Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Early Liver Transplantation
Caricato da
CunCunAlAndraCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Early Liver Transplantation
Caricato da
CunCunAlAndraCopyright:
Formati disponibili
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Early Liver Transplantation
for Severe Alcoholic Hepatitis
Philippe Mathurin, M.D., Ph.D., Christophe Moreno, M.D., Ph.D.,
Didier Samuel, M.D., Ph.D., Jérôme Dumortier, M.D., Ph.D., Julia Salleron, M.S.,
François Durand, M.D., Ph.D., Hélène Castel, M.D., Alain Duhamel, M.D., Ph.D.,
Georges-Philippe Pageaux, M.D., Ph.D., Vincent Leroy, M.D., Ph.D.,
Sébastien Dharancy, M.D., Ph.D., Alexandre Louvet, M.D., Ph.D.,
Emmanuel Boleslawski, M.D., Ph.D., Valerio Lucidi, M.D., Thierry Gustot, M.D., Ph.D.,
Claire Francoz, M.D., Christian Letoublon, M.D., Denis Castaing, M.D.,
Jacques Belghiti, M.D., Vincent Donckier, M.D., Ph.D.,
François-René Pruvot, M.D., and Jean-Charles Duclos-Vallée, M.D., Ph.D.
A BS T R AC T
Background
From Hôpital Claude Huriez, Services Ma- A 6-month abstinence from alcohol is usually required before patients with severe
ladies de l’Appareil Digestif and INSERM alcoholic hepatitis are considered for liver transplantation. Patients whose hepatitis
Unité 995 (P.M., H.C., S.D., A.L.), Services
de Chirurgie Digestive et de Transplanta- is not responding to medical therapy have a 6-month survival rate of approximately
tion (E.B., F.-R.P.), and the Department 30%. Since most alcoholic hepatitis deaths occur within 2 months, early liver trans-
of Biostatistics and INSERM EA2694 plantation is attractive but controversial.
(J.S., A.D.), Centre Hospitalier Universi-
taire (CHU) de Lille and Université Nord
de France, Lille; Assistance Publique– Methods
Hôpitaux de Paris Hôpital Paul Brousse, We selected patients from seven centers for early liver transplantation. The patients
Centre Hépato-Biliaire and INSERM Uni- had no prior episodes of alcoholic hepatitis and had scores of 0.45 or higher accord-
té 785, Université Paris-Sud — both in
Villejuif (D.S., D.C., J.-C.D.-V.); Hôpital ing to the Lille model (which calculates scores ranging from 0 to 1, with a score ≥0.45
Edouard Herriot, Unité de Transplanta- indicating nonresponse to medical therapy and an increased risk of death in the ab-
tion Hépatique, Lyon (J.D.); Hôpital sence of transplantation) or rapid worsening of liver function despite medical therapy.
Beaujon, Hepatology and Liver Intensive
Care, INSERM Unité 773 (F.D., C.F.), and Selected patients also had supportive family members, no severe coexisting condi-
Hepatobiliary and Pancreatic Surgery tions, and a commitment to alcohol abstinence. Survival was compared between pa-
(J.B.), University Denis Diderot–Paris VII, tients who underwent early liver transplantation and matched patients who did not.
Clichy; Hôpital Saint Eloi, Service d’Hépato-
Gastroentérologie et Transplantation Hé-
patique, Montpellier (G.-P.P.); and Hôpital Results
Albert Michallon, Service d’Hépatogas In all, 26 patients with severe alcoholic hepatitis at high risk of death (median Lille
troentérologie and INSERM Unité 823 score, 0.88) were selected and placed on the list for a liver transplant within a median of
(V. Leroy), and Service de Transplantation
Hépatique (C.L.), CHU de Grenoble, Gre 13 days after nonresponse to medical therapy. Fewer than 2% of patients admitted for
noble — all in France; and the Departments an episode of severe alcoholic hepatitis were selected. The centers used 2.9% of available
of Gastroenterology, Hepatopancreatology, grafts for this indication. The cumulative 6-month survival rate (±SE) was higher among
and Digestive Oncology (C.M., T.G.), and
Hepatobiliary Surgery and Liver Transplanta- patients who received early transplantation than among those who did not (77±8% vs.
tion (V. Lucidi, V.D.), Erasme Hospital, Uni- 23±8%, P<0.001). This benefit of early transplantation was maintained through 2 years
versité Libre de Bruxelles, Brussels. Address of follow-up (hazard ratio, 6.08; P = 0.004). Three patients resumed drinking alcohol: one
reprint requests to Dr. Mathurin at Hôpital
Claude Huriez, Services Maladies de l’Appa at 720 days, one at 740 days, and one at 1140 days after transplantation.
reil Digestif et INSERM Unité 995 CHU, Uni-
versité Lille Nord de France, F-59000 Lille, Conclusions
France, or at philippe.mathurin@chru-lille.fr. Early liver transplantation can improve survival in patients with a first episode of
N Engl J Med 2011;365:1790-1800. severe alcoholic hepatitis not responding to medical therapy. (Funded by Société
Copyright © 2011 Massachusetts Medical Society. Nationale Française de Gastroentérologie.)
1790 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
L
iver transplantation for alcoholic holic hepatitis not responding to medical therapy.
liver disease has a favorable outcome but Alcoholic hepatitis was considered to be severe if
remains controversial.1,2 Reluctance to per- the Maddrey’s discriminant function was greater
form transplantation in patients with alcoholism than 32, calculated as follows: 4.6 × (patient’s
is often based on the view that they are responsi- prothrombin time in seconds − matched control’s
ble for their illness and are likely to resume alco- prothrombin time in seconds) + patient’s serum
hol use after transplantation.3 To select the most bilirubin level in milligrams per deciliter. A Mad-
appropriate patients with severe forms of alco- drey’s discriminant function of greater than 32 is
holic liver disease for transplantation, most pro- the threshold for initiating glucocorticoid treat-
grams require a 6-month abstinence period be- ment.6 Nonresponse to medical therapy was de-
fore patients can be considered. Nevertheless, fined according to the Lille model as a score of
data regarding the 6-month rule as a predictor of 0.45 or more after 7 days of medical therapy or a
long-term sobriety are controversial.4 Despite the continuous increase in the Model for End-Stage
frequent use of the rule, the United Network for Liver Disease (MELD) score,11 reflecting an early
Organ Sharing and the French Consensus Confer- worsening of liver function. Medical therapy con-
ence5 do not consider it to be a formal guideline. sisted of standard medical care for severe liver
Glucocorticoids have been recommended by insufficiency and use of glucocorticoids (40 mg
recent U.S. guidelines to treat severe alcoholic per day of prednisolone for at least 7 days). Non-
hepatitis.6 The Lille model enables early identifi- response to medical therapy is associated with
cation of patients unlikely to respond to medical 6-month survival of approximately 30%.7
treatment.7,8 Strict application of the rule requiring We selected patients with severe alcoholic
6 months of sobriety 9,10 may be disadvantageous hepatitis who were considered to be candidates
to such patients, 70 to 80% of whom die within for early transplantation, according to the fol-
that period. Consequently, early liver transplan- lowing criteria: nonresponse to medical therapy
tation should be evaluated in pilot studies re- (as defined above), severe alcoholic hepatitis as
stricted to carefully selected patients, as recom- the first liver-decompensating event, presence of
mended by the latest French consensus.5 close supportive family members, absence of
The aims of this study were to determine severe coexisting or psychiatric disorders, and
whether early liver transplantation improves the agreement by patients (with support from family
6-month survival rate among patients whose se- members) to adhere to lifelong total alcohol
vere alcoholic hepatitis is unresponsive to medi- abstinence. The selection process consisted of
cal management, to evaluate the rate of alcohol several meetings between four medical team
relapse after transplantation in patients selected circles, the patient’s family, and the patient. The
without applying the 6-month rule, and to evaluate team circles were as follows: first, the inner
the burden of early transplantation on the overall circle, closest to the patient, comprising nurses,
transplantation activity of participating centers. one resident, and one fellow; second, a specialist
in addiction; third, senior hepatologists; and
Me thods fourth, the outermost circle, consisting of an
anesthetist and surgeons. The four team circles
Study Conduct had to reach complete consensus on selection.
Scientific committees from the Association Fran- This selection process was performed at all
çaise d’Etude du Foie, the Association Française de seven participating centers, which provided data
Chirurgie Hépato-Biliaire et de Transplantation, on all early transplantations performed until
and the Agence de Biomédecine (the French govern- September 1, 2010. The Lille and Brussels cen-
ment agency in charge of graft allocation) approved ters started the program in November 2005; the
the study. All selected patients provided written others began later. Two study patients did not
informed consent for transplantation surgery. receive glucocorticoids because their physicians
considered the benefits to be negligible. Addi-
Selection of the Study Patients tional details about the selection process are
Seven transplant centers agreed to perform early provided in the Supplementary Appendix, avail-
liver transplantation in patients with severe alco- able with the full text of this article at NEJM.org.
n engl j med 365;19 nejm.org november 10, 2011 1791
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Assessment of Alcohol Use after transplantation), we recorded data on all
after Transplantation infections and subsequent treatment as well as
After transplantation, alcohol use was assessed at any alcohol relapses, including those occurring
short intervals during informal interviews of pa- more than 6 months after transplantation.
tients and their families performed according to
the design of previous studies.10,12,13 (See the Sup- Burden of Early Liver Transplantation
plementary Appendix for additional details on as- The total number of transplantations and the
sessment of alcohol use after transplantation.) number of transplantations for alcoholic liver
disease were reported annually by all centers,
Data Collection starting with the first early transplantation and
Development of biologic features of abnormal until September 1, 2010. Only the Lille and Brus-
liver or kidney function was ascertained at least sels centers had prospective databases of patients
weekly from the first day of medical therapy until with biopsy-proven severe alcoholic hepatitis.
the patient was placed on the transplantation These databases systematically recorded data for
list. During the data collection period (i.e., the all patients with severe alcoholic liver disease
first day of medical therapy through 24 months meeting the criteria for nonresponse to medical
Table 1. Characteristics of the 26 Study Patients with Severe Alcoholic Hepatitis.*
Characteristic Value
Male sex — no. (%) 15 (58)
Age — yr
Median 47.4
Range 34.9–60.5
Glucocorticoid therapy — no. (%) 24 (92)
Duration of glucocorticoid therapy — days
Median 12
Range 7–31
First day of medical therapy
Prothrombin time — sec
Median 23.2
Range 14.3–82.0
International normalized ratio
Median 2.5
Range 1.3–5.8
Bilirubin — mg/dl
Median 27.7
Range 10.0–61.3
Serum creatinine — mg/dl
Median 0.82
Range 0.47–6.10
Albumin — g/liter
Median 25
Range 14–33
Maddrey’s discriminant function†
Median 76
Range 36–165
MELD score‡
Median 30.1
Range 22.0–47.3
1792 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
Table 1. (Continued.)
Characteristic Value
After 7 days of medical therapy
Prothrombin time — sec
Median 33.5
Range 11.0–56.0
International normalized ratio
Median 2.2
Range 1.3–4.7
Bilirubin — mg/dl
Median 28.4
Range 9.6–48.7
Serum creatinine — mg/dl
Median 0.96
Range 0.48–4.95
Albumin — g/liter
Median 27
Range 18–37
Lille score‡
Median 0.880
Range 0.260–0.996
MELD score§
Median 28.5
Range 23.0–52.4
* To convert the values for serum creatinine to micromoles per liter, multiply by 88.4. To convert the values for bilirubin to mi-
cromoles per liter, multiply by 17.1.
† Maddrey’s discriminant function is a measure of severity of alcoholic hepatitis and is calculated as follows: 4.6 × (patient’s
prothrombin time in seconds − matched control’s prothrombin time in seconds) + patient’s serum bilirubin level in milligrams
per deciliter. A score of more than 32 indicates severe alcoholic hepatitis and is the threshold for initiating glucocorticoid
treatment.
‡ A Lille score of 0.45 or higher indicates nonresponse to medical therapy. The Lille score ranges from 0 to 1 and is calculated
(www.lillemodel.com) with the use of the following formula: Exp (−R)/(1 + Exp [−R]), where R = (3.19 − 0.101 × age in years) +
(0.147 × albumin on day 0 in grams per liter) + ([0.0165 × change in bilirubin between day 0 and day 7 of medical therapy, in
micromoles per liter] − [0.206 × renal insufficiency {rated as 0 if absent and 1 if present}] − [0.0065 × bilirubin level on day 0 in
micromoles per liter] − [0.0096 × prothrombin time in seconds]). In patients who received albumin infusions, the last available
albumin value before infusion was used.
§ The Model for End-Stage Liver Disease (MELD) score is calculated (www.mayoclinic.org/meld/mayomodel7.html) as follows:
(9.57 × log creatinine in milligrams per deciliter) + (3.78 × log bilirubin in milligrams per deciliter) + (11.20 × log international nor-
malized ratio) + 6.43. Scores range from 6 to 42, with higher scores indicating a worse prognosis.
therapy and, for those not selected for early trans- discriminant function, and Lille score (see the
plantation, the primary reason for exclusion. Supplementary Appendix).
Second, we randomly sampled control patients
Case–Control Study from a set of patients with severe alcoholic hepa-
Two patients whose disease was not responding titis who were listed in a combined prospective
to medical therapy — a case patient who under- database of the Lille center. To avoid the risk of
went early transplantation and a control patient selecting the same control in the two matching
who did not — were matched with the use of two procedures (nonrandom and random), we excluded
matching-selection processes. First, we nonran- all the matched controls who were already se-
domly selected the control patient who was the lected with the nonrandom matching procedure.
best fit for each case patient who underwent The final combined database contained a total
transplantation, according to age, sex, Maddrey’s of 651 potential control patients. The random
n engl j med 365;19 nejm.org november 10, 2011 1793
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
selection was performed by means of the global R e sult s
optimal algorithm14 (SAS software, version 9.2;
SAS Institute) with the following preestablished Characteristics of the Study Population
ranges or values: age, ±10 years of the case pa- Twenty-six patients with severe alcoholic hepati-
tient’s age; sex, same as the case patient; Mad- tis that had failed to respond to medical manage-
drey’s discriminant function, same category as ment underwent liver transplantation at the seven
the case patient’s (<60, 60 to 90, or >90); and Lille centers (Table 1). Alcoholic hepatitis was proved
score, ±0.15 of the case patient’s score (see the by biopsy specimens obtained by the transjugu-
Supplementary Appendix). lar route in 23 of the 26 case patients (88%) and
We also examined whether patients who un- confirmed in all case patients by means of histo-
derwent early liver transplantation owing to non- logic analysis of explants. The first transplantation
response to medical therapy had outcomes simi- was performed under this selection process on
lar to patients whose disease had responded to August 24, 2006, and the final one was conducted
medical therapy (i.e., those with a Lille score on June 16, 2010.
<0.45). To address this question, control patients Nonresponse to medical therapy was defined
with Lille scores less than 0.45 were matched to as a Lille score of 0.45 or more in 25 patients and
case patients on the basis of the global optimal early worsening of liver function in 1 patient whose
algorithm, with terms for age, sex, and Maddrey’s MELD score increased from 23 at day 7 to 36 at
discriminant function (but not Lille score). day 21, the day of listing (albeit whose Lille score
was 0.26). A total of 24 of 26 patients were treated
Statistical Analysis with glucocorticoids for 12 days (95% confidence
Assuming 6-month survival rates of 70% among interval [CI], 7 to 18). The remaining 2 patients did
patients who underwent transplantation and 30% not receive glucocorticoids before referral to the
among the matched controls,15,16 we calculated transplantation unit. One had type 1 hepatorenal
that at least 18 patients and 18 controls would syndrome, and both had high Lille scores (0.88
have to be included for the study to have a sta- and 0.66) within 7 days after hospitalization and
tistical power of at least 80% to show a signifi- before transfer to the transplantation center. For
cant difference in the survival rate between the these 2 patients, the transplantation physicians
two groups. Variables were compared between believed that glucocorticoid therapy would have
the two groups with the use of chi-square tests a negligible effect.17
and t-tests. The follow-up time was defined as
the period from the first day of medical therapy MELD Scores and Transplantation
to the last follow-up visit. In the case–control The median MELD score at the time of listing as a
study, we estimated patients’ rate of survival candidate for transplantation was 34 (Table 2). The
(expressed as a percentage ±SE) by means of the decision to list patients for transplantation was
Kaplan–Meier method and compared survival made soon after ascertainment of nonresponse to
between the two groups by using the log-rank medical therapy (median, 13 days), and transplan-
test. The first day of medical therapy was de- tation was performed soon after listing (median,
fined as the first day of glucocorticoid adminis- 9 days afterward). Nonresponse to medical therapy
tration or, for the two patients not treated with was confirmed by the worsening of MELD scores
glucocorticoids, the first day of admission. The until the time of listing. Substantial improvement
rate of 6-month survival — the primary end before the time of listing (i.e., >10% decrease in the
point — was measured from the first day of MELD score) was observed in three patients who
medical therapy to the date of death from any underwent transplantation, after treatment with
cause. In addition, we performed an analysis hepatic or renal support, which decreased bilirubin
over an extended follow-up period of 2 years. and creatinine levels.
Data for patients without events of interest were
censored at the date of the last follow-up visit. Survival
A Cox proportional-hazards analysis, after ad- Liver grafts were obtained from cadaveric donors
justment for the MELD score and center (Lille (see the Supplementary Appendix). Patients who
vs. other centers), was also performed. All P val- underwent transplantation and controls were
ues are two-tailed. well-matched (Table 3). The 6-month survival rate
1794 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
was significantly higher among patients undergo-
Table 2. Clinical and Biologic Events between Study Enrollment and Listing for
ing transplantation (77±8%) than among matched Liver Transplantation in the 26 Study Patients with Severe Alcoholic Hepatitis.
controls (23±8%, P<0.001) (Fig. 1). The benefit of
performing early transplantation was supported by Event Value
the fact that 90% of deaths (18 of 20) among con- Bacterial infection — no. (%)* 18 (69)
trol patients occurred within 2 months after identi- Ascites 6 (23)
fication of nonresponse to medical therapy (Fig. 1). Pulmonary 5 (19)
After transplantation, five of six deaths were Urinary 4 (15)
related to infection occurring within 2 weeks Bacteremia 5 (19)
after surgery; the infection was invasive asper- Other 2 (8)
gillus infection in four cases. Cerebral aspergil-
Gram-negative bacteria 9 (35)
losis developed in one patient who had under-
Gram-positive cocci 6 (23)
gone transplantation and survived; it was rapidly
Pneumocystis carinii 2 (8)
treated with voriconazole. The patients undergoing
transplantation who died did not differ signifi- Fungal infection 3 (12)
cantly from those who remained alive, although Spontaneous bacterial peritonitis without identifiable 2 (8)
bacteria
the duration of glucocorticoid therapy was longer
Hepatorenal syndrome — no. (%) 15 (58)
(see the Supplementary Appendix).
Renal support or molecular adsorbent recirculating sys- 10 (38)
Additional analysis with extension of follow-up tem — no. (%)
to 2 years showed that transplantation remained
Gastrointestinal bleeding — no. (%) 4 (15)
associated with survival in univariate analyses
Mechanical ventilation — no. (%) 4 (15)
(71±9% vs. 23±8%, P<0.001) (Fig. 1) and multi-
Time from end of glucocorticoid treatment to listing —
variate analyses (hazard ratio, 6.08; 95% CI, 1.77 days
to 20.88; P = 0.004) adjusted for the center (Lille Median (95% CI) 13 (6 to 17)
vs. other centers) and the MELD score.
Range 1 to 46
Use of the global optimal algorithm resulted
MELD at time of listing
in the random selection of 69 additional matched
Median (95% CI) 34 (29 to 37)
controls who were nonresponders to medical
therapy and 92 additional matched controls who Range 25 to 41
were responders. The 69 randomly selected matched Difference in MELD between nonresponse and listing†
controls whose disease was nonresponsive to Median (95% CI) −1.9 (−6.0 to 0.0)
medical therapy were not significantly different Range −14.2 to 14.4
from the 26 patients who underwent transplan- Time from listing to liver transplantation — days
tation in terms of male sex (59.4%, P = 0.90), Median (95% CI) 9 (3 to 11)
median age (control group, 51.8 years; 95% CI, Range 1 to 37
47.0 to 53.8; P = 0.19 for comparison with case
patients), median Maddrey’s discriminant func- * Infection developed at multiple sites in four patients.
† Nonresponse to medical therapy was determined after 7 days of medical therapy.
tion (control group, 70.8; 95% CI, 64.2 to 82.3; All improvements were related to the use of a molecular adsorbent recirculating
P = 0.79), and Lille score (control group, 0.87; system or renal-replacement therapy.
95% CI, 0.80 to 0.93; P = 0.66). The 92 randomly
selected matched controls whose disease did than among the nonresponder controls (77±8%
respond to medical therapy were not signifi- vs. 30±6%, P<0.001) but not significantly differ-
cantly different from the 26 case patients in ent than the rate among the responder controls
terms of male sex (57.7%, P = 0.60), median age (77±8% vs. 85±4%, P = 0.33) (Fig. 2).
(control group, 46.2 years; 95% CI, 45.0 to 48.1;
P = 0.37), and median Maddrey’s discriminant Burden of Early Liver Transplantation
function (control group, 68.2; 95% CI, 65.4 to During the study period, 891 transplantations
76.0; P = 0.33), but as expected, the responder were performed at the seven centers; 315 of these
control group had lower Lille scores (0.18; 95% CI, transplantations were for alcoholic liver disease.
0.10 to 0.21; P<0.001) than the case-patient group. A total of 26 of all 891 procedures (2.9%) and 26
The 6-month survival rate was higher among the of the 315 procedures for alcoholic liver disease
26 case patients who underwent transplantation (8.3%) were early transplantations.
n engl j med 365;19 nejm.org november 10, 2011 1795
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 3. Results of Case–Control Comparisons of the 26 Study Patients and 26 Matched Controls.*
Characteristic Patients Who Underwent Transplantation Matched Controls P Value
Living with a partner — no. (%) 17 (65) 13 (50) 0.19
Employed — no. (%) 17 (65) 16 (62) 0.92
Male sex — no. (%) 15 (58) 15 (58) 1.00
Age — yr 0.34
Median (range) 47.4 (34.9–60.5) 50.6 (34.5–60.6)
95% CI 42.6–52.4 46.5–52.6
First day of medical therapy
Maddrey’s discriminant function 0.56
Median (range) 76.0 (35.6–165.0) 80.6 (48.4–202.0)
95% CI 61.2–91.0 66.4–97.5
Lille score 0.28
Median (range) 0.880 (0.260–0.996) 0.827 (0.250–0.999)
95% CI 0.760–0.950 0.690–0.874
MELD score 0.27
Median (range) 30.1 (22.0–47.3) 29.1 (19.1–40.0)
95% CI 27.1–33.4 25.6–32.4
Prothrombin time — sec 0.63
Median (range) 23.2 (14.3–82.0) 24.1 (16.7–51.5)
95% CI 18.9–27.8 20.7–26.6
Bilirubin — mg/dl 0.61
Median (range) 27.7 (10.0–61.3) 26.2 (4.7–65.0)
95% CI 19.1–31.8 17.4–34.7
Serum creatinine — mg/dl 0.11
Median (range) 0.8 (0.5–6.1) 1.1 (0.6–3.8)
95% CI 0.6–1.1 0.8–1.4
Albumin — g/liter 0.42
Median (range) 25 (14–33) 24 (11–36)
95% CI 23–29 21–26
After 7 days of medical therapy
MELD score 0.47
Median (range) 28.5 (23.0–52.4) 29.4 (19.4–60.2)
95% CI 26.2–33.7 25.6–31.8
Prothrombin time — sec 0.63
Median (range) 22.2 (14.2–59.0) 23.5 (14.7–70.0)
95% CI 20.7–24.5 20.3–26.3
Bilirubin — mg/dl 0.58
Median (range) 28.4 (9.6–48.7) 27.7 (4.3–66.8)
95% CI 24.7–34.1 20.1–34.6
Creatinine — mg/dl 0.26
Median (range) 1.0 (0.5–5.0) 1.2 (0.6–5.2)
95% CI 0.6–1.2 0.9–1.4
Albumin — g/liter 0.52
Median (range) 27 (18–37) 27 (21–51)
95% CI 24–30 24–30
* To convert the values for serum creatinine to micromoles per liter, multiply by 88.4. To convert values for bilirubin to micromoles per liter,
multiply by 17.1.
1796 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
100
77±8% Patients undergoing transplantation
75 71±9%
Survival (%)
P<0.001 at 6 mo P<0.001 at 24 mo
50 (primary end point) (extended follow-up)
25 23±8% Matched controls 23±8%
0
0 6 12 18 24
Months
No. at Risk
Patients undergoing 26 20 15 14 13
transplantation
Matched controls 26 6 6 5 4
Figure 1. Kaplan–Meier Estimates of Survival in the 26 Study Patients and the 26 Best-Fit Matched Controls.
In all, 233 patients were admitted for severe deciliter (32.5 μmol per liter) (95% CI, 1.5 to 3.0 mg
alcoholic hepatitis at the Brussels center (52 pa- per deciliter [25.6 to 51.3 μmol per liter]) at 1 month
tients) and the Lille center (181 patients). A totalto 0.7 mg per deciliter (12.0 μmol per liter) (95% CI,
of 18 of the 233 underwent transplantation (see 0.6 to 1.1 mg per deciliter [10.3 to 18.8 μmol per
Table 1 in the Supplementary Appendix), 14 of liter]) at 6 months (P<0.001).
whom had been referred by community hospitals. After transplantation, patients were followed at
The remaining 4 were directly selected by the short intervals, with a median of 11 visits (95% CI,
Brussels and Lille centers through their own re- 9 to 13) during the 6-month period. Since that time,
cruitment of patients with severe alcoholic hepa- follow-up is ongoing, with a median of 11 visits
titis (representing 1.8% of the 219 patients who (95% CI, 5 to 14) at a median interval of 1.8 months
had not undergone transplantation or referral by (95% CI, 0.7 to 2.3). No alcoholic relapse was ob-
community hospitals). The reason for exclusion served within the initial 6-month follow-up period.
from early transplantation was a predisposition Three of 26 patients later resumed drinking alco-
to addiction or unfavorable social or familial pro- hol, one at 720 days, one at 740 days, and one at
files in approximately 90% of nonresponders with 1140 days after transplantation. Despite counsel-
severe alcoholic liver disease. ing by an addiction specialist, 2 patients remained
daily consumers (30 g per day and >50 g per day),
Follow-up and Assessment of Alcohol Relapse whereas 1 drank occasionally (approximately 10 g
In case patients who were alive at 6 months, per week). None of them has had graft dysfunction.
liver tests and creatinine levels returned to nor-
mal ranges within the first month after trans- Discussion
plantation. There was no significant difference
between the 1-month and 6-month values of the The high risk of early death7,17 in patients with
aminotransferases, γ-glutamyltransferase, cre- severe alcoholic hepatitis not responding to med-
atinine, or international normalized ratio (see ical therapy11,18,19 makes it necessary to consider
the Supplementary Appendix), although the me- all available treatment options, including trans-
dian total bilirubin level declined from 1.9 mg per plantation, in targeted patients.20 Choosing the
n engl j med 365;19 nejm.org november 10, 2011 1797
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
100
Responder controls
85±4%
P=0.33
75 Patients undergoing transplantation
77±8%
Survival (%) P<0.001
50
Nonresponder controls
25 30±6%
0
0 2 4 6
Months
No. at Risk
Responder controls 92 77 75 71
Patients undergoing 26 21 21 20
transplantation
Nonresponder controls 69 21 21 19
Figure 2. Kaplan–Meier Estimates of Survival among the 26 Study Patients and Randomly Selected Matched Controls.
appropriate moment for transplantation is cru- tation, and the tailoring of immunosuppressive
cial, to avoid adverse effects of intervening too regimens are warranted in light of the deaths
soon or too late.21 This prospective multicenter due to aspergillosis.
study showed that early transplantation clearly Our findings challenge both the notion of a
improves the probability of 6-month survival prescribed abstinence period as the only alco-
among patients in whom medical therapy failed. holism-related criterion for transplant eligibility23
We selected control patients by using two differ- and the opinion of experts that alcoholic hepatitis
ent processes of matching so as to reduce inves- is a contraindication for transplantation.24 How-
tigator bias and limit period and cohort effects. ever, the stringency of our selection process re-
Team members requested stringent selection sulted in our selecting a very small number of
for at least two reasons. First, donor grafts remain patients with alcoholic hepatitis for early trans-
in short supply. Second, in the allocation system plantation. Although numerous studies have lent
based on MELD scores, patients with severe alco- support to the validity of a sobriety period, they
holic hepatitis who are not having a response also have observed that the enforcement of this
to medical therapy are likely to rank at the top of period alone delays listing for transplantation a
the transplant waiting list. Therefore, team mem- considerable number of candidates with a low
bers believed that patients who were unaware of probability of relapse.10,25-30 Indeed, the duration
their underlying liver disease constituted the most of abstinence before transplantation is a poor pre-
urgent problem. However, the exclusion of patients dictor of relapse of alcoholism.31 Organization of
with previous episodes of liver decompensation the medical staff into four team circles should
raises an ethical question, since there is no agree- have ensured a balanced selection process. No
ment about the rationale for excluding alcoholic relapse of alcoholism was observed during the
patients from transplantation.22 6 months following transplantation, although
Studies evaluating the usefulness of fungal three patients had a relapse later. This low rate
prophylaxis before transplantation, duration of of relapse was probably related to our stringent
glucocorticoid use before and after transplan- selection of candidates for transplantation; for
1798 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
instance, physicians from Lille and Brussels se- Supported by a grant from the Société Nationale Française de
Gastroentérologie.
lected fewer than 2% of the patients with severe Dr. Dharancy reports receiving consulting fees from Roche
alcoholic hepatitis recruited at their centers. and lecture fees from Astellas and serving as a board member of
Regarding organ shortage,32 early liver trans- Novartis. Dr. Dumortier reports receiving consulting fees, lec-
ture fees, and grant support from Novartis and serving as a
plantation accounted for only 2.9% of grafts used board member of Novartis; receiving lecture fees from Janssen-
during the study period. Nevertheless, modifica- Cilag; receiving grant support from and serving as a board mem-
tions in guidelines for liver transplantation in pa- ber of Astellas; receiving grant support from and serving as a
board member of Roche; receiving grant support from Schering-
tients with alcoholism may conflict with public
Plough; and serving as a board member of GlaxoSmithKline.
preferences for liver-transplant allotment33,34 and Dr. Durand reports receiving consulting fees from Astellas and
may decrease willingness to donate.3 However, consulting fees and grant support from Novartis. Dr. Leroy re-
this has not occurred in response to transplanta- ports receiving lecture fees and grant support from and serving
as a board member of Roche; receiving lecture fees and grant
tion being offered to patients with fulminant support from and serving as a board member of Bristol-Myers
hepatic failure due to voluntary acetaminophen Squibb; receiving lecture fees and grant support from and serv-
poisoning, nor to intravenous-drug users with ing as a board member of Gilead; receiving lecture fees from and
serving as a board member of Merck; and serving as a board
acute hepatitis B virus infection. The limited supply member of Janssen-Cilag. Dr. Louvet reports receiving consulting
of donor organs frequently biases what should be fees from Schering-Plough and Bristol-Myers Squibb. Dr. Mathu
equal access to potential medical benefits for all rin reports receiving lecture fees and grant support from and
serving as a board member of Roche; receiving lecture fees from
patients.35 Development of an international data- and serving as a board member of Schering-Plough; receiving
base collecting information on survival and ad- lecture fees from and serving as a board member of Bristol-
diction is warranted to provide more facts and Myers Squibb; receiving lecture fees from and serving as a board
member of Gilead; receiving lecture fees from Bayer Healthcare;
less conjecture in future discussions of the role receiving grant support from and serving as a board member
of early transplantation in the treatment of se- of Janssen-Cilag; and serving as a board member of Norgine.
vere alcoholic hepatitis.36 Dr. Pageaux reports receiving lecture fees, grant support, and
reimbursement for travel expenses from Roche; receiving lec-
Although our data are encouraging, the study ture fees from Bayer HealthCare and Gilead; receiving grant
did have limitations. The design did not allow support from and serving as a board member of Astellas; and
for rigorous assessment of long-term outcomes. receiving grant support from Novartis. Dr. Pruvot reports re-
ceiving lecture fees and reimbursement for travel expenses
Matched controls may not have been comparable from Roche. Dr. Samuel reports receiving consulting fees, lecture
to patients in terms of support of family mem- fees, and grant support from Roche; consulting fees and lecture
bers, intentions of patients to remain alcohol- fees from Schering-Plough; consulting fees from Merck; con-
sulting fees, lecture fees, and grant support from Astellas; con-
free, or availability of counseling in the event of sulting fees, lecture fees, and grant support from Novartis;
a return to drinking. Future studies elucidating consulting fees from Janssen-Cilag; consulting fees and lec-
long-term outcomes will require a control group ture fees from Bristol-Myers Squibb; consulting fees and lecture
fees from Gilead; and consulting fees and lecture fees from
of patients with alcoholism undergoing trans- Laboratoire Français du Fractionnement et des Biotechnologies.
plantation after abstaining from alcohol for a No other potential conf licts were reported.
6-month period who are matched to patients on Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
the basis of social and familial characteristics.
We thank Nicole Declerck, Olivier Cottencin, Hamid Aftisse,
Previous studies of patients with alcoholism who Benjamin Rolland, and Christelle Bouquignaud (Hôpital Huriez,
underwent transplantation suggest that the rate Lille, France); Corinne Antoine (Agence de la Biomédecine,
of relapse over the long term may be approxi- Saint-Denis La Plaine, France); Delphine Degré, Nathalie Boon,
Nadine Bourgeois, Michael Adler, Alexis Buggenhout, Nicolas
mately 25 to 35%.10,12,13 Finally, reproducibility Clumeck, and Brigitte Ickx (Hôpital Erasme, Brussels); René
of the selection process needs to be attempted. Adam, Daniel Azoulay, Chady Salloum, Eric Vibert, Faouzi Sali-
In summary, early liver transplantation may be ba, Philippe Ichai, Teresa Antonini, Audrey Coilly, Rodolphe
Sobesky, Amine Benyamina, Lisa Blecha Magali Belnard, Colette
an appropriate rescue option for selected patients Danet, Elisabeth Pasdeloup, Catherine Tanguy, and Gael Berthe-
whose first episode of severe alcoholic hepatitis lot (Hôpital Paul-Brousse, Villejuif, France); Sophie Kalama-
is not responsive to medical therapy, after careful rides, Pauline Houssel, and Vanessa Esnault (Hôpital Beaujon,
Clichy, France); and all the nurses of the transplant teams and
assessment of their addiction profile. Our encour- hepatology units of all participating centers for their contribu-
aging results must be confirmed by other groups. tions to this study.
References
1. Burra P, Senzolo M, Adam R, et al. 2. Burroughs AK, Sabin CA, Rolles K, et 3. Shawcross DL, O’Grady JG. The
Liver transplantation for alcoholic liver al. 3-Month and 12-month mortality after 6-month abstinence rule in liver trans-
disease in Europe: a study from the ELTR first liver transplant in adults in Europe: plantation. Lancet 2010;376:216-7.
(European Liver Transplant Registry). Am predictive models for outcome. Lancet 4. Beresford TP, Everson GT. Liver trans-
J Transplant 2010;10:138-48. 2006;367:225-32. plantation for alcoholic liver disease: bias,
n engl j med 365;19 nejm.org november 10, 2011 1799
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Early Liver Tr ansplantation for Alcoholic Hepatitis
beliefs, 6-month rule, and relapse — but and simulated controls. Lancet 1994;344: alcoholic liver disease. Gastroenterol Clin
where are the data? Liver Transpl 2000; 502-7. Biol 2004;28:845-51.
6:777-8. 16. Poynard T, Naveau S, Doffoel M, et al. 26. Bird GL, O’Grady JG, Harvey FA,
5. Consensus conference: Indications for Evaluation of efficacy of liver transplanta- Calne RY, Williams R. Liver transplanta-
Liver Transplantation, January 19 and 20, tion in alcoholic cirrhosis using matched tion in patients with alcoholic cirrhosis:
2005, Lyon-Palais Des Congrès: text of rec- and simulated controls: 5-year survival. selection criteria and rates of survival and
ommendations (long version). Liver Transpl J Hepatol 1999;30:1130-7. relapse. BMJ 1990;301:15-7.
2006;12:998-1011. 17. Mathurin P, O’Grady J, Carithers RL, 27. Bravata DM, Olkin I, Barnato AE,
6. O’Shea RS, Dasarathy S, McCullough AJ. et al. Corticosteroids improve short-term Keeffe EB, Owens DK. Employment and
Alcoholic liver disease. Hepatology 2010; survival in patients with severe alcoholic alcohol use after liver transplantation for
51:307-28. hepatitis: meta-analysis of individual pa- alcoholic and nonalcoholic liver disease:
7. Louvet A, Naveau S, Abdelnour M, et al. tient data. Gut 2011;60:255-60. a systematic review. Liver Transpl 2001;7:
The Lille model: a new tool for therapeu- 18. Forrest EH, Evans CD, Stewart S, et al. 191-203.
tic strategy in patients with severe alco- Analysis of factors predictive of mortality 28. Kumar S, Stauber RE, Gavaler JS, et al.
holic hepatitis treated with steroids. Hepa- in alcoholic hepatitis and derivation and Orthotopic liver transplantation for alcohol
tology 2007;45:1348-54. validation of the Glasgow alcoholic hepa- ic liver disease. Hepatology 1990;11:159-64.
8. Louvet A, Wartel F, Castel H, et al. titis score. Gut 2005;54:1174-9. 29. Osorio RW, Ascher NL, Avery M, Ba-
Infection in patients with severe alcoholic 19. Srikureja W, Kyulo NL, Runyon BA, chetti P, Roberts JP, Lake JR. Predicting
hepatitis treated with steroids: early re- Hu KQ. MELD score is a better prognostic recidivism after orthotopic liver trans-
sponse to therapy is the key factor. Gastro- model than Child-Turcotte-Pugh score or plantation for alcoholic liver disease.
enterology 2009;137:541-8. discriminant function score in patients Hepatology 1994;20:105-10.
9. Everhart JE, Beresford TP. Liver trans- with alcoholic hepatitis. J Hepatol 2005;42: 30. Yates WR, Martin M, LaBrecque D,
plantation for alcoholic liver disease: a 700-6. Hillebrand D, Voigt M, Pfab D. A model to
survey of transplantation programs in the 20. Lucey MR, Mathurin P, Morgan TR. examine the validity of the 6-month absti-
United States. Liver Transpl Surg 1997;3: Alcoholic hepatitis. N Engl J Med 2009; nence criterion for liver transplantation.
220-6. 360:2758-69. Alcohol Clin Exp Res 1998;22:513-7.
10. Foster PF, Fabrega F, Karademir S, 21. Olthoff KM, Brown RS Jr, Delmonico 31. DiMartini A, Day N, Dew MA, et al.
Sankary HN, Mital D, Williams JW. Pre- FL, et al. Summary report of a national Alcohol consumption patterns and pre-
diction of abstinence from ethanol in conference: evolving concepts in liver al- dictors of use following liver transplan-
alcoholic recipients following liver trans- location in the MELD and PELD era. Liver tation for alcoholic liver disease. Liver
plantation. Hepatology 1997;25:1469- Transpl 2004;10:Suppl 2:A6-A22. Transpl 2006;12:813-20.
77. 22. Benjamin M, Turcotte JG. Ethics, alco- 32. McMaster P. Transplantation for alco-
11. Dunn W, Jamil LH, Brown LS, et al. holism and liver transplantation. In: Lucey holic liver disease in an era of organ
MELD accurately predicts mortality in pa- MR, Merion RM, Beresford TP. Liver trans- shortage. Lancet 2000;355:424-5.
tients with alcoholic hepatitis. Hepatology plantation & the alcoholic patient. New 33. Neuberger J. Transplantation for alco-
2005;41:353-8. York: Cambridge University Press, 1994: holic liver disease: a perspective from Eu-
12. Pageaux GP, Bismuth M, Perney P, et al. 113-30. rope. Liver Transpl Surg 1998;4:Suppl 1:
Alcohol relapse after liver transplantation 23. Lucey MR, Brown KA, Everson GT, S51-S57.
for alcoholic liver disease: does it matter? et al. Minimal criteria for placement of 34. Ubel PA, Jepson C, Baron J, Mohr T,
J Hepatol 2003;38:629-34. adults on the liver transplant waiting McMorrow S, Asch DA. Allocation of
13. Pageaux GP, Michel J, Coste V, et al. list: a report of a national conference transplantable organs: do people want to
Alcoholic cirrhosis is a good indication organized by the American Society of punish patients for causing their illness?
for liver transplantation, even for cases of Transplant Physicians and the American Liver Transpl 2001;7:600-7.
recidivism. Gut 1999;45:421-6. Association for the Study of Liver Dis- 35. Surman OS, Cosimi AB, DiMartini A.
14. Rosenbaum PR, Rubin DB. Construct- eases. Liver Transpl Surg 1997;3:628- Psychiatric care of patients undergoing
ing a control group using multivariate 37. organ transplantation. Transplantation
matched sampling methods that incorpo- 24. Bathgate AJ. Recommendations for 2009;87:1753-61.
rate the propensity score. Am Stat 1985;39: alcohol-related liver disease. Lancet 2006; 36. Dureja P, Lucey MR. The place of liver
33-8. 367:2045-6. transplantation in the treatment of severe
15. Poynard T, Barthelemy P, Fratte S, et 25. Miguet M, Monnet E, Vanlemmens C, alcoholic hepatitis. J Hepatol 2010;52:759-
al. Evaluation of liver transplantation in et al. Predictive factors of alcohol relapse 64.
alcoholic cirrhosis by a case-control study after orthotopic liver transplantation for Copyright © 2011 Massachusetts Medical Society.
1800 n engl j med 365;19 nejm.org november 10, 2011
The New England Journal of Medicine
Downloaded from nejm.org on July 7, 2012. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
Potrebbero piacerti anche
- The Liver Graft Before Transplantation: Defining Outcome After Liver TransplantationDa EverandThe Liver Graft Before Transplantation: Defining Outcome After Liver TransplantationXavier VerhelstNessuna valutazione finora
- AKIKI TrialDocumento12 pagineAKIKI TrialNaifmxNessuna valutazione finora
- 10 1016@j Jhep 2020 10 009Documento6 pagine10 1016@j Jhep 2020 10 009Adelina HorhatNessuna valutazione finora
- Colombia Médica: An Experience of Liver Transplantation in Latin America: A Medical Center in ColombiaDocumento6 pagineColombia Médica: An Experience of Liver Transplantation in Latin America: A Medical Center in ColombiaAlejandro Vesga VinchiraNessuna valutazione finora
- Top Trials in Gastroenterology & HepatologyDa EverandTop Trials in Gastroenterology & HepatologyValutazione: 4.5 su 5 stelle4.5/5 (7)
- Liver Diseases in the Pediatric Intensive Care Unit: A Clinical GuideDa EverandLiver Diseases in the Pediatric Intensive Care Unit: A Clinical GuidePhilippe JouvetNessuna valutazione finora
- Effect of Continuous Renal Replacement Therapy On Outcome in Pediatric Acute Liver FailureDocumento10 pagineEffect of Continuous Renal Replacement Therapy On Outcome in Pediatric Acute Liver FailureZakirin WeinNessuna valutazione finora
- Early Use of TIPS in Cirrhosis and Variceal BleedingDocumento10 pagineEarly Use of TIPS in Cirrhosis and Variceal Bleedingray liNessuna valutazione finora
- The Critically Ill Cirrhotic Patient: Evaluation and ManagementDa EverandThe Critically Ill Cirrhotic Patient: Evaluation and ManagementRobert S. RahimiNessuna valutazione finora
- Dialyzer Membrane Permeability and Survi PDFDocumento7 pagineDialyzer Membrane Permeability and Survi PDFNurul SaufikaNessuna valutazione finora
- Adler 2015Documento7 pagineAdler 2015nathaliepichardoNessuna valutazione finora
- Trial of Early, Goal-Directed Resuscitation For Septic ShockDocumento11 pagineTrial of Early, Goal-Directed Resuscitation For Septic Shockapi-308365861Nessuna valutazione finora
- 1 s2.0 S0140673606691113 MainDocumento7 pagine1 s2.0 S0140673606691113 MainLuis Angel Ruiz ZamoraNessuna valutazione finora
- Simultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDocumento8 pagineSimultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDr Shiv ChopraNessuna valutazione finora
- Complementary and Alternative Medical Lab Testing Part 8: UrologyDa EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyValutazione: 3 su 5 stelle3/5 (1)
- Rehabilitation of Patients With End-Stage Renal DiseaseDocumento11 pagineRehabilitation of Patients With End-Stage Renal DiseaseDefan Dapat Titik TerangNessuna valutazione finora
- Liver Intensive CareDocumento3 pagineLiver Intensive CareSureddi KumarNessuna valutazione finora
- Nej Mo A 1412278Documento10 pagineNej Mo A 1412278amiralevishNessuna valutazione finora
- Nutrients: Eating Patterns in Patients With Compensated Cirrhosis: A Case-Control StudyDocumento13 pagineNutrients: Eating Patterns in Patients With Compensated Cirrhosis: A Case-Control StudyNutrición DietéticaNessuna valutazione finora
- Top Trials in Gastroenterology & Hepatology, 2nd EditionDa EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionNessuna valutazione finora
- Posthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)Documento12 paginePosthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)drsubramanianNessuna valutazione finora
- Essentials in Lung TransplantationDa EverandEssentials in Lung TransplantationAllan R. GlanvilleNessuna valutazione finora
- Joi 130081Documento9 pagineJoi 130081Hana MitayaniNessuna valutazione finora
- JournalDocumento15 pagineJournalDelfi Dwi IkamadyaNessuna valutazione finora
- Vann Ucch I 2015Documento10 pagineVann Ucch I 2015gigibesiNessuna valutazione finora
- Cristal TrialDocumento9 pagineCristal TrialJorge Barrios FloresNessuna valutazione finora
- In Uence of A Pre-Dialysis Education Programme (PDEP) On The Mode of Renal Replacement TherapyDocumento6 pagineIn Uence of A Pre-Dialysis Education Programme (PDEP) On The Mode of Renal Replacement Therapyandrada14Nessuna valutazione finora
- Stevens JohsonDocumento8 pagineStevens JohsonDaily RomeroNessuna valutazione finora
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDocumento3 pagineGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghNessuna valutazione finora
- Criterio Nuevo para Transfusion 2014Documento2 pagineCriterio Nuevo para Transfusion 2014Humberto Liu BejaranoNessuna valutazione finora
- Shawn SenDocumento3 pagineShawn SenDhruv MahajanNessuna valutazione finora
- Perioperative Care For Kidney Patients: KeywordsDocumento6 paginePerioperative Care For Kidney Patients: KeywordsAziil LiizaNessuna valutazione finora
- HDFVVC EfectoDocumento11 pagineHDFVVC Efectogiseladelarosa2006Nessuna valutazione finora
- Renal Disease in Cancer PatientsDa EverandRenal Disease in Cancer PatientsKevin W. FinkelNessuna valutazione finora
- Central Nervous System Tumours of ChildhoodDa EverandCentral Nervous System Tumours of ChildhoodEdward EstlinNessuna valutazione finora
- 2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisDocumento2 pagine2014 Prednisolone vs. Pentoxifylline For Severe Alcoholic HepatitisJairo Torres SoteloNessuna valutazione finora
- Measurement For Improvement in AnaesthesiaDocumento4 pagineMeasurement For Improvement in AnaesthesiavvvNessuna valutazione finora
- Gfy 046Documento10 pagineGfy 046Andika ArifiansyahNessuna valutazione finora
- Restrictive Fluids in Septic Shock. NEJM 2022Documento12 pagineRestrictive Fluids in Septic Shock. NEJM 2022neeraj SinghNessuna valutazione finora
- 2012 Best Parctice Medical O Grady TH en FHADocumento7 pagine2012 Best Parctice Medical O Grady TH en FHASol Del Mar SarmientoNessuna valutazione finora
- Liver Transplantation For Bile Duct Injury After Open and Laparoscopic CholecystectomyDocumento6 pagineLiver Transplantation For Bile Duct Injury After Open and Laparoscopic Cholecystectomymedodido94Nessuna valutazione finora
- Timing RRT AkiDocumento9 pagineTiming RRT AkidharmaNessuna valutazione finora
- Acute Kidney Disease and The CommunityDocumento3 pagineAcute Kidney Disease and The CommunityAriNessuna valutazione finora
- Boyd Et Al - (2012)Documento2 pagineBoyd Et Al - (2012)nuiv iyvbivboiuNessuna valutazione finora
- Nonsense Mutation Correction in Human Diseases: An Approach for Targeted MedicineDa EverandNonsense Mutation Correction in Human Diseases: An Approach for Targeted MedicineNessuna valutazione finora
- Critical Care for Potential Liver Transplant CandidatesDa EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNessuna valutazione finora
- Denosumab For Treatment of Hypercalcemia of MalignancyDocumento9 pagineDenosumab For Treatment of Hypercalcemia of MalignancySandra PargaNessuna valutazione finora
- TIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent AscitesDocumento7 pagineTIPS With Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent Ascitesray liNessuna valutazione finora
- Articles: BackgroundDocumento7 pagineArticles: BackgroundERIKANessuna valutazione finora
- Critical Care Goals and ObjectivesDocumento28 pagineCritical Care Goals and ObjectivesjyothiNessuna valutazione finora
- Survival Advantage of Hemodialysis Relative To Peritoneal Dialysis in Patients With End-Stage Renal Disease and Congestive Heart FailureDocumento8 pagineSurvival Advantage of Hemodialysis Relative To Peritoneal Dialysis in Patients With End-Stage Renal Disease and Congestive Heart FailureaduhbingungNessuna valutazione finora
- IJCRT2108180Documento6 pagineIJCRT2108180Anchana KsNessuna valutazione finora
- Liver Disease: A Clinical CasebookDa EverandLiver Disease: A Clinical CasebookStanley Martin CohenNessuna valutazione finora
- Acute Alcoholic HepatitisDocumento11 pagineAcute Alcoholic HepatitisDoc_NethoNessuna valutazione finora
- Management of Acute Liver Failure. Clinical Guideline From The Catalan Society of DigestologyDocumento14 pagineManagement of Acute Liver Failure. Clinical Guideline From The Catalan Society of DigestologyPhan Nguyễn Đại NghĩaNessuna valutazione finora
- Arthritis Rheumatism - 2002 - Houssiau - Immunosuppressive Therapy in Lupus Nephritis The Euro Lupus Nephritis Trial A (1) - 220727 - 183333Documento11 pagineArthritis Rheumatism - 2002 - Houssiau - Immunosuppressive Therapy in Lupus Nephritis The Euro Lupus Nephritis Trial A (1) - 220727 - 183333HPNessuna valutazione finora
- Journal of DiabetesDocumento6 pagineJournal of DiabetesSartika Rizky HapsariNessuna valutazione finora
- Evaporative Condenser Engineering Manual: Technical ResourcesDocumento18 pagineEvaporative Condenser Engineering Manual: Technical ResourcesMohamed IbrahimNessuna valutazione finora
- Expansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 3Documento1 paginaExpansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 3CunCunAlAndraNessuna valutazione finora
- Evaporative Condenser Engineering Manual: Technical ResourcesDocumento18 pagineEvaporative Condenser Engineering Manual: Technical ResourcesMohamed IbrahimNessuna valutazione finora
- Expansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 1Documento1 paginaExpansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 1CunCunAlAndraNessuna valutazione finora
- Evaporative Condenser Engineering Manual: Technical ResourcesDocumento18 pagineEvaporative Condenser Engineering Manual: Technical ResourcesMohamed IbrahimNessuna valutazione finora
- Expansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 2Documento1 paginaExpansion Tank Design Guide, How To Size and Select An Expansion Tank For A Chilled Water System 2CunCunAlAndraNessuna valutazione finora
- Management Gathering 0718 - Distribution - v5 CoverDocumento1 paginaManagement Gathering 0718 - Distribution - v5 CoverCunCunAlAndraNessuna valutazione finora
- Consulting Business ModelDocumento1 paginaConsulting Business ModelCunCunAlAndraNessuna valutazione finora
- Process Plant Layout - Seán Moran 3-4Documento2 pagineProcess Plant Layout - Seán Moran 3-4CunCunAlAndraNessuna valutazione finora
- GF Signet 515 2536 Manual02Documento1 paginaGF Signet 515 2536 Manual02CunCunAlAndraNessuna valutazione finora
- DA38 Safety Data Shett FAME (Fatty Acid Methyl Ester) V4 - en - DEDocumento14 pagineDA38 Safety Data Shett FAME (Fatty Acid Methyl Ester) V4 - en - DECunCunAlAndraNessuna valutazione finora
- RicoDocumento62 pagineRicoCunCunAlAndraNessuna valutazione finora
- Process Plant Layout - Seán Moran 1-2Documento2 pagineProcess Plant Layout - Seán Moran 1-2CunCunAlAndra100% (1)
- GF Signet 515 2536 Manual01Documento1 paginaGF Signet 515 2536 Manual01CunCunAlAndraNessuna valutazione finora
- Daftar Obat AnesDocumento44 pagineDaftar Obat AnesCunCunAlAndraNessuna valutazione finora
- 1348493956.2409obstetrics Handbook PDFDocumento48 pagine1348493956.2409obstetrics Handbook PDFdrng48Nessuna valutazione finora
- Frontline Gastroenterol 2014 Dyson Flgastro 2013 100404Documento11 pagineFrontline Gastroenterol 2014 Dyson Flgastro 2013 100404CunCunAlAndraNessuna valutazione finora
- Kjae-68-101 Transfusion-Related Acute Lung InjuryDocumento5 pagineKjae-68-101 Transfusion-Related Acute Lung InjuryCunCunAlAndraNessuna valutazione finora
- Gastro Enter Oh Epa ToDocumento29 pagineGastro Enter Oh Epa TodeliaintanNessuna valutazione finora
- NonalcoholicFattyLiverDisease2012 25762 FTPDocumento19 pagineNonalcoholicFattyLiverDisease2012 25762 FTPbudi_26690Nessuna valutazione finora
- RicoDocumento62 pagineRicoCunCunAlAndraNessuna valutazione finora
- Problem 5 Git: Ivan MichaelDocumento68 pagineProblem 5 Git: Ivan MichaelCunCunAlAndraNessuna valutazione finora
- RCOG Guidelines - Gestational Trophoblastic DiseaseDocumento12 pagineRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- RCOG Guidelines - Gestational Trophoblastic DiseaseDocumento12 pagineRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- Pitri - GI.Pemicu 4. GE+ Tifus AbdominalisDocumento154 paginePitri - GI.Pemicu 4. GE+ Tifus AbdominalisCunCunAlAndraNessuna valutazione finora
- MAPAX1Documento2 pagineMAPAX1CunCunAlAndraNessuna valutazione finora
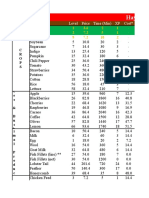
- Hay Day Price Profit AnalysisDocumento112 pagineHay Day Price Profit AnalysisCunCunAlAndraNessuna valutazione finora
- Hay Day Price Profit AnalysisDocumento112 pagineHay Day Price Profit AnalysisCunCunAlAndraNessuna valutazione finora
- Hay Day Price Profit AnalysisDocumento112 pagineHay Day Price Profit AnalysisCunCunAlAndraNessuna valutazione finora
- Excretion and Homeostasis.Documento70 pagineExcretion and Homeostasis.philomenanjuguna72Nessuna valutazione finora
- Cardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionDocumento7 pagineCardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionGuilherme LimaNessuna valutazione finora
- Obstructed LabourDocumento24 pagineObstructed LabourNatukunda Dianah50% (4)
- Assessment, Northwick ParkDocumento2 pagineAssessment, Northwick ParkMelian Anita100% (1)
- September 26, 2018 by Sagar Aryal: Antigen-Properties, Types and Determinants of AntigenicityDocumento23 pagineSeptember 26, 2018 by Sagar Aryal: Antigen-Properties, Types and Determinants of AntigenicityEzekiel GantiedNessuna valutazione finora
- Presentation List Language Disorders in ChildrenDocumento3 paginePresentation List Language Disorders in Childrenramandeep kaurNessuna valutazione finora
- Low Cost Thermal Camera For Use in Preclinical Detection of Diabetic PeripheralDocumento8 pagineLow Cost Thermal Camera For Use in Preclinical Detection of Diabetic PeripheralEDGAR ISMAEL REYES DEZANessuna valutazione finora
- Preoperative Assessment, Premedication & Perioperative DocumentationDocumento18 paginePreoperative Assessment, Premedication & Perioperative DocumentationOxy GenNessuna valutazione finora
- ReferensiDocumento2 pagineReferensiYuanita RosalinaNessuna valutazione finora
- Knowledge Regarding Immunization Among Mothers of Under Five ChildrenDocumento3 pagineKnowledge Regarding Immunization Among Mothers of Under Five ChildrenEditor IJTSRDNessuna valutazione finora
- Abreviaciones ChatDocumento4 pagineAbreviaciones ChatrojarodNessuna valutazione finora
- Bile Esculine TestDocumento2 pagineBile Esculine TestVincent OngNessuna valutazione finora
- Excel Dentistry 3rd Year Sample 2022Documento25 pagineExcel Dentistry 3rd Year Sample 2022Mohammed hisham khanNessuna valutazione finora
- Pembahasan CBT COMBO 3Documento802 paginePembahasan CBT COMBO 3Sari Dewi WiratsihNessuna valutazione finora
- Full Download Test Bank For Essentials of Genetics 8th Edition by Klug PDF Full ChapterDocumento36 pagineFull Download Test Bank For Essentials of Genetics 8th Edition by Klug PDF Full Chapterfencingvesper9dgb04100% (17)
- A Drug Study On PrednisoneDocumento5 pagineA Drug Study On PrednisonePrincess Alane MorenoNessuna valutazione finora
- Pediatrics - Hesi Practice ExamDocumento10 paginePediatrics - Hesi Practice ExamWizzardNessuna valutazione finora
- PEDIA Nursing NCLEX Bullets Part 1Documento166 paginePEDIA Nursing NCLEX Bullets Part 1Russel Myron Adriano AdvinculaNessuna valutazione finora
- Questions and Answers 1Documento7 pagineQuestions and Answers 1api-382372564Nessuna valutazione finora
- Surgery MCQDocumento24 pagineSurgery MCQMoiz Khan88% (8)
- Cardiac PanelDocumento6 pagineCardiac Panellinjinxian444Nessuna valutazione finora
- Seminar On: Organisation and Management of Neonatal Services and NicuDocumento27 pagineSeminar On: Organisation and Management of Neonatal Services and NicuDimple SweetbabyNessuna valutazione finora
- Black SeedDocumento26 pagineBlack SeedAslam Aly Saib100% (1)
- Nu 712 Health DisparitiesDocumento5 pagineNu 712 Health Disparitiesapi-555218722Nessuna valutazione finora
- ECGC PO Descriptive BookDocumento74 pagineECGC PO Descriptive BookAmar Pandey100% (2)
- A Proposed Pediatric Medical Center Research ThesisDocumento3 pagineA Proposed Pediatric Medical Center Research ThesisMarielle AbanteNessuna valutazione finora
- Employers Guide - InteractiveDocumento24 pagineEmployers Guide - Interactiveapi-285398586Nessuna valutazione finora
- Budget Justification Fy2021Documento418 pagineBudget Justification Fy2021Lisa FabianNessuna valutazione finora
- The Nurse Leader's Role: Crisis ManagementDocumento3 pagineThe Nurse Leader's Role: Crisis Managementravsab GaikwadNessuna valutazione finora
- FM - Hse.020 Statistik HSE TahunanDocumento2 pagineFM - Hse.020 Statistik HSE TahunanEka Nanda HermarianyNessuna valutazione finora