Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Malaria Research
Caricato da
YosfikriansyahYosfiqarCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Malaria Research
Caricato da
YosfikriansyahYosfiqarCopyright:
Formati disponibili
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Protection against a Malaria Challenge
by Sporozoite Inoculation
Meta Roestenberg, M.D., Matthew McCall, M.D., Joost Hopman, M.D.,
Jorien Wiersma, Adrian J.F. Luty, Ph.D., Geert Jan van Gemert, B.Sc.,
Marga van de Vegte-Bolmer, B.Sc., Ben van Schaijk, M.Sc., Karina Teelen,
Theo Arens, Lopke Spaarman, B.Sc., Quirijn de Mast, M.D., Will Roeffen, Ph.D.,
Georges Snounou, Ph.D., Laurent Rnia, Ph.D., Andre van der Ven, M.D.,
Cornelus C. Hermsen, Ph.D., and Robert Sauerwein, M.D.
A bs t r ac t
Background
From the Departments of Medical Micro- An effective vaccine for malaria is urgently needed. Naturally acquired immunity to
biology (M.R., M.M., J.H., J.W., A.J.F.L., malaria develops slowly, and induction of protection in humans can be achieved
G.J.G., M.V.-B., B.S., K.T., T.A., L.S., W.R.,
C.C.H., R.S.) and General Internal Medi- artificially by the inoculation of radiation-attenuated sporozoites by means of more
cine (Q.M., A.V.), Radboud University than 1000 infective mosquito bites.
Nijmegen Medical Center, Nijmegen, the
Netherlands; the Department of Parasi-
tology, INSERM Unit 511, Hpital Piti Methods
Salptrire, and the Universit Pierre et We exposed 15 healthy volunteers with 10 assigned to a vaccine group and 5 as-
Marie Curie both in Paris (G.S.); and signed to a control group to bites of mosquitoes once a month for 3 months
the Laboratory of Malaria Immunobiology,
Singapore Immunology Network, Agency while they were receiving a prophylactic regimen of chloroquine. The vaccine group
for Technology and Research, Biopolis, was exposed to mosquitoes that were infected with Plasmodium falciparum, and the
Singapore (L.R.). Address reprint requests control group was exposed to mosquitoes that were not infected with the malaria
to Dr. Sauerwein at the Department of
Medical Microbiology 268, Radboud Uni- parasite. One month after the discontinuation of chloroquine, protection was as-
versity Nijmegen Medical Center, P.O. Box sessed by homologous challenge with five mosquitoes infected with P. falciparum.
9101, 6500 HB Nijmegen, the Netherlands, We assessed humoral and cellular responses before vaccination and before the chal-
or at r.sauerwein@mmb.umcn.nl.
lenge to investigate correlates of protection.
Drs. Roestenberg and McCall contributed
equally to this article. Results
N Engl J Med 2009;361:468-77. All 10 subjects in the vaccine group were protected against a malaria challenge with
Copyright 2009 Massachusetts Medical Society. the infected mosquitoes. In contrast, patent parasitemia (i.e., parasites found in the
blood on microscopical examination) developed in all five control subjects. Adverse
events were mainly reported by vaccinees after the first immunization and by con-
trol subjects after the challenge; no serious adverse events occurred. In this model,
we identified the induction of parasite-specific pluripotent effector memory T cells
producing interferon-, tumor necrosis factor , and interleukin-2 as a promising
immunologic marker of protection.
Conclusions
Protection against a homologous malaria challenge can be induced by the inocula-
tion of intact sporozoites. (ClinicalTrials.gov number, NCT00442377.)
468 n engl j med 361;5 nejm.org july 30, 2009
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Protection against a Malaria Challenge by Sporozoite Inoculation
M
alaria is responsible for a sig- induced by this approach in humans and to ex-
nificant burden of morbidity and mor- plore the immune responses elicited.
tality in the developing world, and an
effective vaccine against this disease is urgently Me thods
needed.1 Despite decades of research, a licensed
vaccine is still not available, largely because im- Study Subjects
munity to Plasmodium falciparum malaria is consid- We recruited 15 healthy volunteers between the
ered difficult to acquire, whether through natu- ages of 18 and 45 years who had no history of
ral exposure or artificially through vaccination. malaria or of living in an area in which malaria
A further critical factor is our incomplete under- is endemic in the 6 months before study entry.
standing of precisely what constitutes protective Only one volunteer had ever been in an endemic
antimalarial immunity in humans. area, several years earlier. All volunteers under-
The possibility of vaccinating humans against went routine physical examination and hemato-
P. falciparum malaria was raised originally by the logic and biochemical screening at the Clinical
success of the radiation-attenuated sporozoite Research Center at Radboud University Nijmegen
model developed several decades ago.2,3 Irradia- Medical Centre. The results of serologic analysis
tion of infectious mosquitoes disrupts the gene for the human immunodeficiency virus (HIV),
expression of sporozoites, which remain capable hepatitis B and C, and asexual P. falciparum para-
of hepatocyte invasion but are no longer capable sites were negative in all subjects.
of complete liver-stage maturation or progression
to the pathogenic blood stage.4 Infection of hu- Study Oversight
man volunteers with irradiated sporozoites thus All subjects provided written informed consent.
exposes them to liver-stage antigens and generates The trial was approved by the institutional review
pre-erythrocytic immunity. However, the require- board at the Radboud University Nijmegen Medi-
ment of a minimum of 1000 bites by irradiated cal Centre. The study sponsor, the Dioraphte Foun-
mosquitoes during five or more immunization ses- dation, was not involved in the design of the
sions in order to successfully induce sterile immu- study, in the gathering or analysis of the data, or
nity in humans5 precludes this method for routine in the writing of the manuscript. All authors vouch
immunization. for the accuracy and completeness of the data.
A subunit vaccine can be developed on the basis
of antigens expressed by pre-erythrocytic, intra- Study Design
erythrocytic, or sexual stages of the parasite. Un- We randomly assigned the subjects in a double-
fortunately, results of many such subunit vaccines blind fashion to two study groups: 10 to a vaccine
in humans have been disappointing. To date, only group and 5 to a control group (Fig. 1). The mean
one candidate vaccine, which is based on the cir- (SD) age of the subjects was 22.01.5 years in
cumsporozoite protein and known as RTS,S, has the vaccine group and 24.01.4 years in the con-
progressed to phase 3 field trials. The protection trol group; seven subjects in the vaccine group were
induced by this vaccine is encouraging, but the women, as were four subjects in the control group.
ultimate success of this approach remains to be Chloroquine was provided to all subjects in a
determined.6-9 standard prophylactic regimen of a loading dose
In rodent models, sterile protection against of 300 mg on each of the first 2 days and then
malaria can be achieved by the inoculation of in- 300 mg once a week, starting on day 7, for a total
tact sporozoites while treating the animals con- duration of 13 weeks. While receiving chloro-
comitantly with chloroquine,10 a drug that kills quine, subjects in the vaccine group were exposed
parasites in the asexual blood stage but not in on three occasions at monthly intervals to bites
the pre-erythrocytic stage.11 The efficacy of this of 12 to 15 mosquitoes that had been infected
treatment is significantly higher than that of the with P. falciparum, for a total exposure of bites from
radiation-attenuated sporozoite model.12 We there- 36 to 45 infected mosquitoes per subject. Control
fore designed a proof-of-concept study in volun- subjects received bites from an equal number of
teers who had not been previously exposed to uninfected mosquitoes on the same occasions.
malaria to investigate whether protection can be Anopheles stephensi mosquitoes were reared ac-
n engl j med 361;5 nejm.org july 30, 2009 469
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
an outpatient basis, and blood was drawn for stan-
Screening dard whole-blood counts and daily peripheral-
(N=28 volunteers) blood smears. Any signs and symptoms were re-
corded by the attending physician as follows: mild
Enrollment events (easily tolerated), moderate events (inter-
(N=15)
Vaccine group Control group feres with normal activity), or severe events (pre-
(N=10) Double-blind (N=5) vents normal activity).
7
randomization
Day Eight weeks after the last immunization dose
0 Start chloroquine prophylaxis and 4 weeks after the discontinuation of chloro-
Uninfected mosquito bites
I-1
Infected mosquito bites
Immunization Phase
quine prophylaxis, all 15 subjects were challenged
Immunologic assessment
7
by exposure to the bites of five mosquitoes that
35 were infected with the homologous NF54 strain
of P. falciparum. This period was considered to be
63 sufficient for chloroquine levels to drop below
Days
those that might be inhibitory to parasite multi-
90 Stop chloroquine prophylaxis
plication.14 All subjects were checked twice daily
Day on an outpatient basis from day 5 to day 21 for
C-1
symptoms and signs of malaria, and hemato-
Challenge Phase
Challenge by
118 infected mosquito bite logic tests and peripheral-blood smears were
performed.
Clinical follow-up;
treatment if positive If results of peripheral-blood testing were posi-
140
results on blood testing tive, subjects were treated with a standard curative
combination regimen of 80 mg of artemether and
154 480 mg of lumefantrine, followed by five identical
Discharge from Study doses at 8, 24, 36, 48, and 60 hours. The subjects
were then followed closely for 3 days. Complete
Figure 1. Study Design and Enrollment.
cure was confirmed on the basis of peripheral-
Immunologic assessment was performed 1 day before the first immuniza-
tion (day I-1) and 1 day before challenge infection (day C-1). A final chal- blood smears. All subjects who continued to have
lenge with infectious mosquito bites was performed 28 days after the dis- negative results on the peripheral-blood smear
continuation of chloroquine prophylaxis. from the day of infection until day 21 after the
challenge were presumptively treated with arte-
COLOR FIGURE
metherlumefantrine.
Draft 3 6/30/09
cording to standard procedures
Author
atSauerwein
our insectary. Hematologic and biochemical measures were
Infected mosquitoes were obtained
Fig # 1 by feeding on determined in routine fashion at the hospitals
gametocytes of NF54, a Title chloroquine-sensitive
Malaria
central clinical laboratory. The use of nucleic acid
strain of P. falciparum, as described
ME
previously.13 sequencebased amplification and real-time poly-
NF54 is genetically homogeneous
DE Badenbut has not merase-chain-reaction (PCR) assays to determine
TV
been formally cloned. OnlyArtisttheAUTHOR technicians
PLEASE NOTE:
who the densities of P. falciparum parasites have been
prepared the mosquitoes were aware ofcarefully
their in-
Figure has been redrawn and type has been reset
Please check described previously.15,16 Chloroquine levels were
fectivity status, and these staff
Issue datemembers
7/30/09 had no measured by liquid chromatography.17,18 Minimum
clinical involvement with the subjects or the in- therapeutic concentrations for plasma chloroquine
vestigators. Blood-engorged mosquitoes were dis- levels maintained by the laboratory were 30 g
sected to confirm the presence of sporozoites. If per liter.14
necessary, feeding sessions were repeated until
precisely the predefined number of infected Immunologic Analysis
mosquitoes had fed. However, a single feeding Venous whole blood was collected in Vacutainer
session was sufficient in 49 of 60 instances of cell-preparation tubes (CPT, Becton Dickinson) be-
immunization or challenge, whereas a second ses- fore the first immunization and again before the
sion was required in just 10 instances and a third malaria challenge. Plasma was collected and stored
session in only 1 instance. at 70C. Peripheral-blood mononuclear cells were
On days 6 to 10 after each immunization by isolated by density gradient centrifugation, frozen
mosquito exposure, all subjects were followed on in fetal-calf serum containing 10% dimethyl
470 n engl j med 361;5 nejm.org july 30, 2009
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Protection against a Malaria Challenge by Sporozoite Inoculation
sulfoxide, and stored in liquid nitrogen. Antibody
A Immunization Phase
titers were assessed by enzyme-linked immuno-
100,000
sorbent assay (ELISA) and immunofluorescence
assay, according to standard protocols.19-21 Cellu-
lar responses to cryopreserved asexual parasites 10,000
P. falciparum (no./ml)
were assessed by 24-hour in vitro peripheral-blood
stimulation assays,22 followed by intracellular cy-
tokine staining with the use of a Fix and Perm Kit 1,000
(Caltag Laboratories) and flow cytometry. A more
detailed description of these immunologic assays
is provided in the Supplementary Appendix, avail- 100
able with the full text of this article at NEJM.org.
Statistical Analysis 10
1 6 7 8 9 10 1 6 7 8 9 10 1 6 7 8 9 10
We performed flow cytometric analysis using Cell- Immunization Immunization Immunization
Quest software, and all analyses were performed Phase I Phase II Phase III
with the use of SPSS software. Differences in re- MPS 0/10 0/10 0/10
sponses among subjects at various time points NASBA 10/10 6/10 3/10
and between subjects in the vaccine group and
B Challenge Phase
those in the control group were analyzed by non- 100,000
parametric measures (Wilcoxon and MannWhit-
ney tests, respectively). A two-sided P value of less
than 0.05 was considered to indicate statistical 10,000
P. falciparum (no./ml)
significance.
R e sult s 1,000
Control
Study Subjects
100
All 15 subjects completed the immunization phase
of the study. All subjects received chloroquine pro- Vaccine
phylaxis and subsequently underwent a malaria
10
challenge (Fig. 1). 0 2 4 6 8 10 12
No parasites were seen in the peripheral-blood Days after Infection
smears of any of the 10 subjects in the vaccine
group after each of the three immunization ses- Figure 2. Parasitemia in the Vaccine Group and the Control Group.
AUTHOR: Roestenberg RETAKE 1st
sions during chloroquine prophylaxis. However, Panel A showsICM the mean number of Plasmodium falciparum parasites per
2nd
REG F FIGURE:
milliliter, as measured 2 of 3acid sequencebased amplification
by nucleic
after the first immunization, a brief submicro- 3rd
(NASBA), after each of three immunizations on days before
CASE Revised infection and
scopic parasitemic episode was detected in all during expected Line 4-C
blood-stage parasitemia (days 6 to 10) inSIZE
EMail the vaccine
vaccinees (Fig. 2A). This finding was not unex- ARTIST: ts H/T positive
H/Tresults 22p3
group. The numbers
Enon of subjects who had on peripheral-
Combo
pected, since chloroquine has no effect against blood smears for malarial parasites (MPS) and NASBA are shown below
AUTHOR, PLEASE NOTE:
either sporozoites, liver-stage parasites, or the the graph. Panel BFigure
shows the mean number of P. falciparum parasites in
has been redrawn and type has been reset.
early ring forms of the first generation of blood- 5 subjects in the control group and check
Please 10 subjects
carefully.in the vaccine group, as
determined by real-time polymerase-chain-reaction assay before treatment
stage parasites that are caused by merozoites re- with artemetherlumefantrine. The I bars denote standard errors.
JOB: 36105 ISSUE: 07-30-09
leased from mature hepatic schizonts.11 After each
of the subsequent two immunizations, a progres-
sively reduced incidence and burden of submicro- events were most commonly reported after the
scopic parasitemia was seen. first immunization (in 9 of 10 subjects), with
In line with these findings, all vaccinees re- headache being the most frequent symptom (re-
ported solicited or unsolicited symptoms that were ported by 7 subjects) (Table 1). Only a few adverse
recorded as adverse events at least once during events were reported in the vaccine group subse-
the immunization phase. With the exclusion of quently (in two subjects after the third immuni-
local itching after the mosquito bites, adverse zation). Severe adverse events were reported by
n engl j med 361;5 nejm.org july 30, 2009 471
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
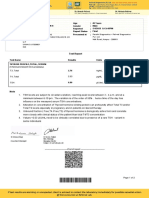
Table 1. Adverse Events after the First, Second, and Third Exposures to Immunizing Mosquito Bites and after Challenge with Infectious
Mosquito Bites.*
Adverse Event Vaccine Group (N=10) Control Group (N=5)
After After
After Immunization Challenge After Immunization Challenge
Exposure I Exposure II Exposure III Exposure I Exposure II Exposure III
Abdominal pain no.
Mild 2
Moderate
Severe
Fatigue no.
Mild 1 1 7 1 2
Moderate 2 1 1 2
Severe 1
Fever no.
Mild 2
Moderate 1
Severe 2 5
Headache no.
Mild 4 7 2 3 2
Moderate 2 1 1 1 1 3
Severe 1 1
Loss of appetite no.
Mild 1
Moderate
Severe
Malaise no.
Mild 1 1 1
Moderate 2 1
Severe 1 1 5
Myalgia no.
Mild 1 2 3
Moderate 2 1 4
Severe 1
Nausea no.
Mild 3 1 1 1 1
Moderate 1 1 1 1
Severe 1
Vomiting no.
Mild 1
Moderate 1
Severe
Total no. (%)
Mild 4 (40) 1 (10) 8 (80) 1 (20) 3 (60)
Moderate 3 (30) 1 (10) 1 (20) 2 (40) 1 (20)
Severe 2 (20) 1 (10) 1 (20) 5 (100)
* Subjects could have more than one adverse event, and reports of events could have been either solicited or unsolicited. Only adverse events
that were possibly or probably related to the study are listed.
The highest-grade event is listed per subject per infection.
472 n engl j med 361;5 nejm.org july 30, 2009
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Protection against a Malaria Challenge by Sporozoite Inoculation
three vaccinees: two had a fever above 39C after (range, <5 to 14) and less than 5 g per liter, re-
the first immunization, and one reported severe spectively, which were deemed to be below the
malaise after the last immunization. minimum therapeutic concentrations in vivo.14
After challenge with the homologous NF54 Furthermore, blood-stage parasite multiplication
strain of P. falciparum, asexual blood-stage para- kinetics in the control subjects were identical to
sites were detected in peripheral-blood smears of those in previous studies,24 which suggested that
all five control subjects between days 7 and 11 any residual chloroquine levels had no measurable
after exposure (mean prepatent period, 9.2 days). parasiticidal effect.
Real-time PCR analyses revealed the expected After immunization, antibody responses to
cyclical multiplication of blood-stage parasites both sporozoites and blood-stage parasites de-
(Fig. 2B). The clinical course and kinetics of para- veloped in vaccinees but not in control subjects,
site multiplication were similar to those in previ- as shown by ELISA (Table 2) and immunofluo-
ous studies involving subjects who had not been rescence assay (Fig. 1 in the Supplementary Ap-
exposed to malaria,23,24 with all control subjects pendix). Seroconversion to the circumsporozoite
reporting severe events, in particular fever above protein, an immunodominant sporozoite-stage and
39C and malaise (Table 1). In contrast, there was liver-stage antigen, occurred in eight vaccinees. In
no evidence of blood-stage parasites in any of the contrast, seroconversion to crude asexual-stage
vaccinees at any time during the post-challenge antigen occurred in only three vacinees. Antibod-
follow-up period until day 21, either by repeated ies to two predominantly asexual antigens, apical
microscopy of peripheral-blood smears or by real- membrane antigen 1 (AMA-1) and glutamate-rich
time PCR analyses (Fig. 2B). Interestingly, in the protein (GLURP), both of which are leading vac-
week after the malaria challenge, nine vaccinees cine candidates, were undetectable. These data are
reported mild-to-moderate events. No serious ad- consistent with the relatively low-dose exposure
verse events occurred during any part of the trial, to asexual blood-stage antigens in the vaccinees.
and all 15 subjects completed follow-up according Cellular immune responses were assessed by
to protocol. counting cytokine-producing cells in peripheral-
Mean peak plasma levels of chloroquine and blood specimens from the subjects, with the use
desethylchloroquine were 76 g per liter (range, of intracellular cytokine staining and flow cytom-
58 to 104) and 13 g per liter (range, 5 to 33), re- etry after 24 hours of in vitro stimulation with
spectively, 24 hours after administration; levels erythrocytes infected with the homologous strain
did not differ significantly between vaccinees and of P. falciparum or with uninfected erythrocytes
control subjects. The day before the malaria chal- (Fig. 3, and Fig. 2 and 3 in the Supplementary
lenge, mean plasma levels of chloroquine and Appendix). Whereas cellular responses to unin-
desethylchloroquine had dropped to 8 g per liter fected erythrocytes did not differ in any experi-
Table 2. Antibody Reactivity.*
Test Day I-1 Day C-1
Vaccine Group (N=10) Control Group (N=5) Vaccine Group (N=10) Control Group (N=5)
No. of Median Antibody No. of Median Antibody No. of Median Antibody No. of Median Antibody
Subjects Titer Subjects Titer Subjects Titer Subjects Titer
AU AU AU AU
CSP 0 <12 0 <12 8 33 (21210) 0 <12
AMA-1 ND ND 0 <5.8 0 <5.8
GLURP ND ND 0 <42 0 <42
Asexual blood- stage 0 <0.6 0 <0.6 3 1.7 (1.52.0) 0 <0.6
antigen
* Data are for subjects who had a detectable response. Numbers in parentheses are ranges. All analyses were performed with the use of an
enzyme-linked immunosorbent assay. Plasma was collected from all subjects before immunization (day I-1) and before the malaria challenge
(day C-1). A plasma pool obtained from 100 Tanzanian adults living in an area in which malaria was endemic was used as a reference posi-
tive control, set at 100 arbitrary units (AU). Thresholds for circumsporozoite protein (CSP), apical membrane antigen 1 (AMA-1), glutamate-
rich protein (GLURP), and asexual blood-stage positivity were 12, 5.8, 42, and 0.6 AU, respectively. ND denotes not done.
n engl j med 361;5 nejm.org july 30, 2009 473
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
ment from responses to culture medium alone,
Figure 3 (facing page). In Vitro Pluripotent Cytokine
stimulation with infected erythrocytes elicited Responses to Plasmodium falciparum Parasites
small percentages of lymphocytes producing on Flow Cytometry.
interferon- or TNF-, but not interleukin-2, in The proportion of lymphocytes that produced inter
the two groups before immunization (see day I-1 feron- (IFN-) and interleukin-2 (Panel A), tumor ne-
in Figure 2 in the Supplementary Appendix). crosis factor (TNF-) and interleukin-2 (Panel B), or
IFN-, TNF-, and interleukin-2 (Panel C) after in vitro
Although there was no significant difference
stimulation with erythrocytes infected with the homol-
in the overall proportion of cells producing indi- ogous strain of P. falciparum (PfRBC), with uninfected
vidual cytokines (interferon- or TNF-) in either erythrocytes (uRBC), or with phytohemagglutinin (PHA)
group after immunization (day C-1), a significant as a positive control are shown before immunization
increase was observed in the proportion of cells (day I-1) and before malaria challenge (day C-1). Dashed
lines represent the proportion of positive cells in un-
producing multiple cytokines in response to in-
stimulated wells (culture medium only). The geomet-
fected erythrocytes in vaccinees, as compared with ric mean fluorescence intensity of cells producing
baseline: P=0.03 for the within-group compari- IFN- (Panel D), TNF- (Panel E), and interleukin-2
son for interferon- and interleukin-2; P=0.046 (Panel F) that were isolated from vaccinees on day C-1
for TNF- and interleukin-2; and P=0.03 for is shown after stimulation in vitro with infected eryth-
rocytes. Cells are grouped according to their positivity
interferon-, TNF-, and interleukin-2 (Fig. 3A, 3B,
or negativity for each of the other two cytokines. In
and 3C). The importance of these pluripotent Panels G, H, and I, the proportion of lymphocytes that
lymphocytes in acquired immune protection is produced IFN- and interleukin-2 in response to in-
suggested by their higher cytokine content and fected erythrocytes are shown on day I-1 and day C-1
may reflect better effector function (Fig. 3D, 3E, for lymphocyte phenotypes, including naive T cells
(CD3+CD45RO), memory T cells (CD3+CD45RO+),
and 3F). The major contributors to this increase
and non-T lymphocytes (CD3CD45RO) (Panel G); for
in pluripotent lymphocytes with a response to in- T-cell phenotypes, including helper T cells (CD4+CD8),
fected erythrocytes were CD3+CD45RO+ memory- cytotoxic T cells (CD4CD8+), and other lymphocytes
like T cells (P=0.02 for the comparison with day (CD4CD8) (Panel H); and for memory phenotypes,
I-1) (Fig. 3G, and Fig. 3 in the Supplementary Ap- including naive T cells (CD62L+CD45RO), central
memory T cells (CD62L+CD45RO+), effector memory
pendix). CD4+CD8 cells showed a particularly
T cells (CD62LCD45RO+), and other lymphocytes
marked response (P=0.005 for the comparison (CD62LCD45RO) (Panel I). The proportions of lym-
with day I-1) (Fig. 3H). Most noticeably, these new phocytes that produced IFN- and interleukin-2 after
pluripotent lymphocytes were predominantly of stimulation with uninfected erythrocytes were below
the effector memory CD62LCD45RO+ pheno- 0.005% (not shown). All P values are for the compari-
son between the vaccine group and the control group
type (P=0.005 for the comparison with day I-1),
and were calculated with the use of the MannWhitney
although there was also a small but significant test. The T bars represent standard errors.
increase in the numbers of responding central
memory CD62L+CD45RO+ cells in vaccinees
(P=0.02 for the comparison with day I-1) (Fig. 3I). develop into a first generation of blood-stage
parasites,11 thus presenting to the hosts immune
Discussion system a broader array of pre-erythrocytic antigens,
as well as erythrocytic-stage antigens (albeit at
Our study shows that the inoculation of intact relatively low dose).
sporozoites induces more effective protection The contribution of intraerythrocytic antigens
against a homologous challenge with P. falciparum to the development of protective immunity is sug-
malaria than does irradiation-attenuated sporo- gested by Pombo et al.,25 who reported that re-
zoite immunization. In the endemic situation, how- peated intravenous injection of ultra-low densities
ever, nonsterile semi-immunity is acquired only of blood-stage parasites, followed by drug cure
after years of repeated natural exposure. We be- with atovaquoneproguanil, induced protection in
lieve that the improved efficiency of our approach human volunteers against a similarly low-dose
was due to a critical balance of exposure to pre- blood-stage challenge. However, caution needs to
erythrocytic and intraerythrocytic antigens. In be exercised when interpreting the latter results,
contrast to irradiated sporozoites that arrest ear- since residual concentrations of antimalarial drugs
ly during liver-stage development,4 intact sporo- may partially or even fully have accounted for the
zoites under chloroquine cover mature fully and observed protection.26
474 n engl j med 361;5 nejm.org july 30, 2009
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Protection against a Malaria Challenge by Sporozoite Inoculation
A IFN- and Interleukin-2 B TNF- and Interleukin-2 C IFN-, TNF-, and Interleukin-2
Vaccine Control Vaccine Control Vaccine Control
5
00
0.
0.045 0.100 0.04
P=
Percent of Lymphocytes
Percent of Lymphocytes
Percent of Lymphocytes
01
0.040
0.
P=
0.035 0.075 0.03
8
0.030
31
00
0.
0.
08
0.025
P=
P=
0.050 0.02
0.
0.020
31
P=
0.
0.015
P=
0.010 0.025 0.01
0.005
0.000 0.000 0.00
A
A
BC
BC
BC
BC
BC
BC
C
C
PH
PH
PH
PH
PH
PH
RB
RB
RB
RB
RB
RB
uR
uR
uR
uR
uR
uR
Pf
Pf
Pf
Pf
Pf
Pf
Day I-1 Day C-1 Day I-1 Day C-1 Day I-1 Day C-1
D IFN- E TNF- F Interleukin-2
200 400 600
Geometric Mean Fluore-
Geometric Mean Fluore-
Geometric Mean Fluore-
scence Intensity (AU)
scence Intensity (AU)
scence Intensity (AU)
500
300
400
100 200 300
200
100
100
0 0 0
2+
2+
-2
-2
-2
-2
-
n-
n-
n-
n-
in
in
in
in
FN
FN
FN
FN
ki
ki
ki
ki
uk
uk
uk
uk
leu
leu
leu
leu
,I
,I
,I
,I
rle
rle
rle
rle
er
er
er
er
te
te
te
te
F-
F-
F-
F-
nt
nt
nt
nt
in
in
in
in
TN
TN
TN
TN
,i
,i
,i
,i
+,
+,
,
+
-
F-
F-
F-
F-
N
TN
TN
TN
TN
IF
IF
IF
IF
G Lymphocyte Phenotypes H T-Cell Phenotypes I Memory Phenotypes
CD3+, CD3+, CD3, CD4+, CD4, CD4, CD62L+, CD62L+, CD62L, CD62L,
CD45RO CD45RO+ CD45RO CD8 CD8+ CD8 CD45RO CD45RO+ CD45RO+ CD45RO
P=0.048 P=0.001 P=0.001
IFN-+, Interleukin-2+ (%)
IFN-+, Interleukin-2+ (%)
IFN-+, Interleukin-2+ (%)
0.30 0.30 0.55
0.50
0.25 0.25 P=0.04 0.45
0.40
0.20 P=0.37 0.20 P=0.08 0.35
0.15 0.15 0.30
0.25
P=0.68 0.20 P=0.68
0.10 0.10
0.15
0.05 0.05 0.10
0.05
0.00 0.00 0.00
e
e
l
l
ro
ro
ro
ro
ro
ro
in
in
in
in
in
in
nt
nt
nt
nt
nt
nt
cc
cc
cc
cc
cc
cc
Co
Co
Co
Co
Co
Co
Va
Va
Va
Va
Va
Va
Day I-1 Day C-1 Day I-1 Day C-1 Day I-1 Day C-1
In the field, in contrast, patent parasitemia
ICM
AUTHOR:Thus, patent
Roestenberg parasitemia
(Sauerwein) RETAKE and
1st probably chronic
typically develops before patients seek REGtreatment.
F FIGURE: 3subpatent
of 3 parasitemia, which 2nd
3rd
occur regularly in
In such patients, acute blood-stage infection
CASE may children in endemic Revised areas, appear to induce in-
Line 4-C
suppress the induction of protective pre-erythro-
ARTIST: hibitory
ts mechanisms that
SIZEdelay the generation of
H/T H/T 36p6
cytic immunity, as has been shown in rodent protective
Enon
antiparasite immunity. Meta-analysis of
Combo
models.27 Indeed, parasitemic episodes or attacks AUTHOR, studiesPLEASE
of intermittent
NOTE: preventive therapy in in-
Figure has been redrawn and type has been reset.
of febrile malaria in Kenyan children are prospec- fants has decreased
Please check carefully. the concern about a rebound
tively associated with a poorer induction and more effect of prophylaxis and in some cases even in-
rapid attrition of cellular ex vivo andJOB:
memory
36105 re- dicates sustained protection after discontinuation
ISSUE: 07-30-09
sponses to a pre-erythrocytic P. falciparum antigen.28 of prophylaxis,29 thus further indicating that the
n engl j med 361;5 nejm.org july 30, 2009 475
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
acquisition and maintenance of protective immu- would suggest that the protection in our model
nity do not depend on chronic blood-stage ex- was primarily due to pre-erythrocytic immunity.
posure. However, a component of blood-stage immunity
Thus, the salient feature of our approach (i.e., the inhibition of erythrocyte invasion and
seems to be the exposure of the immune system maturation of minute liver-derived merozoite in-
to a greater array of pre-erythrocytic and intra- ocula that cannot be detected on PCR) is also pos-
erythrocytic antigens, while restricting the devel- sible. Indeed, we found that cellular responses to
opment of symptomatic and potentially immuno- asexual blood-stage parasites before challenge
suppressive parasitemia.30 Since NF54 is known were a discriminative marker of exposure and
to be a chloroquine-sensitive strain in vitro,31 we protection in our subjects, and similar immune
cannot formally exclude a synergistic effect of responses may have contributed to protection in
residual subtherapeutic chloroquine levels on im- the rodent model.12 However, many of the best-
munologic parasite clearance. However, chloro- studied P. falciparum antigens conferring protective
quine levels before the malaria challenge ap- immunity are shared among sporozoite, liver-
proached or fell below the limit of detection and stage, and blood-stage parasites.35,36 Thus, it is
had no measureable parasiticidal effect in control plausible that our findings represent the response
subjects. Of more importance, the longevity of to a broad antigenic repertoire that transcends
immunologic responses, both naturally acquired parasitic developmental stages,37 making a divi-
and vaccine-induced, remains a critical issue in sion between pre-erythrocytic immunity and in-
malaria, and follow-up studies are planned to ad- traerythrocytic immunity inappropriate. At pres-
dress this issue. ent, the stage specificity of the protective immune
In this model, we have identified responses of response must remain formally unresolved, al-
pluripotent effector memory T cells as being as- though one way to further address this issue in
sociated with protection. In one study,32 undefined future studies would be a blood-stage challenge.
subgroups of lymphocytes with the same cytokine Although the methods described here do not
profile were associated with the induction and represent a widely implementable vaccine strat-
maintenance of antigen-specific T-cell memory in egy, the induction of sterile protection against a
subjects who were immunized with pre-erythro- homologous malaria challenge suggests that the
cytic candidate malaria vaccines, but associations concept of a whole-parasite malaria vaccine war-
with protection were not explored. However, the rants further consideration. In addition, this model
potent effector function of pluripotent cells, as allows the nature of protective immune responses
suggested by their high cytokine content, has been against malaria, both stage-specific and antigen-
noted in other investigations that showed their specific, to be further investigated.
protective role in other infectious diseases.33,34 Supported by the Dioraphte Foundation, by a fellowship from
the European Union FP6 Network of Excellence (to Dr. McCall),
Further detailed investigations will be necessary and by grants from the NutsOhra Foundation (to Dr. van der Ven)
to determine the longevity of this immunologic and Agence Nationale de la Recherche in France (to Dr. Snounou).
response, its association with central memory-type Dr. Snounou reports receiving consulting fees from Sigma
Tau and GlaxoSmithKline. No other potential conflict of inter-
T-cell activity, and its ability to serve as a true est relevant to this article was reported.
correlate of protection. We thank the study volunteers for their participation; K.
Since the magnitude of the first wave of para- Nganou Makamdop for help with the RT-PCR assays; J. Bakkers
and W. Melchers for parasite genotyping; W. Arts, N. Huibers,
sitemia is thought to directly reflect the burden and P. Beckers for reading blood slides; P. Houze and D. Mazier
of erupting mature liver schizonts, the stepwise for chloroquine measurements; J. Klaassen, L. Pelser-Posthu-
decrease of such organisms after each subsequent mus, J. Kuhnen, and A. Pouwelsen for technical assistance gen-
erating infected mosquitoes; the safety monitors for the study,
immunizing infection and the absence of PCR- B. Schouwenberg and P. Smits; and independent physician A.
detectable parasitemia after the malaria challenge Brouwer.
References
1. Greenwood BM, Fidock DA, Kyle DE, derberg JP. Immunization of man against duced by the injection of x-irradiated
et al. Malaria: progress, perils, and pros- sporozite-induced falciparum malaria. sporozoites of plasmodium berghei. Na-
pects for eradication. J Clin Invest 2008; Am J Med Sci 1973;266:169-77. ture 1967;216:160-2.
118:1266-76. 3. Nussenzweig RS, Vanderberg J, Most 4. Mellouk S, Lunel F, Sedegah M, Beau-
2. Clyde DF, Most H, McCarthy VC, Van- H, Orton C. Protective immunity pro- doin RL, Druilhe P. Protection against
476 n engl j med 361;5 nejm.org july 30, 2009
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Protection against a Malaria Challenge by Sporozoite Inoculation
malaria induced by irradiated sporozo- amplification is more convenient than atovaquone-proguanil administration.
ites. Lancet 1990;335:721. real-time PCR for quantification of Plas- Antimicrob Agents Chemother 2005;49:
5. Hoffman SL, Goh LM, Luke TC, et al. modium falciparum. J Clin Microbiol 4421-2.
Protection of humans against malaria by 2005;43:402-5. 27. Orjih AU. Acute malaria prolongs sus-
immunization with radiation-attenuated 17. Houz P, de Reynies A, Baud FJ, Bena- ceptibility of mice to Plasmodium berghei
Plasmodium falciparum sporozoites. J In- tar MF, Pays M. Simultaneous determina- sporozoite infection. Clin Exp Immunol
fect Dis 2002;185:1155-64. tion of chloroquine and its three metabo- 1985;61:67-71.
6. Alonso PL, Sacarlal J, Aponte JJ, et al. lites in human plasma, whole blood and 28. Bejon P, Mwacharo J, Kai O, et al. The
Duration of protection with RTS,S/AS02A urine by ion-pair high-performance liquid induction and persistence of T cell IFN-
malaria vaccine in prevention of Plasmo- chromatography. J Chromatogr 1992;574: gamma responses after vaccination or
dium falciparum disease in Mozambican 305-12. natural exposure is suppressed by Plas-
children: single-blind extended follow-up 18. Lejeune D, Souletie I, Houz S, et al. modium falciparum. J Immunol 2007;
of a randomised controlled trial. Lancet Simultaneous determination of monodes- 179:4193-201.
2005;366:2012-8. ethylchloroquine, chloroquine, cyclogua- 29. Grobusch MP, Egan A, Gosling RD,
7. Abdulla S, Oberholzer R, Juma O, et nil and proguanil on dried blood spots by Newman RD. Intermittent preventive
al. Safety and immunogenicity of RTS,S/ reverse-phase liquid chromatography. therapy for malaria: progress and future
AS02D malaria vaccine in infants. N Engl J Pharm Biomed Anal 2007;43:1106-15. directions. Curr Opin Infect Dis 2007;
J Med 2008;359:2533-44. 19. Bousema JT, Roeffen W, van der Kolk 20:613-20.
8. Bejon P, Lusingu J, Olotu A, et al. Ef- M, et al. Rapid onset of transmission- 30. Sutherland CJ, Drakeley CJ, Schellen-
ficacy of RTS,S/AS01E vaccine against reducing antibodies in Javanese migrants berg D. How is childhood development of
malaria in children 5 to 17 months of age. exposed to malaria in Papua, Indonesia. immunity to Plasmodium falciparum en-
N Engl J Med 2008;359:2521-32. Am J Trop Med Hyg 2006;74:425-31. hanced by certain antimalarial interven-
9. Aponte JJ, Aide P, Renom M, et al. 20. Hermsen CC, Verhage DF, Telgt DS, et tions? Malar J 2007;6:161.
Safety of the RTS,S/AS02D candidate ma- al. Glutamate-rich protein (GLURP) in- 31. Davis JR, Cortese JF, Herrington DA,
laria vaccine in infants living in a highly duces antibodies that inhibit in vitro et al. Plasmodium falciparum: in vitro
endemic area of Mozambique: a double growth of Plasmodium falciparum in a characterization and human infectivity of
blind randomised controlled phase I/IIb phase 1 malaria vaccine trial. Vaccine a cloned line. Exp Parasitol 1992;74:
trial. Lancet 2007;370:1543-51. 2007;25:2930-40. 159-68.
10. Beaudoin RL, Strome CP, Mitchell F, 21. Remarque EJ, Faber BW, Kocken CH, 32. Bejon P, Keating S, Mwacharo J, et al.
Tubergen TA. Plasmodium berghei: im- Thomas AW. A diversity-covering ap- Early gamma interferon and interleukin-2
munization of mice against the ANKA proach to immunization with Plasmodi- responses to vaccination predict the late
strain using the unaltered sporozoite as um falciparum apical membrane antigen resting memory in malaria-naive and
an antigen. Exp Parasitol 1977;42:1-5. 1 induces broader allelic recognition and malaria-exposed individuals. Infect Im-
11. Yayon A, Vande Waa JA, Yayon M, growth inhibition responses in rabbits. mun 2006;74:6331-8.
Geary TG, Jensen JB. Stage-dependent ef- Infect Immun 2008;76:2660-70. 33. Darrah PA, Patel DT, De Luca PM, et
fects of chloroquine on Plasmodium falci- 22. McCall MB, Netea MG, Hermsen CC, al. Multifunctional TH1 cells define a cor-
parum in vitro. J Protozool 1983;30: et al. Plasmodium falciparum infection relate of vaccine-mediated protection
642-7. causes proinflammatory priming of hu- against Leishmania major. Nat Med 2007;
12. Belnoue E, Costa FT, Frankenberg T, man TLR responses. J Immunol 2007; 13:843-50.
et al. Protective T cell immunity against 179:162-71. 34. Precopio ML, Betts MR, Parrino J, et
malaria liver stage after vaccination with 23. Verhage DF, Telgt DS, Bousema JT, et al. Immunization with vaccinia virus in-
live sporozoites under chloroquine treat- al. Clinical outcome of experimental hu- duces polyfunctional and phenotypically
ment. J Immunol 2004;172:2487-95. man malaria induced by Plasmodium fal- distinctive CD8(+) T cell responses. J Exp
13. Ponnudurai T, Lensen AH, van Gemert ciparum-infected mosquitoes. Neth J Med Med 2007;204:1405-16.
GJ, Bensink MP, Bolmer M, Meuwissen JH. 2005;63:52-8. 35. Hogh B, Thompson R, Zakiuddin IS,
Infectivity of cultured Plasmodium falci- 24. Hermsen CC, de Vlas SJ, van Gemert Boudin C, Borre M. Glutamate rich Plas-
parum gametocytes to mosquitoes. Parasi- GJ, Telgt DS, Verhage DF, Sauerwein RW. modium falciparum antigen (GLURP).
tology 1989;98:165-73. Testing vaccines in human experimental Parassitologia 1993;35:Suppl:47-50.
14. Rombo L, Bergqvist Y, Hellgren U. malaria: statistical analysis of parasitemia 36. Silvie O, Franetich JF, Charrin S, et al.
Chloroquine and desethylchloroquine measured by a quantitative real-time poly- A role for apical membrane antigen 1 dur-
concentrations during regular long-term merase chain reaction. Am J Trop Med ing invasion of hepatocytes by Plasmodi-
malaria prophylaxis. Bull World Health Hyg 2004;71:196-201. um falciparum sporozoites. J Biol Chem
Organ 1987;65:879-83. 25. Pombo DJ, Lawrence G, Hirun- 2004;279:9490-6.
15. Hermsen CC, Telgt DS, Linders EH, et petcharat C, et al. Immunity to malaria 37. Krzych U, Lyon JA, Jareed T, et al.
al. Detection of Plasmodium falciparum after administration of ultra-low doses of T lymphocytes from volunteers immu-
malaria parasites in vivo by real-time red cells infected with Plasmodium falci- nized with irradiated Plasmodium falci-
quantitative PCR. Mol Biochem Parasitol parum. Lancet 2002;360:610-7. parum sporozoites recognize liver and
2001;118:247-51. 26. Edstein MD, Kotecka BM, Anderson blood stage malaria antigens. J Immunol
16. Schneider P, Wolters L, Schoone G, et KL, et al. Lengthy antimalarial activity of 1995; 155:4072-7.
al. Real-time nucleic acid sequence-based atovaquone in human plasma following Copyright 2009 Massachusetts Medical Society.
n engl j med 361;5 nejm.org july 30, 2009 477
The New England Journal of Medicine
Downloaded from nejm.org on September 17, 2013. For personal use only. No other uses without permission.
Copyright 2009 Massachusetts Medical Society. All rights reserved.
Potrebbero piacerti anche
- Activity 6 - INFECTIONS OF THE SKIN GROUP 4 FINAL.Documento6 pagineActivity 6 - INFECTIONS OF THE SKIN GROUP 4 FINAL.the someone100% (2)
- Health and Safety Manual Company TemplateDocumento55 pagineHealth and Safety Manual Company Templatepandu_chemengNessuna valutazione finora
- Textbook of Regional Anesthesia PDFDocumento1.268 pagineTextbook of Regional Anesthesia PDFDinu Tiberiu George75% (4)
- Dencover ClaimformDocumento4 pagineDencover Claimformd763106Nessuna valutazione finora
- Antigen-Stimulated PBMC Transcriptional Protective Signatures For Malaria ImmunizationDocumento18 pagineAntigen-Stimulated PBMC Transcriptional Protective Signatures For Malaria Immunizationyowan wandikboNessuna valutazione finora
- Management of Infections in the Immunocompromised HostDa EverandManagement of Infections in the Immunocompromised HostBrahm H. SegalNessuna valutazione finora
- Malaria VaccineDocumento65 pagineMalaria VaccineAkula Sai PrasannaNessuna valutazione finora
- Kelompok10 (20Documento11 pagineKelompok10 (20Gufront MustofaNessuna valutazione finora
- Molecular Biology, Pathogenesis and Pathology of MumpsDocumento10 pagineMolecular Biology, Pathogenesis and Pathology of MumpsHarry SalomoNessuna valutazione finora
- Paula FM, Gryschek RCB, Chieffi PP - 2019 - Diagnosis of Strongyloides StercoralisDocumento3 paginePaula FM, Gryschek RCB, Chieffi PP - 2019 - Diagnosis of Strongyloides StercoralisayresrenatoNessuna valutazione finora
- Nanoparticle Adjuvant Sensing by Tlr7 Enhances Cd8 T Cell Mediated Protection From Listeria Monocytogenes InfectionDocumento9 pagineNanoparticle Adjuvant Sensing by Tlr7 Enhances Cd8 T Cell Mediated Protection From Listeria Monocytogenes InfectionEverton MonteiroNessuna valutazione finora
- Fase 1.2Documento11 pagineFase 1.2Verliatesya TugasNessuna valutazione finora
- Seguridad Vacunal: Precauciones y Contraindicaciones de Las Vacunas. Reacciones Adversas. FarmacovigilanciaDocumento25 pagineSeguridad Vacunal: Precauciones y Contraindicaciones de Las Vacunas. Reacciones Adversas. FarmacovigilanciaMaribel Catalan HabasNessuna valutazione finora
- Human Trophoblasts Confer Resistance To Viruses ImDocumento8 pagineHuman Trophoblasts Confer Resistance To Viruses Imonline videoNessuna valutazione finora
- 1 s2.0 S222116911530366X MainDocumento10 pagine1 s2.0 S222116911530366X MainNatália FreitasNessuna valutazione finora
- Nej Mo A 0807381Documento12 pagineNej Mo A 0807381Mildred MontNessuna valutazione finora
- Articulo MalariaDocumento19 pagineArticulo MalariaAndres Felipe DuqueNessuna valutazione finora
- Advances in The Development of Vaccines Against Neisseria MeningitidisDocumento10 pagineAdvances in The Development of Vaccines Against Neisseria MeningitidisstephaniedianNessuna valutazione finora
- T Cells Expands A Population of Memory Infection of Mice: Staphylococcus AureusDocumento14 pagineT Cells Expands A Population of Memory Infection of Mice: Staphylococcus AureusTrysmonika7Nessuna valutazione finora
- Vaccine Tcell FluDocumento7 pagineVaccine Tcell Fluortizalvarez_arturoNessuna valutazione finora
- Live Attenuated Human Rotavirus Vaccine, Rotarix™: David I. Bernstein, MD, MADocumento7 pagineLive Attenuated Human Rotavirus Vaccine, Rotarix™: David I. Bernstein, MD, MACagar Irwin TaufanNessuna valutazione finora
- 2015 The Comparison Between Microhematocrit and Automated Methods For Hematocrit DeterminationDocumento10 pagine2015 The Comparison Between Microhematocrit and Automated Methods For Hematocrit DeterminationAgri Febria SariNessuna valutazione finora
- Joc 50057Documento10 pagineJoc 50057Sudarman Abdul RahmanNessuna valutazione finora
- Immunological Reviews - 2019 - Kurtovic - Complement in Malaria Immunity and VaccinesDocumento19 pagineImmunological Reviews - 2019 - Kurtovic - Complement in Malaria Immunity and VaccinesFaiz SheeNessuna valutazione finora
- (Jean Langhorne (Editor) ) Immunology and ImmunopatDocumento239 pagine(Jean Langhorne (Editor) ) Immunology and Immunopatclaudia lilianaNessuna valutazione finora
- MonkeypoxDocumento6 pagineMonkeypoxAaron Thomas LeonardNessuna valutazione finora
- Journal Pone 0286224Documento29 pagineJournal Pone 0286224nutritionist1234567Nessuna valutazione finora
- KulitDocumento9 pagineKulitPandaNessuna valutazione finora
- Osong Public Health and Research PerspectivesDocumento6 pagineOsong Public Health and Research PerspectivesbrianNessuna valutazione finora
- Tumor - Comment 825full - 230515 - 075912Documento4 pagineTumor - Comment 825full - 230515 - 075912Sol SoriaNessuna valutazione finora
- Amphibian VirologyDocumento13 pagineAmphibian VirologyanitacmontoyaNessuna valutazione finora
- Antigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFDocumento5 pagineAntigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFGabriel CoutoNessuna valutazione finora
- Next Generation Sequencing of Microbial Cell Free DNA To Rapidly Detect Fluoribacter Bozemanae Pneumonia in An Immunocompromised HostDocumento4 pagineNext Generation Sequencing of Microbial Cell Free DNA To Rapidly Detect Fluoribacter Bozemanae Pneumonia in An Immunocompromised HostAthenaeum Scientific PublishersNessuna valutazione finora
- TreatmentDocumento3 pagineTreatmentNarasimharao HarnoorNessuna valutazione finora
- Vaccine InformaticsDocumento10 pagineVaccine InformaticsSumathiNessuna valutazione finora
- Parasitic Infections and the Immune SystemDa EverandParasitic Infections and the Immune SystemFelipe KierzenbaumNessuna valutazione finora
- Bacteriology - Classification of BacteriaDocumento51 pagineBacteriology - Classification of BacteriaMarc Imhotep Cray, M.D.100% (3)
- Containment PlanDocumento6 pagineContainment Planapi-488592120Nessuna valutazione finora
- Ni Hms 316844Documento15 pagineNi Hms 316844ntnquynhproNessuna valutazione finora
- Poxviruses: Chapter 37: Herpesviruses, Poxviruses, & Human Papilloma VirusDocumento4 paginePoxviruses: Chapter 37: Herpesviruses, Poxviruses, & Human Papilloma Virustheodore_estradaNessuna valutazione finora
- Corticosteroids For Bacterial Meningitis in Adults in Sub-Saharan AfricaDocumento10 pagineCorticosteroids For Bacterial Meningitis in Adults in Sub-Saharan AfricaMutiara KhalishNessuna valutazione finora
- Journal Pone 0284296Documento16 pagineJournal Pone 0284296Alifia nadyraNessuna valutazione finora
- Transplant Infectious Dis - 2022 - Chang - Mycoplasma Hominis Infections in Solid Organ Transplant Recipients ClinicalDocumento8 pagineTransplant Infectious Dis - 2022 - Chang - Mycoplasma Hominis Infections in Solid Organ Transplant Recipients Clinical---Nessuna valutazione finora
- Combined Tetanus, Diphtheria, and 5-Component Pertussis Vaccine For Use in Adolescents and AdultsDocumento10 pagineCombined Tetanus, Diphtheria, and 5-Component Pertussis Vaccine For Use in Adolescents and Adultsatika sgrtNessuna valutazione finora
- 1 s2.0 S0065266005540112 MainDocumento33 pagine1 s2.0 S0065266005540112 MainComodin PiterNessuna valutazione finora
- Kroemer 2015Documento11 pagineKroemer 2015ADanAlfaNessuna valutazione finora
- Thannesberger 2017Documento15 pagineThannesberger 2017Денис КрахоткинNessuna valutazione finora
- What Can We Learn and What Do We Need To Know Amidst The Iatrogenic Outbreak of Exserohilum Rostratum Meningitis?Documento8 pagineWhat Can We Learn and What Do We Need To Know Amidst The Iatrogenic Outbreak of Exserohilum Rostratum Meningitis?Galuh Kresna BayuNessuna valutazione finora
- 1 s2.0 S0264410X21006113 MainDocumento10 pagine1 s2.0 S0264410X21006113 Mainflor rodriguezNessuna valutazione finora
- 2019 First-In-Human, Randomized, Double-Blind Clinical Trial of Differentially Adjuvanted PAMVAC, A Vaccine Candidate To Prevent Pregnancy-Associated MalariaDocumento8 pagine2019 First-In-Human, Randomized, Double-Blind Clinical Trial of Differentially Adjuvanted PAMVAC, A Vaccine Candidate To Prevent Pregnancy-Associated MalariaSethawud ChaikitgosiyakulNessuna valutazione finora
- CD14CD16 PDFDocumento16 pagineCD14CD16 PDFAde OktiviyariNessuna valutazione finora
- Is Hospital Mortality Higher at Weekends? If So, Why?: CommentDocumento4 pagineIs Hospital Mortality Higher at Weekends? If So, Why?: CommentRatna KusumasariNessuna valutazione finora
- 149 FullDocumento10 pagine149 Fullসোমনাথ মহাপাত্রNessuna valutazione finora
- s41541 022 00534 5 F1e5e53258Documento11 pagines41541 022 00534 5 F1e5e53258Psirico bahiaNessuna valutazione finora
- Gamma Interferon-Producing CD4 T-Cells Correlate With Resistance To Mycoplasma Mycoides Subsp. Mycoides S.C. Infection in CattleDocumento17 pagineGamma Interferon-Producing CD4 T-Cells Correlate With Resistance To Mycoplasma Mycoides Subsp. Mycoides S.C. Infection in CattleNancy Riv CorNessuna valutazione finora
- 6 Vol. 7 Issue 9 September 2016 IJPSR RE 1915Documento9 pagine6 Vol. 7 Issue 9 September 2016 IJPSR RE 1915Nur KhasanahNessuna valutazione finora
- Virus: Course Code: FET-2117 Course Title: Basic Food MicrobiologyDocumento21 pagineVirus: Course Code: FET-2117 Course Title: Basic Food MicrobiologyMuhibullah MuhibNessuna valutazione finora
- Nejmoa 061760Documento16 pagineNejmoa 061760nqchi180418Nessuna valutazione finora
- Embor 2013103 ADocumento1 paginaEmbor 2013103 AAchmad ArifiyantoNessuna valutazione finora
- Journal PNTD 0009324Documento11 pagineJournal PNTD 0009324Maria Astika DewiNessuna valutazione finora
- Drug-Resistant And-Vaccine For Parasitic DiseasesDocumento34 pagineDrug-Resistant And-Vaccine For Parasitic DiseasesTamara ElyasNessuna valutazione finora
- Created By: Michael Anthony C. Macaballug, R.NDocumento115 pagineCreated By: Michael Anthony C. Macaballug, R.NRubyFranzCabangbang-QuilbanNessuna valutazione finora
- Development of Novel Carrier(s) Mediated Tuberculosis Vaccine: More Than A Tour de ForceDocumento17 pagineDevelopment of Novel Carrier(s) Mediated Tuberculosis Vaccine: More Than A Tour de ForceDrMuhamad Luthfi AsyharNessuna valutazione finora
- Cancers Related To Immunodeficiencies: Update and PerspectivesDocumento13 pagineCancers Related To Immunodeficiencies: Update and PerspectivesHabiby Habibaty QolbiNessuna valutazione finora
- NCP (Diarrhea)Documento2 pagineNCP (Diarrhea)Rodj Bilang Jr.83% (30)
- Bio PoemDocumento3 pagineBio Poemapi-4039173890% (1)
- Ankylosing SpondylitisDocumento5 pagineAnkylosing SpondylitisHarry IsraNessuna valutazione finora
- Bacteria Cell CalloDocumento16 pagineBacteria Cell CalloAngelo CalloNessuna valutazione finora
- M M Rvaxpro ProspectDocumento57 pagineM M Rvaxpro ProspectNicoleta CiobotarNessuna valutazione finora
- Hand, Foot and Mouth Disease What Is It?Documento2 pagineHand, Foot and Mouth Disease What Is It?leslie_macasaetNessuna valutazione finora
- Patient Report BALRAM SINGHDocumento2 paginePatient Report BALRAM SINGHNeeraj KumarNessuna valutazione finora
- 10 - Dr. McDaniel - Sudden Onset Diplopia Should I Be AfraidDocumento6 pagine10 - Dr. McDaniel - Sudden Onset Diplopia Should I Be AfraidTamara AudreyNessuna valutazione finora
- Final Announcement Liver UpdateDocumento13 pagineFinal Announcement Liver Updatenerissa arvianaNessuna valutazione finora
- PATH - Bony Injuries (Fractures) (8p) PDFDocumento8 paginePATH - Bony Injuries (Fractures) (8p) PDFandreeaNessuna valutazione finora
- Lista Preturi Teste Genetice GendiaDocumento227 pagineLista Preturi Teste Genetice GendiaMatei FloriNessuna valutazione finora
- P Blood Group SystemDocumento2 pagineP Blood Group SystemMiguel SabillenaNessuna valutazione finora
- Unlocking The BrainDocumento3 pagineUnlocking The BrainPsychedelicBaronNessuna valutazione finora
- Abruptio Placenta Drug StudyDocumento5 pagineAbruptio Placenta Drug StudyJayne Angelie A. NuevaespañaNessuna valutazione finora
- 6 SbarDocumento11 pagine6 Sbarsathish kumarNessuna valutazione finora
- Ocular Myasthenia: DR Maruthi Prasad UpputuriDocumento36 pagineOcular Myasthenia: DR Maruthi Prasad UpputuriAinul NurrahmahNessuna valutazione finora
- Potential of rDNA Technology in Revolutionizing FutureDocumento23 paginePotential of rDNA Technology in Revolutionizing FutureNusra FaizNessuna valutazione finora
- Cholelithiasis (Case Presentation)Documento19 pagineCholelithiasis (Case Presentation)Ian CiarNessuna valutazione finora
- Medical Terminology CourseDocumento197 pagineMedical Terminology CourseAnnaNessuna valutazione finora
- 124-Manuzon vs. ECCDocumento5 pagine124-Manuzon vs. ECCNimpa Pichay100% (1)
- Nursing Diagnosis For Gerd: Lifestyle ChangesDocumento3 pagineNursing Diagnosis For Gerd: Lifestyle ChangesSharmaine MadlaNessuna valutazione finora
- Definitions and Pillars For Safemother HoodDocumento39 pagineDefinitions and Pillars For Safemother HoodMayom Mabuong90% (29)
- Date Assessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale Evaluation Objective SubjectiveDocumento2 pagineDate Assessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale Evaluation Objective SubjectivePauline CañoNessuna valutazione finora
- Pedia BAIEDocumento49 paginePedia BAIEDarlene Clarice V. LabacladoNessuna valutazione finora
- Lesson Exemplar in Mapeh Grade Level Learning Area QuarterDocumento8 pagineLesson Exemplar in Mapeh Grade Level Learning Area QuarterErwin Balid GasconNessuna valutazione finora
- CPR 3: Standards For Protection Against Radiation: Belinda Dancel-San Juan, MD, MSCDocumento33 pagineCPR 3: Standards For Protection Against Radiation: Belinda Dancel-San Juan, MD, MSCMark RoldanNessuna valutazione finora