Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Shachar2014 PDF
Caricato da
Mahlina Nur Laili0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
21 visualizzazioni1 paginaTitolo originale
shachar2014.pdf
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
21 visualizzazioni1 paginaShachar2014 PDF
Caricato da
Mahlina Nur LailiCopyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 1
www.AJOG.
org Prematurity, Physiology Poster Session V
759 Unexpected finding in vaginal microbiome assessment STUDY DESIGN: We analyzed approximately a million California
in PPROM births 2007-10. Logistic regression was used to estimate odds ratios
Elizabeth Baldwin1, Marina Walther-Antonio2, Brian Brost1, (ORs) for risk of PTB, with an IPI of 18-23 months serving as the
Arij Faksh1, Mari Charisse Trinidad1, Wendy White1, reference interval. Risks for extreme (20-23 weeks), early (24-31
Norman Davies1, Carl Rose1, Kristi Borowski1, Nicholas Chia2, weeks) and medium to late PTB (32-36 weeks) were assessed. ORs
Douglas Creedon1 were adjusted for maternal age, race, medical insurance payment,
1
Mayo Clinic College of Medicine, Maternal Fetal Medicine, Rochester, MN, and education.
2
Mayo Clinic College of Medicine, Department of Surgical Research, RESULTS: Women with an IPI of <6 months after a live birth had an
Rochester, MN increased risk of PTB with adjusted ORs of 2.29, 2.12 and 1.71 for
OBJECTIVE: Altered vaginal microbial population and subclinical extreme, early and late PTB, respectively. Similarly, women with an
infection have long been posited as major contributors to preterm IPI of 6-11 months had an increased risk of PTB with ORs of 1.45,
birth, the leading cause worldwide for infant morbidity and mor- 1.21 and 1.22, respectively. Long IPI of > 59 months was associated
tality. We sought to describe the vaginal microbiome using high with an increased risk for PTB with ORs of 1.53, 1.57 and 1.22 for
throughput genomic technology in the setting of preterm premature the above groups. Women with an IPI of <6 months after pregnancy
rupture of membranes (PPROM). termination had a decreased risk for PTB, with ORs of 0.71 and 0.84
STUDY DESIGN: We recruited women diagnosed with PPROM be- for early and late PTB, respectively. All noted ORs had 95% confi-
tween 23 and 34 weeks gestation. Antenatal care per standard pro- dence intervals that excluded one.
tocol included 7 days of latency antibiotics. Serial posterior fornix CONCLUSION: Short and long IPIs were associated with PTB in this
vaginal swabs were collected from diagnosis until delivery. 48 sam- large US cohort. It is possible that etiologies other than maternal
ples from 13 subjects were obtained every 3 days for 2 weeks, then depletion and maternal underweight may underlie the association of
weekly until delivery. DNA was extracted using MoBio Powersoil. PTB with shortened IPI. Given that IPI is potentially a modifiable
Bacterial 16S rDNA was amplified using universal probes. When risk factor for PTB, more efforts toward elucidating the association
bacterial DNA was identified, the microbial composition was profiled between IPI and risk could make substantial contribution to PTB
using 16S rDNA hypervariable tag sequencing of the V3-V5 region prevention.
using the Illumina MiSeq platform.
RESULTS: Bacterial DNA was identified in 15 of 48 samples. Of the 13 761 Fetal and placental hemodynamic responses to acute
subjects, only 5 were found to have bacterial DNA present at any cardiac outflow tract occlusion in an experimental sheep
point following diagnosis of PPROM and initiation of antibiotics. model
Only 1 subject was found to have quantifiable bacterial DNA at the Juulia Junno1, Juha Räsänen5, Heikki Huhta1, Mervi Haapsamo1,
time of diagnosis and only 2 subjects had any positive samples Tiina Erkinaro2, Roger Hohimer3, Lowell Davis3, Ganesh Acharya4
1
during the course of latency antibiotics. University of Oulu, Obstetrics and Gynecology, Oulu, Finland, 2University of
CONCLUSION: Our study is the first to describe the vaginal microbial Oulu, Anesthesiology, Oulu, Finland, 3Oregon Health and Science University,
pattern in PPROM using next generation sequencing techniques. In Obstetrics and Gynecology, Portland, OR, 4University Hospital of Northern
addition, this study illustrates a novel finding in the absence of Norway, Obstetrics and Gynecology, Tromso, Norway, 5University of Eastern
Finland, Obstetrics and Gynecology, Kuopio, Finland
bacterial DNA identifiable by non-culture dependent state of the art
OBJECTIVE: In fetal circulation, right (RVCO) and left (LVCO) ven-
metagenomic methods in vaginal samples from subjects with
PPROM. Prior work using similar methodology has not shown tricular cardiac outputs are arranged parallelly. Myocardial, brain
undetectable levels of bacterial DNA from vaginal swabs in normal and upper body blood supply is provided by LVCO, and RVCO is
pregnant women or women with symptoms of preterm labor; this mainly responsible for lower body and placental circulation. We
appears to be unique to PPROM. Further investigation is warranted investigated fetal sheep arterial and venous, as well as placental he-
and ongoing but this preliminary finding was unexpected given the modynamic responses to acute occlusion of ascending aorta (AAo)
conventional understanding of subclinical infection as a major and pulmonary artery (PA).
STUDY DESIGN: At 120-126 gestational days (term 145 days), 7 ewes
contributor in PPROM.
underwent surgery for the placement of a vascular occluder around
760 Interpregnancy interval length and risk of preterm birth, fetal PA and in 9 ewes a vascular occluder was placed around fetal
a large US study AAo. Fetal carotid artery and jugular vein were cannulated. After a 5-
Bat zion Shachar1, Jonathan Mayo1, Deirdre Lyell2, day recovery, fetal systemic cardiac output (SCO), umbilical artery
David Stevenson1, Gary Shaw1 (UA), descending aorta (DAo), ductus venosus (DV) and inferior
1
Stanford University School Of Medicine, On behalf of the March of Dimes vena cava (IVC) pulsatility indices (PI) were obtained. Placental
prematurity center, Stanford, CA, 2Stanford University School Of Medicine, volume blood flow (Qplac) was calculated from intraabdominal
Department of Obstetrics and Gynecology, Stanford, CA umbilical vein. Data were collected at baseline, 15 and 60 minutes
OBJECTIVE: Short interpregnancy interval (IPI), time between end of after PA/AAo occlusion, and 15 minutes after release of PA/AAo
pregnancy and next conception, is associated with preterm birth occlusion. Fetal mean arterial (mABP) and central venous (CVP)
(PTB) in developing countries. Data from developed countries are pressures, and blood gas values were monitored.
scant and outdated. US women often give birth at more advanced RESULTS: PA occlusion decreased SCO about 50% (p<0.001) from
age and subsequent births with shorter IPIs. However, they may be the baseline, while in the AAo occlusion group the corresponding
less prone to suffer from underweight or maternal depletion syn- drop was about 16% (p<0.01). In both groups, UA and DAo PIs
drome, a possible underlying mechanism for the association between were unaffected. However, PA occlusion decreased Qplac about 44%
short IPI and PTB. Our objective was to determine whether short IPI from the baseline. In the AAo occlusion group Qplac remained
is associated with PTB in the US. unchanged. PA occlusion increased (p<0.05) DV and IVC PIs, as
Supplement to JANUARY 2014 American Journal of Obstetrics & Gynecology S373
Potrebbero piacerti anche
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDa EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNessuna valutazione finora
- Acta Obstet Gynecol Scand - 2004 - Olofsson - Low Umbilical Artery Vascular Flow Resistance and Fetal OutcomeDocumento3 pagineActa Obstet Gynecol Scand - 2004 - Olofsson - Low Umbilical Artery Vascular Flow Resistance and Fetal OutcomeSiti AminathinNessuna valutazione finora
- 61 Goepfert2004Documento7 pagine61 Goepfert2004angela_karenina_1Nessuna valutazione finora
- Vasa Praevia PDFDocumento6 pagineVasa Praevia PDFAlwinNessuna valutazione finora
- Good18.Prenatally Diagnosed Vasa Previa A.30Documento9 pagineGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- Are Women With Recurrent Spontaneous Preterm Births Different From Those Without Such HistoryDocumento9 pagineAre Women With Recurrent Spontaneous Preterm Births Different From Those Without Such HistoryMichael HusainNessuna valutazione finora
- The Problems of Moderate Preterm Infants: Seminars in PerinatologyDocumento4 pagineThe Problems of Moderate Preterm Infants: Seminars in Perinatologysam crushNessuna valutazione finora
- Administrator,+Journal+Manager,+1469 4991 1 CEDocumento5 pagineAdministrator,+Journal+Manager,+1469 4991 1 CESamarNessuna valutazione finora
- Meconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhageDocumento5 pagineMeconium-Stained Amniotic Fluid: A Risk Factor For Postpartum HemorrhagelaniNessuna valutazione finora
- Neonatal Complications of Term Pregnancy: Rates by Gestational Age Increase in A Continuous, Not Threshold, FashionDocumento6 pagineNeonatal Complications of Term Pregnancy: Rates by Gestational Age Increase in A Continuous, Not Threshold, FashionAndreea BorislavschiNessuna valutazione finora
- Validation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent Placenta PDFDocumento2 pagineValidation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent Placenta PDFOmpNessuna valutazione finora
- Validation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent PlacentaDocumento2 pagineValidation of The Placenta Accreta Index (PAI) - Improving The Antenatal Diagnosis of The Morbidly Adherent PlacentaOmpNessuna valutazione finora
- Neonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkDocumento14 pagineNeonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkKattia FloresNessuna valutazione finora
- Murphy2002 Posthaemorrhagic Ventricular DilatationDocumento6 pagineMurphy2002 Posthaemorrhagic Ventricular DilatationModou NianeNessuna valutazione finora
- Placenta Accreta Is Associated With IVF Pregnancies: A Retrospective Chart ReviewDocumento6 paginePlacenta Accreta Is Associated With IVF Pregnancies: A Retrospective Chart ReviewGladstone AsadNessuna valutazione finora
- Natural History of Fetal Position During Pregnancy.11Documento6 pagineNatural History of Fetal Position During Pregnancy.11PutriNessuna valutazione finora
- 070Documento8 pagine070Ella ChiraNessuna valutazione finora
- Jp2011191a 2Documento6 pagineJp2011191a 2AnapaolaNessuna valutazione finora
- RM 12021Documento4 pagineRM 12021liana devi oktaviaNessuna valutazione finora
- Doppler Prediction of Adverse Perinatal Outcome in PIH and IugrDocumento8 pagineDoppler Prediction of Adverse Perinatal Outcome in PIH and IugrsiminithinNessuna valutazione finora
- Plasma Soluble Endoglin Concentration in Pre-Eclampsia Is Associated With An Increased Impedance To Flow in The Maternal and Fetal CirculationsDocumento8 paginePlasma Soluble Endoglin Concentration in Pre-Eclampsia Is Associated With An Increased Impedance To Flow in The Maternal and Fetal CirculationsHerry SasukeNessuna valutazione finora
- Kobayashi 2014Documento7 pagineKobayashi 2014Mauricio Lopez MejiaNessuna valutazione finora
- Prognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisDocumento6 paginePrognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisWulan CerankNessuna valutazione finora
- State University of New York, Downstate Medical Center, USADocumento2 pagineState University of New York, Downstate Medical Center, USAronynoorNessuna valutazione finora
- MTHFR Genetic Polymorphism and The Risk of Intrauterine Fetal Death in Polish WomenDocumento6 pagineMTHFR Genetic Polymorphism and The Risk of Intrauterine Fetal Death in Polish WomenMauro Porcel de PeraltaNessuna valutazione finora
- Predictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyDocumento7 paginePredictive value of maternal s erum β-hCG concentration in the ruptured tubal ectopic pregnancyyayayaNessuna valutazione finora
- 77754571Documento7 pagine77754571stephaniedianNessuna valutazione finora
- Prenatal DiagnosisDocumento8 paginePrenatal DiagnosisEstefania GutierrezNessuna valutazione finora
- FIGO (International Federation Obstetrics and Gynecology) Pre-Eclampsia 2019Documento58 pagineFIGO (International Federation Obstetrics and Gynecology) Pre-Eclampsia 2019Haykal Estu BhismoroNessuna valutazione finora
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocumento8 pagineAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNessuna valutazione finora
- Nascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesDocumento3 pagineNascimento Et Al. - 2012 - Bloody Nipple Discharge in Infancy - Report of Two CasesflashjetNessuna valutazione finora
- Linear Correlation of Uterine Artery Pulsatility Index (PI) in Mid Trimester in Pregnant Female With Foetal Birth WeightDocumento5 pagineLinear Correlation of Uterine Artery Pulsatility Index (PI) in Mid Trimester in Pregnant Female With Foetal Birth WeightInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Abruptio PlacentaeDocumento5 pagineAbruptio PlacentaeindahNessuna valutazione finora
- Fracture of The Clavicle in The Newborn Following Normal Labor and DeliveryDocumento6 pagineFracture of The Clavicle in The Newborn Following Normal Labor and DeliveryAlberto OrtizNessuna valutazione finora
- Prediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery DopplerDocumento6 paginePrediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery Dopplerganesh reddyNessuna valutazione finora
- Can Placental Growth Factor in Maternal Circulation Identify Fetuses With Placental Intrauterine Growth RestrictionDocumento7 pagineCan Placental Growth Factor in Maternal Circulation Identify Fetuses With Placental Intrauterine Growth RestrictionagusNessuna valutazione finora
- Are Routine Cranial Ultrasounds Necessary in Premature Infants Greater Than 30 Weeks Gestation?Documento5 pagineAre Routine Cranial Ultrasounds Necessary in Premature Infants Greater Than 30 Weeks Gestation?Wulan CerankNessuna valutazione finora
- Gim 20047Documento4 pagineGim 20047Sabhina AnseliaNessuna valutazione finora
- First-Trimester Maternal Ophthalmic Artery Doppler Analysis For Prediction of Pre-EclampsiaDocumento8 pagineFirst-Trimester Maternal Ophthalmic Artery Doppler Analysis For Prediction of Pre-EclampsiaTopan AzzuriniNessuna valutazione finora
- Caos PaperDocumento6 pagineCaos PaperMauricio Lopez MejiaNessuna valutazione finora
- (Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Documento7 pagine(Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Moh RamliNessuna valutazione finora
- 1 s2.0 S000293781502579XDocumento6 pagine1 s2.0 S000293781502579XsaryindrianyNessuna valutazione finora
- Scopus (29) Many2017Documento7 pagineScopus (29) Many2017ika puspitaNessuna valutazione finora
- Umbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialDocumento5 pagineUmbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialAffah MustafaNessuna valutazione finora
- 33873-Article Text-121761-1-10-20170831Documento6 pagine33873-Article Text-121761-1-10-20170831AnggaNessuna valutazione finora
- 08-Premature ThelarcheDocumento6 pagine08-Premature ThelarcheBruno SantanaNessuna valutazione finora
- Jurnal Placenta PreviaDocumento9 pagineJurnal Placenta Previasheva25Nessuna valutazione finora
- 6 PGS缩短受孕时间Documento8 pagine6 PGS缩短受孕时间zjuwindNessuna valutazione finora
- Acute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisDocumento6 pagineAcute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisIntan Wahyu CahyaniNessuna valutazione finora
- Mihu 2015Documento7 pagineMihu 2015Nuryasni NuryasniNessuna valutazione finora
- Antecedents of CPDocumento8 pagineAntecedents of CPЯковлев АлександрNessuna valutazione finora
- Uog 21870Documento9 pagineUog 21870Djlatino LatinoNessuna valutazione finora
- Prolonged Latency of Preterm Premature Rupture of Membranes and Risk of Neonatal SepsisDocumento6 pagineProlonged Latency of Preterm Premature Rupture of Membranes and Risk of Neonatal SepsisYudhi AuliaNessuna valutazione finora
- Jurnal KedokteranDocumento6 pagineJurnal Kedokteranusk.ppdsobgynganjil2022Nessuna valutazione finora
- Guía Preeclampsia IJGO 2019Documento33 pagineGuía Preeclampsia IJGO 2019teresita vargasNessuna valutazione finora
- Avitanrg RG RDocumento2 pagineAvitanrg RG RPrasetio Kristianto BudionoNessuna valutazione finora
- Poster Session I: Results: Study DesignDocumento2 paginePoster Session I: Results: Study DesignFatih AkbarNessuna valutazione finora
- The Efficacy of Quantitative Fetal Fibronectin in Predicting Spontaneous Preterm Birth in Symptomatic Women: A Retrospective Cohort StudyDocumento6 pagineThe Efficacy of Quantitative Fetal Fibronectin in Predicting Spontaneous Preterm Birth in Symptomatic Women: A Retrospective Cohort StudyGeztaNasafirHermawanNessuna valutazione finora
- Vol9 Issue1 06Documento4 pagineVol9 Issue1 06annisaNessuna valutazione finora
- Absceso Hepático NeonatalDocumento6 pagineAbsceso Hepático NeonatalNabila Peña ZapataNessuna valutazione finora
- Journal Pone 0022115 PDFDocumento10 pagineJournal Pone 0022115 PDFMahlina Nur LailiNessuna valutazione finora
- Impact of Advanced Maternal AgeDocumento7 pagineImpact of Advanced Maternal AgeEgyed Fülöp AndreaNessuna valutazione finora
- 2065 1378 1 PB PDFDocumento11 pagine2065 1378 1 PB PDFDwi Fitri WNessuna valutazione finora
- 0 - 2 Tahun Laki-Laki PDFDocumento1 pagina0 - 2 Tahun Laki-Laki PDFMahlina Nur LailiNessuna valutazione finora
- OswegoDocumento6 pagineOswegoMahlina Nur LailiNessuna valutazione finora
- Prediction of Preeclampsia by A Combination of Body Mass Index (BMI), Mean Arterial Pressure (MAP), and Roll Over Test (ROT)Documento4 paginePrediction of Preeclampsia by A Combination of Body Mass Index (BMI), Mean Arterial Pressure (MAP), and Roll Over Test (ROT)Mahlina Nur LailiNessuna valutazione finora
- Anemia Pregnancy OutcomeDocumento10 pagineAnemia Pregnancy OutcomeRaissa Metasari TantoNessuna valutazione finora
- Ijpho 5 211Documento8 pagineIjpho 5 211Mahlina Nur LailiNessuna valutazione finora
- Jtptunimus GDL Rinikumala 6031 2 Babiik IDocumento8 pagineJtptunimus GDL Rinikumala 6031 2 Babiik IMahlina Nur LailiNessuna valutazione finora
- Sha Char 2014Documento5 pagineSha Char 2014Mahlina Nur LailiNessuna valutazione finora
- Sha Char 2014Documento5 pagineSha Char 2014Mahlina Nur LailiNessuna valutazione finora
- Tanduumba 2015Documento6 pagineTanduumba 2015Mahlina Nur LailiNessuna valutazione finora
- Coo 2017Documento14 pagineCoo 2017Mahlina Nur LailiNessuna valutazione finora
- Shachar2014 PDFDocumento1 paginaShachar2014 PDFMahlina Nur LailiNessuna valutazione finora
- S0007114515001166a PDFDocumento8 pagineS0007114515001166a PDFMahlina Nur LailiNessuna valutazione finora
- Short Interpregnancy Intervals and Unfavourable Pregnancy Outcome: Role of Folate DepletionDocumento4 pagineShort Interpregnancy Intervals and Unfavourable Pregnancy Outcome: Role of Folate DepletionMahlina Nur LailiNessuna valutazione finora
- Ann Am Raju 2016Documento5 pagineAnn Am Raju 2016Mahlina Nur LailiNessuna valutazione finora
- Ijpho 5 211Documento8 pagineIjpho 5 211Mahlina Nur LailiNessuna valutazione finora
- SaudiMedJ 36 146Documento4 pagineSaudiMedJ 36 146Mahlina Nur LailiNessuna valutazione finora
- HHS Public AccessDocumento16 pagineHHS Public AccessMahlina Nur LailiNessuna valutazione finora
- Hanley 2017Documento8 pagineHanley 2017Mahlina Nur LailiNessuna valutazione finora
- 80 (11) 871 1 PDFDocumento5 pagine80 (11) 871 1 PDFMahlina Nur LailiNessuna valutazione finora
- Bab Ii PDFDocumento16 pagineBab Ii PDFfaisalfachrurarifinNessuna valutazione finora
- Pen Pal Lesson Plan 3Documento3 paginePen Pal Lesson Plan 3api-664582820Nessuna valutazione finora
- Electronics 11 02566Documento13 pagineElectronics 11 02566卓七越Nessuna valutazione finora
- Chapter 4: Thermal ComfortDocumento16 pagineChapter 4: Thermal ComfortWengelNessuna valutazione finora
- CBSE 10th ResultsDocumento1 paginaCBSE 10th ResultsAkshit SinghNessuna valutazione finora
- Makalah Bahasa Inggris TranslateDocumento14 pagineMakalah Bahasa Inggris TranslatevikaseptideyaniNessuna valutazione finora
- Visi RuleDocumento6 pagineVisi RuleBruce HerreraNessuna valutazione finora
- Transactions List: Marilena Constantin RO75BRDE445SV93146784450 RON Marilena ConstantinDocumento12 pagineTransactions List: Marilena Constantin RO75BRDE445SV93146784450 RON Marilena ConstantinConstantin MarilenaNessuna valutazione finora
- SCIENCE 11 WEEK 6c - Endogenic ProcessDocumento57 pagineSCIENCE 11 WEEK 6c - Endogenic ProcessChristine CayosaNessuna valutazione finora
- Linux ProgramDocumento131 pagineLinux ProgramsivashaNessuna valutazione finora
- Art Integrated ProjectDocumento14 pagineArt Integrated ProjectSreeti GangulyNessuna valutazione finora
- Lesson Plan For DemoDocumento9 pagineLesson Plan For DemoJulius LabadisosNessuna valutazione finora
- The DIRKS Methodology: A User GuideDocumento285 pagineThe DIRKS Methodology: A User GuideJesus Frontera100% (2)
- Diagnosis ListDocumento1 paginaDiagnosis ListSenyorita KHayeNessuna valutazione finora
- Glossary of Blasting TermsDocumento13 pagineGlossary of Blasting TermsNitesh JainNessuna valutazione finora
- Quotation - 1Documento4 pagineQuotation - 1haszirul ameerNessuna valutazione finora
- Learning Competency PDFDocumento1 paginaLearning Competency PDFLEOMAR PEUGALNessuna valutazione finora
- APJ Abdul Kalam Success StoryDocumento1 paginaAPJ Abdul Kalam Success StorySanjaiNessuna valutazione finora
- Prediction of CBR From Index Properties of Cohesive Soils: Magdi ZumrawiDocumento1 paginaPrediction of CBR From Index Properties of Cohesive Soils: Magdi Zumrawidruwid6Nessuna valutazione finora
- The Original Lists of Persons of Quality Emigrants Religious Exiles Political Rebels Serving Men Sold For A Term of Years Apprentices Children Stolen Maidens Pressed and OthersDocumento609 pagineThe Original Lists of Persons of Quality Emigrants Religious Exiles Political Rebels Serving Men Sold For A Term of Years Apprentices Children Stolen Maidens Pressed and OthersShakir Daddy-Phatstacks Cannon100% (1)
- Developpments in OTC MarketsDocumento80 pagineDeveloppments in OTC MarketsRexTradeNessuna valutazione finora
- Subeeka Akbar Advance NutritionDocumento11 pagineSubeeka Akbar Advance NutritionSubeeka AkbarNessuna valutazione finora
- Written Report SampleDocumento16 pagineWritten Report Sampleallanposo3Nessuna valutazione finora
- Ode To The West WindDocumento4 pagineOde To The West WindCharis Mae DimaculanganNessuna valutazione finora
- French Cuisine RecipeDocumento6 pagineFrench Cuisine RecipeJimmy AchasNessuna valutazione finora
- 2022 AMR Dashboard Funding Opportunity Announcement 11.18.2022Documento16 pagine2022 AMR Dashboard Funding Opportunity Announcement 11.18.2022Tuhin DeyNessuna valutazione finora
- Caroline Coady: EducationDocumento3 pagineCaroline Coady: Educationapi-491896852Nessuna valutazione finora
- Concise Selina Solutions Class 9 Maths Chapter 15 Construction of PolygonsDocumento31 pagineConcise Selina Solutions Class 9 Maths Chapter 15 Construction of Polygonsbhaskar51178Nessuna valutazione finora
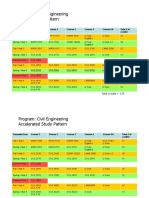
- HKUST 4Y Curriculum Diagram CIVLDocumento4 pagineHKUST 4Y Curriculum Diagram CIVLfrevNessuna valutazione finora
- BAMDocumento111 pagineBAMnageswara_mutyalaNessuna valutazione finora
- Springs: All India Distributer of NienhuisDocumento35 pagineSprings: All India Distributer of NienhuisIrina DroliaNessuna valutazione finora