Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clasper
Caricato da
Sartini Roma Dame NainggolanCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clasper
Caricato da
Sartini Roma Dame NainggolanCopyright:
Formati disponibili
Limb Compartment Syndrome And Fasciotomy
1 70
2 71
3 72
4 73
5 74
6 75
7 76
8
9
JC Clasper1, D Standley2, S Heppell3, S Jeffrey4, PJ Parker5 77
78
10 79
11
1
Defence Professor Trauma & Orthopaedics, Academic Department of Military Surgery and Trauma, Royal Centre for Defence 80
12 Medicine, Birmingham; 2 Consultant Orthopaedic Surgeon, Royal Devon and Exeter NHS Foundation Trust; 3 Consultant 81
13 Plastic and Reconstructive Surgeon, Portsmouth Hospitals NHS Trust; 4 Consultant Plastic and Reconstructive Surgeon, 82
14 University Hospital Birmingham NHS Foundation Trust; 5 Senior Lecturer, Academic Department of Military Surgery and 83
15 Trauma, Royal Centre for Defence Medicine, Birmingham 84
16 85
17 86
18 87
19 88
20 89
21 Introduction diagnosis has been made in hospital, fasciotomy must take place 90
22 immediately. Any delay in treatment is associated with an adverse 91
23 A limb acute compartment syndrome (ACS) occurs when an outcome and an increase in complications such as amputation and 92
24 increase in the pressure in a closed fascial compartment results in even death [2]. 93
25 microvascular compromise resulting in muscle ischaemia. As the In the military environment there is little place for pressure 94
26 duration and magnitude of the pressure increase, myoneural monitoring even in an unconscious patient due to prolonged 95
27 function is impaired and necrosis of the soft tissue eventually evacuation, and the potential difficulties with regular observation 96
28 develops [1]. This can lead to significant morbidity, amputation and treatment during evacuation. A twelve hour CCAST 97
29 and even death [2]. Treatment of suspected ACS is by urgent evacuation at high altitude in darkness, where resuscitation and 98
30 decompression of the compartment. transfusion are often ongoing after IED injury, is no place for a 99
31 As in previous conflicts, the majority of casualties from Iraq and latent compartment syndrome : Put simply, a fasciotomy should be 100
32 Afghanistan have sustained limb injuries [3,4]. ACS clearly occurs carried out if there is any clinical suspicion of, or significant 101
33 in severely injured limbs following injury, but due to different potential for, compartment syndrome [5]. 102
34 methodology used in published work, it is difficult to determine 103
35 the exact incidence of ACS in civilian populations. It is generally General Principles 104
36 accepted to be approximately 1-5% following leg injuries, and less 105
37 than 1% within the upper limb [2]. This compares to a recent Fasciotomy can be associated with a high rate of complications [5] 106
38 military publication when 16% of casualties evacuated out of Iraq which in many cases is due to poor technique rather than 107
39 and Afghanistan had undergone a fasciotomy [5]. underlying injury. Regrettably most of the following consensus 108
40 Due to this relatively low incidence in civilian populations, it is statements and guidelines below have had to be re-learnt in recent 109
41 infrequently seen during civilian surgical training, with a mean of conflicts. They represent what we believe to be current best 110
42 only 3 fasciotomies, seen across 6 years of training in Trauma and practice. 111
43 Orthopaedic Surgery [6]. This article offers trainees and 112
44 consultants within the deployed surgical team guidelines on 1. Following diagnosis, fasciotomy should be carried out as 113
45 performing fasciotomies for the treatment or prevention of ACS. soon as practical due to the increase in complications with delay 114
46 ACS can occur in any in any muscle compartment, but is [2]. 115
47 commonest in the leg followed by the forearm [2,5]. The cardinal 116
48 symptom of a compartment syndrome is excessive pain. The 2. All compartments should be decompressed. In the lower leg 117
49 compartment is tense, and any further pressure worsens the pain, failure to decompress the deep posterior compartment is relatively 118
50 as does passive stretching of the muscles within the compartment common: Missed compartment syndrome is associated with a very 119
51 such as extending the toes or fingers. Absence of distal pulses (and high complication rate [5]. 120
52 sensation) is a very late sign, and only occurs after arterial 121
53 occlusion. 3. Full length incisions must be performed. A common error is 122
54 The diagnosis is clinical, although pressure monitoring can be that the incision is too short; usually the decompression appears 123
55 used if the condition is anticipated or suspected and accurate adequate but post-operative muscle swelling leads to ACS 124
56 clinical examination is not possible, such as with a head injured recurrence due to the tourniquet effect of tight skin and fascia at 125
57 patient, or an anaesthetic limb [7]. As pressure monitoring has not the extremes of the incision (Figure 1). 126
58 been shown to be more accurate than clinical monitoring [8], it is 127
59 not indicated in a conscious patient if regular assessment is 128
60 possible. Clinical suspicion remains the key. 129
61 Regular re-assessment is required as there may be a delay in 130
62 presentation, with a recent paper reporting a mean delay between 131
63 injury and fasciotomy of 22 hours even in monitored patients [9]. 132
64 Even though the development of ACS may be delayed, once the 133
65 134
66 Corresponding Author: Lt Col J Clasper, Professor of Trauma 135
67 and Orthopaedics, Academic Department of Military Surgery 136
and Trauma, Royal College of Defence Medicine, Birmingham Figure 1 An inadequate lower limb fasciotomy. These short incisions
68 have not allowed full compartment decompression 137
69 Email: Prof.TandO@rcdm.bhm.ac.uk 138
298 JR Army Med Corps 155(4): 298-301
139 4. Incisions should be placed with regard to later reconstructive Forearm 208
140 options. If the medial incision to decompress the lower leg (vide The forearm has superficial and deep flexor compartments and an 209
141 infra) is placed too posteriorly, the perforating vessels may be extensor compartment. Release can be performed through a single 210
142 damaged, limiting the options for local flaps. curved volar incision and several modifications are possible 211
143 [10,11]. For the inexperienced, it is advisable to carry this release 212
144 5. All planned incisions must be pre-marked with a pen, through two separate incisions avoiding inadequate release and 213
145 including possible surgical extensions prior to any incision wound closure compromise. The following method is 214
146 being made. It should be noted that significant swelling might recommended: 215
147 obscure the normal anatomical features Mark the midpoint of a line joining the two humeral 216
148 epicondyles and mark a second point midway between this and the 217
149 6. Any associated fracture should be reduced and stabilised. medial epicondyle. At the proximal wrist crease mark a point in 218
150 Most fasciotomies are carried out through a longitudinal skin line with the ulnar border of the ring finger. A straight incision is 219
151 incision. If the incision is performed in the presence of an unstable then made joining the two (Figure 4). The incision does not release 220
152 displaced fracture, particularly with rotational abnormalities, the the less commonly affected lateral forearm muscles. These require 221
153 final incision, after reduction of the fracture may expose bone, or a separate longitudinal incision along a line joining the lateral 222
154 again compromise reconstructive options. External fixation, epicondyle of the humerus with the radial tuberosity. An incision 223
155 traction and plaster of Paris are all viable options. along the proximal 1/3 to 1/2 of this line is required. 224
156 Extension into the palm may be required to release the carpal 225
157 7. Un-necessary exposure of the bone must be avoided, as this tunnel if the wrist/hand is within the zone of injury. Although the 226
158 will also compromise reconstructive options, possibly necessitating pain of carpal tunnel syndrome is neurological from compression 227
159 free or local flap rather than split skin graft coverage. If the medial of the median nerve rather than muscle pain, it may co-exist with 228
160 incision to decompress the lower leg is placed too anteriorly, the forearm ACS. A short transverse incision is made in the proximal 229
161 subcutaneous surface of the tibia may be exposed (Figure 2). The wrist crease to a point marked in line with the radial side of the ring 230
162 upper tibia may also be over-exposed by failure to appreciate its finger. The incision is then extended longitudinally into the palm 231
163 proximal flare. (Figure 4) with division of the transverse carpal ligament. To avoid 232
164 contractures, transverse or oblique incisions should always be used 233
165 when the flexor surface of a joint is crossed. 234
166 If extension into the upper arm is required a transverse incision 235
167 is made from the proximal point (half-way between the mid point 236
168 of a line joining the epicondyles and the tip of the medial 237
169 epicondyle) to just anterior to the medial epicondyle. 238
170 239
171 240
172 241
173 242
174 243
175 244
176 245
177 246
178 Figure 2 Incorrectly sited left lower limb fasciotomy. The tibia is 247
179 exposed due to an incorrectly placed skin incision and the anterior skin 248
180 bridge is too narrow placing it at risk of ischaemia. The foot is to the 249
181 left and knee to the right of the picture. Figure 4 The initial forearm incision with planned extension into the 250
182 carpal tunnel. The midpoint between the two epicondyles is marked 251
183 Site specific technique and the incision commences half way between it and the medial 252
184 epicondyle. 253
185 Upper arm 254
186 This has flexor and extensor compartments which are Hand 255
187 decompressed by a single longitudinal incision; this may be The compartments of the hand contain the small muscles that 256
188 possible through local wound extension. If exposure of the vessels provide fine motor control of the digits. Missed or untreated 257
189 is also required, the incision can be placed medially (Figure 3). A compartment syndrome of the hand is devastating for true hand 258
190 lateral longitudinal incision may be used to avoid exposing the function as only very crude reconstruction is then possible. If hand 259
191 brachial artery, but if external fixation is also required, closure of compartment syndrome is suspected – it must be treated by 260
192 this lateral wound then becomes more difficult. emergent surgical release. The compartments are released as 261
193 follows: 262
194 263
195 264
196 Thenar and Hypothenar eminences 265
197 The thenar and hypo-thenar eminences are released via 266
198 longitudinal incisions along each of their radial and ulnar borders. 267
199 Half of patients may have separate compartments within the 268
200 thenar eminence and this must be checked for by direct inspection 269
201 at surgery. 270
202 271
203 Interossei, lumbricals and adductor pollicis 272
204 The interossei are approached via 2 longitudinal incisions on the 273
205 dorsum of the hand, the first over the 2nd metacarpal and the 274
206 Figure 3 The medial incision to decompress left upper arm, allowing second over the 4th metacarpal (Figure 5). The incisions are 275
207 access to the neurovascular bundle deepened either side of the metacarpals and care should be taken to 276
JR Army Med Corps 155(4): 298-301 299
277 leave the paratenon of the extensor tendons undisturbed. This compartments are decompressed, the intermuscular septum 406
278 allows release of not only the interossei but also, via the radial dividing the anterior and lateral compartments is identified as a 407
279 extension of the first incision, the adductor policis muscle, which is depression. When a 3 cm superficial transverse cut is made in this, 408
280 deep to the 1st dorsal interosseus (Figure 5). the septum feels like a blunt knife-edge. Both the anterior and 409
281 Following fasciotomy the hand should be dressed and placed in lateral (peroneal) compartments are then fully released proximally 410
282 a well-padded splint in the “Safe” or “Edinburgh” position – MCP and distally in an H-shaped fashion with the transverse incision as 411
283 flexion to 90 degrees, IPJs fully extended, thumb extended and the centre bar of the H. 412
284 adducted. The hand should be elevated to prevent further oedema. 413
285 The wounds should be re-inspected following the general 414
286 guidelines for all fasciotomies detailed below. 415
287 416
288 417
289
A B 418
290 419
291 420
292 421
293 422
294 423
295 424
296 Figure 6 Lateral incision for lateral decompression of right lower leg 425
297 426
298 On the medial side a line is drawn 1-1.5 cm (1 finger breadth) 427
299 posterior to the medial border of the tibia. Incisions too anterior 428
300 Figure 5 The incisions required will leave exposed bone, and incisions too posterior may damage 429
301 to decompress the hand. A) the perforators and compromise subsequent plastic surgical options 430
302 Dorsal incisions to decompress (Figure 7). 431
303 the lumbricals and interossei. B) 432
304 Decompression of the 433
305 hypothenar muscles and C) 434
306 Incision to decompress thenar 435
307 muscles 436
308 437
309 438
310 C 439
311 440
312 441
313 Thigh 442
314 The thigh contains flexor, extensor and medial adductor 443
315 compartments. In most situations release of the anterior and 444
316 posterior compartments, through a single lateral incision, is 445
317 sufficient, but penetrating injuries to the thigh may require release 446
318 of the medial compartment, particularly when associated with a 447
319 vascular injury. This requires a separate incision. Figure 7 The medial incision for medial decompression of left lower leg 448
320 449
321 Lower leg This line begins just below the medial tibial flare and is extended 450
322 There are four compartments, the anterior and the lateral, the distally to a point four fingers above the tip of the medial malleolus. 451
323 superficial and the deep posterior. Failure to release the deep Once both lines are drawn (and before any incision is made), care 452
324 posterior compartment is the most common error in lower limb is taken to ensure that there is a now a minimum 7cm skin bridge 453
325 fasciotomy, and occurs when the release of the soleus muscle from between the two lines in the upper/mid portion of the leg to avoid 454
326 the posterior aspect of the tibia is mistaken for releasing the compromise of the potentially at-risk anterior skin bridge between 455
327 compartment. The posterior tibial artery is located between the the two incisions (Figure 8). 456
328 two posterior compartments, and this can be used as a landmark 457
329 during surgery. A two-incision technique is mandatory in the lower 458
330 limb. There is no place for the single incision/fibulectomy 459
331 technique which is medicolegally indefensible. In the lower limb, 460
332 fasciotomy incisions are not usually extended across joints. For 461
333 decompression of the thigh or foot separate incisions are required. 462
334 463
335 Technique 464
336 Incisions must be marked on both sides before commencement, 465
337 but it is ususal to first incise the side on which the landmarks are 466
338 easier to feel. For the lateral incision a point is marked midway 467
339 between the tibial tuberosity and the fibular head. A second point 468
400 is marked midway between the anterior border of the upper aspect 469
401 of the lateral malleolus and the lateral border of the tibia. A line is 470
402 drawn joining these two points, which must extend distally to just 471
403 above lateral malleolus. This is vital, as failure to extend the formal 472
404 incision distally is one of the most common reasons for an 473
405 inadequate fasciotomy (Figure 6). To ensure that both Figure 8 An adequate skin bridge (over 7cm) in the right lower leg 474
300 JR Army Med Corps 155(4): 298-301
475 The filmy fascia over gastrocnemius and soleus is easily released; Conclusion 544
476 however the deep posterior compartment cannot be correctly 545
477 decompressed if the medial attachment of the soleus to the tibia is Fasciotomy should be carried out if there is any clinical suspicion 546
478 not divided. There is a small bundle of 2-3 veins – the ‘soleal leash’ of, or significant potential for development of, compartment 547
479 located medially which when coagulated or tied act as a suitable syndrome. 548
480 marker for entry. There is a well-defined layer of fascia that is 549
481 thicker proximally than distally over the deep compartment. This References 550
482 must be entered and then fully released – again proximally and 551
483 distally. Finger dissecting with exposure of the posterior 1. Schwartz Jr JT, Brunback RJ, Lakatos R et al. Acute compartment syndrome 552
484 interosseous membrane confirms complete release. The deep of the thigh. A spectrum of injury. J Bone Joint Surg [Am] 1989;71–A:392- 553
485 posterior compartment may also be identified, with care, by the 400. 554
486 neurovascular bundle, which runs between the superficial and deep 2. Hayakawa H, Aldington D, Moore RA. Acute traumatic compartment 555
487 compartments. syndrome: a systematic review of results of fasciotomy. Trauma 2009;11:5-15. 556
3. Dougherty AL, Mohrle CR, Galarneau MR, Woodruff SI, Dye JL, Quinn
488 KH. Battlefield extremity injuries in Operation Iraqi Freedom Injury 557
489 Foot 2009;40:772-7. 558
490 The main indication for foot fasciotomy is to reduce the morbidity 4. Owens BD, Kragh JF, Macaitis J, Svoboda SJ, Wenke JC. Characterization of 559
491 (claw toes) associated with muscle necrosis but must be balanced Extremity Wounds in Operation Iraqi Freedom and Operation Enduring 560
492 against the significant morbidity of the procedure, where there is a Freedom. J Orthop Trauma 2007;21:254-7. 561
5. Ritenour AE, Dorlac WC, Fang R et al. Complications after fasciotomy
493 risk of infection if an open fracture is created. Wound closure is revision and delayed compartment release in combat patients. J Trauma
562
494 complex. The evidence base for either approach is poor and is 2008;64:S153-S162. 563
495 currently under review by the Academic Department of Military 6. https://www.elogbook.org/PD/logon/?ReturnUrl=%2fPD% 564
496 Surgery & Trauma. If foot fasciotomy is indicated is then two 2fdirector%2fDefault.aspx (Restricted Access – last accessed 13 Oct 09) 565
497 dorsal incisions are made centred over the 2nd and 4th metatarsal 7. McQueen MM, Court-Brown CM. Compartment monitoring in tibial 566
fractures. The pressure threshold for decompression. J Bone Joint Surg
498 shafts. The adductor compartment is released medially at the back [Br].1996;78-B:99-104.
567
499 of the instep. The posterior extent of the incision is approximately 8. Janzing HM, Broos PL. Routine monitoring of compartment pressure in 568
500 3cm anterior to the back of the heel, and 3cm above the sole of the patients with tibial fractures: Beware of overtreatment Injury 2001;32:415-21. 569
501 foot (Figure 9). 9. Al-Dadah OQ, Darrah C, Cooper A, Donell ST, Patel AD. Continuous 570
502 compartment pressure monitoring vs clinical monitoring in tibial diaphyseal 571
503 fractures. Injury 2008;39:1204-9. 572
10. Gelberman RH, Zakaib GS, Mubarak SJ, Hargens AR, Akeson WH.
504 Decompression of forearm compartment syndromes. Clin Orthop 573
505 1978;134:225-9. 574
506 11. Ronel DN, Mtui E, Nolan WB. Forearm compartment syndrome: Anatomical 575
507 analysis of surgical approaches to the deep space. Plast Recon Surg 576
508 2004;114:699-705 577
509 578
510 579
511 580
512 581
513 582
514 583
515 584
516 585
517 586
518 587
519 588
520 Figure 9 A line diagram of the three incisions required for 589
521 decompressing the right foot 590
522 591
523 Dressings and Re-inspection 592
524 593
525 Fluffed gauze is laid within the incisions. A layer of plain absorbent 594
526 material such as gamgee or velband is then applied. A well-applied 595
527 crepe bandage maintains the dressing but is not applied so tightly 596
528 as to restrict circulation. The wounds are re-inspected if any 597
529 increase in pain is noted. Plans for closure should begin at 3-5 days. 598
530 Early cover or closure leads to better mobilisation and less infective 599
531 complications. Often the medial side of the lower limb fasciotomy 600
532 is primarily closed and the lateral side split-skin grafted. 601
533 602
534 Complications 603
535 604
536 There are a number of complications associated with the 605
537 performing limb fasciotomy, however, those of non-performance 606
538 vastly outweigh them. Fasciotomy complications include, 607
539 haemorrhage, nerve damage especially the superficial peroneal 608
540 nerve laterally and the saphenous nerve medially and infection, 609
541 both bacterial and fungal. The closure itself may cause 610
542 complications and cosmesis may be an issue. 611
543 612
JR Army Med Corps 155(4): 298-301 301
The author has requested enhancement of the downloaded file. All in-text references underlined in blue are linked to publications on ResearchGate.
Potrebbero piacerti anche
- Limb Compartment Syndrome and Fasciotomy: JC Clasper, D Standley, S Heppell, S Jeffrey, PJ ParkerDocumento4 pagineLimb Compartment Syndrome and Fasciotomy: JC Clasper, D Standley, S Heppell, S Jeffrey, PJ ParkerMarius RisteaNessuna valutazione finora
- Rhino and Orthognathic SurgeryDocumento10 pagineRhino and Orthognathic SurgeryLaureano FilhoNessuna valutazione finora
- The Current Role and The Future of Minimally Invasive Temporomandibular Joint SurgeryDocumento19 pagineThe Current Role and The Future of Minimally Invasive Temporomandibular Joint SurgeryMohammedNessuna valutazione finora
- Mentoring, Education, and Training Corner: How To Approach A Patient With Ampullary LesionDocumento7 pagineMentoring, Education, and Training Corner: How To Approach A Patient With Ampullary LesionGustavo UriondoNessuna valutazione finora
- Art ColecisititisDocumento7 pagineArt ColecisititisFernando MontalvoNessuna valutazione finora
- Sternal Wound Procedures Require Coding Accuracy OpDocumento4 pagineSternal Wound Procedures Require Coding Accuracy OpbushaesNessuna valutazione finora
- The Richards Compression and Sliding Hip Screw System in The Treatment of Intertrochanteric Fractures PDFDocumento8 pagineThe Richards Compression and Sliding Hip Screw System in The Treatment of Intertrochanteric Fractures PDFVenky TarunNessuna valutazione finora
- Relationship Between Two Arrhythmias Sinus Node Dysfunction and Atrial Fibrillation.Documento5 pagineRelationship Between Two Arrhythmias Sinus Node Dysfunction and Atrial Fibrillation.Raul OrtegaNessuna valutazione finora
- Scientific Letter: Rev Esp Cardiol. 2022 XX (X) :XXX-XXXDocumento3 pagineScientific Letter: Rev Esp Cardiol. 2022 XX (X) :XXX-XXXapi-626131140Nessuna valutazione finora
- Post-Keratoplasty Astigmatism Management by RelaxiDocumento7 paginePost-Keratoplasty Astigmatism Management by Relaximedamif3Nessuna valutazione finora
- Siemens Somatom Sensation Cardiac A60 Users Manual 410406 PDFDocumento128 pagineSiemens Somatom Sensation Cardiac A60 Users Manual 410406 PDFronny sierraNessuna valutazione finora
- Complications Associated With Cataract SurgeryDocumento24 pagineComplications Associated With Cataract SurgeryEvenjelina EveNessuna valutazione finora
- Perioperative Management of Antithrombotic TherapyDocumento37 paginePerioperative Management of Antithrombotic TherapyjuanpbagurNessuna valutazione finora
- Clinical StudyDocumento7 pagineClinical StudyAndre Liang longNessuna valutazione finora
- Neils 2014Documento5 pagineNeils 2014DinNessuna valutazione finora
- Risk Assessment of HVAC PDFDocumento9 pagineRisk Assessment of HVAC PDFMohammad IsmailNessuna valutazione finora
- I (Eratomileusis - Clinical Results: Keratophakia andDocumento7 pagineI (Eratomileusis - Clinical Results: Keratophakia andMariana Luzardo bravoNessuna valutazione finora
- PM 070 E0Documento23 paginePM 070 E0Radu HarliscaNessuna valutazione finora
- Asd NurulDocumento8 pagineAsd NurulSiti AisyahNessuna valutazione finora
- Acute Iatrogenic Complications After Mitral Valve RepairDocumento7 pagineAcute Iatrogenic Complications After Mitral Valve Repairricardo villaNessuna valutazione finora
- ICD9CM-Procedure Index-A5Documento274 pagineICD9CM-Procedure Index-A5Rosdiana OceNessuna valutazione finora
- Medical Coding Mock PapersDocumento16 pagineMedical Coding Mock PapersSathya Kishore100% (4)
- The PERT Concept Q1 A Step-By-Step Approach To Managing Pulmonary EmbolismDocumento9 pagineThe PERT Concept Q1 A Step-By-Step Approach To Managing Pulmonary EmbolismntnquynhproNessuna valutazione finora
- Admin, Journal Manager, 08-GazzottiDocumento9 pagineAdmin, Journal Manager, 08-GazzottistedorasNessuna valutazione finora
- Bleeding and Thrombotic Complications in Patients With CirrhosisDocumento14 pagineBleeding and Thrombotic Complications in Patients With CirrhosisRoatgen LustNessuna valutazione finora
- Surgical Management of Postkeratoplasty AstigmatismDocumento13 pagineSurgical Management of Postkeratoplasty AstigmatismSss SzNessuna valutazione finora
- Dorsal Bridge Plating or Transarticular Screws For Lisfranc Fracture DislocationsDocumento7 pagineDorsal Bridge Plating or Transarticular Screws For Lisfranc Fracture DislocationsmaudiaNessuna valutazione finora
- Delta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesDocumento4 pagineDelta Wiring Technique To Treat Bony Mallet Fracture Technique Description and Case SeriesInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Hypertensive Thalamic Hemorrhage: Analysis of Short-Term OutcomeDocumento6 pagineHypertensive Thalamic Hemorrhage: Analysis of Short-Term OutcomeErwin Chiquete, MD, PhDNessuna valutazione finora
- IungDocumento8 pagineIungReda SoNessuna valutazione finora
- May 2016 Exam ReportDocumento16 pagineMay 2016 Exam ReportJane KoNessuna valutazione finora
- ATLS Practice Test 1 Answers & ExplanationsDocumento10 pagineATLS Practice Test 1 Answers & ExplanationsYou Wei Lin87% (15)
- Word - TEVARDocumento6 pagineWord - TEVARPutra AchmadNessuna valutazione finora
- Narakas 1985Documento8 pagineNarakas 1985Juan HoyosNessuna valutazione finora
- CVC Guia 2019 PDFDocumento20 pagineCVC Guia 2019 PDFKarenAlejandraRiveraRivera1705Nessuna valutazione finora
- Quantitative Analysis - Montgomery - Back Up File For Nov 16 Webinar PDFDocumento9 pagineQuantitative Analysis - Montgomery - Back Up File For Nov 16 Webinar PDFEmNessuna valutazione finora
- 18 FullDocumento5 pagine18 FullAgusAchmadSusiloNessuna valutazione finora
- Capnografia Volumétrica VAA Bumbacher2017Documento10 pagineCapnografia Volumétrica VAA Bumbacher2017Mariángeles DiazNessuna valutazione finora
- Chronic Total OcclusionsDocumento37 pagineChronic Total OcclusionsValentin CHIONCELNessuna valutazione finora
- Complications from the pacemaker pocket: prophylaxis, treatment and resultsDocumento4 pagineComplications from the pacemaker pocket: prophylaxis, treatment and resultsFahreza CaesarioNessuna valutazione finora
- AF Catheter AblationDocumento37 pagineAF Catheter AblationSnehal JayaramNessuna valutazione finora
- Complications of MsicsDocumento40 pagineComplications of MsicsSukhman kaur ButtarNessuna valutazione finora
- Be-Lab-100-Finals-Act-1-Bsmls-2c 2Documento9 pagineBe-Lab-100-Finals-Act-1-Bsmls-2c 2Cee James RafuelaNessuna valutazione finora
- Part of The LCP Periarticular Plating System.: Surgical TechniqueDocumento32 paginePart of The LCP Periarticular Plating System.: Surgical TechniqueLouis MiuNessuna valutazione finora
- Video-Assisted Thoracoscopic Surgery For Early Evacuation of Traumatic Clotted HemothoracesDocumento6 pagineVideo-Assisted Thoracoscopic Surgery For Early Evacuation of Traumatic Clotted Hemothoracesdella oktavianiNessuna valutazione finora
- Op Tech HybridDocumento46 pagineOp Tech Hybridopbhi3Nessuna valutazione finora
- Handandwristinjuries: Common Problems and SolutionsDocumento27 pagineHandandwristinjuries: Common Problems and SolutionsTeja LaksanaNessuna valutazione finora
- A Clinical Study of Functional Outcome of Surgical Management of Proximal Humerus FractureDocumento7 pagineA Clinical Study of Functional Outcome of Surgical Management of Proximal Humerus FractureInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- CardiothoracicsurgicallogbookrevisedDocumento8 pagineCardiothoracicsurgicallogbookrevisedprofarmah6150Nessuna valutazione finora
- Efectos de Laser Aplicado en Puntos Gatillos Vs Puntos Acupunturales en Dolor Miofascial CervicalDocumento9 pagineEfectos de Laser Aplicado en Puntos Gatillos Vs Puntos Acupunturales en Dolor Miofascial CervicalAilen CastroNessuna valutazione finora
- Injury: Jérôme Pierrart, Thierry Bégué, Pierre Mansat, GeecDocumento5 pagineInjury: Jérôme Pierrart, Thierry Bégué, Pierre Mansat, GeecJair FigueroaNessuna valutazione finora
- CBCT in OA PDFDocumento8 pagineCBCT in OA PDFHồ TiênNessuna valutazione finora
- FocusOn WristArthritisDocumento5 pagineFocusOn WristArthritisNicholas Raphael JohanNessuna valutazione finora
- Aerospace Science and Technology: P. Panagiotou, K. YakinthosDocumento13 pagineAerospace Science and Technology: P. Panagiotou, K. YakinthosKaspul AnuarNessuna valutazione finora
- Murali ThesisDocumento103 pagineMurali Thesissaikrishna645Nessuna valutazione finora
- 3dprinting in Orthopedic OncologyDocumento26 pagine3dprinting in Orthopedic OncologyAnto Anand GopurathingalNessuna valutazione finora
- PIIS0003497509012442Documento5 paginePIIS0003497509012442Tri RachmadijantoNessuna valutazione finora
- Management of 219 Consecutive Cases of Postcatheterization PseudoaneurysmDocumento6 pagineManagement of 219 Consecutive Cases of Postcatheterization PseudoaneurysmdrelvNessuna valutazione finora
- Rosen Et Al 2010 25837 PDFDocumento11 pagineRosen Et Al 2010 25837 PDFAlla MushkeyNessuna valutazione finora
- Phacoemulsification Referat Provides OverviewDocumento24 paginePhacoemulsification Referat Provides OverviewSartini Roma Dame NainggolanNessuna valutazione finora
- Bab III Fako ReferatDocumento2 pagineBab III Fako ReferatSartini Roma Dame NainggolanNessuna valutazione finora
- Morning Report Mrs AlbineDocumento50 pagineMorning Report Mrs AlbineTito Haposan TobingNessuna valutazione finora
- How to Manage Shortness of Breath: Steps and Treatment OptionsDocumento22 pagineHow to Manage Shortness of Breath: Steps and Treatment OptionsSartini Roma Dame NainggolanNessuna valutazione finora
- FF0089 01 Free Healthcare Presentation Template 16x9Documento22 pagineFF0089 01 Free Healthcare Presentation Template 16x9Sartini Roma Dame NainggolanNessuna valutazione finora
- FactSheet Children en PDFDocumento4 pagineFactSheet Children en PDFSartini Roma Dame NainggolanNessuna valutazione finora
- 10 1016@j Yjmcc 2017 07 026Documento1 pagina10 1016@j Yjmcc 2017 07 026Sartini Roma Dame NainggolanNessuna valutazione finora
- IntroductionDocumento1 paginaIntroductionSartini Roma Dame NainggolanNessuna valutazione finora
- ArticleDocumento5 pagineArticleSartini Roma Dame NainggolanNessuna valutazione finora
- Complications of Pregnancy: Clinical Guidelines O MDocumento12 pagineComplications of Pregnancy: Clinical Guidelines O MAlif FaqihNessuna valutazione finora
- Practice Guidelines: ACCP Releases Statement On Dyspnea Treatment in Patients With Advanced Lung or Heart DiseaseDocumento2 paginePractice Guidelines: ACCP Releases Statement On Dyspnea Treatment in Patients With Advanced Lung or Heart DiseaseSartini Roma Dame NainggolanNessuna valutazione finora
- MDCVJ 10 038Documento3 pagineMDCVJ 10 038Sartini Roma Dame NainggolanNessuna valutazione finora
- BF 01262564Documento2 pagineBF 01262564Sartini Roma Dame NainggolanNessuna valutazione finora
- BF 01262564Documento2 pagineBF 01262564Sartini Roma Dame NainggolanNessuna valutazione finora
- Dyspnea Grading ScaleDocumento5 pagineDyspnea Grading ScaleSartini Roma Dame NainggolanNessuna valutazione finora
- 4960 4843 1 PB PDFDocumento21 pagine4960 4843 1 PB PDFSartini Roma Dame NainggolanNessuna valutazione finora
- Frink2009 PDFDocumento11 pagineFrink2009 PDFSartini Roma Dame NainggolanNessuna valutazione finora
- Buku Bedah UmumDocumento126 pagineBuku Bedah UmumSilvia Kamal100% (7)
- Daftar Pusaka EtiologiDocumento2 pagineDaftar Pusaka EtiologiSartini Roma Dame NainggolanNessuna valutazione finora
- Drowning ClassificationDocumento5 pagineDrowning ClassificationSartini Roma Dame NainggolanNessuna valutazione finora
- Trauma and Non Trauma Airway ManagementDocumento2 pagineTrauma and Non Trauma Airway ManagementNadyaFachFudyanaNessuna valutazione finora
- Wrist or Hand Disability IndexDocumento1 paginaWrist or Hand Disability IndexHumza HamidNessuna valutazione finora
- 101 Love Making IdeasDocumento103 pagine101 Love Making IdeasJames Tong100% (2)
- Thanksgiving Cootie Catcher PDFDocumento1 paginaThanksgiving Cootie Catcher PDFManuel Orlando Sarmiento Vasquez100% (1)
- Lewis Ganson - Reelistic MagicDocumento66 pagineLewis Ganson - Reelistic MagicLuis MiguelNessuna valutazione finora
- Introduction To The Ten Element Concept Of Traditional Chinese MedicineDocumento33 pagineIntroduction To The Ten Element Concept Of Traditional Chinese MedicineJ SNessuna valutazione finora
- 2: Hand Skills: Occupational Therapy: Children, Young People & Families DepartmentDocumento54 pagine2: Hand Skills: Occupational Therapy: Children, Young People & Families DepartmentSuperfixenNessuna valutazione finora
- Finger Amputations: Aviram M. Giladi and Kevin C. ChungDocumento12 pagineFinger Amputations: Aviram M. Giladi and Kevin C. ChungREM biusNessuna valutazione finora
- Muscles of The Arm and ForearmDocumento8 pagineMuscles of The Arm and ForearmالبراءNessuna valutazione finora
- TLE9-NAILCARE9-Q3-M3 - EVELYN YARINDocumento14 pagineTLE9-NAILCARE9-Q3-M3 - EVELYN YARINMark Cris Fabella Fabaliña67% (3)
- Retdem Part 2Documento4 pagineRetdem Part 2gave maternityNessuna valutazione finora
- Bed BathDocumento10 pagineBed BathMurfaiza OmarNessuna valutazione finora
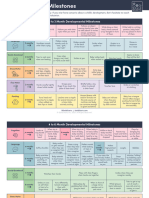
- Occupational Therapy - Developmental MilestonesDocumento3 pagineOccupational Therapy - Developmental MilestonesEndahRatnaningrumNessuna valutazione finora
- Erotic Encounters by Bonnie WilliamsDocumento11 pagineErotic Encounters by Bonnie WilliamsCorazon del RosarioNessuna valutazione finora
- Suturing Skills Ebook Marshall SuturingDocumento23 pagineSuturing Skills Ebook Marshall SuturingErbert De Langer100% (2)
- Volleyball Hand Signals GuideDocumento32 pagineVolleyball Hand Signals GuideMa Elaine TrinidadNessuna valutazione finora
- DEN 015L - General Anatomy 1 Student'S Activity Sheet Dentistry / First YearDocumento20 pagineDEN 015L - General Anatomy 1 Student'S Activity Sheet Dentistry / First YearMhdv Ndn McmNessuna valutazione finora
- Jodo ManualDocumento74 pagineJodo Manualsrbjkd100% (1)
- Solid Starts - Developmental MilestonesDocumento6 pagineSolid Starts - Developmental Milestonestohru89Nessuna valutazione finora
- Joint Mobilization To The Elbow, Wrist and Hand2Documento43 pagineJoint Mobilization To The Elbow, Wrist and Hand2Tripty Khanna Karwal100% (1)
- Brachial Plexus PowerpointDocumento37 pagineBrachial Plexus PowerpointMuhammad Naqiuddin JalaluddinNessuna valutazione finora
- CommonwordsjapaneseDocumento7 pagineCommonwordsjapaneseArjun ArjunNessuna valutazione finora
- Demo Nail Care 7Documento21 pagineDemo Nail Care 7Naddie SlaNessuna valutazione finora
- Kata Karate Vol2Documento87 pagineKata Karate Vol2Victor FariasNessuna valutazione finora
- Anatomy Course NotesDocumento75 pagineAnatomy Course Notesradu900Nessuna valutazione finora
- Healing Hands Technique OutlineDocumento6 pagineHealing Hands Technique OutlineThigpen FockspaceNessuna valutazione finora
- Traffic Direction and ControlDocumento56 pagineTraffic Direction and ControlArvin Cornejo100% (1)
- Art LessonDocumento2 pagineArt Lessonapi-515604081Nessuna valutazione finora
- Books on fingerprint science and investigationDocumento3 pagineBooks on fingerprint science and investigationasb231Nessuna valutazione finora
- NCM 207Documento29 pagineNCM 207Iligan, JamaicahNessuna valutazione finora
- Notes On Unarmed Combat - Sykes PDFDocumento4 pagineNotes On Unarmed Combat - Sykes PDFAlexJKDCQCNessuna valutazione finora