Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Gastroenteritis Leaflet Final
Caricato da
Riony GusbaniansyahCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Gastroenteritis Leaflet Final
Caricato da
Riony GusbaniansyahCopyright:
Formati disponibili
How long will the symptoms last?
Useful Contacts Oxfordshire
Clinical Commissioning Group
Diarrhoea usually lasts five to seven days but may
continue for up to two weeks. Vomiting usually does
If you need advice:
Find your local pharmacy at www.nhs.uk
Gastroenteritis
not last for more than three to four days. Health Visitor: .......................................................... (diarrhoea and/or vomiting)
Please see the traffic light advice overleaf to help you
monitor the condition of your child. Your GP Surgery: ...................................................... Advice Sheet for parents and carers of children
Please contact your GP when the surgery is open
Unwell children will often refuse fluids
or call NHS 111 when the GP surgery is closed.
but can be persuaded, so it is important What Is Gastroenteritis?
NHS 111 provides advice for urgent care needs.
to persevere. Keep trying to give them NHS 111 is available 24 hours a day, 365 days a year. Calls from
drinks. Little and often is best. landlines and mobile phones are free. • Gastroenteritis is an upset tummy that can cause
diarrhoea and / or vomiting.
For online advice and information NHS Choices: www.nhs.uk • It is caused by viruses, is mild and can usually be
managed at home.
Caring for your child at home • Your child may first have tummy ache and fever
• Most children with diarrhoea and vomiting get better
• Most children can be looked after at home with simple very quickly, but some children can get worse.
advice, time and patience.
• One of the main risks of gastroenteritis in children and
• The most important thing is to replace fluid your child
will be losing due to vomiting and / or diarrhoea. especially babies is they may become dehydrated
• It is fine if they do not want to eat, drinks are most • You need to regularly check your child and follow the
important and food can wait till they are better advice in this leaflet
• Make sure you try and continue breastfeeding or
bottle-feeding
• For a child under one, you can give small sips every Preventing Dehydration
few minutes (using a teaspoon or a plastic syringe, try
5mls every five minutes). With the plastic syringe aim Signs of dehydration include:
the fluids into the side of the baby’s mouth as they If
If you
you are
are worried
worried about
about your
your • Dry mouth
may swallow it more easily then. child, trust your instincts. • Dry tongue and lips
• For all children, give drinks little and often e.g. every child, trust your instincts. • Less tears when crying
Contactyour
yourGPGP • Sunken eyes
oror dial 111.
10 minutes. If they are thirsty and take too much at a
time ,it make cause them to vomit. Contact dial NHS 111. • Passing less urine than normal
• For older children, try using ice lollies or encourage • Weakness
drinking through a straw Based on: Diarrhoea and vomiting in children
under 5 2009 NICE clinical guideline 84 • Being irritable or lethargic
TOP TIPS The most important thing is to replace the fluid
that your child will be losing when they have diarrhoea
• Oral Rehydration Solution (ORS) such as Diaorlyte and/ or vomiting
or Electrolade should not be used in infants under Published 1st December 2014 Review 30th November 2015
3 months without speaking to your GP. In children
under a year it should be added to freshly boiled This guidance is written in the following context
GOOD FLUIDS BAD FLUIDS
and cooled water according to the directions. In This document was arrived at after careful consideration of the evidence available including
but not exclusively NICE, SIGN, EBM data and NHS evidence, as applicable. Healthcare
older children it can be added to full sugar squash professionals are expected to take it fully into account when exercising their clinical Oral Rehydration Sachets (see Fruit Juice
to taste nicer (blackcurrant works well!). judgement. The guidance does not, however, override the individual responsibility of advice in Top Tips) Fizzy drinks (can make
healthcare professionals to make decisions appropriate to the circumstances of the individual
• It is useful to keep a record of the number of drinks patient in consultation with the patient and / or carer. Water diarrhoea worse)
and the number of wees that your child has had Squash (not sugar free)
each day This was approved by Oxfordshire CCG Clinical Ratification Group on Milk
4th December 2014.
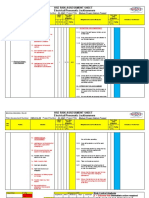
What to keep in your medicine cabinet What do I do if my child has gastroenteritis? (traffic light advice)
Keep the following items in your medicine cabinet
ready for when you may need them: Most children with diarrhoea and/or vomiting get better very quickly but some children can
• Oral Rehydration Solution (ORS) Sachets (eg. get worse. You need to regularly check your child and follow the advice in this leaflet.
Dioralyte or Electrolade)
• Liquid Paracetamol (eg. Calpol / Medinol)
• Liquid Ibuprofen (eg. Nurofen) – Please note that You need EMERGENCY HELP
if your child has been diagnosed with Asthma, If your child has signs of dehydration and: Call 999 - you need to be seen at the A&E department
Ibuprofen is not recommended, unless discussed • Becomes unresponsive
first with your doctor. Nearest Hospitals (open 24 hours, seven days a week):
• or is breathing faster than usual •John Radcliffe, Oxford
Please check the Use-By dates and keep out of
the reach of children. These medicines are all
• or has unusually pale or mottled skin
• or has cold extremities (colder hands and
u •Horton, Banbury
•Royal Berkshire, Reading
available over the counter from a pharmacist. The
pharmacy or supermarket own brands are cheaper feet than usual) •Great Western, Swindon
RED •Stoke Mandeville, Aylesbury
and work just as well. If you are unsure , ask your
pharmacist. Bring your child’s Red Book with you.
If your child:
Preventing the spread of gastroenteritis • Appears to be getting worse or if you
are worried
Hand washing - The most effective way is for you
• or is getting more thirsty despite drinking Seek Medical Advice Today
• or is not drinking
and/or your child to wash your hands with liquid • or has signs of dehydration such as a dry Ring your GP surgery - Mon-Fri 8am to 6.30pm
soap ideally in warm running water and then mouth, no tears, sunken eyes, the soft spot
dry them carefully: at the top of the head is more dipped in Most practices will want to speak to you on the
• After going to the toilet
• After changing nappies
than usual, more sleepy than usual, they
wee less or seem generally unwell u phone first to give you medical advice. They will
arrange to see your child if it is appropriate
• Before touching food • or has blood in the stool (poo)
AMBER • or has had 6 or more bouts of diarrhoea in At all other times and bank holidays call NHS 111
Your child should not:
• Share his or her towels with anyone 24 hours
• or has 3 or more vomits in 24 hours Bring your child’s Red Book with you.
• Go to school or any other childcare facility until
48 hours after the last episode of diarrhoea • or has a high temperature
and or vomiting • or is in constant pain
• Swim in swimming pools until two weeks after
the diarrhoea has stopped.
Self care
Using the advice on this leaflet you can care for
Most children with diarrhoea and /or your child at home. The most important advice is
u
Children who are younger than one year or
vomiting can be safely looked after to keep your child well hydrated.
were born at a low birth weight are more
at home If you feel you need advice please contact your
vulnerable.
If your child has none of the symptoms Health Visitor, GP surgery or your local
If you have concerns about looking after your child in the red or amber boxes above you pharmacy (follow the links at www.nhs.uk)
at home, please contact your GP or call NHS 111.
GREEN can look after them at home. You can also call NHS 111
Potrebbero piacerti anche
- English File: Grammar, Vocabulary, and PronunciationDocumento4 pagineEnglish File: Grammar, Vocabulary, and PronunciationFirstName100% (2)
- Holistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaDocumento4 pagineHolistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaPriyesh Dubey100% (2)
- English Gastroenteritis PDFDocumento2 pagineEnglish Gastroenteritis PDFkatyweymNessuna valutazione finora
- Job Description: Jette Parker Young Artists ProgrammeDocumento2 pagineJob Description: Jette Parker Young Artists ProgrammeMayela LouNessuna valutazione finora
- 02 - Zapatos Vs PeopleDocumento2 pagine02 - Zapatos Vs PeopleRhev Xandra Acuña67% (3)
- Ed-Child Febrile FitDocumento2 pagineEd-Child Febrile Fitmanish708345Nessuna valutazione finora
- Pediatric OSCEs 2016 ModifiedDocumento113 paginePediatric OSCEs 2016 ModifiedAbdulKhaleq AlkadimiNessuna valutazione finora
- TonsillitisDocumento2 pagineTonsillitisJohn ChalukuluNessuna valutazione finora
- Cancer Treatment, Going Home After (Let's Talk About... Pediatric Brochure) SpanishDocumento4 pagineCancer Treatment, Going Home After (Let's Talk About... Pediatric Brochure) SpanishY GNessuna valutazione finora
- ColicDocumento2 pagineColicYeliz SzeremyNessuna valutazione finora
- What Is ColicDocumento2 pagineWhat Is ColicVinod SharmaNessuna valutazione finora
- Febrile Autism AdhdDocumento57 pagineFebrile Autism Adhdj2x5h4ffbbNessuna valutazione finora
- Gastroenteritis Pregnancy July 2019Documento2 pagineGastroenteritis Pregnancy July 2019Tochukwu IgboanugoNessuna valutazione finora
- Preparing Your Medicine Cabinet For A New BabyDocumento2 paginePreparing Your Medicine Cabinet For A New BabyWilliam ImpNessuna valutazione finora
- ColicDocumento6 pagineColicRucelyn CampitaNessuna valutazione finora
- Colic EDocumento1 paginaColic EAlbraa Ibn MalikNessuna valutazione finora
- Bedwetting: Signs of A Medical ProblemDocumento2 pagineBedwetting: Signs of A Medical Problemgk0% (1)
- Fever in Children PDFDocumento2 pagineFever in Children PDFDaerobbi NurwansyahNessuna valutazione finora
- Course Task #8Documento6 pagineCourse Task #8ANGEL MICAH DAVIDNessuna valutazione finora
- Basic Training For Barangay Health Workers Calasiao, PangasinanDocumento18 pagineBasic Training For Barangay Health Workers Calasiao, Pangasinan700AIDANNessuna valutazione finora
- EnuresisDocumento4 pagineEnuresisDalene KirstenNessuna valutazione finora
- ColicDocumento6 pagineColicGracia NievesNessuna valutazione finora
- BedwettingDocumento12 pagineBedwettingVenus SteveNessuna valutazione finora
- Tips For Families Series SomaliDocumento8 pagineTips For Families Series SomaliOmar AwaleNessuna valutazione finora
- Infant Colic, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandInfant Colic, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- GastroenteritisDocumento2 pagineGastroenteritisTiara Sekar AyudhipashaNessuna valutazione finora
- Untitled DocumentDocumento5 pagineUntitled DocumentNawanjan RupasingheNessuna valutazione finora
- Integrated Management of Childhood IllnessDocumento43 pagineIntegrated Management of Childhood IllnessMark LugtuNessuna valutazione finora
- BedDocumento6 pagineBedNiamh_O_Shea_6318Nessuna valutazione finora
- Guidelines For New Diarrhea Treatment Protocols: For Community-Based Healthcare WorkersDocumento23 pagineGuidelines For New Diarrhea Treatment Protocols: For Community-Based Healthcare WorkersFebria Valentine AritonangNessuna valutazione finora
- NauseaDocumento2 pagineNauseaRomadhona KhoiriNessuna valutazione finora
- Common Newborn Problems Infantile Colic: Helen Trotman-Edwards Senior Lecturer Department of Child HealthDocumento7 pagineCommon Newborn Problems Infantile Colic: Helen Trotman-Edwards Senior Lecturer Department of Child Healthgdudex118811Nessuna valutazione finora
- Crying Infant: Review ArticleDocumento5 pagineCrying Infant: Review ArticleLê Nhật HoàngNessuna valutazione finora
- Febrile Seizures StandardDocumento3 pagineFebrile Seizures StandardRizky FajriNessuna valutazione finora
- Common Child InfectionsDocumento5 pagineCommon Child InfectionsAnonymous L3W8LlpMPWNessuna valutazione finora
- Oral Rehydration Salts 2Documento2 pagineOral Rehydration Salts 2William ImpNessuna valutazione finora
- Survival-Guide Hyperemesis GravidarumDocumento7 pagineSurvival-Guide Hyperemesis GravidarumLullaby LullabyNessuna valutazione finora
- Pneumonia PDFDocumento3 paginePneumonia PDFSari RamadhanNessuna valutazione finora
- Gastroenteritis (Gastro) : Signs and Symptoms of GastroDocumento2 pagineGastroenteritis (Gastro) : Signs and Symptoms of GastrokatyweymNessuna valutazione finora
- Crying - Dr. Shwan: Causes?!Documento2 pagineCrying - Dr. Shwan: Causes?!Muhammed BarznjiNessuna valutazione finora
- Tic Disorder LeafletDocumento2 pagineTic Disorder LeafletAndreia SilvaNessuna valutazione finora
- Kawasaki DiseaseDocumento2 pagineKawasaki DiseasejaehankimNessuna valutazione finora
- Anal DilationDocumento3 pagineAnal DilationrynaldiandriansyaNessuna valutazione finora
- Diarrhea EDocumento1 paginaDiarrhea Eabdalballah1151Nessuna valutazione finora
- Succinic Acid For Mitchondrial Disease 2Documento2 pagineSuccinic Acid For Mitchondrial Disease 2William ImpNessuna valutazione finora
- Common DiseasesDocumento15 pagineCommon DiseasesKoyal HowtarNessuna valutazione finora
- Tonsillitis in Children: Acute Paediatric Department Information For Parents, Carers and Older ChildrenDocumento2 pagineTonsillitis in Children: Acute Paediatric Department Information For Parents, Carers and Older Childrengulfam321Nessuna valutazione finora
- Childhood IllnessesDocumento12 pagineChildhood IllnessesRonea MiaNessuna valutazione finora
- KALIBANGADocumento3 pagineKALIBANGAPhil Edward Marcaida VillanuevaNessuna valutazione finora
- Colico Del LactanteDocumento5 pagineColico Del LactanteGil Alfonso Guzmán MaldonadoNessuna valutazione finora
- Common Diseases of The InfantDocumento131 pagineCommon Diseases of The Infanthed-janquillanoNessuna valutazione finora
- Vomiting in ChildrenDocumento3 pagineVomiting in Childrenartz_dhanaNessuna valutazione finora
- Sodium Phenylbutyrate For Urea Cycle Disorders 1Documento2 pagineSodium Phenylbutyrate For Urea Cycle Disorders 1William ImpNessuna valutazione finora
- Bed WettingDocumento5 pagineBed WettingLeah ValenciaNessuna valutazione finora
- Crying-And-Feeding-Issues - CCG LeafletDocumento16 pagineCrying-And-Feeding-Issues - CCG LeafletWaleed AsadNessuna valutazione finora
- Covid19 Advice For Parents When Child Unwell or Injured PosterDocumento1 paginaCovid19 Advice For Parents When Child Unwell or Injured PosterPsiho PupelNessuna valutazione finora
- QUIZ-2-NCM-109-LECTURE (NOVENO, Jamaica N2A)Documento4 pagineQUIZ-2-NCM-109-LECTURE (NOVENO, Jamaica N2A)Kenneth NovenoNessuna valutazione finora
- Diarrhea NCPDocumento34 pagineDiarrhea NCPchezian smartNessuna valutazione finora
- OBS Nausea eDocumento2 pagineOBS Nausea epseshagiriraoNessuna valutazione finora
- Bowel Management ProgramDocumento28 pagineBowel Management ProgramPCMC Dietitians NDDNessuna valutazione finora
- Addressing Common Developmental Concern Among Infants: Care of Mother, Child at Risk or With Problems (Acute & Chronic)Documento50 pagineAddressing Common Developmental Concern Among Infants: Care of Mother, Child at Risk or With Problems (Acute & Chronic)Marie Ashley CasiaNessuna valutazione finora
- Care of The Perineum After The Birth of Your Baby: Oxford University HospitalsDocumento8 pagineCare of The Perineum After The Birth of Your Baby: Oxford University HospitalsSharief SkNessuna valutazione finora
- Care of The Child Applying Integrated Management of Childhood Illnesses (Imci)Documento22 pagineCare of The Child Applying Integrated Management of Childhood Illnesses (Imci)Jesena SalveNessuna valutazione finora
- MSDS Blattanex GelDocumento5 pagineMSDS Blattanex GelSadhana SentosaNessuna valutazione finora
- SoapDocumento10 pagineSoapAira RamoresNessuna valutazione finora
- 9 Electrical Jack HammerDocumento3 pagine9 Electrical Jack HammersizweNessuna valutazione finora
- Chelsea Bellomy ResumeDocumento1 paginaChelsea Bellomy Resumeapi-301977181Nessuna valutazione finora
- Excel For MAC Quick Start GuideDocumento4 pagineExcel For MAC Quick Start GuideMalaquías HuamánNessuna valutazione finora
- 39 Nts General Merit List 22 Mar 18Documento26 pagine39 Nts General Merit List 22 Mar 18Lakshmi VedanarayananNessuna valutazione finora
- The Malacca Strait, The South China Sea and The Sino-American Competition in The Indo-PacificDocumento21 pagineThe Malacca Strait, The South China Sea and The Sino-American Competition in The Indo-PacificRr Sri Sulistijowati HNessuna valutazione finora
- Computer Science Past Papers MCQS SolvedDocumento24 pagineComputer Science Past Papers MCQS SolvedLEGAL AFFAIRS DIVISION100% (1)
- Bos 22393Documento64 pagineBos 22393mooorthuNessuna valutazione finora
- Palladium Skill Book 1a.Documento10 paginePalladium Skill Book 1a.Randy DavisNessuna valutazione finora
- Chapter 11 Towards Partition Add Pakistan 1940-47Documento5 pagineChapter 11 Towards Partition Add Pakistan 1940-47LEGEND REHMAN OPNessuna valutazione finora
- SurrealismDocumento121 pagineSurrealismLaurence SamonteNessuna valutazione finora
- Bartolome vs. MarananDocumento6 pagineBartolome vs. MarananStef OcsalevNessuna valutazione finora
- Timothy L. Mccandless, Esq. (SBN 147715) : Pre-Trial Documents - Jury InstructionsDocumento3 pagineTimothy L. Mccandless, Esq. (SBN 147715) : Pre-Trial Documents - Jury Instructionstmccand100% (1)
- 4 Thematic AnalysisDocumento32 pagine4 Thematic Analysisapi-591181595Nessuna valutazione finora
- Gprs/Umts: IAB Workshop February 29 - March 2, 2000 Jonne Soininen NokiaDocumento34 pagineGprs/Umts: IAB Workshop February 29 - March 2, 2000 Jonne Soininen NokiaSajid HussainNessuna valutazione finora
- CS3 Backup 2023 01 31 02 41Documento1 paginaCS3 Backup 2023 01 31 02 41Fans Page1Nessuna valutazione finora
- Musical Notes and SymbolsDocumento17 pagineMusical Notes and SymbolsReymark Naing100% (2)
- 2 - (Accounting For Foreign Currency Transaction)Documento25 pagine2 - (Accounting For Foreign Currency Transaction)Stephiel SumpNessuna valutazione finora
- A Manual For A Laboratory Information Management System (Lims) For Light Stable IsotopesDocumento131 pagineA Manual For A Laboratory Information Management System (Lims) For Light Stable IsotopesAlvaro Felipe Rebolledo ToroNessuna valutazione finora
- COPARDocumento21 pagineCOPARLloyd Rafael EstabilloNessuna valutazione finora
- King of Chess American English American English TeacherDocumento6 pagineKing of Chess American English American English TeacherJuliana FigueroaNessuna valutazione finora
- BCMSN30SG Vol.2 PDFDocumento394 pagineBCMSN30SG Vol.2 PDFShemariyahNessuna valutazione finora
- 2007.01 What Does Jesus Think of Science?Documento2 pagine2007.01 What Does Jesus Think of Science?William T. PelletierNessuna valutazione finora
- Soft Skills PresentationDocumento11 pagineSoft Skills PresentationRishabh JainNessuna valutazione finora
- 3 Pseudoscience and FinanceDocumento11 pagine3 Pseudoscience and Financemacarthur1980Nessuna valutazione finora