Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pathophysiology ARDS
Caricato da
Kim AmboyaDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pathophysiology ARDS
Caricato da
Kim AmboyaCopyright:
Formati disponibili
Pathophysiology
The pathophysiology of ARDS is complex and multifaceted. It may be considered as 3 distinct
components, which are the nature of the stimulus that initiates or causes ARDS, the host
response to this stimulus, and, finally, the role that iatrogenic damage plays in the progression
and outcome of this condition. There are 3 pathohistologic stages of ARDS which are further
discussed under histology.
An initiating stimulus leads to a cascade of effects, the most immediate of which is an increase
in alveolar and pulmonary capillary permeability. Protein-rich fluid engulfs the alveolus, activated
neutrophils and macrophages follow, and an inflammatory cascade is initiated. This cascade
involves the release of interleukins (ILs), tumor necrosis factor, and other inflammatory
mediators. Neutrophils release oxidants, leukotrienes, and various proteases. The net effect at a
cellular level is massive cell damage, alveolar denudation, and sloughing of cell debris into the
lumen of the alveolus. Furthermore, surfactant is markedly inactivated.
Meanwhile, in the pulmonary capillary, endothelial cells swell, platelets aggregate, and a
procoagulant cascade may arise, leading to small-vessel thrombosis. At a physiologic level, the
consequences of the reactions outlined above are myriad.
Surfactant depletion, alveolar flooding, cellular debris within the alveoli, and increased airway
resistance all lead to increased work of breathing. Surfactant loss leads to alveolar collapse
because of increased surface tension, which is analogous to the situation observed in
premature infants with infant RDS (IRDS). As alveoli collapse, closing lung volume decreases
below the patient's functional residual capacity (FRC), further increasing the work of breathing.
This is reflected as reduced compliance; that is, additional pressure is required to generate a
unit volume.
A widened interstitial space between the alveolus and the vascular endothelium decreases
oxygen-diffusing capacity. Hypoxia arises as a result of the change described above. Collapsed
alveoli result in either low ventilation-perfusion (V/Q) units or a right-to-left pulmonary shunt. The
end result is marked venous admixture, the process whereby deoxygenated blood passing
through the lungs does not absorb sufficient oxygen and causes a relative desaturation of
arterial blood when it mixes with blood that is oxygenated adequately. Hence, relatively
deoxygenated arterial blood attempts to supply respiratory muscles that are working harder than
usual. These muscles become fatigued; the body is unable to maintain such sustained work of
breathing, and respiratory failure ensues.
In addition, hypoxia, hypercarbia, and small-vessel thrombosis combine to elevate pulmonary
artery pressures, leading to increased right ventricular work, increased right ventricular filling,
and, ultimately, a septal shift toward the left ventricle. These changes, in turn, may decrease
cardiac output, further reducing oxygen delivery to the tissues.
Iatrogenic problems may further complicate the patient's clinical picture. High-inspired oxygen
concentration (FiO2>95%) may cause absorption atelectasis, further reducing the number of
patent alveoli. Oxygen toxicity can be seen with FiO2 more than 60% over time, leading to
additional inflammation secondary to free radical damage.
High mean airway pressures during attempts to maintain adequate oxygenation and ventilation
may decrease cardiac output. In addition, high peak airway pressures may cause air leaks (eg,
pneumothoraces), which may acutely compromise cardiac and respiratory function. Ventilator-
induced lung injury (VILI), discussed in detail below, may further complicate and accelerate
disease progression.
Finally, fluid resuscitation may lead to further alveolar and pulmonary interstitial flooding, with
worsening compliance and oxygenation.
Potrebbero piacerti anche
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Acute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandAcute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
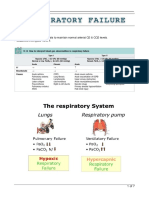
- Acute Respiratory Failure For StudentDocumento41 pagineAcute Respiratory Failure For Studentapi-379952350% (4)
- ARDSDocumento57 pagineARDSnesjohnvNessuna valutazione finora
- Pulmonary CirculationDocumento4 paginePulmonary CirculationDr Md Abedur RahmanNessuna valutazione finora
- Pulmonary EmbolismDocumento8 paginePulmonary EmbolismspoilttbrattNessuna valutazione finora
- Pulmonary EmbolismDocumento21 paginePulmonary EmbolismMadhu Bala100% (2)
- Managing COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskDocumento2 pagineManaging COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskAl RizkyNessuna valutazione finora
- CopdDocumento60 pagineCopdRizqy Shofianingrum100% (1)
- Cardiac Fluid ManagementDocumento9 pagineCardiac Fluid ManagementroseasNessuna valutazione finora
- Acute Respiratory Distress SyndromeDocumento3 pagineAcute Respiratory Distress Syndromekarenkaren09Nessuna valutazione finora
- Nursing Care Plans For Activity IntoleranceDocumento3 pagineNursing Care Plans For Activity Intoleranceravenshadow100% (2)
- Bronchiectasis PathophysiologyDocumento1 paginaBronchiectasis PathophysiologyRayne Dunstan Pascual VergaraNessuna valutazione finora
- Women's Pneumonia ReportDocumento9 pagineWomen's Pneumonia ReportNohaira SADANGNessuna valutazione finora
- PneumoniaDocumento71 paginePneumoniafrancis00090100% (1)
- BRONCHIECTASISDocumento36 pagineBRONCHIECTASISNishanth ReddyNessuna valutazione finora
- Case Study - EmphysemaDocumento6 pagineCase Study - Emphysemamackie_041992Nessuna valutazione finora
- COPD Nursing Care GuideDocumento16 pagineCOPD Nursing Care GuideJay-ar Zars0% (1)
- Renal Dialysis PeritonealDocumento7 pagineRenal Dialysis Peritonealmardsz100% (2)
- 13.acute Respiratory FailureDocumento34 pagine13.acute Respiratory Failurekarim hassan100% (1)
- Cor Pulmonale Lesson PlanDocumento49 pagineCor Pulmonale Lesson PlanRadha Sri50% (2)
- Acute Respiratory Distress Syndrome (Ards)Documento12 pagineAcute Respiratory Distress Syndrome (Ards)Vin Grace Tiqui - GuzmanNessuna valutazione finora
- Tension Pneumothorax: Modifiable FactorsDocumento3 pagineTension Pneumothorax: Modifiable FactorsJustin MaverickNessuna valutazione finora
- 2 NCP Chronic Heart FailureDocumento5 pagine2 NCP Chronic Heart FailureLovely CacapitNessuna valutazione finora
- Pathophysiology of COPD - The BasicsDocumento11 paginePathophysiology of COPD - The BasicstiaranindyNessuna valutazione finora
- Pleurisy (Pleuritis): Causes, Symptoms, Tests and TreatmentDocumento17 paginePleurisy (Pleuritis): Causes, Symptoms, Tests and TreatmentkamilahfernandezNessuna valutazione finora
- Management of ARDSDocumento57 pagineManagement of ARDSRajaNessuna valutazione finora
- Acute Respiratory Distress SyndromeDocumento30 pagineAcute Respiratory Distress SyndromeNikhil GhubadeNessuna valutazione finora
- Respiratory AcidosisDocumento16 pagineRespiratory AcidosisIssa GutierrezNessuna valutazione finora
- COPD NotesDocumento4 pagineCOPD NotesjisooNessuna valutazione finora
- Understanding the Pathophysiology of Coronary Artery DiseaseDocumento14 pagineUnderstanding the Pathophysiology of Coronary Artery DiseasejohnhenryvNessuna valutazione finora
- Congestive Heart FailureDocumento25 pagineCongestive Heart FailuredevianiamalinaNessuna valutazione finora
- Respiratory FailureDocumento16 pagineRespiratory FailurealzaabiBMNessuna valutazione finora
- Pathophysiology ARDSDocumento1 paginaPathophysiology ARDSRoderick Agbuya100% (1)
- Lung abscess diagnosis and treatmentDocumento25 pagineLung abscess diagnosis and treatmentIskandar HasanNessuna valutazione finora
- Bronchiectasis: By: Karunesh KumarDocumento21 pagineBronchiectasis: By: Karunesh KumarAnkan DeyNessuna valutazione finora
- ARDSDocumento27 pagineARDSChloie Marie RosalejosNessuna valutazione finora
- HSNS264 A1 COPDDocumento2 pagineHSNS264 A1 COPDKC Nilam100% (1)
- Acute Respiratory Distress SyndromeDocumento17 pagineAcute Respiratory Distress SyndromeSanjeet SahNessuna valutazione finora
- Pneumonia Case Study: Toddler Diagnosis and TreatmentDocumento5 paginePneumonia Case Study: Toddler Diagnosis and TreatmentcrisolandNessuna valutazione finora
- COPD: Epidemiology, Pathogenesis, & Pathophysiology: Wyatt E. Rousseau, MD May 11, 2006Documento50 pagineCOPD: Epidemiology, Pathogenesis, & Pathophysiology: Wyatt E. Rousseau, MD May 11, 2006Mahmmoud Fuqaha100% (1)
- PathophysiologyDocumento2 paginePathophysiologyKarla Karina Dela CruzNessuna valutazione finora
- Pulmonary EdemaDocumento14 paginePulmonary EdemaRizzamwah Catague100% (1)
- BronchiectasisDocumento69 pagineBronchiectasisienNessuna valutazione finora
- SinusitisDocumento6 pagineSinusitisRae Marie AquinoNessuna valutazione finora
- COPD and Asthma: Causes, Symptoms, Diagnosis and TreatmentDocumento138 pagineCOPD and Asthma: Causes, Symptoms, Diagnosis and TreatmentMonique Reyes0% (1)
- Pulmonary EmbolismDocumento80 paginePulmonary EmbolismVarun B Renukappa100% (1)
- Acute Respiratory Distress SyndromeDocumento36 pagineAcute Respiratory Distress Syndromedr9348345000Nessuna valutazione finora
- Acute Respiratory Distress Syndrome (Ards)Documento45 pagineAcute Respiratory Distress Syndrome (Ards)ukht marutu100% (1)
- 07.03.53 Mechanical VentilationDocumento5 pagine07.03.53 Mechanical VentilationSuganya BalachandranNessuna valutazione finora
- Acute Respiratory Distress Syndrome - PathophysiologyDocumento5 pagineAcute Respiratory Distress Syndrome - PathophysiologyJoann67% (3)
- Respiratory FailureDocumento7 pagineRespiratory FailureLulu100% (1)
- Acute Dyspnea First RevisionDocumento56 pagineAcute Dyspnea First RevisionAradhanaRamchandaniNessuna valutazione finora
- PneumothoraxDocumento52 paginePneumothoraxtrisna satrianaNessuna valutazione finora
- Pathophysiology of Septic ShockDocumento19 paginePathophysiology of Septic ShockRoberto López MataNessuna valutazione finora
- ARDS With PathophysiologyDocumento79 pagineARDS With Pathophysiologymabec pagaduan95% (19)
- Asthma: A. DefinitionDocumento6 pagineAsthma: A. DefinitionElvando SimatupangNessuna valutazione finora
- PBL Copd: 1) Mechanics of RespirationDocumento34 paginePBL Copd: 1) Mechanics of RespirationAhmadNessuna valutazione finora
- Prioritized Nursing Interventions for AtelectasisDocumento7 paginePrioritized Nursing Interventions for AtelectasisJinaan MahmudNessuna valutazione finora
- A Simple Guide to Cerebral Aneurysm, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Cerebral Aneurysm, Diagnosis, Treatment and Related ConditionsNessuna valutazione finora
- Medical Physics - RespiratoryDocumento9 pagineMedical Physics - RespiratoryAhmad wastiNessuna valutazione finora
- Literature Review On LeukemiaDocumento8 pagineLiterature Review On Leukemiaafdtukasg100% (2)
- ICSE X Biology Board Paper 2017 SolutionDocumento8 pagineICSE X Biology Board Paper 2017 SolutionKing YashasNessuna valutazione finora
- EAU Pocket Guideline 2021Documento525 pagineEAU Pocket Guideline 2021Maria Angelica Rodriguez100% (1)
- Illinois UniDocumento5 pagineIllinois UniMamato MarcelloNessuna valutazione finora
- MiconazoleDocumento3 pagineMiconazoleapi-3797941Nessuna valutazione finora
- 3rd Ed General Cheat Sheet PDFDocumento9 pagine3rd Ed General Cheat Sheet PDFAlan RideoutNessuna valutazione finora
- Alkalizing Nutritional Therapy in The Prevention and Treatment of Any Cancerous Condition by Robert Young Galina Migalko (Young, Robert Migalko, Galina)Documento51 pagineAlkalizing Nutritional Therapy in The Prevention and Treatment of Any Cancerous Condition by Robert Young Galina Migalko (Young, Robert Migalko, Galina)Maria S100% (1)
- Plasmid Curing of Escherichia Coli Cells With Ethidium BromideDocumento4 paginePlasmid Curing of Escherichia Coli Cells With Ethidium BromideLucasJ.LenziNessuna valutazione finora
- (English) About Your Heart Attack - Nucleus Health (DownSub - Com)Documento2 pagine(English) About Your Heart Attack - Nucleus Health (DownSub - Com)Ken Brian NasolNessuna valutazione finora
- Investigation of Blood Culture Using BACTEC SystemsDocumento36 pagineInvestigation of Blood Culture Using BACTEC SystemsGregorio De Las CasasNessuna valutazione finora
- Pediatric Doses For Commonly Used OTCsDocumento7 paginePediatric Doses For Commonly Used OTCsCharles Xavier KimNessuna valutazione finora
- Disease Prevention & Health PromotionDocumento21 pagineDisease Prevention & Health PromotionHajra MirzaNessuna valutazione finora
- 16 Stroke SyndromesDocumento32 pagine16 Stroke SyndromesRos Potter100% (2)
- SPD 200 RS Disability Comparison TemplateDocumento18 pagineSPD 200 RS Disability Comparison TemplateMUSYOKA KITUKUNessuna valutazione finora
- STROKE-pathophysiology, Diagnosis, and Management, 4th EditionDocumento3 pagineSTROKE-pathophysiology, Diagnosis, and Management, 4th EditionNishi RuciNessuna valutazione finora
- Monitored Anesthesia Care Notes Jag2007Documento49 pagineMonitored Anesthesia Care Notes Jag2007Suresh KumarNessuna valutazione finora
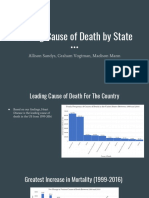
- Leading Cause of Death by State: Allison Sandys, Graham Vogtman, Madison MannDocumento10 pagineLeading Cause of Death by State: Allison Sandys, Graham Vogtman, Madison MannGrahamVogtmanNessuna valutazione finora
- DBQ FOCUS: Columbian Exchange: Document-Based Question FormatDocumento5 pagineDBQ FOCUS: Columbian Exchange: Document-Based Question Formatbaruc barranco50% (2)
- Cancer DiseaseDocumento7 pagineCancer Diseasenbs saraswathiNessuna valutazione finora
- Pityriasis AlbaDocumento6 paginePityriasis AlbaLee Eng SiangNessuna valutazione finora
- Lectura Adn MitocondrialDocumento13 pagineLectura Adn MitocondrialIvan Berrios VillegasNessuna valutazione finora
- June 2007-NPT 1 - RationaleDocumento15 pagineJune 2007-NPT 1 - Rationaleяoxel яayмoи eитяeиaNessuna valutazione finora
- Hypertension in PregnancyDocumento68 pagineHypertension in PregnancyAbdul MoizNessuna valutazione finora
- Hesi Hints Part 4Documento2 pagineHesi Hints Part 4Sharon TanveerNessuna valutazione finora
- The History of Extra Corporeal Membrane Oxygenation ECMO From StartDocumento230 pagineThe History of Extra Corporeal Membrane Oxygenation ECMO From StartFercho MedNessuna valutazione finora
- Emergency Department Triage Prediction Ofclinical Outcomes Using Machine Learning Models PDFDocumento13 pagineEmergency Department Triage Prediction Ofclinical Outcomes Using Machine Learning Models PDFOscar Julian Perdomo CharryNessuna valutazione finora
- Our Lady of Fatima UniversityDocumento5 pagineOur Lady of Fatima UniversityEmmanuel De LeonNessuna valutazione finora
- ToxicologyDocumento9 pagineToxicologyarnav15magicNessuna valutazione finora
- Acute Necrotizing PancreatitisDocumento37 pagineAcute Necrotizing PancreatitisVania SuSanchezNessuna valutazione finora