts About Your Heart: Educational VersionDa Everand14 Fun Facts About Your Heart: Educational VersionNessuna valutazione finora
- Summative m108Documento2 pagineSummative m108Thulasi tootsieNessuna valutazione finora
- Renal Patho QuizDocumento5 pagineRenal Patho QuizThulasi tootsieNessuna valutazione finora
- Summative IV M207Documento2 pagineSummative IV M207Thulasi tootsieNessuna valutazione finora
- Hearts PDFDocumento30 pagineHearts PDFLaura RodriguezNessuna valutazione finora
- Renal Past Year QuestionsDocumento3 pagineRenal Past Year QuestionsThulasi tootsieNessuna valutazione finora
- Mskcns Sum m107Documento2 pagineMskcns Sum m107Thulasi tootsieNessuna valutazione finora
- Past Year RespiDocumento5 paginePast Year RespiThulasi tootsieNessuna valutazione finora
- Ovary PathologyDocumento2 pagineOvary PathologyThulasi tootsieNessuna valutazione finora
- Summative m107 Endo, Repro, RenalDocumento6 pagineSummative m107 Endo, Repro, RenalThulasi tootsieNessuna valutazione finora
- Pass Year CVSDocumento6 paginePass Year CVSThulasi tootsieNessuna valutazione finora
- RENAL and Reproductive Systems - Q & ADocumento13 pagineRENAL and Reproductive Systems - Q & AThulasi tootsieNessuna valutazione finora
- MSK Formative 2012Documento13 pagineMSK Formative 2012Thulasi tootsieNessuna valutazione finora
- MEQ AnswerDocumento9 pagineMEQ AnswerThulasi tootsieNessuna valutazione finora
- Past Year ReproDocumento4 paginePast Year ReproThulasi tootsieNessuna valutazione finora
- Examination of The Cranial Nerves. Cranial Information. Patient - Patient - CoDocumento7 pagineExamination of The Cranial Nerves. Cranial Information. Patient - Patient - CoThulasi tootsieNessuna valutazione finora
- M208 MSK+CNS Summative (12 Nov 2010)Documento11 pagineM208 MSK+CNS Summative (12 Nov 2010)Thulasi tootsieNessuna valutazione finora
- Past Year Me110Documento2 paginePast Year Me110Thulasi tootsieNessuna valutazione finora
- MalariaDocumento1 paginaMalariaThulasi tootsieNessuna valutazione finora
- By WehloongDocumento5 pagineBy WehloongThulasi tootsieNessuna valutazione finora
- Male Genital TractDocumento4 pagineMale Genital TractThulasi tootsieNessuna valutazione finora
- M109 MSKCNSSummativeDocumento5 pagineM109 MSKCNSSummativeThulasi tootsieNessuna valutazione finora
- Important MechanismDocumento2 pagineImportant MechanismThulasi tootsieNessuna valutazione finora
- MEQDocumento1 paginaMEQThulasi tootsieNessuna valutazione finora
- M208 Sum 5Documento3 pagineM208 Sum 5Thulasi tootsieNessuna valutazione finora
- Female Genital TractDocumento2 pagineFemale Genital TractThulasi tootsieNessuna valutazione finora
- ME110 Summative Sem 5Documento17 pagineME110 Summative Sem 5Thulasi tootsieNessuna valutazione finora
- HematologyDocumento39 pagineHematologyThulasi tootsieNessuna valutazione finora
- CNS Formative 2012Documento17 pagineCNS Formative 2012Ho Yong WaiNessuna valutazione finora
- GI+hemato Past YearDocumento9 pagineGI+hemato Past YearThulasi tootsieNessuna valutazione finora
- Model Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20Documento1 paginaModel Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20SwarnA TamtaNessuna valutazione finora
- Lactose intolerance diagnosis and treatmentDocumento12 pagineLactose intolerance diagnosis and treatmentNico BatallaNessuna valutazione finora
- BSN 4A Group 5 Nigerian AmericanDocumento39 pagineBSN 4A Group 5 Nigerian AmericanAngelie PantajoNessuna valutazione finora
- References Style and Writing GuideDocumento23 pagineReferences Style and Writing GuideHarshal SabaneNessuna valutazione finora
- Clinical Rehabilitation: Does Electrical Stimulation Reduce Spasticity After Stroke? A Randomized Controlled StudyDocumento9 pagineClinical Rehabilitation: Does Electrical Stimulation Reduce Spasticity After Stroke? A Randomized Controlled StudyArkar SoeNessuna valutazione finora
- A Review On Aleurites MoluccanaDocumento18 pagineA Review On Aleurites Moluccanabharatkhurana85Nessuna valutazione finora
- Konsep Latihan Plyometric PDFDocumento27 pagineKonsep Latihan Plyometric PDFDwinda Abi PermanaNessuna valutazione finora
- IRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)Documento4 pagineIRB Definitions (Is It Research? and Definitions of Exempt, Expedited and Full)analyn123Nessuna valutazione finora
- 05thjan Assignment Abroad TimesDocumento8 pagine05thjan Assignment Abroad TimesSameer ShaikNessuna valutazione finora
- Zocor (Simvastatin)Documento3 pagineZocor (Simvastatin)E100% (1)
- YOU IN SURGICAL - Product CatalogDocumento222 pagineYOU IN SURGICAL - Product CatalogfarazNessuna valutazione finora
- Chapter 8 Spelling WordsDocumento2 pagineChapter 8 Spelling Wordsapi-3705891Nessuna valutazione finora
- Planes Systems OrganizationDocumento36 paginePlanes Systems OrganizationR. EssoNessuna valutazione finora
- Forearm Fracture in ChildrenDocumento45 pagineForearm Fracture in ChildrenMagnusNessuna valutazione finora
- Bonifacio V. Romero High School Tle Beauty Care 9 1st Quarter Examination S.Y. 2018-2019Documento6 pagineBonifacio V. Romero High School Tle Beauty Care 9 1st Quarter Examination S.Y. 2018-2019Virginia Saavedra100% (1)
- Vitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsDocumento70 pagineVitamins Are Organic Compounds Required in The Diet in Small Quantities To Perform Biological FunctionsRose LiteNessuna valutazione finora
- Inserto CHOL - LIQ SPINREACTDocumento2 pagineInserto CHOL - LIQ SPINREACTIng BiomédicoNessuna valutazione finora
- Grievously: News Item 9: EARTHQUAKE 2Documento2 pagineGrievously: News Item 9: EARTHQUAKE 2roxana_boraNessuna valutazione finora
- DR Wong Teck WeeipadDocumento2 pagineDR Wong Teck Weeipadtwwong68Nessuna valutazione finora
- Medicine in Situ Panchen TraditionDocumento28 pagineMedicine in Situ Panchen TraditionJigdrel77Nessuna valutazione finora
- Influence of The Quality of The FinishedDocumento6 pagineInfluence of The Quality of The Finishedmehdi chahrourNessuna valutazione finora
- Pre Conference Final ProgDocumento2 paginePre Conference Final ProgkeithlyndNessuna valutazione finora
- Blood Pressure Log 30Documento2 pagineBlood Pressure Log 30Yousab KaldasNessuna valutazione finora
- Philips Respironics Bipap ST Niv Noninvasive VentilatorDocumento2 paginePhilips Respironics Bipap ST Niv Noninvasive Ventilatorsonia87Nessuna valutazione finora