Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Management of Children and Young People With Headache: William P Whitehouse, Shakti Agrawal
Caricato da
Xiomara CuadrosTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Management of Children and Young People With Headache: William P Whitehouse, Shakti Agrawal
Caricato da
Xiomara CuadrosCopyright:
Formati disponibili
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.
com
Review
Management of children and young
people with headache
William P Whitehouse,1,2 Shakti Agrawal3
1
Department of Paediatric ABSTRACT paediatrics and paediatric headache disor-
Neurology, Nottingham
Children's Hospital, Nottingham
Headache is very common in children and young ders in particular, the better the advice
University Hospitals NHS Trust, people. The correct advice and treatment you will give and the better will be the
Nottingham, UK requires consideration of a wide differential treatment options you can offer your
2
School of Medicine, University
of Nottingham, Nottingham, UK
diagnosis between primary and secondary patients.
3
Department of Paediatric headaches, and also of the different types of Headache can be thought of as pain
Neurology, Birmingham primary headache. The International referred to the forehead, orbits, temples
Children's Hospital, Birmingham,
UK
Classification of Headache Disorders gives useful or scalp, and does not usually cover pain
descriptions and diagnostic criteria that are isolated to the face or neck. Pain is a
Correspondence to especially useful for primary headaches. The complicated, all be it real, experience that
Dr William P Whitehouse, National Institute for Health and Care Excellence demands and deserves medical attention.
Division of Academic Child
Health, School of Medicine,
(NICE) Clinical Guideline 150 provides evidence- The International Association for the
E Floor East Block, Queen's based recommendations on treatments for adults Study of Pain defined it as an unpleasant
Medical Centre, Nottingham and young people from age 12 years. However, sensory and emotional experience asso-
NG7 2UH, UK;
william.whitehouse@
the same principles can be applied to younger ciated with actual or potential tissue
nottingham.ac.uk children when a specific diagnosis can be made. damage, or described in terms of such
Key recommendations from the NICE Quality damage.1 Therefore, pain can be caused
Received 10 August 2016
Revised 30 October 2016
Standards include, establishing a precise by actual or incipient tissue injury, a dis-
Accepted 2 November 2016 diagnosis if possible, avoiding, diagnosing and order of the pain pathways or an illness
Published Online First treating medication overuse headache, and behaviour, and in all cases is a powerful
20December2016
combining a triptan with a non-steroidal anti- interpersonal communication. It is not
inflammatory drug or paracetamol as the first- surprising then, that some drugs that are
line acute/rescue treatment for migraine with or very effective for pain associated with
without aura. Although rare in children and tissue injury, for example, opiates and
young people, it is important to diagnose new anti-inflammatory drugs, are often only
daily persistent headache, as it responds poorly partially effective in other situations.
or not at all to medication; and paroxysmal Psychological support and interventions
hemicrania as it responds very well to can make important contributions to
indomethacin but not to other commonly used restoring function in patients with pain
analgesics. When faced with difficulties in generally and especially in migraine.
reaching a precise diagnosis or in finding Acknowledging the condition, allaying
effective therapies, further advice should be fear and addressing worries will help ease
sought from a childrens headache clinic or the suffering.
specialist. Recent reviews of headache in child-
hood,2 3 and in preschool children,4
INTRODUCTION provide excellent summaries of the topic,
Although this article will focus on the and more comprehensive knowledge can
drug therapy of primary headaches, it is be gleaned from Childhood Headache
vital that prescribers understand how to 2nd Edition,5 and the Childhood
differentiate primary from secondary Headache Training courses run in the UK
headaches and also the varieties of by the British Paediatric Neurology
primary headache that will present in Association.6 The National Institute for
childhood. Diagnosis and therapeutic Health and Care Excellence (NICE)
To cite: WhitehouseWP,
decisions are often complicated by evidence-based guideline on headache in
AgrawalS. Arch Dis Child comorbidities, and different primary young people and adults is an accessible,
Educ Pract Ed 2017;102:58 headaches can coexist. So the more you succinct and invaluable resource, which
65.
know and understand about general covers the diagnosis and management of
58 WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
primary headaches in children and young people aged
12 years and above.7 It is currently being reviewed Box 2 Headache intensity (severity)8
and updated. Formal diagnostic criteria for primary
and secondary headaches have been revised and pub- 0: No headache
lished in the International Classification of Headache 1: Mild headache: does not interfere with
Disorders 3rd edition.8 usual activities, for example, carries on with work or play
2: Moderate headache: inhibits but
TREATMENT DECISIONS does not wholly prevent usual activities, for example,
After a careful clinical assessment, including a full stops playing and just watches a film
history and tailored examination, decide on the most 3: Severe headache: prevents all purposeful activities,
likely diagnosis and the important differentials. This for example, just lies down quietly or sleeps
will usually require no further investigations, and will
allow you to give the child and their family reassur-
ance and sensible advice. Occasionally, and especially
when faced with an unclassified headache, for Box 3 Medication overuse headache8
example, a non-specific chronic daily headache with
no features to further define the diagnosis, investiga- Consider the possibility of medication overuse headache
tions for symptomatic headache will be indicated.9 (MOH) in patients developing a chronic headache, that is,
Box 1 summarises the key red flags, warning symp- on 15 days a month, for 3 months, who had previ-
toms and signs, suggestive of a secondary headache, as ously episodic tension-type headache, migraine without
does the HeadSmart campaign.10 aura or migraine with aura while taking the following,
alone or in combination:
ADVISING NO MEDICATION triptans, ergot alkaloids, opiates or combination
The most important consideration is that, very often, analgesics on 10 days a month
it is best to recommend no medication. A mild head- paracetamol, aspirin or any non-steroidal anti-
ache (see box 2)8 may cause concern even when the inflammatory drug on 15 days a month
pain is slight and not interfering with function and MOH typically presents when a bad patch of migraine
participation. In this situation, clinical assessment, with or without aura has transformed into a chronic daily
diagnosis, explanation and reassurance will usually headache, including chronic migraine.
address the concerns. Withdraw the suspect medication abruptly, and give
Often the child or young person will already have advice on alternative treatments including in some cases
found out that simple analgesics ( paracetamol or ibu- prophylactic medication.
profen) have not helped and will be, quite rightly, Complete remission after withdrawal is no longer a diag-
unwilling to use them. Primary stabbing headache8 is nostic criterion.
an intense focal head pain lasting 13 s and occurring
unpredictably without any trigger or autonomic symp-
toms or signs. It often occurs in people with migraine unpredictable to treat, but diagnosis and explanation
without aura, at a site within their usual migraine site, do help. If frequent, indomethacin, as for paroxysmal
typically frontally. It is too short lived and hemicrania (see section paroxysmal hemicranias
within the section trigeminal autonimic cephalalgias),
is worth considering. New daily persistent headache8
is usually refractory to medication. However, in
Box 1 Red flags general it is worth checking the doses used in case a
sufficiently high dose has not been tried. In patients
Change in personality, behaviour, worsening school with primary headache, however, be sure to advise
work or lethargy them about medication overuse headache (MOH,
First severe headache see box 3).8 Use the doses in your recommended ref-
Unclassified headache erence source, for example, in the UK the British
Accelerated course National Formulary for Children (BNF C)11 unless
Change in headache ( people with migraine can otherwise stated.
develop brain tumours, albeit rarely)
Mainly when lying down or asleep or bending down,
PREVENTING MEDICATION OVERUSE HEADACHE
straining or coughing
MOH is common, especially in people with primary
Abnormal growth or puberty
headaches, for example, migraine without aura or epi-
New neurological signs: ataxia, cranial nerve deficit,
sodic tension-type headache,8 which becomes trans-
head-tilt, papilloedema, visual impairment
formed by frequent use of any single analgesic into a
Convulsions/epileptic seizures
chronic daily headache, less intense but just as
WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803 59
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
upsetting as the original primary headache. It can be
Box 4 Lifestyle advice explained as a rebound headache, in people where
the pathology is in the pain pathways rather than due
Encourage to tissue damage. All patients with a primary headache
As full participation in work and play activities as should be warned about this and prescriptions for
possible, between incapacitating headaches analgesics should state as well as the dose and
Regular and sufficient sleep maximum dose that can be taken in 24 hours, not to
Regular rest and relaxation use them on more than 2 (or occasionally 3) days a
Regular meals ( particularly breakfast) week.
Adequate hydration (drinking enough non-caffeinated
fluids)
NON-DRUG TREATMENTS AND ADVICE
Regular exercise, between incapacitating headaches
A variety of physical, complementary and lifestyle
Their understanding of primary headache, when
interventions are available, mostly with little empir-
applicable
ical evidence of efficacy. However, acupuncture is
Discourage
included in the NICE guideline for chronic tension-
Prohibitions on normal activities, foods or drinks,
type headache and as a second-line treatment for
unless there is very clear evidence that one has been
migraine prophylaxis.7 Low-risk common sense
harmful in a particular case
advice has also traditionally been recommended
Table 1 Simple analgesics for the acute/rescue treatment of migraine with and without aura
Beware: Patients are susceptible to medication overuse headache, so use full doses but usually on no more than 2 days/week
Age Route Dose Preparation (pack) Contraindications/cautions
1. Paracetamol
011 years Oral 20 mg/kg 46 hrly, max 75 mg/kg/day Tabs: 500 mg; dispersible tabs Hepatic impairment
120, 500 mg; Renal impairment
Oral suspension: 120 mg/5 mL,
250 mg/5 mL
Per rectum 40 mg/kg, then 20 mg/kg 46 hrly, Suppositories: 60, 125, 250,
max 75 mg/kg/day 500 mg
1050 kg Intravenous 15 mg/kg 46 hrly (max 60 mg/kg/day) Intravenous infusion: 10 mg/mL
>50 kg 1 g 46 hrly (max 4 g daily)
1218 years Oral 0.51 g 46 hrly, max 4 g/day
PR/intravenous doses as above
2. Ibuprofen (NSAID)
26 years Oral 100 mg three times a day, max 30 mg/kg/day Tabs: 200, 400, 600 mg; Gastro pain, bleeding, ulceration,
allergic reactions
711 years 200 mg three times a day, max Oral suspension: 100 mg/5 mL;
30 mg/kg/day, max 2.4 g/day Orodispersible melts: 200 mg
1218 years 400 mg three times a day, max 600 mg four
times a day
3. Diclofenac (NSAID)
118 years Oral/PR 0.31 mg/kg three times a day, Tabs: 25, 50 mg; Gastro pain, bleeding, ulceration,
max 150 mg/day Dispersible tabs: 10, 50 mg allergic reactions
Suppositories: 100 mg
218 years Intravenous/ 0.31 mg/kg twice daily max 150 mg/day Injection: 25 mg/mL
intramuscular
4. Ketorolac (NSAID)
115 years Intravenous (slow) 0.51 mg/kg (max 15 mg) stat then Injection: 30 mg/mL Gastro pain, nasty taste, flushing,
0.5 mg/kg (max 15 mg) confusion
6 hrly, max 60 mg/day for 48 h
1618 years 10 mg stat then 1030 mg 4 hrly,
max 90 mg daily for 48 hours
Some of the drugs/doses below are those suggested/used by the authors and may be outside the marketing authorisation. Always check usual reference
sources/guidelines when using unfamiliar medicines.11
Hrly, hourly; max, maximum; NSAID, non-steroidal anti-inflammatory drug; tabs, tablets.
60 WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
including healthy lifestyle habits (see box 4). We rou- probably at the level of the trigeminovascular system
tinely encourage the use of distraction (especially for and its connections.5 Offer a triptan taken together
mild and moderate headaches), cold or warm com- with ibuprofen or paracetamol (or both) for attacks of
presses and balms applied to the forehead and/or migraine with or without aura.7 These combinations
temples, for example, Tiger Balm White, 4-Head, are more effective and cost-effective than using either
etc. Excess caffeine, aspartame, monosodium glutam- in isolation.7 A nasal triptan, for example, sumatriptan
ate, nitrites, alcohol and chocolate can cause head- or zolmitriptan will have a more rapid onset of action
ache (and vomiting); however, the role of exclusion than oral or orodispersible formulations. The triptan
diets per se in childhood migraine is still unproven. can be repeated after 2 hours if required, but give the
patient and parent/carer clear instructions on the
GENERAL ACUTE/RESCUE TREATMENTS maximum dose, for example, two doses in 24 hours
Simple over-the-counter analgesics, paracetamol and/ and on no more than two days a week. A nasal
or ibuprofen are first-line treatments for symptomatic triptan may not be tolerated because of the taste or,
and most primary headaches, especially episodic very rarely, it can produce an unpleasant feeling or
tension-type headaches.7 Opiate analgesia should be dizziness. If this happens, it is worth trying an alter-
offered for severe symptomatic headaches where there native triptan or formulation. If tolerated, a triptan
is known tissue damage, for example, for post- should be tried for three different attacks before
operative pain, but is not recommended for primary giving up for lack of efficacy. Three different triptans
headaches. It seems less effective and more prone to should be tried before accepting that this class of
dose escalation and dependency in patients with medicine is ineffective for a particular patient.
primary headaches, with associated incapacitating sed- Although sumatriptan and zolmitriptan are the only
ation, constipation, nausea and itching. See tables 13 triptans currently in the BNF C,11 and only sumatrip-
for most useful medicines for migraine with or tan has marketing authorisation (a licence) for young
without aura. people aged 1218 years, there are no particular con-
Give the child or young person a headache diary to traindications to triptan use in this population or
use.12 This will help establish their headache diagno- younger children, for example, of primary school age.
ses and whether the current acute/rescue and prophy- We will occasionally use triptans, in the smaller doses
lactic treatments are working. available, in younger children off-label, in accord-
ance with the UK Royal College of Paediatrics and
MIGRAINE WITH OR WITHOUT AURA Child Health advice to use the best treatment available
Triptans are a class of serotonin irrespective of pharmaceutical company marketing
(5-hydroxytryptamine) 1B/1D/1F receptor agonists, strategies, especially when no licensed product of
which exert a particular antimigraine attack effect, that class is available.13
Table 2 Antiemetics for the acute/rescue treatment of migraine with and without aura
5. Cyclizine
25 years Oral 0.51 mg/kg three times a day, Tabs: 50 mg; Drowsiness, dystonia is rare
Per rectum max 3 mg/kg/day, max single dose Suppository:12.5, 25, 50, 100 mg;
Intravenous 25 mg Injection: 50 mg/mL
Subcutaneous
611 years 25 mg up to three times a day
1218 years 50 mg up to three times a day
6. Domperidone
218 years Oral/ 250 mg/kg three times a day, Tabs: 10 mg Avoid in hepatic impairment
35 kg Per rectum 10 mg three times a day, Suspension: 5 mg/5 mL Can prolong QT-interval, so caution in heart
>35 kg Suppository: 30 mg disease, or with other drugs that can do the
same
7. Prochlorperazine
511 years Oral 250 mg/kg up to three times a day Tabs: 5 mg; syrup: 5 mg/5 mL Dystonia, akathisia, tardive dyskinesia, all
Per rectum 5 mg three times a day Suppository: 5, 25 mg rare
Intramuscular 6.25 mg, max three times a day Buccal prep: 3 mg tabs placed high
between upper lip and gum
1218 years Oral 510 mg, max three times a day Injection: 12.5 mg/mL
Per rectum 12.525 mg three times a day
Buccal 12 tabs twice daily
Intramuscular 12.5 mg up to three times a day
Some of the drugs/doses below are those suggested/used by the authors and may be outwith the marketing authorisation. Always check usual reference
sources/guidelines when using unfamiliar medicines.11
Tabs, tablets.
WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803 61
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
Table 3 Triptans: specific acute/rescue treatments for primary headaches
Beware: To avoid medication overuse headache, use on no more than 2 days/week
8. Sumatriptan
69 years Oral 25 mg at onset, repeat once after at least Tabs: 50 mg Cardiac disease.
2 hours if needed, max 2 days/week Tingling, tightness, flushing,
dizziness, nasty taste (nasal
1018 years Oral 50100 mg at onset, repeat once after at Injection: 6 mg/0.5 mL spray)
least 2 hours, max 2 days/week Nasal spray: 10 mg /0.1 mL actuation
Subcutaneous 6 mg at onset, repeat once after at least (2 and 6 unit dose sprays available)
1 hour, max 2 days/week
Intranasal 1020 mg at onset, repeat once after at least
2 hours, max 40 mg/day, max 2 days/week
9. Zolmitriptan
1218 years Oral 2.55 mg at onset, repeat once after at least Tabs: 2.5 mg Cardiac disease.
2 hours, max 10 mg/day, max 2 day/week Orodispersible: melts 2.5 mg Tingling, tightness, flushing,
Intranasal 5 mg at onset, repeat once after at least Nasal spray: 5 mg /0.1 mL actuation dizziness, nasty taste (nasal
2 hours, max 10 mg/day, max 2 day/week spray)
Other triptans include rizatriptan (halve the dose if on propranolol), almotriptan, eletriptan, frovatriptan, naratriptan, with less experience in children and
young people
Used together with NSAID or paracetamol.
Some of the drugs/doses below are outwith the marketing authorisation. Always check usual reference sources/guidelines when using unfamiliar
medicines.11
Max, maximum; NSAID, non-steroidal anti-inflammatory drug; tabs, tablets.
Many prescribers avoid triptans and similar vaso-
constrictor drugs in hemiplegic migraine, a particular Box 5 Useful combinations
type of migraine with aura,8 even though a link to
migrainous infarction or ischaemic arterial stroke has For migraine with or without aura
not been observed.14 Advise a triptan and a NSAID
There is no particular contraindication to oral Sumatriptan nasal spray and
contraceptive use by young people with migraine Ibuprofen or
without aura; however, specialist advice should be Paracetamol; max 2 days a week
sought for those with migraine with aura.7 And with severe nausea and vomiting
Antiemetic medication is often needed early on in a Consider a parenteral triptan and a parenteral NSAID
migraine attack, together with specific treatment for or rectal paracetamol or intravenous ketorolac or
the headache (as above), for example, cyclizine, dom- intravenous paracetamol and a parenteral antiemetic
peridone, prochlorperazine. Metoclopramide is par- Sumatriptan nasal spray and
ticularly associated with acute dystonic reactions Diclofenac suppository and
including oculogyric crises, and is now only indicated Prochlorperazine buccal; max 2 days a week
as second-line treatment for postoperative or NSAID, non-steroidal anti-inflammatory drug.
chemotherapy-related nausea and vomiting. We have
therefore omitted metoclopramide and the
paracetamol-metoclopramide combination (Paramax) TREATING MEDICATION OVERUSE HEADACHE
from table 2. However, if a patient has previously MOH (see box 3 for diagnostic criteria) is best
benefitted from metoclopramide without adverse treated by abrupt withdrawal of the likely causative
effect, it should not be withheld. Another analgesic or triptan.7 Warn the patient that headaches
analgesic-antiemetic combination in frequent use may get worse over a couple of weeks before the
(Migraleve) contains codeine, which is not generally chronic daily headache improves. Physical treatments
recommended for primary headaches. There are a and lifestyle advice (see section on non-drug treat-
range of formulations for different routes of adminis- ments and advice) can help, and sometimes migraine
tration (see box 5). prophylaxis will be appropriate during and following
Occasionally, vomiting and incapacitation are so withdrawal (see section prophylactic treatment for
severe in a migraine attack that the child or young migraine).
person will need emergency department assessment
and treatment with intravenous fluids for dehydration,
and a parenteral triptan and a parenteral non-steroidal TRIGEMINAL AUTONOMIC CEPHALALGIAS
anti-inflammatory drug (NSAID) or paracetamol, and Although comparatively rare in children, the trigem-
parenteral antiemetics. inal autonomic cephalalgias (TACs)8 are important to
62 WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
recognise as they are very painful and incapacitating, seen more often in young people aged 1218 years
and their pathology and treatment is different from than in younger children, and may be mistaken for an
migraine. However, effective first-line treatment is epilepsy, or psychogenic non-epileptic attacks, or
available, so if you are unfamiliar with them do con- other medically unexplained illness behaviour.15 High
sider referring to a paediatric or adult headache clinic, flow (12 L/min) 100% oxygen by a non-rebreathing
depending on the patients age and local resources, face mask with a reservoir bag is usually very effective
for diagnostic and treatment advice. acutely. When indicated, home and ambulatory
Cluster headache,8 especially when lacking some of oxygen will need to be provided.7 Triptans, subcuta-
the typical features (ie, probable cluster headache), is neously or nasally can also help.7
Table 4 Prophylactic treatments for primary headaches: migraine with or without aura, episodic tension-type headache, chronic
migraine, chronic tension-type headache
Regular prophylactic treatments
1. Topiramate (antiepileptic)
218 years Oral 0.5 mg/kg slowly up to 10 mg/kg/day, Tabs: 25, 50, 100, 200 mg Weight loss, paraesthesia, fatigue,
max 10 mg/kg/day, max 200 mg/day Sprinkle caps: 15, 25, 50 mg drowsiness, impaired memory. There is a
smaller risk of teratogenicity than with
sodium valproate.
2. Propranolol (-blocker)
24 years Oral 200500 mg/kg twice daily, max 4 mg/kg/day Tabs: 10, 40, 80, 160 mg Avoid abrupt withdrawal
Oral solution: 5, 10, Avoid in asthma
58 years 10 mg twice daily, increasing to 30 mg twice daily 50 mg/5 mL Sleep problems
812 years 20 mg twice daily, increasing to 40 mg twice daily
1218 years 30 mg twice daily, increasing to 60 mg twice daily
3. Gabapentin (antiepileptic)
212 years Oral 1020 mg/kg three times a day Caps: 100, 300, 400 mg Avoid sudden withdrawal
Tabs: 600, 800 mg
1218 years 300 mg three times a day, then up to max 1.2 g
three times a day
4. Sodium valproate (antiepileptic)
118 years Oral 10 slowly up to 40 mg/kg/day, max 1.5 g Tabs: 100, 200, 500 mg Weight gain, tremor. Avoid in young
twice daily Oral solution: 200 mg/5 mL females of 12 years and more because of
teratogenicity, intellectual disability after
fetal valproate exposure and irregular
periods.
5. Flunarizine (calcium channel blocker, in the UK only on a named-patient basis)5 17 18
59 years Oral 0.10.3 mg/kg/day, 2.55 mg once daily, Tabs: 5, 10 mg Give as evening dose
(2040 kg) max 10 mg once daily Sedation, weight gain, tremor, irregular
periods
1018 years 10 mg once daily
(>40 kg) max 20 mg
6. Amitriptyline (tricyclic antidepressant)
611 years Oral 1020 mg at night Coated tabs: 10, 25, 50 mg Dry mouth, sedation, blurred vision,
Oral solution: 25 mg/5 mL constipation
1218 years 2550 mg at night Beware risk of cardiovascular fatality in
overdose
7. Riboflavin (vitamin B2)
118 years Oral 50100 mg once daily-twice daily, Tabs: 10, 50, 100 mg Bright yellow urine
max 400 mg/day
8. Pizotifen (serotonin 5-HT2 antagonist)
511 years Oral 500 mg increasing to 1 mg at night, Tabs: 500 mg, 1.5 mg Drowsiness, increased appetite, weight
max 1.5 mg/day Elixir: 250 mg/5 mL gain, nausea, dizziness, anxiety,
aggression
1218 years 1.5 mg increasing to 3 mg at night,
max 4.5 mg/day
Some of the drugs/doses below are outwith the marketing authorisation. Always check usual reference sources/guidelines when using unfamiliar
medicines.11
5-HT, 5-hydroxytryptamine; max, maximum; caps, capsules; tabs, tablets.
WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803 63
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
Paroxysmal hemicranias8 is another TAC experi- are ineffective and/or not tolerated, consider a triptan
enced rarely in children from preschool to secondary twice or three times a day, on the days migraine
school ages, which is very effectively treated with indo- attacks are expected, even if that is a few consecutive
methacin (combined with omeprazole, or ranitidine or days. Good evidence for this approach exists for zol-
similar). Response to indomethacin is so typical that it mitriptan and frovatriptan.7
is formally a diagnostic criterion,8 so children with
some but not all the typical features should be tried PROPHYLACTIC TREATMENTS FOR TACS
with indomethacin, for example, for 23 weeks. Cluster headache and probable cluster headache in
children and young people are generally best diag-
PROPHYLACTIC TREATMENT FOR MIGRAINE nosed and treated in specialist paediatric or adult
Because episodic tension-type headache, migraine headache clinics. There is good evidence to support
without aura and migraine with aura are on a con- verapamil as a prophylactic.7
tinuum,16 it is unusual to find someone with episodic Paroxysmal hemicrania responds within a few days
tension-type headache requiring prophylactic treat- of reaching an effective dose of indomethacin.8 This is
ment who does not also have migraine with or true for some cases not fulfilling all the diagnostic cri-
without aura. Similarly, chronic tension-type head- teria, that is, probable paroxysmal hemicrania.
aches8 would not usually require prophylactic treat- Treatment should be combined with omeprazole or
ment, but if it did the diagnosis should be reviewed, ranitidine or similar drug to reduce the risk of gastro-
thinking of a symptomatic headache (eg, idiopathic intestinal adverse effects, particularly ulceration and
intracranial hypertension, sinusitis, etc), or more likely
chronic migraine.8
When incapacitating headaches, particularly
Test your knowledge
migraine with or without aura, occur three or four
times a month or more, depending on their severity
and impact, offer a daily prophylactic medication. Select the best single answer:
The choice will depend on preferences and comorbid- 1. Pain
ities. Most drugs should be titrated up if starting low A. is an unpleasant sensory experience caused by
doses prove to be ineffective, and the drug should be tissue injury
reduced or abandoned if there are adverse effects or B. involves an emotional experience component as
relatively high doses prove to be ineffective. Avoid well as (A)
combinations of prophylactic treatments, except C. includes the description of (B) but with potential
during switching (see table 4). or actual tissue injury
Topiramate is effective for patients with chronic D. includes the description of (B) even in the
daily headache, for example, in adults with chronic absence of potential/actual tissue injury
migraine.19 It is also a first-line prophylactic treatment E. is not definable, but can reliably be recognised.
for migraine with or without aura in younger chil- 2. Medication overuse headache
dren,20 as well as in young people and adults.7 A. can happen with primary and secondary
Although recommended doses are lower than those headaches
often used for epilepsies, these patients are at no more B. can happen with prophylactic and acute/rescue
risk of adverse effects than children with epilepsies. analgesia
The risk of teratogenicity in young women is signifi- C. can happen when acute/rescue analgesia is used
cantly less than for sodium valproate. on more than 14 days a month
Other drugs with reasonable evidence of efficacy in D. can happen when acute/rescue analgesia is used
migraine in children and young people include pro- on more than 20 days a month
pranolol and gabapentin.7 Some weaker evidence is E. is best treated with gradual withdrawal of the
also available for valproate,7 flunarizine,17 18 amitrip- offending medication.
tyline7 and riboflavin.7 Unfortunately, there is no 3. A triptan with a NSAID
good evidence for pizotifens efficacy7 despite being a A. is the most effective treatment for attacks of
licensed and popular treatment in the UK and it cer- migraine with or without aura
tainly seems to work well for some children and B. is recommended for new daily persistent head-
young people, in the authors experience. Moreover, ache and migraine without aura
as it is now off-patent, it seems unlikely that a prop- C. is recommended for migraine with aura in young
erly powered trial will ever be funded, unless a novel people 16 years of age or older
formulation is developed and patented. D. should not be used before trying at least one
NSAID and one triptan on its own
MENSTRUAL-RELATED MIGRAINE E. should not be used together at the same time.
Some young women have predictable menstrual-
The answers are after the references
related migraine.8 If first-line acute/rescue treatments
64 WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Review
bleeding. It can be continued for 23 weeks then 6 Childrens Headache Training (CHaT). http://www.bpna.org.
stopped, but will need to be reinstated promptly when uk/headache/ (accessed 14 Feb 2015).
the paroxysmal hemicrania relapses. The paroxysmal 7 National Institute for Health and Care Excellence (NICE).
Diagnosis and management of headaches in young people and
hemicrania may settle in months or continue for
adults. September 2012. https://www.nice.org.uk/guidance/
years. Relatively low maintenance doses can often
cg150 (accessed 14 Feb 2015).
work.21 If indomethacin is not tolerated, further 8 Classification Committee of the International Headache
expert advice should be sought. Society. The international classification of headache
disorders, 3rd edition (beta version). Cephalalgia 2013;
CONCLUSIONS 33:629808.
The management of children and young people with 9 Ahmed MAS, Martinez A, Cahill D, et al. When to image
headache therefore depends on the correct diagnosis neurologically normal children with headaches: development
and differential diagnosis. This article for the of a decision rule. Acta Paediatr 2010;99:9403.
Medicines Update has focussed on drug treatments. 10 HeadSmart. http://www.headsmart.org.uk/ (accessed 14 Feb
However, it is important to stress that drug treatment 2015).
11 BNF and BNF C. https://www.medicinescomplete.com/about/
is not always needed, and certainly prophylactic treat-
subscribe.htm (accessed 14 Feb 2015).
ment is not usually needed in migraine with or
12 BPNA Headache Diary. http://www.bpna.org.uk/audit/
without aura, and almost never needed in tension-type Headache%20diary.PDF (accessed 14 Feb 2015).
headache. Acute/rescue treatments for severe and 13 Fox A, Sammons for the RCPCH. The use of unlicensed
incapacitating primary headaches and for secondary medicines or licensed medicines for unlicensed applications in
headaches with tissue damage will be needed, but the paediatrics. December 2013. http://www.rcpch.ac.uk/system/
correct choice depends on the precise diagnosis. files/protected/page/The%20use%20of%20unlicensed%
Resources to help in the diagnosis and holistic man- 20medicines%20or%20licensed%20medicines.pdf (accessed 14
agement have been sign-posted. Feb 2015).
14 Artto V, Nissil M, Wessman M, et al. Treatment of hemiplegic
Acknowledgements We are grateful to all our patients and their migraine with triptans. Eur J Neurol 2007;14:10536.
families, our students and teachers and especially to colleagues
15 McNabb S, Whitehouse W. Cluster headache-like disorder in
who have taught us so much about childrens headaches: Dr
Judith Hockaday, Dr Richard Newton, Dr Ishaq Abu-Arafeh, childhood. Arch Dis Child 1999;81:51112.
Dr Dilip Nathan, Dr Rachel Howels and colleagues on the 16 Viswanathan V, Bridges SJ, Whitehouse W, et al. Childhood
NICE gc150 guideline development group. headaches: discrete entities or continuum? Dev Med Child
Contributors WPW reviewed the literature, wrote most of the Neurol 1998;40:54450.
first draft and reviewed and edited the article following editors 17 Sorge F, De Simone R, Marano E, et al. Flunarazine in
and reviewers suggestions, read and approved the final version. prophylaxis of childhood migraine. A double-blind,
SA reviewed the literature, compiled the first draft of the tables
and helped edit the article following the editors and reviewers placebo-controlled, crossover study. Cephalalgia 1988;8:16.
comments, read and approved the final version. 18 Mohamed BP, Goadsby PJ, Prabhakar P. Safety and efficacy of
Competing interests None declared. flunarazine in childhood migraine: 11 years experience, with
emphasis on its effect in hemiplegic migraine. Dev Med Child
Provenance and peer review Commissioned; externally peer
reviewed. Neurol 2012;54:2747.
19 Silberstein S, Lipton R, Dodick D, et al. Topiramate treatment
of chronic migraine: a randomized placebo-controlled trial of
REFERENCES
quality of life and other efficacy measures. Headache
1 International Association for the Study of Pain (IASP)
2009;49:115362.
Subcommittee on Taxonomy. Pain terms: a list with definitions
20 Buch ML. Use of topiramate in preventing pediatric migraine.
and notes on usage. Pain 1979;6:24752.
Pediatr Pharmacother 2013;19:14.
2 Newton RW. Childhood headache. Arch Dis Child Edu Pract
21 Blankenburg M, Hechler T, Dubbel G, et al. Paroxysmal
Ed 2008;93:10511.
hemicrania in childrensymptoms, diagnostic criteria, therapy
3 Abu-Arafeh I. Diagnosis and management of headache in
and outcome. Cephalalgia 2009;29:87382.
children and adolescents. Prog Neurol Psychiatry
2014;18:1620.
4 McCrea N, Howells R. Fifteen minute consultation: headache
in children under 5 years of age. Arch Dis Child Edu Pract Ed Answers to the multiple choice questions
2013;98:1815.
5 Abu-Arafeh I, ed. Childhood headache. 2nd edn. London: Mac
1. D; 2. C; 3. A.
Keith Press, 2013.
WhitehouseWP, AgrawalS. Arch Dis Child Educ Pract Ed 2017;102:5865. doi:10.1136/archdischild-2016-311803 65
Downloaded from http://ep.bmj.com/ on July 13, 2017 - Published by group.bmj.com
Management of children and young people
with headache
William P Whitehouse and Shakti Agrawal
Arch Dis Child Educ Pract Ed 2017 102: 58-65 originally published online
December 20, 2016
doi: 10.1136/archdischild-2016-311803
Updated information and services can be found at:
http://ep.bmj.com/content/102/2/58
These include:
References This article cites 14 articles, 1 of which you can access for free at:
http://ep.bmj.com/content/102/2/58#BIBL
Email alerting Receive free email alerts when new articles cite this article. Sign up in the
service box at the top right corner of the online article.
Topic Articles on similar topics can be found in the following collections
Collections Editor's choice (41)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
Potrebbero piacerti anche
- Pediatric Headache: An OverviewDocumento22 paginePediatric Headache: An OverviewntnquynhproNessuna valutazione finora
- Annals - Concussão Cerebral em Pediatria - 2020Documento5 pagineAnnals - Concussão Cerebral em Pediatria - 2020Juliana MeirelesNessuna valutazione finora
- Patniyot Irene Headache in AdolescentsDocumento16 paginePatniyot Irene Headache in AdolescentsAnonymous tG35SYROzENessuna valutazione finora
- 2012 33 562 Heidi K. Blume: Pediatric Headache: A ReviewDocumento17 pagine2012 33 562 Heidi K. Blume: Pediatric Headache: A ReviewLAURA CAMILA CACERES DELGADONessuna valutazione finora
- Admin,+11 +winarno +Migraine+Headache+in+ChildrenDocumento12 pagineAdmin,+11 +winarno +Migraine+Headache+in+ChildrenadjenglunaNessuna valutazione finora
- Management of Headaches in Children and AdolescentsDocumento13 pagineManagement of Headaches in Children and Adolescentsebmanansala0771pamNessuna valutazione finora
- Pediatr - Rev CEFALEA AlternDocumento9 paginePediatr - Rev CEFALEA AlternIvan LiconNessuna valutazione finora
- Headache FacultyDocumento25 pagineHeadache FacultyTyra TusingNessuna valutazione finora
- Pediatric Headache: A Review: Pediatrics in Review December 2012Documento18 paginePediatric Headache: A Review: Pediatrics in Review December 2012JayantiNessuna valutazione finora
- Headache - Seminars in NeurologyDocumento7 pagineHeadache - Seminars in NeurologyandreaNessuna valutazione finora
- Headache and Facial Pain: Key PointsDocumento5 pagineHeadache and Facial Pain: Key PointsCaesar Muhammad WijayaNessuna valutazione finora
- Effectiveness of Mindfulness Meditation Vs Headache Education Rebecca WellsDocumento12 pagineEffectiveness of Mindfulness Meditation Vs Headache Education Rebecca WellsYunita Christiani BiyangNessuna valutazione finora
- 213 1499018212 - 02-07-2017 PDFDocumento5 pagine213 1499018212 - 02-07-2017 PDFEditor IJRITCCNessuna valutazione finora
- Headaches in Children - Diagnosis and Treatment - Reader ModeDocumento8 pagineHeadaches in Children - Diagnosis and Treatment - Reader Modeedward nodzoNessuna valutazione finora
- Medi 100 E23469Documento7 pagineMedi 100 E23469Belva EdinaNessuna valutazione finora
- Managing Cluster HeadacheDocumento8 pagineManaging Cluster HeadacheAndreea AtănăsoaeiNessuna valutazione finora
- 118 123 PDFDocumento6 pagine118 123 PDFZH LimNessuna valutazione finora
- Is This Just A: Headache?Documento6 pagineIs This Just A: Headache?agirl_9807Nessuna valutazione finora
- HeadacheDocumento2 pagineHeadachenomyname234Nessuna valutazione finora
- Pediatric Headaches: Tension HeadacheDocumento8 paginePediatric Headaches: Tension HeadacheUli EmirNessuna valutazione finora
- Cognitive Behavioral Therapy For Treatment of Pediatric Chronic MigraineDocumento3 pagineCognitive Behavioral Therapy For Treatment of Pediatric Chronic MigraineFlory23ibc23Nessuna valutazione finora
- CBTforpediatricchronicmigraine JAMAeditorial Dec2013 PDFDocumento3 pagineCBTforpediatricchronicmigraine JAMAeditorial Dec2013 PDFFlory23ibc23Nessuna valutazione finora
- Cefalee Cronica ZilnicaDocumento8 pagineCefalee Cronica ZilnicaDorina FrunzeNessuna valutazione finora
- Basic of Self-Care and Non-Prescription DrugsDocumento33 pagineBasic of Self-Care and Non-Prescription DrugsMing Yew TingNessuna valutazione finora
- Management of HeadacheDocumento8 pagineManagement of HeadacheRifQi MuhammadNessuna valutazione finora
- 1 s2.0 S0736467917311897 MainDocumento11 pagine1 s2.0 S0736467917311897 MainA2150A N Fikri AbrorNessuna valutazione finora
- Headache: Paul G. Mathew, M.D., and Ivan Garza, M.DDocumento13 pagineHeadache: Paul G. Mathew, M.D., and Ivan Garza, M.DCarlosErnestoMoralesNessuna valutazione finora
- Maju Jurnal MigrainDocumento7 pagineMaju Jurnal MigrainRosyid PrasetyoNessuna valutazione finora
- More Than A Random Bout of Pain: Brain HealthDocumento4 pagineMore Than A Random Bout of Pain: Brain HealthTimes MediaNessuna valutazione finora
- SYMPOSIUM: ACCIDENTS AND POISONINGDocumento6 pagineSYMPOSIUM: ACCIDENTS AND POISONINGDeli IndahNessuna valutazione finora
- Headache and Migraine Guidelines Final Version 2019 1568626549Documento13 pagineHeadache and Migraine Guidelines Final Version 2019 1568626549aslan tonapaNessuna valutazione finora
- Lance Neuro PTHDocumento10 pagineLance Neuro PTHRenju KuriakoseNessuna valutazione finora
- Managing Migraines in TeensDocumento58 pagineManaging Migraines in TeenssaheefaNessuna valutazione finora
- OCD and Migraine Case ReportDocumento4 pagineOCD and Migraine Case ReportRaaqa AnastaNessuna valutazione finora
- The Treatment of Migraine Headaches in Children and AdolescentsDocumento11 pagineThe Treatment of Migraine Headaches in Children and Adolescentsdo leeNessuna valutazione finora
- Panic Disorder: A Common Yet Underdiagnosed and Misunderstood Psychological Illness in PakistanDocumento3 paginePanic Disorder: A Common Yet Underdiagnosed and Misunderstood Psychological Illness in PakistanSharii AritonangNessuna valutazione finora
- Headache Literature ReviewDocumento7 pagineHeadache Literature Reviewafmzuomdamlbza100% (1)
- Cleveland Clinic Journal of Medicine 2002 173 4Documento2 pagineCleveland Clinic Journal of Medicine 2002 173 4Feny JunaidyNessuna valutazione finora
- migraineDocumento6 paginemigraineNatália CândidoNessuna valutazione finora
- Bahan Journal Reading MigraineDocumento9 pagineBahan Journal Reading Migraineleviana aurelliaNessuna valutazione finora
- Nye 2015Documento8 pagineNye 2015Mayra SantanderNessuna valutazione finora
- Chronic headaches in children: Diagnosing and managing migrainesDocumento22 pagineChronic headaches in children: Diagnosing and managing migrainesAbdallah AlquranNessuna valutazione finora
- Pharmalogy ZADocumento133 paginePharmalogy ZASamuel KamocheNessuna valutazione finora
- Diagnosing Secondary Headaches (Practical Neurology) (2020 - 05)Documento5 pagineDiagnosing Secondary Headaches (Practical Neurology) (2020 - 05)Apostolos T.Nessuna valutazione finora
- Dolor Crónico Infantily FTDocumento13 pagineDolor Crónico Infantily FTmonicaNessuna valutazione finora
- Treatment of Pediatric Migraine: Current Treatment Options in Neurology January 2015Documento20 pagineTreatment of Pediatric Migraine: Current Treatment Options in Neurology January 2015akshayajainaNessuna valutazione finora
- Management and Investigation of Neonatal Encephalopathy: 2017 UpdateDocumento13 pagineManagement and Investigation of Neonatal Encephalopathy: 2017 Updatenuge putriNessuna valutazione finora
- Headache - Approach To The Adult PatientDocumento28 pagineHeadache - Approach To The Adult PatientasasakopNessuna valutazione finora
- Clinician's Manual - Treatment of Pediatric Migraine - D. Lewis, (Springer, 2010) WW PDFDocumento75 pagineClinician's Manual - Treatment of Pediatric Migraine - D. Lewis, (Springer, 2010) WW PDFAnonymous VrCndGbKNessuna valutazione finora
- Rizzoli 2017Documento26 pagineRizzoli 2017Dirga Rasyidin LNessuna valutazione finora
- (Applied Clinical Psychology) Gerald Goldstein, Leslie Ruthven (Auth.) - Rehabilitation of The Brain-Damaged Adult-Springer US (1983)Documento368 pagine(Applied Clinical Psychology) Gerald Goldstein, Leslie Ruthven (Auth.) - Rehabilitation of The Brain-Damaged Adult-Springer US (1983)bharavi.vishwasraoNessuna valutazione finora
- Headache 1Documento5 pagineHeadache 1Aden Dhen100% (1)
- Headache CPG Final Jan2012 - EnglishDocumento15 pagineHeadache CPG Final Jan2012 - EnglishMary MarjorieNessuna valutazione finora
- Cerebral Palsy: Nature Reviews Disease Primers January 2016Documento25 pagineCerebral Palsy: Nature Reviews Disease Primers January 2016Firdaus BillyNessuna valutazione finora
- Headaches in Brain Tumor Patients: Primary or Secondary?: Headache CurrentsDocumento10 pagineHeadaches in Brain Tumor Patients: Primary or Secondary?: Headache CurrentsasfwegereNessuna valutazione finora
- Headache LectureDocumento57 pagineHeadache Lecturekhaled alahmadNessuna valutazione finora
- Tension Headache: Tension Headache Atau Tension Type Headache (TTH) Atau Nyeri KepalaDocumento4 pagineTension Headache: Tension Headache Atau Tension Type Headache (TTH) Atau Nyeri KepalaLester KeyNessuna valutazione finora
- Clinical evaluation of cervicogenic headacheDocumento8 pagineClinical evaluation of cervicogenic headacheLuca PellaNessuna valutazione finora
- Headache - 2008 - Conicella - The Child With Headache in A Pediatric Emergency DepartmentDocumento7 pagineHeadache - 2008 - Conicella - The Child With Headache in A Pediatric Emergency DepartmentRenata CardosoNessuna valutazione finora
- Endoscopic Kyoto 2020Documento13 pagineEndoscopic Kyoto 2020Xiomara CuadrosNessuna valutazione finora
- Pathologist ViewpontDocumento12 paginePathologist ViewpontXiomara CuadrosNessuna valutazione finora
- From Sidney To OlgaDocumento7 pagineFrom Sidney To OlgaXiomara CuadrosNessuna valutazione finora
- Current Perspectives in Atrophic Gastritis: Pathogenesis and EpidemiologyDocumento9 pagineCurrent Perspectives in Atrophic Gastritis: Pathogenesis and EpidemiologyFernando BorgesNessuna valutazione finora
- Autoimmune Atrophic Gastritis CurrentDocumento9 pagineAutoimmune Atrophic Gastritis CurrentXiomara CuadrosNessuna valutazione finora
- Review of Dermatofibrosarcoma Protuberans with Fibrosarcomatous Transformation: Our Experience and Literature ReviewDocumento7 pagineReview of Dermatofibrosarcoma Protuberans with Fibrosarcomatous Transformation: Our Experience and Literature ReviewXiomara CuadrosNessuna valutazione finora
- The Immune Microenvironment of Breast Ductal Carcinoma in SituDocumento10 pagineThe Immune Microenvironment of Breast Ductal Carcinoma in SituXiomara CuadrosNessuna valutazione finora
- Flash Card PatologyDocumento529 pagineFlash Card PatologyXiomara Cuadros0% (1)
- Tos Inexplicable. Chest 2015Documento18 pagineTos Inexplicable. Chest 2015Xiomara CuadrosNessuna valutazione finora
- EspondiloartrosisDocumento12 pagineEspondiloartrosisXiomara CuadrosNessuna valutazione finora
- EspondiloartrosisDocumento12 pagineEspondiloartrosisXiomara CuadrosNessuna valutazione finora
- Meta-Analisis Xiomara CuadrosDocumento14 pagineMeta-Analisis Xiomara CuadrosXiomara CuadrosNessuna valutazione finora
- Department of Family Medicine Fpe Headache Syndrome: - Vanaveera Pandian SwethaDocumento106 pagineDepartment of Family Medicine Fpe Headache Syndrome: - Vanaveera Pandian SwethaSuba Saravanan 12Nessuna valutazione finora
- Response of Cluster Headache To Kudzu (Complete)Documento15 pagineResponse of Cluster Headache To Kudzu (Complete)Andy RotsaertNessuna valutazione finora
- Test 2Documento15 pagineTest 2Ding DialyzerNessuna valutazione finora
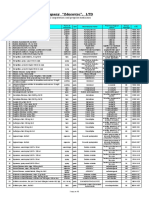
- Pharmaceutical Company "Zdorovye", LTD: Price-List (USD) 03.09.2019Documento10 paginePharmaceutical Company "Zdorovye", LTD: Price-List (USD) 03.09.2019Laura Del valleNessuna valutazione finora
- Diagnosis and Management of HeadacheDocumento12 pagineDiagnosis and Management of HeadacheRay BoettgerNessuna valutazione finora
- Review Article: Cluster Headache-Acute and Prophylactic TherapyDocumento24 pagineReview Article: Cluster Headache-Acute and Prophylactic TherapyPurna Adi PutraNessuna valutazione finora
- Chapter 80 - Headache DisordersDocumento41 pagineChapter 80 - Headache Disordersalina ignatNessuna valutazione finora
- Neuro (Part1) ATIDocumento12 pagineNeuro (Part1) ATIGie Lane Ayuyu100% (8)
- GepantsDocumento14 pagineGepantsmatheus galvãoNessuna valutazione finora
- Farmakologi Obat Anti Migraine: DR - Datten Bangun MSC, SPFK Dept - Farmakologi & Therapeutik Fak - Kedokteran Uhn MedanDocumento53 pagineFarmakologi Obat Anti Migraine: DR - Datten Bangun MSC, SPFK Dept - Farmakologi & Therapeutik Fak - Kedokteran Uhn MedanDion SaputraNessuna valutazione finora
- SIGN 155 - Pharmacological Management of Migraine: A National Clinical Guideline February 2018Documento52 pagineSIGN 155 - Pharmacological Management of Migraine: A National Clinical Guideline February 2018Yahya RizkiNessuna valutazione finora
- Rezitriptan in MigraneDocumento19 pagineRezitriptan in MigraneGurdeep SinghNessuna valutazione finora
- Iron-rich foods for sickle cell anemiaDocumento24 pagineIron-rich foods for sickle cell anemiaZyla MalinaoNessuna valutazione finora
- Formulary Thera Class PDFDocumento33 pagineFormulary Thera Class PDFElla LopezNessuna valutazione finora
- Pebc Evaluating Exam Sample QuestionDocumento39 paginePebc Evaluating Exam Sample Questionmahyar_ro79% (14)
- Quiz 1: General MOADocumento38 pagineQuiz 1: General MOASajeda A. HadiNessuna valutazione finora
- Acute Treatment of Migraine in Adults - UpToDateDocumento42 pagineAcute Treatment of Migraine in Adults - UpToDateClaudio Avalos MorenoNessuna valutazione finora
- MedsDocumento15 pagineMedsJanetteNessuna valutazione finora
- 03 Guidance For Pharmacists On The Safe Supply of Sumatriptan 50mg TabletsDocumento4 pagine03 Guidance For Pharmacists On The Safe Supply of Sumatriptan 50mg TabletssefrounfNessuna valutazione finora
- Ch071 - 001-007 Migraine HeadacheDocumento7 pagineCh071 - 001-007 Migraine Headached_94100% (1)
- MOCA PEDS 2021 Required ReadingDocumento26 pagineMOCA PEDS 2021 Required Readingerica100% (1)
- Newer Formulations of The Triptans: Advances in Migraine ManagementDocumento21 pagineNewer Formulations of The Triptans: Advances in Migraine ManagementShivam BhadauriaNessuna valutazione finora
- Pharma Chronicle JUly 2011Documento55 paginePharma Chronicle JUly 2011Elmer RicoNessuna valutazione finora
- NPLEX Combination Review Neurology - C: Paul S. Anderson, ND Medical Board Review ServicesDocumento46 pagineNPLEX Combination Review Neurology - C: Paul S. Anderson, ND Medical Board Review ServicesValeria AcevedoNessuna valutazione finora
- Treating Yourself Magazine #17Documento132 pagineTreating Yourself Magazine #17murciano207100% (1)
- Management of Migraine Headache: An Overview of Current PracticeDocumento7 pagineManagement of Migraine Headache: An Overview of Current Practicelili yatiNessuna valutazione finora
- Flexin Marketing ReportDocumento68 pagineFlexin Marketing ReportHammad BukhariNessuna valutazione finora
- 11 875 670 Preparation and Utility of SuDocumento142 pagine11 875 670 Preparation and Utility of Suthathpurusha_5Nessuna valutazione finora
- Acute Migraine Treatment.6Documento16 pagineAcute Migraine Treatment.6BryanNessuna valutazione finora