Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Articulos de Biotipos
Caricato da
SUSAN LUCINDA MEJIA TIPAZTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Articulos de Biotipos
Caricato da
SUSAN LUCINDA MEJIA TIPAZCopyright:
Formati disponibili
Periodontics
Gingival biotype: a review
Zeinab Rezaei Esfahrood, DDS, MS n Mahdi Kadkhodazadeh, DDS, MS n Mohammad Reza Talebi Ardakani, DDS, MS
Among the factors that may impede success in dental treatments, This article reviews the characteristics of various gingival biotypes and
gingival biotype is the greatest cause of concern, particularly affecting the many ways to determine them.
the outcomes of periodontal therapy, root coverage procedures, and Received: December 7, 2011
implant placement. Different tissue biotypes respond differently to Accepted: March 19, 2012
inflammation and to surgical and restorative treatment; consequently, it
is crucial to identify tissue biotype before treatment. Special care must Keywords: gingiva, teeth, implant, bone
be taken when treatment planning for cases with a thin gingival biotype.
I
n 1969, Ochsenbein & Ross indicated The alveolar crest in a healthy periodon- Differences in gingival and osseous
that there were 2 main types of gingival tium is positioned approximately 2 mm architecture have a significant impact on
anatomy— flat and highly scalloped.1 more apically than the cementoenamel the outcome of treatments. Therefore,
The authors reported that flat gingiva was junction (CEJ) and mimics the scallop gingival biotype should be evaluated at
associated with a square tooth form, while of the CEJ. In the normal and high scal- the start of the treatment plan for the
scalloped gingiva was associated with loped gingival form, there is more tissue most esthetic results. The characteristics
a tapered tooth form. The authors also coronal to the interproximal bone than of thin and thick gingiva are listed in the
proposed that the gingival contour closely the facial bone. As such, higher scalloped Table.2,3,10,13,23,24
mimics the contour of the underlying gingiva are at greater risk for gingival loss
alveolar bone.1 The term periodontal bio- after tooth extraction.12 Gingival biotype and labial
type was used later by Seibert & Lindhe, In a 1994 article, Kois examined crestal plate thickness
who classified the gingiva as either thin- bone levels and classified them as normal For patients with a thin gingival biotype,
scalloped or thick-flat.2 In a study by De (crestal bone level is 3 mm apical to the extreme care should be taken during
Rouck et al, the thin gingival biotype CEJ), high (crestal bone level is <3 mm extraction to prevent labial plate fracture.
occurred in one-third of the study popu- apical to the CEJ), and low (crestal bone Cook et al evaluated the correlation
lation and was most prominent among level is >3 mm apical to the CEJ and between labial plate thickness and thin or
women, while the thick gingival biotype found in patients with recession).11 thick gingival biotypes—using informa-
occurred in two-thirds of the study popu- Gingival biotype can affect the results tion obtained from cone beam computed
lation and occurred mainly among men.3 of periodontal therapy, root coverage tomography (CBCT), diagnostic impres-
Studies have confirmed that central procedures, and implant placement.3,13-16 sions, and clinical examinations of maxil-
incisors with a narrow crown form are It has been shown that patients with lary anterior teeth—and concluded that
at greater risk of recession than incisors thin gingival biotype were more a significant association existed between
with a wide, square form.4,5 According likely to experience gingival recession gingival biotype and labial plate thick-
to the literature, the alveolar bone and following nonsurgical periodontal ness.25 According to Fu et al, the thickness
the gingival margin surrounding a tooth therapy.13 Mucogingival problems may of the labial gingival tissue has a moderate
with pronounced cervical convexity are result from orthodontic movement of association with the underlying bone.26
located more apically than they would teeth away from the alveolar process,
be in teeth with flat surfaces, suggesting particularly among patients with thin Gingival biotype and Schneiderian
that the gingival margin is affected by the periodontium.17,18 The level of gingival membrane thickness
cervical convexity of the crown.6,7 thickness before regenerative surgery The most common complication during
Generally, facial gingival is thicker was found to be a predicting factor for sinus graft procedures is perforation
in the maxilla than in the mandible. further recession.19,20 Kois proposed that of the sinus membrane. This condi-
Maxillary canines and mandibular first postsurgery clinical results were strongly tion may occur after the sinus floor is
premolars have the thinnest gingiva (0.7- associated with the gingival and alveolar accessed through the lateral wall or the
0.9 mm), with a relatively high incidence crest form.12 In cases with low alveolar ridge crest.27-29 Clinical observations have
of gingival recession.8,9 According to crest position, an increased susceptibility prompted clinicians to suggest a correla-
Weisgold, individuals with a thin, scal- for gingival recession may expose restor- tion between the sinus membrane thick-
loped gingiva demonstrated a greater prev- ative margins when finish lines are placed ness and the risk of perforation.30,31
alence of recession.10 Scalloped gingiva can intracrevicularly. Patients with thick A 2008 study by Aimetti et al took
be categorized as high, normal, and flat. gingiva appear less likely to experience maxillary mucosal biopsies from the sinus
The normal scalloped gingiva is 4-5 mm gingival recession after surgical or restor- floor during otorhinolaringologic surgi-
coronal to the free gingival margin.11 ative therapy.19-22 cal interventions, and measured gingival
14 July 2013 General Dentistry www.agd.org
thickness in the area of the maxillary
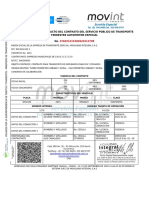
anterior teeth.32 The authors reported that Table. Characteristics of thin and thick gingiva.
the average thickness of the Schneiderian
membrane was 0.97 ± 0.36 mm. Patients Characteristics of thin gingiva Characteristics of thick gingiva
with thick gingiva had a sinus mucosa Narrow zone of keratinized tissue Large amount of keratinized tissue
that was 1.26 ± 0.14 mm thick, compared Gingival thickness is <1.5 mm, width is 3.5-5 mm Gingival thickness is ≥2.0 mm, width is 5-6 mm
to 0.61 ± 0.15 mm thickness among Pronounced scalloped soft tissue and bony Flat soft tissue and bony architecture
patients with thin gingiva. The results architecture Gingival margins usually are coronal to the
showed that gingival thickness is a reli- Slight gingival recession cementoenamel junction
able factor for predicting sinus membrane
Dehiscence and fenestrations are usual findings Thick bony plates
thickness.32 Additional research must be
in thin underlying bone Thick marginal bone
performed to confirm these data.
Thin marginal bone Broad, more apically located contact areas
Tissue biotype in implant Small proximal contact areas located near Square anatomic crowns
treatment planning the incisal edge
Quadratic tooth form
Studies have examined how mucosal Triangular anatomic crowns
Marked cervical convexities in the crown
thickness and biologic width affect crestal Slender tooth form
Deep pocket and intrabony defect formation
bone loss around implants.33,34 A 1996 Subtle cervical convexities in the crown following disease
animal study by Berglundh & Lindhe con- Gingival recession following disease
cluded that thin gingival tissue can lead
to marginal bone loss during formation of
the peri-implant biologic width.35 Another
histologic study by Huang et al reported A 2007 study by Jung et al evaluated key factors in how mucogingival defects
that implant sites with thin mucosa were different materials (titanium, ceramized are treated.43 In cases involving root
prone to angular bone defects, while stable titanium, zirconium, and ceramized zirco- coverage surgeries, a flap thickness of
crestal bone was maintained in implants nium) that were placed under the vestibular 0.8-1.2 mm produced more predictable
surrounded by thick mucosa.14 According mucosa of mandibles of pigs, along with outcomes.14,15,20 An initial gingival thick-
to Abrahamsson et al, thick tissues (that connective tissue grafts of varying thick- ness was found to be the most predictable
is, ≥2.5 mm) can avoid significant crestal ness.40 Tissue color was measured by a spec- factor for predicting the success of com-
bone recession; however, the authors rec- trophotometer. All of the materials changed plete root coverage procedures.20 There is
ommend avoiding supracrestal placement the color of the thin (1.5 mm) mucosa, a correlation between flap thickness and
of implants if an implant is surrounded with titanium producing the greatest complete root coverage.15
by a thin biotype.36 change. In normal (2.0 mm) mucosa, only
Gingival recession is one of the most titanium altered the color. In thick (3.0 Gingival biotype assessment
common complications resulting from mm) mucosa, no changes were observed Many methods (both invasive and non-
single anterior tooth implant placement.37 from any of the materials. The results sug- invasive) have been used to evaluate the
Gingival biotype is a diagnostic key for gest that it is preferable to use pillars of thickness of facial gingival and other parts
predicting the esthetic success of an zirconium for thin peri-implant mucosa, to of the masticatory mucosa. These meth-
implant.12 According to Evans & Chen, avoid color changes of the mucosa.40 ods include conventional histology on
gingival recession increases in patients cadaver jaws, injection needles, transgin-
with thin biotypes immediately after Gingival biotype and ridge gival probing, histologic sections, cepha-
single implant restorations.22 Furthermore, preservation lometric radiographs, probe transparency,
papilla between immediate single implants A thin gingival biotype is associated with a ultrasonic devices, and CBCT.4,5,8,13,20,44-58
and adjacent teeth is significantly associ- thin alveolar plate; more ridge remodeling
ated with a thick gingival biotype. Patients has been found in this biotype when com- Visual evaluation
with thick-flat mucosa tended to maintain pared with thick periodontal biotype. Ridge Simple visual evaluation is used in clinical
the implant papillae height.38 preservation should be considered for most practice to identify the gingival biotype;
Dramatic alveolar resorption in the thin biotype cases. Preservation of alveolar however, it may not be considered a reli-
apical and lingual direction is possible in dimensions (such as socket preservation or able method, as it cannot be used to assess
patients with a thin biotype.39 The loss of ridge preservation techniques after tooth the degree of gingival thickness.1,2,5
peri-implant tissues may result in facial extraction) is critical for achieving optimal
plate loss, with the implant taking on a esthetic results in thin biotypes; atraumatic Probe transparency
grayish color; additional bone and soft extraction also may be necessary.41,42 The gingival tissue’s ability to cover any
tissue grafting surgeries may be neces- underlying material’s color is necessary
sary in such cases. Immediate placement Tissue biotype and root coverage for achieving esthetic results, especially
of an implant in a thick gingival biotype According to McFall, tissue thickness in in cases of implant and restorative den-
offers predictable results.39 the recipient site and the donor site are tistry, where subgingival alloys are used
www.agd.org General Dentistry July 2013 15
Periodontics Gingival biotype: a review
widely.59,60 Using a metal periodontal superior diagnostic ability. Fu et al 10. Weisgold A. Contours of the full crown restoration.
probe in the sulcus to evaluate gingival measured the thickness of labial gingiva Alpha Omegan. 1977;70(3):77-89.
11. Kois JC. Altering gingival levels: The restorative con-
tissue thickness is the simplest way to and bone and reported no statistically
nection. Part 1: biologic variables. J Esthet Dent. 1994;
determine gingival biotype; with a thin significant difference between the clinical 6(1):3-7.
biotype, the tip of the probe is visible measurements made with a caliper and 12. Kois JC. Predictable single-tooth peri-implant esthetics:
through the gingiva. This method is mini- radiographic measurements utilizing CBCT five diagnostic keys. Compend Contin Educ Dent. 2004;
mally invasive, and periodontal probing scans; however, CBCT measurements may 25:895-900.
13. Claffey N, Shanley D. Relationship of gingival thickness
procedures are performed routinely during be a more objective method than direct and bleeding to loss of probing attachment in shallow
periodontal and implant treatments.50 measurement.26 A plastic lip, tongue retrac- sites following nonsurgical periodontal therapy. J Clin
tors, and wooden spatulas can be used to Periodontol. 1986;13(7):654-657.
Modified caliper better visualize soft tissue margins.58 14. Huang LH, Neiva RE, Wang HL. Factors affecting the
outcomes of coronally advanced flap root coverage
A tension-free caliper can only be used at
procedure. J Periodontol. 2005;76(10):1729-1734.
the time of surgery and cannot be used for Conclusion 15. Hwang D, Wang HL. Flap thickness as a predictor of
pretreatment evaluation. A 2010 study by By understanding the nature of tissue root coverage: a systematic review. J Periodontol.
Kan et al of the facial gingival biotype in biotypes, clinicians can employ appropri- 2006;77(10):1625-1634.
maxillary anterior teeth compared visual ate periodontal management to minimize 16. Zigdon H, Machtei EE. The dimensions of keratinized
mucosa around implants affect clinical and immuno-
evaluations, the use of a periodontal probe, tissue resorption and provide more favor- logical parameters. Clin Oral Implants Res. 2008;
and direct measurements with a tension-free able results after dental treatment. A 19(4):387-392.
caliper.61 The authors reported a statistically clear cut classification system should be 17. Foushee DG, Moriarty JD, Simpson DM. Effects of man-
significant difference between visual assess- considered to facilitate gingival biotype dibular orthognathic treatment on mucogingival tis-
sues. J Periodontol. 1985;56(12):727-733.
ment and both the periodontal probe and diagnosis in a practical manner.
18. Zachrisson BU. Orthodontics and periodontics. In:
the tension-free caliper; however, there was Lindhe J, Karring T, Lang NP, eds. Clinical Periodon-
no statistically significant difference when Author information tology and Implant Dentistry, 3rd ed. Copenhagen:
comparing the periodontal probe assess- Dr. Esfahrood is an assistant professor, Munksgaard; 1997:741-793.
ment and the tension-free caliper. Based Department of Periodontics, Dental 19. Anderegg CR, Metzler DG, Nicoll BK. Gingiva thickness
in guided tissue regeneration and associated recession
on these results, a periodontal probe in the School, Shahid Beheshti University of at facial furcation defects. J Periodontol. 1995; 66(5):
sulcus is an adequately reliable and objective Medical Sciences, Evin, Tehran, Iran, 397-402.
way to evaluate tissue thickness, whereas where Drs. Kadkhodazadeh and Ardakani 20. Baldi C, Pini-Prato G, Pagliaro U, et al. Coronally ad-
visual evaluation of the gingival biotype by are associate professors. vanced flap procedure for root coverage. Is flap thick-
ness a relevant predictor to achieve root coverage? A
itself is not as reliable as the periodontal
19-case series. J Periodontol. 1999; 70(9):1077-1084.
probe or the tension-free caliper.61 References 21. Pontoriero R, Carnevale G. Surgical crown lengthen-
1. Ochsenbein C, Ross S. A reevaluation of osseous sur- ing: a 12-month clinical wound healing study. J Perio-
gery. Dent Clin North Am. 1969;13(1):87-102.
Transgingival probing dontol. 2001;72(7):841-848.
2. Seibert JL, Lindhe J. Esthetics and periodontal therapy. 22. Evans CD, Chen ST. Esthetic outcomes of immediate
Gingival thickness can be measured by In: Lindhe J, ed. Textbook of Clinical Periodontology, implant placements. Clin Oral Implants Res. 2008;
using a periodontal probe; a thick biotype 2nd ed. Copenhangen, Denmark: Munksgaard; 1989: 19(1):73-80.
has a thickness of ≥1.5 mm.45 However, 477-514. 23. Muller HP, Eger T. Masticatory mucosa and periodontal
such measurements can be affected by the 3. De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. phenotype: a review. Int J Periodontics Restorative
The gingival biotype revisited: transparency of the Dent. 2002;22(2):172-183.
precision of the probe, the angulation of periodontal probe through the gingival margin as a 24. Kao RT, Fagan MC, Conte GJ. Thick vs. thin gingival
the probe, and the distortion of the tissue method to discriminate thin from thick gingiva. J Clin biotypes: a key determinant in treatment planning for
during probing.26 Periodontol. 2009;36(5):428-433. dental implants. J Calif Dent Assoc. 2008;36(3):193-
4. Olsson M, Lindhe J. Periodontal characteristics in indi- 198.
viduals with varying form of the upper central incisors.
Ultrasonic devices 25. Cook DR, Mealey BL, Verrett RG, et al. Relationship
J Clin Periodontol. 1991;18(1):78-82. between clinical periodontal biotype and labial plate
A 1971 study by Kydd et al was the first to 5. Olsson M, Lindhe J, Marinello CP. On the relationship thickness: an in vivo study. Int J Periodontics Restor-
measure the thickness of palatal mucosa between crown form and clinical features of the gingi- ative Dent. 2011;31(4):345-354.
using an ultrasonic device.52 Ultrasonic va in adolescents. J Clin Periodontol. 1993;20(8):570- 26. Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang
devices appear to be the least invasive 577. HL. Tissue biotype and its relation to the underlying
6. Hirschfeld L. A study of skulls in the American Muse- bone morphology. J Periodontol. 2010;81(4):569-574.
method and offer excellent validity and um of Natural History in relation to periodontal dis- 27. Reiser GM, Rabinovitz Z, Bruno J, Damoulis PD, Griffin
reliability.8,62 However, such devices are ease. J Dent Res. 1923;5:241-265. TJ. Evaluation of maxillary sinus membrane response
no longer available commercially; in addi- 7. Morris ML. The position of the margin of the gingiva. following the elevation with the crestal osteotome
tion, they make it difficult to both deter- Oral Surg Oral Med Oral Pathol. 1958;11(9):969-984. technique in human cadavers. Int J Oral Maxillofac Im-
8. Eger T, Muller HP, Heinecke A. Ultrasonic determination
mine the correct position for accurate plants. 2001;16(6):833-840.
of gingival thickness. Subject variation and influence 28. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence
measurement and successfully reproduce of tooth type and clinical features. J Clin Periodontol. of surgical complications of the sinus graft procedure
measurements.26,61 1996;23(9):839-845. and their impact on implant survival. J Periodontol.
9. Serino G, Wennstrom JL, Lindhe J, Eneroth L. The 2004;75(4):511-516.
Cone beam computed tomography prevalence and distribution of gingival recession in 29. Ardekian L,Oved-Peleg E, Mactei EE, Peled M. The clin-
subjects with a high standard of oral hygiene. J Clin ical significance of sinus membrane perforation during
CBCT scans have been used extensively Periodontol. 1994;21(1):57-63.
for hard tissue imaging because of their
16 July 2013 General Dentistry www.agd.org
Published with permission by the Academy of General Dentistry. © Copyright 2013
by the Academy of General Dentistry. All rights reserved. For printed and electronic
reprints of this article for distribution,please contact rhondab@fosterprinting.com.
augmentation of the maxillary sinus. J Oral Maxillofac restorative materials. Int J Periodontics Restorative B-mode ultrasonic diagnostic equipment. J Dent Res.
Surg. 2006;64(2):277-282. Dent. 2007;27(3):251-257. 1989;68(2):95-100.
30. Berengo M, Sivolella S, Majzoub Z, Cardioli G. Endo- 41. Ahmad I. Anterior dental aesthetics: dental perspec- 54. Lytle RB. The management of abused oral tissues in
scopic evaluation of the bone-added osteotome sinus tive. Br Dent J. 2005;199(3):135-141. complete denture construction. J Prosthet Dent. 1957;
floor elevation procedure. Int J Oral Maxillofac Surg. 42. Atwood DA. Post extraction changes in the adult man- 7:27-42.
2004;33(2):189-194. dible as illustrated by microradiographs and mid-sagit- 55. Terakura T. [Non-invasive measurement of the thick-
31. van der Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinz- tal section and serial cephalometric roentgenographs. ness of oral soft tissues]. Nihon Hotetsu Shika Gakkai
ing DB. Anatomical aspects of sinus floor elevations. J Prosthet Dent. 1963;13:810-816. Zasshi. 1986;30(6):1402-1411.
Clin Oral Implants Res. 2000;11(3):256-265. 43. McFall WT Jr. The laterally repositioned flap—criteria 56. Wennstrom JL, Lindhe J, Sinclair F, Thilander B. Some
32. Aimetti M, Massei G, Morra M, Cardesi E, Romano F. for success. Periodontics. 1967;5(2):89-92. periodontal tissue reactions to orthodontic tooth
Correlation between gingival phenotype and Schnei- 44. Yuodelis R, Page RC, Johnson RH, Schluger S. Perio- movement in monkeys. J Clin Periodontol. 1987;14(3):
derian membrane thickness. Int J Oral Maxillofac Im- dontal Diseases: Basic Phenomena, Clinical Manage- 121-129.
plants. 2008;23(6):1128-1132. ment, and Occlusal and Restorative Interrelationships, 57. Lawson RB, Jones ML. An evaluation of a noninvasive
33. Hermann JS, Buser D, Schenk RK, Schoolfield JD, Co- 3rd ed. Philadelphia: Lea and Langer; 1990:561. method of assessing alveolar bone levels in an experi-
chran DL. Biologic width around one- and two-piece 45. Greenberg J, Laster L, Listgarten MA. Transgingival mental model of cleft lip and palate. Cleft Palate Cra-
titanium implants. Clin Oral Implants Res. 2001;12(6): probing as a potential estimator of alveolar bone lev- niofac J. 1998;35(1):1-8.
559-571. el. J Periodontol. 1976;47(9):514-517. 58. Barriviera M, Duarte WR, Janua’rio AL, Faber J, Bezerra
34. Cardaropoli G, Lekholm U, Wennstrom JL. Tissue alter- 46. Pedelton EC. The minute anatomy of the denture bear- AC. A new method to assess and measure palatal
ations at implant-supported single-tooth replace- ing area. J Am Dent Assoc. 1934;21:488-504. masticatory mucosa by cone-beam computerized to-
ments: a 1-year prospective clinical study. Clin Oral 47. Goaslind GD, Robertson PB, Mahan CJ, Morrison WW, mography. J Clin Periodontol. 2009;36(7):564-568.
Implants Res. 2006;17(2):165-171. Olson JV. Thickness of facial gingiva. J Periodontol. 59. Kan JY, Rungcharassaeng K, Morimoto T, Lozada JL.
35. Berglundh T, Lindhe J. Dimension of the periimplant 1977;48(12):768-771. Facial gingival tissue stability after connective tissue
mucosa. Biological width revisited. J Clin Periodontol. 48. Studer SP, Allen EP, Rees TC, Kouba A. The thickness of graft with single immediate tooth replacement in the
1996;23(10):971-973. masticatory mucosa in the human hard palate and tu- esthetic zone: consecutive case report. J Oral Maxillo-
36. Abrahamsson I, Berglundh T, Wennstrom J, Lindhe J. berosity as potential donor sites for ridge augmenta- fac Surg. 2009;67(11 Suppl):40-48.
The periimplant hard and soft tissues at different im- tion procedures. J Periodontol. 1997;68(2):145-151. 60. Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A,
plant systems. A comparative study in the dog. Clin 49. Ostlund SG. The effect of complete dentures on the Hammerle CH. The effect of allceramic and porcelain-
Oral Implants Res. 1996;7(3):212-219. gum tissues: a histological and histopathological in- fused-to-metal restorations on marginal peri-implant
37. Goodacre CJ, Kan JY, Rungcharassaeng K. Clinical vestigation. Acta Odontol Scand. 1958;16:1-40. soft tissue color: a randomized controlled clinical trial.
complications of osseointegrated implants. J Prosthet 50. Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimen- Int J Periodontics Restorative Dent. 2008;28(4):357-
Dent. 1999;81(5):537-552. sions of peri-implant mucosa: an evaluation of maxil- 365.
38. Romeo E, Lops D, Rossi A, Storelli S, Rozza R, Chiapas- lary anterior single implants in humans. J Periodontol. 61. Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith
co M. Surgical and prosthetic management of inter- 2003;74(4):557-562. DH. Gingival biotype assessment in the esthetic zone:
proximal region with single-implant restorations: 51. Daly CH, Wheeler JB 3rd. The use of ultrasonic thick- visual versus direct measurement. Int J Periodontics
1-year prospective study. J Periodontol. 2008;79(6): ness measurement in the clinical evaluation of the oral Restorative Dent. 2010;30(3):237-243.
1048-1055. soft tissues. Int Dent J. 1971;21(4):418-429. 62. Muller HP, Schaller N, Eger T. Ultrasonic determination
39. Nagaraj KR, Savadi CR, Savadi AR, et al. Gingival bio- 52. Kydd WL, Daly CH, Wheeler JB 3rd. The thickness mea- of thickness of masticatory mucosa: a methodological
type—Prosthodontic perspective. J Indian Prosthodont surement of masticatory mucosa in vivo. Int Dent J. study. Oral Surg Oral Med Oral Pathol Oral Radiol En-
Soc. 2010;10(1):27-30. 1971;21(4):430-441. dod. 1999;88(2):248-253.
40. Jung RE, Sailer I, Hammerle CH, Attin T, Schmidlin P. In 53. Uchida H, Kobayashi K, Nagao M. Measurement in
vitro color changes of soft tissues caused by vivo of masticatory mucosal thickness with 20 MHz
www.agd.org General Dentistry July 2013 17
Potrebbero piacerti anche
- 05 Dimensión VerticalDocumento16 pagine05 Dimensión VerticalSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Enfoque y DiagnosticoDocumento4 pagineEnfoque y DiagnosticoSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Enfermedad Renal Crónica Manejo OdontologicoDocumento7 pagineEnfermedad Renal Crónica Manejo OdontologicoSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Articulo de Endo PDFDocumento11 pagineArticulo de Endo PDFSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Articulo de Endo para Semana 6 PDFDocumento13 pagineArticulo de Endo para Semana 6 PDFSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Protocolo de Cementación AdhesivaDocumento4 pagineProtocolo de Cementación AdhesivaSUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- Programa Revisión Literatura I 2020Documento9 paginePrograma Revisión Literatura I 2020SUSAN LUCINDA MEJIA TIPAZNessuna valutazione finora
- 6976 23631 1 SMDocumento27 pagine6976 23631 1 SMMAYRA SERRANONessuna valutazione finora
- 3.3.2. APU - LIC-13454 - v1 - PUENTE-IGLESIA - LA-LORENADocumento73 pagine3.3.2. APU - LIC-13454 - v1 - PUENTE-IGLESIA - LA-LORENAVICTOR HUGO PARRADO LOPEZNessuna valutazione finora
- Mecanismo de Corte y Fabricación Del Cortador PDCDocumento26 pagineMecanismo de Corte y Fabricación Del Cortador PDCLESCANO GABRIEL100% (1)
- Modelo de Formato Contratos de Asociación TecnológicaDocumento6 pagineModelo de Formato Contratos de Asociación TecnológicaMaribel CongonhaNessuna valutazione finora
- Laboratorio N - 2 PbiDocumento2 pagineLaboratorio N - 2 PbiJavier ChiclayoNessuna valutazione finora
- Azúcar de RemolachaDocumento2 pagineAzúcar de RemolachaLuis Lino JimenezNessuna valutazione finora
- Manual Servicio Cirugia InfantilDocumento28 pagineManual Servicio Cirugia InfantilSebastian Alexander Orellana CartesNessuna valutazione finora
- PRÁCTICA FINAL Asignatura Gerencia de Contabilidad y Financiera PDFDocumento4 paginePRÁCTICA FINAL Asignatura Gerencia de Contabilidad y Financiera PDFJose Manuel MorenoNessuna valutazione finora
- INSTRUCTIVO No. 005Documento39 pagineINSTRUCTIVO No. 005Isaac PizarroNessuna valutazione finora
- Tesis CapriDocumento84 pagineTesis CapriIleana Fernandez100% (2)
- EvidencianDiagramannnenCommercenynenBusiness 2960fb59acb59a2Documento2 pagineEvidencianDiagramannnenCommercenynenBusiness 2960fb59acb59a2Julietha GiraldoNessuna valutazione finora
- El Juridico PeriodicoDocumento20 pagineEl Juridico PeriodicoHortencia RestrepoNessuna valutazione finora
- Auditoria y Revisión de La Alta Dirección Del Sistema de Gestión de Seguridad y Salud en El Trabajo SG-SST. Foro 4 SemanaDocumento1 paginaAuditoria y Revisión de La Alta Dirección Del Sistema de Gestión de Seguridad y Salud en El Trabajo SG-SST. Foro 4 SemanaAngie RojasNessuna valutazione finora
- AIA - Manual para Inquilinos en Adaptacion y Remodelacion 2019 Santa Anita-CompressedDocumento55 pagineAIA - Manual para Inquilinos en Adaptacion y Remodelacion 2019 Santa Anita-Compresseddemetrio lopezNessuna valutazione finora
- Presentación Apa 7ma EdDocumento68 paginePresentación Apa 7ma Edkfmon66Nessuna valutazione finora
- MPDFDocumento3 pagineMPDFAnyi murilloNessuna valutazione finora
- Mec LocDocumento33 pagineMec LocLauraNessuna valutazione finora
- Ley Del Contrato de Seguro y Reglamentos Relacionados - 2021Documento40 pagineLey Del Contrato de Seguro y Reglamentos Relacionados - 2021Luz Marina Suarez LlerenaNessuna valutazione finora
- Texto de TopografiaDocumento175 pagineTexto de TopografiaJoel Abdel Bravo Pereira100% (1)
- Presidentes de PanamáDocumento24 paginePresidentes de PanamávicantiNessuna valutazione finora
- Guía de Utilización Herramienta EstelaDocumento7 pagineGuía de Utilización Herramienta EstelaEnrique del ReyNessuna valutazione finora
- S03.s1 - Ejercicio PDFDocumento1 paginaS03.s1 - Ejercicio PDFJULEYSI KATIUSCA NATIVIDAD MONTALBAN CHÁVEZNessuna valutazione finora
- PROYECTO FINAL DE LA CLASE DE Contabilidad Gerencial1Documento20 paginePROYECTO FINAL DE LA CLASE DE Contabilidad Gerencial1Lesly VillatoroNessuna valutazione finora
- TP Bombas FinalDocumento16 pagineTP Bombas FinalLucas NievaNessuna valutazione finora
- Acuerdo #002-2019/TCEDocumento3 pagineAcuerdo #002-2019/TCELa LeyNessuna valutazione finora
- Auto Ingles para El TurismoDocumento32 pagineAuto Ingles para El TurismoSalma AndreaNessuna valutazione finora
- Wilo Bombas MultietDocumento55 pagineWilo Bombas MultietelverNessuna valutazione finora
- Facturas X DescargaDocumento5 pagineFacturas X DescargaJosé Luis PalomaresNessuna valutazione finora
- FORMATO 051 - Check List de RuidoDocumento1 paginaFORMATO 051 - Check List de RuidoluenchiroNessuna valutazione finora
- File 69722Documento22 pagineFile 69722p.rojasc3dNessuna valutazione finora
- Instructivo de Memoria Tecnica de Pasantias o Practicas Pre-ProfesionalesDocumento10 pagineInstructivo de Memoria Tecnica de Pasantias o Practicas Pre-ProfesionalesAlfredo TenelemaNessuna valutazione finora