Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Flow Chart For Diabetic Ketoacidosis in Adults Management of
Caricato da
Josh Burke100%(2)Il 100% ha trovato utile questo documento (2 voti)
946 visualizzazioni1 paginaDKA
Titolo originale
Flow Chart for Diabetic Ketoacidosis in Adults Management of
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoDKA
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
100%(2)Il 100% ha trovato utile questo documento (2 voti)
946 visualizzazioni1 paginaFlow Chart For Diabetic Ketoacidosis in Adults Management of
Caricato da
Josh BurkeDKA
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 1
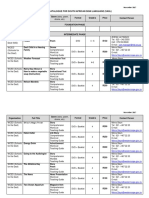
The Management of Diabetic Ketoacidosis in Adults
For young people under the age of 18 years use British Society of Paediatric Endocrinology and Diabetes (BSPED) guidelines: http://www.bsped.org.uk/professional/guidelines/docs/DKAGuideline.pdf
Diagnostic criteria: all three of the following must be present
• capillary blood glucose above 11 mmol/L BOX 3: 60 minutes to 6 hours BOX 5: 12 to 24 HOURS
Aims of treatment: Expectation: By 24 hours the ketonaemia and acidosis should have
• capillary ketones above 3 mmol/L or urine ketones ++ or more • Rate of fall of ketones of at least 0.5 mmol/L/hr OR bicarbonate rise 3 mmol/L/hr resolved. Request senior review if not improving
• venous pH less than 7.3 and/or bicarbonate less than 15 mmol/L and blood glucose fall 3 mmol/L/hr Aim:
• Maintain serum potassium in normal range • Ensure that clinical and biochemical parameters are continuing to improve
• Avoid hypoglycaemia or are normal
• Continue iv fluid replacement if not eating and drinking.
Action 1: Re-assess patient, monitor vital signs
• If ketonaemia cleared and patient is not eating and drinking move to a
BOX 1: Immediate management: time 0 to 60 minutes • Hourly blood glucose (lab blood glucose if meter reading ‘HI’)
variable rate IVII as per local guidelines
• Hourly blood ketones if meter available
(T=0 at time intravenous fluids are commenced) • Venous blood gas for pH, bicarbonate and potassium at 60 minutes, 2 hours and 2
• Re-assess for complications of treatment e.g. fluid overload, cerebral
oedema
If intravenous access cannot be obtained request critical care support immediately hourly thereafter.
• Continue to treat precipitating factors
• If potassium is outside normal range, re-assess potassium replacement and check
• Transfer to subcutaneous insulin if patient is eating and drinking normally.
Action 1: Commence 0.9% sodium chloride solution (use large bore • U&E hourly. If abnormal after further hour seek immediate senior medical advice
cannula) via infusion pump. • FBC Action 1 – Re-assess patient, monitor vital signs
Action 2: Continue fluid replacement via infusion pump as follows:
See Box 2 for rate of fluid replacement • Blood cultures Action 2 – Review biochemical and metabolic parameters
• 0.9% sodium chloride 1L with potassium chloride over next 2 hours
• ECG • At 12 hours check venous pH, bicarbonate, potassium, capillary ketones
Action 2: Commence a fixed rate intravenous insulin infusion (IVII). • 0.9% sodium chloride 1L with potassium chloride over next 2 hours
• CXR and glucose
(0.1unit/kg/hr based on estimate of weight) 50 units human • 0.9% sodium chloride 1L with potassium chloride over next 4 hours
• MSU • Resolution is defined as ketones <0.3 mmol/L, venous pH>7.3
soluble insulin (Actrapid® or Humulin S®) made up to 50ml with • Add 10% glucose 125ml/hr if blood glucose falls below 14 momol/L
• If not resolved review fluid Box 4 Action 1 and insulin infusion Box 3
0.9% sodium chloride solution. If patient normally takes long Action 5: Establish monitoring regimen More cautious fluid replacement in young people aged 18-25 years, elderly,
Action 3
acting insulin analogue (Lantus®, Levemir®) continue at usual • Hourly capillary blood glucose pregnant, heart or renal failure. (Consider HDU and/or central line)
dose and time • Hourly capillary ketone measurement if available If DKA resolved go to Box 6
Action 3: Assess response to treatment
Action 3: Assess patient • Venous bicarbonate and potassium at 60 minutes, 2
Insulin infusion rate may need review if
o Respiratory rate; temperature; blood pressure; pulse; oxygen hours and 2 hourly thereafter
• Capillary ketones not falling by at least 0.5 mmol/L/hr
saturation • 4 hourly plasma electrolytes
• Venous bicarbonate not rising by at least 3 mmol/L/hr
o Glasgow Coma Scale • Continuous cardiac monitoring if required
• Plasma glucose not falling by at least 3 mmol/L/hr
o Full clinical examination • Continuous pulse oximetry if required
• Continue fixed rate IVII until ketones less than 0.3 mmol/L, venous pH over 7.3
Action 6: Consider and precipitating causes and treat appropriately and/or venous bicarbonate over 18 mmol/L. BOX 6: Resolution of DKA
Action 4: Further investigations
If ketones and glucose are not falling as expected always check the insulin
• Capillary and laboratory glucose Expectation: Patient should be eating and drinking and back on normal
infusion pump is working and connected and that the correct insulin residual
• Venous BG insulin.
volume is present (to check for pump malfunction).
If DKA not resolved identify and treat the reasons for failure to respond.
If equipment working but response to treatment inadequate, increase insulin infusion
This situation is unusual and requires senior and specialist input.
rate by 1 unit/hr increments hourly until targets achieved.
Transfer to subcutaneous insulin
Additional measures
HDU/level 2 facility and/or insertion of central line may be required in following circumstances (request urgent senior Convert to subcutaneous regime when biochemically stable (capillary
• Regular observations and Early Warning Score (EWS)
review) ketones less than 0.3 mmol/L, pH over 7.3) and the patient is ready and able
• Accurate fluid balance chart, minimum urine output 0.5ml/kg/hr
to eat. Do not discontinue intravenous insulin infusion until 30
• Young people aged 18-25 years • Venous pH below 7.1 • Consider urinary catheterisation if incontinent or anuric (not passed urine by 60
minutes after subcutaneous short acting insulin has been given
• Elderly • Hypokalaemia on admission (below 3.5 mmol/L) minutes)
Conversion to subcutaneous insulin should be managed by the Specialist
• Pregnant • GCS less than 12 • Nasogastric tube with airway protection if patient obtunded or persistently
Diabetes Team. If the team is not available use local guidelines. If the patient
• Heart or kidney failure • Oxygen saturation below 92% on air (Arterial blood gases vomiting
is newly diagnosed it is essential they are seen by a member of the specialist
• Other serious co-morbidities required) • Measure arterial blood gases and repeat chest radiograph if oxygen saturation less
team prior to discharge.
• Severe DKA by following criteria • Systolic BP below 90 mmHg than 92%
Arrange follow up with specialist team.
• Blood ketones above 6 mmol/L • Pulse over 100 or below 60 bpm • Thromboprophylaxis with low molecular weight heparin
• Venous bicarbonate below 5 mmol/L • Anion gap above16 [Anion Gap = (Na+ + K+) – (Cl- + HCO3-) ] • Consider ECG monitoring if potassium abnormal or concerns about cardiac status
BOX 2: Initial fluid replacement BOX 4: 6 to 12 hours
Restoration of circulating volume is priority Aims: Reassess cardiovascular status at 12 hours; further fluid
Systolic BP (SBP) below 90mmHg • Ensure clinical and biochemical parameters improving may be required.
Likely to be due to low circulating volume, but consider other causes such as heart failure, sepsis, etc. • Continue iv fluid replacement
Check for fluid overload
• Give 500ml of 0.9% sodium chloride solution over 10-15 minutes. If SBP remains below 90mmHg • Avoid hypoglycaemia
repeat whilst requesting senior input. Most patients require between 500 to 1000ml given rapidly. • Assess for complications of treatment e.g. fluid overload, Action 2 – Review biochemical and metabolic parameters
• Consider involving the ITU/critical care team. cerebral oedema • At 6 hours check venous pH, bicarbonate, potassium, capillary
• Once SBP above 90mmHg give 1000ml 0.9% sodium chloride over next 60 minutes. Addition of • Treat precipitating factors as necessary ketones and glucose
potassium likely to be required in this second litre of fluid • Resolution is defined as ketones less than 0.3 mmol/L, venous
Action 1: Re-assess patient, monitor vital signs
pH over 7.3 (do not use bicarbonate as a surrogate at this
Systolic BP on admission 90 mmHg and over • If patient not improving by criteria in Box 3 seek senior advice
stage).
• Give 1000ml 0.9% sodium chloride over first 60 minutes • Continue iv fluid via infusion pump at reduced rate
• Ensure referral has been made to diabetes team Groups represented: Association of British Clinical Diabetologists;
o 0.9% sodium chloride 1L with potassium chloride
Potassium replacement over 4 hours British Society for Endocrinology and Diabetes and Association of
Potassium level (mmol/L) Potassium replacement mmol/L of infusion solution If DKA not resolved review insulin infusion (see BOX 3
o 0.9% sodium chloride 1L with potassium chloride
> 5.5 Nil Action 3) Children’s Diabetes Clinicians; Diabetes Inpatient Specialist Nurse
over 6 hours
3.5-5.5 40 mmol/L If DKA resolved go to BOX 6 (DISN) Group; Diabetes UK; NHS Diabetes (England); Northern Irish
• Add 10% glucose 125ml/hr if blood glucose falls below 14
< 3.5 senior review – additional potassium required momol/L Diabetologists; Society of Acute Medicine; Welsh Endocrine and
Diabetes Society, Scottish Diabetes Group.
Potrebbero piacerti anche
- Facilitated Positional Release FPRDocumento12 pagineFacilitated Positional Release FPRcoahuiltecoNessuna valutazione finora
- Malignant Hyperthermia AlgorithmDocumento1 paginaMalignant Hyperthermia AlgorithmCesar David CaceresNessuna valutazione finora
- Nursing Care PlanDocumento9 pagineNursing Care PlanLura Xstilice B. Galinato100% (1)
- Diabetic Ketoacidosis (DKA)Documento33 pagineDiabetic Ketoacidosis (DKA)Eric Chye Teck100% (1)
- Diabetic KetoacidosisDocumento38 pagineDiabetic KetoacidosisAwatef AbushhiwaNessuna valutazione finora
- Acute Diabetic Ketoacidosis (DKA)Documento21 pagineAcute Diabetic Ketoacidosis (DKA)Madhu Sudhan Pandeya0% (1)
- Diabetic Ketoacidosis Hypoglycemia: DR MD Mamunul Abedin ShimulDocumento18 pagineDiabetic Ketoacidosis Hypoglycemia: DR MD Mamunul Abedin ShimulDr. Mamunul AbedinNessuna valutazione finora
- Sodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyDocumento5 pagineSodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyMorgan Mitchell100% (10)
- Greek TheatreDocumento7 pagineGreek TheatreAllison Nadine Marchand100% (1)
- Dka Guidelines - 2012Documento4 pagineDka Guidelines - 2012djizhieeNessuna valutazione finora
- Diabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyDocumento24 pagineDiabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyGwEn LimNessuna valutazione finora
- DKA Guidelines Version 4.0 28 Dec 2016FINALDocumento4 pagineDKA Guidelines Version 4.0 28 Dec 2016FINALbenNessuna valutazione finora
- DKA Management-2Documento7 pagineDKA Management-2NisaNessuna valutazione finora
- DkaDocumento36 pagineDkaSumit KhetarpalNessuna valutazione finora
- Dka ProtocolDocumento3 pagineDka ProtocolRed DevilNessuna valutazione finora
- MGT of D KetoacidosisDocumento5 pagineMGT of D Ketoacidosisshabatat2002Nessuna valutazione finora
- Diabetc Keto AcidosisDocumento13 pagineDiabetc Keto AcidosisVijiNessuna valutazione finora
- Diabetic Emergencies: Click To Edit Master Subtitle StyleDocumento22 pagineDiabetic Emergencies: Click To Edit Master Subtitle StylenavenNessuna valutazione finora
- Hyperglycaemic Emergencies Inpatient Draft-1-3Documento13 pagineHyperglycaemic Emergencies Inpatient Draft-1-3Cik JaaNessuna valutazione finora
- Diabetic Ketoacidosis (DKA) - Presentation Slide EditedDocumento22 pagineDiabetic Ketoacidosis (DKA) - Presentation Slide EditedTerence Chin0% (1)
- DKA, HONKS, HHS (Theory)Documento26 pagineDKA, HONKS, HHS (Theory)EleanorNessuna valutazione finora
- DKA Canadian ProtocolDocumento2 pagineDKA Canadian Protocolplay_wright2084Nessuna valutazione finora
- The Pathophysiology & Practical Management of Diabetic KetoacidosisDocumento45 pagineThe Pathophysiology & Practical Management of Diabetic KetoacidosisPreetibah PatelNessuna valutazione finora
- Management of Paediatric Diabetic KetoacidosisDocumento21 pagineManagement of Paediatric Diabetic KetoacidosisAsad M AminNessuna valutazione finora
- Diabetic KetoacidosisDocumento27 pagineDiabetic Ketoacidosisjun sianNessuna valutazione finora
- Dka Vs Hhs Edit 1Documento25 pagineDka Vs Hhs Edit 1Razeen RiyasatNessuna valutazione finora
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocumento1 paginaDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- Hyperglycemic Crisis in Acute Care: Purwoko Sugeng HDocumento49 pagineHyperglycemic Crisis in Acute Care: Purwoko Sugeng HBee DanielNessuna valutazione finora
- DM EmergencyDocumento25 pagineDM EmergencyCharleneNessuna valutazione finora
- British Guide Algoritmo CetoacidosisDocumento2 pagineBritish Guide Algoritmo CetoacidosisMon GuevaraNessuna valutazione finora
- Dr. Mohamed Ali Hamedh - DKA - 2023Documento25 pagineDr. Mohamed Ali Hamedh - DKA - 2023ÁýáFáŕőúgNessuna valutazione finora
- 12 - Diabetic Emergencies-DKADocumento13 pagine12 - Diabetic Emergencies-DKABalqis AqisNessuna valutazione finora
- Management of Diabetic KetoacidosisDocumento23 pagineManagement of Diabetic KetoacidosisAjay DherwaniNessuna valutazione finora
- Hyperglycemia, HHS, DKADocumento30 pagineHyperglycemia, HHS, DKAFirdausNessuna valutazione finora
- Diabetes KetoacidosisDocumento23 pagineDiabetes KetoacidosisSalman MajidNessuna valutazione finora
- JBDS 02 Single Page Pathway Amended June 2021Documento2 pagineJBDS 02 Single Page Pathway Amended June 2021Oliverio MéndezNessuna valutazione finora
- Diabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiDocumento23 pagineDiabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiSreekrishnan Trikkur100% (2)
- DKA PosterDocumento2 pagineDKA PosterainizatiNessuna valutazione finora
- Clinical Practice Guidelines: Management of Type 2 Diabetes Mellitus (5 Edition) 2015Documento13 pagineClinical Practice Guidelines: Management of Type 2 Diabetes Mellitus (5 Edition) 2015Azim Abd Razak100% (1)
- Revised DKA 2015 PDFDocumento6 pagineRevised DKA 2015 PDFDr AhmedNessuna valutazione finora
- Guidelines in The Treatment of Hyper Osmolar Non Ketotic Coma (Honk)Documento4 pagineGuidelines in The Treatment of Hyper Osmolar Non Ketotic Coma (Honk)picassowaffleNessuna valutazione finora
- Management of Diabetes Emergencies''Documento85 pagineManagement of Diabetes Emergencies''Princewill SeiyefaNessuna valutazione finora
- Clinical Order Set DKA AdultDocumento2 pagineClinical Order Set DKA AdultBashar Al-HamaidehNessuna valutazione finora
- Diabetic EmergenciesDocumento65 pagineDiabetic EmergenciesManmeet SNessuna valutazione finora
- Diabetic Ketoacidosis (DKA) : BackgroundDocumento9 pagineDiabetic Ketoacidosis (DKA) : Backgroundalyssa_flores_3Nessuna valutazione finora
- Diabetes EmergenciesDocumento7 pagineDiabetes EmergenciesDr.Abdirahman DahirNessuna valutazione finora
- Dka 1Documento45 pagineDka 1jomanabuhaniyehNessuna valutazione finora
- Diabetic Emergencies: 1. Diabetic Ketoacidosis 2. Hyperglycemic Hyperosmolar State 3. HypoglycemiaDocumento24 pagineDiabetic Emergencies: 1. Diabetic Ketoacidosis 2. Hyperglycemic Hyperosmolar State 3. HypoglycemiachooNessuna valutazione finora
- Kad HHS 2019Documento35 pagineKad HHS 2019Friska RamadayantiNessuna valutazione finora
- Diabetic Ketoacidosis PathwayDocumento22 pagineDiabetic Ketoacidosis PathwaySri Nath100% (1)
- Diabetic Ketoacidosis (DKA: Hypoglycemic StatesDocumento41 pagineDiabetic Ketoacidosis (DKA: Hypoglycemic StatesTenzin LhanzeNessuna valutazione finora
- PATIENT WITH ENDOCRINE DYSFUNCTION - PPTX Diabetes EmergenciecyDocumento45 paginePATIENT WITH ENDOCRINE DYSFUNCTION - PPTX Diabetes Emergenciecysembakarani thevagumaranNessuna valutazione finora
- Dka and HHSDocumento25 pagineDka and HHSMouhammad Dawoud100% (2)
- Ketosis DMDocumento33 pagineKetosis DMtiaNessuna valutazione finora
- Early Symptoms: Insidious Increase in Polydipsia and PolyuriaDocumento3 pagineEarly Symptoms: Insidious Increase in Polydipsia and Polyuriabes3rkerNessuna valutazione finora
- Paed Parenteral Fluid ThyDocumento1 paginaPaed Parenteral Fluid ThyZulia Ahmad BurhaniNessuna valutazione finora
- Diabetes Emergencies ComplicationsDocumento30 pagineDiabetes Emergencies Complicationsosamafoud7710Nessuna valutazione finora
- Diabetic Emergencies Case StudiesDocumento32 pagineDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Acute Hyperkalaemia in AdultsDocumento12 pagineAcute Hyperkalaemia in AdultsMeilina FitrianiNessuna valutazione finora
- Contact Details Name: Hospital Telephone:: This Protocol Has 4 PagesDocumento4 pagineContact Details Name: Hospital Telephone:: This Protocol Has 4 PagesCaterina PrepelitaNessuna valutazione finora
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- 400 Calorie MealsDocumento6 pagine400 Calorie MealsAllison Nadine MarchandNessuna valutazione finora
- Name: - Class: - Date: - Hooke's Law ExperimentDocumento2 pagineName: - Class: - Date: - Hooke's Law ExperimentHengLowNessuna valutazione finora
- Student BriefingDocumento3 pagineStudent BriefingAllison Nadine MarchandNessuna valutazione finora
- Meat DishesDocumento277 pagineMeat DishesmilicaNessuna valutazione finora
- 1600 Calorie Meal PlanDocumento4 pagine1600 Calorie Meal PlanChris Theberge100% (110)
- BBA THM Top Up Curriculum Outline TTHTI - 2013 14Documento4 pagineBBA THM Top Up Curriculum Outline TTHTI - 2013 14Allison Nadine MarchandNessuna valutazione finora
- BSC Culinary ManagementDocumento5 pagineBSC Culinary ManagementAllison Nadine MarchandNessuna valutazione finora
- Vinod's GuidelinesDocumento3 pagineVinod's GuidelinesAllison Nadine MarchandNessuna valutazione finora
- Beer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Documento6 pagineBeer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Allison Nadine MarchandNessuna valutazione finora
- B&W Presentation 06 - Decision Making 2 QuantitativeDocumento18 pagineB&W Presentation 06 - Decision Making 2 QuantitativeAllison Nadine MarchandNessuna valutazione finora
- Uncertainty Event 3Documento1 paginaUncertainty Event 3Allison Nadine MarchandNessuna valutazione finora
- B&W Presentation 05 - Decision Making 1 QualitativeDocumento16 pagineB&W Presentation 05 - Decision Making 1 QualitativeAllison Nadine MarchandNessuna valutazione finora
- HBR Ebsco 500 ListDocumento10 pagineHBR Ebsco 500 ListAllison Nadine MarchandNessuna valutazione finora
- Fruit Cake RecipeDocumento2 pagineFruit Cake RecipeAllison Nadine MarchandNessuna valutazione finora
- GMEC2013 14AssignmentAMarkSheetDocumento2 pagineGMEC2013 14AssignmentAMarkSheetAllison Nadine MarchandNessuna valutazione finora
- O L D T E S T A M E N T: Twelve Minor ProphetsDocumento2 pagineO L D T E S T A M E N T: Twelve Minor ProphetsAllison Nadine MarchandNessuna valutazione finora
- Chronicles of NarniaDocumento21 pagineChronicles of NarniaAllison Nadine MarchandNessuna valutazione finora
- Housing DocumentsDocumento1 paginaHousing DocumentsAllison Nadine MarchandNessuna valutazione finora
- How Man SurvivedDocumento7 pagineHow Man SurvivedAllison Nadine MarchandNessuna valutazione finora
- MC Don ArticlesDocumento4 pagineMC Don ArticlesAllison Nadine MarchandNessuna valutazione finora
- Beer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Documento6 pagineBeer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Allison Nadine MarchandNessuna valutazione finora
- India Economy ResearchDocumento5 pagineIndia Economy ResearchAllison Nadine MarchandNessuna valutazione finora
- Alcohol in India - DMITopicGuide2012Documento7 pagineAlcohol in India - DMITopicGuide2012Allison Nadine MarchandNessuna valutazione finora
- Beer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Documento6 pagineBeer Consumption: U.S.-Australia Free Trade Agreement (AUSFTA)Allison Nadine MarchandNessuna valutazione finora
- French AssignmentDocumento14 pagineFrench AssignmentAllison Nadine MarchandNessuna valutazione finora
- GMEC2013 14AssignmentAMarkSheetDocumento2 pagineGMEC2013 14AssignmentAMarkSheetAllison Nadine MarchandNessuna valutazione finora
- India Economy ResearchDocumento5 pagineIndia Economy ResearchAllison Nadine MarchandNessuna valutazione finora
- Chart - Time SpentDocumento2 pagineChart - Time SpentAllison Nadine MarchandNessuna valutazione finora
- ID Pengaruh Self Selected Individual MusicDocumento12 pagineID Pengaruh Self Selected Individual MusicNur AiniNessuna valutazione finora
- Nurs FPX 4020 Assessment 2 Root Cause Analysis and Safety Improvement PlanDocumento5 pagineNurs FPX 4020 Assessment 2 Root Cause Analysis and Safety Improvement PlanEmma WatsonNessuna valutazione finora
- (HSO) Medical Examination FormDocumento1 pagina(HSO) Medical Examination FormKrizel LagundiNessuna valutazione finora
- Block Learning Guide (BLG) : Block II Hematoimmunology System (HIS)Documento6 pagineBlock Learning Guide (BLG) : Block II Hematoimmunology System (HIS)ASTAGINA NAURAHNessuna valutazione finora
- Radiation PhysicsDocumento307 pagineRadiation PhysicsHarley Alejo MNessuna valutazione finora
- Bechara and Damasio, 2005Documento37 pagineBechara and Damasio, 2005Sumer VaidNessuna valutazione finora
- Reimplantation of Avulsed Tooth - A Case StudyDocumento3 pagineReimplantation of Avulsed Tooth - A Case Studyrahul sharmaNessuna valutazione finora
- Accredited BAI Laboratory Animal Shelters 2018Documento8 pagineAccredited BAI Laboratory Animal Shelters 2018ShanaiaNessuna valutazione finora
- Advert MBCHB Bds 2014 Applicants3Documento9 pagineAdvert MBCHB Bds 2014 Applicants3psiziba6702Nessuna valutazione finora
- DBE South African Sign Language National Catalogue 2018Documento7 pagineDBE South African Sign Language National Catalogue 2018Anonymous ozd4aLKhNessuna valutazione finora
- Plant Master Plan (PMP) 2012-2016: Holcim Indonesia Narogong PlantDocumento114 paginePlant Master Plan (PMP) 2012-2016: Holcim Indonesia Narogong PlantSafrin SangiaNessuna valutazione finora
- Impact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsDocumento10 pagineImpact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsValarmathiNessuna valutazione finora
- Dupuytren's ContractureDocumento273 pagineDupuytren's Contractureslaughteringtheposer100% (1)
- Ulvac Ulvoil r7Documento5 pagineUlvac Ulvoil r7Hiskia Benindo PurbaNessuna valutazione finora
- Soares - Como Escolher Um Anestesico Local - 2005 PDFDocumento9 pagineSoares - Como Escolher Um Anestesico Local - 2005 PDFjvb sobralNessuna valutazione finora
- Httpsjkbopee Gov InPdfDownloader Ashxnid 13580&type NDocumento221 pagineHttpsjkbopee Gov InPdfDownloader Ashxnid 13580&type NMONISNessuna valutazione finora
- Madeleine Leininger TFN Reporting NononoDocumento33 pagineMadeleine Leininger TFN Reporting NononoWinter SonataNessuna valutazione finora
- Patomorfologia Prezentacja - KopiaDocumento14 paginePatomorfologia Prezentacja - KopiaOlgaNessuna valutazione finora
- The Trade Effluents (Prescribed Processes and Substances) Regulations 1992Documento2 pagineThe Trade Effluents (Prescribed Processes and Substances) Regulations 1992Lúcio FernandesNessuna valutazione finora
- AREMT Registration Form 2014Documento3 pagineAREMT Registration Form 2014Reinhold AcacioNessuna valutazione finora
- NFPA Codes & Standards - 10Documento1 paginaNFPA Codes & Standards - 10karpanaiNessuna valutazione finora
- Intussusception: DR Phillipo Leo ChalyaDocumento19 pagineIntussusception: DR Phillipo Leo ChalyaSibabaong'ombe MasakaNessuna valutazione finora
- Jain College, Bangalore Mock Paper - 1, March - 2021 II PUC - EnglishDocumento6 pagineJain College, Bangalore Mock Paper - 1, March - 2021 II PUC - EnglishSuchit KarnamNessuna valutazione finora
- Caravan Tourism in West BengalDocumento2 pagineCaravan Tourism in West BengalUddipan NathNessuna valutazione finora
- Accomplishment ReportDocumento5 pagineAccomplishment ReportTuTit100% (1)
- HR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenDocumento2 pagineHR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenMiltonGreenNessuna valutazione finora
- Gn-31 Qms Cad (Dec 2012) FinalDocumento19 pagineGn-31 Qms Cad (Dec 2012) FinalSeanNessuna valutazione finora
- ACTIVITY DESIGN-first AidDocumento4 pagineACTIVITY DESIGN-first AidShyr R Palm0% (1)
- MSDS Bleach PDFDocumento5 pagineMSDS Bleach PDFAlfonso Alejandro Loayza RodriguezNessuna valutazione finora