Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Icbt05i2p139 PDF
Caricato da
SuperModTheHeroTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Icbt05i2p139 PDF
Caricato da
SuperModTheHeroCopyright:
Formati disponibili
S y m p o s i u m on G r o w t h and Its Disorders
Growth Hormone Therapy
Anurag Bajpai 1 and P.S.N. M e n o n
1Division of Pediatric Endocrinology, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi,
India and Department of Pediatrics, Armed Forces Hospital, Kuwait.
Abstract. Growth hormone (GH) therapy has revolutionized treatment of children with growth hormone deficiency (GHD).
Improved height outcome with final height in the target height range has been achieved in these children. Identification of
Creutzfeldt-Jakob disease, a deadly prion mediated disorder, in recipients of pituitary GH accelerated the transition from pituitary
derived GH to recombinant GH. Once daily subcutaneous administration of the freeze-dried preparation at evening is the
recommended mode of GH therapy. Studies have led to use of higher dose of GH for improving height outcome (0.33 mg/kg/
week or 0.14 IU/kg/day) albeit at a significantly high cost. Growth velocity increases from 3-4 cm/year before therapy to 10-
12 cm/year during the first two years of therapy and is maintained at 7-8 cm/year after a period of two years. Close follow-up
with regular clinical and laboratory monitoring is essential for achieving a desirable height outcome. A theoretical unlimited
supply has led to wide spread use of GH in a variety of disorders other than GHD. Initially started in children with Turner
syndrome, GH has now been used in chronic renal failure, idiopathic short stature and intrauterine growth restriction besides
a wide array of newly emerging indications. [Indian J Pedlatr 2005; 72 (2) : 139-144] Emaih psnmenon@hotmail.com
Key words : Growth hormone; Growth hormone deficiency; Idiopathic short stature; Tumer syndrome
Growth hormone (GH) therapy forms the cornerstone of IGF response and better metabolic profile compared to
management of children with growth hormone deficiency m o r n i n g or a f t e r n o o n a d m i n i s t r a t i o n . -~Once d a i l y
(GHD). Pituitary derived GH was used for over 25 years administration at evening is the recommended mode of
with r e m a r k a b l e success. Limited s u p p l y h o w e v e r GH therapy.
r e s t r i c t e d its w i d e s p r e a d use. I d e n t i f i c a t i o n of
Preparations and Mode of Administration
Creutzfeldt-Jakob disease, a d e a d l y p r i o n - m e d i a t e d
disorder, in recipients of pituitary GH accelerated the Freeze-dried preparations are the commonest forms of
transition from pituitary derived GH to recombinant GH. G H available. Liquid p r e p a r a t i o n s of G H h a v e the
A theoretical unlimited supply has led to widespread use advantage of ease of administration. A long acting analog
of GH in a variety of disorders other than GHD. of GH has shown promising results in initial studies. 6 GH
has traditionally been injected with a syringe. Automated
Route of Administration
pen devices have the advantage of ease of administration,
Intramuscular route was initially recommended for GH accuracy of dose and less inconvenience to the patient.
due to the possible immunogenic effect of subcutaneous
Dose Expression
injection. Efficacy, p h a r m a c o k i n e t i c effects and
immunogenic potential of subcutaneous injection of GH The dose of GH has traditionally been expressed as unit/
are similar to i n t r a m u s c u l a r a d m i n i s t r a t i o n . 1.2 kg/day. Recently there is a trend of using m g / k g / d a y or
Subcutaneous injection is currently the route of choice for m g / m 2 / w e e k for calculation of dose of GH. As per WHO
GH administration. Trials on intranasal administration of standards 1 mg of recombinant G H has a bioactivity
GH are under way. e q u i v a l e n t to 3 IU. Expressing dose by surface area
compared to b o d y weight has the advantage of lower
Time of Administration
v a r i a t i o n f r o m infancy to a d o l e s c e n c e and is m o r e
Pituitary derived GH was administered two to three times representative of body requirement. 7 Estimation of GH
in a week. Studies have shown that daily GH is superior dose a c c o r d i n g to b o d y w e i g h t is in p a r t i c u l a r
to intermittent administration with regard to growth, IGF nonphysiological in obese children as GH levels correlate
response and serum GH levels.3 Twice daily GH has not negatively with body fat content. Despite these limitations
b e e n s h o w n to be s u p e r i o r to once daily. 4 E v e n i n g GH dose is expressed according to body weight in most
administration of GH leads to higher GH levels, greater countries.
Correspondence and Reprint requests : Dr. P.S.N. Menon, Dosage
Consultant & Chairman, Department of Pediatrics, Armed Forces The endogenous production rate of GH is variable and
Hospital, PO Box 5819,Salmiya 22069,Kuwait. Fax : (965)4760324
Indian Journal of Pediatrics, Volume 72--February, 2005 139
Anurag Bajpai and P.S.N. Menon
ranges from 20 ~tg/kg/day during pre-pubertal period to Treatment of Concomitant Anterior Pituitary
35 ~tg/kg/day during puberty? Dose of 0.16 m g / k g / Deficiencies
week (0.07 I U / k g / d a y , 22 ~ t g / k g / d a y ) therefore
Cortisol should be the first hormone to be replaced in a
represents physiological replacement dose for GH. Initial
child with multiple pituitary hormone deficiency.
dose recommendations for patients with GHD have been
Replacement doses of glucocorticoids in these patients (8-
based on these estimates. Studies on GH therapy in GHD
12 mg/m2/day) are low compared to those with primary
have shown that this dose is unlikely to produce
adrenal insufficiency (12-15 mg/m2/day).
sustained catch-up growth and have led to use of higher
Mineralocorticoid replacement is not required. Free
dose for improving height outcome (0.33 mg/kg/week,
thyroxine (FF4) levels should be maintained in the normal
0.14 IU/kg/day, 45 Ilg/kg/day). In conditions other than
range. It is important to emphasize that overtly aggressive
GHD higher doses of GH are required to achieve
thyroid replacement may lead to inappropriate skeletal
pharmacological effects.
maturation and compromised height. Replacement of sex
hormones should be delayed (12 years in girls and 14
GH THERAPY IN DIFFERENT DISORDERS
years in boys) to provide adequate time for GH therapy.
The scope of GH therapy has been expanded dramatically Follow-up
in the last two decades with use in a variety of genetic
Children on GH therapy should be followed-up every
syndromes, skeletal dysplasias and chronic diseases.
three months. Evaluation at each visit should include
GHD however remains the most important indication of
measurements of height, weight, height SDS, growth
GH therapy.
velocity SDS and assessment for complications of therapy.
Growth Hormone Deficiency Bone age is of limited utility in follow-up of children on
GH therapy except for the patient nearing completion of
GH therapy has been shown to significantly improve statural growth. IGF-1 and IGFBP-3 levels should be
height outcome in GHD. Close follow-up with regular measured annually and maintained at high normal range
clinical and laboratory monitoring.is essential for for the age and gender of the child. ~4GH therapy may
achieving desirable height outcome. unmask hypothyroidism in children with borderline
Diagnosis thyroid status. Diabetogenic effect of GH may induce
insulin resistance and result in impaired glucose tolerance
The diagnosis of GHD should be based on a combination or overt type 2 diabetes mellitus. Blood sugar and FT4
of auxological and laboratory parameters. Compromised levels should be estimated after an interval of three, six
height (standard deviation score, SDS < -2) with low and twelve months of initiation of GH therapy. Thereafter
growth velocity (SDS < -1) in the presence of annual estimation of blood sugar and FT4 levels should
inappropriate response to two stimulation tests is be performed. It is important to emphasize that intra-
required for establishing the diagnosis of GHD. 9 Recent cranial tumors may be missed on initial CNS imaging
recommendations suggest that peak GH levels below 10 leading to a misdiagnosis of idiopathic GHD. These
ng/ml are diagnostic of GHD compared to previously children should be closely monitored for development of
used levels of 5-7 ng/ml. features indicating CNS involvement.
Initiating Therapy Response to Therapy
GH therapy should be initiated only after other anterior GH therapy is associated with significant improvement in
pituitary hormone deficiencies have been excluded or growth velocity, which increases from 3-4 cm/year before
treated. Parents should be explained about the cost of therapy to 10-12 cm/year during the first two years of
therapy and the need of long-term follow-up. Giving GH treatment. ~s This catch-up response, however is not
for less than two years is futile and should be strongly maintained and growth velocity declines to 7-8 cm/year
discouraged. Initial GH dose is determined according to after a period of two years. This apparent loss of effect of
age, skeletal maturation and pubertal status of the patient. GH does not represent failure of therapy but
Thus while lower dose may be acceptable in a four-year- demonstrates growth at a normal rate following
old child, higher doses are definitely indicated in a nine- correction of GH deficient state. ~6Inappropriate response
year-old girl approaching puberty. Prediction models, a to GH therapy should prompt evaluation of compliance,
recent advance in the management of children with GHD, injection technique, hypothyroidism or reconsideration of
may be used for determining appropriate GH dose for the the diagnosis of GHD (Table 2). Decline in growth
patient. ~~ Initial dose of 0.17-0.33 m g / k g / w e e k (0.07- velocity following an initial increase suggest the
0.14 IU/kg/day, or 4.6-9.2 mg/m2/week) has been used possibility of unmasking of hypothyroidism while no
for treatment of GHD. Studies have however shown that response should prompt reconsideration of the diagnosis
higher doses of GH may be helpful in improving height of GHD (Fig 1). Doses of GH should be adjusted
outcome albeit at a significantly higher cost. ~2,13 according to growth velocity, pubertal status and IGF-1
140 Indian Journal of Pediatrics, Volume 72--February, 2005
Growth Hormone Therapy
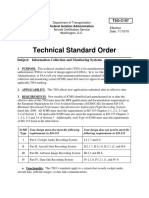
TASTE1. Follow-up of Patients on GH Therapy height SDS -1.3) c o m p a r e d to GH alone (height SDS -
Parameter Frequency 2.7). ~ GnRH analog therapy should be used for a period
of at least two years as treatment for shorter duration may
Clinical lead to initial acceleration of puberty due to the agonist
Height SDS 3 months activity of the hormone.
Growth velocity SDS 3 months
Complications of therapy 3 months D i s c o n t i n u a t i o n of Therapy
Injection technique, compliance 3 months
GH therapy should be continued till final height has been
Laboratory achieved. Growth velocity below 2 cm in the preceding
Free thyroxine (FT4) At 3, 6 and 12 mo of therapy, year with bone age of 14 years in girls and 16 years in
Annually thereafter boys is considered as indicator of final height. The issue of
Blood sugar Annually
IGF-1, IGFBP-3 Annually continuation of GH therapy during adulthood should be
discussed with the family.
TAerE2. Reasons for Poor Response to GH Therapy Effect o n Final H e i g h t
Drug related Lower dose Studies involving a large number of patients with GHD
Poor compliance have s h o w n significant i m p r o v e m e n t in final height
Improper technique following GH therapy. 2~26Most of these studies however
Disease related Wrong diagnosis
GHD type IA with anti GH antibodies have used historical controls for comparison. Untreated
Patient related severe G H D is associated with final height SDS in the
Poor nutrition range of--4 to -6 while long term GH therapy is associated
Malabsorption with final height SDS in the range of -1 to -2. This could
Complication related Hypothyroidism translate in a height gain of 20-30 cm. The efficacy of GH
in children with severe G H D remains unequivocal; its
12 impact on milder forms of disease may not be as dramatic.
Factors I n f l u e n c i n g O u t c o m e
GHD
An understanding of factors influencing height outcome
thyrodism is helpful in appropriate management of these children.
~" 4 Studies have shown that early diagnosis, higher dose,
J ~ Non-GHD higher target height SDS, greater height SDS at the time of
~2
onset of p u b e r t y and longer d u r a t i o n of t h e r a p y are
0 associated with better height outcome. 2~29Height gain
0 1 yr 2 yr 3 yr 4 yr 61ff during first year of therapy is an important predictor of
Treatment Duration (Years) overall response. This emphasizes the need of appropriate
Fig 1. Response following GH therapy management and close monitoring during initial part of
GH therapy. Table 3 s u m m a r i z e s factors influencing
and IGFBP-3 levels. Prediction models have been used for height outcome in GHD and interventions directed at
optimizing GH dose. 1~ improving outcome. Children with combined pituitary
Optimization of Therapy During Puberty deficiency have better height outcome compared to those
with isolated GHD. ~ This may be due to delay in puberty
Pubertal g r o w t h in children with G H D is similar to due to concomitant gonadotropin deficiency.
normal individuals27,~8 Compromised height at puberty is
therefore invariably associated with compromised final TABrE3. Factors Influencing Height Outcome in GHD and
height. Two different approaches have been tried for Possible Intervention for Improving Outcome
maximizing benefits of GH therapy in individuals who
are short at the onset of puberty. In the first approach Factor influencing outcome Impact Intervention
higher doses of GH (up to 0.15-0.2 I U / k g / d a y ) have been Age at initiation Negative Early diagnosis
used during puberty. 19In a randomized controlled trial Initial height SDS Positive Early diagnosis
high dose GH during puberty (0.7 m g / k g / w e e k , 0.3 IU/ Height SDS at puberty Positive
kg/day) was associated with significantly higher growth Pubertal height gain Positive GnRH analog,
velocity compared to lower dose (0.3 m g / k g / w e e k , 0.13 higher dose
Duration of therapy Positive Increaseduration
I U / k g / d a y ) ? ~ Prolongation of puberty with the use of Dose Variable Higher dose
gonadotropin releasing hormone analogs forms the basis Target height Positive -
of the other approach. 21 In a randomized controlled trial Height gain during first year Positive High initial dose,
combination of GnRH analog with GH for a period of close monitoring
three years was associated with better outcome (final Multiple pituitary defects Positive
Indian Journal of Pediatrics, Volume 72--February, 2005 141
Anurag Bajpai and P.S.N. Menon
Cost of T h e r a p y growth. Recent studies have shown that GHD in adults is
One of the major limitations of GH therapy is high cost. In associated with significant complications in the form of
a study conducted in United States the cost of G H therapy risk of atherosclerosis, altered body composition and poor
for a 20 kg child with G H D was estimated to be $15,000 quality of life. 39 These complications improve with G H ? ~
per year. In India the approximate cost for a 20 kg child These observations have led to the recommendations of
would be Rs 200,000 per year. Cost considerations are the G H t h e r a p y in adults with G H D . Retesting for G H D
major limiting factors of wide spread use of G H therapy should be performed after discontinuing the d r u g for a
in resource-poor settings. period of 1 month. A significant number of children with
isolated idiopathic G H D (50-70%) w o u l d not be G H
A d v e r s e Effects
deficient during re-testing. This m a y reflect inaccuracies
Recombinant G H has been s h o w n to be safe during its of initial G H test on one h a n d and transient nature of
w i d e s p r e a d use (Table 4). The m o s t c o m m o n initial G H D on the other. Patients with peak G H levels below 3
adverse effects include headache and v o m i t i n g due to n g / m l (cutoff levels for adults) should be started on 0.5
pseudotumor cerebri and edema due to fluid and sodium m g / d a y of GH. These r e c o m m e n d a t i o n s h o w e v e r are
retention. 31 These effects improve over time without any difficult to follow in resource-poor setting.
intervention. It is however important to emphasize that
headache in a child with a diagnosis of idiopathic G H D GH THERAPY IN NON-GHD SHORT STATURE
m a y be a pointer of an intra-cranial t u m o r and should
p r o m p t a p p r o p r i a t e CNS i m a g i n g . Initial r e p o r t s Turner S y n d r o m e
s u g g e s t e d an i n c r e a s e d risk of l e u k e m i a in subjects
Turner syndrome was the first disorder besides G H D for
receiving GH; subsequent studies have however failed to
which G H therapy was a p p r o v e d . L o n g - t e r m studies
substantiate these findings. 32-~The use of G H in children
h a v e suggested significant i m p r o v e m e n t in final height
with intra-cranial tumors is In particular a major cause of
following G H ranging from 4-9 cm over predicted height
concern due to the theoretical possibility of reappearance
at initiation of therapy. 41-43The dose of G H in T u r n e r
of tumors. In a large study involving 1000 children with
s y n d r o m e is higher c o m p a r e d to G H D (0.35 m g / k g /
intra-cranial malignancy G H therapy was not associated
week or 0.15 I U / k g / d a y ) . Use of even higher dose (0.3
with increased risk of t u m o r recurrence. ~ G H therapy
I U / k g / d a y ) has been s h o w n to produce height gain in
m a y u n m a s k h y p o t h y r o i d i s m and induction of insulin
the range of 16 cm. 44 Early G H therapy is r e c o m m e n d e d
resistance mandating the need of close follow-up for these
for maximizing benefits. G H therapy should be started in
complications during therapy. 36 Slipped capital femoral
girls with Turner syndrome when height falls below 5 th
e p i p h y s e s and obstructive sleep a p n e a h a v e not b e e n
centile for the normal growth curve. G H stimulation test
s h o w n to be higher in children receiving G H t h e r a p y
is not required. Oxandrolone (50 ~tg/kg/day) should be
compared to children with G H D who are not on GH. 37~
added after the age of 8 years. Early initiation of G H along
Therapy F o l l o w i n g C o m p l e t i o n of Statural G r o w t h with delayed induction of p u b e r t y (at least four years
Initially G H t h e r a p y w a s limited to p e r i o d s of active a f t e r s t a r t i n g G H ) c o m b i n e d w i t h o x a n d r o l o n e is
TaSLE4. Adverse Effects with GH Therapy
Adverse effect Incidence Suggested intervention
Psuedotumor cerebri* 0.16%/year Rule out CNS tumor
Glucose intolerance 1% Reversible
Slipped capital femoral epiphyses** 70-150/lO0000/year Orthopedic evaluation
Hypothyroidism Thyroxin replacement
Recurrence of tumor Unproven Delay treatment
Second malignancy Unproven
* Higher in Turner syndrome and chronic renal failure
**Higher in organic GHD
TABLE5. Benefits of GH Therapy for Established Indications
Disorder Indication Initial dose Benefit Evidence
GHD All subjects 0.07-0.1 IU/kg/d 15-20 cm Definite benefit
Turner Height < 5~'centile 0.14-0.2 IU/kg/d 6-8 cm Definite benefit
CRF All subjects 0.14-0.2 IU/kg/d 6-8 cm Unclear
ISS Height SDS < -3 0.14-0.2 IU/kg/d 4-6 crn Questionable
IUGR No catch up growth 0.10-0.2 IU/kg/d 8-10 cm Unclear
Prader Willi All subjects 0.14-0.2 IU/kg/d 15-20 cm Definite benefit
CRF - Chronic renal failure, ISS - Idiopathic short stature, IUGR - Intrauterine growth restriction
142 Indian Journal of Pediatrics, Volume 72--February, 2005
Growth Hormone Therapy
a s s o c i a t e d w i t h best h e i g h t o u t c o m e in T u r n e r o u t c o m e h o w e v e r r e m a i n s u n c l e a r in m o s t of these
syndrome. 45 conditions. GH therapy has also been tried in catabolic
disorders like bums, HIV infection and anorexia nervosa.
Chronic Renal Failure (CRF)
Chronic renal failure is associated with significant growth REFERENCES
c o m p r o m i s e that persists despite renal r e p l a c e m e n t
1. Russo L, Moore WV. A comparison of subcutaneous and
therapy. High dose G H i m p r o v e s height o u t c o m e in
intramuscular administration of human growth hormone in
children with CRF. ~ In a randomized controlled study therapy of human growth hormone deficiency. J Clin
involving 38 pre-pubertal children with CRF, treatment Endocrinol Metab 1982;55 : 1003-1006.
with GH led to increase in height SDS by 1.4 compared to 2. Wilson DM, Baker B, Hintz RL, Rosenfield RG. Subcutaneous
decline in height SDS by 0.6 in the control group. 47 This versus intramuscular growth hormone therapy: growth and
response however is not sustained over a long period of acute somatostatin response. Pediatrics 1985;76: 361-364.
3. MacGillivary MH, Bapista J, Johanson A. Outcome of a four-
time without kidney transplantation. year randomized study of daily versus three times weekly
Idiopathic Short Stature (ISS) somatotropin treatment in prepubertal naive growth hormone
deficient children. J Clin Endocrinol Metab 1996;81- 1806-1809.
Idiopathic short stature represents a mix of children with 4. Van Teunenbroek A, de Munick Keizer-SchramaS, Stijnen T et
al. Growth response and levels of growth after two years
mild defects of the GH and IGF axis and low genetic
growth hormone treatment are similar for once or twice daily
potential. Marginal benefits have been reported with the regimen in girls with Turner syndrome. Clin Endocrinol
use of GH. A gain of 5-7 cm c o m p a r e d to historical (Oxford) 1997;46: 451-459.
controls was observed in a study using high dose GH 5. ZadikZ, Liberman E, Altman Y, Chen M, LimoniY, Landau H.
(0.33 m g / k g / w e e k or 0.14 I U / k g / d a y ) . 4s In a meta- Effect of timing of growth hormone on plasma growth-
analysis involving 1089 patients with idiopathic short hormone-binding activity, insulin like growth factor-1 and
growth in children with subnormal secretion of growth
stature treated with GH height gain of 4-6 cm was noted. 49 hormone. Horm Res 1993;39: 188-191.
The cost of therapy remains exorbitant at $13000 for every 6. Silverman BL, Blethen SL, Reiter EO, Attie KM, Neuwirth RB,
cm of height gained. Trial of GH therapy in children with Ford KM. A long-acting human growth hormone (Nutropin
idiopathic short stature should be continued for at least Depot): efficacyand safety following two years of treatment in
six months. The d r u g m a y be discontinued in children children with growth hormone deficiency.
J Pediatr EndocrinoI Metab 2002; 15 (Suppl 2): 715-722.
who do not show catch up growth. GnRH analog could be
7. Wit JM. Growth hormone therapy. Clinical Endocrinol Metab
combined with GH for maximizing height gain. 2002; 16: 483-504.
8. Martha PM, Gorman KM, Blizzard RM, Rogol AD, Veldhuls
Intra-uterine Growth Restriction (IUGR)
JD. Endogenousgrowth hormone secretion and clearance rates
IUGR comprises of a heterogeneous mix of individuals in normal boys, as determined by deconvolution analysis:
relationship to age, pubertal status and body mass. J Clin
with genetic, environmental and placental compromise.
Endocrinol Metab 1992;74: 336-344.
Majority of these patients show catch up g r o w t h with 9. Hintz RL. Management of disorders of size. In Brook CGD,
final height in the low normal range. H o w e v e r 15% of Hindmarsh PC, eds. Clinical Pediatric Endocrinology, 4~ edn.
these individuals have compromised height and are at London: Blackwell Science 2001; 124-139.
risk of s h o r t stature. In a r a n d o m i z e d c o n t r o l trial 10. Ranke MB, Lindberg A, Chatelain P, Wilton P, Cutfield W,
Albertson-Wikland K, Price DA. Derivation and validation of
i n v o l v i n g 54 c h i l d r e n w i t h IUGR, G H t h e r a p y w a s
a mathematical model for predicting the response to
a s s o c i a t e d w i t h i n c r e a s e in h e i g h t SDS by 2 SDS. 5~ exogenous recombinant human growth hormone (GH) in
Importantly, children receiving lower dose (0.1 I U / k g / prepubertal children with GH deficiency. J Clin Endocrinol
day) had similar height gain compared to those on higher Metab 1999;84 : 1174-1183.
dose (0.2 I U / k g / d a y ) . 11. Muller V, HoepffnerW, Kiess W, Keller E. Prediction of height
velocity of prepubertal children with growth hormone
Prader-Willi S y n d r o m e deficiency in the first year of treatment with recombinant
human growth hormone. J Pediatr Endocrinol Metab 2000; 13:
C h i l d r e n w i t h this s y n d r o m e h a v e s i g n i f i c a n t 893-897.
complications like obesity, low muscle mass, hypotonia 12. Radetti G, Buzi F, Paganini C, Pilotta A, Felappi B. Treatment
and compromised height. GH therapy in a dose of 0.1 I U / of GH-deficient children with two different GH doses: effect
k g / d a y has been a s s o c i a t e d with i m p r o v e d h e i g h t on final height and cost-benefit implications. Eur ] Endocrinol
2003; 148:515-518.
outcome, fat mass, b o d y composition and respiratory 13. BlethenSL, Bapista J, Kuntze J, Foley T, LaFranchi S, Johanson
functions. 5~ A. Adult height in growth hormone deficient children treated
Other Disorders with biosyntheticGH: the Genetech growth study group. ] Clin
Endocrinol Metab 1997;82: 418-420.
The list of d i s o r d e r s for w h i c h GH has been used is 14. Tanaka T, Cohen P, Clayton PE, Laron Z, Hintz TL,
i n c r e a s i n g e v e r y day. F a v o r a b l e results h a v e b e e n Sizoneneko PC. Diagnosis and management of growth
reported in dysmorphic syndromes like Seckel and Silver hormone deficiency in childhood and adolescence. Part 2:
Growth hormone treatment in growth hormone deficient
Russel s y n d r o m e s a n d b o n e d i s o r d e r s like skeletal children. Growth Horm IGF Res 2002; 12: 323-341.
dysplasia and h y p o p h o s p h a t e m i c rickets. Long-term 15. Rosenfield GR, Cohen P. Disorders of growth hormone/
Indian Journal of Pediatrics, Volume 72--February, 2005 143
Anurag Bajpal and P.S.N. Menon
insulin like growth factor and action. In Sperling MA, ed. occurrence of leukemia in growth hormone treated patients in
Pediatric Endocrinology, 2~ edn. Philadelphia, WB Saunders, Japan. J Clin Endocrinol Metab 1999; 84: 1961-1965.
2002; 211-288. 35. Swerdkow AJ, Reddubgius RE, Higgins CD et al. Growth
16. Clayton PE, Cowell CT. Safety issues in children and hormone treatment of children with brain tumors and risk of
adolescents during growth hormone therapy- a review. recurrence. J Clin Endocrinol Metab 2000; 85" 44~4A4~9.
Growth Horm IGF Res 2000; 10: 306-317. 36. Blethen SL, Allen DB, Graves D, August G, Moshang T,
17. Buckler JM. A longitudinal study of adolescent growth. Rosenfield R. Safety of recombinant deoxyribonucleic acid
London, Springer 1990. derived growth hormone: the national cooperative growth
18. Tanaka T, Konatsu K, Takada G, Miyashita M, Ohno T. study experience. J Clin Endocrinol Metab 1996;81: 1704-1710.
Prediction of adult height in healthy Japanese children. Acta 37. Rappaport EB, Fife D. Slipped capital femoral epiphysis in
Pediatr 1996; 417 (suppl): 57-60. growth hormone deficient patients. Am J Dis Child 1985; 139:
19. Stanhope R, Uruena M, Hindmarsh P, Leiper AD, Brook CG. 396-399.
Management of growth hormone deficiency through puberty. 38. Blethen SL, Rundle AC. Slipped capital femoral ephiphysis in
Acta Pediatr Scand 1998; 372 (suppl): 47-52. children treated with growth hormone. Horm Res 1996;46:113-
20. Albertson-Wikland K, Aim F, Aronsson S et al. Effect of 116.
growth hormone (GH) during puberty in GH-deficient 39. Vahi N, Juul A, Jorgenesen JO et al. Continuation of growth
children: preliminary results form an ongoing trial with hormone (GH) treatment I GH deficient patients during
different dose regimens. Acta Pediatr 1998; 428 (suppl): 80-84. transition form childhood to adulthood: a two year placebo-
21. Tanaka T, Satoh M, Yasunaga T, Horikawa R, Tanae A, controlled study. J Clinical Endocrinol Metab 2000;85: 1874-1881.
Katsumata N, Tachibana K, Nose O, Hibi I. When and how to 40. SaggeseG, Ranke MB, Saenger Pet al. Diagnosis and treatment
combine growth hormone with a luteinizing hormone- of growth hormone deficiency in children and adolescents:
releasing hormone analogue. Acta Pediatr 1999;Supp188: 85-88. towards a consensus. Ten years after availability of
22. Merciq MV, Eggers M, Avila A, Cutler GB Jr, Cassorola F. recombinant growth hormone. Horm Res 1998;50: 320-340.
Near final height in pubertal growth hormone (GH) deficient 41. Rosenfield R, Attie K, Frane Jet al. Growth hormone therapy
parents treated with GH alone or in combination with of Turner syndrome: beneficial effect on adult final height. J
leutenizingreleasing hormone analog: results of a prospective, Pediatr 1998; 132 : 319-324.
randomized trial. J Clin Endocrinol Metab 2000; 85: 569-573. 42. Carel J, Mathivon L, Gendrel C et al. Near normalization of
23. Cutfield WS, Lindberg A, Chatelain Pet al. Final height final height with adapted doses of growth hormone in Turner
following growth hormone treatment idiopathic growth syndrome. J Clin Endocrinol Metab 1998; 83: 1462-1466.
hormone deficiency in KIGS. In Ranke MB, Wilton P, eds. 43. NiUson K, Albertson-Wikland K, Alto J et al. Improved final
Growth Hormone Therapy in KIGS- 10 Year Experience. height in girls with Turner syndrome treated with growth
Heidelberg 1999. Pp 93-109. hormone and oxandrolone. J Clin Endocrinol Metab 1996; 81:
24. August GP, Julius JR, Blethen SL. Adult height in growth 635-640.
hormone deficient children treated with biosynthetic GH. The 44. Sas T, de Munic Keizer-Schrama S, Stijen T et aL Near-
national cooperative growth study experience. Pediatrics 1998; normalization of heights in girls with Turner syndrome after
49: 80-85. long term growth hormone treatment: results of a randomized
25. Cacciari E, Cicognani A, Pirazolli Pet al. Final height of dose trial. J Clin Endocrinol Metab 1999; 84: 4607-4612.
patients treated for isolated GH deficiency examination on 83 45. Saenger P. Albertson-Wikland K, Cowy Get al. Recommen-
patients. Eur J Endocrinol 197; 137: 53-60. dations of diagnosis and management of Turner syndrome. J
26. Ranke MB, Price DA, Albertsson-Wikland K, Maes M, Lindbe Clin Endocrinol Metab 2001; 86: 3061-3069.
A. Factors determining pubertal growth and final height in 46. Hokken-Kolega A, Mulder P, De Jong R et al. Long term effects
growth hormone treatment of idiopathic growth hormone of growth hormone treatment on growth and puberty in
deficiency. Horm Res 1997;48: 62-71. patients with chronic renal insufficiency. Pediatr Nephro12000;
27. Bums EC, Tanner JM, Preece MA, Cameron N. Final height 14: 701-706.
and pubertal development in 55 children with idiopathic 47. Haffner D, Schaefer F, Nissel R, Wuhl E, Tonshoff B, Mehls O.
growth hormone deficiency. Eur J Pediatr 1981; 137 : 155-164. Effect of growth hormone treatment on the adult height of
28. Hibi I, Tanaka T. Final height of patients with idiopathic children with chronic renal failure. German Study Group for
growth hormone deficiency after long-term growth hormone Growth Hormone Treatment in Chronic Renal Failure. N Engl
treatment. Committee for Treatment of Growth Hormone J Med 2000 28; 343: 923-930.
Deficient Children, Growth Science Foundation, Japan. Acta 48. Buchlis JG, Irizarry L, Crotzer BC et al. Comparison of final
Endocrinol (Copenh) 1989; I20: 409-415. height of growth hormone treated versus untreated children
29. Rikken MB, Massa GG, Wit JM. Final height in a large cohort with idiopathic growth failure. J Clin Endocrinol Metab 1998;83:
of Dutch patients with growth hormone deficiency treated 1075-1079.
with growth hormone. Horm Res 1997;48: 62-71. 49. Van Pareren Y, Mulder P, Houdijk M, Jansen M, Reeser M,
30. Tanaka T, Takano K, Igarashi Y et al. Growth hormone (GH) Hokken-Koelega A. Adult height after long-term, continuous
treatment and puberty in GH treated GH children. Clin Pediatr growth hormone (GH) treatment in short children born small
Endocrinol 1999; 8 (Suppl 12): 37-44. for gestational age: results of a randomized, double-blind,
31. Lampit M, Nave T, Hochberg Z. Water and sodium retention dose-response GH trial. J Clin Endocrinol Metab 2003; 88: 3584-
during short-term administration of growth hormone to short 3590.
normal children. Horm Res 1998; 50: 83-88. 50. Coutant R, Carel JC, Letrait M, Bouvattier C, Chatelain P,
32. Watanabe S, 'I'sunematsu Y, Fujimoto J, Korniyama A. Coste Jet al. Short stature associated with intrauterine growth
Leukemia in patients treated with growth hormone. Lancet retardation: final height of untreated and growth hormone-
1989; 80: 822-825. treated children. J Clin Endocrinol Metab 1998; 83: 1070-1074.
33. Allen DB, Rundle AC, Graves DA, Blethen SL. Risk of 51. Myers SE, Carrel AL, Whitman BY, Allen DB. Sustained
leukemia in children with growth hormone: review and benefit after 2 years of growth hormone treatment on body
reanalysis. J Pediatr 1997; 131 : $32-$36. composition, fat utilization, physical strength, agility and
34. Nishi Y, Tanaka T, Takano K et al. Recent status in the growth in Prader-WiUisyndrome. Eur J Pediatr 1999; 158 : 245-
249.
144 Indian Journal of Pediatrics, Volume 72--February, 2005
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- 1ST Term J1 Fine Art-1Documento22 pagine1ST Term J1 Fine Art-1Peter Omovigho Dugbo100% (1)
- Propp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeDocumento10 paginePropp Function's Types:: 1-Absentation: One of The Members of A Family Absents Himself From HomeRohith KumarNessuna valutazione finora
- Tso C197Documento6 pagineTso C197rdpereirNessuna valutazione finora
- FT FocusDocumento19 pagineFT Focusobi1kenobyNessuna valutazione finora
- Online Shopping MallDocumento17 pagineOnline Shopping MallMerin LawranceNessuna valutazione finora
- Hansen Aise Im Ch12Documento66 pagineHansen Aise Im Ch12Rizki19maretNessuna valutazione finora
- EPSS 627: DescriptionDocumento2 pagineEPSS 627: DescriptionudayakumartNessuna valutazione finora
- RIBA PoWUpdate 131009 ProbynMiersDocumento28 pagineRIBA PoWUpdate 131009 ProbynMiersYellowLightNessuna valutazione finora
- Shades Eq Gloss Large Shade ChartDocumento2 pagineShades Eq Gloss Large Shade ChartmeganNessuna valutazione finora
- Module 4 How To Make Self-Rescue Evacuation Maps?Documento85 pagineModule 4 How To Make Self-Rescue Evacuation Maps?RejieNessuna valutazione finora
- @InglizEnglish-4000 Essential English Words 6 UzbDocumento193 pagine@InglizEnglish-4000 Essential English Words 6 UzbMaster SmartNessuna valutazione finora
- AREMA Shoring GuidelinesDocumento25 pagineAREMA Shoring GuidelinesKCHESTER367% (3)
- 2018 H2 JC1 MSM Differential Equations (Solutions)Documento31 pagine2018 H2 JC1 MSM Differential Equations (Solutions)VincentNessuna valutazione finora
- 2011 - Papanikolaou E. - Markatos N. - Int J Hydrogen EnergyDocumento9 pagine2011 - Papanikolaou E. - Markatos N. - Int J Hydrogen EnergyNMarkatosNessuna valutazione finora
- T10 - PointersDocumento3 pagineT10 - PointersGlory of Billy's Empire Jorton KnightNessuna valutazione finora
- Haymne Uka@yahoo - Co.ukDocumento1 paginaHaymne Uka@yahoo - Co.ukhaymne ukaNessuna valutazione finora
- Whitepaper ITES Industry PotentialDocumento6 pagineWhitepaper ITES Industry PotentialsamuraiharryNessuna valutazione finora
- EC105Documento14 pagineEC105api-3853441Nessuna valutazione finora
- COMMISSIONING COUPLE Aafidavit SANKET DOCTORDocumento2 pagineCOMMISSIONING COUPLE Aafidavit SANKET DOCTORYogesh ChaudhariNessuna valutazione finora
- Encapsulation of Objects and Methods in C++Documento46 pagineEncapsulation of Objects and Methods in C++Scott StanleyNessuna valutazione finora
- Vignyapan 18-04-2024Documento16 pagineVignyapan 18-04-2024adil1787Nessuna valutazione finora
- Makerere University Is Inviting Applications For Undergraduate Admissions On Private Sponsorship For Academic Year 2015/2016Documento9 pagineMakerere University Is Inviting Applications For Undergraduate Admissions On Private Sponsorship For Academic Year 2015/2016The Campus TimesNessuna valutazione finora
- 3.2.1 The Role of Market Research and Methods UsedDocumento42 pagine3.2.1 The Role of Market Research and Methods Usedsana jaleelNessuna valutazione finora
- Crown BeverageDocumento13 pagineCrown BeverageMoniruzzaman JurorNessuna valutazione finora
- Bakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TDocumento46 pagineBakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TAlif NakyukoNessuna valutazione finora
- The Attachment To Woman's Virtue in Abdulrazak Gurnah's Desertion (2005)Documento7 pagineThe Attachment To Woman's Virtue in Abdulrazak Gurnah's Desertion (2005)IJELS Research JournalNessuna valutazione finora
- DescriptiveDocumento1 paginaDescriptiveRizqa Anisa FadhilahNessuna valutazione finora
- Travelstart Ticket (ZA10477979) PDFDocumento2 pagineTravelstart Ticket (ZA10477979) PDFMatthew PretoriusNessuna valutazione finora
- SetupDocumento4 pagineSetupRsam SamrNessuna valutazione finora
- Tanque: Equipment Data SheetDocumento1 paginaTanque: Equipment Data SheetAlonso DIAZNessuna valutazione finora