Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Recent Advances in The Pathogenesis and Treatment of Osteoporosis
Caricato da
Anil JohnTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Recent Advances in The Pathogenesis and Treatment of Osteoporosis
Caricato da
Anil JohnCopyright:
Formati disponibili
HORIZONS IN MEDICINE Clinical Medicine 2016 Vol 16, No 4: 360–4
Recent advances in the pathogenesis and treatment
of osteoporosis
Authors: Elizabeth M Curtis, A Rebecca J Moon,B Elaine M Dennison,C Nicholas C HarveyD and Cyrus CooperE
Over recent decades, the perception of osteoporosis has and propensity to fracture. Worldwide, there are nearly 9
ABSTRACT
changed from that of an inevitable consequence of ageing, to million osteoporotic fractures each year, and the US Surgeon
that of a well characterised and treatable chronic non-commu- General's report of 2004, consistent with data from the UK,
nicable disease, with major impacts on individuals, healthcare suggested that almost one in two women and one in five men
systems and societies. Characterisation of its pathophysiol- will experience a fracture in their remaining lifetime from
ogy from the hierarchical structure of bone and the role of its the age of 50 years.1 The cost of osteoporotic fracture in the
cell population, development of effective strategies for the UK approaches £3 billion annually and, across the EU, the
identification of those most appropriate for treatment, and estimated total economic cost of the approximately 3.5 million
an increasing armamentarium of efficacious pharmacologi- fragility fractures in 2010 was €37 billion.2 In this article we
cal therapies, have underpinned this evolution. Despite this review the pathogenesis of osteoporosis and approaches to
marked progress, individuals who experience a fragility fracture improving bone strength, aimed at reducing the immense
remain under-treated in many areas of the world, and there is burden of osteoporotic fracture.
substantial need for investment both in secondary and primary
prevention globally. In this brief article, we give an overview of Pathogenesis
the pathogenesis of osteoporosis, and summarise current and
future approaches to its assessment and treatment. Hierarchical structure
Fractures occur when the force applied to a bone exceeds its
KEYWORDS: osteoporosis, epidemiology, pathophysiology,
strength. A bone needs to be both stiff and flexible to resist
treatment, risk assessment, dxa
fracture, which is achieved through a hierarchical structure.
Collagen type-1 fibrils are wound in a triple helical structure,
linked together with non-collagenous proteins, which help to
Introduction prevent shearing. Hydroxyapatite crystals deposited on the
Osteoporosis is characterised by deterioration of bone mass collagen structure add strength, particularly in compression.
and microarchitecture, resulting in increased bone fragility Cross-linkage between collagen fibrils with non-collagenous
proteins is reduced in osteoporotic bone, leading to reduced
tensile strength.3 In addition, larger hydroxyapatite crystals are
found in osteoporosis, making bone more brittle and prone to
Authors: Aacademic clinical fellow, MRC Lifecourse Epidemiology fracture.4
Unit, University of Southampton, Southampton, UK; Bclinical
research fellow, MRC Lifecourse Epidemiology Unit, University of
Bone cells
Southampton, Southampton, UK, and Paediatric Endocrinology,
Southampton University Hospitals NHS Foundation Trust, Osteoblasts, osteocytes and osteoclasts are the three main
Southampton, UK; Cprofessor of musculoskeletal epidemiology, types of bone cells. Osteoblasts are bone forming and
MRC Lifecourse Epidemiology Unit, University of Southampton, may become embedded within bone mineral as mature
Southampton, UK; Dprofessor of rheumatology and clinical osteocytes (comprising 90–95% of the cells within bone)
epidemiology, MRC Lifecourse Epidemiology Unit, University or remain on the surface as bone-lining cells. Osteoclasts
of Southampton, Southampton, UK, and NIHR Southampton are multinucleated cells responsible for bone resorption.
Biomedical Research Centre, University of Southampton and Osteoblasts and osteoclasts work together in a coordinated
University Hospital Southampton NHS Foundation Trust, fashion at specific sites on the surface of trabecular or
Southampton, UK; Edirector and professor of rheumatology, cortical bone, forming ‘bone multicellular units’. During
MRC Lifecourse Epidemiology Unit, University of Southampton, bone formation, osteoblasts lay down new osteoid collagen
Southampton, UK, NIHR Southampton Biomedical Research Centre, matrix and over a period of weeks to months, crystals of
University of Southampton and University Hospital Southampton calcium hydroxyapatite form on the collagen fibrils. Bone is
NHS Foundation Trust, Southampton, UK, and NIHR Musculoskeletal laid down during growth and repair and through adaptation
Biomedical Research Unit, University of Oxford, Oxford, UK to mechanical loading in a process known as modelling.
360 © Royal College of Physicians 2016. All rights reserved.
CMJv16n4-Cooper.indd 360 14/07/16 4:53 PM
Pathogenesis and treatment of osteoporosis
Remodelling, in contrast, involves a cycle of resorption
Table 2. The spectrum of antifracture efficacy of
and formation of existing bone. Osteocytes play a key
role in the regulation of modelling and remodelling. The pharmacological interventions for osteoporosis.
arrangement of the osteocytes around Haversian canals acts Intervention Vertebral Non-vertebral Hip
as a mechanosensory system and allows communication Alendronate + + +
both directly between neighbouring osteocytes and through
the release of endocrine, paracrine and autocrine signalling Risedronate + + +
factors to other bone cells. The various pathways important Zoledronic acid + + +
to the regulation of osteoblast and osteoclast activity, such Etidronate + – –
as receptor activator of nuclear factor kappa B–receptor
activator of nuclear factor kappa B ligand (RANK–RANKL) Ibandronate + +* –
and Wnt signalling, are increasingly recognised as targets for Raloxifene + – –
anti-osteoporosis agents. Strontium ranelate + + +*
Teriparatide + + –
Changes in bone structure across the life course
Denosumab + + +
The balance of formation and resorption has a critical influence *post hoc analysis in a subset of patients.
on bone mass and strength throughout life. There is a positive
balance during childhood until achievement of peak bone mass
in early adulthood,5 with a subsequent period of stability and
then a negative balance in older age, with osteoclast activity Clinical risk factors
greater than osteoblast activity, leading to bone loss. In women, There are many factors that influence fracture risk, either
this process is accelerated after the menopause. At the level of the through bone mineral density (BMD) or through independent
whole bone, the cellular mechanisms and associated influences mechanisms. These include age, glucocorticoid therapy, a
result in differences in structure between males and females, previous personal history of fracture, a family history of hip
and alterations with advancing age. Males typically have a fracture, current smoking practice, alcohol abuse and certain
larger bone cross-sectional area than females, and in addition diseases associated with osteoporosis eg rheumatoid arthritis,
there is a significant reduction in cortical thickness in females diabetes, osteogenesis imperfecta in adults, untreated long-
following the menopause, contributing to the well established standing hyperthyroidism, hypogonadism or premature
sex differences in fracture risk. The structure of the trabeculae menopause (<45 years), chronic malnutrition, malabsorption
differs between the sexes, with young women having fewer and and chronic liver disease. These are summarised in Table 1,
thinner trabeculae than young men, and a greater reduction in and have, in terms of risk assessment, been incorporated into
trabecular number in women as they age.6 In addition, cortical the FRAX® tool,8 a WHO supported initiative which uses risk
porosity increases at a faster rate in female ageing.7 factors, with or without BMD measurement, to estimate a
10-year probability of either hip fracture or major osteoporotic
Table 1. Risk factors for osteoporosis. fracture. FRAX® is by far the most commonly used such tool
Risk factors independent Risk factors dependent globally, covering 75% of the world's population, and may, as in
of BMD on BMD the UK, be linked to assessment algorithms to define thresholds
for intervention with treatment.9
Age Untreated hypogonadism,
premature menopause
Treatment of osteoporosis
Previous personal history of Malabsorption
fragility fracture Vitamin D and calcium supplementation
Maternal history of hip fracture Endocrine disease eg The role of vitamin D and calcium supplementation has been
– heritable influences hyperthyroidism much debated in recent years with numerous meta-analyses
Glucocorticoid therapy Chronic renal disease suggesting conflicting findings. A large UK randomised
controlled trial demonstrated that supplementation with either
Smoking Chronic liver disease
calcium, vitamin D or both for secondary fracture prevention
Alcohol intake ≥3 units/day Chronic obstructive pulmonary at the population level appeared ineffective,10 although
disease supplementation in high-risk settings where deficiencies are
Rheumatoid arthritis Immobility expected, for example in nursing homes, may be beneficial.11
A recent individual patient data meta-analysis demonstrated
Body mass index ≤19 kg/m2 Drugs eg androgen deprivation
that overall, there appeared to be a modest benefit for combined
therapy, aromatase inhibitors
vitamin D and calcium supplementation for hip fractures,
Falls total fractures and probably vertebral fractures, but that there
Caucasian was no benefit for vitamin D alone.12 Although there has been
Geography – latitudes furthest
discussion from one research group that excess calcium intake
from equator
may be associated with increased cardiovascular risk,13 this
has not been substantiated across many other studies. Indeed,
BMD = bone mineral density.
it is reassuring to note that a recent individual-patient-data
© Royal College of Physicians 2016. All rights reserved. 361
CMJv16n4-Cooper.indd 361 14/07/16 4:53 PM
Elizabeth M Curtis, Rebecca J Moon, Elaine M Dennison et al
meta-analysis of the anti-fracture studies suggests that calcium for myocardial infarction: 1.6), in addition to the previously
and vitamin D supplementation in combination is associated known risk of venous thromboembolism (VTE). Therefore
with an improvement in mortality, which is not observed its use is now restricted to treatment of severe osteoporosis
with vitamin D supplementation alone.14 Almost all of the in postmenopausal women with high risk of fracture and in
randomised control trial evidence for the efficacy of anti- men at increased risk of fracture, but with no cardiovascular
osteoporosis drugs comes from patients who were prescribed or cerebrovascular disease. However, within this selected
concomitant calcium and vitamin D supplementation; both group of patients, particularly now that many individuals have
should therefore usually be prescribed adjunctively with undergone long-term bisphosphonate treatment, strontium
treatment for osteoporosis. ranelate does still offer a useful alternative.17
Bisphosphonates Selective oestrogen receptor modulators – raloxifene
Bisphosphonates are synthetic analogues of the naturally Raloxifene is a selective oestrogen receptor modulator that
occurring compound pyrophosphate and bind strongly to has antiresorptive oestrogenic effects on the skeleton without
hydroxyapatite, inhibiting bone resorption by inactivating the unwanted risks of oestrogen in the breast. Its use is also
osteoclasts. The most commonly prescribed oral associated with a significant decrease in the risk of breast
bisphosphonate is alendronate. If taken properly (in the cancer. It has been shown to be effective in preventing post-
morning with a glass of water, 45 minutes before food, drink or menopausal bone loss and in preventing vertebral fractures.
other medications and remaining upright for 30–60 minutes However there is no evidence that raloxifene prevents hip or
after the dose), upper GI side effects are uncommon. However, non-vertebral fractures.18 Adverse effects include leg oedema,
for those who are unable to tolerate oral bisphosphonates, or cramps, hot flushes and a two- to three-fold increase in the risk
in whom they are contraindicated (for example malabsorption of VTE.
or dysphagia), then an intravenous bisphosphonate, such as
zoledronate (given yearly in a dose of 5 mg by infusion over a Teriparatide
minimum of 15 minutes) is an alternative.
Teriparatide (recombinant human 1–34 parathyroid-hormone
peptide) is the only agent in current widespread use with truly
Denosumab
anabolic effects on bone. It is administered by subcutaneous
Denosumab, a fully humanised antibody to RANKL, is a injection in daily doses of 20 µg. It increases bone formation
newer antiresorptive agent. RANKL, secreted by osteoblasts, is and produces large increases in BMD, leading to approximately
a major activator of osteoclastic bone resorption and mimics 70% reduction in the incidence of new moderate or severe
the action of osteoprotegerin. Denosumab is administered as a vertebral fractures over 18 months of treatment, together
subcutaneous injection once every six months and its efficacy with reductions in non-vertebral fractures.19 Side effects are
has been demonstrated in patients with renal impairment, uncommon but may include nausea, headache and dizziness;
although due consideration should be given to the possibility in addition, transient hypercalcaemia and hypercalciuria
of underlying renal bone disease in chronic kidney disease may occur. Studies have shown added benefit in combination
4–5. Three-year fracture data show a 68% reduction in treatments such as teriparatide plus denosumab or teriparatide
vertebral fracture and 40% reduction in hip fracture.15 Side plus zoledronate,20 although such approaches are not yet
effects are uncommon, and may rarely include skin infections, approved clinically in the UK, and use of teriparatide in the UK
predominantly cellulitis. This is not typically seen at the is currently limited to those older patients at highest fracture
injection site and may be secondary to an immunomodulatory risk and who may have failed other therapies.
effect of the drug. Hypocalcaemia can also be a risk,
particularly if the patient is vitamin D deficient, or has renal Adverse effects and duration of therapy
impairment.
Atypical femoral factures of the subtrochanteric region
and femoral shaft may also rarely occur in patients taking
Strontium ranelate
bisphosphonates or denosumab. These are usually located
Strontium, an element directly below calcium in group 2 of in the lateral cortex around which endosteal thickening may
the periodic table, is combined with ranelic acid as a carrier be observed prior to fracture occurrence. Individuals may
to form strontium ranelate. It is taken as a single daily oral have prodromal pain and fractures typically are transverse,
dose. Its mechanism of action remains a subject of research, sometimes bilateral and occur after minimal trauma. Although
but there is evidence that it increases bone strength by altering these fractures can occur in bisphosphonate-/denosumab-naïve
bone material properties. Administration of strontium individuals, they appear more commonly in patients taking
ranelate leads to a substantial increase in BMD at the spine these therapies for a prolonged duration. It is thought that the
and hip, though part of this increase is artefactual, due to reason for this increased incidence is related to oversuppression
incorporation of strontium (which has a greater atomic weight of bone turnover. Overall, the fractures prevented greatly
than calcium) into bone. Studies have shown a 36% relative outnumber those atypical events potentially resulting from
risk reduction in hip fracture over three years in osteoporotic medication.21 Osteonecrosis of the jaw is extremely rarely
patients.16 In 2013 a Medicines and Healthcare Products observed during therapy for osteoporosis (as low as 1/100,000/
Regulatory Agency warning on strontium ranelate was issued year for individuals on oral bisphosphonates),22 but appears
due to increased risk of cardiovascular disorders (relative risk more commonly when higher doses of bisphosphonates are
362 © Royal College of Physicians 2016. All rights reserved.
CMJv16n4-Cooper.indd 362 14/07/16 4:53 PM
Pathogenesis and treatment of osteoporosis
given intravenously for treatment of bone metastases. A Conclusion
causal link to bisphosphonates is unproven but international
guidance suggests a prudent approach, encouraging patients In recent decades, our understanding of the pathogenesis of
to maintain good oral hygiene and have regular dental visits, osteoporosis has dramatically increased, with development of a
with invasive dental work performed before commencement of wide range of effective pharmaceutical approaches to fracture
bisphosphonate or denosumab therapy.23 prevention. Given the enormous prevalence of osteoporosis, and
Current UK guidance has therefore moved towards a frequency and burden of resulting fragility fractures, one of the
reassessment of the need for treatment after three years of key concerns going forward remains the optimal identification of
intravenous bisphosphonate/subcutaneous denosumab, and those requiring treatment.27 The tools for fracture risk assessment
five years of oral bisphosphonate.9 For high-risk patients, are widely available, in the form of the FRAX® calculator, and
continuation of treatment is usually warranted, but where there new medications are undergoing testing. It is vital that awareness
have been no incident fractures and BMD has improved, a of osteoporosis is promoted among all health professionals, in
period without treatment may be recommended. order to ensure closure of the so-called ‘treatment gap’, and with
a consequent reduction in the burden of osteoporotic fracture for
Novel therapies individuals, healthcare systems and societies. ■
Cathepsin-K inhibitors
Acknowledgements
Odanacatib is a once weekly oral treatment for osteoporosis in We would like to thank Medical Research Council (UK), Arthritis
which phase-III clinical trials have recently been performed. Research UK, National Osteoporosis Society (UK), International
It inhibits cathepsin-K, a cysteine protease expressed in Osteoporosis Foundation and NIHR for supporting this work.
osteoclasts which degrades type-1 collagen. In postmenopausal
women with low BMD, 24 months of treatment with odanacatib
was shown to produce increases in lumbar spine and total-hip Note
BMD by 5.5% and 3.2%, respectively, whereas BMD at these This article was originally published in the 2015 Clinical Medicine
sites was essentially unchanged with placebo (−0.2% and supplement Horizons in Medicine 27. All articles in this supplement
−0.9%).24 However, later trial outcomes also demonstrated a are available at www.clinmed.rcpjournal.org/content/15/Suppl_6
possible increase in cerebrovascular events, which has led to a
delay in FDA approval while outcomes are further adjudicated. References
1 van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology
Anti-sclerostin antibodies
of fractures in England and Wales. Bone 2001;29:517–22.
Sclerostin, an osteocyte-secreted protein, negatively regulates 2 Hernlund E, Svedbom A, Ivergard M et al. Osteoporosis in the
osteoblasts and inhibits bone formation through the low- European Union: medical management, epidemiology and economic
density lipoprotein receptor-related protein 5 (LRP5)/ burden : A report prepared in collaboration with the International
Wnt signalling pathway. The role of sclerostin in bone Osteoporosis Foundation (IOF) and the European Federation of
Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos
mass homeostasis was highlighted by the finding that two
2013;8:136.
rare high-bone-mass diseases, van Buchem disease and 3 Saito M, Marumo K. Collagen cross-links as a determinant of bone
sclerostosis have been linked to inactivating mutations in the quality: a possible explanation for bone fragility in aging, osteopo-
sclerostin gene. A monoclonal antibody against sclerostin, rosis, and diabetes mellitus. Osteoporos Int 2010;21:195–214.
romosozumab, was administered intravenously to healthy men 4 Boskey A. Bone mineral crystal size. Osteoporos Int 2003;14 Suppl
and postmenopausal women and was shown to increase bone- 5:S16–20; discussion S-1.
formation markers, along with a dose-related decrease in bone- 5 Hernandez CJ, Beaupre GS, Carter DR. A theoretical analysis of
resorption markers. Statistically significant increases in BMD the relative influences of peak BMD, age-related bone loss and
of up to 5.3% at the lumbar spine and 2.8% at the total hip menopause on the development of osteoporosis. Osteoporos Int
compared with placebo were observed on day 85 of treatment.25 2003;14:843–7.
6 Macdonald HM, Nishiyama KK, Kang J et al. Age-related patterns of
A randomised, double-blind, placebo-controlled multicentre
trabecular and cortical bone loss differ between sexes and skeletal sites:
phase-II clinical trial of a second agent, blosozumab (a a population-based HR-pQCT study. J Bone Miner Res 2011;26:50–62.
humanised monoclonal antibody targeted against sclerostin), 7 Zebaze RM, Ghasem-Zadeh A, Bohte A et al. Intracortical remodel-
demonstrated statistically significant dose-related increases ling and porosity in the distal radius and post-mortem femurs of
in spine, femoral neck and total hip BMD as compared with women: a cross-sectional study. Lancet 2010;375:1729–36.
placebo. In the highest dose group, BMD increases from 8 Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and
baseline reached 17.7% at the spine, and 6.2% at the total hip. the assessment of fracture probability in men and women from the
Biochemical markers of bone formation also increased during UK. Osteoporos Int 2008;19:385–97.
blosozumab treatment, while resorption markers decreased.26 9 Compston J, Bowring C, Cooper A et al. Diagnosis and manage-
These findings present promise for future use of anti-sclerostin ment of osteoporosis in postmenopausal women and older men in
the UK: National Osteoporosis Guideline Group (NOGG) update
antibodies as anabolic osteoporosis therapies. Other potential
2013. Maturitas 2013;75:392–6.
areas for investigation include new selective oestrogen receptor 10 Grant AM, Avenell A, Campbell MK et al. Oral vitamin D3 and
or androgen receptor modulators, calcilytics (calcium receptor calcium for secondary prevention of low-trauma fractures in
antagonists), the nitric oxide pathway and interventions aimed elderly people (Randomised Evaluation of Calcium Or vitamin
at sarcopenia, in what is an exciting and rapidly changing field of D, RECORD): a randomised placebo-controlled trial. Lancet
osteoporosis treatment and fracture prevention. 2005;365:1621–8.
© Royal College of Physicians 2016. All rights reserved. 363
CMJv16n4-Cooper.indd 363 14/07/16 4:53 PM
Elizabeth M Curtis, Rebecca J Moon, Elaine M Dennison et al
11 Chapuy MC, Pamphile R, Paris E et al. Combined calcium and 20 Tsai JN, Uihlein AV, Lee H et al. Teriparatide and denosumab, alone
vitamin D3 supplementation in elderly women: confirmation of or combined, in women with postmenopausal osteoporosis: the
reversal of secondary hyperparathyroidism and hip fracture risk: DATA study randomised trial. Lancet 2013;382:50–6.
the Decalyos II study. Osteoporos Int 2002;13:257–64. 21 Shane E, Burr D, Abrahamsen B et al. Atypical subtrochanteric and
12 DIPART (Vitamin D Individual Patient Analysis of Randomized diaphyseal femoral fractures: second report of a task force of the
Trials) Group. Patient level pooled analysis of 68 500 patients from American Society for Bone and Mineral Research. J Bone Miner Res
seven major vitamin D fracture trials in US and Europe. BMJ 2014;29:1–23.
2010;340:b5463. 22 Khan AA, Morrison A, Hanley DA et al. Diagnosis and management
13 Bolland MJ, Avenell A, Baron JA et al. Effect of calcium supple- of osteonecrosis of the jaw: a systematic review and international
ments on risk of myocardial infarction and cardiovascular events: consensus. J Bone Miner Res 2015;30:3–23.
meta-analysis. BMJ 2010;341:c3691. 23 Khosla S, Burr D, Cauley J et al. Bisphosphonate-associated oste-
14 Rejnmark L, Avenell A, Masud T et al. Vitamin D with calcium onecrosis of the jaw: report of a task force of the American Society
reduces mortality: patient level pooled analysis of 70528 patients for Bone and Mineral Research. J Bone Miner Res 2007;22:1479–91.
from eight major vitamin D trials. J Clin Endocrinol Metab 24 Bone HG, McClung MR, Roux C et al. Odanacatib, a cathepsin-K
2012;97:2670–81. inhibitor for osteoporosis: A two-year study in postmenopausal
15 Cummings SR, Martin JS, McClung MR et al. Denosumab women with low bone density. J Bone Miner Res 2010;25:937–47.
for Prevention of Fractures in Postmenopausal Women with 25 Padhi D, Jang G, Stouch B et al. Single-dose, placebo-controlled,
Osteoporosis. N Engl J Med 2009;361:756–65. randomized study of AMG 785, a sclerostin monoclonal antibody.
16 Reginster JY, Seeman Vernejoul MCD E et al. Strontium ranelate J Bone Miner Res 2011;26:19–26.
reduces the risk of nonvertebral fractures in postmenopausal 26 Recker RR, Benson CT, Matsumoto T et al. A randomized, double-
women with osteoporosis: treatment of peripheral osteoporosis blind phase 2 clinical trial of blosozumab, a sclerostin antibody,
(TROPOS) study. J Clin Endocrinol Metab 2005;90:2816–22. in postmenopausal women with low bone mineral density. J Bone
17 Reginster JY, Brandi ML, Cannata-Andia J et al. The position Miner Res 2015;30:216–24.
of strontium ranelate in today's management of osteoporosis. 27 Kanis JA, Svedbom A, Harvey N, McCloskey EV. The osteoporosis
Osteoporos Int 2015;26:1667–71. treatment gap. J Bone Miner Res 2014;29:1926–8.
18 Ettinger B, Black DM, Mitlak BH et al. Reduction of vertebral
fracture risk in postmenopausal women with osteoporosis treated
with raloxifene: results from a 3-year randomized clinical trial.
JAMA 1999;282:637–45. Address for correspondence: Professor C Cooper, MRC
19 Neer RM, Arnaud CD, Zanchetta JR et al. Effect of parathyroid Lifecourse Epidemiology Unit, University of Southampton,
hormone (1-34) on fractures and bone mineral density in postmeno- Southampton General Hospital, Southampton SO16 6YD, UK.
pausal women with osteoporosis. N Engl J Med 2001;344:1434–41. Email: cc@mrc.soton.ac.uk
364 © Royal College of Physicians 2016. All rights reserved.
CMJv16n4-Cooper.indd 364 14/07/16 4:53 PM
Potrebbero piacerti anche
- Pathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDocumento15 paginePathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDeddy ZulkarnaenNessuna valutazione finora
- Maxilary Sinus Graft ArunDocumento181 pagineMaxilary Sinus Graft ArunJose Fernando Fragozo MendozaNessuna valutazione finora
- 1042 FullDocumento9 pagine1042 Fulloki harisandiNessuna valutazione finora
- Pathophysiology of Bone MetastasesDocumento5 paginePathophysiology of Bone MetastasesdyahNessuna valutazione finora
- Osseteointegration of Dental ImplantDocumento24 pagineOsseteointegration of Dental ImplantFajar Kusuma Dwi KurniawanNessuna valutazione finora
- The Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationDocumento12 pagineThe Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationBrenda MartinsNessuna valutazione finora
- JCM 11 06434 v2Documento17 pagineJCM 11 06434 v2NeelamNessuna valutazione finora
- Maxillary Sinus Bone GraftingDocumento181 pagineMaxillary Sinus Bone GraftingTuấn Hành TrầnNessuna valutazione finora
- Mechanisms of Bone Metastasis Roodman GDDocumento10 pagineMechanisms of Bone Metastasis Roodman GDKresensiaNessuna valutazione finora
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocumento17 pagineA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNessuna valutazione finora
- Osteoporosis The Evolution in DiagnosisDocumento12 pagineOsteoporosis The Evolution in DiagnosisPakistan RevolutionNessuna valutazione finora
- Bone Grafts and Their SubstitutesDocumento4 pagineBone Grafts and Their SubstitutesIndriastuti SoetomoNessuna valutazione finora
- BP MecanismDocumento14 pagineBP MecanismAdryana StefyNessuna valutazione finora
- Bonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonDocumento19 pagineBonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonJason LeeNessuna valutazione finora
- Death&Birth 00Documento23 pagineDeath&Birth 00kyz79Nessuna valutazione finora
- CGJ 18 29Documento7 pagineCGJ 18 29ZenithaMeidaNessuna valutazione finora
- HHS Public AccessDocumento30 pagineHHS Public AccessAni RusNessuna valutazione finora
- Iannitti Et Al., 2012 BPSDocumento19 pagineIannitti Et Al., 2012 BPSTommaso IannittiNessuna valutazione finora
- HHS Public Access: The Potential of Probiotics As A Therapy For OsteoporosisDocumento26 pagineHHS Public Access: The Potential of Probiotics As A Therapy For OsteoporosisBagastyoNessuna valutazione finora
- OsteoporosisDocumento19 pagineOsteoporosisTsedhonNessuna valutazione finora
- Osteoporosis JunaidDocumento130 pagineOsteoporosis JunaidMohammed JunaidNessuna valutazione finora
- Bone Tissue EngineeringDocumento9 pagineBone Tissue EngineeringKevinNessuna valutazione finora
- Module 4 HomeworkDocumento4 pagineModule 4 HomeworkCj LinceNessuna valutazione finora
- Osteoporosis: Chandraprakash D. Khedkar Gulab Dattarao KhedkarDocumento7 pagineOsteoporosis: Chandraprakash D. Khedkar Gulab Dattarao Khedkardafa bintangNessuna valutazione finora
- Capture The Fracture - Use of Bone Turnover MarkerDocumento7 pagineCapture The Fracture - Use of Bone Turnover MarkergusdeNessuna valutazione finora
- Update Osteoporosis Management (Listo)Documento18 pagineUpdate Osteoporosis Management (Listo)Jossie AcuñaNessuna valutazione finora
- Foc 2003 14 2 9Documento8 pagineFoc 2003 14 2 9Andy HongNessuna valutazione finora
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocumento13 paginePathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNessuna valutazione finora
- Alveolar Bone Loss: Mechanisms, Potential Therapeutic Targets, and InterventionsDocumento9 pagineAlveolar Bone Loss: Mechanisms, Potential Therapeutic Targets, and InterventionsDiamanta Yalomit CirsteaNessuna valutazione finora
- JAAOS - Volume 03 - Issue 01 January 1995Documento63 pagineJAAOS - Volume 03 - Issue 01 January 1995kenthepaNessuna valutazione finora
- Regulatory Pathways Revealing New Approaches2008Documento14 pagineRegulatory Pathways Revealing New Approaches2008Cami GutierrezNessuna valutazione finora
- Biomedicine & Pharmacotherapy: Zhou-Shan Tao, Wan-Shu Zhou, Hong-Guang Xu, Min YangDocumento11 pagineBiomedicine & Pharmacotherapy: Zhou-Shan Tao, Wan-Shu Zhou, Hong-Guang Xu, Min YangrosanaNessuna valutazione finora
- Thyroid Diseases and Bone HealthDocumento11 pagineThyroid Diseases and Bone Healthmiguel saba sabaNessuna valutazione finora
- Advances in Biology of Orthodontic Tooth Movement - A ReviewDocumento10 pagineAdvances in Biology of Orthodontic Tooth Movement - A ReviewMarwan AlareqiNessuna valutazione finora
- Thesis On Bone CancerDocumento5 pagineThesis On Bone Cancerkvpyqegld100% (2)
- AnimalmodelsDocumento10 pagineAnimalmodelsFalira MuthiaNessuna valutazione finora
- Elaine Dennison (Eds.) - Osteoporosis Treatment - A Clinical Overview (2021, Springer) (10.1007 - 978!3!030-78128-6) - Libgen - LiDocumento229 pagineElaine Dennison (Eds.) - Osteoporosis Treatment - A Clinical Overview (2021, Springer) (10.1007 - 978!3!030-78128-6) - Libgen - Liarber mulolliNessuna valutazione finora
- Factors of Bone Resorption of The Residual Ridge Ortman1962Documento12 pagineFactors of Bone Resorption of The Residual Ridge Ortman1962AbdelKhalek BouararaNessuna valutazione finora
- Bone DissertationDocumento5 pagineBone DissertationGhostWriterCollegePapersHartford100% (1)
- Biomechanics and Biomaterials in Orthopedic SurgeryDocumento11 pagineBiomechanics and Biomaterials in Orthopedic SurgeryManiventhan NachimuthuNessuna valutazione finora
- Research Paper On BonesDocumento5 pagineResearch Paper On Bonesvshyrpznd100% (1)
- LID201112052004Documento10 pagineLID201112052004Gia BảoNessuna valutazione finora
- 3.osteoporosis Fragility FXDocumento7 pagine3.osteoporosis Fragility FXThanawat SimaNessuna valutazione finora
- Gluco Induced OsteopDocumento13 pagineGluco Induced Osteopmatheus galvãoNessuna valutazione finora
- Week 12 Article 1 BrickleyDocumento16 pagineWeek 12 Article 1 BrickleyJean-Claude TissierNessuna valutazione finora
- 06 KnightDocumento5 pagine06 Knightcristina ArraisNessuna valutazione finora
- Guidelines For Diagnosis and Management of OsteoporosisDocumento17 pagineGuidelines For Diagnosis and Management of OsteoporosisVanessaCockerNessuna valutazione finora
- Craniofacial Bone Grafting Wolff's Law RevisitedDocumento13 pagineCraniofacial Bone Grafting Wolff's Law RevisitedR KNessuna valutazione finora
- Osteop Intl 07Documento9 pagineOsteop Intl 07szarysimbaNessuna valutazione finora
- Osteoporosis and Fracture 2329 9509 1000185Documento2 pagineOsteoporosis and Fracture 2329 9509 1000185Rezky PutriNessuna valutazione finora
- Journal of Orthopaedic Science: Hidenori Matsubara, Hiroyuki TsuchiyaDocumento8 pagineJournal of Orthopaedic Science: Hidenori Matsubara, Hiroyuki TsuchiyaNeta Aza MaineztNessuna valutazione finora
- Osteosarcopenia - Uma Nova Condição PropostaDocumento9 pagineOsteosarcopenia - Uma Nova Condição PropostaAfonsoNessuna valutazione finora
- 151 FullDocumento11 pagine151 FullIvo Baaron ZarkovNessuna valutazione finora
- Fimmu 13 1005665Documento14 pagineFimmu 13 1005665sopha seyhaNessuna valutazione finora
- Adipose Derived Stromal Cells For Skeletal Regenerative Medicine 2012Documento16 pagineAdipose Derived Stromal Cells For Skeletal Regenerative Medicine 2012m_nurul_aminNessuna valutazione finora
- Biology of Bone Formation, Fracture Healing, and Distraction OsteogenesisDocumento10 pagineBiology of Bone Formation, Fracture Healing, and Distraction OsteogenesisenviNessuna valutazione finora
- Capitulo Do Livro Bone BiologyDocumento15 pagineCapitulo Do Livro Bone BiologyLuiz Guilherme FiorinNessuna valutazione finora
- Nihms-1641529 Mechanisms of Bone Development and RepairDocumento41 pagineNihms-1641529 Mechanisms of Bone Development and Repairhennysusanto18Nessuna valutazione finora
- OsteoporosisDocumento12 pagineOsteoporosispolog.jm610Nessuna valutazione finora
- Escitalopram 2018Documento2 pagineEscitalopram 2018Anil JohnNessuna valutazione finora
- High Yield PsychiatryDocumento43 pagineHigh Yield Psychiatryconfusedmage91% (11)
- Al Liver Dis PDFDocumento7 pagineAl Liver Dis PDFAnil JohnNessuna valutazione finora
- Green Tea Health BenefitsDocumento13 pagineGreen Tea Health BenefitsAnil JohnNessuna valutazione finora
- Al Liver Dis PDFDocumento7 pagineAl Liver Dis PDFAnil JohnNessuna valutazione finora
- 4 Psychopharmacological Therapies & Nursing ImplicationsDocumento27 pagine4 Psychopharmacological Therapies & Nursing ImplicationsAnil JohnNessuna valutazione finora
- Al Liver Dis PDFDocumento7 pagineAl Liver Dis PDFAnil JohnNessuna valutazione finora
- CBT For JealouseyDocumento16 pagineCBT For JealouseyAnil John100% (1)
- CBT For JealouseyDocumento16 pagineCBT For JealouseyAnil John100% (1)
- AllergyDocumento5 pagineAllergyAnil JohnNessuna valutazione finora
- Mental HealthDocumento4 pagineMental HealthAnil JohnNessuna valutazione finora
- 138 144Documento7 pagine138 144Anil JohnNessuna valutazione finora
- AllergyDocumento5 pagineAllergyAnil JohnNessuna valutazione finora
- DM MXDocumento7 pagineDM MXAnil JohnNessuna valutazione finora
- ClaimApplication DisasterDocumento5 pagineClaimApplication DisasterAnil JohnNessuna valutazione finora
- AllergyDocumento5 pagineAllergyAnil JohnNessuna valutazione finora
- CBT For JealouseyDocumento16 pagineCBT For JealouseyAnil John100% (1)
- Cervical RadiculopathyDocumento181 pagineCervical RadiculopathyE=MC2100% (2)
- Agra HaraDocumento40 pagineAgra HaraAnil JohnNessuna valutazione finora
- Windows10 TutorialDocumento123 pagineWindows10 TutorialmarkoNessuna valutazione finora
- PHD Thesis On Coronary Artery DiseaseDocumento5 paginePHD Thesis On Coronary Artery Diseasebdg9hkj6100% (1)
- 07 RPM Chapter Feb 2021 V9 508 Clean FinalDocumento143 pagine07 RPM Chapter Feb 2021 V9 508 Clean FinalShubhamNessuna valutazione finora
- Seal of Good Local Governance For Barangay (SGLGB)Documento2 pagineSeal of Good Local Governance For Barangay (SGLGB)Ponciano AlveroNessuna valutazione finora
- Employees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationDocumento3 pagineEmployees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationSaikatNessuna valutazione finora
- Miranda Miracell NewDocumento2 pagineMiranda Miracell NewPablo FaldutiNessuna valutazione finora
- Segmentos Ica 2022 PDFDocumento9 pagineSegmentos Ica 2022 PDFRoberto RodríguezNessuna valutazione finora
- Extra Reading Comprehension Questions (Unit 1, Page 10) : Top Notch 3Documento13 pagineExtra Reading Comprehension Questions (Unit 1, Page 10) : Top Notch 3Michelle Wara Mamani TiconaNessuna valutazione finora
- Biobanking in The PhilippinesDocumento17 pagineBiobanking in The PhilippinesLeidi Chua BayudanNessuna valutazione finora
- Giving Injection &applying InfusionDocumento17 pagineGiving Injection &applying InfusionIsmaNessuna valutazione finora
- Fundamentals of Nursing Part 1Documento8 pagineFundamentals of Nursing Part 1Evergreen Verds100% (1)
- Applying 5S ProceduresDocumento70 pagineApplying 5S ProceduresSanta Best100% (3)
- Health Economics: Which of The Following Is Not A Reason For Increased Health Spending?Documento8 pagineHealth Economics: Which of The Following Is Not A Reason For Increased Health Spending?Arjun Aryal100% (1)
- Tuskegee ExperimentDocumento2 pagineTuskegee ExperimentAniya LewisNessuna valutazione finora
- Copper Toxicity ChecklistDocumento12 pagineCopper Toxicity ChecklistHenia Eden Florin100% (1)
- US Embassy List of HospitalsDocumento4 pagineUS Embassy List of HospitalsJay SorianoNessuna valutazione finora
- Purpose 1Documento4 paginePurpose 1Rizzah MagnoNessuna valutazione finora
- Application Form For Accreditation SPDocumento4 pagineApplication Form For Accreditation SPMyk Twentytwenty NBeyondNessuna valutazione finora
- A.offer D. Furniture: HumanDocumento5 pagineA.offer D. Furniture: Humansoyeondan bangtanNessuna valutazione finora
- Shofa Aji Setyoko (N101 12 051)Documento4 pagineShofa Aji Setyoko (N101 12 051)ShofaajiNessuna valutazione finora
- Conduct Effective Quantitative Risk Assessment (QRA) - StepsDocumento14 pagineConduct Effective Quantitative Risk Assessment (QRA) - Stepsamal118Nessuna valutazione finora
- Punjab General Industries Private Limited: Hazard Identification and Risk Assessment (HIRA)Documento9 paginePunjab General Industries Private Limited: Hazard Identification and Risk Assessment (HIRA)Rohit VishwakarmaNessuna valutazione finora
- Brochure Kombitroll2000 2064411Documento16 pagineBrochure Kombitroll2000 2064411Jmi AzimNessuna valutazione finora
- Safety Data Sheet For NEBNext End Prep Reaction BufferDocumento9 pagineSafety Data Sheet For NEBNext End Prep Reaction BufferNabilahNessuna valutazione finora
- L 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Documento56 pagineL 65 - Prevention of Fire and Explosion, and Emergency Response On Offshore Installations - Approved Code of Practice and Guidance - HSE - 2010Barkat UllahNessuna valutazione finora
- Common Causes of Paediatric Alopecia: EpidemiologyDocumento5 pagineCommon Causes of Paediatric Alopecia: EpidemiologyLiya SuwarniNessuna valutazione finora
- Shaukat Khanum Memorial Cancer Hospital & Research CentreDocumento2 pagineShaukat Khanum Memorial Cancer Hospital & Research CentreMa BeNessuna valutazione finora
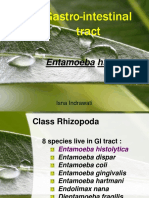
- Gastro-Intestinal Tract: Entamoeba HistolyticaDocumento25 pagineGastro-Intestinal Tract: Entamoeba Histolyticanh2411Nessuna valutazione finora
- Addis Ababa Science and Technology University (AASTU)Documento24 pagineAddis Ababa Science and Technology University (AASTU)Wasihun DanielNessuna valutazione finora
- Chlamydia SeminarDocumento110 pagineChlamydia Seminarsuvarnaramesh2007100% (1)
- Sharon Jones Amended ComplaintDocumento35 pagineSharon Jones Amended ComplaintMichael_Lee_RobertsNessuna valutazione finora