Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
74 418 PDF
Caricato da
Muhammad Fadhil Abdan SyakuroDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
74 418 PDF
Caricato da
Muhammad Fadhil Abdan SyakuroCopyright:
Formati disponibili
Circulation Journal
Official Journal of the Japanese Circulation Society
REVIEW
http://www. j-circ.or.jp
Role of the SDF-1/CXCR4 System in Myocardial Infarction
Masafumi Takahashi, MD
Myocardial infarction (MI) is accompanied by an inflammatory response, leading to the recruitment of leukocytes
and subsequent myocardial injury and healing. Chemokines are potent chemoattractant cytokines that regulate
leukocyte trafficking in inflammatory processes. Recent evidence indicates that chemokines play a role not only
in leukocyte trafficking but also in angiogenesis and cardioprotection. In particular, stromal cell-derived factor-1α
(SDF-1α) has generated considerable interest for its role in the pathophysiology of MI. This review will focus
on the role of SDF-1 and its receptor CXC chemokine receptor 4 (CXCR4; ie, the SDF-1/CXCR4 system) in the
pathophysiology of MI and discuss their potential as therapeutic targets for MI. (Circ J 2010; 74: 418 – 423)
Key Words: Cardioprotection; Chemokines; Endothelial progenitor cells; Leukocytes; Myocardial infarction
I
schemic heart disease is a common occurrence, and in based therapy for ischemic heart disease, including MI.9–12
the near future it is predicted to be the leading cause of The results obtained from these clinical studies support the
death worldwide. Myocardial infarction (MI) is a com- important role of bone marrow-derived cells in angiogenesis.
mon presentation of ischemic heart disease and is defined as However, because some clinical studies on ischemic heart
interruption of the blood flow to the heart because of the disease did not find the cell-based therapy to be significantly
occlusion of a coronary artery and the replacement of necrotic beneficial,13,14 the efficacy of this therapy remains contro-
myocardium by a dense fibrotic scar. The main functional versial.
consequence of MI is a decrease in systolic compliance (ie, Chemokines are potent chemoattractant cytokines that
progressive loss of pump function in the chamber where the regulate leukocyte trafficking in homeostatic and inflamma-
muscle has been lost). In addition, MI often results in elec- tory processes.15 Depending on their topical concentration,
trical instability within the heart and the generation of fatal chemokines directly recruit circulating leukocytes to the site
arrhythmias. Therefore, the development of ischemic heart of inflammation or injury. Many experimental and clinical
disease, including MI, is an important issue requiring study. studies have demonstrated that a substantial number of
Despite the advancement in revascularization procedures chemokines are involved in the pathophysiology of ischemic
for ischemic heart disease, including MI, a substantial num- heart diseases.16 Among them, stromal cell-derived factor-1α
ber of patients are either not eligible for these procedures (SDF-1α, also known as CXCL12α) is thought to play a key
or only partial revascularization can be achieved for them. role in angiogenic processes after MI. In particular, bone
Inducing angiogenesis by the administration of exogenous marrow-derived cells, which express the SDF-1 receptor CXC
angiogenic factors or the transfer of genes coding for these chemokine receptor 4 (CXCR4, also known as fusin and
factors has emerged as an alternative strategy for salvaging CD184), have been shown to act as vascular stem/progenitor
ischemic cardiomyocytes.1–4 Although initial trials involving cells (including EPCs) and promote angiogenesis after MI.
the delivery of angiogenic factors, such as vascular endothe- Furthermore, recent investigations showed that SDF-1α also
lial growth factor-A (VEGF-A), were associated with short- exerts direct cardioprotective effects after MI.17,18 This review
term improvement, follow-up studies have yet to show long- will focus on the role of the SDF-1/CXCR4 system in the
term benefits.5 Evidence for the role of bone marrow-derived pathophysiology of MI and discuss whether this system is a
cells in angiogenesis has accumulated since endothelial potential therapeutic target for MI. Although a large amount
progenitor cells (EPCs) were identified and bone marrow- of evidence indicates the role of the SDF-1/CXCR4 system
or peripheral blood-derived EPCs have been recruited and in the development of atherosclerosis in the coronary arteries,
incorporated into the site of angiogenesis in the ischemic which is the principal cause of MI, I will not discuss this
tissue.6,7 In fact, a multicenter trial, the Therapeutic Angio- issue because several reviews on the same have already been
genesis using Cell Transplantation (TACT) trial, showed that published.
autologous implantation of bone marrow-derived mono-
nuclear cells induced angiogenesis and improved clinical
parameters in patients with severe limb ischemia caused by Chemokines in MI
peripheral arterial disease.8 Since then, a number of clinical Chemokines
studies have proven the efficacy and safety of autologous cell- A number of components have been shown to be involved
Received December 22, 2009; accepted January 7, 2010; released online January 30, 2010
Division of Bioimaging Sciences, Center for Molecular Medicine, Jichi Medical University, Shimotsuke, Japan
Mailing address: Masafumi Takahashi, MD, Division of Bioimaging Sciences, Center for Molecular Medicine, Jichi Medical Univer-
sity, 3311-1 Yakushiji, Shimotsuke 329-0498, Japan. E-mail: masafumi2@jichi.ac.jp
ISSN-1346-9843 doi: 10.1253/circj.CJ-09-1021
All rights are reserved to the Japanese Circulation Society. For permissions, please e-mail: cj@j-circ.or.jp
Circulation Journal Vol.74, March 2010
SDF-1/CXCR4 in MI 419
Figure 1. Potential role of the SDF-1/CXCR4 system in myocardial infarction. At the site of tissue ischemia, such as the ischemic
myocardium, HIF-1α is induced in response to reduced oxygen tension and then stimulates SDF-1α expression. Binding of
SDF-1α to CXCR4 protects cardiomyocytes from apoptotic cell death. SDF-1α recruits bone marrow-derived stem/progenitor
cells and induces the production of angiogenic factors, thereby leading to angiogenesis. SDF-1α also simulates the migration of
endothelial cells and enhances angiogenesis. CXCR4, CXC chemokine receptor 4; HIF-1α, hypoxia-inducible factor-1α; SDF-1α,
stromal cell-derived factor-1α.
in the pathophysiology of MI. Among these, chemokines are cesses. Recently, however, it has been observed that chemo-
believed to be one of the key regulators because they are kines are also expressed by non-hematopoietic cells such as
expressed in the infarcted myocardium and also because endothelial cells and cardiomyocytes, and their function
they play a crucial role in the process of myocardial inflam- extends far beyond leukocyte migration and activation.16,20
mation and healing.19 Chemokines have been divided into 2 Thus, chemokines are key mediators not only in inflamma-
main subfamilies on the basis of the conserved structural tory responses but also in other responses involved in the
features. In the CXC chemokines, a single amino acid is pres- pathophysiology of ischemic diseases.
ent between the 2 amino-terminal cysteine residues. In con-
trast, in the CC chemokines, no amino acid is present between Chemokines in MI
the 2 cysteines. Other minor chemokine subfamilies that are Many experimental and clinical studies have shown that che-
currently known include fractalkine/CX3CL1 (CX3C chemo- mokines are involved in the pathophysiology of MI. The CXC
kines) and lymphotactin/XCL1. The effects of chemokines chemokines interleukin-8 (IL-8),21–24 SDF-1α25–27 GRO-α/
are mediated via their interaction with specific chemokines KC (known as CXCL1),22 and IP-10 and the CC chemo-
receptors that are expressed on a wide range of cell types. kines monocyte chemoattractant protein-1 (MCP-1, known
These chemokine receptors are 7-transmembrane (TM) G- as CCL2)28,29 and macrophage inflammatory protein-1α/β
protein-coupled receptors and are unusual among the many (MIP-1α/β, known as CCL3/4)30 appear to be upregulated
characterized members of the superfamily in that a single in various animal models of experimental MI. Two types of
receptor possesses multiple high-affinity ligands. Therefore, MI models are currently used: the permanent MI model and
initially, the chemokine network might appear to be a redun- the ischemia–reperfusion (I/R) injury model. Several differ-
dant cellular signaling system; however, analysis of che- ent features exist between the pathophysiology of permanent
mokines or gene disruption of their receptors in mice has MI and I/R injury.31,32 Reperfusion releases a large excess
revealed that certain chemokines possess unique and non- of reactive oxygen species (ROS) and causes “reperfusion
redundant roles in leukocyte trafficking, inflammation, and injury”. Inflammatory responses such as infiltration by neu-
immune responses. trophils and macrophages are much stronger in the reperfused
The basic function of chemokines involves the regulation heart than in the infarcted heart. Because the inflammatory
of leukocyte trafficking in basal and inflammatory pro- responses after MI determine tissue healing,19 collagen de-
Circulation Journal Vol.74, March 2010
420 TAKAHASHI M
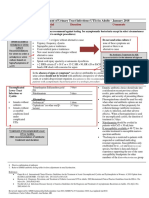
Figure 2. Therapeutic potential of the SDF-1/CXCR4 system for treating myocardial infarction. Several therapeutic strategies
using the SDF-1/CXCR4 system have been proposed: (1) local SDF-1α delivery and inhibition of SDF-1α cleavage, (2) up-
regulation of CXCR4 in cardiomyocytes and cardiac stem cells, (3) mobilization of CXCR4+ cells from the bone marrow into
peripheral circulation, or (4) upregulation of CXCR4 in bone marrow-derived cells and MSCs. CXCR4, CXC chemokine receptor
4; MSC, mesenchymal stem cells; SDF-1α, stromal cell-derived factor-1α.
position during MI may be accelerated in the reperfused levels on both vascular and hematopoietic progenitor cells,
heart. Furthermore, neovascularization is more enhanced in play a critical role in the development of the heart and blood
the reperfused heart than in the infarcted heart. Therefore, it is vessels and in the regulation of the motility and differen-
necessary to consider the MI models used in different studies. tiation in hematopoietic stem cells (HSCs). SDF-1, which
Consistent with the results of the experimental studies, belongs to the CXC chemokine subfamily, is produced in
elevated serum concentrations of several chemokines were 2 forms, SDF-1α (CXCL12α) and SDF-1β (CXCL12β), by
observed in patients with MI,33 suggesting the clinical sig- alternative splicing of the same SDF-1 gene.38 Different splic-
nificance of chemokines in the pathophysiology of MI. ing variants are characterized by distinct activities.39 SDF-1α,
The mechanisms responsible for the upregulation of che- which is the predominant isoform, is susceptible to pro-
mokines in the infarcted heart have not been fully under- teolytic degradation in the blood, whereas SDF-1β is more
stood. To date, however, it is known that several factors resistant to this proteolytic process. SDF-1 binds to CXCR4,
implicated in initiating the inflammatory responses are likely G-protein-coupled receptors with 7 TM domains. The bind-
to induce the production of these chemokines. The induction ing of SDF-1α to CXCR4 stimulates the dimerization of
of IL-8 and MCP-1 is regulated by the transcription factor the receptor and activates downstream signaling molecules,
NF-κB, which contributes to the regulation of inflammation including the activation of the focal adhesion kinase, extra-
and is activated in the infarcted heart.34,35 Another important cellular signal-regulated kinases, protein kinase C, JAK/Stat,
transcription factor involved in MI is hypoxia-inducible and NF-κB transcription pathways.40 The interaction between
factor-1α (HIF-1α), which is induced by hypoxia (low O2 SDF-1α and CXCR4 has been previously considered exclu-
tension) and regulates VEGF induction. HIF-1αwas reported sive, but it was recently identified that SDF-1α can also bind
to be in the active form in the infarct myocardium after MI with CXCR7.41,42
and induced SDF-1α in hypoxic conditions (Figure 1).36,37 In SDF-1α was initially isolated from bone marrow stromal
addition to inducing SDF-1α, HIF-1α enhances the expres- cells, and it is expressed in most normal tissues, such as
sion and function of CXCR4 in bone marrow-derived cells. the heart, liver, spleen, and kidney, but not in leukocytes.
Different from other chemokines, which are induced by
inflammatory stimuli, the constitutive expression of SDF-1α
SDF-1/CXCR4 System in MI in bone marrow stromal cells suggests a fundamental role
SDF-1/CXCR4 System in organ homeostasis and development. The experimental
SDF-1α and its receptor CXCR4, which is expressed at high deficiency of SDF-1α or CXCR4 in mice causes embryonic
Circulation Journal Vol.74, March 2010
SDF-1/CXCR4 in MI 421
lethality because of multiple defects, such as a cardiac ven- hypoxic preconditioning of cardiac stem/progenitor cells
tricular septal defect and the defective formation of the large (CLK: cardiosphere-derived, Lin– c-kit+ progenitor) upregu-
vessels in the gastrointestinal tract.43–45 In addition to these lates CXCR4 and increases the recruitment of these cells
defects, hematopoiesis is severely impaired, with deficien- into the ischemic myocardium, thereby reducing the infarct
cies in the development of B cells, decreased myelopoiesis, size and improving the cardiac function after MI.55 On the
and HSC colonization of the bone marrow. Postnatally, other hand, intravenous delivery of genetically modified mes-
SDF-1α exerts various effects in a variety of cells, including enchymal stem cells (MSCs) expressing CXCR4 has shown
leukocytes, bone marrow stem/progenitor cells, and endothe- to improve cardiac function and remodeling after MI.56
lial cells. The main biological effects of SDF-1α are related Several factors such as C3a, hyaluronic acid, and soluble
to its ability to induce chemotaxis, adhesion, motility, and the vascular cell adhesion molecule-1 (VCAM-1) were recently
secretion of matrix metalloproteinase (MMP) and angiogenic identified as priming agents of CXCR4+ cells and found
factors,40 its involvement in the retention and recruitment of to increase SDF-1-dependent homing and engraftment of
bone marrow stem/progenitor cells, and its involvement in HSCs.40 Recently, we demonstrated that cultivation spe-
the process of angiogenesis (Figure 1). SDF-1α also directly cifically upregulated CXCR4 expression in bone marrow-
stimulates endothelial cell migration and promotes angio- derived cells and the implantation of these cells enhanced
genesis.20,46 Moreover, Jin et al reported that hematopoietic therapeutic angiogenesis and restored blood flow to the
cytokines stimulates the release of SDF-1α from platelets, ischemic tissue.57 In addition, a direct link between CXCR4
augmenting the recruitment of CXCR4+VEGFR1+ heman- expression and angiogenic factor production was demon-
giocytes, thereby accelerating angiogenesis.47 Therefore, the strated using bone marrow-derived cells isolated from CXCR4
SDF-1/CXCR4 system is now recognized as playing an im- hetero-deficient mice. On the other hand, the administration
portant role in a wide array of disease processes. of several factors, such as granulocyte colony-stimulating
factor (G-CSF), macrophage colony-stimulating factor, and
SDF-1/CXCR4 System in MI erythropoietin, has been shown to stimulate the mobilization
SDF-1α has generated considerable interest for its role in of CXCR4+ cells from the bone marrow to the peripheral
pathophysiology of MI. As mentioned earlier, the SDF-1/ circulation and to exert beneficial effect in MI.58–60 Thus,
CXCR4 system plays a critical role in cardiogenesis and the modification of CXCR4 expression may enable the
angiogenesis in the mouse embryo,43,44 indicating the role of enhancement of the angiogenic activity and homing capacity
this system in adult cardiovascular diseases. Indeed, studies of vascular stem/progenitor cells.
conducted using various experimental models of MI show that In terms of SDF-1α, the administration or adenoviral gene
SDF-1α is upregulated in the ischemic myocardium.26,48–50 transfer of SDF-1α into the injured myocardium improved
Although it is well known that the presence of SDF-1α is cardiac function and infarct size after MI through the anti-
essential in the ischemic myocardium, the value of serum apoptotic and angiogenic effects of SDF-1α.17,18 SDF-1α is
SDF-1αlevels is currently controversial. Chang et al recently reported to exert its beneficial effects through 2 mechanisms:
reported that although the serum levels of SDF-1α do not inhibition of cardiomyocyte apoptosis and promotion of
differ between patients with acute MI and normal subjects; angiogenesis (Figure 1). SDF-1α protects cardiomyocytes
patients with serious clinical conditions had significantly from apoptotic cell death after hypoxic insult. This anti-
higher serum SDF-1α levels than those in a relatively stable apoptotic effect is mediated by the PI-3 kinase/Akt signaling
condition and in normal subjects.51 They also showed that pathway.18 On the other hand, SDF-1α recruits bone marrow-
increased levels of serum SDF-1α were significantly corre- derived stem/progenitor cells and induces the production of
lated with an elevated number of circulating EPCs. angiogenic factors, thereby leading to angiogenesis. SDF-1α
also simulates the migration of preexisting endothelial cells
Therapeutic Implications and enhances angiogenesis. Thus, SDF-1 has a therapeutic
effect in MI; however, there is a potential limitation to
of the SDF-1/CXCR4 System the use of the SDF-1α protein because of its sensitivity to
Since the SDF-1/CXCR4 system has been shown to have cleavage by several proteases, including MMP-2 and CD26/
not only cardioprotective effects but also angiogenic effects dipeptidylpeptidase IV (DPPIV). In this regard, Segers et al
in several experimental models of MI, this system can be a recently designed a new chemokine called S-SDF-1 (S4V)
therapeutic target for the treatment of MI (Figure 2). From a that is resistant to MMP-2 and DPPIV but retains its chemo-
historic point of view, the discovery of CXCR4 and its func- tactic activity, and they showed that S-SDF-1 (S4V) delivery
tion as a coreceptor for the human immunodeficiency virus promoted the recruitment of CXCR4+/c-kit+/Flk-1+ cells and
(HIV) generated great interest in the development of small improved cardiac function after MI.61 More recently, Zaruba
molecular CXCR4 receptor antagonists for treating HIV et al demonstrated that combination therapy by using G-CSF
infection.52 In addition, the SDF-1/CXCR4 system might play to mobilize EPCs from the bone marrow and DPPIV inhibi-
a role in the spread and progression of many different types tion to prevent proteolytic cleavage of SDF-1α increased the
of malignancies.40 Therefore, several CXCR4 antagonists, recruitment of EPCs to the infarct myocardium, and sub-
such as AMD3100, have been developed as agents for treat- sequently improved cardiac function after MI.62 These find-
ing HIV infection and malignancies and shown to dramati- ings indicate that SDF-1α is a promising target for thera-
cally increase the mobilization of CD34+ hematopoietic stem/ peutic interventions in MI. However, because SDF-1α is
progenitors from the bone marrow into the peripheral circu- produced in the ischemic myocardium and the chemotactic
lation in humans.53,54 However, it would be difficult to use effect of chemokines is generally regulated by their topical
these agents for the treatment of MI because this may negate concentrations,63–65 the precise effect of SDF-1αmay depend
their beneficial effects such as cardioprotection and angio- upon the situation (ie, its local concentration, duration, and
genesis in the myocardium. time period after MI).
The modification of CXCR4 expression and function by
factors and/or conditions has been shown.12,40 For instance,
Circulation Journal Vol.74, March 2010
422 TAKAHASHI M
in acute myocardial infarction. N Engl J Med 2006; 355: 1199 –
Conclusions 1209.
14. Janssens S, Dubois C, Bogaert J, Theunissen K, Deroose C, Desmet
A large number of studies have suggested that chemokines W, et al. Autologous bone marrow-derived stem-cell transfer in
are key regulators of MI. Of these, SDF-1αis one of the most patients with ST-segment elevation myocardial infarction: Double-
important involved in the pathophysiology of MI. In this blind, randomised controlled trial. Lancet 2006; 367: 113 – 121.
review, I have discussed the role of SDF-1α and its receptor 15. Gerard C, Rollins BJ. Chemokines and disease. Nat Immunol 2001;
CXCR4, which together constitute the SDF-1/CXCR4 sys- 2: 108 – 115.
16. Frangogiannis NG, Entman ML. Chemokines in myocardial isch-
tem, in the processes of MI and the role of this system as emia. Trends Cardiovasc Med 2005; 15: 163 – 169.
a potential target in the treatment of MI. However, before 17. Hu X, Dai S, Wu WJ, Tan W, Zhu X, Mu J, et al. Stromal cell de-
clinical application, further studies are necessary to elucidate rived factor-1 alpha confers protection against myocardial ischemia/
the precise role and mechanism of the SDF-1/CXCR4 sys- reperfusion injury: Role of the cardiac stromal cell derived factor-1
alpha CXCR4 axis. Circulation 2007; 116: 654 – 663.
tem in the pathophysiology of MI. 18. Saxena A, Fish JE, White MD, Yu S, Smyth JW, Shaw RM, et al.
Stromal cell-derived factor-1alpha is cardioprotective after myo-
cardial infarction. Circulation 2008; 117: 2224 – 2231.
Acknowledgments 19. Frangogiannis NG, Smith CW, Entman ML. The inflammatory re-
The author thanks Dr Uichi Ikeda and the members of the Division sponse in myocardial infarction. Cardiovasc Res 2002; 53: 31 – 47.
of Cardiovascular Medicine, Shinshu University Graduate School of 20. Salcedo R, Oppenheim JJ. Role of chemokines in angiogenesis:
Medicine for their invaluable support of this work. This work was partly CXCL12/SDF-1 and CXCR4 interaction, a key regulator of endo-
supported by research grants from the Ministry of Education, Culture, thelial cell responses. Microcirculation 2003; 10: 359 – 370.
Sports, Science and Technology, the Ministry of Health, Labor and 21. Kukielka GL, Smith CW, LaRosa GJ, Manning AM, Mendoza LH,
Welfare, and Takeda Science Foundation. Daly TJ, et al. Interleukin-8 gene induction in the myocardium after
ischemia and reperfusion in vivo. J Clin Invest 1995; 95: 89 – 103.
22. Kocher AA, Schuster MD, Bonaros N, Lietz K, Xiang G, Martens
Disclosure TP, et al. Myocardial homing and neovascularization by human bone
Conflict of Interest: none. marrow angioblasts is regulated by IL-8/Gro CXC chemokines.
J Mol Cell Cardiol 2006; 40: 455 – 464.
23. Ivey CL, Williams FM, Collins PD, Jose PJ, Williams TJ. Neutrophil
References chemoattractants generated in two phases during reperfusion of
1. Udelson JE, Dilsizian V, Laham RJ, Chronos N, Vansant J, Blais ischemic myocardium in the rabbit: Evidence for a role for C5a
M, et al. Therapeutic angiogenesis with recombinant fibroblast and interleukin-8. J Clin Invest 1995; 95: 2720 – 2728.
growth factor-2 improves stress and rest myocardial perfusion 24. Kilgore KS, Park JL, Tanhehco EJ, Booth EA, Marks RM, Lucchesi
abnormalities in patients with severe symptomatic chronic coro- BR. Attenuation of interleukin-8 expression in C6-deficient rabbits
nary artery disease. Circulation 2000; 102: 1605 – 1610. after myocardial ischemia/reperfusion. J Mol Cell Cardiol 1998;
2. Schumacher B, Pecher P, von Specht BU, Stegmann T. Induction of 30: 75 – 85.
neoangiogenesis in ischemic myocardium by human growth factors: 25. Ma J, Ge J, Zhang S, Sun A, Shen J, Chen L, et al. Time course of
First clinical results of a new treatment of coronary heart disease. myocardial stromal cell-derived factor 1 expression and beneficial
Circulation 1998; 97: 645 – 650. effects of intravenously administered bone marrow stem cells in
3. Losordo DW, Vale PR, Hendel RC, Milliken CE, Fortuin FD, rats with experimental myocardial infarction. Basic Res Cardiol
Cummings N, et al. Phase 1/2 placebo-controlled, double-blind, 2005; 100: 217 – 223.
dose-escalating trial of myocardial vascular endothelial growth 26. Abbott JD, Huang Y, Liu D, Hickey R, Krause DS, Giordano FJ.
factor 2 gene transfer by catheter delivery in patients with chronic Stromal cell-derived factor-1alpha plays a critical role in stem cell
myocardial ischemia. Circulation 2002; 105: 2012 – 2018. recruitment to the heart after myocardial infarction but is not suffi-
4. Baumgartner I, Pieczek A, Manor O, Blair R, Kearney M, Walsh K, cient to induce homing in the absence of injury. Circulation 2004;
et al. Constitutive expression of phVEGF165 after intramuscular 110: 3300 – 3305.
gene transfer promotes collateral vessel development in patients 27. Pillarisetti K, Gupta SK. Cloning and relative expression analysis
with critical limb ischemia. Circulation 1998; 97: 1114 – 1123. of rat stromal cell derived factor-1 (SDF-1): SDF-1 alpha mRNA is
5. Yla-Herttuala S, Alitalo K. Gene transfer as a tool to induce thera- selectively induced in rat model of myocardial infarction. Inflam-
peutic vascular growth. Nat Med 2003; 9: 694 – 701. mation 2001; 25: 293 – 300.
6. Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, 28. Kumar AG, Ballantyne CM, Michael LH, Kukielka GL, Youker
et al. Isolation of putative progenitor endothelial cells for angio- KA, Lindsey ML, et al. Induction of monocyte chemoattractant
genesis. Science 1997; 275: 964 – 967. protein-1 in the small veins of the ischemic and reperfused canine
7. Jia L, Takahashi M, Yoshioka T, Morimoto H, Ise H, Ikeda U. myocardium. Circulation 1997; 95: 693 – 700.
Therapeutic potential of endothelial progenitor cells for cardiovas- 29. Dewald O, Zymek P, Winkelmann K, Koerting A, Ren G, Abou-
cular diseases. Curr Vasc Pharmacol 2006; 4: 59 – 65. Khamis T, et al. CCL2/monocyte chemoattractant protein-1 regu-
8. Tateishi-Yuyama E, Matsubara H, Murohara T, Ikeda U, Shintani lates inflammatory responses critical to healing myocardial infarcts.
S, Masaki H, et al. Therapeutic angiogenesis for patients with limb Circ Res 2005; 96: 881 – 889.
ischaemia by autologous transplantation of bone-marrow cells: A 30. Maekawa N, Wada H, Kanda T, Niwa T, Yamada Y, Saito K, et al.
pilot study and a randomised controlled trial. Lancet 2002; 360: Improved myocardial ischemia/reperfusion injury in mice lacking
427 – 435. tumor necrosis factor-alpha. J Am Coll Cardiol 2002; 39: 1229 –
9. Tatsumi T, Ashihara E, Yasui T, Matsunaga S, Kido A, Sasada Y, 1235.
et al. Intracoronary transplantation of non-expanded peripheral 31. Kloner RA, Jennings RB. Consequences of brief ischemia: Stun-
blood-derived mononuclear cells promotes improvement of car- ning, preconditioning, and their clinical implications. Part 1. Circu-
diac function in patients with acute myocardial infarction. Circ J lation 2001; 104: 2981 – 2989.
2007; 71: 1199 – 1207. 32. Vandervelde S, van Amerongen MJ, Tio RA, Petersen AH, van
10. Assmus B, Honold J, Schachinger V, Britten MB, Fischer-Rasokat Luyn MJ, Harmsen MC. Increased inflammatory response and neo-
U, Lehmann R, et al. Transcoronary transplantation of progenitor vascularization in reperfused vs non-reperfused murine myocardial
cells after myocardial infarction. N Engl J Med 2006; 355: 1222 – infarction. Cardiovasc Pathol 2006; 15: 83 – 90.
1232. 33. Soejima H, Ogawa H, Yasue H, Kaikita K, Takazoe K, Nishiyama
11. Schachinger V, Erbs S, Elsasser A, Haberbosch W, Hambrecht R, K, et al. Angiotensin-converting enzyme inhibition reduces mono-
Holschermann H, et al. Intracoronary bone marrow-derived pro- cyte chemoattractant protein-1 and tissue factor levels in patients
genitor cells in acute myocardial infarction. N Engl J Med 2006; with myocardial infarction. J Am Coll Cardiol 1999; 34: 983 – 988.
355: 1210 – 1221. 34. Kawano S, Kubota T, Monden Y, Tsutsumi T, Inoue T, Kawamura
12. Limbourg A, Limbourg F, Drexler H. Cell-based therapies for N, et al. Blockade of NF-kappaB improves cardiac function and sur-
ischemic heart disease: “Trick and treat”. Circ J 2009; 73: 2179 – vival after myocardial infarction. Am J Physiol Heart Circ Physiol
2182. 2006; 291: H1337 – H1344.
13. Lunde K, Solheim S, Aakhus S, Arnesen H, Abdelnoor M, Egeland 35. Onai Y, Suzuki J, Maejima Y, Haraguchi G, Muto S, Itai A, et al.
T, et al. Intracoronary injection of mononuclear bone marrow cells Inhibition of NF-{kappa}B improves left ventricular remodeling
Circulation Journal Vol.74, March 2010
SDF-1/CXCR4 in MI 423
and cardiac dysfunction after myocardial infarction. Am J Physiol myocardial infarction undergoing primary coronary angioplasty.
Heart Circ Physiol 2007; 292: H530 – H538. Circ J 2009; 73: 1097 – 1104.
36. Ceradini DJ, Gurtner GC. Homing to hypoxia: HIF-1 as a mediator 52. Burger JA, Kipps TJ. CXCR4: A key receptor in the crosstalk be-
of progenitor cell recruitment to injured tissue. Trends Cardiovasc tween tumor cells and their microenvironment. Blood 2006; 107:
Med 2005; 15: 57 – 63. 1761 – 1767.
37. Ceradini DJ, Kulkarni AR, Callaghan MJ, Tepper OM, Bastidas N, 53. Liles WC, Broxmeyer HE, Rodger E, Wood B, Hubel K, Cooper S,
Kleinman ME, et al. Progenitor cell trafficking is regulated by et al. Mobilization of hematopoietic progenitor cells in healthy
hypoxic gradients through HIF-1 induction of SDF-1. Nat Med volunteers by AMD3100, a CXCR4 antagonist. Blood 2003; 102:
2004; 10: 858 – 864. 2728 – 2730.
38. De La Luz Sierra M, Yang F, Narazaki M, Salvucci O, Davis D, 54. Devine SM, Flomenberg N, Vesole DH, Liesveld J, Weisdorf D,
Yarchoan R, et al. Differential processing of stromal-derived factor- Badel K, et al. Rapid mobilization of CD34+ cells following admin-
1alpha and stromal-derived factor-1beta explains functional diver- istration of the CXCR4 antagonist AMD3100 to patients with
sity. Blood 2004; 103: 2452 – 2459. multiple myeloma and non-Hodgkin’s lymphoma. J Clin Oncol
39. Janowski M. Functional diversity of SDF-1 splicing variants. Cell 2004; 22: 1095 – 1102.
Adh Migr 2009; 3: 243 – 249. 55. Tang YL, Zhu W, Cheng M, Chen L, Zhang J, Sun T, et al. Hypoxic
40. Kucia M, Jankowski K, Reca R, Wysoczynski M, Bandura L, preconditioning enhances the benefit of cardiac progenitor cell ther-
Allendorf DJ, et al. CXCR4-SDF-1 signalling, locomotion, chemo- apy for treatment of myocardial infarction by inducing CXCR4
taxis and adhesion. J Mol Histol 2004; 35: 233 – 245. expression. Circ Res 2009; 104: 1209 – 1216.
41. Balabanian K, Lagane B, Infantino S, Chow KY, Harriague J, 56. Cheng Z, Ou L, Zhou X, Li F, Jia X, Zhang Y, et al. Targeted
Moepps B, et al. The chemokine SDF-1/CXCL12 binds to and sig- migration of mesenchymal stem cells modified with CXCR4 gene
nals through the orphan receptor RDC1 in T lymphocytes. J Biol to infarcted myocardium improves cardiac performance. Mol Ther
Chem 2005; 280: 35760 – 35766. 2008; 16: 571 – 579.
42. Burns JM, Summers BC, Wang Y, Melikian A, Berahovich R, Miao 57. Shiba Y, Takahashi M, Hata T, Murayama H, Morimoto H, Ise H,
Z, et al. A novel chemokine receptor for SDF-1 and I-TAC involved et al. Bone marrow CXCR4 induction by cultivation enhances ther-
in cell survival, cell adhesion, and tumor development. J Exp Med apeutic angiogenesis. Cardiovasc Res 2009; 81: 169 – 177.
2006; 203: 2201 – 2213. 58. Morimoto H, Takahashi M, Shiba Y, Izawa A, Ise H, Hongo M, et
43. Tachibana K, Hirota S, Iizasa H, Yoshida H, Kawabata K, Kataoka al. Bone marrow-derived CXCR4+ cells mobilized by macrophage
Y, et al. The chemokine receptor CXCR4 is essential for vascular- colony-stimulating factor participate in the reduction of infarct area
ization of the gastrointestinal tract. Nature 1998; 393: 591 – 594. and improvement of cardiac remodeling after myocardial infarc-
44. Nagasawa T, Hirota S, Tachibana K, Takakura N, Nishikawa S, tion in mice. Am J Pathol 2007; 171: 755 – 766.
Kitamura Y, et al. Defects of B-cell lymphopoiesis and bone- 59. Misao Y, Takemura G, Arai M, Ohno T, Onogi H, Takahashi T, et
marrow myelopoiesis in mice lacking the CXC chemokine PBSF/ al. Importance of recruitment of bone marrow-derived CXCR4+
SDF-1. Nature 1996; 382: 635 – 638. cells in post-infarct cardiac repair mediated by G-CSF. Cardiovasc
45. Zou YR, Kottmann AH, Kuroda M, Taniuchi I, Littman DR. Func- Res 2006; 71: 455 – 465.
tion of the chemokine receptor CXCR4 in haematopoiesis and in 60. Brunner S, Winogradow J, Huber BC, Zaruba MM, Fischer R, David
cerebellar development. Nature 1998; 393: 595 – 599. R, et al. Erythropoietin administration after myocardial infarction in
46. Salcedo R, Ponce ML, Young HA, Wasserman K, Ward JM, mice attenuates ischemic cardiomyopathy associated with enhanced
Kleinman HK, et al. Human endothelial cells express CCR2 and homing of bone marrow-derived progenitor cells via the CXCR-4/
respond to MCP-1: Direct role of MCP-1 in angiogenesis and tumor SDF-1 axis. FASEB J 2009; 23: 351 – 361.
progression. Blood 2000; 96: 34 – 40. 61. Segers VF, Tokunou T, Higgins LJ, MacGillivray C, Gannon J,
47. Jin DK, Shido K, Kopp HG, Petit I, Shmelkov SV, Young LM, et Lee RT. Local delivery of protease-resistant stromal cell derived
al. Cytokine-mediated deployment of SDF-1 induces revasculariza- factor-1 for stem cell recruitment after myocardial infarction. Cir-
tion through recruitment of CXCR4+ hemangiocytes. Nat Med culation 2007; 116: 1683 – 1692.
2006; 12: 557 – 567. 62. Zaruba MM, Theiss HD, Vallaster M, Mehl U, Brunner S, David
48. Wei YJ, Tang Y, Li J, Cui CJ, Zhang H, Zhang XL, et al. Cloning R, et al. Synergy between CD26/DPP-IV inhibition and G-CSF
and expression pattern of dog SDF-1 and the implications of altered improves cardiac function after acute myocardial infarction. Cell
expression of SDF-1 in ischemic myocardium. Cytokine 2007; 40: Stem Cell 2009; 4: 313 – 323.
52 – 59. 63. Takahashi M, Masuyama J, Ikeda U, Kasahara T, Kitagawa S,
49. Askari AT, Unzek S, Popovic ZB, Goldman CK, Forudi F, Takahashi Y, et al. Induction of monocyte chemoattractant protein-
Kiedrowski M, et al. Effect of stromal-cell-derived factor 1 on stem- 1 synthesis in human monocytes during transendothelial migration
cell homing and tissue regeneration in ischaemic cardiomyopathy. in vitro. Circ Res 1995; 76: 750 – 757.
Lancet 2003; 362: 697 – 703. 64. Takahashi M, Masuyama J, Ikeda U, Kitagawa S, Kasahara T, Saito
50. Proulx C, El-Helou V, Gosselin H, Clement R, Gillis MA, M, et al. Suppressive role of endogenous endothelial monocyte che-
Villeneuve L, et al. Antagonism of stromal cell-derived factor- moattractant protein-1 on monocyte transendothelial migration in
1alpha reduces infarct size and improves ventricular function after vitro. Arterioscler Thromb Vasc Biol 1995; 15: 629 – 636.
myocardial infarction. Pflugers Arch 2007; 455: 241 – 250. 65. Takahashi M, Masuyama J, Ikeda U, Kitagawa S, Kasahara T, Saito
51. Chang LT, Yuen CM, Sun CK, Wu CJ, Sheu JJ, Chua S, et al. Role M, et al. Effects of endogenous endothelial interleukin-8 on neu-
of stromal cell-derived factor-1alpha, level and value of circulating trophil migration across an endothelial monolayer. Cardiovasc Res
interleukin-10 and endothelial progenitor cells in patients with acute 1995; 29: 670 – 675.
Circulation Journal Vol.74, March 2010
Potrebbero piacerti anche
- Cellular, Molecular, and Environmental Contribution in Cardiac Remodeling: From Lab Bench Work to its Clinical PerspectiveDa EverandCellular, Molecular, and Environmental Contribution in Cardiac Remodeling: From Lab Bench Work to its Clinical PerspectiveNessuna valutazione finora
- Repair After Myocardial Infarction, Between Fantasy and RealityDocumento6 pagineRepair After Myocardial Infarction, Between Fantasy and RealitydanielcpnkimoNessuna valutazione finora
- 2021 CURR ORIBK CARDIOL Septic Cardiomiopathy From Basics To Management ChoicesDocumento18 pagine2021 CURR ORIBK CARDIOL Septic Cardiomiopathy From Basics To Management ChoicesConny MuñozNessuna valutazione finora
- In Ammatory Response Post-Myocardial Infarction and Reperfusion: A New Therapeutic Target?Documento10 pagineIn Ammatory Response Post-Myocardial Infarction and Reperfusion: A New Therapeutic Target?CRAULNessuna valutazione finora
- Bowel ObstructionDocumento23 pagineBowel Obstructiondwi yuniariNessuna valutazione finora
- The Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalDocumento9 pagineThe Effect of Hypoxia On Mesenchymal Stem Cell Biology: PharmaceuticalYolan TiaraNessuna valutazione finora
- EndhotheliumDocumento18 pagineEndhotheliumDzikrul Haq KarimullahNessuna valutazione finora
- IJC Heart & Vasculature: Molecular Mechanisms and Genetic Regulation in AtherosclerosisDocumento10 pagineIJC Heart & Vasculature: Molecular Mechanisms and Genetic Regulation in Atherosclerosisuser1818Nessuna valutazione finora
- Atypical Chemokine Receptors in Cardiovascular DiseaseDocumento8 pagineAtypical Chemokine Receptors in Cardiovascular DiseasespraptamaNessuna valutazione finora
- Bone Marrow Mesenchymal Stem Cell-Derived ExosomesDocumento9 pagineBone Marrow Mesenchymal Stem Cell-Derived Exosomesiam_ca2Nessuna valutazione finora
- Cell Therapy in Patients With Critical Limb IschemiaDocumento27 pagineCell Therapy in Patients With Critical Limb IschemiaAsep HrNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento20 pagineNIH Public Access: Author ManuscriptLeonardo SánchezNessuna valutazione finora
- FCVM 08 750510Documento11 pagineFCVM 08 750510Joseph SebastianNessuna valutazione finora
- A Novel Paradigm For Heart Failure With Preserved Ejection FractionDocumento9 pagineA Novel Paradigm For Heart Failure With Preserved Ejection FractionviannikkkyNessuna valutazione finora
- Project Injectable Hydrogels As Recent Advances in Treatment of Myocardial InfarctionDocumento16 pagineProject Injectable Hydrogels As Recent Advances in Treatment of Myocardial Infarctionvarshankpathak2001Nessuna valutazione finora
- 1 s2.0 S0735109716000139 MainDocumento13 pagine1 s2.0 S0735109716000139 MainFilip MarkovićNessuna valutazione finora
- Pi Is 0021915021011977Documento12 paginePi Is 0021915021011977spraptamaNessuna valutazione finora
- Inflammatory Biomarkers in Acute Coronary Syndromes: Clinician UpdateDocumento9 pagineInflammatory Biomarkers in Acute Coronary Syndromes: Clinician UpdateSandi AuliaNessuna valutazione finora
- Neutrofils in Post Myocardial Infarction InflammationDocumento9 pagineNeutrofils in Post Myocardial Infarction InflammationMeutia SavitriNessuna valutazione finora
- Increased Level of Circulating Endothelial Microparticles and Cardiovascular Risk FactorsDocumento6 pagineIncreased Level of Circulating Endothelial Microparticles and Cardiovascular Risk FactorsFilipos ConstantinNessuna valutazione finora
- Atherosclerosis PathophysiologyDocumento11 pagineAtherosclerosis PathophysiologyCandice ChengNessuna valutazione finora
- Coronary Microvascular Dysfunction Across The SpectrumDocumento34 pagineCoronary Microvascular Dysfunction Across The SpectrumChristian BuesaquilloNessuna valutazione finora
- Matrix MetalloproteinasesDocumento7 pagineMatrix MetalloproteinasesJesús Eduardo SánchezNessuna valutazione finora
- Atherosclerosis As InflammationDocumento9 pagineAtherosclerosis As InflammationCandice Cheng0% (1)
- Rol de CaMKII en AritmiaDocumento5 pagineRol de CaMKII en AritmiaAlexis Jesus GomezNessuna valutazione finora
- Microparticles in Vascular DiseaseDocumento5 pagineMicroparticles in Vascular DiseaseRichard ChandraNessuna valutazione finora
- Role and Importance of Biochemical Markers in Clinical CardiologyDocumento10 pagineRole and Importance of Biochemical Markers in Clinical CardiologybernadethNessuna valutazione finora
- Cec y Respuesta InflamatoriaDocumento11 pagineCec y Respuesta InflamatoriamaritzabericesNessuna valutazione finora
- 0271678x20953912 PDFDocumento19 pagine0271678x20953912 PDFHana Elsi putriNessuna valutazione finora
- Qin, Et Al. 2022Documento29 pagineQin, Et Al. 2022Ignacio BarbieriNessuna valutazione finora
- Colip 27 408Documento6 pagineColip 27 408taniasolisNessuna valutazione finora
- Journal of Intensive Medicine: Florence Boissier, Nadia AissaouiDocumento9 pagineJournal of Intensive Medicine: Florence Boissier, Nadia AissaouiMaudiel BrionesNessuna valutazione finora
- Joim 12367Documento21 pagineJoim 12367Andian IkbarNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento12 pagineNIH Public Access: Author ManuscriptMuhammad Dadan KurniawanNessuna valutazione finora
- Mechanisms of Cardiac HypertrophyDocumento11 pagineMechanisms of Cardiac HypertrophyantothesaberNessuna valutazione finora
- Circulation 2004 Zhu 2109 15Documento8 pagineCirculation 2004 Zhu 2109 15gekayuuNessuna valutazione finora
- Journal of Molecular and Cellular Cardiology: SciencedirectDocumento2 pagineJournal of Molecular and Cellular Cardiology: SciencedirectCarolina RicárdezNessuna valutazione finora
- Oppi Et Al 2019 - Athero FrontierDocumento8 pagineOppi Et Al 2019 - Athero FrontierOlry Le NobelNessuna valutazione finora
- Mesenchymal Stem Cell Treatment of Diabetes Mellitus CryovidaDocumento6 pagineMesenchymal Stem Cell Treatment of Diabetes Mellitus CryovidaMartín EspinozaNessuna valutazione finora
- Thesis On Ischemic Heart DiseaseDocumento5 pagineThesis On Ischemic Heart DiseaseOrderCustomPapersCanada100% (2)
- Cardiac Rehabilitation and Endothelial Function: Clinical MedicineDocumento15 pagineCardiac Rehabilitation and Endothelial Function: Clinical Medicinetri windartiNessuna valutazione finora
- Cytokines Their Role in Stroke and Potential Use As Biomarkers A 2014Documento14 pagineCytokines Their Role in Stroke and Potential Use As Biomarkers A 2014Ana GabrielaNessuna valutazione finora
- Mitochondrial Dysfunction in Pathophysiology of Heart FailureDocumento12 pagineMitochondrial Dysfunction in Pathophysiology of Heart FailureBernardus MartinoNessuna valutazione finora
- Mechanisms of Cardiovascular Homeostasis and Pathophysiology Expression, Signal Transduction To Cellular CommunicationDocumento2 pagineMechanisms of Cardiovascular Homeostasis and Pathophysiology Expression, Signal Transduction To Cellular CommunicationRyan Carlo CondeNessuna valutazione finora
- 2019 Article 73Documento10 pagine2019 Article 73Radu AvramNessuna valutazione finora
- The Role of Cytokines in Acute Myeloid Leukemia: A Systematic ReviewDocumento12 pagineThe Role of Cytokines in Acute Myeloid Leukemia: A Systematic Reviewhoangphuong08101992Nessuna valutazione finora
- Do We Know Enough About The Immune Pathogenesis of Acute Coronary Syndromes To Improve Clinical Practice?Documento14 pagineDo We Know Enough About The Immune Pathogenesis of Acute Coronary Syndromes To Improve Clinical Practice?Erika KennedyNessuna valutazione finora
- Shenmai Injection Attenuates Myocardial Ischemia/Reperfusion Injury by Targeting Nrf2/GPX4 Signalling-Mediated FerroptosisDocumento9 pagineShenmai Injection Attenuates Myocardial Ischemia/Reperfusion Injury by Targeting Nrf2/GPX4 Signalling-Mediated Ferroptosis14-120 RahmaNessuna valutazione finora
- Ischemic Heart Disease Pathophysiology Paradigms Overview: From Plaque Activation To Microvascular DysfunctionDocumento30 pagineIschemic Heart Disease Pathophysiology Paradigms Overview: From Plaque Activation To Microvascular DysfunctionFannyNessuna valutazione finora
- 5 Troxerutin Cerebral Ischemia MMR2019Documento11 pagine5 Troxerutin Cerebral Ischemia MMR2019Mtro. Javier Alfredo Carballo PereaNessuna valutazione finora
- Clinic Trăilă of StemDocumento22 pagineClinic Trăilă of StemRadu AvramNessuna valutazione finora
- Bba - Molecular Basis of Disease: SciencedirectDocumento12 pagineBba - Molecular Basis of Disease: SciencedirectBiancaNessuna valutazione finora
- TMP 4 DEDDocumento6 pagineTMP 4 DEDFrontiersNessuna valutazione finora
- Post Translational Modifications On B Myosin Heavy Chain 1653708664Documento24 paginePost Translational Modifications On B Myosin Heavy Chain 1653708664Happy InsightsNessuna valutazione finora
- jcm-08-00537 YDA 7Documento11 paginejcm-08-00537 YDA 7Muhammad Sandy Ali YafieNessuna valutazione finora
- The Cardiac Wound Healing Response To Myocardial InfarctionDocumento19 pagineThe Cardiac Wound Healing Response To Myocardial Infarctionluis sanchezNessuna valutazione finora
- Dutka2019 Article TheRelevanceOfInPost-iDocumento12 pagineDutka2019 Article TheRelevanceOfInPost-igeorgiaNessuna valutazione finora
- Pathophysiology of Sepsis-Induced Myocardial Dysfunction: Review Open AccessDocumento9 paginePathophysiology of Sepsis-Induced Myocardial Dysfunction: Review Open AccessjessicaesmrldaNessuna valutazione finora
- Bioquimica de La Isquemia y Reperfusion ArticuloDocumento35 pagineBioquimica de La Isquemia y Reperfusion ArticulofelipeNessuna valutazione finora
- Cell Death Pathways in Ischemic Stroke and Targeted PharmacotherapyDocumento18 pagineCell Death Pathways in Ischemic Stroke and Targeted PharmacotherapyHeath HensleyNessuna valutazione finora
- ABC of Chemotherapy April 27Documento2 pagineABC of Chemotherapy April 27tricia_casas9370Nessuna valutazione finora
- PSAvs PsadDocumento6 paginePSAvs PsadRaga ManduaruNessuna valutazione finora
- Koding Bpjs CMF Rs. Swasta Regional 1 - Permenkes No. 64 Tahun 2016Documento33 pagineKoding Bpjs CMF Rs. Swasta Regional 1 - Permenkes No. 64 Tahun 2016eviNessuna valutazione finora
- Diseases of The Central AirwaysDocumento385 pagineDiseases of The Central AirwayspcygbNessuna valutazione finora
- LungIndia323241-4636559 125245Documento5 pagineLungIndia323241-4636559 125245Nishant AggarwalNessuna valutazione finora
- ELSA 2019 Program Scientific ProgramDocumento22 pagineELSA 2019 Program Scientific ProgramShinta DeboraNessuna valutazione finora
- Uterine ProlapseDocumento35 pagineUterine ProlapsecitidotnetNessuna valutazione finora
- Chapter 1 - "Anti-Angiogenesis Property of Eleucine Indica in CAM Assay"Documento5 pagineChapter 1 - "Anti-Angiogenesis Property of Eleucine Indica in CAM Assay"alche mae legasteNessuna valutazione finora
- Malignant Hypertension - Dr. Todung PDFDocumento12 pagineMalignant Hypertension - Dr. Todung PDFMuhammad Khoirul SodiqNessuna valutazione finora
- International Obstetric and Gynecology Conference 2019 ScheduleDocumento6 pagineInternational Obstetric and Gynecology Conference 2019 ScheduleAndianto IndrawanNessuna valutazione finora
- CAMAF Benefit Brochure 2014Documento2 pagineCAMAF Benefit Brochure 20140796105632Nessuna valutazione finora
- Endocrine System DisordersDocumento83 pagineEndocrine System DisordersJerilee SoCute Watts0% (1)
- Tumors of SpineDocumento13 pagineTumors of Spinebosnia agusNessuna valutazione finora
- Sexually Transmitted Disease 4th YearsDocumento77 pagineSexually Transmitted Disease 4th YearsAakashNessuna valutazione finora
- ThyroidectomyDocumento51 pagineThyroidectomyPopey Moore100% (1)
- Agreement and Thesis Proposal ArnelDocumento5 pagineAgreement and Thesis Proposal ArnelarnelNessuna valutazione finora
- Journal of Learning InsightsDocumento12 pagineJournal of Learning InsightsJisel-Apple Bulan100% (2)
- Proposal of Breast CancerDocumento52 pagineProposal of Breast CancerOm Communication SatationeryNessuna valutazione finora
- A Mathematical Model For Analysis of The Cell Cycle in Human TumoursDocumento24 pagineA Mathematical Model For Analysis of The Cell Cycle in Human TumoursObetz ClNessuna valutazione finora
- SyncopeDocumento12 pagineSyncopeSuha AbdullahNessuna valutazione finora
- DRUG NAME: Rituximab: Synonym (S) : Common Trade Name (S) : ClassificationDocumento12 pagineDRUG NAME: Rituximab: Synonym (S) : Common Trade Name (S) : ClassificationpmuftiaNessuna valutazione finora
- UTI Guideline Example 2 Appendix B PDFDocumento4 pagineUTI Guideline Example 2 Appendix B PDFamira catriNessuna valutazione finora
- Nephrotic SyndromeDocumento56 pagineNephrotic SyndromeMurugesan100% (1)
- Noninvasive Radiofrequency Ablation of Cancer Targeted by Gold NanoparticlesDocumento8 pagineNoninvasive Radiofrequency Ablation of Cancer Targeted by Gold NanoparticlesMiguel Castañeda LeonNessuna valutazione finora
- 31 Surprising Benefits of Onions For Skin, Hair and HealthDocumento40 pagine31 Surprising Benefits of Onions For Skin, Hair and HealthPriyakrishnaVasamsettiNessuna valutazione finora
- PancytopeniaDocumento9 paginePancytopeniadrhammadtufailNessuna valutazione finora
- Lin Syndrome PDFDocumento2 pagineLin Syndrome PDFdavidninrio50% (2)
- 7 Bali Cardiology Update 2018Documento14 pagine7 Bali Cardiology Update 2018nova cintyaNessuna valutazione finora
- Acute GastroenteritisDocumento29 pagineAcute GastroenteritisMASII100% (13)
- Script Ma'am PrescyDocumento9 pagineScript Ma'am PrescyErl Joseph G. EvangelioNessuna valutazione finora