Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
OJOLHNS-11 Issue-I Jan-June-2017
Caricato da
DR K C MALLIKCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
OJOLHNS-11 Issue-I Jan-June-2017
Caricato da
DR K C MALLIKCopyright:
Formati disponibili
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
ORISSA JOURNAL OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY
(An Internationally & Nationally Indexed Journal)
VOLUME - XI ISSUE I, JANUARY-JUNE, 2017
Journal is listed in:- ICMJE- International Committee Of Medical Journal Editors (08.08.2016)
NLM.(Medline)-Uniquie ID- 101648238
Indexed in :- Index Copernicus International plc, (Poland), Google scholar,
Cosmos indexing(Germany), CiteFactor (USA), DRJI- Directory of research journals indexing(India), WCOSJ-World
Catalogue of science journals (Poland), SciLit (Switzerland), ISI- International society of Indexing (India),
RootIndexing (India), Infobase Indexing (India), SiFactor- Systematic Impact Factor (India)
Sci- Scientific citation indexing,Polindex (Poland) And Scribd.
This journal is an Official Publication of the Association of Otolaryngologists of India, Orissa State Branch. All rights
owned by the Association of Otolaryngologists of India, Odisha State Branch (OSB.) ISSN-0974-5262
Email- editorodishaentjournal@gmail.com, Website: www.ojolhns.com URL https://www.ojolhns.com DOI - 10.21176/ojolhns.0974-5262
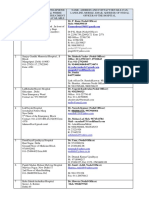
EDITORIAL BOARD
Editorial Chairman/Editor-in Chief Address for Correspondence
Prof Abhoya Kumar Kar Cell- 09437165625, 09437036411
Editorial Advisory Board Member of International Email: rudra.biswal7@yahoo.com
Journal of Phonosurgery & Laryngology, JIMA,
Associate Editor
World Articles in ENT, ORL Clinics International
Journal,Indian Journal of Clinical Medicine, Dr K. C. Mallik
Elsevier(India) Publications, IJLO & HNS. Associate Professor, Dept of ENT andHNS
PANACEA & OMJ. S.C.B. Medical College, Cuttack, Odisha,
Correspondence address:
Cell- 09437092087
10703 Elliston Way NE REDMOND,
WA-98053,USA. Email: drkrishnachandramallik@gmail.com
Phone(Res): +1-425-216-3700 / (Cell): )425-638-9286. Assistant Editor
Email- abhoya.kar@gmail.com Dr. Subhalaxmi Rautray
Editor Assistant Professor, Dept of ENT and HNS
Prof. R. N. Biswal
S.C.B. Medical College, Cuttack, Odisha,
Professor of ENT and Head and Neck Surgery,
Kalinga Institute of Medical Sciences (KIMS), Mob.82802165585
KIIT University, Bhubaneswar Email: drsubhalaxmirautray123@gmail.com
NATIONAL EDITORIAL ADVISORY BOARD
Prof. G. C. Sahoo Prof. Sanjeev Mohanty
M.S., FIMSA, MANFP & TMJO (USA) Prof and HOD, ENT. SRMC, PORUR S33, I-Block, Jains
Dean & Principal Avantika Apartment Manapakkam,
Gouri Devi Institute of Medical Sciences & Hospital Chennai-600116 ,
G T Road, Rajbandh, Durgapur, 713212 Mob-: 9840131091
West Bengal E mail: drsanjeevmohanty@gmail.com
Mob- 9083249550 Prof. Bachi T. Hathiram;
Email- gcsent99@gmail.com Flat No.-2, Ground Floor;
Prof. Dipak Ranjan Nayak, M.N.Banaji Building;
Department of ENT-Head & Neck Surgery, Forjett Street Cross Road;
Kasturba Medical College, Opp. Saibaba Temple;
Manipal, KARNATAK Mumbai- 400 036; Maharashtra, India
E-mail: drnent@gmail.com Email: bachi.hathiram@rediffmail.com
Prof. S. K. Behera Prof. B. Viswanatha
Department of ENT-Head & Neck Surgery, # 716, 10th Cross, 5th Main; MC Layout, Vijayanagar;
S.C.B.Medical College, Cuttack, Odisha. Bangalore 560030;
Mob- 9437015511 Email: drbviswanatha@yahoo.co.in
ii Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
Prof. K. K. Ramalingam Prof. P. S. N. Murthy,
K.K.R ENT Hospital & Research Institute, Head of Dept of E.N.T.,
274 Poonamalllee High Road, P.S.I. Medical College, Chinoutpalli,
Kilpauk, Chennai- 600 010, At/P.O. Gannavaram, Vijayawada,
Tamil Nadu. Andhra Pradesh.
Phon: 044-26411444. E mail: drmurtypsn@gmail.com
E mail: kkramalingam@hotmail.com
Prof. Mohan Kameswaran
Dr. Madan Kapre; Madras E.N.T. Research Foundation(P) Ltd; 1,
Neeti Clinics & Nursing Home (ENT);
1st Cross Street; Off. 2nd Main Road;
NeetiGaurav Complex; 21, Central Bazar Road;
Raja Annamalaipuram; Chennai-600028; Tamil Nadu.
Ramdaspeth; Nagpur 440010; Maharashtra.
E mail: merfmk@yahoo.com
Email: madankapre@gmail.com
Prof R. Jayakumar, Prof T. V. Krishna Rao
Senior Consultant, Dept ofE.N.T., Uma Krishna; 5-9-30-1/27 AB,
Kerala Institute of Medical Sciences(KIMS), Basheerbagh Palace; Hyderabad-500053;
P.B. No. 1, P.O. Anayara, Trivandrum-695029, Kerala Andhra Pradesh.
Email: jkrmenon@rediffmail.com E mail: drrao@mmdsofttech.com
Prof. Achal Gulati; Prof. Krishna Kishore T.
Prof ENT, Mualana Azad Medical College Superintendent, and HOD, Dept. of ENT & HNS,
A-72, SwasthyaVihar; Delhi-110092. Govt ENT Hospital and Andhra Medical College,
Email: achalgulati@rediffmail.com China Waltair, Visakhapatnam, 500017,
Prof T.S. Anand; A P India, Mob.919849116868
4, Hemkunt Colony;Opp. Nehru Place; New Delhi-110048. Email: drkktent@hotmail.com
Email: doctoranand50@yahoo.com Dr. Kumar Pravash
Prof. Vikash Sinha, Senior Consultant,Tata Memorial Hospital
Dean, MP Shah Medical College, Shivam-6, TMC Colony, SION Tromba, Mumbai-88
Pt. Nehru Road, Jamnagar-361008, Gujerat. Mob.09224182898
E mail: dr_sinhavikas@yahoo.co.in E mail: kpravashi1@gmail.com
INTERNATIONAL EDITORIAL ADVISORY BOARD
Prof. Ashutosh Kacker M.D Prof. Sylvester Fernandes
Professor of Clinical Otorhinolaryngology 22 Kelton St Cardiff NSW Australia
Weill Cornell Medical College, Sylvester.
NY, NY 10021, USA Email: fernandes@newcastle.edu.au
Personal address:- Dr. Sharat Mohan
1305 York Avenue, 5th floor, NY, NY 10021 ENT & Voice surgeon
USAT:(646)962-5097, F: 646) 962-0100 National Health Services
Email: ask9001@med.cornell.edu Derby, United Kingdom
Prof. Arun K. Gadre, MD, FACS Email: sharatmohan@hotmail.com
Heuser Hearing Institute Prof.Ullas Raghavan
Professor of Otology and Neurotology, Department of ENT, Doncaster Royal Infirmary,
Division of Otolaryngology Armthorpe Road, Doncaster DN2 5LT UK
Email: ullasraghavanent@yahoo.com
Head and Neck Surgery, University of Louisville,
Prof. Prepageran Narayanan
401 E Chestnut St Suite 710,Louisville,
Dept ofOtolaryngologyand Head & Neck Surgery.
KY 40202, USA
University Malaya Medical Center, Malaysia.
Email: arungadre@yahoo.com
Email: prepageran@yahoo.com
Prof.Ludwig Moser
Prof. Peter Catalano, MD, FACS, FARS
University of Wuerzburg Chief of Otolaryngology
Department of Oto-Rhino- St. Elizabeths Medical Center
Laryngology, Plastic, Aesthetic, Professor of Otolaryngology
and Reconsructive Head and Neck Surgery Tufts University School of Medicine
Wuerzburg, Bavaria, Germany Medical Director of ResearchSteward Health Care
Email: l_u_moser@hotmail.com Email: peter.Catalano@steward.org
Vol.-11, Issue-I, January-June - 2017 iii
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Prof.Sady Selaimen da Costa Prof. Dan M. Fliss
Federal University of Rio Grande do Sul, Professor and Chairman Deprtment of
Faculty of Medicine, Department of Otolaryngology Head and Neck Surgery
Ophthalmology and Otorhinolaryngology,
Tel Aviv Sourasky Medical Center
Rua Ramiro Barcelos, 2350
Zone 19 Room 1922Good End, 6 WEIXMANN ST.TELAVIV-64239 ISRAEL,
Porto Alegre, RS. TEL-972-3-697-3573,
Brazil - CEP 90035-003 Email - fliss@tlvmc.gov.il
Email: selaimen@gmail.com Prof. Shigeru Hirano, M.D., Ph.D.
Prof. Douglas D. Backous, MD, FACS. Department of Otolaryngology
Medical Director Head & Neck Surgery
Center dor Hearing&SSkull Base Surgery
Kyoto Prefectural University of Medicine,
Swedish Neurosciences Institute Seattle
Washington, USA JAPAN, Ph.: 075-251-5603
Email: douglas.backous@swedish.org Email: hirano@koto.kpu-m.ac.jp
STATISTICAL ADVISORY BOARD
Dr. Kaushik Mishra Dr. Sandeep Kumar Panigrahi
Associate Professor (RHTC) Assistant Professor,
Dept. of Community Medicine Dept. of Community Medicine
SCB Medical College, Cuttack IMS & SUM Hospital, Bhubaneswar
Mob.: 9437228312 Mob: 9439369093
Email: kaushikmishra1965@gmail.com Email: dr.sandeepvss@gmail.com
INTERNATIONAL CO-ORDINATOR
PROF. DEEPAK RANJAN NAYAK
Dept of ENT and Head and Neck Surgery, Kasturba Medical College, Manipal, Karnatak
E-mail: drnent@gmail.com
The views expressed in the articles are entirely of individual author. The Journal bears no responsibillity about
authenticity of the articles or otherwise any claim how-so-ever. This Journal does not guarantee directly or
indirectly for the quality or efficiency of any product or services described in the advertisements in this issue,
which is purely commercial in nature.
STATEMENT OF OWNERSHIP & OTHER PARTICULARS OF ODISHA JOURNAL OF
OTOLARYNGOLOGY AND HEAD & NECK SURGERY
1. Place of Publication : Cuttack, Odisha
2. Periodicity of Publication : Half yearly
3. Nationality of Publisher : Indian
4. Publishers name & Address : Dr. K.C. Mallik, Plot. No. 460 / C-03, Sector-8,
CDA, Cuttack, Odisha, India, 753014
5. Owner of the Journal : Association of Otolaryngologists of India, Odisha State Branch.
6. Printers Name and Address : Bani Press, Tulasipur, Cuttack - 8
I Dr K.C.Mallik hereby declare that, the particulars given above are true to the best of my knowledge &
belief.
Sign. of Publisher
Dr. K.C.Mallik
iv Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
INSTRUCTIONS TO AUTHORS
The Orissa Journal of otolaryngology and Head & Biomedical journals. Published by the international
Neck Surgery is a half yearly medical journal indexed Committee of Medical Journal, Editorswebsite- http://
, Internationally (Index Copernicus international plc, www.icmje.org. The manuscript should be computer
Poland: http: // indexcopernicus.com) & Nationally typed in MS Word (Office 97 onwards) in point.size of
(Nircar, ISSN 0974-5262) Indexed], which publishes 12 on white opaque paper. Use double spacing through
original articles and case reports. Case Reports (clinical out out for typing the manuscript. Provide margins of
records) should be very brief and should be confined to 2.5 cms on all sides. Type on the side of paper only.
single cases without precedent in Indian literature or to Submit 2 copies of manuscript. The author (S) should
cases which illustrate some, entirely new fact in send a copy of the article in a compact disc (CD) along
management and investigation. with Publication cost. The diskette should be labelled
All articles are reviewed by one or more experts to with the name of the author (S), title of article and the
determine validity, significance, originality of context name and version of the word processor used (Microsoft
and conclusions. Articles should not exceed 5000 words. word).
Case reports should be restricted to 2000 words. Photographs, if included in the electronic format should
All submissions should include (i) a letter transferring he scanned at 300 dpi and sent as jpeg format. Images or
the copyright of manuscript to the Association of photographs should be in separate files or folders.
Otolaryngologists of India,Orissa State Branch (ii) 2 copies of 2. Title Pages: The title of the paper should be typed with
the manuscript (iii) 2 sets of illustrations, tables etc, state the capital letters on the top. The name of the authors should
name and address in full of the author to whom be given below the title. The initials and surname should
correspondence should be made giving contact numbers and be slated. Titles such as Dr of Mr and academic
e-mail ID. qualifications should not be mentioned either below
Authors should not be more than five. The copyright the title or in the footnote. The footnote should mention
transfer letter can be downloaded from the website of journal the names of the authors, the name of the institution, the
- https://www.ojolhns.com meeting at which the paper was read and
From the year 2017 we are encouraging the authors to acknowledgements and address for correspondence
submit the articles only on website - https://www.ojolhns.com with the main author. The footnote should appear on
Only one copy of the manuscript and illustrations will the title page. The title of the articles should not contain
be returned in case the manuscript is not accepted for more than 50 characters.
publication. The letter transferring copyright should 3. Abstract and keywords: A concise abstract of not more
be addressed to the Associate Editor and should state than 200 words is required for all original clinical and
that, the manuscript has not been published in a part or basic science contributions to facilitate rapid indexing
in whole elsewhere and is solely contributed to the Orissa and assimilation into the medical literature. Abstracts
Journal of Otolaryngology and Head & Neck Surgery. should be organized according to the outline below.
It should mention that, the authors undersigned hereby Objective: Brief clear statement of the main goals of the
transfer, assign and otherwise convey all copyright investigation.
ownership to the Association of Otolaryngologist of Study design: eg. Randomized,prospective double blind,
India, Orissa State Branch and that the authors do not retrospective case review)
have any objection to reviewing and editing of this Setting: eg. Primary care Vs Tertiary referral centre,
submission of the Editorial Board. ambulatory Vs Hospital.
Manuscripts sent without covering letter transferring Patients: Primary eligibility criteria and key
copyright, signed by all the authors of the manuscript demographic features, interventions: Diagnostic,
will not be reviewed and accepted for publication. therapeutic and/or rehabilitative. Main outcome
1. Manuscript : Manuscripts are sent out for blinded peer Measure (S): The most essential criterion that addresses
review. Do not include authors names or institutions the studys central hypothesis.
on text pages or on figures in the manuscript. The Results: Include statistical measure as appropriate.
authors names and institutional affiliations should Conclusions : Include only those conclusions that are
appear only on the Manuscripts submitted to directly supported by data generalized from that study.
Vol.-11, Issue-I, January-June - 2017 v
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Basic Science Reports: The top should be marked with an arrow. Illustrations
Hypothesis: Brief clear statement of the main goals of should be of very high contract and very clear Line-
the investigation diagrams should be drawn on separate sheets with black
Background: Concise, designed for orientation of the Indian ink on thick white paper. The size should be at
reader, who is unfamillar with this line of investigation. least twice that of final reproduction. Lettering should
Methods: Succint summary of techniques and materials be professionally done and not handwritten or typed.
used. Each illustration should be described in a legend and
Results: Include statistical measures where appropriate. grouped on a separate sheet of paper. The legends of
Conclusions: Include only those directly supported by micro-photographs should mention the stain as well as
date generated from this study. Emphasize clinical the magnification. The illustration should not be folded
relevance wherever possible. On the same manuscript during transmission and protected by cardboard. Two
page as the structured abstract, list in alphabetical order, sets of illustrations must be submitted with the
key words (maximum of seven) for indexing using manuscript. The illustration of any patients must be
Medical Subject Headings (MeHS) from Index Medicus. shadowed with black rectangles over their eyes so as to
cover / nullify their identities.
Disclosures
5. Tables: Tables should be given Roman numbers and
Authors must declare the disclosures as given below &
referred to in the text as Table No. They should be as
also send the certificates regarding permission of ethical
few as possible and contain only essential data. They
committee while submitting the main articles (both
should be type written on separate sheets of paper. The
prospective & retroprospective studies). All these will be
tables must have a descriptive.
displayed at the end of each article before the reference
section . 6. Statistics: Statistics should be completed in consultation
(a) Competing interests/Interests of Conflict- None/If any with a biostatistician.
(b) Sponsorships - None/If any 7. Abbreviations: Abbreviations should be standard
abbreviations.
(c) Funding - None/If any
8. Drug names: Use generic name with the trade names in
(d) Written consent of patient- Taken/not applicable
parentheses.
(e) Animal rights- Maintained/not applicable.
9. Bibliography: Bibliography should be given at the end
(f) Plagiarism not done/not crossed the limit.
of the article on a separate sheet of paper in ICMJE
4. References: References must be numbered consecutively style. The names of the journals should be underlined
according to the order of their citation in the text. Use and should appear with standard abbreviation. The full
numbers in parentheses for the citations. Personal
title of the paper should be given. Mention et al after
communication and unpublished data may be cited as
writing the names of three authors, if the authors are
such in the text, but are not listed in the references.
less than three of write the names of all the authors.
Journal title should be abbreviated according to
Adapted From:
Index Medicus. Reference should be made giving the
National Information Standards Organization NISO
authors surname with the year of publication in
Z39.29-2005 (R2010) Bibliographic References as
parentheses. Only papers closely related to the subject
adapted by the National Library of Medicine for its
should be quoted. Original papers should not have more
databases
than 16 references and case reports should not have more
than 6 references. 1. Standard journal article
It is most important that the authors should verify List the first six authors followed by et al. Halpern SD,
personally the accuracy of the exact reference. The Ubel PA, Caplan AL. Solid-organ transplantation in
responsibility of having permission to reproduce. HIV-infected patients. N Engl J Med. 2002 Jul 25;
Illustrations and photographs from others published 347(4):284-7.
work will rest with the authors. A. More than six authors:
Illustrations: Illustrations should be referred to the text Rose ME, Huerbin MB, Melick J, Marion DW, Palmer
as figs and given Arabic numbers. They should be AM, Schiding JK, et al. Regulation of interstitial
marked lightly with pencil on the back with the figure excitatory amino acid concentrations after cortical
number, caption, names of authors and title of the paper. contusion injury. Brain Res. 2002;935(1-2):40-6.
vi Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
B. Optional addition of a databases unique identifier 8. Issue with part
for the citation: Ahrar K, Madoff DC, Gupta S, Wallace MJ, Price RE,
Halpern SD, Ubel PA, Caplan AL. Solid-organ Wright KC. Development of a large animal model for
transplantation in HIV-infected patients. N Engl J Med. lung tumors. J Vasc Interv Radiol. 2002;13(9 Pt 1):923-8.
2002 Jul 25; 347(4):284-7. Pub Med PMID: 12140307. 9. Issue with no volume
Forooghian F, Yeh S, Faia LJ, Nussenblatt RB. Uveitic Banit DM, Kaufer H, Hartford JM. Intraoperative frozen
foveal atrophy: clinical features and associations. Arch section analysis in revision total joint arthroplasty. Clin
Ophthalmol. 2009 Feb;127(2):179-86. PubMed PMID: Orthop. 2002;(401):230-8.
19204236; PubMed Central PMCID: PMC2653214.
10. No volume or issue
C. Optional addition of a clinical trial registration
Outreach: bringing HIV-positive individuals into care.
number:
HRSA Careaction. 2002 Jun:1-6.
Trachtenberg F, Maserejian NN, Soncini JA, Hayes C,
11. Pagination in roman numerals
Tavares M. Does fluoride in compomers prevent future
caries in children? J Dent Res. 2009 Mar;88(3):276-9. Chadwick R, Schuklenk U. The politics of ethical
PubMed PMID: 19329464. ClinicalTrials.gov consensus finding. Bioethics. 2002;16(2):iii-v.
registration number: NCT00065988. 12. Type of article indicated as needed
2. Organization as author Tor M, Turker H. International approaches to the
Diabetes Prevention Program Research Group. prescription of long-term oxygen therapy [letter]. Eur
Hypertension, insulin, and proinsulin in participants Respir J. 2002;20(1):242.
with impaired glucose tolerance. Hypertension. Lofwall MR, Strain EC, Brooner RK, Kindbom KA,
2002;40(5):679-86. Bigelow GE. Characteristics of older methadone
3. Both personal authors and organization as author (List maintenance (MM) patients [abstract]. Drug Alcohol
all as they appear in the byline.) Depend. 2002;66 Suppl 1:S105.
Vallancien G, Emberton M, Harving N, van Moorselaar Books and Other Monographs
RJ; Alf-One Study Group. Sexual dysfunction in 1, 274 13. Personal author(s)
European men suffering from lower urinary tract Murray PR, Rosenthal KS, Kobayashi GS, Pfaller MA.
symptoms. J Urol. 2003;169(6):2257-61. Medical microbiology. 4th ed. St. Louis: Mosby; 2002.
Margulies EH, Blanchette M; NISC Comparative 14. Editor(s), compiler(s) as author
Sequencing Program, Haussler D, Green ED.
Gilstrap LC 3rd, Cunningham FG, VanDorsten JP,
Identification and characterization of multi-species
editors. Operative obstetrics. 2nd ed. New York:
conserved sequences. Genome Res. 2003 Dec; 13(12):
McGraw-Hill; 2002.
2507-18.
Charges Payable: According to the decision of the AOI,
4. Article not in English
Orissa State Branch contributors of the articles are to
Ellingsen AE, Wilhelmsen I. Sykdomsangst blant
pay Rs. 2,500/- for printing charges. Diagrams & Tables
medisin- og jusstudenter. Tidsskr Nor Laegeforen.
over 2 diagrams or 2 tables or 1 diagram and 1 table is
2002;122(8):785-7. Norwegian.
charged extra at the rate of Rs. 250/- for each diagram/
5. Volume with supplement
table in addition to Rs. 2,000/- The total Publication
Geraud G, Spierings EL, Keywood C. Tolerability and
cost should be sent along with the CD by Registered/
safety of frovatriptan with short- and long-term use for
Speed Post. D.D. for such payments are to be made in
treatment of migraine and in comparison with
the name of Orissa Journal of Otolaryngology & HNS
sumatriptan. Headache. 2002;42 Suppl 2:S93-9.
Payable at Cuttack, Odisha.
6. Issue with supplement
Addressed To:-
Glauser TA. Integrating clinical trial data into clinical
Dr. K. C. Mallik
practice. Neurology. 2002;58(12 Suppl 7):S6-12.
7. Volume with part Associate Editor,OJOLHNS
Abend SM, Kulish N. The psychoanalytic method from Plot. No. 460/3C, Sector -8, CDA, Cuttack,
an epistemological viewpoint. Int J Psychoanal. Odisha, India, PIN-753014, Cell- 09437092087
2002;83(Pt 2):491-5. Email: editorodishaentjournal@gmail.com
Vol.-11, Issue-I, January-June - 2017 vii
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
EDITORIAL
AN OBITUARY TO PROF A.MAHADEVAIAH
Doyen of Otology
NOBILITY THY NAME IS MAHDEVAIAH
A Short Biography of Dr. Mahadevaiah
Its a great honor for me to write the biography his friend who was moderately deaf and for want of
of one of the great ENT surgeon of the country who monetary circumstances could not get his deficiency
is none other than Dr.Agadurappa Mahadevaiah. Dr. repaired. This all the more prompted Dr.Mahadevaiah
Mahadevaiah was born on 16th August 1935 in the to adore the role of an ENT surgeon so as to restore
outskirts of Bangalore. He was the 1 st son to hearing of moderately deaf patient.
Mr.Agadurappa and Mrs Nanjappa along with 6 At that point of time the ENT faculty of India
brothers and 3 sisters. His rural background and sense was grossly under developed. Since he has immense
of human service, influenced his aspirations to become thirst for Otology he moved to US with the hope of
a doctor. However, at the point of time the acquiring Otologic surgical skills. Having landed in the
independence moment in our country was active and US in 1963 he proceeded to Canada for his internship
Dr. Mahadevaiah used to take part in the Bhoodana for one year and six months in Neurosurgery under
movement launched by Vinoba Bhave during his school Dr.Eric Peterson and another 6 months in ENT under
holidays in 1950s. He did his MBBS from Bangalore Dr. Guy Lambramboise at Ottawa General Hospital
Medical College in 1956. Having been reared up in rural Ottawa. To obtain his ENT training he proceeded back
platform, his thinking was molded to serve the people to US, but it necessitated one year residency program
by offering them good health. This motivation in general surgery that he completed successfully at
transpired him to enter medical profession. As a medical Norwalk hospital, Norwalk, Connecticut. This was the
student, he aspired to become an ENT surgeon since turning point in his life. He was very much aspired for
viii Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
Otologic program and applied for the same. However surgeries and was first to repair C.S.F. leak by external
as there was immense competition for ENT training ethmoid route using operating microscope in India. As
program, he was put on a waiting list for several years started rolling by, he felt that he should have his
months. Probably this might have been the most own organization and that saw the birth of
depressive feeling for a man with such a positive, BASAVANGUDI ENT CARE CENTRE, Bangalore
blossoming and optimistic outlook. During the waiting which is the alma mater to many practicing ENT
period, to prolong his stay in USA, he has to do some surgeon including me.
other residency for which he has to sign a contract to Having commenced his ENT practice at the above
do pediatric residency at Hale University in New centre from 1976, there was no looking back. He has
Heaven, Connecticut. Before starting that residency performed more than 25000 chronic ear surgeries and
program, fortunately with the blessings of God, he got had done innumerable number of nasal surgeries. Even
ENT residency at St. Lukes Hospital, New York with till recently before he demised, he was one of the best
the help of Dr. Stanley Whitefield, Director of ENT rhinoplasty surgeon in India in comparison with any
Department in a second interview. plastic surgeon. He could have accomplished all these
When he joined the residency in 1965, in St.Lukes at USA with more monetary gain. But he felt Honor
Hospital, New York, he was blessed with 100 temporal and Pride was above the external advantages of rank
bones given by Lempert Institute. At that point of time and fortitude. He was an absolute non commercial
he utilized the opportunity and dissected many person and was very particular that no one should walk
temporal bones to master temporal bone anatomy. As out of his centre for want of money to cure their disease.
a resident he had performed more than 714 ENT Further he commenced temporal bone dissection and
surgeries which included 21 stapedectomies and 2 live surgical demonstration in his own centre along with
spheno-ethmoidectomy and open external Dr.Vijayendra. Together they have conducted more
ethmoidectomy for CSF repair. In 1968 he obtained than 25 courses in the past decade. These courses were
his American Board degree in Otorhinolaryngology widely attended by ENT surgeons across the country.
in the first attempt. This is the most difficult He was the past president of AOI 1995-96 and president
examination where the candidate is examined by 21 of Indian society of Rhinology from 2004-2005. He
external examiners. After passing the American Board, was also the President of Karnataka state of AOI and
he underwent 18 months fellowship in otology at Bangalore branch of AOI. In the domestic front he
Columbia University. In 1969 October he left the USA
was blessed with beloved wife and two daughters.
for India to serve fellow Indians. He had forfeited a
lucrative carrier in the US for the benefit of poor and It was a dream comes true when he wrote a book
downtrodden. Many of his Professors in US refused on Surgical techniques in chronic otitis media and
to relieve him but Dr. Mahadevaiah was steadfast and otosclerosis. For which he had burnt the midnight
bound open coming to India to live with our people oil for several months and accomplished the same. As a
and train young ENT surgeons. He was a great human being one had duties to God, to his family,
nationalist with deep involvement in Gandhian neighbors, and countrymen. Dr Mahadevaiah has
principle. accomplished his duties to God in a divine manner. To
his family member he was an excellent husband and
Having landed in India, he stated his ENT practice
father. To his neighbors he had acted on the square
in a small way and had a short stint of Govt. service as
such that he could do what he felt must be done. To
a lecturer in Bangalore Medical College. At this point
his fellow countrymen he had done charity, practiced
of time there were a few otologists in our country to
honesty and served his best.
perform ear surgeries. Since he had acquired the
advanced otological experience, he could effectively put What has been mentioned above is just the tip of
into practice in Bangalore. Which slowly but steadily iceberg of Dr Mahadevaiahs life. His sudden demise
established his name. He was also associated with has shocked the entire ENT fraternity of the country.
NIMHANS, Bangalore as a ENT and Skull Base Our deepest condolences
surgeon. He had performed numerous skull base Dr. H. Vijayendra
Vol.-11, Issue-I, January-June - 2017 ix
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
ORISSA JOURNAL OF OTOLARYNGOLOGY AND HEAD & NECK SURGERY
(An Internationally & Nationally Indexed Journal)
Volume-XI, Issue-I, January-June 2017
Contents
Sl.No Tittle and authors Pages
Editorial Board : ii - iv
Instructions to Authors : v - vii
EDITORIAL
An Obituary to Prof. A. Mahadevaiah
Dr. A. Mahadevaiah : viii - ixi
MAIN RESEARCH ARTICLES
1. Deep Neck Space Infections: Presentations and Management
G.M Puttamadaiah, H.S. Satish, B. Viswanatha : 01-06
2. Prevalence and Factors Related to Hearing Impairment among mainstream
Primary School Children in rural Southern India
Jeeva Thankom Philip, Rejee Ebenezer Renjit : 07-15
3. Oncological outcome analysis of trans-nasal minimally invasive endoscopi
resection of sino-nasal malignancy not transgressing the DURA:
A single centre study
Dipak Ranjan Nayak, Suraj Nair, Apoorva N Reddy, Balakrishnan
Ramaswamy, Rohit Singh : 16-24
4. Anterior Nasal Packing vs Septal clips type III, in Post Nasal Septal
Submucus Resection & Septoplasty Surgeries: A Comparative Study
CB Nandyal, Ravy Udgir, LR Shankar Naik, Vinayak Kurle : 25-31
5. Comparison of Hearing Results of Type III Tympanoplasty with
Mastoidectomy with or without Augmentatiion of Stapes Head
Netra A Pathak, Vidya V Rokede : 32-36
6. Utility of Hadad Flap in Reconstruction of Anterior Skull Base Defects
Following Endoscopic Transnasal, Trans Sphenoidal Approach to
Pituitary- Our Experience
Harshita V. Sabhahit, Shruthi GS, Santosh AN, G Prabhakar, Ananthkrishnan : 37-42
7. An Analysis of Inside out Mastoidectomy with Tympanoplasty with or
without Ossiculoplasty for Management of Middle Ear Cleft Cholesteatoma
Chandra Manish, Rajeev Krishna Gupta, Satveer Singh Jassal, Sikhar Saxena : 43-48
8. 4 Hands Reaching out Endoscopically to the Pituitary- Our Experience
G Sundhar Krishnan, George Nitha Mary : 49-53
CASE REPORTS:
9. A Case Report of Papillary carcinoma in Toxic Multinodular Goitre
Gopalakrishnan Midhun P, Sajikumar NR : 54-56
10. Wooden Foreign Body in Nasal Cavity: An Unusual Case Report
Subrat K Behera, Girija S Mohanta, Pitabas Nayak : 57-59
11. Tornwaldts Cyst - A Hidden Entity- A Case Report
Sanket D Vakharia, Seema R Gupta, Maya Shankar B Vishwakarma, S A Jaiswal : 60-62
x Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
MAIN RESEARCH ARTICLE
DEEP NECK SPACE INFECTIONS:
PRESENTATIONS AND MANAGEMENT
*
G.M Puttamadaiah, **H.S Satish, ***B.Viswanatha
HOW TO CITE THIS ARTICLE Date of receipt of article - 19-11-2016
Puttamadaiah GM, Satish HS, Viswanatha B. Deep neck space Date of acceptance 09-01-2017
infections: presentations and management.Orissa J
Otolaryngology Head Neck Surgery 2017 June; 11(1): 1-6. DOI:
DOI- 10.21176/ojolhns.2017.11.1.1
10.21176/ojolhns.2017.11.1.1 DOI URL- https://doi.org/10.21176 ojolhns.2017.11.1.1
ABSTRACT:
Deep neck space infections include, infections involving para-pharyngeal, retropharyngeal and submandibular
spaces. Intrinsic or deep neck space infections usually represent the overgrowth of the normal flora with most
infections being polymicrobial. The infections are of dental origin in a majority of the cases. The purpose of this
study was to determine the various presentation, diagnosis and management outcomes of deep neck space infections.
This study was conducted in the department of ENT, Bangalore Medical College and Research Institute, Bangalore
from January 2014 to December 2015. Fifty (50) cases presenting with signs and symptoms of deep neck space
infections to our Centre in the above period were evaluated. Dental infections were the most common aetiology
followed by recurrent tonsillitis. Ludwigs angina was the most common form of abscess, Incision and drainage
was the most effective treatment. Diabetes mellitus (18%) was the most common associated systemic disease &
complications encountered were airway obstruction and necrotizing fasciitis.
Key words: Deep neck space, infections, management.
INTRODUCTION: surgical and medical management are very important
Deep neck space infections include infections in the management of deep neck space infections.
involving para-pharyngeal, retropharyngeal and The objectives of this study to determine the
submandibular spaces1. Intrinsic or deep neck space following aspects with respect to deep neck space
infections usually represent the overgrowth of the infections are:- 1. Aetio-pathogenesis and risk factors
normal flora; with most infection being polymicrobial2. associated, 2. Clinical presentation, 3. Different
Deep neck infections spread along the fascial planes and diagnostic modalities available & 4.Management and
spaces of the head and neck region. Despite the outcome.
widespread use of antibiotics for the early treatment
Affiliation:
of cervical infections and improvements in dental care
*,**,***-ENT Department, Bangalore Medical College
and oral hygiene, deep neck infections still remain & Research institute, Bangalore, India
relatively frequent3. Address of correspondence:-
B. Viswanatha
The management protocols of these infections Professor, ENT department
have not been well defined and are often challenging Bangalore Medical College & Research Institute
due to the proximity of vital neck structures. Decision Bangalore, INDIA
email: drbviswanatha@yahoo.co.in
making between only medical management versus Mob.: 91984594283
Vol.-11, Issue-I, January-June - 2017 1
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
METHODOLOGY: trismus, that seen in 40 patients (90%), followed by
This study was conducted in the department of neck swelling (38 patients,84%), poor oral hygiene
ENT, Bangalore Medical College and Research (32patients,64%), and caries tooth (34 patients 68%).
Institute, Bangalore from January 2014 to December Cause was not known in 18patients (36%). Dental
2015. The prospective study was conducted on patients infections were the cause in 25patients (50%), followed
with deep neck space infections, presenting with by Recurrent Tonsillitis in 5patients (10%) [Graph-1].
complaints of throat pain, dysphagia, odynophagia,
fever, neck swelling, trismus, halitosis, and change in
voice. A total of 50 patients with deep neck space
infections were chosen for the study. A detailed physical
examination was carried out to determine the extent
and cause of the deep neck space infections. In cases
where clinical diagnosis was uncertain, radiological
investigations were done to confirm the diagnosis.
Only clinically or radiologically confirmed cases
of deep neck space infections of all age groups and both
sexes were included in the study. Needle aspiration or
incision and drainage were done at the earliest stage in Graph- 1: Showing the etiology of dental space
majority of the patients. Pus was sent for culture and infection.
sensitivity analysis. All patients were initially started
on a combination of third generation cephalosporin The most common infection was Ludwigs angina
and metronidazole. The antibiotics were modified on seen in 32 patients (64%), followed by peritonsillar
culture sensitivity reports or on clinical responses. abscess (12 patients, 24%), parapharyngeal abscess (3
Supportive therapy, in the form of intravenous fluid, patients, 6%), sub mental abscess (1 patient, 2%),
analgesics, antipyretics, mouth washes was given. Retropharyngeal Abscess (3 patients, 6%), Parotid
RESULTS: Abscess (2 patients, 4%). In 47 patients (94%) single
space was involved. In 3 patients, more than one space
This study consists of 50 cases of deep neck space
was involved. All three patients had co-existing
infections seen over a period of 3years. Youngest
Ludwigs angina (fig 1) and parapharyngeal abscess.
patient seen was 6yrs old and the oldest patient was 76
Clinical diagnosis was certain in 20 cases (40%) and
years old. It was observed that, the maximum numbers
of cases were seen in the age group of 31-40. Of 50
patients studied, 34 were male and 16 were female. The
male/female ratio is 1:0.47 with a slight male
preponderance. The most common symptoms with
which the patient presented were odynophagia
(45patients-90%), restricted mouth opening or trismus
(40 patients 80%) , pain in the throat (34patients 68%),
Neck Swelling (39 patients 78%), Neck pain (31patients,
62%), difficulty in breathing (11patients, 22%). 18
patients (36%) had associated systemic disease. 9 patients
(18%) had history of diabetes mellitus and were on
irregular treatment, 1patient (2%)was on treatment for
hypertension, 6 patients (12%) had coexisting diabetes
mellitus and hypertension. 1patient (3.3%) had
Retroviral infection and 1 patient had tubercular
infection. The most common clinical finding was Fig. 1: Photograph showing Ludwigs angina.
2 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
patients improved symptomatically. In the remaining complications [Table-1]. Two patients had necrotizing
cases, diagnosis was made radiologically (fig. 2). fasciitis requiring repeated dressing and skin grafting.
Ultrasound was used in 2 cases (35.71%) of parotid Five patients with Ludwigs angina developed airway
abscess, 5 cases (10%) of Ludwigs angina. In 40 cases
obstruction and expired. One patient with HIV positive
(80%) X-rays neck, antero-posterior and lateral views
status developed multi-organ failure and expired. The
were taken to assess the airway.
complications were seen in patients with
immunocompromised status Of the 8patients, 2
patients had coexisting DM+HTN (4%), 3 patients had
DM(2%), 1 patient had HIV(2%), one patient had
HTN(2%).
All patients were under antibiotic coverage. Pus
was sent for culture and sensitivity in 46 patients.
It was sterile in 16 samples (32%). Organisms were
isolated in 34 samples (68%).Culture yielded growth
of polymicrobial organisms in 2 samples (4%)
[Table-2].
Fig.-2: Photograph showing submandibular And DISCUSSION:
parapharyngeal abscess. The cervical fascia represents the condensation of
connective tissue lying between adjacent anatomic
Table-1: Showing the percentage of different structures and are generally described as being composed
complications. of a superficial layer and a deep layer.4 The greatest
clinical importance of the cervical fascia is that it divides
the neck into potential spaces that function as a unit
but are anatomically separated.
For those infections involving the neck, the hyoid
bone is considered the most important structure
limiting the spread of infection. For this reason,
infections of the neck are classified by dividing the
potential spaces into three general divisions. Spaces
involving entire length of the neck, Suprahyoid spaces,
Infrahyoid spaces.4,5,6,7
Spaces of head and neck:
In 9 (18%) patients of Ludwigs angina Spaces of the face:
Computerized Tomogram (CT) was used to diagnose
Maxillary spaces, Buccal space, Canine space,
and in three cases contrast was used. Of the 50 patients,
36(72%) cases were treated successfully by incision and Mental space.
drainage (fig 3). Out of them 27 cases were Ludwigs Spaces of the neck:
angina, 6 cases of peritonsillar abscess and one case of
1. Spaces involving the entire length of the neck.
parotid abscess. 10(20%) patients were treated with
needle aspiration. 4(8%)patients with minimal abscess Superficial space (space 1), Deep neck spaces (all
were treated conservatively. Nine patients developed involve only posterior side of neck), Retropharyngeal
Vol.-11, Issue-I, January-June - 2017 3
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
space (space 3, posterior visceral space, Danger space severe respiratory embarrassment and dysphagia. Hence
(space 4) Prevertebral space (space 5), Visceral vascular the treating surgeon should have a high index of
space (within carotid sheath). suspicion in making the diagnosis of deep neck space
2. Suprahyoid spaces infections. Clinical examination alone seems to
underestimate the extent of disease in 70% of cases,
Masticator space, Superficial temporal space, Deep
hence appropriate radiologic imaging can reveal
temporal space, Masseteric space, Pterygomandibular
infection spreading between spaces.3
space , Mandibular spaces, Submandibular space,
Submental space, Sublingual space, Space of the body In this study, out of fifty patients, the maximum
of the mandible, Lateral pharyngeal space numbers of patients were seen in their third to fourth
(pharyngomaxillary, peripharyngeal or decade of life. About 64% of patients were in the age
parapharyngeal), Peritonsillar space, Parotid space. group of 21-50, which correlates with the study
conducted by Parhiscar8 in which almost 50% of their
3. Infrahyoid spaces (involves anterior aspect of
patients were in their third or fourth decade of life6.The
the neck only)
most common presenting complaints in our series was
Pretracheal space, Suprasternal space of Burn, odynophagia (90%).This was followed by pain in throat
Supraclavicular space. (68%), difficulty in opening mouth and neck swelling.
The etiology of deep neck infections varies Earlier studies have also shown neck pain, odynophagia
depending on the space involved such as Dental and fever to be the commonest presenting complaints.3,
8,9,10
infections, Oropharyngeal infections, Upper aero
digestive tract trauma, Retropharyngeal lymphadenitis, In more than 50% of cases etiology was found to
Potts disease, Sialadenitis, Bezolds abscess, Infections be of dental etiology as the cause for deep neck infections
of congenital cysts and fistula, Injection of illicit drugs, in our study. Parhiscar8, DS Sethi3 and Kamath10 have
Malignancies. found dental infections as the commonest etiology in
Pain and swelling of upper neck are the commonest their studies.
symptoms present in all patients. Other symptoms were Ludwigs Angina was the commonest deep neck
fever, odynophagia, respiratory distress. Trismus is space infection in our series, followed by peritonsillar
present when the anterior (prestyloid) compartment is abscess. 3 patients had co-existing Ludwigs angina and
involved ,because of inflammation of the pterygoid para parapharyngeal abscess. In our study culture was
muscles but trismus may be absent when only the negative in 16 cases (32%), which might be attributed
posterior (post-styloid), compartment is involved.5,6 to improper or inadequate use of antibiotics prior to
These infections are frequently accompanied with presenting to our Centre. Pseudomonas aeruginosa was
systemic toxicity and localized aero-digestive tract the commonest organism isolated, followed by
compromise, and sometimes by life-threatening sequelae Staphylococcus and Beta hemolytic streptococcus.
like severe airway obstruction, mediastinitis, Polymicrobial infections were diagnosed in 2cases. Most
pericarditis, internal jugular vein thrombosis, epidural of the organisms isolated in our study showed good
abscess and carotid artery erosion. These are attributable susceptibility to Cephalosporins, Gentamycin and
to the delayed presentation of the patient to a tertiary Amoxycillin+clavalunate potassium.
care center and diagnostic dilemma posed in certain Out of the 50 cases, 36(72%) cases were treated
cases.4 with Incision & Drainage, 10 cases were treated with
They present with a wide variety of needle aspiration, and 4 cases were treated
symptomatology ranging from vague throat pain to conservatively. All cases received antibiotic treatment
4 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
empirically with third generation Cephalosporins, aspiration or conservatively. The complications of deep
gentamycin and metronidazole later modified according neck infection although less common now are still
to sensitivity report. present and are higher in immunocompromised patients
In study by D. S. Sethi 3 , 19% of patients requiring aggressive management.
developed complications, 6 developed necrotizing
cervical fasciitis. One had aspiration pneumonia, two Table 2: Showing Organisms isolated.
developed acute myocardial infarctions, and four
patients developed septicemia and multi organ failure.
Mortality rate was 8%.
In our study, we encountered two cases of
necrotizing fasciitis, five cases of airway obstruction,
one case of multi organ failure.
In our study six patients (12%) expired, amongst
whom five patients expired due to cardio respiratory
arrest & one patient due to multi organ failure.
Mortality rate was 12%.
CONCLUSION:
Deep neck space infections continue to occur
despite the wide spread use of antibiotics. In our study, DISCLOSURES
Deep neck space infections have a male preponderance
(a) Competing interests/Interests of Conflict- None
and are more common in third and fourth decade of
life. Ludwigs angina is the commonest deep neck (b) Sponsorships None
infection. Patients with coexisting immunocom- (c) Funding - None
promised states such as Diabetes Mellitus and HIV tend (d) Written consent of patient- taken
to have severe presentation, prolonged course and (e) Animal rights- Not applicable
higher complication rate.
ABBREVIATIONS:-
Contrast enhanced computed tomography
DM-diabetes melitus
(CECT) is essential in the appropriate management of
deep neck infections especially in those involving HTN-hypertension
Parapharayngeal and Retropharyngeal spaces. Early HIV-human immune deficiency virus
presentation of the patients to the hospital, has led to a
REFERENCES:
decrease in the morbidity and mortality.
1. Clarke P.Benign neck disease: Infections and
Antibiotic coverage should include Gram positive,
Swellings, Clarke M, Browning CG, Burtan MJ,
Gram negative and anaerobic microorganisms. A
Clarke R, Hibbert J, Jones NS et al .Eds., in Scot-
combination of third generation Cephalosporins,
Browns Otorhinolaryngology & Head and Neck
Aminoglycosides and Metronidazole are effective in the
surgery, 7 th edition, Volume 3, (Great Britain,
treatment of deep neck space infections. Incision and
Hodder Arnold, (2008) 1785
drainage as a treatment for deep neck space infections
is successful and cost effective in most of the cases. 2. Eric R. Oliver, M. Boyd Gillespie. Chapter 14,
Smaller abscesses can be managed either by needle Charles W. Cumming, Paul W. Flint, Lee A.
Vol.-11, Issue-I, January-June - 2017 5
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Harker, Bruce H. Haughey, Mark A. Richardson,
K. Thomas Robbins, Cummings
Otorhinolaryngology & Head and neck surgery, 5th
edition, volume 1, part 2 (Elsevier Mosby, 2010)
201.
3. Sethi DS, Stanley RE, Deep neck abscesses-changing
trends. J Laryngol Otol, J Laryngol Otol. 1994
Feb;108(2):138-43
4. Neil W. Ancient History, Chapter 2,
Otolaryngology, An Illustrated History
Neil. Weir, London,Butterworths, 1990;10-23.
5. Sethi DS, Stanley RE, Parapharyngeal abscess. J
Laryngol Otol . 1991 Dec;105(12):1025-
1030.DOI: https://doi.org/10.1017/
S0022215100118122
6. Yellon R.F. Head and Neck Space Infections, in
Paediatric Otolaryngology, IV Edition,C D
Bluestone et al.Eds.,Vol.2,pp. 1681-
1701.Saunders, Philadelphia,USA. 2003
7. Gerd Jrgen Ridder et.al. Spectrum and
Management of Deep Neck Space Infections: An 8-
Year Experience of 234 Cases. Otolaryngol Head
Neck Surg .11 2005;133 (5): 709-714.
8. Parhiscar A, Har-El G, Deep neck abscess: A
retrospective review of 210 cases.Ann Otol Rhinol
Laryngol. 2001 Nov;110(11):1051-4
9. Neil W, The middle ages and Renaissance, Chapter
3, Otolaryngology : An Illustrated History, Neil
Weir (London, Butterworths,1990:24-38.
10. Kamath P, Shetty AB, Hegde MC, Sreedharan S,
Bhojwani K, Padmanabhan K et al. Presentation
and management of deep neck space abscess, Indian
J Otolaryngol Head and Neck Surg (Oct-Dec, 2003)
55:270-274.
6 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
PREVALENCE AND FACTORS RELATED TO HEARING
IMPAIRMENT AMONG MAINSTREAM PRIMARY SCHOOL
CHILDREN IN RURAL SOUTHERN INDIA
*
Jeeva Thankom Philip, **Rejee Ebenezer Renjit
HOW TO CITE THIS ARTICLE Date of receipt of article -24-11-2016
Philip J T, Rejee E R . Prevalence and factors related to hearing Date of acceptance 09-01-2017
impairment among mainstream primary school children in Rural
Southern India. Orissa J Otolaryngology Head Neck Surgery DOI- 10.21176/ojolhns.2017.11.1.2
2017 June; 11(1): 7-15. DOI : 10.21176/ojolhns.2017.11.1.2 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.2
ABSTRACT:
Background and objective: Hearing impairment among children is a momentous health problem which has
adverse consequences on their functional development and academic performance. In this context the present
study was conducted to determine the prevalence and factors related to hearing impairment among primary
school children in rural Kerala, India.
Materials and methods: 1160 children between 5-10 years were subjected to otoscopy and tuning fork testing.
Children with abnormal tuning fork test results were further evaluated by pure tone audiometry and
tympanometry.
Results: The prevalence of hearing impairment was 8.10%. The mean value of hearing loss was 32.36dB with a
standard deviation of 8.95dB. Permanent and possibly progressive sensorineural type of hearing loss was detected
in 4.3% of cases, whereas treatable conductive type hearing loss was in 95.7% of cases.
Conclusions: Majority of the aetiological factors of hearing impairment identified were preventable or treatable.
This highlights the relevance and requirement of effective school screening programmes for eliminating these
preventable cases of deafness from our community, as there is no such well-established programme in the country.
Keywords: cerumen, child health, hearing loss, otitis media with effusion, prevalence, suppurative otitis media.
INTRODUCTION: avoidable. Hence early identification of risk factors of
The sense of hearing enriches our lives and enables deafness and timely intervention in the childhood itself
us to participate in social life. It plays a critical role in is of high significance in eliminating the preventable
the development of speech and language in children.
Nevertheless hearing impairment among school-going
Affiliations:
children is still a momentous health problem in the *Department of ENT, Dr. S.M.C.S.I. Medical College & Hospital,
developing world. Karakonam, Trivandrum, Kerala.
** Professor and Head of the Department of ENT, Dr. S.M.C.S.I. Medical
Prevalence of hearing impairment among rural College & Hospital, Karakonam, Trivandrum, Kerala.
school children reported by various Indian studies is Address of Correspondence:
about 9.311.9%1, 2, 3. WHO has estimated that about Dr. Rejee Ebenezer Renjit, MBBS, DLO, MS,
50% of causes of hearing impairment are preventable Professor and HOD of ENT,
Dr. SMCSI Medical College & Hospital, Karakonam,
and 30% are treatable, though not preventable 4. Trivandrum, Kerala State, India - 695504.
Therefore overall 80% of all cases of deafness are E-mail: rejee72@gmail.com, Tel: +91 9447700355
Vol.-11, Issue-I, January-June - 2017 7
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
cases of deafness from our community. It is a well- Inclusion criteria
established fact that moderately severe to profound Children of the mainstream schools in the age
hearing impairment in children has a detrimental and group of 5-10 years, who attend the school on the day
devastating effect on their linguistic, social, scholastic of the screening programme.
and emotional development. Such major degrees of
Exclusion criteria
hearing impairment are easily identified by parents or
teachers in early age itself and are dealt with. Children in special schools
Meanwhile, even mild degrees of hearing loss is Sampling technique
also proven to have adverse effects on the functional Random sampling technique.
development and scholastic performance of Sample size
children5,6,7.Nevertheless, children with this type of
It is calculated by the formula 4pq/d2, where p =
hearing impairment are not readily identified and are
Available local prevalence rate in the target population
often mistaken for having attention deficit disorder,
learning disabilities or cognitive disorders8. Therefore (from comparable studies1,2 ), i.e. 11.9.
an effective school hearing screening programme is q = 100-p
essential for the detection of such children, thereby d = Relative precision (20% of previous
ensuring early intervention and prevention of prevalence)
complications. Hence required sample size = 741
Relevance of a school hearing screening
Tools/instruments
programme in addition to new born screening is further
highlighted by the fact that for every 10 children with 1 . The questionnaire
permanent bilateral hearing impairment detected by Personal details - name, age, sex
universal newborn screening, there are other 5 to 9 Antenatal history- gestational diabetes,
children with late onset hearing impairment9. About hypertension, hypothyroidsm, exanthematous
10-20% cases of permanent childhood hearing loss are fever, typhoid
late in onset and are unlikely to be detected by neonatal
Perinatal history - prematurity, low birth weight,
hearing screening programmes10. Furthermore, the
neonatal respiratory distress or ventilator
prevalence of permanent hearing loss is estimated to
dependence, neonatal jaundice, neonatal sepsis
increase from 3/1000 in infants to 9-10/1000 in the
school age population11. Therefore, even after successful Past medical history - meningitis, mumps, measles,
implementation of neonatal hearing screening head trauma, ototoxic drug intake, significant
programmes, many school children are likely to have noise exposure
undetected hearing impairment, which can be detected Past or present otological history - ear pain, ear
by effective school hearing screening programmes. discharge, hearing impairment, tinnitus, blocked
Efforts put forth to bring the children with sensation in ear.
hearing impairment to manstream by providing 2. Otoscopy
effective therapeutic as well as rehabilitative services will
All the lower primary school children in the study
create a rights-based and barrier-free society for these
sample were subjected to otoscopic examination by
differently able persons. In this context a study was
residents pursuing Masters in Otorhinolaryngology and
conducted to determine the prevalence and factors
positive findings were noted down.
related to hearing impairment and the pattern of ear
disease among primary school children. 3. Tuning fork testing
MATERIALS AND METHODS: Rinne, Weber and absolute bone conduction tests
This is a prospective cross-sectional study were performed in all children, using 512 Hz tuning
conducted in rural Trivandrum district, Kerala state, fork. Those children with abnormal or equivocal test
India from December 2012 to September 2014. results were subjected to audiometric assessment.
8 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
4. Pure tone audiometry membrane or middle ear pathologies co-existing with
Audiometric assessment was conducted by a wax was ruled out.
qualified audiologist in the quietest room in each school, Acute and chronic otitis media were diagnosed
using a calibrated Classic I portable audiometer. Those based on tympanic membrane findings. Otitis media
children having air conduction threshold levels more with effusion was diagnosed on the basis of tympanic
than 20dB at any of 0.5K, 1K, 2K or 4K frequencies membrane findings and type B tympanogram. Cases
were considered to have possible hearing loss. Such having tympanic membrane retraction and type C
children were referred to the ENT department in our tympanogram were diagnosed to have Eustachian tube
tertiary care centre for further detailed evaluation of dysfunction (without effusion).
air and bone conduction thresholds in a sound 7. Data analysis
protected environment, on a later date. A pure tone
The data collected was entered in Microsoft Excel
average above 25 dB at 0.5K, 1K, 2K and 4K Hz was
and was analysed using SPSS software. The factors
considered as abnormal. Hearing impairment was
related to hearing impairment which were analysed
grouped to mild (26-40dB HL), moderate (41-55dB
include age, sex, antenatal, perinatal & past medical
HL), moderately severe (56-70dB HL), severe (71-90dB
history and various ear examination findings. Bi-
HL) or profound (>90dB HL), according to WHO
variable analysis using Chi square test and Odds ratio
classification.
with 95% confidence interval was used to find out the
5. Tympanometry association between hearing impairment and various
Tympanometric assessment was done using a factors related to it. P value less than 0.05 was considered
portable GSI Autotymp Tympanometer in children to be statistically significant. Binary logistic regression
having any abnormal otoscopic or tuning fork test was used for finding out the independent predictors of
findings. hearing impairment.
6. Data collection process RESULTS:
At first, all primary schools in the specified area A total of 1160 school children were included in
were enumerated. From this, 12 schools were selected the study. The age-gender distribution of the study
by random sampling technique. The study details were subjects is shown in Table I. The mean age was 7.68.
explained to the school management and consent was Out of the 1160 children, 578 (49.8%) were boys and
obtained. A detailed questionnaire was issued before 582 (50.2%) were girls.
the date of screening to be filled in by the parents, which 1. Hearing impairment prevalence, characteristics
contains details pertaining to the antenatal, perinatal and aetiological factors
and childhood medical history as well as informed
The prevalence of hearing impairment in the
consent, so that the children could bring back the
present study was 8.10%, i.e. 94 out of 1160 children
questionnaire on the date of screening.
were detected to have some degree of hearing
A total of 1160 lower primary school children impairment by pure tone audiometry, even though 145
were included in the study. During screening, otoscopic cases were initially evaluated in view of abnormal or
examination and tuning fork testing were done in all equivocal tuning fork test results.
children. Pure tone audiometry and tympanometry
Of these 94 cases, 90 (95.7%) had conductive and
were performed by quailified audiologists, in children
4 (4.3%) had sensorineural type of hearing loss.
with abnormal initial findings.
Moreover, out of the 94 cases with hearing impairment,
After confirming hearing loss by pure tone 24 cases (25.53%) had right sided, 33 cases (35.11%) had
audiometry, appropriate therapeutic interventions were left sided and 37cases (39.36%) had bilateral
initiated. Children with impacted wax were prescribed involvement.
wax solvents and directed for further follow up in our
The mean value of hearing loss was 32.36dB with
hospital, during which wax removal and otoscopic
a standard deviation of 8.95dB. Out of the 94 cases
examination was done and the incidence of any tympanic
with hearing impairment, the majority (87 cases i.e.,
Vol.-11, Issue-I, January-June - 2017 9
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
92.6%) had mild degree of hearing loss (26-40dB HL). dysfunction without middle ear effusion (4 out of 121
Moderate (41-55dB HL), moderately severe (56-70dB ears). On performing bi-variable analysis, significant
HL), severe (71-90dB HL) and profound (>90dB HL) association was detected between hearing impairment
degrees of hearing loss was detected in 5(5.3%), 0(0.0%), and impacted wax [Odds ratio (95% CI) - 2.017 (1.238 -
1(1.1%), 1(1.1%) cases respectively. 3.286); p value- 0.004], otitis media with effusion [Odds
Considering the aetiology of hearing impairment, ratio (95% CI) - 214.106 (62.425 - 734.345); p value- 0.001]
the major proportion (42.6% in the right side and 45.7% and chronic otitis media tubotympanic type [Odds ratio
in the left side) was contributed by impacted wax. The (95% CI) - 48.761 (5.005 - 475.094); p value- 0.001].
distribution of various aetiological factors is shown in DISCUSSION:
Figure I and II. 1. Study tools
2. Factors associated with hearing impairment Tuning fork tests, pure tone audiometry and
Bi-variable analysis using chi-square test was done tympanometry were included as our study tools, in
to find out the association between hearing impairment addition to the detailed questionnaire collected from
and various socio-demographic factors. Prevalence of the parents of the study subjects and otoscopic
hearing impairment was more in 5-7 yrs age group examination findings. It has been established that for a
(8.5%) compared to 8-10 yrs age group (7.7%); more hearing screening protocol to be acceptable, the
among boys (8.8%) than girls (7.4%); more among sensitivity and specificity of the tool must be at least 90
children studying in government schools (9.6%) 95%12. In other words it should accurately detect at
compared to children in private schools (7.3%). least 90 95% of persons having hearing loss and it
However these differences were found to be statistically shouldnt fail more than 5 10% of persons having
insignificant [Table II]. normal hearing12.
3. Role of antenatal, perinatal and childhood Burkey et al.13 established the sensitivity of Rinne
factors in the incidence of sensorineural hearing test using 512 Hz tuning fork in detecting conductive
loss. hearing loss more than 10,20, 30 dB by experienced
Out of the 4 cases with sensorineural hearing loss, otologists using masking were 89.1, 100 and 100
3 had bilateral mild degree of hearing loss and the other respectively, when equivocal results are included. In
child had moderately severe loss in one ear and unmasked situations, the sensitivity was 72.5, 92.3 and
profound loss in the other ear. Two of the cases with 100 respectively. Browning et al.14 found the specificity
mild loss had maternal history of gestational of Rinne test using 512 Hz tuning fork to be more
hypertension as well as perinatal history of prematurity than 90%. Hence the acceptance of tuning fork tests as
and low birth weight. One of them had childhood the primary screening tool in our study is justifiable.
history of mumps and measles also. However, it was In this study, all children with abnormal or
not possible to make any statistical analyses on the role equivocal tuning fork test results were subjected to
of these factors in the incidence of sensorineural hearing audiometric assessment. Children with air conduction
loss, due to the limited number of cases. threshold levels more than 20dB at any of 0.5K, 1K,
4. Pattern of ear diseases 2K or 4K Hz frequencies were considered to have
possible hearing loss and were referred to the ENT
The pattern of ear diseases is tabulated in Table
department, for further detailed evaluations. According
III. The prevalence of hearing impairment among
to American National Standards Institute, the cut off
various ear diseases was analysed and found to be 8.22%
intensity levels for identifying hearing impairment
in impacted cerumen (58 out of 706 ears), 18.18% in
varies between 20 to 30dB12. In literature, there is
acute otitis media (2 out of 11 ears), 80.00% in otitis
evidence for greater sensitivity of screening level at 20dB
media with effusion (48 out of 60 ears), 88.89% in
HL than 25dB HL in identifying minimal hearing loss
tubotympanic type of chronic otitis media (8 out of 9
and educationally significant hearing loss 15. The
ears), 100.00% in atticoantral type of chronic otitis
sensitivity/specificity rates for identifying minimal
media (1 out of 1 ear) and 3.31% in eustachian tube
hearing loss at 20 dB HL screening levels were 100/53
10 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
respectively. For detecting educationally significant higher than that of males is Kerala (1084 females per
hearing loss, these rates were 100/92.2 respectively16. 1000 males)19. This pattern of sex ratio is reflected in
Hence we used 20dB HL as the cut off screening level present study also (1007 females per 1000 males).
for referring the children after the preliminary 3. Prevalence and characteristics of hearing
audiometric assessment. impairment.
Various studies have shown that for identifying The prevalence of hearing impairment among rural
the maximum number of cases of newly detected hearing children in the present study (8.10%) is considerably
loss, a single failure in any of the frequencies must be higher than that among urban children in the same state
considered as a failure12. The American Speech Language (2.2%) as observed in a study by Ebenezer et al.19.
Hearing Association (ASHA-1990) screening guidelines However this is lower than the prevalence among rural
recommended screening at 500, 1000, 2000 and 4000 children in neighbouring states like Karnataka and
Hz frequencies12. FitzZaland et al17 while evaluating the Tamilnadu (11.9%)1,2 and also the urban areas of a
screening ability of 20 dB HL at 1000 & 2000 Hz and Northern state (9.3%) 3 . Reports regarding the
25 dB HL at 500 & 4000 Hz have found out that 15% prevalence of hearing impairment from neighbouring
of children with confirmed conductive hearing loss had countries including Nepal, Myanmar etc. vary between
failed only at 500 Hz level. Therefore in our study, 5.5% and 21.63%20,21.
children with air conduction threshold levels more than As this was primarily a hearing screening study,
20dB at any of 0.5K, 1K, 2K or 4K Hz were considered children having normal hearing in spite of ear wax were
to have possible hearing loss and were evaluated not followed up further. Tympanic membranes of such
further. After detailed evaluation, the hearing children were not visualized. Hence a proportion of
impairment was classified to mild (26-40dB HL), cases having tympanic membrane or middle ear
moderate (41-55dB HL), moderately severe (56-70dB pathologies but with normal hearing, might have been
HL), severe (71-90dB HL) and profound (>90dB HL) missed while estimating the prevalence of ear diseases
as per the WHO guidelines18. In present study, 95.7% of hearing loss was of
2. Socio demographic factors conductive type. Similar studies in India also showed
In this cross sectional study conducted among 87.1% to 91.2% of conductive hearing loss among the
school children in rural Kerala, out of the 1160 children total hearing loss cases2,3. The overall prevalence of
in the age group of 5-10 years, 49.8% were boys and sensorineural hearing loss in the present study was
50.2% were girls. As per Indian population census 2011, 0.34%, which also accounted for 4.3% of cases of
hearing impairment, similar to a comparable study in
the only Indian state where the number of females is
Kerala19.
Table-I: Age - gender distribution (n=1160) 4. Aetiology of hearing impairment
The major proportion (42.6% in the right side and
45.7% in the left side) of hearing impairment in our
study was contributed by impacted wax. In other Indian
studies also, the most important aetiological factor was
detected to be impacted wax, contributing to 41.9 -
86.3% of cases with hearing impairment1,3,19.
The proportion of hearing impairment
contributed by otitis media with effusion was
disproportionately high in the present study (36.1-
37.1%) compared with some Indian studies3,19 (3.5-
6.5%), but this is in accordance with another study by
Jacob et al.2 in rural south India (41.9%) and various
studies in Egypt22 (30.7%) and Saudi Arabia23 (34.9%).
Chronic otitis media contributed to 4.3-9.8% of hearing
Vol.-11, Issue-I, January-June - 2017 11
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Table - II: Hearing impairment versus demographic
factors.
Fig-1: Aetiology of right sided hearing impairment (n=61).
loss cases in our study, which is significantly lower than
that in other Indian3 as well as foreign studies22 (13.2-
23.3%). This lower incidence could be due to better
health awareness and utilization of health care facilities
in Kerala.
5. Pattern of ear diseases
In present study, the most prevalent ear disease
was found to be impacted wax (37.41%). Various south
Indian studies also have revealed a prevalence of wax
Fig-2: Aetiology of left sided hearing impairment (n=70).
impaction between 29.8-63.0%, which was the most
Table - III: Pattern of ear diseases (n=1160). common ear disease1,2,19. A prevalence of 60.6-62.0% was
reported in other countries in Indian subcontinent24,25.
In the present study, 8.25% of ears with wax
impaction had associated hearing impairment. A similar
study conducted among the urban children of the same
district had revealed lower prevalence (3.91%) of hearing
impairment among the children with wax impaction19.
Other external ear diseases like foreign body and otitis
externa were found in only 0.09% and 0.26% of
children in our study which was comparable with the
prevalence detected by another study in a nearby urban
area (0.08% and 0.04% respectively)19. Among the
middle ear pathologies, Eustachian tube dysfunction
without middle ear effusion was detected to be the most
common disease with a prevalence of 5.86%, higher than
the prevalence in a comparable study (2.8%) in urban
Kerala19.
12 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
The prevalence of otitis media with effusion Advantages of early identification and treatment
(3.10%) in our study was comparable with other studies of cases
in other parts of India and neighbouring countries (3.3- When to suspect hearing impairment in class
4.7%), but significantly higher than the prevalence rooms and the methods of identification of
detected in urban areas of the same state19,24,25,26. In our probable cases
study, 80.0% of ears having otitis media with effusion
Availability of treatment and rehabilitative options
had associated hearing impairment. Similar studies in
south India also have revealed 50.0-100.0% prevalence CONCLUSION:
of hearing impairment among the cases with middle This study has revealed the magnitude of hearing
ear effusion1,19. However, it is known that 50-75% of impairment and other otological morbidities prevailing
the OME will resolve during 3-6 months without in our rural community. We would like to give special
leaving permanent sequelae. Hence these cases are reference to the preventable or treatable cases of hearing
unlikely to cause any permanent hearing impairment loss identified in our study, which constitute the major
and associated developmental or educational deficits. proportion (95.7%). Children with mild degree of
The prevalence of chronic otitis media was hearing impairment are not readily identified and are
significantly lower in the present study (0.69%) often mistaken for having attention deficit disorder,
compared to various other studies in India and learning disabilities or cognitive disorders. Meanwhile,
neighbouring countries (5.2-7.8%)2,24-26. The significantly such degrees of hearing loss is proven to have adverse
lower prevalence of chronic middle ear disease in our effects on the functional development and scholastic
study could be secondary to the better socioeconomic performance of children, even though the effects are
environment, improved health education and effective not so detrimental and devastating as in moderately
utilization of health facilities prevailing in Kerala, the severe to profound hearing impairment. In this context,
most literate state of India 19. The further lower we would like to highlight the magnitude of the
prevalence of chronic ear disease in a comparable study preventable or treatable deafness in our school children
among the urban children of the same state also and to emphasis on the relevance and requirement of
indicates the role of favourable socioeconomic factors effective school screening programmes for eliminating
in urban area compared to rural areas. The inverse these types of deafness from our community, as there
relationship between prevalence of chronic middle ear is no such well-established programme in the country.
diseases and better socioeconomic background has been
LEGENDS:
established in literature also21,27,28
AOM - Acute otitis media
5. Strategy adopted to tackle the problem in our
area. OME - Otitis media with effusion
The individual cases having hearing loss identified CSOM TTD - Chronic otitis media tubotympanic type
by the school screening programme were referred to CSOM AAD - Chronic otitis media atticoantral type
the ENT department in the tertiary care centre for ETD - Eustachian tube dysfunction
further detailed evaluations, necessary interventions and
SNHL - Sensorineural hearing loss
rehabilitation, after informing the parents with the help
of class teachers. Un Ex HL - Unexplained hearing loss.
In order to tackle the problem on community DISCLOSURES:
basis, we have addressed the following aspects in a (a) Competing interests/Interests of Conflict- None
Teachers awareness programme conducted by our (b) Sponsorships - None
institution: (c) Funding - None
Adverse developmental and scholastic effects of (d) No financial disclosures
even mild degrees of hearing loss (e) Animal rights-Not applicable
Vol.-11, Issue-I, January-June - 2017 13
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
REFERENCES: 9. Fortnum HM, Davis A, Summerfield AQ,
1. Rao RP, Subramanyam MA, Nair NS, Marshall DH, Davis AC, Bamford JM, Yoshinaga-
Rajashekhar B. Hearing impairment and ear Itano C, Hind S. Prevalence of permanent
diseases among children of school entry age in rural childhood hearing impairment in the United
South India. Int J Pediatr Otorhinolaryngol. 2002 Kingdom and implications for universal neonatal
Jun 17;64(2):105-10.PMID:12049823 hearing screening: questionnaire based
ascertainment study Commentary: Universal
2. Jacob A, Rupa V, Job A, Joseph A. Hearing
newborn hearing screening: implications for
impairment and otitis media in a rural primary
coordinating and developing services for deaf and
school in South India. Int J Pediatr
hearing impaired children. Bmj. 2001;323
Otorhinolaryngol. 1997 Mar 6;39 (2):133-8.
(7312):536.
PMID:9104621
10. Grote JJ. Neonatal screening for hearing
3. Saud LC, Sajad H, Lateef I, Mohd LC, Asef W. A
impairment.Lancet.2000;355(9203):513-4.
prospective study of hearing impairment in school
11. White K. Twenty years of early hearing detection
going children of Ghaziabad city attending a
and intervention (EHDI): where weve been and
tertiary care hospital. Online Journal of
what weve learned. In ASHA Audiology Virtual
Otolaryngology. 2014;4(4):28-41. www.
Conference 2010.
scopemed.org / ? mno=172027
12. K. Bright, J. Eichwald, G. Tanner.American
4. World Health Organization. State of hearing and
Academy of Audiology Childhood Hearing
ear care in the South East Asia Region. WHO
Screening Guidelines. (2011). Available at<http:/
Regional Office for South East Asia. WHO-
/iranaudiology.ir/fa/images/stories/ Guidelines/
SEARO.SEA/Deaf/9. Available at <http://
guideline% 20aaa% 20% 20childhood%
www.searo.who.int/LinkFiles/
20hearing% 20screening%202011.pdf>[Last
Publications_HEARING_&_EAR_CARE.pdf accessed on 2015 Nov 22].
>[Last accessed on 2013 Jul 9].
13. Burkey JM, Lippy WH, Schuring AG, Rizer FM.
5. Blumsack JT, Anderson KL. Back to school! 13 Clinical utility of the 512-Hz Rinne tuning fork
facts revisited. Hearing Review. 2004; 11(10) :62- test. Am J Otol. 1998 Jan;19(1):59-62.
63.
14. Browning GG, Swan IR. Sensitivity and specificity
6. Johnson DeConde C, Seaton J. Educational of Rinne tuning fork test. Bmj.
audiology handbook. 2 nd edition; New 1988;297(6660):1381-2.
York,USA. Delmar Cengage Learning; 2012.
15. Dodd-Murphy J, Murphy W. School hearing
7. American speech language hearing association, screening referral and DPOAEs. In Scottsdale,
Audiology information series-Effect of hearing loss AZ.: presented at the annual meeting of the
on development. Available at< http:// American Auditory Society 2006.
www.asha.org/uploadedFiles/AIS-Hearing-Loss- 16. Dodd-Murphy J, Murphy W, Bess FH. Accuracy
Development-Effects.pdf>[Last accessed on 2015 of school screenings in the identification of
Nov 22]. minimal sensorineural hearing loss. American
8. Smaldino J, Flexer C, Madell J, Flexer C. journal of audiology. 2014;23(4):365-73.
Classroom acoustics: Personal and sound field FM 17. FitzZaland RE, Zink GD. A comparative study
and IR systems. Pediatric audiology diagnosis, of hearing screening procedures. Ear and Hearing.
technology, and management. 2008:192-202. 1984;5(4):205-10. Gell FM, White EM, Newell K,
14 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
Mackenzie I, Smith A, Thompson S, Hatcher J. 25. A.K. Agarwal, S.K. Chadha, V. Malhotra, School
Practical screening priorities for hearing screening pilot-School screening camps: New
impairment among children in developing Delhi, India. Available at <http://
countries. Bull World Health Organ. 1992; www.soundhearing2030.org/school
70(5):645-55 screening.php> [Last accessed on 2015 Nov 22].
18. Renjit RE, Manonmony S, Philip JT, Jose DJ. 26. Chadha SK, Agarwal AK, Gulati A, Garg A. A
Spectrum of ENT diseases among urban school comparative evaluation of ear diseases in children
children in South Kerala, India. International of higher versus lower socioeconomic status. J.
Journal of Biomedical Research. 2014;5(5):355-8. Laryngol. Otol. 2006;120:1619.
19. Maharjan M, Bhandari S, Singh I, Mishra SC. 27. Dutton DB. Socioeconomic status and childrens
Prevalence of otitis media in school going children health. Medical Care. 1985 Feb;23(2):142-156.
in Eastern Nepal. Kathmandu University medical
journal (KUMJ). 2005;4(4):479-82.
20. Shaheen MM, Raquib A, Ahmad SM. Prevalence
and associated socio-demographic factors of
chronic suppurative otitis media among rural
primary school children of Bangladesh.Int J
Pediatr Otorhinolaryngol. 2012;76(8):1201-4.
DOI: 10.1016/j.ijporl.2012.05.006. Epub 2012
May 29
21. Abdel-Hamid O, Khatib OM, Aly A, Morad M,
Kamel S. Prevalence and patterns of hearing
impairment in Egypt: a national household
survey. East Mediterr Health J. 2007 Sep-
Oct;13(5):1170-80.
22. Al-Rowaily MA, AlFayez AI, AlJomiey MS,
AlBadr AM, Abolfotouh MA. Hearing
impairments among Saudi preschool children. Int
J Pediatr Otorhinolaryngol 2012; 76:16741677.
23. Adhikari P. Pattern of ear diseases in rural school
children: Experiences of free health camps in
Nepal. Int J of Pediatric Otorhinolaryngology.
2009;73(9):1278-80.
24. Adhikari P, Kharel DB, Ma J, Baral DR, Pandey
T, Rijal R, et al. Pattern of otological diseases in
school going children of Kathmandu valley. Arq
Int Otorrinolaringol 2008;12:502-5.
Vol.-11, Issue-I, January-June - 2017 15
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
ONCOLOGICAL OUTCOME ANALYSIS OF TRANS-NASAL
MINIMALLY INVASIVE ENDOSCOPIC RESECTION OF SINO-
NASAL MALIGNANCY NOT TRANSGRESSING THE DURA:
A SINGLE CENTRE STUDY
*Dipak Ranjan Nayak, **Suraj Nair, **Apoorva N Reddy ,*Balakrishnan Ramaswamy, ***Rohit Singh
HOW TO CITE THIS ARTICLE Date of receipt of article -27-5-2016
Nayak D R, Nair S, Reddy A N, Ramaswamy B, Singh R.Oncological Date of acceptance 30-05-2017
outcome analysis of trans-nasal minimally invasive endoscopic resection
of sino-nasal malignancy not transgressing the dura: a single centre DOI- 10.21176/ojolhns.2017.11.1.3
study.Orissa J Otolaryngology Head Neck Surgery 2017 June; 11(1):
16-24. DOI: 10.21176/ojolhns.2017.11.1.3
DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.3
ABSTRACT:
Objective: To evaluate the oncological results and efficacy of trans-nasal minimally invasive endoscopic resection
of nose and para nasal sinus malignancy.
Methods: A retrospective observational study including 29 cases of nose and paranasal sinus malignancy stage I-
IV of varied histopathological types operated from January 2006 to July 2016. All the patients underwent trans-
nasal laser/microdebrider assisted endoscopic resection of the primary tumor with adequate margins. Neck
dissection was carried out in 8 cases. All stage III/IV cases and 5 cases of stage-II including olfactory neuroblastoma
received post operative radiotherapy/ Chemo-radiotherapy and one case of malignant melanoma referred for
post-operative immunotherapy. Average follow up period was 7 months. Data was analysed using Kaplan Meier
method to estimate the overall and disease specific survival rate along with the median survival time wherever
applicable. Statistical analysis was carried out using STATA 13.
Results: The age range was 39-64 years with a mean of 49.4yrs. 67 % of the patients were males. Overall, there
were 2cases (7.1%) in T1, 8 (28.5%) in T2, 12(42.8%) in T3 and 6 cases (21.4%) in T4 stage. 22 patients (75.8%)
were N0, 5(17.2%) were N1 and 2(6.8%) were N2 to begin with. 24/ 29 patients had no disease on their last
follow up. One case of olfactory neuroblastoma in Kadish stage B had no recurrence on last follow-up after 18
months. 5 cases had local recurrence of which T1 and T2 cases had no contribution. Out of the 2 cases of
recurrence in T3, one at 14 months was managed with endoscopic re-excision and the other at 28 months with
external resection. 3 recurrences in T4were observed and open approach adopted for 2 cases at 16 and 34 months
respectively and one case refused treatment at 19 months. 2 patients had lung metastasis after 3 years. 15 out of
the 18 patients followed up for 2 years were disease free. The study showed an overall survival rate of 82.7%
while the 2 year disease specific survival rate was found to be 83.33%.
Conclusion: Endoscopic resection of paranasal sinus malignancy has provided an efficient tool to the skull base
surgeon for providing good oncological results with favourable cosmesis avoiding the potential morbidities of
open approaches.
Keywords: Endoscopic resection, paranasal sinus malignancy, microdebrider, skull base.
INTRODUCTION: Affiliations:
*Professor, **Resident, ***Associate Professor, Department of ENT-
Sino-nasal malignancies comprise 3-4 % of all head
Head & Neck Surgery, Kasturba Medical College, Manipal University,
and neck oncology workload. They have been Manipal.
traditionally attributed to poor prognosis owing to Address for correspondence:
Prof.Dipak Ranjan Nayak, Department of ENT-HNS,
close anatomical proximity to anterior skull base, orbit, Kasturba Medical College, Manipal University, Manipal-576104
cranial nerves, carotid vessels and morbid surgical Email: drnent@gmail.com
16 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
approaches1. The landmark open craniofacial resection excluded. Cases with tumour transgressing dura
(CFR) by Ketcham in 1963, Moores lateral rhinotomy requiring resection were carried out by craniotomy
and Weber-Fergussons approach with its modifications instead of trans-nasal neurosurgical intervention and
have been the standard options for surgical resection hence excluded from the study. Various
of sinonasal malignancies for a long time1,2. However, histopathological sub-types of sinonasal malignancies
the recent advances in endoscopic surgical in stages I-IV operated from January 2006 to July 2016
instrumentation, intra-operative image guidance were included in the study. The cases had undergone
technology, powered instruments, optical gadgets and purely endoscopic resection of the sinonasal mass with
training programmes in endoscopic sinus surgery have microscopically negative margins. The primary site of
revolutionised the concept of trans-nasal endoscopic origin in all cases was located in maxillo-ethmoidal
resection of sinonasal tumours 3. Benign sinonasal complex with variable local spread. Stringent inclusion
tumours were managed earlier using endoscopic and exclusion criteria were formalised for the selection
approach and the excellent results provided an impetus of patients. All the subjects had undergone routine head
to tackle malignant lesions with oncological results and neck clinical examination followed by nasal
comparable to open approaches. The changing endoscopy and contrast enhanced CT scan for
paradigms in the management of sinonasal malignancies assessment of the lesion. Minimum follow-up period
were based on the results of various studies comparing was 7 months.
the endoscopic and open approaches2,3. Records were evaluated for patient age, sex,
The two major advantages of open approaches are diagnosis, tumour staging, histopathological findings,
an en-bloc resection and easy reconstruction of anterior operative procedure, operative time, estimated blood
skull base defect. Endoscopic resection includes a piece- loss, complications, hospital stay, intensive care unit
meal excision of the lesion due to the complex anatomic (ICU) stay, postoperative course, follow-up, recurrence
location and access4. This piece-meal resection with rates, and metastasis, mortality and survival rates.
microscopically clear margin provides similar Olfactory neuroblastoma was staged according to the
oncological results as an en-bloc resection. The recent Kadish staging system8. Other malignant tumours were
techniques in endoscopic skull base reconstruction staged according to the tumour, node, and metastases
has made it possible to reconstruct defects with (TNM) staging system for nasal cavity and ethmoid
precision4, 5. With the advances in instruments and sinus malignancy of the seventh edition of the American
training workplaces, endoscopic surgeons have Joint Committee on Cancer (AJCC) 9. Staging was based
continued to improve their knowledge of the complex on preoperative examination, computed tomography
paranasal sinus and skull base anatomy. Endoscopic (CT) and magnetic resonance imaging (MRI).
resection provides the major advantage of minimal Management of neck was individualised depending on
morbidity, shortened intra-operative time, faster post- the nodal status. Adjuvant radiotherapy was provided
operative recovery and cosmetically superior with to all stage III/IV cases and those with poor histology.
similar oncological safety6,7. Patients with tumours deemed unresectable
MATERIALS AND METHODS: endoscopically due to its extension into orbit, intradural
and intracranial compartments, nasal bones, hard palate
A retrospective observational analysis of data was
were excluded. Cases with massive involvement of the
conducted at our tertiary care centre with a total of 31
frontal sinuses, lateral bony wall of the maxillary sinus
cases of biopsy proven sinonasal malignancy; those have
and lacrimal apparatus were managed with combined
undergone trans-nasal endoscopic resection. Out of
approach resection. Patients with recurrent or residual
these, 29 cases are included in this study for analysis. 1
lesions and also the radio-residual ones were not part
case each of rhabdomyosarcoma and metastatic
of the study group. None of the patients were subjected
malignant eccrine spiroadenoma of nape of neck were
to palliative resection or debulking procedure thus
excluded in this study due to incomplete/palliative
strictly following oncological protocols. Cases requiring
treatment. Patients undergoing external approach for
cribriform plate resection were included and the defect
facial and cranial access, aided with endoscopy were
Vol.-11, Issue-I, January-June - 2017 17
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
was repaired after complete tumour excision. Data was Disassembling tumour using powered
analyzed using Kaplan Meier method of estimation to instrumentation and/or cutting instruments
estimate the overall survival and 2 year disease specific which reduces the bulk of the tumour and helps
survival rate along with the median survival time to visualise the margins clearly
wherever applicable. Statistical analysis was carried out Removal of the posterior nasal septum & sphenoid
using STATA 13. rostrum.
Surgical technique: Draf type IIb frontal sinusostomy in the case of
10
Goffart et al (2000) and Casiano et al (2001) 11 Unilateral mass with frontal sinus extension and
popularised the technique of endoscopic resection of Draf type III median frontal sinusostomy is
sinonasal tumours. The addition of navigation and performed if the lesion involves both sides by
powered instruments has provided a helping hand to identifying the cribriform plate.
the skull base surgeon. Centripetal Removal: Exposure of antero-superior
Some surgical landmarks which are of prime and posterior inferior margin.
importance: Endoscopic medial maxillectomy type III
Superior turbinate and Ostium of the sphenoid Nasoethmoidosphenoidal complex is isolated and
sinus. pushed towards the central part of the nasal fossa
The maxillary sinus roof is used as a robust (centripetal technique) and removed12.
landmark to allow safe dissection and debulking Skull Base Removal: Can be extended to resect
of pathology. anterior cranial base.
Maxillary ostium guides the removal of pathology. Reconstruction: Endoscopic multilayer technique.
An alternative way is by proceeding posteriorly Reconstruction of skull base defect was done by
to enable a safe entry to the sphenoid sinus, and thus using fascia lata. The second layer was followed by
the true skull base, when normal structures such as the superiorly based local septal mucosal reflected from
superior turbinate and sphenoid ostium are not other side of the septum or a pedicled nasoseptal flap
available.
The primary aim in endoscopic tumour excision
is radical removal of the lesion with safe margins, as in
traditional procedures. The cornerstone of oncological
surgery i.e. enbloc resection to avoid the risk of
tumour spillage is outdated and is replaced by the
concept of disassembling of the lesion, having under
view the limits between normal and diseased mucosa10,11.
Surgical technique varies slightly from one patient to
another according to the site of origin and extent of
the lesion.We used a powered instrument like
microdebrider or/and KTP-532 laser for reducing the
bulk of the primary tumour for better manipulation
and visualisation of margins and assessment of extent
of resection. Bony cuts were then made with
osteotome/drill from the healthy area with a good
margin. Figure-1: Adenocarcinoma (a&b) CT scan paranasal sinus
showing the tumour extention, (c) intra operative endoscopic
Some basic steps are followed during the resection picture before resection (d) post operative endoscopic picture
which can be modified depending on type of disease after one year post operative period with no evidence of
and extent: (Fig 1, 2, 3, 4, 5) disease.
18 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
Figure-3: Olfactory Neuroblastoma (a,b ) pre operative CT), (c,
d) post operative CT), (e)showing the lesion occupying the superio
aspect of nasal cavity, (f) showing exposure of skull floor of frontal
sinus anterior to 1st olfcory neurone. Note the tumour along with
Figure-2: Squamous Cell Carcinoma (a)pre operative& (b) healthy mucosal margin has been separated (g) A Draf-II sinusostomy
post operativeCT scan. has been performed to identify the skull base & the tumour has been
resected completely from dura after removal of adjacent bone, (h)
Showing reflection of septal flap from opposite side to cover the
dura.
Figure-4: Inverted Papilloma with Transitional Cell Figure-5: Residual Chordoma following neurosurgical
Carcinoma (a ) Showing the lesion (b) A Draf-II procedure resection in nasal cavity extending into into the sphenoid sinus
in progress (c) Showing resection of soft tissue attached to and nasal cavity (a) Showing the lesion, (b) Resection of
tumour that was extended to the nasopharynx with KTP laser tumour from nasal cavity ethmoid and sphenoid sinus, (c)
from skull base after a posterior septectomy(d) Additional showing posterior septectomy being done to facilitate tumor
drilling of bone is being done for clearance from sphenoid removal from the floor of the sphenoid sinus and clivus (d)
sinus floor and nasopharynx). Showing the removal of the tumor from the roof of
nasopharynx.
Vol.-11, Issue-I, January-June - 2017 19
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
(Haddad flap) for support13. Nasal packing was done Malignancy of Salivary gland origin
with moistened absorbable nasal packs. All cases (Adenocarcinoma and Adenocystic carcinoma)
anticipated for CSF leak, were provided complete bed- comprised the majority (34.4%) of cases followed by
rest keeping the head in a 20 degree elevated position squamous cell carcinoma (24.1%), malignant melanoma
until the 3rd post-operative day. Intravenous third- (3.4%) and others. 1 case of olfactory neuroblastoma
generation cephalosporin therapy was started the day belonging to Kadish stage B was a part of the study
before surgery and continued for at least 7days. Nasal group. The remaining 28 cases were stage-wise
irrigation and cleaning with normal saline solution was categorised as given in Table 2. Adjuvant radiotherapy
started after 2-3 days with topical antibiotic ointment. was advised in stage III/IV cases and in cases with
Regular nasal endoscopic cleaning of the nasal cavity aggressive tumour behaviour. One patient of malignant
was done and looked for suspicious lesions. All patient melanoma received immunotherapy. A case of smooth
with T3 and T4 disease and 5 cases of stage II disease muscle tumour of unknown malignant potential was
received post operative adjuvant Radiotherapy/Chemo- treated with endoscopic resection only.14 24 of the 29
Radiotherapy. patients had no disease on their last follow up. 5 cases
RESULTS: had loco-regional recurrence of which stage I and II
cases had no contribution. We had 2 recurrences in
The age range was 39-64 years with a mean of
stage III out of which one at 14 months was re-excised
49.4yrs. 67 % of the patients were males. The histological
using endoscopic technique and the other one at 28
subtypes of the sinonasal malignancies managed via
endoscopic approach are given in Table 1.
Table 2: Stage Wise Classification Of Cases.
Table 1: Histological Subtypes (Includes tumours14,15,16
treated with endoscopic approach only)
20 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
months was managed with an external total maxillo-
ethmoidectomy. In stage IV with extension of disease
into sphenoid or frontal sinuses, 3 cases had loco-
regional recurrences, two of which at 16 and 19 months
respectively were managed with external approach using
total maxillo-ethmoidectomy and sphenoidotomy or
external frontoetmoidectomy procedure. One patient
with recurrence at 34 months, refused any further
treatment. 2 patients had lung metastasis after 3 years
(1 death at 42 months).
No significant complication was noted intra-
operatively and during post-operative recovery.
Epistaxis was noted in 3 cases and was managed
conservatively during post-operative period. Hyposmia
was observed in 2 patients who are still on regular
follow-up. We did not encounter any CSF leak
Figure 6b: Kaplan-Meir graph showing 2 year specific survival
probably due to the multi-layered skull base defect rate.
closure technique and vigilant post- operative care. The
overall survival rate for the study population was found surgeons all over the globe realise the possibility of
to be 82.7%. 15 out of the 18 patients followed up for managing sinonasal tumours with this approach4. While
2 years were found to be disease free and hence the 2 there have been many reports describing its use in
year disease specific survival rate was 83.33% (Fig.6) benign tumours, there has been a dearth in literature
DISCUSSION: on its efficacy in managing malignant lesions17.In
The extensive use of endoscopic approach for addition to the excellent visualization owing to better
dealing with chronic sinusitis made the skull base optics and imaging advances, endoscopic approaches
have significantly reduced the need for craniofacial soft-
tissue dissection, skeletal disassembly, and cerebral
retraction for tumor access and resection 17,18.The
endoscopic approach facilitated better access to difficult
areas such as the frontal recess, sphenoid sinus, orbital
apex, pterygomaxillary space and inferior part of the
septum while avoiding dissection of vital non-involved
structures thus providing an added advantage over open
techniques 18. The lack of external incisions and
improved cosmesis makes it a patient friendly and
compliance inducing approach. Dave et al19stated the
advantages including , avoidance of craniotomy, facial,
gingival, and bi-coronal incisions, extensive facial
osteotomies, lumbar drains, tracheotomy, and frontal
lobe retraction in this endoscopic technique. Other
potential advantages include decreased operative time,
reduced anesthetic risk, shorter hospital stay, less
postoperative pain, and fewer complications4,18,19. These
advantages probably provided an impetus for the
increased adoption of endoscopic approaches for
Figure 6a: Kaplan-Meir Graph showing Overall survival rate. surgical management of selected sinonasal malignancies.
Vol.-11, Issue-I, January-June - 2017 21
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
With respect to oncological results, Nicolai et al20 surgery. Proper selection of cases amicable to endoscopic
reported the largest series to date, with 184 patients resection forms the backbone of success in endoscopic
with naso-ethmoidal malignancies of which one resection of sinonasal tumors. Accurate clinical and
hundred thirty-four patients (72.8%) were managed radiological assessment of the lesion with neurosurgical
exclusively by an endoscopic approach, whereas 50 back-up is an added advantage 25,26. Tumors with
required an adjunct craniotomy with mean follow-up involvement of dura, orbital contents, palate and those
of 34.1 months. The overall rates of disease-free survival, with intra-cranial extension were better managed with
alive with disease, died of disease, and died of other open approaches26.
causes were 80.9%, 4.4%, 11.4%, and 2.2%, respectively. On the other hand, various concerns have been
Ehab et al17 concluded that out of his 120 patients, 18 raised regarding the safety and efficiency of this
(15%) experienced local recurrence, with local disease technique as well. En-bloc resection of tumour was not
control of 85%. The 5- and 10-year disease-specific possible in most cases using this technique but literature
survival rates were 87% and 80%, respectively. The 5- suggests that piece-meal resection has no oncological
and 10-year overall survival rates were 76% and 50%, disadvantage4,18,19,. Generous margins are often not
respectively. Lund et al21in their work, reported a 49- possible even in external approach owing to the close
patient prospective cohort that underwent endoscopic proximity to critical structures and the delicate ethmoid
resection as an alternative to CFR. Overall survival was septations which prevent the specimen from being
88% at 5 years, with 36 patients free of disease, seven intact. Moreover, multiple endoscopic series employing
patients with residual disease, and six patients died of the piecemeal approach have not demonstrated
disease. Ganly et al22 reviewed pooled data on 334 compromise in survival17, 18, 19, 24. The anterior skull base
patients from 17 institutions and noted overall survival reconstruction was also an area of concern. However,
and recurrence-free survival of 48% and 46%, use of local flaps and free non-vascularised flaps with
respectively. Dulguerov et al23retrospectively reviewed fat and absorbable nasal packing material in multi-
220 patients of olfactory neuroblastoma from 1975 to layered technique provided excellent results13.Whereas
1994 with a minimum 4-year follow-up. The 5-year the endoscopic approach allows clear visualization
actuarial survival rate was 63% with 57% local control through different angled endoscopes, an external
rate. Batra et al18 studied 31 patients and calculated approach relies primarily on tactile discrimination,
overall survival was 86.2% and 58.6% at 2 and 5 years direct visualization and preoperative anatomic imaging
respectively. They also found the disease-free survival during tumour resection. The lack of tactile sensation
to be 64% and 51.7% at 2 and 5 years respectively. in endoscopic resection is compensated by the advanced
Literature has witnessed better oncological results optics, powered instruments, magnified view and
with Esthesioneuroblastoma compared with other navigation system17, 18, 19. The addition of intra operative
sinonasal malignancies and hence results on only these frozen section examination has undoubtedly improved
tumors cannot be extrapolated on other pathological resection margins and oncological results, but is only
types22,24. The pathology of primary tumor was noted optimal when combined with adequate visualization
to be an important predictor of survival in the using an endoscope18, 19.
international collaborative study4. The 5-year disease- Despite the debate on the surgical approach, the
free survival rates for Esthesioneuroblastoma, SCC, and oncological objective of complete tumour removal with
melanoma were 75%, 50%, and 27%, respectively. This adequate margins must be balanced with minimal
is very comparable to the 5-year disease-specific rates morbidity and better quality of life. At this juncture,
of 88%, 51%, and 18% for the same three pathologies data from multiple reports suggests that the endoscopic
reported by Bentz et al24. This comparison must be approach provides similar surgical objectives while
viewed keeping in mind the small sample size in each decreasing intra operative complications and
subgroup. We had 1 case of olfactory neuroblastoma minimizing long-term patient morbidity compared to
which was disease free on their last follow-up. Our 3 the open techniques 1,4,17 . Our study is a single
cases of malignant melanoma were managed institutional one, with a small sample size which needs
endoscopically and adjuvant radiotherapy was taken further addition over the next few years. Local
by one patient. One case received immunotherapy post- recurrence, poor outcomes, and decreased survival are
22 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
all associated with positive surgical margins4, 18.In our modulated radiotherapy has improved the outcomes
series, there were no positive margins. Some of the cases with minimal toxicity18.
with significant inferior extension to the floor of the CONCLUSION:
nose, anterior extension onto the facial soft tissues,
Endoscopic resection of malignant sinonasal
lateral extension to the maxillary sinus, orbit,
tumours has made a path-breaking change in the
pterygomaxillary space, or Infratemporal fossa were
management of these cases. Providing similar
taken up for a combined endoscopy assisted open
oncological safety with minimal morbidity and
approach and are not included in this study. We had 3
improved cosmesis forms the corner-stone of this
cases (10%) of post-operative epistaxis which were
technique. We uphold the fact that endoscopic
managed conservatively and 2 cases (6%) of hyposmia
approaches are not a replacement to conventional open
on regular follow-up. Nicolai et al. noted mean
techniques which have to be the choice in advanced
hospitalization time of 3.7 days for the exclusive
cases. However, with proper case selection, we could
endoscopic group while it was 4.2 days for our patients.
provide the patient in selected cases with this alternative
Moreover, major complication noted in the exclusive
option of endoscopic resection provided; the surgeon
endoscopic approaches (6% CSF leaks), following dural
is oncologically skilled and equipped to manage the
resection and repair. Successful separation of the
expected complications. Adequate expertise in skull base
intracranial and sinonasal compartments and multilayer
reconstruction is also mandatory prior to embarking
reconstruction provides the best opportunity for water
on such surgical voyages, especially when dural breach
tight closure for large skull base defects 4,5 .
is noted, necessitating resection and reconstruction.
Reconstruction was not a major problem in this series
Endoscopic technique of resection and reconstruction
as tumours transgressing the dura were not in the study.
is indeed a boon to the new generation of skull base
In accordance with the work by Bentz et al24, adjuvant
surgeons in providing patient friendly results with
radiotherapy was provided in tumors that had higher
improved compliance.
T stage, high-grade pathology, positive margins, large
volume of disease, or extensive local invasion, bone DISCLOSURES:
invasion, positive nodal status. Atrophic rhinitis, (a) Competing interests/Interests of Conflict- None
blindness, frontal lobe necrosis, and radiation induced (b) Sponsorships - None
malignancies were some adverse effects of radiotherapy (c) Funding - None
at this site noted in literature. (d) No financial disclosures
The challenges in endoscopic management of (e) Animal rights-Not applicable
sinonasal tumors begin with a proper case selection REFERENCES :
using strict endoscopic and radiological parameters for 1. J. A. Eloy, R.J. Vivero, K. Hoang et
successful outcome and to prevent mishaps intra- al.Comparison of transnasal endoscopic and open
operatively4,5. The operating surgeon must be well- craniofacial resection for malignant tumors of the
versed in both; endoscopic nasal surgery and surgical anterior skull base.Laryngoscope, 2009;119:834
oncology principles which needs a prolonged learning 840.
curve. The hospital should be dedicated and equipped
2. T.Z.Shipchandler, P.S.Batra, M.J.Citardi et al
for managing critical patients with a good neurosurgical
Outcomes for endoscopic resection of sinonasal
support. A tailor-made, incremental, systematic
squamous cell carcinoma. Laryngoscope,
approach to increasing complex cases may improve
2005;115:1983-1987.
outcomes and decrease risk of complications. Relative
3. Thaler ER, Kotapka M, Lanza DC, Kennedy DW.
contraindications for endoscopic resection include
Endoscopically assisted anterior cranial skull base
highly vascular tumors, extensive bilateral disease, and
resection of sinonasal tumors. Am J Rhinol
significant orbital or Infra temporal fossa
1999;13:303310.
involvement25,26. The surgeon must be well equipped
with skills and instruments to convert the planned 4. McCutcheon IE, Blacklock JB, Weber RS, et al.
endoscopic procedure into an open approach if need Anterior transcranial (craniofacial) resection of
arises. Adjuvant radiotherapy using Intensity tumors of the paranasal sinuses: surgical technique
Vol.-11, Issue-I, January-June - 2017 23
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
and results. Neurosurgery 1996;38:471479. 16. R Kudva, S Sharma, R Gurijala, D R Nayak,
5. Har-El G, Casiano RR. Endoscopic management Sinonasal Type Hemangiopericytoma of Nasal
of anterior skull base tumors. OtolaryngolClin Cavity: A Rare Neoplasm, RRJMHS, Volume 3,
North Am 2005;38:133144. Issue 3, July - September, p 31-36, 2014
6. Y. Bi, SHe,T.Guo.Modifiedtransnanal endoscopic 17. E.Hanna, F. DeMonte, S. Ibrahim et al,Endoscopic
maxillectomy: a novel surgery style of maxillary Resection of Sinonasal Cancers with and Without
malignant tumor. Int J ClinExp Med Craniotomy. Arch OtolaryngolHeadNeckSurg.
2016;9(6):11361-11366.
2009;135(12):1219-1224.
7. S.K.Singhal, N.M.Nagarkar, A.Dass et al.
18. P.S. Batra, A. Luong, S.J.Kanowitz et al, Set
Endoscopic removal of tumours of nose and
paranasal sinuses- our experience. Clinical Outcomes of Minimally Invasive Endoscopic
rhinology: an international journal, jan-april Resection of Anterior Skull Base Neoplasm.
2011,4(1), 27-37. Laryngoscope 2010:120:916, 2010
8. C. Walch, HStammberger, W. Anderhuber et al. 19. S.P. Dave, A.Bared,R. R. Casiano et al, Surgical
The Minimally Invasive Approach to Olfactory outcomes and safety of transnasalendoscopic
Neuroblastoma: Combined Endoscopic and resection for anterior skull tumors.
Stereotactic Treatment. Laryngoscope OtolaryngologyHead and Neck Surgery (2007)
2000:110:635640. 136, 920-927.
9. Edge SB, Compton CC. The American Joint 20. Nicolai P, Battaglia P, Bignami M, et al.
Committee on Cancer: the 7th edition of the Endoscopic surgery for malignant tumors of the
AJCC cancer staging manual and the future of sinonasal tract and adjacent skull base: a 10-year
TNM.Ann SurgOncol. 2010 Jun;17(6):1471-4.
experience. Am J Rhinol 2008;22:308316.
10. Goffart Y, Jorissen M, Daele J,. Minimally
21. Lund V, Howard DJ, Wei WI. Endoscopic
invasive endoscopic management of malignant
resection of malignant tumors of the nose and
sinonasaltumours. ActaOtorhinolaryngol Belg.
2000;54:221-232. sinuses. Am J Rhinol 2007; 21:8994.
11. Casiano RR, Numa WA, Falquez AM (2001) 22. Ganly I, Patel SG, Singh B, et al. Craniofacial
Endoscopic resection of esthesioneuroblastoma. resection for malignant paranasal sinus tumors:
Am J Rhinol 15:271279. Report of an International Collaborative Study.
12. P. Castelnuovo , M. Turri-Zanoni, P. Battaglia et Head Neck 2005;27:575584.
al, Endoscopic Endonasal Approaches for 23. Dulguerov P, Calcaterra T. Esthesioneuro-
Malignant Tumours Involving the Skull Base; blastoma: the UCLA Experience 19701990.
CurrOtorhinolaryngol Rep 2013: 1:197205. Laryngoscope 1992; 102:843849.
13. Hadad G, Bassagasteguy L, Carrau RL et al, A 24. Bentz BG, Bilsky MH, Shah JP, Kraus D.
novel reconstructive technique after endoscopic Anterior skull base surgery for malignant tumors:
expanded endonasal approaches: vascular pedicle a multivariate analysis of 27 years of experience.
nasoseptal flap. Laryngoscope 2006:116:18821886.
Head Neck 2003;25: 515520.
14. D.R.Nayak, A.D.Ghanpur, A.N.Reddy et al,
25. Roh HJ, BatraPS, Citardi MJ. Endoscopic
Smooth muscle tumor of uncertain malignant
potentialin the nasal cavity: an incidental finding. resection of sinonasal malignancies: a preliminary
BMJ Case reports ,Nov 2016. report. Am J Rhinol 2004;18:239246.
15. D.R.Nayak, A.M.Bhandarkar, A.Gudiseva et al, 26. Stammberger H, Anderhuber W, Walch C, et al.
Paranasal Sinus Malignancies A 6 Year Tertiary Possibilities and limitations of endoscopic
Hospital Experience. Indian Journal of Applied management of nasal and paranasal sinus
Research 4(2):2014 February 2014 Doi: 10.15373/ malignancies. Arch Otolaryngol HeadNeck Surg
2249555x/feb2014/123. 1999;53:199205.
24 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
ANTERIOR NASAL PACKING VS SEPTAL CLIPS TYPE III, IN POST
NASAL SEPTAL SUBMUCUS RESECTION & SEPTOPLASTY
SURGERIES: A COMPARATIVE STUDY
*CB Nandyal, **Ravy Udgir, ***LR Shankar Naik, ****Vinayak Kurle
HOW TO CITE THIS ARTICLE Date of receipt of article -30-12-2016
Nandyal C B, Udgir R , Shankar Naik L R, Kurle V.Anterior
nasal packing vs septal clips type III in post nasal septal submucus Date of acceptance 24-02-2017
resection & septoplasty surgeries: a comparative study. Orissa J DOI- 10.21176/ojolhns.2017.11.1.4
Otolaryngology Head Neck Surgery 2017 June; 11(1): 25-31.
DOI: 10.21176/ojolhns.2017.11.1.4 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.4
ABSTRACT:
Background & Objectives: The objective of present study is to compare 2 techniques of nasal packing after
SMR (submucus resection) or septoplasty surgeries i.e anterior nasal packing (ANP) & nasal septal clip type III
(NSCT).
Materials & methods: This is a prospective randomized comparative study including 50 patients above 18 years
who underwent SMR or septoplasty for deviated nasal septum (DNS). The patients were randomly divided into
two equal groups for nasal packing using NSCT or ANP.
Results: Intra operatively, packing with NSC was easier, faster. And support provided to the septum could be
assessed visually when compared to ANP (t = 7.52, p < 0.001). Trauma to mucous membrane occurred during
packing was 8% in ANP and 4% in NSC group. In immediate post op we noted headache, 20 % in NSC and 92%
in ANP, epiphora 12% in NSC and 100% in ANP. Sleep disturbance 16 % in NSC and 18 % in ANP, dysphagia
80% in ANP and 0 % in NSC and bleeding 20% in NSC who were managed with nasal decongestants (p<0.001).
At pack removal severe pain was experienced in 100% ANP and 8 % in NSC. Bleeding occurred during pack
removal was16% in ANP and 8 % in NSC (x2= 12.39, p<0.05). Follow up complications noted were synechiae
in 8% in ANP, 4% in NSC, septal hematomas in 4% in each. The necrosis of the mucous membrane was noted
in 4% in ANP group and treated conservatively. None suffered septal perforation.
Conclusion: Purpose of packing was served by both methods more or less equally but NSC was better tolerated
in post operative period with less post operative discomfort and follow up complications when compared to
ANP.
Keywords: Deviated nasal septum (DNS); SMR; Septoplasty; Nasal septal clip type III (NSC); conventional
anterior nasal packing (ANP).
Affiliations:
*Associate Professor &HOD,**Senior Resident,*** & ****Post graduate,
INTRODUCTION: Department of ENT
Though the history of nasal packing after Mahadevappa Rampure Medical College (MRMC)
Gulbarga, Karnataka, India
septoplasty or SMR dates back to 1847 from the time
Address of Correspondence:
of Gustay Killian of Germany & Otto Tiger Freer of Dr. Vinayak Kurle
USA, yet the systematic nasal packing post septoplasty Post Graduate
or SMR was started in 1882 by Ephraim in Chicago & Dept of ENT
M.R.Medical College
Peterson in Germany1 which was routinely followed Kalaburgi, Karnataka, India
for many decades to give the functional support to the Ph.: 9844035399.
Vol.-11, Issue-I, January-June - 2017 25
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
nasal septum with good flap opposition minimizing conventional anterior nasal packing with saline soaked
the risk of complication like bleeding & adhesions. antibiotic ribbon gauze (fig2) or with Nasal septal clip
However nasal packing itself causes postoperative type III (fig 1) on both sides of nose by dividing 25
distress, periorbital oedema, excessive lacrimation, patients for each study group randomly.
sleeplessness, dry mouth, cardiopulmonary In NSC Type III group after completion of
complications2, 3, 4 & some says its removal as the most surgery, the horizontal incision at lower border of
painful experience of their life2. Thus alternatives like mucoperiosteal flap on one side to drain any residual
BIPP gels5, Vaseline gauze, merocel6 were used to blood or collection in between the septal flaps. A cut
address mainly bleeding but other complications were was given along the dotted line in the middle of the
debatable7. septal soft rubber splint & lubricating it with
In this view Stucker & Ansel8 questioned the soframycin ointment was gently inserted by crimping
benefits of nasal packing, since then with alternative the splint through the nostrils and then along the floor
techniques using absorbable materials like platelet rich of nasal cavity & manipulated to pass medial to middle
gels6, tissue adhesives6, bovine gelatin mixed with & inferior turbinate to approximate both the flaps on
thrombin9, modified hyaluronase6 to obviate the need both sides. A thread is passed into the holes in the splint
of pack removal, but biocompatibility & cost issue was and tied loosely in front of columella. Then holding
raised9. To get out from this customary nasal packing the thread loop, the septal clip is held open by the nasal
alternative techniques like, through & through speculum and is introduced over the splint to make
absorbable sutures10, septal splints with quilting sutures sure that the metallic septal clip does not touch the
or clips 4,11, septal magnets12, were used with comparisons mucosa to maintain the septum in corrected position
with merits & demerits introduced without & post nasal bleed was checked to confirm the
standardization regarding the complete details of the hemostasis.
technique & purpose served along with postoperative
morbidity & complications. Hence a clinical
comparative study was conducted between customary
antibiotics soaked gauze nasal packing with that of
commercially available nasal septal clip type III
consisting of soft rubber splint & septal clip, to see
which technique is better overall & to give functional
support to nasal septum after post SMR & septoplasty
surgeries.
MATERIALS AND METHODS:
This is a prospective, comparative study of 50
patients conducted at M.R Medical College attached
Fig. 1- Nasal septal clip type III.
to Basaweshwara Teaching and General Hospital,
Kalaburgi from September 2010 to September 2011.
Ethical clearance was taken from the institute.
Informed and written consent was taken from all
patients of 18 yrs & above with thorough history and
clinical examination. Those who were diagnosed as
having DNS as the only cause for nasal obstruction
were included in study. They were all operated on the
basis of Cottles line, those DNS that were anterior to
line were subjected to Septoplasty and posterior to the
line were subjected to SMR.Post-surgery, bilateral nasal
packing was done after complete hemostasis using Fig.2- Anterior nasal packing.
26 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
In anterior nasal packing group, nasal packing was commercially available. As insertion of pack was
done using saline soaked ribbon gauze treated with concerned it was easy to introduce NSC T III but not
soframycin antibiotic cream was inserted to fill the nasal so easy with ANP .The time required for ANP was
cavity stalked layer by layer from floor to roof gently more compared to NSC T III.Mean and S.D for ANP
to approximate & support the nasal septal flaps on both is 4.32+/-1.12 and Mean and S.D for NSC T III is
sides & post nasal bleeding was checked for hemostasis. 2.04+/-1.03. Hence the statistical difference of time
Postoperative signs & symptoms like headache, required in packing is highly significant.
epiphora, dysphagia, disturbance of sleep, bleeding was The postoperative symptoms Headache, epiphora,
noted & tabulated. One day later nasal packing removed dysphagia, sleep disturbance, bleeding which occur after
& assessed for signs & symptoms suffered during pack surgery due to packing were compared and found that
removal. Follow up done weekly for one month & with NSC T III symptoms noted were Headache in 5
clinical observations were noted & any complication patients(20%), Epiphora in 3 patients(12%), dysphagia
was managed with minor intervention, conservatively. in 0 patients(0%), sleep disturbance in(4) patients(16%),
Finally both the groups were compared along with bleeding in 5 patients(20%).
statistical significance.
RESULTS: Table 2. Post- operative subjective signs & symptoms.
50 patients attending ENT, OPD with clinical
features of DNS were selected randomly. According
to Cottles line those who had anterior deviation were
subjected to Septoplasty and those posterior to line
were subjected to SMR. Two groups were made of 25
in each group irrespective of type of surgery for nasal
packing in the form of NSC Type III and anterior nasal
packing randomly. The following observations were
made, tabulated as below (Table-1).
Intraoperatively nasal packs were available in the
OT i.e ribbon gauze piece and antibiotic
soframycin,whereas NSC Type III were to make it
Table-1: Intra operative nasal comaprision.
Sense of discomfort in 4 patients (16%) out of total
25 patients (100%).Whereas in ANP group Headache
in 23 patients(92%), Epiphora in 25 patients (100%),
dysphagia in 20 patients (80%), sleep disturbance in 20
patients (80%), bleeding in 0 patients(0%), Senses of
discomfort in 23 pts (92%) out of total 25 patients (100%)
were noted (Table-2).
Looking at the x2 and p value for individual signs
and symptoms the study carries a significant difference
Vol.-11, Issue-I, January-June - 2017 27
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
between the two groups.In ANP group pain occurred (4%), synechiae 2pt (8%), septal perforation 0patient
in all 25 patients during pack removal and bleeding in (0%) of total 25pt (100%). Statistically there is no much
4 patients, whereas in NSC T III group 2 suffered pain difference between the two groups (Table-4).
during clip removal and 2 had bleeding. Statistically
DISCUSSION:
x2=12.39, p<0.05 hence a significant difference
between the symptoms suffered during pack removal In our study 50 patients were taken with only
(Table-3). symptomatic DNS in which 26 patients had anterior
deviation who underwent septoplasty and 24 patients
Table 3: Signs & Symptoms at pack technique and had posterior deviation that underwent SMR
findings removal. respectively. Accordingly 2 groups were made; 25 in
each group irrespective of type of surgery for nasal
packing in the form of NSC TYPE III & conventional
anterior nasal packing randomly. Among study group
patients were in the age group of 18-50years with 26
males (41.7%) & 24 females (58.3%).
In all other studies the age group selected is 15
years and above11, 13, 15& in our study was 18 years and
above, for better compliance in terms of giving accurate
subjective signs and symptoms suffered in the immediate
post-operative period and in follow up period. The
other reason would be that the septal splint and clip
Statistically x2=12.39, p<0.05. are available in sizes to fit this age group. As far as
ANP is considered it can be done in any age group. In
FOLLOW UP INDEX total the age distribution & sex does not have any
Table 4: Follow up index. significant attribute towards our study.
The parameters of intra-operative technique of
packing have not been commented upon in literature
for comparison.
As insertion of pack was concerned it was easy
to introduce NSC Type III but not so easy with ANP
with minor difference in mucosal trauma which varies
& depends on the care taken during the insertion of
nasal packing technique used. The time required for
ANP was more as it require more time in assessing the
pack insertion layer by layer with equal amount of pack
to be inserted on both sides when compared to NSC T
After follow up for a period of one month on III which can be directly applied under direct vision
regular basis we found that with ANP group following with equal pressure on both sides of nasal septum.
complications occurred necrosis of mucous membrane Visual Assessement of bilateral pressure was possible
in 0 pt (0%), septal haematoma in 1 patient (4%), with the NSC TypeIII as the pressure is constant and
synechiae in 1 patient (4%), septal perforation in 0 predetermined as per the make whereas with ANP this
patient (0%) of total 25patient (100%). In NSC T III was not so because the volume of gauze could fill any
group the complications seen were necrosis of mucous of the corner of nasal cavity. So mean time consumed
membrane 1patient(4%), septal haematoma 1patient for ANP is more than NSC type III as the mean time
28 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
S.D for ANP is 4.32+/-1.12 and Mean time S.D for septal clips showed headache was 15%, dysphagia 2%,
NSC T III is 2.04+/-1.03. Hence the statistical epiphora 3%, bleeding 0%, dryness of mouth 4%4 . In
difference (p<0.001) of time required in packing is this regard if we look at the data in the table the
highly sinificant. In Anand et al study on septal clips technique of NSC T III and through and through
and ANP group4, the technical details & advantages of suturing, quilting suturing with 30 vicryl5 or septal
insertion & time duration was not mentioned. clips4 had not much significant difference in terms of
So technically when intraoperatively compared for subjective signs and symptoms except bleeding in
conventional ANP, NSC type III is better as it is more immediate post- op up to 24 hrs period.
easy, quick, under direct vision for proper assessement Coming back to our comparative clinical study it
to support the operated septum except the cost & is evident by our data that for the individual
availablity. postoperative signs & symptoms the study carries a
Postoperative observation on symptom & sign significant difference between the two groups as the
noted in our study in ANP group were Headache in p<0.05 for all postoperative symptoms where NSC
92%, Epiphora in 100%, Dysphagia in 80%, Sleep Type III scores 5-8 times more better than the ANP.
disturbance in 80%, bleeding in 0%, Sense of discomfort During Pack removal in our study in ANP group
in 92% as compared to study conducted by Md Sohail pain was seen in 100% and some complained it as most
Awan et.al in ANP group Headache in 90.90%, horrible experience of life .Similarly in Md Sohail
Epiphora in 100%, Dysphagia in 95.50%, Sleep study it was 97.80%13 and in M.M.Adrehali study it
disturbance in 81.8%, bleeding in 0%, Sense of was 10%11. Bleeding was seen 16% and in Md Sohail
discomfort was not commented13. In M.M.Adrehali study 13 and in M.M.Adrehali study it was not
et.al study, pain as per Visual Analogue Scale (VAS) - 5 commented, whereas in Al Raggad study it was 4.8%14.
was noted11. In Al Raggad et.al study bleeding noted So when compared to other studies, pain and bleeding
was 13% in the ANP group14. In Anand et al study is directly attributed to ANP as it causes pressure and
headache was 72.5%, dysphagia 95%, epiphora 100%, ulceration on nasal mucus membrane.
bleeding 3%, dryness of mouth 40%4. As per the above In NSC T III group in our study pain was noted
data the subjective signs and symptoms suffered in in 8%, in Md Sohail study it was 0%13 and in M.M
immediate post operative period were more or less Adrehali study it was 0% in suturing group11. Bleeding
similar when compared to ANP groups of other studies. was noted in 8%, in Md Sohail study it was 0%13 and in
The post operative complaints are attributed to the effect M.M Adrehali study it was 0% in suturing group11.
of complete block of Nasal Cavity and pressure of the Minimal pain and bleeding experienced in our study is
ANP on Lateral wall of the nose. attributed to pressure effect of clipping on nasal septum
In our study with NSC TypeIII we noted and in other study the suture material used is absolutely
Headache in 20%, Epiphora in 12%, Dysphagia in 0%, not removed in post operative period. Coming back
Sleep disturbance in 16%, bleeding in 20 %, Sense of to our study pain and bleeding is 10 times less in NSC
discomfort in 16%. In the study by Md Sohail Awan T III group when compared to ANP group. So NSCT
et.al they used through and through suture and III is an excellent packing method compared to ANP
observed Headache in 20.50%, Epiphora in 11.40%, as far as pack removal is considered.
Dysphagia in 4.50%, Sleep disturbance in 15.90%, During follow up period of one month in our
bleeding in 2.30%, Sense of discomfort were not study of ANP group we noted necrosis of mucous
commented13. In M.M.Adrehali et.al study quilting membrane in 4%, septal haematoma in 4% and
suture group, pain as per Visual Analogue Scale (VAS) synechiae in 8% was less when compared to Anand et
2 was noted11. In Al Raggad et.al study suture group, al study had synechiae in 12.5% & raw area/mucosal
bleeding noted was 15.3 %14. In Anand et al study on necrosis in 25% & residual DNS 7.5% 4, in Md Sohail
Vol.-11, Issue-I, January-June - 2017 29
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Awan (et.al) study which were necrosis of mucous with minimal tolerable pain. The subjective signs and
membrane in 57% and septal haematoma in 7%, symptoms in the immediate postoperative period and
synechiae in 18%13, in M.M.Ardehali (et.al) study 3% the follow up complications were significantly less
synechiae and 3% septal perforation was noted11, in Al compared to ANP group. As far as ANP is concerned
Raggad et. al study septal haematoma in 4.8% synechiae except for its availability and cheaper cost we did not
in 5.9% and septal perforation in 2.4% was noted14. In find any advantage.
Z.M.Raahat et.al study 2.7%, septal haematoma was
So we conclude that, those who underwent septal
noted10. The lower incidence of complications in our
surgeries with NSC T III as a packing method, were
study is attributed to use of saline soaked antibiotic
benefited more though being costly.
ribbon gauze.
In the last in our opinion when NSC T III is
In our study in NSC type III group septal
available it is advisable to use the same to merit its
haematoma in 4% and synechiae in 4% was noted and
when compared to Anand et al study had synechiae in advantages to the patients.
2.5%, raw area /mucosal necrosis in 17.5% & residual DISCLOSURES:
DNS 7.5% 4, in M M Ardehali (et.al) study synechiae (a) Competing interests/Interests of Conflict- None
in 2% and septal perforation in 1%11, in Al Raggad (et.al) (b) Sponsorships None
study synechiae in 1.1% was noted14. In our study all (c) Funding - None
the complications which occurred were treatable. The (d) Written consent of patient- taken
complication which occurred in Anand et al (residual (e) Animal rights- Not applicable
DNS), in M.M.Ardehali et.al study and Al Raggad
study (i.e. septal perforation) caused due to the suture REFERENCES:
which causes trauma to flaps bilaterally and the knot 1. Wolfgang Pirsig; The origins of systematic SMR
pulls on itself were difficult to treat. The treatment of the nasal septum, facial plastic surgery;
protocols for septal perforation & residual DNS repair 2006;22:217-22.
are also controversial.
2. Fairbanks DN. Complications of nasal packing.
In our comparative study the complications noted Otolaryngol Head Neck Surg 1986 Mar;
in both groups except synechiae which occurred in 8% 94(3):412-15.
in ANP group as compared to 4% in NSC T III group.
3. Sunita C, Inita Matta, Pratima Marker .
This is because the packs exert pressure on both the
Comparision of blind nasal packing vs endoscopic
septum and lateral wall of nose when compared to NSC
control of epistaxis in emergency setting;
T III which exerts pressure on the septum only and the
pressure induced is less than the capillary pressure as international journal of head & neck surgery, may-
per the make. august 2011;2(2); 79-82.
So NSC T III is better in giving less follow up 4. Anand V, Sachin H, Santosh S. Nasal septal clips:
complications than ANP. An alternative to nasal packing after septal
surgery? Indian J otolaryngol head neck surg;
CONCLUSION:
Oct- Dec 2012; 64(4): 346-350; DOI 10.1007/
The Comparative results confirmed that patients
s12070-011-0388-2.
with ANP and NSC T III were benefited more or less
equal as per the purpose of nasal packing was considered 5. S Shah, S Kumara, N Thappa. Outcomes of
to give functional support to septum but the objective endoscopic quilting of nasal septum versus nasal
evidence suggests that, NSC T III was technically quick, packing following septoplasty. The internet
easy to insert under direct vision in giving uniform Journal of Otorhinolaryngology; 2010; vol 13;
support on both sides of septum and can be removed No 2.
30 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
6. Weber RK .Nasal Packing & Stenting, GMS
current topics in Otorhinolaryngology- head &
neck surgery 2009, vol 8, https://
www.ncbi.nlm.nih.gov/pmc/articles/
PMC3199821.
7. Basha SI, Gupta D, Kaluskar SK. Routine nasal
packing following nasal surgery-Is it necessary?
Indian J Otolaryngol Head & Neck Surg, 2005
Jan;57(1):69-71. DOI:10.1007/BF02907637.
8. Stucker FJ, Ansel DG. A case against nasal
packing. Laryngoscope 1978;88(8 Pt 1):1314-17.
9. Reiter D, Alford E, Jabourian Z. Alternatives to
packing in septorhinoplasty. Arch Otolaryngol
Head Neck Surg 1989 Oct;115(10):1203-5.
10. Z.M.Raahat, Nadeem Uddin Naqvi,
NusratRaza,Qazi Ahsan Azeem,RajaMushtaq
Hussain JavedIqbal,Babar Hussain : Post SMR
Intranasal Packing Do We Really Need It?
Pakistan Journal Of Otolaryngology
2008;24:66-67.
11. M.M.Ardehali, S Bastaninejad. Use of nasal packs
and intranasal septal splints following septoplasty.
International J Oral Maxillofac. Surg.
2009oct;38(10):1022-24, doi:10.1016/
j.ijom.2009.05.012.Epub2009Jul 4
12. Albert P seltzer, The use of magnets to maintain
centralization of the nasal septum following
submucus resection: Journal of the national
medical association; 1968 May; 60( 3).210-12
13. Md sohail Awan, MoghiraIqbal. Nasal packing
after septoplasty: a randomized comparison of
packing versus no packing in 88 patients. Ear Nose
Throat J. 2008 Nov;87(11):624-7, PMID:19006062
14. Al-Raggad Daifallah K; El-Jundi Ali M; Al-
Momani Osama S; Al-Serhan Mefleh M;
Nawasrah Omar O; Qhawi Muafaq A;
Husban Adnan M; Suturing Of The Nasal
Septum After Septoplasty, Is It An Effective
Alternative To Nasal Packing?Saudi Medical
Journal 2007, Oct; 28(10):1534-36
15. Muhammad Hafeez, Inayatullah, Kamran Iqbal,
Zakirullah; Septoplasty without nasal packing
Gomal Journal of Medical Sciences July-December
2010, Vol. 8, No. 2:141- 142.
Vol.-11, Issue-I, January-June - 2017 31
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
COMPARISON OF HEARING RESULTS OF TYPE III
TYMPANOPLASTY WITH MASTOIDECTOMY WITH OR
WITHOUT AUGMENTATION OF STAPES HEAD
*Netra A Pathak, *Vidya V Rokade
HOW TO CITE THIS ARTICLE Date of receipt of article - 08-02-2017
Pathak Netra A, Rokade Vidya V. Comparison of Hearing results of Date of acceptance 21-02-2017
type III tympanoplasty with mastoidectomy with or without
augmentation of stapes head. Orissa J Otolaryngology Head Neck DOI- 10.21176/ojolhns.2017.11.1.5
Surgery 2017 June; 11(1): 32-36. DOI: 10.21176/ojolhns.2017.11.1.5
DOI URL- https://doi.org/10.21176ojolhns.2017.11.1.5
ABSTRACT:
Background: To assess and compare the hearing results in patients undergoing tympano mastoidectomy with
classical type III tympanoplasty using temporalis fascia alone and with cartilage augmented type III tympanoplasty.
Methods: Patients of 5 years of age or more with the diagnosis of chronic otitis media (squamous) with conductive
or mixed hearing loss, who underwent classical type III tympanoplasty with or without cartilage augmentation,
were included in the study. Pure tone audiometry (PTA) was performed and patients were clinically evaluated.
Post- operative hearing was assessed in terms of average air bone gap (ABG) and size of ABG closure. Post-
operative hearing results were compared in between classical type III and cartilage augmented type III tympanoplasty
groups.
Results: When comparing average post-operative ABG and size of ABG closure between classical and cartilage
augmented type III tympanoplasty, cartilage augmented group showed marginally better results but this difference
was statistically not significant.
Conclusions: Hearing results after type III tympanoplasty varied widely. There was no statistically significant
improvement in post-operative hearing results in cartilage augmented tympanoplasty when compared to classical
type III tympanoplasty, suggesting possibility of the effects of multiple other factors.
INTRODUCTION: The goal of tympanoplasty is to restore sound
Chronic otitis media (COM) is a common pressure transformation at the oval window by coupling
condition, affecting 0.530% of any community. an intact tympanic membrane with a mobile stapes
Therefore, a conservative estimate of the number of footplate via an intact or reconstructed ossicular chain
people in the world suffering from COM is over 20 and to provide sound protection for the round window
million1. The prevalence of squamous type of chronic
Affiliations:
suppurative otitis media (CSOM) is 3.5%2. The objective
*Professor,** Associate Professor
of tympanomastoid surgery for chronic otitis media, Smt. Kashibai Navale Medical College & General Hospital, Pune
in decreasing order of priority are elimination of disease (Maharashtra)
to produce safe and dry ear; alteration of anatomy to Corresponding address:
prevent recurrent disease, optimization of cleaning and Dr.Vidya V.Rokade
A-2,303 Sun Empire, Sun City Road
otological monitoring; and reconstruction of the middle Vadgaon Bk., Pune-51
ear to achieve serviceable and stable postoperative Phone no. 9922160881
E-mail- vidyarokade@hotmail.com
hearing 4.
32 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
membrane by a closed, air containing, mucosa lined Postoperative ABG closure was calculated by taking
middle ear3. The modern era of tympanoplasty was the difference between preoperative and postoperative
ushered in by Wullstein and Zollner. Wullstein ABG of the average frequencies of 500, 1000, 2000 and
classified the operations as types I through V4. 4000 Hz. Audiometry results were reported. For
In classical type III tympanoplasty or classical type III tympanoplasty, a temporalis fascia graft
myringostapediopexy, disease is removed from was used to bridge the middle ear air space and placed
tympanomastoid compartment and advancement of the in contact with the stapes head. For cartilage
tympanic membrane (TM) or placement of tissue graft augmentation, thin disc of conchal cartilage of partial
is done on top of the stapes capitulum. After this thickness and of 4-6 mm in diameter was interposed
procedure, air-bone gap (ABG) range is around 10-60dB. between the stapes head and temporalis fascia graft.
Merchant et al. in laboratory model demonstrated that Cartilage disc did not touch the external auditory canal
improved hearing results could be achieved in or facial nerve canal.
myringostapediopexy by interposing a thin cartilage The follow up was performed after 10th week
disc between the graft and stapes head4. For augmented postoperatively. During follow up, patients were
type III tympanoplasty, either cartilage or sculptured subjected to pure tone audiometry (PTA) assessment.
cortical bone can be kept between the intact stapes and Results were analyzed in terms of average postoperative
the fascial graft3. ABG and ABG closure. The results between both were
Cartilage disc was hypothesized to improve the compared. The data analysis was performed with the
effective vibrating area of the graft that was coupled help of SPSS 11.5 software package. P value was
to the stapes head. Cartilage also offers the advantage calculated using the independent samples test and P
of higher mechanical stability compared with value of < 0.05 was taken as significant.
membranous transplants thus preventing retraction of RESULTS:
tympanic membrane in the long run but others argue
Total numbers of patients enrolled during the
that it may alter the acoustic transfer characteristics of
study were 80. Out of which CWD mastoidectomy
the graft due to its increasing mass and stiffness of the
and classical type III tympanoplasty was done in 40
reconstructed tympanic membrane.
patients and CWD mastoidectomy and cartilage
MATERIALS AND METHODS: augmented type III tympanoplasty in another 40
A Prospective study was performed from October patients.
2006 to April 2008. Patients who were 5 years and
The difference in post-operative ABGs between
above of both sexes with intact and mobile stapes
classical type III tympanoplasty and cartilage augmented
suprastructure at tympanomastoidectomy surgery for
type III tympanoplasty at different frequencies (500Hz,
COM squamous type were included. Total number of
1000Hz, 2000Hz, and 4000Hz) were analyzed and
patients enrolled during the study were 80. Out of
found to be statistically not significant. The difference
which CWD(canal wall down) mastoidectomy.and
in four frequency average post-operative ABG between
classical type III tympanoplasty was done in 40 patients
these two groups was also found to be statistically not
and CWD mastoidectomy and cartilage augmented type
significant with p value of >0.001.
III tympanoplasty in another 40 patients.
However, the post-operative ABG was better by
Pure Tone Audiometry was performed within
2.5dB and 1.5dB at frequencies 500Hz and 2000Hz in
seven days prior to the operation. The test was
cartilage augmented type III tympanoplasty as
performed through Air Conduction and Bone
compared to classical type III tympanoplasty, but it
Conduction mode. Air and Bone Conduction threshold
was worse by 1.3dB and 2.2dB at frequencies 1000Hz
were calculated by taking the averages of 500, 1000,
and 4000Hz in cartilage augmented type III
2000 and 4000 Hz frequencies. The ABG was calculated
by taking differences between Air conduction and Bone tympanoplasty as compared to classical type III
Conduction threshold. The Air and Bone conduction tympanoplasty. On an average, there was 0.1dB
threshold were recorded both pre and post-operatively. improvement in cartilage augmented type III
Vol.-11, Issue-I, January-June - 2017 33
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
tympanoplasty as compared to classical type III However, in CWD mastoidectomy and cartilage
tympanoplasty, which was statistically not significant augmented type III tympanoplasty, ABG closure was
(Table 1). good at frequencies of 1000Hz, 2000Hz, and 4000Hz
and was average as compared to CWD mastoidectomy
Table 1 : Comparison of frequency wise post-operative and classical type III tympanoplasty whereas it was
PTA-ABG between patients with classical type III worse in 500Hz . The ABG closure was again divided
tympanoplasty and cartilage augmented type III into different categories like 0-5dB, 0-10dB, 0-20dB, 0-
tympanoplasty(n=40 each group)
30dB and 0-40dB. It was noted that 3(7.5%) cases fell
within 0-5dB and 12(30%) cases within 0-20dB in CWD
mastoidectomy and cartilage augmented type III
tympanoplasty whereas 4(10%) cases within 0-5dB and
12(30%) within 0-20dB in CWD mastoidectomy and
classical type III tympanoplasty. (Table 2).
DISCUSSION:
The objectives of this study were to access, analyze
and compare post-operative hearing results in terms of
average ABG and the size of ABG closure in patients
of classical type III tympanoplasty using temporalis
fascia alone and with cartilage augmented type III
tympanoplasty with masoidectomy. During the length
of follow up, there were no cases of cartilage extrusion.
Different methods have been used by different authors
to report the pure tone audiometric post-operative
hearing results in middle ear surgery in the literature.
Among these ABG closure, post operative ABG
presented in 10 dB bins and air conduction threshold
gain are commonly reported indicators of
tympanoplasty outcome. We had applied average PTA-
ABG and size of the ABG closure for audiological
assessment. For calculation of the size of the post-
operative PTA- ABG closure ABGs were divided into
different bins of 0-5dB,0-10dB,0-20 dB,0-30 dB, and
Table 2: ABG Closures in different categories (n=40
>30 dB.
each group)
In our study, while comparing the average post
operative air bone gaps between classical type III
tympanoplasty and cartilage augmented type III
tympanoplasty at various frequencies the differences
were found to be statistically not significant (P>0.001).
The difference in four frequency average post-operative
air bone gap between these two groups was also found
to be statistically not significant with a p value of 0.965.
However, the post-operative ABG was better by 2.5
dB and 1.6 dB at frequencies 500Hz and 2000Hz in
cartilage augmented type III tympanoplasty as
compared to classical type III tympanoplasty but it was
worse by 1.4 dB and 2.3 dB at frequencies 1000Hz and
34 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
4000 Hz in cartilage augmented type III tympanoplasty for stapes head report that post-operative PTA-ABG
as compared to classical type III tympanoplasty. Our of 25dB or less was achieved in 41 (79%) of patients and
findings are to some extent in agreement with those of of 20 dB or less in 54% of patients12. However their
Merchant et al who observed a 5 dB improvement at study included both canal wall up and canal wall down
250Hz, 500Hz and 2000Hz with interposition of thin procedures13. One year after surgery, a post-operative
disc of cartilage between the graft and the stapes head ABG of 20 dB or less occurred in 84.3% (n=27) of
in both of their temporal bone model as well as in their patients and this after a mean follow-up of 7 years, post-
clinical study6. Variation in functional hearing results operative ABG of 20 dB or less occurred in 81% (n =
between the two studies may also have occurred due to 26) of patients. Another factor leading to failure of
this difference in the technique used. While analyzing tympanoplasty is total or partial non-functional results
the frequency wise post-operative average PTA-ABG which are often influenced by wide variability in the
in both the groups it was seen that ABG was the smallest surgical techniques employed, criteria used to evaluate
at 2000 Hz as compared to other frequencies. Similar hearing results and a number of other anatomical,
findings were also noted by Merchant et al in 20037. physiological and pathological events that occur post-
Similarly, there is no clear explanation for the cause of operatively in the middle ear as mentioned above. It
the air conduction thresholds showing to be the lowest must be remembered that fibrosis could be due to the
at 2000Hz however; it could have resulted from underlying middle-ear or upper airway pathology that
resonances generated in the mastoid cavity and ear canal. caused the disease it may not be caused, in part or
Twenty (52.6%) cases in classical type III full, by surgery. Equally important may be the extent
tympanoplasty of our study fall within 30 dB ABG of destruction by the disease that may adversely affect
closure. Our result following classical type III the ultimate functional results. Such issues may be more
tympanoplasty compare well with myringos- relevant in an underdeveloped country like ours.
tapediopexy as a tympanoplasty procedure in canal wall CONCLUSION:
down mastoid surgery as reported by Cheang et al (n The post-operative PTAABG ranged from 15
=22) who observed PTA-ABG closure within 30 dB 61.2 dB in classical type III tympanoplasty while the
in 61.9 % of his patients8. post-operative PTA ABG ranged from 15 47.5 dB in
Our results however are different from those of cartilage augmented type III tympanoplasty, suggesting
natural myringostapediopexy (n=15) and surgical canal the possibility of effect of multiple other factors .The
down myringostapediopexy (n=35) as reported by post-operative PTA-ABG was 2.5dB and 1.6dB less at
Dawes who observed PTA ABG closure within 30 dB frequencies 500Hz and 2000Hz in cartilage augmented
in 87.0 % and 90.0% of his cases in these two groups type III tympanoplasty as compared to classical type
respectively 9 ,10. III tympanoplasty but this difference was not
Another study performed by Cook et al showed statistically significant. In comparison of size of ABG
that the ABG closure in CWD mastoidectomy with closure between classical and cartilage augmented type
cartilage from stapes to drum technique were 30% III tympanoplasty, cartilage augmented group showed
within 10 dB, 69% within 20 dB and 75% within 30 dB marginally better results. In classical type III
which are close to our results11. In our study, 20 (58.8%) tympanoplasty 30% (12) cases and 32.5% (13) cases in
cases in cartilage augmented type III tympanoplasty fell cartilage augmented type III tympanoplasty fell within
within 30 dB ABG closure. Cheang et al in his 30 dB ABG closure. But this difference was statistically
myringolenticulopexy group (n= 20) achieved an ABG not significant. However, cartilage augmentation type
of less than 30 db in 92 % and ABG of less than 20 dB III tympanoplasty in canal wall down mastoid surgery
in 64% of has cases8. Moustafa and Khalifa in their is a worthwhile procedure.
myringo-cartilago-stapediopexy group (n=95) achieved DISCLOSURES:
an ABG of less than 20 dB in 84%10. Kyrodimos et al in (a) Competing interests/Interests of Conflict- None
their cartilage shield type III tympanoplasty (n=52) (b) Sponsorships None
using a 0.8 mm thick cartilage piece with no capitulum
(c) Funding - None
Vol.-11, Issue-I, January-June - 2017 35
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
(d) Written consent of patient- taken (stapes columella): II clinical studies. Otol
(e) Animal rights- Not applicable Neurotol 2003; 24(2):186 94.
REFERENCES: 7. Goode RL, Friedrichs R, Falk S. Effect on hearing
1. Sad J. Introduction. (eds) Cholesteatoma and threshold of surgical modification of the external
mastoid surgery. illus, Kugler Publications BV, ear. Ann Otol Rhinol Laryngol.1977; 86:441451.
Amsterdam, The Netherlands, p-1-3. 1982. 8. Cheang PP, Kim D, Rockley TJ.
2. Adhikari P, Sinha BK, Pokhrel NR, Kharel B, Myringostapediopexy and myringolenticulopexy
Aryal R, Ma J. Prevalence of chronic suppurative in mastoid surgery. J Laryngol Otol. 2008;
otitis media in school children of Kathmandu 17(3):1-5.
District. Journal of Institute of Medicine. 2007; 9. Dawes PJ. Myringostapediopexy: surgical
29(3):10-12. expectation The Journal of Laryngology &
3. Merchant SN, Rosowski JJ. Auditory Otology. 2003 March; 117:182185.
physiology.Glassock-Shambough Surgery of the 10. Moustafa HM, Khalifa MA. Tympano-cartilago-
Ear, 5th edition. Elsevier India, New Delhi.2003, stapediopexy: a method to improve hearing in open
64-78. technique tympanoplasty. J Laryngol Otol. 1990;
4. Merchant SN, McKenna MJ, Rosowski JJ. 104:942-4.
Current status and future challenges of 11. Cook JA, Krishnan S, Fagan PA. Hearing results
tympanoplasty. Eur Arch Otorhinolaryngol. following modified radical versus canal-up
1998; 255:221228. mastoidectomy. Ann Otol Rhinol Laryngol .1996;
5. American Academy of Otolaryngology-Head 105(5):379-83.
Neck Surgery Foundation, Inc. Committee on 12. Kyrodimos E, Sismanis A, Santos D. Type III
Hearing and Equilibrium guidelines for the cartilage shield tympanoplasty: an effective
evaluation of results of treatment of conductive procedure for hearing improvement. Otolaryngol
hearing loss. Otolaryngol Head Neck Surg. 1995; Head Neck Surg. 2007; 136(6):982-5.
113:186-7. 13. Malafronte G, Filosa B,and Mercone F. A new
6. Merchant SN, McKenna MJ, Mehta RP, et al. double cartilage block ossiculoplasty: long term
Middle ear mechanics of type III tympanoplasty results. Otol Neurotol 2008; 29:531-33.
36 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
UTILITY OF HADAD FLAP IN RECONSTRUCTION OF
ANTERIOR SKULL BASE DEFECTS FOLLOWING
ENDOSCOPIC TRANSNASAL, TRANS SPHENOIDAL
APPROACH TO PITUITARY-OUR EXPERIENCE
*Harshita V. Sabhahit, **Shruthi GS, ***Santosh AN, ****G Prabhakar, *****Ananthkrishnan
HOW TO CITE THIS ARTICLE Date of receipt of article -08-02-2017
Harshita V.S, Shruthi GS, Santosh AN, G Prabhakar, Ananthkrishnan.
Utility of Hadad flap in reconstruction of anterior skull base defects Date of acceptance 25-04-2017
following endoscopic transnasal, Trans sphenoidal approach to DOI- 10.21176/ojolhns.2017.11.1.6
pituitary-our experience. Orissa J Otolaryngology Head Neck Surgery
2017 June; 11(1): 37-42. DOI: 10.21176/ojolhns.2017.11.1.6 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.6
ABSTRACT:
Objective: To study the utility of Hadad flap in reconstruction of anterior skull base defects following endoscopic
transnasal, transsphenoidal approach to pituitary tumours in conjunction with multi-layered reconstruction.
Setting: The study was conducted in the departments of Otorhinolaryngology and Neurosurgery in a tertiary
care referral hospital.
Patients: 20 consecutive patients with pituitary tumours underwent endoscopic transnasal transsphenoidal
approach for resection followed by reconstruction of consequent skull base defects with Hadad flap in conjunction
with multilayered approach.
Results: 3 out of 20 (15%) patients had early postoperative CSF leak, 2 out of which ceased after repositioning
of malaligned Hadad flap.1/20 (5%) patients continued to have delayed postoperative CSF leak.
Conclusion: Hadad flap has proved itself to be the workhorse of anterior skull base reconstruction in most
instances. It has heralded an era of vascularised flap based reconstruction in endoscopic transnasal transsphenoidal
surgeries.
Key words: Nasoseptal flap, endoscopic transnasal transsphenoidal surgery.
INTRODUCTION: transnasal transsphenoidal surgeries as an approach to
Hadad flap has been proven to be the work horse pituitary tumours.
for anterior skull base defects in most instances. It is
very effective in separating the nasal cavity from the
Affiliations:
cranial cavity and has proven to be very robust. It helps *, ** Assistant Professors,Dept of ENT, ***Associate Professor,Dept. of
in preventing ascending infection into the cranial cavity ENT, ****Professor ,Dept of ENT, *****Professor and HOD, Dept of
and is very useful in preventing CSF leaks. It is based Neurosurgery. Vydehi Institute of Medical Sciences and Research Center,
Bangalore.
on the posterior septal branches of sphenopalatine Corresponding Author:
artery. The pedicle is very stable and provides adequate Dr Harshita V.Sabhahit
supply to the flap ensuring good reconstructive results. #1052, 11th Main, Judicial Layout, GKVK Post,
Bangalore- 560065
In this study we present our experience with
Ph: 9886025627
reconstruction using the Hadad flap for endoscopic Email id: havisa276@gmail.com
Vol.-11, Issue-I, January-June - 2017 37
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
MATERIALS AND METHODS: resected after visualizing internal carotid artery bulge
20 patients who came to our institute with and optico carotid recess. Sella was identified and the
pituitary tumours were operated. Detailed history was floor was thinned out upto the limit of tuberculum
taken and a complete clinical examination including sellae superiorly and cavernous sinuses bilaterally thus
neurological work up, ophthalmological work up and exposing the dura. After placing incision over the dura,
hormonal level evaluation was done. CT scan of nose, the tumour was visualized and resected meticulously
paranasal sinuses and brain with one millimetre cuts in using a two surgeos, two/four handed technique
all planes along with MRI of the brain was done. wherein one surgeon handled the endoscope and a
Informed and written consent was taken from all dissector and the other surgeon provided suction and
patients. The institutional ethics committee approval was held a forceps. After excision of the tumour, the
taken.The procedures were performed by a team of reconstruction was done using surgicel, fascia lata, fibrin
neurosurgeons and otolaryngologists at our institute. glue and flap. The dead space after tumour removal
After intubation and an oropharyngeal pack, the nasal was filled with surgicel, fascia lata was placed in an
mucosal corridor was decongested with cottonoids underlay fashion and then the dural defect along with
dipped in a combination of 4% lignocaine and 1:10,000 sellar floor was covered with Hadad flap sealed with
adrenalines. The nasal septums on either sides or middle fibrin glue. This was followed by packing bilateral nasal
turbinates were infiltrated adequately with 1 in 100,000 cavities with Merocel after ensuring haemostasis. Prior
adrenaline under endoscopic guidance (zero degree, to this, a barrier of gelfoam was created over the flap
4mm wide, and 18cm length). Partial middle so as to prevent misplacement of the graft during nasal
turbinectomy was done in order to visualize superior pack removal. Under the cover of intravenous
turbinate and sphenoidal ostium. The first incision was antibiotics, the nasal pack remained insitu for 3 days.
made at the junction between nasal floor and septum Imaging was done in the form of CT scan with contrast
postero-anteriorly. If a larger defect was expected, the on the first post operative day to check for evidence of
incision was taken more laterally along the floor of the residual tumours. Patients were placed on bed rest with
nose to increase the width of the flap. The second head end elevation of 30 degrees and asked to avoid
incision was made along the inferior most aspect of straining. The pack was removed on the 3 rd post
the sphenoidal opening and advanced superiorly and operative day.
anteriorly, the limit being the septo columellar junction. The patients were followed up after 1 week, 2
Care was not to include the olfactory mucosa and the weeks, one, two , three and six months and one year
dorsal strip of cartilage. The third vertical incision after surgery.
connected to the most anterior aspect of the previous RESULTS:
two incisions. The nasoseptal flap was then elevated
Out of the 20 consecutive patients who were
using an elevator in the mucoperichondrial and
operated, eight were females and twelve patients were
mucoperiostial plane from anterior to posterior
males, with ages ranging from nineteen to sixty two(19-
direction till the posterior choana. A relaxing incision
62yrs.). Most of the patients presented with headache
was made along the arch of the choana to increase the
and diminished vision. 3 patients had
range of rotation. This flap was placed temporarily in
craniopharyngioma, one with Rathkes pouch cyst,
the nasopharynx or the maxillary sinus after rotating
while the rest had pituitary macroadenoma. Patients
so as to prevent damage during tumour removal and
were operated using endoscopic transnasal
to obtain a better access to the tumour site. This was
transsphenoid approach. All the skull base defects were
followed by posterior septectomy. Mucoperiostium of
repaired using Hadad flap and fibrin glue. Fascia lata
the sphenoidal rostrum was elevated bilaterally.
was used in 18 patients in an underlay fashion for added
Widening of the sphenoid ostium was done bilaterally
support to the flap. Intraoperative CSF leak was noted
so as to open the anterior face of sphenoid and gain
on table in 10 patients. Three (15%) of the above patients
access into the sphenoid cavity. Intersinus septum was
who had intraoperative CSF leak had post operative
identified and dissected. Mucosa of the sphenoid sinus
leak too. When re-explored surgically, the Hadad flap
38 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
had misaligned due to loss of alignment between the
bony defect and the flap in two patients. CSF leak
ceased after repositioning the flap. One (5%) of the
patient continued to have CSF leak after replacing flap
Fig.-4: Incisions on superior part of septum and floor.
Fig.-5: Tumour Exposure.
Fig.-1. Preoperative CT images showing Pituitary
tumours.
Fig.-6: Skull base defect after tumour resection.
Fig.-2: Inferior limit of pedicle above choana.
Fig.-3: Superior limit of pedicle below sphenoid os. Fig.-7: Reconstruction with surgicel.
Vol.-11, Issue-I, January-June - 2017 39
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
unanimously considered as the workhorse for closure
of skull base defects and has heralded an era of
vascularised flaps in sealing the skull base defects
following transnasal endoscopic skull base surgeries.
The nasoseptal artery lies within a strip of
mucoperisotium between the inferior margin of the
natural sphenoid ostium and superior edge of the
choanae, thus making these the superior and inferior
limits of Hadad-Bassagasteguy pedicle1,3. The use of this
flap to separate the nasal cavity from intracranial space
Fig.-8: Reconstruction with Hadad flap. minimizes the risk of postoperative CSF leaks,
pneumocephalus and meningitis. The nasoseptal flap is
a versatile flap with a wide arc of rotation that allows
and this had to be strengthened with additional fascia
lata, fat and fibrin glue. In this particular patient the the flap to reach the defects from the frontal sinus to
tumour had invaded the arachnoids membrane. Minimal lower clivus. It has decreased the incidence of CSF
crusting was noted in the immediate postoperative leak significantly.
followup period which may be attributed to the post One of the significant advantages of the nasoseptal
posterior septectomy status. Thus 1 /20 (5%) patients flap is that it can be endoscopically harvested prior to
had late post operative CSF leak in our study. forming a skull base defect, therefore alleviating the
DISCUSSION: need for external flap harvesting. Additionally, being a
The advent of endoscopes has revolutionized a new vascularised flap, it promotes faster healing, lower
era in modern pituitary surgeries. Transnasal, chances of graft migration in addition to providing a
transsphenoidal endoscopic surgeries have become the large surface area to cover larger defects. The nasoseptal
mainstay of management in pituitary and skull base flap is a safe, no cost, malleable, easy to harvest flap in
lesions in the recent past. Transnasal approaches have the same field of surgery without causing any
many advantages over the traditional open transcranial complications or side effects4.
approaches, which includes absence of brain retraction Depending on the dimensions of the nasal septum,
and manipulation, better visualization using endoscopes, HBF flap can extend from the frontal recess anteriorly
lesser post operative morbidity and better cosmesis. to the clivus posteriorly in length and from one lamina
However, it comes with its own complication which papyracea to the other in width. The robust blood
includes a high rate of post operative CSF leakage supply of the flap, pliability and extensive arc of rotation
consequent to large skull base defects after tumour allows the coverage of a wide array of anterior, middle
removal. The introduction of nasoseptal flap famously and posterior cranial base defects3,5.
known as Hadad- Bassagasteguy flap in 20061, a novel Hadad et al1, in their landmark paper, reported a
reconstruction technique based on the pedicle nasoseptal 4.7% rate of post operative fistula based on a study on
flap with blood supply from posterior septal branch 43 patients which included 20 cases of pituitary macro
of sphenopalatine artery, a terminal branch of the adenomas. Kassam3 et al demonstrated a 10.66% rate of
internal maxillary artery, has been the most significant post operative CSF fistula in patients who required intra
advance in transnasal endoscopic surgeries. This arachnoid dissection and also pointed out that, there
technique was earlier devised by Oskar Hirsh in 19522, was a learning curve associated with the success of HBF.
but it was based on random vascular supply. Ever since In our study including 20 cases, there was a persistent
the reintroduction of a modified, robust nasoseptal flap post operative CSF leak of 5%, which is consistent with
based on the posterior septal artery, it has been the results obtained in similar contemporary studies.
40 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
In addition to adequate exposure and complete extranasal flaps include palatal flap, pericranial flap, and
resection of the lesion, the outcome of endoscopic facial buccinator flap and temporoparietal fascial flap14.
surgery depends largely on the ability to reconstruct CONCLUSION:
the skull base defects. Smaller skull base defects can be
Hadad - Bassagasteguy flap is a reliable method in
sealed with materials like fat, fascia lata, middle turbinate
repairing skull base defects after transnasal
mucosa etc6. However, due to expansion of the horizon
transsphenoidal skull base surgeries in conjunction with
of endoscopic surgeries to the extent of resecting larger
multilayered reconstruction. Its use has considerably
lesions and the consequent larger skull base defects, the
reduced incidences of post operative CSF leaks even
need for self sustaining flaps arises and this is addressed
after large skull base defects and plays a pivotal role in
adequately by the nasoseptal flap. The average surface
endoscopic skullbase surgeries.
area of HBF is approximately 25cm2.7The flap is tailored
DISCLOSURES:
the size of the defect expected, although it is wise to
overestimate the size and later resect the excess flap if (a) Competing interests/Interests of Conflict- None
necessary. (b) Sponsorships - None
Many authors4,8 emphasize on the need for using (c) Funding - None
a multilayered approach to reconstruction , even while (d) No financial disclosures
using a vascularised flap in order to support the flap, (e) Animal rights-Not applicable
to help it remain fixed and reduce the effect of
REFERENCES:
cerebrospinal fluid. Most importantly, it must be
ensured that the flap must not be twisted during 1. Hadad G, Bassagasteguy L, Carrau RL, et al. A
reconstruction and the mucosal surface is facing the novel reconstructive technique after endoscopic
nasal cavity and not the intracranial defect and that the expanded endonasal approaches: Vascular pedicle
flap is covering the bony edges of the defect. nasoseptal flap.Laryngoscope 116:1882-1886,2006.
Advance planning is of paramount importance as 2. James K.Liu , Richard F. Schmidt, Osamah J et
posterior septectomy during transsphenoidal surgery al. Surgical nuances for nasoseptal flap
can hamper its usage because of destruction of the reconstruction of cranial base defects with high
vascular pedicle9. Addressing this issue, Rivera Serrano flow cerebrospinal fluid leaks after endoscopic
et al developed nasoseptal rescue flap (NSRF)5, in which skull base surgery.Neurosurg Focus 32(6):E7,2012.
HBF is only partially raised ,permitting access to the 3. Kassam AB, Thomas A, Carrau R, et al.
anterior face of the sphenoid avoiding injury to the Endoscopic reconstruction of the cranial base using
feeding vessels. If there is an intraoperative CSF leak, a pedicled nasoseptal flap. Neurosurgery. 2008
the NSRF can be completely harvested and converted Jul;63(1 Suppl 1):ONS44-52; discussion ONS52-
to HBF. His observation was further supported by 3. doi: 10.1227/01.NEU.0000297074.13423.F5.
Rawal RB et al10 who in their study stated that the 4. Wang Xuejan, Hu Fan, Zhang Xaobao, Yu
success rate of nasoseptal flap was 100%. Yong et al. Endonasal Endoscopic Skull Base
Other endonasal pedicled flaps that could be used Multilayer Reconstruction Surgery with Nasal
in cases where HBF is contraindicated consequent to Pedicled Mucosal Flap to Manage High Flow
the compromised vascular supply are posterior inferior CSF Leakage. Turkish Neurosurgery 2013;23( 4):
turbinate flap based on inferior turbinate artery11, 439-445.
middle turbinate flap12 based on middle turbinate artery 5. Riverra Serrano CM, Synderman CH, et al. The
which are both branches of posterior lateral nasal artery posterior pedicle inferior turbinate flap:A new
and lateral nasal wall flap (HB2)13 flap based on branches vascularized flap for skull base reconstruction.
of facial and anterior ethmoidal arteries. Pedicled Laryngoscope. 2007;117:1329-1332.
Vol.-11, Issue-I, January-June - 2017 41
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
6. Neto CDP, Pinheiro SD.Use of Pedicled Flaps 13. Hadad G, Rivera Serrano CM, , Bassagasteguy LH
for Skull Base Reconstruction after Expanded et al. Anterior pedicle lateral nasal wall flap: a
Endonasal Approaches. Int.Arch. Otorhin- novel technique for the reconstruction of anterior
olaryngol. 2007;11(3):324-329. skull base defects.Laryngoscope.2011 Aug;
7. Pinheiro- Neto CD, Prevedello DM, Carrau RL 121(8):1606-10. doi: 10.1002/lary.21889.
et al.Improving the design of pedicled nasoseptal 14. Camilo Reyes,Eric Mason et al. Panorama of
flap for skull base reconstruction:a radioanatomic reconstruction of skull base defects: from
study.Laryngoscope 2007 Sep;117(9):1560-9. traditional open to endonasal endoscopic
8. Cavallo LM, Messina A, Esposito F et al. Skull approaches, from free grafts to microvascularflaps.
base reconstruction in the extended endoscopic Int. Arch. Otorhinolaryngo l.2014Oct; 18(suppl
transsphenoidal approach for suprasellar lesions.J 2):S179-86.
Neurosurg. 2007 Oct;107(4):713-20.
9. Joseph Brunworth, Tina Lin, David b Keschner
et al. Use of Hadad Bassagasteguy flap for repair
of recurrent cerebrospinal fluid leak after prior
transsphenoidal surgery.Allergy and Rhinology (
Providence). 2013 Fall;4(3): e155-e161. doi:
10.2500/ar.2013.4.0072
10. Rawal RB, Kimple AJ ,Dugar DR et al.
Minimizing morbidity in endoscopic pituitary
surgery:outcomes of the novel nasoseptal rescue
flap technique.Otolaryngol Head Neck Surg2012
Sep;147(3):434-7.
11. Fortes FS, Carrau RL, Synderman CH et al. The
posterior pedicle inferior turbinate flap: a new
vascularized flap for skull base reconstruction.
Laryngoscope 2007Aug; 117(8):1329-32.
12. Prevedello DM, Barges Coll J, Fernandez-
Miranda JC et al. Middle turbinate flap for skull
base reconstruction: cadaveric feasibility
study.Laryngoscope 2009 Nov;2094-8. doi:
10.1002/lary. 20226.
42 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
AN ANALYSIS OF INSIDE OUT MASTOIDECTOMY WITH
TYMPANOPLASTY WITH OR WITHOUT OSSICULOPLASTY FOR
MANAGEMENT OF MIDDLE EAR CLEFT CHOLESTEATOMA
*Chandra Manish, **Rajeev Krishna Gupta, ***Satveer Singh Jassal, ****Sikhar Saxena
HOW TO CITE THIS ARTICLE Date of receipt of article -9-1-2017
Chandra Manish, Gupta R K, Jassal S S, Saxena S. An analysis of
inside out mastoidectomy with tympanoplasty with or without Date of acceptance 21-02-2017
ossiculoplasty for management of middle ear cleft cholesteatoma. DOI- 10.21176/ojolhns.2017.11.1.7
Orissa J Otolaryngology & Head & Neck Surgery 2017 June; 11(1):
43-48. DOI: 10.21176/ojolhns.2017.11.1.7 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.7
ABSTRACT:
AIMS: To evaluate the advantages and shortcomings of inside out mastoidectomy with tympanoplasty with or
without ossiculoplasty for management of middle ear cleft cholesteatoma.
Material and Methods: It is a Prospective Observational study. 40 patients of chronic otitis media with
cholesteatoma in the age group of 10 years to 50 years who underwent inside out mastoidectomy were included
in the study. Reconstruction was done with autologus ossicle, PORP or TORP as required. Temporalis fascia
graft was placed over the assembly.
Results: 21(52.5%) patients had attic cholesteatoma, 17(42.5%) had postero-superior retraction pocket and 2
(5%) patients had both attic cholesteatoma and postero-superior retraction pocket on otoscopic examination.
During follow up 2 patients (5%) had persistent ear discharge within 6months of surgery and 2 patients (5%)
developed ear discharge after 7 months and 1 year after surgery. Recurrence rate was 10%.The mean gain in air
conduction was 16.2dB.
Conclusion: By this study it can be concluded that inside out mastoidectiomy provides advantages over both
outside in canal wall down mastoidectomy and intact canal wall mastoidectomy.
Keywords: Cholesteatoma, Canal wall down mastoidectomy, canal wall up mastoidectomy, inside out technique.
INTRODUCTION: associated with higher recidivism rate than canal wall
Surgical management of cholesteatoma has down mastoidectomy due to poor visualization and
underwent numerous changes since the 1st published Affiliation:
report of mastoidectomy 350 yrs ago by Schwartze and * Assistant Professor,
Eysell who popularized Cortical mastoidectomy in year **,*** & **** Resident,
Department of ENT,
1873. Radical mastoidectomy was described by Zaufal Eras Lucknow Medical College, Lucknow,
in 18901. Bondy revised this Technique2. With the Uttar Pradesh,India-226003
advent of operating microscope, mastoidectomy Address of Correspondence:
underwent further refinement. At present debate Dr. Rajeev Krishna Gupta,
Department of ENT
between canal wall up and canal wall down Eras Lucknow Medical College.
mastoidectomy is ongoing 3 . Canal wall up Sarfrazganj, Hardoi road, Lucknow
Uttar Pradesh,India-226003
mastoidectomy provides good hearing outcome and is +919506890745
not associated with mastoid cavity problem but it is Email: dr.rajeevgupta11@gmail.com
Vol.-11, Issue-I, January-June - 2017 43
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
increased chances of postoperative retraction pocket after discharge from hospital, then after 3, 6, 12,
formation4. Canal wall up mastoidectomy is not a 18months, and in between if required.
suitable option in situations like extensive disease, low Surgical Tehnique:
lying dura, disease in a well pneumatised mastoid,
A Post auricular approach was used in all the
anterior placed sigmoid or a cleft palate. In these
patients. Meatotomy was performed and microscopic
situations canal wall down procedure is the surgery of
findings were noted. Tympanomeatal flap was elevated
choice5. Recurrence of cholesteatoma and occurrence
and ossicular status was checked. Inside out
of postoperative retraction pocket is low in canal wall
mastoidectomy was started with the widening of EAC
down mastoidectomy due to good intraoperative
followed by drilling of outer attic wall. Drilling was
exposure.
continued posteriorly depending on the extent of
Canal wall down mastoidectomy allows better cholesteatoma sac. Cholesteatoma sac was removed along
visualization, greater confirmation of cholesteatoma with granulations. Drilling was stopped once the
eradication and lower rate of recurrence than canal wall healthy mucosa was seen(Fig 1). When cholesteatoma
up mastoidectomy but at the cost of need for a lifelong extended beyond the aditus canal wall down
cavity care 6,7,8. Canal wall down mastoidectomy can be mastoidectomy was performed. Sinus tympani region
approached either through outside in or inside out was inspected by drilling the posterior canal wall upto
technique. the level of base of pyramid, to look for hidden
Inside out mastoidectomy is performed through cholesteatoma, which was subsequently removed. Incus
trans-meatal route via retro auricular or endaural along with head of malleus and occasionally whole
approach. There has been very few published studies malleus was removed to facilitate eradication of disease
on the technique and surgical outcomes after inside out from anterior attic.
mastoidectomies.Our study gains importance as we have Reconstruction:
analyzed 40 cases of inside out mastoidectomy with a
Reconstruction was done with autologus ossicle,
minimum follow up period of 1.5 yrs in homogenous
PORP or TORP as required. Reconstruction was done
study condition.
in same sitting. Incus long process was drilled and a
MATERIAL AND METHODS: groove was created with a diamond burr on the body
This is a prospective observational study carried to accommodate the capitulum of stapes. The short
out at Eras Lucknow Medical College, Lucknow process was placed under the malleus long process to
between May 12 to May 15. 40 patients of chronic complete the ossicular continuity. When the stapes
otitis media with cholesteatoma in the age group of suprastructures were absent incus was refashioned and
10years to 50 years who underwent inside out placed over the stapes footplate. Conchal cartilage was
mastoidectomy during this period were included in used to construct the attic and posterior canal
study. wall.Temporalis fascia graft was placed over the
Otomicroscopic findings, preoperative pure tone assembly. Meatoplasty when required was done.
audiometry were noted, HR C.T. temporal bone and Analyzed Parameters:
middle ear cleft was done in all the patients. All the We analyzed the intraoperative advantages and
patients were operated by single surgeon. All the disadvantages, postoperative hearing status, recidivism
patients were operated under general anesthesia. All the of cholesteatoma, complications and postoperative
patients were admitted and 1 dose of injection healing of cavity.
ceftriaxone was given prior to surgery, postoperatively
RESULTS:
injection ceftriaxone was continued for 3 days and then
patients were kept on oral medications. Sutures were Of 40 patients included in study 24(60%) were
removed on 7th post operative day. male and 16(40%) were female(Table-1) with mean age
24.8 years (range10-50 years)(Table-2) .21 patients had
Patients were followed up for minimum period
attic cholesteatoma, 17 had posterosuperior retraction
of 1.5 years. Follow up were done at 1st, 2nd, 3rd week
pocket and 2 patients had both attic cholesteatoma and
44 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
posterosuperior retraction pocket on otoscopic
examination(Table-3). Otorrhoea was present in
39(97.5%) cases. Hearing loss was present in all cases.
1(2.5%) case presented with only hearing loss. Extent
of disease as revealed during surgery was as
follows.Cholesteatoma was limited to tympanum in 14
patients while in 26 patients it extended to mastoid.
Ossicles were eroded in 30 patients. Long process of
incus was eroded in 20 patients, body of incus in 6
patients, stapes suprastructure was eroded in 12 patients
and malleus was eroded in 4 patients. Tympanic sinus
was involved in 14 patients and disease extended Fig.-1: Mastoid cavity after completion of inside out
anteriorly to Eustachian tube in 4 patients. mastoidectomy.
Ossicular reconstruction was performed in 30 cases
using remodeled incus (n=17), malleus head (n=4), Table-1: Distribution of patients according to sex
partial ossicular reconstruction prosthesis (n=6)
(PORP)or total ossicular replacement prosthesis (
n=3)(TORP).
Post operative complications:- Postoperative
transient vertigo in 4 patients and postoperative
transient facial palsy observed in 3 patients. All cases Table-2: Distribution of according to age group:
were followed up for a minimum period of 1.5 years.
A dry and trouble- free ear was found in 36 (90%)
patients in follow-up.
Complications during follow-up period (Table-
4) were as follows-
(a) 2 patient had persistent ear discharge.(5%)
(b) 2 patient developed ear discharge after follow up
period of 7months and 1 year respectively. (5%)
(c) 1 patient developed perichondritis postoperatively. Table-3: Distribution of patients according to otoscopic
(2.5%) findings:
(d) 2 patient had temporalis fascia graft infection.(5%)
Maximum patients achieved a dry cavity in 3
months time duration (Table-5). The postoperative
hearing assessment was done 6 months after surgery
(Table-6). In 4 Patients(10%) postoperative air
conduction gain was between 21-30 dB, in 11
patients(27.5%) it was between 10-20 dB, in 19(47.5%)
it was less than 10 dB. In 6 patients (15%) there was no
gain in air conduction. The mean hearing gain was 16.2
dB. In none of the patient deterioration in hearing status
was noted. The mean preoperative bone conduction
was 13.16 dB and remained unchanged postoperatively
at six months after surgery.
Vol.-11, Issue-I, January-June - 2017 45
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Table-4: Post operative Complications. Cholesteatoma itself is a morbid condition. The
surgical management of cholesteatoma also results in
detoriation of quality of life because of mastoidectomy
cavities which require lifelong care from moisture and
cleaning by trained personal.
Closed technique for management of
cholesteatoma entails preservation of posterior wall of
EAC but at cost of risk for recurrence of cholesteatoma
due to limited intraoperative exposure and occurrence
of post operative retraction pocket. Second stage
surgery is frequently recommended 9-12 months after
the initial surgery4,11. Canal wall down mastoidectomy
provides good exposure and lower recidivism rate but
at the cost of lifelong mastoid care. Inside out
Table-5- Time of drying of cavity. mastoidectomy provides the advantages of both canal
wall down and canal wall up technique12,13. In our study
40 patients of chronic otitis media with cholesteatoma
were managed with inside out mastoidectomy. All the
patients were followed for a minimum period of 1.5
years. A dry and trouble free ear was found in 36
patients (90%) which is similar to previous studies13,14,15.
2 patient developed persistent ear discharge within 6
months of surgery and 2 patient developed ear discharge
after 7 months and 1 year after surgery. We defined
Note: 4 patients had persistent discharge posoperatively.
residual disease as persistent ear discharge starting within
Table-6: Post op hearing status at 6 months. 6 months of surgery and recurrent disease as persistent
ear discharge after 6 months of surgery. HRCT was
done at end of 6 months to look for cholesteatoma and
differentiate between residual and recurrent disease.
Residual disease was due to incomplete removal of
cholesteatoma during surgery and recurrent disease was
due to new cholesteatoma formation because of
persistence of predisposing factors. Both residual and
recurrent diseases were designated as recidivism. A total
of 4 patients developed persistent ear discharge after
DISCUSSION: surgery making recidivism rate 10% which is in
The 1st published description of cholesteatoma accordance with previous literature16,17,18,19,20.
dates back to 16th century when Duverney described it This study elucidates the advantages of inside out
to be abscess of bone originating from auditory canal9. mastoidectomy. Intraoperative advantages included
Cholesteatoma can be defined as cystic lesion formed early identification of ossicles, facial nerve, lateral
from keratinizing stratified squamous epithelium, the semicircular canal and dural plate. Surgery could be
matrix of which is composed of epithelium that rests stopped once the healthy bone is encountered thus
on stroma of varying thickness, the perimatrix9.Its reducing the size of the cavity as compared to outside
incidence can be upto 10% in people of chronic in canal wall down mastoidectomy, where cavity size
suppurative ottitis media.There has been statistically is usually large. Facial recess could be explored more
significant decline in the incidence of cholesteatoma10. easily and early in the procedure. Limited size of cavity
46 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
favored easy reconstruction. A chance of injury to 4. Ethical approval: All procedures performed in
lateral semicircular canal, dural plate and sigmoid sinus studies involving human participants were in
plate is minimal because of early identification of accordance with the ethical standard of institution.
important landmarks. Ability to deal with Korners REFERENCES:
septum is better as the aditus and lateral semicircular
canal comes into the operating view early in the surgery. 1. Bennett M, Warren F, Haynes. Indications and
Reduced cavity size favors small meatoplasty which technique in mastoidectomy. Otolaryngol Clin
looks cosmetically better. Maximum patients had a dry North Am. 2006 Dec;39(6):1095-113.
cavity within 3 months time duration which is better 2. Shambaugh G E, Glasscock MEIII: Surgery of the
than those stated in literature21. Postoperative air ear, ed 3. Philadelphia, 1980, WB Saunders Co,
conduction gain 6 months after surgery was between pp 248249. Google Scholar
10-30 dB in 15 patients and in 19 patients it was less 3. Syms MJ and Luxford WM. Management of
than 10 dB. In 6 patients preoperative and 6 months cholesteatoma: status of the canal wall.
postoperative air conduction was same. Postoperative Laryngoscope.2003;113(3):443448.
hearing gain in this study was better than that stated in
studies of conventional mastoidectomy, this can be due 4. Sanna M, Zini C, Scandellari R, Jemmi G .Residual
to small cavity size and ease of reconstruction 22,23,24. It recurrent cholesteatoma in closed tympanoplasty.
is a technically demanding surgery and should be Am J Otol. 1984;;5:277-82.
practiced after doing good number of temporal bone 5. Abramson M. Open or closed tympanoma-
dissection. The results of inside out mastoidectomy are stoidectomy for cholesteatoma in children. Am J
similar to outside in mastoidectomy but intraoperative Otol.1985; 6:167-9.
and postoperative advantage gives this technique an edge 6. Khalil HS,Windle-Taylor PC . Canal wall down
over the outside in technique. mastoidectomy:A long term commitment to the
CONCLUSION: outpatients. BMC Ear, Nose and Throat
It can be concluded that inside out mastoidectiomy Disorders.2003 December;3:1.doi. 10.1186/1472-
provides advantages of both outside in canal wall down 6815-3-1.available at link.springer.com/article/
mastoidectomy and canal wall up mastoidectomy. By 10.1186/1472-6815-3-1.
this approach both eradication of disease and minimal 7. Quaranta A, Cassano P, Carbonara G.
disturbance to functional status of ear can be achieved. Cholesteatoma surgery: open versus closed
Because of early identification of landmarks chances of
tympanoplasty. Am J Otol. 1988 May; 9(3):
injury to vital structures are less. For limited
229-31.
cholesteatoma this approach provides the clear
advantage of being minimally invasive. Postoperative 8. Sheehy JL.Cholesteatoma surgery. Canal wall
cavity related problems are less, hearing status is better down procedure. Ann Otol Rhinol Laryngol.
compared to outside in mastoidectomy. 1988;97:30-5.
Aknowledgement: 9. Semaan M T, Megerian CA .The pathophysiology
Article was presented at AIIMS, in Otology of cholestetoma. Otolaryngologic Clinics of
workshop and conference, New Delhi, India, held North America.2006;39( 6):11431144.
between 3rd -5th September 2015. 10. Djurhuus BD, Faber CE, and Skytthe A.
DISCLOSURES: Decreasing incidence rate for surgically treated
1. Funding: There is no source of funding for this middle ear cholesteatoma in Denmark 19772007.
study. Danish Medical Bulletin.2010; 57( 10):1-5. Article
ID A4186.
2. Conflict of interest: The authors declare that they
have no conflict of interest. 11. Hirsch BE, Kamerer DB, Doshi D . Single stage
3. Informed consent: Informed consent was taken management of cholesteatoma. Otolaryngol Head
from every patient. Neck Surg.1992; 106(4): 351354.
Vol.-11, Issue-I, January-June - 2017 47
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
12. Dornhoffer JL. Retrograde mastoidectomy. canal wall tympanoplasty in the management of
Otolaryngologic Clinics of North America.2006; cholesteatoma. Laryngoscope. 1976; 86:16391657.
39( 6) :11151127. doi: 10.1288/ 00005537- 197611000-00005.
13. Roth TN,Haeusler R.Inside-out technique [PubMed] [Cross Ref].
cholestetoma surgery:A retrospective long -term 20. Mahadeviah A, Parikh B.Modified intact canal wall
analysis of 604 operated ears between 1992 and mastoidectomy-long term results in hearing and
2006.Otology and neurotology. 2008;30:59-63. healing.Indian J otolaryngol Head Neck Surg.2008;
14. Godinho RA, Kamil SH, Lubianca JN, Keogh 60(4): 317-323.
IJ, Eavey RD. Pediatric cholesteatoma: canal wall 21. Singh M, Jain S, Rajput R, Khatua R, Sharma D.
window alternative to canal wall down Retrospective and prospective study of singapore
mastoidektomie. Otol Neurotol. 2005;26:466-71. swing method on healing of mastoid cavity . Indian
15. Mukherjee P, Saunders N, Liu R, Fagan P . Long- J Otolaryngol Head Neck Surg. 2010 Oct; 62(4):
term outcome of modified radical mastoidectomy. 365371. Published online 2011 Jan 4.
J Laryngol Otol. 2004;118:612-6. doi: 10.1007/s12070-010-0058-9.
16. Schimd H, Dort JC, Fisch U . Long-term results 22. Artuso A, Nardo W, Corso E, Marchese MR,
of treatment of childrens cholesteatoma. Am J Quaranta N .Canal wall down tympanoplasty
Otol. 1991;;12:83-7. surgery with or without ossiculoplasty in
cholesteatoma: hearing results. Acta
17. Dornhoffer JL.Retrograde mastoidectomy with
otorhinolaryngol Ital 24, 2-7, 2004.
canal wall reconstruction: a follow-up report. Otol
Neurotol. 2004 Sep;25(5):653-60. 23. Cook JA, Krishnan S, Fagan PA Hearing results
following modified radical versus canal-up
18. Vadiya S, Kedia Anuja . Atticotomy, attic
mastoidectomy. Cook J A Krishnan S Fagan P
reconstruction, tympanoplasty with or without
A Hearing results following modified radical
ossiculoplaty, canalplasty and cortical
versus canalup mastoidectomy Ann Otol Rhinol
mastoidectomy as part of intact canal wall
Laryngol 1996. May;105537983. [PubMed]
technique for attic cholestetoma. Indian J
Otolaryngol Head Neck Surg. 2015 Jun; 67(2): 24. Berenholz LP, Rizer FM, Burkey JM, Schuring
128131.Published online 2015 Jan AG, Lippy WH. Ossiculoplasty in canal wall
9. doi: 10.1007/s12070-015-0821-z. down mastoidectomy.Otolaryngol Head Neck
Surg. 2000 Jul;123(1 Pt 1):30-3.
19. Glasscock ME, Miller GW . Intact canal wall
tympanoplasty in management of cholesteatoma.
Laryngoscope Glasscock ME, Miller GW. Intact
48 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
4 HANDS REACHING OUT ENDOSCOPICALLY TO THE
PITUITARY OUR EXPERIENCE
*G Sundhar Krishnan, **George Nitha Mary
HOW TO CITE THIS ARTICLE Date of receipt of article -10-10-2016
G Sundhar Krishnan, George N M.4 hands reaching out Date of acceptance 21-02-2017
endoscopically to the pituitary our experience. Orissa j
otolaryngology head neck surgery 2017 June; 11(1): 49-53. DOI: DOI- 10.21176/ojolhns.2017.11.1.8
10.21176/ojolhns.2017.11.1.8 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.8
ABSTRACT:
Objective: To examine three minimally invasive techniques of approaching the sella in pituitary tumors.
Study design: Retrospective case review of patients out of whom 275 patients were underwent Endoscopic
endonasal pituitary adenoma resection and rest by conventional methods between January 1996 and October
2016.
Patients: 500 cases of pituitary adenoma requiring surgical intervention were included in the study and thoroughly
investigated prior to surgical intervention. The various techniques of endoscopic hypophysectomy have been
compared in this study.
Main outcome Measure (S): Remission was defined as no radiological or hormonal evidence of recurrence
within the time-frame of the follow-up.
Results: 10% recurrence was noted at the end of 1 year- 5% in Trans septal trans sphenoidal, 3% in Trans
sphenoidal and 2 % by the 4 hand technique, which were re-operated successfully by the endoscopic trans
sphenoidal 4 hand technique. Mean follow-up period was 24.2 months.
Conclusions: In our 20 yrs of experience, endoscopic trans sphenoidal 4 handed technique is a safe and effective
method for complete pituitary tumor removal with better surgical outcomes and fewer complications compared
to the trans septal trans sphenoidal technique
Keywords: Endoscopic hypophysectomy, Four hand technique, Trans sphenoidal.
INTRODUCTION:
precise delineation of the sellar mass from its
Horseley (1906) was the first to decompress the
surrounding structures ensuring comprehensive tumor
pituitary gland by the transcranial route1. In 1909,
Cushing performed the sub labial trans septal approach.
Affiliations:
Chiari was credited for his demonstration of the trans
*Director & Chief ENT Surgeon,
ethmoidal trans sphenoid operation in 1912. By early **Junior ENT Consultant,
1980s trans sphenoidal approach came to stand.With Krishna Eye and ENT Hospitals,
No 39, Burkitt road, T Nagar, Chennai-600017
the advent of modern endoscopic techniques, the Tamil Nadu
momentum in the field of endoscopic pituitary surgery Address for correspondence:
has steamed up providing panoramic view, superior Prof (Dr) G Sundhar Krishnan,
visualization of microscopic relevant anatomy, better Krishna Eye and ENT Hospitals,
No 39, Burkitt road, T Nagar,
magnification and illumination for identification of Chennai-600017,Tamil Nadu
critical anatomical landmarks within the sphenoid and Phone-no:9500040702.
Vol.-11, Issue-I, January-June - 2017 49
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
removal with favorable results and reduced Extensive lesions:
postoperative morbidity 3 . In addition, angled Anterior to tuberculum over the planum
endoscopes allow tumor remnants extending into the sphenoidale
supra and parasellar areas to be seen improving the
Behind the clivus into the posterior fossa
surgeons ability to achieve complete tumor resection
reducing the likelihood of recurrence4. An added AIM & OBJECTIVE:
advantage in endoscopic approaches is the possibility To compare three minimally invasive techniques
of a 4 hand technique for faster & accurate dissection of approaching the sella in pituitary tumors and
by appropriate retraction and prompt hemostasis in a conclude on the most conducive option for best patient
magnified surgical field as against the single hand results.
endoscopic or 2 hand microscopic technique5.
MATERIALS AND METHODS:
Endoscopic pituitary surgery is a well-established
A long-term retrospective study was done in
technique for the treatment of sellar tumors. The
patients who underwent Endoscopic Endonasal
efficacy and minimally invasive nature of Trans nasal
pituitary adenoma resection between January 1996 and
endoscopic approach in the treatment of pituitary
October 2016. The data in patient records as well as
adenomas and other sellar lesions have provided a
benchmark to ambitious skull base surgeons6. the data obtained from postoperative follow-up visits
were used to determine outcomes. From a total of 500
Pituitary adenomas can present in any age equally
pituitary adenomas, (75)15% were hormonally active,
affecting males and females. The clinical presentation
while (425)85 % were non-functioning. The male to
of pituitary adenomas varies depending upon the
location and severity of the tumor. Pituitary adenomas female ratio was 1: 1.5 (Male200:Female300), with
are a diverse group of benign neoplasms. The average age group 35-50 years. In our 500 patints we
hormonally inactive, generally come to clinical attention have operated 10(2%) patients by trans- septal trans-
secondary to local mass effect or pituitary deficiency. sphenoidal approach and in the 215(43%) by trans-
Whereas, the hormonally active tumors present with sphenoidal technique and in 275(55%) of them (2005
well-recognized syndromes and include growth onwards) were by the 4 hand technique.
hormone adenoma, prolactinoma, and corticotrophin Detailed notes on history of Headache, visual
adenoma7. symptoms, amenorrhea, galactorrhea, general physical
Indications for endoscopic hypophysectomy8: examination (Acromegalic features), CNS examination,
Tumor with mass effect (Macro adenoma: > 1cm) complete ophthalmic and ENT examination, from the
Chiasmal compression and objective visual field records were taken. Patients were subjected to various
defect imaging studies. The CT scan gave invaluable
information of the bony surgical anatomy of the nose
Raised intracranial pressure Pituitary dependent
and sphenoid sinus whilst the MRI was extremely useful
Cushings disease GH secreting tumor.
for parasellar and vascular information. Hormonal
Prolactinoma
assays like LH, FSH, T3 T4 TSH, Prolactin, GH and
Failure of medical of treatment cortisol were done in patients suspected to have
Intolerance of medical management secreting tumors.
Patient preference Surgery was indicated whenever there was
TSHoma evidence of compressive gland enlargement or
Contraindications for endoscopic development of pituitary hormonal imbalances. The
9
hypophysectomy : first 10 patients were operated using the trans- septal
Highly vascular lesion trans-sphenoidal approach and the rest by trans-
Lesions with carotid artery anomaly, where the sphenoidal technique, of which around 275 patients
artery project into the sphenoid sinus and limit safe (2005 onwards) were by the 4 hand technique in trans-
access. sphenoidal technique. The average length of hospital
50 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
stay (LOS) was 1.5 days. Postoperatively, magnetic positioned over the anterior face of the sella. The
resonance imaging (MRI) was done after 1 month to sphenoid sinus is packed with gelfoam. A small merocel
assess residual or recurrent disease and those with sponge is placed in nose. Pack removal was done after
hormonally active tumors had hormonal studies. 24 hours of surgery.
Surgical Technique: In case of a CSF leak, we followed a 3 layered
Following general anaesthesia, the nasal cavities technique wherein the defect was identified and fascia
were decongested with nasal packs of 4% xylocaine with lata graft was first placed with the edges tucked under
1 in 10,000 units adrenaline. The approach could be the dural opening and reinforced with Hadad flap,
done by a Modified four handed technique without fibrin glue and Merocel allowing pressure on the fascia
the active participation of a neurosurgeon where in the during healing which was to be removed after 1week.
Chief Endoscopic ENT surgeon holds the endoscope If the CSF leak was profuse, a lumbar drain was inserted
and one instrument and Assistant ENT surgeon aided postoperatively for 2 to 3 days.
through both nostrils for retraction, irrigation, Patient wass discharged from hospital on the 1st
suctioning etc. offering a bloodless field which would postoperative day and reviewed after 1 week.
aid in finer dissection for tumor removal. Postoperative MRI scan was done 1 month after surgery
The endoscope was advanced to expose the and followed up MRI after 1 year.
anterior wall of the sphenoid sinus in the
sphenoethmoidal recess and ostia identified on both Table-1: Clinical symptoms.
sides. Posterior septal branch of sphenopalatine artery
cauterized bilaterally. Bilateral posterior
ethmoidectomy and posterior septectomy were done
for better visualization and to accommodate various
instruments used in 4 hand technique. Bilateral
sphenoid ostia widened and connected using a
Kerrisons punch till the entire extend of the sphenoid
sinus was well visualized (floor, sellar, planum, optic
nerve and carotid artery bulge, opticocarotid recess
medial and lateral). Intersphenoid septum and sphenoid
mucosa were removed for better access to the anterior
wall of sella whose thickness was assessed with a ball RESULTS AND DISCUSSION:
probe and drilled using a long diamond coarse cutting From a total of 500 pituitary adenomas,(75)15%
burr up to the dura. A horizontal H shaped incision is were hormonally active, while (425) 85 % were non-
made over the dura and dural flap raised. A punch functioning. The male to female ratio was 1: 1.5
biopsy was taken from the prolapsed tumor mass for (Male200:Female300), with average age group 35-50
frozen section histopathology. Blunt ring curettes and years.
2 suctions were used to remove the tumor completely In our study, majority of patients had presented
in a systematic manner, usually starting from the floor, with headache (60%) followed by visual symptoms
then laterally and finally along the supra sellar (25%), acromegalic features (10%) and Cushings disease
component with the help of 30-degree endoscope, (5%) (Table 1). On further evaluation, 85 % were found
thereby eliminating sources of any potential tumor to be non-secreting and 15% secreting in natured as
recurrence. In case of solid tumors, sharp dissection compared to a study done in 300 patients by Kabil MS
was carried out using scissors and tumor removed with et al, who observed that 46 % were hormonally active
the help of forceps until the diaphragm descends freely and 54 % were non-functioning2. Paolo Cappabiancag
with no attachments. et al in their study on 30 patients observed secreting or
In case of bleeding, surgicel was used within the functioning adenomas in 53. 33% and non functioning
sella for hemostasis. The preserved dural flap is adenomas in 46.67%1. In this respect our study is
Vol.-11, Issue-I, January-June - 2017 51
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
30 patients1. DHaens J et al observed that there is not
much significant hormonal improvement in either
endoscopic endonasal surgery or the traditional
microscopic techniques 6 . They reported the
endocrinologic outcome in 2 series of patients at the
same institution using these 2 different techniques6..
The remission rate for the pituitary adenomas in 4 hand
technique was 90 % ( in 248 patients out of 275 patients).
Fig.-1: Pre and post-operative (1yr) MRI of a patient with
DHaens J et al observed remission rate of 63% in
pituitary macro adenoma. endoscopic group and 50% in microscopic group
however they did not mentioned about any 4 hand
techniques and they operated in 60 hormonally active
patients6. Kabil MS et al reported better results as far
as complications are concerned in endoscopic
approaches in comparision to conventional microscopic
approaches 2. However they concluded that more
complete tumor removal is necessary in reducing
complications.We encountered CSF leak in 10 % cases
(28) in 4 hand tchnique which was repaired successfully
by the 3-layer technique. The morbidity with the
endoscopic technique was reported to be higher in
Fig.-2: Chart showing types of surgery adopted. respect to the rate of postoperative CSF leaks (10%)
in the study by DHaens J et al6.
significantly different. In our 500 patints we have In our experience, adopting the endoscopic 4 hand
operated 10(2%) patients by trans- septal trans- technique offers the best approach to the pituitary by
sphenoidal approach and in the 215 (43%) by trans- providing excellent magnification, angular visualization,
sphenoidal technique and in 275 (55%) of them (2005 supra and para sellar tumour access. We noted not just
onwards) were by the 4 hand technique. P Cappabianca a marked reduction in complications but also an
et al in their study in 30 patients 10 surgeries were improved outcome was evident with the above
done by endoscopic endonasal transsphenoidal technique. approach are: less traumatic, faster,
approach and 20 were done by traditional transnasal panoramic magnified view, increased exposure, angled
transsphenoidal approach (TTA)1. Remission was view with the use of different endoscopes, absence of
defined as no radiological or hormonal evidence of skin incisions- brain retraction - cranial nerve dissection
recurrence within the time-frame of the follow-up and possibility to explore the sella for residual tumor
period. In our series 10% recurrence was noted at the at the end of operation. Its disadvantages are the lack
end of 1 year (1% in Trans septal trans sphenoidal, 5% of 3D view and the need for an assistant to hold the
in Trans sphenoidal and 4 % by the 4 hand technique), endoscope10. In our 20 yrs of experience, endoscopic
which were reoperated successfully by the endoscopic trans sphenoidal 4 handed technique is a safe and
trans sphenoidal 4 hand technique. Our Mean follow- effective method for complete pituitary tumor removal
up period was 24.2 months. Mean follow-up period with better surgical outcomes and fewer complications
was 38.2 months in study of Kabil MS et al2. Paolo compared to the trans septal trans sphenoidal technique.
Cappabianca et al followed up their patients after 6 CONCLUSION:
months of follow up by MRI and hormonal study and
Advancements in endoscopy and experience in
found improvement in pituitary function post
pituitary surgery drives endoscopic ENT surgeons
operatively in 4 patients, out of 10 patients whereas toward new horizons. The advantages of endoscopic
pituitary hormone deficiency was present in 14 out of approach are: less traumatic, faster, panoramic
52 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
magnified view, increased exposure, angled view with 5. Cook RS, Jones RA. Experience with the direct
the use of different endoscopes, absence of skin incisions- trans nasal trans sphenoidal approach to the
brain retraction - cranial nerve dissection and possibility pituitary fossa. Br J Neurosurg 1994;8(2):193-196.
to explore the sella for residual tumor at the end of
operation. Its disadvantages are the lack of 3D view 6. Haens J, Van Rompaey K, Stadnik T, Haentjens
and the need for an assistant to hold the endoscope10. P, Poppe K, Velkeniers B. Fully endoscopic trans
In our 20 yrs of experience, endoscopic trans sphenoidal sphenoidal surgery for functioning pituitary
4 handed technique is a safe and effective method for adenomas: a retrospective comparison with
complete pituitary tumor removal with better surgical traditional trans sphenoidal microsurgery in the
outcomes and fewer complications compared to the same institutiont.Surg Neurol. 2009 Oct;72(4):
trans septal trans sphenoidal technique.
336-40. doi: 10.1016/j.surneu. 2009.04.012. Epub
DISCLOSURES: 2009 Jul 14.
(a) Competing interests/Interests of Conflict- None 7. Rajesh Viswakarma, Neeraj Singh, Ratnadeep
(b) Sponsorships - None Ghosh. Endoscopic Hypophysectomy. Indian
(c) Funding - None Journal of Otolaryngology and Head and Neck
(d) No financial disclosures
Surgery 2006 April-June;58(2):162-164.
(e) Animal rights-Not applicable
8. De Divitiis E, Cappabianca P, Cavallo LM.
REFERENCES:
Endoscopic trans sphenoidal approach:
1. Cappabianca P, Alfieri A, De Divitiis E. Adaptability of the procedure to different sellar
Endoscopic endonasal Tran sphenoidal approach lesions. Neurosurgery.2002; 51(3): 699-707.
to the sella: towards functional endoscopic 9. Nishit J. Shah, Mukul Navnit,
pituitary surgery (FEPS). Minim Invasive Chandrashekhar E. Deopujari, Shraddha S.
Neurosurg 1998; 41: 66-73. Mukerji. Endoscopic Pituitary Surgery A
2. Kabil MS, Eby JB, Shahinian H. Fully endoscopic Beginners guide. Indian Journal of
endonasal vs. trans septal trans sphenoidal pituitary Otolaryngology and Head and Neck Surgery.
surgery. Minim Invasive Neurosurg. 2005 Dec;48 January- March 2004. 56 ( 1) 56(1):71-78.
(6):348-54. 10. Landolt AM (2001): History of Pituitary Surgery
3. Jho HD, Alfieri A. Endoscopic Endonasal from the technical aspect. Neurosurgery clinics
Pituitary Surgery: Evolution of surgical technique of North America.2001; Vol 12/Number 1: pp
and equipment in 150 operations. Minim Invas 37-44.
Neurosurg; 2001;44:1-12.
4. Shah S, Har-El. Diabetes Insipidus after pituitary
surgery: incidence after traditional versus
endoscopic trans sphenoidal approaches. Am J
Rhinol 2001;15 (6)377-379.
Vol.-11, Issue-I, January-June - 2017 53
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
CASE REPORT
A CASE REPORT OF PAPILLARY CARCINOMA IN
TOXIC MULTINODULAR GOITRE
*Gopalakrishnan Midhun P, **Sajikumar NR
HOW TO CITE THIS ARTICLE Date of receipt of article -20-11-2016
Gopalakrishnan Midhun P, Sajikumar N R. A Case Report Of Date of acceptance 09-01-2017
Papillary Carcinoma In Toxic Multinodular Goitre. Orissa J
Otolaryngology Head Neck Surgery. 2017 June; 11(1): 54-56. DOI- 10.21176/ojolhns.2017.11.1.9
DOI : 10.21176/ojolhns.2017.11.1.9
DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.9
ABSTRACT:
Introduction: The incidence of papillary carcinoma in toxic multinodular goitre (MNG) is very low. The
prevalence is 1-4%.
Objective: To describe and report a case of papillary carcinoma thyroid in toxic multinodular goitre
with literature review.
Case report: A 39 year old female presented with features of toxic multinodular goitre. After evaluation
and controlling toxicity total thyroidectomy was done. The histopathology report came out as papillary carcinoma
thyroid.
Conclusion: Though rare there is a definite incidence of papillary carcinoma in toxic multinodular goitre.
Total thyroidectomy after controlling toxicity is the treatment of choice.
Key words: Papillary carcinoma, toxicity, multinodular goitre.
INTRODUCTION: (Fig.-5), tachycardia, tremor of hands and moist
Multinodular goitre (MNG) is a common palms were present.
thyroid disease. Development of toxicity is a Thyroid function test showed elevated T3
complication of long standing goiters. Most commonly and T4 with low TSH value.
it affects female population. The incidence of papillary
Patient was started on titrated dose of
carcinoma in toxic multinodular goitre is very low.
carbimazole and propranolol. After attaining
The prevalence is 1-4% 1,2. Such nodules are not
euthyroid status, USG (Ultra Sonogram) Neck and
considered alarming because they are assumed to be
benign3. Most of the diagnosis in such cases will
Affiliations:
come as a surprise after histopathology report. *Senior Resident in Surgical Oncology,
CASE REPORT Malabar Cancer Centre, Thalassery,
Kannur (DT), Kerala 670103
A 39 year old female presented to outpatient E-mail: drmidhungopalakrishnan@gmail.com
department with a thyroid swelling of 5 year duration. **Additional professor,
Department of General Surgery,
There was associated history of increased appetite, Govt. TD Medical College, Alappuzha
loss of weight, prominent eyes, and palpitation for Address for correspondence:
last 6 months. On examination diffusely enlarged Dr. Midhun P Gopalakrishnan,
Senior Resident in Surgical Oncology,
thyroid swelling of size 8x4 cms., nodular surface,
Malabar Cancer Centre, Thalassery,
and firm in consistency was present. No palpable Kannur (DT), Kerala 670103
cervical lymph nodes were there. Bilateral proptosis Email: drmidhungopalakrishnan@gmail.com
Mob. No. 09447314520
54 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
FNAC (fine needle aspiration cytology) were done.
USG Neck showed a thyroid mass containing both
cystic and solid areas with multiple nodules in
both lobes, the largest measuring 2cms x 2 cms.
FNAC was consistent with colloid nodule. Total
thyroidectomy was done and histopathology report
came as nodular colloid goitre with two foci of
papillary carcinoma 1.5cms x 1 cms and 0.5cms x 0.5
cms (Fig 1, 2) along with toxic changes including Fig 5. Patient with bilateral proptosis
hyperplasia of acinii and vacuolated colloid with a
characteristic scalloped pattern (Fig 3). We stopped 131 scan to assess the completion of thyroidectomy
carbimazole immediately after surgery and continued and to detect metastasis if any. There was no
propranolol till 7 days post operatively and stopped. uptake of radio iodine in the neck suggestive of no
As one lesion was more than 1 cm we did Iodine residual thyroid tissue there. There was no metastasis
elsewhere also. Later we put her on suppressive
dose of thyroxine and she is on follow up now.
DISCUSSION:
Papillary thyroid carcinoma constitutes
approximately 80% to 85% of malignant epithelial
thyroid tumors. Grossly, papillary carcinomas have
a variable appearance, from subcapsular white scars
to large tumors more than 5 to 6 cm that invade
nearby structures outside the thyroid gland. Cystic
change, calcification, and even ossification may be
identified4. Microscopically, papillary carcinomas are
characterized by the presence of papillae, the
Fig-1: Nodular colloid goiter with two foci of characteristic nucleus containing Orphan-Annie nuclei,
papillary carcinoma.
nuclear grooves, and intranuclear pseudo inclusions
Fig 2. 1. Orphan Annie eyed nuclei (Fig 1, 2). It may also contain concentric lamellated
calcified structures called Psammoma bodies (Fig 4).
2. Overlapping of nuclei
Because the nuclei are enlarged, they frequently overlap
3. Nuclear ridges one another5. Papillary carcinoma has a propensity
4. Nuclear pseudo inclusion bodies to invade lymphatic spaces and therefore leads to
Fig 3. Toxic changes including hyperplasia of acini microscopic multimodal lesions in the gland as well
and vacuolated colloid with a characteristic scalloped as a high incidence of regional lymph node metastases.
pattern. But the incidence of papillary carcinoma in toxic
multinodular goiter is rare. Overall prevalence is 1-
4%. In thyroid toxicity the TSH will be very low.
Actually in post total thyroidectomy patients for
differentiated thyroid cancers we use thyroxine for
TSH suppression i.e. to attain low TSH level to
prevent recurrence in follow up period. But here
in this case though the TSH is low there were foci
of papillary thyroid carcinoma. In the presence of
toxicity cytological and radiological characteristics
Fig 4. Psammoma Bodies
rarely predict malignancy2.
Vol.-11, Issue-I, January-June - 2017 55
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
CONCLUSION: 4. Vincent T. DeVita , Theodore S. Lawrence, Steven
Total thyroidectomy in all cases of A. Rosenberg,et.al. (Eds.) Cancer: Principles and
thyrotoxicosis after controlling toxicity should be Practice of Oncology; (Eds) 10 th Edition,
the norm in view of malignancy though it is rare Lippincott & Williams and Willkins, 2015: 1179-
to rule out the same. The detection of thyrotoxicosis 1181.
does not exclude the possibility of thyroid carcinoma 5. L. Cheng, David G. Bostwich.(Eds), Essentials
and warrants careful evaluation and appropriate of Anatomic Pathology 4th ed. Springer science
therapy6. and business media, LLC. 2011: 985-986.
Meeting at which the paper was presented: 6. Ruqqeri RM etal. Folicular Variant of Papillary
India Singapore International Conference on Thyroid Carcinoma presenting as Toxic Nodule
Head & Neck cancer, ISCON 2015 held in RCC in an adolescent: Co-existent polymorphism of
Trivandrum in February 2015. the TSHR and GS alpha genes: Thyroid. 2013
Feb; 23(2): 239-242.
Acknowledgements: We acknowledge the
support of Dr. K K Sukumaran, then the HOD
and Professor of General Surgery, Govt. TD Medical
College, Alappuzha in presenting this case report.
DISCLOSURES:
(a) Competing interests/Interests of Conflict- None
(b) Sponsorships - None
(c) Funding - None
(d) Financial disclosures-none
(e) Animal rights -Not applicable
REFERENCES:
1. Sasan Mirfakhraee et al. A Solitary Hyper-
functioning Thyroid Nodule harbouring
Thyroid Carcinoma: : review of the literature
BMC; Thyroid Research. 2013 May, 6:7. avialble
at https://thyroidresearchjournal. biomedcentral.
com/articles/10.1186/1756-6614-6-7.
2. Polyzos etal. Coincidental Thyroid Papillary
Microcarcinoma in a patient treated for Toxic
Adenoma: Archives of Iranian Medicine. 2011
Mar; 14(2): 149-151.
3. Hala M. Ifayili etal. Papillary Thyroid
Carcinoma in a Autonomous Hyperfunctioning
Thyroid Nodule: Thyroid. 2010 Sep; 20(9):
1029-1032.
56 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
WOODEN FOREIGN BODY IN NASAL CAVITY:
AN UNUSUAL CASE REPORT
*Subrat K. Behera, **Girija S.Mohanta, ***Pitabas Nayak
HOW TO CITE THIS ARTICLE Date of receipt of article -22-02-.2017
Behera Subrat K, Mohanta Girija S, Nayak Pitabas. Wooden foreign Date of acceptance 30-02-.2017
body in nasal cavity: an unusual case report. Orissa J Otolaryngology
Head Neck Surgery 2017 June; 11(1): 57-59. DOI : 10.21176/
DOI- 10.21176/ojolhns.2017.11.1.10
ojolhns.2017.11.1.10 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.10
ABSTRACT:
Introduction: Nasal foreign bodies are more commonly encountered in pediatric age group. If an adult comes
with excoriation of nasal dorsum skin or non healing ulcer and have history of fall or road traffic accident, a
thorough clinical examination and diagnostic procedure is required to establish the diagnosis, skilled technique
may be required for removal.
Conclusion: Here we present a case of wooden object in the nose which is a rare of its kind in adult.
Keywords: Wooden foreign body, Nasal cavity.
INTRODUCTION: without any neurological deficit. There was small
Nasal foreign bodies are commonly encountered unhealing ulcer on dorsum of nose, just left lateral to
in emergency departments, particularly among children midline with excoriation of skin (Fig. 1) up to naso-
and mentally retarded patients.1 Nasal FB in adults are facial crease. There was no other wound or nasal
uncommon. Wooden foreign bodies within nasal cavity deformity externally. Local tenderness was present.
may remain asymptomatic for long duration and may Eyeball movements were normal with normal vision.
be missed in plain radiograph and CT scan. On cold spatula test fogging on both side were normal.
Patients are presented with unusual symptoms Anterior rhinoscopy showed a yellow-pinkish,
related to complication of FB. Successful diagnosis and firm foreign body on left nasal cavity. That was
treatment of nasal foreign bodies depend on careful insensitive to touch and did not bleed on probing.
nasal endoscopy and skilled technique of removal. We Posterior rhinoscopic examination was normal.
are presenting a case of a lady , who implanted a wooden Diagnostic nasal endoscopy was revealed, a yellowish
bamboo stick accidentally due to fall from a tree and firm wooden stick foreign body in left nasal cavity
presented to us after 1month of incident with unusual medial to middle turbinate, extending from roof to
complain of excoriation of nasal dorsum skin. the level of inferior turbinate (Fig. 2). The examination
of throat showed no abnormality. X ray of nose and
CASE REPORT:
paranasal sinuses was inconclusive. CT scan was done,
A 32 year old woman was presented to Outpatient which showed left maxillary mucosal thickening; but
department with chief complain of excoriation of nasal
dorsum skin since 15 days. She had history of fall from
a tree and a stick was pierced in to the dorsum which Affiliations:
* Prof and HOD, ** & *** Post Graduate,
was removed in local hospital 1month back. She had Deptt. Of ENT and Head and neck Surgery,
pain and bleeding from nose, which did subsided on S.C.B.Medical.College,Cuttack,Odisha.
medication. The symptoms were not associated with Address of Corresponding Author:-
nasal obstruction, decrease smell perception and nasal Dr. Girija Shankar Mohanta
discharge. There was no history of loss of consciousness, Post Graduate, Deptt. Of ENT and Head and neck Surgery,
S.C.B.Medical.College,Cuttack,Odisha.
vomiting and bleeding from ears. On examination the Contact-9937644983
patient was conscious, cooperative and well oriented Email- girija.mohanta@yahoo.com
Vol.-11, Issue-I, January-June - 2017 57
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
inconclusive.The detail hematological and routine Dry wood has air content 10, 11. On CT scan, in the
works up were done and were within normal limits.The early stage, it presents as low attenuation linear or
patient was planned for exploration of wound under cylindrical focus surrounded by hypo dense
general anesthesia. We removed a 3cm 1 cm of inflammatory soft tissue. In late stage due to mineral
wooden bamboo stick from left nasal cavity found deposition, it becomes hyper dense. Intra nasal wooden
attached to roof and hanging up to the level of inferior foreign body may be missed in early stage on CT because
turbinate through external approach.After removal of apparent air attenuation of FB and lack of contrast
whole nasal cavity was washed with normal saline, with the surrounding intranasal air12 (as in our case).
homeostasis was maintained and antibiotic soaked
The size and shape of the foreign bodies are
anterior nasal pack was given. The pack was removed
determining the method of removal and make difficulty
on 2nd post operative day and patient was discharged.
Patient was follow up on 7th post operative day and in removal. If foreign bodies are left inside may result
found to have normal nasal cavity and wound healed. in chronic sinusitis, FB granulation formation,
secondary infection, osteomyelitis and sinus
DISCUSSION: formation13.
Nasal foreign bodies are most common between
Transnasal endoscopic technique 9,13, 14 offers
age 2-4 group2. They are more common in children
excellent visualization and easy removal of FB. Other
then adults because children are more likely to put
external approaches like lateral rhinotomy may be
anything in to their nose or in to other childrens nose3.
Foreign bodies in adults are mainly seen in psychiatric required in complicated and selected cases like in our
disorder patients, self inflicted harm as seen in suicidal case we removed through external approach.
attempts person5,1,4 or prisoners who sometime attempts Complication during the removal may cause
to temporarily escape justice6. In normal adult, foreign epistaxis, injury to neighboring structure, aspiration,
bodies may be implanted in to nose and Para nasal sinuses orbital hematoma, rhinosinusitis etc.
accidentally like road traffic accident, fall from height If the CT is negative but a wooden foreign body
or drowning. These cases are often associated with is suspected, MRI may be performed. MRI shows the
maxillo-facial injury.Foreign bodies are either animates retained wooden foreign body to be hypo intense to
or inanimates1. Inanimates nasal foreign bodies are skeletal muscle on bothT1 and T2 weighted sequence.
classified as organic and inorganic. The plastics and metal However CT should be performed initially in a patient
s are common as inorganic foreign bodies7. Organic suspected a harboring a FB, Since metallic FB may be
foreign bodies are seeds, food, wood etc. present and result in a severe or fatal injury if the metal
Nasal foreign bodies are generally painless. Any reacts to the magnet of the MRI3.
patient who presents with a unilateral nasal discharge CONCLUSION:
should raise suspicion of a nasal foreign body and in
children this must be regard as the case until proved Foreign body in nose with unusual presentation
otherwise1. Accidentally implanted nasal foreign bodies need nasal endoscopy for diagnosis. Complicated cases
without much external and maxilla-facial injury are may require latral rhinotomy for removal for the same.
difficult to diagnosis. Entry wound are contaminated
and presence of foreign body pieces makes the wound
unhealing. Irritation of wound and surround skin due
to presence of FB may lead to excoriation of skin (as in
our case).
The physical examination of nose involving
anterior rhinoscopy and use of 0 degree rigid endoscope
will often reveal foreign body. However on occasions
mucosal edema or granulation tends to hide it,
vasoconstrictors should be used to decongest the mucosa
prior to examination8.
Although standard plain radiographs clearly show
the presence of FB, for their precise and accurate
localization within the sinuses, orbits& soft tissues CT Fig.1: Small unhealing ulcer on dorsum of nose, just left lateral
scan may be required in high density foreign body9. to midline with excoriation of skin.
58 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
REFERENCES:
1. Kalan A and Tariq M; Foreign bodies in the nasal
cavities; a comprehensive review of the aetiology,
diagnostic pointers and therapeutic measures
Postgrad Med J. 2000 Aug; 76(898): 484-
487.doi: 10.1136/pmj.76.898.484.
2. Kadish HA, corneli HM.Removal of nasal FB in
pediatric population.American journal of
emergency medicine. 1997;15 :54-6.
3. Kenji Takasaki, Kaori Enatsu, Eigo So, Haruo
Fig. 2: A yellowish firm wooden stick foreign body in left Takahashi. Fifty-Four Wooden Toothpicks in the
nasal cavity medial to middle turbinate, extending from roof Nasal Cavity. Otolaryngol Head Neck Surg. 2005;
to the level of inferior turbinate. 132:669-70. doi:10.1016/j.otohns. 2004.09.073.
4. Werman HA. Removal of foreign bodies of the
nose. Emerg MedClin NorthAm1987;5 ;253-263.
5. Loh FC and Ling SY; Analysis of the metallic
composition of orofacial talismans. Oral Surg Oral
Med Oral Pathol 1992;73:281-283.
6. Krupp LB, Gelberg EA, Wormser GP. Prisoners
as medical patients. Am J Public Health
1987;77:859-60.
7. Figueiredo RR, Azevedo AA, K6s AOA, Tomita
S. Corpos estranhos de fossas nasais: descricao de
tipos e complicacoes em 420 casos. Rev Bras
Otorrinolaringol. 2006;72:18-23.
Fig.3: Pre operative photograph.
8. Walby AP. Foreign bodies in the ear or nose. In:
Kerr AG, ed. Scott-Browns otolaryngology. 6th
Ed. Oxford: Butterworth-Heinemann, 1997: 6/
14/16/14/6.
9. Lin WS, Hung HY. Transnasal endoscopic
surgery of sphenoid sinus aspergillosis. J Laryngol
Otol 1993;107:837-9.
10. Jeffrey J. Peterson,Laura W. Bancroft,Mark J.
Kransdorf ;Wooden Foreign Bodies:Imaging
Appearance. AJR 2002;178:557562.
11. Van Thong Ho, James F. McGuckin, Jr, and
Eleanor M. Smergel. Intraorbital Wooden
Fig.4: Post operative photograph. Foreign Body: CT and MR Appearance, AJNR
17:134136. Jan 1996 0195-6108/96/1701013.
DISCLOSURES: 12. Shailesh M Prabhu, Aparna Irodi, Phiji Philip
1. Funding: There is no source of funding for this George , Ranjan sundaresan & VK Anand; Indian
study. J radiol Imaging. 2014 jan. mar ; 24 (1):72-74 doi-
2. Conflict of interest: The authors declare that they 10.4103/0971-3026.130703 PMCID:pmc4028920.
have no conflict of interest. 13. Mohiuddin SA, Rahiman S, Sultana S. Multiple
3. Informed consent: Informed consent was taken glass pieces in paranasal sinuses. Indian J Dent Res.
from every patient. 2011;22:847-9. doi: 10.4103/0970-9290.94683.
4. Ethical approval: All procedures performed in 14. Kitamura A, zeredo JL. Migrated maxillary
studies involving human participants were in implant removed via semilunar hiatus by transnasal
accordance with the ethical standard of institution. endoscope. Implant Dent. 2010;19.
Vol.-11, Issue-I, January-June - 2017 59
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
TORNWALDTS CYST- A HIDDEN ENTITY- A CASE REPORT
*Sanket D Vakharia, **Seema R Gupta, ***Maya Shankar B Vishwakarma, ****S A Jaiswal
HOW TO CITE THIS ARTICLE Date of receipt of article- 08-02-2017
Vakharia S D, Gupta S.R. .Vishwakarma Mb,. Jaiswal Date of acceptance 24-02-2017
S.A.Tornwaldts cyst- a hidden entity- a case report. .orissa j
otolaryngology head neck surgery 2017 june; 11(1):60-62. DOI: DOI- 10.21176/ojolhns.2017.11.1.11
10.21176/ojolhns.2017.11.1.11 DOI URL- https://doi.org/10.21176/ojolhns.2017.11.1.11
ABSTRACT:
Introduction: Tornwaldts cyst is a benign developmental lesion originating within the midline of nasopharynx.
Etiopathogenesis of this cyst is outpouching of the pharyngeal mucosa caused by retraction of notochord. Most
of the cases are asymptomatic and are discovered as an incidental finding in patients undergoing diagnostic nasal
endoscopy or radiological examination. However, recently the cases are on an upsurge which could be attributed
to increased use of nasal endoscopy.
Case Report: Reported here is a case of 27-year-old man who complained of nasal obstruction and repeated nasal
discharge for which diagnostic nasal endoscopy was performed which revealed a deviated nasal septum and a
nasopharyngeal cystic lesion . Instead of CT Paranasal sinus, we opted MRI for further analysis of a
nasopharyngeal cystic lesion following which endoscopic surgery was performed.
Conclusion: This paper emphasises on the importance of radiological and endoscopic examination in the diagnosis
of the Tornwaldts cyst.
Keywords: Nasopharyngeal cyst, Tornwaldts cyst.
INTRODUCTION: Less common symptoms at initial presentation include
This entity is labelled in the memory of Dr. stiff cervical muscles and ear fullness or Eustachian tube
Gustoff L. Tornwaldt (19th century), who first dysfunction. On physical examination, nasal endoscopy
described it. So, the accurate designation for this disease is required to diagnose this cyst which appears as a
is Tornwaldts Cyst and not Thornwaldts 1 . smooth submucosal mass in the nasopharynx. It is
Tornwaldts cyst is a benign developmental lesion superior to the adenoid pad and may have a central
within the nasopharyngeal midline, above the upper dimpling and/or yellow hue if infected or filled with
border of the superior constrictor muscle. It represents fluid from recent irritation. While history and
the embryonic communication between mesenchymal endoscopy can lead to the diagnosis, radiology is
notochord remnant and endodermal-derived recommended to rule out other possibilities in the
nasopharyngeal mucosa 2. It is developmental in nature, differential diagnosis.
usually asymptomatic and found incidentally. So, the
Affiliations:
age of diagnosis represents age of imaging of the *Junior Resident, **Junior Resident, ***Assistant Professor,****
nasopharynx. It has an autopsy prevalence of Professor & HOD
Dept.Of E.N.T.,DR.V.M.G.M.C., SOLAPUR
approximately 4%.3. Most Tornwaldts cysts appear
Address of Correspondence:
clinically in the second and third decades of life, with Dr. Seema R Gupta
both genders affected equally. Tornwaldts cyst Room No.-21, Resident Doctors Hostel
Civil Hospital Chowk, Solapur, Maharastra - 413003
typically presents as occipital headaches, persistent nasal Email: mailmeseema.gupta@gmail.com
discharge (more often post-nasal drainage), and halitosis. Mob.: 9689470189
60 Vol.-11, Issue-I, January-June - 2017
Issue DOI URL- https://doi.org/10.21176/ojolhns.0974-5262.2017.11.1
CASE REPORT: some authors argue that Nasopharyngeal cysts should
A 27 year old male patient reported to the OPD be classified according to their relation to the
with chief complaint of nasal obstruction and nasal pharyngobasilar fascia, which is the aponeurosis
discharge since 6 months. Repeated episodes of upper attachment of the superior constrictor muscle to the
respiratory tract infection, snoring and nasal twang skull base 4. This fascia is only penetrated by the
were accompanying complaints. Past medical and eustachian tubes and the levator veli palatine muscles
family history were not significant. History of multiple and is a tight barrier between the superficial and deep
courses of antibiotics and anti-inflammatory drugs structures of the nasopharynx. Nasopharyngeal cysts
from physician with partial relief of symptoms was can also be classified according to their radiological
present. On anterior rhinoscopy deviated nasal septum appearance, in context to their symptomatology.
to right, nasal mucosal congestion with discharge were Tornwaldts bursa, also known as nasopharyngeal
evident with no mass in the nasal cavity. On Diagnostic bursa, is a recess in the midline of the nasopharynx,
Nasal Endoscopy a single midline well circumscribed which is produced by persistent notochord remnants.
smooth surfaced cystic mass arising from posterior wall In 1912, Huber, in a description of the embryologic
of nasopharynx was seen (fig.1). The mass was covered formation of Tornwaldts bursa, reported that a
with normal looking mucosa. Oral, Ear and Neck potential space could develop in the nasopharynx at
examination did not reveal any significant findings. the point where the notochord retained its union with
MRI of neck (Plain) revealed well defined round to the pharyngeal endoderm. His report was the first to
oval T1 & T2 hyperintense lesion of about 1.6 X 1.3 discuss this pathway for the ingrowth of respiratory
cm in the midline arising from posterior wall of epithelium and the formation of a potential space in
nasopharynx with no evidence of any invasion and intra- the midline of the posterior superior angle of the
cranial extension s/o cystic lesion- Tornwaldts nasopharynx (nasopharyngeal bursa) 5. The cyst is lined
cyst(fig.2). Under general anaesthesia,the cystic lesion by respiratory epithelium and the cystic lumen contains
was marsupialised via endonasal and transoral retrovelar fluid with variable proteins. Tornwaldts cysts may also
approach after endoscopic septoplasty. Patients post- be acquired, following nasopharyngitis, surgical trauma
op period was uneventful with relief of all complaints (adenoidectomy) and chemoradiation for
and the raw surface epithelialized within 14 days. nasopharyngeal carcinoma in adults. Tornwaldts cysts
DISCUSSION: can be classified as crusting cysts and true cystic cysts.6,7
The nasopharynx is a cuboidal compartment The crusting types drain regularly and spontaneously
extending from the base of the skull to the soft palate. into the nasopharynx while the cystic types do not drain
Due to the unique development of the nasopharynx, because the drainage pathway is completely obstructed.
Fig-1: Nasal endoscopic view of Tornwaldts cyst. Fig-2: MRI of skull & skull base in sagital section
showing Tornwaldts cyst.
Vol.-11, Issue-I, January-June - 2017 61
Issue DOI- 10.21176/ojolhns.0974-5262.2017.11.1.
Most cysts are small, measuring less than 1 cm in in the diagnosis and to know the exact extent of the
diameter and are discovered incidentally. Some are disease.
larger, causing nasal obstruction, snoring, halitosis, Acknowledgments- to Dr.PRIYA A. BHAGDE,
clearing of the throat, eustachian tube dysfunction, and Resident of oral pathology, GOVT. DENTAL
a feeling of ear fullness. When the cysts become inflamed COLLEGE, AURANGABAD.
or infected, fluid may accumulate within the cyst
DISCLOSURES:
leading to symptoms of occipital headache, pharyngeal
pain, and purulent postnasal drip with a foul taste, neck (a) Competing interests/Interests of Conflict- None
stiffness and changes in olfaction. The diagnosis of (b) Sponsorships - None
Tornwaldts disease begins with a history of symptoms, (c) Funding - None
followed by confirmation by nasopharyngoscopy and (d) No financial disclosures
other imaging studies. The findings are that of a usually (e) Animal rights-Not applicable
centrally located smooth mass covered with intact REFERENCES:
mucosa having yellowish hue due to the cystic contents. 1. L. Tornwaldt, Zur frage der bursa pharyngea,
The differential diagnosis should include meningocele Deut. Med. Wochenschr 1887; 48 : 10421046.
or meningo-encephalocele. Occasionally, the lesion can 2. H. Miyahara, T. Matsunaga, Tornwaldts disease,
be dark colored due to a hemorrhage or hemosiderin Acta Otolaryngol. 1994;517 : 2936.
content. Computed tomogram (CT) scan shows a well- 3. Illum P. Endoscopic examination of the
defined midline low density cyst on posterior nasopharynx. Acta Otolaryngol 1979;88:273-8.
nasopharyngeal wall. On contrast enhanced CT scan a 4. P. Guggenheim, Cysts of the nasopharynx.
rim of cyst may enhance but tornwaldts cyst itself Laryngoscope .1967;75: 21472168.
remains of low attenuation. MRI is now considered 5. Kwok P, Hawke M, Jahn AF, et al. Thornwaldts
the best radiographic imaging study to diagnose the cyst: clinical and radiological aspects. J Otolaryngol
tornwaldts cyst as the findings are highly characteristic. 1987;16:1047.
On MRI, it may have high signal on both T1- and T2- 6. Ikushima, Y. Korogi, O. Makita, Y. Komohara,
weighted sequences, presumably because the cyst H. Kawano, M. Yamura, K. Arikawa, M.
contains a high concentration of protein, or blood Takahashi, MR imaging of Tornwaldts cysts.AJR
products from prior hemorrhage, or both. Post contrast Am J Roentgenol. 1999 Jun;172(6):1663-5.
studies usually demonstrate peripheral enhancement of 7. S.L. Chang, T.C. Wu, C.Y. Yiu, Tornwaldts cyst
the nasopharyngeal mucosa 8 . Also, it may be formation after concurrent chemoradiotherapy
hyperintense relative to gray matter on fluid-attenuated for nasopharyngeal carcinoma, J. Laryngol. Otol.
inversion recovery images. 2006;120 :959960.
8. Eloy P, Watelet JB, Hatert AS, Bertrand B.
Asymptomatic cysts, which may be an incidental
Thornwaldts cyst and surgery with powered
finding on a CT or MRI, require no treatment9. When
instrumentation. B-ENT. 2006; 2:135-39.
the lesion is large, symptomatic, or close to the
9. Yanagisawa E, Yanagisawa K. Endoscopic view of
eustachian tube torus, surgery by marsupialisation is
Thornwaldt cyst of the nasopharynx. Ear Nose
the treatment option10. For small lesions, the endonasal
Throat J. 1994; 73:884-85.
approach is recommended but for large lesions, a
10. Weissman JL. Thornwaldt cysts. Am J
transoral retrovelar approach using a 70 degree
Otolaryngol. 1992; 13:381-85.
telescope is the method of choice.
11. Tornwaldt,Gustavus Ludwig. Zur frage der bursa
CONCLUSION: pharyngea, Deut. Med. Wochenschr (About the
The diagnosis of a nasopharyngeal cyst is usually importance of Bursa pharyngeal for the detection
incidental unless it is large causing obstructive and treatment of certain diseases of nasopharynx)
symptoms. Diagnostic Nasal endoscopy is a simple and 48 (1887) 10421046.avialable at https://
rapid procedure to visualize such cyst. Depending on archive.org/stream/b22370493
its appearance, surgical intervention may involve either b22370493_djvu.txt.
a simple excision or a marsupialisation of a cyst either 12. H. Miyahara, T. Matsunaga, Tornwaldts disease,
endoscopic or transoral approach. CT/MRI scan helps Acta Otolaryngol. 1994;114(517): 36-39.
62 Vol.-11, Issue-I, January-June - 2017
Potrebbero piacerti anche
- PBCC PDFDocumento1 paginaPBCC PDFMaureen Dela ResmaNessuna valutazione finora
- General and Oral Pathology For Dental Hygiene PracticeDocumento361 pagineGeneral and Oral Pathology For Dental Hygiene Practicepsychposters100% (1)
- Test Bank For Pharmacology Clear and Simple A Guide To Drug Classifications and Dosage Calculations 3rd Edition WatkinsDocumento6 pagineTest Bank For Pharmacology Clear and Simple A Guide To Drug Classifications and Dosage Calculations 3rd Edition WatkinsJean Taylor100% (39)
- 684OSCDirectory-20.05.2020Documento120 pagine684OSCDirectory-20.05.2020Nazim KhanNessuna valutazione finora
- List of Doctors in PhilippinesDocumento2 pagineList of Doctors in PhilippinesMarc Jaylord GuillermoNessuna valutazione finora
- Scribd UplDocumento73 pagineScribd Uplhisham_476Nessuna valutazione finora
- Gynae OncologyDocumento52 pagineGynae OncologyrkNessuna valutazione finora
- Venous Association of IndiaDocumento35 pagineVenous Association of IndiaKriti KumariNessuna valutazione finora
- Masterlist South GMA - GastroDocumento1.125 pagineMasterlist South GMA - GastroNeil SulitNessuna valutazione finora
- NewlisthiniDocumento6 pagineNewlisthinishiva lakshmiNessuna valutazione finora
- Counter Affidavit: Office of The Provincial ProsecutorDocumento2 pagineCounter Affidavit: Office of The Provincial ProsecutorSleepy AssNessuna valutazione finora
- Doctors List 3Documento8 pagineDoctors List 3Aadil PirvaniNessuna valutazione finora
- Sno Provcode Hospname Address City State Pin Code Tele1Documento5 pagineSno Provcode Hospname Address City State Pin Code Tele1Kriti KumariNessuna valutazione finora
- Daftar RSD 2017Documento569 pagineDaftar RSD 2017Hesti HovNessuna valutazione finora
- List of SpecialistsDocumento2 pagineList of SpecialistsiwennieNessuna valutazione finora
- Data RS 2016-Regional 1Documento120 pagineData RS 2016-Regional 1H1H010034Nessuna valutazione finora
- Allied Doctor Bahrain DataDocumento12 pagineAllied Doctor Bahrain DataShibu KavullathilNessuna valutazione finora
- Out Patient Abu Dhabi 2015Documento24 pagineOut Patient Abu Dhabi 2015Desai NileshNessuna valutazione finora
- Competency Standards MOH SingaporeDocumento62 pagineCompetency Standards MOH SingaporepaanarNessuna valutazione finora
- Guwahati Team Revised DR ListDocumento442 pagineGuwahati Team Revised DR ListLoveSahilSharmaNessuna valutazione finora
- Empanelled Service Provider in Minilap - Bulk Data 6Documento19 pagineEmpanelled Service Provider in Minilap - Bulk Data 6Vijay KumarNessuna valutazione finora
- AMA List 2018Documento8 pagineAMA List 2018Shweta jainNessuna valutazione finora
- Healthcare Quality Management Regulatory Compliance Coordinator in Denver CO Resume Mary FrisciaDocumento4 pagineHealthcare Quality Management Regulatory Compliance Coordinator in Denver CO Resume Mary FrisciaMaryFrisciaNessuna valutazione finora
- Doctors DataDocumento3 pagineDoctors DataChhavi AuplishNessuna valutazione finora
- Chennai Number PDFDocumento3 pagineChennai Number PDFkirthika0% (1)
- Ophthalmology Academics Extension and Research PDFDocumento5 pagineOphthalmology Academics Extension and Research PDFShweta jainNessuna valutazione finora
- Radiologist in CoimbatoreDocumento6 pagineRadiologist in CoimbatoreshahulNessuna valutazione finora
- Medi Claim Hospital ListDocumento884 pagineMedi Claim Hospital Listgaurav chauhan0% (1)
- NIAC Hospital Network List PPN and NON PPNDocumento3.464 pagineNIAC Hospital Network List PPN and NON PPNluckynaveenrajNessuna valutazione finora
- 4 5947406296134190606Documento84 pagine4 5947406296134190606ibrahim sengaji100% (1)
- Clinic ListDocumento8 pagineClinic ListWin Aung PyaeNessuna valutazione finora
- List of Doctors 2010 2Documento15 pagineList of Doctors 2010 2slobsNessuna valutazione finora
- Kaiser International List of Accredited Hospitals As of May 2017Documento14 pagineKaiser International List of Accredited Hospitals As of May 2017あいうえおかきくけこ100% (1)
- 2019 May List of Physicians and HospitalsDocumento7 pagine2019 May List of Physicians and HospitalsMuhammad Imteaz AliNessuna valutazione finora
- Consolidated List of Empaneled Hospitals As On 14.12.2020Documento31 pagineConsolidated List of Empaneled Hospitals As On 14.12.2020Ankit SharmaNessuna valutazione finora
- Hospital ListDocumento12 pagineHospital ListK T GohilNessuna valutazione finora
- List of Tie-Up Hospitals To Provide Superspeciality Treatment To Esi BeneficiariesDocumento15 pagineList of Tie-Up Hospitals To Provide Superspeciality Treatment To Esi Beneficiariesecure HealthcareNessuna valutazione finora
- MNGB-31 10 2017Documento114 pagineMNGB-31 10 2017akashrajpalNessuna valutazione finora
- 2009 Northern New York Medical DirectoryDocumento56 pagine2009 Northern New York Medical Directorywdt_rpominville100% (4)
- Bihar: S. No Registration No. Name Institute Phone No. Email Permanent AddressDocumento6 pagineBihar: S. No Registration No. Name Institute Phone No. Email Permanent AddressPratik kr agarwalNessuna valutazione finora
- Accredited Providers As of SEPT RT - 0Documento2 pagineAccredited Providers As of SEPT RT - 0PRC Board100% (2)
- List of SpecialistsDocumento6 pagineList of SpecialistsSamana SyedNessuna valutazione finora
- List-of-Approved-Hospitals-in-India 333Documento119 pagineList-of-Approved-Hospitals-in-India 333raguhvacind4620Nessuna valutazione finora
- The Moldovan Medical Journal Vol 61 MaiDocumento111 pagineThe Moldovan Medical Journal Vol 61 MaiBooker DewittNessuna valutazione finora
- ICRO MEMBER LIST - NEW 2019-20 (Final)Documento12 pagineICRO MEMBER LIST - NEW 2019-20 (Final)Divyansh ChaudharyNessuna valutazione finora
- NMVBDocumento22 pagineNMVBPriya SelvarajNessuna valutazione finora
- Igims Directory PDFDocumento28 pagineIgims Directory PDFBambam KumarNessuna valutazione finora
- Doctors List Aug 06Documento19 pagineDoctors List Aug 06Annu259Nessuna valutazione finora
- Kolkata HospitalsDocumento4 pagineKolkata HospitalsRanabir DebNessuna valutazione finora
- Neet PG 2017 Merit ListDocumento8 pagineNeet PG 2017 Merit ListRrb Jobs Alert0% (1)
- Compendium - ECHSDocumento325 pagineCompendium - ECHSRamesh H T75% (4)
- DM All BOS MembersDocumento13 pagineDM All BOS MemberspupuraniNessuna valutazione finora
- Central Bicol Masterlist Sort AddressDocumento6 pagineCentral Bicol Masterlist Sort Addresskentclark03Nessuna valutazione finora
- Doctors 1Documento202 pagineDoctors 1abhiNessuna valutazione finora
- Listing of SQACQ32019-20Documento18 pagineListing of SQACQ32019-20Space HRNessuna valutazione finora
- N1705749 PDFDocumento49 pagineN1705749 PDFAravind RaviNessuna valutazione finora
- ARMM List of L1 and L2 HospitalsDocumento1 paginaARMM List of L1 and L2 HospitalsMarc Eric RedondoNessuna valutazione finora
- A List of All Doctors of The Government of BiharDocumento32 pagineA List of All Doctors of The Government of BihargauravNessuna valutazione finora
- Nabl 600Documento420 pagineNabl 600AartiNessuna valutazione finora
- Proforma For Students Credit Card Medical CollegeDocumento8 pagineProforma For Students Credit Card Medical CollegeKriti SinhaNessuna valutazione finora
- Private Empanelled Hospital Railway BoardDocumento194 paginePrivate Empanelled Hospital Railway BoardVijaya Ingle100% (2)
- Tie Up KeralaDocumento6 pagineTie Up Keralaakgn92Nessuna valutazione finora
- Admission Year, 2019-20 Post Graduate StudentsDocumento6 pagineAdmission Year, 2019-20 Post Graduate StudentsShiwali SinghNessuna valutazione finora
- Ojolhns 10 Issue II Dec 2016 ColorDocumento66 pagineOjolhns 10 Issue II Dec 2016 ColorAnonymous ST1Ot2GAHxNessuna valutazione finora
- Fellow 2014Documento4 pagineFellow 2014upsc.bengalNessuna valutazione finora
- Mem 2010Documento8 pagineMem 2010Shweta jainNessuna valutazione finora
- List of Fellows (Name-Wise) Upto 2016Documento165 pagineList of Fellows (Name-Wise) Upto 2016Rakesh VermaNessuna valutazione finora
- A Rare Case Report - Intact Eye Ball in MaxillaryDocumento4 pagineA Rare Case Report - Intact Eye Ball in MaxillaryDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Invited Editorial PDFDocumento5 pagineOJOLNS-10 - II - Invited Editorial PDFDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Study of Crushing PDFDocumento5 pagineOJOLNS-10 - II - Study of Crushing PDFDR K C MALLIKNessuna valutazione finora
- Ojolhns-10 Issue-IIDocumento66 pagineOjolhns-10 Issue-IIDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Endoscopic Trans PDFDocumento6 pagineOJOLNS-10 - II - Endoscopic Trans PDFDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Comparative Outcome PDFDocumento6 pagineOJOLNS-10 - II - Comparative Outcome PDFDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Role of Bilateral PDFDocumento4 pagineOJOLNS-10 - II - Role of Bilateral PDFDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Effects of GLOSSOPHARYNGEAL PDFDocumento5 pagineOJOLNS-10 - II - Effects of GLOSSOPHARYNGEAL PDFDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Invited Editorial PDFDocumento5 pagineOJOLNS-10 - II - Invited Editorial PDFDR K C MALLIKNessuna valutazione finora
- 13.diagnostic Dilemmas Leading To Fatality inDocumento6 pagine13.diagnostic Dilemmas Leading To Fatality inDR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Endoscopic Trans PDFDocumento6 pagineOJOLNS-10 - II - Endoscopic Trans PDFDR K C MALLIKNessuna valutazione finora
- Ojolhns Vol II Issue II 2008Documento53 pagineOjolhns Vol II Issue II 2008DR K C MALLIKNessuna valutazione finora
- OJOLNS-10 - II - Comparative Outcome PDFDocumento6 pagineOJOLNS-10 - II - Comparative Outcome PDFDR K C MALLIKNessuna valutazione finora
- 11.second Branchial Sinus Presenting PDFDocumento5 pagine11.second Branchial Sinus Presenting PDFDR K C MALLIKNessuna valutazione finora
- 8-Ojolns-9 Issue-1 F (With Dio No)Documento61 pagine8-Ojolns-9 Issue-1 F (With Dio No)DR K C MALLIKNessuna valutazione finora
- 12.bilateral Antrochoanal Polyp inDocumento4 pagine12.bilateral Antrochoanal Polyp inDR K C MALLIK0% (1)
- 9.nasal Glioma in 18 Month ChildDocumento5 pagine9.nasal Glioma in 18 Month ChildDR K C MALLIKNessuna valutazione finora
- 8.solitary Parotid Mass Presenting As Sarcoidosis Unusual PresentationDocumento5 pagine8.solitary Parotid Mass Presenting As Sarcoidosis Unusual PresentationDR K C MALLIKNessuna valutazione finora
- 4.anterior Nasal Packing and Eustachian Tube DysfunctionDocumento5 pagine4.anterior Nasal Packing and Eustachian Tube DysfunctionDR K C MALLIKNessuna valutazione finora
- 10.congenital Choanal AtresiaDocumento5 pagine10.congenital Choanal AtresiaDR K C MALLIKNessuna valutazione finora
- Insular Carcinoma of Thyroid - Unusual VariantDocumento5 pagineInsular Carcinoma of Thyroid - Unusual VariantDR K C MALLIKNessuna valutazione finora
- 6.paediatric BronchosDocumento7 pagine6.paediatric BronchosDR K C MALLIKNessuna valutazione finora
- Insular Carcinoma of Thyroid - Unusual VariantDocumento5 pagineInsular Carcinoma of Thyroid - Unusual VariantDR K C MALLIKNessuna valutazione finora
- Tissue Myringoplasty PDFDocumento6 pagineTissue Myringoplasty PDFDR K C MALLIKNessuna valutazione finora
- 1-Roleof Ultrasonography in Thyroid SwellingsDocumento6 pagine1-Roleof Ultrasonography in Thyroid SwellingsDR K C MALLIKNessuna valutazione finora
- Editorial... Vol.-9 Issue-I Jan-June - 2015Documento1 paginaEditorial... Vol.-9 Issue-I Jan-June - 2015DR K C MALLIKNessuna valutazione finora
- 2.importance of Pre-Operative HRCT Temporal Bone PDFDocumento5 pagine2.importance of Pre-Operative HRCT Temporal Bone PDFDR K C MALLIKNessuna valutazione finora
- 2.importance of Pre-Operative HRCT Temporal Bone PDFDocumento5 pagine2.importance of Pre-Operative HRCT Temporal Bone PDFDR K C MALLIKNessuna valutazione finora
- Editorial A Tailor Made Approach To Endoscopic Sinus Surgery ForDocumento3 pagineEditorial A Tailor Made Approach To Endoscopic Sinus Surgery ForDR K C MALLIKNessuna valutazione finora
- Database Design Project-Proposal-HIM 650 - Sujata MathewDocumento5 pagineDatabase Design Project-Proposal-HIM 650 - Sujata Mathewjoe wycliffeNessuna valutazione finora
- Ijogr 6 4 444 447Documento4 pagineIjogr 6 4 444 447RachnaNessuna valutazione finora
- Diagnosis, Treatment and Care For People With DementiaDocumento20 pagineDiagnosis, Treatment and Care For People With DementiaAnaStankovićNessuna valutazione finora
- ITI Decision Trees and ChecklistsDocumento6 pagineITI Decision Trees and ChecklistsNay AungNessuna valutazione finora
- "Drug Addiction" The ProblemDocumento2 pagine"Drug Addiction" The ProblemCJ ToraNessuna valutazione finora
- Wadia 2019 The Updated Periodontal ClassificationDocumento4 pagineWadia 2019 The Updated Periodontal ClassificationPatricia CastellanosNessuna valutazione finora
- AP Medical Council Application For No Objection CertificateDocumento1 paginaAP Medical Council Application For No Objection CertificateSANTHILAL ADHIKARLANessuna valutazione finora
- NP1 46 50Documento8 pagineNP1 46 50tristan lloydNessuna valutazione finora
- CLI - Material UFCD 6660 (Food Worries)Documento2 pagineCLI - Material UFCD 6660 (Food Worries)Aurora NarcisoNessuna valutazione finora
- UNIT - II - SUBCENTRE - AnandDocumento34 pagineUNIT - II - SUBCENTRE - AnandAnand gowdaNessuna valutazione finora
- Shehryar Baig Resume 2Documento2 pagineShehryar Baig Resume 2api-491306844Nessuna valutazione finora
- NURS FPX 6214 Assessment 1 Technology Needs AssessmentDocumento6 pagineNURS FPX 6214 Assessment 1 Technology Needs Assessmentfarwaamjad771Nessuna valutazione finora
- Brief Psychological Interventions PDFDocumento6 pagineBrief Psychological Interventions PDFhema angleNessuna valutazione finora
- ASTMH Exam Brochure 18 FNLDocumento17 pagineASTMH Exam Brochure 18 FNLNgô Khánh HuyềnNessuna valutazione finora
- Modern Healthcare - April 13, 2020 PDFDocumento38 pagineModern Healthcare - April 13, 2020 PDFChristian Del BarcoNessuna valutazione finora
- OEC Chapter 4Documento10 pagineOEC Chapter 4Phil McLeanNessuna valutazione finora
- Galaxy SurgeryDocumento2 pagineGalaxy SurgerydesbestNessuna valutazione finora
- EU LCPPV Local Contact Person Requirements 22 July 2022 TepsivoDocumento59 pagineEU LCPPV Local Contact Person Requirements 22 July 2022 TepsivoAnda AndreianuNessuna valutazione finora
- Public Health Surveillance & ScreeningDocumento58 paginePublic Health Surveillance & ScreeningKonjit MitikuNessuna valutazione finora
- Apacible NCM119-LP1 LeadershipDocumento15 pagineApacible NCM119-LP1 LeadershipUlah Vanessa BasaNessuna valutazione finora
- Comprendio, Sean Michael S (1) - BSN 1-F SDLModule2Documento5 pagineComprendio, Sean Michael S (1) - BSN 1-F SDLModule2Sean Michael ComprendioNessuna valutazione finora
- Arulmigu Kalasalingam College of Pharmacy,: Krishnankoil-626126. Online Activity Report - 2020Documento13 pagineArulmigu Kalasalingam College of Pharmacy,: Krishnankoil-626126. Online Activity Report - 2020S Regurathi PandianNessuna valutazione finora
- RPK Kesorga 2018Documento91 pagineRPK Kesorga 2018Indonesia RayaNessuna valutazione finora