Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Assessment
Caricato da
Jeenah Hannah0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
107 visualizzazioni7 pagineThe document describes a nursing care plan for a 52-year-old female patient admitted with chronic kidney disease, hypertension, and community acquired pneumonia. The plan outlines assessments of the patient's condition, diagnoses of impaired breathing and gas exchange, and nursing interventions over 6 hours to improve oxygenation and reduce symptoms like dyspnea and fatigue through medication administration, positioning, breathing exercises, and monitoring of vital signs.
Descrizione originale:
hi
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoThe document describes a nursing care plan for a 52-year-old female patient admitted with chronic kidney disease, hypertension, and community acquired pneumonia. The plan outlines assessments of the patient's condition, diagnoses of impaired breathing and gas exchange, and nursing interventions over 6 hours to improve oxygenation and reduce symptoms like dyspnea and fatigue through medication administration, positioning, breathing exercises, and monitoring of vital signs.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
107 visualizzazioni7 pagineAssessment
Caricato da
Jeenah HannahThe document describes a nursing care plan for a 52-year-old female patient admitted with chronic kidney disease, hypertension, and community acquired pneumonia. The plan outlines assessments of the patient's condition, diagnoses of impaired breathing and gas exchange, and nursing interventions over 6 hours to improve oxygenation and reduce symptoms like dyspnea and fatigue through medication administration, positioning, breathing exercises, and monitoring of vital signs.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 7
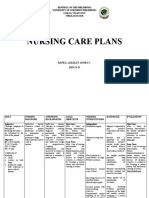
Mrs. G.M.C.
52 years old; Married; G10P0
Address: Carolina, Naga City
Admitting Diagnosis: CAP HR; ESRD HTNephrosis
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION EVALUATION
Independent
Dyspnea Impaired Breathing After 6 hours of nursing Assess patient’s After 6 hours of nursing
Pt appears to be Pattern intervention patient will general condition interventions patient has
pale be able to: Monitor and regained energy and was
Fatigue Regain energy record VS able to demonstrate
Use of accessory Verbalize Assess patient’s effective breathing
muscles understanding capillary refill pattern.
and demonstrate Encourage patient
effective to do deep
breathing breathing exercise
technique Dependent
Administered
nebulizer per
doctor’s order
Position patient to
semi-fowler’s
position
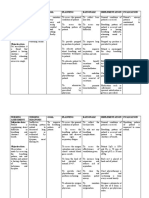
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION EVALUATION
Independent
Productive cough Ineffective Airway After 6 hours of nursing Assess patient’s After 6 hours of nursing
with sputum Clearance related to intervention, the patient’s condition intervention, the patient’s
production Increase sputum respiration will improve Monitor and respiration improved and
Dyspnea production and difficulty in breathing record VS difficulty in breathing shall
Changes in rate will be relieved Auscultate lung have been relieved.
and depth of fills
respiration Assist patient to
Adventitious change position
sound heard upon every 30 minutes
auscultation at Elevate HOB and
patient’s right align head of
lung patient in the
middle
Provide health
teachings
regarding
effective coughing
and deep
breathing exercise
Advise to increase
fluid intake
Dependent
Administer
medication as
ordered
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION EVALUATION
Subjective: Activity intolerance After 6 hours of nursing Independent
“Maluluya ang related to general interventions, the patient Bedside care done After 6 hours of nursing
pagmati ko.” As weakness will report/demonstrate a Monitor and intervention patient was
verbalized by the measurable increase in record VS able to:
patient tolerance activity with Encouraged Identify methods
Body malaise absence of dyspnea and patient to balance to reduce activity
noted excessive fatigue rest and activity intolerance.
Dyspnea Provide Exhibit tolerance
diversional during physical
activities such as activity
reading
newspaper and
watching TV
Advise patient to
perform passive
exercises
Assist patient to
comfortable
position
Provide adequate
rest period
Keep patient safe
on bed
Dependent
Administer
medication per
doctor’s order
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION EVALUATION
Restlessness Impaired Gas Exchange After 6 hours of nursing Independent After 6 hours of nursing
Dyspnea related to altered delivery interventions, the patient Assessed interventions, the patient
of oxygen will demonstrate respiratory rate, was able to:
participate in actions to depth, and ease. maximize
maximize oxygenation. Observed color of oxygenation.
skin, mucous
membranes, and
nail beds, noting
presence of
peripheral
cyanosis (nail
beds) or central
cyanosis
(circumoral).
Assessed mental
status.
Encouraged to
increase fluid
intake.
Maintained
bedrest.
Encourage use of
relaxation
techniques and
diversional
activities.
Elevated head
and encourage
frequent position
changes, deep
breathing, and
effective
coughing.
Assessed anxiety
level and
encourage
verbalization of
feelings and
concerns.
Observed for
deterioration in
condition, noting
hypotension,
copious amounts
of bloody sputum,
pallor, cyanosis,
change in LOC,
severe dyspnea,
and restlessness.
Monitored
oxygen saturation
as per doctors’
order.
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION EVALUATION
Deficient knowledge
After 6 hours of nursing Discuss debilitating aspects
interventions, the patient of disease, length of
related to will: convalescence, and recovery
misinterpretation of verbalize expectations. Identify self-
understanding of care and homemaker needs.
information condition/disease. Provide information in
Initiate necessary written and verbal form.
lifestyle changes Reinforce importance of
continuing
effective coughing and deep-
breathing exercises.
Emphasize necessity for
continuing antibiotic therapy
for prescribed period.
Outline steps to enhance
general health and well-
being: balanced rest and
activity, well-rounded diet,
avoidance of crowds during
cold/flu season and persons
with URIs.
Identify signs and symptoms
requiring notification of
health care
provider: increasing
dyspnea, prolonged fatigue,
weight loss, fever,
chills, persistence of
productive cough, changes
in mentation.
Potrebbero piacerti anche
- NCP Acute BronchitisDocumento9 pagineNCP Acute BronchitisCarl Simon CalingacionNessuna valutazione finora
- NCP - CapDocumento2 pagineNCP - CapbercoaprilgraceNessuna valutazione finora
- Actaul Drug StudyDocumento2 pagineActaul Drug Studyjasper pachingelNessuna valutazione finora
- Assessment Planning Intervention Rationale Evaluation: Nursing DiagnosisDocumento2 pagineAssessment Planning Intervention Rationale Evaluation: Nursing DiagnosisLovely CacapitNessuna valutazione finora
- APOLONIO, Reyjan L. (NCP 1)Documento2 pagineAPOLONIO, Reyjan L. (NCP 1)REYJAN APOLONIONessuna valutazione finora
- Nursing Care Plan: Cystic FibrosisDocumento4 pagineNursing Care Plan: Cystic FibrosisYael EzraNessuna valutazione finora
- Ineffective Breathing PatternDocumento2 pagineIneffective Breathing PatternEna Katherine CanonoNessuna valutazione finora
- UntitledDocumento4 pagineUntitledPie CanapiNessuna valutazione finora
- Nursing Care Plan #1Documento6 pagineNursing Care Plan #1Yamete KudasaiNessuna valutazione finora
- Ineffectuve Breathign PatternDocumento2 pagineIneffectuve Breathign PatternDiana Marie Magango FranciaNessuna valutazione finora
- Cap Nursing Care PlanDocumento6 pagineCap Nursing Care PlanCharlene Grace ReginoNessuna valutazione finora
- Assesment Diagnosis Planning Intervention Rationale EvaluationDocumento3 pagineAssesment Diagnosis Planning Intervention Rationale EvaluationTrisha Suazo100% (1)
- NCP 1 1Documento10 pagineNCP 1 1Samantha VeraNessuna valutazione finora
- Lumunok at Huminga, Nabibilaukan Din Ako Madalas" AsDocumento4 pagineLumunok at Huminga, Nabibilaukan Din Ako Madalas" AsPatricia Ortega100% (1)
- Clinical Case Scenario 6Documento17 pagineClinical Case Scenario 6Sean Menard Flores100% (1)
- NCP SciDocumento3 pagineNCP SciJaylord VerazonNessuna valutazione finora
- Nursing Care Plans: Republic of The Philippines University of Northern Philippines Tamag, Vigan City 2700 Ilocos SurDocumento6 pagineNursing Care Plans: Republic of The Philippines University of Northern Philippines Tamag, Vigan City 2700 Ilocos SurNo EulNessuna valutazione finora
- Cu 4Documento3 pagineCu 4Paul SahagunNessuna valutazione finora
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocumento1 paginaNursing Care Plan: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationsonylynneNessuna valutazione finora
- Case Pres Ncps FinalDocumento13 pagineCase Pres Ncps FinalMariejoy YadaoNessuna valutazione finora
- Bronchitis NCPDocumento8 pagineBronchitis NCPNikael Patun-ogNessuna valutazione finora
- Nursing Care Plan Assessment Diagnosis Outcome Intervention Rationale EvaluationDocumento5 pagineNursing Care Plan Assessment Diagnosis Outcome Intervention Rationale EvaluationMarivic Yuson MalagarNessuna valutazione finora
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocumento7 pagineNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNessuna valutazione finora
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocumento2 pagineAssessment Diagnosis Planning Intervention Rationale EvaluationJustine Mae A. LoriaNessuna valutazione finora
- NCP PotentialDocumento2 pagineNCP PotentialKathleenJoyGalAlmasinNessuna valutazione finora
- Dino File 2Documento6 pagineDino File 2Jhade Danes BalanlayNessuna valutazione finora
- Nursing ProcessDocumento13 pagineNursing ProcessRicha SharmaNessuna valutazione finora
- Nursing Care Plan: Lipa City CollegesDocumento13 pagineNursing Care Plan: Lipa City CollegesVincent Maralit MaterialNessuna valutazione finora
- Nursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocumento3 pagineNursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationCharlynne AraojoNessuna valutazione finora
- Pedia Clinical Enrichment NCPDocumento5 paginePedia Clinical Enrichment NCPIsabelle Hazel BenemileNessuna valutazione finora
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocumento8 pagineNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNessuna valutazione finora
- Subjective: IndependentDocumento2 pagineSubjective: IndependentRea LynNessuna valutazione finora
- DULNUANDocumento2 pagineDULNUANJB tindonganNessuna valutazione finora
- Nursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaDocumento5 pagineNursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaSofiaLopezNessuna valutazione finora
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocumento2 pagineNursing Care Plan: Cues Objectives Interventions Rationale EvaluationBianca Mikaela DosdosNessuna valutazione finora
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocumento7 pagineAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDanica Kate GalleonNessuna valutazione finora
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocumento2 pagineAssessment Diagnosis Planning Nursing Intervention Rationale Evaluationjennelyn losantaNessuna valutazione finora
- Activity Intolerance NCPDocumento3 pagineActivity Intolerance NCPGen RodriguezNessuna valutazione finora
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocumento2 pagineAssessment Diagnosis Planning Intervention Rationale EvaluationFaye Dianne Damian-BuenafeNessuna valutazione finora
- Nursing Care Plan (Pedia)Documento5 pagineNursing Care Plan (Pedia)JA BerzabalNessuna valutazione finora
- Time Chart: Data Action ResponseDocumento2 pagineTime Chart: Data Action ResponseAziil Liiza100% (2)
- NURSING CARE PLAN For TB 2003Documento6 pagineNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- NCP For LEC Act. 5Documento1 paginaNCP For LEC Act. 5Keneth Dave AglibutNessuna valutazione finora
- NCPDocumento2 pagineNCPKrizia TepootNessuna valutazione finora
- Materi Nursing Care PlanDocumento1 paginaMateri Nursing Care PlanSiti nur Kholifatus samsiyahNessuna valutazione finora
- Vi. Nursing Care PlanDocumento3 pagineVi. Nursing Care PlanJopaii TanakaNessuna valutazione finora
- NCP For CAP TB.Documento5 pagineNCP For CAP TB.Cherry Ann BalagotNessuna valutazione finora
- Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDocumento4 pagineAssessment Diagnosis Planning Intervention Rationale Evaluation Subjectivecammel ramos100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocumento8 pagineAssessment Diagnosis Planning Intervention Rationale Evaluationmhean azneitaNessuna valutazione finora
- NANDA Nursing Diagnosis: Ineffective Breathing Pattern Related To As Evidenced by NANDA DefinitionDocumento3 pagineNANDA Nursing Diagnosis: Ineffective Breathing Pattern Related To As Evidenced by NANDA DefinitionTrisha VergaraNessuna valutazione finora
- Nursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDocumento5 pagineNursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDimpal Choudhary100% (1)
- Valerie G. Vergara BSN-3-2Documento4 pagineValerie G. Vergara BSN-3-2Valerie VergaraNessuna valutazione finora
- NCPDocumento1 paginaNCPAnne Nicole ObispoNessuna valutazione finora
- Cez NCPDocumento6 pagineCez NCPaaronjosephsilvaNessuna valutazione finora
- NCP - Ineffective Airway ClearanceDocumento4 pagineNCP - Ineffective Airway ClearanceKen RegalaNessuna valutazione finora
- Assessment Planning Intervention Rationale EvaluationDocumento2 pagineAssessment Planning Intervention Rationale EvaluationIrish Jane GalloNessuna valutazione finora
- Assessment Nursing Diagnosis Planning Interventions EvaluationsDocumento2 pagineAssessment Nursing Diagnosis Planning Interventions EvaluationsAjay SupanNessuna valutazione finora
- NCP Ineffective Airway ClearanceDocumento2 pagineNCP Ineffective Airway ClearanceCharissa Magistrado De LeonNessuna valutazione finora
- The Art and Practice of Hypnotic Induction: Favorite Methods of Master Clinicians: Voices of Experience, #1Da EverandThe Art and Practice of Hypnotic Induction: Favorite Methods of Master Clinicians: Voices of Experience, #1Valutazione: 5 su 5 stelle5/5 (1)
- The Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessDa EverandThe Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessNessuna valutazione finora
- Date Added/EditedDocumento120 pagineDate Added/EditedJeenah HannahNessuna valutazione finora
- Handouts in NGCM103 Oxygenation Cardiovascular SystemDocumento7 pagineHandouts in NGCM103 Oxygenation Cardiovascular SystemJeenah HannahNessuna valutazione finora
- Letter-To-Brgy-Official FinalDocumento1 paginaLetter-To-Brgy-Official FinalJeenah HannahNessuna valutazione finora
- Handouts ALOCDocumento5 pagineHandouts ALOCJeenah HannahNessuna valutazione finora
- About The Diseases. Gallbladder & Biliary Tract DisordersDocumento10 pagineAbout The Diseases. Gallbladder & Biliary Tract DisordersJeenah HannahNessuna valutazione finora
- NMFR - Race MRF - Gender - Age - Trauma: Carpal Tunnel Syndrome PathophysiologyDocumento1 paginaNMFR - Race MRF - Gender - Age - Trauma: Carpal Tunnel Syndrome PathophysiologyJeenah HannahNessuna valutazione finora
- College of NursingDocumento9 pagineCollege of NursingJeenah HannahNessuna valutazione finora
- Mental and Emotional Health PowerpointDocumento36 pagineMental and Emotional Health PowerpointYen Aduana86% (7)
- PAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Documento28 paginePAT, CGMP For The 21st Century and ICH Q8, Q9, Q10Narendrakumar100% (2)
- Paramedical 1Documento156 pagineParamedical 1Iswarya MohanNessuna valutazione finora
- Special Consideration in Neonatal Resuscitation - 2022 - Seminars in PerinatologDocumento8 pagineSpecial Consideration in Neonatal Resuscitation - 2022 - Seminars in PerinatologEduardo Rios DuboisNessuna valutazione finora
- Tranexamic Acid MouthwashDocumento1 paginaTranexamic Acid MouthwashTalal MazharNessuna valutazione finora
- Tarea Nâ°1.es - en Derecho Civil Legalmente RubiaDocumento5 pagineTarea Nâ°1.es - en Derecho Civil Legalmente RubiaMax Alva SolisNessuna valutazione finora
- Slu Brochure Ay 2014-2015Documento2 pagineSlu Brochure Ay 2014-2015Michael BermudoNessuna valutazione finora
- Povidone-Iodine Solution MSDSDocumento3 paginePovidone-Iodine Solution MSDSBoksaRikoBondarNessuna valutazione finora
- Emergency Response Procedures Manual - PT. Saberindo Pacific - 2011Documento15 pagineEmergency Response Procedures Manual - PT. Saberindo Pacific - 2011Indah Rida Afriyanti100% (1)
- The Danger of Microwave TechnologyDocumento16 pagineThe Danger of Microwave Technologyrey_hadesNessuna valutazione finora
- Personal Finance Canadian 2nd Edition Madura Test BankDocumento48 paginePersonal Finance Canadian 2nd Edition Madura Test Bankannabellaauroravb5cf100% (22)
- Clinical Efficacy of Anodized Dental Implants For Implantsupported Prostheses After Different Loading Protocols - A Systematic Review and Meta-Analysis (2021)Documento20 pagineClinical Efficacy of Anodized Dental Implants For Implantsupported Prostheses After Different Loading Protocols - A Systematic Review and Meta-Analysis (2021)Andy LeeNessuna valutazione finora
- Summary of Non Sexist CityDocumento2 pagineSummary of Non Sexist CityIMY KARDAS100% (3)
- Hiradc Om - Talian AtasDocumento57 pagineHiradc Om - Talian AtasapnadiNessuna valutazione finora
- Prevention of Foodborne Disease: The Five Keys To Safer FoodDocumento2 paginePrevention of Foodborne Disease: The Five Keys To Safer FoodThong Boon LeongNessuna valutazione finora
- M5D BRT Ascending, Trav & RappelingDocumento83 pagineM5D BRT Ascending, Trav & RappelingFallucky Santiago100% (1)
- Sinif Ingilizce 8. Unite Calisma Kagidi Test Etkinlik Worksheet FITNESS by Murat DukkanciDocumento13 pagineSinif Ingilizce 8. Unite Calisma Kagidi Test Etkinlik Worksheet FITNESS by Murat DukkanciElif yurtsevenNessuna valutazione finora
- Fall Prevention: How Can Older Adults Prevent Falls?Documento4 pagineFall Prevention: How Can Older Adults Prevent Falls?Amalina ZahariNessuna valutazione finora
- Harga Obat Generik E-KatalogueDocumento4 pagineHarga Obat Generik E-KatalogueMuhammad FarilNessuna valutazione finora
- Resolving Therapeutic Alliance Ruptures: Diversity and IntegrationDocumento11 pagineResolving Therapeutic Alliance Ruptures: Diversity and IntegrationPablo GuerraNessuna valutazione finora
- New Trends in Mechanical VentilationDocumento4 pagineNew Trends in Mechanical Ventilationashley_castro_4Nessuna valutazione finora
- PayseptDocumento1 paginaPayseptJasmine SinglaNessuna valutazione finora
- Msds CatDocumento7 pagineMsds CatraniNessuna valutazione finora
- American Well - Case StudyDocumento13 pagineAmerican Well - Case StudySumitNessuna valutazione finora
- University of Cambridge International Examinations General Certificate of Education Ordinary LevelDocumento8 pagineUniversity of Cambridge International Examinations General Certificate of Education Ordinary LevelKelvin SerimweNessuna valutazione finora
- Uttarakhand Dealers Data, JanviDocumento8 pagineUttarakhand Dealers Data, JanviVAISHNAVI TAYALNessuna valutazione finora
- Reflection Essay - HRM533Documento9 pagineReflection Essay - HRM533Mazatul NadirahNessuna valutazione finora
- Safeminds Flu Vaccination 0809Documento2 pagineSafeminds Flu Vaccination 0809XR500FinalNessuna valutazione finora
- VtM2nded1 Page PDFDocumento1 paginaVtM2nded1 Page PDFJoseph CortesNessuna valutazione finora
- GOVERNMENT Leave - Form - Complete2Documento2 pagineGOVERNMENT Leave - Form - Complete2Marc CaurelNessuna valutazione finora