Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
A Boy With Recurrent Pneumonia
Caricato da
Tonny ChenCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
A Boy With Recurrent Pneumonia
Caricato da
Tonny ChenCopyright:
Formati disponibili
A boy with recurrent
pneumonia E. Mantzouranis
K. Mathianaki
M.D. Fitrolaki
E. Mihailidou
P. Paspalaki
Division of Pulmonary, Allergy and
In the previous two issues of Breathe, the case Immunology, Department of
of a 6-yr-old boy who had been admitted to Pediatrics, University Hospital of
the paediatric department of the University of Heraklion, University of Crete,
Heraklion has been covered. After treatment, Heraklion, Crete, Greece
he was discharged in excellent condition.
Correspondence
E. Mantzouranis
Associate Professor of Pediatrics
12 months later, the boy was readmitted to the right lower hemithorax. Cardiac examination University of Crete
hospital for gradually increasing productive was normal, throat examination showed small Director of the Division of
Pulmonary Allergy and
cough for 9 days and fever (up to 39.5uC) for exudates on tonsils and review of remaining Immunology
3 days. systems was normal. Dept of Pediatrics
He was in good condition. His blood Chest radiograph (CXR) is shown in figure 1. University Hospital of Heraklion
temperature was 38uC, respiratory rate was Heraklion
24 breaths?min-1, heart rate was 120 beats?min-1 Task 1 71110
and O2 saturation was 91%. On chest ausculta- How would you interpret this CXR? Crete
Greece
tion he had decreased breath sounds over the mantzourani@med.uoc.gr
Statement of interest
None declared
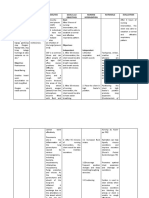
Figure 1
CXR
HERMES syllabus link: module
B.3.6, C.1.10, D.3.1
DOI: 10.1183/20734735.220710 Breathe | September 2011 | Volume 8 | No 1 71
A boy with recurrent pneumonia
Answer 1 Answer 2
The posteroanterior (left) and lateral (right) Bacterial or viral pneumonia.
CXRs show opacification/consolidation of the
right lower and middle lung lobes. There was
blunting of the right costophrenic angle with Due to symptoms, radiographic findings,
small fluid collection. Right hemidiaphragm leukocytosis with increased neutrophils, ESR and
was not seen (positive ‘‘silhouette’’ sign). CRP the diagnosis of bacterial pneumonia was
made. The patient was treated with intravenous
ampicillin–sulbactam 150 mg?kg-1?day-1, oral clar-
Blood test results are shown in table 1. ithromycin (1 g?day-1) and inhaled bronchodila-
Chemistry lab tests were normal and blood tors. Chest auscultation revealed wet crackles
cultures were sent. which were gradually diminished to normal
breath sound. Fever subsided on the 4th day.
Intravenous antibiotics were given for 10 days.
Table 1 Blood test results Repeat lab tests are shown in table 2. Blood
cultures were negative. Cold agglutinins for
White blood cells cells?mm-3 13,700 mycoplasma and pneumococcus antigen in the
Polymorphonucleates % 73.8 urine were negative. Stain of sputum showed
Lymphocytes % 21.8 increased white cells. Sputum culture was
Monocytes % 7 negative.
Eosonophils % 0.62 Repeat CXR 10 days later is shown in
Haemoglobin g?dL-1 11.9 figure 2.
Haematocrit % 35.7
Platelets n?mm-3 248
Erythrocyte sedimentation rate mm?h-1 57
C-reactive protein mg?dL-1 12.6
Task 2
What is your diagnosis?
Table 2 Repeat blood test results
White blood cells cells?mm-3 6,600 Figure 2
Polymorphonucleates % 42.9 CXR
Lymphocytes % 46.4
Monocytes % 7.2
Eosonophils % 2.87 Task 3
Haemoglobin g?dL-1 12.2 How would you interpret the CXR?
Haematocrit % 37.3
Platelets n?mm-3 281
Erythrocyte sedimentation rate mm?h-1 18
C-reactive protein mg?dL-1 0.31
HERMES syllabus link: module
B.3.6, C.1.10, D.3.1
72 Breathe | September 2011 | Volume 8 | No 1
A boy with recurrent pneumonia
Answer 3 Answer 4
The CXR shows normal chest. 1. CXR is not needed now, since there are no
symptoms since last discharge.
2. Chest CT is not needed, for the same
The patient was discharged. A sweat test reason.
was performed to rule out cystic fibrosis and a 3. Spirometry, before and after bronchodila-
return appointment within a week was sched- tor, is indicated due to the history of
uled. In case of recurrence of symptoms, bronchitis and of three admissions for
bronchoscopy and test for primary ciliary recurrent pneumonia.
dyskinesia (PCK) would be performed. 4. Metacholine test is not indicated before
Results of lab tests showed: Mycoplasma spirometry is performed.
pneumoniae immunoglobulin (Ig)G: 14.9 (posi- 5. Bronchoscopy is indicated due to the
tive); IgM: 7.6 (negative); Chlamydia pneumo- history of recurrent pneumonias in the same
niae IgG and IgM: negative; Ricketsia Conorii lobe/region. This procedure can detect dyna-
IgG and IgM: negative; IgG: 1,230 mg?dL-1 mic airway collapse, can reach distal regions
(normal); IgM: 128 mg?dL-1 (normal); IgA: and can obtain samples from airways or
140 mg?dL-1 (normal); serum complement C3c: alveolar spaces for culture and cytologic
189 mg?dL-1 (increased); serum complement examination; however, bronchoscopy should
C4: 32 mg?dL-1 (normal); IgE: 16.2 IU?mL-1 not be done before noninvasive methods fail
(normal). RAST results were pending and sweat to identify the cause of recurrent symptoms.
test was negative.
The patient was referred to the Pediatric
Allergy Pulmonary Outpatient Clinic. Detailed Spirometry before and after bronchodilator is
history revealed that he had frequent cough shown in figure 3.
episodes attributed to viral colds. He was treated
for a short time with inhaled steroids and Flow L·s-1
salbutamol unsuccessfully. In the past, he was 2 0 2 4 6 8 10
evaluated for nasal symptoms and was diag- F/V ex
nosed with allergic rhinitis. He was given
antihistamines on a pro re nata basis.
His mother reported allergic skin rashes and ▲
positive RAST to olive tree pollen. A parental ■
■
cousin had frequent bronchitis episodes until the
2 ▲■
age of 14 yrs. Parental grandfather has chronic
obstructive pulmonary disease. The patient had a ■
▲
cat at home and was exposed to dogs, chicken,
pigeons, a pheasant and a peacock in his ■
▲ ▲ ■
grandparents’ environment. Vol L
On physical examination the patient Time s
0
appeared well; he had normal chest auscultation, 0 2 4 6 8
no clubbing and the rest of the examination was Figure 3
normal. Spirometry before and after bronchodilator
RAST results to known allergens (house dust
mites, olive pollen, parietaria, grass mix, mold
mix, H1 and H2) were negative. RAST to cat, Task 5
dog, chicken, pigeons and peacock were ordered. What do the spirometry data
suggest and can you propose a
diagnosis?
Task 4
Would you now order: 1) CXR; 2)
chest computed tomography (CT);
3) spirometry; 4) metacholine
test; or 5) bronchoscopy.
HERMES syllabus link: module
B.3.6, C.1.10, D.3.1
Breathe | September 2011 | Volume 8 | No 1 73
A boy with recurrent pneumonia
Answer 5 Answer 6
Flows (maximum midexpiratory flow (MMEF) Mild-to-moderate obstruction of small airways.
and forced expiratory flow between 25 and Reversibility of MMEF, FEF25, FEF50 and
75% of forced vital capacity (FEF25–75)) FEV0.5 after bronchodilators suggestive of
show a degree of obstruction, which is not mild-to-moderate asthma.
reversed after bronchodilators. Peak expira-
tory flow (PEF) showed a reversibility of
18.5%. Despite the lack of reversibility of Discussion
forced expiratory volume in 1 s (FEV1) and This report describes a child with three episodes
given that spirometry is not a sensitive of pneumonia. The patient meets the criteria for
test, particularly in children, the diagnosis recurrent pneumonia (RP) which is defined as
of asthma was considered based to the o2 episodes in a single year or o3 episodes
patient’s history and CXR findings. ever, with clearing of x-ray densities between
episodes [1]. Recurrent pneumonia occurs in 7.7–
9% of all children with pneumonia [2–5].
The patient was given inhaled steroids, long The aetiology of RP varies depending upon
acting b2 agonists for 1 month and was asked the location of pneumonia, which can involve a
to record his daily symptoms. single or various lobes or lung regions. This
1 month later, the patient’s diary showed patient’s three episodes of pneumonia occurred
cough induced by exercise, crying, intense odours in the same lung region.
and occasional nasal congestion. His IgE was Recurrent pneumonia involving a single lobe
normal, his additional RAST results were or segment, is caused by localised pathology,
negative. A sinus radiograph showed sinusitis. such as local compression, malformation or
He was prescribed antibiotics and nasal corticos- inflammation, whereas, pneumonias affecting
teroids for sinusitis. He was asked to continue his more than one lobe, suggest a more generalised
asthma treatment for 2 months and return for abnormality, such as mucociliary clearance dys-
assessment. At his next visit, he had improved function, aspiration, immunodeficiency or asthma.
but was still experiencing some symptoms. An The patient’s recurrent infiltrates occurred in right
anti-leukotriene receptor antagonist was added middle and right lower lobe.
to the treatment and, with this adjustment, the Recurrent pneumonia and atelectasis of the
patient was entirely asymptomatic. He would right middle lobe make up a unique entity
only experience exercise-induced cough when he known as ‘‘right middle lobe syndrome’’. This
forgot his medication. lobe is prone to infection and collapse because
Repeat spirometry, performed 1 yr later, is the bronchus arises from the bronchus inter-
shown in figure 4. medius at an acute angle and is relatively long
before it subdivides into segments [6]. Further-
Flow L·s-1 more, there is no collateral ventilation between
2 0 2 4 6 8 10 the right middle lobe and other lobes [7]. The
F/V ex most common noninfectious cause of right
middle lobe syndrome is asthma [8]; the most
■
common infectious cause is tuberculosis.
Task 6 We considered that the patient may have
What do the spiro- ■ ▲
▲
asthma because his abnormal chest radiographs
metry data and
flow–volume curve ■ were similar, affecting the right middle and right
2 ▲
suggest? lower lobe, all of his three episodes happened
■
▲ during spring, he had history of allergic rhinitis
and of recurrent bronchitis. The latter may mask
▲
■ ▲ ■ asthma [9].
Several studies have shown association
Vol L
Time s between RP and asthma. Older children with
0
0 2 4 6 8 asthma may develop recurrent chest infiltrates/
pneumonias [3, 4, 10]. In a study of 125
Figure 4
asthmatic children, 14 of them experienced 70
Repeat spirometry
episodes of recurrent pneumonia [11]. Moreover,
HERMES syllabus link: module undiagnosed or uncontrolled asthma was diag-
B.3.6, C.1.10, D.3.1 nosed f80% of children evaluated for recurrent
74 Breathe | September 2011 | Volume 8 | No 1
A boy with recurrent pneumonia
pneumonia [12], which can also be the initial [21]. Metacholine testing was not done in our
manifestation of asthma [8]. patient since, due to his young age, he could not
Chest radiograph densities, shown during collaborate. In very young children, for whom
asthma exacerbations, may be due to infections, spirometry or metacholine cannot be performed,
atelectasis or both [6, 13, 14]. The patient’s diagnosis of asthma requires an experienced
recurrent chest radiograph densities could paediatrician or a specialist.
represent asthma exacerbations and could be Due to our inability to confirm the diagnosis
due to infections or atelectasis or both. Fast of asthma through spirometry, we tried a 4-week
clearing of his radiographic findings, within a treatment with inhaled corticosteroids and
week, documented during hospitalisations, was bronchodilators. Clinical improvement and recur-
favouring atelectasis rather than pneumonia. rence of symptoms after cessation of therapy
The rate of resolution of infiltrates caused by confirmed the diagnosis of asthma [12].
viruses or bacteria is longer that one week; it During the patient’s admission several
ranges between 2–3 weeks for respiratory syncy- diagnoses were discussed as the underlying
tial virus, 6–8 weeks for pneumococcus [15], or cause of RP.
f12 months for adenovirus [16]. Clearing of chest radiograph and absence of
Asthma exacerbations are frequently trig- symptoms without treatment between admis-
gered by acute viral respiratory infections [12, 17, sions, were against extraluminal compression,
18] which may present with fever, increased congenital structural abnormalities of airways or
mucus secretions, plugging of bronchi, atelectasis lung parenchyma and foreign body aspiration
or occasionally with secondary bacterial infec- which was not considered due to the older age
tion. However, in some patients mucus induced (.3 yrs) of the patient.
atelectasis, without infection, can cause recurrent Immune deficiency could cause RP; however,
chest infiltrates, dyspnoea and fever [10] similar infections usually start at younger age and may
to the symptoms of our patient. involve more than one lobe or systems. Normal
In the hospital, the patient was diagnosed serum immunoglobulins ruled out B-cell defi-
with bacterial pneumonia due to fever, respiratory ciency. Adequate granulocyte count and quick
symptoms, the CXR report of ‘‘consolidation’’ and resolution of CXR findings were against neu-
the increased values of white blood cells, poly- trophil dysfunction which usually presents with
morphonuclear neutrophils, erythrocyte sedimen- persistent staphylococcal or aspergillus infections.
tation rate and C-reactive protein suggesting Cystic fibrosis (CF), another cause for RP, was
bacterial infection. Accordingly, he received anti- ruled out due to normal sweat test. Nevertheless,
biotics and asthma medication, due to previous normal nourishment, absence of gastrointestinal
bronchitis, and the laboratory indices improved. malabsorption, normal CXR between episodes
Paediatricians tend to treat a nonwheezing child were not suggestive of this diagnosis [6].
with antibiotics if the radiograph report states Investigation for primary ciliary dysfunction
‘‘focal airspace consolidation’’ or ‘‘focal infiltrate’’ (PCD) was discussed during the 3rd admission.
[19]. It is unclear whether atelectasis alone This functional inability to clear secretions,
without infection could cause laboratory indices presents with purulent rhinitis, recurrent middle
mimicking bacterial infection and whether these ear disease, situs inversus in one-half of patient’s
indices would improve without antibiotics. and possibly bronchiectasis [6], none of which
At the specialty clinic, we attributed the were present in our patient or shown in chest CT.
patient’s symptoms and chronic cough, triggered A few series have reported RP in children
by viral stimuli, to bronchial hyper-reactivity caused showing that an underlying cause of RP is
by asthma. The initial spirometry, however, did not usually identified and can vary greatly in
show reversibility, despite the presence of CXR different geographic locations [22].
infiltrates, possibly representing inflammation. A In Spain, the most common underlying
study of young adults with mild-to-moderate causes for RP included asthma (30.4%),
asthma, showed that only 36% had positive congenital cardiac defects (29.3%), and aspira-
spirometry suggesting asthma, while 59% had tion syndrome (27.1%) [23]. In the USA, 40%
negative spirometry, but positive radiograph of patients with RP had asthma, 10% aspiration
showing ‘‘increased markings’’ representing inflam- and 5% immunodeficiency syndromes [10]. In
mation [20]. A negative spirometry test does not Turkey, the most common underlying causes of
exclude the diagnosis of asthma in children [6]. RP were asthma (32%), gastro-oesophageal
If spirometry is normal, a metacholine test to reflux (15%), and in children younger than 2 yrs HERMES syllabus link: module
detectbronchial hyperactivity should be considered old, immunodeficiency (10%) and aspiration B.3.6, C.1.10, D.3.1
Breathe | September 2011 | Volume 8 | No 1 75
A boy with recurrent pneumonia
syndromes (3%) [4]. In contrast, in series from We considered this case unusual because
Canada [3] and India [5], aspiration was the of the: presentation of asthma, nonreversibility
leading cause [6]. of spirometry despite recurrent CXR inflamma-
Diagnosis of asthma, even if it can tion, absence of atopy, laboratory tests
frequently cause recurrent pneumonia, was not suggesting bacterial pneumonia, while fast
initially considered in our patient, because he did clearing of CXR infiltrates was suggesting
not have the classic symptoms of episodic atelectasis. However, the response of the
wheezing, atopy, nocturnal or exercise-induced patient to appropriate anti-asthma treatment
cough. Instead, prior to hospital admissions he was excellent. Interestingly, 2 years after the
had fever, cough and dyspnoea. These symptoms treatment started, he is entirely asymptomatic
and not wheezing may be the initial presenta- with his spirometry showing reversibility of
tion of asthma [12, 24–26]. obstruction in small bronchi.
References
1. Wald ER. Recurrent and nonresolving pneumonia. Semin Respir Infect 1993; 8: 46–58.
2. Weigl JA, Bader HM, Everding A, et al. Population-based burden of pneumonia before school entry in Schleswig-
Holstein, Germany. Eur J Pediatr 2003; 162: 309–316.
3. Owayed AF, Campbell DM, Wang EE. Underlying causes of recurrent pneumonia in children. Arch Pediatr Adolesc Med
2000; 154: 190–194.
4. Ciftçi E, Güneş M, Köksal Y, et al. Underlying causes of recurrent pneumonia in Turkish children in a university
hospital. J Trop Pediatr 2003; 49: 212–215.
5. Lodha R, Puranik M, Natchu UC, et al. Recurrent pneumonia in children: clinical profile and underlying causes. Acta
Paediatr 2002; 91: 1170–1173.
6. Panitch HB. Evaluation of recurrent pneumonia. Pediatr Infect Dis J 2005; 24: 265–266.
7. Inners CR, Terry PB, Traystman RJ, et al. Collateral ventilation and the middle lobe syndrome. Am Rev Respir Dis
1978; 118: 305–310.
8. Dees SC, Spock A. Right middle lobe syndrome in children. JAMA 1966; 197: 8–14.
9. Taussig LM, Smith SM, Blumenfeld R. Chronic bronchitis in childhood: What is it? Pediatrics 1981; 67: 1–5.
10. Eigen H, Laughlin JJ, Homrighausen J. Recurrent pneumonia in children and its relationship to bronchial
hypereactivity. Pediatrics 1982; 70: 698–704.
11. Kjellman B. Bronchial asthma and recurrent pneumonia in children. Clinical evaluation of 14 children. Acta Paediatr
Scand 1967; 56: 651–659.
12. Vaughan D, Katkin JP. Chronic and recurrent pneumonias in children. Semin Respir Infect 2002; 17: 72–84.
13. Rushton AR. The role of the chest radiograph in the management of childhood asthma. Clin. Pediatr (Phila) 1982;
21: 325–328.
14. Eggleston PA, Ward BH, Pierson WE, et al. Radiographic abnormalities in acute asthma in children. Pediatrics 1974;
54: 442–449.
15. Jay SJ, Johanson WG Jr, Pierce AK. The radiographic resolution of Streptococcus pneumoniae pneumonia. N Engl J
Med 1975; 293: 798–801.
16. Osborne D, White P. Radiology of epidemic adenovirus 21 infection of the lower respiratory tract in infants and
young children. Am J Roentgenol 1979; 133: 397–400.
17. Glezen P, Denny FW. Epidemiology of acute lower respiratory disease in children. N Engl J Med 1973; 288: 498–505.
18. Papadopoulos NG, Papi A, Psarras S, et al. Mechanisms of rhinovirus-induced asthma. Paediatr Respir Rev 2004; 5:
255–260.
19. Spottswood SE, Liaw K, Hernanz-Schulman M, et al. The clinical impact of the radiology report in wheezing and
nonwheezing febrile children: a survey of clinicians. Pediatr Radiol 2009; 39: 348–353.
20. Rubenstein HS, Rosner BA, LeMay M, et al. The value of the chest X-ray in making the diagnosis of bronchial
asthma. Adolescence 1993; 28: 505–516.
21. Rubin BK. The evaluation of the child with recurrent chest infections. Pediatr Infect Dis 1985; 4: 88–98.
22. Regelmann WE. Diagnosing the cause of recurrent and persistent pneumonia in children. Pediatr Ann 1993; 22:
561–568.
23. Cabezuelo Huerta G, Vidal Micó S, Abeledo Gómez A, et al. [Underlying causes of recurrent pneumonia.] Ann Pediatr
(Barc) 2005; 63: 409–412.
24. Cloutier MM, Loughlin GM. Chronic cough in children: a manifestation of airway hyperactivity. Pediatrics 1981; 67:
6–12.
25. Corrao WM, Braman SS, Irwin RS. Chronic cough as the sole presenting manifestation of bronchial asthma. N Engl J
Med 1979; 300: 633–637.
26. McFadden ERL. Exertional dyspnea and cough as preludes to acute attacks of bronchial asthma. N Engl J Med 1975;
292: 555–559.
HERMES syllabus link: module
B.3.6, C.1.10, D.3.1
76 Breathe | September 2011 | Volume 8 | No 1
Potrebbero piacerti anche
- History Birads PDFDocumento15 pagineHistory Birads PDFTonny ChenNessuna valutazione finora
- Classification AO PediatricDocumento36 pagineClassification AO PediatricdvcmartinsNessuna valutazione finora
- Rectal Prolapse CaseDocumento20 pagineRectal Prolapse CaseTonny ChenNessuna valutazione finora
- Cme SG Guidelines BPHDocumento8 pagineCme SG Guidelines BPHTonny ChenNessuna valutazione finora
- 02 BIRADS Mammography ReportingDocumento20 pagine02 BIRADS Mammography ReportinglPiNGUSlNessuna valutazione finora
- SalmonellaDocumento1 paginaSalmonellaTonny ChenNessuna valutazione finora
- Hirschsprung's Disease - Diagnosis and Management (Kessmann, 2006) PDFDocumento4 pagineHirschsprung's Disease - Diagnosis and Management (Kessmann, 2006) PDFMuhammad ReyhanNessuna valutazione finora
- Congenital Heart Disease Handout CHD PDFDocumento82 pagineCongenital Heart Disease Handout CHD PDFTonny Chen100% (1)
- CMV Induced Neonatal Cholestasis A Success Story PDFDocumento2 pagineCMV Induced Neonatal Cholestasis A Success Story PDFTonny ChenNessuna valutazione finora
- Protokol2 Nefro PDFDocumento8 pagineProtokol2 Nefro PDFTonny ChenNessuna valutazione finora
- Chole StasisDocumento4 pagineChole StasisTonny ChenNessuna valutazione finora
- Dysmorphic InfantDocumento5 pagineDysmorphic InfantTonny ChenNessuna valutazione finora
- Drug Doses 2017Documento127 pagineDrug Doses 2017Yuliawati HarunaNessuna valutazione finora
- Recurrent Pneumonia in ChildrenDocumento13 pagineRecurrent Pneumonia in ChildrenTonny ChenNessuna valutazione finora
- CK NotesDocumento25 pagineCK NotesFahad AliNessuna valutazione finora
- Guideline Kawasaki Disease AHA PDFDocumento8 pagineGuideline Kawasaki Disease AHA PDFTonny ChenNessuna valutazione finora
- Maintenance & Replacement Fluid Therapy: Moderated by DR - Madhuri EngadeDocumento43 pagineMaintenance & Replacement Fluid Therapy: Moderated by DR - Madhuri EngadeTonny ChenNessuna valutazione finora
- Fluid Electrolyte TherapyDocumento15 pagineFluid Electrolyte Therapyaarm1990Nessuna valutazione finora
- 1 s2.0 S1574626716300386 MainDocumento7 pagine1 s2.0 S1574626716300386 MainTonny ChenNessuna valutazione finora
- Recurrent Pneumonia - . - Not!: OmmentaryDocumento2 pagineRecurrent Pneumonia - . - Not!: OmmentaryAnantaBenvenutoNessuna valutazione finora
- Jco 2015 61 5906Documento12 pagineJco 2015 61 5906Tonny ChenNessuna valutazione finora
- Spirometry in PracticeDocumento24 pagineSpirometry in Practiceuser_at_scribd100% (1)
- 2016 Heartfailure - Eurheartj.ehw128.fullDocumento85 pagine2016 Heartfailure - Eurheartj.ehw128.fullTonny ChenNessuna valutazione finora
- The Pathophysiology, Diagnosis and Current Management of Acute Compartment SyndromeDocumento10 pagineThe Pathophysiology, Diagnosis and Current Management of Acute Compartment SyndromeTonny ChenNessuna valutazione finora
- Clemency Is Not Granted by Jokowi To Dui Bali Nine CaseDocumento1 paginaClemency Is Not Granted by Jokowi To Dui Bali Nine CaseTonny ChenNessuna valutazione finora
- JNC 8Documento14 pagineJNC 8amiwahyuniNessuna valutazione finora
- JNC 8Documento14 pagineJNC 8amiwahyuniNessuna valutazione finora
- Easy Way To Learn ABGsDocumento13 pagineEasy Way To Learn ABGsMunaim TahirNessuna valutazione finora
- Personal ReportDocumento1 paginaPersonal ReportTonny ChenNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Anthrax Clinical PathwayDocumento4 pagineAnthrax Clinical PathwayNeurologianak HarkitNessuna valutazione finora
- NAPOLCOM Welfare Benefits For PNPDocumento64 pagineNAPOLCOM Welfare Benefits For PNPIsko Brion55% (11)
- First Aid MnemonicsDocumento27 pagineFirst Aid MnemonicsRafael G. Garcia SanchezNessuna valutazione finora
- Atypical PneumoniaDocumento30 pagineAtypical PneumoniachandanNessuna valutazione finora
- Open Access Textbook of General SurgeryDocumento7 pagineOpen Access Textbook of General SurgeryusamaNessuna valutazione finora
- Diagnosis and Management of Infectious Diseases PDFDocumento477 pagineDiagnosis and Management of Infectious Diseases PDFdanielguerinNessuna valutazione finora
- Noninvasive Airway Management Techniques How and When To Use ThemDocumento16 pagineNoninvasive Airway Management Techniques How and When To Use ThemBulborea MihaelaNessuna valutazione finora
- Case StudyDocumento25 pagineCase StudybomcorNessuna valutazione finora
- INFECTIONS Staphylococcal InfectionsDocumento48 pagineINFECTIONS Staphylococcal InfectionsDr.P.NatarajanNessuna valutazione finora
- BTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Documento2 pagineBTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Corry ApriliaNessuna valutazione finora
- Exam 03.2017 FullDocumento50 pagineExam 03.2017 Fullmichal ben meronNessuna valutazione finora
- IMCI NewDocumento151 pagineIMCI NewDiana Lane CunananNessuna valutazione finora
- FINAL EXAM Grade 8 3rd QuarterDocumento5 pagineFINAL EXAM Grade 8 3rd QuarterPrincess Ciara Yvonne JamuyotNessuna valutazione finora
- Pola Kuman Pasien Pneumonia Di InstalasiDocumento6 paginePola Kuman Pasien Pneumonia Di Instalasiigo riskoNessuna valutazione finora
- Questions PneumoniaDocumento8 pagineQuestions PneumoniaMeliza BancolitaNessuna valutazione finora
- Macrolides and LincosamidesDocumento22 pagineMacrolides and LincosamidesSunilNessuna valutazione finora
- Cues Nursing Diagnosis Analysis GOALS and Objectives Nursing Intervention Rationale Evaluation Subjective: GoalDocumento4 pagineCues Nursing Diagnosis Analysis GOALS and Objectives Nursing Intervention Rationale Evaluation Subjective: GoalMonica Angelique SalayoNessuna valutazione finora
- Jurding TBDocumento26 pagineJurding TBRaja Ahmad Rusdan MusyawirNessuna valutazione finora
- Apea Review QuestionDocumento51 pagineApea Review Questionlisa100% (9)
- MCQ Asthma CopdDocumento26 pagineMCQ Asthma Copdanisa930804Nessuna valutazione finora
- Integrated Management of Childhood Illnesses (IMCI) : Dr. Pushpa Raj SharmaDocumento29 pagineIntegrated Management of Childhood Illnesses (IMCI) : Dr. Pushpa Raj SharmaEarl CorderoNessuna valutazione finora
- BacteriologyDocumento75 pagineBacteriologyHoward BarlomentoNessuna valutazione finora
- Studies On Public Health and Hygiene Condition of Retailers at Fish Markets in South-Central BangladeshDocumento8 pagineStudies On Public Health and Hygiene Condition of Retailers at Fish Markets in South-Central BangladeshHayyina FirdaniNessuna valutazione finora
- Western Mindanao State University College of Nursing: Zamboanga CityDocumento11 pagineWestern Mindanao State University College of Nursing: Zamboanga CitySHAINA ALIH. JUMAANINessuna valutazione finora
- Asthma Bronchiolitis P Nemo NiaDocumento64 pagineAsthma Bronchiolitis P Nemo NiainyesuaNessuna valutazione finora
- NCM112 LP2 TransesDocumento9 pagineNCM112 LP2 TransesChristine CalleyNessuna valutazione finora
- Okuda-Time Series Analysis of Under-Five MortalityDocumento61 pagineOkuda-Time Series Analysis of Under-Five MortalityBoniface Okuda100% (4)
- Katona and Katona-Apte - 2008 - The Interaction Between Nutrition and InfectionDocumento7 pagineKatona and Katona-Apte - 2008 - The Interaction Between Nutrition and InfectionYen Yen NiiNessuna valutazione finora
- NewEarth - University COVID-19 Intelligence BriefDocumento47 pagineNewEarth - University COVID-19 Intelligence BriefTony Lambert100% (1)
- Canada Gateway MCC Qe Questions 1Documento100 pagineCanada Gateway MCC Qe Questions 1Kak KfgaNessuna valutazione finora