Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ig E y Correlacion Enf EBA
Caricato da
Var AndaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ig E y Correlacion Enf EBA
Caricato da
Var AndaCopyright:
Formati disponibili
Acta Derm Venereol 2001; 81: 429 451
LETTERS TO THE EDITOR
Epidermolysis Bullosa Acquisita: Correlation of IgE Levels with Disease Activity under Successful
Betamethasone/Dapsone Combination Therapy
Hideyuki Miyake1, Yohichi Morishima1*, Reiko Komai2, Takashi Hashimoto2 and Saburo Kishimoto3
Departments of Dermatology, 1 Matsushita Memorial Hospital, 5-55 Sotojima-cho, Moriguchi-Shi, Osaka 570-8740, 2 Kurume
University, Fukuoka and 3 Kyoto Prefectural University of Medicine, Kawaramachi Hirokoji, Kyoto, Japan.
*Author for correspondence.
Accepted August 6, 2001.
Sir, then gradually decreased to normal levels as the disease activity
We report on a possible association between epidermolysis decreased.
bullosa acquisita (EBA) and elevated levels of circulating IgE. This appears to be the rst reported case of EBA in which
A 23-year-old man with a 3-month history of intensely itchy IgE has been evaluated. Although the potential pathophysio-
blisters ful lled the diagnostic criteria for EBA (subepidermal logical relevance of our ndings is not clear as yet, we suggest
blisters, linear IgG deposits in basement membrane zone, that it may be useful to evaluate total immunoglobulin levels
circulating IgG antibodies to dermal part of the basement in new patients with EBA and possibly also in other blistering
membrane zone in split skin test, circulating antibodies reacting diseases (3, 4).
with a 290 kD component in dermal extracts by immuno-
blotting) (1, 2). The patient was successfully treated with a REFERENCES
combination of betamethasone and dapsone. After 10 months
1. Woodley DT, Briggaman RA, OKeefe EJ, Inman AO, Queen LL,
of treatment, direct immuno uorescence had become negative, Gammon WR. Identi cation of the skin basement-membrane
and circulating antibodies to basement membrane zone com- autoantigen in epidermolysis bullosa acquisita. N Engl J Med 1984;
ponents could no longer be detected. Treatment was discon- 310: 1007 1013.
tinued after 15 months, and the patient has been in remission 2. Shimizu H, McDonald JN, Gunner DB, Black MM, Bhogal B,
during the 2 months that have elapsed since the treatment Leigh IM, et al. Epidermolysis bullosa acquisita antigen and the
was stopped. carboxy terminus of type VII collagen have a common immuno-
Interestingly, the patient had elevated serum levels of IgE localization to anchoring brils and lamina densa of basement
membrane. Br J Dermatol 1990; 122: 577 585.
(3,480 IU/ml vs. normally < 250 IU/ml ) at the rst visit.
3. Maekawa N, Hosokawa H, Soh H, Kasahara M, Izumi H,
Radio-allergosorbent tests showed polyclonal IgE against a Yodoi J, et al. Serum levels of soluble CD23 in patients with
wide variety of common environmental allergens such as dust- bullous pemphigoid. J Dermatol 1995; 22: 310 315.
and house mites, and Candida albicans. The serum IgE levels 4. Soh H, Hosokawa H, Asada Y. IgE and its related phenomena in
remained high as long as the patient had skin symptoms, but bullous pemphigoid. Br J Dermatol 1993; 128: 371 377.
Addition of Pentoxifylline Could Reduce the Side Eects of Fumaric Acid Esters in the
Treatment of Psoriasis
Markus Friedrich1, Wolfram Sterry1, Anja Klein, Rene Ruckert1, Wolf Dietrich Docke2 and Khusru Asadullah1
1 Department of Dermatology and Allergy and 2 Department of Medical Immunology, University Hospital Charite , Schumannstr.
21/22, 10117 Berlin, Germany. E-mail: markus.friedrich@charite.de
Accepted September 21, 2001.
Sir, by our observation that monocytes secrete TNF-a after FAE
Fumaric acid ester (FAE ) therapy has proved to be eective stimulation in vitro (3). TNF-a is a potent proin ammatory
in several multicentre trials, but while there are bene cial mediator and a likely candidate for gastrointestinal complaints
clinical eects, there are also some negative side eects (1). In (4) and ushing. In speculating that a reduction of FAE-
a recent prospective multicentre trial including 101 patients, induced TNF-a secretion would improve tolerability of the
69% reported adverse eects, mainly gastrointestinal com- compound, in a clinical survey we compared FAE therapy and
plaints (50%; cramps, diarrhoea) and ushing (31%), in the the combination of FAE plus pentoxifylline (PTX ), a potent
rst weeks after FAE treatment. These complaints led to suppressor of TNF-a release.
cessation of the treatment in 4 patients (2). Other reports
suggest a similar high incidence of side eects (1).
MATERIAL AND METHODS
One explanation for the adverse eects could be a FAE-
induced release of tumour necrosis factor-alpha (TNF-a) Forty-four adult patients (18 women and 26 men; mean age
during the initial phase of therapy. This hypothesis is supported 52.9) with moderate to severe psoriasis vulgaris were included
2001 Taylor & Francis. ISSN 0001-5555 Acta Derm Venereol 81
430 Letters to the Editor
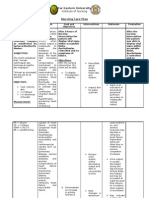
in this open-label prospective trial. Patients were randomly Table I. Side eects during therapy with fumaric acid ester
assigned to one of the two study groups (A and B). All (FAE) alone and in combination with pentoxifylline (PTX)
patients received a daily oral-systemic treatment of psoriasis
FAE FAE1 PTX
with FAE (Fumaderm ) in accordance with standard
(n 5 21) (n 5 23)
ascending doses as recommended by the German consensus
conference (1). The dose of FAE given in each group was Occurrence of side eects 76.2% 52.2%
therefore identical. In group B, patients additionally received Cessation of therapy due to side eects 19.0% 17.4%
PTX (23 400 mg/day, Trental 400; rst application simultan- Mean severity score ( SEM) for side eects 3.48 0.6 1.91 0.58*
eously with FAE ). Patients were also treated topically and
observed over an 8-week period. They were asked for adverse *p < 0.05 signi cantly lower than in patients with FAE monotherapy.
eects after weeks 3, 6 and 8. Severity of the side eects was SEM 5 standard error of the mean.
recorded using a scoring system (0 5 no side eects, 1 5 mild,
2 5 moderate, 3 5 severe, 4 5 very severe for each of the side potential additive antipsoriatic eects of combining TNF
eects). The chi-squared test and the Mann-Whitney U test inhibitors (e.g. higher dosages of PTX and neutralizing anti-
were used for comparing the groups. TNF antibodies) with FAE. Such combinations seem suitable,
since PTX and anti-TNF (7) have also been shown to be
RESULTS eective in treating psoriasis, due to the reduction of TNF-a
(8), and in reducing keratinocyte proliferation (9), suggesting
In group A (FAE monotherapy), 16 out of 21 patients showed
adverse eects; 4 patients ceased the FAE treatment, which is a potential additive antipsoriatic eect.
in line with earlier reports (2). The incidence was slightly
lower in group B (combination therapy FAE plus PTX ), REFERENCES
where 12 patients out of 23 reported adverse eects leading to
1. Mrowietz U, Christophers E, Altmeyer P. Treatment of severe
withdrawal from the study in 4 cases. The most frequent side
psoriasis with fumaric acid esters: scienti c background and guide-
eects in both groups were gastrointestinal complaints (dia- lines for therapeutic use. The German Fumaric Acid Ester
rrhoea, intestinal cramps) and ushing. Adverse eects were Consensus Conference. Br J Dermatol 1999; 141: 424 429.
less frequently reported in the patients receiving PTX 2. Mrowietz U, Christophers E, Altmeyer P. Treatment of psoriasis
co-application. A signi cant reduction in severity of all side with fumaric acid esters: results of a prospective multicentre study
eects was found in the patients with combination therapy (German Multicentre Study). Br J Dermatol 1998; 138: 456 460.
(Table I ). There was no evidence of a dierent response to 3. Asadullah K, Schmid H, Friedrich M, Randow F, Volk HD, Sterry
the antipsoriatic treatment between the two groups. W, et al. In uence of monomethylfumarate on monocytic cytokine
formation explanation for adverse and therapeutic eects in
psoriasis? Arch Dermatol Res 1997; 289: 623 630.
DISCUSSION 4. Neurath MF, Fuss I, Pasparakis M, Alexopoulou L, Haralambous
Our data provide rst evidence that an addition of PTX to S, Meyer zum Buschenfelde KH, et al. Predominant pathogenic
role of tumor necrosis factor in experimental colitis in mice. Eur
the standard FAE therapy regime may be a way to reduce the
J Immunol 1997; 27: 1743 1750.
adverse eects of FAE. We found a reduction of diarrhoea by
5. Beermann B, Ings R, Mansby J, Chamberlain J, McDonald A.
31%, of intestinal cramps by 48%, and of ush symptoms by Kinetics of intravenous and oral pentoxifylline in healthy subjects.
63% in the patients who received PTX additional to the FAE Clin Pharmacol Ther 1985; 37: 25 28.
therapy. It might be speculated that even more pronounced 6. Falanga V, Fujitani RM, Diaz C, Hunter G, Jorizzo J, Lawrence
(and statistically signi cant) eects could be achieved when PF, et al. Systemic treatment of venous leg ulcers with high doses
using higher concentrations of PTX. In fact, it is likely that of pentoxifylline: e cacy in a randomized, placebo-controlled trial.
the PTX plasma levels were not su cient to completely block Wound Repair Regen 1999; 7: 208 213.
TNF-a release. Peak plasma levels of 2.25 mg/ml were 7. Oh CJ, Das KM, Gottlieb AB. Treatment with anti-tumor necrosis
found after oral administration of 400 mg PTX (5), whereas factor alpha ( TNF-alpha) monoclonal antibody dramatically
100 mg/ml PTX is necessary to achieve su cient TNF-a inhibi- decreases the clinical activity of psoriasis lesions. J Am Acad
Dermatol 2000; 42: 829 830.
tion in vitro (own results, not shown). In concurrence with
8. Omulecki A, Broniarczyk-Dyla G, Zak-Prelich M, Choczaj-Kukula
this, Falanga et al. (6) have shown that higher doses of PTX A. Is pentoxifylline eective in the treatment of psoriasis? J Am
(800 mg three times a day) are more eective than lower doses Acad Dermatol 1996; 34: 714 715.
(400 mg three times a day) in treating venous leg ulcers. 9. Gilhar A, Grossmann N, Kahanovicz S, Reuven H, Cohen S, Eitan
Further studies, including placebo-controlled trials, should be A. Antiproliferative eect of pentoxifylline on psoriatic and normal
performed to analyse the reduction of side eects and the epidermis. Acta Derm Venereol 1996; 76: 437 441.
Acta Derm Venereol 81
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Role of Physiotherapy in Antenatal and Post-Natal Care: Dr. Venus Pagare (PT)Documento74 pagineRole of Physiotherapy in Antenatal and Post-Natal Care: Dr. Venus Pagare (PT)Haneen Jehad Um Malek100% (1)
- Eeg, PSG, Sleep DisordersDocumento48 pagineEeg, PSG, Sleep DisordersIoana MunteanuNessuna valutazione finora
- Eshre Guideline Endometriosis 2022Documento192 pagineEshre Guideline Endometriosis 2022Patricia100% (1)
- LaQshya Quality Improvement Cycles Resource MaterialDocumento344 pagineLaQshya Quality Improvement Cycles Resource Materialkparasher100% (1)
- Hemodialysis - Different AspectsDocumento321 pagineHemodialysis - Different AspectsIndera VyasNessuna valutazione finora
- Conversion DisorderDocumento27 pagineConversion DisorderKhalil Ullah100% (1)
- Internship Report Pharma CompanyDocumento19 pagineInternship Report Pharma CompanyMuhammad Haider Ali100% (1)
- Unit Plan (3) Child Health NursingDocumento5 pagineUnit Plan (3) Child Health Nursinggill priyaNessuna valutazione finora
- Efluvio TelogenoDocumento13 pagineEfluvio TelogenoVar AndaNessuna valutazione finora
- Cutaneous Warts (Common, Plantar, and Flat Warts) : AuthorsDocumento14 pagineCutaneous Warts (Common, Plantar, and Flat Warts) : AuthorsVar AndaNessuna valutazione finora
- Alopecia Areata ManejoDocumento14 pagineAlopecia Areata ManejoVar AndaNessuna valutazione finora
- Hiperhidrosis Generalizada y Sudoracion NocturnaDocumento13 pagineHiperhidrosis Generalizada y Sudoracion NocturnaVar AndaNessuna valutazione finora
- Rosacea ManejoDocumento18 pagineRosacea ManejoVar AndaNessuna valutazione finora
- Eritema Elevatum DiutinunDocumento8 pagineEritema Elevatum DiutinunVar AndaNessuna valutazione finora
- Curacion de Heridas y Tratamiento de HeridasDocumento17 pagineCuracion de Heridas y Tratamiento de HeridasVar AndaNessuna valutazione finora
- Melasma ActualizadoDocumento9 pagineMelasma ActualizadoVar AndaNessuna valutazione finora
- 10 1016@j Jaad 2014 01 663 PDFDocumento1 pagina10 1016@j Jaad 2014 01 663 PDFVar AndaNessuna valutazione finora
- Penfigoide Anti p200 Similar A EBA PDFDocumento30 paginePenfigoide Anti p200 Similar A EBA PDFVar AndaNessuna valutazione finora
- Ictiosis Trastornos Mendelianos de QueratinizacionDocumento48 pagineIctiosis Trastornos Mendelianos de QueratinizacionVar AndaNessuna valutazione finora
- Norland Swissray Dmo2Documento8 pagineNorland Swissray Dmo2Edison JmrNessuna valutazione finora
- Genitourinary System FinalDocumento8 pagineGenitourinary System FinalKristian DolletonNessuna valutazione finora
- Pharmacoeconomics - Part IIIDocumento29 paginePharmacoeconomics - Part IIISima JabbariNessuna valutazione finora
- DNRS 6630 Final Exam Week 11 February.Documento20 pagineDNRS 6630 Final Exam Week 11 February.Sandra JeffersonNessuna valutazione finora
- Broward Medical Examiner ReportDocumento42 pagineBroward Medical Examiner ReportrabdillNessuna valutazione finora
- Oral Probiotic Treatment of Lactobacillus Rhamnosus Lcr35® Prevents Visceral Hypersensitivity To A Colonic Inflammation and An Acute Psychological StressDocumento13 pagineOral Probiotic Treatment of Lactobacillus Rhamnosus Lcr35® Prevents Visceral Hypersensitivity To A Colonic Inflammation and An Acute Psychological StressMaria TejedaNessuna valutazione finora
- Bupa Hero Consolidated PDF (brochure+SOB+TOS)Documento64 pagineBupa Hero Consolidated PDF (brochure+SOB+TOS)yuki michaelNessuna valutazione finora
- Resume Viola RDHDocumento2 pagineResume Viola RDHapi-247540600Nessuna valutazione finora
- Nerium OleanderDocumento20 pagineNerium OleanderGeneizzel GotuatoNessuna valutazione finora
- Antenatal CareDocumento26 pagineAntenatal CarepluiedecielNessuna valutazione finora
- Nursing Seminar 1 SAS Session 2Documento9 pagineNursing Seminar 1 SAS Session 2ZiaNessuna valutazione finora
- Knowledge Deficit and Risk For DiarrheaDocumento3 pagineKnowledge Deficit and Risk For DiarrheaRico Mae ValenciaNessuna valutazione finora
- Fped 2019 00227Documento7 pagineFped 2019 00227Syaifudin LutfiNessuna valutazione finora
- Heidi Agustin Joseph Azevedo Alternative Nutrition CounselingDocumento16 pagineHeidi Agustin Joseph Azevedo Alternative Nutrition Counselingapi-242435158Nessuna valutazione finora
- Institute of Nursing: Far Eastern UniversityDocumento3 pagineInstitute of Nursing: Far Eastern UniversityaleccespirituNessuna valutazione finora
- Surveilans Terpadu Puskesmas: Umur (Tahun) 0-7hr 8-28hr 1 1-4 L P L P L P L PDocumento3 pagineSurveilans Terpadu Puskesmas: Umur (Tahun) 0-7hr 8-28hr 1 1-4 L P L P L P L PkusNessuna valutazione finora
- Arnica Montana - FayazuddinDocumento13 pagineArnica Montana - FayazuddinMohammad AtaNessuna valutazione finora
- Birth Defects and Prenatal DiagnosisDocumento49 pagineBirth Defects and Prenatal DiagnosiskurniaNessuna valutazione finora
- DownloadDocumento27 pagineDownloadKHAIRUNNISA FADILANessuna valutazione finora
- Medical Reimbursement Claim FormDocumento2 pagineMedical Reimbursement Claim FormHimanshu JainNessuna valutazione finora
- NSTP Common Module 2 Drug EducationDocumento33 pagineNSTP Common Module 2 Drug EducationMerylle Shayne GustiloNessuna valutazione finora
- Introduction To Chemicals in MedicinesDocumento5 pagineIntroduction To Chemicals in MedicinesP balamoorthyNessuna valutazione finora