Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Effect of Maternal Hypertension On Neonatal Outcome
Caricato da
atika sgrt0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
12 visualizzazioni6 pagineEffect of Maternal Hypertension on Neonatal Outcome
Titolo originale
Effect of Maternal Hypertension on Neonatal Outcome
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoEffect of Maternal Hypertension on Neonatal Outcome
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
12 visualizzazioni6 pagineEffect of Maternal Hypertension On Neonatal Outcome
Caricato da
atika sgrtEffect of Maternal Hypertension on Neonatal Outcome
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 6
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
Effect of Maternal Hypertension on Neonatal Outcome
in Diyala Province, Iraq
* Kareem Assi Obaid
** Maan Baker Kadoori
*** Ghasaq Maan Baker
Abstract
Background: Maternal hypertension and preeclampsia are a multisystem, highly variable
disorder unique to pregnancy and a leading cause of maternal and fetal/neonatal morbidity
and mortality. Given the progressive nature of the disorder, delivery is often necessary to
minimize maternal morbidity and mortality; obstetricians must balance the need for achieving
in utero fetal maturation with the maternal and fetal risks of continuing pregnancy.
Objectives: To evaluate the maternal burden and neonatal outcomes of infants delivered to
mothers with preeclampsia, to review the outcomes of late-preterm infants, and potential
strategies to optimize fetal outcomes in pregnancies complicated by preeclampsia.
Materials and Methods: A cohort prospective study done in Albatool Maternity Teaching
Hospital from October 2011 to April 2012 for 55 mothers coming for antenatal follow up how
hypertension and preeclampsia had been followed till delivery with their delivered neonates
looking for the maternal hypertension, medication, liver function, complete blood picture,
complications of preeclampsia and neonatal condition at birth, weight, respiratory function,
feeding, complete blood picture and liver function, small for gestational age (SGA),
respiratory distress syndrome (RDS), and neonatal death (NND) .
Results: Infants of women with preeclampsia were more likely to be SGA 27(49% ) and have
RDS 6 (10.1%); Frequency of preterm delivery at <37 weeks' gestation rose greatly with
increasing severity of maternal hypertension 16 (29%). Fetal distress was seen in 12 cases
(21.8%) with meconium staining of liquor in 8 cases 14.5% ,33 neonates (60%) required
admission for many reasons. Mothers with hypertension have high risk of ante partum
hemorrhage 40(72%), 17 delivered normally (30%) while 38 delivered by caesarean section
(70%).
Conclusion: Compared with neonates delivered prematurely because of other etiologies,
neonates born to preeclamptic mothers were more likely to be SGA and have less RDS, but
had a decrease in mortality. This may be a reflection of the differences in the underlying
pathophysiology behind indicated preterm birth due to preeclampsia.
Key Words: Maternal hypertension, Neonatal outcome, Diyala province, Iraq.
*Department of Pediatrics/ College of Medicine/ Diyala University/ Diyala/ Iraq.
**, *** Al-Batool Teaching Hospital/ Diyala Health Governorate/ Diyala/ Iraq.
Diyala Journal of Medicine 69 Vol. 5, Issue 2, December 2013
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
Introduction maternal morbidity and mortality. On
Maternal hypertension and preeclampsia the other hand, one of the primary goals of
are a multisystem, highly variable disorder obstetricians is to deliver infants who are
unique to pregnancy and a leading cause of functionally mature and capable of adapting
maternal and fetal/neonatal morbidity and to the extrauterine environment without the
mortality [1–7]. While preeclampsia need for intensive care [19]. Therefore, in
complicates 6%–10% of all pregnancies in pregnancies complicated by preeclampsia,
the United States, the incidence is believed to obstetricians must balance the need for
be even higher in underdeveloped countries achieving in utero fetal maturation with the
[8, 9]. Recent evidence suggests that maternal and fetal risks of continuing
preeclampsia accounts for approximately pregnancy, including progression to
15.9% of all maternal deaths in the United eclampsia, abruptio placentae, and HELLP
States and is a major cause of perinatal syndrome, as well as fetal growth restriction
morbidity and death [10, 11]. Therefore, and demise [17, 20–22]. At the present time,
physicians must carefully weigh the risks to delivery is typically recommended for
both mother and fetus in management women who develop preeclampsia,
decisions. To that end, optimal treatment regardless of disease severity, at 37
strategies have not been fully defined, gestational weeks [23]. In addition, delivery
leaving physicians with incomplete data to is recommended for all women with severe
guide their patient care practices [8, 12, 13]. preeclampsia not after than 34 weeks
The increased incidence of perinatal gestation [9, 24].
morbidity and mortality seen in pregnancies In pregnancies complicated by
complicated by preeclampsia, although preeclampsia, thrombocytopenia is generally
complex and multifactorial, is primarily due identified at birth or within the first 2–3 days
to the need for premature delivery and following delivery, with resolution by 10
uteroplacental insufficiency resulting in a days of life in most cases [38]
compromise of blood flow to the fetus [14, Materials and Methods
15]. A cohort prospective study done in
Ante partum diagnosis of mild, moderate, Albetool Maternity Teaching Hospital from
and severe preeclampsia are based on series October 2011 to April 2012 for 55 mothers
of defined criteria occurring after 20 weeks coming for antenatal fellow up how had
of gestation [16]. Severe PE is defined as a preeclampsia had been followed till delivery
blood pressure greater than 160 mm Hg with their delivered neonates looking for the
(systolic) or 110 mm Hg (diastolic) maternal hypertension, medication, liver
associated with proteinuria greater than or function, complete blood picture,
equal to 5 grams per day. In contrast, mild PE complications of preeclampsia and neonatal
is characterized by an elevated blood condition at birth, weight, respiratory
pressure less than 160 mm Hg (systolic) or condition after birth, feeding, complete blood
120 mm Hg (diastolic) with proteinuria picture and liver function .
greater than 300 mg, but less than 5 g, per Results
day [9]. Infants of women with preeclampsia were
The only definitive cure for preeclampsia more likely to be SGA 27 (49% ) and have
is delivery of the fetus and placenta [18]. RDS 6 (10.1%); Frequency of preterm
Given the progressive nature of the disorder, delivery at <37 weeks' gestation rose greatly
delivery is often necessary to minimize with increasing severity of maternal
Diyala Journal of Medicine 70 Vol. 5, Issue 2, December 2013
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
hypertension 16 (29%). Fetal distress was reasons. Mothers with hypertension
seen in 12 cases (21.8%) with meconium have high risk of ante partum hemorrhage
staining of liquor in 8 cases 14.5%, 33 40(72%), 17 delivered normally (30%) while
neonates (60%) required admission for many 38 delivered by caesarean section (70%).
Table (1): Ante partum Maternal Demographic data of the study.
XXXXXXX Preeclampsia (Total 55cases) % from total
No. of cases
Thrombocytopenia 3 5.4
High liver enzymes 3 1.8
Protienuria 2 3.6
Antenatal H. 40 72
Still Birth 1 1.8
Abortion 0 0
Normal delivery 17 30
Caesarian delivery 38 70
Table (2): Neonatal Demographic data of the study.
XXXXXXX (Total 55 cases) % from total
No. of cases
RDS 6 10.1
Sepsis 0 0
Meconium stained liquor 8 14.5
Fetal distress 12 21.8
NICU admission 33 60
Death 0 0
Resuscitation 50 90
Thrombocytopenia 0 0
Low Birth weight 27 49
High liver enzymes 0 0
Discussion respiratory distress syndrome than term
Accumulating evidence suggests that infants (28.9% versus 4.2%) [33,34] ,while
preterm infants are physiologically immature in this study10.1 % cases developed
compared with infants born at term and are at respiratory distress and required neonatal
significant risk for a broad range of intensive care admission (Table 2).
complications [25–29]. Neonatal and infant Importantly, evidence suggests a significant
mortality rates are consistently higher in late- reduction in neonatal respiratory morbidity
preterm infants than in term infants [30–32]. when gestation is extended beyond 34 weeks,
Evidence suggests that late-preterm a benefit seen for each week increase in
infants have nine times greater incidence of gestational age up to term [33, 34]. In a
Diyala Journal of Medicine 71 Vol. 5, Issue 2, December 2013
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
population-based study of neonatal morbidity high risk. National Institute of Child
in the United States, the incidence of RDS Health and Human Development Network of
was 7.4% at 34 weeks, 4.5% at 35 weeks, Maternal-Fetal Medicine Units,” American
2.3% at 36 weeks, and 1.2% at 37 weeks Journal of Obstetrics and Gynecology, vol.
[33]. 179, no. 4, pp. 946–951, 1998.
Stillbirth represents an important cause of [2] K. A. Douglas and C. W. G. Redman,
fetal loss in the preterm infant [34]. Although “Eclampsia in the United Kingdom,” British
greater than 90% of fetal deaths occur in the Medical Journal, vol. 309, no. 6966, pp.
first 20 weeks of gestation, the rate of 1395–1400, 1994.
stillbirth is approximately 3 per 1000 live [3] R. B. Ness and J. M. Roberts,
births beyond 28 weeks gestation in our “Heterogeneous causes constituting the
study % of cases have fetal deaths (table 2) single syndrome of preeclampsia: a
Interestingly, evidence suggests that hypothesis and its implications,” American
beginning at approximately 36 weeks, the Journal of Obstetrics and Gynecology, vol.
risk of intrauterine fetal demise increases 175, no. 5, pp. 1365–1370, 1996.
substantially [35]. Severe preeclampsia [4] C. W. Redman and J. M. Roberts,
represents significant risk factor for “Management of pre-eclampsia,” The Lancet,
intrauterine fetal demise, with estimated vol. 341, no. 8858, pp. 1451–1454, 1993.
stillbirth rate of 21 per 1000 [36]. Maternal [5] J. M. Roberts, “Preventing pre-
preeclampsia can result in neonatal eclampsia,” The Lancet, vol. 348, no. 9023,
thrombocytopenia, typically defined as a pp. 281–282, 1996.
platelet count less than 150,000/uL [37]. [6] J. M. Roberts and D. W. Cooper,
Conclusion “Pathogenesis and genetics of pre-
Historically, there has been a relative lack eclampsia,” The Lancet, vol. 357, no. 9249,
of consideration to the complications of pp. 53–56, 2001.
premature delivery at greater than 34 weeks [7] J. M. Roberts and C. W. G. Redman,
gestation, with the belief that 34 weeks is a “Pre-eclampsia: more than pregnancy-
surrogate marker for fetal maturity. Recent induced hypertension,” The Lancet, vol. 341,
evidence suggests that infants born between no. 8858, pp. 1447–1451, 1993.
34 and 36 weeks gestation are, in fact, [8] H. J. Odendaal, R. C. Pattinson, R. Bam,
physiologically immature compared to term D. Grove, and T. J. V. W. Kotze,
infants. Because of the high variability of “Aggressive or expectant management for
each case, a general recommendation for the patients with severe preeclampsia between
optimal timing of delivery is not possible. 28-34 weeks' gestation: a randomized
However, based on the review of data, we controlled trial,” Obstetrics and Gynecology,
believe that a multidisciplinary, collaborative vol. 76, no. 6, pp. 1070–1075, 1990.
approach between the fields of maternal-fetal [9] B. M. Sibai, “Diagnosis and management
medicine and neonatology is necessary to of gestational hypertension and
weigh the maternal and fetal risks of preeclampsia,” Obstetrics and Gynecology,
prolonging the pregnancy versus the potential vol. 102, no. 1, pp. 181–192, 2003.
benefits of further fetal maturation across [10] C. J. Berg, J. Chang, W. M. Callaghan,
most gestational ages. and S. J. Whitehead, “Pregnancy-related
References mortality in the United States, 1991–1997,”
[1] S. Caritis, B. Sibai, J. Hauth et al., Obstetrics and Gynecology, vol. 101, no. 2,
“Predictors of pre-eclampsia in women at pp. 289–296, 2003.
Diyala Journal of Medicine 72 Vol. 5, Issue 2, December 2013
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
[11] L. Duley, “Pre-eclampsia and the American Journal of Obstetrics and
hypertensive disorders of pregnancy,” British Gynecology, vol. 168, no. 1, part 1, pp. 214–
Medical Bulletin, vol. 67, pp. 161–176, 2003. 227, 1993.
[12] S. M. Khedun, J. Moodley, T. Naicker, [21] B. Haddad and B. M. Sibai, “Expectant
and B. Maharaj, “Drug management of management of severe preeclampsia: proper
hypertensive disorders of pregnancy,” candidates and pregnancy outcome,” Clinical
Pharmacology and Therapeutics, vol. 74, no. Obstetrics and Gynecology, vol. 48, no. 2,
2, pp. 221–258, 1997. pp. 430–440, 2005.
[13] B. M. Sibai, B. M. Mercer, E. Schiff, [22] B. M. Sibai, S. N. Caritis, E. Thom et
and S. A. Friedman, “Aggressive Versus al., “Prevention of preeclampsia with low-
expectant management of severe dose aspirin in healthy, nulliparous pregnant
preeclampsia at 28 to 32 weeks' gestatian: a women. The National Institute of Child
randomized controlled trial,” American Health and Human Development Network of
Journal of Obstetrics and Gynecology, vol. Maternal-Fetal Medicine Units,” The New
171, no. 3, pp. 818–822, 1994. England Journal of Medicine, vol. 329, no.
[14] G. A. Dekker and B. M. Sibai, “Etiology 17, pp. 1213–1218, 1993.
and pathogenesis of preeclampsia: current [23] M. Knuist, G. J. Bonsel, H. A.
concepts,” American Journal of Obstetrics Zondervan, and P. E. Treffers,
and Gynecology, vol. 179, no. 5, pp. 1359– “Intensification of fetal and maternal
1375, 1998. surveillance in pregnant women with
[15] S. A. Friedman, E. Schiff, L. Kao, and hypertensive disorders,” International Journal
B. M. Sibai, “Neonatal outcome after preterm of Gynecology and Obstetrics, vol. 61, no. 2,
delivery for preeclampsia,” American Journal pp. 127–133, 1998.
of Obstetrics and Gynecology, vol. 172, no. [24] J. R. Barton, J. M. O'Brien, N. K.
6, pp. 1785–1792, 1995. Bergauer, D. L. Jacques, and B. M. Sibai,
[16] L. K. Wagner, “Diagnosis and “Mild gestational hypertension remote from
management of preeclampsia,” American term: progression and outcome,” American
Family Physician, vol. 70, no. 12, pp. 2317– Journal of Obstetrics and Gynecology, vol.
2324, 2004. 184, no. 5, pp. 979–983, 2001.
[17] B. M. Sibai, S. Caritis, and J. Hauth, [25] G. G. Dudell and L. Jain, “Hypoxic
“What we have learned about preeclampsia,” respiratory failure in the late preterm infant,”
Seminars in Perinatology, vol. 27, no. 3, pp. Clinics in Perinatology, vol. 33, no. 4, pp.
239–246, 2003. 803–830, 2006.
[18] “ACOG Practice Bulletin. Diagnosis [26] L. Jain and G. G. Dudell, “Respiratory
and management of preeclampsia and transition in infants delivered by cesarean
eclampsia. Number 33, January 2002,” section,” Seminars in Perinatology, vol. 30,
Obstetrics & Gynecology, vol. 99, no. 1, pp. no. 5, pp. 296–304, 2006.
159–167, 2002. [27] J. A. Martin, B. E. Hamilton, P. D.
[19] “ACOG Practice Bulletin No. 97: fetal Sutton et al., “Births: final data for 2005,”
lung maturity,” Obstetrics & Gynecology, National Vital Statistics Reports, vol. 56, no.
vol. 112, no. 3, pp. 717–726, 2008. 6, pp. 1–103, 2007.
[20] G. A. Dekker and B. M. Sibai, “Low- [28] T. N. K. Raju, R. D. Higgins, A. R.
dose aspirin in the prevention of Stark, and K. J. Leveno, “Optimizing care
preeclampsia and fetal growth retardation: and outcome for late-preterm (near-term)
rationale, mechanisms, and clinical trials,” infants: a summary of the workshop
Diyala Journal of Medicine 73 Vol. 5, Issue 2, December 2013
Effect of Maternal Hypertension on Neonatal Outcome in Diyala Province, Iraq Kareem Assi Obaid
sponsored by the national institute of child Journal of Obstetrics and
health and human development,” Pediatrics, Gynecology, vol. 166, pp. 1629–1645, 1992.
vol. 118, no. 3, pp. 1207–1214, 2006. [37] J. H. Richardus, W. C. Graafmans, S. P.
[29] M. L. Wang, D. J. Dorer, M. P. Fleming, Verloove-Vanhorick et al., “Differences in
and E. A. Catlin, “Clinical outcomes of near- perinatal mortality and suboptimal care
term infants,” Pediatrics, vol. 114, pp. 372– between 10 European regions: results of an
376, 2004. international audit,” An International Journal
[30] W. A. Engle, K. M. Tomashek, C. of Obstetrics and Gynaecology, vol. 110, no.
Wallman et al., “"Late-preterm" infants: a 2, pp. 97–105, 2003.
population at risk,” Pediatrics, vol. 120, no.
6, pp. 1390–1401, 2007.
[31] M. S. Kramer, K. Demissie, H. Yang, R.
W. Platt, R. Sauve, and R. Liston, “The
contribution of mild and moderate preterm
birth to infant mortality. Fetal and Infant
Health Study Group of the Canadian
Perinatal Surveillance System,” Journal of
the American Medical Association, vol. 284,
no. 7, pp. 843–849, 2000.
[32] D. D. McIntire and K. J. Leveno,
“Neonatal mortality and morbidity rates in
late preterm births compared with births at
term,” Obstetrics and Gynecology, vol. 111,
no. 1, pp. 35–41, 2008.
[33] L. Jain, “Respiratory morbidity in late-
preterm infants: prevention is better than
cure!,” American Journal of Perinatology,
vol. 25, no. 2, pp. 75–78, 2008.
[34] M. Roth-Kleiner, B. P. Wagner, D.
Bachmann, and J. Pfenninger, “Respiratory
distress syndrome in near-term babies after
caesarean section,” Swiss Medical Weekly,
vol. 133, no. 19-20, pp. 283–288, 2003.
[35] W. M. Gilbert, T. S. Nesbitt, and B.
Danielsen, “The cost of prematurity:
quantification by gestational age and birth
weight,” Obstetrics and Gynecology, vol.
102, no. 3, pp. 488–492, 2003. ·
[36] P. A. Robertson, S. H. Sniderman, R. K.
Laros Jr. et al., “Neonatal morbidity
according to gestational age and birth weight
from five tertiary care centers in the United
States, 1983 through 1986,” American
Diyala Journal of Medicine 74 Vol. 5, Issue 2, December 2013
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Total and Acute Uterine Inversion After Delivery A Case Report PDFDocumento4 pagineTotal and Acute Uterine Inversion After Delivery A Case Report PDFatika sgrtNessuna valutazione finora
- Metabolic Precursors of SurfactantDocumento8 pagineMetabolic Precursors of Surfactantatika sgrtNessuna valutazione finora
- Cervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal DiseaseDocumento6 pagineCervical Insufficiency A New Issue For Guidelines On Prevention of Perinatal Group B Streptococcal Diseaseatika sgrtNessuna valutazione finora
- PLACENTAL LESIONS ASSOCIATED WITH MATERNAL Underperfusion Are More Frequent in Early Onset Pre EclampsiaDocumento22 paginePLACENTAL LESIONS ASSOCIATED WITH MATERNAL Underperfusion Are More Frequent in Early Onset Pre Eclampsiaatika sgrtNessuna valutazione finora
- Preeclampsia and The Risk of Bronchopulmonary Dysplasia in VLBW Infants A Population Based StudyDocumento7 paginePreeclampsia and The Risk of Bronchopulmonary Dysplasia in VLBW Infants A Population Based Studyatika sgrtNessuna valutazione finora
- Clinical Risk Index For Babies (CRIB II)Documento4 pagineClinical Risk Index For Babies (CRIB II)atika sgrtNessuna valutazione finora
- 11 - Chapter 4 Muslim Law PDFDocumento87 pagine11 - Chapter 4 Muslim Law PDFAnfal BarbhuiyaNessuna valutazione finora
- Ownership Data: InstallationDocumento2 pagineOwnership Data: InstallationRoshin99Nessuna valutazione finora
- Ka TurayDocumento6 pagineKa TurayNizelCalmerinBaesNessuna valutazione finora
- Understanding Building Construction Types - Firefighter Nation PDFDocumento3 pagineUnderstanding Building Construction Types - Firefighter Nation PDFRakeshNessuna valutazione finora
- LabreportDocumento4 pagineLabreportDarwinys SamijonNessuna valutazione finora
- Apply Health, Safety and Security Procedures in The WorkplaceDocumento9 pagineApply Health, Safety and Security Procedures in The WorkplaceRene EspenocillaNessuna valutazione finora
- Fdocuments - in - List of Private Laboratories Empanelled by KSPCB As Per of Empanelment LabsDocumento7 pagineFdocuments - in - List of Private Laboratories Empanelled by KSPCB As Per of Empanelment LabsKartik RajputNessuna valutazione finora
- Checklist of Eligibility Requirements For Consulting ServicesDocumento2 pagineChecklist of Eligibility Requirements For Consulting ServicesAndrea BroccoliNessuna valutazione finora
- Final Exam Review AnswerDocumento6 pagineFinal Exam Review AnswerJosh ClickNessuna valutazione finora
- SLL VS NLRCDocumento11 pagineSLL VS NLRCJepski ScopeNessuna valutazione finora
- 2022 CA Security Assessment and Authorization StandardDocumento25 pagine2022 CA Security Assessment and Authorization StandardDonaldNessuna valutazione finora
- Test 6Documento3 pagineTest 6Андрій МедвідьNessuna valutazione finora
- Opiods MorphineDocumento4 pagineOpiods MorphinevysakhmohanannairNessuna valutazione finora
- Assessment of Yalova University Campus According To LEED V.4 Certification SystemDocumento11 pagineAssessment of Yalova University Campus According To LEED V.4 Certification SystemUmitNessuna valutazione finora
- Roofing ActivitiesDocumento2 pagineRoofing ActivitiesArnold Roy Coballes ManaloNessuna valutazione finora
- Formatof Indenity BondDocumento2 pagineFormatof Indenity BondSudhir SinhaNessuna valutazione finora
- Assessing Health Impacts of Air Pollution From Electricity Generation The Case of ThailandDocumento22 pagineAssessing Health Impacts of Air Pollution From Electricity Generation The Case of Thailandcamilo_ortiz_6100% (1)
- Sentinel Node Biopsy For CA BreastDocumento7 pagineSentinel Node Biopsy For CA Breastwasima1956Nessuna valutazione finora
- Notes On Substance AbuseDocumento15 pagineNotes On Substance Abusesarguss14100% (1)
- Literature Review Devin KilburnDocumento4 pagineLiterature Review Devin Kilburnapi-549230129Nessuna valutazione finora
- Class 8 Cbse Science Question Paper Fa 1Documento2 pagineClass 8 Cbse Science Question Paper Fa 1Sunaina Rawat100% (1)
- Iso 27001 PDFDocumento7 pagineIso 27001 PDFMonica MoreiraNessuna valutazione finora
- A Qualitative Study of Depression in Primary Care: Missed Opportunities For Diagnosis and EducationDocumento8 pagineA Qualitative Study of Depression in Primary Care: Missed Opportunities For Diagnosis and EducationTeam BEENessuna valutazione finora
- Aalco Metals LTD - Stainless Steel 201201L202204 - 97 PDFDocumento3 pagineAalco Metals LTD - Stainless Steel 201201L202204 - 97 PDFNaman PrajapatiNessuna valutazione finora
- Learning Activity 4 Evidence: My View On Colombia: 1. Write A Composition Describing What The LifestyleDocumento2 pagineLearning Activity 4 Evidence: My View On Colombia: 1. Write A Composition Describing What The LifestyleYenifer PatiñoNessuna valutazione finora
- The Neurovascular Bundle of The Anterior Compartment ofDocumento30 pagineThe Neurovascular Bundle of The Anterior Compartment ofAnnapurna Bose100% (2)
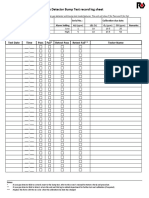
- Gas Detector Bump Test Record Log Sheet: Bump Test Result Test Date Time Pass Fail Retest Pass Retest Fail Tester NameDocumento2 pagineGas Detector Bump Test Record Log Sheet: Bump Test Result Test Date Time Pass Fail Retest Pass Retest Fail Tester NameAndry Kurnia100% (2)
- Pressure Systems Safety Regulations 2000Documento10 paginePressure Systems Safety Regulations 2000Alberico MuratoriNessuna valutazione finora
- W - Paul Smith, William C. Compton and W - Beryl WestDocumento5 pagineW - Paul Smith, William C. Compton and W - Beryl Westefarfan26Nessuna valutazione finora
- Installation Instructions / Operating & Maintenance Manual Reduced Pressure Zone (RPZ) Valves Type "BA" DevicesDocumento3 pagineInstallation Instructions / Operating & Maintenance Manual Reduced Pressure Zone (RPZ) Valves Type "BA" DevicesCire Lop CastroNessuna valutazione finora