Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
RadiotherapyProtocols 2010V2 0
Caricato da
Diana MaicanCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
RadiotherapyProtocols 2010V2 0
Caricato da
Diana MaicanCopyright:
Formati disponibili
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Radiotherapy
Protocols
This paper version of the Radiotherapy Protocols is only valid during 2010.
This will be progressively superceded by electronic dated individual sections
which will be complete for 2011.
Issue Date: 08-July-2010 Page 1 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Introduction to Radiotherapy Protocol Book
This Protocol Book sets out to define standard protocol based treatments. The format
is designed to comply with the 2010 Department of Health Manual for Cancer
Services Radiotherapy Measures. Under these measures we are required to maintain a
list of acceptable treatment protocols, including palliative treatment, for all
radiotherapy modalities used which specifies for each protocol at least the following:
The clinical indication
The modality
The tumour localisation and planning technique
Dose/fractionation and overall treatment time relevant to the modality
The treatment and immobilisation equipment and immobilisation
technique
Any restrictions regarding which department in the network are
authorised to deliver the protocol or parts of the protocol, e.g. planning
The conditions governing retreatment and the dose/fractionation and
overall treatment time which then applies
Where possible local standards are chosen to comply with national and internationally
defined standards and the Department of Health quality measures as follows:
Category status
This follows the Royal College of Radiologists Guidelines for defining categories of
patients.
(see The Timely Delivery of Radical Radiotherapy: standards and guidelines for the
management of unscheduled treatment interruptions; Third Edition 2008).
Definition of GTV and PTV
The measures also require that each department specifies the relationship between
PTV and CTV in a documented procedure. Where appropriate we have chosen to
incorporate this information into our standard protocols. This follows ICRU
definitions and is defined individually by each TSG for the techniques described
taking into account the tumour biology, local (CCO) generic immobilisation
techniques and planning tolerances.
(see appendix – immobilisation techniques and treatment setup variations).
Dose and fractionation
This is in accordance with Royal College of Radiologists Guidance on Radiotherapy
Dose-Fractionation June 2006. Each protocol should conform to the current RCR
Grade A recommendations. Lower grade recommendations may be included at local
discretion of the network.
Critical Structure Tolerance & Acute/Late effects
This is approved by the CCO tumour groups and as defined in peer reviewed clinical
trials
(see appendices – ‘Critical Structure Tolerances’ and ‘Acute/Late Effects definition’).
Issue Date: 08-July-2010 Page 2 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
References
References are included where they are available. A comment is made on the level of
evidence for dose fractionation regimes as defined by RCR guidelines.
The document is also intended to better define those treatments that we at CCO
consider to be ‘standard protocol’ as opposed to ‘non-protocol’. Non-protocol
treatments include those cases where a technique is used to address a “one-off”
clinical need. In this situation a concession is required for treatment subject to its
clinical justification. They also include those techniques that are still under
development and are undergoing a planned assessment/implementation. These are
listed in the development project framework and referenced separately as appendices.
The final decision regarding the clinical use of a technique either under concession or
as part of a development project rests with the Clinical Director for Radiotherapy.
The protocol book will initially be available in paper form, dated ‘2010’. It can be
accessed electronically via the ISO9000 directory, CCOCOMMS or the Intranet. It is
intended to improve the electronic accessibility of individual protocols encouraging
their use as a valuable reference. The protocols are approved annually by the
appropriate Tumour Specific Group and when only available electronically, it will be
possible to update protocols more frequently in response to changes in our knowledge
base. It is intended that the electronic version of the protocols will replace the paper
version by 2011. The format and lay out of the index has been chosen to facilitate this
transition.
Issue Date: 08-July-2010 Page 3 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Contents
Breast
Breast + SCF/Chest Wall + SCF (+/- Axilla)............................................... 6
Breast Boost................................................................................................. 8
Breast/Chest Wall Only................................................................................ 9
Breast/Chest Wall and Axilla (modified monobloc).................................... 10
CNS
Acoustic Neuroma........................................................................................ 11
Brain Metastases (Isolated).......................................................................... 12
Brain Metastases (Multiple)......................................................................... 13
Ependymoma................................................................................................ 14
Glioma (High Grade)................................................................................... 15
Glioma (Low Grade)................................................................................... 16
Malignant Spinal Cord Compression........................................................... 17
Meningioma.................................................................................................. 18
Optic Nerve Glioma – Under Development – Requires Concession .......... 19
Orbital Tumours........................................................................................... 20
Pituitary........................................................................................................ 21
Primary CNS Lymphoma............................................................................. 22
Gastrointestinal
Anal Canal/Anal Margin............................................................................... 23
Oesophagus - Palliative................................................................................. 25
Oesophagus – Radical................................................................................... 26
Pancreas – Under Development – Requires Concession.............................. 28
Rectum.......................................................................................................... 29
Stomach......................................................................................................... 31
Gastrourinary
Bladder.......................................................................................................... 32
Penis............................................................................................................. 33
Prostate......................................................................................................... 34
Testicular...................................................................................................... 38
Gynaecological
Cervix............................................................................................................ 39
Endometrium................................................................................................ 40
Ovary............................................................................................................ 41
Vagina........................................................................................................... 42
Vulva............................................................................................................. 43
Head and Neck
Cervical Oesophagus.................................................................................... 45
Head and Neck Cancer General................................................................... 46
Larynx Glottic Larynx.................................................................................. 47
Sub-Glottic Larynx............................................................... 49
Supragottic............................................................................ 51
Lower Alveolus............................................................................................ 53
Issue Date: 08-July-2010 Page 4 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Maxillary Sinus/Nasal Cavity...................................................................... 55
Nasopharynx................................................................................................ 56
Oropharynx Base of Tongue.................................................................... 58
Buccal Mucosa..................................................................... 59
Floor of Mouth.................................................................... 61
Oral Tongue......................................................................... 62
Parotid Gland............................................................................................... 63
Pyriform Fossa............................................................................................ 64
Retromolar Trigone..................................................................................... 65
Soft Palate................................................................................................... 66
Thyroid....................................................................................................... 68
Tonsil.......................................................................................................... 69
Lung
Mesothelioma............................................................................................. 71
Non-Small Cell Lung.................................................................................. 72
Small Cell Lung.......................................................................................... 74
Lymphoma
Hodgkins..................................................................................................... 75
Non-Hodgkins............................................................................................. 76
Spleen.......................................................................................................... 78
Paediatric............................................................................................................... 79
Skin
Melanoma.................................................................................................... 80
Merkell Cell................................................................................................. 81
Non-Melanoma............................................................................................ 82
Other
Bone Metastases......................................................................................... 83
Soft Tissue Sarcoma.................................................................................... 84
Total Body Irradiation................................................................................ 85
Appendices – Available on CCO intranet
Appendix A – Treatments using IMRT ................................................................. 86
Issue Date: 08-July-2010 Page 5 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group : Breast
Site: Breast + SCF or Chest Wall + SCF (+/- axilla)
Tumour: Invasive primary breast cancer
Intent: Radical RCR Category status: 2
1. Localisation method CT Sim (Brilliance/AcQSim) 5mm slices
Simulator using surface anatomy, position of scar, clips, operation notes
and mammographic findings to localise tumour bed - simple single plane,
with external contour of the central slice of the PTV taken using Osiris.
Wire to scar. Radio-opaque markers placed on lateral and medial ref points
2. Planning technique Simulator - isocentric, coplanar tangentials matched to a single anterior
field at fixed FSD to cover the SCF and axilla as appropriate.
CTSim – single isocentre backedge aligned tangentials matched to an
anterior nodal field using asymmetric jaws. PAB as needed.
3. Immobilisation QUEST board with patient position as per TWR3FISO. Chinstrap.
method
4. Volume definition and CTV = whole of breast tissue (or skin flaps from 5mm below skin surface
if post mastectomy) and including soft tissues down to deep fascia (but not
including underlying muscle and ribcage), and SCF +/- axilla
PTV=CTV+1cm
The field borders for the tangential fields are as follows:
Medial – the midline.
Lateral – 1cm below the breast plate or to the mid-axillary line.
Superiorly – the second intercostal space at the level of the Angle of Louis.
Inferiorly – to 1-2cm below the inferior extent of breast tissue – estimated
extent if post mastectomy.
The field borders for the anterior axilla and SCF field are as follows:
Medial – ipsilateral edge of the vertebral bodies
Lateral – lateral extent of the second rib
Lateral if axilla included – insertion of the Teres major into the humerus
Superior – at least 3cm above the head of the clavicle (ie to cover the SCF).
Inferior – matched to the tangential fields.
A posterior axillary field may occasionally be required for larger axillary
separations. This must be planned on an individual patient basis.
Critical structures Heart-distance of post edge of field to ant border of heart to be < 1.5cm.
Lungs- central lung distance for tangential fields not normally >2cm.
Hot spots > than 105% should be avoided in the skin and ribcage.
Issue Date: 08-July-2010 Page 6 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and 40Gy in 15 daily fractions (Grade B)
Fractionation 50Gy in 25 daily fractions (Grade B)
45Gy in 20 daily fractions
6. Special instructions Attendance at Breast Care Class as per CCO Breast Care Class Standard
Referral to Breast Clinical Nurse Specialist Service at CCO in accordance
with CReST referral criteria
Provide patient with ‘Radiotherapy to the Breast’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 13/04/2010
Issue Date: 08-July-2010 Page 7 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Site: Tumour bed boost
Tumour: Primary invasive breast cancer
Intent: Radical RCR Category status: 2
1. Localisation method CT planned if Oncoplastic surgery. Clipping of tumour bed is encouraged.
The relation of scar to tumour bed should be ascertained from operation
notes, discussion with the operating surgeon and clinical examination.
CT scan - for incisions where scar does not overlie tumour bed. 5mm slices
and wire to scar. The (clipped) tumour bed including seroma if present, is
identified and outlined.
Mark up on set, if confirmed that scar overlies the tumour bed.
2. Planning technique For incisions where the scar does not overlie the tumour bed, planned
photon boost. Normally 3 field requiring 3D dataset. If depth is satisfactory
for an electron boost, moves from origin to tumour bed may be ascertained
from the scan on Prosoma, and an electron field can be marked directly,
using this information in the simulator. Note CT planning should be
employed for ph1 and ph2 for patients who have oncoplastic incisions who
will require identification of the tumour bed for a boost.
Direct single electron field, centred on scar where scar overlies tumour bed.
3. Immobilisation For patients receiving photon boost, position is as ph1 (see TWR2FISO)
method For electron boost, supine position on couch with abduction of ipsilateral
arm. Lateral tumours are best treated with patient rolled slightly to the side.
4. Volume definition and For photon boosts: CTV=the volume enclosed by surgical clips+ changes in
surrounding tissue architecture. The PTV=CTV+ 10mm (this margin may
be increased if close surgical margins or extensive DCIS)
For electron boosts, the treatment field normally consists of the tissue
defect from the surgery and the scar with an adequate margin. The whole
length of the scar does not always require inclusion in the boost field.
Critical structures Lungs, heart, skin.
5. Dose and 15Gy in 5 daily fractions, 16Gy in 8 daily fractions
Fractionation 10Gy in 5 daily fractions
9Gy in 3 daily fractions
6. Special instructions Digital photograph to record field for electron mark up.
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 13/04/2010
Issue Date: 08-July-2010 Page 8 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Breast
Site: Breast or Chest Wall only Tumour: DCIS, invasive primary breast cancer
Intent: Radical RCR Category status: 2
1. Localisation method CT Sim (Brilliance/AcQSim) 5mm slices
Simulator using surface anatomy, position of scar, clips, operation notes
and mammographic findings to localise tumour bed - simple single plane,
with external contour of the central slice of the PTV taken using Osiris.
Wire to scar. Radio-opaque markers on lateral and medial reference points
2. Planning technique Isocentric, coplanar backedge aligned tangentials.
3. Immobilisation QUEST board with patient position as per TWR2FISO.
method
4. Volume definition and CTV = the whole of the breast tissue (or the skin flaps from 5mm below the
skin surface if post mastectomy) and including the soft tissues down to the
deep fascia but not including the underlying muscle and ribcage.
PTV=CTV+1cm
The field borders are as follows:
Medial – the midline.
Lateral – 1cm below the breast plate or to the mid-axillary line.
Superiorly – the second intercostal space at the level of the Angle of Louis.
Inferiorly – to 1-2cm below inferior extent of breast tissue – estimated
extent if post mastectomy.
Critical structures Heart-distance of post edge of field to ant border of heart to be < 1.5cm.
Lungs-central lung distance for tangential fields not normally >2cm.
Hot spots of >105% should be avoided in the skin and ribcage
5. Dose and 40Gy in 15 daily fractions (Grade B) 50Gy in 25 daily fractions (Grade B)
Fractionation 45Gy in 20 daily fractions
6. Special instructions Attendance at Breast Care Class as per CCO Breast Care Class Standard
Referral to Breast Clinical Nurse Specialist Service at CCO in accordance
with CReST referral criteria
Provide patient with ‘Radiotherapy to the Breast’ information leaflet
7. Clinical Trials and Breast Only: IMPORT LOW/ IMPORT HIGH/ PRIME
References Chest Wall Only: SUPREMO
Date of approval by Lead Clinician/TSG: 13/04/2010
Issue Date: 08-July-2010 Page 9 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Breast
Site: Breast/chest wall and axilla (modified monobloc) Tumour: Invasive primary breast cancer
Intent: Radical RCR Category status: 2
1. Localisation method CT Sim (Brilliance/AcQSim) 5mm slices
Wire to scar. Radio-opaque markers placed on medial and lateral ref points
2. Planning technique Isocentric, coplanar modified, extended tangentials.
3. Immobilisation Stable, supine position on QUEST board. Head straight, ipsilateral
method shoulder/arm extended superiorly to exclude all or as much as possible of
the humeral head from the field elbow flexed a little and rotated backwards.
Chinstrap.
4. Volume definition and CTV = whole of breast tissue (or skin flaps from 5mm below skin surface if
post mastectomy) and including soft tissues down to deep fascia (but not
including underlying muscle and ribcage), and the contents of the axilla.
PTV=CTV+1cm
The field borders are as follows:
Medial – the midline (or a little beyond) allowing coverage of breast tissue
inferiorly, after appropriate THR to ensure optimum axillary coverage.
Lateral – mid-axillary line (or slightly post to mid-axillary line) to ensure
all breast tissue encompassed and field border is behind clavicle or
covering axillary contents.
Superiorly – ~ ⅔ of clavicle included, covering level 3 axillary nodes.
Inferiorly – to 1-2cm below the inferior extent of breast tissue.
Heart-distance of post edge of field to ant border of heart to be < 1.5cm.
Critical structures Lungs- central lung distance for tangential fields should not normally
exceed 2.5cm, maximum acceptable in exceptional cases, 3cm.
Hot spots of greater than 105% should be avoided in the skin and ribcage
5. Dose and 45Gy in 20 daily fractions (Grade C)
Fractionation
6. Special instructions Attendance at Breast Care Class as per CCO Breast Care Class Standard
Referral to Breast Clinical Nurse Specialist Service at CCO in accordance
with CReST referral criteria
Provide patient with ‘Radiotherapy to the Breast’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 13/04/2010
Issue Date: 08-July-2010 Page 10 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: ACOUSTIC NEUROMA
Intent: Radical RCR Category Status: 2
1. Localisation method CT/MRI and image registration
2. Planning technique Single plane
Scan using 2mm SRS protocol – co registered with MRI
3. Immobilisation Stereotactic Radiosurgery
method Leibinger frame (fixed)
Stereotactic Conformal Radiotherapy
Radionics frame (tumour ≤ 3cm)
Headfix frame (tumour > 3cm)
Shell if relocatable frame not possible
4. Volume definition and Stereotactic Radiosurgery
CTV = GTV – visible tumour
PTV – visible tumour + 1mm (but not extending into brain stem)
Stereotactic Conformal Radiotherapy
GTV – gross tumour
CTV = GTV
Critical structures Brain stem
5. Dose and Stereotactic Radiosurgery
Fractionation 12.5 Gy / 1# (at 80%)
Stereotactic Conformal Radiotherapy
54Gy / 30# / 6weeks
6. Special instructions
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 11 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: BRAIN METASTASES – Isolated 1-3 (consider Stereotactic Radiosurgery or boost post
whole brain radiotherapy)
Intent: Palliative RCR Category status: 3
1. Localisation Method Stereotactic Radiosurgery (SRS) is suitable for single or limited number
of metastases each ≤3cm max diameter when surgery is not appropriate and
systemic disease controlled or potentially controlled.
2. Planning Technique Planning MRI with image registration
SRS – MRI – co-registration or CT plans
3. Immobilisation Radionics frame (relocatable) and treat on Varian linac
Method
4. Volume Definition and SRS – GTV = enhancing lesion
CTV = GTV
PTV = CTV + 2mm
Critical Structures Brain stem, optic chiasm and nerves, cochlear
5. Dose and SRS – 15/17.5Gy / 1#
Fractionation
6. Special Instructions Steroid – Dex cover, overnight stay post.
Follow up 4/52 post radiotherapy then 3/12 and 6/12.
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 12 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: BRAIN METASTASES – Multiple – Whole Brain Radiotherapy (WBRT)
Intent: Palliative RCR Category status: 3
1. Localisation Method WBRT – Orfit cast – simulator planning same technique for
NB. Prophylactic Cranial Irradiation (PCI) – see small cell lung cancer
2. Planning Technique Simulator planning. Parallel opposed pair (Reids line avoiding eyes)
3. Immobilisation WBRT – Orfit shell – treat on Cobalt or low energy Linac
Method
4. Volume Definition and GTV = Whole cranium, inferior border Reids line = 50% of iso dose
Critical Structures Eyes
5. Dose and WBRT
Fractionation 1. Uncontrolled peripheral disease and multiple mets – 20Gy / 5# / 5days
(Grade A)
1a. Major co-morbidities – 12Gy / 2# / 1week (Grade B)
2. Controlled peripheral disease (prognosis >6/12 – 30Gy / 10# / 2weeks)
or if considering SRS and post excision of sol met.
6. Special Instructions Consider Dexamethasane
TLD eyes
In very palliative cases avoid eyebrows
7. Clinical Trials and None at present.
References Royal College of Radiologists (RCR) – Dose-Fractionation 2006
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 13 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: EPENDYMOMA
Intent: Radical RCR Category status: 2
Ependymomas in childhood are treated as per UKCCCR protocols.
Ependymomas in adults are treated as follows:
1. Localisation method AcQSIM + MR fusion.
Whole CNS is incorporated for disseminated and stage III and infratentorial
disease.
2. Planning technique Planned non-coplanar fields, Spinal fields, Supine – please refer to whole
CNS protocol (TWJSPCNS)
3. Immobilisation Treatment shell
method
4. Volume definition and For stages I-IV supratentorial
critical structures GTV = tumour
PTV = GTV + 2cm margin
For disseminated and stage III and infratentorial
Whole CNS
5. Dose and Local RT: 54-60Gy / 30# / 6weeks
Fractionation Whole CNS: Phase 1 – 35Gy / 21# / 3.5weeks
Phase 2 – Posterior fossa boost – 20Gy / 12# / 2.5weeks
6. Special Instructions
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 14 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: GLIOMA (ASTROCYTOMA & OLIGODENDROGLIOMA)
HIGH GRADE III OR IV AS PER CENTRIC
Intent: Radical or Palliative RCR Category status: 1 / 2 / 3
1. Localisation Method Radical: CT Plan (+ MR co-reg if not well seen on prior CT scan).
Planned fields.
Palliative: Poor prognosis + RPA status. Suitable for Cobalt + orfit
fixation. CT planned as per brain metastasis.
2. Planning Technique Planned fields
Poor prognosis – lateral opposed fields
3. Immobilisation Perspex shell or Orfit cast
Method
4. Volume Definition High grade – Radical (Pre-op Bx only)
Single phase - GTV = enhancing lesion post resection. Surgical tumour bed
plus any residual enhancing tumour on planning scan.
CTV = Margin 2-3cms can be reduced in anatomical boundaries where
spread unlikely eg bone. Post-op image important to take into account any
shift of tumour bed post-op.
PTV = CTV + 0.5cm
Eyes/lens/lac glands, optic nerves and chiasm, pituitary, brain stem and
Critical Structures
cochlear.
5. Dose and 60Gy / 30#
Fractionation Retreat (limited volume after extended duration of survival) 50Gy / 30#
Over 70yrs – 45Gy / 20# / 4weeks
In older patients with poor prognosis – 40Gy / 15# / 3weeks or 30Gy / 10# /
2weeks
6. Special Instructions Concurrent Temodol for Grade IV, PS 0 + 1.
Provide ‘Radiotherapy to the Brain’ information leaflet.
Follow up – Post RT with MRI and repeat 6/12 with scan.
7. Clinical Trials and Centric (Stupp 2004)
References Avaglio
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 15 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: GLIOMA (ASTROCYTOMA & OLIGODENDROGLIOMA)
LOW GRADE I OR II – ASTRO (A), OLIGO (O) AND MIXED (OA)
Intent: Radical or Palliative RCR Category status: 1 / 2 / 3
1. Localisation Method CT + MRI fusion
(T2) + series
2. Planning Technique Planned non-coplanar fields
3. Immobilisation Perspex shell or Orfit cast
Method
4. Volume Definition Low Grade as per BR13 study
GTV = High signal intensity on T2 sequence or FLAIR corresponding to
hypodense area on CT image including any enhancement on CT.
In post-op essential to use post-op images.
CTV = GTV – 1.5-2cm – across midline only when midline structure eg
corpus collosum is invaded. 5mm sufficient in anatomical boundaries eg
tentoria and meningies.
PTV = 0.5-0.7mm – for treatment uncertainties
Critical Structures
Brain stem – contralateral >50-60% of total dose
Eyes/ lens - >5Gy, retina <40Gy, pituitary gland, ear,
optic chasm/nerves/brain stem – No >107% of 55gy
5. Dose and 50.4Gy / 28# / 5½ weeks
Fractionation 54Gy / 30# - poor prognosis eg enhancement imaging - indicates “high”
grade
6. Special Instructions Provide ‘Radiotherapy to the Brain’ information leaflet.
7. Clinical Trials and BR13 - closed
References
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 16 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: MALIGNANT SPINAL CORD COMPRESSION
Intent: Palliative RCR Category status: 1
1. Localisation method Simulator planning based on recent MRI (or CT if contraindicated)
2. Planning technique Single posterior field (under couch) or lateral fields possible for cervical
cord
Occasionally ant/post if bulky anterior disease
Including one vertebra either side of MRI (or good quality CT) abnormality
8 to 9cm wide (cervical-lumbar) with extension to cover lateral disease
Prescribe at 5-8cm depending on particular level of cord (cervical-lumbar)
– measured on MRI/CT.
3. Immobilisation Simple immobilisation
method Mattress used for comfort
4. Volume definition and
critical structures
5. Dose and Good prognosis, i.e. patients presenting with good performance status:
Fractionation either ambulant or with only a short history (< 24 hours) of immobility
20Gy / 5# / 5days (RCR Grade C )
30Gy / 10# / 2weeks (RCR Grade C)
Poor Prognosis, i.e. patients expected to live < 6 months and who have a
poor chance of neurological recovery. In practice this group includes those
with established paraplegia for more than 24 hours. Main aim of treatment
is relief of pain
8Gy / 1# (RCR Grade C)
6. Special Instructions Nurse flat until after ½ of treatment
Dexamethasone 16mg daily initially, reduce over 5-7 days then stop (NICE
clinical guidance 75, Nov 2008)
7. Available trials SCORAD
Date of approval by Lead Clinician/TSG: 23/04/2010
Issue Date: 08-July-2010 Page 17 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: MENINGIOMA
Intent: Radical RCR Category status: 2
1. Localisation method Stereotactic frame or shell
MRI and image registration
2. Planning technique Single phase avoiding critical structures if possible
3. Immobilisation Stereotactic frame (Radionics or Headfix) or shell depending on intended
method treatment volume and patient’s dental condition.
4. Volume definition and GTV = tumour
PTV = GTV + clinical and setup margin
Please refer to volume definitions appendix
Critical structures Eyes, optic nerves and chiasm, pituitary, brain stem
5. Dose and Benign - 54Gy / 30# / 6weeks
Fractionation Atypical/Malignant (Grade II or III) - 60Gy / 30# / 6weeks (if optic
nerve/chiasm not involved)
6. Special instructions TLD eyes if beam is near eyes
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 18 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: OPTIC NERVE GLIOMA – UNDER DEVELOPMENT – REQUIRES CONCESSION
Intent: Radical or Palliative RCR Category status: 1 / 2 / 3
1. Localisation method
2. Planning technique
3. Immobilisation
method
4. Volume definition and
critical Structures
5. Dose and
Fractionation
6. Special instructions
7. Clinical Trials and
References
Date of approval by Lead Clinician/TSG: XX/XX/XXXX
Issue Date: 08-July-2010 Page 19 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: ORBITAL TUMOURS – Exopthalmosis (bilateral treatment)
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation Method CT simulator scan
2. Planning Technique CT Planning
Parallel opposed field with central blocking to avoid lens
3. Immobilisation Perspex shell
Method
4. Volume Definition and Field size 4 – 4.5cm x 8 or 9cm
Critical Structures Central axis is clearly defined line posterior to lens.
5. Dose and 20Gy / 10# / 2weeks
Fractionation
6. Special Instructions TLD eyes
7. Clinical Trials and NB. Other orbital tumours eg uveal melanoma – consider protons
References
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 20 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: PITUITARY
Intent: Radical RCR Category status: 2
1. Localisation method MRI + CT plan image registration
2. Planning technique Conformal
3 field isocentric technique – 2 laterals and a superior field
3. Immobilisation Headfix stereotactic frame (or shell if not dentate)
method
4. Volume definition and GTV = tumour
PTV = GTV + clinical and setup margin
Please refer to volume definitions appendix
Critical structures Optic nerve, optic chiasm
5. Dose and 45Gy / 25# / 5weeks (Grade C)
Fractionation
6. Special instructions Provide ‘Radiotherapy to Brain’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 21 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: CNS
Tumour: PRIMARY CNS LYMPHOMA
Intent: Radical RCR Category status: 2
1. Localisation method Simulate and scan according to TWJSPCNS
2. Planning technique Lateral opposed fields to ‘Helmet’ only
Whole CNS if positive cytology or spinal disease
3. Immobilisation Perspex shell, supine as per TWJSPCNS
method
4. Volume definition and Helmet – whole head down to C2 (optional phase II boost if primary seen
Critical Structures to be localised)
Whole CNS standard technique as per TWJSPCNS
5. Dose and Phase I (helmet) – 45Gy / 25# / 5weeks
Fractionation Phase II (primary lesion + 20mm margin) – 9Gy / 5# / 1week
Whole CNS – 35Gy / 21#
Posterior fossa boost – 20Gy / 12# / 2.5weeks
6. Special Instructions See also specialist planning technique instructions
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 22 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: ANAL CANAL/ANAL MARGIN
Intent: Radical RCR Category status: 2 or 3
1. Localisation method CT SIM or SIM and Virtually simulated
Palpable nodal masses and margin tumours marked with wire
2. Planning technique All prone if possible with full bladder
1) Small tumours grade I or 2/T1N0M0/T2 <3cm N0M0
3 Field (post + 2 laterals)
2) Standard treatment all grades (T2 >3cm / T3-T4N0M0/ grade 3 T1)
2 phases – I – ant and post – large parallel opposed fields
II – 3 fields – post + 2 laterals or ant post to cover nodes
3. Immobilisation Usually prone unless unstable or unable to lie prone. Allows position of
method bolus (wax)
Supine if nodal boost required.
4. Volume definition and 1. Small tumours (grade I – 2/ T1N0M0 / T2 <3cm N0M0)
critical structures GTV = All macroscopic disease
CTV = GTV + 2.5cm margin
PTV = CTV + 5mm margin
2. Standard treatment
Here field borders are indicated as defined in ACT II protocol, this
incoporates GTV, CTV + PTV Phase I and II.
For Phase II PTV represents 3cms expansion on GTV.
Issue Date: 08-July-2010 Page 23 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and 1. Small tumours : 45 / 20# / 2weeks – as ACT I
Fractionation plus iridium boost (15-20Gy in patients with persistent
disease at EUA – 4 - 6 weeks)
or 50Gy / 20# if no boost appropriate
2. Standard : I – 30.6Gy / 17# / 23days
II – 19.8Gy / 11# / 15days
NB. If large fields need to be avoided for phase II – consider electron
boost to nodes and 3 field plan to primary.
1. Palliative patients :
In frail patients who cannot tolerate chemotherapy a single phase I planned
treatment (see above) is possible either parallel opposed pair or 3 field plan
depending on bulk of disease.
2. SPLIT course
Some frail patients benefit from an unfashionable SPLIT course.
Vancouver Technique (Ref). Planning as ACT II for Phase I and II.
Dose fractionation: Phase I – POP – 26Gy / 13# / 17days, 5FU/mito week 1
If tolerates well can proceed to Phase II and convert no radical after 3½
weeks: Phase II – 3 field 24Gy / 12# / 16days, 5FU/mito week 1.
6. Special Instructions
7. Clinical Trials and None at present.
References ACT I, ACT II, Vancouver Technique – B. Cummings
Date of approval by Lead Clinician/TSG: 09/06/2010
Issue Date: 08-July-2010 Page 24 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: OESOPHAGEAL CARCINOMA
Intent: Palliative RCR Category status: 3
1. Localisation method Combination of:
Barium swallow (caution if risk of aspiration)
Position of stent
Diagnostic CT + OGD report (PET if available)
2. Planning technique Simple palliation – conventional simulator planning – POP AP pair
Complex palliation may be planned as per radical treatment*
3. Immobilisation Stable supine, arms by side
method
4. Volume definition GTV = gross primary disease / area of bulk disease causing symptoms
CTV = GTV + 1cm in all directions at discretion of clinician to take
account of total volume + condition of patient
PTV = CTV + 1cm
Critical structures Lungs, Spinal cord, Kidneys
5. Dose and 40Gy / 15# / 3weeks if small tumour and minimal metastases*
Fractionation 30Gy / 10# / 2weeks (Grade D)
20Gy / 5# / 1weeks (Grade D)
Brachytherapy alone – 10Gy to 1cm (Grade B) – good for haemostasis
6. Special Instructions 2x weekly weight
Dietician referral
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 25 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: OESOPHAGEAL CARCINOMA
Intent: Radical (FIT PATIENTS) RCR Category status: 1
1. Localisation method Combination of:
Barium swallow (caution if risk of aspiration)
Stent position
Diagnostic CT
OGD report and PET images or MRI
2. Planning technique CT/Sim – 3D CT Planning
Consider IV contrast to delineate pulmonary artery
3. Immobilisation Stable supine position. Usually on QUEST board with arms up. Indexed
method knee and foot supports
4. Volume definition and GTV = gross primary + nodal disease – defined on planning CT
incorporating information from CT, PET, MRI, OGD, EUS and Barium
CTV = GTV + margin of up to 1cm radially (modified posteriorly where
closer than 1.3cm) and 2cm sup/inf – along the line of the oesophagus.
For tumours within 2cm of OGJ the CTV extends 2cm but includes mucosa
of stomach in direction of nodal stations on the lesser curve.
PTV = Radical PTV = CTV + 5mm
Critical Structures = Sup/inf PTV = CTV + 10mm
Lungs – V20, Spinal cord <80% (40Gy) , Kidneys, heart v80% (v40Gy)
<30% - see SCOPE I trial
5. Dose and Primary chemoradiotherapy – As per SCOPE I trial
Fractionation 50Gy / 25# / 5weeks – with neoadjuvant and concurrent Cisplatin +
Capecitabine or 5FU (Grade B)
MODIFIED RADICAL – For small localised tumours in elderly or frail
patients unfit for true radical treatment or chemotherapy – 40Gy / 15# /
3weeks – boost to compensate for lack of chemo with HDR brachy boost
(10Gy to 1cm from central axis) within 7 days of XRT.
Some poor performance status patients but with good cardiac and renal
function may be considered for 40Gy / 15# / 3weeks + 1 cycle concurrent
Cisplatin/5FU in week 1. Ref: Walsh.
6. Special Instructions 2x weekly weight
and Dietician referral
Provide ‘Radiotherapy to the Oesophagus’ information leaflet
Follow-up 4/52; 3/12 for 1year then 6/12 for 5years.
Issue Date: 08-July-2010 Page 26 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
7. Clinical Trials and SCOPE 1
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 27 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: PANCREAS – UNDER DEVELOPMENT – REQUIRES CONCESSION
Intent: Radical or Palliative RCR Category status: 2 or 3
1. Localisation method
2. Planning technique
3. Immobilisation
method
4. Volume definition and
Critical structures
5. Dose and Radical: 50Gy/25#
Fractionation Palliative: 30Gy/10#
6. Special instructions
7. Clinical Trials and See ESPAC5
References
Date of approval by Lead Clinician/TSG: XX/XX/XXXX
Issue Date: 08-July-2010 Page 28 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: RECTUM
Intent: Radical or Palliative RCR Category status: 2 or 3
1. Localisation method CT, use of oral contrast for post-op or risk of adhesions unless specific
contraindications, comfortably full bladder
2. Planning technique 3 field technique
3. Immobilisation Prone position if possible. Belly board in selected patients to minimize
method small bowel toxicity, ankle stocks (if appropriate shape)
4. Volume definition Preoperative
All radical patients should be CT planned or virtually simulated. The
Clinical target volume should include the gross tumour, the mesorectum,
presacral space and internal iliac lymph nodes. A 1cm margin is added to
the CTV to obtain the PTV. ¹
Post Operative: The Clinical target volume should include tumour bed,
presacral, internal iliac lymph nodes and inferior pelvic space for low rectal
cancers. NB. Pre-op oral barium required to delineate small bowel. Wire
on perineal scar.
Critical Structures Small bowel (v15< 120cc if small bowel outlined)²
Issue Date: 08-July-2010 Page 29 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and Short course preoperative radiotherapy:
Fractionation 25Gy/ 5# / 1week (Grade A) - Surgery should take place within 7 days of
short course pre-op radiotherapy, should be treated Mon-Fri.
Long course preoperative radiotherapy:
45Gy/25#/5 weeks (Grade A) with concurrent chemotherapy +/- boost
For late T3 and T4 tumours and for patients with pelvic side wall lymph
nodes, a smaller volume external beam boost or brachytherapy boost
should be considered. Patients with circumferential tumours are not suitable
for brachytherapy boost.³
5.4-9Gy/3-5#/3-5 days (RCR Grade A) – boost must exclude small
bowel or
HDR brachytherapy 10Gy @ 10mm from surface
Postoperative radiotherapy:
45Gy/25#/5wks (RCR Grade B) +/- boost 5.4-9 Gy/3-5#/3-5 days – boost
must exclude small bowel
10-15Gy to gross macroscopic disease or HDR as above
If unfit for chemotherapy, e.g. ischaemic heart disease, older patients
45Gy/20#/4wks
39Gy/13#/3wks +/- boost
Papillon 30-60Gy/1-2#/14days or HDR as above
Palliative Treatment
‘Radical’ Palliation: 45Gy/20#/4wks or 45Gy/25#/5weeks +/- chemo +/-
boost as above
Simple palliation 10Gy / 1#, 20Gy / 5# / 1week, 30Gy / 10 / 2weeks
6. Special Instructions Concurrent chemotherapy = 5Fu days 1-4 and 29-33 or oral Capecitabine
on the days of radiotherapy only
Comfortably full bladder for radical treatments
Provide ‘Radiotherapy to the Bowel’ information leaflet
7. Clinical Trials and None at present.
References 1. Myerson et al. A radiation therapy oncology group consensus panel
contouring atlas IJROBP Vol. 74 (3) 824-830; Roels et al. Definition and
delineation of the clinical target volume for rectal cancer IJROBP Vol. 65
(4) 1129-1142
2. QUANTEC. Kavanagh et al. Radiation dose–volume effects in the
stomach and small bowel. IJROBP Vol. 76 (3) S101-107
3. German study- pre op vs. post op, 50.4Gy/28# vs. 50.4Gy/28# plus
5.4Gy/3# respectively; Sauer et al. Preoperative versus Postoperative
Chemoradiotherapy for Rectal Cancer. NEJM 2004 Vol. 351: 1731-40
Date of approval by Lead Clinician/TSG: Awaiting final TSG approval
Issue Date: 08-July-2010 Page 30 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gastrointestinal
Tumour: STOMACH – REQUIRES CONCESSION FOR RADICAL
Intent: Radical or Palliative RCR Category status: 2 or 3
Adjuvant postoperative radiotherapy or chemo-radiotherapy is only recommended for high risk
patients with a clear margin of resection. The treatment can be very toxic and requires a patient
with good performance status and intensive support during and after treatment
Palliative treatment can be useful in selected cases
1. Localisation method Empty stomach
2. Planning technique Palliative - Parallel opposed pair
Radical - Conformal
3. Immobilisation Knee support and ankle stocks
method
4. Volume definition and
Critical structures
5. Dose and Palliative: 30Gy / 10# / 2weeks or 20Gy / 5# / 1week
Fractionation
6. Special instructions Post-op: please refer to MacDonald et al technique, NEJM
7. Clinical Trials and MacDonald et al, N Engl J Med. 2002 Jan 17;346(3):210-1.
References
Date of approval by Lead Clinician/TSG: 07/07/2010
Issue Date: 08-July-2010 Page 31 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Genitourinary
Tumour: BLADDER
Intent: Radical and Palliative RCR Category status: TCC 1, other radical 2, palliative 3
1. Localisation method CT scan, image fusion for patients with hip replacement
Empty bladder
2. Planning technique Conformal
3. Immobilisation Supine position, knee and foot supports
method
4. Volume definition and GTV=whole bladder. Margin to PTV=1.5cm. 2 cm margin for a sup tumour
include prostatic urethra in men, particularly for inferior tumours
treat with a phase I (whole bladder) and phase II (10-14 Gy, partial
bladder volume) in small localized tumours, in patients with a large
residual volume or diverticulum
for patients with large residual volume consider indwelling catheter or
treatment of small volume throughout
pelvic lymph nodes are not routinely treated (for exception see
protocol)
Critical structures Small bowel and rectum. Use dose volume constraints as for prostate if
problematic
5. Dose and Radical: 64Gy / 32#s / 6wks or 55Gy/20#/4wks (Grade B)
Fractionation Palliative: 21Gy / 3# /1 wk (Grade A)
30-36 Gy / 6# / 6 wks, 30-35Gy/10-15#, 10 Gy single #
6. Special instructions Empty bladder, weekly FBC, U+E
Concurrent chemo Cisplatin
Provide ‘Radiotherapy to the Bladder’ leaflet
Cystoscopy 2-4 months after completion of radical radiotherapy
7. Clinical Trials and NCRN SPARE (closed)
References
Date of approval by Lead Clinician/TSG: 27/04/2010
Issue Date: 08-July-2010 Page 32 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Genitourinary
Tumour: PENIS
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation Method Clinical examination of patient by consultant.
2. Planning Technique Laterally opposed fields, 100SSD with wax block and wax plug.
3. Immobilisation Wax block and wax plug encasing penis fastened to immobilise.
Method Supine.
4. Volume Definition and Clinically assessed dependent on tumour and patient anatomy.
Critical Structures Ensure penis is held away from the abdomen by wax collar in wax block.
5. Dose and 50-55Gy /20#/ 28days - midplane
Fractionation
6. Special Instructions Needs floor clinic review weeks 3 and 4.
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 33 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Genitourinary
Tumour: PROSTATE
Intent: Radical or palliative RCR Category status: 2 or 3
Referral Criteria: low risk group (PSA<10ng/ml and Gleason score≤6 and T1-T2a),
intermediate risk group (PSA10-20ng/ml or Gleason score 7 or T2b-c),
high risk group (PSA > 20ng/ml or Gleason ≥8ng/ml or T3-T4)
1. Localisation method CT, use MRI/CT image fusion for patients with unilateral or bilateral total
hip replacement
Use Relaxit and drinking protocol. If distended rectum at planning and no
gold seed markers give instructions for low residual diet and laxatives,
rescan after 1 week. No contrast.
2. Planning technique Standard/palliative dose: Conformal CT planned
Dose escalated: Forward or inverse planned IMRT if dose constraints not
reached
Prostate and Pelvic lymph nodes: Rapid Arc IMRT
Postoperative: conformal CT planned
3. Immobilisation Ankle stocks and knee support – supine position
method
Issue Date: 08-July-2010 Page 34 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
4. Volume definition and Dose escalation:
Low risk:
GTV1 = CTV1 = prostate
GTV2 = CTV2 = prostate and base of seminal vesicles
No Fiducial Markers Fiducial markers and daily IGRT
PTV1 CTV1 + 5mm CTV1 + 3mm
PTV2 CTV2 + 10mm CTV2 + 6mm
Moderate risk:
GTV1 = CTV1 = Prostate and base of Seminal Vesicles
GTV2 = CTV2 = Prostate and Seminal Vesicles
No Fiducial Markers Fiducial Markers and daily IGRT
PTV1 CTV1 + 5mm CTV1 + 3mm
PTV2 CTV2 + 10mm CTV2 + 6mm
High risk:
Consider Pelvic Lymph Node RT in fit patients; otherwise treat as per
moderate risk group.
GTV1 = CTV1 = Prostate and base of Seminal Vesicles
GTV2 = CTV2 = Prostate and Seminal Vesicles
GTV3 = CTV3 = Pelvic Lymph Nodes
PTV1 CTV1 +5mm
PTV2 CTV2 +10mm
PTV3 CTV3 +5mm
Low dose protocol:
GTV = CTV = Prostate and (base of) Seminal Vesicles
PTV CTV + 10mm
Postoperative:
GTV = CTV = Prostatic bed including ureteric resection, base of Bladder
and Seminal Vesicles
PTV CTV + 10mm
Critical structures Rectum: Outlined 10mm above and below PTV (Prostate and Seminal
Vesicles)
Small Bowel (if within 1cm of PTV): Outlined 10mm beyond any PTV
Bladder
Femoral Heads
Issue Date: 08-July-2010 Page 35 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
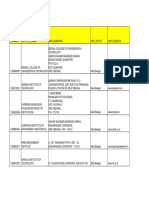
The Dose Constraints to Critical Structures are based on the CHHIP trial.
Rectum
Dose For % of total dose Relative max Volume (%)
74/37 72/32
50.3 47.6 68% 60%
60.0 56.7 81% 50%
65.1 61.6 88% 30%
70.3 66.5 95% 15%
74.0 72.0 100% 3%
Bladder
Dose For % of total dose Relative max Volume (%)
74/37 72/32
50.3 47.6 68% 60%
60.0 56.7 81% 25%
74.0 72.0 100% 5%
Small bowel
Dose For % of total dose Relative max Volume (%)
74/37 72/32
45.1 42.1 61% 78cc
50.3 47.6 68% 17cc
54.7 51.8 74% 14cc
60.0 56.7 81% 1cc
65.1 61.6 88% none
Femoral head
Dose For % of total dose Relative max Volume (%)
74/37 72/32
50.3 47.6 68% 50%
5. Dose and Dose escalation: All treatments are prescribed in 32 fractions.
Fractionation The PTV doses are as follows:
PTV1 = 72 Gy (min 68.4Gy, max 75.6Gy, median 72Gy)
PTV2 = 64 Gy (min 60.8 Gy, median 64Gy)
Where pelvic lymph nodes are included:
PTV3 = 50Gy (min 48Gy, median 50Gy)
Low dose protocol: 30-36 Gy in 6 fractions in 6 weeks or
64 Gy in 32 fractions in 6 weeks
Postoperative: 66 Gy in 33 fractions
6. Special instructions Provide patient with ‘Radiotherapy to the Prostate’ and ‘Patients receiving
radiotherapy to the prostate – preparation for planning and treatment’
information leaflets
Tamsulosin for obstructive bladder symptoms,
Issue Date: 08-July-2010 Page 36 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
7. Clinical Trials and NCRN CHHIP, RADICALS
References
Date of approval by Lead Clinician/TSG: 27/04/2010
Issue Date: 08-July-2010 Page 37 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Genitourinary
Tumour: TESTICULAR (seminoma)
Intent: Radical RCR Category status: 1 / 2 / 3
1. Localisation method CT scan and virtual simulation
2. Planning technique Parallel opposed pair
3. Immobilisation Supine, knee supports, ankle stocks
method
4. Volume definition and Stage I with no risk factors: para-aortic node from D10/11 to L5/S1
Critical structures Stage I with risk factors para-aortic and ipsilateral pelvic nodes : D10/11 to
ipsilateral groin
Stage II A/B or residual disease post chemo: define nodes on CT scan
5. Dose and Stage I with no risk factors for pelvic node disease
Fractionation POP 20Gy / 10# / 2weeks
Stage I and Stage IIA or IIB seminoma with risk of pelvic node disease
30Gy / 15# / 3weeks
6. Special instructions Radiotherapy as adjuvant treatment for stage I seminoma is only used if
there is a contraindication for adjuvant single agent carboplatin
7. Clinical Trials and None at present.
References
Comments Radiotherapy is an effective treatment modality for relapsed, chemo
resistant disease either with non seminomatous and seminoma histology.
Planning method, volume and dose needs to be individualised.
Date of approval by Lead Clinician/TSG: 27/04/2010
Issue Date: 08-July-2010 Page 38 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gynaecological
Tumour: CERVIX
Intent: Radical or Palliative RCR Category status: 1 or 3
1. Localisation method CT with contrast as appropriate. Full bladder
2. Planning technique Radical Planning
Conformal
Palliative Planning
Conformal or virtual simulation or simulator
3. Immobilisation Supine position, knee and foot supports, arms on chest
method
4. Volume definition and Outline gross tumour and enlarged nodes (GTV). Field should be at least to
Critical Structures L5 superiorly, in case of vaginal involvement 2-3cm below the lower extent
of disease. Lateral border 1cm beyond pelvic brim. Posterior border at
junction of S2 and S3 vertebrae or 2cm anterior to the most concave part of
anterior sacrum. Take into account MRI images to cover the sacrum if
necessary.
Upper border top of sacrum, lower border at bottom of Obturator foramen.
In case of vaginal involvement, 2cm-3cm below the lower extent of
disease.
5. Dose and 45Gy / 25# / 35days (Grade B)
Fractionation + Brachytherapy: HDR – 21Gy / 2# to point “A”
If bulky lymph nodes
Consider 50.4Gy / 28# / 38days (Grade B)
+ Brachytherapy: HDR – 21Gy / 3# to point “A”
+/- parametrial boost if disease extends to parametrium – 5.4Gy/ 3# / 3days
If brachytherapy not appropriate consider a small volume EBRT boost as
phase 2, dose 14.4-16Gy / 8#
For patients with locally advanced disease concomitant platinum based
chemotherapy is recommended (Grade A).
Palliative
20Gy / 5# / 7days or 30Gy / 10# / 14days
8-10Gy / 1# - this can be repeated if necessary
6. Special Instructions Provide ‘Radiotherapy to the female pelvis’ information leaflet
Gynae CNS support and use of vaginal dilators
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 20/05/2010
Issue Date: 08-July-2010 Page 39 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gynaecological
Tumour: ENDOMETRIUM
Intent: Adjuvant or Palliative RCR Category status: 2 or 3
1. Localisation method Adjuvant: CT for field definition for virtual simulation
Palliative: simulator for AP POP
2. Planning technique Virtual simulation – 3 or 4 fields to pelvis. Or AP POP
3. Immobilisation Supine with knee and foot supports. Arms on chest, comfortably full
method bladder.
4. Volume definition and Adjuvant radiotherapy to pelvis: PTV includes upper half of vagina,
lower common iliac, external iliac and internal iliac nodes. Laterally PTV
bisects S2/S3 and anteriorly to the anterior aspect of symphisis pubis.
Shielding to normal tissues as appropriate
Superiorly – include top of sacrum
Inferiorly – include upper half of vagina
Laterally – 1cm clear of pelvic side walls
Palliative radiotherapy: PTV – encompassing gross disease using smaller
field sizes to minimise acute toxicity
Critical structures Small bowel
5. Dose and Adjuvant radiotherapy: 45Gy/25# (Grade C)
Fractionation HDR to vault - 6Gy at 5mm from applicator surface treating top 2-4cm
Radical radiotherapy: external beam as per adjuvant followed by HDR –
6Gy x 2 fractions at the uterine serosa
Pelvic recurrences in untreated patients: external beam as per adjuvant
radiotherapy followed by HDR to vault – 6Gy x 2 fractions at 5mm
Palliative radiotherapy: 20Gy/5#, 30Gy/10#, 40Gy/15#, 8-10Gy/1#,
single HDR insertion for vaginal bleeding
6. Special instructions Provide ‘Radiotherapy to the female pelvis’ information leaflet
7. Clinical Trials and PORTEC-3 (see trial protocol for planning and dose specifications)
References
Date of approval by Lead Clinician/TSG: 08/04/2010
Issue Date: 08-July-2010 Page 40 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gynaecological
Tumour: OVARY
Intent: Palliative RCR Category status: 2 or 3
1. Localisation method CT scan for field definition using virtual simulation
2. Planning technique AP POP or 4 field
3. Immobilisation Supine, knee and foot supports
method
4. Volume definition and Gross tumour with 2cm margin
Critical structures
5. Dose and 30Gy / 10# over 14 days
Fractionation 8Gy / 1#
6. Special Instructions Small volume if treating pelvis to reduce morbidity
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 29/04/2010
Issue Date: 08-July-2010 Page 41 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gynaecological
Tumour: VAGINA
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method CT scan for field definition using virtual simulation
2. Planning technique Dependent on anatomical site of primary:
AP POP if inguinal lymph nodes included in field
4 fields for mid/upper vaginal disease
3. Immobilisation Supine, arms by side, radio-opaque marker at introitus
method
4. Volume definition and GTV primary disease identified using clinical examination/EUA/imaging
CTV depends upon position of tumour, as differing lymphatic drainage
lower 1/3 vagina to include whole vagina and inguinal nodes
middle and upper vagina to include whole vagina, internal, external and
common iliac nodes
Critical structures Small bowel
5. Dose and Phase 1 45Gy/25#
Fractionation Phase 2 14-16Gy/7-8#
6. Special instructions Provide "Radiotherapy to female pelvis" information leaflet
Gynae CNS support and use of vaginal dilators
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 14/04/2010
Issue Date: 08-July-2010 Page 42 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Gynaecological
Tumour: VULVA
Intent: Radical or Palliative RCR Category status: 1 or 3
1. Localisation method CT can for field definition using virtual simulation
2. Planning technique Radio-opaque marker is used to define extent of palpable disease and
lymph nodes.
AP POP or direct field in case of primary disease when no need to treat
nodes.
3. Immobilisation Supine, arms across chest with comfortably full bladder
method
4. Volume definition and Radical Treatment
Critical structures Initial volume – gross tumour and sites of potential microscopic disease
Usually parallel opposed fields
Superior border – 2cm above inferior border of SI joint
Inferior border – 2cm below inferior extend of disease
Lateral border – include all of femoral neck
Fields can be weighted anteriorly to improve dose distribution
Electrons can be used to treat groin nodes
Adjuvant Treatment – Positive Groin Nodes
Fields as for radical treatment but shield vulva if possible ie clear margins
Inguinal nodes – inferior border 2cm inferior to lesser trochanter
Close or +ve margins with –ve groin nodes
Treat tumour bed with 2cm margin
Nodal areas not treated
Un-dissected Groin
When using electrons CT/MRI images are helpful in choosing appropriate
energy.
Palliative Volume
Small fields to cover gross tumour and margin
Issue Date: 08-July-2010 Page 43 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and Radical schedules
Fractionation 45Gy / 25# / 5weeks followed by boost: 16Gy / 8# (Grade B)
50.4Gy / 28# / 5.5weeks with chemotherapy (Grade B)
Adjuvant
45Gy / 25# / 5weeks
Concurrrent Chemoradiation
50.4Gy / 20# / 5.5weeks with concurrent 5 Fluorouracil infustion plus
cisplatin 60mg/m2 week 1 and 5 Fluorouracil infusion on week 5. A small
volume boost taking the dose to 60Gy can be considered (photons,
electrons or brachytherapy) (Grade B)
Palliative schedules
30Gy / 10# / 2weeks
6Gy weekly over 3-6weeks
10-20Gy / 5# / 1week
8-10Gy single fraction
6. Special instructions Provide ‘Radiotherapy to female pelvis – use of vaginal dilators’
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 29/04/2010
Issue Date: 08-July-2010 Page 44 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: CERVICAL OESOPHAGUS
Intent: Radical RCR Category status: 1
1. Localisation method CT scan
2. Planning technique Conformal field arrangements:
Isocentric anterior oblique fields
Isocentric anterior and posterior fields (phase 1) with IMRT
fields(phase 2)
Compensators or a double wedge would be used with the anterior
oblique fields
3. Immobilisation Patient supine in treatment shell on 5 point IMRT board
method
4. Volume definition and Dependent upon EUA findings and MRI scans with an adequate margin
Critical Structures
5. Dose and Phase 1: 40-46Gy / 20-23#
Fractionation Phase 2: 18-20Gy / 9-10#
Total – 60-64Gy / 30-32# / 6weeks
6. Special Instructions Usually chemo radiation unless post op
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 45 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: HEAD AND NECK CANCER GENERAL
Intent: Radical or Palliative RCR Category status: 1 , 2 or 3
1. Localisation method CT Scan +/- MRI for specialised
2. Planning technique As per protocol
3. Immobilisation Perspex shell or orfit cast
method
4. Volume definition and CTV = only macroscopic disease with 2cm margin
Critical Structures
5. Dose and Good performance (WHO 0-2/young patients/prognosis <3months)
Fractionation 40.5Gy / 15# / 21days
30Gy / 6# / 2weeks (max cord dose = 27Gy / 6#)
30Gy / 10# / 2weeks
Stage III or IV (fit patients offered definitive radiotherapy)
Moderately accelerated radiotherapy eg
66-68Gy in 2Gy fractions / x6 a week / over 5.5weeks (Grade A)
72Gy / in 6weeks using concomitant boost (Grade A)
66-70Gy / in 6.5-7weeks plus synchronous chemotherapy (Grade A)
Poor performance (WHO 3-4/elderly/frail patients/prognosis
>3months)
Consider carefully whether radiotherapy is indicated
Anterior neck fields only
An applied dose using 5/6 MV photons with midline shielding to cord. If
significant lymphadenopathy in the lower neck use AP opposing fields
Non-Computed Opposing Fields
Palliative treatment – mid plane dose
6. Special Instructions Consider all appropriate shielding requirements
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 46 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: LARYNX – GLOTTIC LARYNX (tumour limited to true vocal cords and 5mm below)
Intent: Radical RCR Category status: 1
1. Localisation method T1 or T2
Simulator (CT scan for those patients with very short neck – PTV + virtual
simulation)
T3 or T4
Simulator – examine patients neck for nodes (CT scan to produce data set
in some circumstances)
2. Planning technique T1 or T2
Simple isocentric lateral fields, single central axis contour (short neck
patients = ant oblique fields, CT scanned + virtually simulated)
T3 or T4
Isocentric lateral fields – large fields may require a CT scan to produce a
data set in order to achieve a uniform homogeneous distribution
3. Immobilisation Supine, clear shell
method Head in neutral position to achieve straight spinal cord. Shoulders
extended towards feet.
4. Volume definition T1 and T2 N0
Superior – Hyoid bone
Inferior – 10mm below cricoid
Anteriorly – clear front of cast
Posteriorly – front of vertebral bodies or to include the anterior ⅓ of
vertebral bodies
T3 or T4
Superior – arch of atlas
Inferior – root of neck
Anteriorly – clear front of cast
Posteriorly – posterior to vertebral bodies or spinous process
Critical Structures Spinal cord
Issue Date: 08-July-2010 Page 47 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and T1 or T2
Fractionation 55Gy/20# /28days (Grade C)
66Gy / 33# / 47days (Grade B)
T3 or T4
Total: 65Gy / 30# / 6weeks - Phase 1: 43Gy / 20# - Phase 2: 22Gy / 10#
(Grade A)
Total: 66-70Gy / 33-35# = 6.5-7weeks - Phase 1: 44Gy / 22# - Phase 2:
22Gy / 11# (Grade A)
Post electron boost: 10Gy / 5#
16Gy / 8# (involved ipsilateral neck +ve)
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 48 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: LARYNX – SUB-GLOTTIC LARYNX
Intent: Radical RCR Category status: 1
1. Localisation method T1 and T2 N0
Examine patient’s neck for neck nodes.
In simulator determine plane of treatment and produce localisation film.
Simulation with access to previous CT/MRI scans
CT scan – PTV – Virtual Simulated - verified
T3 and T4 node +ve
Examine patients neck (if no neck resection)
Simulation with access to previous CT/MRI scans
CT scan for data set
2. Planning technique T1 and T2 N0
Isocentric lateral opposed fields
More commonly ant oblique fields and 0.5cm of wax on front of cast
T3 and T4 node +ve
Isocentric lateral opposed fields
Isocentric sup oblique fields (compensators or segmental field technique)
3. Immobilisation Supine – neck extended and shoulders extended towards feet, clear shell
method
4. Volume definition T1 and T2 N0
Incorporate prophylactic irradiation of 1st station nodes (levels III + IV)
Superior – hyoid bone
Inferior – 2cm below tumour on scan
Anteriorly – to clear front of cast
Posteriorly – back edge of vertebral body
T3 and T4 node +ve
Phase 1: Superior – 2cm above C1/C2 junction
Inferior – to include stoma or 1cm below sSN or below clavicles
to include level IV nodes
Anteriorly – to clear front of cast
Posteriorly – include spinous process of C2
Phase 2: Reduce off cord – add post neck electrons
Critical Structures Spinal cord
Issue Date: 08-July-2010 Page 49 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and T1 and T2 N0
Fractionation Total: 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Total: 65Gy / 30# / 6weeks - Phase 1: 41Gy / 19# - Phase 2: 24Gy / 11#
(Grade B)
Total: 66-70Gy / 33-35# / 6.5-7weeks - Phase 1: 44Gy / 22# - Phase 2:
22Gy / 11# (Grade A)
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Adjacent field dose (post neck off spinal cord): 10Gy / 5#
16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 50 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: LARYNX – SUPRAGLOTTIC LARYNX
Intent: Radical RCR Category status: 1
1. Localisation method T1 and T2 Node –ve + Node +ve
Examine patients neck (if no neck resection)
Simulation with access to previous CT/MRI scans
CT scan for data set if necessary to produce a homogenous dose
distribution.
T3 and T4
Simulation with access to previous CT/MRI scans. CT scan for data set
2. Planning technique T1 and T2 Node –ve + Node +ve
Isocentric lateral opposed fields – ant split field added if node +ve.
T3 and T4
Isocentric lateral opposed fields
Isocentric superior oblique fields – compensator technique or segmental
field technique
3. Immobilisation Supine – head in neutral position and shoulders extended towards feet,
method clear shell. NB. Thermoplastic mask for palliative patients
4. Volume definition T1 and T2 N0
Incorporate prophylactic irradiation of 1st station nodes (levels II & III)
Phase 1:
Superior – 2cm above C1/C2 junction
Inferior – lower border of cricoid or root neck along clavicle
Anteriorly – to clear the front of the cast
Posteriorly – if nodes are present include spinous process of C2. If node -
ve post border lies in front of the vertebral bodies.
Volume of anterior split field
Superior – to match lower border or upper fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Phase 2 treatment volume if nodes present
Reduced off cord – electron adjacent fields may be used depending upon
nodal disease status.
Critical Structures Spinal cord
Issue Date: 08-July-2010 Page 51 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and Total: 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Fractionation Total: 64Gy / 32# / 6.5weeks - Phase 1: 56Gy / 28# - Phase 2: 8Gy / 4#
(Grade B)
Total: 65Gy / 30# / 6weeks - Phase 1: 43Gy / 20# - Phase 2: 22Gy / 10#
(Grade B)
Total: 70Gy / 35# / 7weeks- Phase 1: 44-46Gy / 22-23# - Phase 2: 20-22Gy
/ 10-11# (Grade A)
Anterior spilt field: 50Gy / 25# / 5weeks
Post electron boost: 10Gy / 5#
16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 52 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: LOWER ALVEOLUS
Intent: Radical RCR Category status: 1 / 2 / 3
1. Localisation method Simulator + CT scan
2. Planning technique Wedged pair or similar
3. Immobilisation Perspex Shell
method
4. Volume definition and Isocentric right-angled wedge pair – depending on nodal status a half
Critical Structures anterior split field may be added
Isocentric lateral/anterior oblique wedge pair – depending upon nodal
status a half anterior split field may be added
Phase 1 treatment volume
Superior – 1.5cm above tumour, for larger lesions, the pterygoids should be
covered
Inferior – hyoid
Anteriorly – symphysis
Posteriorly – to include spinous process of C2
If nodes present add half anterior split field
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
If nodes present phase 2 treatment volume
Reduced off cord – electron adjacent fields may be used depending upon
nodal disease status
5. Dose and 55Gy / 20# / 4weeks
Fractionation Total: 60-70Gy / 30-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase 2:
16-24Gy / 8-12# (Grade A)
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Adjacent field dose (post neck off spinal cord): 10Gy / 5#
16Gy / 8#
Issue Date: 08-July-2010 Page 53 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 54 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: MAXILLARY SINUS/NASAL CAVITY
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method CT planned with contrast (PTV only)
2. Planning technique CT – Isocentric anterior and 2 lateral fields
Segmental field arrangement or IMRT may be required to produce
homogenous plan
3. Immobilisation Supine, Clear shell, Mouth bite – is desirable to spare dose to tongue if
method patient can tolerate it. Head in neutral and comfortable position
4. Volume definition and Governed by PTV. 5mm margin around PTV.
Anterior field
Superior – 1cm above cribiform plate or supraorbital ridge
Inferior – upper alveolus through mouth bite
Medial - contralateral inner canthus
Lateral – to cover gingivo-buccal sulcus
Lateral fields
Anterior – 2cm anterior to tumour
Posterior – to include the pterygoid fossa and lateral retrophayngeal node
Critical Structures Optic nerves, chiasm, brain stem, retina and lens.
5. Dose and Total: 64-70Gy / 32-35Gy / 6.5weeks - Phase 1: 44-46Gy / 22-23# - Phase
Fractionation 2: 20-22Gy / 10-11#
NB – dose may need to be reduced to respect tolerance of critical normal
tissues
6. Special Instructions The dose is biased from the anterior field with a weighting of 2 or 3:1.
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 55 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: NASOPHARYNX
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Chemo-radiation: Used for stage III/IV patients (1987 UICC) using the
intergroup regime
CT planning is required with MR fusion for image registration.
Delineate targets and organs at risk (OAR)
3. Immobilisation Perspex shell
method
4. Volume definition and GTV= gross tumour and involved nodes
Critical structures CTV1= GTV+5mm (may be reduced to 1mm adjacent to critical OAR)
CTV2= adjacent involved structures and high risk nodes
CTV3= lower risk nodes
PTV1= CTV1+5mm(reduced to 1mm adjacent to spinal cord and/or
brainstem)
PTV2= CTV2+5mm (reduce as above)
PTV3= lower neck fields (conventional)
If nodes present add anterior split field
Superior – to match upper fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
NB – if positive nodes in the lower neck use anterior/posterior fields
5. Dose and Total: 66-70Gy / 33-35# / 6.5-7weeks (Grade A)
Fractionation Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
If positive nodes in lower neck:
Ant/post fields 50Gy /25#/ 5 weeks Phase I
20Gy/ 10#/ 2weeks Phase II
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
Issue Date: 08-July-2010 Page 56 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
7. Clinical Trials and None at present
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 57 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: OROPHARYNX – BASE OF TONGUE
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed pair – depending upon disease extent an anterior
split field may be added
3. Immobilisation Perspex shell
method
4. Volume definition and Phase 1 treatment volume
Critical structures Superior – 1cm above base of tongue
Inferior – level of glottis
Anteriorly – to include faucial pillar and portion or oral tongue
Posteriorly – to include spinous process of C2
If nodes present add anterior split field
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavical
If nodes present phase 2 treatment volume: Reduced off cord
Electron adjacent fields may be used depending upon nodal disease status
5. Dose and 50-55Gy / 20# / 4weeks
Fractionation Total – 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Total – 66-70Gy / 33-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase
2: 20-26Gy / 10-13# (Grade A)
Anterior split field – 50Gy / 25# / 5weeks or 40.5Gy / 15# / 3weeks
Post Electron Boost – 10Gy / 5# (if neck –ve)
16Gy / 8# (involved ipsilateral neck +ve)
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 58 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: OROPHARYNX – BUCCAL MUCOSA
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric wedge pair – depending upon nodal status a half anterior split
field may be added
Isocentric lateral opposed pair – depending upon nodal status an anterior
split field may be added
3. Immobilisation Perspex shell
method
4. Volume definition and Isocentric wedge pair fields phase 1 treatment volume
Critical Structures Superior – 2cm above tumour or 1cm beyond graft
Inferior – hyoid
Medially – depends on extend of tumour
Anteriorly – 2cm above tumour or 1cm beyond graft
Posteriorly – to include spinous process of C2
Isocentric parallel opposed fields phase 1 treatment volume
Superior – 2cm above tumour or 1cm beyond graft
Inferior – hyoid
Anteriorly – 2cm above tumour or 1cm beyond graft
Posteriorly – to include spinous process of C2
If nodes present add anterior split
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicle
Medial – lateral edge of vertebral bodies
If nodes present – phase 2 treatment volume: Reduced off cord
Add electron adjacent fields to boost area overlying cord
Issue Date: 08-July-2010 Page 59 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and 50-55Gy / 20# / 4weeks
Fractionation Total – 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Total – 66-70Gy / 33=35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# -Phase
2: 16-24Gy / 8-12# (Grade A)
Post RT to a total dose of 60-64Gy / 30-32# / 6weeks in one or two phases
Anterior split field – 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Post boost off spinal cord - 10Gy/5# (non-involved contralateral neck +ve)
16Gy/8# (involved ipsilateral neck +ve)
16Gy electrons / 8# (bilateral neck +ve)
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 60 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: OROPHARYNX - FLOOR OF MOUTH
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed pair – for lesions at or crossing midline.
Depending upon disease extent an anterior split field may be added.
3. Immobilisation Mouth bite, Perspex shell
method
4. Volume definition and Phase 1:
Critical structures Superior – through mouth bite
Inferior – Hyoid
Anteriorly – to include palpable disease with a 2cm margin
Posteriorly – to include anterior ⅔ of vertebral goodies or to include
spinous process of C2
If nodes present add anterior split field
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicals
Lateral – to include medial ⅔ of clavicles
If nodes present phase 2 treatment volume: Reduced off cord – electron
adjacent fields may be used depending upon nodal disease status
5. Dose and Total: 50-55Gy / 20# / 4weeks
Fractionation Total: 60-77Gy / 33-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase 2:
20-24Gy / 10-13# (Grade A)
Post RT to a total dose of 60-64Gy / 30-32# / 6weeks in one or two phases
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Post Electron Boost: 10Gy / 5# (non-involved contralateral neck +ve)
16Gy / 8# (involved ipsilateral neck +ve)
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 61 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: OROPHARYNX – ORAL TONGUE
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed pair – depending upon nodal status an anterior
split field may be added
Isocentric right-angled wedge pair – depending upon nodal status a half
anterior split field may be added
3. Immobilisation Perspex shell
method
4. Volume definition and Phase 1 treatment volume
Critical structures Superior – 1.5cm above dorsum of tongue, sparing hard palate if possible
Inferior – vallecula
Anteriorly – to include palpable disease with a 2cm margin
Posteriorly – to mid vertebral unless node +ve when it should include
spinous process of C2
If nodes present add anterior split field
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
If nodes present phase 2 treatment volume: Reduced off cord – electron
adjacent fields may be used depending upon nodal disease status.
5. Dose and 55Gy / 20# / 4weeks
Fractionation Total: 60-70Gy / 30-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase 2:
16-24Gy / 8-12# (Grade A)
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Post Electron Boost: 10Gy / 5# or 16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 62 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: PAROTID GLAND
Intent: Radical RCR Category status: 2
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric right-angled wedge pair – depending upon nodal status a half
anterior split field may be added
Isocentric anterior and posterior oblique wedge pair – depending upon
nodal status a half anterior split field may be added
NB –take care to avoid exit of post oblique field through contralateral eye
3. Immobilisation Perspex shell
method
4. Volume definition and Superior – Zygomatic arch or 2cm above most superior extent of disease
Critical Structures (must be inferior to the eyes)
Inferior – hyoid or 1cm inferior to the mandible
Anteriorly – anterior border of the masseter muscle
Posteriorly – through the mastoid process
Medially – the lateral pharyngeal wall or 2cm beyond the medial extent of
the tumour
If nodes present add anterior split field
Superior – to match lower border of lateral fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
If nodes present phase 2 treatment volume: Reduced off cord
5. Dose and Total: 66-70Gy / 33-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase 2:
Fractionation 20-26Gy / 10-13# (Grade A)
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 63 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: PYRIFORM FOSSA
Intent: Radical RCR Category status: 1 or 2
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed fields
Isocentric superior oblique fields (compensators would be used)
NB – technique is dependent upon the position of the lower border. If the
supraclaviular fossa needs treating, superior oblique fields should be used
3. Immobilisation Perspex shell
method
4. Volume definition and Small treatment volume
Critical Structures Superior – angle of jaw
Inferior – 1cm below cricoid cartilage
Anteriorly – to clear neck
Posteriorly – to lie in front of the spinal cord
Large treatment volume – Phase 1
Superior – 2cm above C1/C2 junction
Inferior – to include stoma or 1cm below SSN or root of neck – must be at
least 2cm below cricoid cartilage
Anteriorly – to clear the front of the cast
Posteriorly – if nodes are present include spinous process of C2. If no
nodes, post. Border is to lie in front of the vertebral bodies
Phase 2 volume if nodes present: Reduced off cord – electron adjacent
fields may be used depending upon nodal disease status
5. Dose and Total: 65Gy / 30# / 6weeks -Phase 1: 43Gy / 20# - Phase 2: 22Gy / 120#
Fractionation Total: 66-70Gy / 33-35# / 6-7weeks - Phase 1: 44-46Gy / 22-23# - Phase 2:
20-26Gy / 10-13# (Grade A)
Post Electron Boost: 10Gy / 5#
16Gy / 8#
Post RT: 60-64Gy / 30-32# / 6.5weeks in one or two phases
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 64 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: RETROMOLAR TRIGONE
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric right-angled wedge pair – depending upon nodal status a half
anterior split field my be added
Isocentric ipsilateral oblique fields – depending upon nodal status a half
anterior split field may be added
3. Immobilisation Perspex shell
method
4. Volume definition and The CTV must extend superiorly to include the madibular ramus because
Critical Structures of the high risk of microscopic spread. The temporomandibular joint
should be avoided if possible to minimise the risk of trismus
Treatment Volume*
Superior – temporomandibular junction
Inferior – hyoid
Anteriorly – masseter muscle
Posteriorly – mid vertebral body
If nodes present add half anterior split field
Superior – to match lower border of upper fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
5. Dose and 55Gy / 20# / 4weeks
Fractionation Total: 66Gy / 33# / 6.5wks - Ph1: 44Gy / 22# - Ph 2: 22Gy / 11# (Grade A)
Half anterior split field: 50Gy / 25# / 5weeks or 40.5Gy / 15# / 3weeks
Post Electron Boost: 10Gy / 5# or 16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 65 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: SOFT PALATE
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed pair – depending upon disease extent an anterior
split field may be added
Isocentric right-angled wedge pair – depending upon nodal status a half
anterior split field may be added
3. Immobilisation Perspex shell
method
4. Volume definition and Lateral fields phase 1 treatment volume
Critical Structures Superior - Zygomatic arch
Inferior – hyoid
Anteriorly – 2cm anterior to tumour
Posteriorly – spinous process of C2
Phase 2 treatment volume if nodes present: Reduced off cord – electron
adjacent fields may be used depending upon nodal disease status
Wedge pair phase 1 treatment volume
Superior – Zygomatic arch
Inferior – hyoid
Anteriorly – 2cm anterior to tumour
Posteriorly – centre of vertebral bodies
Medially – midline to 2cm beyond midline
Phase 2 treatment volume
Primary disease only
If nodes present add anterior split field
Superior – to match lower border of upper fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
Issue Date: 08-July-2010 Page 66 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and 50-55Gy / 20# / 4weeks
Fractionation Total: 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Total: 66Gy / 33# / 6.5weeks - Phase 1: 44Gy / 22# - Phase 2: 22Gy / 11#
(Grade A)
Anterior split field: 50Gy / 25# / 5weeks or 40.5Gy / 15# / 3weeks
Post Electron Boost: 10Gy / 5# or 16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 67 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: THYROID
Intent: Radical RCR Category status: 2
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric anterior oblique wedge pair
Isocentric anterior and posterior opposed fields
Consider use of 2:1 weighting ant/post
3. Immobilisation Perspex shell
method
4. Volume definition and Anterior Oblique Fields
Critical Structures Superior – mastoid tip
Inferior – carina
Posterior – anterior to spinal cord
Anterior and Posterior Opposed Fields
Phase 1
Superior – mastoid tip
Inferior – carina
Lateral – medial ⅔ of clavicle
Phase 2
A more localised volume to bulk disease
5. Dose and 50Gy / 20# / 4weeks
Fractionation Total: 60-64Gy / 30-32# / 6.5weeks in one or two phases
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 68 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Head and Neck
Tumour: TONSIL
Intent: Radical RCR Category status: 1
1. Localisation method Simulator + CT scan
2. Planning technique Isocentric lateral opposed pair – depending upon disease extent an anterior
split field may be added
Isocentric anterior and posterior oblique wedge pair – depending upon
nodal status a half anterior split field may be added.
3. Immobilisation Perspex shell
method
4. Volume definition and Wedge Pair Phase I treatment volume
Critical Structures Superior – top of the hard palate
Inferior – bottom of the hyoid bone
Anteriorly – middle ⅓ of the tongue
Posteriorly – just in front of the spinal cord
Medially – midline of palate
Phase 2 treatment volume
Primary disease only
Lateral opposed fields Phase I treatment volume
Superior – top of the hard palate
Inferior – bottom of the hyoid bone
Anteriorly – middle ⅓ of the tongue
Posteriorly – to include spinous process of C2
Phase 2 treatment volume if nodes present: Reduced off cord – electron
adjacent fields may be used depending upon nodal disease status
If nodes present add anterior split field
Superior – to match lower border of upper fields
Inferior – to include heads of the clavicles
Lateral – to include medial ⅔ of clavicles
Medial – lateral edge of vertebral bodies
Issue Date: 08-July-2010 Page 69 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and Total: 63Gy / 30# / 6weeks - Phase 1: 42Gy / 20# - Phase 2: 21Gy / 10#
Fractionation Total: 66Gy / 33# / 6.5weeks - Phase 1: 44Gy / 22# - Phase 2: 22Gy / 11#
(Grade A)
Anterior split field: 50Gy / 25# / 5weeks
40.5Gy / 15# / 3weeks
Post Electron Boost: 10Gy / 5#
16Gy / 8#
6. Special Instructions To be weighed weekly
Referral to CNS and/or dietician as appropriate
Provide ‘Radiotherapy to the Head or Neck’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 70 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lung
Tumour: MESOTHELIOMA
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Simulator or planning scan no localisation required (drain site)
2. Planning technique Template to mark area for treatment
3. Immobilisation Radical : Lung board, knee and foot supports
method Palliative : As appropriate for comfort and stability
4. Volume definition and Symptomatic (eg pain, SVC, oesophageal obstruction)
Critical structures
5. Dose and Tumour masses – 20-25Gy / 5# / 1week or 30-32.5Gy / 10# / 2weeks
Fractionation Hemi-thorax – 12.5-20Gy / 5# / 1week (12.5Gy/5# may be given at same
time as chemotherapy is troublesome local symptoms and immediate
chemotherapy required)
To intrathoracic drains, biopsy sites etc (unless life expectancy
<3months)
10-12Gy / 1# (MV or HVX)
12.5Gy / 1# (Cobalt) with 0.5cm bolus
Thoracotomy scars – 25Gy / 5# / 1week, tangent pair or electrons with
bolus (eg post decortication)
6. Special Instructions
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 71 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lung
Tumour: NON-SMALL CELL LUNG
Intent: Radical or Palliative RCR Category status: 1 or 3
1. Localisation method CT scan or Simulator planning dependent on stage or 4D scan dependent
on site in lung – fluoroscopy to check tumour motion where significant
respiratory motion suspected prior to 4D scanning.
2. Planning technique Radical: Conformal
Palliative: Conformal or simple AP parallel pair (as appropriate for
comfort and stability)
3. Immobilisation Lung board - Additional immobilisation device if stereotactic body
method radiotherapy is used. Please see SBRT protocol
4. Volume definition and Lung – V20 preferably ≤ 30% maximum 35%
Cord – usually ≤ 45Gy but for paravertebral or pancoast tumours cord dose
of 52.5Gy / 20# justifiable
Oesophagus – for prescribed doses >52.5Gy, ≤12 cm oesophagus should be
included in PTV
Critical structures Normal lung tissue, Spinal cord, Myocardium, Oesophagus, Brachial
Plexus
5. Dose and Radical Treatment:
Fractionation SBRT: 18 Gy x 3#/1 week or 11 Gy x 5#/2 weeks (please see protocol)
64Gy / 32# / 6.5weeks (Grade B) when overlap with previous radiotherapy
treatment or concerns for normal tissue toxicity.
55 Gy/ 20#/ 4 weeks.
a) Dose to isocentre can be increased to 60 Gy if GTV cold
b) 50-52.5 Gy/ 20#/ 4 weeks if spinal cord in field or post operative
Palliative Treatment:
37.5 Gy / 15# / 3weeks (for field lengths ≥ 10 cm, cord max 37.5Gy)
If cord and oesophagus are not in field – 39Gy / 13# / 17days (Grade B)
36Gy / 12# / 16days
30-32.5Gy / 10# / 2weeks (cord max 32.5Gy / 10#)
27Gy / 6# / 2weeks - treatment on alternate days (Grade D)
20-25Gy / 4-5# / 1week (cord max in 5# 22.5Gy if concerns re: lung
function use V12 <30%)
Consider – 20Gy / 5# / 1week (Grade B)
16- 17Gy / 2# / over 8days (Grade A) – for moderate to poor performance
status patients (spinal cord shielding may be necessary)
8-10Gy / 1# (Not preferred if left ventricle is in irradiated volume)
Chemo-Radiotherapy: 55Gy / 20# / 26days
Issue Date: 08-July-2010 Page 72 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
6. Special instructions Standard chemotherapy regime = Cisplatin 20mg/m² concurrent with
fractions 1-4 and 16-20 plus Vinorelbine 15mg/m² days 1-8 and 16-20. Or
cisplatin single agent 20 mg/m2 depending on comorbidity, PS and field
size.
If there is evidence of response and the patient’s performance status is
maintained, this is followed by:
Cisplatin 80mg/m² day 1 and Vinorelbine 30mg/m² days 1, 8 and 21 day
intervals commencing 4weeks after completion of concurrent treatment
Provide ‘Radical Radiotherapy to the Chest’ or ‘Palliative Radiotherapy to
the Chest’ information leaflet as appropriate
7. Clinical Trials and IDEAL-CRT is process of being opened. Isotoxic radiotherapy dose
References escalation over seven weeks with standard chemotherapy. See protocol for
full details
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 73 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lung
Tumour: SMALL CELL LUNG
Intent: Radical or Palliative RCR Category status: 1 or 3
1. Localisation method Simulator/CT dependent on stage
Verify if required
2. Planning technique Radical : Conformal
Palliative : Simple parallel pair or Conformal
3. Immobilisation Radical : Lung board, knee and foot supports
method Palliative : As appropriate for comfort and stability
4. Volume definition and For concurrent: gross disease as seen on scan, No Elective nodal irradiation
Critical structures For sequential: Nodal sup/inf length as seen on pre-chemotherapy scan but
primary volume as seen on post-chemotherapy scan
5. Dose and Radical:
Fractionation 40Gy / 15# / 3weeks
Palliative: 30Gy / 10# / 2weeks
20Gy / 5# / 5-7days
27 Gy/ 6#/ 2 weeks6-10Gy / 1#
For selected patients with SCLC, prophylactic cranial radiotherapy:
25 Gy/ 10#/ 2 weeks
6. Special instructions Provide ‘Radical Radiotherapy to the Chest’ or ‘Palliative Radiotherapy to
the Chest’ information leaflet as appropriate
7. Clinical Trials and None at present. CONVERT in the process of being opened for LD SCLC.
References Cisplatin/etoposide with concurrent radiotherapy starting with second
cycle. Randomising between 45 Gy/30#/3 weeks bd vs. 66 Gy/33#. Please
see protocol for details
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 74 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lymphoma
Tumour: HODGKINS DISEASE
Intent: Radical / Palliative RCR Category status: 2 / 3
1. Localisation method CT planned
2. Planning technique Dependent on site. May use virtual sim. Parallel Opposed Pair may be
useful but for more difficult sites in the abdomen 3 fields may cover
volume better. Consider half beam blocking off cord if one side of neck.
3. Immobilisation Supine, orfit cast if appropriate.
method
4. Volume definition and Outline enlarged lymph node areas based on CT scan at presentation and
after chemotherapy. Areas positive on PET scan should be included in the
GTV even if not enlarged. Negative enlarged nodes may still contain
lymphoma and should be included. Treat the clinically involved lymph
node region with/without the adjacent lymph node regions.
Margin to PTV: 1-2cm lateral and 2-5cm superior/inferior.
If initial disease displaced adjacent extranodal tissues without infiltration
then the initial tumour bulk does not need to be covered, e.g. mediastinal
nodes
Always treat unilateral SCF with axilla, the bilateral SCF with upper
mediastinum and the whole neck from mastoid to below clavicle
Critical structures Commonly mouth and cord
5. Dose and Bulky residual disease or bony involvement: 40Gy/20#
Fractionation Small volume residual disease: 30Gy/15# (Grade B)
Large field sizes in mediastinum or abdomen: 35Gy/20# (Grade C)
Palliative radiotherapy: 30Gy/10#, 20Gy/5#, 8Gy/1# (all Grade D)
6. Special instructions
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 26/04/2010
Issue Date: 08-July-2010 Page 75 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lymphoma
Tumour: Non-Hodgkins Lymphoma (NHL)
Intent: Radical or Palliative RCR Category status: 2 or 3
1. Localisation method CT, Simulator or mark up on set dependent on site/stage Use
pre-chemotherapy CT and PET to define GTV extent
2. Planning technique CT – Conformal or virtually simulated
Simulator – Direct field/parallel pair
Mark up on set – define lesion clinically, (skin and conjunctiva)
3. Immobilisation CNS, eye, conjunctiva and neck and extra-nodal sites neck:
method oroplast
All other: supine leg and ankle support
4. Volume definition CNS: Whole brain including both orbits if ocular involvement
and critical structures Cranio-spinal axis radiotherapy may be used if chemo-resistant –
see CNS protocol and involve Consultant authorised to prescribe
in this area
Eyes and conjunctiva (high grade): Fit patients with CNS
directed chemotherapy followed by radiotherapy to the eye
Orbital NHL: CTV=orbit
Conjunctiva NHL : CTV=anterior orbit
Neck nodes: CTV= affected nodes and 1 cm margin AP, RL, 2.5
cm SI
Extra-nodal sites, e.g. Waldeyer’s ring, thyroid, salivary
gland, nose and sinus: GTV dependent on extent, planning
principles as per relevant head and neck protocol. Avoid bilateral
parotid irradiation if possible.
Mediastinum: : CTV= affected nodes and 1.5 cm margin AP,
RL, 2.5 cm SI
Abdomen and pelvis : CTV= affected nodes and 1.5 cm margin
AP, RL, 2.5 cm SI
Stomach: CT planning to limit kidney/liver dose. CTV stomach
and any lymphadeopathy
Spleen: CT planning to limit kidney/liver dose. DIBH gating if
possible (see spleen protocol)
Testis: Treat contra-lateral testis, direct anterior field with lead
shielding; post chemotherapy may not include inguinal lymph
nodes
Issue Date: 08-July-2010 Page 76 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
5. Dose and Radical intent:
Fractionation CNS: Whole brain: 45Gy/25#. If ocular involvement : 30Gy/20#
Intraocular NHL: 30Gy/15#
High grade DLBCL NHL: 30Gy/15# post chemotherapy,
consider 40Gy /20# for primary treatment
Low grade NHL: 24Gy/12#
Bone: 40Gy/20# to whole bone
Skin: 8Gy single fraction (T or Bcell) consider fractionated
course for large lesion
Palliative intent: depends on histology, bulk and fitness15Gy/5
fraction or equivalent for high grade NHL, 4Gy/2# for low grade
6. Special instructions Refer to lymphoma protocol and CNS protocols for more details
7. Clinical Trials and FORT for low grade NHL
References
Date of approval by Lead Clinician/TSG: 26/04/2010
Issue Date: 08-July-2010 Page 77 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Lymphoma
Tumour: SPLEEN
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Indication for treatment :
radical low grade non Hodgkins lymphoma / maltoma of the spleen, high
grade NHL or Hodgkin’s post chemotherapy
Palliative: Hypersplenism (CML, CLL, MGUS)
Localisation:
Radical: CT planning consider gating or breath hold
Palliative: Simulate and check palpate spleen prior to each treatment.
2. Planning technique Radical: CT plan
Palliative: Parallel opposed pair
3. Immobilisation Radical: ankle stocks and knee support – supine position
method Palliative: mattress
4. Volume definition and CTV: spleen no margin
PTV: according to respiratory motion 1.5-2.5 cm less with gating
Critical structures Kidney
5. Dose and Radical low grade non Hodgkins lymphoma / maltoma of the spleen
Fractionation 24Gy/12~#; high grade NHL or Hodgkin’s post chemotherapy 30Gy/15#
Palliative 5Gy/5# weekly
6. Special instructions Regular FBC check, may drop quickly; consider antibiotic prophylaxis and
vaccination for radical patients
7. Clinical Trials and FORT for low grade non Hodgkins lymphoma / maltoma
References
Date of approval by Lead Clinician/TSG: 26/04/2010
Issue Date: 08-July-2010 Page 78 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Paediatric
Paediatric radiotherapy should only be carried out by (or in occasional circumstances,
under the supervision of), a clinician experienced in the provision of radiotherapy to
children and who is a member of the CCLG Radiotherapy group.
Children should be treated according to nationally agreed guidelines or within
national and international clinical trials and the clinician should be familiar with and
have access to the latest version of these protocols.
A significant proportion of paediatric diagnoses are eligible for Department of Health
funding to travel abroad for high energy proton therapy. The up to date list and
guidance may be found at https://www.rcr.ac.uk/content.aspx?PageID=1527 (RCR
website).
Issue Date: 08-July-2010 Page 79 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Skin
Tumour: MELANOMA
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Dependent on site
2. Planning technique Dependent on site
3. Immobilisation Dependent on site
method
4. Volume definition and Malignant Melanoma metastatic to nodes
Critical structures PTV: to include the next station of nodes to a radical dose
5. Dose and Lentigo Maligna
Fractionation Field size1-2.9cm 35Gy/5#; 3-4.9cm 45 Gy/10#, >5cm50Gy/16# or
55Gy/20# using MVX or electrons (prescription dose to 95%, requires
mould room prep)
Malignant Melanoma metastatic to nodes
Inguinal nodes only 45 gy/20 fractions (option to prescribe with a 3:2
weighting)
Inguinal nodes in elderly/frail patients, 30Gy/6 fractions 3 times weekly.
Large volume postoperative radiotherapy after axillary dissection and
inguinal dissection including the iliac nodes 60Gy/30 fractions
For the axilla, use a shell, virtual simulation with mantle type lung
shielding and CT planning with segments to ensure dose homogeneity. For
the pelvis I have hitherto used 3D conformal radiotherapy.
Melanoma Metastases
Use standard skin technique and dose appropriate for site
6. Special instructions Provide ‘Radiotherapy to Skin Cancers’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 80 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Skin
Tumour: MERKEL CELL
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Dependent on site
2. Planning technique Dependent on site
3. Immobilisation Dependent on site
method
4. Volume definition and Treatment of primary tumour bed + regional lymphnodes should be
Critical Structures considered in high risk cases of good performance status.
5. Dose and Treat axillary + nodes as per melanoma protocol.
Fractionation Treating primary site with close/involved margins = 60-66Gy/30-33# or
45Gy / 15# / 21days in elderly patients or small volume tumours.
6. Special Instructions Provide ‘Radiotherapy to Skin Cancers’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 81 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Skin
Tumour: NON MELANOMA
Intent: Radical / Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Clinical set up
2. Planning technique Planned on set; complex shapes and HDR selectron need mould room input
orthovoltage (most sites) or electrons (scalp, lower leg or hand) or perspex
mask for HDR selectron (scalp, lower leg or hand)
Large lesion with invasion of underlying structures are best CT planned in
Perspex mask with bolus
3. Immobilisation Dependent on site
method
4. Volume definition and MVX BCC 5-7mm margin 10mm for morphoeic lesion)
Critical structures SCC 10-15 mm depending on size
Electrons use wax build up (normally 5mm) to increase skin dose to 100%
BCC 10mm margin, 15mm for morphoeic lesion)
SCC 15mm
HDR selectron 10-15mm
5. Dose and 35Gy / 5# / 5days (30 Gy for microscopic residual disease post surgery)
Fractionation 45Gy / 10# / 12days (40 Gy for microscopic residual disease post surgery)
50Gy / 15# / 19days (45 Gy for microscopic residual disease post surgery)
22Gy / 1# / 1days
6. Special instructions Provide ‘Radiotherapy to Skin Cancers’ information leaflet
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 30/04/2010
Issue Date: 08-July-2010 Page 82 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Other
Tumour: BONE METASTASES
Intent: Palliative RCR Category status: 3
1. Localisation method Simulator or HVX dependent on site
2. Planning technique Dependent on site. Simple field arrangement - usually single field or
parallel opposed pair. Linac or Cobalt is appropriate. HVX may be used in
some cases.
Examples:
Rib metastases: Direct field on HVX
Deeper lesions: Direct field or parallel pair on Cobalt
Scattered lesions: Upper or lower hemibody
3. Immobilisation Simple immobilisation aimed at improving comfort as well as stability.
method Exact immobilisation dependent on site, e.g. knee support, mattress
4. Volume definition and Dependent on site
Critical structures
5. Dose and Examples:
Fractionation Rib Metastases: 8Gy / 1# (Grade A)
Deeper Lesions: 8Gy / 1# *Grade A) or 20Gy / 5# / 1week (Grade C)
Scattered Lesions: Upper hemibody: 6Gy / 1# - Lower hemibody: 8Gy /
1# (Grade C)
Initial Therapy of Pain: 8Gy / 1# (Grade A)
6. Special instructions Dependent on site
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 22/04/2010
Issue Date: 08-July-2010 Page 83 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Other
Tumour: SOFT TISSUE SARCOMA
Intent: Radical or Palliative RCR Category status: 2 or 3
1. Localisation method CT/Simulator – dependent on site and intent
2. Planning technique Conformal or simple parallel pair
3. Immobilisation Dependent on site – may need vacubag
method
4. Volume definition and Dependent on site
Critical Structures
5. Dose and Pre-op: 50Gy/25# (Grade C) (rare – age, disease dependent)
Fractionation Post-op: 60-66Gy/30-33#
Unresectable tumours: 66Gy/33# (Grade C) (phased where possible –
patient status dependent)
Palliation: 6-8Gy/1# up to 40Gy/15# depending on clinical circumstances
and field size (Grade D)
6. Special Instructions
7. Clinical Trials and VORTEX
References
Date of approval by Lead Clinician/TSG: 10/05/2010
Issue Date: 08-July-2010 Page 84 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Tumour Group: Other
Tumour: TOTAL BODY IRRADIATION
Intent: Radical or Palliative RCR Category status: 1 / 2 / 3
1. Localisation method Clinical measurements and CT
2. Planning technique CT to define lung compensator and hip separation, clinical measurements
to define head compensator and bolus; refer to TPJBITR and TWJTBIDE
for details
3. Immobilisation Pillow to support arms over chest
method Bolus for neck, waist and legs
4. Volume definition and
Critical structures Lung
5. Dose and 14.4 Gy / 8# / 4days on M10-5
Fractionation
6. Special instructions Need test dose to check compensator and bolus
7. Clinical Trials and None at present.
References
Date of approval by Lead Clinician/TSG: 26/04/2010
Issue Date: 08-July-2010 Page 85 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
CCO, Radiotherapy Quality System 2010
Quality Procedure Radiotherapy Protocols
Treatments using IMRT
Mesothelioma
Prostate
Issue Date: 08-July-2010 Page 86 of 86 Filename: TPCPROTS.d20 Issue No: 2.0
Author: TSG Leads Authorised by: Dr B J Haylock Copy No:
Potrebbero piacerti anche
- Treatment Planning 01Documento43 pagineTreatment Planning 01Amr MuhammedNessuna valutazione finora
- Extracranial Stereotactic Radiotherapy and RadiosurgeryDocumento368 pagineExtracranial Stereotactic Radiotherapy and Radiosurgeryhanghouse824467% (3)
- KN Govinda - Radiation Safety in Radiation OncologyDocumento455 pagineKN Govinda - Radiation Safety in Radiation OncologyMaranda RoleaNessuna valutazione finora
- ICRU Reporte 38Documento30 pagineICRU Reporte 38Marco Herrera100% (1)
- Radiation TherapyDocumento69 pagineRadiation TherapyRamesh BabuNessuna valutazione finora
- Diagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoireDocumento5 pagineDiagnostic Reference Level in Lumbar Radiography in Abidjan, Côte D'ivoiretheijesNessuna valutazione finora
- Vmat QaDocumento31 pagineVmat QaJoseLuisDumontNessuna valutazione finora
- Rtog 0813 Marina CousinsDocumento22 pagineRtog 0813 Marina Cousinsapi-426094285Nessuna valutazione finora
- Radiotherapy Head N NeckDocumento90 pagineRadiotherapy Head N Neckyunia chairunnisaNessuna valutazione finora
- Principles RadiotherapyDocumento71 paginePrinciples RadiotherapyHasan AlomariNessuna valutazione finora
- Problem Solving in Oncology 1st 2008Documento26 pagineProblem Solving in Oncology 1st 2008Anirban Halder100% (1)
- Off Budgell FRCR - VerificationDocumento46 pagineOff Budgell FRCR - VerificationAmr MuhammedNessuna valutazione finora
- 2.37 Rso Training Standard Syllabi For Training Courses On Radiological SafetyDocumento96 pagine2.37 Rso Training Standard Syllabi For Training Courses On Radiological SafetyashwiniNessuna valutazione finora
- Calibration of Ionisation ChamberDocumento76 pagineCalibration of Ionisation ChamberArmin DurakovićNessuna valutazione finora
- 01-Quantities and Units in Radiation Protection-RSRC-2018-EEIDocumento44 pagine01-Quantities and Units in Radiation Protection-RSRC-2018-EEIMichael Murillo BaraquioNessuna valutazione finora
- Solutions: Radiation Medicine QaDocumento128 pagineSolutions: Radiation Medicine QaHashir SaeedNessuna valutazione finora
- Detecting and Measuring Radiation Lect 4Documento22 pagineDetecting and Measuring Radiation Lect 4Tonyo LinaNessuna valutazione finora
- Basic radiobiology: fractionation, 5 Rs, α/β ratio, QUANTEC: ESO Masterclass in Oncology Basics for BeginnersDocumento32 pagineBasic radiobiology: fractionation, 5 Rs, α/β ratio, QUANTEC: ESO Masterclass in Oncology Basics for BeginnersAji PatriajatiNessuna valutazione finora
- 4 Background RadiationDocumento1 pagina4 Background Radiationsomu1100% (1)
- Part 2 Week 9 - Treatment PlanningDocumento50 paginePart 2 Week 9 - Treatment PlanningdanNessuna valutazione finora
- Treatment Planning 04Documento42 pagineTreatment Planning 04Amr MuhammedNessuna valutazione finora
- Radiation Burn - WikipediaDocumento12 pagineRadiation Burn - WikipediaLiviuNessuna valutazione finora
- QUANTEC RT ConstraintsDocumento41 pagineQUANTEC RT ConstraintsNika Topuria100% (2)
- Radiation Oncology A Physicists Eye ViewDocumento332 pagineRadiation Oncology A Physicists Eye Viewquyen2012100% (1)
- IAEA - Radiation Protection For LINACsDocumento343 pagineIAEA - Radiation Protection For LINACsSuhey07Nessuna valutazione finora
- MOSAIQ Radiation Oncology BrochureDocumento8 pagineMOSAIQ Radiation Oncology Brochurealeksandar markovicNessuna valutazione finora
- OPAL ReactorDocumento21 pagineOPAL ReactorbenshtanNessuna valutazione finora
- The Role of Radiotherapy in Cancer TreatmentDocumento9 pagineThe Role of Radiotherapy in Cancer TreatmentarakbaeNessuna valutazione finora
- Imrt VmatDocumento29 pagineImrt VmatandreaNessuna valutazione finora
- SBRT-VMAT Pulmón: DR Enrique CHAJON Département de Radiothérapie Centre Eugène Marquis Rennes, FranceDocumento37 pagineSBRT-VMAT Pulmón: DR Enrique CHAJON Département de Radiothérapie Centre Eugène Marquis Rennes, FranceCristian Max Rau VargasNessuna valutazione finora
- Nuclear Medicine Resources ManualDocumento544 pagineNuclear Medicine Resources ManualHend Ayman Azazy100% (2)
- P1153 1Documento500 pagineP1153 1jiar001Nessuna valutazione finora
- Curriculum of Diploma in X-Ray Technician Course: Syllabus andDocumento27 pagineCurriculum of Diploma in X-Ray Technician Course: Syllabus andAshish Kumar DwivediNessuna valutazione finora
- New Advanced in RadiotherapyDocumento49 pagineNew Advanced in RadiotherapyIndonesian Journal of CancerNessuna valutazione finora
- Chapter 16 Radiation Protection and Safety PDFDocumento236 pagineChapter 16 Radiation Protection and Safety PDFAshutosh SinghNessuna valutazione finora
- Application of Radiobiology in RTDocumento61 pagineApplication of Radiobiology in RTnilesh kumarNessuna valutazione finora
- (OTHER) QC of Nuclear Medicine Equipment 2010 PDFDocumento12 pagine(OTHER) QC of Nuclear Medicine Equipment 2010 PDFMark DenhamNessuna valutazione finora
- Radio PharmaceuticalsDocumento825 pagineRadio PharmaceuticalsMustafa IdaisNessuna valutazione finora
- Various Immobilization Devices in RadiotherapyDocumento39 pagineVarious Immobilization Devices in RadiotherapyDr. Musaib Mushtaq100% (1)
- RADIOBIOLOGY Speaker Sharib Ahmed On 19-11-2013Documento32 pagineRADIOBIOLOGY Speaker Sharib Ahmed On 19-11-2013Waqar Ahmed0% (1)
- Treatment Calculations JohnsonDocumento116 pagineTreatment Calculations Johnsonmedical HunterNessuna valutazione finora
- Elements of Radiobiology and Radioprotection: Dr. A. Iftime, Dr. E. KatonaDocumento12 pagineElements of Radiobiology and Radioprotection: Dr. A. Iftime, Dr. E. KatonaAlexandra StoikNessuna valutazione finora
- 2012 - Handbook of Treatment Planning in Radiation Oncology OCRDocumento127 pagine2012 - Handbook of Treatment Planning in Radiation Oncology OCRRoxana MacarieNessuna valutazione finora
- Intraoperative RadiotherapyDocumento42 pagineIntraoperative RadiotherapyDr Sasikumar SambasivamNessuna valutazione finora
- Chapter (2) Part (1) 15-11-2021Documento38 pagineChapter (2) Part (1) 15-11-2021Ahmed HamdyNessuna valutazione finora
- ICRP 53 - Radiation Dose To Patients From RadiopharmaceuticalsDocumento340 pagineICRP 53 - Radiation Dose To Patients From Radiopharmaceuticalsraymond_lane_7Nessuna valutazione finora
- Radiology PDFDocumento81 pagineRadiology PDFrawaNessuna valutazione finora
- Health PhysicsDocumento33 pagineHealth Physicsg1381821Nessuna valutazione finora
- Contemporary IMRT PDFDocumento477 pagineContemporary IMRT PDFmabidsaleemNessuna valutazione finora
- Radiopharmaceuticsdrmallhi 160425162404Documento39 pagineRadiopharmaceuticsdrmallhi 160425162404Khalid HussainNessuna valutazione finora
- CT ScanDocumento5 pagineCT ScanAsdur KhanNessuna valutazione finora
- Basics Principles of RadiologyDocumento55 pagineBasics Principles of RadiologyJunaedy HfNessuna valutazione finora
- Colorectal Cancer Structured Reporting Protocol (3nd Edition 2016)Documento77 pagineColorectal Cancer Structured Reporting Protocol (3nd Edition 2016)Shafrina IrzaNessuna valutazione finora
- Bladder Cancer Structured Reporting Protocol v2 11 FinalDocumento88 pagineBladder Cancer Structured Reporting Protocol v2 11 FinaldrelvNessuna valutazione finora
- Coloretal - IccrDocumento120 pagineColoretal - IccrAna CanastraNessuna valutazione finora
- AdultRoutineChest CTDocumento14 pagineAdultRoutineChest CTwanwaqiuddinNessuna valutazione finora
- GMP For Biologicals Version Post ECBS PDFDocumento38 pagineGMP For Biologicals Version Post ECBS PDFAbdullah Omar NasseefNessuna valutazione finora
- Te - 1621 Dose Reduction CTDocumento62 pagineTe - 1621 Dose Reduction CTRoshi_11Nessuna valutazione finora
- Poct14 SampleDocumento12 paginePoct14 SampleNadyely RibeiroNessuna valutazione finora
- Dataset For Histopathological Reporting of Primary Invasive Cutaneous Squamous Cell Carcinoma and Regional Lymph NodesDocumento57 pagineDataset For Histopathological Reporting of Primary Invasive Cutaneous Squamous Cell Carcinoma and Regional Lymph NodesMajid KhanNessuna valutazione finora
- Appendix A - Prostate Cancer Stratified Follow Up Pathway GuidelinesDocumento26 pagineAppendix A - Prostate Cancer Stratified Follow Up Pathway GuidelinesDiana MaicanNessuna valutazione finora
- Radiotherapy For Rectal Cancer - A5 v2.0Documento24 pagineRadiotherapy For Rectal Cancer - A5 v2.0Diana MaicanNessuna valutazione finora
- Clinical Practice GuidelinesDocumento6 pagineClinical Practice GuidelinesDiana MaicanNessuna valutazione finora
- Generatorul Van de Graaff, Acceleratorul Liniar, Ciclotronul - Accelerator de Particule ReferatDocumento6 pagineGeneratorul Van de Graaff, Acceleratorul Liniar, Ciclotronul - Accelerator de Particule ReferatDiana MaicanNessuna valutazione finora
- Miniature Daisy: Crochet Pattern & InstructionsDocumento8 pagineMiniature Daisy: Crochet Pattern & Instructionscaitlyn g100% (1)
- (Jones) GoodwinDocumento164 pagine(Jones) Goodwinmount2011Nessuna valutazione finora
- Aluminum PorterDocumento2 pagineAluminum PorterAmir ShameemNessuna valutazione finora
- Sample Monologues PDFDocumento5 pagineSample Monologues PDFChristina Cannilla100% (1)
- WBDocumento59 pagineWBsahil.singhNessuna valutazione finora
- Deep Hole Drilling Tools: BotekDocumento32 pagineDeep Hole Drilling Tools: BotekDANIEL MANRIQUEZ FAVILANessuna valutazione finora
- Baseline Scheduling Basics - Part-1Documento48 pagineBaseline Scheduling Basics - Part-1Perwaiz100% (1)
- Cisco BGP ASPATH FilterDocumento115 pagineCisco BGP ASPATH FilterHalison SantosNessuna valutazione finora
- Obligatoire: Connectez-Vous Pour ContinuerDocumento2 pagineObligatoire: Connectez-Vous Pour ContinuerRaja Shekhar ChinnaNessuna valutazione finora
- Jakub - BaZi CalculatorDocumento3 pagineJakub - BaZi Calculatorpedro restinxNessuna valutazione finora
- Sem4 Complete FileDocumento42 pagineSem4 Complete Fileghufra baqiNessuna valutazione finora
- Umwd 06516 XD PDFDocumento3 pagineUmwd 06516 XD PDFceca89Nessuna valutazione finora
- Assessment of The Genitourinary System: GeneralDocumento2 pagineAssessment of The Genitourinary System: GeneralMaharani UtamiNessuna valutazione finora
- SASS Prelims 2017 4E5N ADocumento9 pagineSASS Prelims 2017 4E5N ADamien SeowNessuna valutazione finora
- Acer N300 ManualDocumento50 pagineAcer N300 Manualc_formatNessuna valutazione finora
- Acute Appendicitis in Children - Diagnostic Imaging - UpToDateDocumento28 pagineAcute Appendicitis in Children - Diagnostic Imaging - UpToDateHafiz Hari NugrahaNessuna valutazione finora
- Inside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineDocumento40 pagineInside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineJoe BloggsNessuna valutazione finora
- Pathology of LiverDocumento15 paginePathology of Liverערין גבאריןNessuna valutazione finora
- An Annotated Bibliography of Timothy LearyDocumento312 pagineAn Annotated Bibliography of Timothy LearyGeetika CnNessuna valutazione finora
- Sample Resume For Supply Chain Logistics PersonDocumento2 pagineSample Resume For Supply Chain Logistics PersonAmmar AbbasNessuna valutazione finora
- Music CG 2016Documento95 pagineMusic CG 2016chesterkevinNessuna valutazione finora
- Canon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFDocumento13 pagineCanon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFRita CaselliNessuna valutazione finora
- Comparison Between CompetitorsDocumento2 pagineComparison Between Competitorsritesh singhNessuna valutazione finora
- Sources of Hindu LawDocumento9 pagineSources of Hindu LawKrishnaKousikiNessuna valutazione finora
- Notes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0MDocumento1 paginaNotes:: Reinforcement in Manhole Chamber With Depth To Obvert Greater Than 3.5M and Less Than 6.0Mسجى وليدNessuna valutazione finora
- Configuring BGP On Cisco Routers Lab Guide 3.2Documento106 pagineConfiguring BGP On Cisco Routers Lab Guide 3.2skuzurov67% (3)
- Disassembly Procedures: 1 DELL U2422HB - U2422HXBDocumento6 pagineDisassembly Procedures: 1 DELL U2422HB - U2422HXBIonela CristinaNessuna valutazione finora
- Economic Review English 17-18Documento239 pagineEconomic Review English 17-18Shashank SinghNessuna valutazione finora
- UntitledDocumento216 pagineUntitledMONICA SIERRA VICENTENessuna valutazione finora
- ML Ass 2Documento6 pagineML Ass 2Santhosh Kumar PNessuna valutazione finora