Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
7 Assessing The Motor Component of The GCS Scoring System PDF
Caricato da
Widya WidyariniTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
7 Assessing The Motor Component of The GCS Scoring System PDF
Caricato da
Widya WidyariniCopyright:
Formati disponibili
NATIONAL JOURNAL OF EMERGENCY MEDICINE
ASSESSING THE MOTOR COMPONENT OF THE GCS SCORING SYSTEM
AS A BETTER PREDICTOR OF OUTCOME
Meyei S Appachi*1, Mahadevan D2, Eswaran VP3
ABSTRACT Conclusions: The motor component of GCS scoring
Background: Components of the Glasgow Coma Scale system is a better predictor of 3 month outcome while
[GCS] alone are simpler and can predict outcome in TBI the GCS in its summed form is a better indicator for
and acute stroke [AS]. requirement of endotracheal intubation in TBI and AS.
Objectives: To assess whether motor component of the Keywords: Acute Stroke, Endotracheal intubation,
GCS on initial presentation is enough as a better predictor Glasgow coma scale, Outcome predictors, Traumatic
of outcome and better indicator of endotracheal brain injury.
intubation [ETI] in patients with TBI and AS. INTRODUCTION
Methods: Patients aged above 14 years diagnosed of The Glasgow Coma Scale [GCS] also known as the
having TBI and AS presenting within 24 hours were Glasgow Coma Score is a neurological scale which aims to
included. Patient's arrival GCS in Emergency Room and give a reliable, objective way of recording the conscious
GCS during ETI either on arrival or during course of state of a person, for initial as well as continuing
hospital stay were recorded. The outcomes were assessment (1). Teasdale and Jennett in 1974 wrote
determined in terms Glasgow Outcome Scale [GOS] at 3 Impaired consciousness is an expression of dysfunction
months and requirement of ETI. The ability of total GCS in the brain as a whole that may be due to agents acting
and its Components to predict outcome using receiver diffusely . . . or to the combination of remote and local
operating characteristic [ROC] analysis was carried out. effects produced by brain damage which was initially
Results: Of 375 patients, 68.8% were TBI and 31.2% were focal (2). The GCS is typically praised for its ease of use
AS. 65.1% of all patients had a good outcome at 3 months and has been used to grade individual levels of
and 45.1% was intubated. For outcome at 3 months, area consciousness, compare effectiveness of treatment, and
under curve [AUC] was greatest for motor component in as a prognostic indicator.
all patients [0.937] as well as in TBI [0.959]. But in AS, AUC GCS has enjoyed universal acceptance as an important
was greatest for total GCS [0.909] with similar magnitude standard tool for communication of mental status in both
for motor component [0.908]. Among AS, AUC was traumatized and non-traumatized patients, and in the
greatest for motor component in ischemic stroke [0.892] care of trauma patients (3, 4). It is incorporated into many
and greatest for total GCS [0.944] followed by motor scoring systems due to the ease and appeal of the GCS.
component [0.919] in haemorrhagic stroke. For GCS is used as part of several intensive care unit [ICU]
requirement of ETI, AUC was greatest for total GCS in all scoring systems, including Acute Physiology and Chronic
patients [0.977], TBI [0.982] and AS [0.967]. Among AS, Health Evaluation II [APACHE II], Simplified Acute
AUC was greatest for eye component [0.969] in ischemic Physiology Score II [SAPS II], and Sepsis-related Organ
stroke and greatest for total GCS [0.981] in haemorrhagic Failure Assessment [SOFA], to assess the status of the
stroke. central nervous system and is a component of the Trauma
1
Assistant Professor, Department of Accident, Emergency & Critical Care Medicine, Vinayaka Mission's Kirupananda Variyar Medical College & Hospitals,
Vinayaka Mission University, Sankari Main Road [NH-47], Veerapondi-Post, Salem-636308, Tamilnadu,India. Email: docmeyei@gmail.com
2
Associate Professor, Department of Neurology, Vinayaka Mission's Kirupananda Variyar Medical College & Hospitals,
Vinayaka Mission University, Sankari Main Road [NH-47], Veerapondi-Post, Salem-636308, Tamilnadu,India. Email: drdmahadevan@gmail.com
3
Prof of General Medicine, Academic Director Dept of Accident, Emergency & Critical Care Medicine, Vinayaka Mission's Kirupananda Variyar
Medical College & Hospitals, Vinayaka Mission University, Sankari Main Road [NH-47], Veerapondi-Post, Salem-636308, Tamilnadu,India.
Email: info@vinayakahospital.com mailto:drvpchandru@gmail.com
August - October 2012, Vol : 1, Issue : 1 41
NATIONAL JOURNAL OF EMERGENCY MEDICINE
and Injury Severity Score [TRISS], the Circulation, decisions and also helps in the efficient use of resources and
Respiration, Abdomen, Motor, Speech [CRAMS] Scale communicating with the families of the victims (17, 18).
and the Revised Trauma Score (1, 4, 5, 6). As stroke may cause localized motor, speech or language
Traumatic Brain Injuries [TBI] are a major public health deficits, the accuracy of GCS to measure the level of
problem in India, resulting in deaths, injuries and consciousness as well as its prognostic predictability may
disabilities of young and productive people of our society. be affected (3). Similarly in head injury, there could be
India has the rather unenviable distinction of having the inaccuracy in GCS measurement due to un-testable
highest rate of head injury in the world. In India, more components due to sedation paralysis, intubation,
than 100,000 lives are lost every year with over 1 million alcohol or illicit drug intoxication or in facial injury causing
suffering from serious head injuries and 1 out of 6 trauma periorbital swelling (19, 20, 21, 22).
victims die. Most road traffic accident victims are in the Simplicity of the GCS was the principle concern with the
20- to 40-year age group, the main bread-earners of the goal to provide a method to quantify and communicate
family, putting the whole family below the poverty line, with other members of the health care system describing
while depriving society of vital drivers of economy as in the degree of altered consciousness or coma (23, 24). The
many cases these are entrepreneurs or professionals (7). correct assessment of the GCS shows variability among
The economic losses to India are phenomenal, though health care providers and it is unnecessarily complex for
unmeasured. As India progresses to greater growth and the initial assessment in the out-of-hospital setting (3,
development in terms of motorization, urbanization, TBIs 25). The GCS is most often reported as a single and overall
would increase in India. By 2050, India would have the score, although the scale authors did not recommend the
greatest number of automobiles on the planet, summary score for use in clinical practice. The use of a
overtaking the United States (8). global summary score may result in a loss of information
Stroke is defined as a sudden loss of brain function that adversely affects the predictive accuracy of the GCS
resulting from an interference with blood supply to the (26, 27, 28).
brain. It limits stroke to an acute vascular phenomenon Various simplified scoring systems have been formulated
that includes ischemic strokes and haemorrhagic strokes to predict the outcome in TBI and stroke (3, 29). As the
(9). Brain stroke is the third largest killer in India and the motor response forms the major component of the GCS
second largest in the world, and the incidence in India is scoring system and due to the complexity of GCS, the
around 130 per 100,000 population every year according motor component alone could replace The Glasgow
to the World Health Organization (10). The last few Coma Scale in prediction of outcome in TBI and stroke.
decades have seen a rise in the incidence and prevalence Motor component is a simpler, quicker and easier
of stroke in India, attributable to increasing life span, method of measurement.
urbanization, and better survival, and the rates are now
The aim of this study is to assess the components of the
matching western figures (11).
GCS on initial presentation and to see if motor score
As a result of both TBI and Stroke, there is an increase in alone is enough as a better predictor of outcome and as a
mortality and long-term or lifelong disability that will better indicator of endotracheal intubation [ETI] in
need for help in performing activities of daily living (12). A patients with TBI and acute stroke [AS].
patient's condition during the first few weeks after a TBI is
MATERIALS AND METHODOLOGY
extremely unstable and life-threatening. During such
critical periods, accurate neurological assessment is Study Design:-
essential for predicting recovery (13). The GCS is a quick, The proposed study was submitted to the institutional
simple, and objective tool widely used and accepted review board of our hospital. Following approval we
prognostic score for both traumatic and non-traumatic performed a prospective observational study from
altered conscious level (14, 15, 16). The ability to predict October 2009 to July 2011.
the outcome in TBI and stroke can influence clinical
42 August - October 2012, Vol : 1, Issue : 1
NATIONAL JOURNAL OF EMERGENCY MEDICINE
Study Setting and Population:- assessed against the criteria of the scale and the resulting
Vinayaka Mission Hospitals is the one of the Level 1 points give a score between 3 being the lowest [worst]
trauma centers located in Salem, in the southern part of and 15 being the highest [best] score. The patient's best
India. The hospital has got a well equipped and initial summed GCS score as well as the GCS score that is
sophisticated thirty bedded emergency room with a good broken down in to components [eye, motor and verbal],
quantum of varied cases with agile emergency after fluid resuscitation and stabilization of the patient,
physicians, vigilant staff nurses and paramedics round are recorded by experienced emergency physician at the
the clock. The Emergency Department [ED] treats about time of arrival to the ED. The GCS score calculated by
5000 patients per year from a population of paramedics on the scene is not considered as it had no
approximately over thirty lakh inhabitants in an area of prognostic value (30). For AS patients presenting with
5200 square kilometers, 50% of the population live in an aphasia, the GCS verbal score is arbitrarily assigned as
urban environment. Our 450 bedded hospital treats 'one' (31). When assessing the motor sub-score, the best
more than 20,000 patients per year, with 3000 location for applying a painful stimulus is the nail bed and
admissions to intensive care units. the best response is recorded from either arm. For those
with more experience, supraorbital pressure was used as
All the patients aged above 14 years diagnosed of having
a painful stimulus (32).
TBI and AS presenting within 24 hours were included.
Patients who are intubated and/or sedated on Outcome Measures:-
presentation, patients with hypoxia [SpO2 < 92%], The main outcome considered in this study was
hypotension [Systolic Blood Pressure < 90 mm Hg], measurement of functional disability by the five-point
alcohol or illicit drug intoxication on presentation, Glasgow Outcome Scale [GOS] score at 3 months (33)
patients with bilateral orbital edema, traumatic paralysis [TABLE 2]. For ease of analysis and reporting, the five-
[high spinal cord injury], previous functional/cognitive point GOS score was modified into broader outcome
disabilities, causes of mortality other than TBI and AS, categories as good outcome [good recovery or moderate
and patients who are unable to be followed-up at 3 disability] and bad outcome [severe disability, persistent
months were excluded from the study. vegetative state or dead] (34, 35) [TABLE 3]. The follow up
Methods:- GOS was rated by an expert physician unaware of the
study protocol, on the basis of the response to a
All consecutive patients attending the ED of our Hospital
structured telephone call or neurological examination at
with TBI or AS included in the study were treated
3 months (36). Additionally, the requirement for ETI was
according to Advanced Trauma Life Support [ATLS] and
also assessed.
American Stroke Association [ASA] guidelines
respectively. Data collected on all patients on admission Data Analysis:-
included age, sex, GCS [eye, motor and verbal], vital signs, All data were compiled into Microsoft Excel 2007 spread
pupil size and response, time and cause of injury, and sheet and statistical analysis was accomplished using
Computed Tomography [CT] brain result. The CT brain statistical method for calculations provided within
scanning in stroke was performed to exclude any non- Statistical package for social science software [version
vascular cause of neurological deficit (29). The GCS 11.5]. The logistic regression analysis was performed and
during ETI either on arrival or during course of hospital classifications of observed and predicted outcomes were
stay was also recorded. identified. The Receiver Operating Characteristic [ROC]
The Glasgow Coma Scale: analysis was carried out by Non-parametric Receiver
Operating Characteristic Analysis Software [Version 2.5]
GCS is the sum of three coded values that describe a
for GCS and its components, and measured the areas
patient's best motor [16], verbal [15] and eye [14]
under these curves [AUCs] to compare the predictive
response to speech or pain [TABLE 1]. The patient is
valve for outcome at 3 months in TBI and AS patients. The
August - October 2012, Vol : 1, Issue : 1 43
NATIONAL JOURNAL OF EMERGENCY MEDICINE
same method was used for analysis of GCS and its good outcome and 92.1% correctly classified overall
components in predicting requirement for ETI in TBI and outcome by the logistic regression. For acute
AS patients. p < 0.05 was considered statistically haemorrhagic stroke, it is found that 90% correctly
significant. classified the bad outcome, 83.3% correctly classified the
RESULTS good outcome and 87% correctly classified overall
outcome by the logistic regression. The ROC curve
The study sample analyzed consisted of 375 cases, of
analysis showed the AUC was greatest for motor
which 81.33% were male and 18.67% were female. The
component in acute ischemic stroke [AUC = 0.892, 95% CI
median age was 40 years [IOR = 29 years]. Of 375 patients
= 0.783 to 1.001] with p < 0.001. In acute haemorrhagic
in the study, 68.8% were TBI and 31.2% were AS. Out of
stroke, the AUC was greatest for total GCS [AUC = 0.944,
258 cases of TBI, 36.4% were due to mild TBI, 17.4% were
95% CI = 0.886 to 1.001] followed by motor component
due to moderate TBI and 46.1% were due to severe TBI.
[AUC = 0.919, 95% CI = 0.845 to 0.993] with p < 0.001
Out of 117 cases of AS, 53.8% were due to ischemic stroke
[GRAPH 4, 5, TABLE 6].
and 46.2% were due to haemorrhagic stroke. At
admission, median of total GCS score was 10 [TBI - 9 and From the classification of observed and predicted cases
AS - 10]. Highest frequency of total GCS occurred for 15 in for overall patients, it is found that 91.1% correctly
81 [21.6%] patients followed by 7 in 43 [11.5%] patients. classified the non intubated cases, 96.7% correctly
45.1% of patients were intubated either on arrival or classified the intubated cases and 93.3% correctly
during the course of hospital stay [TABLE 4]. The median classified the overall requirement of ETI by the logistic
GCS for requirement of ETI was 6 [TBI - 7 and AS - 6]. regression. For TBI, it is found that 92.7% correctly
65.1% of patients had a good outcome as per GOS at 3 classified the non intubated cases, 94.1% correctly
months [67.8% for TBI and 59% for AS]. classified the intubated cases and 93.3% correctly
classified the overall requirement of ETI by the logistic
From the classification of observed and predicted cases
regression. For AS, it is found that 91.5% correctly
for overall patients, it is found that 80.9% correctly
classified the non intubated cases, 87% correctly
classified the bad outcome, 96.3% correctly classified the
classified the intubated cases and 89.7% correctly
good outcome and 90.9% correctly classified overall
classified the overall requirement of ETI by the logistic
outcome by the logistic regression. For TBI, it is found that
regression. The ROC curve analysis showed the AUC was
85.5% correctly classified the bad outcome, 96%
greatest for total GCS [AUC = 0.977, 95% CI = 0.964 to
correctly classified the good outcome and 92.6%
0.991] in all patients with p < 0.001. In TBI and AS, the AUC
correctly classified overall outcome by the logistic
was greatest for total GCS [AUC = 0.982, 95% CI = 0.968 to
regression. For AS, it is found that 75% correctly classified
0.997 and 0.967, 95% CI = 0.938 to 0.996 respectively]
the bad outcome, 94.2% correctly classified the good
with p < 0.001 [GRAPH 6, 7, 8, TABLE 7].
outcome and 86.3% correctly classified overall outcome
by the logistic regression. The ROC curve analysis showed From the classification of observed and predicted cases
the AUC was greatest for motor component in all patients for acute ischemic stroke, it is found that 93.2% correctly
[AUC = 0.937] {95% confidence interval [CI] = 0.909 to classified the non intubated cases, 84.2% correctly
0.965} as well as in TBI [AUC = 0.959, 95% CI = 0.936 to classified the intubated cases and 90.5% correctly
0.982] with p < 0.001. In AS, the AUC was greatest for total classified the overall requirement of ETI by the logistic
GCS [AUC = 0.909, 95% CI = 0.854 to 0.964] with similar regression. For acute haemorrhagic stroke, it is found
magnitude for motor component [AUC = 0.908, 95% CI = that 92.6% correctly classified the non intubated cases,
0.847 to 0. 0.968], with p < 0.001 [GRAPH 1, 2, 3, TABLE 5]. 92.6% correctly classified the intubated cases and 92.6%
correctly classified the overall requirement of ETI by the
From the classification of observed and predicted cases
logistic regression. The ROC curve analysis showed the
for acute ischemic stroke, it is found that 72.2% correctly
AUC was greatest for eye component [AUC = 0.969, 95%
classified the bad outcome, 100% correctly classified the
CI = 0.933 to 1.006] followed by total GCS [AUC = 0.944,
44 August - October 2012, Vol : 1, Issue : 1
NATIONAL JOURNAL OF EMERGENCY MEDICINE
95% CI = 0.882to 1.006] in acute ischemic stroke with p < Good/Favourable Bad/Unfavourable
0.001. In acute haemorrhagic stroke, the AUC was
greatest for total GCS [AUC = 0.981, 95% CI = 0.952 to Severe Disability
1.009] with p < 0.001 [GRAPH 9, 10, TABLE 8]. Good recovery
Persistent Vegetative State
Moderate Disability
Dead
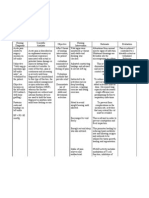
Parameter Response Score
Spontaneous 4 TABLE 3 : Broader outcome categories of GOS
Eye To speech 3
opening To pain 2
None 1
Variables Details n [%]
Oriented 5
Best Confused conversation 4 Mean - 41.47
verbal Inappropriate words 3
response Age Median - 40
Incomprehensible sounds 2
None 1 IQR - 29
Obeys commands 6 Male 305 [81.3%]
Localizes pain 5 Sex
Best Female 70 [18.7%]
Withdrawal (normal flexion) 4
motor
response Abnormal flexion (decorticate) 3 Traumatic Brain Injury 258 [68.8%]
Extension (decerebrate) 2 Diagnosis
None 1 Acute Stroke 117 [31.2%]
TABLE 1 : GLASGOW COMA SCALE Mild Head Injury 94 [36.4%]
Severity of TBI Moderate Head Injury 45 [17.4%]
1 Dead Non-survival Severe Head Injury 119 [46.1%]
Vegetative Nature of Ischemic Stroke 63 [53.8%]
2 Minimal responsiveness
state acute stroke
Haemorrhagic Stroke 54 [46.2%]
Conscious and able to follow
Severe commands Endotracheal
3 Traumatic Brain Injury 115 [44.6%]
disability Dependent on others for daily intubation
support 54 [46.2%]
Acute stroke
Able to live independently
Moderate Unable to return to work or All Patients 169 [45.1%]
4
disability school TABLE 4: Demographic and injury characteristics
Can work in sheltered setting
Able to return to work or school
5 Good recovery Resumption of normal life
despite minor deficits
TABLE 2 : The Five-Point GOS
August - October 2012, Vol : 1, Issue : 1 45
NATIONAL JOURNAL OF EMERGENCY MEDICINE
Asymptotic Asymptotic
95% 95%
Confidence Patient Test Result Std. Confidence
Patient Test Result Std. Area p Interval
Area p Interval Groups Variable[s] Error
Groups Variable[s] Error
Lower Upper
Lower Upper Bound Bound
Bound Bound
Eye
Eye component 0.804 0.071 <0.001 0.665 0.942
0.829 0.023 <0.001 0.784 0.873
component
Ischemic Verbal
0.677 0.070 0.029 0.540 0.814
Verbal stroke component
All 0.833 0.021 <0.001 0.792 0.874
component [n=63] Motor
Patients 0.892 0.056 <0.001 0.783 1.001
component
[n=375] Motor
0.937 0.014 <0.001 0.909 0.965 Total GCS 0.869 0.055 <0.001 0.760 0.978
component
Total GCS 0.931 0.013 <0.001 0.906 0.956 Eye
component 0.860 0.054 <0.001 0.753 0.966
Eye Haemorrhagic Verbal
0.843 0.026 <0.001 0.792 0.893 0.881 0.051 <0.001 0.780 0.982
component stroke component
[n=54] Motor
Verbal 0.919 0.038 <0.001 0.845 0.993
TBI 0.866 0.022 <0.001 0.823 0.909 component
component
[n=258] Total GCS 0.944 0.029 <0.001 0.886 1.001
Motor
0.959 0.012 <0.001 0.936 0.982
component TABLE 6 : AUCS FOR TOTAL AND INDIVIDUAL GCS COMPONENTS
Total GCS 0.948 0.012 <0.001 0.924 0.972 ROC CURVES FOR OUTCOME AT 3 MONTHS ACCORDING TO
NATURE OF ACUTE STROKE: [N=258]
Eye
0.839 0.040 <0.001 0.760 0.917
component Asymptotic 95%
Confidence
Acute Verbal Patient Test Result Std. Interval
0.760 0.044 <0.001 0.672 0.847 Groups Variable[s]
Area
Error
p
Stroke component Lower Upper
[n=117] Motor Bound Bound
0.908 0.031 <0.001 0.847 0.968
component
Eye component 0.942 0.013 <0.001 0.917 0.968
Total GCS 0.909 0.028 <0.001 0.854 0.964
All Verbal
Patients 0.899 0.017 <0.001 0.866 0.931
component
TABLE 5 : AUCS FOR TOTAL AND INDIVIDUAL GCS [n=375]
Motor
COMPONENTS ROC CURVES FOR OUTCOME AT component
0.938 0.011 <0.001 0.916 0.961
3 MONTHS
Total GCS 0.977 0.007 <0.001 0.964 0.991
Eye component 0.938 0.017 <0.001 0.905 0.971
Verbal
TBI 0.950 0.014 <0.001 0.923 0.976
component
[n=258]
Motor
0.945 0.012 <0.001 0.921 0.970
component
Total GCS 0.982 0.008 <0.001 0.968 0.997
Eye component 0.956 0.018 <0.001 0.921 0.990
Acute Verbal
0.808 0.040 <0.001 0.731 0.886
Stroke component
[n=117] Motor
0.928 0.025 <0.001 0.880 0.976
component
Total GCS 0.967 0.015 <0.001 0.938 0.996
TABLE 7 : AUCS FOR TOTAL AND INDIVIDUAL GCS COMPONENTS
ROC CURVES FOR REQUIREMENT OF ENDOTRACHEAL INTUBATION
46 August - October 2012, Vol : 1, Issue : 1
NATIONAL JOURNAL OF EMERGENCY MEDICINE
Asymptotic
95%
Patient Test Result Std. Confidence
Area p Interval
Groups Variable[s] Error
Lower Upper
Bound Bound
Eye
0.969 0.019 <0.001 0.933 1.006
component
Ischemic Verbal
0.770 0.058 0.001 0.655 0.884
stroke component
[n=63] Motor
0.880 0.047 <0.001 0.787 0.973
component
Total GCS 0.944 0.032 <0.001 0.882 1.006
Eye
0.930 0.038 <0.001 0.856 1.004
component
GRAPH 2 : AUCS FOR TOTAL AND INDIVIDUAL GCS COMPONENTS
Haemorrhagic Verbal
0.874 0.052 <0.001 0.773 0.976 ROC CURVES FOR OUTCOME AT 3 MONTHS IN TBI : [N=258]
stroke component
[n=54] Motor
0.968 0.019 <0.001 0.930 1.006
component
Total GCS 0.981 0.015 <0.001 0.952 1.009
TABLE 8 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR REQUIREMENT OF
ENDOTRACHEAL INTUBATION ACCORDING TO NATURE
OF ACUTE STROKE: [N=258]
GRAPH 3 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR OUTCOME AT 3 MONTHS
IN ACUTE STROKE:[N=117]
GRAPH 1 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR OUTCOME AT 3 MONTHS
IN ALL PATIENTS: [N=375]
GRAPH 4 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR OUTCOME AT 3
MONTHS IN ACUTE ISCHEMIC STROKE: [N=63]
August - October 2012, Vol : 1, Issue : 1 47
NATIONAL JOURNAL OF EMERGENCY MEDICINE
GRAPH 5 : AUCS FOR TOTAL AND INDIVIDUAL GCS GRAPH 8 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR OUTCOME AT 3 MONTHS COMPONENTS ROC CURVES FOR REQUIREMENT OF
IN ACUTE HEMORRHAGIC STROKE: [N=54] ENDOTRACHEAL INTUBATION IN ACUTE STROKE:[N=117]
GRAPH 6 : AUCS FOR TOTAL AND INDIVIDUAL GCS GRAPH 9 : AUCS FOR TOTAL AND INDIVIDUAL GCS COMPONENTS
COMPONENTS ROC CURVES FOR REQUIREMENT OF ROC CURVES FOR REQUIREMENT OF ENDOTRACHEAL
ENDOTRACHEAL INTUBATION IN ALL PATIENTS:[N=375] INTUBATION IN ACUTE ISCHEMIC STROKE: [N=63]
GRAPH 10 : AUCS FOR TOTAL AND INDIVIDUAL GCS
GRAPH 7 : AUCS FOR TOTAL AND INDIVIDUAL GCS
COMPONENTS ROC CURVES FOR REQUIREMENT OF
COMPONENTS ROC CURVES FOR REQUIREMENT OF
ENDOTRACHEAL INTUBATION IN ACUTE HAEMORRHAGIC
ENDOTRACHEAL INTUBATION IN TBI: [N=258]
STROKE:[N=54]
48 August - October 2012, Vol : 1, Issue : 1
NATIONAL JOURNAL OF EMERGENCY MEDICINE
DISCUSSION et al (3, 40). In AS patients, the verbal component was the
The main issues ensuing from TBI are cognitive and weakest predictor which was a comparable with the
personality problems, rather than physical disability (37). results of Diringer et al and Kameshwar Prasad et al but is
TBI and AS patients with poor prognosis receiving an different to findings of C J Weir et al (29, 38, 41). The
effective treatment may benefit only by surviving and components of the GCS may be affected due to focal
become completely dependent with poor quality of life deficits in these patients misjudging the actual level of
resulting in a huge burden of care, largely borne by the consciousness. Another explanation to the varied results
immediate relatives (29). Continuous efforts are being may be the false recording of the best motor and verbal
made by researchers to identify the prognostic indicators response due to paralysis and dysphasia respectively
in these patients that would help the family for an (29).
efficient planning of their income and funds. Unlike many Further in AS patients, the performance of the GCS and its
other studies, we assessed the outcome predictive ability components according to the nature of the stroke in
of GCS and its components in both TBI and AS patients. predicting outcome were not studied earlier. The results
We also carried out a similar analysis in subgroup of AS of this subgroup analysis obtained in our study for
patients according to the nature of stroke [hemorrhagic hemorrhagic stroke showed that the total GCS yields
and ischemic stroke]. equivalent prediction rates as the motor component
In this study, we found that the motor component of the since they occupied similar magnitude of AUC when
GCS scoring system performed better than the total GCS, compared to the eye and verbal components. But in
eye and verbal components of GCS in predicting outcome ischemic stroke patients, the motor component
in all patients [both TBI and AS together] as well as in TBI performed greatest with a marginal difference from that
patients alone. In AS patients alone, the total GCS and the of the total GCS. There was no evidence to support or
motor component accurately predicted outcome in an refute this finding from the literature.
equivalent manner. Our findings were similar to the Very few studies have used ETI as TBI outcome measure
results of previous studies by Healey et al, Kameshwar (3, 39, 40, 45). This outcome measure was not considered
Prasad et al, Gill et al and Al-Salamah et al using ROC in any of the previous studies in AS patients. The
curves that reported the motor component of the GCS requirement of ETI was analyzed to determine which
occupied nearly the same area under an ROC curve as did components of the GCS will display similar, better, or
the total GCS score in their ability to predict outcome (28, worse associations. Our data analysis reveals that the
38, 39, 40). Similarly, Diringer et al, Meredith et al and total GCS scoring system performed better than the
Ross et al also reported that the motor component of the individual components of GCS in predicting ETI in all
GCS score accurately predicted outcome which is also patients [both TBI and AS] as well as in patients with TBI
comparable to our result (41, 42, 43). It appears that the and AS separately. In agreement with our finding, studies
motor response being the largest component of the GCS by Michelle Gill et al and Haukoos JS et al also found the
scoring system practically contains all the information of total GCS was accurate in predicting the requirement of
the GCS itself and thereby better outcome predictive ETI in TBI patients (3, 45). However this finding differed
value. In contrast, a study using ROC analysis by C J Weir from the end result of a study by Al-Salamah et al in which
et al in assessing AS patients and a study by Moore et al in they reported eye component was the best predictor of
TBI patients reported that the total GCS accurately ETI followed by the total GCS (40).
predicts outcome than the individual GCS components While studying the requirement of ETI according to the
(29, 44). nature of the stroke, the greatest predictive ability was
Data analysis from our study showed that the eye retained by the total GCS in hemorrhagic stroke patients.
component was the weakest predictor for TBI similar to But observations in ischemic stroke patients showed that
the results of studies by Michelle Gill et al and Al-Salamah the ability to correctly predict ETI by the eye component
August - October 2012, Vol : 1, Issue : 1 49
NATIONAL JOURNAL OF EMERGENCY MEDICINE
was the best followed by the total GCS when compared to design, purpose, goals, and results. J Neurosurg. 1983
Aug;59(2):276-84.
the motor and verbal components. This was similar to
findings of Al-Salamah et al in their study which was 8. I n d i a n H e a d I n j u r y Fo u n d a t i o n .
http://indianheadinjuryfoundation.org/facts.html
described as an isolated finding requiring further
9. PK Sethi. Stroke - Incidence in India and Management of
validation (40).
Ischaemic stroke. Neurosciences Today. July -September
By evaluating the GCS and its individual components in 2002;6(3).
both TBI and AS patients, we have shown that the motor 10. http://www.tribuneindia.com/2009/20091030/delhi.htm#11
response has a good or better predictive value in 11. Subhash Kaul. Stroke in India: Are we different from the world?
assessing GOS. Due to simplicity of measuring the motor Pak J Neurol Sci. 2007;2(3):158-164.
response as well as its applicability in intubated patients, 12. National Center for Injury Prevention and Control.
the variability of its assessment among healthcare Epidemiology of traumatic brain injury in the United States.
http://www.cdc.gov/ncipc/tbi/TBI.htm. Updated March 19,
workers would reduce (3, 25). Hence, we believe that the 2009. Accessed May 12, 2009.
total GCS could simply be replaced by the motor
13. HyunSoo Oh and WhaSook Seo. Functional and Cognitive
component in predicting outcome of TBI and AS patients Recovery of Patients with Traumatic Brain Injury. Crit Care
while maintaining higher specificity. Since the Nurse. 2009;29: 12-22.
predictability of ETI by the motor score is not greater than 14. Teasdale G, Gentlemen D. The description of 'conscious level ':
total GCS, we suggest the GCS in its summed form should a case for the Glasgow Coma Scale. Scott Med j. 1982
not be replaced by the motor component in both TBI and Jan;27(1):7-9.
AS patients. The application of these findings could be 15. Jagger J, Jane JA, Rimel R. The Glasgow Coma Scale: To sum or
not to sum? Lancet. 1983 Jul 9;2(8341):97.
extended to out-of-hospital environment as well (3).
16. Levy DE, Bates D, Caronna JJ, Cartlidge NE, Knill-Jones RP,
CONCLUSION Lapinski RH, et al. Prognosis in non traumatic coma. Ann Intern
In the assessment of TBI and AS patients, the motor Med. 1981 Mar;94(3):293-301.
component of GCS scoring system is a better predictor of 17. Ramesh VG, Thirumaran KP, Raja MC. A new scale for
prognostication in head injury. . 2008 Oct;15(10):1110-3;
3 month outcome while the GCS in its summed form is a
discussion 1113-4. Epub 2008 Jul 23.
better indicator for requirement of endotracheal
18. Kaufmann MA, Buchmann B, Scheidegger D, Gratzl O, Rad
intubation. EW. Severe head injury: should expected outcome influence
REFERENCES resuscitation and first-day decisions. Resuscitation. 1992 Jun-
Jul;23(3):199-206.
1. http://www.bioportfolio.com on Friday, December 18, 2009.
19. Schreiber MA, Aoki N, Scott BG, Beck JR. Determinants of
2. Teasdale G, Jennett B. Assessment of coma and impaired
mortality in patients with severe blunt head injury. Arch of
consciousness. A practical scale. Lancet. 1974 Jul
Surgery. 2002 Mar;137(3):285-90.
13;2(7872):81-4.
20. Oppenheim JS, Camins MB. Predicting outcome in brain-
3. Gill M, Steele R, Windemuth R, Green SM. A Comparison of
injured patients. Using the Glasgow Coma Scale in primary
Five Simplified Scales to the Out-of-hospital GCS for the
care practice. Postgrad Med. 1992 Jun;91(8):261-4, 267-8.
prediction of traumatic Brain Injury Outcomes. Acad Emerg
Med. 2006 Sep;13(9):968-73. Epub 2006 Aug 7. 21. Rutledge R, Lentz CW, Fakhry S, Hunt J. Appropriate use of the
Glasgow Coma Scale in intubated patients: a linear regression
4. George L. Sternbach. The Glasgow Coma Scale. The Journal of
prediction of the Glasgow verbal score from the Glasgow eye
Emergency Medicine. 2000;19(1):6771.
and motor scores. J. Trauma. 1996 Sep;41(3):514-22.
5. Champion HR, Sacco WJ, Carnazzo AJ, Copes W, Fouty WJ.
22. Demetriades D, Kuncir E, Murray J, Velmahos GC, Rhee P, Chan
Trauma score. Crit Care Med. 1981 Sep;9(9):672-6.
L. Mortality prediction of head Abbreviated Injury Score and
6. Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Glasgow Coma Scale: analysis of 7,764 head injuries.
Flanagan ME. A revision of the Trauma Score. J Trauma. 1989 J.Am.Coll.Surg. 2004 Aug;199(2):216-22.
May;29(5):623-9.
23. Molly McNett. Predictive Ability of Glasgow Coma Scale Scores
7. Marshall LF, Becker DP, Bowers SA, Cayard C, Eisenberg H, in Head-Injured Patients: GCS and Other Predictor Variables. J
Gross CR, et al. The National Traumatic Coma Data Bank. Part I: Neurosci Nurs. 2007 Apr;39(2):68-75.
50 August - October 2012, Vol : 1, Issue : 1
NATIONAL JOURNAL OF EMERGENCY MEDICINE
24. Heim C, Schoettker P, Gilliard N, Spahn DR. Knowledge of 36. Fabbri A, Servadei F, Marchesini G, Stein SC, Vandelli A. Early
Glasgow coma scale by air-rescue physicians. Scand J Trauma predictors of unfavourable outcome in subjects with
Resusc Emerg Med. 2009 Sep 1;17:39. moderate head injury in the emergency department. J Neurol
25. Rowley G, Fielding K. Reliability and accuracy of the Glasgow Neurosurg Psychiatry. 2008 May;79(5):567-73. Epub 2007 Aug
Coma Scale with experienced and inexperienced users. 31.
Lancet. 1991 Mar 2;337(8740):535-8. 37. Jonathan Bird. Unexpected aspects of head injury. 02 Feb 04.
26. Teasdale G, Jennett B, Murray L, Murray G. Glasgow coma http://www.pulsetoday.co.uk.
scale: to sum or not to sum. Lancet. 1983 Sep 17;2(8351):678. 38. Prasad K, Menon GR. Comparison of the Three Strategies of
27. Teoh LS, Gowardman JR, Larsen PD, Green R, Galletly DC. Verbal Scoring of the Glasgow Coma Scale in Patients with
Glasgow Coma Scale: variation in mortality among Stroke. Cerebrovasc Dis. 1998 Mar-Apr;8(2):79-85.
permutations of specific total scores. Intensive Care Med. 39. Gill M, Windemuth R, Steele R, Green SM. A comparison of the
2000 Feb;26(2):157-61. Glasgow Coma Scale score to simplified alternative scores for
28. Healey C, Osler TM, Rogers FB, Healey MA, Glance LG, Kilgo PD, the prediction of traumatic brain injury outcomes. Ann Emerg
et al. Improving the Glasgow Coma Scale score: motor score Med. 2005 Jan;45(1):37-42.
alone is a better predictor. J. Trauma. 2003 Apr;54(4):671-8; 40. Al-Salamah MA, McDowell I, Stiell IG, Wells GA, Perry J, Al-
discussion 678-80. Sultan M, et al. Initial emergency department trauma scores
29. Weir CJ, Bradford AP, Lees KR. The prognostic value of the from the OPALS study: the case for the motor score in blunt
component of the Glasgow coma scale following acute stroke. trauma. Acad Emerg Med. 2004 Aug;11(8):834-42.
Q J Med. 2003 Jan;96(1):67-74. 41. Diringer MN, Edwards DF. Does modification of the Innsbruck
30. Jennett B, Teasdale G, Galbraith S, Pickard J, Grant H, and the Glasgow Coma Scales improve their ability to predict
Braakman R, et al. Severe head injuries in three countries. J functional outcome? Arch Neurol. 1997 May;54(5):606-11.
Neurol Neurosurg Psychiatry. 1977 Mar;40(3):291-8. 42. Meredith W, Rutledge R, Hansen AR, Oller DW, Thomason M,
31. Balestreri M, Czosnyka M, Chatfield DA, Steiner LA, Schmidt Cunningham P, et al. Field triage of trauma patients based
EA, Smielewski P, et al. Predictive value of Glasgow coma scale upon the ability to follow commands: A study in 29,573
after brain trauma: change in trend over the past ten years. J patients. Journal of Trauma. 1995 Jan;38(1):129-35.
Neurol Neurosurg Psychiatry. 2004 Jan;75(1):161-2. 43. Ross SE, Leipold C, Terregino C, O'Malley KF. Efficacy of the
32. Teasdale G, Knill-Jones R, Van Der Sande J: Observer variability Motor Component of the Glasgow Coma Scale in Trauma
in assessing impaired consciousness and coma. J Neurol Triage. J Trauma. 1998 Jul;45(1):42-4.
Neurosurg Psychiatry. 1978 Jul;41(7):603-10. 44. Moore, Lynne MSc; Lavoie, Andr PhD; Camden, Stephanie
33. Jennett B, Bond M. Assessment of outcome after severe brain BSc; Le Sage, Nathalie MD, PhD; Sampalis, John S. PhD;
damage. Lancet. 1975 Mar 1;1(7905):480-4. Bergeron, Eric MD, MSc; Abdous, Belkacem PhD. Statistical
Validation of the Glasgow Coma Score. J Trauma. 2006
34. Narayan RK, Greenberg RP, Miller JD, Enas GG, Choi SC, Kishore
Jun;60(6):1238-43; discussion 1243-4.
PR, et al. Improved confidence of outcome prediction in severe
head injury. A comparative analysis of the clinical examination, 45. Haukoos JS, Gill MR, Rabon RE, Gravitz CS, Green SM.
multimodality evoked potentials, CT scanning, and intracranial Validation of the Simplified Motor Score for the prediction of
pressure. Journal of Neurosurgery. 1981 Jun;54(6):751-62. brain injury outcomes after trauma. Ann Emerg Med. 2007
Jul;50(1):18-24. Epub 2006 Nov 16.
35. Choi SC, Ward JD, Becker DP. Chart for outcome prediction in
severe head injury. Journal of Neurosurgery. 1983
Aug;59(2):294-7.
Online Journal : www.emergencymedicine.co
Manuscripts can be submitted at : submit@emergencymedicine.co
Contact : chiefeditor@emergencymedicine.co
August - October 2012, Vol : 1, Issue : 1 51
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Care of A Child With Cardiovascular DysfunctionDocumento71 pagineCare of A Child With Cardiovascular DysfunctionMorgan Mitchell100% (1)
- 380 Final PaperDocumento46 pagine380 Final Paperapi-538048965Nessuna valutazione finora
- Yoga Your Home Practice CompanionDocumento257 pagineYoga Your Home Practice Companionjohncoltrane97% (33)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- PIDSR Other DiseasesDocumento45 paginePIDSR Other DiseasesMichelle TuraNessuna valutazione finora
- KPI - Foruth EditionDocumento30 pagineKPI - Foruth EditionAnonymous qUra8Vr0SNessuna valutazione finora
- NCP - Acute Pain - FractureDocumento1 paginaNCP - Acute Pain - Fracturemawel73% (22)
- Basic Concepts of Fluid and Electrolyte TherapyDocumento136 pagineBasic Concepts of Fluid and Electrolyte Therapynoorgianilestari100% (2)
- STP 1560-2013Documento346 pagineSTP 1560-2013HieuHTNessuna valutazione finora
- Syringe CompatibilityDocumento1 paginaSyringe CompatibilityRaju NiraulaNessuna valutazione finora
- Adult gliomas guide for patientsDocumento123 pagineAdult gliomas guide for patientsWidya WidyariniNessuna valutazione finora
- Berlin ARDS Definition 2012Documento25 pagineBerlin ARDS Definition 2012Widya WidyariniNessuna valutazione finora
- Effects of atracurium besylateDocumento3 pagineEffects of atracurium besylateWidya WidyariniNessuna valutazione finora
- Acs Cardiovascular Emergency Jadi PDFDocumento95 pagineAcs Cardiovascular Emergency Jadi PDFWidya WidyariniNessuna valutazione finora
- Tuberculous spinal arachnoiditis case reportDocumento1 paginaTuberculous spinal arachnoiditis case reportWidya WidyariniNessuna valutazione finora
- ASA Classifications 4-09 PDFDocumento2 pagineASA Classifications 4-09 PDFWidya WidyariniNessuna valutazione finora
- ASA Risk Classifications-Wilkens 10th Ed and Malamed 5th EdDocumento2 pagineASA Risk Classifications-Wilkens 10th Ed and Malamed 5th EdWidya WidyariniNessuna valutazione finora
- Art TECH GComaScale PDFDocumento2 pagineArt TECH GComaScale PDFWidya WidyariniNessuna valutazione finora
- JNC 8Documento14 pagineJNC 8amiwahyuniNessuna valutazione finora
- Adult Acute Bact Rhino PDFDocumento1 paginaAdult Acute Bact Rhino PDFWidya WidyariniNessuna valutazione finora
- 3 +Hypovolemic+Shock+Resuscitation PDFDocumento21 pagine3 +Hypovolemic+Shock+Resuscitation PDFWidya WidyariniNessuna valutazione finora
- A Healthy Home For Everyone PDFDocumento16 pagineA Healthy Home For Everyone PDFWidya WidyariniNessuna valutazione finora
- 15 - Male - Infertility - LR II PDFDocumento64 pagine15 - Male - Infertility - LR II PDFWidya WidyariniNessuna valutazione finora
- Sindrome de Guillain BarreDocumento12 pagineSindrome de Guillain BarreLuis DubonNessuna valutazione finora
- 10.1 Life-Threatening Electrolyte AbnormalitiesDocumento6 pagine10.1 Life-Threatening Electrolyte AbnormalitiesWidya WidyariniNessuna valutazione finora
- Jurnal Laser TerapiDocumento17 pagineJurnal Laser TerapiWidya Widyarini100% (1)
- WHO HSE GAR DCE 2010.2 EngDocumento6 pagineWHO HSE GAR DCE 2010.2 Engangelabety88Nessuna valutazione finora
- Success Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseDocumento11 pagineSuccess Manual and Cheat Sheet Notes To Pass Your Basic Life Support (BLS) CourseanthonyNessuna valutazione finora
- Congenital LaryngomalaciaDocumento8 pagineCongenital LaryngomalaciaRettha SigiroNessuna valutazione finora
- The Effect of Warm Ginger Compress on Hypertension Headache Scale in the ElderlyDocumento7 pagineThe Effect of Warm Ginger Compress on Hypertension Headache Scale in the Elderlyjembatan gantungNessuna valutazione finora
- Stress Amongst Healthcare Professionals and Migrant Workers During Covid-19 PandemicDocumento6 pagineStress Amongst Healthcare Professionals and Migrant Workers During Covid-19 PandemicIJAR JOURNALNessuna valutazione finora
- Paul B. Bishop, DC, MD, PHD, Jeffrey A. Quon, DC, PHD, FCCSC, Charles G. Fisher, MD, MHSC, FRCSC, Marcel F.S. Dvorak, MD, FRCSCDocumento10 paginePaul B. Bishop, DC, MD, PHD, Jeffrey A. Quon, DC, PHD, FCCSC, Charles G. Fisher, MD, MHSC, FRCSC, Marcel F.S. Dvorak, MD, FRCSCorlando moraNessuna valutazione finora
- API SM Part 1Documento7 pagineAPI SM Part 1Ronaldo JanglinNessuna valutazione finora
- Jacked at Home - Bodyweight Muscle-Building WorkoutsDocumento6 pagineJacked at Home - Bodyweight Muscle-Building Workoutsmohamed aliNessuna valutazione finora
- KT Instructions AC Joint PDFDocumento1 paginaKT Instructions AC Joint PDFariel JaldinNessuna valutazione finora
- Posters Whofic 2020Documento107 paginePosters Whofic 2020Kristel HurtadoNessuna valutazione finora
- Risk for Infection AssessmentDocumento7 pagineRisk for Infection AssessmentLouis RoderosNessuna valutazione finora
- PORNOGRAPHICDocumento13 paginePORNOGRAPHICcarlos ortizNessuna valutazione finora
- 2020 DWTC Event Calendar EnglishDocumento4 pagine2020 DWTC Event Calendar EnglishMustazhar0% (1)
- Tolterodine Tartrate (Detrusitol SR)Documento11 pagineTolterodine Tartrate (Detrusitol SR)ddandan_2Nessuna valutazione finora
- Class 7 PolityDocumento10 pagineClass 7 PolityNakka nikithaNessuna valutazione finora
- Snap Glass CleanerDocumento7 pagineSnap Glass Cleanerlovenan02Nessuna valutazione finora
- IFUk en 310250 07 PDFDocumento14 pagineIFUk en 310250 07 PDFKhaled AlkhawaldehNessuna valutazione finora
- Journal On The Impact of Nursing Informatics To Clinical PracticeDocumento2 pagineJournal On The Impact of Nursing Informatics To Clinical PracticeLhara Vhaneza CuetoNessuna valutazione finora
- Week 4-Physical Fitness TestDocumento38 pagineWeek 4-Physical Fitness TestCatherine Sagario OliquinoNessuna valutazione finora
- Eo No. 013 - 2018 Reorganization of BhertDocumento2 pagineEo No. 013 - 2018 Reorganization of BhertAnne Kimberly Peñalba BabaanNessuna valutazione finora
- Package List Swasthysathi 2018-Grade BDocumento150 paginePackage List Swasthysathi 2018-Grade BKuntal GuptaNessuna valutazione finora
- Table : Number of Population, Hospitals and Beds in All Over JordanDocumento8 pagineTable : Number of Population, Hospitals and Beds in All Over JordanjNessuna valutazione finora
- MANAGEMENT AND PREVENTIONDocumento6 pagineMANAGEMENT AND PREVENTIONIrina BalutaNessuna valutazione finora