Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Goals and Objectives For Ehr Implementation
Caricato da
rhvenkatDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Goals and Objectives For Ehr Implementation
Caricato da
rhvenkatCopyright:
Formati disponibili
Goals and Objectives for
Electronic Health Record
(EHR) Implementation
Guidelines
Provided By:
The National Learning Consortium (NLC)
Developed By:
Health Information Technology Research Center (HITRC)
Colorado Regional Extension Center (CO – REC)
Doctor's Office Quality Information Technology (DOQ-IT)
The material in this document was developed by Regional Extension Center staff in the performance of technical
support and EHR implementation. The information in this document is not intended to serve as legal advice nor
should it substitute for legal counsel. Users are encouraged to seek additional detailed technical guidance to
supplement the information contained within. The REC staff developed these materials based on the technology
and law that were in place at the time this document was developed. Therefore, advances in technology and/or
changes to the law subsequent to that date may not have been incorporated into this material.
March 31, 2012 • Version 1.0
1
NATIONAL LEARNING CONSORTIUM
The National Learning Consortium (NLC) is a virtual and evolving body of knowledge and tools designed
to support healthcare providers and health IT professionals working towards the implementation, adoption
and meaningful use of certified EHR systems.
The NLC represents the collective EHR implementation experiences and knowledge gained directly from
the field of ONC’s outreach programs (REC, Beacon, State HIE) and through the Health Information
Technology Research Center (HITRC) Communities of Practice (CoPs).
The following resource is an example of a tool used in the field today that is recommended by “boots-on-
the-ground” professionals for use by others who have made the commitment to implement or upgrade to
certified EHR systems.
DESCRIPTION
These guidelines are intended to aid providers and health IT implementers in planning for EHR
implementation through the definition of goals and objectives. This resource can help define goals for
quality improvement and help identify which features of the EHR are critical to the established goals. If
you can define your goals, you can define your needs. If you can define your needs, then you can select
an EHR system that will meet your needs.
Establishing realistic, measureable goals and objectives for EHR implementation is critical to determine
whether or not an implementation was successful. These guidelines include examples that can be used
to assist with goal and objective development. They also outline several dimensions upon which a
practice can establish goals and objectives. The last section provides a template to document specific
goals and objectives.
INSTRUCTIONS
Review the guidelines to identify goals and objectives for EHR implementation. Use the template
provided in section 7 to document specific goals and objectives. Use the template in section 8 to
document benchmarks and track progress at 6 and 12 months post implementation.
March 31, 2012 • Version 1.0 2
TABLE OF CONTENTS
1 “WHY” implement EHRs? ....................................................................................................................... 4
2 Getting Started........................................................................................................................................ 4
3 Goal Definition ........................................................................................................................................ 4
4 Action Plan.............................................................................................................................................. 5
5 Measuring Success ................................................................................................................................ 5
5.1 Examples ........................................................................................................................................ 5
6 Example Goals and Objectives .............................................................................................................. 6
6.1 System ............................................................................................................................................ 6
6.2 Vendor ............................................................................................................................................ 6
6.3 Billing .............................................................................................................................................. 6
6.4 Office Staff ...................................................................................................................................... 7
6.5 Providers And Clinical Functions .................................................................................................... 7
6.6 Clinical Data management ............................................................................................................. 7
6.7 Medical Records And Document Management .............................................................................. 8
6.8 Patients ........................................................................................................................................... 8
6.9 Costs............................................................................................................................................... 8
7 Goals and Objectives for Your Practice ................................................................................................. 8
7.1 System: ........................................................................................................................................... 8
7.2 Vendor: ........................................................................................................................................... 8
7.3 Billing: ............................................................................................................................................. 9
7.4 Office Staff: ..................................................................................................................................... 9
7.5 Providers and Clinical Functions: ................................................................................................... 9
7.6 Clinical Data Management: .......................................................................................................... 10
7.7 Medical Records and Document Management: ........................................................................... 10
7.8 Patients: ........................................................................................................................................ 10
7.9 Costs:............................................................................................................................................ 10
8 EHR Benchmark Data Points ............................................................................................................... 11
LIST OF EXHIBITS
Exhibit 1: Examples ....................................................................................................................................... 5
Exhibit 2: EMR Site Readiness Assessment: Clinic Overview And Demographics .................................... 11
March 31, 2012 • Version 1.0 3
1 “WHY” implement EHRs?
This EHR implementation step should help practice leadership evaluate their current state to determine
what is working well and what can be improved. Some of the questions providers ask themselves during
this phase include:
“Am I accomplishing what I thought I would be doing when I decided to go to medical school?”
“Are we providing the best possible care to our patients, or are we simply trying to make it through the
week?”
“If I had more time, what would I do differently?”
“What would it be like to leave the office yet stay connected to my practice?”
At this stage, practice leadership and staff should consider the practice’s clinical goals, needs, financial
and technical readiness as they transition.
2 Getting Started
Start with a workflow analysis and identify the bottlenecks and inefficiencies that exist today. Decide
which bottlenecks and inefficiencies you want to improve and assign them a priority. It doesn’t matter so
much where you start — as long as you start somewhere.
In setting priorities, you may want to consider the following:
In what areas is our performance far from ideal?
What improvements do we think our patients will notice most?
Where do we think we can be successful in making change?
What groups of clinicians and staff should we involve in each item, and what is their readiness for
change?
3 Goal Definition
Goals and needs should be documented to help guide decision-making throughout the implementation
process. They may need to be re-assessed throughout the EHR implementation steps to ensure a
smooth transition for the practice and all staff.
Set goals in areas that are important and meaningful to your practice. These may be clinical goals,
revenue goals, or goals related to work environment. Goals in all three areas will help assure balanced
processes after the implementation. Goals that are important to you will help you and your staff through
the change process. We recommend you follow the “SMART” goals process. This process includes
setting objectives and goals that meet the following criteria:
Specific – Achieving the goal would make a difference for our patients and our practice
Measureable – We can quantify the current level and the target goal
March 31, 2012 • Version 1.0 4
Attainable – Although the goal may be a stretch, we can achieve it
Relevant – This is worth the effort
Time bound – There are deadlines and opportunities to celebrate success!
These goals become the guide posts for an EHR implementation project, and achieving these goals will
motivate providers and practice staff to make necessary changes and attain new skills.
Have some fun with goal setting. Involve everyone in the office by asking for creative suggestions on
ways to eliminate inefficiency.
4 Action Plan
For each goal, define a plan of action for achieving the goal. What specific steps do you need to take to
reach your goal?
Successes should be celebrated along the way. Implementing an EHR is a long process. Keeping the
momentum and support of staff is important, so acknowledging success and interim milestones will help
to sustain the effort.
5 Measuring Success
Determine how to measure the success of your action plan. Keep it simple! Don’t get hung up on
statistics, sample size and complicating factors. However utilize any baseline data you may have, so
you’ll have something to compare your quality improvement efforts to.
If you don’t meet your measurement for success the first time, re-evaluate, and try again. Quality
improvement is a never-ending task.
5.1 EXAMPLES
Exhibit 1: Examples
Goal Action Plan Measure of Success
Decrease the number of pharmacy Use the e-prescribing feature in the EHR In two months, have an 85%
phone calls regarding prescriptions to eliminate paper and handwritten reduction in pharmacy phone calls
prescriptions. Utilize the drug interaction
checking feature of the EHR to guard
against drug interactions
Decrease transcription turnaround time Use clinical charting within the EHR to Within two months of EHR live,
and reduce transcription cost eliminate the need for transcription reduce the cost of transcription by
services 80%
Improve the quality of patient care for Use the EHR’s health maintenance 95% of patients with CAD have been
CAD patients tracking to monitor antiplatelet therapy prescribed antiplatelet therapy
March 31, 2012 • Version 1.0 5
Goal Action Plan Measure of Success
Decrease waiting room time for patients Encourage patients to use the PCs in the Within one month, 75% of patients
waiting room to update their wait no longer than 10 minutes in
demographics and insurance information the waiting room
More sample goals to consider:
Improve patient access to the physician.
Decrease the number of times the physician leaves the exam room during a visit.
Increase the quantity/quality of patient education materials given to the patient.
Decrease the number of calls to the lab for results/follow up.
Increase the number of patients who receive reminders for age/sex appropriate preventative health
measures.
Increase the number of patients who actually receive preventative health exams/procedures.
6 Example Goals and Objectives
6.1 SYSTEM
EHR system must fully integrate with PMS.
EHR system must be reliable with virtually no down-time.
EHR system must be very fast and use a secure, wireless intra-office connection.
EHR system must be compatible with systems used by local hospitals, consultant specialists, labs,
and imaging facilities with easily adaptable interfaces.
EHR system must be compliant with present technology standards for reporting of data to MCOs and
Medicare.
EHR system must be expandable to a multi-site use and allow for growth in the size of practice.
EHR system must be redundant with disaster recovery procedure that is easily accomplished.
6.2 VENDOR
Vendor must be a financially stable/viable company with strong presence in the local healthcare
community and experience with small, primary care practices.
Vendor must have reputation for exceptional customer service and support.
Vendor must provide sufficient training of present and future staff in an efficient, cost-effective
manner.
Vendor must have availability and expertise to assist us in adapting the EHR to changing
requirements for reporting, billing or clinical needs.
6.3 BILLING
EHR system needs to maintain or improve present AR time.
EHR system must provide easy coding assistance and provide documentation to support codes.
March 31, 2012 • Version 1.0 6
EHR system should be user-friendly and allow for generation of reports to track trends in charges,
AR, payer mix, denials, etc.
EHR system should facilitate “clean claims” and limit denials.
EHR system should adapt easily to changes in requirements for claims submission.
6.4 OFFICE STAFF
EHR should allow for and promote eventual goal of having all communication with patients, medical
specialists’ offices, labs, imaging facilities and MCOs accomplished electronically rather than by
phone in order to enhance efficiency and documentation.
EHR should be user-friendly and require minimal training for new employees.
EHR should be efficient with very few clicks to most-frequently used screens/functions.
EHR should support multi-resource scheduling easily and efficiently.
EHR should improve workflow for all functions including patient check-in, proscription refills,
management of referrals, record requests, appointment scheduling, etc.
6.5 PROVIDERS AND CLINICAL FUNCTIONS
EHR visit documentation should be user-friendly and easily adaptable to provider preferences.
EHR documents should be easy to read with useful document structure.
EHR should allow for remote access from any computer with internet connection without loading
special software.
EHR should have software that accommodates multiple visit types as well as visits in which multiple
problems are addressed.
EHR needs to have a system by which covering doctors can see and review results and labs
requiring urgent attention for providers who are not in the office.
EHR system should allow for providers to block their inbox (at least for urgent messages) when they
are not in the office.
EHR should provide efficient means for communication with specialists.
EHR should streamline communication with patients and allow for electronic reporting of results.
EHR should interface with labs for electronic receipt of results as well as electronic order entry.
EHR should allow for easy use of digital photography for patient identification as well as
documentation of exam findings.
6.6 CLINICAL DATA MANAGEMENT
EHR should have adaptable systems for disease management and programs targeting improvements
in patient care as well as pay-for-performance goals.
EHR should have easily generated reports of patients by diagnosis, visit type, demographics, etc.
EHR should allow for easy reporting of data to MCOs, Medicare, and PHO.
March 31, 2012 • Version 1.0 7
6.7 MEDICAL RECORDS AND DOCUMENT MANAGEMENT
EHR should allow for rapid scanning of documents.
EHR should generate work notes, school excuses, immunization records, etc.
EHR should allow for efficient completion and management of multiple forms from outside agencies
that need to be completed by our providers, such as WIC forms, PT1 transportation forms, DMV
forms, school physicals, etc.
EHR should allow for maintaining a patient education “library” with materials that are easily accessed
and printed for patients.
6.8 PATIENTS
The EHR system should improve patient access to services.
The EHR system should improve patient satisfaction.
The EHR system should allow patients to undertake all communication with the office electronically, if
they choose.
The EHR system should allow patients to give insurance, demographic information, and eventually
some clinical history online before their office visits.
6.9 COSTS
Systems should help us save transcription costs.
Systems should save on payroll costs eventually as system efficiencies are achieved and workforce
shrinks by attrition.
System should decrease cost for supplies, courier services, and paper management.
System should increase revenue through MCO and Medicare incentive programs.
7 Goals and Objectives for Your Practice
7.1 SYSTEM:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.2 VENDOR:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
March 31, 2012 • Version 1.0 8
7.3 BILLING:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.4 OFFICE STAFF:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.5 PROVIDERS AND CLINICAL FUNCTIONS:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
March 31, 2012 • Version 1.0 9
7.6 CLINICAL DATA MANAGEMENT:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.7 MEDICAL RECORDS AND DOCUMENT MANAGEMENT:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.8 PATIENTS:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
7.9 COSTS:
1. Click here to enter text.
2. Click here to enter text.
3. Click here to enter text.
March 31, 2012 • Version 1.0 10
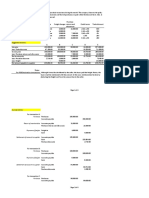
8 EHR Benchmark Data Points
Exhibit 2: EMR Site Readiness Assessment: Clinic Overview And Demographics
Completed By: Click here to enter text. Title: Click here to enter text. Phone: Click here to enter text.
General Information Date of Completion Date of Completion Date of Completion
Clinic Name: Click here to enter text. Click here to enter a date. Click here to enter a date. Click here to enter a date.
Clinic Address: Click here to enter text.
Clinic Phone Number: Click here to enter text.
Clinic Fax Number: Click here to enter text.
PRE-EMR 6 Months POST EMR 12 Months POST EMR
What is your average number of patient visits per day? Click here to enter text. Click here to enter text. Click here to enter text.
What is your provider FTE count? Click here to enter text. Click here to enter text. Click here to enter text.
What percentage of your providers are dictating notes? Click here to enter text. Click here to enter text. Click here to enter text.
What is the rate of Hemoglobin A1c in patients diagnosed with Click here to enter text. Click here to enter text. Click here to enter text.
DM? % < 7?
What is the average length of time your providers take to close Click here to enter text. Click here to enter text. Click here to enter text.
encounters?
What is the average percentage of patients seen without the Click here to enter text. Click here to enter text. Click here to enter text.
medical chart each day?
What is your average chart pull time? Click here to enter text. Click here to enter text. Click here to enter text.
What is your average turnaround time from receipt of chart Click here to enter text. Click here to enter text. Click here to enter text.
request to delivery to provider?
What is your average number of inbound calls from patients, Click here to enter text. Click here to enter text. Click here to enter text.
pharmacists, consulting providers, etc. each day? What
percentage requires a chart pull?
March 31, 2012 • Version 1.0 11
General Information Date of Completion Date of Completion Date of Completion
What is your average number of outbound calls from patients, Click here to enter text. Click here to enter text. Click here to enter text.
pharmacists, consulting providers, etc. each day? What
percentage requires a chart pull?
What is your average patient cycle time from check-in to check- Click here to enter text. Click here to enter text. Click here to enter text.
out?
For your JCAHO Core Measurements for Ambulatory Care, how Click here to enter text. Click here to enter text. Click here to enter text.
many are currently meeting established benchmarks? How
many are not meeting benchmarks?
March 31, 2012 • Version 1.0 12
Potrebbero piacerti anche
- Blaine Ray HandoutDocumento24 pagineBlaine Ray Handoutaquilesanchez100% (1)
- Unseen WarfareDocumento79 pagineUnseen WarfareНАША БИБЛИОТЕКА ЕНГЛЕСКИ100% (8)
- HL7Documento13 pagineHL7sony100% (3)
- ADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeDocumento1 paginaADT DFT ORU: The Most Commonly Used HL7 Message Types IncludeRafi Uddin ShaikNessuna valutazione finora
- Grief and BereavementDocumento4 pagineGrief and BereavementhaminpocketNessuna valutazione finora
- Introduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Documento56 pagineIntroduction To Electronic Medical Record - Non-CHKD Employees - August - 2023 V2Ahmad AhmadNessuna valutazione finora
- Post Market Surveillance SOPDocumento8 paginePost Market Surveillance SOPgopinathNessuna valutazione finora
- White Paper Patient Centered Care ModelDocumento16 pagineWhite Paper Patient Centered Care ModelRodrigoSachiFreitasNessuna valutazione finora
- Ecw EMR Workbook II - Updated - Portage Health PDFDocumento63 pagineEcw EMR Workbook II - Updated - Portage Health PDFSyed Mudussir HusainNessuna valutazione finora
- Cerner - PATIENT JOURNEYDocumento18 pagineCerner - PATIENT JOURNEYtimNessuna valutazione finora
- 01 Wonhyo Web PDFDocumento370 pagine01 Wonhyo Web PDFAaron Nelson100% (1)
- Section II: Evidence-Based PracticeDocumento52 pagineSection II: Evidence-Based PracticeSugiantoNessuna valutazione finora
- Healthcare and TechnologyDocumento14 pagineHealthcare and Technologytrobi017Nessuna valutazione finora
- 2) Session 2 - Design and Development of HMISDocumento59 pagine2) Session 2 - Design and Development of HMISyusuf zekeriya mohammedNessuna valutazione finora
- EHR Contracts UntangledDocumento56 pagineEHR Contracts UntangledTheo100% (1)
- 365 Daily QuotesDocumento32 pagine365 Daily QuotesAna SilivestruNessuna valutazione finora
- Final Project Part-3 Marketing PlanDocumento8 pagineFinal Project Part-3 Marketing PlanIam TwinStormsNessuna valutazione finora
- Electronic Health Records: A Guide For Clinicians and AdministratorsDocumento17 pagineElectronic Health Records: A Guide For Clinicians and AdministratorsLIS_141Nessuna valutazione finora
- Evaluation and Implementation of Telemedicine in An Independent Allergy Practice Business PlanDocumento14 pagineEvaluation and Implementation of Telemedicine in An Independent Allergy Practice Business PlanNaomi SargeantNessuna valutazione finora
- American EHR Market ShareDocumento17 pagineAmerican EHR Market ShareBhushan ShinkreNessuna valutazione finora
- Process MapDocumento7 pagineProcess Mapapi-535002543100% (1)
- Online Adult QuestionnaireDocumento5 pagineOnline Adult QuestionnaireDiyan UzunovNessuna valutazione finora
- App Synch v4.3 Install - Service Manual (MAN-05940) English Rev - 002 10-2019Documento160 pagineApp Synch v4.3 Install - Service Manual (MAN-05940) English Rev - 002 10-2019Lyht TVNessuna valutazione finora
- Standards and EHR InteroperabilityDocumento26 pagineStandards and EHR InteroperabilityONC for Health Information Technology100% (2)
- EHRA InteroperabilityRoadmap 20090310 v3Documento40 pagineEHRA InteroperabilityRoadmap 20090310 v3Anonymous JE7uJR100% (1)
- Archaeology - October 2016 PDFDocumento72 pagineArchaeology - October 2016 PDFOmer CetinkayaNessuna valutazione finora
- MPRA Paper 70218Documento231 pagineMPRA Paper 70218TRYVERN MAMIZANessuna valutazione finora
- Concept of PeaceDocumento22 pagineConcept of PeaceTrí Giải100% (1)
- Accenture EMR Markets Whitepaper VfinalDocumento16 pagineAccenture EMR Markets Whitepaper VfinalcapaxtremeNessuna valutazione finora
- HIS Lesson 4. Health Information SystemsDocumento29 pagineHIS Lesson 4. Health Information SystemsJannela EscomiendoNessuna valutazione finora
- 5 Informatics and HealthcareDocumento32 pagine5 Informatics and HealthcareKyla OnaNessuna valutazione finora
- Satellite Value Chain: Snapshot 2017Documento13 pagineSatellite Value Chain: Snapshot 2017syrijal26Nessuna valutazione finora
- US Healthcare System Analysis v2-0Documento31 pagineUS Healthcare System Analysis v2-0Achintya KumarNessuna valutazione finora
- AHA Patient Centered Medical HomeDocumento21 pagineAHA Patient Centered Medical Homein678Nessuna valutazione finora
- New Life in Christ - Vol05 - Engl - Teacher GuideDocumento29 pagineNew Life in Christ - Vol05 - Engl - Teacher GuideOliver Angus100% (1)
- Guidelines For Programme ManagementDocumento25 pagineGuidelines For Programme ManagementAdelChNessuna valutazione finora
- @ 2 Effects of Electronic Medical Records On Patient Safety Culture: The Perspective of NursesDocumento7 pagine@ 2 Effects of Electronic Medical Records On Patient Safety Culture: The Perspective of NursesElizabeth CotenNessuna valutazione finora
- HIMSS EHR Reporting Program RFI Comment LetterDocumento9 pagineHIMSS EHR Reporting Program RFI Comment LetterSpit FireNessuna valutazione finora
- Selenium L2Documento81 pagineSelenium L2rhvenkat33% (3)
- HL7 Integration Analyst in Nashville TN Resume Éilís CreanDocumento6 pagineHL7 Integration Analyst in Nashville TN Resume Éilís CreanEilisCreanNessuna valutazione finora
- The Future of Comparative Literary StudiesDocumento14 pagineThe Future of Comparative Literary StudiesNabeesath ArifaNessuna valutazione finora
- DNP 800 Philosophy of NursingDocumento7 pagineDNP 800 Philosophy of Nursingapi-247844148Nessuna valutazione finora
- Performance Improvement (PI) Plan and Template: Health Care Association of New JerseyDocumento46 paginePerformance Improvement (PI) Plan and Template: Health Care Association of New JerseyRógini HaasNessuna valutazione finora
- Health Information System A Complete Guide - 2019 EditionDa EverandHealth Information System A Complete Guide - 2019 EditionNessuna valutazione finora
- Health Information Technology A Complete Guide - 2020 EditionDa EverandHealth Information Technology A Complete Guide - 2020 EditionNessuna valutazione finora
- The "Epic" Challenge of Optimizing Antimicrobial Stewardship: The Role of Electronic Medical Records and TechnologyDocumento9 pagineThe "Epic" Challenge of Optimizing Antimicrobial Stewardship: The Role of Electronic Medical Records and TechnologyMr XNessuna valutazione finora
- eHEALTH - HealthDocumento68 pagineeHEALTH - HealthElets TechnomediaNessuna valutazione finora
- Healthcare Trends in AmericaDocumento101 pagineHealthcare Trends in Americapriya_psalms100% (1)
- Refining A Self-Assessment of Informatics Competency Scale Using Mokken Scaling AnalysisDocumento9 pagineRefining A Self-Assessment of Informatics Competency Scale Using Mokken Scaling AnalysisTenIs ForMeNessuna valutazione finora
- Tiger Report - Informatics CompetenciesDocumento34 pagineTiger Report - Informatics CompetenciesJustus K Gatheru100% (1)
- HIMSS10 GuideDocumento24 pagineHIMSS10 Guidemr_histalk5532Nessuna valutazione finora
- Guidelines FOR Implementing Drug Utilization Review Programs IN HospitalsDocumento58 pagineGuidelines FOR Implementing Drug Utilization Review Programs IN HospitalsMuhammad Faris MahmudNessuna valutazione finora
- Joint Commission Patient-Centered Communication Standards 2011Documento4 pagineJoint Commission Patient-Centered Communication Standards 2011Institute of CaliforniaNessuna valutazione finora
- Utilization Review Coordinator: Passbooks Study GuideDa EverandUtilization Review Coordinator: Passbooks Study GuideNessuna valutazione finora
- Philosophy of Nursing Practice DNP Timothy Blake BoothDocumento2 paginePhilosophy of Nursing Practice DNP Timothy Blake Boothapi-555804657Nessuna valutazione finora
- CCM DiabetesDocumento21 pagineCCM DiabetesRobertNessuna valutazione finora
- Dictionary of Acronyms in HealthcareDocumento1.353 pagineDictionary of Acronyms in HealthcaremeaningfulhealthitNessuna valutazione finora
- Telehealth June 2019Documento62 pagineTelehealth June 2019MarcNessuna valutazione finora
- Information Technology in Quality Services and Patient Safety (Electronic Medical Record)Documento48 pagineInformation Technology in Quality Services and Patient Safety (Electronic Medical Record)Asri ParantriNessuna valutazione finora
- Intravenous InsulinDocumento4 pagineIntravenous Insulingiseladelarosa2006Nessuna valutazione finora
- EPIC InfoDocumento8 pagineEPIC InfoVijay TupakulaNessuna valutazione finora
- Registered Nurse Shortage in Rural Healthcare SettingsDocumento9 pagineRegistered Nurse Shortage in Rural Healthcare SettingsShelley KrumwiedeNessuna valutazione finora
- Health Policy Commission StudyDocumento28 pagineHealth Policy Commission StudyThe Republican/MassLive.comNessuna valutazione finora
- Disadvantages of EHR Systems - Dispelling Your FearsDocumento10 pagineDisadvantages of EHR Systems - Dispelling Your FearsElijah WisdomNessuna valutazione finora
- Health Advocate's StoryDocumento4 pagineHealth Advocate's StoryHealth Advocate, Inc.Nessuna valutazione finora
- 2022 MUSE Inspire Conference - Sessions - February 9 2022Documento17 pagine2022 MUSE Inspire Conference - Sessions - February 9 2022Michele LambertNessuna valutazione finora
- Synthesis PosterDocumento1 paginaSynthesis Posterapi-483044745Nessuna valutazione finora
- Healthcare Domain QuestionsDocumento5 pagineHealthcare Domain QuestionsNikhil SatavNessuna valutazione finora
- Telehealth Interoperability White PaperDocumento15 pagineTelehealth Interoperability White PaperJohn MillerNessuna valutazione finora
- Qip LeadershipDocumento16 pagineQip Leadershipapi-431252101Nessuna valutazione finora
- Value Based Healthcare Further Together PerspectiveDocumento5 pagineValue Based Healthcare Further Together PerspectiveCYNTHIA SILITONGA100% (1)
- Evidence Based RUADocumento12 pagineEvidence Based RUAAsma AliNessuna valutazione finora
- EvaluationprogramplanDocumento32 pagineEvaluationprogramplanapi-523878990Nessuna valutazione finora
- Navigating Powerchart For Ed Ob orDocumento2 pagineNavigating Powerchart For Ed Ob orapi-224958119Nessuna valutazione finora
- Agile Sales and Business DevelopmentDocumento16 pagineAgile Sales and Business DevelopmentrhvenkatNessuna valutazione finora
- KhambhatDocumento5 pagineKhambhatparthivshahNessuna valutazione finora
- The Mystics Ascetics and Saints of India 1000028898Documento354 pagineThe Mystics Ascetics and Saints of India 1000028898Dr.Shibly MansurNessuna valutazione finora
- Characteristic of Agile ScrumDocumento5 pagineCharacteristic of Agile ScrumrhvenkatNessuna valutazione finora
- Performance Appraisal GuidelineDocumento8 paginePerformance Appraisal GuidelinerhvenkatNessuna valutazione finora
- Agile MethodesDocumento41 pagineAgile MethodesAbdelkrim OuadrhiriNessuna valutazione finora
- Values-Kohlberg Stages of Moral DevelopmentDocumento7 pagineValues-Kohlberg Stages of Moral Developmentcnn90Nessuna valutazione finora
- Web TestingDocumento6 pagineWeb TestingarpitamondalNessuna valutazione finora
- Text Entered For Unstructured: Patient DetailsDocumento1 paginaText Entered For Unstructured: Patient DetailsrhvenkatNessuna valutazione finora
- I Don't Want To Work. I Want To Be Quite, and Rest. Yours Affectionately Vivekanand Aristotle Onassis QuotesDocumento1 paginaI Don't Want To Work. I Want To Be Quite, and Rest. Yours Affectionately Vivekanand Aristotle Onassis QuotesrhvenkatNessuna valutazione finora
- Vol 1 No 3Documento55 pagineVol 1 No 3rhvenkatNessuna valutazione finora
- 1 7Documento7 pagine1 7rhvenkatNessuna valutazione finora
- AgilecandidatesDocumento1 paginaAgilecandidatesrhvenkatNessuna valutazione finora
- Patient Currently Takes Medications As of 09-Apr-2017 22:12 Documented in Structured NotesDocumento2 paginePatient Currently Takes Medications As of 09-Apr-2017 22:12 Documented in Structured Notesrhvenkat100% (1)
- SirDocumento1 paginaSirrhvenkatNessuna valutazione finora
- 413Documento4 pagine413rhvenkatNessuna valutazione finora
- EnglishDocumento16 pagineEnglishrhvenkatNessuna valutazione finora
- FGDFGDFGDFG: Patient DetailsDocumento1 paginaFGDFGDFGDFG: Patient DetailsrhvenkatNessuna valutazione finora
- KarmaDocumento1 paginaKarmarhvenkatNessuna valutazione finora
- A Study of Software MetricsDocumento6 pagineA Study of Software MetricsrhvenkatNessuna valutazione finora
- 10 Deadly Sins of EstimationDocumento26 pagine10 Deadly Sins of Estimationaroopam1636Nessuna valutazione finora
- 1.7 Project ManagementDocumento18 pagine1.7 Project Managementabdolali64Nessuna valutazione finora
- Brochure Delegation Training For LeadersDocumento6 pagineBrochure Delegation Training For LeadersSupport ALProgramsNessuna valutazione finora
- Number SystemsDocumento25 pagineNumber SystemsMehwish BilalNessuna valutazione finora
- Obat Keras N0vember 2021Documento137 pagineObat Keras N0vember 2021antonNessuna valutazione finora
- User Instructions: Installation Operation Maintenance NAF Duball DL Pocket ValveDocumento12 pagineUser Instructions: Installation Operation Maintenance NAF Duball DL Pocket ValveMauricio Contreras R.Nessuna valutazione finora
- Bleeding Disorders in Pregnancy: Table 1Documento7 pagineBleeding Disorders in Pregnancy: Table 1KharismaNisaNessuna valutazione finora
- VisualizationDocumento2 pagineVisualizationKIRAN H SNessuna valutazione finora
- B2 UNIT 6 Test StandardDocumento6 pagineB2 UNIT 6 Test StandardКоваленко КатяNessuna valutazione finora
- Combustion FundamentalsDocumento30 pagineCombustion FundamentalsPrem SagarNessuna valutazione finora
- User Manual For Scanbox Ergo & Banquet Line: Ambient (Neutral), Hot and Active Cooling. Scanbox Meal Delivery CartsDocumento8 pagineUser Manual For Scanbox Ergo & Banquet Line: Ambient (Neutral), Hot and Active Cooling. Scanbox Meal Delivery CartsManunoghiNessuna valutazione finora
- Somanabolic+Muscle+Maximizer+PDF+ +eBook+Free+Download+Kyle+LeonDocumento34 pagineSomanabolic+Muscle+Maximizer+PDF+ +eBook+Free+Download+Kyle+LeonAaron BarclayNessuna valutazione finora
- CH 3 TestDocumento50 pagineCH 3 TestVK ACCANessuna valutazione finora
- NewspaperDocumento2 pagineNewspaperbro nabsNessuna valutazione finora
- 7th Nani Palkhiwala Research Paper CompetitionDocumento31 pagine7th Nani Palkhiwala Research Paper CompetitionhridhaykhuranaNessuna valutazione finora
- ISO StandardsDocumento7 pagineISO StandardsHusnain BaigNessuna valutazione finora
- AH Business-Management All 2011Documento11 pagineAH Business-Management All 2011Sanam PuriNessuna valutazione finora
- Cottrell Park Golf Club 710Documento11 pagineCottrell Park Golf Club 710Mulligan PlusNessuna valutazione finora
- Theater InstallationDocumento7 pagineTheater InstallationtemamNessuna valutazione finora
- Handout No. 03 - Purchase TransactionsDocumento4 pagineHandout No. 03 - Purchase TransactionsApril SasamNessuna valutazione finora
- Cel2106 SCL Worksheet 6Documento3 pagineCel2106 SCL Worksheet 6HarryJoy JackNessuna valutazione finora
- Concept MapDocumento1 paginaConcept Mapapi-402935758Nessuna valutazione finora
- Defining The Christian Faith PaperDocumento8 pagineDefining The Christian Faith Paperlin tongNessuna valutazione finora
- The Role of Leadership On Employee Performance in Singapore AirlinesDocumento42 pagineThe Role of Leadership On Employee Performance in Singapore Airlineskeshav sabooNessuna valutazione finora