Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Prolapso Iris
Caricato da
Felippe CorreiaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Prolapso Iris
Caricato da
Felippe CorreiaCopyright:
Formati disponibili
DE LONG: Congenital Anterior- Staphyloma 315
63. Stahlin: Arch. f. Augenh., 1931, civ, p. 222.
64. Nettleship: Tr. Ophth. Soc. U. Kingdom, 1903, xxiii, p. 108.
65. von Hippel: Arch. f. Ophth., 1932, cxxviii, p. 23.
66. Thompson: Tr. Ophth. Soc. U. Kingdom, 1892, xii, p. 157.
67. von Hippel: Graefe-Saemisch Handbuch, 1921, Ed. 2, p. 323, cited by
Rehsteiner, Ref. 68.
68. Rehsteiner: Arch. f. Ophth., 1930, cxxv, p. 14.
CONGENITAL ANTERIOR STAPHYLOMA*
PERCE DE LONG, M.D.
Philadelphia
The extreme rarity of this condition, together with the
lack of definite knowledge as to its cause, makes an addi-
tional case worthy of. record. Congenital anterior staphy-
loma illustrates not only an ocular pathologic process, but
also certain obscure intra-uterine processes which may be
contributory factors. In this condition a child is born with
a lesion which resembles the end-result of a perforating
ulcer of the cornea in postnatal life. The cornea is opaque
and bulges forward between the eyelids. It is lined
posteriorly by uveal pigment, which, in the thinner parts,
shows through and gives a bluish tinge to the cornea.
Microscopically there is a striking similarity to a postnatal
anterior staphyloma. The epithelium is altered, and lies on
a changed stroma, the regular lamellae of which are replaced
by an irregular atrophic cellular tissue (cicatricial tissue).
Bowman's and Descemet's membranes are either entirely
absent or are present only in part. The iris is totally or
partially adherent to the posterior surface of the altered
cornea. The pigment layer may be preserved. The lens
may be in position, its remains may be adherent to the
cornea, or it ~nay be entirely absent. The ciliary body is
distorted and pulled forward. The vitreous, choroid, and
*
Candidate's thesis for membership accepted by the Committee on Theses.
316 DE LONG: Congenital Anterior Staphyloma
retina are not necessarily involved in any pathologic process.
The papilla may or may not be atrophied.
In 1827 F. A. von Ammon' reported the first clinical case,
which was quoted by Schoen.2 In this report there is no
detailed description of the conditions present. Treitel3 pub-
lished the first case with a pathologic study, but did not
report it in detail. Hirschberg and Birnbacher4 presented
the first extensive pathologic description. Up to the present
time I have been able to find but 15 cases that have been
reported with pathologic findings.
By some writers congenital anterior staphyloma has been
ascribed to an ulceration occurring in intra-uterine life;
others regard it as a lack of differentiation. G. Coats5 desig-
nates these conceptions as the "ulcerative hypothesis" and
the "malformation or non-differentiation hypothesis."
1. Ulcerative Hypothesis.-According to this theory, the
one most widely accepted, an infection must have gained
access to the fetal cornea. In a large number of diseases
transmission of an infection from mother to fetus has been
proved. In the majority of these cases the infection has
been endogenous; i. e., through the placental circulation.
In the eye, the occurrence of fetal keratitis, iritis, cyclitis,
and choroiditis of endogenous origin has been proved.
It is difficult to explain the method by which the infection
gains access to the cornea. Two pathways are possible:
(1) through the circulation (endogenous), and (2) through
the amniotic fluid (exogenous). Endogenous infections
might manifest themselves by a deep-seated keratitis of
sufficient severity to lead to a sloughing of the cornea, but
the main difficulty in the acceptance of this hypothesis, as
demonstrated by Leber and Schobl, is that, throughout fetal
life, the cornea, with the exception of the peripheral capillary
loop, is an avascular structure. Hence endogenous infection
through the blood stream is out of the question so far as
bacterial invasion is concerned.
DE LONG: Congenital Anterior Staphyloma 317
It is true that toxins may escape from the blood stream
and reach the non-vascular parts of the cornea. The absence
of blood vessels may determine a diminished resistance, and
then necrosis may set in. Or the infection may invade the
cornea from behind, and the bacilli or toxins may enter
through the anterior chamber, causing a perforation of the
fetal cornea. In the majority of cases reported there is no
evidence of posterior infection. It is, however, hardly
possible to conceive of a severe inflammatory process in the
anterior segment of an eye with no sign of inflammation in
the deeper lying structures.
Exogenous infections, which are the most probable, enter
through the vagina and infect the amniotic fluid. Bacteria
can pass from the vagina to the unimpregnated uterus, as
is shown by the occurrence of endometritis and salpingitis.
In the case of antepartum ophthalmia the organisms travel
upward and damage the fetal membranes and so gain access
to the liquor amnii. If the gonococcus can travel in this
manner, other micro-organisms can do likewise. It is true
that the spread of the infective agent will be more difficult
in the early stages of pregnancy, since the os is not patulous
and the cervical canal is filled with a plug of mucus; but
probably neither of these conditions offers an impassable
obstacle to the passage of organisms along the mucous
membrane. On the other hand, considering the frequency
of vaginal inflammation, if this manner of infection were at
all common, and if no other factors were necessary, con-
genital anterior staphyloma might be expected to occur
more frequently than it does.
In many histories it is stated definitely that no vaginal
discharge was present. Furthermore, it is difficult to con-
ceive that bacteria so virulent as to cause corneal ulceration
and secondary anterior staphyloma could spread upward
along a healthy mucous membrane without producing some
inflammation en route. It must be remarked, however, that
318 DE LONG: Congenital Anterior Staphyloma
pneumococci may lodge in the conjunctival sac and not
cause any inflammation until the epithelium is abraded.
Infection from the uterine mucous membrane would
require a lesion of that membrane, such as a localized endo-
metritis, which could arise from an exogenous source, e. g.,
from the vagina, or from an endogenous source, as the blood.
An extensive inflammatory process would not be necessary,
as a mere pyogenic organism entering the amniotic fluid
would be sufficient to contaminate the fluid. Any infection
of the placenta, either exogenous or endogenous, which
breaks through to the amniotic fluid would have the same
effect as an endometritis, and might cause an infection of
the fetal cornea.
An exogenous infection must enter the cornea through the
amniotic fluid, but the fetal eyelids, which normally are
closed from the third month until shortly after birth, would
not permit infection to take place. If there is a small defect
in the fusion of the fetal eyelids, an infection might enter;
or, as is occasionally the case, the amniotic fluid may possess
toxic properties, and it may be these toxins which enter
through the defect in the fusion of the eyelids and cause
ulceration of the cornea.
2. The Malformation or Non-Differentiation Hypothesis.
The principal basis of this theory is the lack of differentiation
in the embryonic cell layers. The mesoblast, from which
the iris and pupillary membranes are formed, is usually
separated from the cornea by the formation of a cleft-the
anterior chamber-but it must be remembered that the
anterior chamber is not a cleft between the cornea and the
iris, but between the cornea and the pupillary membrane,
and that the ingrowth of the iris is a later development.
The substantia propria of the cornea, Descemet's mem-
brane, the endothelium, and the anterior fibrovascular
sheath of the lens are the products of the "associated
paraxial mesoderm" (Mann),6 which grows in from the
DE LONG: Congenital Anterior Staphyloma 319
sides in front of the lens vesicle to separate it from the
surface epiblast. At an early stage this mesoblastic tissue
is composed of uniform cells, but it soon divides into two
parts: an anterior part, which quickly thickens and the
cells of which elongate, and a posterior portion, in which the
cells are round and arranged in two rows. The two parts
soon become separated by a membrane (Descemet's mem-
brane), which is probably the product of the reaction of the
cells on the posterior surface which later develop into the
endothelium. The portion of the mesoblast in front of the
membrane remains devoid of blood vessels and is transferred
into the laminated -fibrous tissue of the substantia propria
of the cornea.
Posterior to Descemet's membrane, among the round cells,
blood vessels gradually extend in from the anterior ciliary
arteries, and the round cells become the anterior fibro-
vascular sheath of the lens, the "anterior or pupillary portion
of the 'tunica vascularis lentis' " (Mann6).
The anterior fibrovascular sheath plays an important role
in the development of the iris, for the anterior layers of the
iris are mainly produced from it. Beneath it the two layers
of the second optic vesicle, "neural ectoderm" (Mann6),
become the posterior pigment-epithelial layers of the iris,
which extend inward. The muscle tissue of the iris is also
developed from the ectoderm. Therefore if any one of these
processes fail, we would have one of several malformations:
the mesoblast would remain adherent and neither the iris
nor the cornea would develop normally. Drainage would
be interfered with, the intra-ocular tension would rise, and
the fused iris and pseudocornea would bulge out from be-
tween the eyelids, producing a congenital anterior staphy-
loma.
Ophthalmia neonatorum can hardly be considered as a
cause. It is true that ophthalmia may be present at birth,
and one may assume that the infection took place in utero,
320 DE LONG: Congenital Anterior Staphyloma
due to a premature rupture of the fetal membrane. The
formation of a staphyloma requires time, and it is doubtful
whether in ophthalmia there would be sufficient time
between the period of rupture of the membrane and the
birth of the child for a staphyloma to develop.
From a study of clinical histories, however, it is quite
certain that if the gonococcus has played any part in the
causation of congenital anterior staphyloma, it has done
so only in exceptional cases. Coats states that "the gono-
coccus is not the only cause of corneal ulceration apart
from ophthalmia neonatorum, and it is not even a common
cause." Exceptions may be found in Egypt. The pneumo-
coccus is a far more frequent cause, and the pseudocornea
of congenital anterior staphyloma presents the same patho-
logic picture as the postnatal staphyloma.
In some of the reported cases the familial incidence,
supporting the non-differentiation hypothesis, is quite strik-
ing. The condition, however, has not been encountered in
members of more than one generation.
Crompton7 and Kruckow8 each report the cases of two
brothers with congenital anterior staphyloma. The most
remarkable incident is Steinheim's9 case, in which the chil-
dren were as follows: (1) A boy, aged six years, in whom
both eyes were staphylomatous; (2) a girl, aged five years,
whose eyes were normal; (3) a girl, aged four years, with
right eye total staphyloma, left eye small, with cystic
ectasia; (4) a girl, aged three years, with total staphyloma
in both eyes; (5) a boy, aged two months, in whom both
eyes were white and shrunken.
Instances of the transmission of an acquired disease, as,
for example, syphilis, in successive conceptions are not
wanting. In a familial incidence of congenital anterior
staphyloma, however, transmission is not implied except. in
the restricted sense of an infection (as syphilis) by the
mother. Hereditary transmission of a true malformation is
DE LONG: Congenital Anterior Staphyloma 321
quite common and admitted, but there is no evidence in any
of the cases reported of the transmission of a congenital
anterior staphyloma from one generation to another.
The case which I had the opportunity of examining was
seen at the Wills Hospital, in the service of Dr. Thomas
O'Brien. The clinical diagnosis was corneal staphyloma
from intra-uterine infection.
R. S., a Polish, white, male infant, aged eleven days.
History. -At birth it was noticed that the left cornea was opaque
and protruded through the palpebral fissure. The child was unable
to close the eyelids. The patient was the thirteenth child. Two
children died in infancy; ten were living and normal; no ocular
defects or diseases being present. The parents knew of no ocular
defects or disease in their respective families, and they also denied
any venereal infection. The Wassermann tests for both mother
and child were negative. The mother claimed that no vaginal
discharge was present.
Right Eye: The lids and lacrimal sac were normal. The con-
junctiva was normal. The cornea showed a small nebula at 12
o'clock. The anterior chamber was somewhat shallow. The iris
was blue-gray in color. The pupil was small and oval, measuring
from 1.5 to 2 mm. in diameter, and reacted to light. There was a
posterior synechia at 12 o'clock. Through the small pupil the disc
was found to be slightly oval, with a small physiologic cup. The
margins were well defined. The retinal vessels appeared to be
healthy, as did the macula. No lesions of the choroid or retina
were present.
Left Eye: The lids and lacrimal sac were normal. There was
no defect or malformation of the lids, which were separated by the
protruding globe. On the anterior surface of the cornea there was
some granulation tissue with scattered islands of epithelium. This
area stained faintly, and was the probable site of the perforation.
On raising the lid it was seen that the other portions of the cornea
were opaque. The sclera was bluish-white. Transillumination
showed anteriorly a homogeneous, translucent globe. No pig-
mentation was noted in the cornea. Digital palpation of the globe
disclosed the fact that tension was well within the normal range.
The patient was seen by Drs. Zentmayer, Pontius, and Griscom.
11
322 DE LONG: Congenital Anterior Staphyloma
The consensus of opinion was that the eye should be enucleated.
This was done, and no postoperative complications developed.
Pathologic Findings.-The globe measured 34 mm. antero-
posteriorly, 19 mm. transversely, and 20 mm. vertically. The
posterior pole at the entrance of the optic nerve presented a bulging
mass which measured 4 mm. anteroposteriorly and 7 mm. trans-
versely.
Macroscopic Findings.-The eyeball, when sectioned, revealed
an absence of the anterior chamber. The vitreous cavity occupied
the entire globe and was partially filled with a fibrinous coagulum.
The retina was in position. There was a deep cupping of the nerve
head. There was an ectasia of the sclera anteriorly.
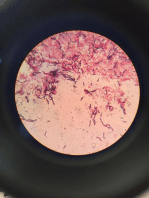
Microscopic Findings.-The corneal epithelium was markedly
thickened, showing down-growths forming true papillae; in certain
areas it was typically epidermoid. Bowman's membrane was ab-
sent. The pathologic change was the result of a chronic irritative
process.
The irregularly arranged epithelial cells lay on the stroma, which
was much altered and thin, and was composed of irregular cellular
tissue (cicatricial tissue), with many blood vessels coursing in all
directions. This presence of blood vessels in the altered corneal
stroma is an indication that a previous inflammation or a suppura-
tive ulcerative process had been present. Descemet's membrane
was absent, and nowhere was there any trace of endothelial cells,
again indicating that the process must have been an early one,
affecting the anterior fibrovascular layer before Descemet's mem-
brane and the endothelial cells had developed.
The posterior surface of the pseudocornea was lined by a glass
membrane which was difficult to recognize over the whole surface,
but it could be identified as the lens capsule-, which normally is
extremely resistant to any pathologic process. Just adjacent to
the lens capsule, and behind it, were the uniform and easily recog-
nized epithelial cells of the lens. These cells, together with some
degenerated lens material, which in certain areas revealed some
hyaline degeneration, formed the posterior border of the staphy-
lomatous cornea. This adherence of the degenerated lens to the
posterior border of the pseudocornea, together with the absence
of the formation of the fetal cleft, is support for the non-differen-
tiation hypothesis, as stated in Peters' article. This observer re-
garded congenital anterior staphyloma as clearly a deformity
which develoyed as the result of the lens remaining too long on
the posterior surface of the cornea.
-b
~~~~~~~~~~~~~~~~~~~~~~~~~~
Section of the whole globe showing-a, The epithelium is typically epider-
anterior staphyloma. Note the absence of moid, with true papillae. The very
both the anterior and posterior chamber. superficial cells are devoid of nuclei or
b, thin-walled ectasia adjacent to the nasal corneous. Note the blood vessels in
side of the ciliary body. c, coloboma of the the cicatrized cornea.
nerve entrance.
by c
d
Note the fibrous stump and Pseudocornea showing-a,
the mass of pigmented epi- many blood vessels; b, lens cap-
thelial cells, the only remain- sule; c, lens epithelium; d,
ing evidence of the ciliary degenerated lens showing some
body and processes, with hyaline changes.
degenerated lens substance
lying adjacent anteriorly.
DE LONG: Congenital Anterior Staphyloma 323
There was no evidence of any iris stroma or pigment in the
pseudocornea, indicating that the process must have been an
active one before these layers had differentiated from the anterior
fibrovascular sheath. If pigment had been present in the posterior
layers of the pseudocornea, it could have been accounted for by
some irregularity in the distribution of the deeper layers of the iris,
which had not separated. If pigment had been present in the an-
terior layers of the pseudocornea, it could have been accounted
for only by a perforation with iris prolapse. In this case there was
no evidence of any pigmentation in any portion of the pseudo-
cornea. This condition supports Meller's hypothesis. This inves-
tigator expressed the opinion that congenital anterior staphyloma
is the result of a primary malformation of the iris causing hydroph-
thalmus.
There was no evidence of Schlemm's canal, nor of any of the
other structures of the filtration angle. The zonular fibers were
also absent. The ciliary body appeared as a small nodule of fibrous
tissue. There were no ciliary processes, and the only other evidence
of this structure was a small group of flattened pigment-epithelial
cells, which appeared to be drawn forward.
The choroid showed signs of a previous chronic inflammation,
manifested by the formation of connective tissue, which had taken
the place of the stroma and was present to a greater degree in the
capillary layer. Here there was a striking absence of the capillaries,
whereas in the posterior layer the larger vessels were still present
and distended, showing that the tension must have been low, as
in increased tension small and collapsed vessels are found.
In the usual course of pathologic events organization of granula-
tion tissue in the choroid causes the destruction of the normal
blood vessels, a process which occurs partly as the result of oblitera-
tive endovascular changes, but chiefly from the constrictive effects
of contracting fibrous tissue. Chronic inflammatory processes lead
to cicatrization. The former was evident in this case. The cho-
roidal pigment had not as yet developed.
The retina showed evidence of chronic inflammation and the
usual secondary degeneration. There was no longer any evidence
of edema or of round-cell infiltration. In certain areas the struc-
ture was disorganized, whereas in others it showed fairly normal
relations. No ganglion cells were seen, and the rods and cones
were broken down to a granular debris. The nerve-fiber layer was
markedly thickened and was partially replaced by fibrous tissue;
324 DELONG: Congenital Anterior Staphyloma
the surface of the retina also showed an organizing exudate that was
most marked about the disc, which too was organized into fibrous
tissue. The optic nerve was deeply cupped and definitely revealed
the formation of a true congenital coloboma.
Four years after enucleation the child, a moron, was again ex-
amined. The ophthalmologic findings were as follows: In the
right eye vision was unquestionably reduced. There was an ele-
vated corneal nebula at the limbus at 12 o'clock, with minute
vessels entering it from the sclera, but the cornea was clear. The
anterior chamber was of normal depth. The pupil was vertically
oval, and at 12 o'clock, below the level of the corneal nebula, there
was a posterior synechia. Otherwise the iris appeared to be healthy.
The lens was clear, as. was also the vitreous. The retinal vessels
were normal, as were also the choroid, retina, and macula. The
optic nerve was small and vertically oval. A central light spot,
absence of cupping, and slight haziness of the disc margins were
noted.
Dr. Alfred Cowan's slit-lamp findings were as follows:
"At the upper part of the cornea near the limbus there is a
dense, white, elevated opacity, which contains a few superficial
vessels. The rest of the cornea is normal and there are no precipi-
tates on the posterior surface. The aqueous is clear. At 12 o'clock
at the pupillary border there is a broad posterior synechia which
spreads out slightly on the surface of the lens. The rest of the iris
is intact. The lens shows no abnormalities."
The few cases of congenital anterior staphyloma that
have been placed on record have aroused much contro-
versy. In reviewing the literature, particularly the German
literature from 1899 to 1916, it is apparent that much evi-
dence has been presented as to the probable cause of the
condition. The following are abstracts from some of the
leading articles on the subject:
E. von Hippel,'0 in 1899, asserted that disease of the
posterior surface of the cornea tends to produce a predisposi-
tion to the development of anterior staphyloma. For in-
stance, a purulent infection of the cornea, with thick infil-
tration, may be the immediate cause of a staphyloma. In
190611 he published a second article in which he disagreed
DE LONG: Congenital Anterior Staphyloma 325
with Peters' theory of a failure in lens segmentation and held
to his original theory of an endogenous development from
a purulent ulcer, depending upon two possibilities: dis-
turbance in development in the beginning of the second
month and a disease process in the later months. The second
of these was deemed the more probable. Seefelder and
Wolfram"2 agreed with von Hippel's theory.
In 1927 E. von Hippel'3 presented two cases and attributed
the condition to a developmental disturbance. In this
article he also stated that the pathologic findings were
opposed to this hypothesis, and that he could not arrive at
any definite conclusion as to the cause of the congenital
anterior staphyloma. He also stated that Peters' hypothesis
of failure of lens segmentation as a cause was not convincing.
The following is a quotation from von Hippel's paper, in
which he summarized the various theories and opinions held:
"1. Endogenous disease, of unknown type, of the posterior
corneal wall, originating in late fetal life. (E. von Hippel.)
"2. Primary lack of formation of the central posterior
corneal sheath developing in earliest fetal life and caused by
disturbance in the segmentation of the lens (Peters) or
through primary lack of development of the endothelium.
(Seefelder, 1911.)
"3. Primary malformation of the iris causing rise in
pressure, which in turn causes stretching of the cornea,
followed by defect in Descemet's membrane through rup-
ture, the opacity in the center of the cornea protruding as
a result. (Meller.)
"4. Central parenchymatous luetic keratitis with secon-
dary necrosis in the deep corneal sheath, Descemet's mem-
brane, and endothelium. (Fuchs.)"
Parsons'4 considered congenital anterior staphyloma to be
of an inflammatory origin. Marchesani'5 regarded it as an
inflammatory development. Treacher Collins'6 agreed with
Parsons, but believed that non-differentiation played a part.
326 DE LONG: Congenital Anterior Staphyloma
Mohr"7 presented a theory that the condition was an inflam-
matory one, localizing itself in the non-differentiated cells.
Coats5 was also of the opinion that congenital anterior
staphyloma was an inflammatory development. He stated:
"If the ulcerative process be granted, it is undeniable that
the structural details actually found in the specimen are in
the main explained. The malformation hypothesis, on the
contrary, encounters the more serious difficulty that the
details of structure do not easily fall into line with the
explanation. In the first case the difficulties are negative,
in the second, positive."
Fuchs18 described congenital anterior staphyloma as a
parenchymatous luetic keratitis with necrosis of the deep
corneal layer and Descemet's membrane. This theory was
later combatted, since there was no symptom of lues in any
of the cases reported.
Pagenstecher"9 suggested that these anomalies might de-
velop through toxic influences.
Meller"0 expressed the opinion that the condition arose
from primary malformation of the iris causing hydroph-
thalmus and staphyloma.
Peters2' (1906) believed that congenital anterior staphy-
loma was clearly a deformity developing as the result of the
lens remaining too long on the posterior surface of the cornea.
In his second work he relinquished his former hypothesis,
but still held to the theory of developmental disturbance.
Nieder,22 Meller,20 Schlafke,23 Wirths,24 and Schomann25
agreed with Peters that the condition was purely develop-
mental.
In 1912 Peters26 presented a new theory. He regards
congenital anterior staphyloma as an abnormal differentia-
tion of the epithelium and corneal sheath, causing a dis-
turbance in the segmentation of the lens. In support of his
theory he gives the following five factors:
"1. Complete lack of inflammatory phenomena in his
cases, as well as in those of Reis and Meller.
DE LONG: Congenital Anterior Staphyloma 327
"2. The combination of congenital corneal opacities with
other forms of malformation of the eye and of the body.
"3. The pronounced hereditary nature of the condition.
"4. The symmetry of the defect.
"5. Complete lack of other eye or bodily disease of the
child or mother, so far as could be ascertained."
From the abstracts and hypotheses cited above it is
apparent that the cause of congenital anterior staphyloma
is still in question.
CONCLUSION
It is my opinion that congenital anterior staphyloma, like
the postnatal form, is due to an ulcer perforating the cornea
from without, which may develop just as easily before as
after birth.
In the case presented there is no doubt but that there had
been a chronic inflammation, since we have the evidence of
a chronic process manifested by characteristic changes both
in the epithelium and in the substantia propria. Bowman's
membrane was absent, indicating that the beginning of the
process must have antedated the formation of this mem-
brane. Descemet's membrane and the endothelial cells had
not as yet developed, since there was no evidence of any
separation of the fetal cleft. The posterior portion of the
pseudocornea was composed of cicatricial tissue with many
blood vessels, and there was no sign of pigmentation. Al-
though the ciliary body appeared as a fibrous stump, it is
proper to assume that the inflammatory process was present
in the anterior fibrovascular layer before specialization had
taken place in this group of cells, and therefore before the
development of the iris and the formation of the fetal cleft.
The lens capsule and lens epithelium, with some degenerated
lens substance, formed the posterior border of the pseudo-
cornea. All these findings point to an early perforation, but
in the cases recorded it is certain that perforations do not
occur at a corresponding period in all instances.
328 DE LONG: Congenital Anterior Staphyloma
The choroid showed evidences of a chronic inflammation,
as did also the retina to a minor degree. The optic nerve
showed a deep cupping, which might have been due to
increased tension, but the pathologic picture has all the
aspects of a congenital coloboma of the optic nerve.
Coats states that there are "no cases on record of con-
genital anterior staphyloma being associated with what may
be called a pure malformation in other parts of the eye."
Clinically, we have the sequela of an inflammatory process
in the form of a leukoma of the cornea in the right eye. This,
together with the posterior synechia and an organized exu-
date on the lens surface in an otherwise healthy eye, supports
the hypothesis that there had been an infection of the cornea
and iris. Personally, I believe that the infection or toxin
localized itself in a group of non-differentiated cells which
were undergoing developmental changes, and the final
pathologic findings give evidence of an inflammation that
prevented normal development of the cornea.
REFERENCES
1. von Ammon: Froriep's Notizen No. 407, December, 1827 (quoted by
Schoen).
2. Schoen: Handbuch d. path. Anat. d. menschlich. Aug., 1828, p. 68.
3. Treitel: Arch. f. Ophth 1876 xxi, p. 3.
4. Hirschberg and Birnbacier: dentralbi. f. prakt. Augenh., 1886, x, p. 225.
5. Coats: Ophthalmoscope, 1910, viii, p. 248.
6. Mann: The Development of the Human Eye, 1928.
7. Crompton: London Medical Gazette, 1840, p. 432.
8. Kruckow: Arch. f. Ophth., 1875, xxi, pt. 2, p. 213.
9. Steinheim: Centralbl. f. prakt. Auge 1897, xxi, p. 353.
10. von Hippel: Arch. f. Ophth., 1918, xcv.
11. von Hippel: Klin. Monatsbl. f. Augenh., 1906, i.
12. Seefelder and Wolfram: Graefe's Arch. f. Ophth., 1907, lxv, pt. 2, p. 320.
13. von Hippel: Ophth. Gesellsch., Heidelberg, 1927, p. 129.
14. Parsons: Lancet, 1904, i, p. 579.
15. Marchesani: Arch. f. Augenh., 1930, ciii, p. 632.
16. Collins: Tr. Ophth. Soc. U. Kingdom, 1909, xxix, p. 169.
17. Mohr: Klin. Monatsbl. f. Au,eh., 1910, xlviii, p. 338.
18. Fuchs: Graefe's Arch. f. Ophth., ii, 1916, No. 92.
Me¶ler: Graefe'sMonographia,
19. Pagenstecher: 1912, Verlag S. Hitzel, Leipzig.
20. Arch. f. Ophth., 1909, iii, No. 72, p. 483.
21. Peters: Kiln. Monatsbl. f. Augenh., 1906, i, p. 27.
22. Nieder: Dissertation, Rostock, 1909.
23. Schlafke: Disertation, Rostock, 1913.
24. Wirths: Beitr. z. Augenh. 1913, p.521
25. Schomann: Dissertation, istock, 1914.
26. Peters: Centralbl. f. prakt. Augenh., 1912, p. 330.
Potrebbero piacerti anche
- Resume Ulkus CorneaDocumento10 pagineResume Ulkus CorneaNita RosianiNessuna valutazione finora
- Treatise on the Anatomy and Physiology of the Mucous Membranes: With Illustrative Pathological ObservationsDa EverandTreatise on the Anatomy and Physiology of the Mucous Membranes: With Illustrative Pathological ObservationsNessuna valutazione finora
- Bscess AND Hlegmon: Tlas OF EAD AND ECK Athology Bscess AND LegmonDocumento4 pagineBscess AND Hlegmon: Tlas OF EAD AND ECK Athology Bscess AND LegmonDanis Diba Sabatillah YaminNessuna valutazione finora
- Branchial Cleft CystsDocumento8 pagineBranchial Cleft CystsHere LeafsNessuna valutazione finora
- Chronic Adhesive Otitis Media 1956Documento10 pagineChronic Adhesive Otitis Media 1956Teuku Ahmad HasanyNessuna valutazione finora
- Excision of Branchial Cleft CystsDocumento10 pagineExcision of Branchial Cleft Cystssjs315Nessuna valutazione finora
- Infected Preauricular SinusDocumento9 pagineInfected Preauricular SinussyafiqNessuna valutazione finora
- 2000 Ocular PathDocumento26 pagine2000 Ocular Pathdeta hamidaNessuna valutazione finora
- SEMINAR On Eyelid Echi 3rd YearDocumento93 pagineSEMINAR On Eyelid Echi 3rd Yearsushmitabiswas052Nessuna valutazione finora
- Cholesteatoma Congenital, PediatricDocumento6 pagineCholesteatoma Congenital, PediatricMeilina Elin WardhaniNessuna valutazione finora
- Background: View Media GalleryDocumento8 pagineBackground: View Media GalleryAza Patullah ZaiNessuna valutazione finora
- Mosca 2008Documento5 pagineMosca 2008Militanisa ZamzaraNessuna valutazione finora
- Midline Nasal Dermoids - Best - With FiguresDocumento6 pagineMidline Nasal Dermoids - Best - With FiguresVinay JacobNessuna valutazione finora
- A New Theory On The Pathogenesis of Acquired CholesteatomaDocumento14 pagineA New Theory On The Pathogenesis of Acquired CholesteatomaReynaVG19Nessuna valutazione finora
- Major Review: Ocular ColobomataDocumento20 pagineMajor Review: Ocular ColobomataPriyankaNessuna valutazione finora
- Abses Preaurikula Final 1Documento9 pagineAbses Preaurikula Final 1syafiqNessuna valutazione finora
- AOP Krásný ENDocumento9 pagineAOP Krásný ENDavid MartínezNessuna valutazione finora
- Oral Cysticercosis: Case Report and Review of The LiteratureDocumento4 pagineOral Cysticercosis: Case Report and Review of The LiteraturePeiterGozaliNessuna valutazione finora
- 14 Review ArticleDocumento3 pagine14 Review ArticleShriya ShahuNessuna valutazione finora
- Hematometrocolpos 1. DefinisiDocumento5 pagineHematometrocolpos 1. DefinisiMelanieNessuna valutazione finora
- MainDocumento11 pagineMainMuhammad Nur Ardhi LahabuNessuna valutazione finora
- Eye Pathology: Dr. Jusuf FantoniDocumento8 pagineEye Pathology: Dr. Jusuf Fantonitutor tujuhNessuna valutazione finora
- Neuroscience - The Brain and Spiral CordDocumento4 pagineNeuroscience - The Brain and Spiral CordAnn MutisyaNessuna valutazione finora
- The Vermiform Appendix: AnatomyDocumento10 pagineThe Vermiform Appendix: AnatomyBereket temesgenNessuna valutazione finora
- Merlo Panoramic p20 6sc Drive Train Hydraulic Electrical Manual enDocumento22 pagineMerlo Panoramic p20 6sc Drive Train Hydraulic Electrical Manual enkidixarov100% (39)
- Cysts of The Oral CavityDocumento11 pagineCysts of The Oral CavityGhada YaakoubNessuna valutazione finora
- MedscapeDocumento12 pagineMedscapeRissa WatlolyNessuna valutazione finora
- Wo MSKK Week 5Documento7 pagineWo MSKK Week 5GabrielaNessuna valutazione finora
- 7.5 Minor Surgical Conditions of ChildhoodDocumento13 pagine7.5 Minor Surgical Conditions of ChildhoodΜατθαίος ΠαππάςNessuna valutazione finora
- Cisitcercosis: enfermedad parasitariaDa EverandCisitcercosis: enfermedad parasitariaNessuna valutazione finora
- Branchial Cleft Cyst: A Case Report and Review of LiteratureDocumento3 pagineBranchial Cleft Cyst: A Case Report and Review of LiteratureValonia IreneNessuna valutazione finora
- CholesteatomaDocumento9 pagineCholesteatomamakintosh88Nessuna valutazione finora
- Kongenitalne Ciste I Fistule VrataDocumento2 pagineKongenitalne Ciste I Fistule VrataRoppeNessuna valutazione finora
- Grand Rounds Index UTMB Otolaryngology Home PageDocumento6 pagineGrand Rounds Index UTMB Otolaryngology Home PageWiwie Dwi FitriNessuna valutazione finora
- Skin StructDocumento11 pagineSkin StructWidya AstriyaniNessuna valutazione finora
- Branchial Cleft CystDocumento6 pagineBranchial Cleft CystIvana SupitNessuna valutazione finora
- Complications in UveitisDa EverandComplications in UveitisFrancesco PichiNessuna valutazione finora
- Nasolabial CystDocumento7 pagineNasolabial CystathaNessuna valutazione finora
- Friedberg 1940Documento14 pagineFriedberg 1940YPramudiyaNessuna valutazione finora
- Huge Pathology FileDocumento143 pagineHuge Pathology FilePaul GoodyearNessuna valutazione finora
- GPEmpyemaClinicalCommentaryDixon Et Al-2016-Equine Veterinary EducationDocumento6 pagineGPEmpyemaClinicalCommentaryDixon Et Al-2016-Equine Veterinary EducationRojelio SousaNessuna valutazione finora
- Abnormal ImplantationDocumento3 pagineAbnormal ImplantationMuhammet Fatih CantepeNessuna valutazione finora
- Chapter 20: Branchial Cleft Anomalies, Thyroglossal Cysts and Fistulae P. D. M. EllisDocumento9 pagineChapter 20: Branchial Cleft Anomalies, Thyroglossal Cysts and Fistulae P. D. M. EllisDrsreeram ValluriNessuna valutazione finora
- D. Amal Entamoeba Coli-1 (Muhadharaty)Documento10 pagineD. Amal Entamoeba Coli-1 (Muhadharaty)محمد عبدالوهاب ابراهيم الطباطبائيNessuna valutazione finora
- Oral Pathology: Non-Epithelialized Primary Bone CystDocumento4 pagineOral Pathology: Non-Epithelialized Primary Bone Cystعلي صادق جعفرNessuna valutazione finora
- Venkatraman K PDFDocumento3 pagineVenkatraman K PDFRana Zara AthayaNessuna valutazione finora
- Conjuctiva 1Documento47 pagineConjuctiva 1maleeha shahzadNessuna valutazione finora
- Pterigium PDFDocumento152 paginePterigium PDFArizkamhNessuna valutazione finora
- Ho Song Pak Cutaneous Bronchogenic Cyst Over The SternumDocumento4 pagineHo Song Pak Cutaneous Bronchogenic Cyst Over The SternumDr AmalNessuna valutazione finora
- Diseases of The ConjunctivaDocumento18 pagineDiseases of The Conjunctivadykesu1806Nessuna valutazione finora
- Group 8 Parasitic CystsDocumento47 pagineGroup 8 Parasitic CystsMariam Abd ElhadiNessuna valutazione finora
- Incidental Reportzaharopoulos2000Documento4 pagineIncidental Reportzaharopoulos2000maglangitmarvincNessuna valutazione finora
- Case Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureDocumento6 pagineCase Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureIrsalinaHusnaAzwirNessuna valutazione finora
- Occur Largely in The Newborn and in Children Younger Than 5 Years, and Rarely in Older IndividualsDocumento6 pagineOccur Largely in The Newborn and in Children Younger Than 5 Years, and Rarely in Older IndividualsElle ReyesNessuna valutazione finora
- Congenital Malformations of Nose and SinusesDocumento24 pagineCongenital Malformations of Nose and SinusesDr. T. BalasubramanianNessuna valutazione finora
- Bacte Reviewer MidtermDocumento30 pagineBacte Reviewer MidtermShiella Mae SalamanesNessuna valutazione finora
- Pink Pigtail in A Skin Biopsy: ScabiesDocumento12 paginePink Pigtail in A Skin Biopsy: ScabiesDeba P SarmaNessuna valutazione finora
- Eye Problem 1Documento11 pagineEye Problem 1Josette Mae AtanacioNessuna valutazione finora
- Mazzotta 2020Documento6 pagineMazzotta 2020StefanieNessuna valutazione finora
- Sense OrgansDocumento8 pagineSense OrgansKeelah BennNessuna valutazione finora
- Correspondence: The Fishmouth Phenomenon in Retinal DetachmentDocumento1 paginaCorrespondence: The Fishmouth Phenomenon in Retinal DetachmentSushi HtetNessuna valutazione finora
- Ophthalmology - Diseases of CorneaDocumento18 pagineOphthalmology - Diseases of CorneajbtcmdtjjvNessuna valutazione finora
- Refleksi Kasus BKMM-Benda Asing Di KonjungtivaDocumento11 pagineRefleksi Kasus BKMM-Benda Asing Di KonjungtivaAnnisa Westania DanialNessuna valutazione finora
- 7 Key Indicators That You'Re An Ideal Candidate For LASIK Vision CorrectionDocumento8 pagine7 Key Indicators That You'Re An Ideal Candidate For LASIK Vision Correctionsmartvisioneyehospitals12Nessuna valutazione finora
- Laporan Kasus SACG Dan Katarak Kongenital Pada AniridiaDocumento15 pagineLaporan Kasus SACG Dan Katarak Kongenital Pada AniridiaIntan EkarulitaNessuna valutazione finora
- Amblyopia - Diagnosis and Treatment: Pamela J. Kutschke, BS, CoDocumento6 pagineAmblyopia - Diagnosis and Treatment: Pamela J. Kutschke, BS, CoKhushbu DedhiaNessuna valutazione finora
- OphthalDocumento10 pagineOphthaldrjanggeum0% (1)
- LASIK Eye Surgery - Media DiscourseDocumento4 pagineLASIK Eye Surgery - Media DiscourseSafitri KhoirunnisaNessuna valutazione finora
- SquintDocumento7 pagineSquintMohamed GhanemNessuna valutazione finora
- ZEISS I.profilerDocumento1 paginaZEISS I.profilerHéctor RamírezNessuna valutazione finora
- Diagnosis MataDocumento168 pagineDiagnosis Mata19. Moh Hidayatullah AL AhyaNessuna valutazione finora
- December 2018 Ophthalmic PearlsDocumento2 pagineDecember 2018 Ophthalmic PearlsFathirNessuna valutazione finora
- CorneaDocumento18 pagineCorneaDrNarayan KRNessuna valutazione finora
- Pentacam: Instruction ManualDocumento67 paginePentacam: Instruction ManualWang JYNessuna valutazione finora
- Glaucoma ImplantsDocumento8 pagineGlaucoma Implantsarindamjha7041Nessuna valutazione finora
- Bionic EyeDocumento20 pagineBionic EyeMegha BhatiaNessuna valutazione finora
- Delhi Govt Panel Hospital ListDocumento12 pagineDelhi Govt Panel Hospital ListjjagdishhNessuna valutazione finora
- CataractDocumento45 pagineCataractAmit Martin100% (2)
- Slit LampDocumento23 pagineSlit LampShubhangi ShuklaNessuna valutazione finora
- Red Reflex Test: ProcedureDocumento6 pagineRed Reflex Test: ProcedureFitri Amelia RizkiNessuna valutazione finora
- Management of Pterygium: DR Vidyashankar G K Shekar Nethralaya BangaloreDocumento18 pagineManagement of Pterygium: DR Vidyashankar G K Shekar Nethralaya BangaloreelisgretyNessuna valutazione finora
- Glaucoma Drainage DevicesDocumento171 pagineGlaucoma Drainage DevicesCarlos Hernan Castañeda RuizNessuna valutazione finora
- Tonometry and Care of Tonometers: Journal of Current Glaucoma Practice September 2012Documento8 pagineTonometry and Care of Tonometers: Journal of Current Glaucoma Practice September 2012Mukhlisa RahmanNessuna valutazione finora
- International Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)Documento4 pagineInternational Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)zaidoonys1Nessuna valutazione finora
- Clinical Profile of Ptosis in A Tertiary Care CentreDocumento5 pagineClinical Profile of Ptosis in A Tertiary Care CentreInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Rle or Cases FormatDocumento4 pagineRle or Cases FormatArlyn MarcelinoNessuna valutazione finora
- Dynamic RetinosDocumento6 pagineDynamic RetinosguybarnettNessuna valutazione finora